Schizoaffective disorder symptoms bipolar type
Schizoaffective Disorder | NAMI: National Alliance on Mental Illness
- Overview
- Treatment
- Support
- Discuss
Schizoaffective disorder is a chronic mental health condition characterized primarily by symptoms of schizophrenia, such as hallucinations or delusions, and symptoms of a mood disorder, such as mania and depression.
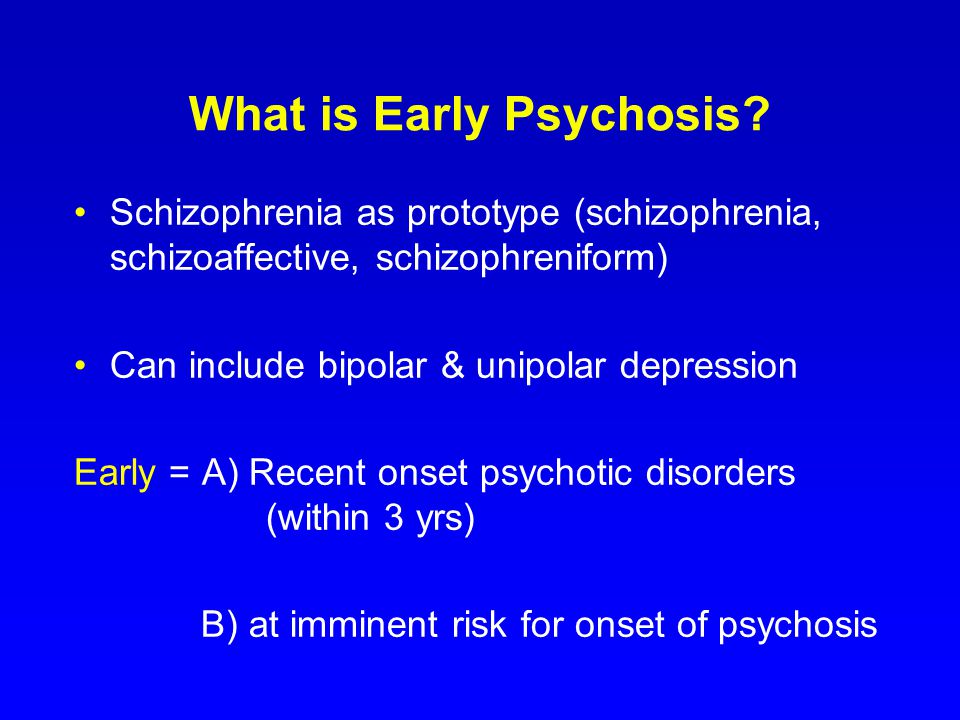
Many people with schizoaffective disorder are often incorrectly diagnosed at first with bipolar disorder or schizophrenia. Because schizoaffective disorder is less well-studied than the other two conditions, many interventions are borrowed from their treatment approaches.
Schizoaffective is relatively rare, with a lifetime prevalence of only 0.3%. Men and women experience schizoaffective disorder at the same rate, but men often develop the illness at an earlier age. Schizoaffective disorder can be managed effectively with medication and therapy. Co-occurring substance use disorders are a serious risk and require integrated treatment.
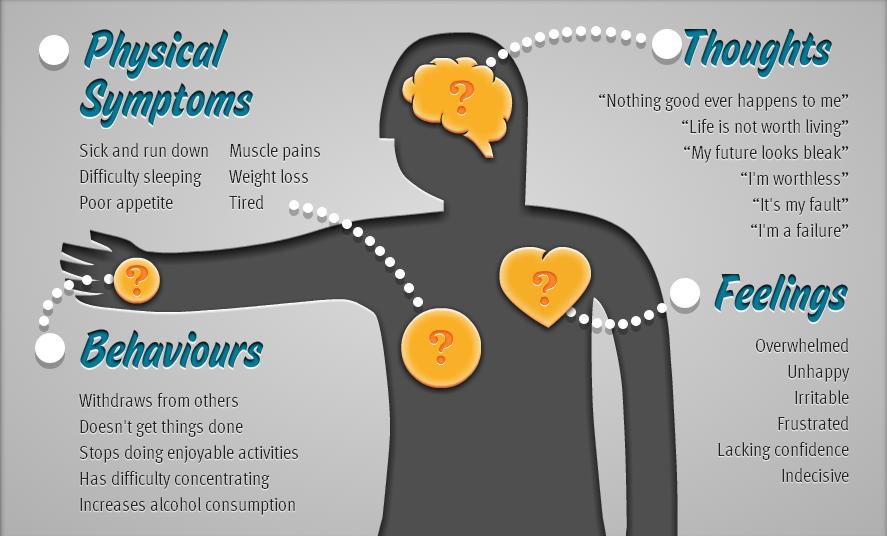
Symptoms
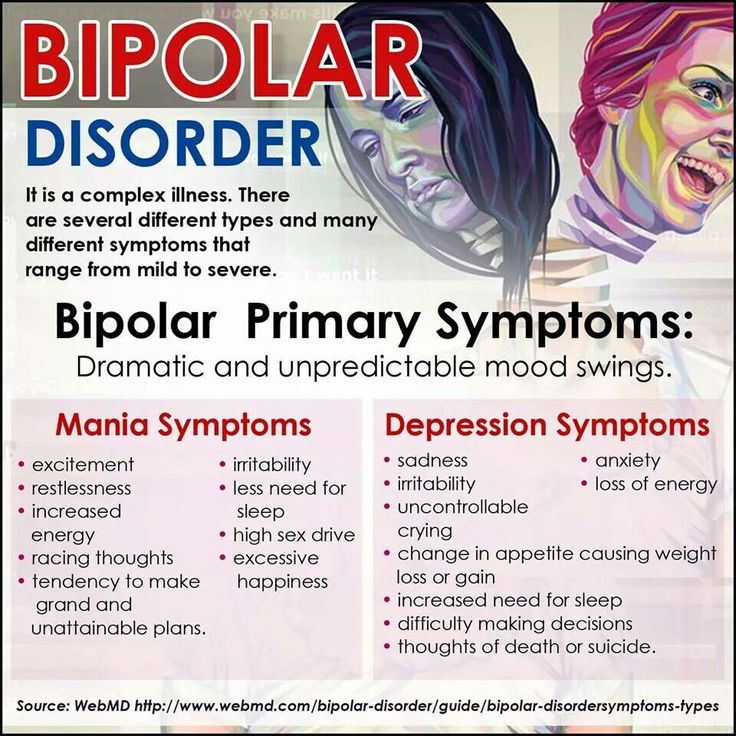
The symptoms of schizoaffective disorder can be severe and need to be monitored closely. Depending on the type of mood disorder diagnosed, depression or bipolar disorder, people will experience different symptoms:
- Hallucinations, which are seeing or hearing things that aren’t there.
- Delusions, which are false, fixed beliefs that are held regardless of contradictory evidence.
- Disorganized thinking. A person may switch very quickly from one topic to another or provide answers that are completely unrelated.
- Depressed mood. If a person has been diagnosed with schizoaffective disorder depressive type they will experience feelings of sadness, emptiness, feelings of worthlessness or other symptoms of depression.
- Manic behavior. If a person has been diagnosed with schizoaffective disorder: bipolar type they will experience feelings of euphoria, racing thoughts, increased risky behavior and other symptoms of mania.
Causes
The exact cause of schizoaffective disorder is unknown.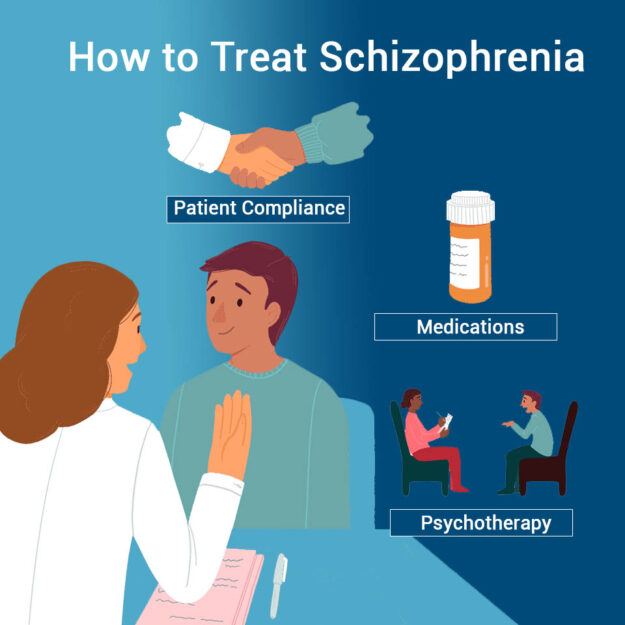 A combination of causes may contribute to the development of schizoaffective disorder.
A combination of causes may contribute to the development of schizoaffective disorder.
- Genetics. Schizoaffective disorder tends to run in families. This does not mean that if a relative has an illness, you will absolutely get it. But it does mean that there is a greater chance of you developing the illness.
- Brain chemistry and structure. Brain function and structure may be different in ways that science is only beginning to understand. Brain scans are helping to advance research in this area.
- Stress. Stressful events such as a death in the family, end of a marriage or loss of a job can trigger symptoms or an onset of the illness.
- Drug use. Psychoactive drugs such as LSD have been linked to the development of schizoaffective disorder.
Diagnosis
Schizoaffective disorder can be difficult to diagnose because it has symptoms of both schizophrenia and either depression or bipolar disorder. There are two major types of schizoaffective disorder: bipolar type and depressive type. To be diagnosed with schizoaffective disorder a person must have the following symptoms.
There are two major types of schizoaffective disorder: bipolar type and depressive type. To be diagnosed with schizoaffective disorder a person must have the following symptoms.
- A period during which there is a major mood disorder, either depression or mania, that occurs at the same time that symptoms of schizophrenia are present.
- Delusions or hallucinations for two or more weeks in the absence of a major mood episode.
- Symptoms that meet criteria for a major mood episode are present for the majority of the total duration of the illness.
- The abuse of drugs or a medication are not responsible for the symptoms.
Treatment
Schizoaffective disorder is treated and managed in several ways:
- Medications, including mood stabilizers, antipsychotic medications and antidepressants
- Psychotherapy, such as cognitive behavioral therapy or family-focused therapy
- Self-management strategies and education
Related Conditions
A person with schizoaffective disorder may have additional mental health conditions:
- Anxiety disorders
- Posttraumatic stress disorder (PTSD)
- Attention-deficit hyperactivity disorder (ADHD)
- Substance use disorders / Dual Diagnosis
Bipolar Schizoaffective Disorder: Know the Facts
Schizoaffective disorder is a rarer type of mental illness.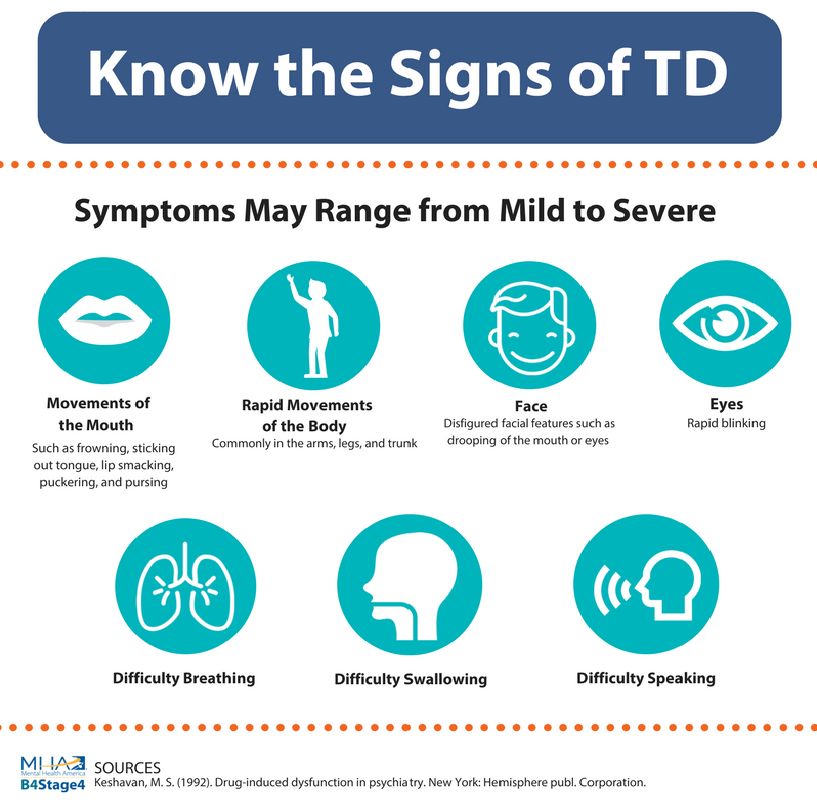 It’s characterized by symptoms of both schizophrenia and symptoms of a mood disorder. This includes mania or depression.
It’s characterized by symptoms of both schizophrenia and symptoms of a mood disorder. This includes mania or depression.
The two types of schizoaffective disorder are bipolar and depressive.
Episodes of mania occur in the bipolar type. During a manic episode, you may alternate between feeling overly excited to feeling extremely irritable. You may or may not experience depressive episodes.
People who have the depressive type experience episodes of depression.
According to National Alliance on Mental Illness (NAMI), schizoaffective disorder affects 0.3 percent of people in the United States. It affects men and women equally, and men may develop the disorder earlier in life.
With proper treatment and care, this disorder can be effectively managed. Read on to learn more.
Your symptoms will depend on the mood disorder. They can vary from mild to severe and may also vary depending on the person experiencing them.
Manic symptoms are like those seen in bipolar disorder.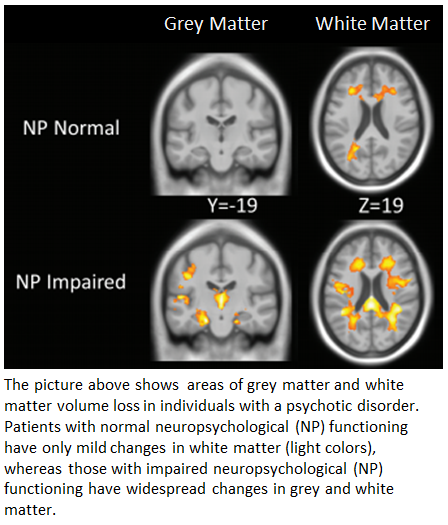 A person with manic symptoms may appear hyperactive or overly restless, talk very fast, and sleep very little.
A person with manic symptoms may appear hyperactive or overly restless, talk very fast, and sleep very little.
Doctors may refer to your symptoms as positive or negative, but this doesn’t mean “good” or “bad.”
Psychotic symptoms are similar to those of schizophrenia. This may include positive symptoms, like:
- hallucinations
- delusions
- disorganized speech
- disorganized behavior
Negative symptoms can occur when something seems to be missing, like the ability to experience pleasure or the ability to think clearly or concentrate.
It isn’t clear what causes schizoaffective disorder. The disorder typically runs in families, so genetics may play a role. You aren’t guaranteed to develop the disorder if a family member has it, but you do have an increased risk.
Birth complications or exposure to toxins or viruses before birth may also contribute to the development of this disorder. People may also develop schizoaffective disorder as a result of certain chemical changes in the brain.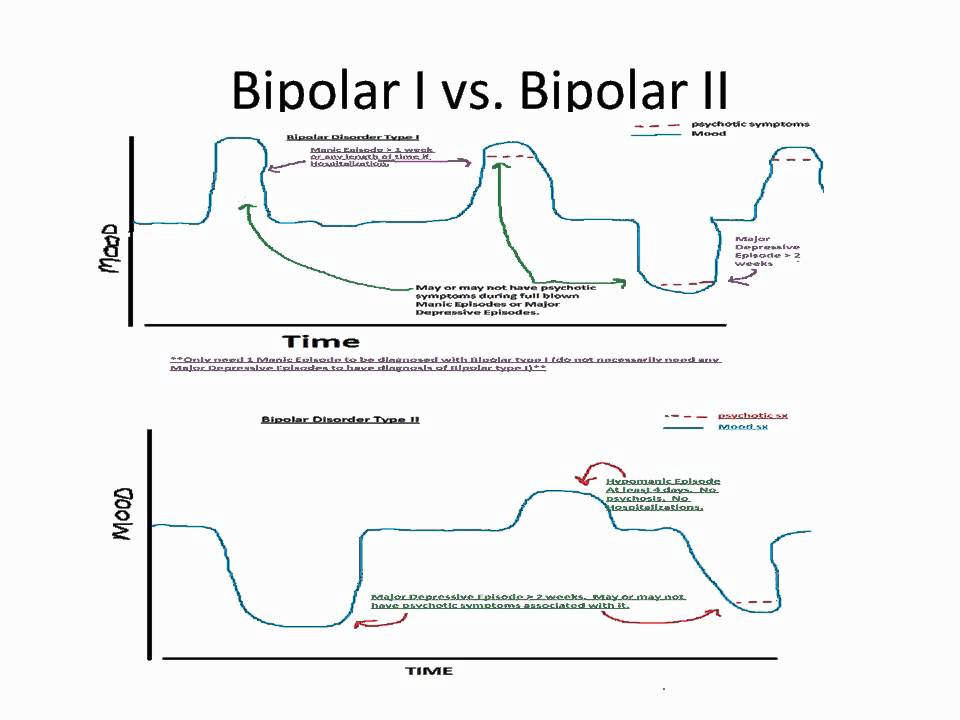
It can be difficult to diagnose schizoaffective disorder because it has many of the same symptoms as other conditions. These symptoms can appear at different times. They can also appear in different combinations.
When diagnosing this type of schizoaffective disorder, doctors will look for:
- major manic symptoms that occur along with psychotic symptoms
- psychotic symptoms that last at least 2 weeks, even when the mood symptoms are under control
- a mood disorder that’s present for most of the course of the illness
Blood or laboratory tests can’t help your doctor diagnose schizoaffective disorder. Your doctor may do certain tests to rule out other diseases or conditions that can cause some of the same symptoms. This includes substance misuse or epilepsy.
People with the bipolar type of schizoaffective disorder usually respond well to a combination of medications. Psychotherapy or counseling may also help to improve quality of life.
Medications
Medications can help relieve the psychotic symptoms and stabilize changes in mood.
Antipsychotics
Antipsychotics control the schizophrenia-like symptoms. This includes hallucinations and delusions. Paliperidone (Invega) is the only drug approved by the Food and Drug Administration (FDA) specifically for schizoaffective disorder. But doctors can still use medications off-label to treat these symptoms.
Similar drugs include:
- clozapine
- risperidone (Risperdal)
- olanzapine (Zyprexa)
- haloperidol
Mood stabilizers
Mood stabilizers like lithium can level out the highs and lows of bipolar symptoms.
You may need to take the mood stabilizers for several weeks or so before they become effective. Antipsychotics work much quicker to control symptoms. So, it isn’t uncommon to use mood stabilizers and antipsychotics together.
Other drugs
Certain drugs for treating seizures can also treat these symptoms. This includes carbamazepine and valproate.
Psychotherapy
Psychotherapy, or talk therapy, can help people with schizoaffective disorder to:
- solve problems
- form relationships
- learn new behaviors
- learn new skills
Talk therapy can generally help you manage your life and your thoughts.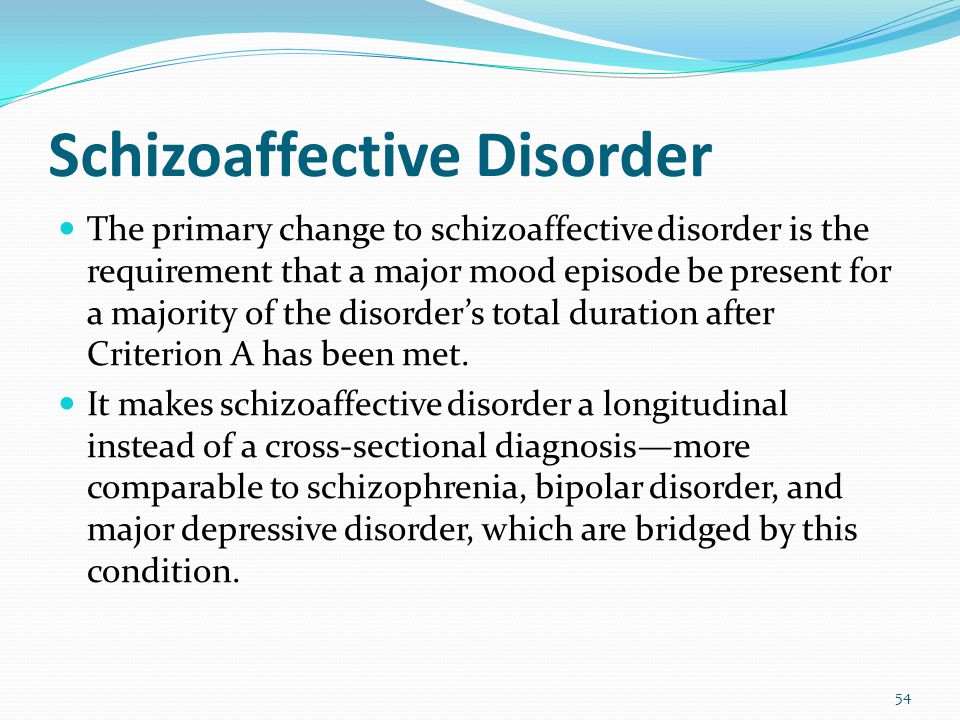
You can get one-on-one therapy with a psychologist, counselor, or another therapist, or you can go to group therapy. Group support can reinforce new skills and allow you to connect with other people who share your concerns.
Although schizoaffective disorder isn’t curable, many treatments can help you effectively manage your condition. It’s possible to manage the symptoms of schizoaffective disorder and have a better quality of life.
Find support
Medication can help your symptoms, but you need encouragement and support to function well. Help is available for you, your family, and your friends.
One of the first steps is to learn as much as you can about the disorder. It’s important that you or your loved one gets the right diagnosis and treatment.
These organizations can help you learn more about schizoaffective disorder, keep up with new research and treatments, and find local support:
Mental Health America (MHA)
MHA is a national nonprofit advocacy group with over 200 affiliates throughout the country. Its website has more information about schizoaffective disorder and links to resources and support in local communities.
Its website has more information about schizoaffective disorder and links to resources and support in local communities.
National Alliance on Mental Illness (NAMI)
NAMI is a large grassroots organization that offers more details about mental illnesses, including schizoaffective disorder. NAMI can help you find resources in your local community. The organization also has a toll-free helpline. Call 800-950-NAMI (6264) for referrals, information, and support.
National Institute of Mental Health (NIMH)
The NIMH is a leading agency for research on mental illnesses. It offers information about:
- medications
- therapies
- links for finding mental health services
- links for participating in clinical research trials
National Suicide Prevention Lifeline
If you or someone you know is in crisis, at risk for self-harm or hurting others, or considering suicide, call the National Suicide Prevention Lifeline at 1-800-273-8255.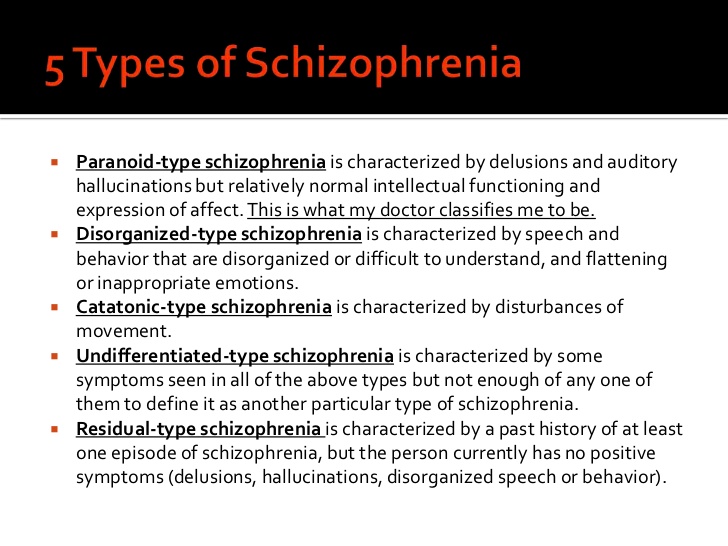 Calls are free, confidential, and they’re available 24/7.
Calls are free, confidential, and they’re available 24/7.
Be patient
Although antipsychotic medications usually work very quickly, drugs for mood disorders can often take several weeks before producing visible results. If you’re worried about this in-between period, discuss solutions with your doctor.
Talk to your doctor
Always talk with your doctor about your treatment plan and options. Be sure to discuss any side effects you’re experiencing or if any medication you’re taking isn’t having an effect.
A simple switch in medications or dosages may make a difference. Working closely with them can keep your condition managed.
FGBNU NTsPZ. ‹‹Endogenous mental illness››
Feedback form
Question about the work of the siteQuestion to a specialistQuestion to the administration of the clinic
email address
Name
Message text
The opinion about the clinical heterogeneity of schizoaffective psychoses is generally accepted. By analogy with affective psychoses, mono- and bipolar forms are distinguished [Angst J., 1989; Marneros A. et al., 1990], and the latter are regarded by some authors as the most characteristic of schizoaffective psychoses [Gamkrelidze Sh. A., 1980; Andreasen N. C., Coryell W. et al., 1988]. At the same time, G. Winokur (1984) considers such a division illegal.
By analogy with affective psychoses, mono- and bipolar forms are distinguished [Angst J., 1989; Marneros A. et al., 1990], and the latter are regarded by some authors as the most characteristic of schizoaffective psychoses [Gamkrelidze Sh. A., 1980; Andreasen N. C., Coryell W. et al., 1988]. At the same time, G. Winokur (1984) considers such a division illegal.
U. H. Peters (1983, 1989) proposes to talk about two forms of schizoaffective psychoses, depending on whether or not their other psychopathological formations follow or do not follow from affect.
A number of authors [Tsuang M. T., 1979; Angst J., 1989] subdivide schizoaffective psychoses into three variants: close to affective psychosis; close to schizophrenia; intermediate or undifferentiated with equal severity of affective and schizophrenic symptoms.
Essentially the same position was held by A.K. Anufriev (1969), T.F. Papadopoulos (1975), AA. Severny (1980), who allowed for the possibility of "schizoaffective" transitional forms between manic-depressive psychosis and recurrent schizophrenia.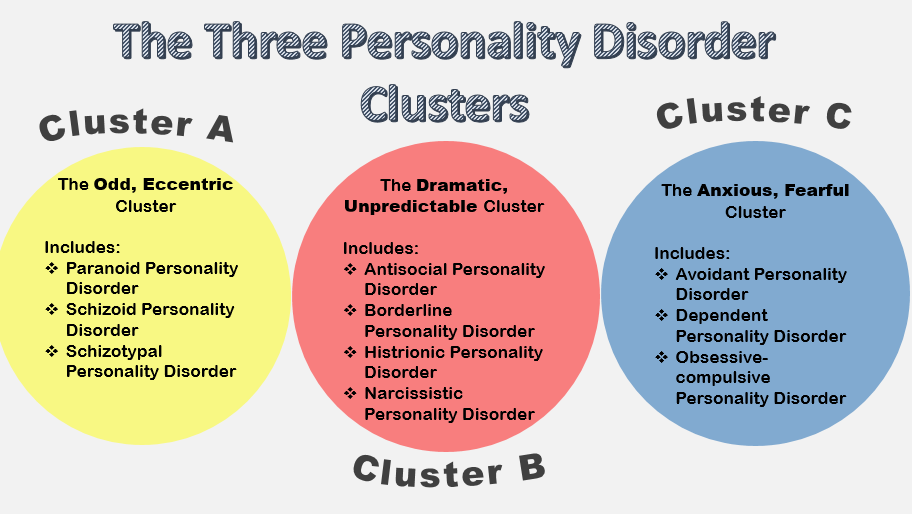 A close position was occupied by V. N. Favorina (1959) and A.V. Semke (1988), who considered schizoaffective psychoses as a variant of recurrent schizophrenia.
A close position was occupied by V. N. Favorina (1959) and A.V. Semke (1988), who considered schizoaffective psychoses as a variant of recurrent schizophrenia.
Recently, the division of schizoaffective psychoses into affect-dominant and schizodominant forms has become more common [Angst J., 1989; Marneros A., 1989, 1990]. It corresponds to the "Research Diagnostic Criteria (RDC)" [Spitzer R. L., Endicott J., Robins E., 1978], which is the basis for the diagnostic criteria for schizo-affective psychosis in DSM-IV and in ICD-10. The affect-dominant form is said to be when the disease develops with a “high level of premorbid adaptation” and the absence of schizophrenic symptoms in the picture of a schizoaffective state for at least 1 week in persistent affective disorders; schizodominant form is understood as psychosis, when affective pathology is not observed in the picture of a schizoaffective episode for at least 1 week, while remaining constant schizophrenic (delusional) symptoms.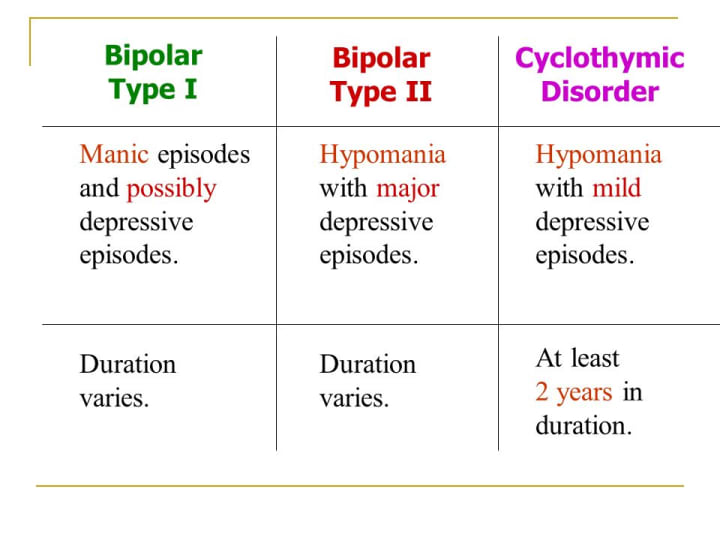 Thus, a syndromic assessment of an attack is necessary. Based on the quantitative ratio during the course of the disease as a whole affective, schizoaffective and schizophrenic in terms of the pattern of seizures, A. Marneros (1988) additionally introduces an “intermediate” form into the differentiation of schizoaffective psychoses, substantiating such a division by the degree of severity of the “schizoaffective focus”.
Thus, a syndromic assessment of an attack is necessary. Based on the quantitative ratio during the course of the disease as a whole affective, schizoaffective and schizophrenic in terms of the pattern of seizures, A. Marneros (1988) additionally introduces an “intermediate” form into the differentiation of schizoaffective psychoses, substantiating such a division by the degree of severity of the “schizoaffective focus”.
To date, the division of schizoaffective psychosis into affective-dominant and schizodominant forms is essentially based on the criteria for the predominance of affective or schizophrenic disorders in the picture of a schizoaffective seizure and does not reflect the clinical peculiarity of schizoaffective psychosis as an independent endogenous disease. This division corresponds to the above descriptions of those authors who, in accordance with their own diagnostic positions, defined schizoaffective psychosis as an endogenous disease, "close to an affective disorder" or "close to schizophrenia. "
"
Domestic researchers A. N. Korenev (1994), V. I. Dikai et al. (1995, 1998), G. P. Panteleeva et al. (1996, 1998), P. V. Bologov (1998) developed detailed differentiation of schizoaffective psychosis on the basis of the psychopathological structure of non-affective delusional syndromes and the mechanisms of delusion formation in the picture of a schizoaffective seizure. Within the framework of the affect-dominant form, three variants of schizoaffective states are described, characterized by a picture of acute sensory delusion: with the dominance of delusion of perception; with a predominance of visual-figurative delusions of the imagination; with predominant intellectual delirium of the imagination. In the schizodominant form, three other variants of schizoaffective states with a picture of acute delusional disorders, qualified as acute paranoid ones with a picture of an acute Kandinsky-Clerambault syndrome, were identified. Such states are characterized by mixed delusion formation; during their formation, the mechanisms of acute sensual delusion are combined with delusion formation according to the type of its ideational forms, developing in the picture of acute delusion of perception with elements of interpretive delusion, in the structure of the dominant visual-figurative delusion of the imagination with elements of interpretive delusion, on the basis of predominantly acute (unsystematized) interpretive nonsense with elements of sensual nonsense. The proposed typology also takes into account the features of the dynamics of psychosis and the degree of its progression.
The totality of the signs identified by the indicated authors for each of the varieties of the course of schizoaffective psychosis allowed them to raise the question of the legitimacy of distinguishing a nosologically independent schizoaffective psychosis.
Given the clinical heterogeneity of schizoaffective psychosis, in everyday clinical work, its variants and types of seizures are usually distinguished within each of the forms.
The "nuclear" variant of schizoaffective psychosis can be spoken of as a nosologically independent disease, it corresponds to affect-dominant schizoaffective psychoses with dominance of delusions of perception in their picture. Two other varieties - with a dominant visual-figurative delusion within the affect-dominant form and with the formation of paranoid psychosis in the structure of a delusion of perception with elements of interpretation within the framework of the schizodominant form - are considered in their manifestations as "marginal" variants of nosologically independent schizoaffective psychosis, which also correspond to its definition , but some of its symptoms appear atypically.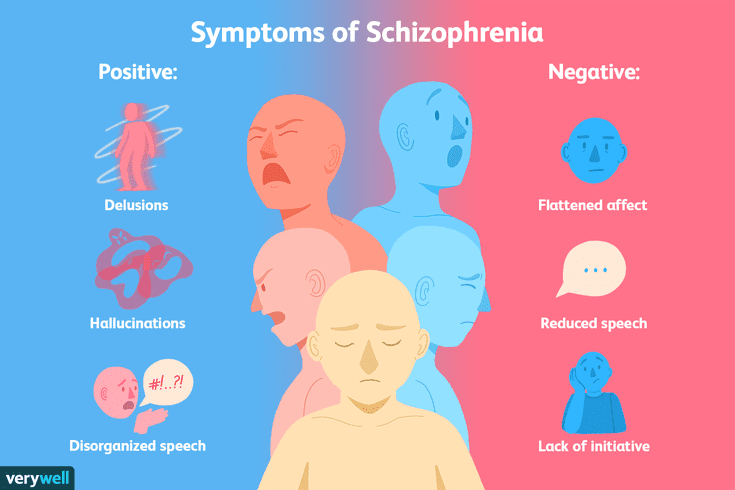 The remaining three varieties of schizoaffective psychosis proceed with a predominance of ideational forms of delusion. In the dynamics and clinical manifestations of the disease in these cases, there are signs of at least slight progression. They are more justified both clinically and prognostically attributable to schizophrenia, considering them as schizoaffective variants of its paroxysmal forms. A comparison of the main variants of schizoaffective psychosis with their corresponding disorders according to ICD-10 is given in Table. 13.
The remaining three varieties of schizoaffective psychosis proceed with a predominance of ideational forms of delusion. In the dynamics and clinical manifestations of the disease in these cases, there are signs of at least slight progression. They are more justified both clinically and prognostically attributable to schizophrenia, considering them as schizoaffective variants of its paroxysmal forms. A comparison of the main variants of schizoaffective psychosis with their corresponding disorders according to ICD-10 is given in Table. 13.
Table 13. Schizoaffective psychosis (SAP): comparison of ICD-10 diagnostic criteria and Russian classification
| Typological variants of ShAP in the domestic classification | ICD-10 | ||
| diagnostic criteria | the code | ||
| 1. | I. Schizoaffective disorder. Bipolar affective disorder (or recurrent depressive disorder), acute and transient psychotic disorders | F25+ | |
| Schizoaffective state with dominance of delusions of perception (acute paranoid) | Schizoaffective disorder, manic (depressive, mixed) type; other acute, predominantly delusional, psychotic disorders | F25.0—2+ | |
| Schizoaffective state with dominance of visual-figurative delusions of imagination (oriented oneiroid, antagonistic delusions) | Schizoaffective disorder, manic (depressive, mixed) type. | F25.0— 2+ +F23.0 | |
| Schizoaffective state with dominance of intellectual delusions of the imagination (acute fantastic, acute paraphrenic delusions) | Schizoaffective disorder, manic (depressive, mixed) type. Acute schizophrenia-like psychotic disorder | F25.0— 2+ | |
| II. schizodominant form | II. Schizoaffective disorder, acute and transient psychotic disorders, bipolar affective disorder | F25+F23+ | |
| Acute polymorphic delusional state with delirium of the type of acute paranoid with elements of interpretive delirium | e Other acute and transient psychotic disorders. | F23.8+ | |
| Acute Kandinsky-Clerambault Syndrome with Delusion Formation as Unsystematized Interpretive Delusion | - Acute polymorphic psychotic disorder with symptoms of schizophrenia. Schizoaffective disorder, manic (depressive, mixed) type | F21.3+ | |
In the guidelines of the Ministry of Health of the Russian Federation on adapting the ICD-10 to the Russian classification , schizoaffective psychosis is wholly assigned to schizoaffective variants of paroxysmal schizophrenia (heading F25 - Schizoaffective disorder) and is divided into manic (F25.0) and depressive type (F25.1).
The clinical characteristics of schizoaffective psychosis presented in this manual are based primarily on the description of its two traditional forms, affect-dominant and schizo-dominant, reflecting the different ratio of affective and schizophrenic delusional disorders during a schizoaffective attack, which are not subject to broad nosological interpretation.
how I live with schizoaffective disorder
This text was written by a reader in the Community. Carefully edited and formatted according to editorial standards.
Egor Kamaev
lives with schizoaffective disorder
Author profile
I am 19 years old. Six months ago, I was diagnosed with schizoaffective disorder of the depressive type.
Ironically, I am a medical student and plan to become a psychiatrist. For some time I doubted whether it was worth continuing my studies with my illness. But now I see my purpose in this: I want to help people with mental disorders in the same way that they helped me.
I'll tell you how my story began, why it took me a long time to be diagnosed, and how, as a result, a treatment was chosen that changed my life.
What is schizoaffective disorder?
The prefix "schizo" indicates the presence of psychotic symptoms characteristic of schizophrenia: delusions or hallucinations. Delusions are understood as persistent false beliefs - for example, a person may experience an inexplicable feeling of guilt, worthlessness, think that those around him are watching or reading his thoughts. With hallucinations, the patient feels something that is not there - for example, he hears non-existent voices or smells.
Delusions are understood as persistent false beliefs - for example, a person may experience an inexplicable feeling of guilt, worthlessness, think that those around him are watching or reading his thoughts. With hallucinations, the patient feels something that is not there - for example, he hears non-existent voices or smells.
In addition to psychotic, the disease is accompanied by affective symptoms, i.e. mood changes. There are two types of schizoaffective disorder:
- Bipolar type - in this case, the patient experiences strong emotional upsurges, or episodes of mania, and sometimes strong emotional downturns, or episodes of depression.
- Depressive type - it is characterized only by episodes of depression.
The disease periodically aggravates, then subsides. Exacerbations last at least a month. At the same time, psychotic and affective symptoms can be combined or replace each other for two weeks.
Why schizoaffective disorder develops is not exactly clear.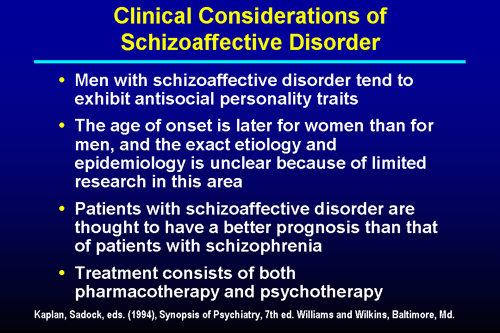 Among the causes are genetic predisposition, stressful events, childhood psychological trauma and disruption in the production of neurotransmitters - substances that help brain cells exchange signals.
Among the causes are genetic predisposition, stressful events, childhood psychological trauma and disruption in the production of neurotransmitters - substances that help brain cells exchange signals.
Typically, symptoms first appear in adolescence or early 30s. Due to the similarity of the disease with schizophrenia and bipolar affective disorder, it can be difficult for psychiatrists to make a diagnosis.
It is impossible to get rid of schizoaffective disorder once and for all, but it is possible to achieve a long-term remission - a state in which a person feels normal.
Treatment includes psychotherapy and drug therapy. Antipsychotics are prescribed as the main drugs, they help to eliminate delusions and hallucinations. Antidepressants and mood stabilizers are recommended to stabilize mood. Medications are usually taken for the rest of one's life, but sometimes a doctor may reduce the doses of medications or stop them.
Without treatment, schizoaffective disorder worsens: exacerbations become more frequent and prolonged, and patients are at increased risk of suicide.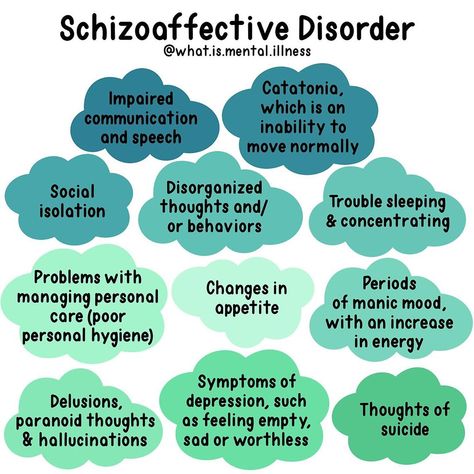
How I first felt bad
The first time the disease manifested itself at the age of 14. The symptoms were similar to depression: I was in a depressed mood, I thought that I was insignificant and nobody needed me.
In the next three years, bouts of "despondency" were repeated annually and lasted about a month. They ended with me trying to commit suicide. It was lucky that all attempts were childishly inept. For example, one day I decided to poison myself and took the first pills I came across from the first-aid kit - in the end I just vomited. Another time he tried to starve himself to death, but nothing came of it either. After the suicide attempt, the disease let go, and I returned to normal life for several months.
My condition scared my parents very much, but they were afraid of being registered with a psychiatrist, so they started taking me to psychologists. I visited several private specialists, and I also went to the school one. I no longer remember what we talked about, I only remember how I passed countless boring tests.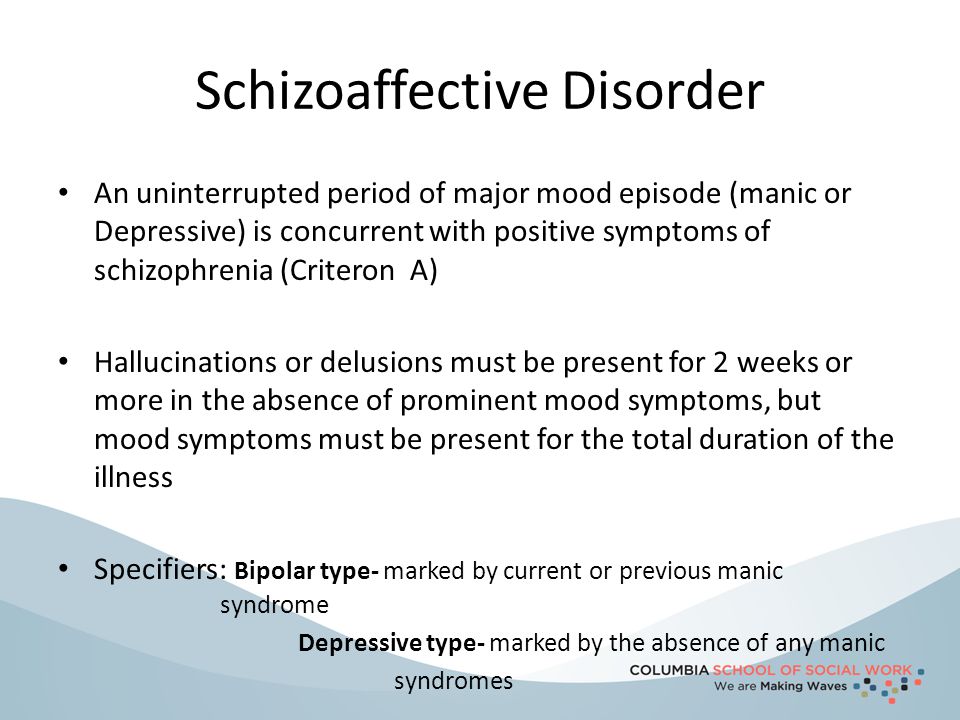 Once, after one of them, the school psychologist said that I had depression. I asked: "So what to do now?" In response, I heard: "I don't know."
Once, after one of them, the school psychologist said that I had depression. I asked: "So what to do now?" In response, I heard: "I don't know."
Although the psychologists did not help much, by the age of 17 the disease subsided, and I forgot about my strange behavior.
/psychotherapy-search/
How to choose a psychotherapist
See a doctor
We do not make recommendations in this article. Please consult with your doctor before deciding on treatment. The responsibility for your health rests solely with you.
How I got worse
The aggravation happened again in the second year of university. During this period, I not only studied, but also worked a lot: I was a courier and a steward at sports matches. I wanted to become independent as soon as possible and move away from my parents, so I went to work almost every day. Sometimes the voice of reason still prevailed, and I allowed myself to rest. But due to greed and the desire to accumulate the required amount as soon as possible, this was rare.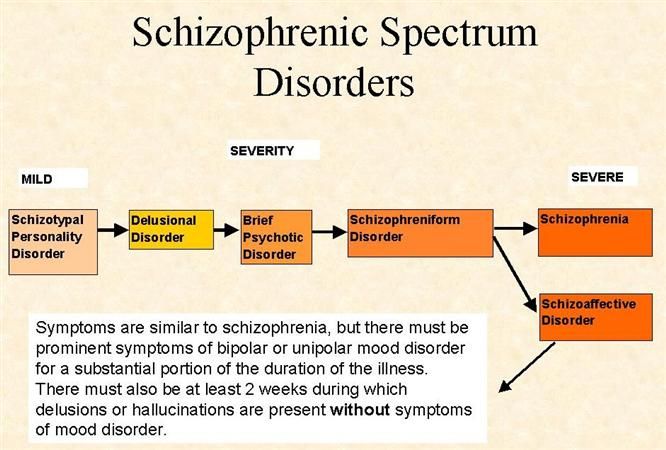
I stopped devoting enough time to my studies, even though the material at the university became more and more difficult. The tension built up every day. The situation was aggravated by the fact that, despite the exhausting schedule, I did not earn enough to separate from my parents.
Community 11/23/21
What is depression?
Against this background, several other problems arose in life - not so significant, but probably also contributed to mental health. As a result, the delusional idea of worthlessness and insignificance returned to me. It seemed that by my very existence I bring people great inconvenience, and if I leave this life, it will become easier for everyone.
At first, these thoughts flashed through my head from time to time, and then they began to repeat themselves with frightening frequency. This condition was much worse than what I experienced before.
My treatment
Day hospital in a psychiatric hospital A month and a half after the onset of symptoms, I went to a neuropsychiatric dispensary.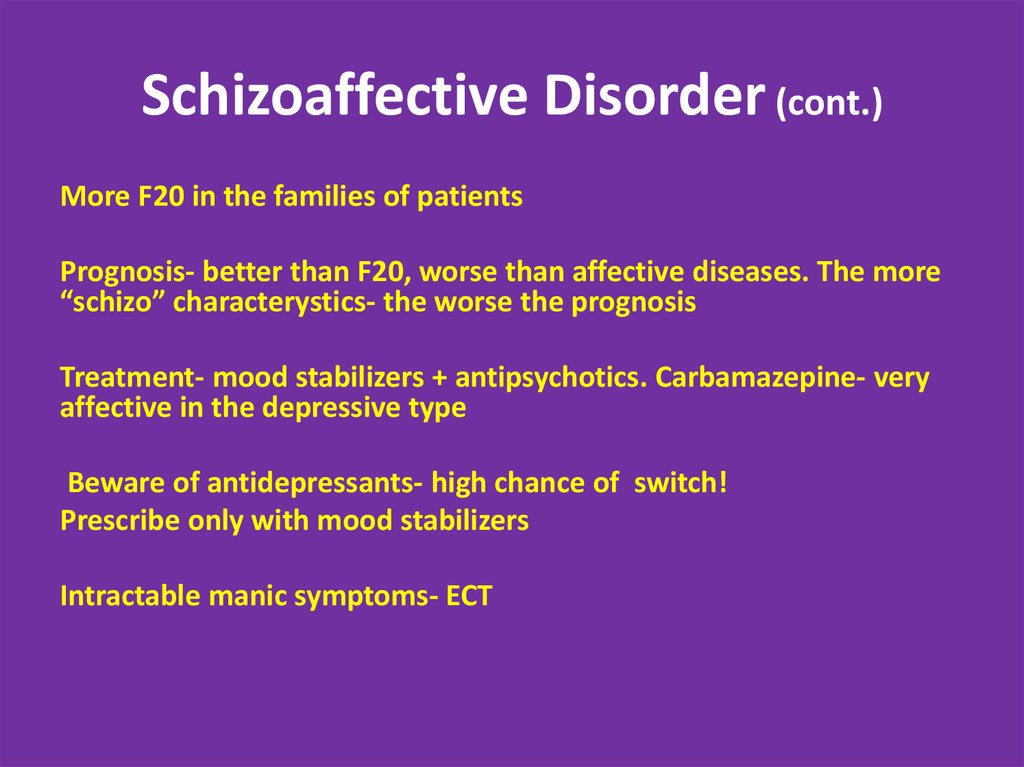 I didn’t tell my parents about this: they were still afraid of psychiatrists and offered the help of psychologists.
I didn’t tell my parents about this: they were still afraid of psychiatrists and offered the help of psychologists.
The doctor at the dispensary diagnosed me with depression and offered to go to the hospital, but I refused. At that moment, hospitalization seemed an unaffordable luxury, you had to work and get rid of the tails for your studies. In addition, I didn’t want to inform my parents about the diagnosis: until the last moment I pretended that everything was fine with me - I was just “a little sad”.
We discussed various options with the doctor and came to a compromise - a day hospital. Treatment in the hospital was organized as follows: I came and talked with a psychiatrist for about half an hour. He asked about my well-being. After the conversation, they gave me a Rocon antidepressant pill, and I left.
I took an antidepressant for two weeksHow I tried to commit suicide
I did not feel the effect of the antidepressant: every day I got worse.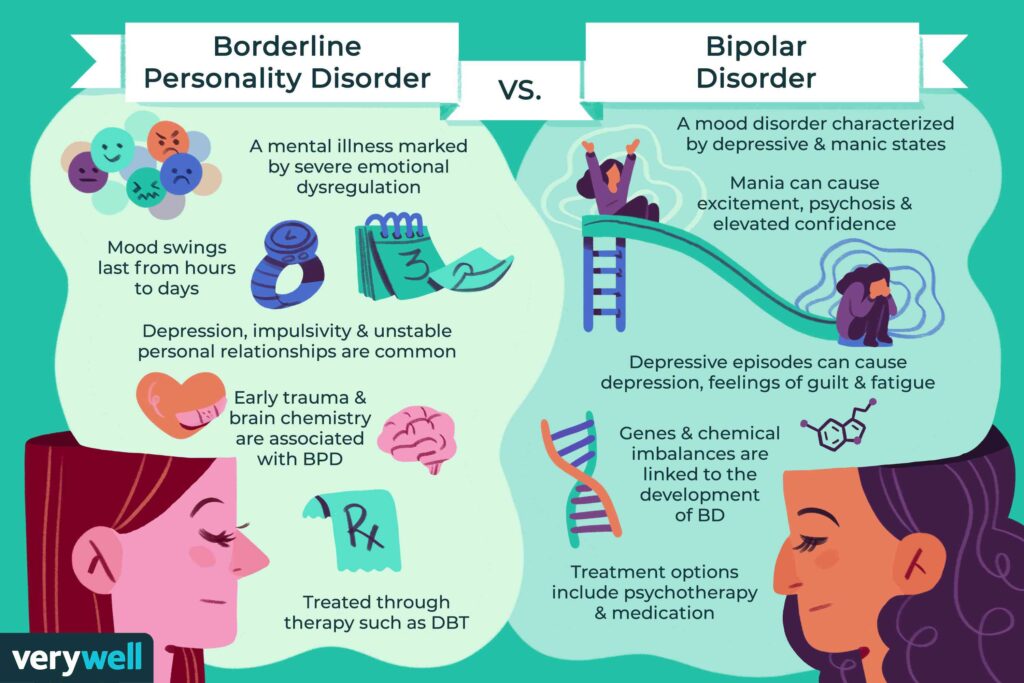 The thought grew stronger in my head that there was only one way to end suffering - by dying.
The thought grew stronger in my head that there was only one way to end suffering - by dying.
About two weeks after starting treatment, I made another suicide attempt. The idea matured in one day. I remember that around 5 pm I returned home, sat on the bed and started thinking. I considered three options: poison myself with pills, jump under a train, or jump out of a window. The first option seemed vulgar, the second was inconvenient for others, and the third was the most suitable.
I decided that in the morning I would withdraw all the money that I had accumulated from my accounts, go to the railway station and get to any city by the first train. There I will rent a hotel room on the highest floor and do what I have in mind.
/list/psihiatr/
12 important questions for psychiatrist Kirill Sychev
Having made my decision, I looked at my watch: it was 5 in the morning. It turned out that I spent 12 hours in my thoughts.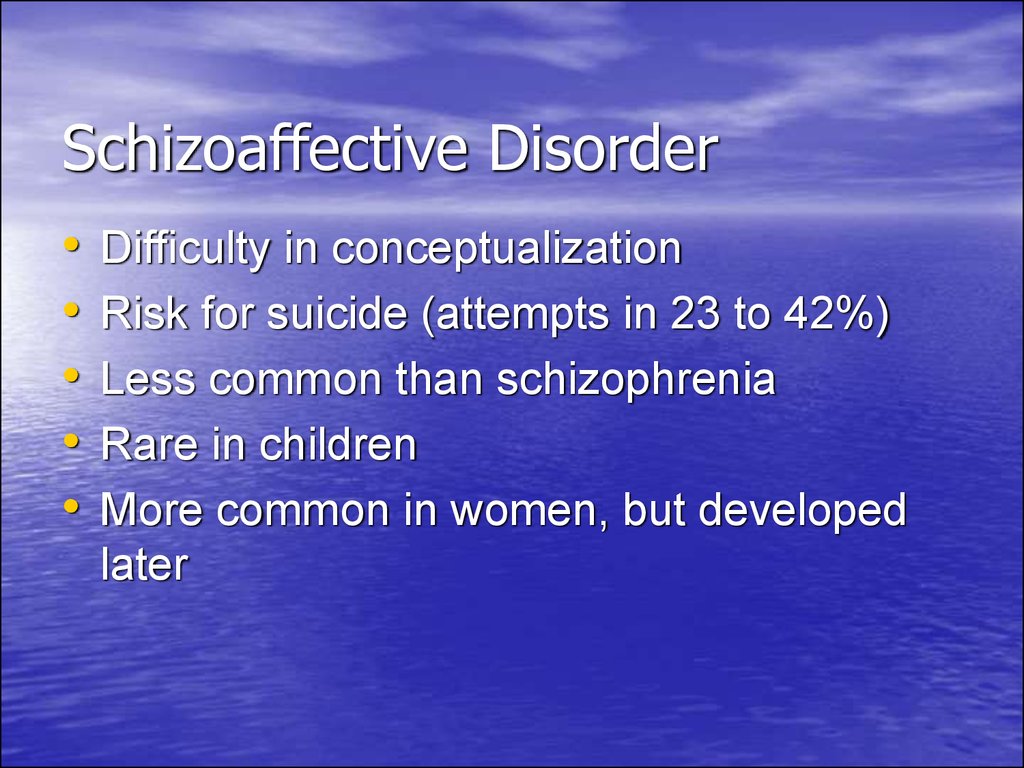 I went to bed, and two hours later my mother woke me up: it was time to get ready for the university.
I went to bed, and two hours later my mother woke me up: it was time to get ready for the university.
I remember that I did not want to leave. I told my mom that I didn't feel well, but she wasn't convinced. We left the house, and she gave me a ride in a car to the subway. I went down, then went back to the surface. I went to Dodo Pizza and ordered my favorite milkshake and a slice of pizza. I thought maybe if I please myself, I will feel like dying. But it didn't get any easier.
I went down to the subway again and realized that I would not go to the station anymore. I transferred money to my mother, wrote to a friend that I would not be able to come to his birthday party in two days, took off my jacket, put it in a backpack and put it against the wall. And then he jumped under the approaching train. What happened next, I don't remember.
My treatment
24-hour hospital in a psychiatric hospital Woke up in the hospital with a bunch of injuries.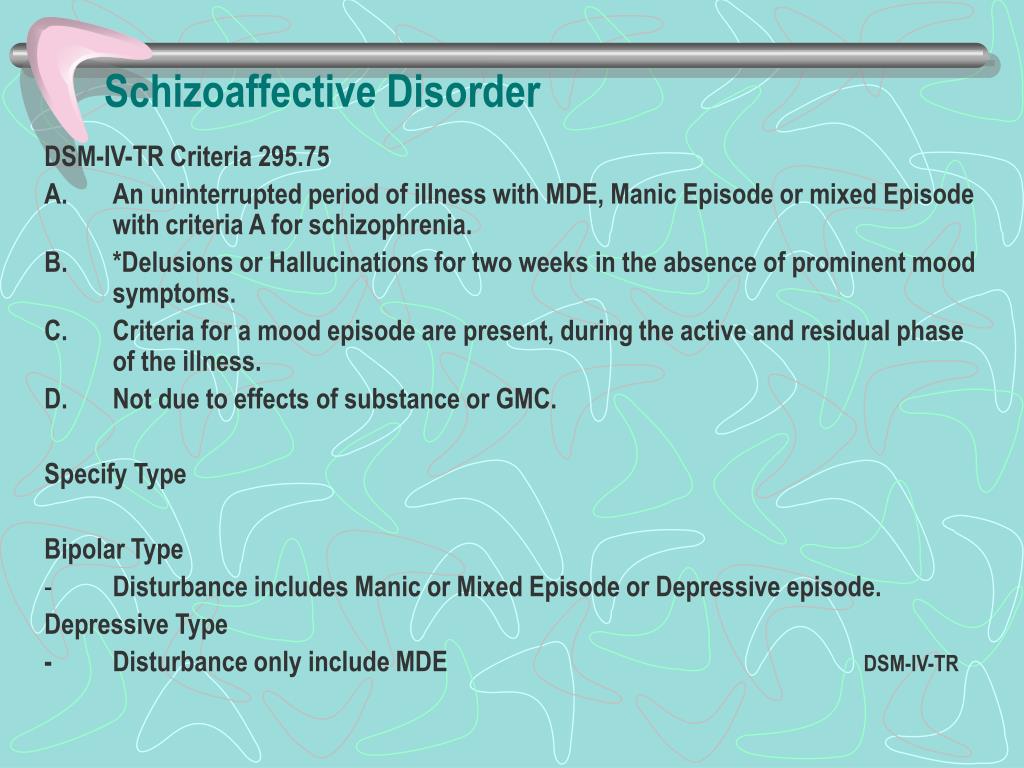 I was diagnosed with fractures of the bones of the skull, fractures of the bones of the pelvis, one rib, sternum, processes of two lumbar vertebrae, bruises of the brain, lungs and heart.
I was diagnosed with fractures of the bones of the skull, fractures of the bones of the pelvis, one rib, sternum, processes of two lumbar vertebrae, bruises of the brain, lungs and heart.
For the first two weeks I was in the intensive care unit. During this period, various doctors visited me, but there was no psychiatrist among them. Then I was transferred to another hospital to have an MRI. There I was visited by a staff psychiatrist. The doctor talked to me, but superficially: she did not collect a detailed history. Suicidal thoughts by this moment no longer bothered me, but there was a feeling of depression, shame and longing for missed opportunities. I cried a lot, which was generally uncharacteristic for me.
I was diagnosed with depression again, started taking antidepressants, and a week later, still bedridden, I was transferred to a psychiatric hospital. The translation went badly. Already in the hospital, I was asked to sign a voluntary consent for treatment. At the same time, the doctor, in my opinion, behaved unethically: he said that if I did not sign the document, I would be hospitalized by force - by a court decision.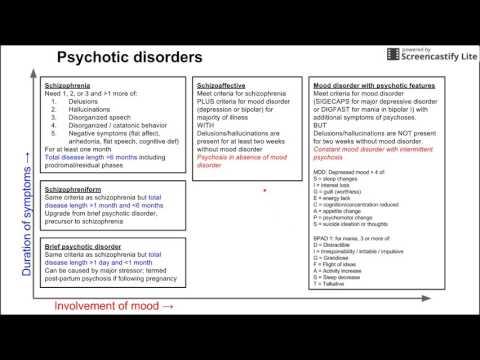 In this case, it will take longer to treat me. I wanted to stay in the hospital and was not going to argue with the psychiatrist.
In this case, it will take longer to treat me. I wanted to stay in the hospital and was not going to argue with the psychiatrist.
/bipolyarnoe-rasstroystvo/
How much does the treatment of bipolar affective disorder cost? I was asked in detail about how the disease developed and what preceded it. Depression was eventually ruled out and schizoaffective disorder of the depressive type was assumed.
After some time of observation, the diagnosis was confirmed and the antipsychotic Latuda was prescribed. This medicine helps to eliminate delusional ideas, in my case, the idea of worthlessness. Therapy almost immediately made me feel better.
The psychiatric hospital also had its own department of physiotherapy and a polyclinic with doctors of various specialties - they helped me recover from injuries.
Closer to discharge, I contracted the coronavirus. I was transferred to the covid ward, then back to the "clean" one. To be discharged from the “clean” department, one had to pass a test from a psychologist. And I could not meet him for a long time, because the time of his appointments coincided with the physiotherapy procedures. As a result, I left the hospital only after two months.
And I could not meet him for a long time, because the time of his appointments coincided with the physiotherapy procedures. As a result, I left the hospital only after two months.
How do I continue to be treated at home
I am being followed up by compulsory medical insurance in a psycho-neurological dispensary. It is necessary to visit a psychiatrist once a month, but I do not always manage to keep this schedule. I try to go for consultations at least once every one and a half months.
I continue to take Latuda. I get the drug for free - on preferential prescriptions.
Recently, my anxiety increased, I went to the dispensary unscheduled. The psychiatrist put me on the Rocon antidepressant again. But, remembering the previous experience, I doubted that it would help, so I turned to a private psychiatrist. He prescribed a tranquilizer tofisopam, this drug should eliminate the feeling of anxiety.
How much the doctor's consultation cost, I don't know exactly - it was paid by my father.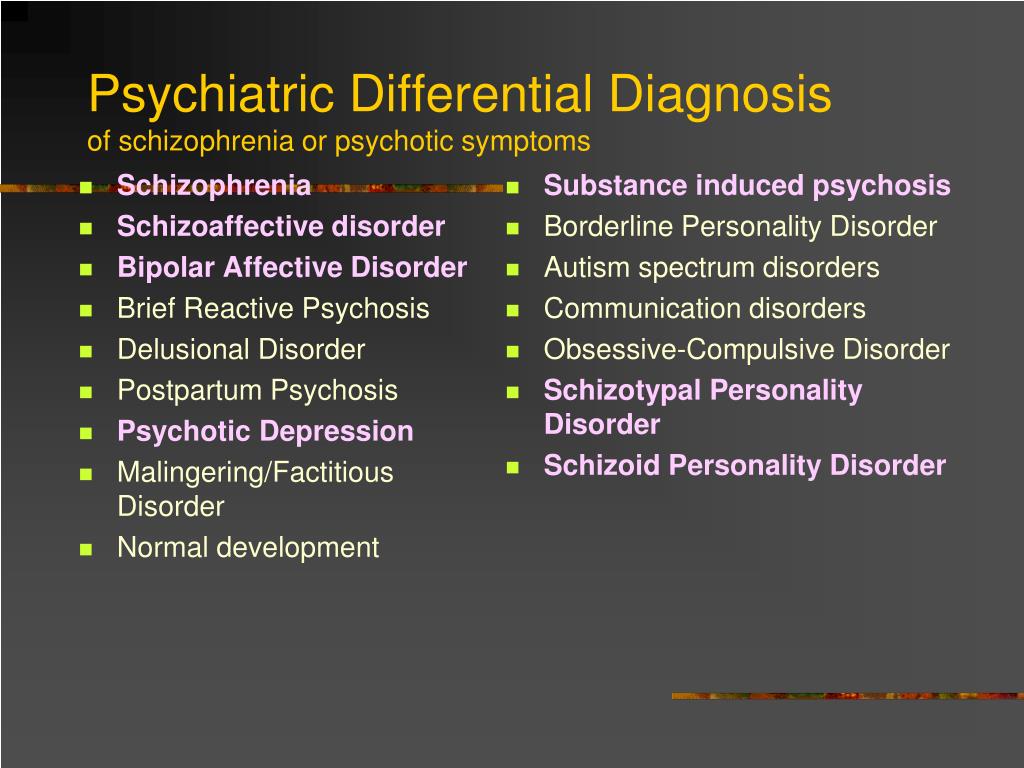
 Affect dominant form
Affect dominant form 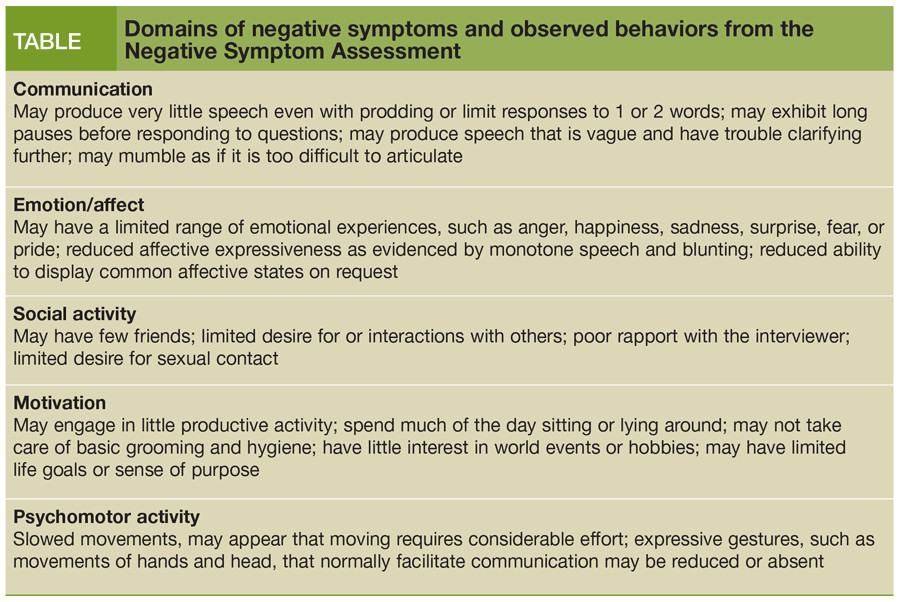 Acute polymorphic psychotic disorder without symptoms of schizophrenia
Acute polymorphic psychotic disorder without symptoms of schizophrenia 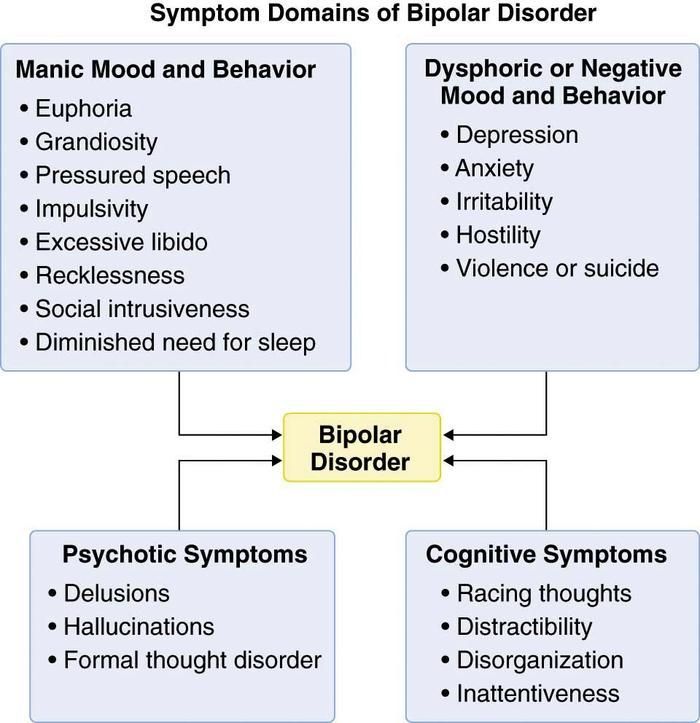 Schizoaffective disorder, manic (depressive, mixed) type
Schizoaffective disorder, manic (depressive, mixed) type