Sex therapy cost
How Does Sex Therapy Work?
Skip to contentPublished: March 23, 2022 Updated: October 18, 2022
Published: 03/23/2022 Updated: 10/18/2022
Sex therapy is an effective way to achieve satisfaction in your sex life. Seeking consultation with a credentialed and knowledgeable provider can help both couples and individuals address common sexual concerns. Typical rates for a certified sex therapist are on the upper end of private pay therapy rates in your area, and treatment can last anywhere from a few sessions to a few years, depending on the issues being addressed.
What Is Sex Therapy?
Sex therapy affirms the fundamental value of sexuality as an inherent, essential, and beneficial dimension of being human. Sex therapists use a non-pathologizing approach, emphasizing sexual freedom of thoughts, feelings, fantasies and healthy modes of sexual activity. Sex therapy allows clients to consider (often for the first time) what their sexual experience has been like over their lifespan, what their sexual experience is currently like and what priorities they have for sexual expression in the future.
Therapeutic goals are established by the client in areas of their sex life that cause them difficulty or dissatisfaction, whether that be through internal thought patterns or outward expression. These goals are often addressed in tandem with other therapeutic topics typical to counseling, such as a sexless marriage or relationship, conflict in the relationship, stress, sexual trauma, anxiety, or depression.
You Keep Your Clothes On When You Work With a Sex Therapist
Sex therapy will never include sexual contact with your therapist. Sex therapy is NOT sex surrogacy or a euphemism for sex work of any kind.
Talkspace (Online Therapy For Individuals & Couples)
In couples counseling, you can work together on improving communication, building trust, and resolving conflict. Also, you can work on making sex more enjoyable and fulfilling. Talkspace works with several major insurers including Optum, Cigna, Aetna, and UnitedHealthCare. Check Your Insurance Eligibility
Choosing Therapy partners with leading mental health companies and is compensated for referrals by Talkspace.
Try Talkspace
What Can Sex Therapy Help With?
Sex therapy addresses a wide array of sexual concerns that impact both individuals and relationships. Topics include issues with arousal, frequency, sexual pain, difficulty achieving orgasm, out of control sexual behavior, physiological shifts after childbirth or menopause and changes in the sexual dynamic of a couple over time.
When sexual issues cause distress, a sex therapist can help discern what physiological factors to rule out (or refer to other providers for treatment) and what psychological factors can be examined and addressed. Sex therapists typically work closely with general practitioners, psychiatrists, physical therapists, gynecologists and urologists so that a coordination of care can provide the best treatment.
Stress, Anxiety, & Big Life Changes
Common stressors and phase-of-life shifts tend to precipitate the issues presented in a sex therapist’s office. Knowing what these factors are can be helpful in deciding whether sex therapy is the right choice for you or for your relationship.
Knowing what these factors are can be helpful in deciding whether sex therapy is the right choice for you or for your relationship.
Stress-inducing factors to look out for include:
- Anxiety
- Depression
- First sexual experience
- History of sexual trauma or other forms of trauma
- History of sex negativity or shame around sex
- Gender fluidity or transition
- Lack of education/information about healthy sexual practices
- STIs
- Disability/illness/medical issues
- Marriage/cohabitation
- Childbirth/child rearing
- Stressful job requirements
- Divorce
- Change in sexual partner(s)
- Aging/perimenopause/menopause
Sex therapy can help mitigate how much impact these factors have on a satisfying sex life. A sex therapist will help identify what the issue is, what physiological components to address, what structural changes can be made and what psychological processes are contributing to the problem.
Sexual Distress
Topics that clients report experiencing distress about include:
- Not having enough sex, as a couple or individually
- Wanting sex more or less frequently than their partner(s)
- Lack of interest in sex
- Pain or discomfort when having sex
- Inability to get aroused or stay aroused
- Inability to have an orgasm
- Having an orgasm too quickly
- Misalignment between gender identity and biological sex/genitalia
- Having intrusive or disturbing thoughts about sex
- Masturbating or having sex compulsively
- Desire to expand the range of sexual experience, as a couple or individually
- Physical Sexual Problems
In addition to these common problems, clients may have received a medical diagnosis from a doctor or believe a medical diagnosis may be relevant to their situation.
Diagnosable psychological and physiological issues that are relevant to treatment by a sex therapist include:1
- Premature Ejaculation/Early Ejaculation
- Delayed Ejaculation
- Erectile Disorder/Erectile Dysfunction
- Vestibulodynia/Genito-Pelvic Pain Disorder
- Anorgasmia/Female Orgasmic Disorder
- Male Hypoactive Sexual Desire Disorder
- Female Sexual Arousal Disorder
- Gender Dysphoria
- Substance/Medication Induced Sexual Dysfunction
- Unspecified Sexual Dysfunction
Do My Partner and I Need to See a Sex Therapist?
If you’re on the fence about sex therapy, consider how your sex life is now versus how you want it to be. If there are specific issues holding you back, a sex therapist can likely help you address them and make appropriate changes to move forward.
If there are specific issues holding you back, a sex therapist can likely help you address them and make appropriate changes to move forward.
There are a number of issues that a sex therapist can help with, including:
- Dealing with and addressing pain with intercourse, including physical pain vs. psychosomatic pain
- Dealing with trauma from your past including sexual contact or penetration
- Uncovering your true libidos as individuals in a relationship
- Discovering or wanting to explore your gender identity and sexual orientation
- Learning how to navigate open relationships
- Addressing issues of shame related to sex and sexuality
What Does a Sex Therapist Do During Sessions?
Sex therapists come from a wide range of backgrounds and employ techniques unique to their own therapeutic style. However, there are a few standard components to sex therapy that are widely regarded for their efficacy and which you are likely to experience in treatment with most sex therapists.
Mindfulness
A sex therapist may help you utilize mindfulness practices, a category of tools which has been studied and proven to be effective when used to address sexual dysfunction. Mindfulness as applied to sex therapy, in the words of Lori Brotto PhD, is “the practice of noticing what is happening inside us and of being kind to ourselves, even when we struggle to do so.”3 Mindfulness improves nonjudgmental attention, one of the precursors to satisfying sex.
Sensate Focus
One type of mindfulness technique, if you are in sex therapy with a partner or partners, is Sensate Focus. Sensate focus exercises are used to reduce anxiety around sexual interactions by slowing down the process of intimacy.4 Partners are directed to incrementally explore basic touch sensations over a series of weeks, dismantling the habitual ways in which they have engaged in physical touch and sexual interaction in the past. The goal is to cultivate awareness around touch and arousal in order to foster a positive feedback loop that increases desire and connection.
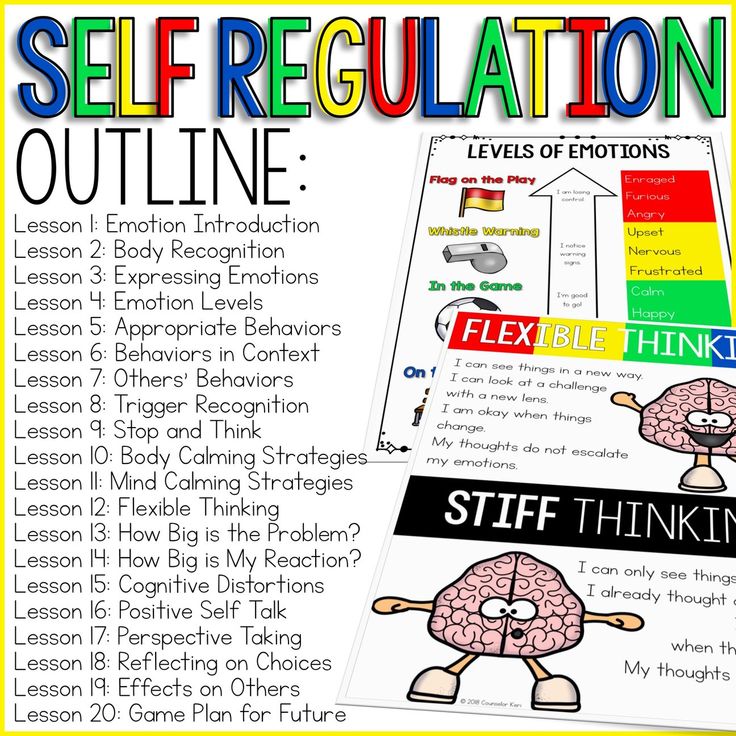
Sex Therapy Exercises & Homework
Homework often starts with communication and being able to be vulnerable with one another. Your sex therapist will work with you and your partner to come up with questions that can open up the lines of communication. The goal of these questions and exercises are to continue to build a foundation of safety and security when it comes to sexuality in the relationship.
Physical Issues Won’t Be Ignored in Sex Therapy
It is important to consider physical and medical issues that may be a barrier to a fulfilling sex life. There are various types of conditions such as endometriosis, fibroids, medications, and sexually transmitted infections (STIs) that can cause pain and difficulty with intercourse. Getting treatment for these or ruling out medical issues is a big step in getting a treatment plan for you and your partner.
Evaluate Intimate Dance
Another approach commonly utilized in partnered sex therapy is assessment of the Intimate Dance that partners engage in around sex. This includes how partners initiate sex, who tends to have a higher desire for sex, and what structural factors in the clients’ lives have contributed to an intimate dance that is no longer satisfying to one or more partners.
This includes how partners initiate sex, who tends to have a higher desire for sex, and what structural factors in the clients’ lives have contributed to an intimate dance that is no longer satisfying to one or more partners.
Dual Control Model
A sex therapist will often employ the Dual Control Model for sexuality in assessing a relationship’s intimate dance.5 The dual control model posits that the context in which our sexuality exists matters. Not only do we need to take a look at what turns us on and the mechanisms of our sexual excitation system, but also what turns us off, or our sexual inhibition system. Utilizing the lens of the dual control model, a sex therapist will help a couple make crucial changes in their intimate dance in order to reach a connected and contented equilibrium in sexual interactions.
Popular Choices For Online Therapy
BetterHelp (review) – World’s largest network of licensed therapists, starting at $60 per week. Get Matched With A Therapist
Get Matched With A Therapist
Online-Therapy.com (review) – Video and text based therapy starting at $5o per week. Learn More
Talkspace (review) – Well known online therapy service, endorsed by multiple celebrities. Try Talkspace
Choosing Therapy partners with leading mental health companies and is compensated for referrals by BetterHelp, Online-Therapy, and Talkspace.
Sex Therapy Examples
There are many reasons why an individual or a couple would seek out sex therapy. This section elaborates on some of the more common examples for why clients come to see a sex therapist and what the trajectory of their therapy might look like.
Infrequent Sex & Trouble Maintaining Erections
Angela and Tony have been married for 36 years. They have a loving partnership, but their sex life has dwindled to an infrequent pattern of sex once every 2 months. Their interactions tend to be brief and awkward. Tony has also begun to have difficulty maintaining an erection. If penetrative sex is unsuccessful, they usually stop their interaction. Both Tony and Angela would like to have more frequent and more satisfying sex.
Tony has also begun to have difficulty maintaining an erection. If penetrative sex is unsuccessful, they usually stop their interaction. Both Tony and Angela would like to have more frequent and more satisfying sex.
Their sex therapist refers Tony to a urologist specializing in sexual medicine to assess for any underlying medical issues for his erectile dysfunction. She then assesses the habits the couple has in initiating sex and asks them to dismantle their preconceived notions of what sex should look like. She has them create more space in their lives for sensual touch and quality time. She asks them to follow the Sensate Focus model to build a new kind of intimacy. After 8 months Angela and Tony report a higher frequency of sexual interactions and a higher satisfaction in their sex life. Tony is more able to maintain an erection and the couple also has an expanded sexual repertoire for when his erection dissipates.
Pain During Sex
Paul and Jessica have been in a relationship for 3 years. Their sex is not able to be penetrative or involve direct touch to Jessica’s vulva due to pain she experiences when touched. Jessica has never had a physically pleasurable experience or orgasm involving penetrative sex. Their sex therapist assesses Jessica for a history of sexual trauma. She then refers Jessica to a gynecologist and physical therapist specializing in pelvic pain.
Their sex is not able to be penetrative or involve direct touch to Jessica’s vulva due to pain she experiences when touched. Jessica has never had a physically pleasurable experience or orgasm involving penetrative sex. Their sex therapist assesses Jessica for a history of sexual trauma. She then refers Jessica to a gynecologist and physical therapist specializing in pelvic pain.
Jessica is diagnosed with vestibulodynia and is given dilators in conjunction with regular physical therapy. Their sex therapist addresses the anxiety cycle in the couple that has evolved as a repercussion of Jessica’s pain symptoms. She assigns mindfulness work for the couple to explore in order to reduce the anxiety and increase pleasure. After 14 months Jessica has made significant progress in being able to receive touch pleasurably from Paul and they are working toward penetrative sex.
Compulsive Masturbation
Sam is 27 years old and has never had a sexual relationship. He watches porn and masturbates 1-3 times a day and sometimes is late to work or misses social activities as a result. The frequency that Sam masturbates has escalated over the last year and he worries that his masturbation behavior has become compulsive and that he doesn’t have control over his life. Sam would like to limit the amount of focus he is giving to masturbation and would also like to explore more meaningful relationships.
The frequency that Sam masturbates has escalated over the last year and he worries that his masturbation behavior has become compulsive and that he doesn’t have control over his life. Sam would like to limit the amount of focus he is giving to masturbation and would also like to explore more meaningful relationships.
His sex therapist works with Sam to understand why his behavior has increased in frequency and feels outside his control. She explores how his childhood and family background may have made it difficult to form satisfying relationships. She helps Sam establish therapeutic goals for modified behavior and cultivate mindfulness practices to achieve those goals. After 11 months Sam has reduced the frequency of his masturbation. He feels less anxious, more confident and more in control of his own life. He is beginning to date someone he has developed feelings for and has experienced partnered sex for the first time.
Cost of Sex Therapy
Most sex therapists see individual clients for 45-60 minute sessions at rates between $120-$180 and relationships/couples for 75-90 minute sessions at rates between $190-$310. These rates may vary widely based on the availability of certified sex therapists in your area and on general mental health costs in your state.
These rates may vary widely based on the availability of certified sex therapists in your area and on general mental health costs in your state.
Insurance Coverage
You may be wondering if your insurance benefits can cover some or all of the cost of sex therapy. Insurance companies typically only offer mental health benefits when there is a diagnosable issue. Some sex therapy topics do indicate a billable diagnosis that most insurance companies will accept, such as female orgasmic disorder or delayed ejaculation. If that diagnosis is the primary reason for seeking therapy, your insurance company may cover the cost.
When seeking sex therapy as an individual, there may be a concurrent or contributing diagnosis, such as an anxiety disorder, which can be billed to insurance companies. In that instance, even if the sexual issues you are presenting with are not billable, your insurance provider may cover therapy.
One other factor to consider in seeking insurance coverage for sex therapy is whether you are required by your insurance provider to see an in-network practitioner. Many insurance companies do not have a certified sex therapist on their panel of providers. If that is the case for your geographical area, you may have only out-of-network reimbursement options.
Many insurance companies do not have a certified sex therapist on their panel of providers. If that is the case for your geographical area, you may have only out-of-network reimbursement options.
Alternatives for payment include utilizing your HSA or FSA accounts through your employee benefits, which typically can be used to see any mental health practitioner, including a certified sex therapist.
Where to Find the Right Sex Therapist for You
When seeking a sex therapist you want to make sure to find an adequately trained and certified provider. “Sex therapy” and “sex therapist” are not protected terms under any current state laws. What that means is that anyone can call themselves a sex therapist without having had the training to do so.
Be Picky When Looking for a Sex Therapist
Fortunately, the American Association of Sex Counselors, Educators and Therapists (AASECT) is a credible body of oversight which has been the gold standard in certification for sex therapy since 1967. With its history of impeccable standards for training, experience and ethical behavior, AASECT is increasingly recognized as the guardian of professional standards in sexual health. Sex therapists may receive their education and supervision at a number of universities and sex therapy training institutions across the globe. If the training they receive meets the rigorous requirements of AASECT, they can become a Certified Sex Therapist (CST) in addition to being a licensed therapist in their respective field.
With its history of impeccable standards for training, experience and ethical behavior, AASECT is increasingly recognized as the guardian of professional standards in sexual health. Sex therapists may receive their education and supervision at a number of universities and sex therapy training institutions across the globe. If the training they receive meets the rigorous requirements of AASECT, they can become a Certified Sex Therapist (CST) in addition to being a licensed therapist in their respective field.
If you’re searching an online therapist directory, in order to receive the best care, always look for an AASECT Certified Sex Therapist (CST).
How to Prepare for Sex Therapy
Sex therapy can feel foreign for many people, and there are things you’ll want to talk through with your partner and a a therapist before your first session, including:
Compatibility
Like in any kind of relationship, it’s important to consider compatibility. Your therapist should feel like a natural fit with you and your partner so you feel safe discussing delicate topics. If you feel like you are not getting what you need from your sex therapist, continuing your search is recommended.
If you feel like you are not getting what you need from your sex therapist, continuing your search is recommended.
Couples vs. Individual Sex therapy
Many people think sex therapy is only for couples to discuss sexual issues, however you can attend by yourself. It’s important to consider what your issues are and the benefits of both couples and individual sex therapy. You can always start one way and decide that you want to bring in your partner or attend solo.
Practical Things Like Scheduling
Figuring out where and when you can go to sex therapy is another thing to consider. If you are looking to go weekly, you may need to consider rearranging your schedule to ensure you can attend at a standing time. Some therapists offer virtual therapy which may be an option. Talking with the therapist beforehand is important so you know all your options.
Insurance Coverage
Some insurance plans offer more coverage than others, however it’s important to know what is covered before your first session. Checking with the therapist to see what a copay would be and checking with your insurance to see if you have any deductibles is important.
Checking with the therapist to see what a copay would be and checking with your insurance to see if you have any deductibles is important.
Treatment Plan & Length
Coming up with a treatment plan will take a few sessions as the therapist gets to know you. At times, some people need a couple months of treatment while others need longer. This all depends on your needs as an individual and/or a couple.
What to Expect at Your First Appointment
Your initial session with a sex therapist will primarily entail information gathering and creating a treatment plan. The therapist will inquire about what brings you to therapy, what changes you would like to make in your life, and what measurable goals you would like to achieve.
Your therapist will also ask for a detailed history of your current and past relationships and sexual practices. Your therapist is also likely to inquire about your mental health history, any medications, your current and past substance use, your childhood and family of origin and any history of trauma..jpg)
Therapy is most effective when you are able to be honest and forthcoming about the details of your life and what brought you into the therapist’s office. However, you should never feel pressure to answer a question you are not ready to or are uncomfortable with.
Sex therapy and all forms of talk therapy are most effective if you feel a strong therapeutic alliance, or professional rapport, with your therapist. Your initial session is a time to assess whether this therapist is the right fit for you. Make sure that you utilize this time to ask any necessary questions of your provider in order to make an informed decision about proceeding with treatment.
Is Sex Therapy Effective?
Based on the issues you present with in therapy and how entrenched they have become, therapy can last anywhere from a few sessions to a few years in order to see the results you are hoping for. Much of that success depends on how frequently you attend therapy, how motivated you are for change and how active you are between sessions in implementing the tools assigned by your therapist. Results may also depend on coordination of care with other medical providers such as primary care physicians, gynecologists, urologists, psychiatrists or physical therapists.
Results may also depend on coordination of care with other medical providers such as primary care physicians, gynecologists, urologists, psychiatrists or physical therapists.
Although many presenting issues in sex therapy have a physiological component and can sometimes be treated with medication or other medical intervention, optimal outcomes occur when an appropriately trained therapist addresses psychological issues concurrently with medical professionals. A consensus statement from the 2015 International Consultation on Sexual Medicine recommended that both women and men with sexual dysfunction should be offered psychosocial evaluation (sex therapy) in addition to any medical intervention they receive in order to achieve the most positive outcome for treatment.6
While studies in the field of sex therapy are somewhat limited, the studies that have been conducted have largely shown promising results. In a study conducted in 2017, participants in mindfulness-based sex therapy reported significant improvements in sexual desire, sexual function and sex-related distress. 7 A meta-analysis of the study found evidence that mindfulness-based sex therapy was effective for treating female sexual dysfunction and held promise for treating men with situational erectile dysfunction.8
7 A meta-analysis of the study found evidence that mindfulness-based sex therapy was effective for treating female sexual dysfunction and held promise for treating men with situational erectile dysfunction.8
Additional Resources
Education is just the first step on our path to improved mental health and emotional wellness. To help our readers take the next step in their journey, Choosing Therapy has partnered with leaders in mental health and wellness. Choosing Therapy may be compensated for referrals by the companies mentioned below.
Talkspace (Online Therapy For Individuals & Couples) – In couples counseling, you can work together on improving communication, building trust, and resolving conflict. Also, you can work on making sex more enjoyable and fulfilling. Talkspace works with several major insurers including Optum, Cigna, Aetna, and UnitedHealthCare. Try Talkspace
BetterHelp (Online Therapy) – Sexual issues are much more common than you think, and often treatable with therapy. BetterHelp has over 20,000 licensed therapists who provide convenient and affordable online therapy. BetterHelp starts at $60 per week. Complete a brief questionnaire and get matched with the right therapist for you. Get Started
BetterHelp has over 20,000 licensed therapists who provide convenient and affordable online therapy. BetterHelp starts at $60 per week. Complete a brief questionnaire and get matched with the right therapist for you. Get Started
Online-Therapy.com (Online Therapy) – Would you like sex to be a source of joy instead of frustration or pain? Try Therapy. The Online-Therapy.com standard plan includes a weekly 45 minute video session, unlimited text messaging between sessions, and self-guided activities like journaling. Recently, they added instructional Yoga videos. Get Started
Choosing Therapy’s Directory – Find an experienced therapist who specializes in sex therapy. You can search for a therapist by specialty, availability, insurance, and affordability. Therapist profiles and introductory videos provide insight into the therapist’s personality so you find the right fit. Find a therapist today.
Choosing Therapy partners with leading mental health companies and is compensated for referrals by BetterHelp and Online-Therapy. com
com
For Further Reading
- American Association of Sexuality Educators Counselors and Therapists
- National Coalition for Sexual Freedom
- Sexual Health Alliance
- Society for Sex Therapy and Research
- Best Books on Sex & Intimacy
- Sex Therapy Books
10 sources
Choosing Therapy strives to provide our readers with mental health content that is accurate and actionable. We have high standards for what can be cited within our articles. Acceptable sources include government agencies, universities and colleges, scholarly journals, industry and professional associations, and other high-integrity sources of mental health journalism. Learn more by reviewing our full editorial policy.
-
American Psychiatric Publishing. (2013). Diagnostic and statistical manual of mental disorders: Dsm-5. Washington (D.C.).
-
Phd, A. M. C. (2015). Sex Made Simple:Clinical Strategies for Sexual Issues in Therapy.
 Ashland: Pesi Publishing & Media LLC.
Ashland: Pesi Publishing & Media LLC. -
Brotto, L. A. (2018). Better sex through mindfulness: how women can cultivate desire. Vancouver: Greystone Books.
-
Weiner, L., & Avery-Clark, C. (2017). Sensate focus in sex therapy: the illustrated manual. New York: Routledge, Taylor & Francis Group.
-
Nagoski, E. (2015). Come as you are: the surprising new science that will transform your sex life. New York, London, Toronto, Sydney, New Delhi: Simon et Schuster Paperbacks.
-
McCabe, M. P., Sharlip, I. D., Lewis, R., Atalla, E., Balon, R., Fisher, A. D., … Segraves, R. T. (2016, February 18). Risk Factors for Sexual Dysfunction Among Women and Men: A Consensus Statement From the Fourth International Consultation on Sexual Medicine 2015. Retrieved from https://www.sciencedirect.com/science/article/pii/S1743609515000508
-
Bossio, J.A., Basson, R., Driscoll, M., Correia, S., Brotto, L. (2018, October).
 Mindfulness-Based Group Therapy for Men With Situational Erectile Dysfunction: A Mixed-Methods Feasibility Analysis and Pilot Study. Retrieved from https://www.jsm.jsexmed.org/article/S1743-6095(18)31154-8/
Mindfulness-Based Group Therapy for Men With Situational Erectile Dysfunction: A Mixed-Methods Feasibility Analysis and Pilot Study. Retrieved from https://www.jsm.jsexmed.org/article/S1743-6095(18)31154-8/ -
Brotto, L. (n.d.). Effects of Mindfulness-Based Therapies for Female Sexual Dysfunction: A Meta-Analytic Review. Retrieved from https://www.tandfonline.com/doi/abs/10.1080/00224499.2017.1331199
-
American Association of Sexuality Educators, Counselors and Therapists |. (n.d.). Retrieved from https://www.aasect.org/
-
The Kinsey Institute . (n.d.). Retrieved from https://kinseyinstitute.org/
update history
We regularly update the articles on ChoosingTherapy.com to ensure we continue to reflect scientific consensus on the topics we cover, to incorporate new research into our articles, and to better answer our audience’s questions. When our content undergoes a significant revision, we summarize the changes that were made and the date on which they occurred. We also record the authors and medical reviewers who contributed to previous versions of the article. Read more about our editorial policies here.
We also record the authors and medical reviewers who contributed to previous versions of the article. Read more about our editorial policies here.
-
Originally Published: April 28, 2020
Original Author: Indigo Stray Conger, LMFT, CST
Original Reviewer: Meera Patel, DO -
Updated: March 23, 2022
Author: No Change
Reviewer: No Change
Primary Changes: Updated for readability and clarity; Reviewed and added relevant resources; Added “Do My Partner and I Need to See a Sex Therapist?” and “How to Prepare for Sex Therapy”. New material written by Silvi Saxena, MBA, MSW, LSW, CCTP, OSW-C and reviewed by Dena Westphalen, PharmD.
If you are in need of immediate medical help:
Medical
Emergency
911
Suicide Hotline
800-273-8255
How Much Does Sex Therapy Cost?
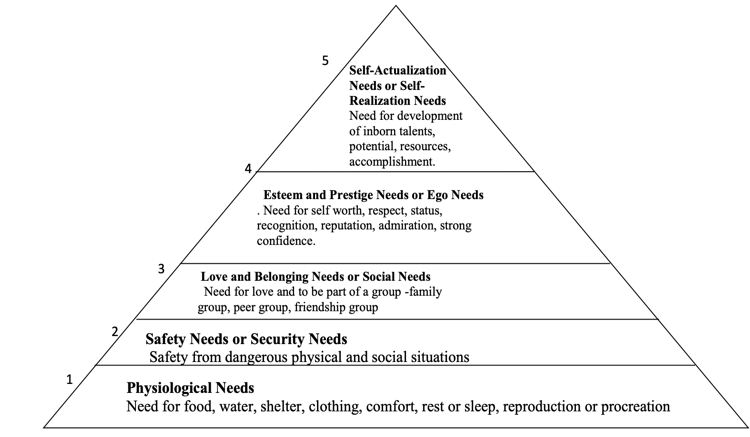
Seeking help requires a combination of security and awareness. You need to understand there is a problem, know that help is available, and be comfortable seeking that help.
You need to understand there is a problem, know that help is available, and be comfortable seeking that help.
This is difficult enough for routine problems, more difficult for medical issues, and extremely difficult for sensitive issues. Even in seeking help, adhering to a treatment plan and engaging in sex therapy exercises proves difficult for many.
Part of this is society's general discomfort with talking about sex. Another factor is finding time and energy to improve one's life.
Even though a person's sex life underpins several elements of health, sex therapy isn't always covered under general healthcare. This results in individuals and couples weighing the cost to value ratio in finding therapy. Read on to learn more.
Sex therapy exercises
Sex therapy programs are generally integrative, meaning a sex therapist will draw on a range of approaches to help an individual or couple.
Sex therapy aims to support people to have the sex life that works for them. The different options have many overlaps but each also offers something different that can help a person engage with the therapy. The comfort of clients is crucial to reaping the benefits for everyone involved.
The different options have many overlaps but each also offers something different that can help a person engage with the therapy. The comfort of clients is crucial to reaping the benefits for everyone involved.
Getting what you pay for is as much about the efforts you put in as the program serving to meet your needs. Avoid incompatibility between the therapeutic modality, the therapist, and the frequency of appointments.
It's key that everyone involved is forthcoming with their expectations and status as the therapy progresses.
In face-to-face therapy, a series of touch exercises may be given. Clients engage in these exercises at home, they do not take place in the session or involve the therapist at all
Face-to-face therapy
The traditional (read oldest) sex therapy option involves sitting in an office (or home). This is done either one-on-one with a therapist or with the therapist and a partner.
After initial screening sessions expect to have couple's sessions. If you find that solo sessions are needed, other forms of therapy are likely a better fit.
If you find that solo sessions are needed, other forms of therapy are likely a better fit.
The approach used in face-to-face sex therapy can draw on behavioural techniques, cognitive behavioural therapy (CBT), couples communication, or emotion-focused therapy, amongst many more.
If trauma is the root of issues, for either partner, this could be an opportunity for them to seek out individual therapy to work beyond that. Sex therapy is often about working together and best undertaken from an otherwise healthy space.
Self-awareness is the key at the centre of these techniques. Engaging the client couple to be aware and active in their sexual experiences assists with many types of problems.
Benefits
One benefit of face-to-face therapy is that it can be easier to form a supportive connection with a therapist in person. Often a lack of connection and a feeling of being abandoned to deal with their struggles alone is why people seek out therapy.
For couples, being asked to listen intently but without distractions does heavy lifting in creating a more mindful space.![]() Being on the neutral ground together, away from their shared space, can help foster problem-solving together.
Being on the neutral ground together, away from their shared space, can help foster problem-solving together.
Costs
Face-to-face options cost the most because they require the most effort on the part of a therapist. Not only are you paying for elements of the brick and mortar office but also the furniture, note-taking, reception, and everything else that goes into a business.
The costs for these programs range from about £50-£120 per session ( on the higher end for couples therapy), depending on your therapist and where they are based.
Telehealth (online)
Telehealth services are becoming more popular currently. People find it difficult to travel to an office when video conferencing technologies are adequate. This allows for talking and that all-important body language component to happen remotely.
Telehealth makes it easier to schedule appointments in a hectic life as it takes only the time to turn on a device and engage. It removes drive times to and from a session and the associated stress.
Benefits
Time savings is one of the biggest benefits. The ability to put the exercises from online sex therapy into practice without the cooldown period of a drive home is another.
People feel comfortable having difficult, intimate conversations when they're speaking from their own homes. The distance that a monitor provides, combined with being in a familiar space, allows some people to open up and engage more.
Costs
Online sex therapy can cost less because there may be less overhead for the therapist
Digital therapy
Digital therapy options build on the less intense face-to-face approach provided by telehealth. The major difference in digital therapy is that you don’t have to talk to anyone, except your partner. Instead, you are guided through a program created by the therapist that walks you through a series of sex therapy exercises and reminders.
The programs are dynamic and supplemented by a therapist who can be reached for additional information.
Benefits
The principal benefit of digital therapy is taking out feelings of embarrassment or feeling judged. As you are dealing with a program, not a person, it can be easier to open up and engage with the material. Said materials are constructed by a therapist, ensuring the same professional interaction as face-to-face options.
The second benefit is time. Digital therapy allows for engagement throughout a day and week in bits and pieces. The only reason therapy currently runs in hour frameworks is to facilitate the therapist's journal.
This helps to remove some of the energy-drain of a day-to-day workweek from interfering with therapy. Working on digital therapy separately and together also helps couples break down communication barriers gradually in a way that being in an office can hinder.
Client's find they prefer to work at their own pace. Having on-demand access beats waiting for a scant hour. It's also more convenient to start touch exercises at home without delay.
Opt-in schedules match client goals: better communication, a fulfilling sex life, or a stronger relationship. Each of these benefits from the adjustable time commitments and frequencies that digital therapy offers.
Costs
Digital therapy offers value as well. With subscriptions, options are offered as weekly or monthly engagements instead of billed as time per session. This allows clients to experience more exercises for less cost.
Sex apps for couples may include a second subscription free for a partner, adding to the overall value for time.
Take heart
A fulfilling sex life isn't just good for physical health, but also a general quality of life. Engaging with sex therapy exercises increases understanding and responsiveness to others.
With digital options, it's easy to engage on your schedule and improve from the comfort of home. You and your partner can grow together privately but with guided assistance.
If you feel ready to get back in touch with sex again, check out how with the Blueheart app here.
- Invitro
- Profiles
- infections transmitted ...
- Sex in the Bolshoi City: ...
-
- COVID-19
- Surveys for office employees
- Household personnel examination
- Cardiovascular risk assessment
- Antiphospholipid syndrome (APS) diagnosis
- Liver function assessment
- Healthy child: for children from 0 to 14 years old
- infections transmitted by sexually (IPP)
- Problems of weight
- VIP examinations
- Respiratory diseases
- Allergy
- Determination of microelements in the body
- Beauty
- Vitamins
- Diets
- Pre-diet laboratory tests
- Sports profiles
- Hormonal tests for men
- Differential diagnosis of depression
- Evaluation of the blood coagulation system
-
- Covid-19
- Biochemical Studies
- Glucose and metabolites of carbohydrate metabolism
- Poems 9000 9000 9000 9000 9000 9000 9,000
- Inorganic substances/electrolytes:
- Vitamins
- Proteins involved in iron metabolism
- Cardiospecific proteins
- Study of the structure of renal stone
- Rest urine
- Clinical urine analysis
- Biochemical analysis of urine
- Study Kala
- Calamin
- Biochemical analysis of feces
-
- Viral infections
- Bacterial infections
- Fungal infections
- Diseases of the gastrointestinal tract
- Diseases of the central nervous system
- Oncological diseases
- Metabolic disorders
- Description of the results of genetic studies by a geneticist
- Pharmacogenetics
- 9000 9000 9000
- of the Red fetal factor
- Antitrium Antitrium Antitriors infectious diseases
- Hereditary diseases
- Hereditary metabolic diseases
- Examination of newborns to detect hereditary metabolic diseases
- Additional studies (after screening and consultation with a specialist)
- Determination of biological relationship: paternity and motherhood
- Determination of biological relationship in the family: paternity and motherhood
- Water quality survey
- Soil quality survey
- Diagnostics of the Pathology of the liver without biopsy: fibromax, fibrotest, steatoscrin
- Calculation tests performed according to the results of steatoskrin without blood taking
- Dybiotic states of the intestines (inbioflore, foflore, microbiosenosis of Urogenital.
 microflora of the body
microflora of the body - Study of microbiocenosis of the urogenital tract (INBIOFLOR)
- Femoflor: profiles of studies of dysbiotic conditions of the urogenital tract in women
- Specific assessment of the natural microflora of the body
- Test results form in English
-
- Blood
- Urine
- Kal
- Spermogram
- Gastropanel
-
- Endoscopy
- Functional diagnostics
- ultrasound
-
- Research We Don't Do
- New tests
- Getting Results
- Additional order of studies
- Medical consultant service
- Professional position
The cost of analyzes is indicated without taking biomaterial
Composition
Human herpes virus type 1 and 2 (herpes simplex virus type 1 and 2), DNA detection (Human herpesvirus 1, 2, Herpes simplex virus 1, 2 (HSV-1, HSV-2), DNA) in scraping of epithelial cells of the urogenital tract
• Detection of DNA of herpes simplex virus type 1 (labial or labial) and type 2 (genital) in scrapings of epithelial cells of the urogenital tract.
• Confirmation of infection and assessment of the activity of the infectious process, including when planning pregnancy, in pregnant women, to examine people with immunodeficiency states.
Cytomegalovirus, detection of DNA (Cytomegalovirus, DNA) in a scraping of epithelial cells of the urogenital tract
• Confirmation of CMV infection.
• Comprehensive preconception examination of partners.
Differential detection of HPV DNA (Human papillomavirus, HPV) of high oncogenic risk type 2 (16, 18) in the scraping of epithelial cells of the urogenital tract
Detection of HPV DNA in the urogenital scraping is used to confirm infection and persistence of HPV 16 -th and 18th types, to assess the carcinogenic risk in dysplasia of the epithelium of the cervix.
Gonococcus, DNA detection (Neisseria gonorrhoeae, DNA) in the scraping of epithelial cells of the urogenital tract
Detection of Neisseria gonorrhoeae DNA in the urogenital scraping is used to confirm infection in the presence of clinical manifestations of gonorrhea, in the chronic course of infection, during pregravid examination.
Gardnerella, detection of DNA (Gardnerella vaginalis, DNA) in scrapings of epithelial cells of the urogenital tract
Detection of DNA of Gardnerella vaginalis in urogenital scrapings is used to confirm infection with manifestations of bacterial vaginosis (gardnerellosis) in women of reproductive age, for the differential diagnosis of diseases with similar symptoms .
Mycoplasma, detection of DNA (Mycoplasma hominis, DNA) in scrapings of epithelial cells of the urogenital tract
Detection of Mycoplasma hominis DNA in urogenital scrapings is used to confirm infection in the absence of other pathogenic pathogens, with an erased picture of inflammation, with complicated pregnancy. May be seen in clinically healthy individuals.
Mycoplasma, detection of DNA (Mycoplasma genitalium, DNA) in a scraping of epithelial cells of the urogenital tract
• Confirmation of infection in the presence of an erased picture of inflammation, during preconception examination, during pregnancy, in infertility, for the differential diagnosis of urogenital infections.
Ureaplasma, determination of DNA (Ureaplasma urealyticum + parvum, DNA) in the scraping of epithelial cells of the urogenital tract
• Confirmation of infection in the presence of characteristic signs, with an erased picture of inflammation, when planning pregnancy, infertility.
• Can be detected in clinically healthy individuals.
Chlamydia, determination of DNA (Chlamydia trachomatis, DNA) in the scraping of epithelial cells of the urogenital tract
• Confirmation of infection in the presence of clinical manifestations of inflammation of the urogenital tract, when planning pregnancy, in case of infertility, to control the effectiveness of antibiotic therapy.
Candida, determination of DNA (Candida albicans, DNA) in the scraping of epithelial cells of the urogenital tract
Detection of Candida albicans DNA in urogenital scraping is used to confirm infection in the presence of characteristic clinical manifestations of urogenital candidiasis, as well as to evaluate the effectiveness of antifungal therapy in candidiasis.
Trichomonas, detection of DNA (Trichomonas vaginalis, DNA) in scrapings of epithelial cells of the urogenital tract
Detection of Trichomonas vaginalis DNA in urogenital scrapings is used to confirm infection in the presence of clinical manifestations of trichomoniasis, during pregravid examination, for the differential diagnosis of urogenital infections.
Description
In what cases is the study "Sex and the City: 12 infections + UCM (urogenital scraping)":
- if you suspect the presence of sexually transmitted infections.
Synonyms: Analysis for twelve sexually transmitted infections.
Sex in City: 12 Infections, urogenital scraping.
Profile composition:
No. 309URO Human herpes virus type 1 and 2 (herpes simplex virus type 1 and 2), DNA determination (Human herpesvirus 1, 2, Herpes simplex virus 1, 2 (HSV-1, HSV -2), DNA) in the scraping of epithelial cells of the urogenital tract
No. 310URO Cytomegalovirus, detection of DNA (Cytomegalovirus, DNA) in scrapings of epithelial cells of the urogenital tract
310URO Cytomegalovirus, detection of DNA (Cytomegalovirus, DNA) in scrapings of epithelial cells of the urogenital tract
No. 312C-URO Differential determination of HPV DNA (Human papillomavirus, HPV) of high oncogenic risk of two types (16, 18) in scraping of epithelial cells of the urogenital tract
Nr.0487
No. 302URO Mycoplasma, determination of DNA (Mycoplasma hominis, DNA) in the scraping of epithelial cells of the urogenital tract
No. 308URO Mycoplasma, determination of DNA (Mycoplasma genitalium, DNA) in the scraping of epithelial cells of the urogenital tract
No. urealyticum+parvum, DNA) in a scraping of epithelial cells of the urogenital tract
No. 301URO of Chlamydia, determination of DNA (Chlamydia trachomatis, DNA) in a scraping of epithelial cells of the urogenital tract
No. 344Candida DNA (Candida albicans, DNA) in the scraping of epithelial cells of the urogenital tract
No. 307URO Trichomonas, DNA (Trichomonas vaginalis, DNA) in the scraping of the epithelial cells of the urogenital tract
Brief description of the profile "Sex and the City" : 12 infections + UCM (urogenital scraping)»
A significant place in the structure of the infectious pathology of the genitourinary system is occupied by inflammatory processes caused by opportunistic microorganisms, including genital mycoplasmas: the frequency of detection of Ureaplasma spp. and Mycoplasma hominis varies widely in different population groups, ranging from 10 to 50% (according to some authors, up to 80%).
and Mycoplasma hominis varies widely in different population groups, ranging from 10 to 50% (according to some authors, up to 80%).
Mycoplasma hominis, Ureaplasma urealyticum, Ureaplasma parvum are opportunistic microorganisms that, when their pathogenic properties are realized, can cause urethritis (Ureaplasma urealyticum), cervicitis, cystitis, as well as pregnancy complications, postpartum and postabortion complications.
Mycoplasma genitalium is a pathogenic microorganism that causes diseases of the genitourinary tract. Mycoplasmas are transmitted through sexual contact, can cause non-gonococcal urethritis and prostatitis, inflammatory diseases of the pelvic organs, pathology of pregnancy and fetus, infertility in women and men.
Gardnerella vaginalis is a bacteria commonly found in the vaginal microbiota of healthy women. However, this microorganism is much more often detected in the vagina of women with bacterial vaginosis (BV) and plays a key role in the pathogenesis of this disease. In BV, protective lactobacilli are replaced by anaerobic microorganisms. More often, patients complain of profuse discharge with the smell of stale fish, which can increase after sperm or soapy solution enters the vagina, discomfort in the introitus area, dyspareunia, burning, itching, and irritation of the vulva are rare. The presence of BV is associated with severe infectious and inflammatory diseases in obstetric and gynecological practice.
In BV, protective lactobacilli are replaced by anaerobic microorganisms. More often, patients complain of profuse discharge with the smell of stale fish, which can increase after sperm or soapy solution enters the vagina, discomfort in the introitus area, dyspareunia, burning, itching, and irritation of the vulva are rare. The presence of BV is associated with severe infectious and inflammatory diseases in obstetric and gynecological practice.
Yeast-like fungi of the genus Candida are considered to be representatives of the normal microbiota of the urogenital tract (UGT) and are most often localized on the vaginal mucosa and vulvar skin. Under certain conditions, the growth of yeast fungi increases, which provokes vulvovaginal candidiasis (VVC), which is accompanied by genital itching, burning and / or vaginal discharge. The dominant pathogen is Candida albicans. It accounts for up to 90% of VVC cases.
Urogenital trichomoniasis is an infectious disease of the genitourinary organs caused by Trichomonas vaginalis and sexually transmitted. Trichomoniasis is more common in women of reproductive age. Complications of trichomoniasis include premature birth, the birth of children with low body weight. Women with Trichomonas infection are significantly more likely to become infected with HIV and are significantly more likely to infect their sexual partners with HIV. There is also a higher risk of infection with sexually transmitted infections and oncogenic papillomaviruses in women with urogenital trichomoniasis than in healthy women.
Trichomoniasis is more common in women of reproductive age. Complications of trichomoniasis include premature birth, the birth of children with low body weight. Women with Trichomonas infection are significantly more likely to become infected with HIV and are significantly more likely to infect their sexual partners with HIV. There is also a higher risk of infection with sexually transmitted infections and oncogenic papillomaviruses in women with urogenital trichomoniasis than in healthy women.
Urogenital chlamydial infection is a common sexually transmitted infection caused by Chlamydia trachomatis. The prevalence of chlamydial infection in the population varies with age, with the highest incidence observed in persons younger than 25 years of age. Chlamydial infection is dangerous during pregnancy, as it can lead to premature birth, miscarriage, low birth weight, and fetal death.
Gonococcal infection is a sexually transmitted infection caused by Neisseria gonorrhoeae. With gonorrhea, the mucous membranes are most often affected by the genital tract, but the rectal mucosa, conjunctiva, and oropharynx can be affected. More than 70% of women have a subjectively asymptomatic course of the disease. In women, it manifests itself as urethritis, bartholinitis, endocervicitis, endometritis, salpingitis and pelvioperitonitis. In men, the causative agent of gonorrhea is the cause of urethritis, urethral stricture, epididymitis, prostatitis, orchitis and other diseases of the testicles and its appendages.
With gonorrhea, the mucous membranes are most often affected by the genital tract, but the rectal mucosa, conjunctiva, and oropharynx can be affected. More than 70% of women have a subjectively asymptomatic course of the disease. In women, it manifests itself as urethritis, bartholinitis, endocervicitis, endometritis, salpingitis and pelvioperitonitis. In men, the causative agent of gonorrhea is the cause of urethritis, urethral stricture, epididymitis, prostatitis, orchitis and other diseases of the testicles and its appendages.
Genital herpes is a predominantly sexually transmitted viral disease caused by the herpes simplex virus (HSV) II and/or type I. This is the most common erosive and ulcerative disease of the genitals. Genital herpes infections are mostly asymptomatic or go unrecognized, but can cause symptoms such as painful blisters or sores at the site of infection. Although genital herpes is caused by both HSV type I and type II, the incidence of HSV type II is higher. In the epidemiology of genital herpes, asymptomatic viral shedding is important: up to 70% of cases of transmission of genital HSV occurs with an asymptomatic course of the infectious process in a patient. Primary herpes infection and reactivation of the infection (to a much lesser extent) during pregnancy can cause pregnancy pathology, intrauterine infection of the fetus or infection of the child during childbirth.
In the epidemiology of genital herpes, asymptomatic viral shedding is important: up to 70% of cases of transmission of genital HSV occurs with an asymptomatic course of the infectious process in a patient. Primary herpes infection and reactivation of the infection (to a much lesser extent) during pregnancy can cause pregnancy pathology, intrauterine infection of the fetus or infection of the child during childbirth.
Human papillomavirus (HPV) refers to small DNA-containing viruses that infect epithelial cells and induce proliferative lesions of the skin and mucous membranes. Currently, about a hundred types of HPV with different oncogenic potential are known, which are conditionally combined into groups of high and low oncogenic risk. Most often in the biomaterial from tumors of the cervix, the 16th and 18th types are found. Detection of HPV DNA does not confirm the presence of a malignant process, in the majority (up to 90%) of cases within 12-36 months, the elimination of the virus and self-healing occurs. With prolonged chronic persistence of the virus and depending on its type, the risk of developing an oncological process increases.
With prolonged chronic persistence of the virus and depending on its type, the risk of developing an oncological process increases.
Cytomegalovirus (CMV) infection is a viral infection of the body, which refers to the so-called opportunistic infections, usually occurring latently. Cytomegalovirus belongs to the herpesvirus family. With primary infection of a pregnant woman with cytomegalovirus (in 35-50% of cases) or reactivation of the infection during pregnancy (in 8-10% of cases), intrauterine infection develops. With the development of intrauterine infection, there is a risk of fetal malformations, spontaneous abortion, intrauterine growth retardation, hypo- or dysplasia of internal organs, etc. are possible.
What is the purpose of the study "Sex and the City: 12 infections + UCM (urogenital scraping)"
The tests included in the profile are aimed at identifying the causative agents of the most common sexually transmitted infections.
The specifics of the study "Sex and the City: 12 infections + UCM (urogenital scraping)"
It is not recommended to take biological material for cytological examination and PCR on the same day!
- Do not take material for research earlier than 48 hours after sexual contact.

- Samples should not be taken for examination earlier than 48 hours after ultrasound with a vaginal probe.
- Samples should not be taken for examination earlier than 48 hours after colposcopy.
- It is not recommended to take the material during menstrual bleeding.
- It is not recommended to douche on the eve and on the day of taking biological material.
- For microbiological studies (planting on flora) and PCR studies, it is recommended to take biological material before the start of the use of antibacterial and chemotherapeutic drugs or not earlier than 10-14 days after their cancellation (for local antibiotics and antiseptics) and not earlier than one month after the systemic use of antibiotics (oral, intramuscular, intravenous). If it is necessary to conduct a study against the background of antibiotic therapy, be sure to indicate this information in the referral form.
 The biomaterial should be taken before the next intake/administration of the drug.
The biomaterial should be taken before the next intake/administration of the drug. - The patient is advised to refrain from urinating for 1.5-3 hours before taking a scraping from the urethra (for women - 3 hours, for men - 1.5-2 hours).
Test material
See relevant tests.
Method of determination
See relevant tests.
Units
See relevant tests.
Reference values
See related tests.
Interpretation of results
Interpretation of test results contains information for the attending physician and is not a diagnosis. The information in this section should not be used for self-diagnosis or self-treatment. An accurate diagnosis is made by the doctor, using both the results of this examination and the necessary information from other sources: anamnesis, results of other examinations, etc.
Please note that the timing of PCR tests may be extended when confirmatory tests are performed.
See related tests.
Basic literature
- WHO. Newsletters. Human papillomavirus (HPV) and cervical cancer. – 2020.
- WHO. Newsletters. Herpes simplex virus. − 2020.
- WHO. Newsletters. Sexually transmitted infections (STIs). – 2019.
- Global health sector strategy on sexually transmitted infections (2016–2021). World Health Organization. − 2016.
- Clinical guidelines. Cervical cancer. – 2018.
- Kovalyk VP et al. Clinical significance of ureaplasmas in urogenital pathology //Clinical practice. - 2019. - T. 10. - No. 1.
- Krysanova AA Gardnerella vaginalis: genotypic and phenotypic diversity, virulence factors and role in the pathogenesis of bacterial vaginosis // Journal of Obstetrics and Women's Diseases. – 2019. - T. 68. - No. 1.
- Kubanov A.A. et al. Bacterial vaginosis. Russian Society of Dermatovenerologists and Cosmetologists.
 Clinical guidelines. − 2020.
Clinical guidelines. − 2020. - Kubanov A.A. et al. gonococcal infection. Russian Society of Dermatovenerologists and Cosmetologists. Clinical guidelines. − 2020.
- Kubanov A.A. et al. Urogenital trichomoniasis. Russian Society of Dermatovenerologists and Cosmetologists. Clinical guidelines. − 2020.
- Kubanov A.A. et al. Chlamydial infection. Russian Society of Dermatovenerologists and Cosmetologists. Clinical guidelines. − 2020.
- Kuznetsova IV, Chilova RA Bacterial vaginosis and vulvovaginal candidiasis //Obstetrics and gynecology. – 2018. – no. 5. - S. 143-148.
- Prilepskaya VN et al. Clinical guidelines for the diagnosis and treatment of diseases accompanied by pathological discharge from the female genital tract //M.: ROAG; − 2019. – 56 p.
- Rakhmatulina MR, Galkina IS Diagnosis of infectious urogenital pathology by quantitative PCR // Bulletin of the Russian State Medical University.
 – 2019. – no. 6.
– 2019. – no. 6.
Preparation
Rules for preparing for the study "Sex and the City: 12 infections + UCM (urogenital scraping)"
Examination of women should be carried out in the first half of the menstrual cycle, not earlier than the 5th day. Examination in the second half of the cycle is acceptable, no later than 5 days before the expected start of menstruation. If there are pronounced symptoms of inflammation, the material is taken on the day of treatment. The day before and on the day of the examination, the patient is not recommended to perform vaginal douching. It is not recommended to take biomaterial against the background of antibiotic therapy (general / local) and during menstruation, earlier than 24-48 hours after sexual contact, intravaginal ultrasound and colposcopy.
For both men and women, it is recommended that specimens be collected no earlier than 14 days after the use of antibiotics and topical antiseptics, and no earlier than one month after the use of oral antibiotics.
If a scraping from the urethra is taken for examination, the collection of the material is carried out before or not earlier than 2-3 hours after urination.
General guidelines for exam preparation can be found here.
Questions
and answers
{{{this.PREVIEW_TEXT}}}
Did the answer help you?
{{/each}}When choosing where to take the "Sex and the City: 12 Infections + UCM (Urogenital Scraping)" analysis profile at an affordable price in Temryuk and other cities of Russia, do not forget that the cost, methods and terms of the examinations in regional medical offices may differ.
Sex therapy for soldiers: how surrogate partners help in rehabilitation
- Yolanda Nell, Phil Marzouk Air Force
- , Tel Aviv
9 minutes ago
18 +
In many countries, surrogate sex therapy—that is, involving the patient's hired sex partners—is controversial and not widely practiced. However, in Israel, such treatment is carried out as part of a state program for military personnel who are seriously injured and need sexual rehabilitation.
However, in Israel, such treatment is carried out as part of a state program for military personnel who are seriously injured and need sexual rehabilitation.
Israeli sexologist Ronit Alon's office in Tel Aviv looks just as you'd expect. There is a small comfortable couch for clients, and on the walls are biological diagrams of male and female genitalia, which she uses to explain.
But what is interesting is what happens in the next room, where there is a large sofa bed and candles.
- “How do you want to be touched?”. Sex among people with disabilities in Ukraine
- Female Orgasm: The Princess Who Pioneered Sex Research
Here, paid surrogate partners help teach Alon's clients the art of intimate relationships and, finally, how to have sex.
“It doesn't feel like a hotel, it's more like a house for an apartment,” says Dr. Ka Alon. There is a bed, a CD player, a separate shower, and erotic artworks adorn the walls.
“Sex therapy is very much therapy for couples, and without a partner, you can't complete the process,” she continues. - a surrogate partner - she or he - fulfills the role of a partner in a regular couple."
Although critics compare it to prostitution, in Israel this therapy has become widespread: soldiers with injuries that affect their ability to have sex are covered by the state.
"People need to feel like they can please someone else and they can please someone," says Dr. Ka Alon, who has a PhD in Sexual Rehabilitation.
“People come to therapy. They don't come for pleasure. There is nothing like prostitution in this, she adds firmly. - In addition, 85% of the sessions are about intimacy, touch, communication, they are about how to be a person and about relating to other people. The moment you start a sexual relationship is the end of the process."
Our interlocutor, who introduced himself as Mr. A, was one of the first soldiers to obtain reimbursement from the Israeli Ministry of Defense for the cost of surrogate sex therapy after an accident that changed his life almost 30 years ago.
As an Israel Defense Forces reservist, after falling from a great height, he was paralyzed from the waist down and unable to have sex as before.
“When I got injured, I made a list of things to learn how to do,” he says. “It included showering, eating, dressing, driving and having sex on your own.”
Panel A was already married and had children, but his wife did not feel comfortable talking about sex with doctors and psychologists, so she advised him to seek help from doctor Alon.
He explains how Dr. Ka Alon provided guidance and guidance to him and his surrogate before and after each session.
“You have to start from the very beginning: you touch your partner here, there, and gradually, step by step, the process develops into the last stage of orgasm,” he says.
Panel A thinks it's right that the state paid for his weekly sessions, like other elements of the rehabilitation program. Today, the cost of a three-month course of treatment is $5,400.
“Having sex with a surrogate partner was not my goal. Yes, I was injured and I wanted to rehabilitate in all aspects of my life,” he says, sitting in his wheelchair in a tracksuit: he is going to play table tennis. I didn't fall in love with my partner. I was married. I just wanted to learn the technique of reaching the goal. I took it as a very logical thing to do."
In his opinion, Western obsession with sex leads to mistakes.
"Sex is part of life, it's the pleasure of life," he says. "It's not that I'm a Casanova, that's not the problem."
People of all ages and backgrounds flock to Dr. RCT Alon's clinic trying not to draw attention to themselves.
Many visitors have difficulty trying to start a romantic relationship, due to physical intimacy problems or anxiety, or through sexual abuse. Others have physical and mental health problems.
From the very beginning of her career, Dr. Alon has paid special attention to clients with disabilities. Several of his close relatives lost their health, in particular her father, a pilot, received a head injury after a plane crash.
Several of his close relatives lost their health, in particular her father, a pilot, received a head injury after a plane crash.
“All my life I have been around people who have had to deal with and overcome various forms of disability,” she says. “All these people have successfully rehabilitated, so I looked at things very optimistically.”
Dr. Ka Alon developed a close relationship with a surrogate partner who worked with the disabled while studying in New York.
When she returned to Israel in the late 1980s, she received approval from leading rabbis to use sex surrogates and began therapy at a rehabilitation center in a religious kibbutz, a rural community.
the rabbis had one requirement: married men and married women cannot be surrogate partners. Dr. Ka Alon still does it today.
Subsequently, she enlisted the support of the Israeli authorities. Of the approximately 1,000 people who underwent surrogate sex therapy at her clinic, dozens of Israeli army veterans were injured.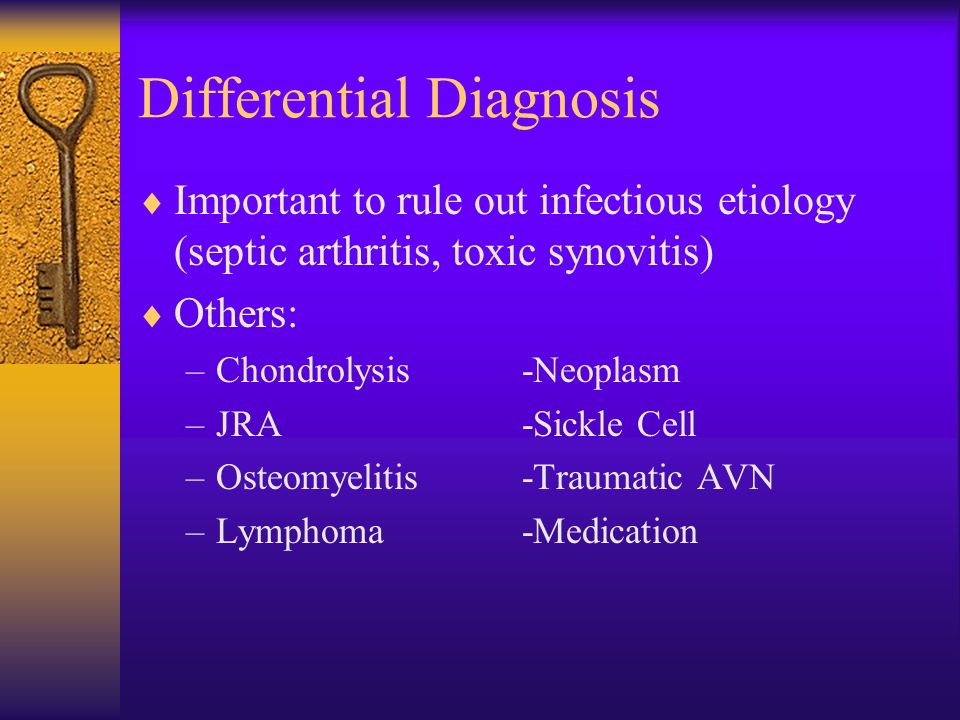 Their treatment was financed by the state. Many have brain or spinal cord injuries.
Their treatment was financed by the state. Many have brain or spinal cord injuries.
Dr. Ka Alon believes Israel's family-oriented culture and attitude towards its military has worked in her favor. At the age of 18, most Israelis would be drafted into the military, and then they would remain in the reserve for decades.
“Since the founding of the country, we have been at war all the time,” she says. “Everyone in Israel knows someone who has been injured or died and is positive about compensating those people. We feel indebted to them."
A tall man in his 40s sits in the garden with a blanket on his lap. he is a former reserve soldier whose life was radically changed during the 2006 Lebanon War.
David (let's call him that) can neither speak nor move.
he can only communicate with the help of his therapist - if she supports his hand and at the same time a pencil in his fingers, then he can write on the board.
“I was an ordinary person. I have just returned from a trip to the Far East. I went to university and worked as a bartender. I used to love sports and hanging out with friends,” says David.
I have just returned from a trip to the Far East. I went to university and worked as a bartender. I used to love sports and hanging out with friends,” says David.
When his military unit was attacked, he suffered serious leg and head injuries and spent three years in hospital.
According to him, during this time he lost the will to live.
The situation began to change only after the doctors offered him surrogate sexual therapy.
“When I started surrogate therapy, I felt like a failure, a nonentity. And during therapy, I felt like a man, young and beautiful, says David. “It was the first time I felt like this since the injury. It gave me strength and gave me hope."
However, it was an intimate relationship that inevitably had to end, and David knew. Was there a risk that he would get emotionally hurt?
“At first it was difficult for me, because I wanted the surrogate partner to belong only to me,” he says. - But I realized that even if we are no longer partners, we are still good friends. And it's worth it, really. It just helps you rebuild yourself from scratch."
And it's worth it, really. It just helps you rebuild yourself from scratch."
Generally, the rules prohibit clients and their surrogate partners from having relationships outside of therapy. However, David and his partner - a woman under the pseudonym Serafina - received special permission from Dr. Alon's clinic to remain in touch after the end of treatment.
David's relatives say that after the therapy he changed and focused on plans for the future.
Although his sex life remains very difficult, before the start of the Covid-19 epidemic, he began to communicate more with people, to go out with the help of carers.
Serafina has been a surrogate partner at the Ronit Alon clinic for over ten years. This is a slender woman with a short haircut, open and lively.
She recently published a book about her experience. it's called "More Than a Sex Surrogate" and the publishers describe it as "unique intimacy memories, secrets et cetera in the way we love. "
"
Like other surrogate partners of the Tel Aviv clinic, Serafina has other work. She does art. She says she joined the clinic for altruistic reasons.
“I wanted to help all those who suffer and hide their suffering and their secrets because I knew I had the ability,” she explains. I had no problem with the idea of using sexuality and my body in therapy. and it was captivating, the sexuality captured me."
Serafina describes herself as "a bit of a tour guide", a guide on the journey she takes her clients on.
she has worked for about 40 clients, including another member of the military, but says the severity of David's injuries was a unique problem. She learned to help him write so they could talk in private.
“David is an extreme case. It was like walking in the desert - not sure where to go, ”she says.
“You had to be very resourceful because he doesn't move at all. I moved his body the way I imagined he would move himself if he could. he felt his body, but he couldn't move,” Serafina continues. - he always said: "She knows exactly what I want, even if I don't say anything." It was very nice."
he felt his body, but he couldn't move,” Serafina continues. - he always said: "She knows exactly what I want, even if I don't say anything." It was very nice."
In addition to surrogate partners, Serafina also had her own relationships with men. According to her, her partners accept what she does. But she knows other women and men who have left sex surrogate work for their own partners or for marriage.
She explains that saying goodbye to clients after an intimate relationship is necessary but difficult: “It's like going on vacation. we have the opportunity to build great relationships for a short time - do we use it or give it up? and this is a calm break in relations that can be. there are good reasons for this. Sometimes I may cry, but at the same time I am so happy. When I find out that someone has had a baby or got married, it's impossible to imagine how happy, excited and grateful I am for what I'm doing."
Late in the evening, Ronit Alon is still at work giving an online lecture to a group of sexologists from Europe and South America.
She talks about individual cases and cites studies showing that sex surrogates are more effective than classical psychological therapy in treating sexual problems.
“This is very interesting. Therapists who have already worked with surrogates all say they will do it again,” she tells them.
She believes that with the modern development of surgery, which allows seriously wounded soldiers to survive, treatment with the help of surrogate partners could be used more widely.
“It is impossible to rehabilitate a person without rehabilitating his self-esteem, her perception of herself as a man or a woman,” she says. This part of our lives cannot be ignored. It is very important. This is the center of our personality. And you can't just talk about it. Sexuality is something dynamic, it's something that needs to exist between us and other people."
According to Dr. Star Alon, there is an unhealthy attitude towards sex in modern society.
- How sex is sold through social networks
- How sex will change in the future
- Teens have changed: time with family is more important than sex
“We know how to joke about sexuality.