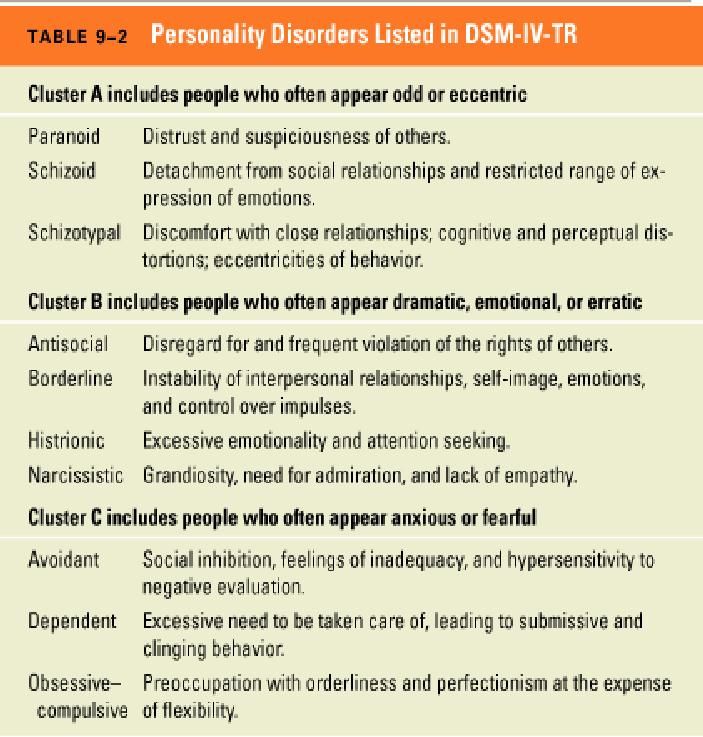
Psychological disorders list and symptoms
Types of mental health issues and illnesses
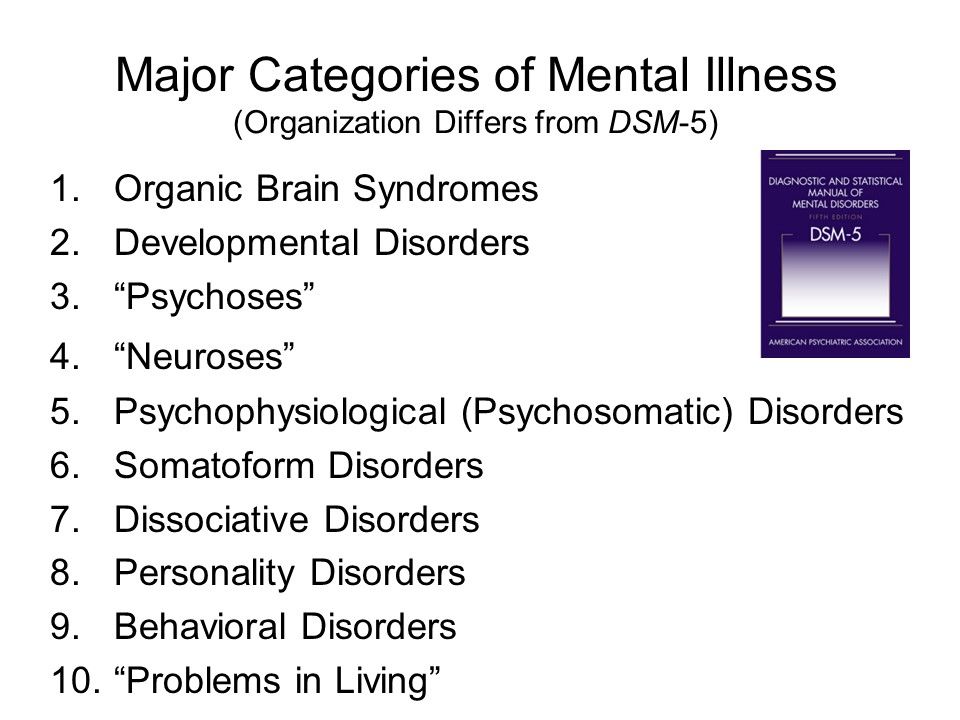
Mental illness is a general term for a group of illnesses that may include symptoms that can affect a person’s thinking, perceptions, mood or behaviour. Mental illness can make it difficult for someone to cope with work, relationships and other demands. The relationship between stress and mental illness is complex, but it is known that stress can worsen an episode of mental illness. Most people can manage their mental illness with medication, counselling or both.This page lists some of the more common mental health issues and mental illnesses.
Anxiety disorders
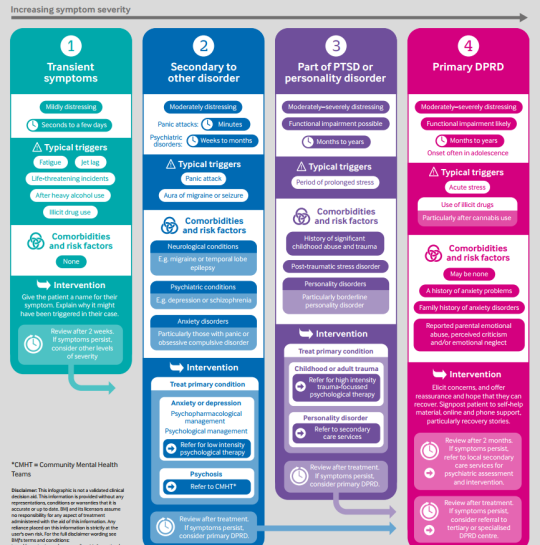
Anxiety disorders is a group of mental health disorders that includes generalised anxiety disorders, social phobias, specific phobias (for example, agoraphobia and claustrophobia), panic disorders, obsessive compulsive disorder (OCD) and post-traumatic stress disorder. Untreated, anxiety disorders can lead to significant impairment on people’s daily lives.
For more information see: Anxiety disorders.
Behavioural and emotional disorders in children
Common behaviour disorders in children include oppositional defiant disorder (ODD), conduct disorder (CD) and attention deficit hyperactivity disorder (ADHD). Treatment for these mental health disorders can include therapy, education and medication.
For more information see: Behavioural disorders in children.
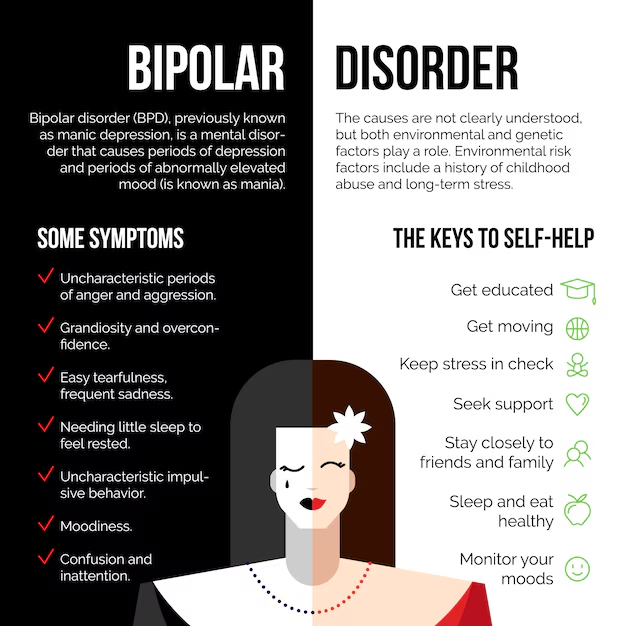
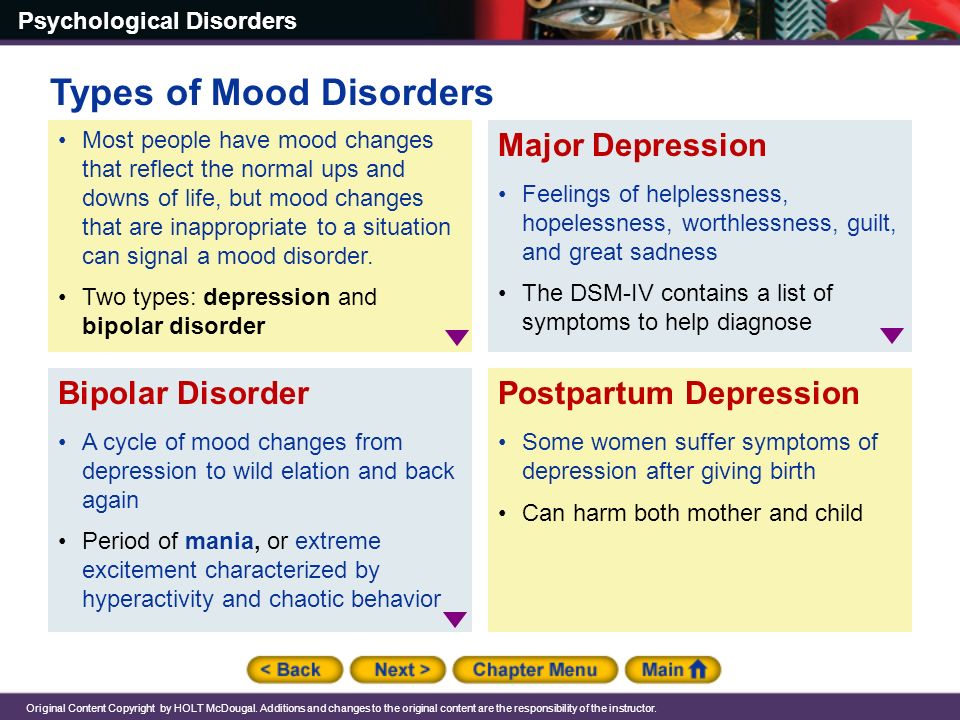
Bipolar affective disorder
Bipolar affective disorder is a type of mood disorder, previously referred to as ‘manic depression’. A person with bipolar disorder experiences episodes of mania (elation) and depression. The person may or may not experience psychotic symptoms. The exact cause is unknown, but a genetic predisposition has been clearly established. Environmental stressors can also trigger episodes of this mental illness.
For more information see: Bipolar disorder.
Depression
Depression is a mood disorder characterised by lowering of mood, loss of interest and enjoyment, and reduced energy.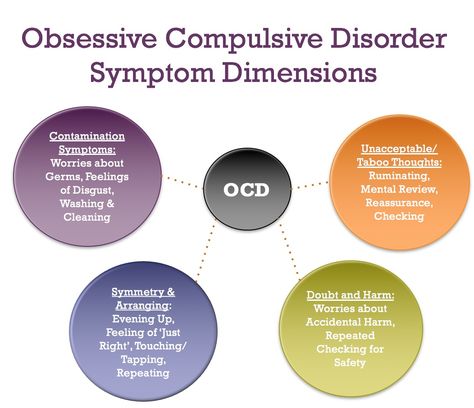 It is not just feeling sad. There are different types and symptoms of depression. There are varying levels of severity and symptoms related to depression. Symptoms of depression can lead to increased risk of suicidal thoughts or behaviours.
It is not just feeling sad. There are different types and symptoms of depression. There are varying levels of severity and symptoms related to depression. Symptoms of depression can lead to increased risk of suicidal thoughts or behaviours.
For more information see: Depression.
Dissociation and dissociative disorders
Dissociation is a mental process where a person disconnects from their thoughts, feelings, memories or sense of identity. Dissociative disorders include dissociative amnesia, dissociative fugue, depersonalisation disorder and dissociative identity disorder.
For more information see: Dissociation and dissociative disorders.
Eating disorders
Eating disorders include anorexia, bulimia nervosa and other binge eating disorders. Eating disorders affect females and males and can have serious psychological and physical consequences.
For more information see: Eating disorders.
Obsessive compulsive disorder
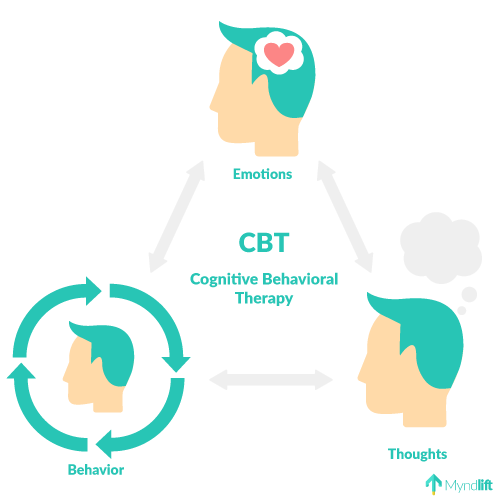
Obsessive compulsive disorder (OCD) is an anxiety disorder. Obsessions are recurrent thoughts, images or impulses that are intrusive and unwanted. Compulsions are time-consuming and distressing repetitive rituals. Treatments include cognitive behaviour therapy (CBT), and medications.
Obsessions are recurrent thoughts, images or impulses that are intrusive and unwanted. Compulsions are time-consuming and distressing repetitive rituals. Treatments include cognitive behaviour therapy (CBT), and medications.
For more information see: Obsessive compulsive disorder.
Paranoia
Paranoia is the irrational and persistent feeling that people are ‘out to get you’. Paranoia may be a symptom of conditions including paranoid personality disorder, delusional (paranoid) disorder and schizophrenia. Treatment for paranoiainclude medications and psychological support.
For more information see: Paranoia.
Post-traumatic stress disorder
Post-traumatic stress disorder (PTSD) is a mental health condition that can develop as a response to people who have experienced any traumatic event. This can be a car or other serious accident, physical or sexual assault, war-related events or torture, or natural disasters such as bushfires or floods.
For more information see: Post-traumatic stress disorder.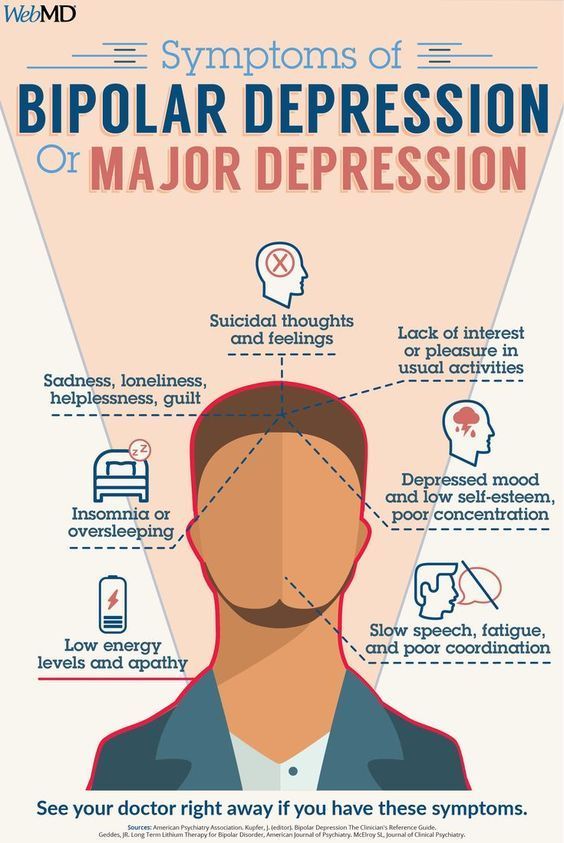
Psychosis
People affected by psychosis can experience delusions, hallucinations and confused thinking.. Psychosis can occur in a number of mental illnesses, including drug-induced psychosis, schizophrenia and mood disorders. Medication and psychological support can relieve, or even eliminate, psychotic symptoms.
For more information see: Psychosis.
Schizophrenia
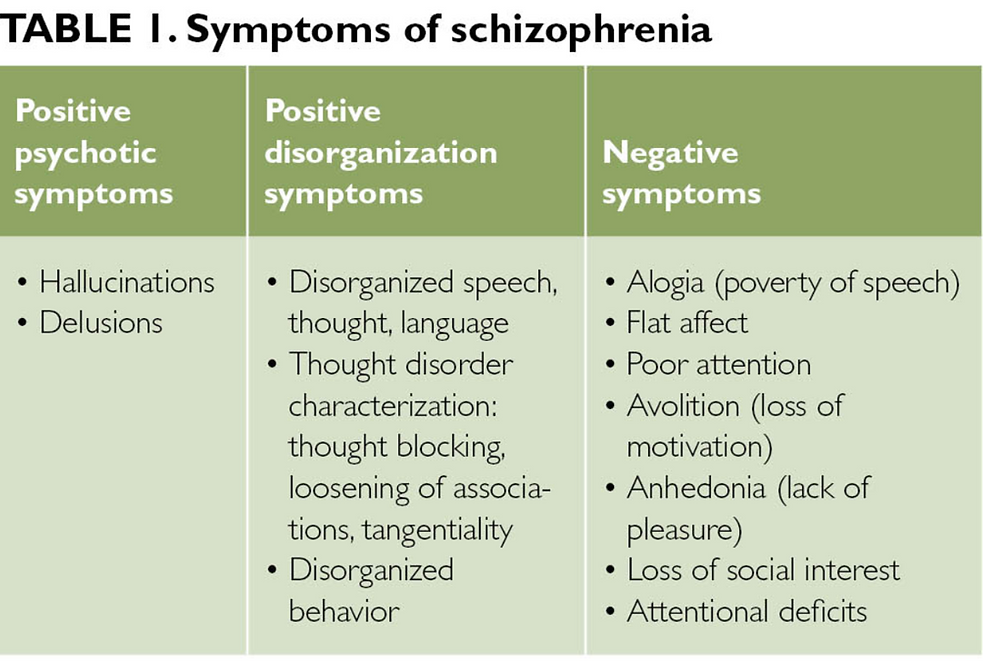
Schizophrenia is a complex psychotic disorder characterised by disruptions to thinking and emotions, and a distorted perception of reality. Symptoms of schizophrenia vary widely but may include hallucinations, delusions, thought disorder, social withdrawal, lack of motivation and impaired thinking and memory. People with schizophrenia have a high risk of suicide. Schizophrenia is not a split personality.
For more information see: Schizophrenia.
Where to get help
- Your GP (doctor)
- Mental health services
Mental illness - Symptoms and causes
Overview
Mental illness, also called mental health disorders, refers to a wide range of mental health conditions — disorders that affect your mood, thinking and behavior. Examples of mental illness include depression, anxiety disorders, schizophrenia, eating disorders and addictive behaviors.
Examples of mental illness include depression, anxiety disorders, schizophrenia, eating disorders and addictive behaviors.
Many people have mental health concerns from time to time. But a mental health concern becomes a mental illness when ongoing signs and symptoms cause frequent stress and affect your ability to function.
A mental illness can make you miserable and can cause problems in your daily life, such as at school or work or in relationships. In most cases, symptoms can be managed with a combination of medications and talk therapy (psychotherapy).
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms
Signs and symptoms of mental illness can vary, depending on the disorder, circumstances and other factors. Mental illness symptoms can affect emotions, thoughts and behaviors.
Examples of signs and symptoms include:
- Feeling sad or down
- Confused thinking or reduced ability to concentrate
- Excessive fears or worries, or extreme feelings of guilt
- Extreme mood changes of highs and lows
- Withdrawal from friends and activities
- Significant tiredness, low energy or problems sleeping
- Detachment from reality (delusions), paranoia or hallucinations
- Inability to cope with daily problems or stress
- Trouble understanding and relating to situations and to people
- Problems with alcohol or drug use
- Major changes in eating habits
- Sex drive changes
- Excessive anger, hostility or violence
- Suicidal thinking
Sometimes symptoms of a mental health disorder appear as physical problems, such as stomach pain, back pain, headaches, or other unexplained aches and pains.
When to see a doctor
If you have any signs or symptoms of a mental illness, see your primary care provider or a mental health professional. Most mental illnesses don't improve on their own, and if untreated, a mental illness may get worse over time and cause serious problems.
If you have suicidal thoughts
Suicidal thoughts and behavior are common with some mental illnesses. If you think you may hurt yourself or attempt suicide, get help right away:
- Call 911 or your local emergency number immediately.
- Call your mental health specialist.
- Contact a suicide hotline. In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline, available 24 hours a day, seven days a week. Or use the Lifeline Chat. Services are free and confidential.
- Seek help from your primary care provider.
- Reach out to a close friend or loved one.
- Contact a minister, spiritual leader or someone else in your faith community.
Suicidal thinking doesn't get better on its own — so get help.
Helping a loved one
If your loved one shows signs of mental illness, have an open and honest discussion with him or her about your concerns. You may not be able to force someone to get professional care, but you can offer encouragement and support. You can also help your loved one find a qualified mental health professional and make an appointment. You may even be able to go along to the appointment.
If your loved one has done self-harm or is considering doing so, take the person to the hospital or call for emergency help.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you. If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices. You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Causes
Mental illnesses, in general, are thought to be caused by a variety of genetic and environmental factors:
- Inherited traits. Mental illness is more common in people whose blood relatives also have a mental illness. Certain genes may increase your risk of developing a mental illness, and your life situation may trigger it.
- Environmental exposures before birth.
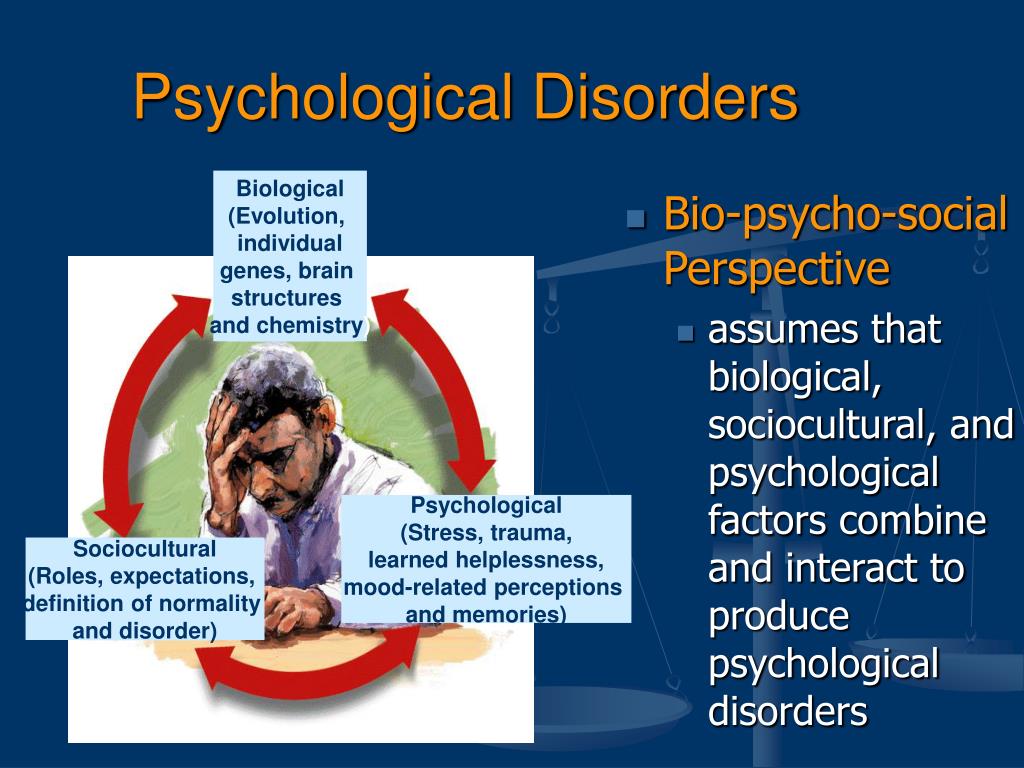 Exposure to environmental stressors, inflammatory conditions, toxins, alcohol or drugs while in the womb can sometimes be linked to mental illness.
Exposure to environmental stressors, inflammatory conditions, toxins, alcohol or drugs while in the womb can sometimes be linked to mental illness. - Brain chemistry. Neurotransmitters are naturally occurring brain chemicals that carry signals to other parts of your brain and body. When the neural networks involving these chemicals are impaired, the function of nerve receptors and nerve systems change, leading to depression and other emotional disorders.
Risk factors
Certain factors may increase your risk of developing a mental illness, including:
- A history of mental illness in a blood relative, such as a parent or sibling
- Stressful life situations, such as financial problems, a loved one's death or a divorce
- An ongoing (chronic) medical condition, such as diabetes
- Brain damage as a result of a serious injury (traumatic brain injury), such as a violent blow to the head
- Traumatic experiences, such as military combat or assault
- Use of alcohol or recreational drugs
- A childhood history of abuse or neglect
- Few friends or few healthy relationships
- A previous mental illness
Mental illness is common.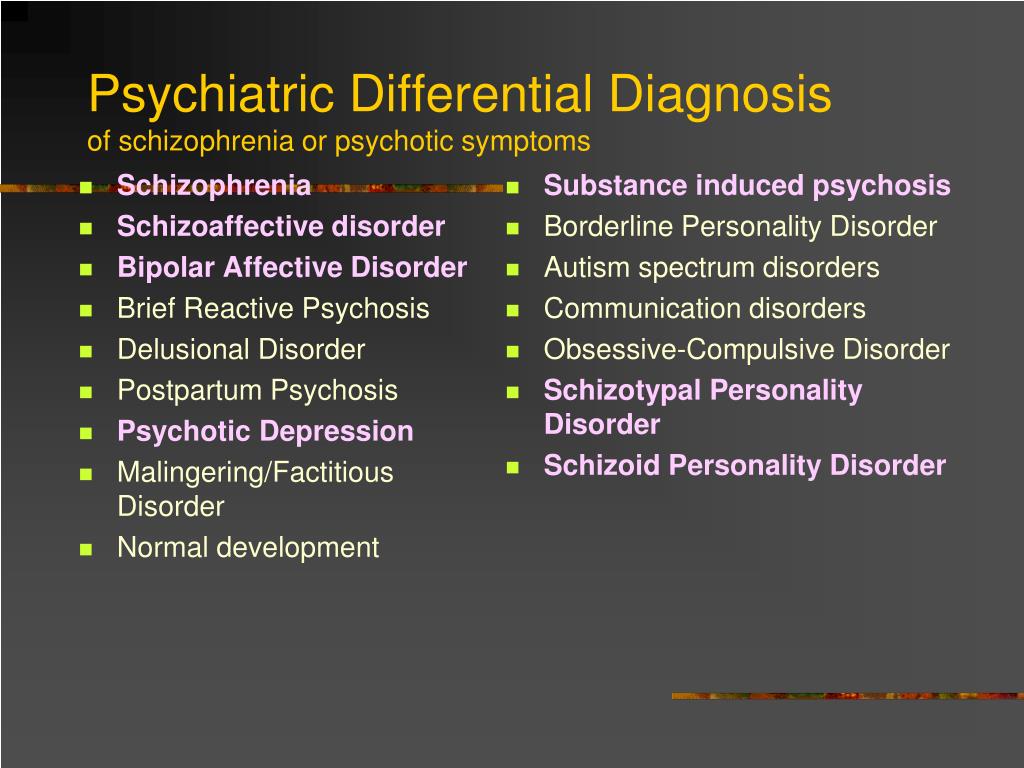 About 1 in 5 adults has a mental illness in any given year. Mental illness can begin at any age, from childhood through later adult years, but most cases begin earlier in life.
About 1 in 5 adults has a mental illness in any given year. Mental illness can begin at any age, from childhood through later adult years, but most cases begin earlier in life.
The effects of mental illness can be temporary or long lasting. You also can have more than one mental health disorder at the same time. For example, you may have depression and a substance use disorder.
Complications
Mental illness is a leading cause of disability. Untreated mental illness can cause severe emotional, behavioral and physical health problems. Complications sometimes linked to mental illness include:
- Unhappiness and decreased enjoyment of life
- Family conflicts
- Relationship difficulties
- Social isolation
- Problems with tobacco, alcohol and other drugs
- Missed work or school, or other problems related to work or school
- Legal and financial problems
- Poverty and homelessness
- Self-harm and harm to others, including suicide or homicide
- Weakened immune system, so your body has a hard time resisting infections
- Heart disease and other medical conditions
Prevention
There's no sure way to prevent mental illness. However, if you have a mental illness, taking steps to control stress, to increase your resilience and to boost low self-esteem may help keep your symptoms under control. Follow these steps:
However, if you have a mental illness, taking steps to control stress, to increase your resilience and to boost low self-esteem may help keep your symptoms under control. Follow these steps:
- Pay attention to warning signs. Work with your doctor or therapist to learn what might trigger your symptoms. Make a plan so that you know what to do if symptoms return. Contact your doctor or therapist if you notice any changes in symptoms or how you feel. Consider involving family members or friends to watch for warning signs.
- Get routine medical care. Don't neglect checkups or skip visits to your primary care provider, especially if you aren't feeling well. You may have a new health problem that needs to be treated, or you may be experiencing side effects of medication.
- Get help when you need it. Mental health conditions can be harder to treat if you wait until symptoms get bad. Long-term maintenance treatment also may help prevent a relapse of symptoms.
- Take good care of yourself. Sufficient sleep, healthy eating and regular physical activity are important. Try to maintain a regular schedule. Talk to your primary care provider if you have trouble sleeping or if you have questions about diet and physical activity.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Schizophrenia
Schizophrenia- Healthcare issues »
- A
- B
- B
- G
- D
- E
- and
- 9000 About
- P
- P
- With
- T
- in
- F
- x
- 9 h
- K.
- S
- B
- E
- S
- I
- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Data and statistics »
- Newsletter
- The facts are clear
- Publications
- Find country »
- A
- B
- C
- g
- D
- E
- and
- th
- K
- L
- 9000 N
- 9000
- in
- Ф
- x
- C hours
- Sh
- Sh.
- K
- E 9000 WHO in countries »
- Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A nine0005
- Developments
- Photo reports
- Questions and answers
- Update
- Emergencies "
- News "
- Disease Outbreak News
- WHO Data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Highlights " nine0005
- About WHO »
- General director
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center /
- Newsletters/
- Read more/ nine0004 Schizophrenia
Key Facts
- Schizophrenia is a severe mental disorder that affects approximately 24 million people, or 1 in 300 people worldwide.
- Schizophrenia causes psychosis, is associated with severe disability, and can negatively affect all areas of life, including personal, family, social, academic and work life.
- People with schizophrenia are often subject to stigma, discrimination and human rights violations. nine0286
- Worldwide, more than two thirds of people with psychosis do not receive specialized mental health care.
- There are a number of effective care options for patients with schizophrenia that can lead to a complete recovery of at least one in three patients.
Symptoms
Schizophrenia is characterized by significant disturbances in perception of reality and behavioral changes such as:
- persistent delusions: the patient has a persistent belief in the truth of certain things, despite evidence to the contrary;
- persistent hallucinations: the patient hears, sees, touches non-existent things and smells non-existent smells;
- feeling of external influence, control or passivity: the presence in the patient of the feeling that his feelings, impulses, actions or thoughts are dictated from outside, put in or disappear from consciousness at the will of others, or that his thoughts are broadcast to others; nine0005
- disorganized thinking, often expressed in incoherent or pointless speech;
- Significant disorganization of behavior, which is manifested, for example, by the patient performing actions that may seem strange or meaningless, or in an unpredictable or inappropriate emotional reaction that does not give the patient the opportunity to organization of their behavior;
- "negative symptoms" such as extreme poverty of speech, smoothness of emotional reactions, inability to feel interest or pleasure, social autism; and/or
- Extreme agitation or, on the contrary, slowness of movements, freezing in unusual postures.

People with schizophrenia often also experience persistent cognitive or thinking problems that affect memory, attention, or problem-solving skills.
At least one third of patients with schizophrenia experience complete remission of symptoms (1). In some, periods of remission and exacerbation of symptoms follow each other throughout life, in others there is a gradual increase in symptoms. nine0322
Scope and impact
Schizophrenia affects approximately 24 million people, or 1 in 300 people (0.32%) worldwide. Among adults, the rate is 1 in 222 (0.45%) (2). Schizophrenia is less common than many other mental disorders. Onset is most common in late adolescence and between the ages of 20 and 30; while women tend to have a later onset of the disease. nine0322
Schizophrenia is often accompanied by significant stress and difficulties in personal relationships, family life, social contacts, studies, work or other important areas of life.
Individuals with schizophrenia are 2-3 times more likely to die early than the population average (2).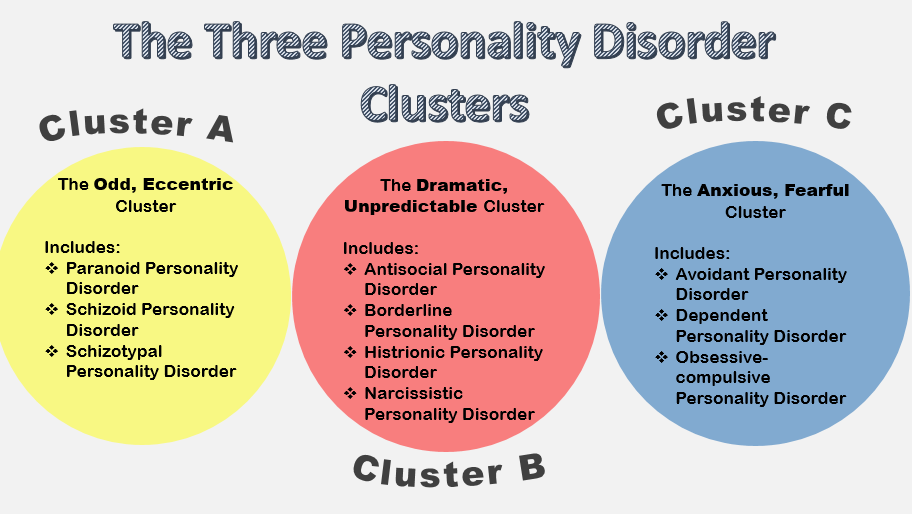 It is often associated with physical illnesses such as cardiovascular disease, metabolic disease, and infectious disease.
It is often associated with physical illnesses such as cardiovascular disease, metabolic disease, and infectious disease.
Patients with schizophrenia often become the object of human rights violations both within the walls of psychiatric institutions and in everyday life. Significant stigmatization of people with this disease is a widespread phenomenon that leads to their social isolation and has a negative impact on their relationships with others, including family and friends. This creates grounds for discrimination, which in turn limits access to health services in general, education, housing and employment. nine0322
Humanitarian emergencies and health crises can cause intense stress and fear, disrupt social support mechanisms, lead to isolation and disruption of health services and supply of medicines. All these shocks can have a negative impact on the lives of people with schizophrenia, in particular by exacerbating existing symptoms of the disease. People with schizophrenia are more vulnerable during emergencies to various human rights violations and, in particular, face neglect, abandonment, homelessness, abuse and social exclusion. nine0322
nine0322
Causes of schizophrenia
Science has not established any one cause of the disease. It is believed that schizophrenia may be the result of the interaction of a number of genetic and environmental factors. Psychosocial factors may also influence the onset and course of schizophrenia. In particular, heavy marijuana abuse is associated with an increased risk of this mental disorder.
Assistance services
At present, the vast majority of people with schizophrenia do not receive mental health care worldwide. Approximately 50% of patients in psychiatric hospitals are diagnosed with schizophrenia (4). Only 31.3% of people with psychosis get specialized mental health care (5). Much of the resources allocated to mental health services are inefficiently spent on the care of patients admitted to psychiatric hospitals.
Available scientific evidence clearly indicates that hospitalization in psychiatric hospitals is not an effective treatment for mental disorders and is regularly associated with the violation of the basic rights of patients with schizophrenia. Therefore, it is necessary to ensure the expansion and acceleration of work on the transfer of functions in the field of mental health care from psychiatric institutions to the level of local communities. Such work should begin with the organization of the provision a wide range of quality community-based mental health services. Options for community-based mental health care include integrating this type of care into primary health care and hospital care. general care, setting up community mental health centres, outpatient care centres, social housing with nursing care and social home care services. Involvement in the care process is essential the patient with schizophrenia, his family members and members of local communities. nine0322
Therefore, it is necessary to ensure the expansion and acceleration of work on the transfer of functions in the field of mental health care from psychiatric institutions to the level of local communities. Such work should begin with the organization of the provision a wide range of quality community-based mental health services. Options for community-based mental health care include integrating this type of care into primary health care and hospital care. general care, setting up community mental health centres, outpatient care centres, social housing with nursing care and social home care services. Involvement in the care process is essential the patient with schizophrenia, his family members and members of local communities. nine0322
Schizophrenia management and care
There are a number of effective approaches to treating people with schizophrenia, including medication, psychoeducation, family therapy, cognitive behavioral therapy, and psychosocial rehabilitation (eg, life skills education).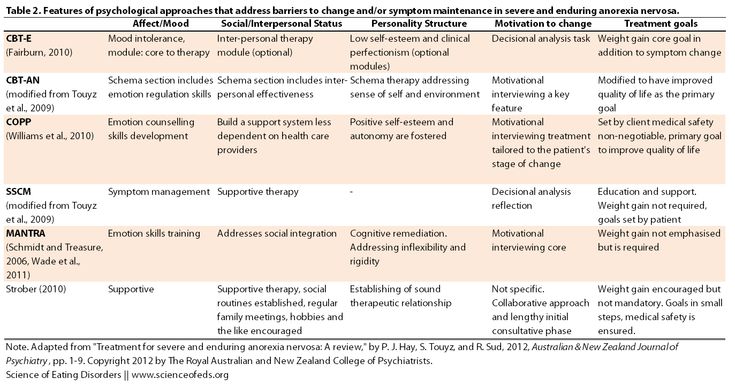 The most important interventions for helping people with schizophrenia are assisted living, special housing and employment assistance. It is extremely important for people with schizophrenia and their families and/or caregivers to a recovery-centered approach that empowers people to participate in decisions about their care. nine0322
The most important interventions for helping people with schizophrenia are assisted living, special housing and employment assistance. It is extremely important for people with schizophrenia and their families and/or caregivers to a recovery-centered approach that empowers people to participate in decisions about their care. nine0322
WHO action
steps are in place to ensure that appropriate services are provided to people with mental disorders, including schizophrenia. One of the key recommendations The action plan is to transfer the function of providing assistance from institutions to local communities. WHO Special Mental Health Initiative aims to further progress towards the goals of the Comprehensive Plan mental health action 2013–2030 by ensuring that 100 million more people have access to quality and affordable mental health care. nine0322
The WHO Mental Health Gap Action Program (mhGAP) is working to develop evidence-based technical guidelines, tools and training packages to scale up services in countries, especially in low-resource settings.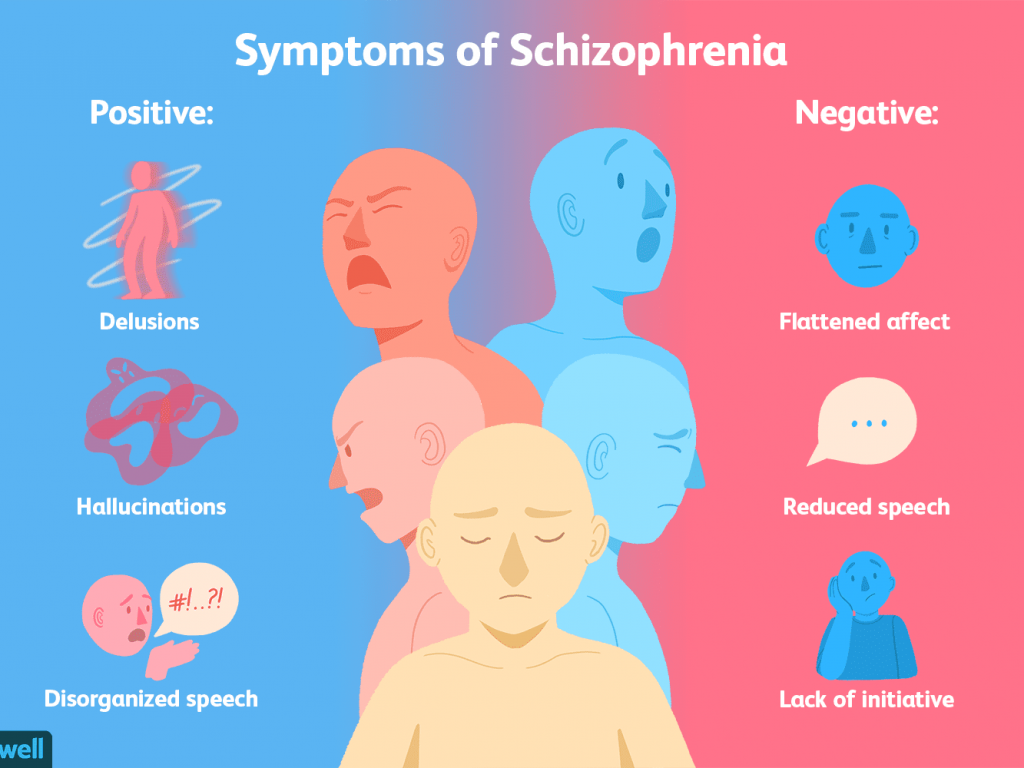 The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in as part of an integrated approach to mental health care at all levels of care. To date, the mhGAP Program has been implemented in more than 100 WHO Member States. nine0322
The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in as part of an integrated approach to mental health care at all levels of care. To date, the mhGAP Program has been implemented in more than 100 WHO Member States. nine0322
The WHO QualityRights project aims to improve the quality of care and better protect human rights in mental health and social care settings and to expand opportunities of various organizations and associations to defend the rights of persons with mental disorders and psychosocial disabilities.
The WHO guidelines on community mental health services and human rights-based approaches provide information for all stakeholders who intend to develop or transform mental health systems and services. health in accordance with international human rights standards, including the UN Convention on the Rights of Persons with Disabilities. nine0322
Bibliography
(1) Harrison G, Hopper K, Craig T, Laska E, Siegel C, Wanderling J.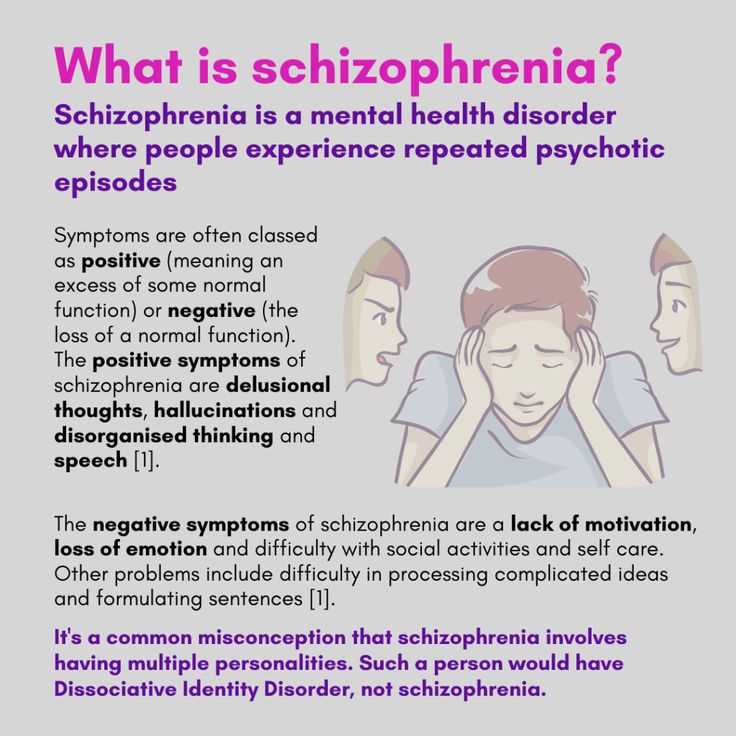 Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry 2001;178:506-17.
Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry 2001;178:506-17.
(2) Institute of Health Metrics and Evaluation (IHME). Global Health Data Exchange (GHDx). http://ghdx.healthdata.org/gbd-results-tool?params=gbd-api-2019-permalink/27a7644e8ad28e739382d31e77589dd7 (accessed 25 September 2021)
(3) LaursenTM, Nordentoft M, Mortensen PB. Excess early mortality in schizophrenia. Annual Review of Clinical Psychology , 2014;10, 425-438.
(4) WHO. Mental health systems in selected low- and middle-income countries: a WHO-AIMS cross-national analysis. WHO: Geneva, 2009
(5) Jaeschke K et al. Global estimates of service coverage for severe mental disorders: findings from the WHO Mental Health Atlas 2017 Glob Ment Health 2021;8:e27.
Autism
Autism- Healthcare issues »
- A
- B
- B
- G
- D
- E
- and
- 9000 O
- M
- R
- S
- T
- Y
- F
- X
- C
- W
- B
- S
- B
- E
- S
- I
4 SC
- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Data and statistics »
- Newsletter
- The facts are clear
- Publications
- Find a country »
- A
- B
- in
- g
- D
- E
- С
- and
- L
- m
- N
- P
- Since
- T
- in
- x
- hours
- Sh
- 9000 WHO in countries » nine0003
- Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A nine0005
- Developments
- Photo reports
- Questions and answers
- Update
- Emergencies "
- News "
- Disease Outbreak News
- WHO Data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Highlights " nine0005
- About WHO »
- General director
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center /
- Newsletters/
- Read more/ nine0004 Autism
Key Facts
- Autism, also called autism spectrum disorder, is a diverse group of pathological conditions caused by the development of the brain.
- Signs of autism can be detected in early childhood, but often it is not diagnosed until later in life.
- Approximately 1 in 100 children have autism.
- The abilities and needs of people with autism can vary and change over time. Some people with autism are able to lead independent and productive lives, while others become severely disabled and require lifelong care and support.
- Evidence-based psychosocial interventions can improve communication skills and social behavior that positively impact the well-being and quality of life of people with autism and their caregivers. nine0286
- Care for people with autism must be accompanied by local and community action to make physical and social environments and relationships more accessible, inclusive and supportive.
Introduction
Autism Spectrum Disorders (ASD) are a group of different conditions.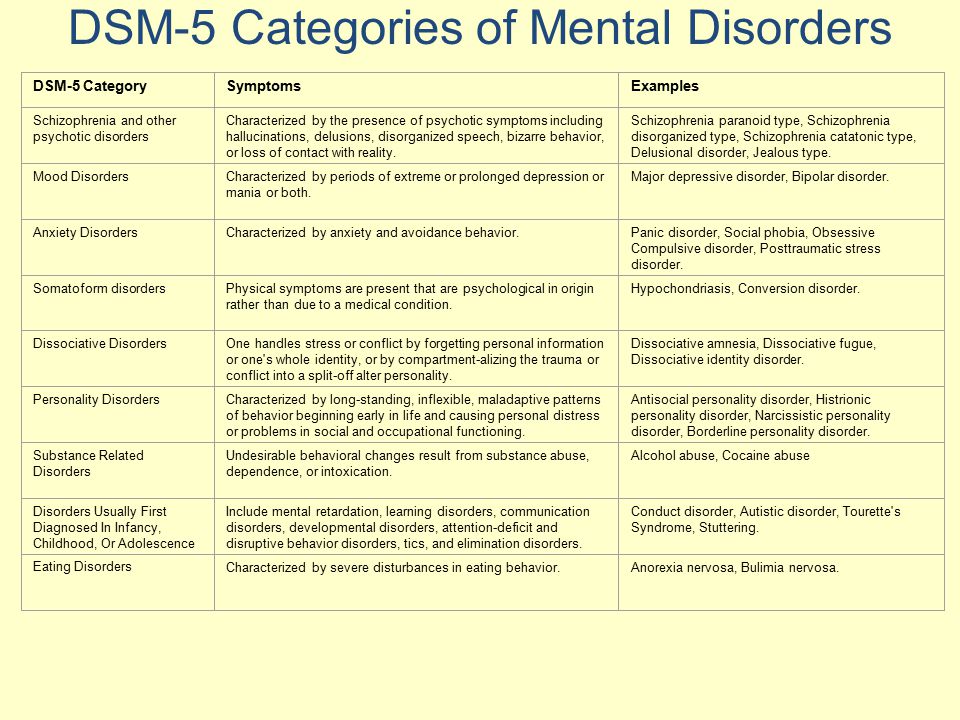 All of them are characterized by certain difficulties with social interaction and communication. Other features include atypical patterns of action and behaviors, such as difficulty moving from one activity to another, focus on details, and unusual responses to external stimuli. nine0322
All of them are characterized by certain difficulties with social interaction and communication. Other features include atypical patterns of action and behaviors, such as difficulty moving from one activity to another, focus on details, and unusual responses to external stimuli. nine0322
The abilities and needs of people with autism can vary and change over time. Some people with autism are able to live independent and productive lives, while others become severely disabled and require lifelong care and support. Autism often negatively affects educational or employment opportunities. In addition, for family members of people with autism, care and support responsibilities can often be a source of significant stress. Community attitudes and the level of support from local and national governments are important determinants of the quality of life of people with autism. nine0322
Signs of autism can be identified in early childhood, but the condition is often diagnosed at much later stages.
People with autism often have comorbid conditions and illnesses, including epilepsy, depression, anxiety, and attention deficit hyperactivity disorder, as well as behavioral problems such as sleep disturbances or self-harm. The level of intellectual abilities of people with autism varies in a wide range from severe cognitive impairment to a high level of intelligence. nine0322
Epidemiology
Worldwide, autism is estimated to affect about 1 in 100 children (1). At the same time, we are talking about an average indicator, and the prevalence rates of autism recorded according to different studies vary widely. Nevertheless, according to some reputable controlled studies, the real numbers are much higher. The prevalence of autism in many low- and middle-income countries is unknown.
Causes
Available scientific evidence indicates many factors that may increase the likelihood of children developing autism, including environmental and genetic factors.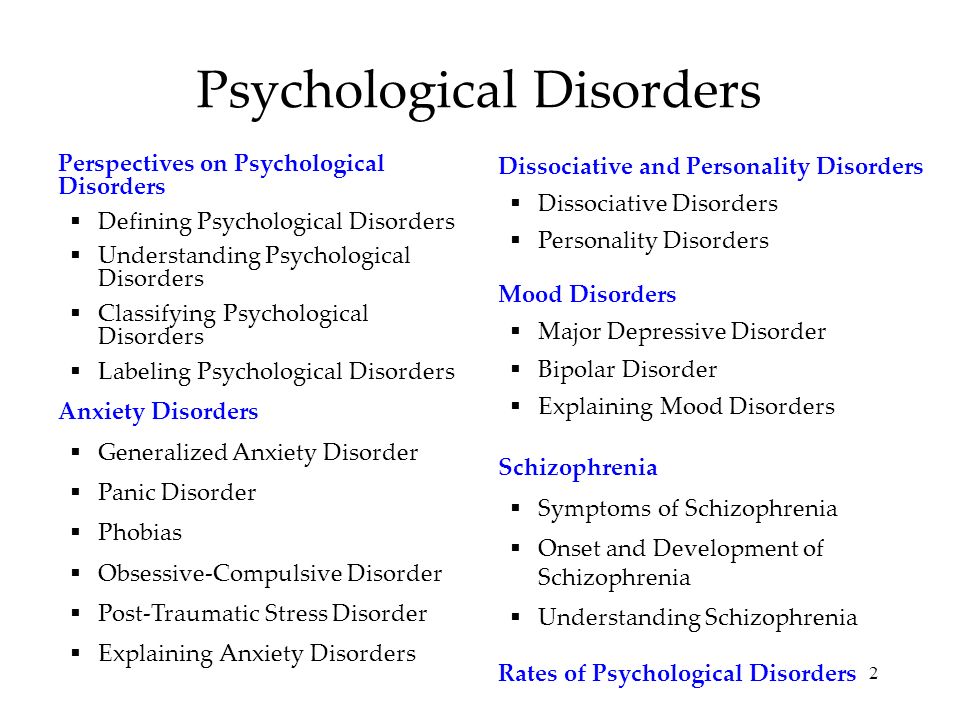
Available epidemiological data do not establish a causal relationship between autism and measles, mumps and rubella vaccination. Past studies suggesting such a causal relationship have been many methodological problems were found (2), (3). nine0322
Similarly, there is no evidence that any childhood vaccine can increase the risk of developing autism. Evidence reviews on a potential association between the preservative thiomersal and aluminum adjuvants contained in inactivated vaccines and the risk of developing autism strongly suggest that vaccines do not lead to an increase in this risk.
Needs Assessment and Care Management
A range of interventions, from early childhood and throughout life, can contribute to the optimal development, well-being and quality of life of people with autism. Timely evidence-based psychosocial interventions at an early age can improve the ability of children with autism to communicate and interact effectively with others. It is recommended to monitor the development of children as part of the planned provision of medical care to mothers and children. nine0322
It is recommended to monitor the development of children as part of the planned provision of medical care to mothers and children. nine0322
It is important that immediately after diagnosis, children, adolescents and adults diagnosed with autism and their caregivers have access to relevant information, referrals and practical support tailored to their individual needs. constantly changing needs and preferences.
The health care needs of people with autism are complex and therefore they require comprehensive services, including health promotion, care and rehabilitation services. Therefore, it is important to ensure cooperation with other sectors, in particular with the education system, employment and the social sector. nine0322
Interventions to help people with autism and other developmental disabilities should be planned and implemented with the participation of people with these conditions themselves. Caring for people with autism should be accompanied by local action. and at the level of society as a whole, in order to make the physical and social environment and relationships more accessible, inclusive and supportive.
and at the level of society as a whole, in order to make the physical and social environment and relationships more accessible, inclusive and supportive.
Human rights
All people, including those with autism, have the right to the highest attainable standard of physical and mental health. nine0322
Yet people with autism often face stigma and discrimination: their health care and education rights are unfairly denied, and their opportunities to participate in society are limited.
People with autism may experience the same health problems as the rest of the population. In addition, they may have special health care needs related to autism and other related conditions. They can be are more vulnerable to chronic noncommunicable diseases associated with behavioral risk factors such as physical inactivity and poor diet, and are at greater risk of violence, injury and abuse. nine0322
People with autism, like the rest of the population, need affordable health services to meet general health needs, including health promotion and prevention services, as well as acute and chronic care. However less than in the general population, the level of satisfaction of the medical needs of people with autism is at a lower level. These people are also more vulnerable in humanitarian emergencies. One of the common barriers is the insufficient level of knowledge and understanding of the specifics of autism by medical professionals. nine0322
However less than in the general population, the level of satisfaction of the medical needs of people with autism is at a lower level. These people are also more vulnerable in humanitarian emergencies. One of the common barriers is the insufficient level of knowledge and understanding of the specifics of autism by medical professionals. nine0322
WHO Resolution on Autism Spectrum Disorders
In May 2014, the Sixty-seventh World Health Assembly adopted a resolution on "Comprehensive and concerted efforts for the management of autism spectrum disorders", supported by over 60 countries.
The resolution calls on WHO to work with Member States and partner agencies to strengthen national capacity to address ASD and other developmental disabilities. nine0322
WHO activities
WHO and partners recognize the need to strengthen countries' capacity to promote the optimal health and well-being of all people with autism.
The main activities of WHO in this regard are:
- promoting the adoption of targeted measures by national governments to improve the quality of life of people with autism;
- develop recommendations for policies and action plans to address autism in the broader context of physical, mental, brain health and care for people with disabilities; nine0005
- help to empower healthcare professionals to provide appropriate and effective care for people with autism and achieve optimal health and well-being; and
- promote and support an inclusive and supportive environment for people with autism and other developmental disabilities.

WHO comprehensive mental health action plan 2013–2030 and World Health Assembly Resolution WHA73.10 "Global action against epilepsy and other neurological disorders" contain calling on countries to address significant gaps in the early detection, care, treatment and rehabilitation of people with mental and neurodevelopmental disorders, including and autism. The resolution also calls on countries to take action to meet the social, economic, educational and other needs of people living with mental and neurological disorders and their families, and to develop surveillance and related research activities. nine0322
References
(1) Global prevalence of autism: A systematic review update. Zeidan J et al. Autism Research 2022 March.
(2) Wakefield's affair: 12 years of uncertainty whereas no link between autism and MMR vaccine has been proven. Maisonneuve H, Floret D. Presse Med. 2012 Sep; French https://pubmed.