Rapid cycling mood disorders
Rapid Cycling Bipolar Disorder - DBSA
Bipolar disorder with rapid cycling is diagnosed when a person experiences four or more episodes of mania, hypomania, or depressive episodes in any 12-month period. Rapid cycling can occur with any type of bipolar disorder, and maybe a temporary condition for some people.
What is rapid cycling?People who live with bipolar experience the “highs” that come with mania or hypomania, they also experience “lows” that come with depression. When Rapid Cycling occurs, it means that four or more manic, hypomanic, or depressive episodes have taken place within a twelve-month period. Changes in mood here can happen quickly and occur over a few days or even over a few hours. If there are four mood changes within a month, it is called ultra-rapid cycling. While the phrase “rapid cycling” may make it seem that there is a regular cycle to these shifts in mood, most cycles do not follow a pattern.
Who develops rapid cycling?As many as half of all individuals who live with bipolar may develop rapid cycling at some time. For most, rapid cycling is a temporary occurrence. For a small number of individuals, the pattern of cycling can continue indefinitely. While there are no hard rules for who will develop rapid cycling, it may be more likely to develop in women. Bipolar is equally common in both genders.
The cause of rapid cycling is unknown however, there are several theories that have been posed:
KindlingThe kindling theory proposes that early episodes are triggered by actual or anticipated life events. Stressful circumstances such as loss of a job or of a loved one may become ‘triggers’ for that individual. Again, this can be actual or anticipated. Perceived or actual stress associated with these circumstances may result in the cycling of mood seen in rapid cycling. As the triggers continue to present themselves an individual can experience the increase of cycling.
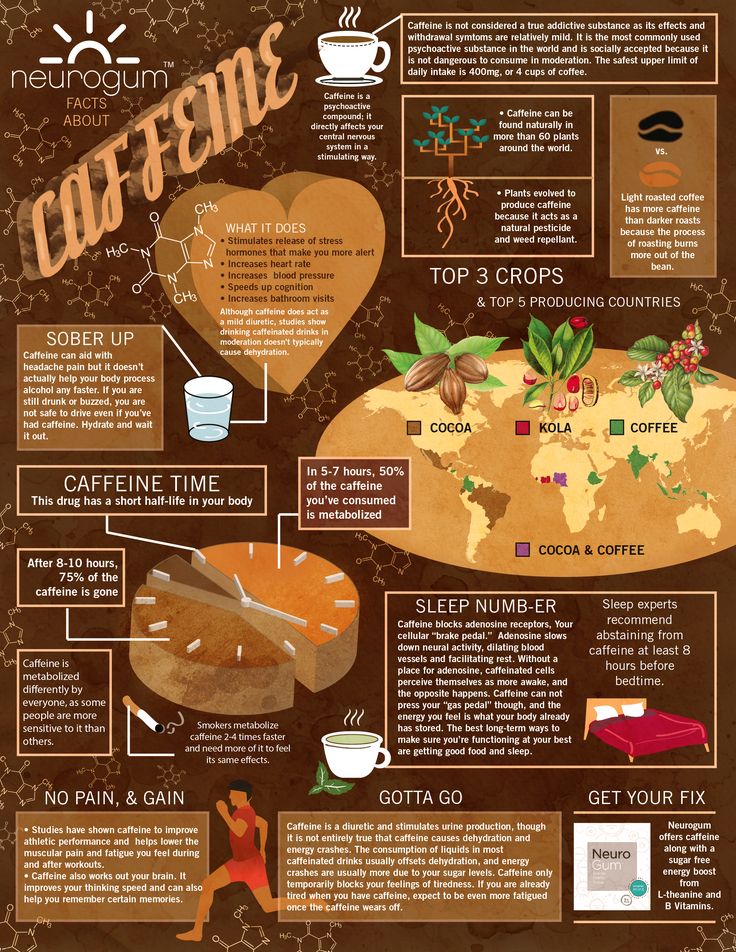
Circadian or Biological RhythmsThis theory proposes that individuals who experience rapid cycling are “out of sync” with their typical biological rhythms.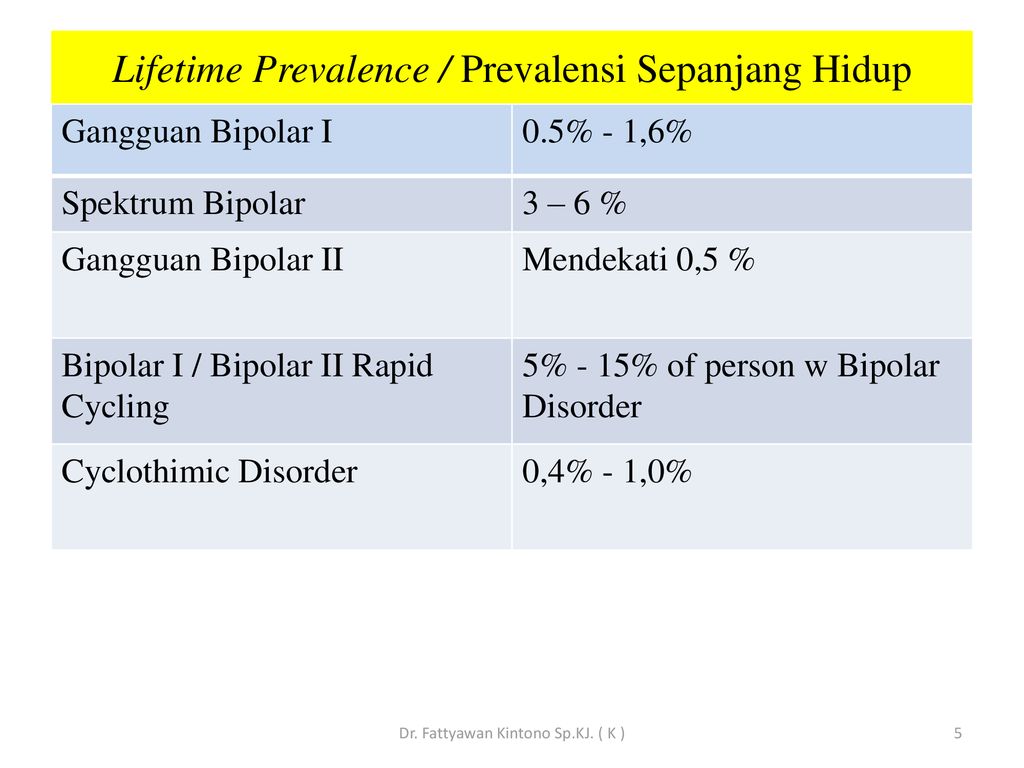 Circadian rhythms represent the 24-hour cycle that people experience each day. This rhythm keeps people in sync with dusk and dawn, sleep, and activity. While it is uncertain if inconsistency with circadian rhythms can cause rapid cycling, it is understood that good sleep hygiene can mitigate symptoms associated with bipolar.
Circadian rhythms represent the 24-hour cycle that people experience each day. This rhythm keeps people in sync with dusk and dawn, sleep, and activity. While it is uncertain if inconsistency with circadian rhythms can cause rapid cycling, it is understood that good sleep hygiene can mitigate symptoms associated with bipolar.
Hypothyroidism means that the thyroid is underactive in the system and is not producing enough of the thyroid hormone for the brain. Some with rapid cycling have responded to treatment with the thyroid hormone.
Anti-DepressantsIt has been found that anti-depressants can increase the frequency of cycling. Some experts have advised against the use of anti-depressants in individuals living with bipolar, especially for the long term. More commonly individuals living with bipolar are prescribed mood-stabilizing drugs which can be a treatment for rapid cycling. Before changing medication, talk to your physician.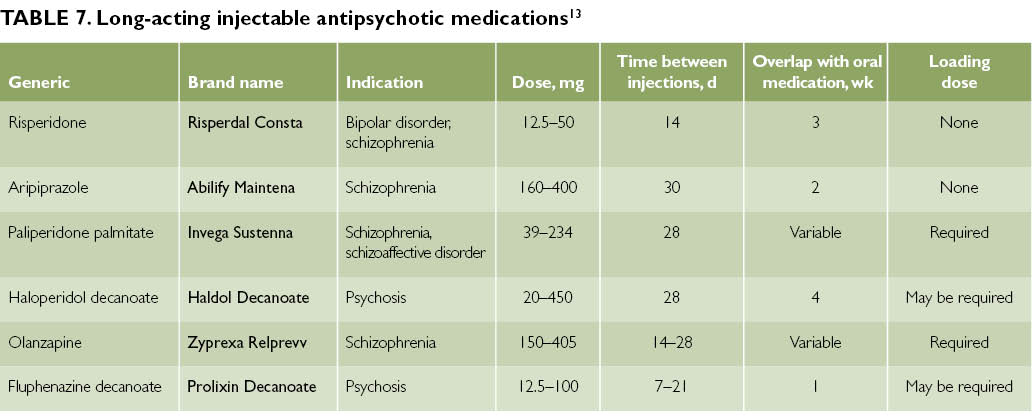 Do not stop medication without first consulting with your physician.
Do not stop medication without first consulting with your physician.
Rapid cycling is not its own diagnosis, rather a specifier that defines how the course of a bipolar diagnosis is experienced. It can be difficult to treat rapid cycling, however, people may find benefit in talk therapy and tracking their mood.
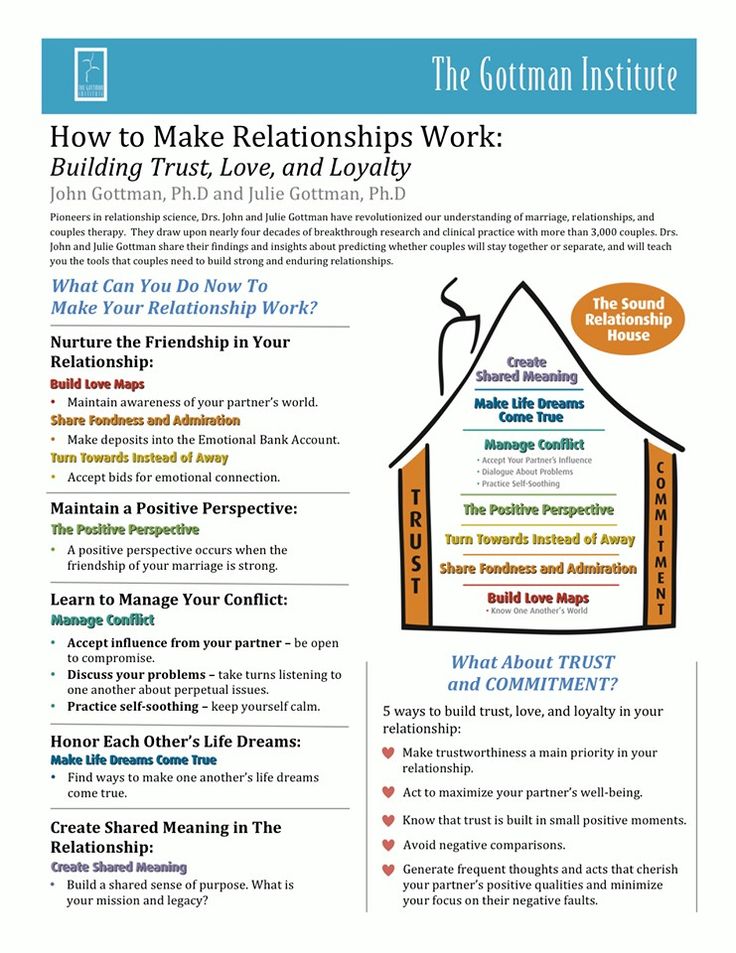
Mood TrackingKeeping track of your mood may help you understand patterns that cause stress. By keeping records of mood changes, as well as lifestyle factors such as sleep, diet, exercise you can better understand what may trigger mood shifts.
Talk TherapyTalk therapy can help people to identify and stick to a specific treatment plan. Collaborating with a therapist can help people who are experiencing rapid cycling. Feelings such as irritability, sadness, and racing thoughts can interfere with day to day life. By talking to a therapist those feelings can be explored in a “judgment free zone. ” Establishing a treatment plan with a therapist can help you keep track of what improves or worsens symptoms.
” Establishing a treatment plan with a therapist can help you keep track of what improves or worsens symptoms.
Rapid Cycling Bipolar Disorder Symptoms, Treatments, Causes, and More
Written by Matthew Hoffman, MD
In this Article
- What Is Rapid in Cycling Bipolar Disorder?
- Who Gets Rapid Cycling Bipolar Disorder?
- What Are the Features of Bipolar Disorder?
- How Is Rapid Cycling Bipolar Disorder Identified?
- How Is Bipolar Disorder with Rapid Cycling Treated?
- What Are the Risks of Rapid Cycling Bipolar Disorder?
What Is Rapid in Cycling Bipolar Disorder?
Rapid cycling is a pattern of frequent, distinct episodes in bipolar disorder. In rapid cycling, a person with the disorder experiences four or more episodes of mania or depression in one year. It can occur at any point in the course of bipolar disorder, and can come and go over many years depending on how well the illness is treated; it is not necessarily a "permanent" or indefinite pattern of episodes.
Who Gets Rapid Cycling Bipolar Disorder?
Virtually anyone can develop bipolar disorder. About 2.5% of the U.S. population suffers from some form of bipolar disorder - nearly 6 million people. A rapid cycling pattern may occur in about 10% to 20% of people with the disorder. Women, and people with bipolar II disorder, are more likely to experience periods of rapid cycling.
Most people are in their late teens or early 20s when symptoms of bipolar disorder first start. Nearly everyone with bipolar disorder develops it before age 50. People with an immediate family member with bipolar disorder are at higher risk.
What Are the Features of Bipolar Disorder?
The major features of bipolar disorder include:
- At least 1 episode of mania or hypomania in the patient's lifetime
- Episodes of depression (major depressive disorder), which are often recurrent
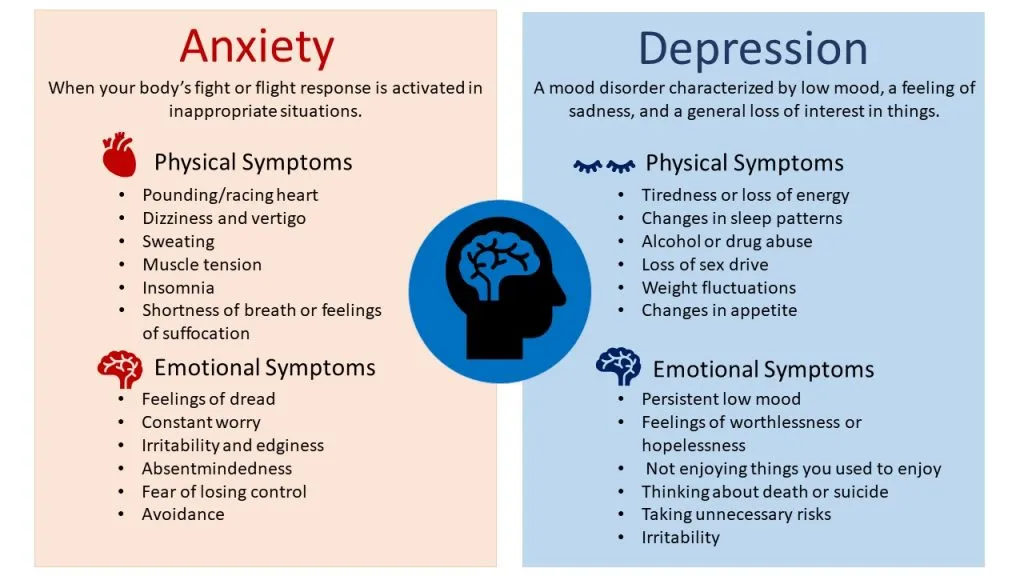
Mania is a period of abnormally elevated mood and high energy, usually accompanied by erratic behavior lasting at least seven days at a time. Hypomania is an elevated mood not reaching full-blown mania and lasting a minimum of four days.
Hypomania is an elevated mood not reaching full-blown mania and lasting a minimum of four days.
A few people with rapid cycling bipolar disorder alternate between periods of hypomania and major depressive disorder. Far more commonly, though, repeated and distinct episodes of depression dominate the picture. Repeated periods of depression are punctuated by infrequent, shorter periods of elevated or normal mood.
How Is Rapid Cycling Bipolar Disorder Identified?
Bipolar disorder is diagnosed after someone experiences a hypomanic or manic episode along with multiple additional episodes of either mania, hypomania or depression. Rapid cycling in itself is not a diagnosis, but rather a "course specifier" or descriptor of the course of illness. In bipolar disorder rapid cycling is identified when four or more distinct episodes of depression, mania, or hypomania occur during a one year period.
Rapid cycling bipolar disorder can be difficult to identify, because a single mood episode can sometimes simply wax and wane without resolving. As a result, they don't necessarily represent multiple separate and distinct episodes. Rapid cycling may seem to make the changing mood states of bipolar disorder more obvious, but because most people with rapid cycling bipolar disorder spend far more time depressed than manic or hypomanic, they are often misdiagnosed with unipolar depression.
As a result, they don't necessarily represent multiple separate and distinct episodes. Rapid cycling may seem to make the changing mood states of bipolar disorder more obvious, but because most people with rapid cycling bipolar disorder spend far more time depressed than manic or hypomanic, they are often misdiagnosed with unipolar depression.
For example, in one study of people with bipolar II disorder, the amount of time spent depressed was more than 35 times the amount of time spent hypomanic. Also, people often don't take note of their own hypomanic symptoms, mistaking them for a period of unusually good mood.
How Is Bipolar Disorder with Rapid Cycling Treated?
Because symptoms of depression dominate in most people with a rapid cycling course of bipolar disorder, treatment is usually aimed toward stabilizing mood, mainly by relieving depression while preventing the comings-and-goings of new episodes.
Antidepressants such as fluoxetine (Prozac), paroxetine (Paxil,) and sertraline (Zoloft) have not been shown to treat the depression symptoms of rapid cycling bipolar disorder, and may even increase the frequency of new episodes over time. Many experts therefore advise against the use of antidepressants (especially long term) in bipolar patients with rapid cycling.
Many experts therefore advise against the use of antidepressants (especially long term) in bipolar patients with rapid cycling.
Mood-stabilizing drugs -- such as carbamazepine (Tegretol), lamotrigine (Lamictal ), lithium (Lithobid), and valproate (Depakote)-- are the core treatments of rapid cycling. Often, a single mood stabilizer is ineffective at controlling episode recurrences, resulting in a need for combinations of mood stabilizers. Several antipsychotic medicines such as olanzapine (Zyprexa) or quetiapine (Seroquel) also have been studied in rapid cycling and are used as part of a treatment regimen, regardless of the presence or absence of psychosis (delusions and hallucinations).
Treatment with mood stabilizers is usually continued (often indefinitely) even when a person is symptom-free. This helps prevent future episodes. Antidepressants, if and when used, are generally tapered as soon as depression is under control.
What Are the Risks of Rapid Cycling Bipolar Disorder?
The most serious risk of a rapid cycling course in bipolar disorder is suicide.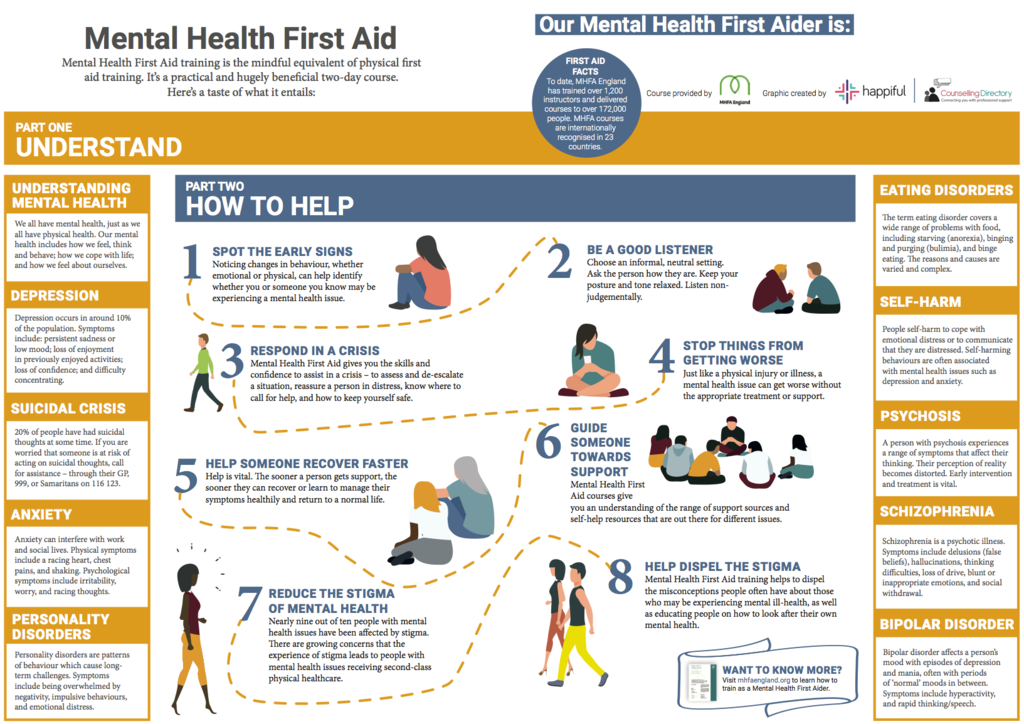 People with bipolar disorder are 10 times to 20 times more likely to commit suicide than people without bipolar disorder. Tragically, 8% to 20% of people with bipolar disorder eventually lose their lives to suicide.
People with bipolar disorder are 10 times to 20 times more likely to commit suicide than people without bipolar disorder. Tragically, 8% to 20% of people with bipolar disorder eventually lose their lives to suicide.
People with a rapid cycling course may be at even higher risk for suicide than those with nonrapid cycling bipolar disorder. They are hospitalized more often, and their symptoms are usually more difficult to control long term.
Treatment reduces the likelihood of serious depression and suicide. Lithium in particular, taken long term, has been shown to reduce the risk.
People with bipolar disorder are also at higher risk for substance abuse. Nearly 60% of people with bipolar disorder abuse drugs or alcohol. Substance abuse is associated with more severe or poorly controlled bipolar disorder.
Bipolar Disorder Guide
- Overview
- Symptoms & Types
- Treatment & Prevention
- Living & Support
All About Bipolar Affective Disorder
What is Bipolar Affective Disorder?
Bipolar affective personality disorder, or manic-depressive psychosis, is a complex, mental illness characterized by constant mood swings.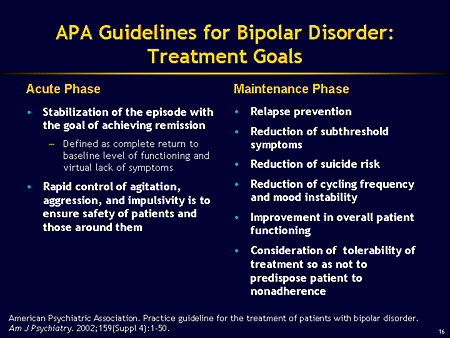 This is not an ordinary mood change that happens to every person, but a systematic psycho-emotional drop with a short-term normal state. It is the episodes from depression to an extremely agitated state that are called affective. In Russia, 1% of the population is affected by this disease. As a rule, it is observed among young women aged 20 to 30 years. However, men are also prone to bipolar disorder, and they begin it earlier than women. And if in women it begins with a depressive phase, then in men it starts with a manic phase. The appearance of symptoms of bipolar disorder in women is often associated with hormonal disorders and the characteristics of the menstrual cycle.
This is not an ordinary mood change that happens to every person, but a systematic psycho-emotional drop with a short-term normal state. It is the episodes from depression to an extremely agitated state that are called affective. In Russia, 1% of the population is affected by this disease. As a rule, it is observed among young women aged 20 to 30 years. However, men are also prone to bipolar disorder, and they begin it earlier than women. And if in women it begins with a depressive phase, then in men it starts with a manic phase. The appearance of symptoms of bipolar disorder in women is often associated with hormonal disorders and the characteristics of the menstrual cycle.
Bipolar affective disorder can destroy personal relationships, impair the quality of work, reduce academic performance, and in some cases even lead to suicide. Therefore, it is so important to diagnose it in time and prescribe appropriate treatment.
Causes of bipolar affective disorder
To date, doctors cannot answer the question about the exact causes of this disease. It is known for certain that it can be genetically transmitted, but sometimes it is in "sleep mode" until it is triggered by some stressful event. Also, pushing factors for the development of BAD can be:
It is known for certain that it can be genetically transmitted, but sometimes it is in "sleep mode" until it is triggered by some stressful event. Also, pushing factors for the development of BAD can be:
- chronic fatigue;
- overwork;
- emotional burnout;
- dissatisfaction with personal life;
- death of a loved one;
- financial problems;
- dissatisfaction with life;
- sensitivity and susceptibility to things;
- melancholic character;
- head injury;
- use of drugs and alcohol.
Disease pathogenesis
The pathogenesis of bipolar affective disorder, that is, the onset and development of the disease, is currently not fully understood. At 95%, we can only say that it is transmitted genetically and is associated with neurochemistry. According to studies, in 80% of cases the nature of the disease is associated with the environment of the patient and only 20% is transmitted genetically. The causes of manic phases are increased tone of the central nervous system, as well as hyperfunction of the thyroid gland and pituitary gland.
The causes of manic phases are increased tone of the central nervous system, as well as hyperfunction of the thyroid gland and pituitary gland.
Symptoms or how the disease manifests itself
As a rule, signs of bipolar affective disorder are observed in patients in the autumn-winter and winter-spring periods. And the point is not only in climatic features, but also in weakened immunity at the indicated times of the year.
BAD is divided into 2 phases: depressive and manic, and can manifest itself equally in both phases. The frequency of the phases and their change is very individual for each individual patient and lasts from 2 weeks to 2 years. However, even the duration of the disease cannot lead to any mental defects, such as schizophrenia, on the contrary, rather, patients with schizophrenia develop a “bipolar disorder”.
Bipolar affective disorder is characterized precisely by the sequence of the above phases. A patient with mania can be recognized by the following features:
- increased hyperactivity;
- excitability for more than a week;
- fast speech;
- great flow of speech and confusion of thought;
- rapid change in mood;
- increased self-esteem.

The latter entails performing overwhelming tasks that patients cannot afford. Also, the patient is accompanied by irritability, mild euphoria, excessive frankness in conversations and behavior. A person sleeps little, and 2 hours of sleep is enough for him to feel good. In rare cases, the phase is accompanied by delusions of grandeur or persecution, sound and / or auditory hallucinations. At the same time, the symptoms of the depressive phase are slightly different. It:
- laziness and apathy;
- depressed mood;
- constant desire to sleep;
- physical ailment;
- anxiety;
- heaviness in legs and head;
- unwillingness to do something.
At the slightest detection of symptoms and signs of bipolar affective disorder in a patient, an early diagnosis and surgical treatment of the disease is required. This applies to any course of the disease, even if the depressed mood or the sudden change of mood in a person lasts only a few days. Any timely help will be salvation and help for the patient and will help to survive the course of the disease more easily. Painful perception of criticism, shallow depression, anxiety, unreasonable anxiety - all this, too, should alert and serve as an impetus for taking decisive action. As mentioned above, both men and women are prone to bipolar disorder, although they are more common in the latter. This is due not only to menstrual irregularities and hormonal disorders, but also to a severe course during childbirth, the so-called postpartum depression. As a rule, women are more susceptible to the unipolar course of bipolar disorder, when the course of the disease is accompanied by only one of the phases: manic or depressive. The latter is usually more common.
Any timely help will be salvation and help for the patient and will help to survive the course of the disease more easily. Painful perception of criticism, shallow depression, anxiety, unreasonable anxiety - all this, too, should alert and serve as an impetus for taking decisive action. As mentioned above, both men and women are prone to bipolar disorder, although they are more common in the latter. This is due not only to menstrual irregularities and hormonal disorders, but also to a severe course during childbirth, the so-called postpartum depression. As a rule, women are more susceptible to the unipolar course of bipolar disorder, when the course of the disease is accompanied by only one of the phases: manic or depressive. The latter is usually more common.
Bipolar affective disorder symptoms in women are accompanied by rapid cycles and mixed episodes. The prerequisites for them are eating disorders, alcohol or drug addiction, abuse of antidepressants. In addition, women are more prone to migraines, thyroid disorders, diabetes and obesity. It is these external stimuli that become the prerequisites for the development of BAD. Childbirth also becomes one of the factors in the development of the depressive phase, if a woman has already been diagnosed with this disease before them. In this case, the risks of developing the disease increase several times. Women are also more likely to have suicidal thoughts.
It is these external stimuli that become the prerequisites for the development of BAD. Childbirth also becomes one of the factors in the development of the depressive phase, if a woman has already been diagnosed with this disease before them. In this case, the risks of developing the disease increase several times. Women are also more likely to have suicidal thoughts.
But in men, the symptoms of bipolar affective disorder largely depend on external factors, and the course of the disease is a little milder. The periods between phases are long and get worse over time. With inadequate and untimely treatment, the disease progresses and it becomes more difficult to get rid of it. Mostly in men, a mixed type of disorder is observed, which is accompanied by a short-term remission. In men, more often than women, the ability to do something is lost, concentration of attention decreases, and insomnia appears. And if in women one phase of BAD can last longer than another, then in men the duration is almost the same.
In addition to external factors that influence the development of bipolar disorder in men, such as unsettled life, problems in personal life and at work, financial difficulties, a common cause of the development of the disease is long-term alcohol consumption.
Classification of affective disorder
This disease is classified into different types and phases. So, according to the international classification of diseases (ICD-11), types of bipolar affective disorder are divided into 1 and 2. The classic course, as mentioned earlier, is manic and depressive, and one phase can either last a long time or change abruptly to another. Another phase is due to a sharp transition - from manic to depressive without any interruptions. Frequent, long phases with rapid cyclicity - 4 or more phases significantly affect the patient's condition, his quality of life and are a poor prognosis for the course of the disease.
Bipolar affective disorder type 1 is accompanied by an aggravation of mania and pronounced depression, which leads to a violation of normal functioning. As a result - frequent hits in hospitals or police stations. Patients have a pronounced apathy, a complaint about themselves, the inability to do any business. The patient, as a rule, begins to blame himself, to consider himself incapable of anything.
And if BAD type 1 is characterized by a phase change, then bipolar affective disorder type 2 is due to the presence of only a depressive episode without mania. The course of the disease is similar to unipolar depression, however, these are two completely different diseases. If in patients in the first case, with prolonged use of antidepressants, everything returns to normal, then in patients with BAD type 2, they are not only contraindicated, sometimes, but can also cause hypomania, which has an extremely negative effect on the course of the disease. The phases last longer, replace each other faster, a mixed state occurs, which a person can hardly endure.
By phases, bipolar disorder is divided into the following types: manic, depressive, and also, a mixed episode of bipolar affective disorder is distinguished. The latter can be manifested by sudden outbursts of fun in a state of melancholic mood.
Other indicators are:
As a rule, the symptoms of this episode last about 1 week or quickly change. Sometimes a patient with a disorder is accompanied by insomnia, suicidal thoughts, lack of appetite. Pronounced symptoms are the reason for the patient's social and professional maladaptation and a significant deterioration in the quality of life.
If we talk about the depressive phase of bipolar affective disorder, then it is caused by several factors and is accompanied by the following symptoms:
- Endogenous depression (permanent depressed mood) accompanied by vitality - feeling alive, able to move, energetic.

- In the stage of the depressive triad, when a person does not feel like a full-fledged member of society and melancholy is fully manifested, slowness in speech and movement is observed.
- Pronounced change of mood. From the morning bad mood with a feeling of melancholy and anxiety, nothing remains by the evening.
- Disorder of appetite. Not a single meal seems tasty to the patient, he begins to lose weight, and in women there may be a violation of the monthly cycle up to complete disappearance.
- May present with psychomotor retardation.
- Constant feeling of melancholy.
- Complete decrease in sexual desire and loss of maternal instinct.
- Periodic occurrence of suicidal thoughts.
- Occasionally, some patients experience tachycardia, constipation and mydriasis - dilated pupils.
- Rarely, delusions, hallucinations may occur.
It is important to understand that patients are at high risk of suicide during this phase. According to statistics, this phenomenon occurs in 40% of cases. Therefore, it is so important to diagnose it in time for subsequent timely treatment.
According to statistics, this phenomenon occurs in 40% of cases. Therefore, it is so important to diagnose it in time for subsequent timely treatment.
The manic phase of bipolar affective disorder varies in severity from elevated mood to severe mania. In the first state there is no self-criticism, a person is adaptive to the environment. This phase is characterized by the following symptoms:
- Manic triad: increased mood, accelerated thinking, movements.
- Activity, energy, burst of energy. The patient takes on many things, but does not complete any one.
- Lack of concentration.
This phase has 5 stages:
- Hypomanic, which is characterized by increased mood and cheerfulness. Patients experience an increase in appetite and sleep duration.
- Expressive, which is accompanied by constant jokes and chatter against the background of short-term outbursts of anger.
- A violent state in which a prolonged excited state is accompanied by disorder and incoherent speech.
- Motor calmness.
- Reactive with the return of all symptoms of mania to normal. Sometimes in this scenario, patients may experience amnesia and some episodes of mania are simply forgotten.
If the main symptom of the manic phase of bipolar affective disorder is increased excitability, then in the depressive phase, on the contrary, the mood is constantly sluggish. Patients with a manic stage of development cannot soberly assess their behavior or completely deny it. In parallel with euphoria, irritability and anxiety develop. A person is uncomfortable in this state.
It is possible to make a diagnosis with a prolonged course of the disease - more than 1 week with the preservation of the phase at the main time of the day. Along with irritability, 4 additional symptoms will certainly appear. Symptoms can shift in different directions, turn from hypomania - a mild state, high activity and high spirits, into a manic psychosis. Patients with psychosis are visibly active, behaving erratically, sometimes screaming, sometimes singing. Excitation reaches its climax, the state is not stable, irritability increases, sometimes delusions or hallucinations develop. Manic psychosis is often confused with schizophrenia.
Excitation reaches its climax, the state is not stable, irritability increases, sometimes delusions or hallucinations develop. Manic psychosis is often confused with schizophrenia.
Mixed bipolar affective disorder is a mixture of two phases that literally drives the patient crazy. On the one hand, he has a pronounced stream of brilliant thoughts, on the other, suicidal thoughts and feelings of guilt. This is a very dangerous phase, which is a prerequisite for suicide. The feeling of anxiety grows even more than in the other two phases, especially if it is caused by alcohol.
A patient with bipolar disorder cannot perceive criticism and does not adequately assess his condition. Any episodes can cause rash actions, unreasonable risks that pose a threat to both him and other people.
No matter what type a person has and no matter how the course of bipolar affective disorder passes, timely diagnostics will help stop the course of the disease and prevent future complications. It is important to understand that a person's life is divided into several bands with the development of this disease: months of impenetrable darkness and the same amount of time of euphoria. The person himself does not understand that he needs help, and he does not consider himself sick.
It is important to understand that a person's life is divided into several bands with the development of this disease: months of impenetrable darkness and the same amount of time of euphoria. The person himself does not understand that he needs help, and he does not consider himself sick.
If a person develops bipolar disorder against the background of other concomitant mental illnesses, such as:
- obsessive state;
- alcohol or drug addiction;
- eating disorders;
- Attention deficit coupled with hyperactivity;
- social phobia;
- panic attacks and other diseases, the course of the disease can worsen significantly.
Complications of bipolar affective disorder
Complications of bipolar affective disorder are characterized by the development of non-medical diseases, namely asocial adaptation. Thought processes also change, mental ability and attention decrease, memory deteriorates. In some patients, the worldview changes completely.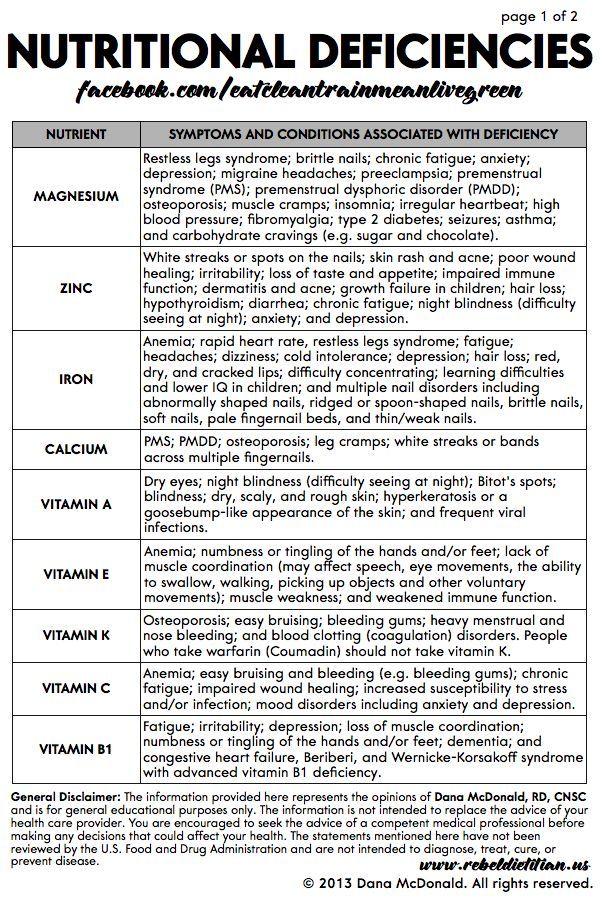 According to the conducted research, it was revealed that the creative potential directly depends on the course of BAD. People could not make contact with others. This applies, by the way, to both adults and children.
According to the conducted research, it was revealed that the creative potential directly depends on the course of BAD. People could not make contact with others. This applies, by the way, to both adults and children.
Patients with a depressive phase and suicidal thoughts are prone to it, which can also serve as a sad outcome for a person. A constant change of mood, a complete change in thoughts and consciousness, the inability to lead a full life, live in a family and raise children, the inability to adequately assess one's condition and others - these and many other possible consequences of bipolar affective disorder that need to be nipped in the bud and prevent the disease from developing .
When to see a doctor?
You need to consult a doctor already if one or two of the above symptoms occur, regardless of the phase, for 1 or more weeks.
When you understand that a person close to you is constantly in a depressed state and immediately becomes cheerful, when a person gets bored with life, his hands drop, or he is energetic, excited, grabs at everything, but does not complete everything to the end, then it is worth sounding the alarm. Only a doctor will be able to diagnose whether it is a disorder, what degree it has, and how the course develops.
Diagnostics
Diagnosis of bipolar affective disorder is based, first of all, on a survey of the patient himself. After all, he does not admit to the presence of hypomania or mania until he is asked. Questions about suicide, plans for the future, can be good helpers in identifying the disease. The second key point is the delivery of hormones to check the functions of the thyroid gland. Among other things, it is necessary to obtain an anamnesis for the use of drugs and alcohol by collecting urine and blood.
It is important to periodically evaluate people with schizophrenia for manic symptoms, however, unlike people who have bipolar disorder, they cannot return to normal between phases. Panic attacks, phobias, obsessive-compulsive disorders can make the diagnosis much more difficult.
Panic attacks, phobias, obsessive-compulsive disorders can make the diagnosis much more difficult.
Treatment
Treatment of bipolar affective disorder is possible both with the help of therapy and medication.
Treatment consists of several stages:
- Relief and control of symptoms.
- Long-term treatment until remission is achieved.
- Treatment maintenance and prevention. Trying to keep remission.
The choice of medicines is a little complicated by their possible side effects, moreover, no medicine can be called universal. It is important to apply the drugs previously prescribed to the patient, which gave a positive result. If the treatment will take place for the first time, then the appointment of drugs depends on the history of the disease and symptoms. Treatment of severe forms may be accompanied by the appointment of specific antidepressants, the effectiveness of which, however, has not been proven.
Among the drugs for the treatment of bipolar affective disorder, mood stabilizers and antipsychotics of the 2nd generation are distinguished.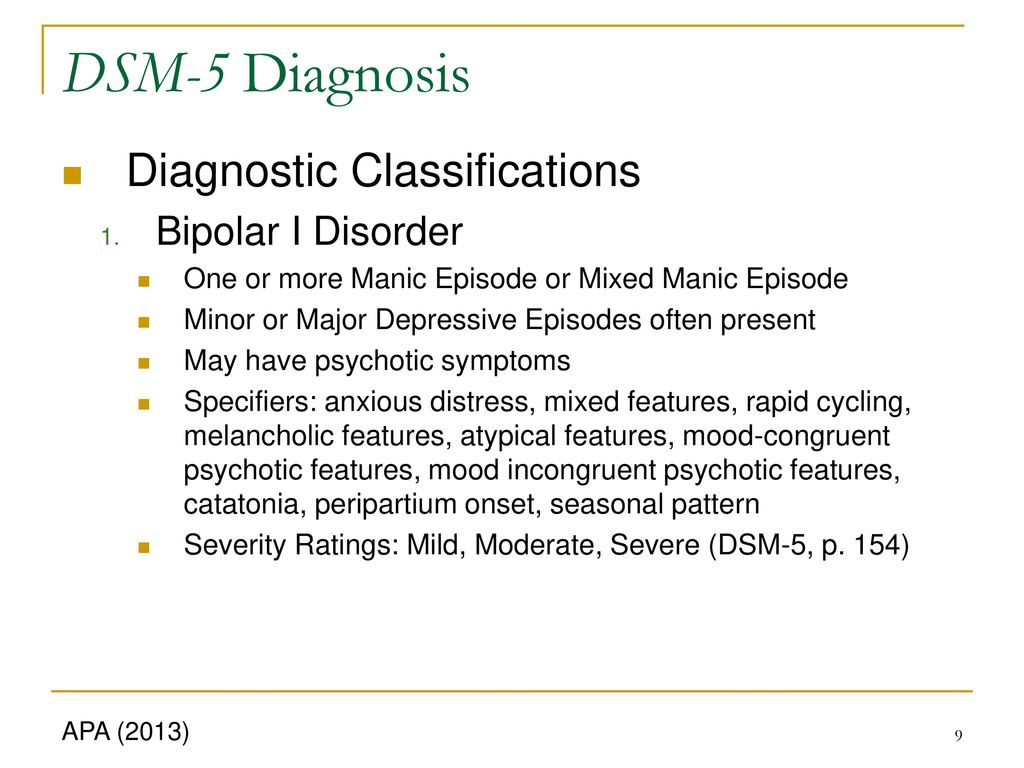 They can be used both separately and in combination with each other. For a more effective recovery, the patient needs to independently work to improve his condition. Hospitalization is possible, but only in a manic episode with type 1 bipolar disorder. At the same time, treatment can be both voluntary and compulsory. Staying in the clinic during this period is a long stage, as full outpatient treatment is carried out.
They can be used both separately and in combination with each other. For a more effective recovery, the patient needs to independently work to improve his condition. Hospitalization is possible, but only in a manic episode with type 1 bipolar disorder. At the same time, treatment can be both voluntary and compulsory. Staying in the clinic during this period is a long stage, as full outpatient treatment is carried out.
In addition to drug treatment, therapy for bipolar affective disorder is used. This can be phototherapy during the bipolar season of any type. However, this method is concomitant. The main treatment is medication and symptomatic relief.
It is also important to correctly predict the further course of the disease, because the quality of treatment depends on this. Among all types of phases and periods, a fast-cyclic disorder can be predicted the worst, since it is often diagnosed incorrectly, which entails subsequent incorrect treatment.
+7 (495) 121-48-31
Prevention or advice in case of illness
There are no clinical guidelines for bipolar affective disorder as such. It is important not only to maintain therapy, but also to exclude factors that can cause the development of the disease and eliminate all negative factors:
It is important not only to maintain therapy, but also to exclude factors that can cause the development of the disease and eliminate all negative factors:
- exclude alcohol and any psychotropic substances;
- observe sleep and food intake;
- lead a healthy lifestyle;
- actively communicate with colleagues and friends;
- try not to be alone;
- find any hobbies outside of work.
These simple rules will help, if not cured, then delay the approach of the disease for a long time and make it easier to endure its course. If you notice any of the above symptoms in yourself or your loved ones, be sure to consult a doctor. The specialists of our clinic will help to make a timely diagnosis, highlight the phase of bipolar disorder and prescribe the right treatment that will give a positive result. Be healthy!
References:
- Zhmurov V.A. Mental disorders
- Tyuvina N. A., Stolyarova A.
 E., Smirnova V. N. Bipolar affective disorder: gender characteristics of the course and therapy
E., Smirnova V. N. Bipolar affective disorder: gender characteristics of the course and therapy - Tiganov A.S., Snezhnevsky A.V., Orlovskaya D.D., Manual of Psychiatry
- Tiganov A.S. Manual of Psychiatry - M. Medicine
- Bukhanovsky A.O., Kutyavin Yu.A., Litvak M.E. General psychopathology
- A.V. Snezhnevsky - Clinical Psychiatry
- Gert Sauer Siberian Lectures on Analytical Psychology
Bipolar disorders: clinical picture and principles of therapy :: DIFFICULT PATIENT
N.V. Sturov, O.L. Romanova
Peoples' Friendship University of Russia, Moscow
Introduction
Bipolar disorder (BD) is a widespread severe chronic mood pathology characterized by episodes of mania or hypomania that alternate or are combined with episodes of depression [1]. In the absence of treatment, BD is accompanied by high mortality from suicidal acts: the suicide rate in patients with BD is 15 times higher than in the general population [2].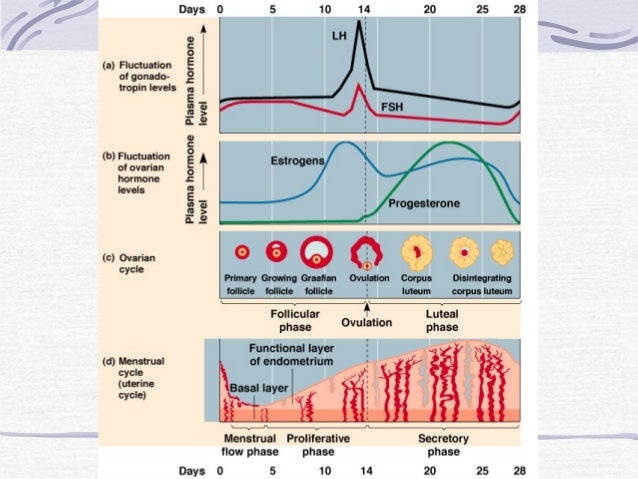 In addition, among the causes of death in patients with BD, cardiovascular, cerebrovascular diseases and malignant neoplasms are significantly more common [3].
In addition, among the causes of death in patients with BD, cardiovascular, cerebrovascular diseases and malignant neoplasms are significantly more common [3].
Patients with BD, due to the characteristics of the disease, have a negative impact on the psycho-emotional state of the immediate environment - family, work colleagues, neighbors. For this reason, among patients with BD, the percentage of unemployment is quite high, about half of them are childless [4, 5]. Dissatisfaction with the quality of life (while maintaining criticism of their condition) in these patients is observed much more often than among healthy people [6]. Direct and indirect financial losses associated with treatment, disability, social support and adaptation of patients are quite large: from this position, BD is recognized as the most expensive behavioral disorder in economic terms [7].
Etiology of BD
BD is a disease with a strong genetic predisposition. It has been shown that the risk of developing BD among the offspring of people suffering from this disease is 13%, the risk of developing unipolar depression is 15%, and the risk of schizoaffective disorders is 1% [8, 9]. According to studies conducted on identical twins, the role of the hereditary factor in the development of BD is 79%, the remaining 21% is the impact of environmental factors (stress, sexuality disorders, abuse of psychotropic drugs) [10].
According to studies conducted on identical twins, the role of the hereditary factor in the development of BD is 79%, the remaining 21% is the impact of environmental factors (stress, sexuality disorders, abuse of psychotropic drugs) [10].
Epidemiological studies have revealed the highest prevalence of BD in the age group from 18 to 24 years [11], and without gender differences [12]. The appearance of BD at a later age, as a rule, is a consequence of traumatic brain injury, stroke, etc. [4].
Classification of BD and clinical manifestations
The American Psychiatric Association 4th revision (DSM-IV) classification distinguishes [13]:
• Type I BD - the presence of at least one manic or mixed episode. Episodes of major depressive disorder are often observed, but they are not mandatory;
• BD type II - having at least one hypomanic and one depressive episode. There are no manic or mixed episodes;
• BR without further specification.
In the same classification, the following current episodes of BD are distinguished: episodes of mania, hypomania, major depressive disorders, mixed episodes, cyclothymia and rapid cycling.
A manic episode is characterized by an inappropriately elevated mood that can range from nonchalant gaiety to almost uncontrollable excitement. The elevation of mood is accompanied by increased energy, leading to hyperactivity, speech pressure, and reduced need for sleep. The patient becomes immune to social inhibition, does not hold attention, marked distractibility, increased self-esteem, over-optimistic ideas and ideas of greatness are easily expressed. Perceptual disturbances may occur. The patient may perform extravagant and impractical acts, spend money thoughtlessly, or be aggressive, amorous, hypersexual, playful in inappropriate circumstances. In some manic episodes, the patient's condition can be characterized as irritable and suspicious, rather than elated.
Mania with psychotic symptoms is experienced by 86% of patients with BD during their lifetime [4]. At the same time, increased self-esteem and ideas of superiority turn into delusional ideas of greatness, irritability and suspicion transform into delusions of persecution. In severe cases, there may be expansive-paraphrenic feelings of grandeur or delusional ideas about noble birth. As a result of the jump of thoughts and verbal pressure, the patient's speech often turns out to be incomprehensible to others.
In severe cases, there may be expansive-paraphrenic feelings of grandeur or delusional ideas about noble birth. As a result of the jump of thoughts and verbal pressure, the patient's speech often turns out to be incomprehensible to others.
Hypomania is a mild degree of mania that is not accompanied by psychotic symptoms (delusions or hallucinations). Patients have a constant slight rise in mood (at least for several days), increased energy and activity, a sense of well-being. Also, increased social activity, talkativeness, familiarity, hypersexuality, and reduced need for sleep are often noted. Women often put on excessive make-up on their faces, wear unusual and bright clothes. These symptoms do not lead to serious disturbances in work or social rejection of patients. Sometimes, instead of the usual cheerful mood, irritability, increased conceit and rude behavior can be observed.
According to DSM-IV [13], for the diagnosis of mania, it is necessary that its symptoms have been observed for at least 7 days, hypomania - for at least 4 days.
In the phase of depression, patients usually stay most of their lives. Thus, patients with type I BD are on average 32% of the time in a state of depression and 9% in a state of mania/hypomania. Patients with type II BD spend 50% of their time in the depressed phase and only 1% in a state of hypomania [14]. Depression is usually the first symptom of BD, especially in women. The risk of suicide in this phase is maximum. Criteria for depressive and manic episodes are given below.
Depressive episode. Five or more symptoms that persist for two weeks, at least one of the symptoms is either depressed mood or loss of interest in life:
emptiness, tearfulness). In children and adolescents, an irritable mood can be a symptom of depression.
2. Significantly reduced interest in life in everything (almost everything) that happens most of the day (according to one's own observations or according to the observations of others).
3. Significant loss in body weight, even if the patient is not on a diet (weight loss of more than 5% per month), or sharp fluctuations in appetite.
4. Insomnia or drowsiness.
5. Psychomotor agitation or lethargy.
6. Feeling tired.
7. Feelings of worthlessness or excessive guilt (may be delusional).
8. Decreased attention, inability to concentrate.
9. Persistent thoughts of death, suicidal thoughts in the absence of a special plan or suicide attempt, the presence of a suicide plan.
Episode of mania. Three or more symptoms (four if one of the symptoms is irritability):
1. Increased self-esteem, a sense of self-worth.
2. Reduced need for sleep.
3. Increased talkativeness, desire to strike up conversations.
4. "Flight of Thought".
5. Instability of attention.
6. Increased social, sexual activity, psychomotor excitability.
7. Involvement in risky transactions with securities, recklessly large expenses, etc.
Mixed manic-depressive episodes are conditions that meet the criteria for both mania and depression and have been symptomatic for more than 7 days.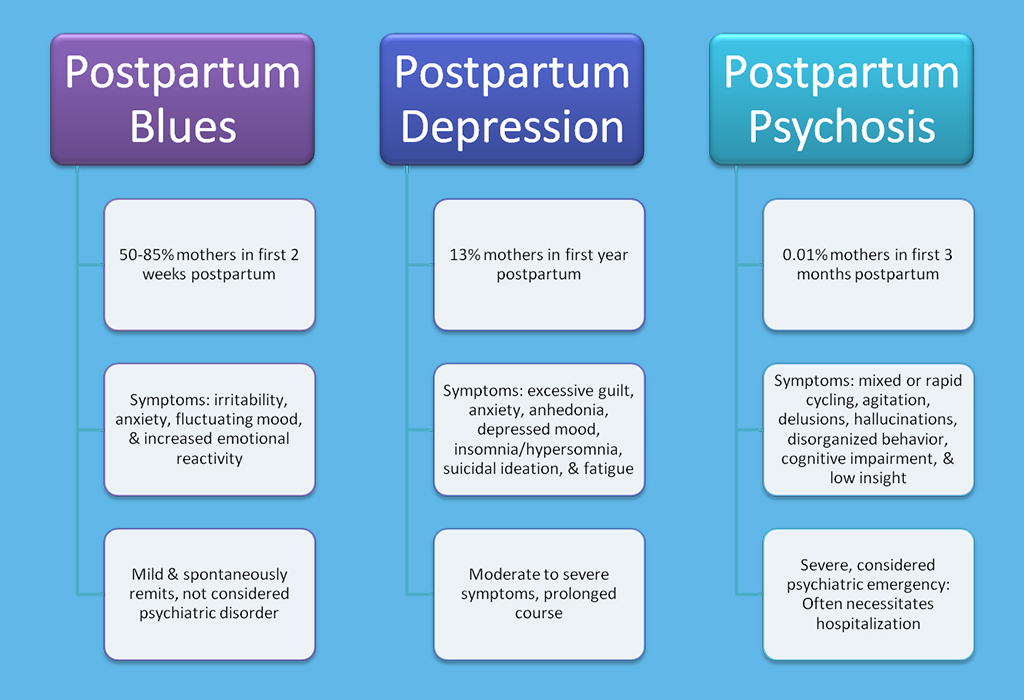 Mixed episodes can occur at any stage of the disease, and their appearance is considered a predictor of poor patient prognosis [1].
Mixed episodes can occur at any stage of the disease, and their appearance is considered a predictor of poor patient prognosis [1].
Cyclothymia is characterized by the presence of prolonged subdepressive and hypomanic symptoms [1, 13]. Severe depressive disorders or mania are absent. Cyclothymia is diagnosed if, for at least 2 years, the patient has experienced frequent bouts of depressed mood, alternating with bouts that meet the criteria for hypomania. Subsequently, cyclothymia can transform into a typical BD.
The criterion for rapid cycling is the presence of at least 4 episodes of BD per year with partial or complete remission between them or a direct switch from one polarity to another (from mania to depression or vice versa). Rapid cycling is typical for approximately 10-15% of patients. Rapid cycling is more common in the later stages and is usually recorded in women with type II BD [15]. Rapid cycling can be induced by hypothyroidism, alcohol, skull trauma, and multiple sclerosis [16].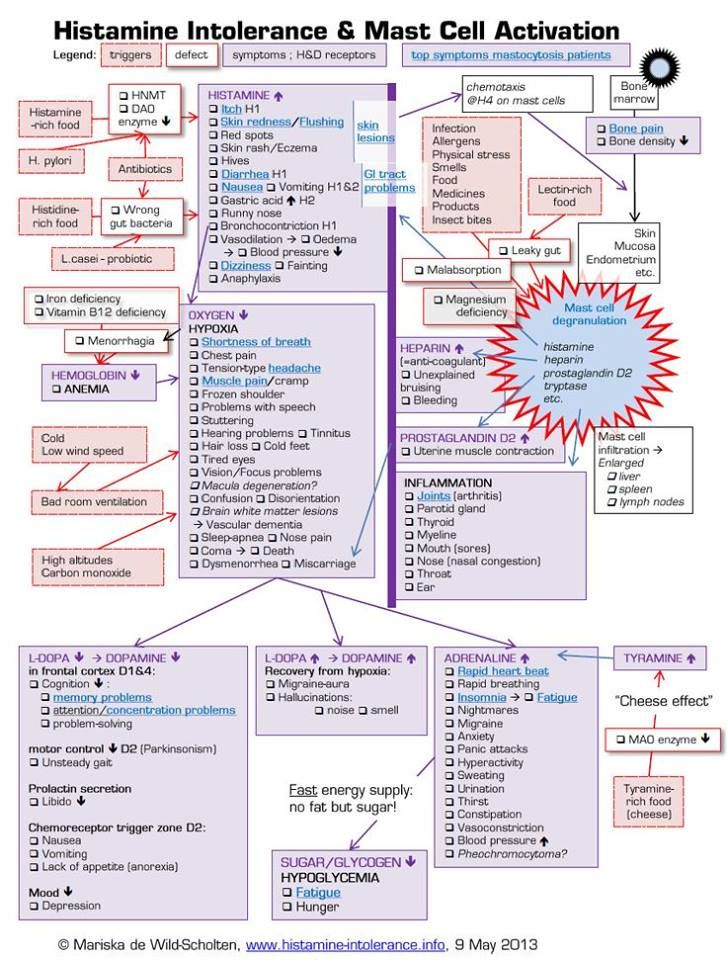
Features of BD in children and adolescents
The most common manifestation of mania in children is hyperactivity [17]. Other symptoms include ostentatious irritability and outbursts of anger [18]. BD in children often has to be differentiated from attention deficit hyperactivity disorder and schizophrenia [19].
Symptoms of mania in adolescents are similar to those in children. Difficulties are presented by differential diagnosis from schizophrenia. Normal adventurous-bravado behavior in adolescence must be distinguished from the inherently reckless, reckless behavior of mania.
Features of BD in pregnancy and lactation
Under ideal circumstances, the possibility of pregnancy should be discussed jointly by the obstetrician-gynecologist, psychiatrist and the patient's family doctor. If it is possible to stop taking psychotropic drugs for the period of pregnancy (in order to avoid teratogenies), their cancellation should occur gradually, otherwise a rapid relapse of BD may be provoked [20].
Recurrent BD during pregnancy requires aggressive treatment with mood stabilizers in a hospital setting. If it is necessary to prescribe lithium salts, the risk of cardiovascular malformations in the fetus should be assessed. Breastfeeding is stopped during treatment with lithium preparations, since lithium enters the mother's milk [21].
In the postpartum period, a relapse of BD is often observed, moreover, in a severe form, including in the form of rapid cycling, resistant to drug therapy [22].
Drug therapy BR
The specifics of the use of essential drugs are summarized in Table 1. It should be noted that in the published regimens of different countries there is no complete agreement in terms of the choice of first-line mood stabilizer: in North American recommendations, valproate is given priority, while in European guidelines more often are recommended lithium salts [23].
Lithium preparations
Lithium salts as normotimics have been in the lead for quite a long time: their psychotropic properties have been known to medicine since the beginning of the 19th century. For a long time, there were no clinical studies confirming their effectiveness, but this did not prevent the successful use of these drugs for the treatment of BD. Subsequently, complications after taking lithium salts were widely publicized, primarily a decrease in renal function, hypothyroidism and gastrointestinal disorders, which seriously limit their use.
For a long time, there were no clinical studies confirming their effectiveness, but this did not prevent the successful use of these drugs for the treatment of BD. Subsequently, complications after taking lithium salts were widely publicized, primarily a decrease in renal function, hypothyroidism and gastrointestinal disorders, which seriously limit their use.
Lithium salts are ineffective in mixed bipolar episodes, rapid cycling, and the presence of some comorbid disorders. In the acute phase of depression, the action of lithium preparations develops very slowly (from one to two months).
Valproate
In connection with the above disadvantages of lithium, in a number of modern guidelines preference among mood stabilizers is given to valproate. Valproate, in addition to stabilizing mood, has moderate antidepressant properties [25], has a more favorable side effect profile compared to lithium salts, and is better tolerated by patients [16].
Carbamazepine (Finlepsin)
Despite a significant amount of literature pointing to the methodological flaws of studies of the effectiveness of carbamazepine in BD [26], the drug is still widely used in the treatment of this disease as a mood stabilizer. It is considered that carbamazepine should be included in the current therapy in the presence of a patient with BD mixed episodes (i.e., simultaneously meeting the criteria for mania and depression), as well as in BD with rapid cycling.
It is considered that carbamazepine should be included in the current therapy in the presence of a patient with BD mixed episodes (i.e., simultaneously meeting the criteria for mania and depression), as well as in BD with rapid cycling.
Carbamazepine serves as an alternative to lithium preparations in case of impaired renal function, which is especially important due to the prevalence of somatic pathology that depresses renal function (diabetes mellitus, arterial hypertension, nephritis of infectious origin, etc.). In Russia, carbamazepine is traditionally used as an effective treatment for alcohol withdrawal syndrome, which is also used in patients with BD. Recently, a randomized, double-blind study demonstrated the efficacy of a prolonged dosage form of carbamazepine in acute mania [27].
Dosing features and the most common side effects when taking mood stabilizers are presented in Table 2.
Antidepressants
Modern guidelines for the treatment of BD recommend avoiding antidepressant monotherapy and, if necessary, prescribing them in combination with mood stabilizers [28].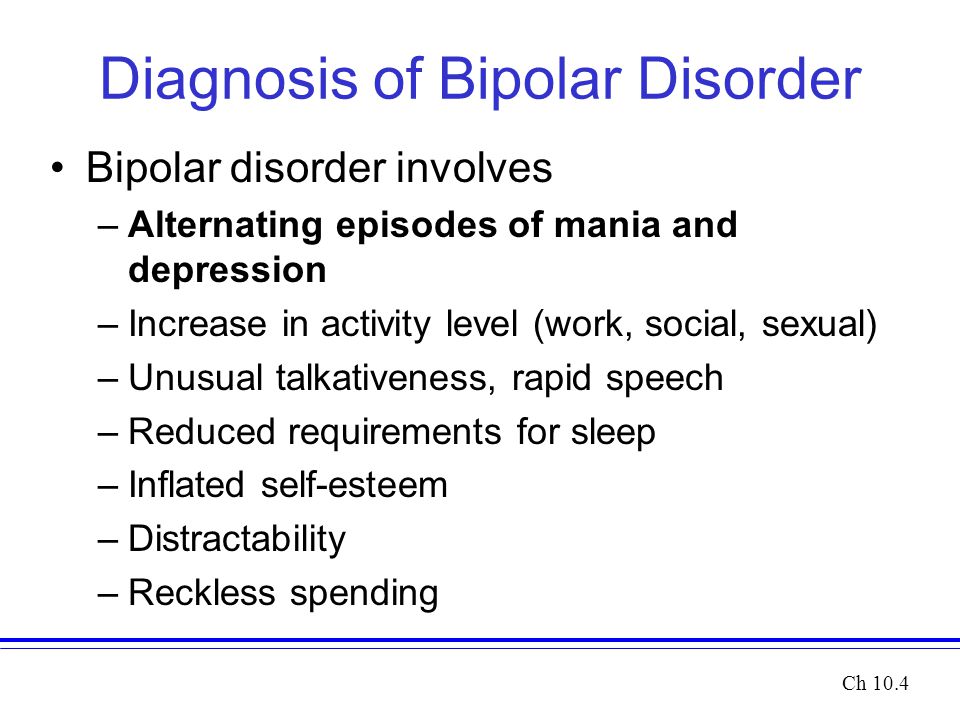 Taking antidepressants is associated with the risk of reversing the polarity towards mania, while their withdrawal may contribute to the relapse of depression.
Taking antidepressants is associated with the risk of reversing the polarity towards mania, while their withdrawal may contribute to the relapse of depression.
Antipsychotics
Typical antipsychotics (haloperidol, chlorpromazine) are significantly less effective than mood stabilizers [29]. Among atypical antipsychotics, the use of olanzapine, risperidone, ziprasidone, aripiprazole, and quetiapine is the most justified [16].
Conclusion
Despite the large number of psychotropic drugs on the market, theoretically able to have a beneficial effect on patients with BD, mood stabilizers (normothymics) retain leading positions in the treatment of this disease. With the right choice of therapy, the quality of life of both the patient and his environment improves significantly, which increases the level of mental health of modern society as a whole.
Literature
1. Ushkalova A.V. Bipolar disorders: classification, epidemiology, diagnosis and treatment // Farmateka. 2007; 7:142:18-27.
2007; 7:142:18-27.
2. Access Economics and SANE Australia. Bipolar disorder: costs. An analysis of the burden of bipolar disorder and related suicide in Australia. Melbourne: SANE Australia, 2003.
3. Angst J., Sellaro R. Historical perspectives and natural history of bipolar disorder // Biol Psychiatry. 2000; 48:6:445-57.
4. Mitchell P.B., Ball J.R., Best J.A. et al. The management of bipolar disorder in general practice. MJA 2006; 184(11): 566-70.
5. Manning J.S., Haykal R.F., Connor P.D. et al. On the nature of depressive and anxious states in a family practice setting: the high prevalence of bipolar II and related disorders in a cohort followed longitudinally // Compr Psychiatry. 1997; 38:2:102-08.
6. Michalak E.E., Yatham L.N., Lam R.W. Quality of life in bipolar disorder: a review of the literature // Health Qual Life Outcomes. 2005; 3: 72.
7. Peele P.B., Xu Y., Kupfer D.J. Insurance expenditures on bipolar disorder: clinical and parity implications // Am J Psychiatry. 2003: Jul; 160:7:1286-90.
2003: Jul; 160:7:1286-90.
8. Werder S.F. An update on the diagnosis and treatment of mania in bipolar disorder // Am Fam Physician 1995; 51:1126-36.
9. Gershon E.S., Hamovit J., Guroff J.J. et al. A family study of schizoaffective, bipolar I, bipolar II, unipolar, and normal control probands // Arch Gen Psychiatry. 1982; 39:1157-67.
10. Kendler K.S., Pedersen N.L., Neal N.K. et al. A pilot Swedish twin study of affective illnesse including hospital- and population – ascertained subsamples: results of model fitting // Behav Genet. 1995; 25:217-32.
11. Robins L.N., Regier D.A. Psychiatric disorders in America: the epidemiologic catchment area study. New York, N.Y.: Free Press, 1991.
12. Keller M.B., Baker L.A. Bipolar disorder: epidemiology, course, diagnosis, and treatment // Bull Menninger Clin. 1991; 55:172-81.
13. Diagnostic and Statistical Manual of Mental Disorders. American Psychiatric Association. 4th ed. Washington, DC: American Psychiatric Assoc 1994: 327.
14. Judd L.L., Akiskal H.S., Schettler P.J. et al. The long-term natural history of the weekly symptomatic status of bipolar I disorder // Arch Gen Psychiatry. 2002; 59: 530-37.
15. Calabrese J.R., Shelton M.D., Rapport D.J. et al. Current research on rapid cycling bipolar disorder and its treatment // J Affect Disord. 2001; 67:1-3:241-55.
16. Vieta E. Managing Bipolar Disorder in Clinical Practice. Published by Current medicine group Ltd, Porters South, London, UK, 2006.
17. Faedda G.L., Baldessarini R.J., Suppes T. et al. Pediatric-onset bipolar disorder: a neglected clinical and public health problem // Harv Rev Psychiatry. 1995; 3:171-95.
18. Hechtman L., Greenfield B. Juvenile onset bipolar disorder // Curr Opin Pediatr. 1997; 9:346-53.
19. Weller E.B., Weller R.A., Fristad M.A. Bipolar disorder in children: misdiagnosis, underdiagnosis, and future directions // J Am Acad Child Adolesc Psychiatry. 1995; 34:709-14.
20. Altshuler L.L., Cohen L.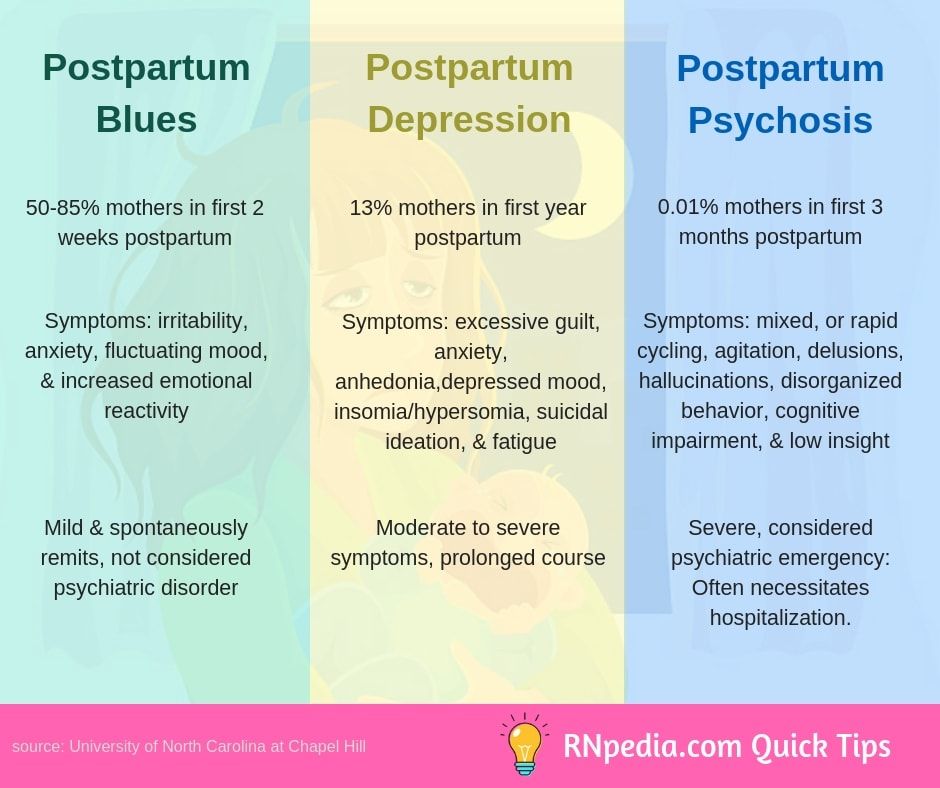 , Szuba M.P. et al. Pharmacologic management of psychiatric illness during pregnancy: dilemmas and guidelines // Am J Psychiatry. 1996; 153:592-606.
, Szuba M.P. et al. Pharmacologic management of psychiatric illness during pregnancy: dilemmas and guidelines // Am J Psychiatry. 1996; 153:592-606.
21. Packer S. Family planning for women with bipolar disorder // Hosp Community Psychiatry. 1992; 43:479-82.
22. Altshuler L.L., Hendrick V., Cohen L.S. Course of mood and anxiety disorders during pregnancy and the postpartum period // J Clin Psychiatry. 1998; 59: Suppl 2: 29-33.
23. Vestergaard P. Guidelines for maintenance treatment of bipolar disorder: are there discrepancies between European and North American recommendations? // Bipolar Discord. 2004; 6:519-22.
24. Treatment of bipolar disorder. The Expert Consensus Guideline Series // J Clin Psychiatry. 1996; 57: Suppl 12A: 3-88.
25. Malhi G.S., Mitchell P.B., Salim S. Bipolar depression: management options // CNS Drugs. 2003; 17:1:9-25.
26. Bowden C.L. New concepts in mood stabilization: evidence for the effectiveness of valproate and lamotrigine // Neuropsychopharmacology.