Treatment for hair pulling disorder
Trichotillomania (hair pulling disorder) - NHS
Trichotillomania, also known as trich, is when someone cannot resist the urge to pull out their hair.
They may pull out the hair on their head or in other places, such as their eyebrows or eyelashes.
Trich is more common in teenagers and young adults.
Symptoms of trichotillomania
People with trich feel an intense urge to pull their hair out and they experience growing tension until they do. After pulling their hair out, they feel a sense of relief.
A person may sometimes pull their hair out in response to a stressful situation, or it may be done without really thinking about it.
Most people with trich pull out hair from their scalp, but some pull out hair from other areas, such as their:
- eyebrows
- eyelashes
- genital area
- beard or moustache
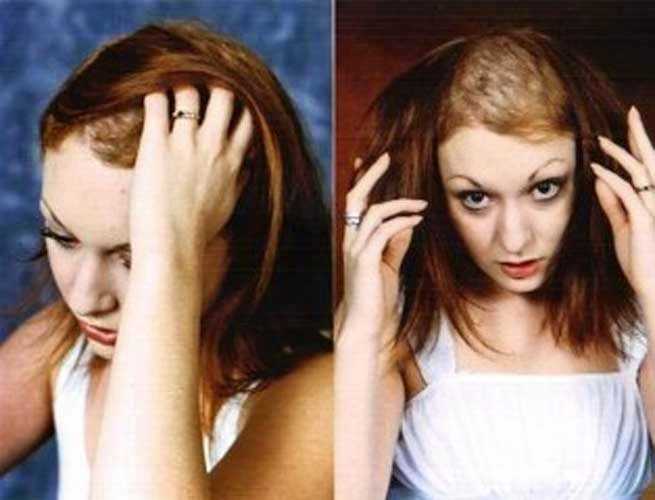
Bald patches on the head may have an unusual shape and affect 1 side of the head more than the other.
Trich may cause feelings of shame and low self-esteem. Those affected may try to keep their condition to themselves.
Causes of trichotillomania
It's not entirely clear what causes trich. It could be:
- your way of dealing with stress or anxiety
- a chemical imbalance in the brain, similar to obsessive compulsive disorder (OCD)
- changes in hormone levels during puberty
For some people, hair pulling can be a type of addiction. The more they pull their hair out, the more they want to keep doing it.
When to see a GP
See your GP if you're pulling your hair out or if you notice that your child is.
You should also see your GP if you or your child has a habit of eating hair. This can cause hairballs to form in the stomach, leading to serious illness.
This can cause hairballs to form in the stomach, leading to serious illness.
Your GP may examine areas where the hair is missing to check that nothing else is causing the hair to come out, such as a skin infection.
If your GP thinks you have trich, you may be referred for a type of treatment called cognitive behavioural therapy (CBT).
Treating trichotillomania
Trich is commonly treated using a type of CBT called habit reversal training.
This aims to help you replace a bad habit with something that's not harmful. Treatment usually involves:
- keeping a diary of your hair pulling
- working out the triggers for your hair pulling and learning how to avoid them
- replacing hair pulling with another action, like squeezing a stress ball
- loved ones providing emotional support and encouragement
Antidepressants are not are not usually prescribed to treat trich.
Things you can try yourself
Here are some tips from people with trich that may help when you feel the urge to pull your hair:
- squeeze a stress ball or something similar
- form a ball with your fist and tighten the muscles in that arm
- use a fidget toy
- wear a bandana or a tight fitting hat, such as a beanie
- come up with a saying that you repeat out loud until the urge to pull passes
- take a soothing bath to ease any stress or anxiety
- practise deep breathing until the urge to pull goes away
- exercise
- put plasters on your fingertips
- cut your hair short
Getting support
It may also help to open up about your trich to people you trust, as hiding it can sometimes make your anxiety worse.
Many people who have learned to manage their trich say that speaking to others about the condition led to a reduction in hair pulling.
The charity Trichotillomania Support has information on treatments and self-help advice.
Page last reviewed: 29 January 2021
Next review due: 29 January 2024
What It Is, Causes & Treatment
Overview
Missing patches of hair are a possible sign of trichotillomania.What is trichotillomania?
Trichotillomania (often abbreviated as TTM) is a mental health disorder where a person compulsively pulls out or breaks their own hair. This condition falls under the classification of obsessive-compulsive disorder (OCD). When it’s severe, it often has extremely negative effects on a person’s happiness, well-being and overall quality of life.
Trichotillomania (pronounced trick-oh-till-oh-main-ee-uh) comes from three Greek words:
- Tricho: hair.

- Tillo: pull.
- Mania: excessive behavior or activity.
What is the difference between trichotillomania and obsessive-compulsive disorder?
TTM falls under the overall category of obsessive-compulsive disorder, but it has some key differences from OCD itself.
- Obsessions. OCD involves obsessions, which are thoughts or urges that a person can’t control and doesn’t want. TTM doesn’t involve obsessions.
- Feeling of reward. When people with TTM pull out their hair, they often feel relief or other positive emotions. OCD doesn’t involve positive feelings in that way.
Who does it affect?
TTM is especially common in children and adolescents. In young children and infants, it’s usually a short-lived concern and goes away on its own. The more serious form most commonly starts between ages 10 and 13.
In children, it happens equally between men and women. In adults, women outnumber men with this condition by as much as 9 to 1.
How common is this condition?
TTM is relatively uncommon. Research studies estimate it affects 0.5% to 3.4% of adults at some point in their lifetime.
How does this condition affect my body?
People with TTM compulsively pull out their hair, usually one strand at a time. Many people will pull hair from the same spot. The most common places people pull hair from are their scalp, eyelashes and eyebrows, and pubic hair.
The effects of trichotillomania also depend on the age at which it happens. Children commonly pull their hair in this way, but that behavior is often a self-soothing act. Children often grow out of this behavior and don’t have any long-term negative effects. Adolescents, teenagers and adults with this condition tend to have much more severe problems.
Mental health effects
People with TTM commonly feel anxiety, embarrassment or shame about this condition. This can affect their work and social lives. Many people with this condition don’t seek treatment because they feel embarrassed or ashamed.
Trichophagia
About 20% of people with this condition eat their hair after pulling it, a condition known as trichophagia (from Greek words “tricho” for hair and “phagia” for eating). This can lead to hairball-like blockages in their digestive tract. Those blockages are sometimes dangerous and often cause damage that needs surgery to repair.
People with TTM commonly hold back from telling their healthcare provider about this even after revealing details about TTM. This is often because they’re waiting until they feel they can trust their provider more before sharing that amount of detail.
Hair, skin and tissue damage
People who pull out their hair often cause damage to their skin and tissue just underneath the skin’s surface, especially if they use any kind of personal care tool like tweezers. Skin and tissue damage sometimes need repair or skin grafting to fix. Damage to skin caused by hair pulling can also cause permanent hair loss in affected areas.
Symptoms and Causes
What are the symptoms of trichotillomania?
According to the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders Fifth Edition (better known as the DSM-5), the diagnosis of TTM requires a person to meet five criteria:
- Repeated pulling out of hair that causes hair loss.
- Trying multiple times to stop this behavior or do it less often.
- Feeling that hair pulling negatively affects your life, especially your work and social life.
- The hair pulling or hair loss isn’t happening because of another condition (such as a skin-related disorder or problem).
- The hair pulling isn’t happening because of another mental health condition. An example of this is body dysmorphia, where hair pulling happens because a person believes there’s a problem with their appearance and is trying to fix it).
Some people with TTM pull their hair deliberately, such as when they feel a hair is out of place or looks different from others around it. Other people pull their hair automatically without thinking about it.
What causes trichotillomania?
While experts suspect several possible factors could lead to TTM, there aren’t any confirmed causes of this condition. Some of the suspected factors include:
- Genetics.
 TTM may happen because of certain DNA mutations. More research is needed to confirm this.
TTM may happen because of certain DNA mutations. More research is needed to confirm this. - Changes in brain structure or chemistry. People with TTM often have changes to certain areas in their brains or differences in their brain chemistry.
- Coping mechanism. Many people with TTM describe it as starting after a stressful time in their life. Others describe it starting because of boredom and that pulling their hair became a habit over time.
Other conditions that happen with TTM
There are several mental health conditions that a person is much more likely to have along with TTM. These can happen either as separate conditions or because of TTM (especially anxiety and depression). These include:
- OCD (this condition is a common misdiagnosis for people who, in reality, have TTM).
- Major depressive disorder.
- Anxiety disorders.
- Substance use disorders (alcohol and drugs).
Is it contagious?
No, TTM isn’t contagious, and it can’t spread to others. While some experts suspect it might be something you can inherit from your parents, more research is necessary to confirm that.
While some experts suspect it might be something you can inherit from your parents, more research is necessary to confirm that.
Diagnosis and Tests
How is trichotillomania diagnosed?
Diagnosing TTM involves a combination of a physical exam, where your healthcare provider looks for visible signs of the condition. They'll also ask questions about your health history, current circumstances and anything else that might have a connection to a medical problem.
TTM is a relatively straightforward condition to diagnose, but people with this condition often hide it out of shame or embarrassment. That can make it harder for your healthcare provider to diagnose this condition based solely on asking questions. That’s why a specific type of skin test may also help.
What tests will be done to diagnose it?
In some cases, a “punch biopsy” (where your healthcare provider takes a skin sample for lab analysis) is necessary to confirm a diagnosis of TTM. This test can also rule out other skin conditions that might be the true cause of hair loss or hair pulling.
In cases where your healthcare provider suspects a blockage from swallowed hair, you might also undergo other diagnostic tests. These include imaging tests like a computerized tomography (CT) scan, blood testing for anemia and more.
Management and Treatment
How is it treated, and is there a cure?
Treating TTM often involves therapy, medication or a combination of both. Ongoing research shows some medications for other mental health conditions might help TTM, but more research is necessary before any specific medication becomes a part of the standard care.
What medications and treatments are used?
Medication alone often isn’t enough to treat TTM. Healthcare providers may use combinations of medications, therapy techniques or both.
Medications
Medications that may treat, either on their own or in combinations, TTM include:
- Antidepressants. Selective serotonin reuptake inhibitors (commonly referred to as SSRIs) and tricyclic antidepressants can sometimes help with reducing the impulse to pull hair.
- Antipsychotics. These medications help balance your brain chemistry. While the name sounds like they have only one use, they actually treat many conditions, including dementia, bipolar disorder and schizophrenia.
- Anticonvulsants. These medications typically help treat seizures and other disorders that affect muscle movements, but they also can help with TTM.
- Nutraceuticals. These are nutrition products, such as amino acid supplements, that can help treat medical conditions.
Therapies
Therapy methods that may help treat TTM include:
- Habit reversal therapy. This method involves helping you become more aware of your behaviors and activity patterns. By helping you become more aware, this therapy teaches you to break habits like hair pulling. This method has the best odds of success out of any treatment option for TTM.
- Group therapy and peer support.
 People with TTM may benefit from specific types of group therapy or support.
People with TTM may benefit from specific types of group therapy or support.
People with TTM with hair loss or scarring may need to see other healthcare providers and specialists. In some cases, a dermatologist can help treat related skin problems or damage. Plastic and reconstructive surgeons may also help with skin grafting for affected areas of your body. Other healthcare providers can also offer solutions related to hair regrowth; though, regrowth isn’t always an option.
Complications/side effects of the treatment
The possible side effects that can happen with medications depend on the medications themselves, as well as your medical history and circumstances. Your healthcare provider can tell you more about possible side effects, including potential trouble signs and how you should react if you see those signs. They’re the best source of information about this because they can tailor the information they give you to your specific health needs, situation and circumstances.
How to take care of myself/manage symptoms?
TTM isn’t a condition you should diagnose on your own. That’s because a trained and experienced mental healthcare provider is better prepared to determine if you have TTM or another health condition. It’s also not something you should treat on your own, partly because both medication and therapy methods often need a prescription or other input from a healthcare provider.
How soon after treatment will I feel better?
The time it takes for you to feel better from medication, therapy or a combination of the two can be very different from person to person. Your healthcare provider can tell you more about what you can expect as you undergo treatment and what you can do to help yourself through the process.
Prevention
How can I reduce my risk or prevent this condition?
TTM is a mental health condition, which means it isn’t preventable. There’s also no known way of reducing your risk of developing it.
Outlook / Prognosis
What can I expect if I have this condition?
TTM isn’t usually a danger to your physical health (except in rare cases, especially when a person develops a digestive tract blockage from hair they’ve swallowed). However, it can be very disruptive and damaging to your mental health and quality of life.
Because people with TTM often feel ashamed or embarrassed of this condition, most avoid treatment. Those who avoid or delay treatment are much more likely to have issues like permanent hair loss, scarring and more severe mental health problems.
How long does TTM last?
The available research, while limited, shows that people with TTM have this condition for an average of about 22 years. In some cases, the condition is a lifelong problem. People also often describe that the condition has phases, becoming more or less severe for periods of time. Overall, early diagnosis and treatment are the best chance for limiting how long this condition lasts and how severely it impacts your life.
What’s the outlook for this condition?
The overall outlook for this condition depends partly on the age of the person who has it. Infants and children with TTM often have the best outlook, with the condition commonly going away on its own.
However, the older a person gets — especially from adolescence onward — the greater the odds that treating the condition becomes difficult. TTM on its own is rarely a life-threatening problem. But its impacts on a person’s life, especially their mental health, are often severe. Because of this, early diagnosis and treatment are very important.
Living With
How do I take care of myself?
If you have TTM, it’s important to see a healthcare provider (or multiple providers) with specialized training and experience in treating this condition. They can best guide you on what you can do to minimize the impact of this condition on your life.
In general, healthcare providers recommend the following:
- Be honest about what you’re experiencing.
 TTM is a medical condition that affects your mind and behaviors. Much like you would see a healthcare provider for a broken bone or an ear infection, you should also see a healthcare provider for mental health conditions like TTM. They can help treat your condition and help you deal with any negative emotions you’re facing in connection with it.
TTM is a medical condition that affects your mind and behaviors. Much like you would see a healthcare provider for a broken bone or an ear infection, you should also see a healthcare provider for mental health conditions like TTM. They can help treat your condition and help you deal with any negative emotions you’re facing in connection with it. - See your healthcare provider(s) as recommended. This is especially important for therapy sessions and other mental health visits.
- Take medications as prescribed, if prescribed. Medications can often help decrease how strongly or often you feel the urge to pull your hair.
When should I go to ER?
People with TTM who swallow their hair have a higher risk of blockages in their digestive tract. These blockages often cause severe or even life-threatening complications. The following symptoms are likely with a blockage and mean you should call your healthcare provider or go to the hospital:
- Changes in the color of your stool (poop) to dark green or black.

- Nausea and vomiting.
- Unexplained or unexpected weight loss.
- Diarrhea or constipation.
- Belly pain or discomfort.
A note from Cleveland Clinic
Trichotillomania, or hair pulling, can have a severe effect on your mental health. People with this condition often feel ashamed, embarrassed or guilty because of it. If you have TTM or know someone who does, it’s important to remember this is a medical condition and that hair pulling is very difficult to control or stop on your own. But with treatment, it’s possible to limit how often you pull your hair or stop pulling it. That can help you live a life where your hair and appearance don’t make you feel anxious or ashamed, so you can focus on things that matter most to you.
causes, symptoms, diagnosis and treatment
I confirm More
- INVITRO
- Library
- Disease Handbook
- Trichotillomania
Alopecia
Depression
Neurosis
1653 09 September
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
For a correct assessment of the results of your analyzes in dynamics, it is preferable to do studies in the same laboratory, since different laboratories may use different research methods and units of measurement to perform the same analyzes.
Trichotillomania: causes, symptoms, diagnosis and treatment.
Definition
Trichotillomania (TTM) is a chronic traumatic alopecia caused by a mental disorder characterized by regular pulling out of one's own hair from the scalp, eyebrows, eyelashes, pubis and other parts of the body. Patients with TTM often suffer from other mental disorders (eg, depression, neurosis).
Trichotillomania can be an independent disease or develop against the background of bipolar disorder, schizophrenia, organic brain damage.
The first signs of trichotillomania appear, as a rule, in childhood or adolescence, although cases of TTM manifestation in adults have been described - in this case, the prognosis for cure is less favorable.
Statistics show that the prevalence of pathology is approximately 0.9%, but doctors say that the numbers may be higher, since many patients do not seek medical help.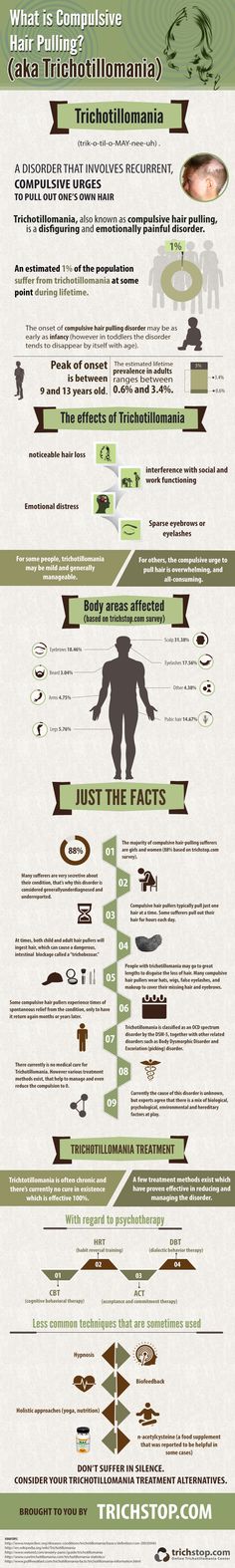 Women suffer from trichotillomania twice as often as men.
Women suffer from trichotillomania twice as often as men.
Causes of trichotillomania
The main reason for the formation of the hair pulling habit lies in the psychological problems of the patient: the disease can develop against the background of stress, increased anxiety, self-doubt, difficult relationships in the family (lack of mutual understanding causes chronic stress in the child, which can become trichotillomania).
There is a theory, which does not yet have solid evidence, about the hormonal nature of TTM. Its supporters focus on the fact that in many patients the manifestation of the disease coincides with the period of puberty, when there are significant changes in the hormonal background.
Classification of the disease
According to the ICD-10 classification, trichotillomania belongs to section F63 “Disorder of habits and drives”.
Trichotillomania can be unconscious (automatic), when the patient does not realize that he is pulling out his hair, and conscious, when pulling out his hair becomes a response to a stressful situation, increased tension and allows for some time to get rid of anger, frustration and anxiety. A combination of these two types of TTM is also possible.
A combination of these two types of TTM is also possible.
Trichotillomania is classified based on the age of the patient when the disease debuted:
- childhood trichotillomania occurs in children 2-6 years of age;
- adolescent trichotillomania develops at 11-15 years of age;
- bidominal trichotillomania is manifested by two clinical peaks: first in preschool and then in adolescence;
- adult trichotillomania.
Symptoms of trichotillomania
Specific manifestations of trichotillomania include pulling out one's own hair, twisting it around a finger, sucking, cases are described when patients chew and swallow their torn hair. Patients with TTM can often touch their hair without even pulling it out, and the act of pulling out their hair always brings them emotional relief.
The clinical picture of the disease is represented by foci of total alopecia of irregular shape (bald patches can be localized where there is hair, but more often on the crown and crown) or areas with sparse hair (in this case, hair broken off at different heights, with split ends, or rolled into rings).
Pinpoint hemorrhages (hemorrhages) can be visualized on the skin due to hair pulling. With total hair pulling, hemorrhagic crusts and erosions, foci of lichenification (thickening and thickening of the skin) are often formed.
Hair pulling usually does not bring any pain to patients, since the sensitivity in these areas of the skin is reduced.
Diagnosis of trichotillomania
Diagnosis of TTM is difficult, because patients do not recognize the fact of hair pulling, and the clinical picture of trichotillomania is similar to other alopecia, so in about 50% of cases, patients with TTM are initially diagnosed with alopecia areata. Differentiation of two pathologies allows the analysis of the totality of pathological trichoscopic signs and key disease markers. Trichotillomania is characterized by the preservation of pigmented short hair and different lengths of hairs, with alopecia areata, the hair is discolored and thin.
To detect the disease, trichoscopy is considered the main diagnostic method - a computer study of the condition of the hair and scalp using a trichoscope, which is equipped with a video camera and magnifying optics.
Trichotillomania is distinguished by the presence of several types of hair: hair with normal ends, hair with ends in the form of a brush, twisted hair. Many empty follicles are found, some of them with black patches of remnants of the hair shaft (trichomalacia). Histological examination may be required to clarify the diagnosis.
Key disease markers include:
- habit of regularly touching and pulling hair;
- emotional tension before hair-pulling;
- emotional relaxation after hair-pulling;
- absence of other dermatological and trichological pathologies.
The fluorescent test is used in cases where the patient and his relatives do not recognize the fact of hair pulling. To conduct the test, the hair is treated with fluorescent ink, and every other day the skin of the hands is examined under a Wood's lamp. A characteristic glow of the skin indicates that the patient often touches his hair.
To conduct the test, the hair is treated with fluorescent ink, and every other day the skin of the hands is examined under a Wood's lamp. A characteristic glow of the skin indicates that the patient often touches his hair.
The doctor may recommend a study of the composition of the hair for trace elements in order to prescribe drugs for hair restoration.
Small hair trace element screening
Up to 5 working days
Available with home visit
4 410 RUB
Add to cart
Which doctors to contact
With problems of hair thinning and total baldness, patients turn to trichologists and dermatologists. Of course, these specialists are engaged in local therapy.
Nevertheless, trichotillomania is a mental disorder, so its treatment should be comprehensive, and one cannot do without the help of a psychiatrist.
However, if a patient does not present to a doctor for trichotillomania, the disorder may be suspected general practitioner during a visit for a different reason, paying attention to the bald patches and the emotional status of the patient.
Treatment of trichotillomania
First of all, patients with trichotillomania need the help of psychiatrists and psychologists. Doctors find out what factors or circumstances lead to episodes of hair pulling, and give recommendations on how to eliminate or minimize them. For treatment, hypnosis, psychotherapy and antidepressants can be used, and in the presence of itching - glucocorticosteroids locally.
Some studies show that as an adjunctive therapy, the patient, when feeling the urge to pull his hair, can begin to do self-massage of hands, touch beads or rosary.
Complications
Since it is common for some patients to swallow torn hairs (trichophagia), there is a risk of clumps of hairs forming in the stomach, making it difficult to pass and digest food and may require surgery.
Another consequence of constant hair pulling is infection of the injured skin.
If the patient pulls out hair for a long time, hair growth may stop altogether.
Prevention
Preventive measures in childhood are reduced to educational moments: children who are prone to anxiety and self-doubt should not be criticized, set strict limits on them and compared with others - in other words, it is important for such children to ensure a minimum level of stress.
Adolescents and adults should avoid stressful situations as much as possible and relieve emotional tension through sports (eg swimming).
Sources:
- Tikhonovskaya I.V., Lesnichaya O.V. Trichotillomania: clinic, diagnosis, differential diagnosis, treatment // Medical News.
 No. 1, 2014. S. 12-15.
No. 1, 2014. S. 12-15. - Efanova E. N., Rusak Yu. E., Gorshkova A. V., Vasilyeva E. A. Trichotillomania and trichobezoar in a teenager: a clinical case. Questions of modern pediatrics. 2019; 18(2): 134-137. doi:10.15690/vsp.v18i2.2016
IMPORTANT!
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
For a correct assessment of the results of your analyzes in dynamics, it is preferable to do studies in the same laboratory, since different laboratories may use different research methods and units of measurement to perform the same analyzes.
Recommendations
-
Rett syndrome
20118 18 October
-
Keratoconus
219 18 October
-
Clubfoot
19634 17 October
Show 9 more0003
Thyroiditis
Myxedema
Infertility
Osteoarthritis
Gallstone disease
Depression
Dementia
Alopecia
Bradycardia
Hypothyroidism
Hypothyroidism: causes, symptoms, diagnosis and treatment.
More
Climax
Menopause
Hypertension
Diabetes mellitus
Obesity
Hormonal disorders
Migraine
Neurosis
Multiple sclerosis
Myoma
Vulvit
Cervicitis
Depression
Anxiety disorders
Frigidity
Frigidity: causes, symptoms, diagnosis and treatment.
More
Mania
Brad
Depression
Bipolar affective disorder (BAD)
Bipolar affective disorder: causes, symptoms, diagnosis and treatment.
More
Vegetovascular dystonia
Depression
Nervous breakdown
Neuroses
Patients with neuroses are characterized not only by complaints of anxiety and depression, but also by symptoms such as palpitations, feeling of a coma in the esophagus, pain and dyspepsia. At the initial stage, the treatment of neuroses can be very effective, so it is important to notice these disorders in time.
At the initial stage, the treatment of neuroses can be very effective, so it is important to notice these disorders in time.
More
Neurosis
Traumatic brain injury
Asthenia
Attention deficit hyperactivity disorder (ADHD)
Vegetative-vascular dystonia
Depression
Hyperhidrosis
Sleep disorder
Neurasthenia
Neurasthenia: causes, symptoms, diagnosis and treatment.
More
Subscribe to our newsletters
Enter e-mail
I consent to processing of personal data
Subscribe
Trichotillomania — diagnosis and treatment at the Allianz Central Medical Health Center
Trichotillomania is the compulsive pulling of hair on the head, sometimes on the face or body. In this case, visible areas of baldness are formed, often symmetrically located. The area of baldness is gradually increasing. Often patients, especially children, are ridiculed and judged. But it is important to understand that hair pulling is a disease, not a whim, and patients cannot get rid of this habit on their own.
But it is important to understand that hair pulling is a disease, not a whim, and patients cannot get rid of this habit on their own.
Important
Trichotillomania should be diagnosed and treated by an experienced psychotherapist or psychiatrist.
The disease is more common in women. There is also children's trichotillomania. Patients usually try to hide areas of baldness. Often, trichotillomania is combined with trichophagia (eating torn hair) and nail biting.
Causes and diagnosis of trichotillomania
Unfortunately, for trichotillomania, the causes are not fully understood. There is a genetic theory of the occurrence of this disease. The disease often accompanies other mental disorders - schizophrenia, depression, obsessive-compulsive disorder.
Children may experience conflicts in the family, excessive pressure or violence. When a patient—adult or child—pulls out their hair for trichotillomania, the euphoria causes a reduction in stress levels and a release of tension.
With trichotillomania, the hair follicles are preserved. Accordingly, over time, hair can grow back.
Often, patients pull out their hair automatically and do not notice their actions, denying the disease, and sometimes they hide the torn hair or eat it. Unlike hair loss, which is associated with hormonal or other problems in the body, with trichotillomania, the hair follicles are preserved. Accordingly, over time, hair can grow back.
The diagnosis of "trichotillomania" is established in the presence of foci of baldness. To identify concomitant mental disorders and problems, it is necessary to consult a psychotherapist and a pathopsychological study by a clinical psychologist. If indicated, the doctor prescribes a study of hormone levels.
How to help people with trichotillomania
Trichotillomania is treated by a psychotherapist. It will help to reveal the hidden causes that lead to the tension that the patient relieves in such a categorical way. The subconscious mind hides traumatic situations so deeply that it is often not so easy to bring them to the surface, this may require more than one session of work with a doctor. Preventive shaving or wearing a cap have limited effectiveness, because they do not solve the problem, but only affect the manifestation of the disease.
The subconscious mind hides traumatic situations so deeply that it is often not so easy to bring them to the surface, this may require more than one session of work with a doctor. Preventive shaving or wearing a cap have limited effectiveness, because they do not solve the problem, but only affect the manifestation of the disease.
Therefore, the most effective solution for those who are thinking about how to get rid of trichotillomania is to contact an experienced psychotherapist. The doctor will conduct a comprehensive examination, identify the causes and features of the course of the disease and prescribe an effective treatment. In addition to individual psychotherapy for the treatment of trichotillomania, restorative methods can be used - physiotherapy, massage, body-oriented therapy (relaxation), as well as individually selected medication.
Treatment methods for trichotillomania of the first order are individual and family psychotherapy with drug support.