Ptsd zoloft dose
Zoloft Dosage Guide - Drugs.com
Print Save Generic name: SERTRALINE HYDROCHLORIDE 25mg
Dosage forms: tablet, film coated, oral concentrate
Drug class: Selective serotonin reuptake inhibitors
Medically reviewed by Drugs.com. Last updated on Oct 29, 2021.
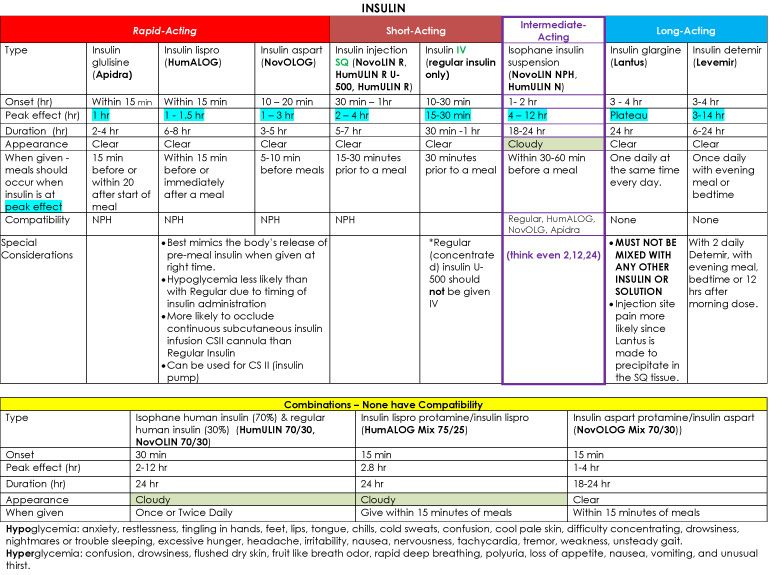
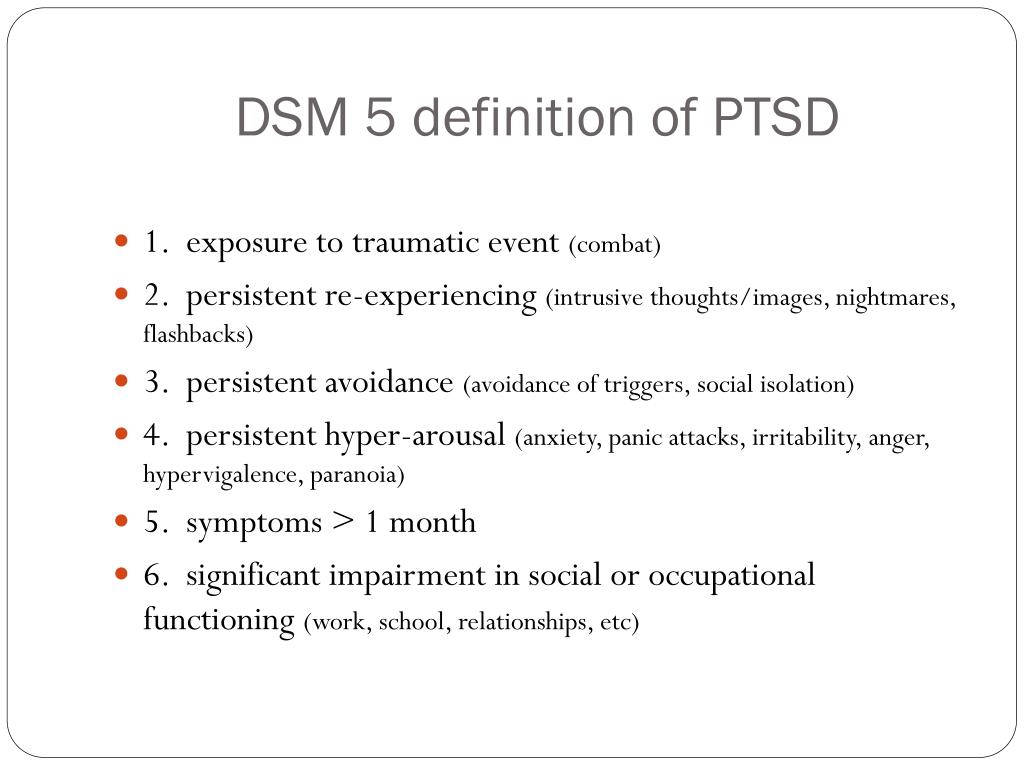
Dosage in Patients with MDD, OCD, PD, PTSD, and SAD
The recommended initial dosage and maximum ZOLOFT dosage in patients with MDD, OCD, PD, PTSD, and SAD are displayed in Table 1 below. A dosage of 25 mg or 50 mg per day is the initial therapeutic dosage.
For adults and pediatric patients, subsequent dosages may be increased in case of an inadequate response in 25 to 50 mg per day increments once a week, depending on tolerability, up to a maximum of 200 mg per day. Given the 24-hour elimination half-life of ZOLOFT, the recommended interval between dose changes is one week.
| Indication | Starting Dose | Therapeutic Range |
|---|---|---|
| Adults | ||
| MDD | 50 mg | 50–200 mg |
| OCD | 50 mg | |
| PD, PTSD, SAD | 25 mg | |
| Pediatric Patients | ||
| OCD (ages 6–12 years old) | 25 mg | 50–200 mg |
| OCD (ages 13–17 years old) | 50 mg | |
Dosage in Patients with PMDD
The recommended starting ZOLOFT dosage in adult women with PMDD is 50 mg per day. ZOLOFT may be administered either continuously (every day throughout the menstrual cycle) or intermittently (only during the luteal phase of the menstrual cycle, i.e., starting the daily dosage 14 days prior to the anticipated onset of menstruation and continuing through the onset of menses). Intermittent dosing would be repeated with each new cycle.
- When dosing continuously, patients not responding to a 50 mg dosage may benefit from dosage increases at 50 mg increments per menstrual cycle up to 150 mg per day.
- When dosing intermittently, patients not responding to a 50 mg dosage may benefit from increasing the dosage up to a maximum of 100 mg per day during the next menstrual cycle (and subsequent cycles) as follows: 50 mg per day during the first 3 days of dosing followed by 100 mg per day during the remaining days in the dosing cycle.
Screen for Bipolar Disorder Prior to Starting ZOLOFT
Prior to initiating treatment with ZOLOFT or another antidepressant, screen patients for a personal or family history of bipolar disorder, mania, or hypomania [See Warnings and Precautions (5. 4)].
4)].
Dosage Modifications in Patients with Hepatic Impairment
Both the recommended starting dosage and therapeutic range in patients with mild hepatic impairment (Child Pugh scores 5 or 6) are half the recommended daily dosage [See Dosage and Administration (2.1, 2.2)]. The use of ZOLOFT in patients with moderate (Child Pugh scores 7 to 9) or severe hepatic impairment (Child Pugh scores 10–15) is not recommended [See Use in Specific Populations (8.6), Clinical Pharmacology (12.3)].
Switching Patients to or from a Monoamine Oxidase Inhibitor Antidepressant
At least 14 days must elapse between discontinuation of a monoamine oxidase inhibitor (MAOI) antidepressant and initiation of ZOLOFT. In addition, at least 14 days must elapse after stopping ZOLOFT before starting an MAOI antidepressant [See Contraindications (4), Warnings and Precautions (5.2)].
Discontinuation of Treatment with ZOLOFT
Adverse reactions may occur upon discontinuation of ZOLOFT [See Warnings and Precautions (5. 5)]. Gradually reduce the dosage rather than stopping ZOLOFT abruptly whenever possible.
5)]. Gradually reduce the dosage rather than stopping ZOLOFT abruptly whenever possible.
Preparation of ZOLOFT Oral Solution
ZOLOFT oral solution must be diluted before use.
- Use the supplied calibrated dropper to measure the amount of ZOLOFT oral solution needed
- Note: The supplied calibrated dropper has 25 mg and 50 mg graduation marks only
- Mix with 4 ounces (1/2 cup) of water, ginger ale, lemon/lime soda, lemonade or orange juice ONLY. After mixing, a slight haze may appear, which is normal.
Instruct patients or caregivers to immediately take the dose after mixing.
Frequently asked questions
- SSRI’s vs SNRI’s - What's the difference between them?
- Lexapro vs Zoloft: How do they compare?
- How long for an increased dose of Zoloft to work?
- How long does Zoloft (sertraline) take to work?
- Does Zoloft (sertraline) cause weight gain?
- Prozac vs Zoloft - What are the Differences & Similarities?
- What are some common side effects of antidepressants?
- Is Zoloft (sertraline) a controlled substance?
- Can I take tramadol with sertraline?
More about Zoloft (sertraline)
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (1,871)
- Drug images
- Side effects
- Patient tips
- During pregnancy
- Generic availability
- Support group
- Drug class: selective serotonin reuptake inhibitors
- Breastfeeding
Patient resources
- Drug Information
- Zoloft (Sertraline Oral Liquid)
- Zoloft (Sertraline Tablets)
Professional resources
- Prescribing Information
Related treatment guides
- Major Depressive Disorder
- Depression
- Panic Disorder
- Obsessive Compulsive Disorder
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Medical Disclaimer
Medications
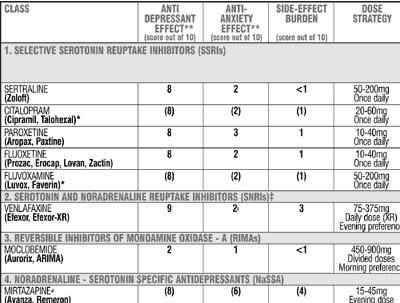
The medications conditionally recommended for the treatment of PTSD are sertraline, paroxetine, fluoxetine and venlafaxine. Each patient varies in their response and ability to tolerate a specific medication and dosage, so medications must be tailored to individual needs.
Introduction
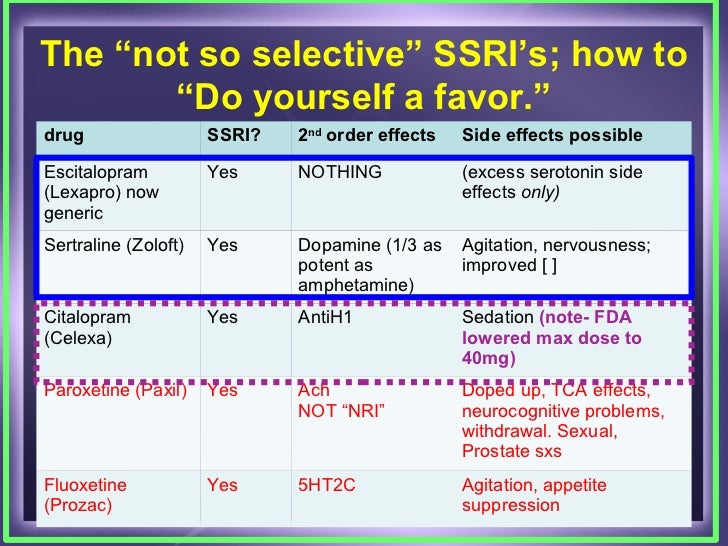
The current evidence base for PTSD psychopharmacology is strongest for the selective serotonin reuptake inhibitors (SSRIs): sertraline, paroxetine and fluoxetine as well as the selective serotonin-norepinephrine reuptake inhibitor (SNRI) venlafaxine. Currently only sertraline (Zoloft) and paroxetine (Paxil) are approved by the Food and Drug Administration (FDA) for PTSD. From the FDA perspective, all other medication uses are “off label” (see footnote), though there are differing levels of evidence supporting their use.
Selective Serotonin Reuptake Inhibitors
The neurotransmitter serotonin has a well-recognized role in the experience of mood and anxiety disorders.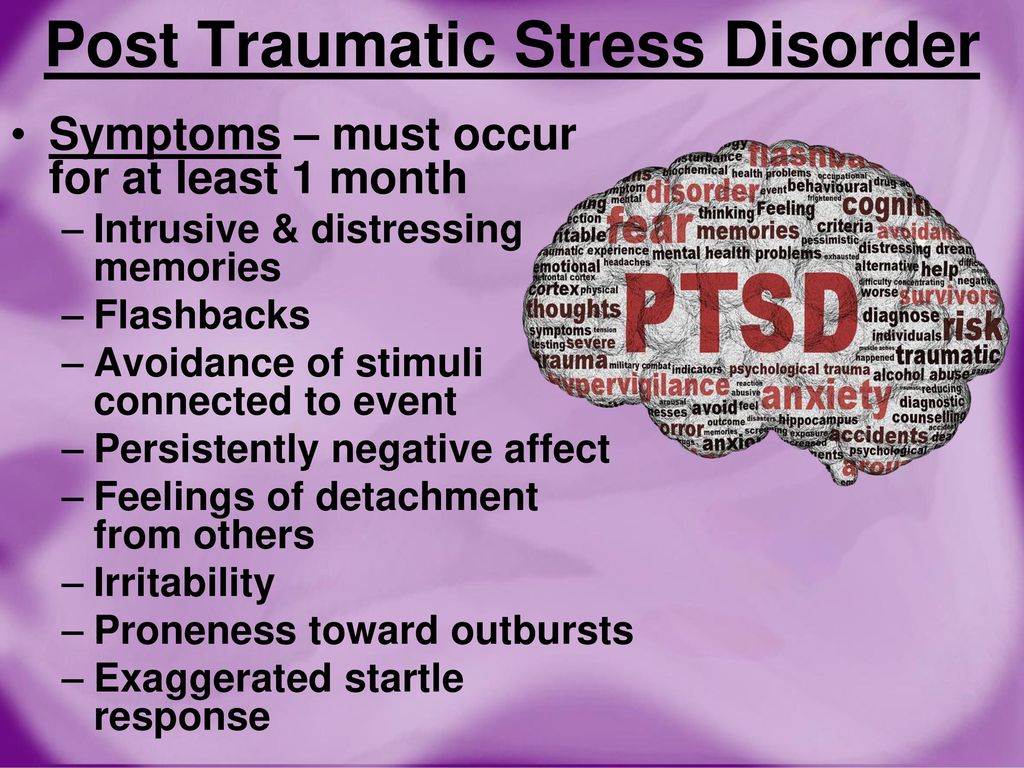 The activity of this neurotransmitter in both the peripheral and central nervous systems can be modulated by SSRIs.
The activity of this neurotransmitter in both the peripheral and central nervous systems can be modulated by SSRIs.
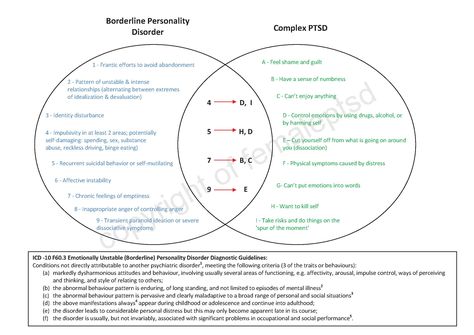
The SSRIs sertraline and paroxetine are the only medications approved by the FDA for PTSD. While SSRIs are typically the first class of medications used in PTSD treatment (Brady et al, 2000; Marshall, Beebe, Oldham & Zaninelli, 2001), exceptions may occur for patients based upon their individual histories of side effects, response, comorbidities and personal preferences.
Examples of an exception would be:
- A patient with PTSD and co-occurring bipolar disorder where an antidepressant could cause mood instability that could be mitigated with a mood stabilizing medication (such as lithium or an anti-epileptic medication) before prescribing an SSRI.
- Intolerable sexual dysfunction or gastrointestinal side effects due to the effects of increased serotonin levels in the peripheral nervous system.
Each patient varies in their response and ability to tolerate a specific medication and dosage, so medications must be tailored to individual needs. Research indicates that maximum benefit from SSRI treatment depends upon adequate dosages and duration of treatment. Ensuring treatment adherence is key to successful pharmacotherapy for PTSD. Some typical dosage ranges for medications:
Research indicates that maximum benefit from SSRI treatment depends upon adequate dosages and duration of treatment. Ensuring treatment adherence is key to successful pharmacotherapy for PTSD. Some typical dosage ranges for medications:
- Sertraline (Zoloft): 50 mg to 200 mg daily
- Paroxetine (Paxil): 20 to 60 mg daily
- Fluoxetine (Prozac): 20 mg to 60 mg daily
Other Antidepressants for PTSD
Antidepressants that affect the balance of serotonergic and noradrenergic neurotransmission, or which alter serotonin neurotransmission through other mechanisms of action, are also helpful in PTSD. Venlafaxine acts primarily as a serotonin reuptake inhibitor at lower dosages and as a combined serotonin and norepinephrine reuptake inhibitor at higher dosages. It is also a conditionally recommended treatment for PTSD. A typical dosage range is:
- Venlafaxine (Effexor): 75 mg to 300 mg daily
All of the antidepressants described above are also effective in treating comorbid major depressive disorder (MDD) which, depending upon the study, accompanies PTSD about 50 percent of the time. Dose-related elevations in blood pressure have been noted with venlafaxine. It should be used with caution in patients with hypertension.
Dose-related elevations in blood pressure have been noted with venlafaxine. It should be used with caution in patients with hypertension.
Other Medications for PTSD
Topiramate is in the anti-epileptic category of medications and is thought to modulate glutamate neurotransmission. There has been recent interest in its use for PTSD. The systematic review that served as the evidence base for the guideline development panel reported moderate strength of evidence for a medium to large magnitude effect for PTSD symptom reduction.
However, the panel concluded that there was insufficient evidence to make a recommendation because the potential side effects/harms for topiramate are greater than they are for SSRI antidepressants. It is not uncommon for patients taking topiramate to note side effects of cognitive dulling. Topiramate has also been found helpful in reducing alcohol consumption in those with an alcohol use disorder, which frequently accompanies PTSD.
Adapted from https://www.ptsd.va.gov/professional/treat/txessentials/clinician_guide_meds.asp with original content written by Matt Jeffreys, MD. Matthew J. Friedman, MD, PhD, Thomas Mellman, MD and Jeffrey Sonis, MD, MPH also contributed.
The FDA regulates approval of medications, not prescribing of medications. An off-label use of a medication means that it is being used for an indication other than one for which is was approved by the FDA. It is estimated that 1 in 5 outpatient prescriptions are written off-label. According to the FDA, “From the FDA perspective, once the FDA approves a drug, healthcare providers generally may prescribe the drug for an unapproved use when they judge that it is medically appropriate for their patient.”
For Patients & Families
How do I choose between medication and therapy?
Choice of treatment should be based on the best scientific evidence, comfort with the options, and consultation with a physician, psychologist or mental health professional.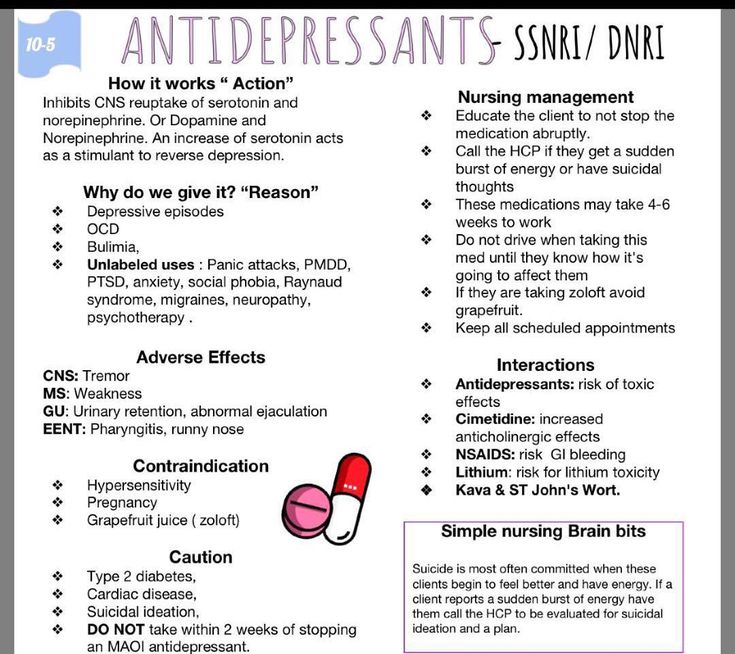
References
Journal Article
Brady, K., Pearlstein, T., Asnis, G. M., Baker, D., Rothbaum, B., Sikes, C. R., & Farfel, G. M. (2000). Efficacy and safety of sertraline treatment of posttraumatic stress disorder: A randomized controlled trial. Journal of the American Medical Association, 283, 1837-1844.
Journal Article
Marshall, R. D., Beebe, K. L., Oldham, M., & Zaninelli, R. (2001). Efficacy and safety of paroxetine treatment for chronic PTSD: A fixed-dose, placebo-controlled study. American Journal of Psychiatry, 158, 1982-1988.
Updated July 31, 2017
Date created: May 2017
Zoloft instructions for use: Side effects, analogues, contraindications
THERE ARE CONTRAINDICATIONS. POSSIBLE SIDE EFFECTS. A SPECIALIST'S CONSULTATION IS REQUIRED.
Author
Khokhrina Kristina Sergeevna,
Provisor
All authorsContent of Article
- Zoloft: active substance
- Zoloft: Side effects
- Goloft: Contraindications
- ZoloFT and alcohol
- 0014
- Zoloft: how to stop drinking it
- Zoloft: analogues
- Abstract
- Ask an expert on the topic of the article
According to WHO estimates, 3.8% of the total population, which is 280 million people, suffer from depression. Among them, 5% of adults and 5.7% of persons over 60 years of age. More than 700,000 people die each year from suicide due to depression. Depression is treatable with medication.
Doctors prescribe antidepressants. Zoloft is one of them. We asked pharmacist Kristina Khokhrina to tell us in more detail: what side effects it can cause, what active ingredient, contraindications, overdose, is the drug compatible with alcohol and how to stop drinking it.
Zoloft is one of them. We asked pharmacist Kristina Khokhrina to tell us in more detail: what side effects it can cause, what active ingredient, contraindications, overdose, is the drug compatible with alcohol and how to stop drinking it.
27 reviews
Zoloft: active ingredient
Zoloft contains the active ingredient - sertraline in the form of hydrochloride. It is produced in tablets with a dosage of 50 mg and 100 mg. Zoloft is an antidepressant. It is used to treat and prevent depression caused by various causes. And also when:
- obsessive-compulsive disorders
- panic disorders
- post-traumatic stress disorder
- social phobias
How Zoloft works
Zoloft helps to eliminate depressive manifestations:
- relieves anxiety
- normalizes sleep
- reduces somatic manifestations: palpitations, disruption of the gastrointestinal tract, increased excitability.
Zoloft does not cause dependence on the drug and does not lead to weight gain in humans.
Zoloft side effects
Monitor your condition closely while using the medicine. If you experience side effects that are not described or if symptoms worsen, contact your doctor immediately.
Zoloft: side effects
- flatulence, nausea, vomiting, diarrhea, constipation, abdominal pain, dry mouth
- increased heart rate, increased blood pressure
- arthralgia, muscle cramps
- gait disturbance, teeth grinding, drowsiness, syncope, headache, migraine, tremor, insomnia, anxiety, hallucinations, psychosis, nightmares, decreased libido, suicide, coma
- yawning, bronchospasm
- bedwetting, urinary retention during the day
- hepatitis, jaundice
- decrease in potency, disruption of the reproductive system, menstrual cycle disorders in women
- visual impairment
- thyroid disorder
- urticaria, pruritus, anaphylactic shock
- flushing, tinnitus, loss of appetite and others
Zoloft: contraindications
- hypersensitivity to any component of the formulation
- concomitant use of monoamine oxidase inhibitors and pimozide
- pregnancy and lactation
- children under 6 years of age
Caution must be taken in: mental retardation, epilepsy, renal and / or liver failure, marked reduced body weight.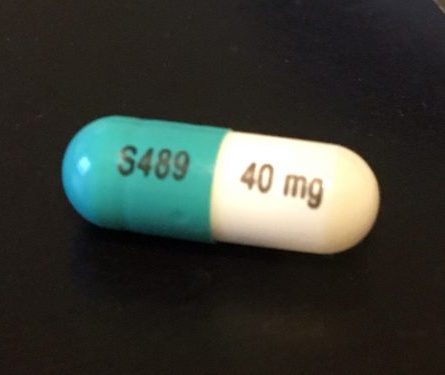
Zoloft and alcohol
Alcohol is not recommended to be taken with the medicine. Its action can increase side effects and lead to overdose.
How to recognize depression is described in the article "Beck Test for Depression"
Zoloft: overdose
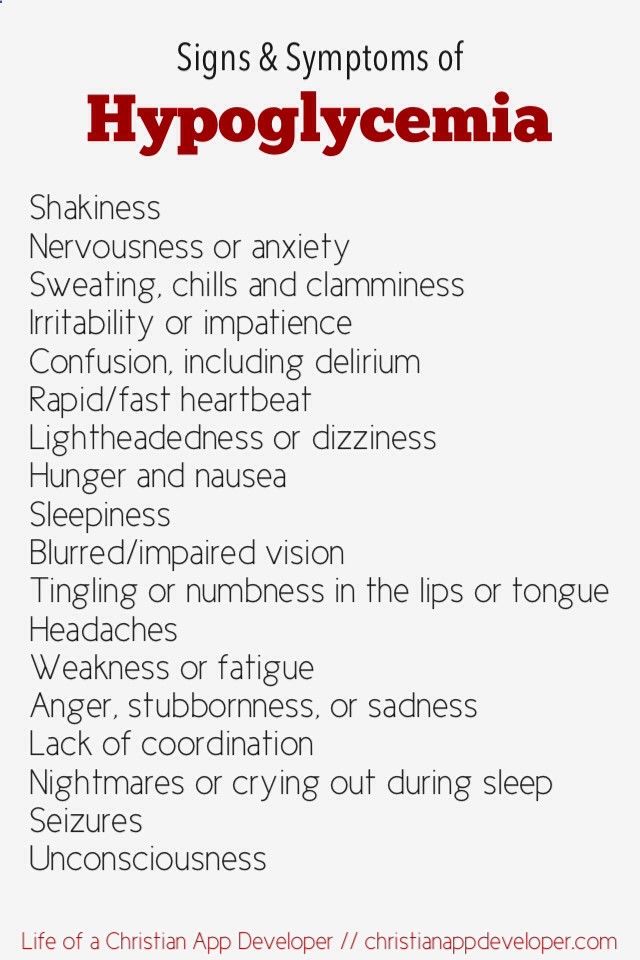
Zoloft overdose occurs when used simultaneously with alcohol or other incompatible drugs. With such combinations, severe poisoning can occur, up to coma and death. Overdose symptoms are:
- nausea
- vomiting
- drowsiness
- increased heart rate
- dizziness
- psychomotor agitation
- diarrhea
- excessive sweating
Hospital observation and constant monitoring of vital signs will be required. When first aid is not recommended to induce vomiting, it is better to give activated charcoal.
Zoloft: how to stop drinking it
"Withdrawal" syndrome is rare. Nevertheless, it is necessary to discuss with the doctor a decrease in the dosage of the drug. Since the termination of treatment is possible:
Nevertheless, it is necessary to discuss with the doctor a decrease in the dosage of the drug. Since the termination of treatment is possible:
- symptoms of depression
- hallucinations
- aggression
- anxiety
- psychosis
Particular attention should be paid to the fact that after the end of the use of Zoloft, within 14 days, you should not take drugs related to monoamine oxidase inhibitors.
Zoloft: analogues
Zoloft has about 10 names of analogues of the active substance. All medicines are prescribed and prescribed by a doctor. Therefore, to choose a remedy or replace your own, consult your doctor first.
Zoloft and Atarax: compatibility
The combined use of these drugs increases the side effects. This manifests itself in the form of dizziness, drowsiness and confusion. Elderly people have difficulty in thinking and coordinating movements.
Do you want to understand analogues of drugs in order to skillfully select drugs for your budget? Our manual from expert pharmacists "Analogues of popular drugs" will help you with this! Getting a training manual is easy: subscribe to our social networks and write “analogues” in the messages.
Megapharmacy in social networks: VKontakte, Telegram, OK
Summary
- Zoloft is an antidepressant that is taken to prevent and treat depression and other disorders.
- Zoloft may have a significant number of side effects.
- The active substance is sertraline, dosage in tablets of 50 mg or 100 mg.
- Zoloft has contraindications that should be taken into account when prescribing it.
- The use of alcohol in conjunction with Zoloft is not recommended to avoid overdose symptoms.
- An overdose of the drug occurs when used simultaneously with certain drugs and alcohol.
- Zoloft is not usually addictive, but you should consult your doctor before stopping it.
- Zoloft has several analogues, but only a doctor can replace them.
Ask an expert about the topic of the article
Still have questions? Ask them in the comments below and our experts will answer you. There you can also share your experience with other readers of Megasovets.
Share the mega tip
Like this article? Tell your mom, dad, grandma and aunt Galya from the third entrance
Copy link
Antidepressant Zoloft in the practice of a general practitioner
Choosing an antidepressant. Focus on the needs of the patient Top page topics
12/29/2016
Antidepressant Zoloft in the practice of a general practitioner The work of a doctor of any profile has its own characteristics. The specifics of the work of a general practitioner is determined by a wide range of his diagnostic and therapeutic activities, sometimes without clear boundaries. In the diagnosis and treatment of diseases of the cardiovascular system, the therapist interacts (collaborates, and sometimes competes) with a cardiologist, in the treatment of diseases of the digestive system - with a gastroenterologist, in the treatment of kidney diseases - with a nephrologist and urologist, etc. Therapists along with traumatologists and rheumatologists often treat patients with osteochondrosis, arthrosis and arthritis. It is the therapist who can be the main doctor for patients with several concomitant diseases, since he has to put into practice the principle “to treat not the disease, but the patient” and sometimes draw up the final comprehensive treatment plan, taking into account the appointments of narrow specialists.
The specifics of the work of a general practitioner is determined by a wide range of his diagnostic and therapeutic activities, sometimes without clear boundaries. In the diagnosis and treatment of diseases of the cardiovascular system, the therapist interacts (collaborates, and sometimes competes) with a cardiologist, in the treatment of diseases of the digestive system - with a gastroenterologist, in the treatment of kidney diseases - with a nephrologist and urologist, etc. Therapists along with traumatologists and rheumatologists often treat patients with osteochondrosis, arthrosis and arthritis. It is the therapist who can be the main doctor for patients with several concomitant diseases, since he has to put into practice the principle “to treat not the disease, but the patient” and sometimes draw up the final comprehensive treatment plan, taking into account the appointments of narrow specialists. The therapist is rightly called the “primary link” of the health care system and the “family doctor”, since he has to deal with the issues of primary diagnosis and treatment of many diseases. Many patients, regardless of the identified pathology, remain under his supervision, and the treatment of the rest (referring to narrow specialists) can subsequently be carried out with his participation. And of course, for each patient, the therapist should ideally be a personal psychotherapist. In his work, the therapist often encounters certain manifestations of depression, which are detected in many patients with a therapeutic profile. According to statistics, 80% of all patients with depressive disorders first turn to a therapist, which is due to both objective and subjective reasons. Among the objective reasons, one can single out the mutual influence of the pathogenetic mechanisms of mental disorders and organic diseases (including internal diseases).
Many patients, regardless of the identified pathology, remain under his supervision, and the treatment of the rest (referring to narrow specialists) can subsequently be carried out with his participation. And of course, for each patient, the therapist should ideally be a personal psychotherapist. In his work, the therapist often encounters certain manifestations of depression, which are detected in many patients with a therapeutic profile. According to statistics, 80% of all patients with depressive disorders first turn to a therapist, which is due to both objective and subjective reasons. Among the objective reasons, one can single out the mutual influence of the pathogenetic mechanisms of mental disorders and organic diseases (including internal diseases).
On the one hand, depression can create conditions for the formation of organic diseases, aggravate and change their course. This is mediated through a variety of neuroendocrine and immunological mechanisms, regarding the interaction of which there is no consensus today. However, it is believed that they are realized through significant violations of autonomic functions, which leads to the formation of "organ neuroses". Pathological enhancement of sympathoadrenal influences may be accompanied by the formation of persistent arterial hypertension, hyperthyroidism, reduced glucose tolerance, and an increase in the content of inflammatory enzymes in the synovial fluid.
However, it is believed that they are realized through significant violations of autonomic functions, which leads to the formation of "organ neuroses". Pathological enhancement of sympathoadrenal influences may be accompanied by the formation of persistent arterial hypertension, hyperthyroidism, reduced glucose tolerance, and an increase in the content of inflammatory enzymes in the synovial fluid.
Parasympathetic pathological influences contribute to the formation of bronchospastic syndrome and hypersecretion of gastric juice. On the other hand, the pathogenesis of long-term chronic somatic diseases involves the formation of certain psychological changes that create prerequisites for the development of depression. The so-called psychosomatic disorders include not only organ neuroses (syndrome of "irritable stomach", "irritable intestines", "irritated bladder" and other "irritated" organs, functional coprostasis, esophageal achalasia), but also angina attacks that occur as a conditioned reflex , bronchospasm, etc. Such disorders are often accompanied by phobias (fear of gas incontinence, inability to use the toilet) and psychoreactive states (neurotic syndromes, affective and pathocharacterological reactions).
Such disorders are often accompanied by phobias (fear of gas incontinence, inability to use the toilet) and psychoreactive states (neurotic syndromes, affective and pathocharacterological reactions).
Thus, one group of patients with depression at the therapist's appointment is made up of "dispensary" patients who have new symptoms, and the other is new patients who turned to the therapist with somatic manifestations of depression. It should be noted that in these difficult conditions, the timely diagnosis of depressive disorders largely depends on the qualifications of the doctor: the appearance of somatic symptoms in a patient with depression is often mistakenly perceived as vegetative manifestations of psychogenic disorders, and the addition of symptoms of depression to the clinic of a somatic disease is considered as astheno-vegetative or " hypochondriacal "syndrome (as part of the clinic of the underlying disease).
The diagnostic principle of searching for one disease that explains the fullness of the symptoms in a particular patient (correct in most cases) often plays a cruel joke with the doctor when diagnosing depression. In addition, the primary appearance of depressive symptoms or its addition to somatic pathology significantly reduces the patient's adherence to treatment. As for the subjective reasons for such a high frequency of patients with depression visiting a therapist, it can be noted that a significant part of patients, even suspecting the nature of their condition, under the influence of subjective factors, prefers to seek help not from a psychiatrist (some fear publicity about the fact of observation by a psychiatrist and related social restrictions, others the alleged negative side effects of psychotropic drugs).
The specificity of the medical activity of a general practitioner also determines the features of the choice of drugs. As their own observations show, general practitioners prefer to start treatment with broad-spectrum drugs with a proven therapeutic effect, without pronounced side effects and adverse interactions with other drugs, which have a positive effect on the most common comorbidities, which have a convenient mode of administration - then There are first-line drugs that are safe and effective in most patients. Thus, in the treatment of arterial hypertension, we often begin therapy with the use of modern calcium antagonists (amlodipine) or angiotensin-converting enzyme inhibitors (quinapril, lisinopril). When choosing antibiotic therapy, we often start treatment with broad-spectrum antibiotics. Selective serotonin reuptake inhibitors (SSRIs), in particular sertraline (Zoloft, Phizer), occupy such a place in the arsenal of a general practitioner for the treatment of depressive conditions.
Thus, in the treatment of arterial hypertension, we often begin therapy with the use of modern calcium antagonists (amlodipine) or angiotensin-converting enzyme inhibitors (quinapril, lisinopril). When choosing antibiotic therapy, we often start treatment with broad-spectrum antibiotics. Selective serotonin reuptake inhibitors (SSRIs), in particular sertraline (Zoloft, Phizer), occupy such a place in the arsenal of a general practitioner for the treatment of depressive conditions.
As a characteristic representative of the SSRI group, Zoloft has all the main advantages of this group of antidepressants. From other drugs used in the treatment of depression, SSRIs differ in fewer and less severe side effects. They do not increase the effect of alcohol and tranquilizers when taken at the same time. The drugs of this group, unlike sulpiride, do not affect the level of prolactin. If you look at the list of side effects of SSRIs, then it becomes uncomfortable (for both the doctor and the patient): anxiety, sleep disturbances, vision, gait, digestive disorders, sexual function and endocrine system organs are possible. However, in our clinical practice, only parasympathicotonic effects of SSRIs were encountered: sweating, hypotension and dizziness, dry mouth, and the frequency of these effects was rather low.
However, in our clinical practice, only parasympathicotonic effects of SSRIs were encountered: sweating, hypotension and dizziness, dry mouth, and the frequency of these effects was rather low.
Indications for the appointment of Zoloft are depression (including accompanied by a sense of anxiety) with or without a history of mania; obsessive-compulsive disorders (OCD) in adults and children; panic disorder, with or without agoraphobia; post-traumatic stress disorder; social phobia (social anxiety disorder). With a satisfactory result of treatment, continuation of sertraline therapy is an effective means of preventing recurrence of the initial episode of depression and its development in the future; recurrence of the initial episode of obsessive-compulsive disorder; panic disorder, initial episode of post-traumatic stress disorder, social phobia.
Sertraline does not cause drug dependence; does not have the stimulating and disturbing effects characteristic of D-amphetamine, or the sedative effect and psychomotor disturbances characteristic of alprazolam; does not have a stimulating, sedative or anticholinergic effect, and also does not show a cardiotoxic effect in the experiment.