Self directed cognitive behavioral therapy
Discovering New Options: Self-Help Cognitive Behavioral Therapy
NOV. 01, 2016
By Seth J. Gillihan
As a therapist, I’ve repeatedly seen the same research conclusions: a few sessions of cognitive-behavioral therapy (or CBT) can be very helpful in treating anxiety and depression. CBT’s simple yet powerful changes to the way we think and act can have profound impacts on our health and well-being.
However, many people don't have access to a CBT therapist—maybe they’re not close by or they're not in-network or they're prohibitively expensive. It’s also tough to take time off work or child care every week to see a therapist.
If you’ve wanted to try CBT for anxiety or depression but aren't able to see a CBT therapist, you may not need to. Many studies have found that self-directed CBT can be very effective. Two reviews that each included over 30 studies (see references below) found that self-help treatment significantly reduced both anxiety and depression, especially when the treatments used CBT techniques.
The average amount of benefit was in the “moderate” range, meaning people didn’t feel 100% better, but were noticeably less anxious and depressed.
(Note: Self-help CBT is probably most appropriate for someone with mild to moderate symptoms who is generally able to function well. A person who is severely depressed and barely able to get out of bed is probably not a good match, and will likely need one-on-one treatment with a professional.)
Studies also show that people tend to maintain their progress over time, which is very encouraging. One of the goals of CBT is to "become your own therapist" by learning skills you can use on your own after treatment to keep feeling well.
If you're interested in self-directed CBT, the Association for Behavioral and Cognitive Therapies maintains a list of books they've given their "seal of merit." I also recently wrote a book on CBT for anxiety and depression called Retrain Your Brain: Cognitive Behavioral Therapy in 7 Weeks.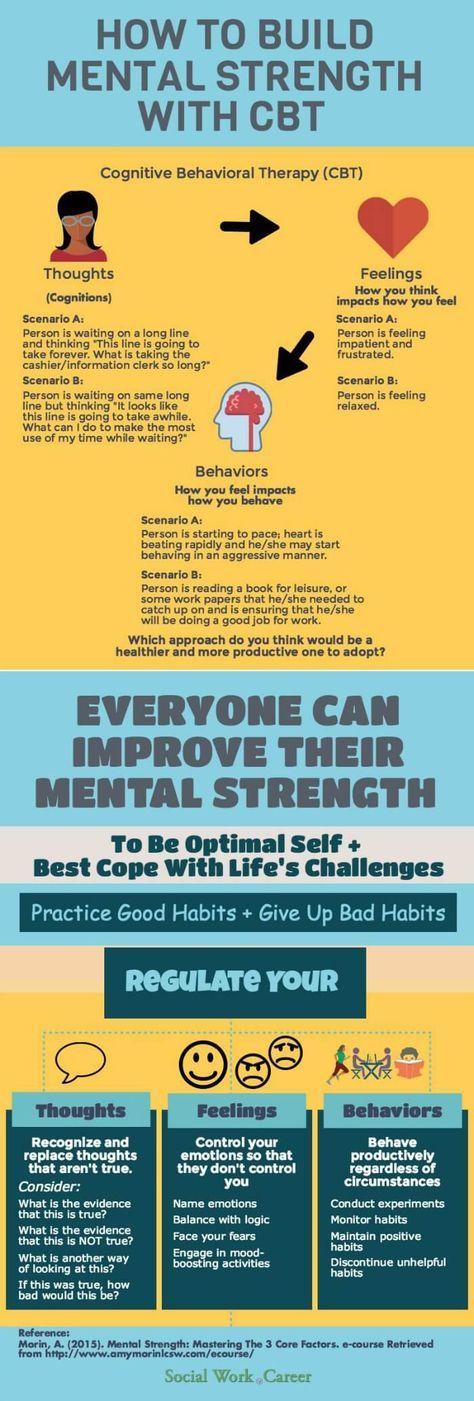 The workbook is meant to present the best-tested tools of CBT in a user-friendly way over the course of several weeks. The exercises included are similar to what I do when I'm working with someone in-person.
The workbook is meant to present the best-tested tools of CBT in a user-friendly way over the course of several weeks. The exercises included are similar to what I do when I'm working with someone in-person.
The cognitive techniques found in my book and others include:
- Identifying your thought patterns.
- Discovering how your thoughts affect your feelings and behaviors.
- Determining if your thoughts are accurate.
- Replacing biased thoughts with more realistic ones.
Common behavioral techniques include:
- Scheduling activities that bring you enjoyment and a sense of accomplishment.
- Recognizing how your actions influence your thoughts and emotions.
- Making the best use of your time.
- Breaking down daunting tasks into more manageable ones.
- Facing your fears gradually so they diminish.
These approaches are fairly simple and obvious. What drew me to CBT was how straightforward and intuitive it was, which also makes it well-suited for self-directed therapy. The following guidelines might be helpful if you decide to pursue self-directed CBT:
The following guidelines might be helpful if you decide to pursue self-directed CBT:
- Find a book that resonates with you. People are drawn to different approaches, tones, level of detail, etc. If a book feels like a good fit, there's a better chance you'll stay engaged with it.
- Choose a book that is based on solid research. Self-help therapy takes considerable time and effort, so it's worth directing your energy toward a program that has a solid grounding.
- Make room in your schedule to focus on the program. While there's a good chance you'll always have competing activities, it's better to avoid periods in your life when you're truly overextended and the therapy is likely to get pushed to the side.
- Follow the program as closely as possible. It's easy to want to skip parts of a program we’re already familiar with or we think won't work. One of the dangers with that is if we find a program doesn't help, we won't know if it's because it wasn't right for us or because we only did part of it.
 Sticking to the instructions gives us the best chance of benefiting.
Sticking to the instructions gives us the best chance of benefiting.
In a time of high anxiety, rising depression rates, soaring health care costs and limited insurance coverage for mental health, self-directed psychological treatments have many advantages. Completing a program that's right for you can lower your anxiety, improve your mood and provide you with skills you can use as often as you need them.
Seth J. Gillihan, PhD, is a licensed psychologist and Clinical Assistant Professor of Psychology in the Psychiatry Department at the University of Pennsylvania. He has a clinical practice in Haverford, PA, where he specializes in CBT and mindfulness-based interventions for the treatment of anxiety, depression, OCD, and insomnia. Dr. Gillihan writes the ThinkActBe blog on PsychologyToday.com, and can be found at sethgillihan.com
We’re always accepting submissions to the NAMI Blog! We feature the latest research, stories of recovery, ways to end stigma and strategies for living well with mental illness.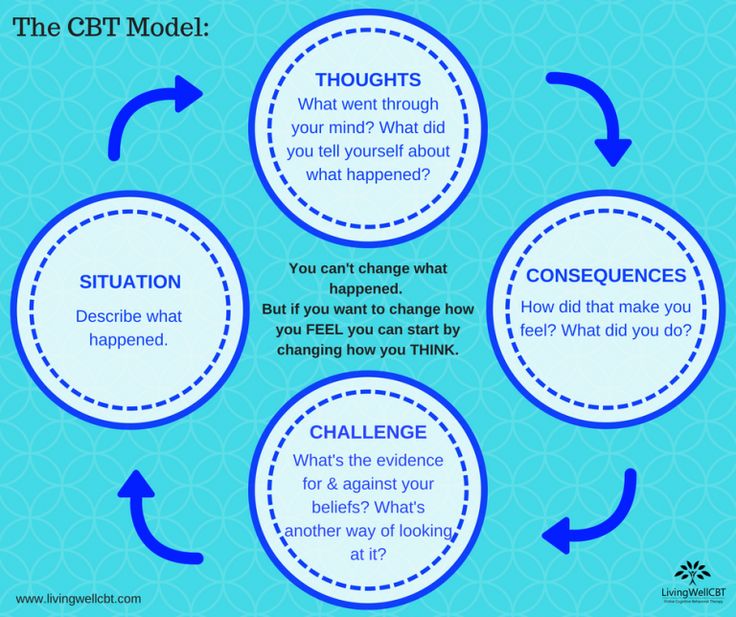 Most importantly: We feature your voices.
Most importantly: We feature your voices.
Check out our Submission Guidelines for more information.
LEARN MORE
Your Ultimate Interoceptive Exposure Therapy Guide
When fearful, we experience a range of physical sensations, including sweating, shaking, shortness of breath, and a pounding heart (McCabe & Milosevic, 2015).
One theory suggests that panic disorder is the outcome of sensitivity to such physical sensations and, as a result, can be treated by intentionally recreating them. Treating this vulnerability can be particularly valuable for clients who are overly sensitive to anxiety (Lee et al., 2006).
This article explores interoceptive exposure therapy, along with some real-life examples, and introduces exercises and worksheets to guide therapists and clients along the journey to a positive outcome.
Before you continue, we thought you might like to download our three Positive Psychology Exercises for free. These science-based exercises explore fundamental aspects of positive psychology, including strengths, values, and self-compassion, and will give you the tools to enhance the wellbeing of your clients, students, or employees.
This Article Contains:
- What Is Interoceptive Exposure in Therapy?
- 4 Real-Life Examples
- 6 Proven Benefits of Interoceptive Exposure
- How to Do Interoceptive Exposure: A Guide
- 6 Worksheets & Exercises for Your Sessions
- Resources From PositivePsychology.com
- A Take-Home Message
- References
What Is Interoceptive Exposure in Therapy?
Interoceptive exposure therapy can be helpful in the treatment of panic and anxiety disorders and phobias.
“This technique involves the planned and predictable confrontation of one’s own feared object or situation” and intentionally exposes clients to the bodily sensations they typically experience at that time (McCabe & Milosevic, 2015, p. 138). They learn that while uncomfortable, such sensations are ultimately not harmful.
This approach is particularly helpful in treating clients who fear the physical sensations accompanying their panic, anxiety, or phobia more than the mental event itself. An essential part of the process involves understanding whether fear of the physical sensations plays a role in their phobia (McCabe & Milosevic, 2015).
An essential part of the process involves understanding whether fear of the physical sensations plays a role in their phobia (McCabe & Milosevic, 2015).
Interoceptive exposure therapy attempts to recreate feared physical sensations through different exercises. Examples include:
- Spinning around on a swivel chair or turning your head from side to side to simulate feelings of dizziness or light-headedness
- Fast, shallow breathing to recreate a racing heart
- Running up stairs and experiencing being out of breath to simulate breathlessness
The above actions recreate sensations that often accompany phobias or panic and may be more feared than the object or event itself.
Interoceptive exposure vs in vivo exposure
“Exposure procedures have two forms: exposure to environmental situations that each person fears, termed in vivo exposure; and exposure to exercises that evoke the physical sensations associated with panic attacks” (Lee et al.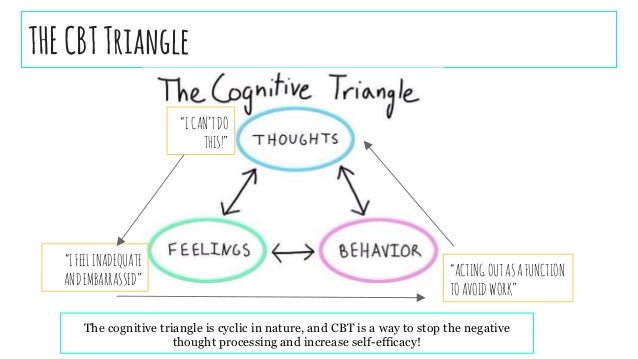 , 2006, p. 2).
, 2006, p. 2).
For example, in vivo exposures may involve taking the client to an airport if they are frightened of flying or increasingly higher in a building if they are fearful of heights. On the other hand, interoceptive exposure focuses on recreating the sensations that accompany flying or heights, perhaps the noise of an airplane, changing pressure in the ears, or feelings of nausea.
Can it help with panic disorders?
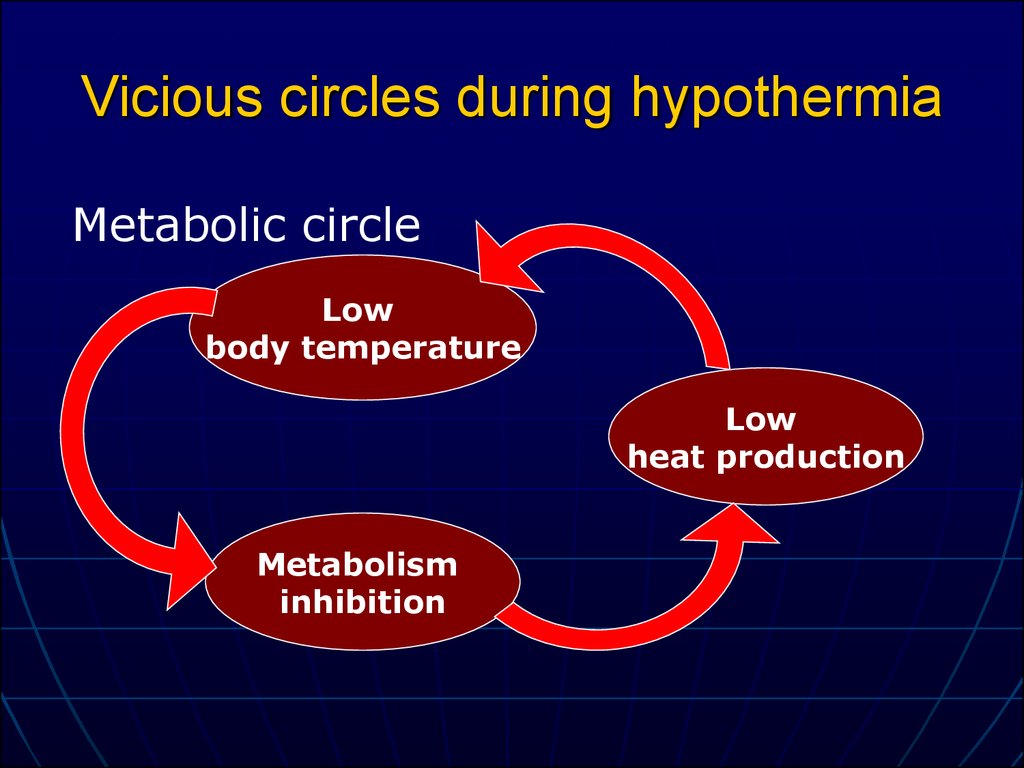
Interoceptive exposure therapy has had considerable success with treating panic disorders. Theory suggests that panic disorder may be “conceptualized as a phobic fear of physical sensations caused by traumatic conditioning from unexpected panic attacks and catastrophic misinterpretation of physical sensations” (Lee et al., 2006, p. 2). This fear of the fear may be tackled head on by re-exposure to sensations causing discomfort.
4 Real-Life Examples
“Interoceptive exposures are often used with individuals who have specific phobias, especially when their fear is related to the physical sensations that are triggered when faced with the feared object or situation” (McCabe & Milosevic, 2015, p.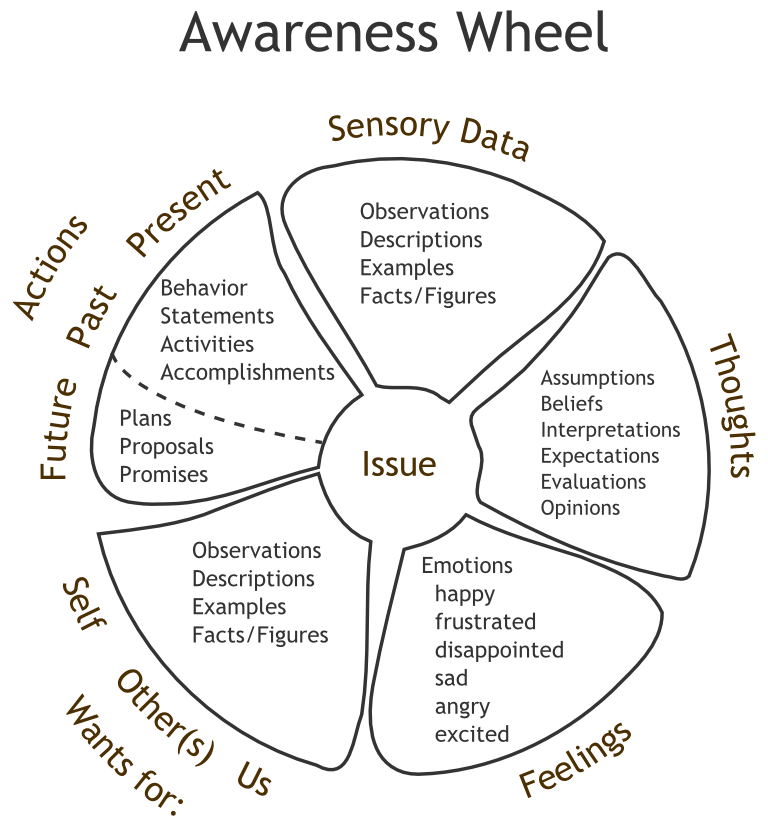 138). Here are some examples of such conditions.
138). Here are some examples of such conditions.
Claustrophobia
An individual who experiences fear of small or enclosed spaces may find extreme discomfort in the physical sensation the situation brings about.
For example, hyperventilation (overly rapid and deep breathing, which is commonly associated with panic) may be perceived as a lack of air and even suffocation, leading to further terror.
Fear of heights
Those with a fear of heights often experience a feeling of weakness in their legs when they are high up. They may perceive such sensations as falling, further exacerbating their fear and increasing feelings of panic.
Injection phobias
A phobia of injections or having blood taken can be accompanied by light-headedness, a source of panic in itself. The fear associated with the symptom may be worse than the needle, event, or environment and spiral the experience out of control.
Post-traumatic stress disorder (PTSD)
PTSD is closely linked to anxiety sensitivity and may enhance symptoms of hyperarousal and hypervigilance.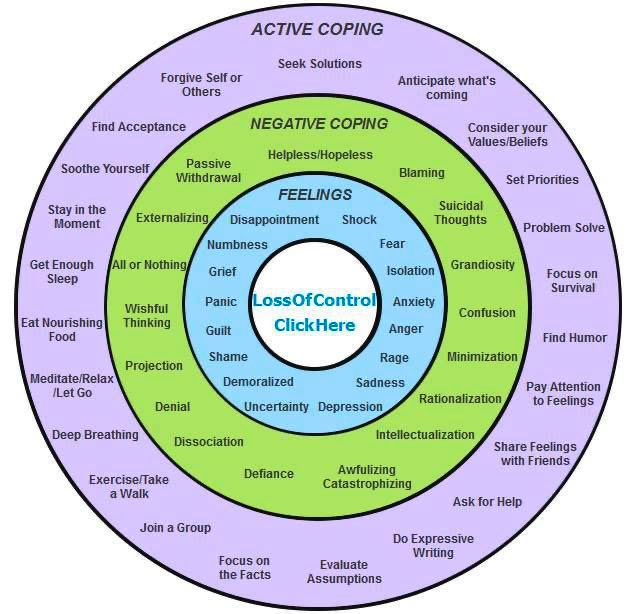 Perhaps unsurprisingly, interoceptive exposure therapy has proven helpful in treating even those PTSD patients with treatment-resistant symptoms (Boettcher, Brake, & Barlow, 2016).
Perhaps unsurprisingly, interoceptive exposure therapy has proven helpful in treating even those PTSD patients with treatment-resistant symptoms (Boettcher, Brake, & Barlow, 2016).
6 Proven Benefits of Interoceptive Exposure
Repeated exposure to physical sensations is a successful treatment plan for clients with anxiety disorders and phobia. Interoceptive exposure therapy offers several benefits, including (Lee et al., 2006; McCabe & Milosevic, 2015):
- “Habituation of anxiety in patients with panic disorder” (Lee et al., 2006, p. 2).
- The practice provides evidence against the belief that physical sensations associated with fear and panic are dangerous.
- Repeatedly practicing interoceptive exposure leads clients to become familiar and even accustomed to their sensations.
- Therapy can be planned, repeated, and is largely predictable.
- The treatments are controllable; the degree of exposure can be managed and reduced as needed, especially when the client is reluctant.

- Exercises can be repeated at home without the need for specialist treatment.
In the future, interoceptive exposure therapy may prove successful in treating other conditions, including depression, eating disorders, and low self-esteem (Boettcher et al., 2016).
How to Do Interoceptive Exposure: A Guide
There are many different exercises to bring on the physical sensations feared by the client; it is, therefore, crucial to understand the client and their experience of their phobia or the nature of their panic (McCabe & Milosevic, 2015).
Treatment process
- Step one:
The therapist must identify which interoceptive exposures will be most helpful in treatment.
Often the treatment begins by inducing a series of different physical sensations and noticing which ones produce the most significant fear or are most similar to those that result from the phobic situation.
- Step two:
Build a hierarchy of interoceptive exposure practices; they should be ranked from least to most anxiety provoking and discussed with the client.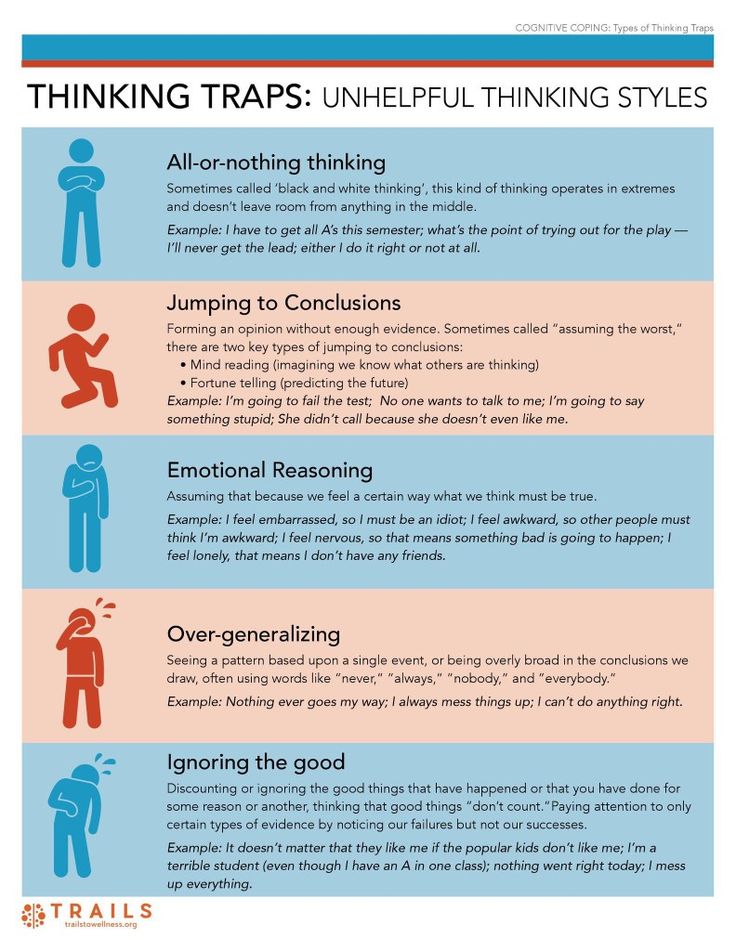 Then work through the list in the order agreed.
Then work through the list in the order agreed. - Step three:
The client needs to practice interoceptive exposure exercises, beginning with practices that invoke a minor reaction. Once these have been mastered, the client will work their way up, finishing with the most reactive techniques.
A gradual, increasingly challenging approach appears most successful with clients, especially those who are reluctant to engage in more impactful practices and are at risk of dropping out (McCabe & Milosevic, 2015).
McCabe and Milosevic (2015) also offer some valuable guidelines that should be reflected in both the design and performance of interoceptive exposure therapy practices.
Exposures should:
- Be planned and predictable (the client retains control)
- Be performed frequently (most likely, daily)
- Lead the client to experience anxiety
- Encourage clients to refrain from avoidance strategies (using distraction, alcohol, etc.
 )
) - Enable clients to stay in the anxiety-provoking space until it decreases
- Be practiced in multiple situations to generalize its effect
- Set the client up for success, not failure
“Through repeated practice, people eventually become accustomed to their sensations” (McCabe & Milosevic, 2015, p. 139).
Typical treatments
Interoceptive exposure procedures began by tackling phobias and panic anxiety using biochemical substances, including caffeine, lactate infusions, and even carbon dioxide inhalation; now, more typically, therapists use a selection of the following methods (Boettcher et al., 2016):
Breathing- Overbreathing, involving fast and deep breathing
- Breathing through a straw while holding your nose
- Holding your breath
- Spinning on a swivel chair with eyes open or closed
- Shaking the head from side to side, then focusing on something straight ahead
- Running in place, up the stairs, or stepping up onto a low bench
- Muscle tensing – one muscle group at a time or the whole body
- Placing your head between your legs then sitting up quickly
All of these exercises can be used by the therapist and practiced by the client to provoke or induce feelings associated with panic or anxiety (Boettcher et al.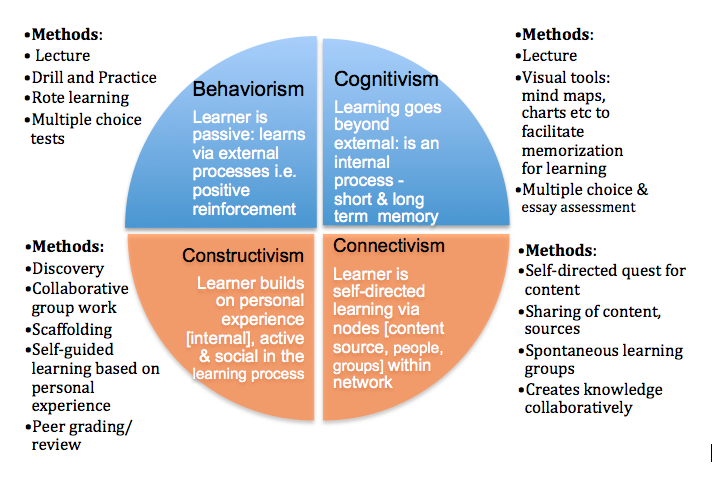 , 2016).
, 2016).
6 Worksheets & Exercises for Your Sessions
Interoceptive techniques often focus on “reproducing sensations from one of the four somatic domains typically reported by patients having panic attacks” (Boettcher et al., 2016, p. 5), including the following:
- Cardiovascular sensations, including racing heart
- Audiovestibular sensations, including dizziness
- Respiratory sensations, including shortness of breath
- Dissociative sensations, including depersonalization and derealization
Therapists and researchers continue to explore other techniques and practices to provoke the sensations clients experience during panic or in connection with phobias.
The following therapy worksheets can help identify and focus on helpful interoceptive exposure techniques.
Understanding Your Anxiety and Triggers
Anxiety, panic, and the fear of the sensations accompanying them can lead people to avoid the situations they believe will trigger those feelings.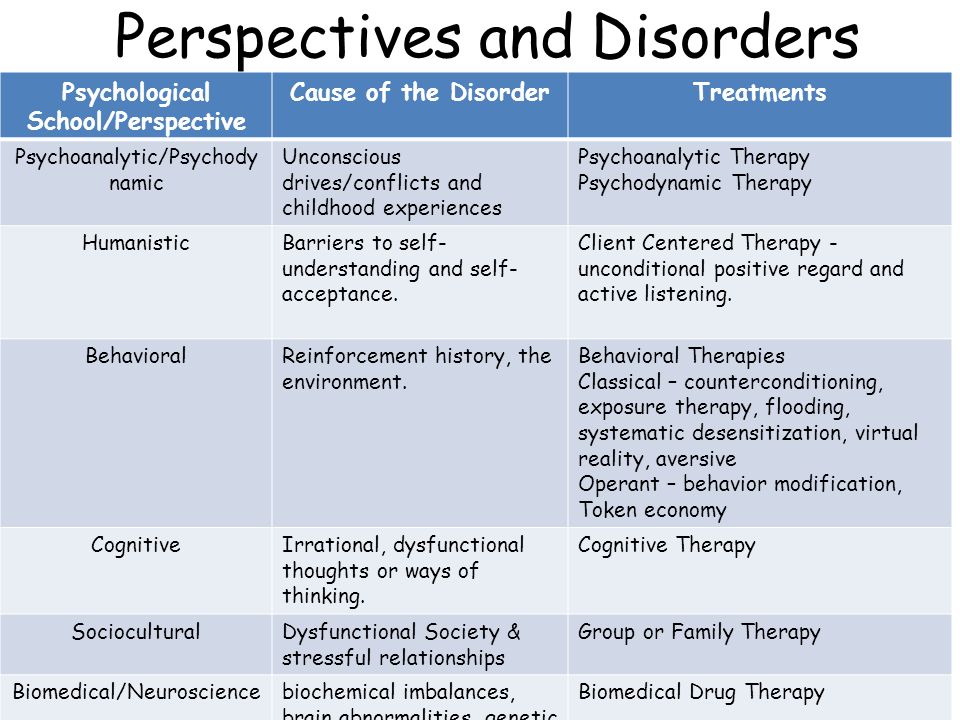
The Understanding Your Anxiety and Triggers worksheet helps clients identify which anxiety triggers lead to avoidance and require focus during interoceptive exposure therapy.
The client is asked to identify five triggers and ask themselves the following questions:
Am I avoiding any of these triggers because of my anxiety?
Are there occasions when I experience the triggers and react in ways I don’t want?
Therapy provides an opportunity to work on these triggers, reduce their impact, and allow the client to continue their life as they wish.
Understanding the Severity of the Panic Disorder
While planning to use interoceptive exposure to treat panic disorder, it is essential to understand its severity and frequency.
The Understanding the Severity of the Panic Disorder worksheet can track the impact of the client’s panic disorder between sessions.
The following is a typical list of symptoms often experienced during a panic attack (Ehrenreich, Mattis, & Pincus, 2008).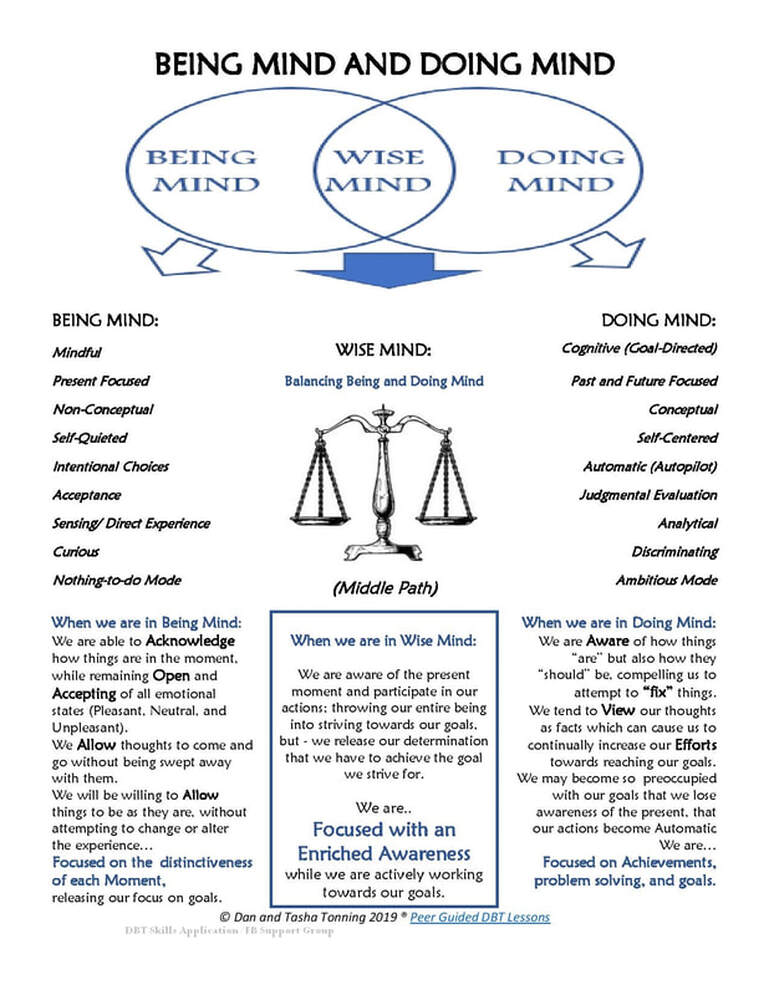
- Rapid heart rate
- Feeling of choking
- Numbness or tingling of muscles or skin
- Sweating
- Trembling
- Breathlessness
- Nausea
- Dizziness
- Feelings of unreality or “going crazy”
- Fear of dying
Experiencing two or more of these symptoms may indicate a panic attack.
Fear Hierarchy
Understanding the activities that cause fear, anxiety, and panic helps target appropriate interoceptive exposure therapy treatment.
The Fear Hierarchy worksheet considers several situations or activities that may induce fear.
For example:
- Going on vacation
- Going shopping
- Going to work
- Giving a presentation
- Going on a date
- Meeting friends
- Meeting new people
- Walking into a busy room
The negative sensations you experience are the ones you will need to focus on as part of interoceptive exposure therapy (Lee et al. , 2006; McCabe & Milosevic, 2015).
, 2006; McCabe & Milosevic, 2015).
Developing Interoceptive Exposure Therapy Interventions
As several interoceptive exposure techniques are available, therapists must first identify the sensations they need to recreate (McCabe & Milosevic, 2015).
The Developing Interoceptive Exposure Therapy Interventions worksheet considers the phobia or panic attack and explores the sensations that the therapist needs to address.
Work through the questions with the client. You may revisit the worksheet several times as understandings grow and you identify helpful practices.
Consider using the following techniques and record those that recreate the targeted sensations:
- Hyperventilating
- Breathing through a straw
- Running in place and stepping up onto a low bench
- Muscle tensing
- Spinning
- Head shaking
Create a plan to try out these techniques, starting with the least reactive practices. Only once the client has mastered them should you move on to more difficult ones.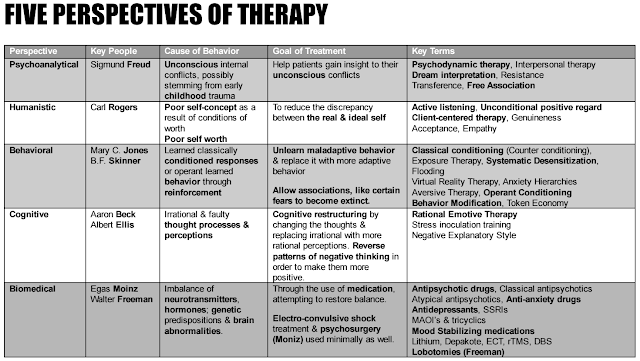
Interoceptive Exposure Therapy Practices
“Interoceptive exposures involve using different types of exercises to bring on feared physical sensations” (McCabe & Milosevic, 2015, p. 138).
The Interoceptive Exposure Therapy Practices worksheet introduces the client to three simple practices that they can try in the session or at home:
- Breathing:
Shallow breathing at a rate of 100–130 breaths per minute. - Dizziness:
Spinning around on a swivel chair (eyes closed if it helps). - Too much warmth:
Wearing multiple layers of clothing in a warm house, sitting in a car that’s too hot, or spending time in a sauna.
Each practice tests the client’s ability to deal with discomfort regarding the sensations they may experience when panicking or reacting to a phobia.
Therapist Interoceptive Exposure Record
It is essential to keep track of the outcome of interoceptive exposure treatments to identify what is appropriate and understand their effectiveness (Ehrenreich et al.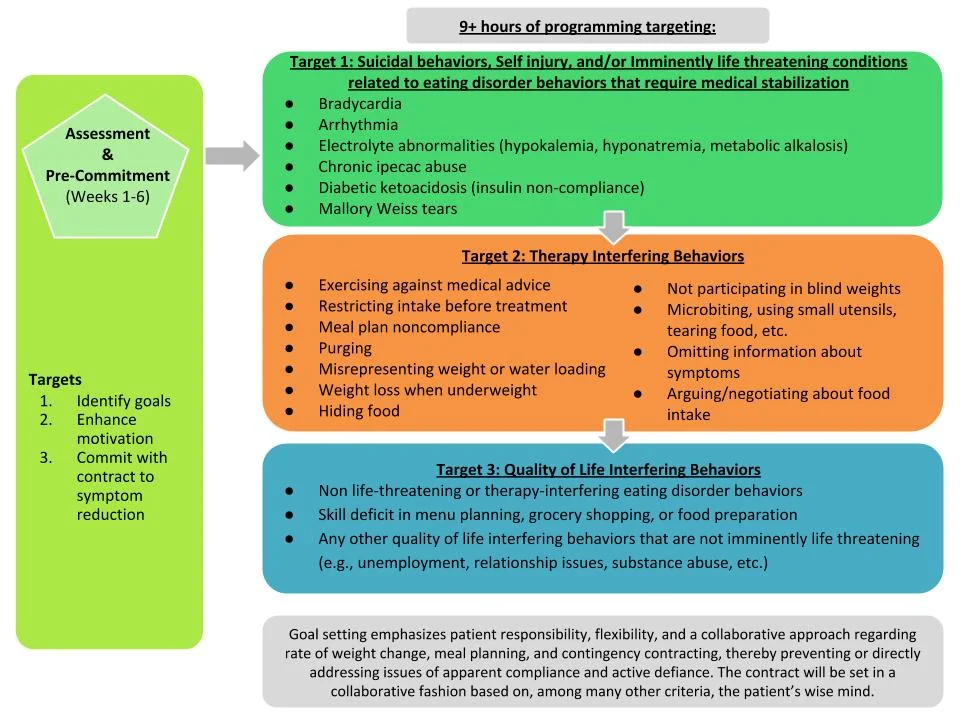.jpg) , 2008).
, 2008).
The Therapist Interoceptive Exposure Record helps the therapist log and track interoceptive exposure interventions.
Resources From PositivePsychology.com
Interoceptive exposure techniques bring on internal physical sensations to help clients learn how to manage fear, anxiety, and phobias.
We also have plenty of other techniques available to help clients cope with stress, anxiety, and panic.
Why not download our free stress and burnout prevention exercises pack and try out the powerful tools contained within? Here are some examples:
- Energy Management Audit
This checklist is designed to provide insights into the individual’s energy strengths and deficits that can leave the client ready for the day ahead or stressed, respectively. - The Stress-Related Growth Scale
This powerful questionnaire was built to assess and reveal the individual’s perceived positive outcomes from a stressful or traumatic event.
Other free resources include:
- Interoceptive Exposure
Learn the steps involved in multiple interoceptive exposure therapy exercises and become aware of the thoughts and physical symptoms that accompany each.
- STOP the Panic
The STOP acronym offers a useful way to manage feelings and thoughts in the moment and regain a state of calm.
More extensive versions of the following tools are available with a subscription to the Positive Psychology Toolkit©, but they are described briefly below:
- The Acceptance or Avoidance Route
Acceptance and Commitment Therapy helps clients live in line with their values. This exercise promotes acceptance of emotions by comparing acceptance-based coping and avoidance-based coping.
Use the tool to remind yourself how it is possible to take action despite the fear you are experiencing.
- Leaving the Comfort Zone
Entering discomfort can be scary and yet can be a way to experience new things and develop resilience.- Step one – Start by considering the difference between comfort, fear, learning, and growth zones.
- Step two – Work through an example to see how entering each zone can shape how you think and behave.
- Step three – Think of an existing situation in which you are firmly in your comfort zone.
- Step four – Consider how you would feel if you moved out of your comfort zone into the learning and growth zones.
- 17 Positive Psychology Exercises
If you’re looking for more science-based ways to help others enhance their wellbeing, check out this signature collection of 17 validated positive psychology tools for practitioners. Use them to help others flourish and thrive.
A Take-Home Message
Experiencing panic and phobias can be distressing, limiting our ability and capacity to interact with our environment and friends and set appropriate goals. And yet, the fear they generate may not be focused on the events or activities themselves, but on the sensations accompanying them.
Interoceptive exposure therapy takes a unique approach, bringing on internal physical sensations to help clients learn how to manage fear, anxiety, or phobia.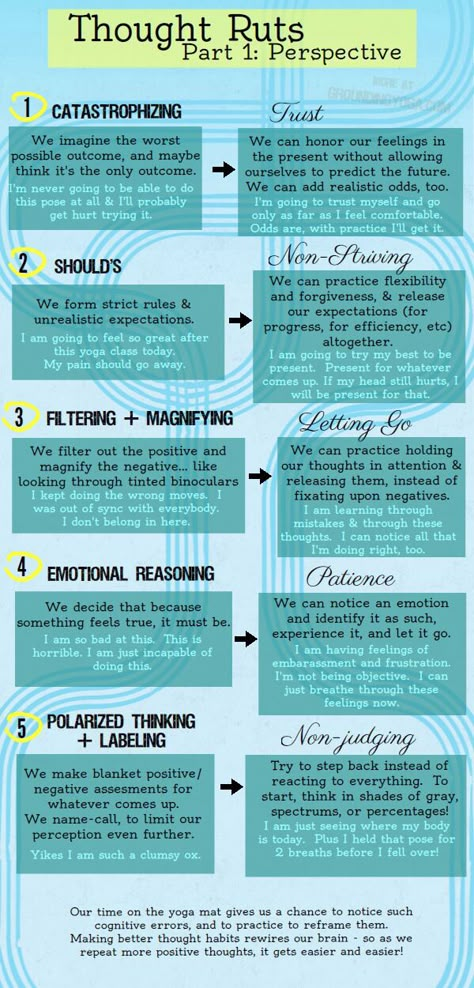 This unique method tackles the senses directly, rather than targeting thoughts and beliefs regarding the event or activity.
This unique method tackles the senses directly, rather than targeting thoughts and beliefs regarding the event or activity.
It may not be the fear of starting a new job or concerns regarding social occasions that need to be addressed, but rather the physical sensations experienced.
Interoceptive exposure engages the client directly in the overwhelming sensations that appear when they experience phobia or panic. Therapists can use these techniques on their own or with other therapeutic approaches to help the client handle situations that keep them from living a full and happy life.
We hope you enjoyed reading this article. Don’t forget to download our three Positive Psychology Exercises for free.
- Boettcher, H., Brake, C. A., & Barlow, D. H. (2016). Origins and outlook of interoceptive exposure. Journal of Behavior Therapy and Experimental Psychiatry, 53, 41–51.
- Ehrenreich, J. T., Mattis, S. G., & Pincus, D. (2008). Mastery of anxiety and panic for adolescents: Riding the wave: Therapist guide.
 Oxford University Press.
Oxford University Press. - Lee, K., Noda, Y., Nakano, Y., Ogawa, S., Kinoshita, Y., Funayama, T., & Furukawa, T. A. (2006). Interoceptive hypersensitivity and interoceptive exposure in patients with panic disorder: Specificity and effectiveness. BMC Psychiatry, 6(1).
- McCabe, R., & Milosevic, I. (2015). Phobias: The psychology of irrational fear. ABC-CLIO.
Cognitive Behavioral Therapy (CBT) or Cognitive Behavioral Psychotherapy (CBT)
FIND A PSYCHOLOGIST
We tell you how one of the most popular psychotherapy techniques works, which allows you to correct thinking and emotional reactions.
alter
DIRECTION GUIDE
Contents
Behaviorism and cognitivism
Basic concepts
Techniques and exercises
When will CBT help?
Course duration
Evidence-based medicine and CBT
Medical therapy and CBT
Case studies
What to read
What is CBT?
Cognitive Behavioral Therapy (or CBT) is a technique that highlights a person's unconscious motivations, transfers them to a conscious level, helps to change beliefs and behavior that cause neurotic and other pathological conditions.
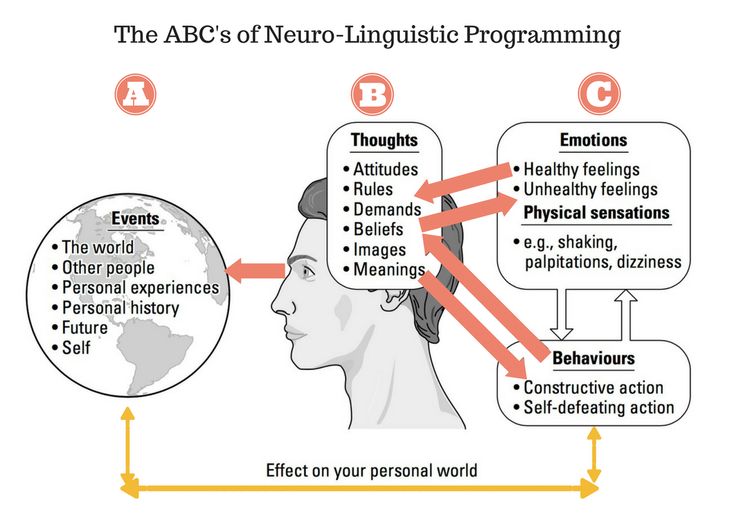
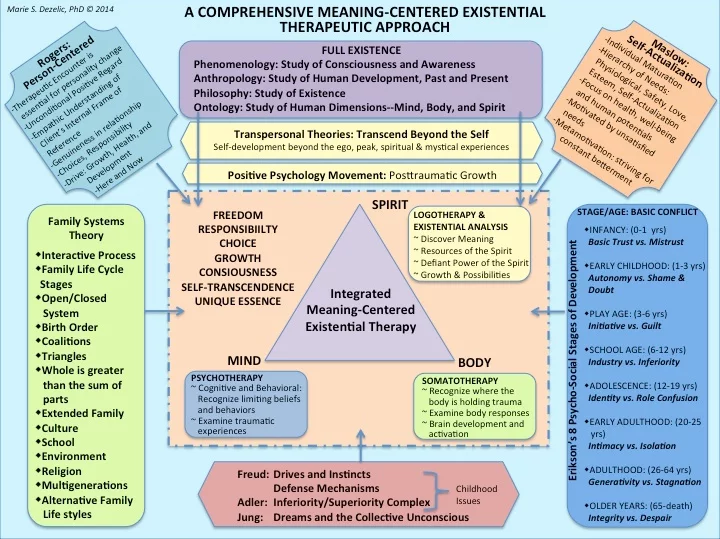
From the name it is clear that CBT combines two scientific psychological approaches: cognitive and behavioral (behavioristic). The first states that psychological problems and neuropsychiatric disorders are caused by thoughts and beliefs, stereotypes of thinking acquired during life. The second argues that human (as well as animal) behavior can be changed by encouraging desirable forms of action and not reinforcing undesirable behavior.
Behaviorism and cognitivism
The theory of behaviorism (from the English behavior - behavior) was developed in the early twentieth century. It considers behavior as a set of reactions (reflexes) to environmental stimuli. One of the basic concepts of behaviorism is positive and negative reinforcement. Positive reinforcement, or encouragement, is applied when the individual has done the right thing, and helps to reinforce the desired form of behavior. Negative reinforcement implies a negative reaction to the undesirable behavior of the trainee.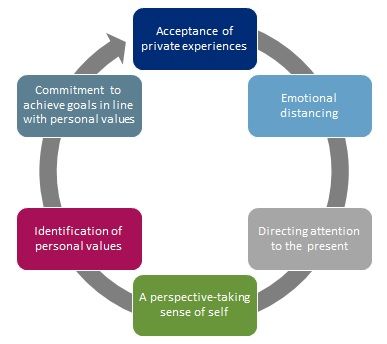 As a rule, the first form of reinforcement is used in CBT: it works faster, clearly indicates what needs to be achieved.
As a rule, the first form of reinforcement is used in CBT: it works faster, clearly indicates what needs to be achieved.
Cognitivism is a scientific movement that originated in the 1960s. It focuses on mental processes: how people perceive, think, remember, learn, solve problems, where they direct their attention. Cognitions are any thoughts and ideas that become the fruits of our thinking. According to the cognitive approach, it is inefficient to work only with a person’s behavior to solve his psychological problems: first, you need to identify beliefs, ideas and thoughts that make him act destructively or feel discomfort, get rid of them, and only then work on the behavioral aspect.
“Cognitions are basically all mental processes, both adequate and dysfunctional. When children are born, they don't know anything about the world yet. Over time, they begin to encounter people and their ideas about the environment. Parents and society help them formulate both adequate and dysfunctional beliefs.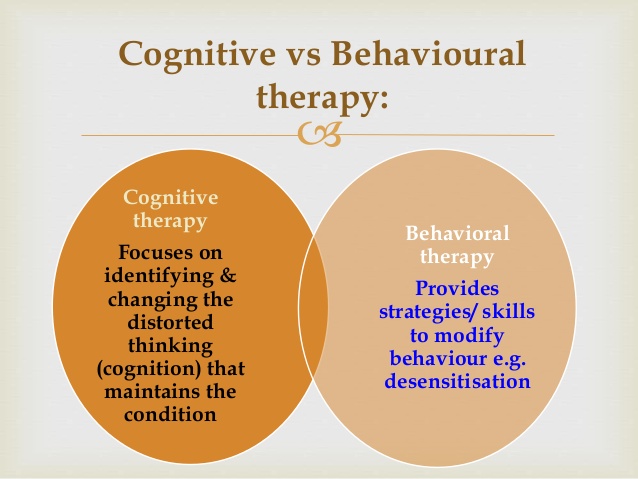 Dysfunctional and maladaptive views make it difficult to adequately assess life situations. Fears, complexes are formed, the child has a feeling that he is doing something wrong. It is this feeling that in the future leads to neurotic and other psychological problems.
Dysfunctional and maladaptive views make it difficult to adequately assess life situations. Fears, complexes are formed, the child has a feeling that he is doing something wrong. It is this feeling that in the future leads to neurotic and other psychological problems.
Anastasia Afanasyeva, Psychotherapist KPT:
Historically, the development of KPT is divided into 4 waves:
The first wave
(1910s-1950s)
Behavioral therapy
Second wave
(1960s)
Classical approach of CBT and rational-emotive psychotherapy
Third wave
(1990s)
Development of new currents within CBT: dialectical-behavioral psychotherapy, schema therapy, mindfulness therapy, acceptance and obligation therapy (ACT)
The fourth wave
(2010s)
The emerging stage associated with the use of modern technologies in therapy: augmented reality gadgets and software applications
In 1913, the American psychologist John Watson publishes the first articles on behaviorism. He urges his colleagues to focus exclusively on the study of human behavior, the study of the connection "external stimulus - external reaction (behavior)". Instead of analyzing the structural components of consciousness, behaviorists looked for reproducible connections between observed events, in particular between stimuli (environment) and responses (observed and measured reactions of people or animals to stimuli). Learning theories were the main model in the psychology of that time. Behaviorists have tried to formulate an explanation for how an organism establishes new connections between stimulus and response. Despite its early and sustained success, the behavioral approach placed many limitations on the therapy process.
He urges his colleagues to focus exclusively on the study of human behavior, the study of the connection "external stimulus - external reaction (behavior)". Instead of analyzing the structural components of consciousness, behaviorists looked for reproducible connections between observed events, in particular between stimuli (environment) and responses (observed and measured reactions of people or animals to stimuli). Learning theories were the main model in the psychology of that time. Behaviorists have tried to formulate an explanation for how an organism establishes new connections between stimulus and response. Despite its early and sustained success, the behavioral approach placed many limitations on the therapy process.
In 1955, the founder of rational-emotional psychotherapy, Albert Ellis, announced the influence of our thoughts and ideas (cognitions) on mental processes. His colleague Aaron Beck begins to study the field of knowledge. After evaluating the results of various methods of therapy, he comes to the conclusion that our emotions and behavior depend on the way we think.
Despite attempts by behavioral therapists to maintain their position in the late 1950s and early 1960s, the ideas of cognitivism became increasingly influential. Publication of the book by A.T. Beck on Cognitive Therapy for Depression (Beck et al., 1979), as well as studies showing that cognitive therapy treats depression as effectively as antidepressants (Rush, Beck, Kovacs & Hollon, 1977), changed psychotherapy forever. In subsequent years, behavioral and cognitive therapy developed together and influenced each other so strongly that they eventually merged into a single cognitive-behavioral approach.
Historical reference
Basic concepts: automatic thoughts, cognitive distortions
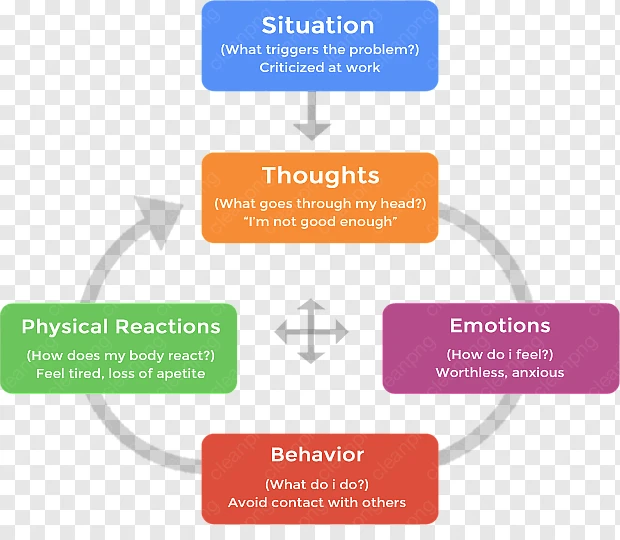
Search and awareness automatic thoughts - the basis of the CBT method. About 20 thousand of such quick thoughts arise in our head per day, which are a response to what is happening to us. They are always appreciated. Evolutionarily automatic thoughts are necessary so that we can quickly respond to changes in the environment. Most of them we do not have time to realize. These thoughts trigger our emotional response. In order to understand why our state has changed (anxiety, fear appeared, mood fell), it is necessary to identify what kind of thought caused this change. CBT suggests looking for quick thoughts in order to process them and translate your judgments into a rational channel.
Most of them we do not have time to realize. These thoughts trigger our emotional response. In order to understand why our state has changed (anxiety, fear appeared, mood fell), it is necessary to identify what kind of thought caused this change. CBT suggests looking for quick thoughts in order to process them and translate your judgments into a rational channel.
“There is always a situation that triggers a state change. For example, a person is walking in the dark and hears something rustling in the bushes. He becomes anxious. Most likely, the thought flashed that there was a danger nearby. In response to this thought and feeling of anxiety, the person decides to leave quickly. However, a quick thought and a reaction to it are not always rational. For example, you are doing a work task and realize that you do not have time to complete it on time. A neurotic person may have automatic thoughts: I am not responsible enough, I will be fired. The emotional response to them is anxiety, fear. Although if you think rationally, it is unlikely that one missed deadline will negatively affect your entire career.
Although if you think rationally, it is unlikely that one missed deadline will negatively affect your entire career.
Anastasia Afanasyeva, psychotherapist CBT:
Cognitive Behavioral Therapy works on cognitive distortions (or errors) that arise from automatic thoughts. Cognitive distortions are erroneous conclusions, irrational ideas that ultimately lead a person to psychological problems. There are over 100 types of cognitive distortions. Here are just a few examples:
Generalization
“I never have relationships”, “I always ruin everything”, “I always have bad luck”. A person carries over the characteristics of a single incident for life.
Catastrophe
“Everything is very bad”, “This is a failure”, “Irreparable happened”. Under the influence of negative judgments and emotions, the feeling of the situation is pumped up to complete hopelessness.
Duty
“I owe”, “They owe me”, “Everything should have turned out this way and not otherwise.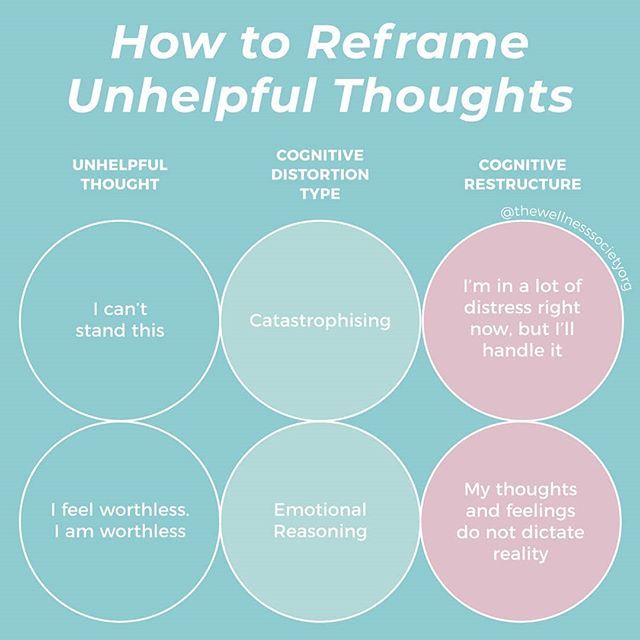 ” Social roles and responsibilities become immutable truths, neither the specifics of the situation, nor the state of the person, nor the complexity of relationships are taken into account.
” Social roles and responsibilities become immutable truths, neither the specifics of the situation, nor the state of the person, nor the complexity of relationships are taken into account.
Conformity
“Everyone does/behaves like this. Those who do otherwise are bad/inferior, etc.” Ideas about norms received from outside cause one to stigmatize the slightest deviation in oneself and others.
The task of the CBT therapist is to identify cognitive distortions that negatively affect the client's quality of life and help develop rational, constructive thought patterns in their place.
Techniques and exercises
One of the main techniques of the method is keeping a CBT diary . Usually it is a table in which you need to enter daily events that caused a strong emotional reaction, and analyze them according to the proposed scheme. Further cases are discussed with the therapist at the session.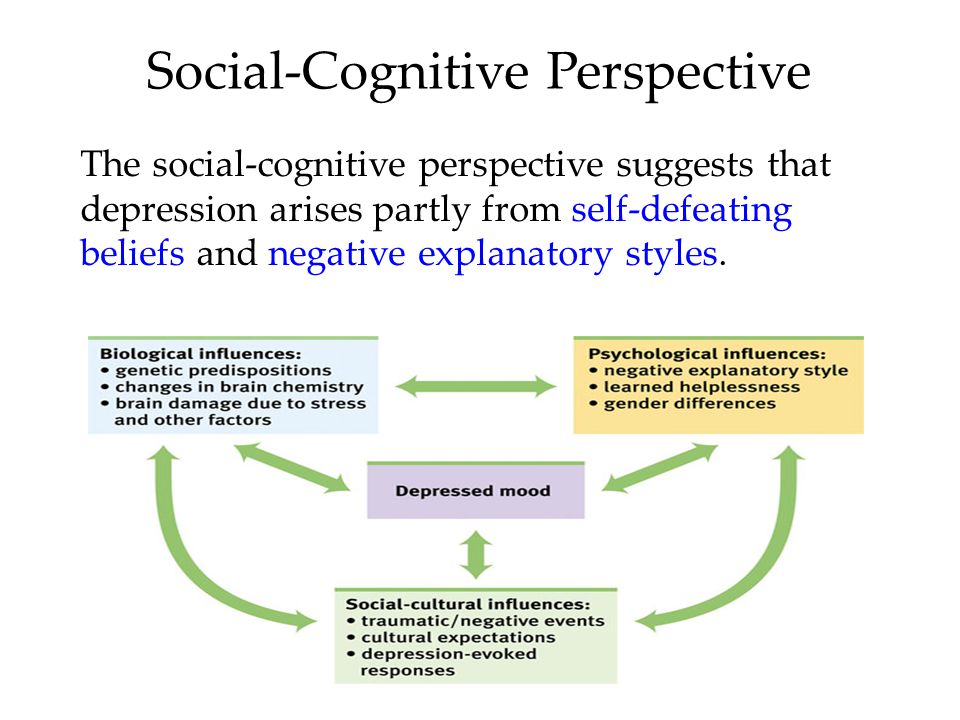
An example of what columns a CBT diary can contain. Each therapist offers his own diary system.
“After the client has learned to identify his automatic thoughts, he begins to keep a diary for a week. We look at what thoughts most often arise in different situations. This may be the fear that the person will look in someone's eyes as optional (that is, bad), or a feeling that he is not successful, or a feeling that he is vulnerable and will not cope. From the automatic thoughts we recognize, core beliefs begin to emerge. Not quick, superficial thoughts, but the foundation on which the human psyche is based. We are working on changing this array of beliefs in a rational direction.”
Anastasia Afanasyeva, CBT psychotherapist:
Another important technique for CBT is exposure . It is especially useful in all kinds of phobias. Exposure helps the client learn not to avoid disturbing situations, but to experience them.
For example, a person is afraid to enter an elevator. When using the exposure technique, the client and therapist approach the booth, stop, and begin to observe the client's reaction. When the anxiety rises, they do exercises with the therapist to help them cope with the anxiety. If the reaction is managed, the client and therapist move on to the next step: they enter the elevator together. The level of anxiety rises again, the therapist again works out with the client his condition. The intensity of the situation gradually increases until the client receives all the necessary skills in order to be aware and rationally assess his condition, to cope with it.
When will CBT help?
The effectiveness of the CPT is proved for the following states:
All types of phobia
Alarm
Panic disorder and panic attacks
Depression
Occupation and compulsive disorders (OKR)
9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 thoughts, actions, rituals
Psychosomatic disorders
irritable intestine, headaches and another
post -traumatic stress disorder
Eating disorders
Difficulties with communication, building contacts and their maintenance, constancy in the work and family relations
Dependencies 9000,0003
Physical and physical mental
Aggressive behavior
CBT in panic attacks
Panic attacks are spontaneous panic attacks that are accompanied by rapid breathing, palpitations, dizziness, tremor, nausea, sweating and other somatic manifestations.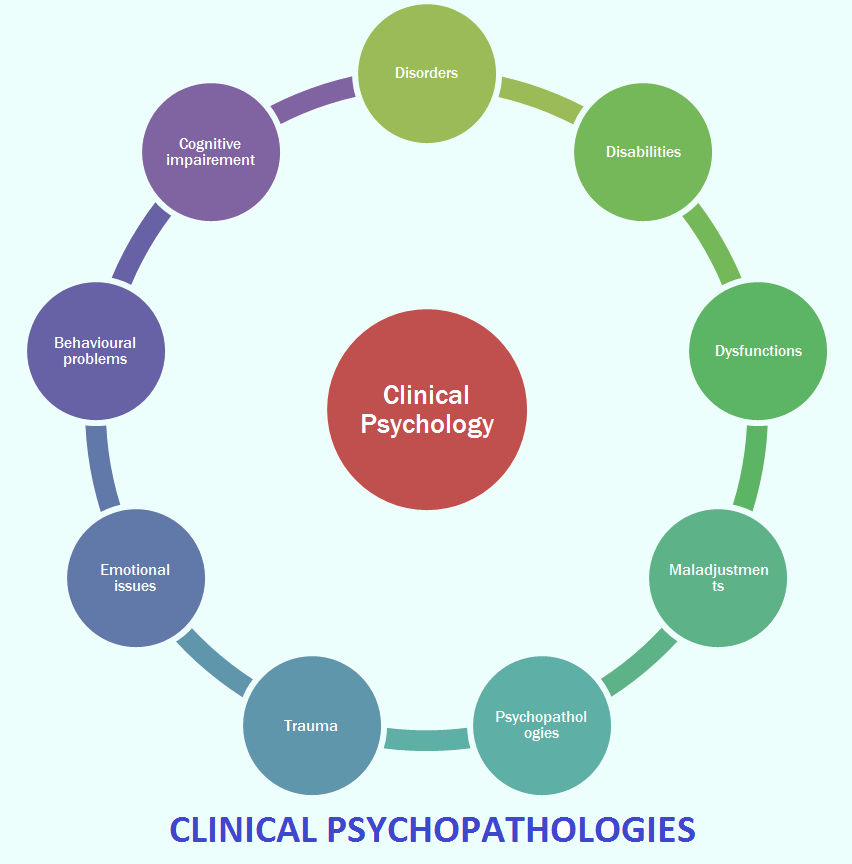
A panic attack may be the result of other psychiatric disorders rather than a single illness. Recurrent panic attacks without other symptoms may be manifestations of panic disorder. Cognitive behavioral therapy is the proven and most effective treatment for it.
“Panic attacks can occur in depressive disorders, generalized anxiety disorder, and hypochondriacal disorders. This is a very non-specific symptom, such as fever. It is found in various diseases. To make an accurate diagnosis, before starting treatment, you need to be diagnosed by a psychiatrist or psychotherapist.
Anastasia Afanasyeva, psychotherapist CBT:
The exposure technique mentioned above is very well the main tool for dealing with panic attacks. The psychotherapist teaches the patient to recognize what is happening to him at the time of the attack, how and to what his body reacts. Gradually, the patient learns to cope with his condition.
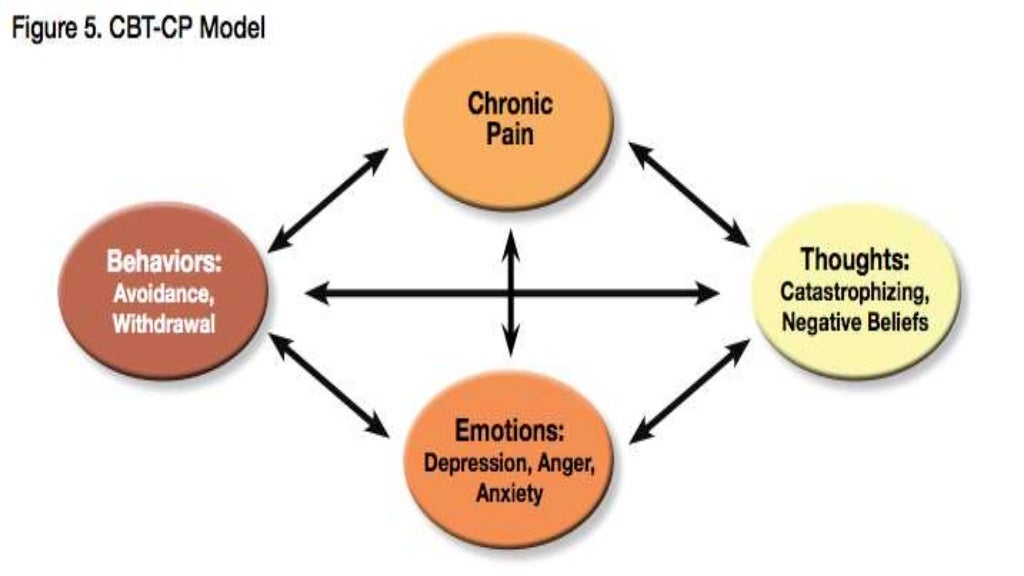
“First, there is a stage of psycho-education: we tell what happens in the patient's body at the time of the attack. We analyze cycles, thoughts, emotions, behavior, we are looking for the reason that starts the process. Further work is based on the fact that in the office we learn to cause symptoms: dizziness, palpitations, hyperventilation. We practice techniques to endure the anxiety that these symptoms cause. Thus, gradually we build tolerance. Anxiety decreases and eventually disappears.
We analyze cycles, thoughts, emotions, behavior, we are looking for the reason that starts the process. Further work is based on the fact that in the office we learn to cause symptoms: dizziness, palpitations, hyperventilation. We practice techniques to endure the anxiety that these symptoms cause. Thus, gradually we build tolerance. Anxiety decreases and eventually disappears.
Shortness of breath can be caused by hyperventilation - rapid shallow breathing. Dizziness - spinning in place. Palpitations - squats or running up the stairs. All exercises are performed together with the therapist. We say that it is not dangerous, the person understands this. When during the session I breathe with the patient, he sees that I normally endure this state. In doing so, he observes what happens to his own sensations.
The essence of a panic attack is that it always goes away. The fear that it will start, most often becomes the trigger for its start. It brings other problems as well, such as avoiding certain situations or carefully checking one's condition.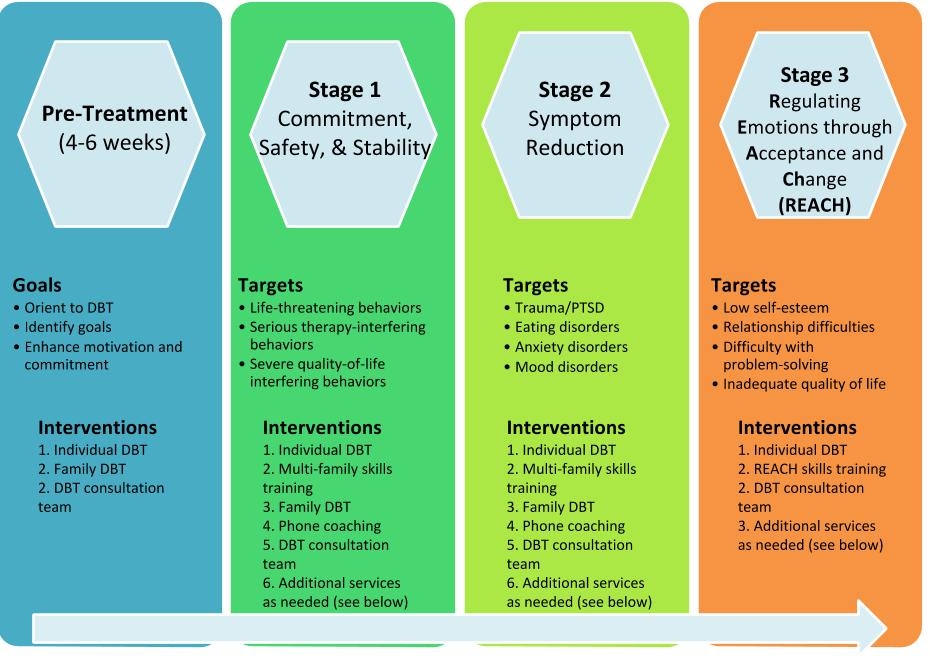 "
"
Anastasia Afanasyeva, psychotherapist CBT:
Duration of the course
CBT is considered a short-term therapy, but the duration of the course depends on many factors. For a specific request, such as a phobia or difficulty falling asleep, about 10 sessions are needed. However, this format involves solving only one problem. For multiple problems and more complex conditions, the course will last from a few months to a year. Treating personality disorders will require even longer work.
Therapy involves a meeting once a week, at a pre-selected time. The duration of the session is 50 minutes. Outside of sessions, the client does homework.
Each session has a structure: agenda, checking homework, discussing specific requests, working through them, debriefing, receiving homework, feedback.
« Terms are always individual and depend on the severity of the condition.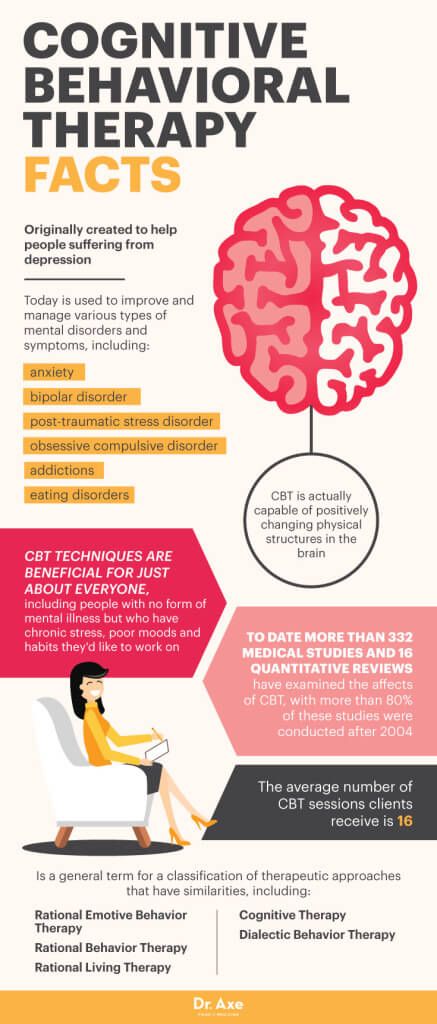 For panic attacks or depression, this is six months to a year. For complex diseases or personality disorders, therapy can be very long. In addition to the form and severity of the disease, the ability and desire of a person to get involved in work play a role. There are people who are more prone to reflection, it is easier for them to realize their own mental processes. There are people who find it harder.
For panic attacks or depression, this is six months to a year. For complex diseases or personality disorders, therapy can be very long. In addition to the form and severity of the disease, the ability and desire of a person to get involved in work play a role. There are people who are more prone to reflection, it is easier for them to realize their own mental processes. There are people who find it harder.
As with any therapy, one should not expect miracles from CBT. You cannot change in a couple of months, and even in six months. But you can learn to see the relationship between your thoughts, emotions and behavior, and this will allow you to weed out unnecessary thoughts, change reactions, not be led by your beliefs left by your parents and the outside world, and not let anxiety and fear rule your life.
Anastasia Afanasyeva, CBT psychotherapist:
Evidence-based medicine and CBT
Cognitive Behavioral Therapy (CBT) is one of the most researched methods of psychotherapy.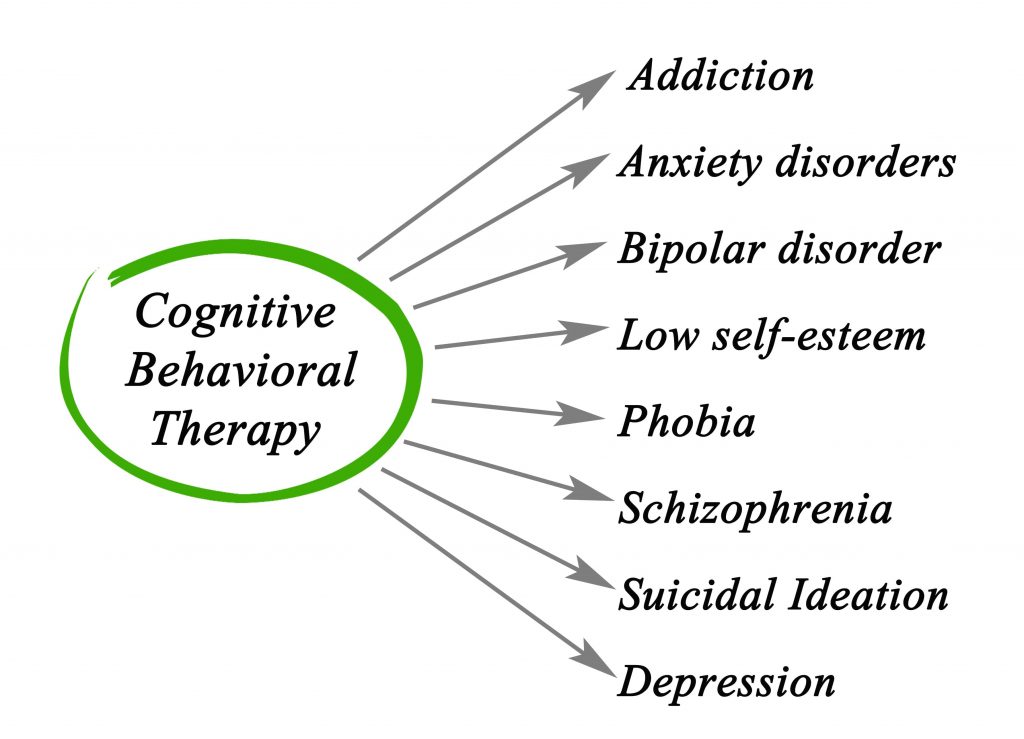 In 2012, a Boston University Department of Psychology Working Group released a seminal systematic review of meta-analyses (1) of various studies, which is the most comprehensive scientific paper on the effectiveness of CBT to date. Based on 269 papers, the researchers concluded that the referral was extremely effective in dealing with anxiety and mood disorders, highly effective in treating phobias, insomnia, and significantly effective in reducing workplace stress. The full text of the review in English can be found here.
In 2012, a Boston University Department of Psychology Working Group released a seminal systematic review of meta-analyses (1) of various studies, which is the most comprehensive scientific paper on the effectiveness of CBT to date. Based on 269 papers, the researchers concluded that the referral was extremely effective in dealing with anxiety and mood disorders, highly effective in treating phobias, insomnia, and significantly effective in reducing workplace stress. The full text of the review in English can be found here.
1 Meta-analysis is a type of data analysis in which the results of a number of randomized clinical trials are combined and analyzed as a single large study. In evidence-based medicine, meta-analysis is assigned the highest level of evidence (IA).
Medication and CBT
There are a number of conditions that can be treated with non-medicated CBT, such as mild generalized anxiety disorder, panic disorder, mild OCD, mild depression.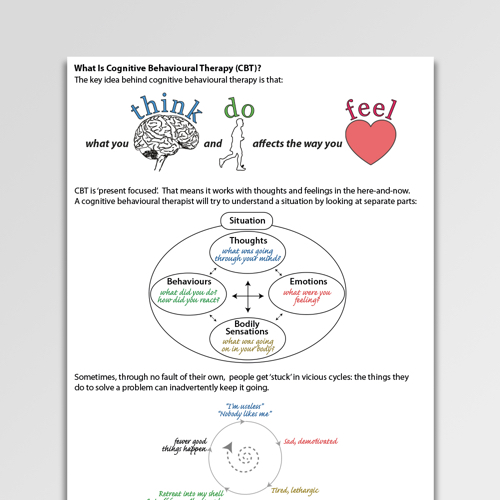 However, in a number of conditions, it is recommended to combine psychotherapy with pharmacotherapy. These include moderate depression and severe depression.
However, in a number of conditions, it is recommended to combine psychotherapy with pharmacotherapy. These include moderate depression and severe depression.
« Fear of pharmacotherapy is quite common and I deal with it regularly. I can say that many fears are unfounded. There is a myth that antidepressants are addictive. According to all studies, no antidepressant causes either mental or physical dependence.
If you have a fear of medication, see a qualified doctor who is trained in psychotherapy and pharmacotherapy. He will conduct a medical diagnosis, decide whether it is really necessary to carry out drug therapy, and help work through your fear using CBT techniques.”
Anastasia Afanasyeva, psychotherapist CBT:
Case reports
“A young man asked for help: after breaking up with a girlfriend, he suffered from depressed mood, anxiety, difficulty falling asleep, obsessive thoughts before going to bed, loss of appetite .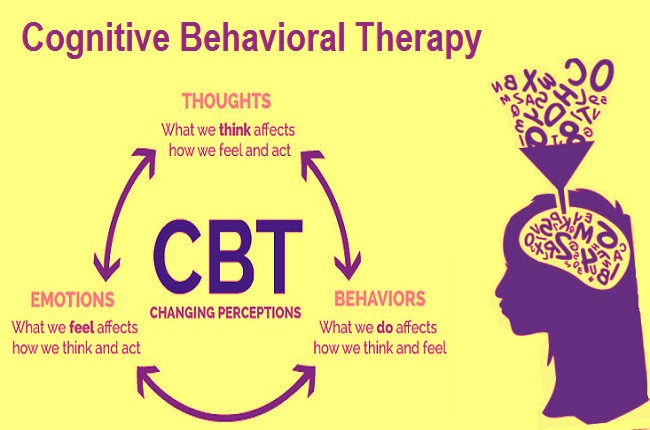 In the course of therapy, we uncovered the hidden beliefs that generated these reactions. He believed that if he could not "keep" the relationship, then this indicates his unreliability, if he failed to choose an "adequate" partner, this indicates weakness. Also, the client could not understand what he needed, he relied on ideas about how "should be".
In the course of therapy, we uncovered the hidden beliefs that generated these reactions. He believed that if he could not "keep" the relationship, then this indicates his unreliability, if he failed to choose an "adequate" partner, this indicates weakness. Also, the client could not understand what he needed, he relied on ideas about how "should be".
During three months of work, the client has learned to be aware of his needs, desires, track thoughts and engage in polemics with them. The young man was able to emotionally distance himself from obsessive thoughts, the mood background leveled off. He built his schedule in accordance with his own goals and values, acquired awareness skills.
Anastasia Afanasyeva, psychotherapist CBT:
What to read?
Cognitive Behavioral Therapy for Anxiety, Fear, Worry and Panic. Michelle Skin, Matthew McKay, Patrick Fanning
This book is for those who are already in therapy and want to understand the basics of the method and get the most out of CBT.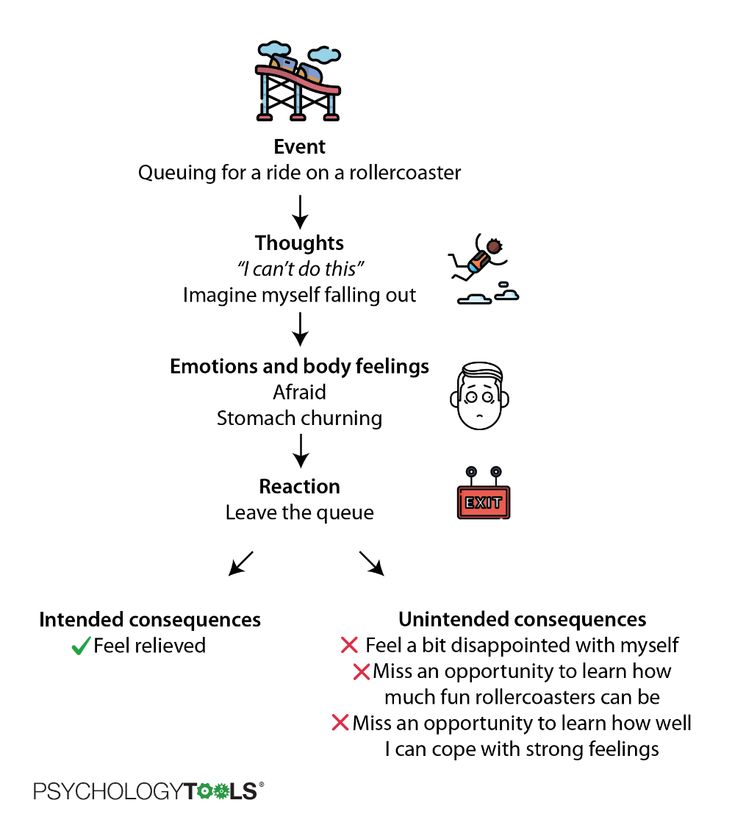 The authors dwell on techniques and exercises that help to cope with the manifestations of anxiety and symptoms of panic attacks.
The authors dwell on techniques and exercises that help to cope with the manifestations of anxiety and symptoms of panic attacks.
Cognitive Behavioral Therapy for Dummies. Rena Branch, Rob Wilson
A book from practicing therapists that explains CBT principles, concepts and how to deal with various disorders in simple language. In addition to practical advice and exercises, you will find many examples from the practice of the authors in it.
FIND A CBT PSYCHOLOGIST
Did you find the material helpful? Share it:
What is Cognitive Behavioral Therapy and how quickly it helps
March 28 Likbez Health
A simple question "Why?" can sort everything out.
What is Cognitive Behavioral Therapy
In essence, Cognitive Behavioral Therapy (CBT) is a way to change the way you think about life and yourself, based on two important steps:
- To realize (cognition) where negative thoughts, feelings, habits come from.
 Assess how they affect your life. Find those logical errors, cognitive distortions that make you worry. Ask yourself, “Why do I choose suffering over joy?”
Assess how they affect your life. Find those logical errors, cognitive distortions that make you worry. Ask yourself, “Why do I choose suffering over joy?” - Change behavior so as to eliminate negative experiences by focusing on positive ones.
Personal life problems, social anxiety, chronic stress, eating disorders, psychological problems that interfere with life - all of these can be dealt with with the help of cognitive behavioral therapy.
Keep in mind that CBT is not a magic pill. It will not save you from the existing objective problem. For example, if you suffer from the fact that your nose is too big, then it will remain the same. If you're going crazy over a divorce, your partner won't come running back with an apology. If you have a major anxiety disorder or clinical depression, psychotherapy is not a substitute for medication.
But CBT can teach you to be more accepting of problems or even turn them to your advantage. So, the same large nose can be a cause of suffering or become a highlight of appearance.
How CBT works
The main idea of this type of psychotherapy is as follows. Your psychological state does not depend on the stressful situation as such, but on how you feel about it. The therapist will teach you to distinguish between different types of emotions, understand how your mind switches between them, and focus on the positive ones.
Here is a simple example: you are invited to a party. On this occasion, you may have such thoughts and feelings:
- “Sounds great! My friends will be there, and I will also be able to meet new interesting people.” Experience: anticipatory, happy, excited.
- “Parties are still not my thing. Today, a new episode of my favorite series is coming out, I’d better stay at home, I don’t want to miss it. ” Experience: neutral.
- “I never know what to do or what to say at these events. They will make me make a toast again, I will make a fool of myself, and they will laugh at me again. Experience: anxious, negative.
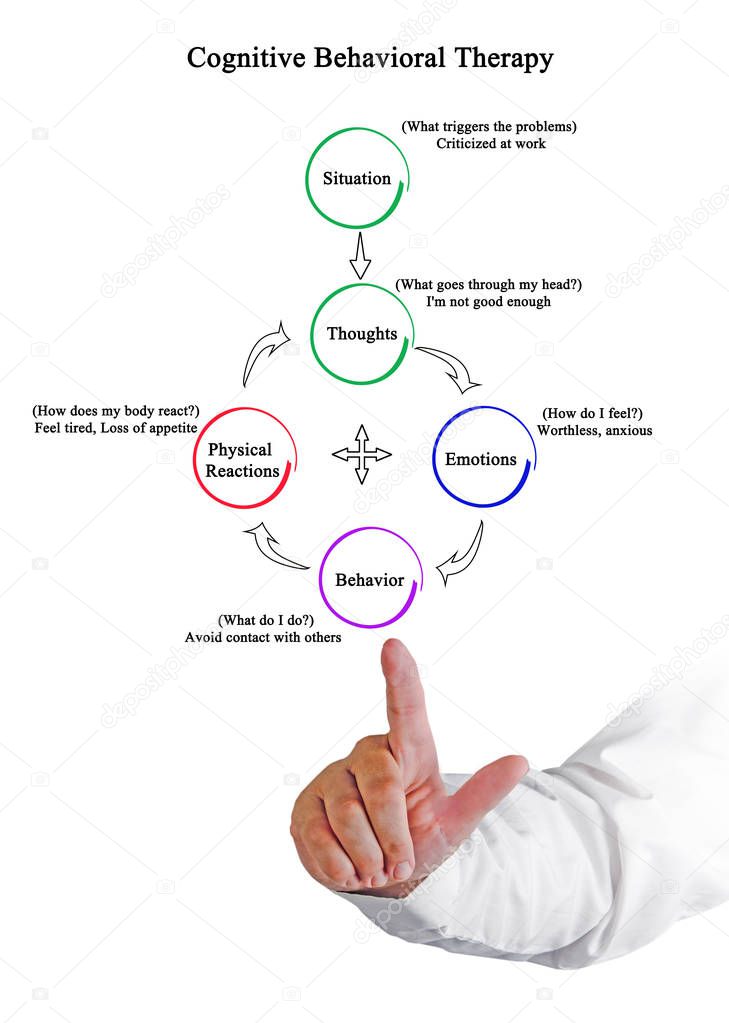
Bottom line: the same event can lead to completely different emotions. Which one to choose is up to you. You must make the selection process conscious. Like in a store: you are offered emotions, they cost the same - which one will you take?
To help you feel like a rational "buyer of emotions", the therapist will do the following.
Will teach you to detect negative thoughts
That is, to catch what exactly you are thinking about when you start to feel anxiety. For example, the thesis “I will be laughed at” is negative.
It will help to evaluate and challenge the negative
To evaluate means to ask questions: “Is the bad thing that scares me really going to happen? And if it does, will it really be catastrophic? Maybe it's not so scary?
Learn to replace negative thoughts with realistic ones
After you have identified and analyzed the disturbing thoughts, they will need to be replaced with more rational and realistic statements. For example: “Who will make me make a toast? I don’t drink at all and don’t plan to raise a glass.”
For example: “Who will make me make a toast? I don’t drink at all and don’t plan to raise a glass.”
How quickly CBT can work
Understanding why a situation makes you nervous can take time. And it will also be needed to teach your brain to choose the right ones from the “range” of emotions - calm and joyful.
It takes on average 5 to 20 psychotherapy sessions to understand and change behavior.
However, the duration of work with a psychotherapist is an individual matter. If your psychological problems are small, two or three meetings with a doctor may be enough. And someone will have to visit a specialist for years. It is impossible to predict the timing in advance. But, as experts note, on average, cognitive behavioral therapy leads to noticeable results faster than other types of intervention.
CBT has another bonus: meetings with a psychotherapist can be held online, and they will be no less effective than in person.