Anxiety tongue tingling
Tingling tongue and anxiety: Causes, treatment, and more
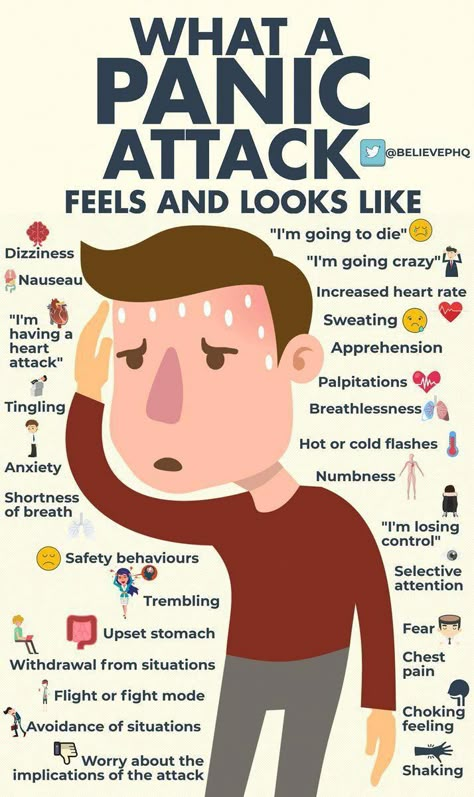
Tingling and numbness are among the most common symptoms of anxiety. While it is common to feel tingling in the hands or feet, it is also possible to notice these symptoms elsewhere, including the tongue.
The medical community refers to a tingling of the tongue as psychogenic lingual paresthesia. Paresthesia is the term for an unusual sensation, and psychogenic means that the origin is psychological.
In this article, we discuss the link between anxiety and a tingling tongue in more detail. We also look at the other physical symptoms of anxiety.
When a person is anxious, their body prepares them for a fight-or-flight response, triggering a wide range of physical changes. One of these changes is that the blood vessels constrict. This constriction reduces blood flow, which can cause numbness and tingling, especially in the feet and hands. It is also possible to experience tingling in the tongue.
A tingling tongue is a relatively common oral symptom. Although it can sometimes be due to physical issues, such as nerve damage, anxiety can also lead to tingling.
A 2015 case study reports on a 32-year-old man who had experienced tingling on the tip and right side of his tongue for 5 months. An examination revealed no physical cause.
Based on the man’s other symptoms, doctors diagnosed him with psychogenic lingual paresthesia, which is tingling in the tongue for psychological reasons, along with mixed anxiety and depressive disorder. The tongue sensation resolved after he began taking an antidepressant.
Sometimes, anxiety causes tics, which are sudden, uncontrolled, repetitive movements. Some tics, such as chewing or sucking motions, can injure the tongue.
Some injuries may lead to numbness, pain, or tingling. Although anxiety is ultimately the cause, it is important to seek medical treatment for the injury.
Anxiety is not the only possible cause of numbness in the tongue. Many people experience tongue numbness following dental procedures or an injury to the face.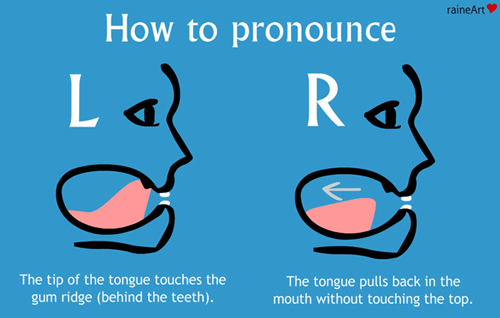 Numbing agents, as well as nerve damage from falls or oral surgery, may cause tongue numbness.
Numbing agents, as well as nerve damage from falls or oral surgery, may cause tongue numbness.
Other conditions that cause compulsive behaviors, such as Tourette’s syndrome and obsessive-compulsive disorder (OCD), can also cause a person to hurt their tongue.
Treatment for anxiety-related tongue tingling begins with ruling out other potential causes. Once a person knows that their symptom stems from anxiety, they may feel less worried about it and more motivated to treat the anxiety itself.
Treating the anxiety usually fixes the sensation. The right treatment depends on the person, the type of anxiety they have, and their symptoms and treatment goals.
In some cases, temporary anxiety from stress goes away on its own when a person’s circumstances improve. Chronic anxiety, though, demands treatment.
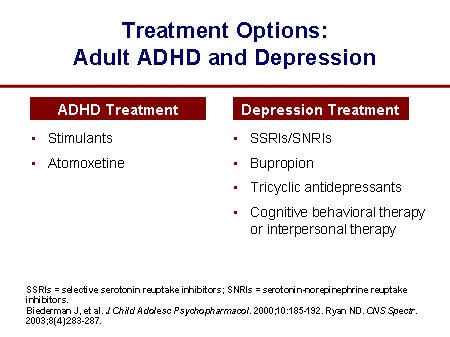
A person’s treatment options may include:
- therapy to discuss the cause of the anxiety and explore coping skills
- medication, such as antidepressants or anti-anxiety drugs
- support from family or friends
- anxiety support groups
- alternative and complementary treatments, such as acupuncture and chiropractic care
- self-care strategies, such as meditating, exercising, or adopting a time management system
If another underlying condition is responsible for tongue tingling, a person may need treatment for that condition. People who notice prolonged tongue numbness may also need dental care.
People who notice prolonged tongue numbness may also need dental care.
A person should contact a doctor if:
- tongue numbness lasts several days or does not improve when a person’s anxiety is better
- anxiety does not get better with home management strategies
- they experience different anxiety symptoms than usual
- they notice numbness after taking a new medication or sustaining an injury to the tongue or mouth
- anxiety medication makes the symptoms worse, does not work, or stops working
- anxiety is severe enough to interfere with daily life
- they experience thoughts of suicide or self-harm
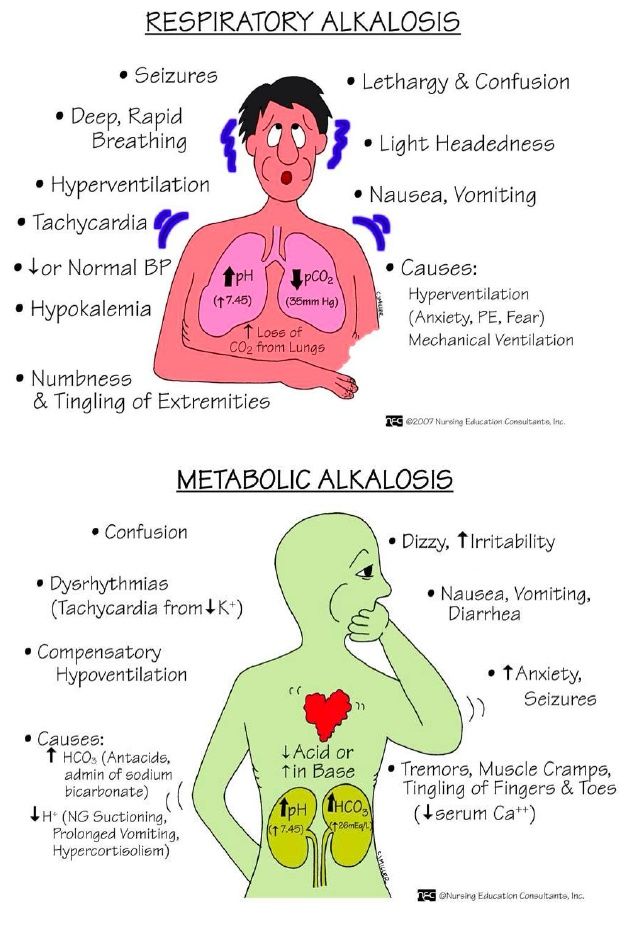
Emergency care is necessary if bodywide tingling occurs alongside other serious symptoms, such as intense chest pain, and anxiety management strategies do not help. Examples of these strategies include deep breathing and muscle relaxation.
Anxiety is more than just an emotional experience. It affects the whole body because the body responds to a perceived threat by initiating the fight-or-flight response to prepare the person to deal with the threat.
Other symptoms of anxiety that a person might notice include:
- rapid heart rate
- high blood pressure that might cause flushing or make it feel as though the heart is beating very fast
- palpitations of the heart, or a very fast heart rate
- the feeling of being unable to catch a breath
- breathing very fast
- numbness elsewhere in the body
- other strange sensations, headaches, or stomach pain
- increased sweating
- feeling more alert, which can make it difficult to sleep or relax
It is easy to worry about a tingling tongue, especially if a person already feels anxious.
Many different conditions can cause a tingling tongue, so it is important not to ignore it. If it disappears as anxiety eases, the anxiety is likely the cause.
A person should contact a doctor if they frequently experience anxiety, panic attacks, or numbness, or if they have persistent tongue numbness and tingling.
What Is Anxiety Tongue and What Are Its Signs?
Anxiety can cause tingling or numbness in your tongue as well as other changes in your mouth.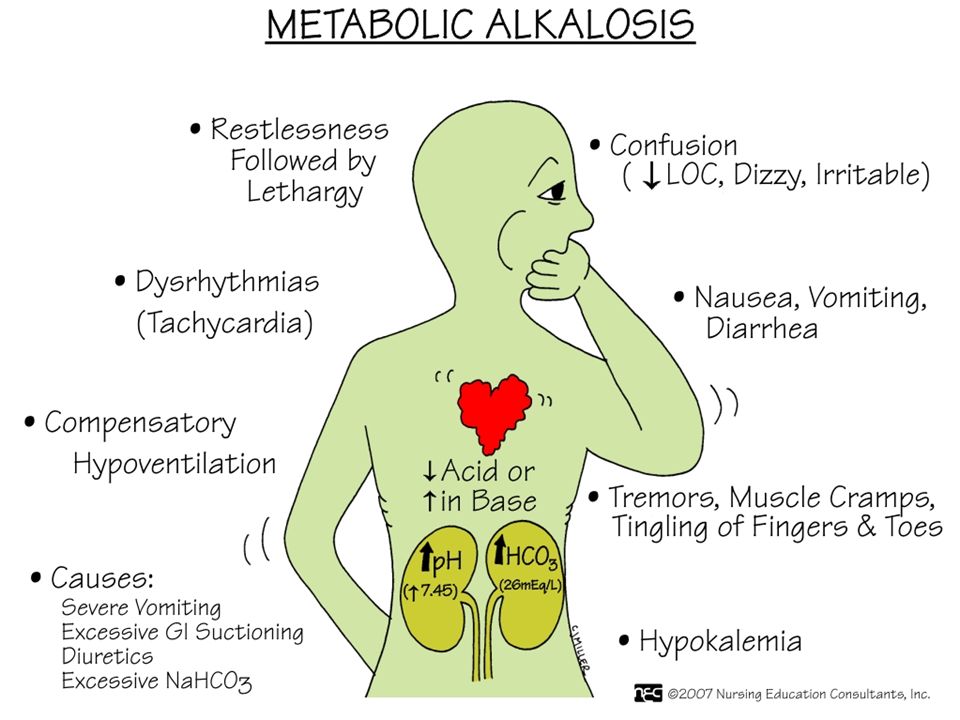 You may need to talk with a health professional if you have these signs.
You may need to talk with a health professional if you have these signs.
Anxiety may cause you to experience mental, emotional, and physical symptoms. This may include a tingling feeling, numbness, or swelling in your tongue.
Some people with anxiety disorders often experience a tingling sensation on their tongue, commonly referred to as “anxiety tongue” or “stress tongue.”
Anxiety tongue may also involve swelling, muscle spasms, or burning sensations.
Anxiety as an emotional response is linked to your stress response. When you perceive a real or imagined threat, your body activates to respond to said threat. This initiates a series of physiological processes that go from hormone secretion to muscle tension to changes in your blood flow.
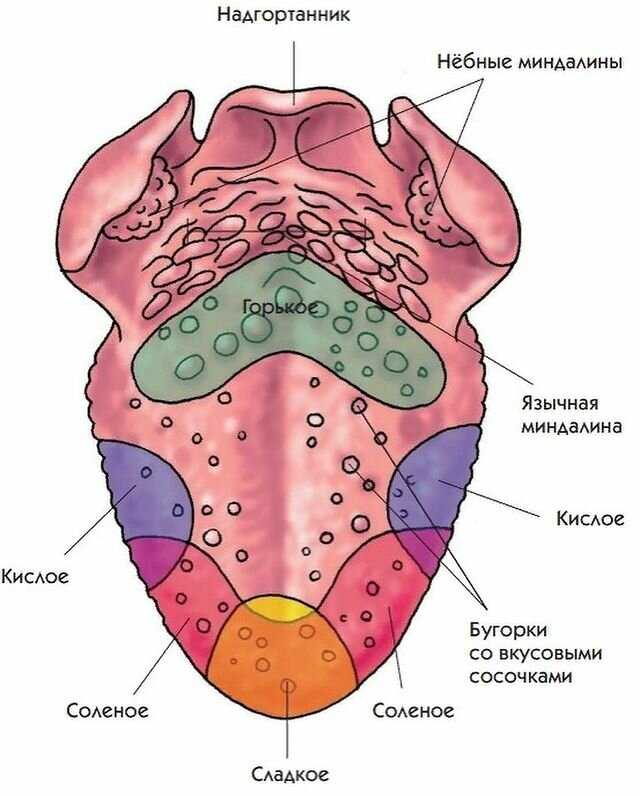
These changes can affect your tongue, which is a combination of muscles, nerves, and blood vessels.
As muscles tense, nerves get stimulated, and blood vessels constrict to restrict blood flow, your tongue may start feeling different. This may include a wide range of sensations.
This may include a wide range of sensations.
A tingling or numb tongue may be the result of psychogenic oral paresthesia, which is an unpleasant oral sensation caused by a psychological trigger, such as stress or anxiety.
In addition to tingling or numbness, psychogenic oral paresthesia can also lead you to experience a sudden prickling, twitching, swelling, or burning feeling.
Anxiety has also been linked to tongue swelling and scalloped tongue, which is a condition that causes waves or ripples along the sides of the tongue.
Can anxiety make your whole mouth feel different?
Anxiety can affect your tongue as well as your whole mouth. Some possible anxiety-related signs include:
- dry mouth
- metallic taste
- changes in taste
- tooth or gum pain
- burning sensation
- uncontrolled sucking motions
- teeth grinding
- halitosis
Addressing the root cause often leads to symptom relief. Managing your anxiety may help reduce the signs of anxiety tongue and other anxiety-related mouth sensations.
If you think you may have an “anxiety tongue,” it’s highly advisable that you talk with a health professional. They’ll be able to rule out any other possible causes of your tingling, numbness, swelling, or pain.
Anxiety treatment often consists of a combination of psychotherapy and medication. Cognitive behavioral therapy (CBT) is an effective psychotherapeutic approach for the management of anxiety symptoms and benzodiazepines are often used as anti-anxiety medication.
If anxiety treatment doesn’t relieve the signs of anxiety tongue, consider discussing the problem with a general physician or another health professional.
In sum, consider visiting a health professional if:
- tongue tingling or numbness persists for several days
- tingling or numbness continues after other anxiety symptoms stop
- tingling or numbness starts after starting anxiety medication
- your anxiety medications make your symptoms worse
- anxiety or stress management techniques don’t help ease your symptoms
- you have thoughts of self-harm
Anxiety tongue often refers to the physical effects that anxiety may have on your tongue and mouth.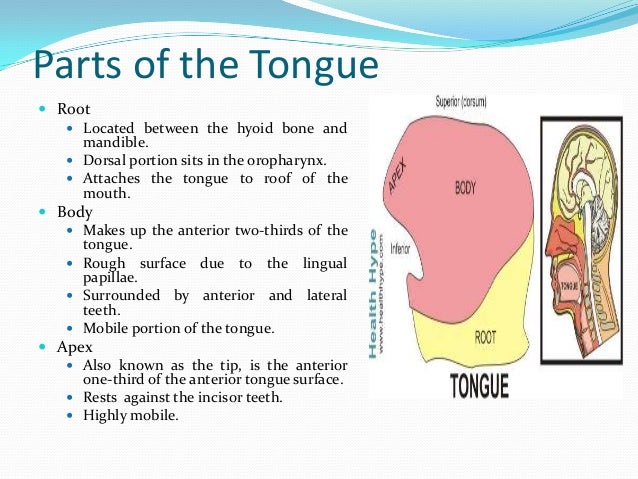 These effects may include tingling, twitching, numbness, burning, or pain in your tongue or mouth.
These effects may include tingling, twitching, numbness, burning, or pain in your tongue or mouth.
Treating anxiety may relieve your tongue symptoms. If it doesn’t, consider discussing these with a health professional so they can rule out any other possible causes of your sensations.
Tongue tingling - causes, diagnosis and treatment
Tongue tingling occurs when it is injured by carious teeth or prostheses, desquamative and hunter's glossitis, xerostomia. The symptom is typical for glossodynia, glossalgia, which develop with endocrine, gastroenterological or neurological pathologies. To diagnose the causes of tingling, a dental examination, microscopic and bacteriological analysis of tongue scrapings, instrumental methods (sonography of the salivary glands, EFGDS, electromyography) are performed. Treatment involves a combination of medication (etiotropic and pathogenetic drugs) and physiotherapy techniques.
Causes of tongue prickling
Physiological factors
Pricking, burning all over the tongue occurs after eating spicy foods, some spices. Unpleasant sensations are noted directly during meals, lasting several hours. To reduce discomfort, a person drinks cool water, rinses his mouth. The tingling is accompanied by increased production of saliva, which must be constantly swallowed. Externally, the tongue is unchanged, sometimes due to irritation and increased blood flow, it looks bright pink.
Unpleasant sensations are noted directly during meals, lasting several hours. To reduce discomfort, a person drinks cool water, rinses his mouth. The tingling is accompanied by increased production of saliva, which must be constantly swallowed. Externally, the tongue is unchanged, sometimes due to irritation and increased blood flow, it looks bright pink.
The second typical cause is drinking too hot drinks or food. There is a superficial burn of the tongue, which is manifested by painful tingling, burning and tingling. With mild damage, the symptoms bother for 12-24 hours, after which the increased sensitivity of the receptors to hot or spicy foods persists for several days.
Diseases of the teeth
Constant tingling occurs when the tongue is traumatized by the sharp edges of carious teeth, improperly selected crowns or prostheses. Discomfort is felt in the same place where there is maximum friction or scratching of the tooth on the surface of the tongue. An epithelium defect is formed in this area, therefore, when spicy food enters, the tingling intensifies.
An epithelium defect is formed in this area, therefore, when spicy food enters, the tingling intensifies.
Xerostomia
Low saliva production causes the tongue to dry out, causing an excruciating feeling of tightness and tingling. The symptoms are aggravated by talking for a long time, eating dry solid food. Gradually, xerostomia progresses, so burning, tingling, discomfort persist constantly. To alleviate the condition, patients regularly rinse their mouths, drink water, but such manipulations help for a short time.
Tingling of the tongue
Glossalgia
With this pathology, the patient complains of a variety of painful sensations: tingling, tingling, rawness. Symptoms are not related to food or hot drinks. The tingling is most pronounced on the lateral surfaces and the tip of the tongue. Localization of sensations periodically changes. Externally, the language is not changed. Secondary glossalgia appear:
- Endocrine disorders : diabetes mellitus, Itsenko-Cushing's disease, hypothyroidism.

- Pathologies of the gastrointestinal tract : gastritis and gastroduodenitis, pancreatitis, hepatitis and cholecystitis.
- Peripheral nerve damage : neuropathy of the glossopharyngeal nerve, ganglionitis of the hypoglossal autonomic ganglion, sympathalgia.
- CNS diseases : encephalitis, neurosyphilis, residual effects after stroke.
- Connective tissue diseases : scleroderma, dermatomyositis.
Glossodynia
There are paresthesias, manifested by tingling, burning, crawling sensation, which have no apparent cause. At first, discomfort symptoms affect only the tip of the tongue, gradually they spread over its entire surface like an “oil spot”. The root of the tongue is the last to be affected, but often there is no tingling at all in this area.
Discomfort lasts for 3-5 minutes, occurs several times a day. As glossodynia progresses, episodes of paresthesia lengthen, accompanied by a feeling of enlargement and swelling of the tongue.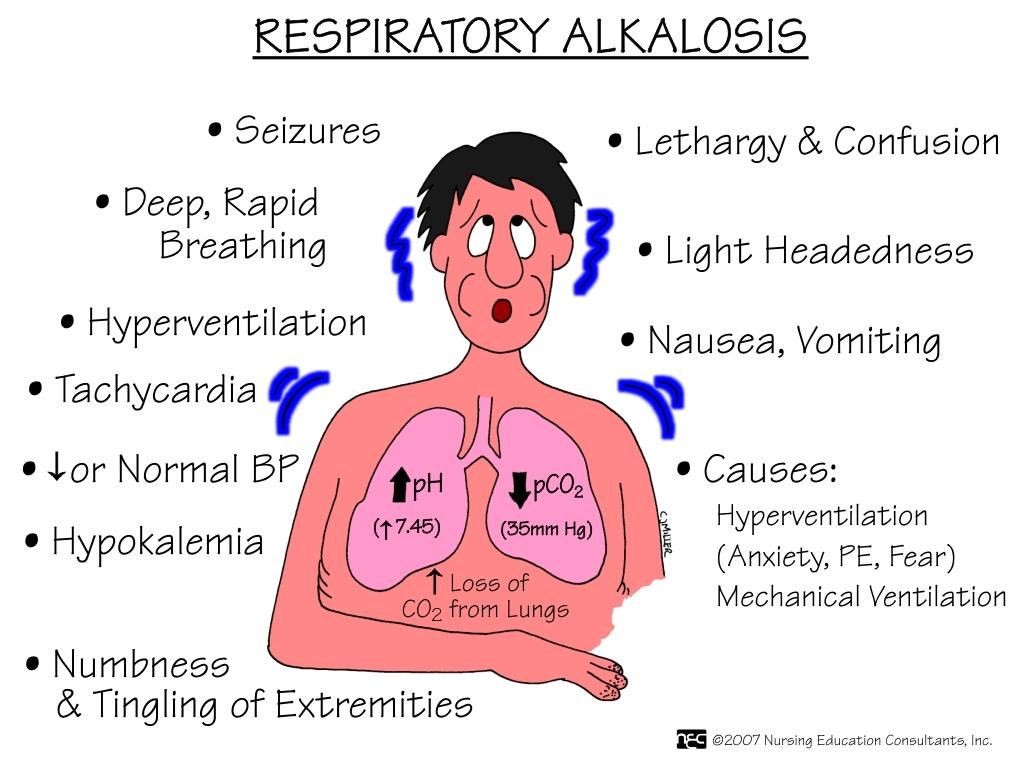 The pathognomonic feature of the disease is the absence of tingling at the time of eating. Therefore, people constantly chew something, which as a result leads to weight gain, carious damage to the teeth.
The pathognomonic feature of the disease is the absence of tingling at the time of eating. Therefore, people constantly chew something, which as a result leads to weight gain, carious damage to the teeth.
Desquamative glossitis
Periodically during the day, patients experience an unpleasant tingling and burning sensation in the mouth. The tingling spreads over the entire surface of the tongue or in its individual areas that are affected by the inflammatory process. Increased discomfort during eating is characteristic, especially when eating hot or spicy foods. Symptoms bother the patient for several weeks or months.
In desquamative glossitis, in contrast to glossalgia and glossodynia, the appearance of the tongue changes. On its mucosa, bright red foci of inflammation appear with exfoliation of the epithelium, noticeable cracks or furrows form. In places of desquamation, pain and tingling are most pronounced. Wounds heal quickly, then new erosions form elsewhere - a constantly changing "geographical pattern" on the tongue.
Hypovitaminosis B12
Tingling and tingling of the tongue due to atrophy of the papillae and the development of Hunter's glossitis. Discomfort is observed constantly, it is not associated with food or other external factors. With increased vitamin B 12 deficiency and the occurrence of macrocytic anemia, symptoms worsen. Patients complain of constant painful burning sensation, soreness when eating. The tongue becomes bright red, "polished" and shiny.
Oral candidiasis
Tingling of the tongue is characteristic of chronic candidiasis, while in the acute form, severe burning and pain are more likely to bother. The feeling of discomfort extends not only to the back of the tongue, but also to the mucous membrane of the cheeks, the red border of the lips. Patients notice a grayish dense plaque, after peeling off which bright red inflamed areas of the epithelium remain. With the development of chronic atrophic candidiasis, tingling is complemented by severe dryness in the mouth.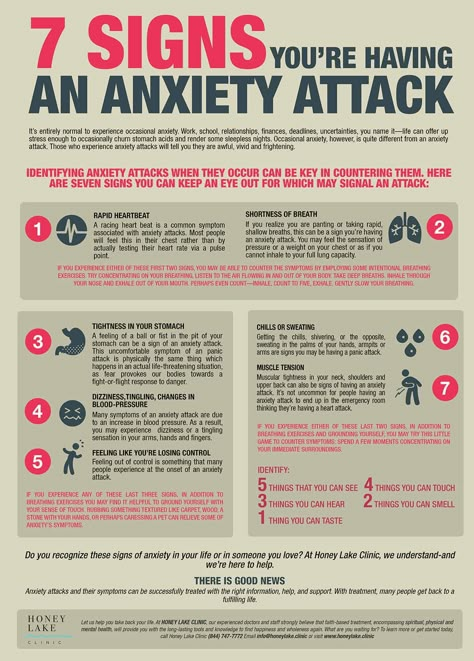
Allergy
Paresthesia on the tongue is one of the signs of a food allergy or reaction to animal hair, pollen. In this case, tingling is combined with excruciating itching, to relieve which patients try to “scratch” the back of the tongue with their teeth, which increases discomfort. Symptoms appear against the background of other allergic manifestations: lacrimation, sneezing, digestive disorders.
Diagnosis
With complaints of tingling of the tongue, first of all, they turn to a dentist, who performs an examination and identifies the most common causes of this condition. If there are no obvious factors, a comprehensive examination is prescribed with the participation of a therapist, a neurologist and other specialists. To detect the etiology of tongue prickling, use:
- Instrumental diagnostics . With dry mouth, ultrasound of the salivary glands and sialography are recommended. To identify diseases of the gastrointestinal tract that cause tingling, EFGDS is performed, an x-ray with oral contrast.
 To determine the zones of paresthesia with glossodynia, electromyography is informative.
To determine the zones of paresthesia with glossodynia, electromyography is informative. - Laboratory testing . In the general blood test, the level of hemoglobin is determined, the presence of macrocytes or megaloblasts, indicating B12 deficiency anemia. Additionally, the content of cyanocobalamin in the blood is examined. For differential diagnosis, saliva analysis is performed with the measurement of the pH value.
- Microbiological analysis . To confirm candidiasis, microscopy of plaque on the tongue is performed, during which pseudomycelium and budding cells are detected. Confirmation of the diagnosis requires inoculation of biomaterial on nutrient media. To exclude syphilitic glossitis, a scraping microscopy is done for pale treponema.
Tongue and mouth exam
Treatment
Pre-diagnosis help
To reduce tingling and burning, doctors recommend diet. All spicy and spicy dishes are excluded from the menu, food should be warm, but not hot. Products are steamed, boiled or stewed so that they are soft and do not injure the surface of the tongue. It is necessary to regularly rinse your mouth with water or a weak solution of chlorhexidine: this helps to get rid of tingling, as well as prevent inflammatory diseases of the oral cavity.
Products are steamed, boiled or stewed so that they are soft and do not injure the surface of the tongue. It is necessary to regularly rinse your mouth with water or a weak solution of chlorhexidine: this helps to get rid of tingling, as well as prevent inflammatory diseases of the oral cavity.
Conservative therapy
Treatment of tingling tongue begins with dental care. The doctor carries out sanitation of the oral cavity, if necessary, changes fillings and improperly selected prostheses. If after this the symptoms do not disappear, treatment of the underlying disease that causes glossalgia is prescribed. Therapeutic schemes are selected by a specialized specialist: a neurologist, an endocrinologist, a gastroenterologist.
Pathogenetic treatment includes drugs that affect the nervous system, which help to reduce painful paresthesias. Herbal sedatives, bromine preparations, "daytime" tranquilizers are effective. For refractory symptoms, injections of B vitamins and trimecaine blockades are used. Local remedies give a quick effect: lubrication of the tongue with anesthesin, pyromecaine, oil solutions (vitamin A, rose hips).
Local remedies give a quick effect: lubrication of the tongue with anesthesin, pyromecaine, oil solutions (vitamin A, rose hips).
Those suffering from desquamative glossitis are often prescribed physiotherapy, which includes drug electrophoresis, ultrasound therapy, SMT therapy. With prolonged glossalgia, reflexology and ozone therapy help to remove tingling. To reduce the intensity of symptoms, laser therapy is used, which has an additional anti-inflammatory effect. Paresthesias of a neurogenic nature require psychotherapy sessions.
Glossary - health articles
11/10/2022
Glossalgia - pain in the area of the tongue without visible changes. Manifested by a burning sensation, tingling, soreness, tingling in the tongue, a feeling of dry mouth, not associated with eating and other irritants. Glossalgia is always secondary to the underlying disease (neurosis, diseases of the gastrointestinal tract, liver, endocrine disorders) or trauma (setting a denture, tooth extraction, oral surgery, etc. ). Eliminating the cause of glossalgia leads to its disappearance.
). Eliminating the cause of glossalgia leads to its disappearance.
Causes
External causes of glossalgia symptoms include trauma to the tongue. You can get such an injury by eating nuts, chips, crackers. Such products are quite easy to scratch the surface of the tongue. It can also be burned with hot drinks, strong alcohol.
Many patients with chronic glossalgia notice that the symptoms appear when they experience stress for a long time, face problems at work or in their personal lives. From this, experts conclude that the disease is psychological in nature. Glossalgia is often noted in people diagnosed with vegetative-vascular dystonia.
There are a number of diseases of the human body systems, accompanied by chronic glossalgia. These include:
- gastrointestinal infections, such as gastritis;
- diabetes mellitus;
- hypothyroidism leading to dysfunction of the thyroid gland;
- advanced stages of syphilis. The disease first affects the skin and mucous membranes, then the internal organs.
 A special form of the disease is neurosyphilis, in which pale treponema affects the components of the human nervous system;
A special form of the disease is neurosyphilis, in which pale treponema affects the components of the human nervous system; - encephalitis of any origin. There are allergic, infectious and other encephalitis. Often the disease is associated with tick bites;
- ischemic heart disease.
It is known that signs of glossalgia are often observed in people with weakened protective functions of the body. Permanent trauma to the tongue with an improperly sized denture, braces, filling or chipped tooth leads to an increase in the symptoms of the disease.
Symptoms
The main symptoms of glossalgia are rawness, tingling, burning sensation in the area of the tongue and oral cavity. These symptoms may be permanent or appear intermittently. It is difficult for patients to talk for a long time. Approximately 30% of patients with glossalgia develop dry mouth. These signs are more pronounced with stress or overwork.
Symptoms of glossalgia may appear periodically at critical moments (public speaking, serious conversation). Interestingly, during meals, manifestations of glossalgia decrease or disappear altogether. This may contribute to the development of bulimia or weight gain in the patient.
Interestingly, during meals, manifestations of glossalgia decrease or disappear altogether. This may contribute to the development of bulimia or weight gain in the patient.
Glossalgia symptoms are most felt at the tip and sides of the tongue. Less often, tingling and burning occurs on the root and back of the tongue. In this case, the localization of pain changes, without a permanent lesion. Sometimes glossalgias disappear without treatment, but then appear elsewhere.
Most patients have no changes in the oral cavity and tongue. Only some of them have swelling of the tongue, coating with plaque, hypertrophic (enlarged) individual papillae of the tongue. In elderly patients with glossalgia, varicose veins of the tongue appear. In the affected areas, pain sensitivity decreases, dystrophic changes in the salivary glands occur, causing a decrease in their secretion.
Diagnosis
Glossalgia must be differentiated from fungal infections of the oral mucosa - candidiasis and leptotrichosis. There are many similarities in the clinical picture of these diseases: dry mouth, burning, discomfort, taste disturbance. Helps in making the correct diagnosis microbiological analysis of scrapings from the tongue: with candidiasis and leptotrichosis, a large amount of candida fungus is sown.
There are many similarities in the clinical picture of these diseases: dry mouth, burning, discomfort, taste disturbance. Helps in making the correct diagnosis microbiological analysis of scrapings from the tongue: with candidiasis and leptotrichosis, a large amount of candida fungus is sown.
It is important to distinguish true glossalgia from galvanic oral syndrome, which occurs in the presence of orthopedic structures made of dissimilar metals. Patients are concerned about a strong burning sensation and a metallic taste.
Treatment
If glossalgia is not treated, it can progress over months or even years, with periodic periods of remission, which after a while will be replaced by exacerbations. Occasionally, glossalgia comes on its own without additional medical intervention.
Initially, after the patient's visit to the doctor, the organization of a complete sanitation of the oral cavity, including prosthetics and treatment of malocclusion, is required.