Borderline personality disorder bpd
NIMH » Borderline Personality Disorder
Overview
Borderline personality disorder is a mental illness that severely impacts a person’s ability to regulate their emotions. This loss of emotional control can increase impulsivity, affect how a person feels about themselves, and negatively impact their relationships with others. Effective treatments are available to manage the symptoms of borderline personality disorder.
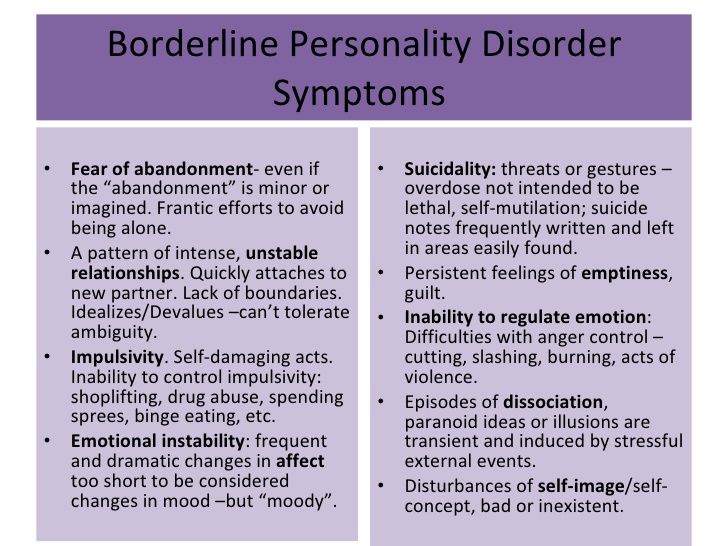
Signs and Symptoms
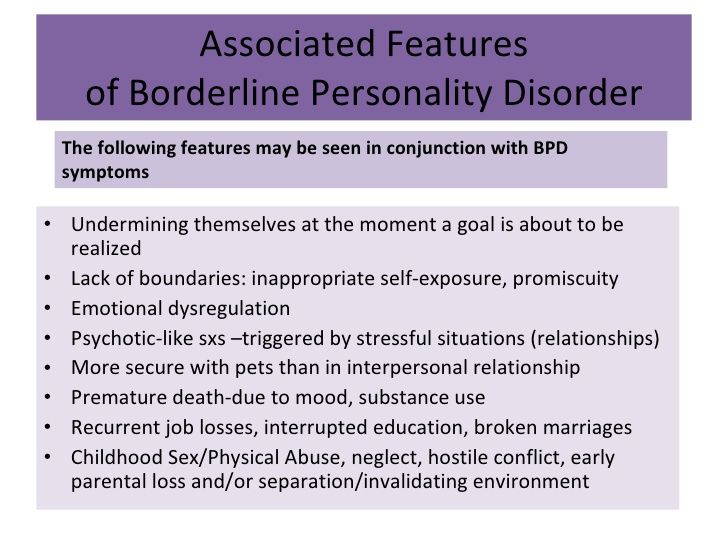
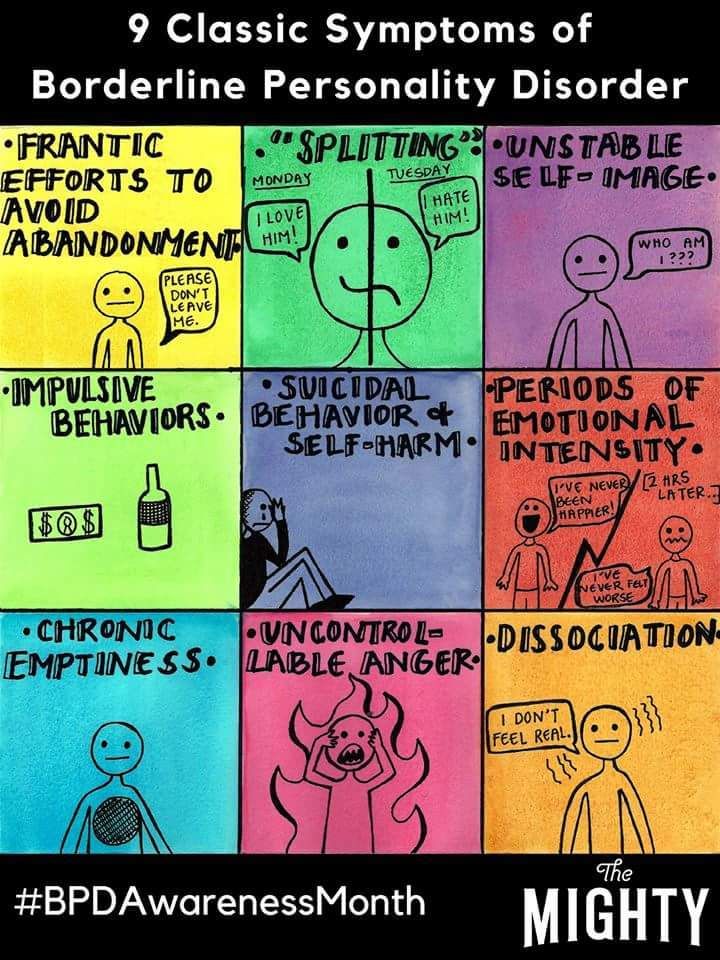
People with borderline personality disorder may experience intense mood swings and feel uncertainty about how they see themselves. Their feelings for others can change quickly, and swing from extreme closeness to extreme dislike. These changing feelings can lead to unstable relationships and emotional pain.
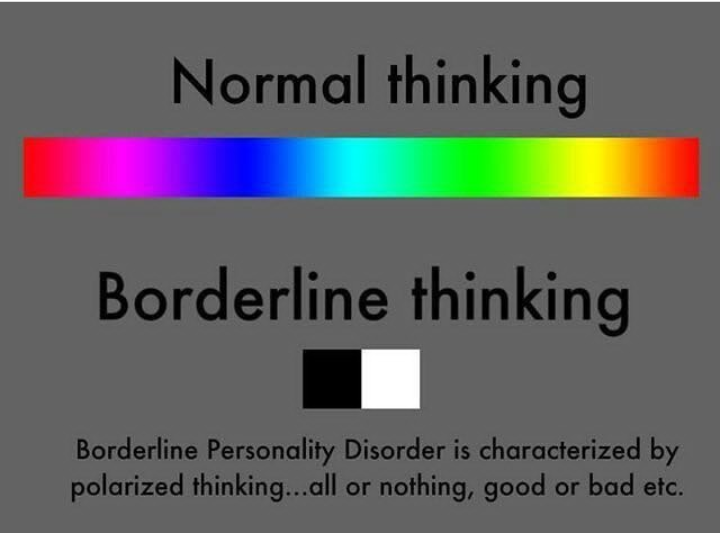
People with borderline personality disorder also tend to view things in extremes, such as all good or all bad. Their interests and values can change quickly, and they may act impulsively or recklessly.
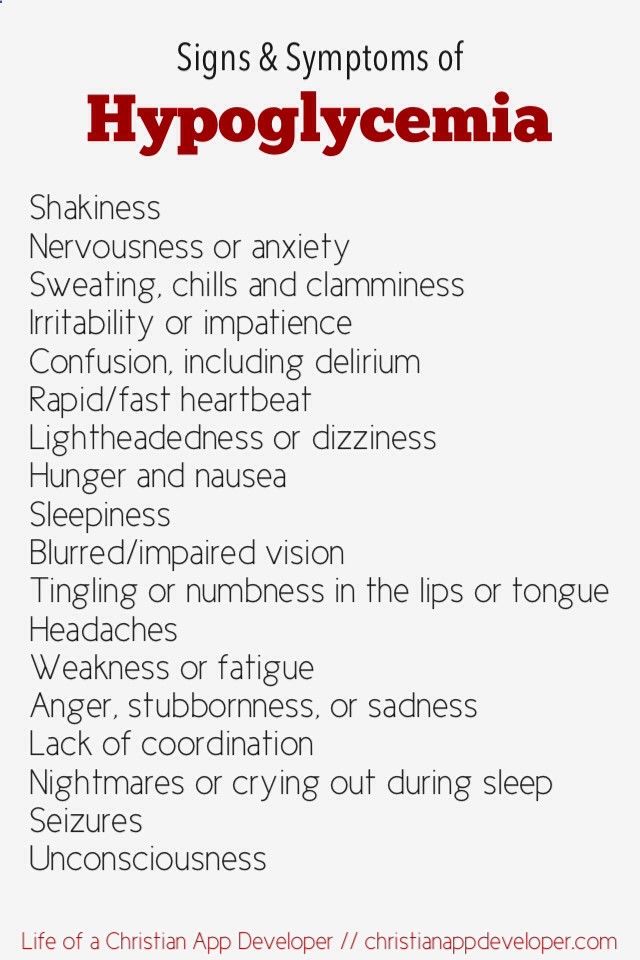
Other signs or symptoms may include:
- Efforts to avoid real or perceived abandonment, such as plunging headfirst into relationships—or ending them just as quickly.
- A pattern of intense and unstable relationships with family, friends, and loved ones.
- A distorted and unstable self-image or sense of self.
- Impulsive and often dangerous behaviors, such as spending sprees, unsafe sex, substance abuse, reckless driving, and binge eating. Please note: If these behaviors happen mostly during times of elevated mood or energy, they may be symptoms of a mood disorder and not borderline personality disorder.
- Self-harming behavior, such as cutting.
- Recurring thoughts of suicidal behaviors or threats.
- Intense and highly variable moods, with episodes lasting from a few hours to a few days.
- Chronic feelings of emptiness.
- Inappropriate, intense anger or problems controlling anger.
- Feelings of dissociation, such as feeling cut off from oneself, observing oneself from outside one’s body, or feelings of unreality.
Not everyone with borderline personality disorder may experience all of these symptoms. The severity, frequency, and duration of symptoms depend on the person and their illness.
People with borderline personality disorder have a significantly higher rate of self-harming and suicidal behavior than the general population.
People with borderline personality disorder who are thinking of harming themselves or attempting suicide need help right away.
If you or someone you know is in immediate distress or is thinking about hurting themselves, call or text the 988 Suicide & Crisis Lifeline at 988 or chat at 988lifeline.org. You can also contact the Crisis Text Line (text HELLO to 741741).
Risk Factors
Researchers aren’t sure what causes borderline personality disorder, but studies suggest that genetic, environmental, and social factors may increase the risk of developing it. These factors may include:
These factors may include:
- Family history: People who have a close family member (such as a parent or sibling) with the illness may be at a higher risk of developing borderline personality disorder.
- Brain structure and function: Research shows that people with borderline personality disorder may have structural and functional changes in the brain, especially in the areas that control impulses and emotion regulation. However, the studies do not demonstrate whether these changes were risk factors for the illness or if such changes were caused by the disorder.
- Environmental, cultural, and social factors: Many people with borderline personality disorder report experiencing traumatic life events, such as abuse, abandonment, or hardship during childhood. Others may have been exposed to unstable, invalidating relationships or conflicts.
Although these factors may increase a person’s risk, it doesn’t mean it is certain that they’ll develop borderline personality disorder.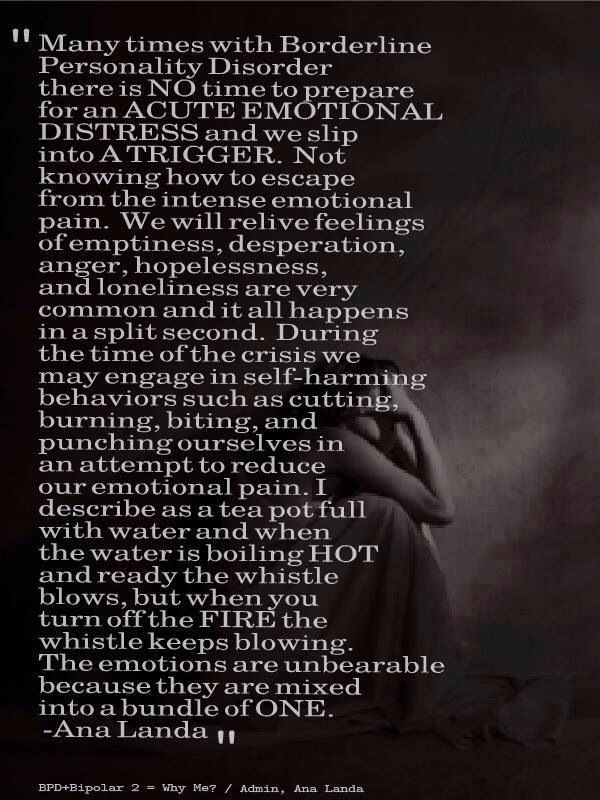 Likewise, people without these risk factors may develop the disorder in their lifetime.
Likewise, people without these risk factors may develop the disorder in their lifetime.
Diagnosis
A licensed mental health professional—such as a psychiatrist, psychologist, or clinical social worker—who is experienced in diagnosing and treating mental disorders can diagnose borderline personality disorder based on a thorough interview and a discussion about symptoms. A careful and thorough medical exam also can help rule out other possible causes of symptoms. In diagnosing the illness, providers will discuss a person’s symptoms and ask about family medical histories, including histories of mental illness.
Borderline personality disorder is usually diagnosed in late adolescence or early adulthood. Occasionally, a person younger than age 18 may be diagnosed with borderline personality disorder if symptoms are significant and last at least a year.
What other illnesses can co-occur with borderline personality disorder?
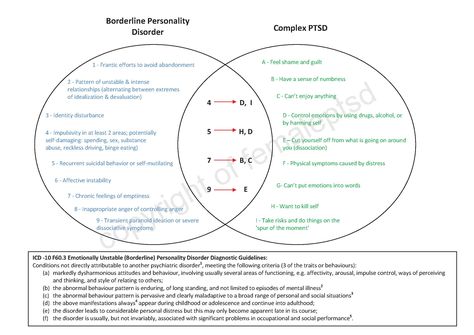
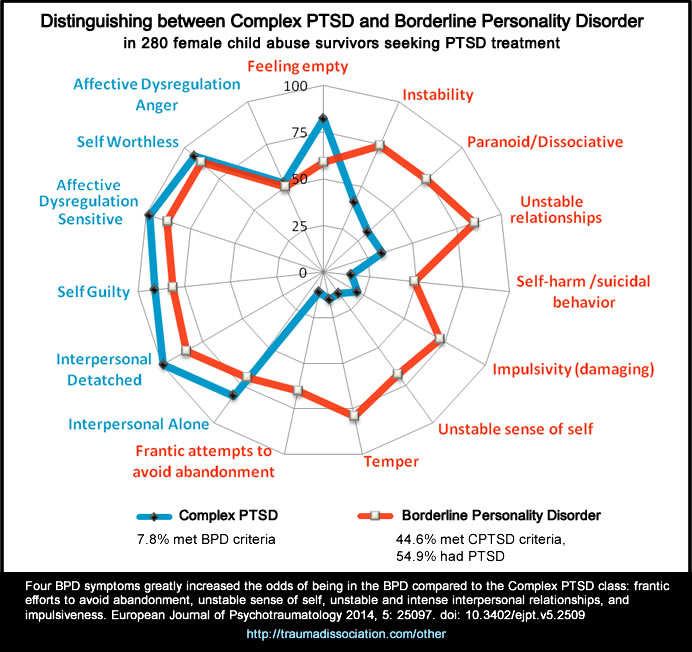
Borderline personality disorder often occurs with other mental illnesses, such as post-traumatic stress disorder (PTSD).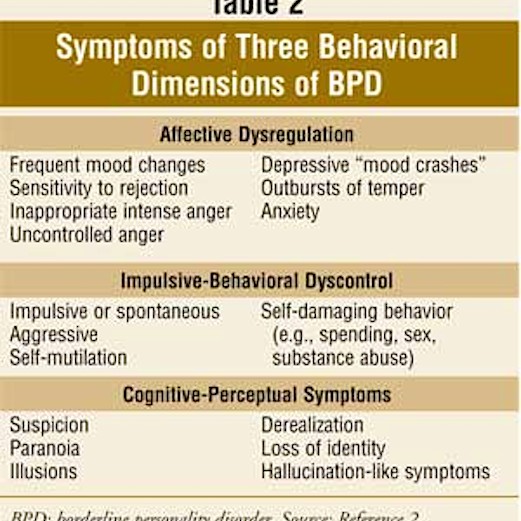 These co-occurring disorders can make it harder to diagnose and treat borderline personality disorder, especially if symptoms of other illnesses overlap with symptoms of the disorder. For example, a person with borderline personality disorder also may be more likely to experience symptoms of major depression, PTSD, bipolar disorder, anxiety disorders, substance abuse, or eating disorders.
These co-occurring disorders can make it harder to diagnose and treat borderline personality disorder, especially if symptoms of other illnesses overlap with symptoms of the disorder. For example, a person with borderline personality disorder also may be more likely to experience symptoms of major depression, PTSD, bipolar disorder, anxiety disorders, substance abuse, or eating disorders.
Treatments and Therapies
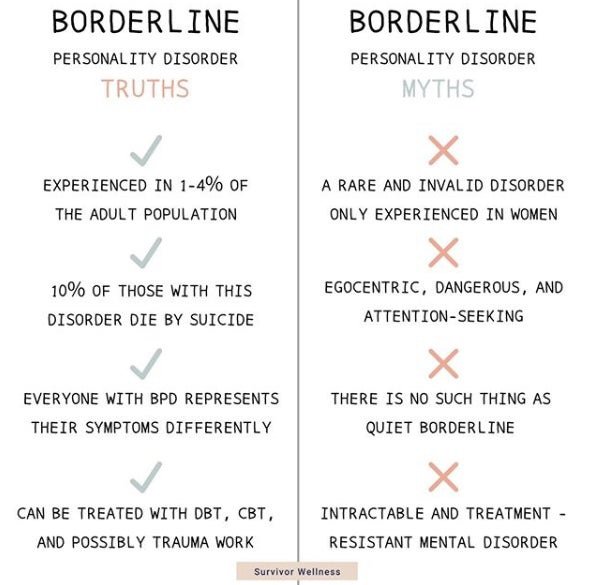
Borderline personality disorder historically has been viewed as challenging to treat. But with newer, evidence-based treatment, many people with this disorder experience fewer and less severe symptoms, improved functioning, and better quality of life. It is important for patients with borderline personality disorder to receive treatment from a licensed mental health professional. Other types of treatment, or treatment from a provider who is not appropriately trained, may be ineffective or dangerous.
Many factors affect the length of time it takes for symptoms to improve once treatment begins.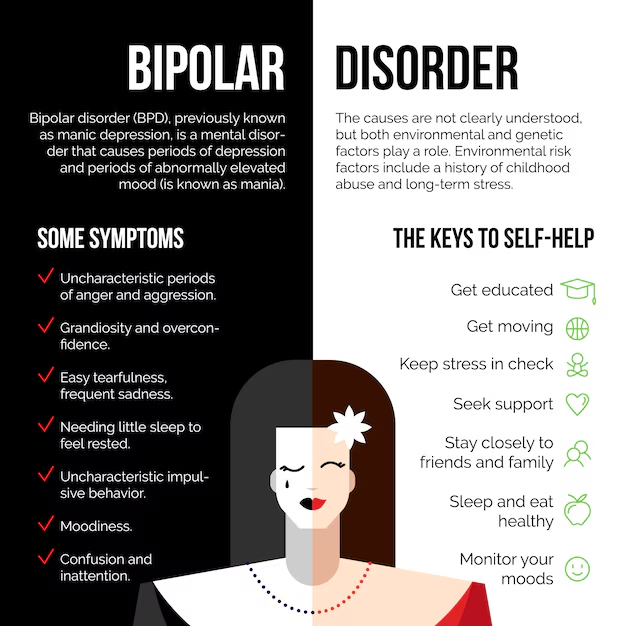 It is important for people with borderline personality disorder and their loved ones to be patient and receive support during treatment.
It is important for people with borderline personality disorder and their loved ones to be patient and receive support during treatment.
Seek—and stick with—treatment.
Studies funded by the National Institute of Mental Health (NIMH) indicate that individuals with borderline personality disorder who don’t receive adequate treatment are more likely to develop other chronic medical or mental illnesses and are less likely to make healthy lifestyle choices.
Psychotherapy
Psychotherapy, sometimes called “talk therapy,” is the first-line treatment for people with borderline personality disorder. Most psychotherapy occurs with a licensed, trained mental health professional in one-on-one sessions or with other individuals in group settings. Group sessions may help teach people with borderline personality disorder to interact with others and express themselves effectively.
Two examples of psychotherapies used to treat borderline personality disorder are:
- Dialectical Behavior Therapy (DBT): This treatment was developed specifically for individuals with borderline personality disorder.
 DBT uses concepts of mindfulness or awareness of one’s present situation and emotional state. DBT also teaches skills to help people control intense emotions, reduce self-destructive behaviors, and improve relationships.
DBT uses concepts of mindfulness or awareness of one’s present situation and emotional state. DBT also teaches skills to help people control intense emotions, reduce self-destructive behaviors, and improve relationships. - Cognitive Behavioral Therapy (CBT): This treatment can help people identify and change core beliefs and behaviors that come from inaccurate perceptions of themselves and others and problems interacting with others. It may help people reduce mood swings and anxiety symptoms and may reduce the number of self-harming or suicidal behaviors.
Read more on NIMH’s Psychotherapies health topic page.
Medications
Because the benefits of prescription medication for borderline personality disorder are unclear, medications aren’t typically used as the primary way to treat the illness. However, in some cases, a psychiatrist may recommend medications to treat specific symptoms or co-occurring mental disorders such as mood swings or depression. Treatment with medications may require coordinated care from more than one medical professional.
Treatment with medications may require coordinated care from more than one medical professional.
Medications also can sometimes cause side effects in some people. Talk to your provider about what to expect from a particular medication. Read more in NIMH’s Mental Health Medications health topic.
Other Elements of Care
Some people with borderline personality disorder experience severe symptoms and need intensive, often inpatient, care. Others may use some outpatient treatments but never need hospitalization or emergency care.
Therapy for Caregivers and Family Members
Having a relative or loved one with the disorder can be stressful, and family members or caregivers may unintentionally act in ways that can worsen their loved one’s symptoms.
Although more research is needed to determine how well family therapy helps with borderline personality disorder, studies on other mental disorders show that including family members can help support a person’s treatment.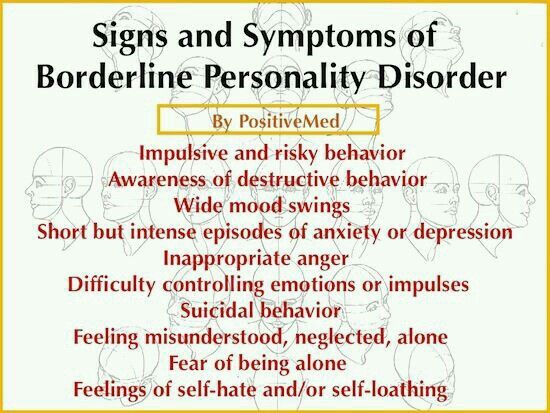 Families and caregivers also can benefit from therapy.
Families and caregivers also can benefit from therapy.
Family therapy helps by:
- Allowing the relative or loved one to develop skills to understand and support a person with borderline personality disorder.
- Focusing on the needs of family members to help them understand the obstacles and strategies for caring for someone with the disorder.
Finding Help
If you’re not sure where to get help, a health care provider can refer you to a licensed mental health professional, such as a psychiatrist or psychologist with experience treating borderline personality disorder. If you need help starting the conversation, check out the Tips for Talking With Your Health Care Provider fact sheet.
Other resources include:
- Substance Abuse and Mental Health Services Administration’s Behavioral Health Treatment Services Locator, a tool for finding mental health services in your area
- NIMH’s Help for Mental Illnesses webpage
- Agency for Healthcare Research and Quality’s website
Tips for Family and Caregivers
Here are some ways to help a friend or relative with the disorder:
- Take time to learn about the illness to understand what your friend or relative is experiencing.
- Offer emotional support, understanding, patience, and encouragement. Change can be difficult and frightening to people with borderline personality disorder, but things can improve over time.
- Encourage your loved one in treatment for borderline personality disorder to ask about family therapy.
- Seek counseling for yourself. Choose a different therapist than the one your relative is seeing.
Join a Study
Clinical trials are research studies that look at new ways to prevent, detect, or treat diseases and conditions. The goal of clinical trials is to determine if a new test or treatment works and is safe. Although individuals may benefit from being part of a clinical trial, participants should be aware that the primary purpose of a clinical trial is to gain new scientific knowledge so that others may be better helped in the future.
Researchers at NIMH and around the country conduct many studies with patients and healthy volunteers. We have new and better treatment options today because of what clinical trials uncovered years ago. Be part of tomorrow’s medical breakthroughs. Talk to your health care provider about clinical trials, their benefits and risks, and whether one is right for you.
We have new and better treatment options today because of what clinical trials uncovered years ago. Be part of tomorrow’s medical breakthroughs. Talk to your health care provider about clinical trials, their benefits and risks, and whether one is right for you.
To learn more or find a study, visit:
- NIMH’s Clinical Trials webpage: Information about participating in clinical trials
- Clinicaltrials.gov: Current Studies on Borderline Personality Disorders: List of clinical trials funded by the National Institutes of Health (NIH) being conducted across the country
Health Hotlines
- 988 Suicide & Crisis Lifeline: The Lifeline provides 24-hour, confidential support to anyone in suicidal crisis or emotional distress. Call or text 988 to connect with a trained crisis counselor. Support is also available via live chat. Para ayuda en español, llame al 988.
- Disaster Distress Hotline: People affected by any disaster or tragedy can call this helpline, sponsored by the Substance Abuse and Mental Health Services Administration, to receive immediate counseling.
 Call or text 1-800-985-5990 to connect with a trained professional from the closest crisis counseling center within the network.
Call or text 1-800-985-5990 to connect with a trained professional from the closest crisis counseling center within the network. - Veterans Crisis Line: This helpline is a free, confidential resource for Veterans of all ages and circumstances. Call 1-800-273-8255, press "1"; text 838255; or chat online to connect with 24/7 support.
- Crisis Text Line: Text HELLO to 741741 for free and confidential support 24 hours a day throughout the U.S.
- More NIH Information Lines
Learn More
Free Brochures and Shareable Resources
- Borderline Personality Disorder: A brochure that offers basic information about borderline personality disorder, including signs and symptoms, treatment, and finding help. Also available en español.
- 5 Action Steps for Helping Someone in Emotional Pain: Infographic presenting five steps for helping someone in emotional pain to prevent suicide.
 Also available en español.
Also available en español. - Suicide in America: Frequently Asked Questions: Fact sheet can help you, or a friend or family member, learn about the signs and symptoms, risk factors and warning signs, and ongoing research about suicide and suicide prevention. Also available en español.
- Warning Signs of Suicide: An infographic presenting behaviors and feelings that may be warnings signs that someone is thinking about suicide. Also available en español.
- Shareable Resources on Borderline Personality Disorder: Help support borderline personality disorder awareness and education in your community. Use these digital resources, including graphics and messages, to spread the word about borderline personality disorder.
Multimedia
- Experts Discuss Borderline Personality Disorder: Learn the signs, symptoms, diagnosis, treatments, and the latest research on borderline personality disorder.
Federal Resources
- Borderline Personality Disorder (MedlinePlus Medical Encyclopedia)
- Introduction to Co-Occurring Borderline Personality Disorder and Substance Use Disorders (Substance Abuse and Mental Health Services Administration)
- Personality Disorders (MedlinePlus - also en español)
Research and Statistics
- Journal Articles: References and abstracts from MEDLINE/PubMed (National Library of Medicine).
- Statistics: Personality Disorders: Webpage listing information on the prevalence of personality disorder among adults.
Last Reviewed: April 2022
Unless otherwise specified, NIMH information and publications are in the public domain and available for use free of charge. Citation of NIMH is appreciated. Please see our Citing NIMH Information and Publications page for more information.
NIMH » Borderline Personality Disorder
What is borderline personality disorder?
Borderline personality disorder is a mental illness that severely impacts a person’s ability to regulate their emotions. This loss of emotional control can increase impulsivity, affect how a person feels about themselves, and negatively impact their relationships with others. Effective treatments are available to manage the symptoms of borderline personality disorder. Learn more about the disorder, how it’s diagnosed, and how to find support.
What are the signs and symptoms?
People with borderline personality disorder may experience intense mood swings and feel uncertainty about how they see themselves. Their feelings for others can change quickly, and swing from extreme closeness to extreme dislike. These changing feelings can lead to unstable relationships and emotional pain.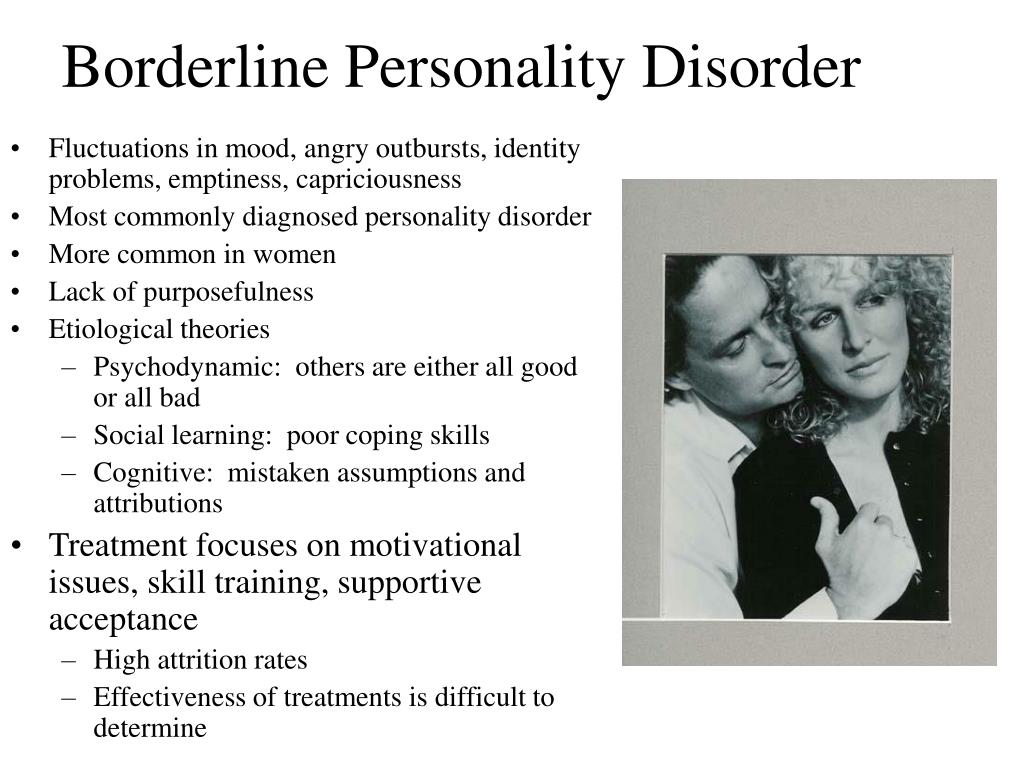
People with borderline personality disorder also tend to view things in extremes, such as all good or all bad. Their interests and values can change quickly, and they may act impulsively or recklessly.
Other signs or symptoms may include:
- Efforts to avoid real or perceived abandonment, such as plunging headfirst into relationships—or ending them just as quickly.
- A pattern of intense and unstable relationships with family, friends, and loved ones.
- A distorted and unstable self-image or sense of self.
- Impulsive and often dangerous behaviors, such as spending sprees, unsafe sex, substance abuse, reckless driving, and binge eating. Please note: If these behaviors happen mostly during times of elevated mood or energy, they may be symptoms of a mood disorder and not borderline personality disorder.
- Self-harming behavior, such as cutting.
- Recurring thoughts of suicidal behaviors or threats.
- Intense and highly variable moods, with episodes lasting from a few hours to a few days.

- Chronic feelings of emptiness.
- Inappropriate, intense anger or problems controlling anger.
- Feelings of dissociation, such as feeling cut off from oneself, observing oneself from outside one’s body, or feelings of unreality.
Not everyone with borderline personality disorder may experience all of these symptoms. The severity, frequency, and duration of symptoms depend on the person and their illness.
People with borderline personality disorder have a significantly higher rate of self-harming and suicidal behavior than the general population.
People with borderline personality disorder who are thinking of harming themselves or attempting suicide need help right away.
If you or someone you know is in immediate distress or is thinking about hurting themselves, call the National Suicide Prevention Lifeline toll-free at 1-800-273-TALK (8255). You also can text the Crisis Text Line (HELLO to 741741) or use the Lifeline Chat on the National Suicide Prevention Lifeline website.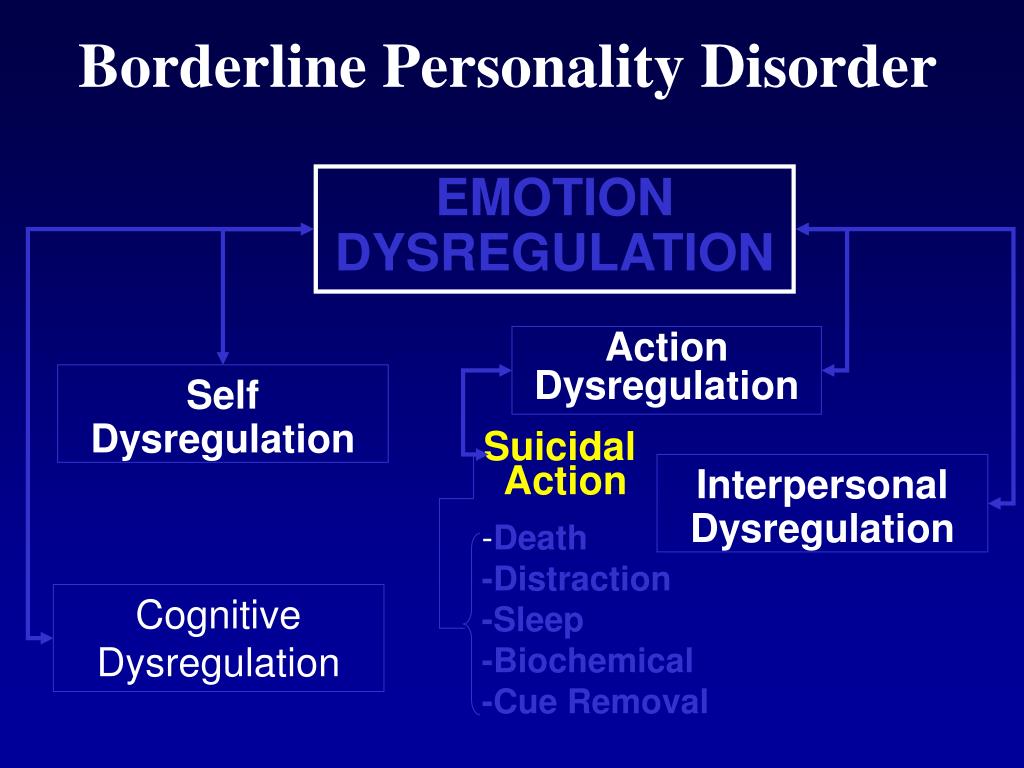
What causes borderline personality disorder?
Researchers aren’t sure what causes borderline personality disorder, but studies suggest that genetic, environmental, and social factors may increase the risk of developing it. These factors may include:
- Family history: People who have a close family member (such as a parent or sibling) with the illness may be at a higher risk of developing borderline personality disorder.
- Brain structure and function: Research shows that people with borderline personality disorder may have structural and functional changes in the brain, especially in the areas that control impulses and emotion regulation. However, the studies do not demonstrate whether these changes were risk factors for the illness or if such changes were caused by the disorder.
- Environmental, cultural, and social factors: Many people with borderline personality disorder report experiencing traumatic life events, such as abuse, abandonment, or hardship during childhood.
 Others may have been exposed to unstable, invalidating relationships or conflicts.
Others may have been exposed to unstable, invalidating relationships or conflicts.
Although these factors may increase a person’s risk, it doesn’t mean it is certain that they’ll develop borderline personality disorder. Likewise, people without these risk factors may develop the disorder in their lifetime.
How is borderline personality disorder diagnosed?
A licensed mental health professional—such as a psychiatrist, psychologist, or clinical social worker—who is experienced in diagnosing and treating mental disorders can diagnose borderline personality disorder based on a thorough interview and a discussion about symptoms. A careful and thorough medical exam also can help rule out other possible causes of symptoms. In diagnosing the illness, providers will discuss a person’s symptoms and ask about family medical histories, including histories of mental illness.
Borderline personality disorder is usually diagnosed in late adolescence or early adulthood. Occasionally, a person younger than age 18 may be diagnosed with borderline personality disorder if symptoms are significant and last at least a year.
Occasionally, a person younger than age 18 may be diagnosed with borderline personality disorder if symptoms are significant and last at least a year.
What other illnesses can co-occur with borderline personality disorder?
Borderline personality disorder often occurs with other mental illnesses, such as post-traumatic stress disorder (PTSD). These co-occurring disorders can make it harder to diagnose and treat borderline personality disorder, especially if symptoms of other illnesses overlap with symptoms of the disorder. For example, a person with borderline personality disorder also may be more likely to experience symptoms of major depression, PTSD, bipolar disorder, anxiety disorders, substance abuse, or eating disorders.
How is borderline personality disorder treated?
Borderline personality disorder historically has been viewed as challenging to treat. But with newer, evidence-based treatment, many people with this disorder experience fewer and less severe symptoms, improved functioning, and better quality of life. It is important for patients with borderline personality disorder to receive treatment from a licensed mental health professional. Other types of treatment, or treatment from a provider who is not appropriately trained, may be ineffective or dangerous.
It is important for patients with borderline personality disorder to receive treatment from a licensed mental health professional. Other types of treatment, or treatment from a provider who is not appropriately trained, may be ineffective or dangerous.
Many factors affect the length of time it takes for symptoms to improve once treatment begins. It is important for people with borderline personality disorder and their loved ones to be patient and receive support during treatment.
It is important to seek—and stick with—treatment.
Studies funded by the National Institute of Mental Health (NIMH) indicate that individuals with borderline personality disorder who don’t receive adequate treatment are more likely to develop other chronic medical or mental illnesses and are less likely to make healthy lifestyle choices.
Psychotherapy
Psychotherapy, sometimes called “talk therapy,” is the first-line treatment for people with borderline personality disorder.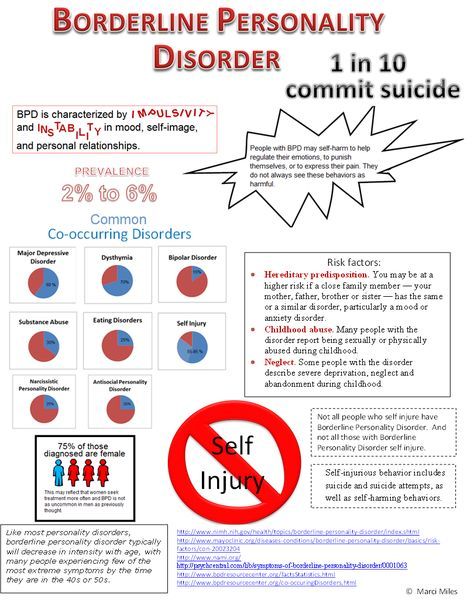 Most psychotherapy occurs with a licensed, trained mental health professional in one-on-one sessions or with other individuals in group settings. Group sessions may help teach people with borderline personality disorder to interact with others and express themselves effectively.
Most psychotherapy occurs with a licensed, trained mental health professional in one-on-one sessions or with other individuals in group settings. Group sessions may help teach people with borderline personality disorder to interact with others and express themselves effectively.
Two examples of psychotherapies used to treat borderline personality disorder are:
- Dialectical Behavior Therapy (DBT): This treatment was developed specifically for individuals with borderline personality disorder. DBT uses concepts of mindfulness or awareness of one’s present situation and emotional state. DBT also teaches skills to help people control intense emotions, reduce self-destructive behaviors, and improve relationships.
- Cognitive Behavioral Therapy (CBT): This treatment can help people identify and change core beliefs and behaviors that come from inaccurate perceptions of themselves and others and problems interacting with others. It may help people reduce mood swings and anxiety symptoms and may reduce the number of self-harming or suicidal behaviors.
Read more on NIMH’s psychotherapies webpage.
Medications
Because the benefits of prescription medication for borderline personality disorder are unclear, medications aren’t typically used as the primary way to treat the illness. However, in some cases, a psychiatrist may recommend medications to treat specific symptoms or co-occurring mental disorders such as mood swings or depression. Treatment with medications may require coordinated care from more than one medical professional.
Medications also can sometimes cause side effects in some people. Talk to your provider about what to expect from a particular medication. Read more on NIMH’s mental health medications webpage.
Where can I find help?
If you’re not sure where to get help, a health care provider can refer you to a licensed mental health professional, such as a psychiatrist or psychologist with experience treating borderline personality disorder. If you need help starting the conversation, check out the Tips for Talking With Your Health Care Provider fact sheet.
If you need help starting the conversation, check out the Tips for Talking With Your Health Care Provider fact sheet.
Other resources include:
- Substance Abuse and Mental Health Services Administration’s Behavioral Health Treatment Services Locator, a tool for finding mental health services in your area
- NIMH’s Help for Mental Illnesses webpage
- Agency for Healthcare Research and Quality’s website
Therapy for Caregivers and Family Members
Having a relative or loved one with the disorder can be stressful, and family members or caregivers may unintentionally act in ways that can worsen their loved one’s symptoms.
Although more research is needed to determine how well family therapy helps with borderline personality disorder, studies on other mental disorders show that including family members can help support a person’s treatment. Families and caregivers also can benefit from therapy.
Family therapy helps by:
- Allowing the relative or loved one to develop skills to understand and support a person with borderline personality disorder.
- Focusing on the needs of family members to help them understand the obstacles and strategies for caring for someone with the disorder.
How can I help a friend or family member with borderline personality disorder?
Here are some ways to help a friend or relative with the disorder:
- Take time to learn about the illness to understand what your friend or relative is experiencing.
- Offer emotional support, understanding, patience, and encouragement. Change can be difficult and frightening to people with borderline personality disorder, but things can improve over time.
- Encourage your loved one in treatment for borderline personality disorder to ask about family therapy.
- Seek counseling for yourself. Choose a different therapist than the one your relative is seeing.
How can I learn more about clinical trials studying borderline personality disorder?
NIMH supports a wide range of research, including clinical trials that look at new ways to prevent, detect, or treat diseases and conditions, including borderline personality disorder.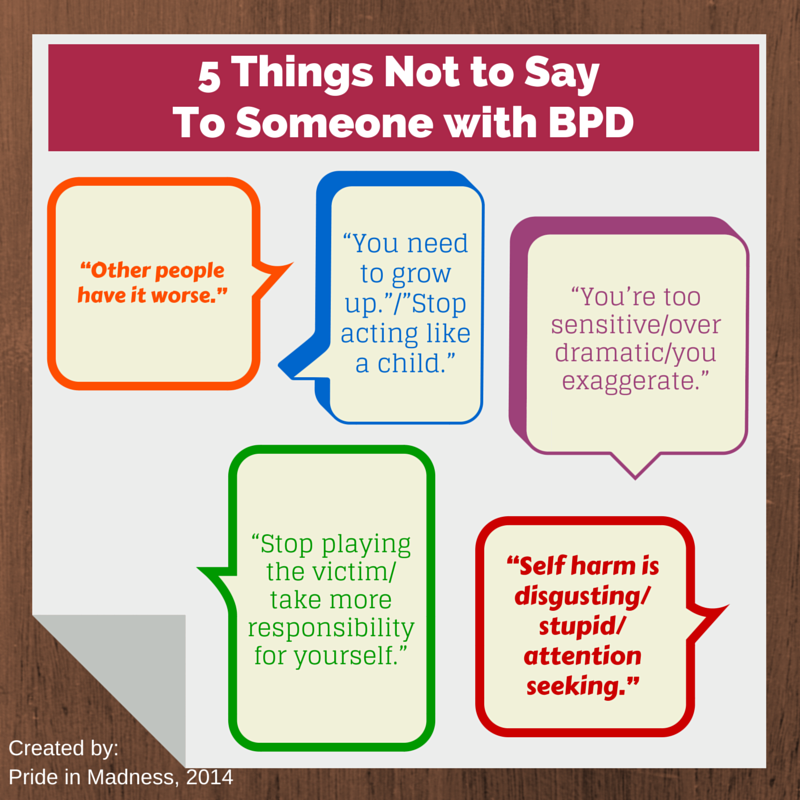 Although individuals may benefit from being part of a clinical trial, participants should be aware that the primary purpose of a clinical trial is to gain new scientific knowledge so that others may be better helped in the future.
Although individuals may benefit from being part of a clinical trial, participants should be aware that the primary purpose of a clinical trial is to gain new scientific knowledge so that others may be better helped in the future.
Researchers at NIMH and around the country conduct clinical trials with patients and healthy volunteers. Talk to a health care provider about clinical trials, their benefits and risks, and whether one is right for you. For more information, visit NIMH’s clinical trials webpage.
Reprints
This publication is in the public domain and may be reproduced or copied without permission from NIMH. We encourage you to reproduce and use NIMH publications in your efforts to improve public health. If you do use our materials, we request that you cite the National Institute of Mental Health. To learn more about using NIMH publications, refer to NIMH's reprint guidelines.
For More Information
Medline Plus (National Library of Medicine) (en español)
ClinicalTrials.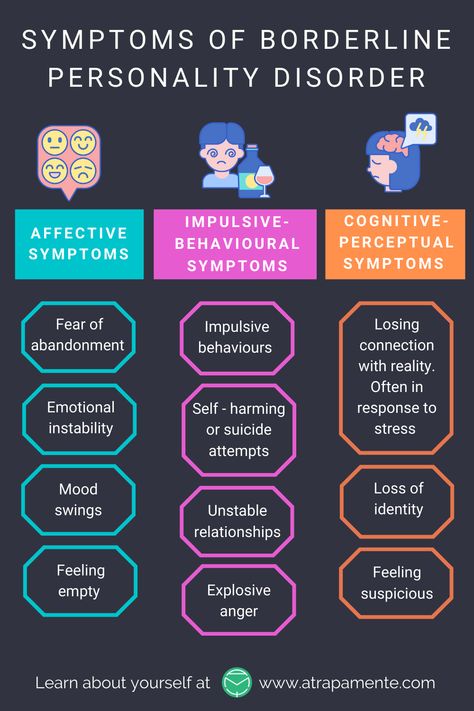 gov (en español)
gov (en español)
U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES
National Institutes of Health
NIH Publication No. 22-MH-4928
Revised 2022
Borderline personality disorder
Borderline personality disorder is associated with unstable mood and behavior that has a significant impact on a person's daily life
Borderline personality disorder is a type of personality disorder in which a person experiences periods of tension, unstable moods and behaviors, and an altered "feeling of self".1 All of these can result in impulsive actions and relationship problems with friends and family members, impairing the person's ability to cope with everyday life. 1.2
Borderline personality disorder is a serious illness associated with self-harm and suicidal attempts. One in ten patients complete suicide. 2
Facts About Borderline Personality Disorder
Borderline personality disorder is a type of personality disorder in which a person experiences periods of tension, unstable mood and behavior, and an altered sense of self. 1
1
One in ten patients complete suicide. 2
Patients with borderline personality disorder are very sensitive to changes in their environment, and may respond inappropriately and acutely to such changes. They may, for example, be afraid of being abandoned by a loved one.2 If the person whom patient
is expecting arrives late, the patient easily changes the feeling of attachment to dislike or anger.1,2 This reflects the extreme perception of the world by the patient, who sees everything and everyone - including oneself – either good or bad.1,2
People with borderline personality disorder are often insecure, may suddenly change their life goals and views on career, life values and friends. .2 They may develop intense unwarranted anger or feelings of emptiness, and are prone to self-harm.2 Patients with borderline personality disorder may also experience depression and anxiety.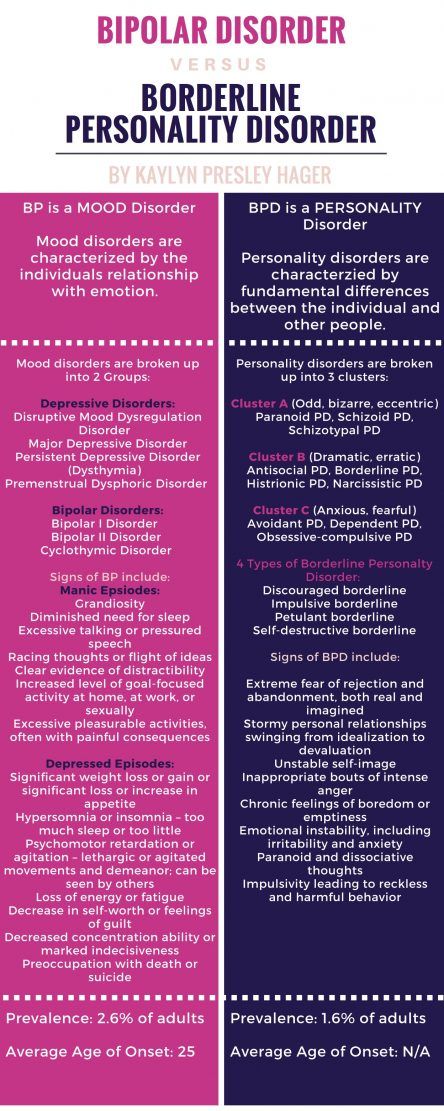 1,2
1,2
Facts about Borderline Personality Disorder
Estimates of the proportion of people who have borderline personality disorder vary from less than 1% to around 6%. 2-4
Borderline personality disorder affects a roughly equal number of men and women, but appears to be more disabling in women the same frequency in men and women, but in women it is more severe.3
Symptoms of borderline personality disorder most often first appear during adolescence.4 The disease is most severe and problematic in young adults and tends to improve with age.2 Symptoms may persist throughout life, but most patients with borderline personality disorder by the age of 30-40 have a stable job and a home.2
People with borderline personality disorder are emotionally and functionally unstable, which places a significant burden on their families.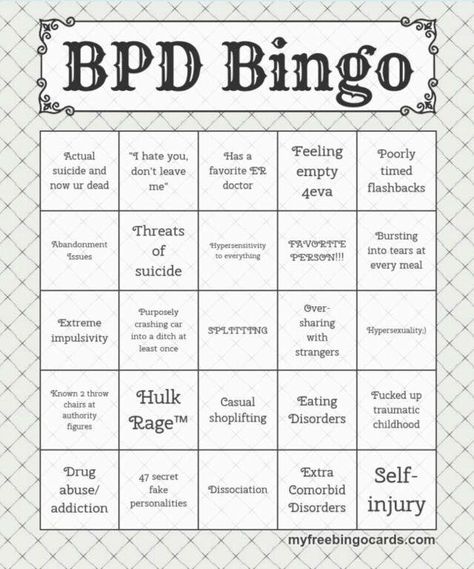 5 Mood swings are a source of stress for both the patient and his/her others, which can lead to the development of mental disorders in the latter.1,5
5 Mood swings are a source of stress for both the patient and his/her others, which can lead to the development of mental disorders in the latter.1,5
People who are concerned that they – or their loved ones – are experiencing symptoms of borderline personality disorder should see their doctor for help and advice.
Borderline personality disorder is diagnosed by a mental health professional using interviews and discussions about symptoms and medical history. 1
Psychotherapy can help people with borderline personality disorder by, for example, teaching them how to interact with others and to express their thoughts and feelings more clearly. 1 It may also be beneficial for caregivers and family members of those affected to receive therapy and guidance on how best to care for a person with borderline personality disorder. 1 There is currently no cure, but one study showed that, after 10 years, 50% of people with borderline personality disorder had recovered, being able to function at work and maintain personal relationships.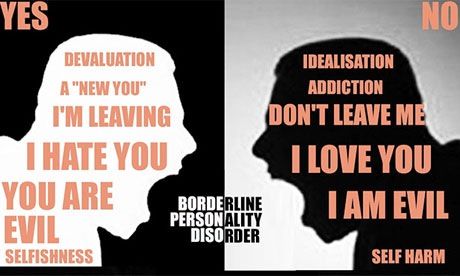 6
6
- National Institute of Mental Health. borderline personality disorder. NIH publication number QF 17-4928. Available from: https://www.nimh.nih.gov/health/publications/borderline-personality-disorder/index.shtml [accessed 30 September 2019].
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013.
- Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2008;69(4):533–545.
- National Institute for Health and Clinical Excellence. Borderline personality disorder: recognition and management. 2009. Available from: https://www.nice.org.uk/guidance/cg78/resources/borderline-personality-disorder-recognition-and-management-pdf-975635141317 [accessed 30 September 2019].
- Bailey RC, Grenyer BFS. Burden and support needs of carers of persons with borderline personality disorder: a systematic review. Harv Rev Psychiatry. 2013;21(5):248–258.
- Zanarini MC, Frankenburg FR, Reich DB, Fitzmaurice G. Time to attainment of recovery from borderline personality disorder and stability of recovery: a 10-year prospective follow-up study. Am J Psychiatry. 2010;167(6):663–667.
1. National Institute of Mental Health. borderline personality disorder. NIH publication number QF 17-4928. Available from: https://www.nimh.nih.gov/health/publications/borderline-personality-disorder/index.shtml [accessed 30 September 2019].
2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013.
3. Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions.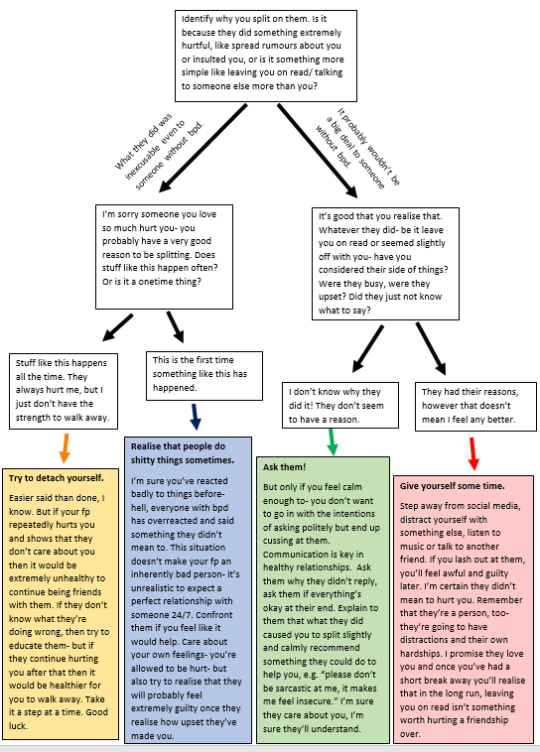 J Clin Psychiatry. 2008;69(4):533–545.
J Clin Psychiatry. 2008;69(4):533–545.
4. National Institute for Health and Clinical Excellence. Borderline personality disorder: recognition and management. 2009. Available from: https://www.nice.org.uk/guidance/cg78/resources/borderline-personality-disorder-recognition-and-management-pdf-975635141317 [accessed 30 September 2019].
Access to Brain Health
We are dedicated to improving access to brain health in accordance with WHO.
Our Science
Lundbeck has developed some of the world’s most widely prescribed therapies.
This is Lundbeck
A specialized pharmaceutical company focused exclusively on brain diseases.
Borderline personality disorder
Olga Vladimirovna Plotnikova
psychiatrist
Borderline personality disorder (hereinafter BPD) is characterized by increased anxiety, impulsive action. All these components greatly affect the quality of life. In addition, antisocial behavior, self-harm and an increased risk of suicide are common in borderline personality disorder.
All these components greatly affect the quality of life. In addition, antisocial behavior, self-harm and an increased risk of suicide are common in borderline personality disorder.
Causes:
Genetics BPD has an evident hereditary factor. It would be more correct to say - predisposition. Like schizophrenia, BPD does not have a single gene that is responsible for the development of the disorder, but the influence of genetics is undeniable.
Neurophysiology or how does it work? Numerous neuroimaging studies (fMRI) have compared patients with BPD and healthy controls. Anomalies were found: a decrease in the level of serotonin, a decrease in the volume of the hippocampus, amygdala and other areas of the medial temporal lobe of the brain. The behavior of patients and their symptoms are a product of the special structure of their brain.
Environmental influences There are a lot of myths here. And, despite the appearance of neuroimaging data, for some reason they are still alive. The most common myth is the influence of childhood trauma on the occurrence of BPD. Indeed, studies of people with BPD show that they have a history of domestic violence, but again, not everyone is without exception. A case of childhood trauma can only provoke and awaken a hereditary predisposition to BPD, but this is not the cause of its development. It's all about the structure of the brain.
And, despite the appearance of neuroimaging data, for some reason they are still alive. The most common myth is the influence of childhood trauma on the occurrence of BPD. Indeed, studies of people with BPD show that they have a history of domestic violence, but again, not everyone is without exception. A case of childhood trauma can only provoke and awaken a hereditary predisposition to BPD, but this is not the cause of its development. It's all about the structure of the brain.
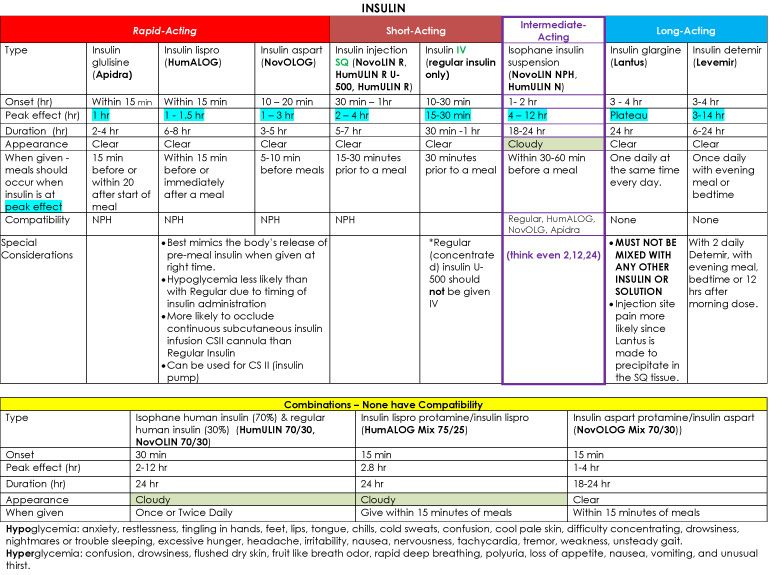
Why is this important? When we talk about diabetes, we don't think that willpower can change insulin levels. BPD is not a whim and cannot be cured by “education”, you need to learn to live with it.
Diagnostic criteria for borderline personality disorder:
- Tendency to make excessive efforts to avoid the real or imagined fate of being abandoned.
- Tendency to engage in intense, tense, and unstable relationships characterized by alternating extremes of idealization and devaluation.
- Identity disorder: marked and persistent instability of the image or feeling of the self.
- Impulsivity in at least two areas that involve self-harm (eg, spending money, substance abuse, traffic violations, habitual overeating).
- Recurrent suicidal behavior, hints or threats of suicide, acts of self-harm.
- Affective instability, very changeable mood (for example, periods of intense irritability or anxiety, usually lasting from several hours to several days).
- Constantly experienced feeling of emptiness.
- Inappropriate manifestations of intense anger or difficulty in controlling anger (eg, frequent irritability.
- Paranoid ideas.
How to treat?
The first line is the psycho-education of the patient and his relatives. This is very important, as it helps to understand what is happening with the patient and outline the tactics of further actions.
Schema therapy patients learn how to respond to their symptoms and then control them.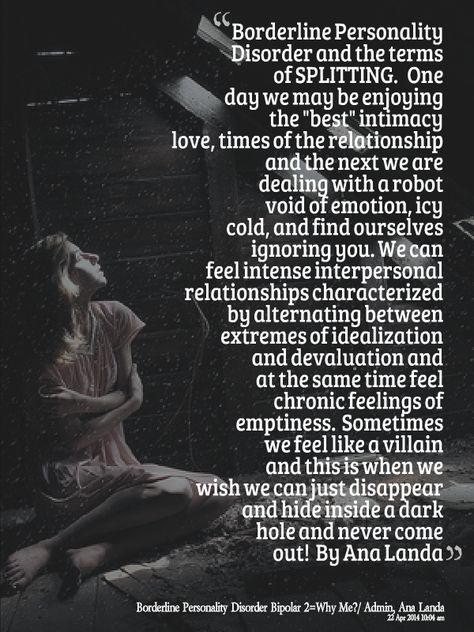
Medication helps to manage the severity of symptoms and gives strength to continue to fight BPD.
Special considerations to consider when choosing therapy
-Second generation antipsychotics should be used in patients with thought disorder, paranoia, identity disorder.
- In patients with mood disorders, outbursts of aggression, mood stabilizers (normotimics) should be used, and not antidepressants.
SUMMARY:
BPD is an anomaly in the structure of the brain, and not a bad upbringing and a complex character.
BPD must be correctly diagnosed using the most up-to-date criteria.
Self-injury is an important, but not the only criterion for diagnosis. Self-cutting in adolescence can be a way to get attention. But! In the presence of self-cuts, one should not scold the teenager, but understand the reasons.
BPD symptoms can be brought into permanent remission and learned to live with.