Skin rash from zoloft
12 Zoloft Side Effects - SSRI Uses & Common Interactions To Know
Remember the original Zoloft commercial? The one where a sad little blob rolled around on screen with a rain cloud hovering over its head?
That commercial first debuted back in 2001, and since then Zoloft, or Sertraline hydrochloride, has become one of the top psychiatric drugs used by American adults, according to one recent study.
“Zoloft is one of the first-line antidepressant medications prescribed for both depression and anxiety, meaning it’s one of the most likely to work,” says Alison Hermann, MD, a clinical psychiatrist at Weill Cornell Medicine and New York-Presbyterian Hospital.
Zoloft is part of a class of drugs called SSRIs, or selective-serotonin reuptake inhibitors. “Their main effect has to do with changing the signaling of one of the main neurotransmitters in the brain, serotonin, which modulates mood,” explains James Murrough, MD, the director of the Mood and Anxiety Disorders Program at the Icahn School of Medicine at Mount Sinai.
“These medicines tend to increase the availability of serotonin in the brain, which can help boost your mood.”
And that’s the goal, right?
In general, antidepressants are well tolerated. But, like with all drugs, there are Zoloft side effects—some of which are merely annoying and some of which can actually be dangerous. “I generally start my patients on the lowest milligram pill and have them cut it in half for the few few doses just to make sure you’re tolerating it before bumping it up,” says Dr. Hermann.
So if you’re prescribed Zoloft, here’s what to look out for.
1
Changes in Weight or Appetite
People taking Zoloft gained nearly two pounds over the course of a year, according to one study published in the journal JAMA Psychiatry.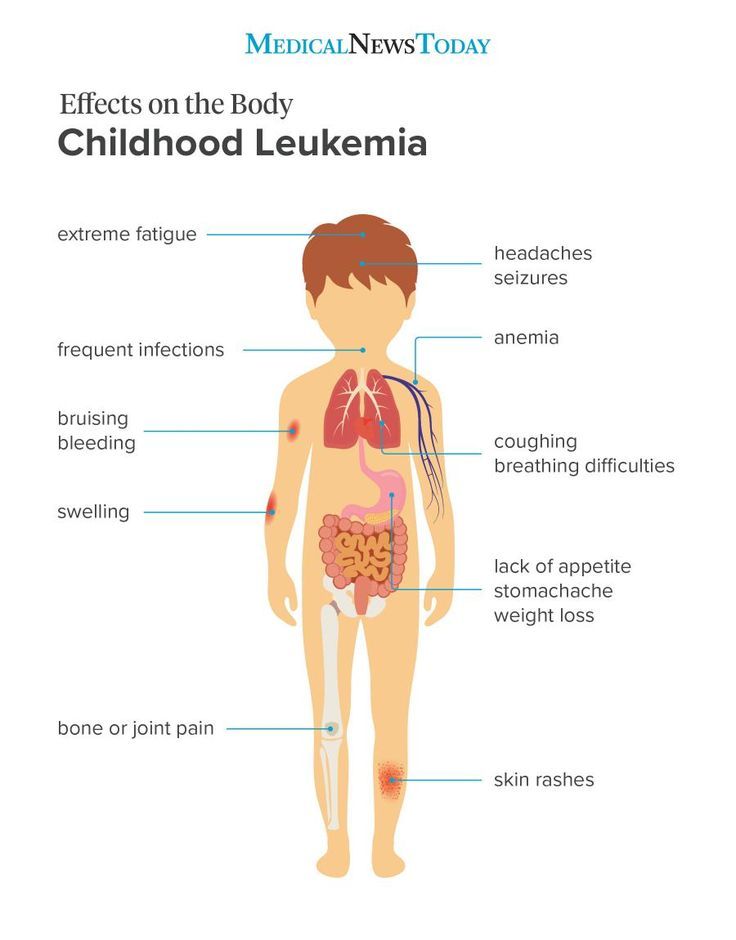 It’s not the only SSRI linked with weight gain, but if that’s a concern for you, talk to your doctor about your options.
It’s not the only SSRI linked with weight gain, but if that’s a concern for you, talk to your doctor about your options.
2
GI Effects
“Interestingly, there’s actually a lot of serotonin in the gastrointestinal tract, so people on Zoloft can experience changes in GI function,” says Dr. Murrough. “That could mean an upset stomach, nausea, or changes in bowel habits like constipation or diarrhea.” Dr. Murrough suggests starting on the lowest possible dose to avoid these issues, then increasing the dosage as your system acclimates to the extra serotonin.
3
Sexual Side Effects
This is one of those side effects no one wants to talk about, but it can affect at least a third of patients on SSRIs, says Dr. Murrough. “We don’t know why drugs like Zoloft have sexual side effects, but people can experience things like difficulty orgasming, a lack of sex drive, or the inability to get or maintain an erection. ” For some people, the benefits of the medicine will outweigh the negative effects on their sex life; for others, a change in medication may be necessary.
” For some people, the benefits of the medicine will outweigh the negative effects on their sex life; for others, a change in medication may be necessary.
4
Increased Anxiety
Another one of the more common Zoloft side effects is called akathisia. “It’s like feeling amped up or restless, like you need to move, or like you’re unable to calm down,” explains Dr. Hermann. In some cases, akathisia can even feel like a panic attack. But akathisia can be mitigated by starting on a really low dose and slowly working your way up, she adds.
5
Mood or Behavior Changes
Obviously, you want your mood to change while taking an antidepressant or anti-anxiety drug. “But the mood or behavior change that we’re most worried about as mental health professionals is increased depression or suicidal thoughts or a switch from depression to mania,” says Dr. Hermann. “Any antidepressant intervention has the potential to flip someone who’s vulnerable, who has bipolar disorder rather than depression, into a mania, which is why it’s so important to make sure you have the right diagnosis before starting medication.”
Hermann. “Any antidepressant intervention has the potential to flip someone who’s vulnerable, who has bipolar disorder rather than depression, into a mania, which is why it’s so important to make sure you have the right diagnosis before starting medication.”
6
Night Sweats
“Nighttime sweating is a common side effects of SSRIs, and Zoloft is one of the drugs where it’s more common,” says Dr. Hermann. “It’s not dangerous at all, provided that the person is seeing an internist regularly and has had a physical exam and lab work within the year to indicate there’s nothing else responsible for it.” It is uncomfortable, though, so Hermann recommends wearing sweat-wicking materials to bed and keeping your bedroom cool enough at night.
7
Serotonin Syndrome
“This is a catch-all term for what happens when there’s too much serotonin in the body,” says Dr. Murrough. “It affects your blood pressure, can cause severe GI symptoms, and can even lead to confusion, fevers, and seizures—in extreme cases, it’s life-threatening.”
Murrough. “It affects your blood pressure, can cause severe GI symptoms, and can even lead to confusion, fevers, and seizures—in extreme cases, it’s life-threatening.”
The risk is very low for people who are just taking one medication, but if someone is on several medications that affect serotonin levels, the risk level rises. “Sometimes, people describe this as a bad flu—so on the off chance that happens, call your doctor right away,” says Dr. Murrough. “The treatment is to simply stop the medication.”
8
Trouble Sleeping
In most cases, antidepressants and anti-anxiety meds help people sleep better. But, occasionally, “people report unusual dreams, restlessness during sleep, or feeling like their sleep is altered in some way,” says Dr. Hermann.
This is a potential risk of taking something that affects your brain, says Dr. Hermann, and if it’s disruptive enough to your life, your doctor might try you on a different drug.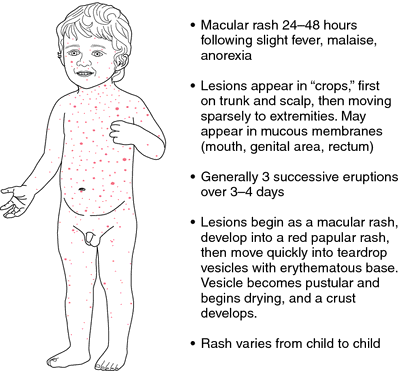
9
Rashes
Sometimes people can develop rashes or increased skin sensitivity while taking Zoloft, says Naema Qureshi, MD, a psychiatrist at Brooklyn Minds. It’ll usually go away on its own, and you can find relief in the mean time with an over-the-counter anti-itch cream.
“However, if you show signs of an allergic reaction, such as hives, itchiness, or throat swelling shortly after you start Zoloft, you should stop taking it and report these symptoms to your doctor immediately,” says Dr. Qureshi.
10
Headaches
Headaches are common when you first start taking Zoloft, or when you increase the dose, says Dr. Qureshi.
“For most people, headaches go away after a week or two as your body adjusts to the medication,” she explains. “If you experience occasional headaches while starting the medication, you can try common over-the-counter pain relievers such as Tylenol. ”
”
If your headaches are persistent, Dr. Qureshi recommends talking to your doctor, as it’s possible you may tolerate a different medication better.
11
Dry Mouth
Dry mouth is another common side effect of Zoloft which can sometimes persist, says Dr. Qureshi.
“It's important to pay attention to dry mouth because it can increase your risk of cavities and other oral issues,” she says. “In addition to maintaining good oral hygiene and hydration, you could consider trying a toothpaste or mouthwash specifically designed for dry mouth.”
12
Rare Side Effects
While most people tolerate Zoloft well, patients can experience rare but serious side effects such as vision changes, seizures, confusion, and dizziness while taking it, says Dr. Qureshi. Talk to your doc about any underlying conditions you have before you start any new meds, how Zoloft might interact with anything you're already taking, and seek immediate help if you start experiencing any of these uncommon side effects.
Ashley Mateo Ashley Mateo is a writer, editor, and UESCA- and RRCA-certified running coach who has contributed to Runner’s World, Bicycling, Women's Health, Health, Shape, Self, and more.
Emilia Benton Emilia Benton is a Houston-based freelance writer and editor.
Itch and skin rash from chocolate during fluoxetine and sertraline treatment: Case report | BMC Psychiatry
- Case report
- Open Access
- Published:
- Jonas Cederberg1,
- Stefan Knight2,
- Svante Svenson3 &
- …
- Håkan Melhus1
BMC Psychiatry volume 4, Article number: 36 (2004) Cite this article
-
92k Accesses
-
5 Altmetric
-
Metrics details
Abstract
Background
The skin contains a system for producing serotonin as well as serotonin receptors. Serotonin can also cause pruritus when injected into the skin. SSRI-drugs increase serotonin concentrations and are known to have pruritus and other dermal side effects.
Serotonin can also cause pruritus when injected into the skin. SSRI-drugs increase serotonin concentrations and are known to have pruritus and other dermal side effects.
Case presentation
A 46-year-old man consulted his doctor due to symptoms of depression. He did not suffer from any allergy but drinking red wine caused vasomotor rhinitis. Antidepressive treatment with fluoxetine 20 mg daily was initiated which was successful. After three weeks of treatment an itching rash appeared. An adverse drug reaction (ADR) induced by fluoxetine was suspected and fluoxetine treatment was discontinued. The symptoms disappeared with clemastine and betametasone treatment. Since the depressive symptoms returned sertraline medication was initiated. After approximately two weeks of sertraline treatment he noted an intense itching sensation in his scalp after eating a piece of chocolate cake. The itch spread to the arms, abdomen and legs and the patient treated himself with clemastine and the itch disappeared. He now realised that he had eaten a chocolate cake before this episode and remembered that before the first episode he had had a chocolate mousse dessert. He had never had any reaction from eating chocolate before and therefore reported this observation to his doctor.
He now realised that he had eaten a chocolate cake before this episode and remembered that before the first episode he had had a chocolate mousse dessert. He had never had any reaction from eating chocolate before and therefore reported this observation to his doctor.
Conclusions
This case report suggests that there may be individuals that are very sensitive to increases in serotonin concentrations. Dermal side reactions to SSRI-drugs in these patients may be due to high activity in the serotonergic system at the dermal and epidermo-dermal junctional area rather than a hypersensitivity to the drug molecule itself.
Peer Review reports
Background
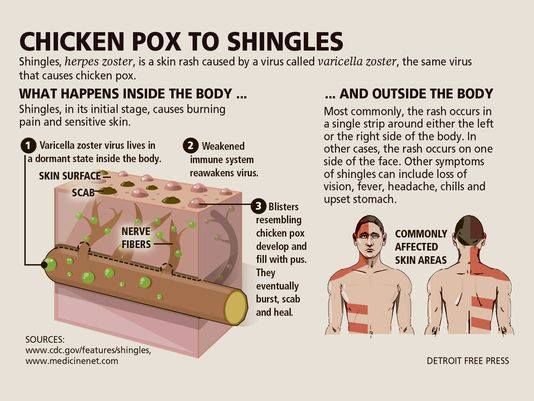
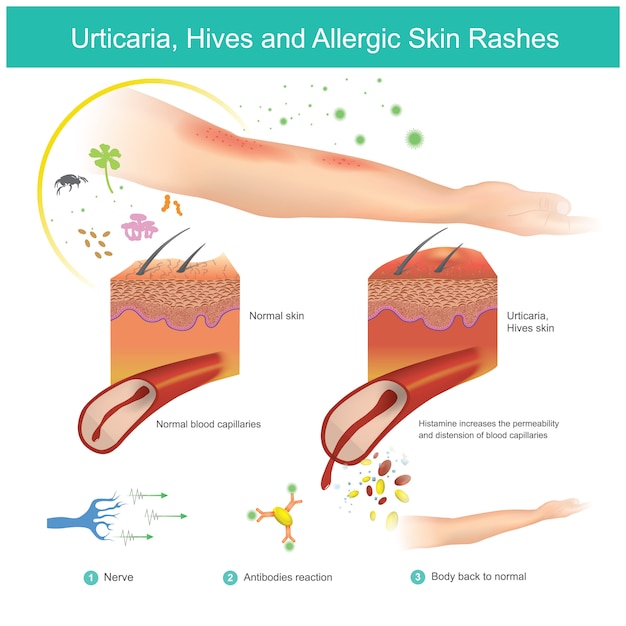
The skin contains a system for producing serotonin as well as serotonin receptors. Serotonin can also cause pruritus when injected into the skin. SSRI-drugs increase serotonin concentrations and are known to have pruritus and other dermal side effects e. g. exanthema, purpura, urticaria and pruritus [1]. In contrast, SSRI-medication has also been used to treat pruritus associated with cholestasis [2] and polycythemia vera [3]. In this report we describe a patient who developed pruritus and skin rash from chocolate, but only when he was under SSRI-treatment. The case is presented and we provide a putative biological rationale for the described phenomenon.
g. exanthema, purpura, urticaria and pruritus [1]. In contrast, SSRI-medication has also been used to treat pruritus associated with cholestasis [2] and polycythemia vera [3]. In this report we describe a patient who developed pruritus and skin rash from chocolate, but only when he was under SSRI-treatment. The case is presented and we provide a putative biological rationale for the described phenomenon.
Case presentation
A 46-year-old man consulted his doctor in September 2003 due to depression. He had then experienced symptoms for a few years that had aggravated during the last six to eight months. Using the Montgomery-Åsberg Depression Rate Scale (MADRS) the patient scored 24 points and was diagnosed as having a clinical depression. He did not take any medication and had no regular medical contact. The patient did not have any history of allergy or dermatological diseases. However, he sometimes suffered from vasomotor rhinitis after drinking red wine. The doctor prescribed fluoxetine 20 mg daily as antidepressive treatment. At the revisit three weeks later the patient was very pleased with the fluoxetine treatment and reported that he "had not felt better in 20 years" although he initially had experienced slight nausea and insomnia.
At the revisit three weeks later the patient was very pleased with the fluoxetine treatment and reported that he "had not felt better in 20 years" although he initially had experienced slight nausea and insomnia.
A week later, he visited his doctor due to an itching rash that had started the day before. The doctor noted partly confluent urticae on the abdomen, a modest periorbital oedema and red, warm palms and wrists. An ADR induced by fluoxetine was suspected and fluoxetine treatment was discontinued. The symptoms were treated with 2 mg clemastine and 6 mg betametasone orally and disappeared within 48 hours. However, the symptoms of depression returned. Sertraline medication was initiated 10 days after the cessation of fluoxetine treatment since SSRI medication had shown good effect. During the weeks of sertraline treatment no urticarial symptoms appeared. The patient improved in his depression although full recovery was not achieved this time. After approximately two weeks of sertraline treatment he noted an intense itching sensation in his scalp after eating a piece of chocolate cake. The itch spread to the arms, abdomen and legs within a few hours. This time the patient did not seek his doctor but treated himself with clemastine and the itch disappeared during the night. He now remembered that he had had a chocolate mousse dessert before the first episode. Since he had never had any reaction from eating chocolate before, he found this observation so striking that he reported it to his doctor. The patient, himself a scientist, later tried small doses of chocolate and skin rash and itch appeared at an intensity that to him seemed dependent on the "dose" of chocolate ingested.
The itch spread to the arms, abdomen and legs within a few hours. This time the patient did not seek his doctor but treated himself with clemastine and the itch disappeared during the night. He now remembered that he had had a chocolate mousse dessert before the first episode. Since he had never had any reaction from eating chocolate before, he found this observation so striking that he reported it to his doctor. The patient, himself a scientist, later tried small doses of chocolate and skin rash and itch appeared at an intensity that to him seemed dependent on the "dose" of chocolate ingested.
It has been known for 30 years that serotonin can stimulate cutaneous C-fibres [4], the type of fibres that is also known to transmit itch [5]. Moreover, serotonin injections into the skin can induce itch [6] and pruritus is a component in 24% of reported skin reactions to fluoxetine in Sweden, the corresponding figure for sertraline is 15 % [1]. However, attempts to treat pruritus using 5-HT3-receptor-antagonists have not given clear-cut results [6–8]. The enzymes necessary for conversion of tryptophan to serotonin are expressed in human skin [9]. In addition, 5-HT2AR are present in one third of unmyelinated axons at the dermal and epidermo-dermal junctional area [10]. An altered localisation pattern of serotonin receptors 5-HT1AR, 5-HT2AR and 5-HT3R has been reported in contact eczematous skin together with increased serotonin concentrations [11, 12] indicating the presence of a serotonin system in the skin that can be altered in pathologic conditions. Moreover, a cross-sensitivity has been reported when skin rash developed after both paroxetine and sertraline medication [13]. Since these substances are structurally different, one interpretation is that the skin can react to an SSRI-induced increase in serotonin concentrations.
The enzymes necessary for conversion of tryptophan to serotonin are expressed in human skin [9]. In addition, 5-HT2AR are present in one third of unmyelinated axons at the dermal and epidermo-dermal junctional area [10]. An altered localisation pattern of serotonin receptors 5-HT1AR, 5-HT2AR and 5-HT3R has been reported in contact eczematous skin together with increased serotonin concentrations [11, 12] indicating the presence of a serotonin system in the skin that can be altered in pathologic conditions. Moreover, a cross-sensitivity has been reported when skin rash developed after both paroxetine and sertraline medication [13]. Since these substances are structurally different, one interpretation is that the skin can react to an SSRI-induced increase in serotonin concentrations.
In the present case the patient experienced skin symptoms from two different SSRIs. However, these symptoms occurred only when he had eaten chocolate. Chocolate contains serotonin, at concentrations which depend on the type of chocolate [14]. A concentration of 1.4 – 5 μg / g has been reported in dark chocolate [14]. The present report suggests an interaction between SSRI-medication and chocolate leading to pruritus and rash. A plausible explanation is that SSRI together with serotonin-containing chocolate has increased serotonin concentration to a level where 5-HT receptors system at the dermal and epidermo-dermal junctional area are affected. Moreover, the patient in this case had previously noted nasal congestion and cough when he was drinking red wine. Red wine can induce release of serotonin from platelets [15] and from the gut [16]. Serotonin can induce nasal itch, sneeze and hypersecretion [17, 18].
A concentration of 1.4 – 5 μg / g has been reported in dark chocolate [14]. The present report suggests an interaction between SSRI-medication and chocolate leading to pruritus and rash. A plausible explanation is that SSRI together with serotonin-containing chocolate has increased serotonin concentration to a level where 5-HT receptors system at the dermal and epidermo-dermal junctional area are affected. Moreover, the patient in this case had previously noted nasal congestion and cough when he was drinking red wine. Red wine can induce release of serotonin from platelets [15] and from the gut [16]. Serotonin can induce nasal itch, sneeze and hypersecretion [17, 18].
Conclusions
Apart from the SSRI – chocolate interaction this patient had another possible sign of sensitivity to serotonin. The present case thus suggests that there may be individuals that are very sensitive to increases in serotonin concentrations. Skin side reactions to SSRI-drugs in these patients may be due to high activity in the serotonergic system system at the dermal and epidermo-dermal junctional area rather than a hypersensitivity to the drug molecule itself. However, the reaction of skin to serotonin from food is poorly studied and further studies are necessary to determine how much alimentary serotonin can increase serum serotonin concentrations and to what extent SSRI-medication affects this process. More knowledge in this field could be of help for physicians who encounter patients with dermal reactions to SSRI-drugs and there might be food and beverages containing serotonin that these patients should avoid. Moreover, possible individual differences in the serotonergic system at the dermal-epidermal junction remain to be studied.
However, the reaction of skin to serotonin from food is poorly studied and further studies are necessary to determine how much alimentary serotonin can increase serum serotonin concentrations and to what extent SSRI-medication affects this process. More knowledge in this field could be of help for physicians who encounter patients with dermal reactions to SSRI-drugs and there might be food and beverages containing serotonin that these patients should avoid. Moreover, possible individual differences in the serotonergic system at the dermal-epidermal junction remain to be studied.
What happened to the patient and his depression? Due to poor anti-depressive effect of sertraline, the treatment was altered back to fluoxetine. He is now free from his depression and experiences no rash or oedema-like adverse reactions as long as he is avoiding chocolate.
Abbreviations
- 5-HT:
-
5-hydroxytryptamine, ADR: Adverse Drug Reaction, SSRI: serotonin selective reuptake inhibitors
References
SWEDIS, the Swedish Drug Information System database.
Browning J, Combes B, Mayo MJ: Long-term efficacy of sertraline as a treatment for cholestatic pruritus in patients with primary biliary cirrhosis. Am J Gastroenterol. 2003, 98: 2736-41. 10.1016/S0002-9270(03)01695-2.
Article CAS PubMed Google Scholar
Tefferi A, Fonseca R: Selective serotonin reuptake inhibitors are effective in the treatment of polycythemia vera-associated pruritus. Blood. 2002, 99: 2627-10.1182/blood.V99.7.2627.
Article CAS PubMed Google Scholar
Beck PW, Handwerker HO: Bradykinin and serotonin effects on various types of cutaneous nerve fibres. Pflugers Arch. 1974, 347: 209-22.
Article CAS PubMed Google Scholar
Schmeltz M, Schmidt R, Bickel A, Handwerker HO, Torebjörk HE: Specific C-receptors for itch in human skin. J Neuosci. 1997, 17: 8003-08.
Google Scholar
Weisshaar E, Ziethen B, Gollnick H: Can a serotonin type 3 (5-HT3) receptor antagonist reduce experimentally-induced itch?. Inflamm Res. 1997, 46: 412-16. 10.1007/s000110050213.
Article CAS PubMed Google Scholar
Ashmore SD, Jones CH, Newstead CG, Daly MJ, Chrystyn H: Ondansetron therapy for uremic pruritus in hemodialysis patients. Am J Kidney Dis. 2000, 35: 827-31.
Article CAS PubMed Google Scholar
Schwörer H, Hartmann H, Ramadori G: Relief of cholestatic pruritus by a novel class of drugs: 5-hydroxytryptamine type 3 (5-HT3) receptor antagonists: effectiveness of ondansetron.
 Pain. 1995, 61: 33-37. 10.1016/0304-3959(94)00145-5.
Pain. 1995, 61: 33-37. 10.1016/0304-3959(94)00145-5.Article PubMed Google Scholar
Slominski A, Pisarchik A, Semak I, Sweatman T, Wortsman J, Szczesniewski A, Slugocki G, McNulty J, Kauser S, Tobin DJ, Jing C, Johansson O: Serotonergic and melatoninergic systems are fully expressed in human skin. FASEB J. 2002, 16: 896-98.
CAS PubMed Google Scholar
Carlton SM, Coggeshall RE: Immunohistochemical localization of 5-HT2A receptors in peripheral sensory axons in rat glabrous skin. Brain Res. 1997, 763: 271-75. 10.1016/S0006-8993(97)00489-7.
Article CAS PubMed Google Scholar
Lundeberg L, El-Nour , Mohabbatti S, Morales M, Azmitia E, Nordlind K: Expression of serotonin receptors in allergic contact excematous human skin. Arch Dermatol Res.
 2002, 294: 393-98.
2002, 294: 393-98.CAS PubMed Google Scholar
Lundeberg L, Liang Y, Sundström E, Nordlind K, Verhofstad A, Liden S, Johansson O: Serotonin in human allergic contact dermatitis. An immunohistochemical and high performance liquid chromatography study. Arch Dermatol Res. 1999, 291: 269-74. 10.1007/s004030050407.
Article CAS PubMed Google Scholar
Warnock CA, Azadian AG: Cross-sensitivity between paroxetine and sertraline. Ann Pharmacother. 2002, 36: 631-33. 10.1345/aph.1A262.
Article PubMed Google Scholar
Herraiz T: Tetrahydro-b-carbolines, potential neuroactive alkaloids, in chocolate and cocoa. J Agric Food Chem. 2000, 48: 4900-04. 10.1021/jf000508l.
Article CAS PubMed Google Scholar
Jarman J, Pattichis K, Peatfield R, Glover V, Sandler M: Red wine-induced release of [14C]5-hydroxytryptamine from platelets of migraine patients and controls. Cephalalgia. 1996, 16: 41-43. 10.1046/j.1468-2982.1996.1601041.x.
Article CAS PubMed Google Scholar
Pattichis K, Louca L, Jarman J, Glover V: Red wine can cause a rise in human whole blood 5-hydroxytryptamine levels. Med Sci Res. 1994, 22: 381-82.
CAS Google Scholar
Tonnesen P, Mygind N: Nasal challenge with serotonin and histamine in normal persons. Allergy. 1985, 40: 350-53.
Article CAS PubMed Google Scholar
Tonnesen P, Schaffalitzky de Muckadell OB, Mygind N: Nasal challenge with serotonin in asymptomatic hay fever patients. Allergy. 1987, 42: 447-50.

Article CAS PubMed Google Scholar
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-244X/4/36/prepub
Download references
Acknowledgements
Written consent was obtained from the patient for publication of study.
Author information
Authors and Affiliations
Department of Clinical Chemistry and Pharmacology, Uppsala Academic Hospital, Uppsala, Sweden
Jonas Cederberg & Håkan Melhus
Department of Molecular Biology, Swedish University of Agricultural Sciences, Uppsala, Sweden
Stefan Knight
Fålhagens Primary Care Center, Uppsala, Sweden
Svante Svenson
Authors
- Jonas Cederberg
View author publications
You can also search for this author in PubMed Google Scholar
- Stefan Knight
View author publications
You can also search for this author in PubMed Google Scholar
- Svante Svenson
View author publications
You can also search for this author in PubMed Google Scholar
- Håkan Melhus
View author publications
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Jonas Cederberg.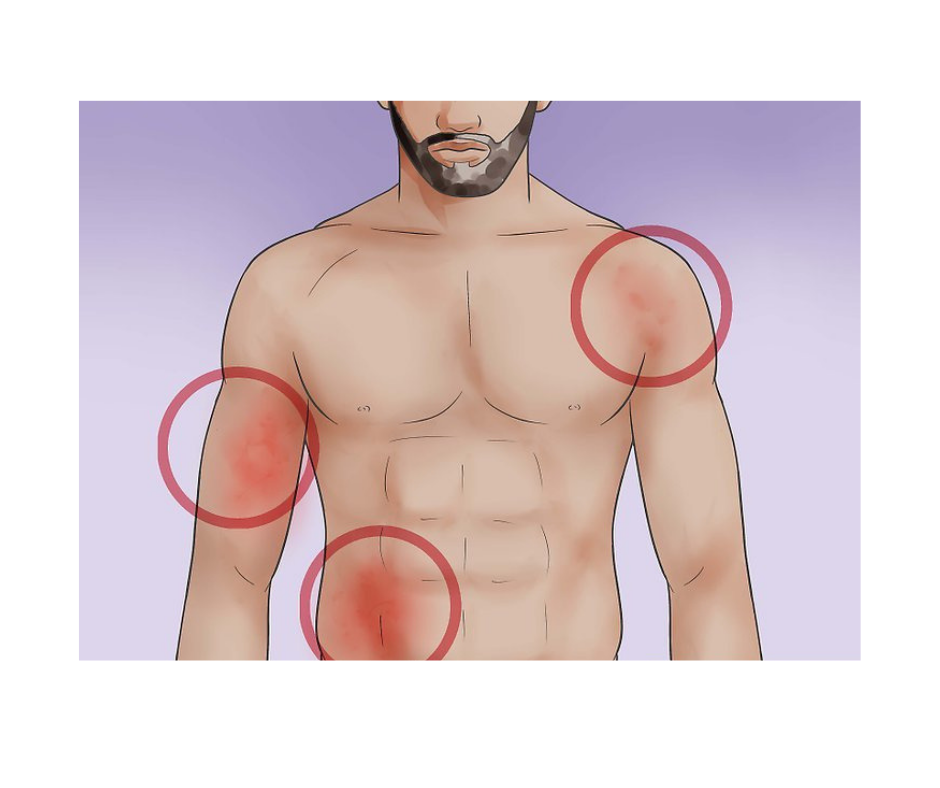
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
SS first described the case, JC and HM performed literature searches and JC first drafted the manuscript. HM and SK took part in the scientific discussion and in finalising the manuscript.
Rights and permissions
Reprints and Permissions
About this article
SIDE EFFECTS OF ANTIDEPRESSANTS (SSRIs) | Clinical Center "Psychiatry - Narcology"
Currently, the most commonly prescribed antidepressants are drugs from the group of selective serotonin reuptake inhibitors (SSRIs). For most, these medicines are safe and effective, but like all medicines, they can cause side effects. According to statistics, about 40% of patients taking antidepressants also experience side effects, in about 25% of cases they are quite unpleasant. Two of the most common side effects (sexual dysfunction and weight gain) are often the reason people stop taking these medications.
Listed below are the 7 most common side effects of antidepressants that patients should be aware of:
1. SOMATIC SYMPTOMS.
When medications are first prescribed to treat depression, the most common physical symptoms are headache, nausea, joint and muscle pain, rash, and diarrhea. These symptoms are usually mild and temporary. The results of clinical studies have shown that nausea and headache are the most common. As a rule, these symptoms are adaptive in nature, as a rule, they pass on their own, without requiring discontinuation of the drug.
2. SLEEP DISTURBANCE.
Many patients, when first prescribed antidepressants, report problems with sleep: difficulty falling asleep or light sleep with frequent awakenings. Also, against the background of taking SSRIs, nightmares and sleepwalking can be observed. Studies have shown that about 22% of people taking antidepressants experience sleep problems.
3. DAY SLEEPNESS .
DAY SLEEPNESS .
Sleepiness during the day may be the result of a poor night's sleep, or the direct sedative effect of the antidepressant. In the case when it is a sedative effect, the problem can be solved by transferring the drug to the evening.
4. MIGRAINES
Due to the fact that people who are prone to depression also often suffer from migraines, you need to be careful when taking medications in combination. Medicines; used to treat migraines, triptans, like SSRIs, increase serotonin levels in the brain. If these drugs are used together, it can lead to the development of serotonin syndrome, which manifests itself in the form of headache, heart palpitations, hot flashes. Be sure to discuss with your doctor how to avoid the development of serotonin syndrome if you are prescribed medications of both groups.
5. WEIGHT SET.
Weight gain is one of the late side effects of antidepressants and is one of the most common reasons for refusing to continue taking or changing the drug. A good prevention of this side effect is moderate physical activity (for example, a 30-minute workout every other day). The likelihood of weight gain also depends on the drug that is prescribed. According to clinical trials, while taking paroxetine, about 25% of patients gain 7% of their weight.
A good prevention of this side effect is moderate physical activity (for example, a 30-minute workout every other day). The likelihood of weight gain also depends on the drug that is prescribed. According to clinical trials, while taking paroxetine, about 25% of patients gain 7% of their weight.
6. SUICIDE .
The risk of suicide while taking antidepressants is currently under extensive investigation. According to most studies, compared with placebo, taking SSRIs or other antidepressants doubles the likelihood of suicidal thoughts. The overall risk of this side effect when taking antidepressants in adolescents and adults is 2 to 4 percent. One of the reasons for suicide while taking antidepressants is that medications increase activity, giving energy for the implementation of a suicidal plan. Regular follow-up by a doctor can reduce the risk of this side effect.
7. SEXUAL DYSFUNCTION.
Sexual dysfunction is one of the most common long-term side effects of SSRIs. These include decreased sexual desire, delayed ejaculation in men, and inability to achieve orgasm in women. Up to 60% of people taking SSRIs experience one of these side effects. And these are the side effects that patients are not ready to endure.
These include decreased sexual desire, delayed ejaculation in men, and inability to achieve orgasm in women. Up to 60% of people taking SSRIs experience one of these side effects. And these are the side effects that patients are not ready to endure.
If you are concerned about any side effects, discuss them with your doctor. As a rule, you can find a solution for any of them. It is not recommended to stop taking medications on your own.
Arpimed
Amitriptyline can be taken no earlier than 14 days after stopping the intake of MAO inhibitors.
Warnings and precautions
Talk to your doctor or pharmacist before using Amitriptyline.
Arrhythmias and hypotension may occur with high doses of amitriptyline. This can also occur at regular doses if you suffer from heart disease.
QT interval prolongation
Cardiac pathology called “QT interval prolongation” (which is recorded on the electrocardiogram, ECG) and arrhythmia (rapid or irregular heartbeat) was observed with the use of Amitriptyline. Tell your doctor if:
Tell your doctor if:
- you have a slow heartbeat,
- you have or have had problems where your heart is not able to supply the body with the blood it needs (a condition called heart failure),
- are taking other medicines that can cause heart problems, or
- have a disorder that leads to a decrease in the level of potassium or magnesium or an increase in the level of potassium in the blood
- if you are preparing for surgery, as it may be necessary to stop taking amitriptyline before administering anesthetics. In case of emergency surgery, the anesthesiologist should be informed about the treatment with amitriptyline.
- have an overactive thyroid or are taking thyroid medication.
Suicidal thoughts and worsening of your depressive disorder
If you are depressed, you may sometimes have suicidal thoughts and desire to hurt yourself. These may be increased the first time antidepressants are used, as these drugs take time to develop an effect, about 2 weeks or more.
This is especially observed in the following categories of patients:
- if you have had suicidal thoughts and desire to hurt yourself in the past,
- if you are young. Data from clinical studies have shown that an increased risk of suicidal tendencies occurs in people under the age of 25 with psychiatric disorders treated with antidepressants.
If you have suicidal thoughts and want to hurt yourself, call your doctor or go to the hospital right away.
It may be helpful to tell a relative or close friend that you are depressed and ask them to read this leaflet. You can ask them to tell you if they think your depression or anxiety is getting worse, or if they are worried about changes in your behavior.
Manic episode
Some patients with manic-depressive illness may enter a manic phase. It is characterized by exuberant and rapidly changing ideas, hyperthymia (persistent high spirits), and excessive physical activity.
Tell your healthcare provider if you have or have recently had health problems, especially if you have
- narrow angle glaucoma (loss of vision due to an abnormal increase in intraocular pressure)
- epilepsy, history of convulsions or seizures
- difficulty urinating
- prostate enlargement
- diseases of the thyroid gland
- bipolar disorder
- schizophrenia
- acute liver diseases
- severe heart disease
- pyloric stenosis (narrowing of the opening at the outlet of the stomach) and paralytic ileus (intestinal obstruction)
- diabetes, as you may need to adjust the dose of your diabetes medicine.
If you are using antidepressants such as selective serotonin reuptake inhibitors (SSRIs), your doctor may consider changing the dose of your medicine (see section Other drugs and Amitriptyline and section How to take Amitriptyline).
Older people are more likely to experience certain side effects, such as dizziness with orthostatic hypotension (see section Possible side effects).
Children and adolescents
Depression, neuropathic pain, chronic tension headache and migraine prophylaxis
Amitriptyline should not be given to children and adolescents under 18 years of age as safety and efficacy have not been established in this age group.
Bedwetting
- ECG should be performed prior to starting amitriptyline therapy to rule out long QT syndrome
- Medicines in this group should not be taken concomitantly with anticholinergics (see also section Other medicines and Amitriptyline)
- Suicidal thoughts and behavior may also develop during early antidepressant treatment for disorders other than depression; in the treatment of patients with bedwetting, the same precautions should be observed as in the treatment of patients with depression.
Other medicines and Amitriptyline
Some medicines can affect the way other medicines work and this can sometimes cause serious side effects.
Tell your doctor or pharmacist if you are taking, have recently taken or should be taking any other medicines such as: (used to treat Parkinson's disease). They should not be taken during a course of treatment with amitriptyline (see section Do not take amitriptyline)
 John's wort - herbal remedy for depression
John's wort - herbal remedy for depression
Also tell your doctor if you are taking, have recently taken or may be taking medicines that can affect your heart rate, including:
- medicines for the treatment of palpitations (including quinidine and sotalol)
- astemizole and terfenadine (used to treat allergic reactions and hay fever)
- medicines used to treat certain mental illnesses (including pimozide and sertindole)
- cisapride (used to treat certain types of indigestion)
- halofantrine (used to treat malaria)
- methadone (used for pain relief and drug detoxification)
- diuretics (including furosemide).
If you are having surgery with general or local anesthetics, you must tell your doctor that you are taking this drug.
You must also tell your dentist that you are taking this drug before you use a local anesthetic.
Amitriptyline with alcohol
It is not recommended to drink alcohol during treatment with this medicine, as this may increase the sedative effect.
Pregnancy and lactation
If you are pregnant or breastfeeding, think you may be pregnant or are planning to become pregnant, please consult your healthcare professional.
Amitriptyline is not recommended during pregnancy unless you and your doctor have discussed the risks and benefits of using the drug.
If you are taking this drug during the last trimester of pregnancy, you should know that your newborn baby may have the following side effects such as irritability, increased muscle tension, tremors, irregular breathing, reluctance to drink fluids, loud crying, urinary retention and constipation.
Your doctor will tell you to start/continue/stop breastfeeding or stop using this drug based on the benefits of breastfeeding for your baby and the benefits of therapy for you.
Influence on the ability to drive and use mechanisms
The drug may cause drowsiness, dizziness, especially at the beginning of treatment. It is unacceptable to drive or work with mechanisms if it negatively affects you.
Important information about the ingredients of amitriptyline tablets
Amitriptyline tablets contain lactose
we carry medicine.
How to take Amitriptyline
Amitriptyline should be taken exactly as directed by your doctor. If you have any doubts, you should consult your doctor or pharmacist.
Not all dosage regimens are possible with different dosage forms and doses of the drug.
The appropriate dosage form and dosage must be selected for starting 3 and subsequent increasing doses.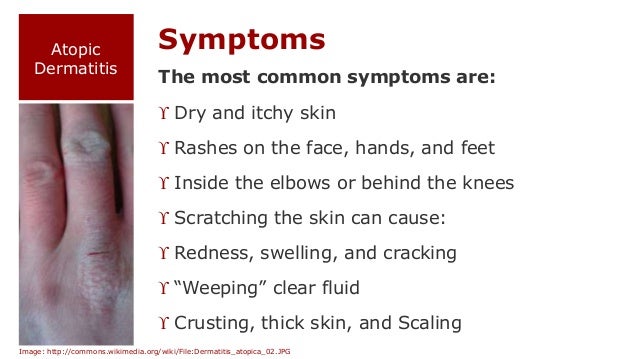
Depression
Adults :
The recommended starting dose is 25 mg twice a day. Depending on the clinical effect, the dose may be increased up to 150 mg/day divided into two doses.
Elderly patients (over 65 years of age) and patients with cardiovascular disease
The recommended starting dose is 10-25 mg per day. Depending on the clinical effect, the dose may be increased to 100 mg / day, divided into two doses. If you are taking 100mg to 150mg of the drug, you may need to see your doctor more often.
Use in children and adolescents
Amitriptyline is not recommended for children and adolescents to treat depression. See section 2 for more information.
Neuropathic pain, chronic headaches tension-type headaches and migraine prophylaxis
Your doctor will adjust the dose to your treatment according to your symptoms and response to your symptoms.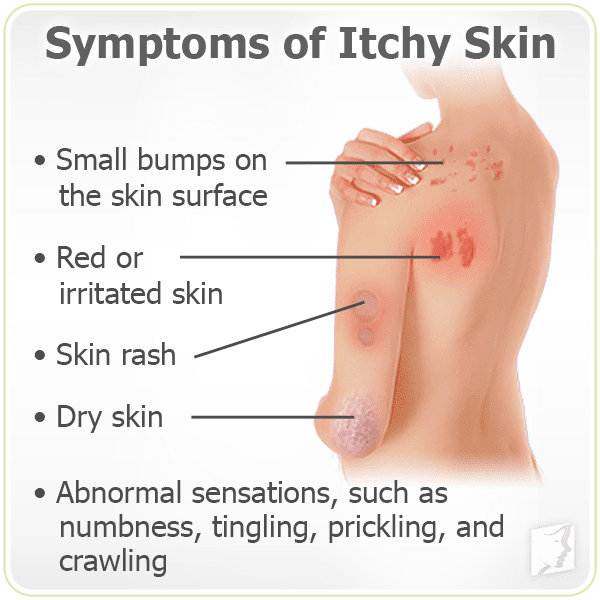
Adults :
The recommended starting dose is 10-25 mg in the evening.
The recommended daily dose is 25-75 mg.
Depending on the clinical effect, the dose may be gradually increased. If you are taking more than 100mg/day, you may need to see your doctor more often. Take the drug once a day or divide the dose into two doses, your doctor will tell you.
Elderly patients (over 65 years of age) and patients with cardiovascular disease
The recommended starting dose is 10-25 mg in the evening.
Depending on the clinical effect of the drug, the dose may be gradually increased.
If you are taking more than 75 mg/day, you may need to see your doctor more often.
Use in children and adolescents
Amitriptyline is not recommended for use in children and adolescents for the treatment of neuropathic pain, chronic tension headache and migraine prophylaxis. For more information, see What you need to know before you use Amitriptyline.
For more information, see What you need to know before you use Amitriptyline.
Bedwetting
Use in children and adolescents
0072
The dose should be increased gradually.
Should be taken 1 to 1.5 hours before bedtime.
Before starting treatment, your healthcare provider should perform an ECG to check for signs of a palpitations.
Your doctor will re-evaluate your condition after 3 months of treatment and, if necessary, perform a repeat ECG.
Do not stop taking this medicine without your doctor's advice.
Special patient populations
Patients with liver disease or known to be "slow metabolizers" are usually given lower doses.
Your doctor may take blood samples to check your amitriptyline level (see What you need to know before you use amitriptyline).
How and when to take Amitriptyline
The drug should be taken during or after a meal.
Tablets should be swallowed whole with water. Tablets should not be chewed.
Treatment period
Do not change the dose of the drug or stop taking the drug without consulting a doctor.
Depression
As with other drugs used to treat depression, this too can take several weeks before you feel any improvement in your condition.
In the treatment of depression, the duration of treatment is individual and is usually at least 6 months. The duration of treatment is determined by your doctor.
Continue taking Amitriptyline for as long as your doctor tells you to. The disease may persist for a long time. If you stop treatment too soon, the symptoms of the disease may recur.
Neuropathic pain, chronic headaches tension type and migraine prevention
It may take a few weeks for your condition to improve.
Talk to your doctor about the duration of treatment and continue taking the drug until the doctor stops it.
Bedwetting
Your doctor will determine if you need to continue treatment after 3 months of taking the drug.
If you have taken more Amitriptyline than recommended
If you have taken more Amitriptyline than prescribed by your doctor, contact your doctor or the nearest hospital emergency department immediately, even if you do not experience any discomfort or symptoms of poisoning . Take the medicine package with you if you go to the doctor or hospital.
Overdose symptoms include:
- dilated pupils
- rapid or irregular heartbeat
- difficulty urinating
- dry mouth or tongue
- intestinal obstruction
- fits
- fever
- anxiety
- confusion
- hallucinations
- involuntary movements
- low blood pressure, weak pulse, pallor
- shortness of breath
- cyanosis of the skin
- Decreased heart rate
- drowsiness
- loss of consciousness
- coma
- various heart diseases such as cardiac conduction block, heart failure, hypotension, cardiogenic shock, metabolic acidosis, hypokalemia.