Side effects of lobotomies
What is a lobotomy? Uses, procedure, and history
A lobotomy is a type of brain surgery that became popular in the 1930s as a treatment for mental health conditions. It involves severing the connection between the frontal lobe and other parts of the brain.
Doctors performed this procedure on people with conditions such as schizophrenia and depression. At the time, there were no effective or widely available treatments for these conditions.
However, lobotomies are dangerous. They carry several serious risks, including seizures and death. Due to the impact of this procedure on people who were lobotomized and their families, it fell out of use in the 1950s, according to 2013 research.
Keep reading to learn more about the history, procedure, and uses of lobotomies, as well as the effects and risks.
Share on PinterestA surgeon using a brace and bit to drill into a patient’s skull before performing a lobotomy, at a mental hospital in England, November 1946. Kurt Hutton/Getty ImagesThe word “lobotomy” refers to several brain surgeries that break connections between the frontal lobe and different parts of the brain. The frontal lobe is involved in many brain processes, including language, voluntary motion, and many cognitive abilities.
The different types of lobotomy include:
- topectomy, in which a surgeon removes parts of the frontal lobe
- leucotomy or leukotomy, in which a surgeon severs connections between the frontal lobe and the thalamus
- neuro-injection of sclerosing agents, in which a surgeon injects drugs that harden the fibers connecting the frontal lobe to the thalamus
According to 2017 research, lobotomies are rare today. Although the techniques have advanced and improved, most doctors consider the surgery obsolete.
However, lobotomies are still legal in some places. A 2019 study reports that after lobotomies became unpopular, most states enacted laws to regulate the use of surgery for mental illness. However, despite this effort, the laws across the United States are inconsistent.
Doctors developed the lobotomy in the late 19th and early 20th centuries, at a time when there were no drug therapies for mental health disorders, and psychotherapy was still in its early stages.
As there were no standardized or effective treatments, people with severe symptoms often lived in psychiatric hospitals and asylums. In Europe, many of these facilities were overcrowded, which led doctors to look for a solution.
Lobotomies in Europe
The inception of lobotomies dates back to 1891 when the Swiss psychiatrist Gottlieb Burckhardt performed surgery on several people with severe schizophrenia. He removed parts of their brains, and noted that after the procedure, those people were quieter.
Burckhardt intended for this treatment to be palliative. It was not a cure. Instead, it was a last resort for people whose conditions did not respond to other treatments. At the time, the medical community rejected his idea.
However, in the 1930s, some doctors revived the idea. The Portuguese neurologist António Egas Moniz collaborated with his colleague, Almeida Lima, to develop the leucotomy. The two began promoting the procedure across Europe, despite a lack of convincing evidence that it was beneficial.
Lobotomies in the U.S.
The popularity of the lobotomy in Europe led to its introduction in North America. Neurologist Walter Freeman and neurosurgeon James Watts modified the procedure to make it slightly less invasive than the European method.
At first, Watts was the member of the duo who performed the surgery. Later, Freeman “simplified” the surgery and began performing it in non-sterile conditions. In response, Watts severed his ties with Freeman due to concerns about the lack of sterility and the crudeness of the simplified procedure.
Lobotomies became a popular treatment in the U.S., with thousands of people undergoing the procedure. Around 1949, doubts increased about the safety of the procedure, as critics felt it did grievous harm.
When the schizophrenia medication chlorpromazine (Thorazine) came onto the market in the 1950s, lobotomies fell out of favor. The drug was a safer and noninvasive treatment option.
The main use of the lobotomy was to treat mental health conditions or reduce their symptoms. Burckhardt used it to reduce aggression in people with schizophrenia, believing that the frontal lobe was responsible for this symptom.
Burckhardt used it to reduce aggression in people with schizophrenia, believing that the frontal lobe was responsible for this symptom.
When Moniz and Lima revived the lobotomy in the 1930s, it was with the explicit goal of changing the disposition of people with mental health conditions. Often, the procedure made people quiet and docile, which they interpreted as a sign of success.
However, what doctors consider a mental health disorder has changed over time. Prejudice and biases also played a role in how doctors used the procedure.
In addition to people who meet current definitions for mental illness, practitioners also performed lobotomies on people:
- with intellectual disabilities
- who were gay
- who were in prison for crimes, which some blamed on “criminal insanity”
A 2018 study also states that most lobotomized people were women.
One analysis of a U.S. hospital revealed that out of 245 lobotomies doctors performed between 1947–1954, 84% were on women, despite the fact that the hospital had more men as patients, and more men had schizophrenia diagnoses.
Often, the reason doctors gave for this was that they needed to “maintain order” in the hospital. Other reasons included a lack of interest in child care and “strange behavior.”
Rarely, doctors used lobotomies in an attempt to treat physical conditions, such as ulcerative colitis or brain tumors.
Learn more about gender bias in medical diagnosis.
There was a range of approaches to performing lobotomies. The first lobotomies involved open brain surgery. When the procedure regained popularity in the 1930s, neurologists refined the technique to make it less invasive.
In the U.S., Watts promoted a technique that involved drilling or cutting a hole in the skull to sever the connection between the frontal lobe and the thalamus. This involved the participation of a surgeon and surgical assistants.
Later, Freeman altered the procedure. Instead of drilling a hole, he used an instrument similar to an ice pick to enter the skull through the eye socket and pierce the brain. This is known as the transorbital lobotomy.
This is known as the transorbital lobotomy.
Freeman claimed this method did not require surgical assistants, sterile operating rooms, or scrubs. According to him, doctors could perform lobotomies anywhere with very little equipment.
Later, doctors tried other techniques, such as injecting radioactive iridium through the eye socket.
Proponents of lobotomies thought that the procedure could address the root cause of mental health symptoms by cutting off the part of the brain they believed was responsible for them.
For example, Freeman theorized that psychosis stemmed from excessive self-reflection. He felt this was due to thoughts that circled repeatedly in the brain. In his view, lobotomies provided a literal way of cutting off these circling thoughts.
However, lobotomies do not treat the causes of mental health conditions. Instead, they reduce the functionality of the frontal lobe, resulting in:
- apathy
- distractibility
- lack of initiative
- lack of restraint, such as in social situations
- euphoria, a feeling of intense happiness
- significant changes in personality
In some cases, people’s symptoms did seem to ease as a result of the procedure, and some were able to return to work. However, the effects varied.
However, the effects varied.
One of the criticisms of the procedure was that it was for the benefit of those looking after the lobotomy recipients rather than for the people themselves, by making them easier to manage.
Many people who underwent lobotomies experienced severe side effects and complications, such as:
- chronic headaches
- seizures
- intracranial hemorrhages, or bleeding inside the skull
- dementia, a condition that causes memory decline and personality changes
- brain abscesses
- death
A lobotomy is a surgical procedure that doctors developed as a treatment for mental health conditions in the late 19th and early 20th centuries. It involves breaking the connection between the frontal lobe and the thalamus.
While lobotomies caused some people with mental illnesses to become calmer, they also frequently caused significant changes in personality, such as apathy and social disinhibition. The procedure had very serious health risks, and doctors sometimes used it in ways that were unethical.
Lobotomy | Definition, Procedure, History, Effects, & Facts
lobotomy
See all media
- Key People:
- António Egas Moniz Walter Jackson Freeman II
- Related Topics:
- brain psychosurgery transorbital lobotomy
See all related content →
Top Questions
What is lobotomy?
Lobotomy is a surgical procedure in which the nerve pathways in a lobe of the brain are severed from those in other areas.
What is the purpose of a lobotomy?
Lobotomies have been used as a radical therapeutic measure intended to calm patients with mental illnesses like schizophrenia and bipolar disorder.
When was the first lobotomy performed?
The first lobotomy was performed in the late 1880s, when Swiss physician Gottlieb Burckhardt removed parts of the brain cortex in patients suffering from auditory hallucinations and other symptoms of schizophrenia. Burckhardt performed the operation on six patients; one died several days after, and another committed suicide.
Burckhardt performed the operation on six patients; one died several days after, and another committed suicide.
Have lobotomies ever been a popular procedure?
Lobotomies were performed on a wide scale in the 1940s, with one doctor, Walter J. Freeman II, performing more than 3,500 by the late 1960s. The practice fell out of favour in the mid-1950s, when less extreme mental health treatments like antidepressants and antipsychotics came into use. They are rarely, but occasionally, used today. Learn more.
What are the effects of a lobotomy?
The intended effect of a lobotomy is reduced tension or agitation, and many early patients did exhibit those changes. However, many also showed other effects, such as apathy, passivity, lack of initiative, poor ability to concentrate, and a generally decreased depth and intensity of their emotional response to life. Some died as a result of the procedure.
Summary
Read a brief summary of this topic
lobotomy, also called prefrontal leukotomy, surgical procedure in which the nerve pathways in a lobe or lobes of the brain are severed from those in other areas. The procedure was formerly used as a radical therapeutic measure to help grossly disturbed patients with schizophrenia, manic depression and mania (bipolar disorder), and other mental illnesses.
The procedure was formerly used as a radical therapeutic measure to help grossly disturbed patients with schizophrenia, manic depression and mania (bipolar disorder), and other mental illnesses.
Evidence that surgical manipulation of the brain could calm patients first emerged in the late 1880s, when Swiss physician Gottlieb Burkhardt, who supervised an insane asylum, removed parts of the brain cortex in patients suffering from auditory hallucinations and other symptoms of mental illness (symptoms later defined medically as schizophrenia). Burkhardt performed his operation on six patients, with the specific purpose not of returning the patients to a state of sanity but of putting them into a state of calm. One of Burkhardt’s patients died several days following the operation, and another later committed suicide (though it is unclear whether the suicide was associated with the surgery). However, several of the patients were easier to manage following the surgery. His idea for the operation had been influenced by the work of German physiologist Friedrich Goltz, who had performed brain ablation (surgical removal of tissue) experiments on dogs and observed distinct changes in the animals’ behaviour.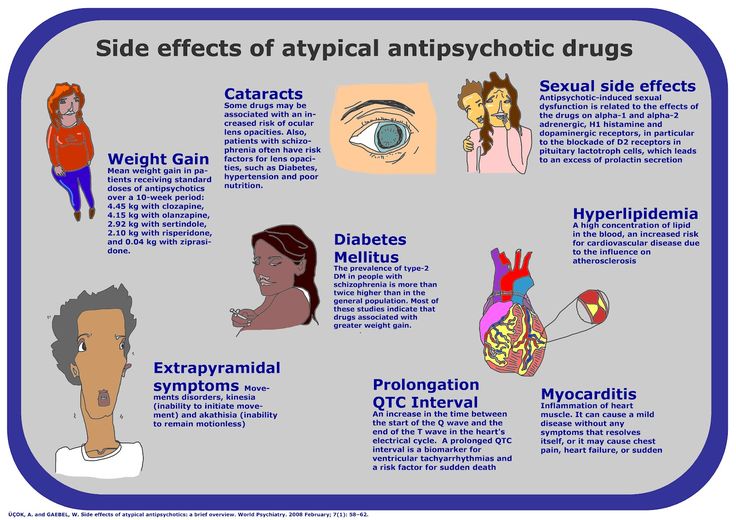 In the decades following Burkhardt’s work, there were few attempts at surgical disruption of the human brain.
In the decades following Burkhardt’s work, there were few attempts at surgical disruption of the human brain.
In 1935, however, American neuroscientists Carlyle F. Jacobsen and John Fulton presented the results of an experiment involving frontal lobe ablation in chimpanzees. Prior to ablation, one of the animals would become agitated when it made an incorrect choice during a memory task; this response was eliminated by the operation. (The other animal in the study experienced the opposite reaction; having been relatively docile, after ablation it experienced agitation during task performance.)
Also in 1935, Portuguese neurophysician António Egas Moniz headed a similar operation on a human. Moniz, who was affected by gout and could not use his hands to perform the surgery, enlisted the help of Portuguese surgeon Pedro Almeida Lima. The surgery consisted of drilling two holes in the patient’s head and then injecting pure ethyl alcohol into the prefrontal cortex. Alcohol was used to disrupt the neuronal tracts that were believed to give rise to and reinforce the recurrent patterns of thought observed in mentally ill patients.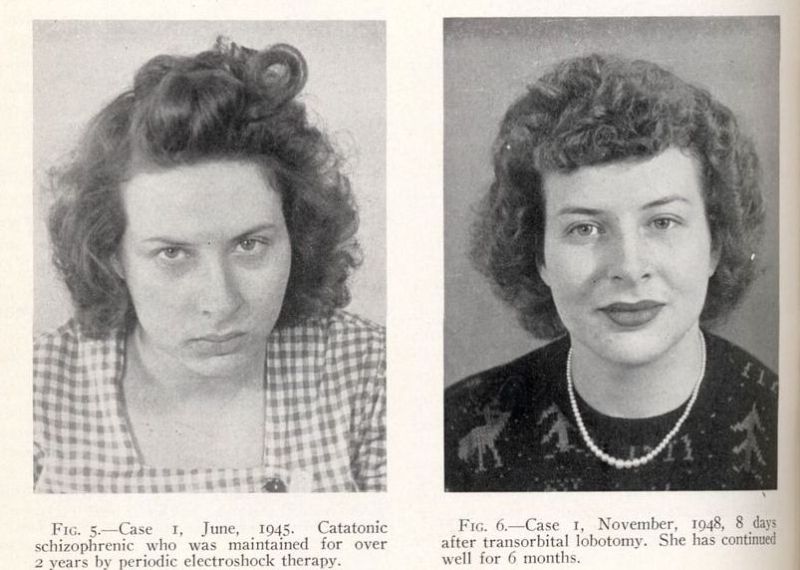 At the time, this first operation was considered a success, since there appeared to be a reduction in the symptoms of severe paranoia and anxiety that the patient had suffered prior to the surgery. Moniz and Lima subsequently performed the operation on a small subset of patients, refining the procedure as they went.
At the time, this first operation was considered a success, since there appeared to be a reduction in the symptoms of severe paranoia and anxiety that the patient had suffered prior to the surgery. Moniz and Lima subsequently performed the operation on a small subset of patients, refining the procedure as they went.
Moniz created an instrument called a leukotome (leucotome), designed specifically to disrupt the tracts of neuronal fibres connecting the prefrontal cortex and thalamus of the brain. Moniz and Lima operated on nearly 40 patients by 1937; however, the results were mixed, with some patients improving, others showing no change in symptoms, and still others relapsing. Despite this, the practice was soon widely adopted, largely because there were few other therapeutic measures available at the time for quieting chronically agitated, delusional, self-destructive, or violent patients.
The prefrontal leukotomy procedure developed by Moniz and Lima was modified in 1936 by American neurologists Walter J. Freeman II and James W. Watts. Freeman preferred the use of the term lobotomy and therefore renamed the procedure “prefrontal lobotomy.” The American team soon developed the Freeman-Watts standard lobotomy, which laid out an exact protocol for how a leukotome (in this case, a spatula) was to be inserted and manipulated during the surgery.
Freeman II and James W. Watts. Freeman preferred the use of the term lobotomy and therefore renamed the procedure “prefrontal lobotomy.” The American team soon developed the Freeman-Watts standard lobotomy, which laid out an exact protocol for how a leukotome (in this case, a spatula) was to be inserted and manipulated during the surgery.
Get a Britannica Premium subscription and gain access to exclusive content. Subscribe Now
The use of lobotomy in the United States was resisted and criticized heavily by American neurosurgeons. However, because Freeman managed to promote the success of the surgery through the media, lobotomy became touted as a miracle procedure, capturing the attention of the public and leading to an overwhelming demand for the operation. In 1945 Freeman streamlined the procedure, replacing it with transorbital lobotomy, in which a picklike instrument was forced through the back of the eye sockets to pierce the thin bone that separates the eye sockets from the frontal lobes. The pick’s point was then inserted into the frontal lobe and used to sever connections in the brain (presumably between the prefrontal cortex and thalamus). In 1946 Freeman performed this procedure for the first time on a patient, who was subdued prior to the operation with electroshock treatment.
The pick’s point was then inserted into the frontal lobe and used to sever connections in the brain (presumably between the prefrontal cortex and thalamus). In 1946 Freeman performed this procedure for the first time on a patient, who was subdued prior to the operation with electroshock treatment.
The transorbital lobotomy procedure, which Freeman performed very quickly, sometimes in less than 10 minutes, was used on many patients with relatively minor mental disorders that Freeman believed did not warrant traditional lobotomy surgery, in which the skull itself was opened. A large proportion of such lobotomized patients exhibited reduced tension or agitation, but many also showed other effects, such as apathy, passivity, lack of initiative, poor ability to concentrate, and a generally decreased depth and intensity of their emotional response to life. Some died as a result of the procedure. However, those effects were not widely reported in the 1940s, and at that time the long-term effects were largely unknown. Because the procedure met with seemingly widespread success, Moniz was awarded the 1949 Nobel Prize for Physiology or Medicine (along with Swiss physiologist Walter Rudolf Hess).
Because the procedure met with seemingly widespread success, Moniz was awarded the 1949 Nobel Prize for Physiology or Medicine (along with Swiss physiologist Walter Rudolf Hess).
Lobotomies were performed on a wide scale during the 1940s; Freeman himself performed or supervised more than 3,500 lobotomies by the late 1960s. The practice gradually fell out of favour beginning in the mid-1950s, when antipsychotics, antidepressants, and other medications that were much more effective in treating and alleviating the distress of mentally disturbed patients came into use. Today lobotomy is rarely performed; however, shock therapy and psychosurgery (the surgical removal of specific regions of the brain) occasionally are used to treat patients whose symptoms have resisted all other treatments.
The Editors of Encyclopaedia BritannicaThis article was most recently revised and updated by Amy Tikkanen.
consequences of brain lobotomy, history of brain lobotomy operation
Gleb Pospelovo lobotomy - the most famous and darkest of psychosurgical operations
- Oh, yes, after treatment, he will turn into a vegetable! to persuade the patient and his relatives to hospitalization. Everyone knows that in psychiatric hospitals people are "zombified", "burned out the brain", "poisoned", "turned into a plant" - in general, they destroy as a person in all possible ways. nine0003
Everyone knows that in psychiatric hospitals people are "zombified", "burned out the brain", "poisoned", "turned into a plant" - in general, they destroy as a person in all possible ways. nine0003
And before the hospital, the patient was just a feast for the eyes, aha!
Actually, this way of thinking has a very scientific name: social stigmatization. In fact, a person who is discharged from a psychiatric hospital is often completely different from what his relatives are used to. Was sociable - became withdrawn, was active, nimble - became inhibited and lethargic. And the media, books, cinema - willingly show exactly how pests in white coats carry out their hellish experiments on people. I will tell you a "secret": if anything turns our patients into "plants", it is not a cure, but a disease. However, this was not always the case…
Do you remember the famous book (or its adaptation) One Flew Over the Cuckoo's Nest and the fate of its main character, McMurphy? Let me remind you: McMurphy was subjected to a lobotomy for violations of the hospital regime. Cheerful, self-confident, groovy rogue-simulant turns into a weak-minded, into a drooling ruin. The author of the novel, Ken Kesey, who worked as an orderly in a mental hospital, described the "frontal syndrome" or "frontal lobe syndrome" that developed in people after lobotomy surgery.
Cheerful, self-confident, groovy rogue-simulant turns into a weak-minded, into a drooling ruin. The author of the novel, Ken Kesey, who worked as an orderly in a mental hospital, described the "frontal syndrome" or "frontal lobe syndrome" that developed in people after lobotomy surgery.
A bold idea
Brain lobotomy was developed in 1935 by the Portuguese psychiatrist and neurosurgeon Egas Moniz. In 1935, at a conference, he heard a report on the consequences of damage to the prefrontal zone in chimpanzees. Although the focus of this report was on learning difficulties associated with damage to the frontal lobes, Moniz was particularly interested in how one monkey became calmer and more docile after surgery. He hypothesized that the intersection of nerve fibers in the frontal lobe can help in the treatment of mental disorders, in particular - schizophrenia (the nature of which was still very vaguely understood). Moniz believed that the procedure was indicated for patients in serious condition or those whom aggressiveness made socially dangerous. Moniz performed his first operation at 1936 year. He called it "leukotomy": a loop was inserted into the brain with the help of a guide, and the white matter of the neuronal connections connecting the frontal lobes with other parts of the brain was cut through with rotational movements.
Moniz performed his first operation at 1936 year. He called it "leukotomy": a loop was inserted into the brain with the help of a guide, and the white matter of the neuronal connections connecting the frontal lobes with other parts of the brain was cut through with rotational movements.
Prefrontal lobotomy, or leucotomy (from other Greek λοβός — share and τομή — cut), — brain surgery, in which a dissection of the white matter of the frontal lobes of the brain is performed on one or both sides, separation of the cortex from the lower parts of the brain. The consequence of such an intervention is the exclusion of the influence of the frontal lobes of the brain on the rest of the structures of the central nervous system. nine0003
Moniz performed about a hundred of these operations and observed patients. He liked the results, and in 1936 the Portuguese published the results of the surgical treatment of twenty of his first patients: seven of them recovered, seven improved, and six showed no positive dynamics.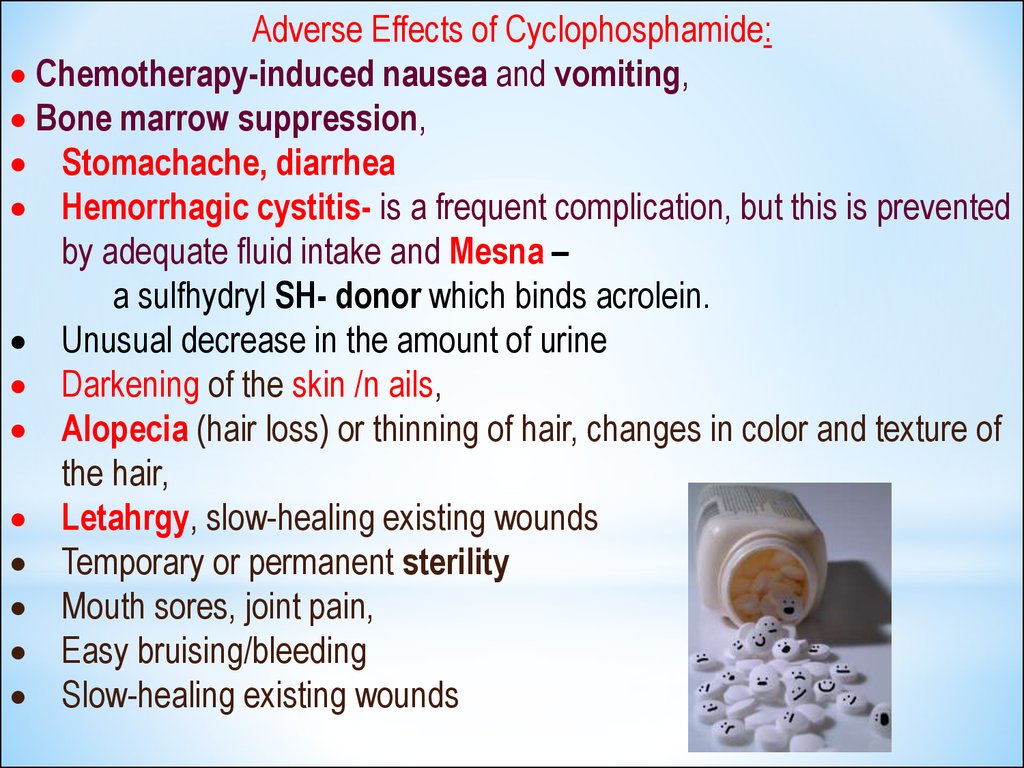
Egas Moniz was awarded the Nobel Prize in Physiology or Medicine in 1949 "for his discovery of the therapeutic effects of leucotomy in certain mental illnesses". Since the Monish Prize, leucotomy has become more widely used. nine0003
So, Egas Moniz, in his “lobotomy” practice, observed hardly two dozen patients; he never saw most of the others after the operation. Moniz has written several articles and books on lobotomy. Criticism followed: opponents argued that the changes after the operation most of all resemble the consequences of a brain injury and, in fact, represent a degradation of the personality. Many believed that brain mutilation could not improve brain function and damage could lead to the development of meningitis, epilepsy, and brain abscesses. Despite this, Moniz's report (Prefrontal leucotomy. Surgical treatment of certain psychoses, Torino, 1937) led to rapid adoption of the procedure on an experimental basis by individual clinicians in Brazil, Cuba, Italy, Romania, and the United States.
In the Land of Opportunity
American psychiatrist Walter Jay Freeman became the leading promoter of this operation. He developed a new technique that did not require drilling of the patient's skull and called it "transorbital lobotomy". Freeman aimed the narrow end of a surgical instrument, resembling an ice pick, at the eye socket bone, pierced a thin layer of bone with a surgical hammer, and inserted the instrument into the brain. After that, the fibers of the frontal lobes of the brain were cut with the movement of the knife handle. Freeman argued that the procedure would remove the emotional component from the patient's "mental illness". The first operations were carried out with a real ice pick. Subsequently, Freeman developed special instruments for this purpose - the leukotome, and then the orbitoclast. nine0003
In the 1940s, lobotomy in the United States became more common for purely economic reasons: the "cheap" method allowed the "treatment" of many thousands of Americans held in closed psychiatric institutions, and could reduce the costs of these institutions by a million dollars a day ! Leading newspapers wrote about the successes of the lobotomy, drawing public attention to it.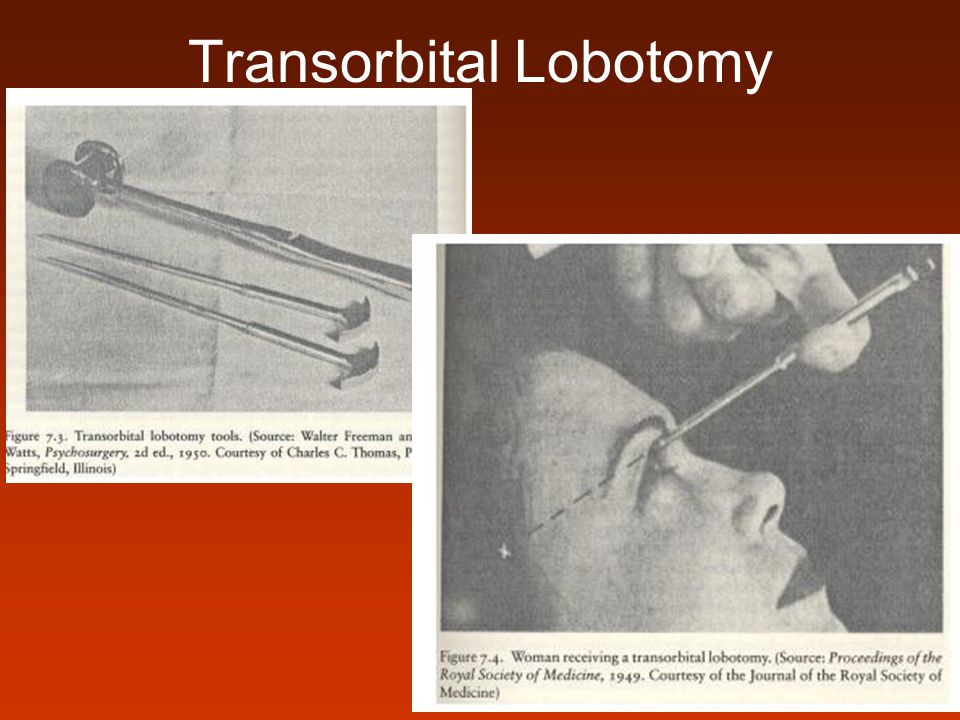 It is worth noting that at that time there were no effective methods of treating mental disorders, and cases of returning patients from closed institutions to the community were extremely rare. nine0003
It is worth noting that at that time there were no effective methods of treating mental disorders, and cases of returning patients from closed institutions to the community were extremely rare. nine0003
In the early 1950s, about five thousand lobotomies were performed in the United States a year. Between 1936 and the late 1950s, between 40,000 and 50,000 Americans were lobotomized. The indications were not only schizophrenia, but also severe obsessive-compulsive disorder. Lobotomy was often performed by doctors who had no surgical training. Although not trained as a surgeon, Freeman nevertheless performed about 3,500 of these operations, traveling around the country in his own van, which he called the "lobotomobile".
Lobotomy was widely used not only in the USA, but also in other countries of the world - Great Britain, Finland, Norway, Sweden, Denmark, Japan, the USSR. In European countries, tens of thousands of patients underwent this operation
The result on the face
Already in the late 40s, psychiatrists "saw" that the first studies of lobotomy were carried out without a solid methodology: they operated with incomparable methods on patients with different diagnoses.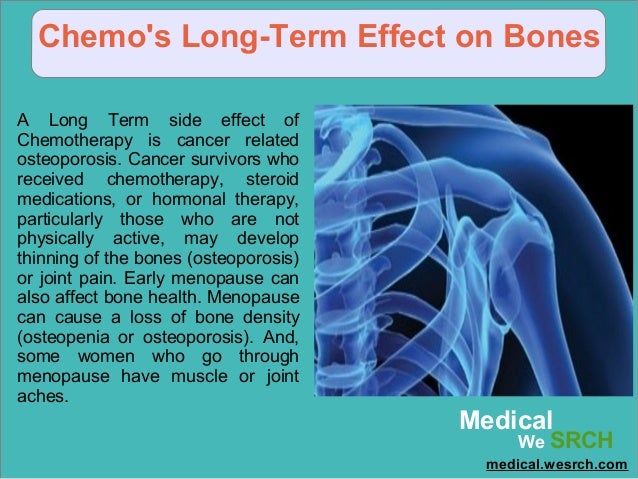 Whether or not recovery has occurred is a question that has often been decided on the basis of such a criterion as improving the patient's manageability. At 19In the 1950s, more thorough research revealed that, in addition to death, which was observed in 1.5–6% of those operated on, lobotomy can cause seizures, large weight gain, loss of coordination, partial paralysis, urinary incontinence and other problems. Standard tests of intelligence and memory usually did not show any significant deterioration. Patients retained all types of sensitivity and motor activity, they did not experience impairments in recognition, practical skills and speech, but complex forms of mental activity disintegrated. More subtle changes have often been reported in the form of reduced self-control, foresight, creativity, and spontaneous action; selfishness and lack of concern for others. At the same time, criticism of one's own behavior was significantly reduced. nine0003
Whether or not recovery has occurred is a question that has often been decided on the basis of such a criterion as improving the patient's manageability. At 19In the 1950s, more thorough research revealed that, in addition to death, which was observed in 1.5–6% of those operated on, lobotomy can cause seizures, large weight gain, loss of coordination, partial paralysis, urinary incontinence and other problems. Standard tests of intelligence and memory usually did not show any significant deterioration. Patients retained all types of sensitivity and motor activity, they did not experience impairments in recognition, practical skills and speech, but complex forms of mental activity disintegrated. More subtle changes have often been reported in the form of reduced self-control, foresight, creativity, and spontaneous action; selfishness and lack of concern for others. At the same time, criticism of one's own behavior was significantly reduced. nine0003
Patients could answer ordinary questions or perform habitual actions, but the performance of any complex, meaningful and purposeful acts became impossible. They stopped experiencing their failures, experiencing hesitation, conflicts, and most often were in a state of indifference or euphoria. People who were previously energetic, restless, or aggressive in nature may develop changes towards impulsiveness, rudeness, emotional breakdowns, primitive humor, and unreasonable ambitions. nine0003
They stopped experiencing their failures, experiencing hesitation, conflicts, and most often were in a state of indifference or euphoria. People who were previously energetic, restless, or aggressive in nature may develop changes towards impulsiveness, rudeness, emotional breakdowns, primitive humor, and unreasonable ambitions. nine0003
In the USSR, special techniques for performing lobotomy were developed - much more accurate in the surgical sense and sparing in relation to the patient. The surgical method was offered only in cases of failure of long-term treatment, which included insulin therapy and electroshock. All patients underwent a general clinical and neurological examination and were carefully studied by psychiatrists. After the operation, both acquisitions in the emotional sphere, behavior and social adequacy, as well as possible losses, were recorded. The lobotomy method itself was recognized as fundamentally acceptable, but only in the hands of experienced neurosurgeons and in cases where the lesion was recognized as irreversible.
nine0003
With maintenance therapy with nootropics and drugs that correct mental disorders, a significant improvement in the condition was possible, which could last for several years, but the end result still remained unpredictable. As Freeman himself noted, after hundreds of operations performed by him, about a quarter of patients were left to live with the intellectual capabilities of a pet, but "we are quite satisfied with these people ...".
Beginning of end
The decline of lobotomy began in the 1950s after serious neurological complications of the operation became apparent. In the future, lobotomy was prohibited by law in many countries - data have accumulated about the relatively low effectiveness of the operation and its greater danger compared to antipsychotics, which were becoming more and more perfect and actively introduced into psychiatric practice.
In the early 70s, the lobotomy gradually faded away, but in some countries continued to operate until the end of the 80s. In France between 19Between 80 and 1986, 32 lobotomies were performed, during the same period - 70 in Belgium and about 15 at the Massachusetts Hospital; about 15 operations were performed annually in the UK.
In France between 19Between 80 and 1986, 32 lobotomies were performed, during the same period - 70 in Belgium and about 15 at the Massachusetts Hospital; about 15 operations were performed annually in the UK.
In the USSR, lobotomy was officially banned in 1950. And this was not only an ideological underpinning. In the foreground were reasons of a purely scientific nature: the absence of a strictly substantiated theory of lobotomy; lack of strictly developed clinical indications for surgery; severe neurological and mental consequences of the operation, in particular "frontal defect". nine0003
“Lobotomy” with a bullet
More than 60 years have passed since the ban on lobotomy in our country. But people continue to get head injuries, get sick with various ailments (Peak's disease, for example), leading to a completely distinct "frontal" symptomatology. I will give a vivid observation of the consequences of the “frontal syndrome” from my own practice.
Two soldiers at the firing range, laughing, began pointing machine guns loaded with live ammunition at each other and shouting something like “Tra-ta-ta!..”. Suddenly he said his "word" and the machine gun ... The result - one had a bullet in the head. The neurosurgeons somehow managed to revive and repair the guy; they inserted several plates into his skull and sent him to us to resolve the issue of further treatment and disability. nine0003
During the conversation, the patient made a strange impression. Formally, his mind was not affected, his memory and stock of knowledge were at a normal level; he behaved quite adequately too — at first glance... An unnatural calmness, up to indifference, was striking; the guy indifferently talked about the injury, as if it did not happen to him; made no plans for the future. In the department he was absolutely passive, subordinating; for the most part, he lay on the bed. They invited me to play chess or backgammon, asked me to help the staff - I agreed. Sometimes it seemed - order him to jump out the window - he will do so, and without hesitation. nine0003
Sometimes it seemed - order him to jump out the window - he will do so, and without hesitation. nine0003
And we received an answer to our questions a week later, when the patient was “caught up” with documents from neurosurgery, where his injury was treated. The surgeons described that the wound channel passed right through the frontal lobes of the guy. After that, all questions about the patient's behavior were removed for us.
By the will of fate, I happened to meet this patient again, almost ten years after we met. It happened in a rehabilitation center where I worked as a consultant. The guy has changed little in appearance. In communication appeared sharpness, rudeness; mental faculties were completely preserved. I did not notice the main thing: self-confidence and independence. The man had empty eyes... In life, he "went with the flow", completely indifferent to what was happening around him. nine0003
In conclusion, as before, I would like to wish: take care of yourself and your loved ones and remember that in most cases even severe and painful treatment is worth defeating a disease that deprives a person of his human appearance.
Nothing better came to mind
Now lobotomy seems to be an attribute of horror films: a crazy villain doctor, armed with thin bayonets and a hammer, punches holes in the skulls of his victims, turning them into obedient zombies. More than 70 years ago, however, this operation was used with might and main in psychiatry: in some countries, lobotomy was prescribed for almost a mild form of anxiety disorder, and the Nobel Prize in Physiology or Medicine was even awarded for the development of the first method of its implementation. About why doctors needed to drill holes in the skulls of patients and whether it really helped, as well as how the Soviet lobotomy differed from the world one, we tell in our material. nine0003
In 1949, the Nobel Prize in Literature (with the wording "for his significant and artistically unique contribution to the development of the modern American novel") was awarded to the American writer William Faulkner. The prize in physics went to the Japanese Hideki Yukawa for predicting the existence of mesons, particles that carry the interaction between protons or neutrons, and in the field of chemistry, William Jioka was noted for his experiments with record-breaking low temperatures.
The prize in physics went to the Japanese Hideki Yukawa for predicting the existence of mesons, particles that carry the interaction between protons or neutrons, and in the field of chemistry, William Jioka was noted for his experiments with record-breaking low temperatures.
The Prize in Physiology or Medicine was shared by two scientists: the Swiss Walter Hess for describing the role of the diencephalon in regulating the functioning of internal organs, and the Portuguese António Egas Moniz for the method of surgical treatment of mental disorders that he developed a few years earlier - leucotomy, better known like a lobotomy. nine0003
By the time Moniz was presented with the award, the number of lobotomies performed around the world had exceeded several tens of thousands and was growing at a fast pace: most of the operations were carried out in the USA, followed by the UK, followed by the Scandinavian countries.
In total, until the 1980s (the last time France banned this operation), about a hundred thousand lobotomies were performed in the world, and not all of them were without irreparable consequences.
Bur and ethanol
The fact that such a terrible surgical operation was noted by the Nobel Committee, now it may seem at least strange. However, it should be borne in mind that at the beginning of the 20th century, diagnostic psychiatry developed very rapidly: doctors found schizophrenia, depression, and anxiety disorders in their patients and did this in much the same way as modern psychiatrists do now.
But it was still far from the medical treatment and prevention of mental disorders: the first antidepressants and antipsychotics appeared on the market only in the middle of the century, and a very life-threatening substance was already recognized in the then popular panacea - opiates. nine0003
Psychotherapy, as well as the then popular psychoanalysis, often did not help, especially in severe cases, and there were a lot of patients in psychiatric clinics. They were treated mainly with shock therapy - but even that often did not bring relief.
In turn, doctors of the early 20th century considered surgery to be almost a universal method of treatment (at least for serious illnesses). Post-mortem autopsies conducted hundreds of years earlier had told enough about the human body to know what to cut and where, and the death rate from surgery had already declined. nine0003
Post-mortem autopsies conducted hundreds of years earlier had told enough about the human body to know what to cut and where, and the death rate from surgery had already declined. nine0003
Physicians were also sure that they were relatively well versed in the workings of the brain. So, Monish, developing the method of leucotomy, was inspired by the work of the American physiologist John Fulton.
In the 1930s, Fulton was studying the function and structure of the primate brain and, in one of his experiments, noted that surgical damage to the white matter fibers of the frontal lobes had a calming effect: one of his subjects, the irascible and untrainable chimpanzee Becky, after surgery became calm and relaxed. nine0003
In principle, the ideas of Fulton, borrowed by Moniz, are correct: the frontal lobes do take part in the cognitive control necessary for the normal functioning of the psyche, and their connection with other parts of the brain - those that lie a little deeper and are responsible for emotional cognition - is in development mental disorders play an important role.
The problem is that no one really understood this role then (now things are a little better, but still not perfect), but Moniz, inspired by experiments on chimpanzees, thought that success could be achieved on humans. Despite Fulton's skepticism about this, the future Nobel laureate performed his first lobotomy (or rather, prefrontal leukotomy) at 1935 year.
Moniz himself, who suffered from gout, did not take the instruments: the operation was performed by his colleague, the neurosurgeon Almeida Lima. The first patient to survive a lobotomy was a 63-year-old woman who suffered from depression and anxiety.
Lima drilled a hole in the frontal part of the skull with a medical drill and filled the area separating the frontal lobes from the rest of the brain with ethyl alcohol: Moniz assumed that ethanol would create a barrier that would ensure the success of the procedure.
The operation was successful, and the doctors subjected seven more patients to the same procedure: in addition to depression and anxiety, the list of indications for it included, in addition to depression and anxiety, schizophrenia and manic-depressive disorder (it is also bipolar disorder). After that, Moniz and Lima modified the procedure: instead of injecting ethanol into the brain, they introduced a cannula with a hook-tip into the frontal lobes, with which small parts of tissue were removed. The operation was performed on another 12 patients, and if the results did not satisfy them, Moniz and Lima could perform it again. nine0003
After that, Moniz and Lima modified the procedure: instead of injecting ethanol into the brain, they introduced a cannula with a hook-tip into the frontal lobes, with which small parts of tissue were removed. The operation was performed on another 12 patients, and if the results did not satisfy them, Moniz and Lima could perform it again. nine0003
In total, 20 patients were included in the "first wave" of lobotomy: 12 women and 8 men aged 22 to 67 years. In seven of them, Moniz noted significant improvements, in seven more insignificant ones, and the condition of six did not change at all.
At the same time, Moniz himself claimed, all the lobotomies performed by Lima did not have irreparable consequences: the patients remained capable, and among the side effects were only nausea, dizziness, slight incontinence and apathy.
Unlike Moniz, not all of his colleagues were optimistic about the results: the painfully manifested side effects resembled the symptoms of severe traumatic brain injuries. nine0003
nine0003
In addition, some physiologists have noted a significant impact of the operation on the very personality of the patient. In their opinion, the ability of the operation to stop the symptoms of mental disorders seemed to be unimportant compared to the fact that the person simply ceased to be himself.
Despite this, after the “success” of Moniz and Lima, lobotomy began to quickly gain popularity among psychiatrists around the world, and medical companies even launched and widely advertised rather frightening-looking leukotomes - instruments for performing the operation. nine0003
Meanwhile in the USSR
Of course, Soviet psychiatrists did not deprive the attention of the popular operation in the West, but they approached the matter much more seriously and responsibly.
The Soviet neurosurgeon and academician Boris Grigoryevich Egorov became the main ideologist of lobotomy in the USSR. The justification for lobotomy in Soviet psychiatry was that the separation of the frontal lobes of the brain from the subcortical zones should weaken the influence of deep structures (for example, the thalamus or the amygdala, which are responsible for the primary regulation of behavior and emotions) on the prefrontal cortex of the brain, and vice versa. nine0003
nine0003
Having rightly decided that it was not advisable to perform such an operation blindly, Egorov modified the method: in the Soviet Union, a lobotomy was performed with a craniotomy - on the open brain, which made the process much more meaningful than with Western colleagues. The indications for the operation were also rather limited: lobotomy was prescribed only for severe forms of schizophrenia in cases where no other treatment common then helped.
After the first successes (improvements were observed in 60 percent of those operated on, and 20 percent became fully capable at all), the operation began to be performed more often. nine0003
Soviet surgeons, however, rather quickly encountered the same problems as their Western colleagues: the operation, even with improved methods of its implementation, was still poorly substantiated theoretically, and also often led to irreparable consequences, such as complete or partial paralysis and other forms of disability.
In addition, lobotomy worked for only one form of schizophrenia, paranoid, and was not as effective in other cases, although it was still prescribed. As a result for 19In the 1940s, only a few hundred patients underwent lobotomy in the USSR.
As a result for 19In the 1940s, only a few hundred patients underwent lobotomy in the USSR.
Fortunately, the Soviet medical authorities recognized the danger of lobotomy very quickly: already in 1950, when the number of operations around the world exceeded several tens of thousands a year, by decree of the Academic Medical Council of the USSR Ministry of Health, decree No. 1003 was signed, prohibiting frontal leucotomy.
President's sister
Despite the fact that Moniz received the Nobel Prize for the development of the lobotomy method, the name of another scientist, American Walter Freeman, is more famous in the sad story of this operation. nine0003
In December 1942, Freeman and his colleague, the neurosurgeon James Watts, published a detailed report on 136 lobotomies performed on psychiatric patients with schizophrenia, depression, mania, and schizotypal disorders.
Of all the patients on the operating table, three died, and eight more died shortly after the operation. In the vast majority - 98 people - Freeman noted significant improvements. He described in vivid colors how the new operation improved the lives of his patients, how they became happier and healthier, and also expressed gratitude to their savior. nine0003
In the vast majority - 98 people - Freeman noted significant improvements. He described in vivid colors how the new operation improved the lives of his patients, how they became happier and healthier, and also expressed gratitude to their savior. nine0003
However, not everything was so colorful: at the hands of Freeman and Watts, for example, perhaps the most famous victim of a lobotomy, the younger sister of the 35th US President John F. Kennedy, Rosemary, suffered.
By the age of 23, the girl spoke and read very poorly, was infantile and quick-tempered, because of which (basically, according to her father) she did not correspond to the other seven - extremely talented - brothers and sisters. In fact, Rosemary Kennedy had developmental delays - certainly limiting, but not canceling a normal daily life. nine0003
At her father's insistence, Rosemary underwent a lobotomy - even though there were no clear indications such as schizophrenia, anxiety disorder or depression (Freeman gave the latter to the girl retroactively - so that there would still be indications for the operation in prison).
Despite the fact that the procedure went according to plan (like any other brain surgery, the lobotomy was performed under local anesthesia, keeping the patient conscious and forcing him to talk), it ended extremely unsuccessfully. Rosemary Kennedy's intelligence level has declined even further (estimated to the level of a two-year-old child), in addition, she has forgotten how to walk and use her hands. nine0003
The older Kennedy couple placed Rosemary in a private psychiatric hospital, where they began to teach her to walk again. The patient's condition, however, did not improve much: Kennedy's eldest daughter spent the rest of her life in the clinic and died of natural causes at the age of 86.
Similar cases, however, did not stop Freeman: after the report published in 1942, he continued to perform lobotomies, and in 1948 he decided to improve and speed up the method of performing the operation - and in a rather radical and frightening way. nine0003
Ice pick
In 1948, Freeman, who, by the way, had practically no surgical training, began to experiment with deep lobotomy - he believed that for greater effectiveness it was necessary to penetrate further into the brain. The leukotomes used during the operation sometimes broke right in the patient’s head, so Freeman once used an ice pick: he plunged it first into one, then into the other eye socket of the patient at an angle so as to penetrate the frontal lobes. nine0003
The leukotomes used during the operation sometimes broke right in the patient’s head, so Freeman once used an ice pick: he plunged it first into one, then into the other eye socket of the patient at an angle so as to penetrate the frontal lobes. nine0003
So Freeman developed another lobotomy device, the orbitoclast. In fact, it was the same ice pick, inserted into the eye socket with hammer blows. Lobotomy using an orbitoclast did not require opening the skull with a drill and, in fact, was carried out almost completely blindly: only the angle of insertion of the instrument and the depth could be adjusted.
Of course, the orbitoclast made lobotomy much more dangerous, but at the same time more popular. Due to the fact that it became easier to perform the operation, it began to be prescribed and carried out much more often: from 1949 to 1952, five thousand frontal lobotomies were performed annually in the United States.
Freeman himself, of course, was at the head of the popularization of lobotomy. In 1950, he stopped working with James Watts, who was struck by the bloodthirstiness and danger of the "improved" method of lobotomy, and began to perform operations on his own, driving around the states in a "lobocar".
In 1950, he stopped working with James Watts, who was struck by the bloodthirstiness and danger of the "improved" method of lobotomy, and began to perform operations on his own, driving around the states in a "lobocar".
Freeman performed operations without gloves and a surgical mask, in almost any conditions. Absolutely confident in the effectiveness and safety of his method, he did not even pay attention to the frighteningly high mortality rate of his patients - 15 percent - and the fact that many became mentally and physically disabled after the operation. nine0003
Freeman's patients included 19 children, the youngest of whom was four years old at the time of the operation. The last time Freeman took an orbitoclast in his hands was in 1967: for his patient Helen Mortensen, it was the third and fatal lobotomy - the woman died of a cerebral hemorrhage during the procedure.
Freeman was removed from surgery and spent the last five years of his life after that, going around old patients and checking their condition.
Roulette on operating table
We can say that the lobotomy still had a certain potential. The work of the brain as a whole system is supported by a huge number of connections within it. These connections are responsible for the activity of the whole organism as a whole: for the recognition of visual images, the performance of automatic movements, the fine work of the hands, and so on.
They are also responsible for the formation of mental disorders, and in order to combat these disorders, it is precisely with the connections in the brain that it is necessary to work first of all. nine0003
The problem is that from the point of view of functional connections, the brain at the time of the rapid development of psychosurgery in general (and lobotomy in particular) was a black box. However, he still remains. The irreparable consequences of a lobotomy, such as paralysis, are not surprising - and inevitable even in cases where not an instrument that would be more suitable for a bartender than a doctor was used, but sterilized medical devices and the latest methods at that time.