Therapy self harm
Self-injury/cutting - Diagnosis and treatment
Diagnosis
Although some people may ask for help, sometimes family or friends discover the self-injury. Or a health care provider doing a routine medical exam may notice signs, such as scars or fresh injuries.
There's no specific test to diagnose self-injury. Diagnosis is based on a physical and psychological evaluation. You may be referred to a mental health professional with experience in treating self-injury for evaluation. This professional talks to you about your life, thoughts, feelings and behaviors.
A mental health professional also may evaluate you for other mental health conditions that could be linked to self-injury, such as depression or personality disorders.
Treatment
The first step is to tell someone about your self-injuring behavior so you can get help. Treatment is based on your specific issues and any related mental health conditions you might have, such as depression. Because self-injury can become a major part of your life, it's best to get treatment from a mental health professional who is experienced in treating self-injury.
If the self-injury behavior is linked with a mental health condition, such as depression or borderline personality disorder, the treatment plan focuses on that condition, as well as the self-injury behavior.
Treating self-injury behavior can take time, hard work and your own desire to recover.
Here's more information about treatment options.
Psychotherapy
Known as talk therapy or psychological counseling, psychotherapy can help you:
- Identify and manage underlying issues that trigger self-injury.
- Learn skills to better manage distress.
- Learn better ways to manage intense emotions.
- Learn how to boost your self-image.
- Develop skills to improve your relationships and social skills.
- Develop healthy problem-solving skills.
Several types of individual psychotherapy may be helpful, such as:
- Cognitive behavioral therapy (CBT), which helps you identify unhealthy, negative beliefs and behaviors and replace them with more effective ones.
 You can also gain skills that help you cope in different situations when needed.
You can also gain skills that help you cope in different situations when needed. - Dialectical behavior therapy, a type of CBT that teaches behavioral skills to help you handle distress, manage or regulate your emotions, and improve your relationships with others.
- Mindfulness-based therapies, which help you live in the present and cope with difficult emotions and negative thoughts. These can help reduce anxiety and depression and improve your general well-being.
In addition to individual therapy sessions, your provider may recommend family therapy or group therapy.
Medicines
There are no medicines to specifically treat self-injuring behavior. However, if you're diagnosed with a mental health condition, such as depression or an anxiety disorder, your health care provider may recommend antidepressants or other medicines to treat the underlying condition that's linked with self-injury. Treatment for these conditions may help reduce the urge to hurt yourself.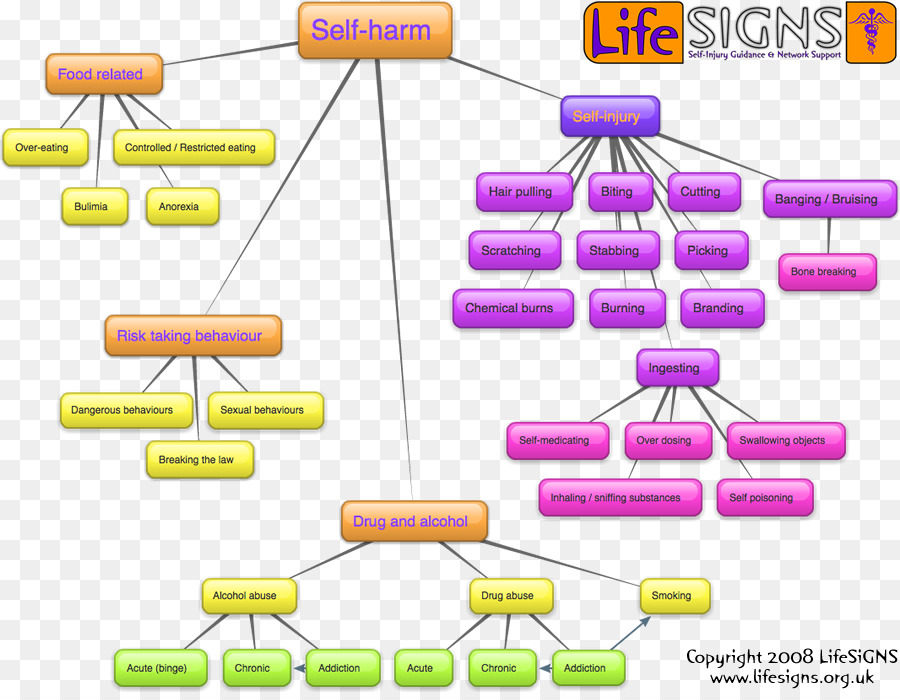
Inpatient care
If you injure yourself severely or repeatedly, your health care provider may recommend that you be admitted to a hospital for psychiatric care. Being cared for in a hospital, often short term, can provide a safe environment and more-intensive treatment until you get through a crisis. Mental health day-treatment programs that focus on learning behavioral coping skills to manage distress also may be an option.
More Information
- Cognitive behavioral therapy
- Psychotherapy
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
In addition to professional treatment, here are some important self-care tips:
- Follow your treatment plan. Keep therapy appointments. Practice and use coping skills learned in therapy. Take any prescribed medicine as directed.

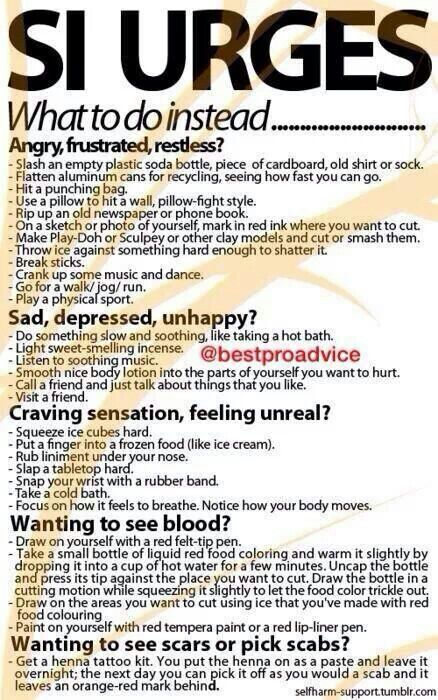
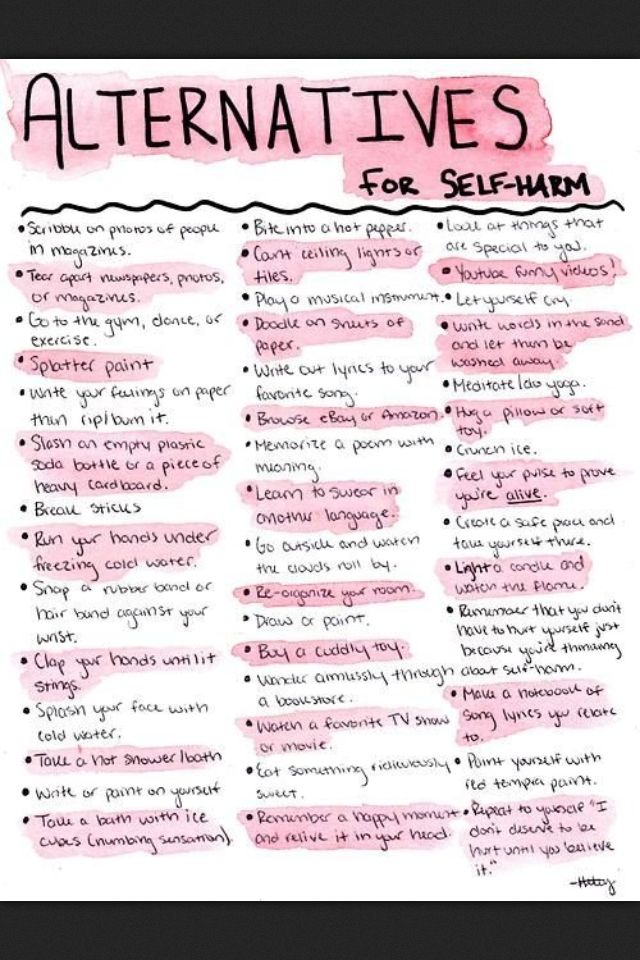
- Recognize the situations or feelings that might trigger your desire to self-injure. Make a plan for other ways to soothe or distract yourself or to get support, so you're ready the next time you feel the urge to self-injure.
- Ask for help. Keep your mental health provider's phone number handy. Tell your provider about all incidents related to self-injury. Choose a trusted family member or friend as the person you'll immediately contact if you have an urge to self-injure or if self-injury happens.
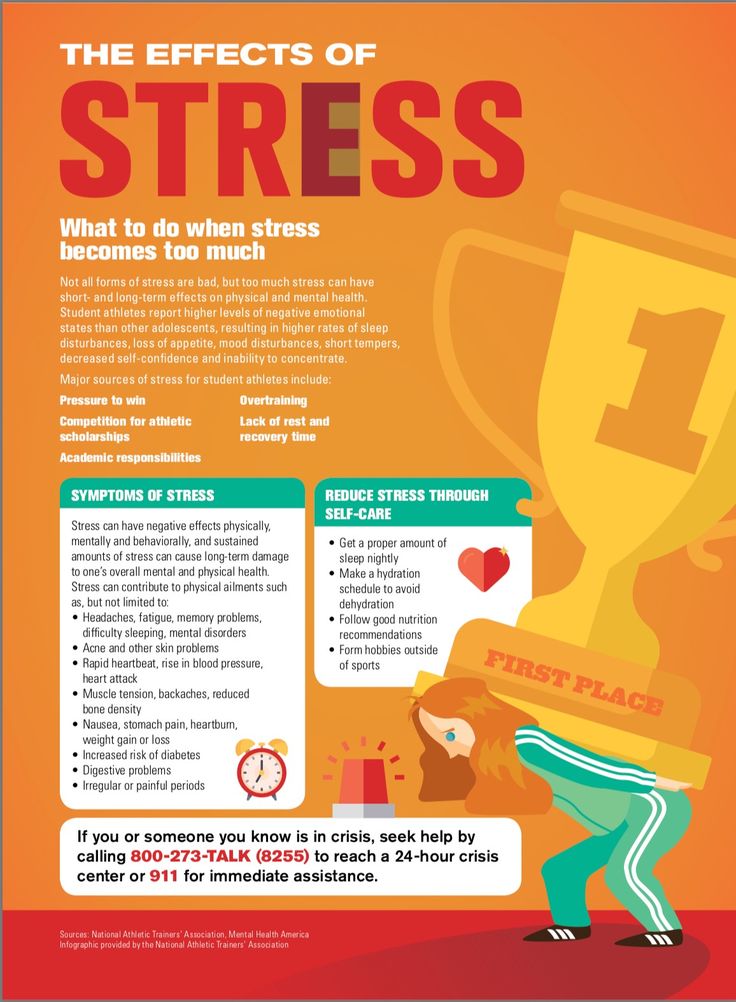
- Take care of yourself. Learn how to include physical activity and relaxation exercises as a regular part of your daily routine. Eat healthy. Ask your health care provider for advice if you have sleep problems, which can have a big impact on behavior.
- Avoid alcohol and recreational drugs. They affect your ability to make good decisions and can put you at risk of self-injury.
- Take care of your wounds if you injure yourself or seek medical treatment if needed.
 Call a trusted family member or friend for help and support. Don't share items used for self-injury. That raises the risk of infectious diseases.
Call a trusted family member or friend for help and support. Don't share items used for self-injury. That raises the risk of infectious diseases.
Coping and support
If you or a friend or family member needs help in coping, consider the tips below. If there's a focus on thoughts of suicide, take action and get help right away.
Coping tips if you self-injure include:
- Connect with others who can support you so that you don't feel alone. For example, reach out to a trusted family member or friend, contact a support group, or contact your health care provider or mental health provider.
- Avoid websites that support or glamorize self-injury. Instead, seek out sites that support your recovery efforts.
- Learn to express your emotions in positive ways. For example, to help balance your emotions and improve your sense of well-being, become more physically active or practice relaxation techniques.
 Or participate in activities that you find personally meaningful, such as dance, art or music.
Or participate in activities that you find personally meaningful, such as dance, art or music.
Coping tips if a friend or loved one self-injures include:
- Get information. Learn more about self-injury to help you understand why it occurs and how you might help stop this harmful behavior. Know the strategies and relapse prevention plan your friend or loved one has developed with the therapist so you can encourage it.
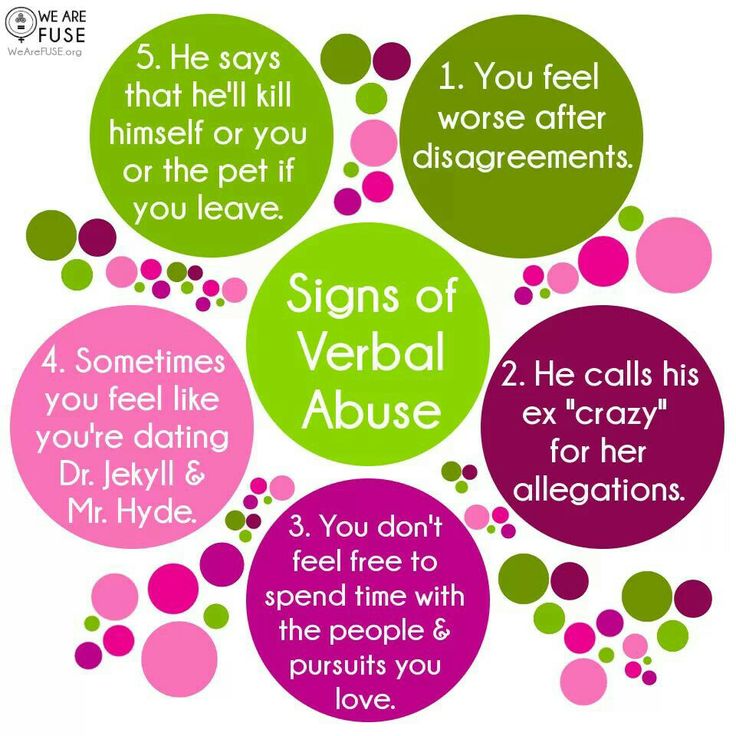
- Try not to judge or criticize. Criticism, yelling, threats or accusations may increase the risk of self-injuring behavior. Offer support, praise efforts to express emotions in healthy ways and try to spend positive time together.
- Let your loved one know you care no matter what. Remind the person that they're not alone and that you're available to talk. Recognize that you may not change the behavior, but you can help the person find resources, identify coping strategies and offer support during treatment.

- Support the treatment plan. Encourage your loved one to take prescribed medicine, if that's part of the plan. Stress the importance of keeping therapy appointments and practicing the skills learned.
- Make a safe home environment. Remove or limit access to matches, knives, razor blades or other items that may be used for self-injury.
- Share coping strategy ideas. Your loved one may benefit from hearing strategies you use when feeling distressed. You also can serve as a role model by using healthy coping strategies.
- Find support. Consider talking to people who've gone through what you're going through. Share your own experiences with trusted family members or friends. Ask the health care provider or mental health provider if there are local support groups for parents, family members or friends of people who self-injure. Or talk to a counselor or therapist.
- Take care of yourself.
 Take some time to do things that you enjoy. And get enough rest and physical activity.
Take some time to do things that you enjoy. And get enough rest and physical activity.
Preparing for your appointment
Your first appointment may be with your primary care provider, a school nurse or a counselor. But because self-injury often requires specialized mental health care, you may be referred to a mental health professional for more evaluation and treatment.
Be ready to provide accurate, thorough and honest information about your situation and your self-injuring behavior. You may want to take a trusted family member or friend along, if possible, for support and to help you remember information.
What you can do
To help prepare for your appointment, make a list of:
- Symptoms you've had, including triggers for self-injury, how long you've been self-injuring, if you use any objects, and where on your body you usually self-injure.
- Key personal information, including any major stresses or recent life changes.

- All medicines, vitamins, herbs or other supplements that you're taking, including the doses.
- Questions to ask your mental health provider.
Questions to ask may include:
- What treatments are available? Which do you recommend for me?
- What side effects are possible with that treatment?
- What are other options to the approach that you're suggesting?
- Are there medicines that might help? Is there a generic version of the medicine you're prescribing?
- What should I do if I have an urge to self-injure between therapy sessions?
- What else can I do to help myself?
- How can I — or those around me — recognize that things may be getting worse?
- Can you suggest resources that would help me learn more about my condition and its treatment?
Don't hesitate to ask other questions during your appointment.
What to expect from your doctor
Your mental health provider is likely to ask you a number of questions, such as:
- When did you first begin harming yourself?
- What methods do you use to harm yourself?
- How often do you cut or injure yourself?
- Where on your body do you self-injure?
- What feelings and thoughts do you have before, during and after self-injury?
- What seems to trigger your self-injury?
- What makes you feel better? What makes you feel worse?
- Do you have a supportive social circle or relationships?
- What emotional issues are you facing?
- How do you feel about your future?
- Have you had previous treatment for self-injury?
- Do you have suicidal thoughts when you're feeling down?
- Do you drink alcohol or use tobacco or recreational drugs?
Your mental health provider may ask more questions based on your responses, symptoms and needs. Preparing for questions will help you make the most of your time with the provider.
Preparing for questions will help you make the most of your time with the provider.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Treatment for Self-Harm - Discovery Mood & Anxiety Program
Unlike most other mental health disorders, there is no defined treatment for self-harm that has been studied extensively with proven clinical results. Treatment is aimed at recognizing and treating the underlying cause such as low-self esteem, impulsivity, depression, family dysfunction and conflict, poverty or abuse. An individual will often enter therapy with complaints not associated with self-harm. These may include difficulty sleeping or feeling depressed. The self-harm injuries are often noticed or asked about by the therapist during the session and skills are learned over the course of time to prevent this self-harm behavior. Learning healthy coping skills and maintaining emotional equilibrium to help manage the feelings of anger, grief and loneliness can help prevent an individual from cutting in response to these negative emotions. The goals of treatment for individuals who practice self-harm behavior are as follows:
The goals of treatment for individuals who practice self-harm behavior are as follows:
- Identify and manage underlying issues that trigger cutting
- Learn skills to better manage distress
- Learn how to regulate and cope with unhealthy emotions
- Learn how to improve self-image and self-esteem
- Develop skills to improve relationships and social skills
- Develop healthy problem-solving skills
The following are other forms of therapy and coping mechanisms used to address underlying feelings resulting in self-harm behavior.
- Psychodynamic psychotherapy
- Mindfulness-based therapies
- Family therapy
- Exercising
- Expressing feelings through art or music
- Taking a hot bath or shower
- Hypnosis
- Meditation
- Group Therapy
Cognitive-behavioral therapy (CBT) for self-harm behavior
Cognitive-behavioral therapy (CBT) has shown to have the most successful and promising results for treating nonsuicidal self-injury disorder (NSSID). Cognitive-behavioral therapy (CBT) helps the individual identify unhealthy and distorted thoughts and replaces these thoughts and teaches them skills to induce healthy and positive thoughts and behaviors. Dialectal behavioral therapy (DBT) is a specific type of cognitive-behavioral therapy that can take place in either a group or individual setting to provide opportunities to improve certain existing skills. The four basic skill sets that are taught through this approach are emotion regulation, mindfulness, interpersonal effectiveness and distress tolerance. These learned skills should be practiced in all settings including therapy sessions, at home, at work and in social settings in order for the individual to become adaptable to certain stressors. This type of therapy focuses on negative emotions and thoughts and attempts to conform these thoughts into positive behaviors by teaching individuals to become desensitized to their stressors and experience and evaluate their current situation in the moment through an objective perspective.
Cognitive-behavioral therapy (CBT) helps the individual identify unhealthy and distorted thoughts and replaces these thoughts and teaches them skills to induce healthy and positive thoughts and behaviors. Dialectal behavioral therapy (DBT) is a specific type of cognitive-behavioral therapy that can take place in either a group or individual setting to provide opportunities to improve certain existing skills. The four basic skill sets that are taught through this approach are emotion regulation, mindfulness, interpersonal effectiveness and distress tolerance. These learned skills should be practiced in all settings including therapy sessions, at home, at work and in social settings in order for the individual to become adaptable to certain stressors. This type of therapy focuses on negative emotions and thoughts and attempts to conform these thoughts into positive behaviors by teaching individuals to become desensitized to their stressors and experience and evaluate their current situation in the moment through an objective perspective. Channeling feeling of guilt, anger, shame and frustration into constructive activities such as art or exercise can prevent the individual from inducing self-harm. The first step to this approach is having the individual recognize their negative feelings and destructive behavior.
Channeling feeling of guilt, anger, shame and frustration into constructive activities such as art or exercise can prevent the individual from inducing self-harm. The first step to this approach is having the individual recognize their negative feelings and destructive behavior.
Treatment for self-harm with pharmacotherapy
Medications are not used to treat self-harm behavior however if there is an underlying or co-occurring disorder such as depression or anxiety, medications can be prescribed to treat those specific disorders. Oftentimes, individuals will be diagnosed with substance abuse, as it is common for individuals to use drugs and/or alcohol to cover up their negative emotions. Depending on the specific substance of abuse, medications can be used to help prevent or lesson the withdrawal symptoms. Co-occurring disorders such as substance abuse or depression should be treated in order for the self-harm behavior to improve.
Therapist
Therapist - multidisciplinary specialist
Therapist is one of the most sought after specialists in the field of medicine. The high demand for the services of this doctor is determined by the fact that the profile of his work is quite wide. The therapist practices the diagnosis and treatment of a whole range of diseases of internal organs.
The high demand for the services of this doctor is determined by the fact that the profile of his work is quite wide. The therapist practices the diagnosis and treatment of a whole range of diseases of internal organs.
What a therapist treats
A therapist specializes in the treatment of an established set of diseases. These primarily include colds and respiratory viral infections (flu, acute respiratory infections, runny nose, other diseases). Also therapist diagnoses vascular and cardiac diseases (VSD, arterial hypertension, ischemia, hypertension), some blood diseases (anemia), general disorders (metabolic disorders, diathesis). In addition, the therapist provides assistance in violation of the functioning of the gastrointestinal tract, respiratory system, intoxication syndrome.
Additional functions of a therapist
The therapist not only treats diseases that relate to his direct specialization, but also performs important general clinical tasks.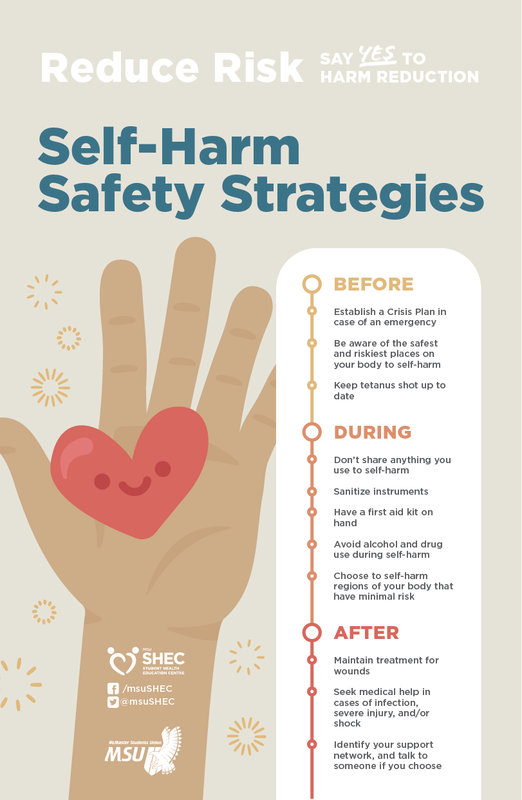 First, it is an informative function. Often a person, feeling unwell, cannot determine the cause of the ailment himself if it is not obvious, as, for example, in case of injury. This requires a professional examination and a qualitative examination. In this case, the therapist prescribes a diagnosis, and also advises the patient on the possible causes of the disease, the proposed ways to eliminate it. Consultations of the therapist are of great psychological importance for the patient, as they allow him to learn more about his illness and the means to overcome it.
First, it is an informative function. Often a person, feeling unwell, cannot determine the cause of the ailment himself if it is not obvious, as, for example, in case of injury. This requires a professional examination and a qualitative examination. In this case, the therapist prescribes a diagnosis, and also advises the patient on the possible causes of the disease, the proposed ways to eliminate it. Consultations of the therapist are of great psychological importance for the patient, as they allow him to learn more about his illness and the means to overcome it.
Secondly, the therapist performs a distributive function. After listening to the patient's complaints, analyzing the symptoms, the therapist refers the patient to one or another specialized specialist (ENT doctor, neuropathologist, endocrinologist, cardiologist, etc.). With an unclear genesis of the disease, it may be recommended to take several specialists. Thirdly, the therapist monitors the condition of patients with chronic diseases, taking the necessary therapeutic measures to improve the patient's well-being.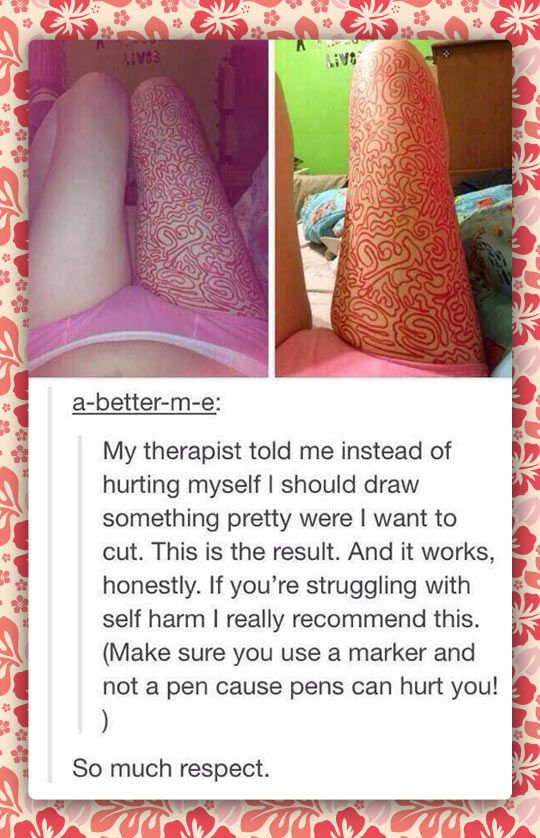 The correct treatment, as well as a quick recovery, often depend on the qualifications and experience of the therapist.
The correct treatment, as well as a quick recovery, often depend on the qualifications and experience of the therapist.
Medicines in therapy
The general practitioner has a wide range of medicines for the treatment of specialized diseases. These are almost all methods available to modern medicine, with the exception of surgical intervention. The methods of treatment used by the therapist can be divided into two groups: 1) medication, 2) physiotherapy. Drug methods are associated with the use of drugs and highly active chemical compounds (chemotherapy). Physiotherapeutic technologies include a number of procedures performed with the help of various physical influences.
Physiotherapy applied by a therapist can include both simple routine procedures (for example, inhalations) and complex techniques that require the use of high-tech equipment (electrophoresis, magnetic, laser, vibration, vacuum therapy). Often, the therapist prescribes medication and physiotherapy in combination to increase the effectiveness of treatment. A separate point of the means used by the therapist is prophylactic. Among them are the use of vitamins, biologically active substances, diets, body cleansing, health improvement in sanatoriums, and a change in climatic living conditions.
A separate point of the means used by the therapist is prophylactic. Among them are the use of vitamins, biologically active substances, diets, body cleansing, health improvement in sanatoriums, and a change in climatic living conditions.
Documentation with a therapist
An important responsibility of the therapist is to complete the proper medical documents relating to the patient's health. These include sick leave certificates, certificates for visiting the pool, certificates for obtaining a voucher for sanatorium treatment, sanatorium cards. When filling out these documents, the therapist requires awareness, knowledge of the rules for registration, accuracy, efficiency.
Therapy » Russian Scientific Medical Society of Therapists
- Therapy
- On journal
- Contacts
- Editions
Therapy Journal - Official Edition of the Russian Scientific Medical Company of therapists (RNEPHORI).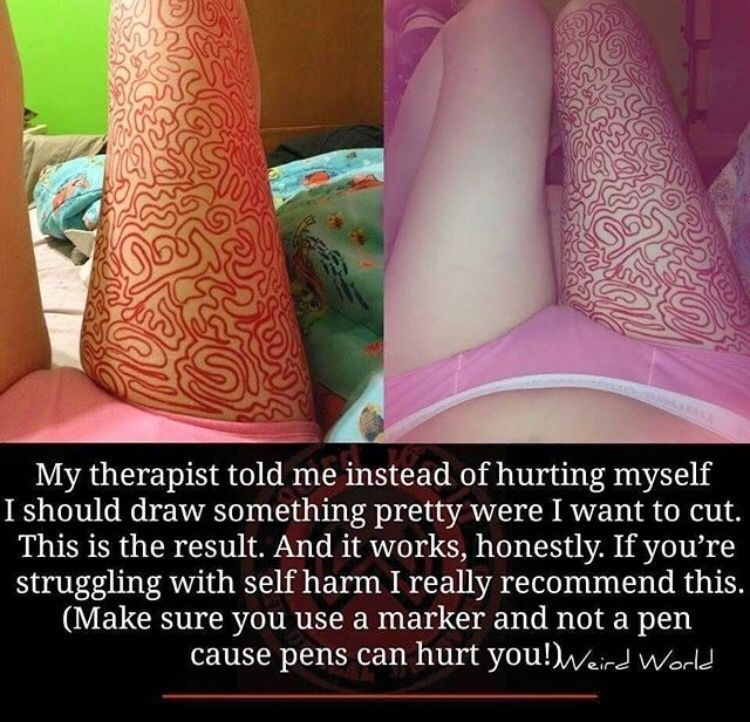
Scientific and practical peer-reviewed journal, included in the list of publications recommended by the Higher Attestation Commission (HAC).
Chief editor - A.I. MARTYNOV, Academician of the Russian Academy of Sciences, Doctor of Medical Sciences, Professor, president of RNMOT.
Deputy Chief Editor - A.G. MALYAVIN, Doctor of Medical Sciences, Professor, Secretary General of the Russian National Medical University
The Therapy Journal aims to promote the most complete and comprehensive development of domestic healthcare, medical science and education, professional growth of medical workers leading research, teaching and practical work in the field of therapy and related disciplines. The journal publishes original articles, literature reviews, lectures, clinical reviews, reviews of newly published specialized literature. Priority in publications - to the full members of the RNMOT.
Publication frequency – 10 issues per year + 2 supplements “Algorithms for diagnosis and treatment”
Circulation – 15,000 copies.
Journal website www.therapy-journal.ru
Target audience: outpatient and inpatient therapists, general practitioners, narrow specialists. Each issue of the journal has a specific thematic focus, covering individual therapeutic specializations.
EDITORIAL BOARD
ALLERGOLOGY, IMMUNOLOGY
Bolieva L.Z. (Vladikavkaz), MD, prof.
Ilyina N.I. (Moscow), MD, prof.
GASTROENTEROLOGY
Lazebnik L.B. (Moscow), MD, prof.
Maev I.V. (Moscow), Doctor of Medical Sciences, Prof., Academician of the Russian Academy of Sciences
Nikonov E.L. (Moscow), MD, prof.
Tarasova L.V. (Surgut), MD, prof.
INTENSIVE CARE, ANESTHESIOLOGY AND REANIMATION
Akselrod B.A. (Moscow), MD, prof.
Petrikov S.S. (Moscow), Doctor of Medical Sciences, Prof., Corresponding Member. RAS
INFECTIOUS DISEASES, EPIDEMIOLOGY
Maleev V.V. (Moscow), Doctor of Medical Sciences, Prof., Academician of the Russian Academy of Sciences
Malinnikova E.Yu. (Moscow), MD, prof.
Nikiforov V.V. (Moscow), MD, prof.
Ploskireva A.A. (Moscow), MD, prof.
CARDIOLOGY
Adasheva T.V. (Moscow), MD, prof.
Arutyunov G.P. (Moscow), Doctor of Medical Sciences, Prof., Corresponding Member. RAS
Boeva OI (Stavropol), Doctor of Medical Sciences, Professor
Kobalava Zh.D. (Moscow), Doctor of Medical Sciences, Prof., Corresponding Member. RAS
V.A. Kokorin (Moscow), MD, prof.
Paleev F.N. (Moscow), Doctor of Medical Sciences, Prof., Corresponding Member. RAS
Shevchenko A. O. (Moscow), Doctor of Medical Sciences, Prof., Corresponding Member. RAS
O. (Moscow), Doctor of Medical Sciences, Prof., Corresponding Member. RAS
Yakushin S.S. (Ryazan), MD, prof.
CLINICAL PHARMACOLOGY
Vertkin A.L. (Moscow), MD, prof.
Sychev D.A. (Moscow), Doctor of Medical Sciences, Prof., Corresponding Member. RAS
MEDICAL REHABILITATION
Razumov A.N. (Moscow), MD, Prof., Academician of RAS
Rassulova M.A. (Moscow), MD, prof.
NEUROLOGY
Martynov M.Yu. (Moscow), Doctor of Medical Sciences, Prof., Corresponding Member of the Russian Academy of Sciences
Piradov M.A. (Moscow), Doctor of Medical Sciences, Prof., Academician of the Russian Academy of Sciences
Shmyrev V.I. (Moscow), MD, prof.
NEPHROLOGY
Batyushin M.M. (Rostov-on-Don), MD, prof.
Sigitova O.N. (Kazan), MD, prof.
Terentiev V.P. (Rostov-on-Don), MD, prof.
Shilov E.M. (Moscow), MD, prof.
GENERAL PATHOLOGY, PATHOMORPHOLOGY
Zayratyants O.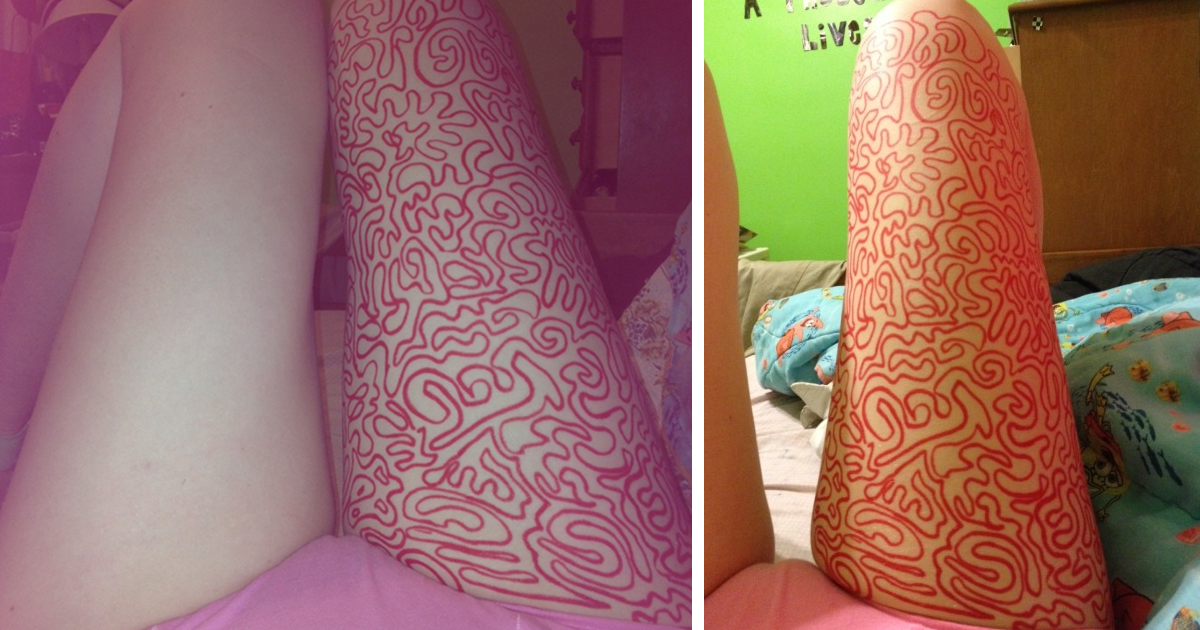 V. (Moscow), MD, prof.
V. (Moscow), MD, prof.
Kaktursky L.V. (Moscow), Doctor of Medical Sciences, Prof., Corresponding Member. RAS
PALLIATIVE MEDICINE
Gens G.P. (Moscow), MD, prof.
Novikov G.A. (Moscow), MD, prof.
PREVENTIVE MEDICINE
Boytsov S.A. (Moscow), Doctor of Medical Sciences, Prof., Academician of the Russian Academy of Sciences
Drapkina O.M. (Moscow), Doctor of Medical Sciences, Prof., Corresponding Member. RAS
PULMONOLOGY
Avdeev S.N. (Moscow), Doctor of Medical Sciences, Prof., Corresponding Member. RAS
Nevzorova V.A. (Vladivostok), MD, prof.
Popova E.N. (Moscow), MD, prof.
RHEUMATOLOGY
Mazurov V.I. (St. Petersburg), Doctor of Medical Sciences, Prof., Academician of the Russian Academy of Sciences
Nasonov E.L. (Moscow), Doctor of Medical Sciences, Prof., Academician of the Russian Academy of Sciences
THERAPY
Vorobyov P.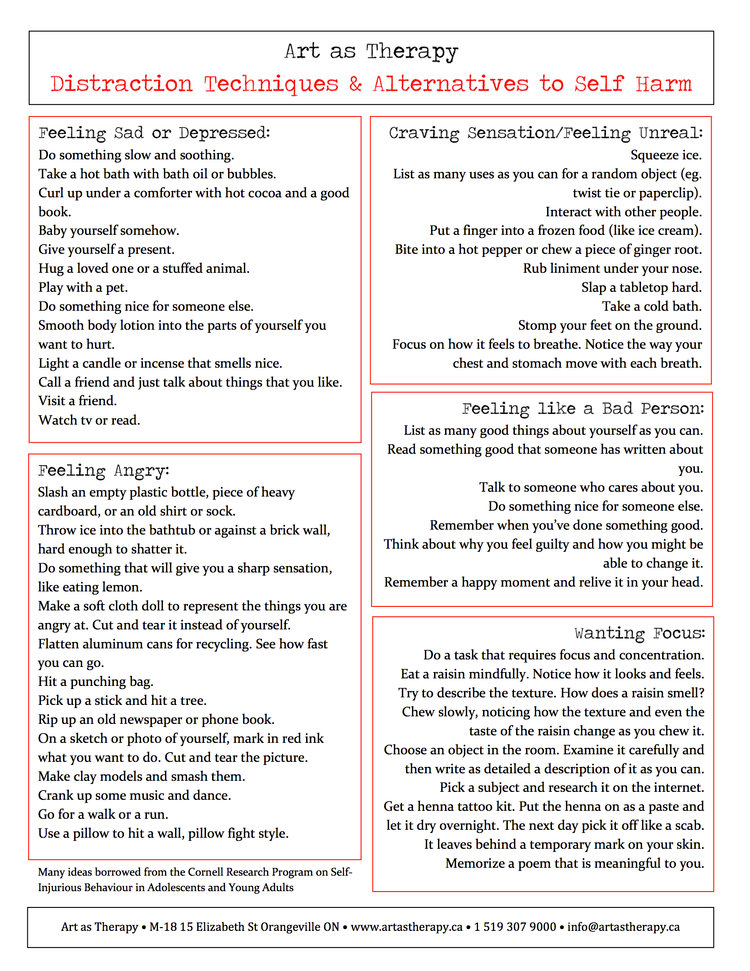 A. (Moscow), MD, prof.
A. (Moscow), MD, prof.
Zadionchenko V.S., Doctor of Medical Sciences, Prof. .
Rebrov A.P. (Saratov), MD, prof.
Saifutdinov R.I. (Orenburg), MD, prof.
Khadzegova A.B. (Moscow), MD, prof.
Yagoda A.V. (Stavropol), MD, prof.
ENDOCRINOLOGY
Demidova T.Yu. (Moscow), MD, prof.
Mkrtumyan A.M. (Moscow), MD, prof.
MEDICAL GENETICS
Voevoda M.I. (Novosibirsk), Doctor of Medical Sciences, Prof., Academician of the Russian Academy of Sciences
Zateyshchikov D.A. (Moscow), MD, prof.
EDITORIAL BOARD
Borovkova N.Yu. (Nizhny Novgorod), MD, prof.
Bosch F. (Netherlands), MD
Vasyuk Yu.A. (Moscow), MD, prof.
Volkova N.I. (Rostov-on-Don), MD, prof.
Gendlin G.E. (Moscow), MD, prof.
Eremina E.Yu. (Saransk), MD, prof.
Zykov K.A. (Moscow), MD, prof.
Zyryanov S.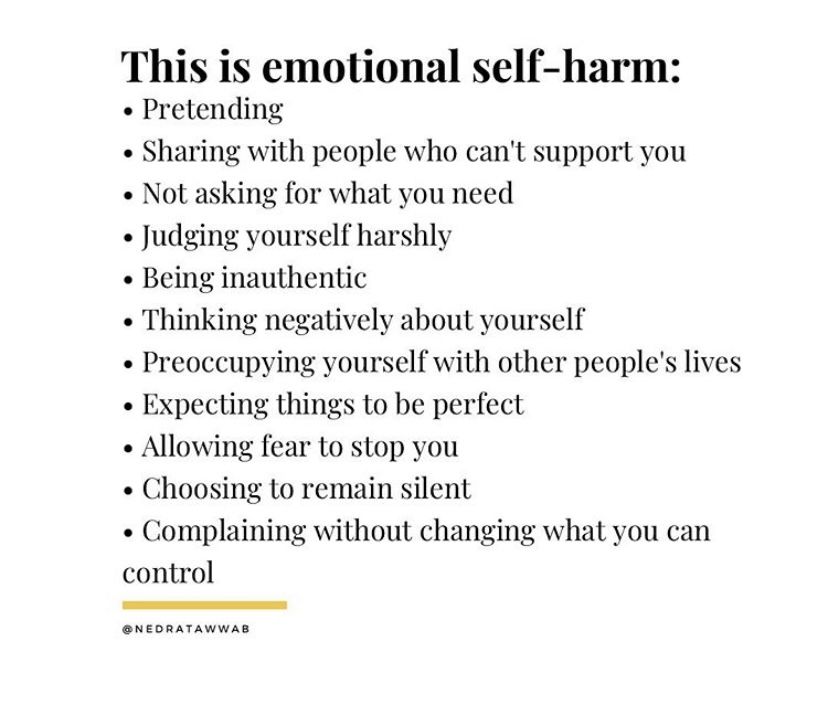 K. (Moscow), MD, prof.
K. (Moscow), MD, prof.
Keller H.P. (Switzerland), MD
Kok A. (South Africa), MD
Corbello K. (Spain), MD
Kunyaeva T.A. (Saransk), MD, prof.
Kuharzh E.J. (Poland), MD
B. Lovich (Serbia), MD
D. Lovich (Serbia), MD
Martsevich S.Yu. (Moscow), MD, prof.
Mikhin V.P. (Kursk), MD, prof.
Montano N. (Italy), MD
Nechaeva G.I. (Omsk), MD, prof.
Nikitin Yu.P. (Novosibirsk), Doctor of Medical Sciences, Prof., Academician of the Russian Academy of Sciences
Osipova I.V. (Barnaul), MD, prof.
Polunina T.E. (Moscow), MD, prof.
Puyol R. (Spain), MD
Simonenko V.B. (Moscow), Doctor of Medical Sciences, Prof., Corresponding Member. RAS
Statsenko M.E. (Volgograd), MD, prof.
Stryuk R.I. (Moscow), MD, prof.
Talibov O.B. (Moscow), Candidate of Medical Sciences, Associate Professor
Tkacheva O.N. (Moscow), MD, prof.
Trofimov V.I. (St.