Periods mood swings boyfriend
5 ways to handle your girlfriend's PMS (you're welcome)
Those mood swings just before her period hits aren't exactly the best time of the month, for her or for you. But before you guys end up fighting (yet again), here's what you can do instead...
Picture courtesy: YouTube
By Somya Abrol: Your girlfriend's PMS (Premenstrual Syndrome, for the uninitiated) can easily turn into the worst phase of your relationship, EVERY month. But don't you dare go around complaining about those mood swings now, because you know what's coming if you do--"Oh, you think you're suffering? Try going through this pain every freakin' month, and have a horrible partner who doesn't understand you, and then we'll see who's suffering!"
advertisement
So, since we're such nice human beings--who are basically aiming at world peace--we'll tell you just what kinds of PMS women are likely to have, and exactly how to handle them mood swings #LikeAPro.
1. The 'will cry at anything' type
Even the picture of a pretty flower. Yes, anything can bring her to tears. ANYthing--babies, puppies, trees, your face. Honestly though, it's not her fault, and she sure as hell can't help it.
Solution: Try to keep your #ToughLove in check. In fact, eliminate it altogether. If you've been with her for a bit, you already know by now just what ticks her off about you. So, please, for a couple of days, dial it down--the world won't come to an end.
If she does end up crying in front of you, do what you'd do with anyone who's crying--a big, warm hug. Caution: This might make her cry even more, but at least she doesn't hate you right now!
2. 'Too blah to function' type
This is the type that usually calls in sick at work and decides to give in to her food cravings--as tiny (Pulse candy) or as huge (margarita pizza) as they may be. When she says she's feeling blah, take that sentence at face value.
Solution: Put on a feel-good movie for her, get her some popcorn (caramel, if she's in the mood to indulge), give her the remote and just Let. Her.Be.
Her.Be.
3. 'Don't even wanna see your face' type
Crabby--that's the word. That pretty much sums up her entire world when PMSing. Now, this might or might not have more to do with your 'irritating quotient' than her PMS. If she thinks having you around might be another thing she 'has to handle'--and we're not saying you are quite the handful--she might not want to be around you; at all. If everything--from the sun, to the breeze, to her boss, to her shoes, to the traffic--is getting to her, here's exactly what you should do...
Solution: Get the f**k out. Seriously. Now.
Expert tip: Getting some chocolates or brownies home-delivered to her place will go a long way.
4. 'Someone, love me, please' type
advertisement
Now, we're not saying she's the clingy type, but some women do need all the lovin' they can get during PMS--even if they're just the opposite for the rest of the month.
Solution: Get your romance on. Think of ways to make her feel wanted, special--even if it's just sending her a text about how pretty she looked the other day, or how she makes your heart melt each time you see her. It's always the little things that count.
Think of ways to make her feel wanted, special--even if it's just sending her a text about how pretty she looked the other day, or how she makes your heart melt each time you see her. It's always the little things that count.
5. 'All I want is food' type
Aaah, yes. This is the most interesting type, because she's going to make you indulge too, and eventually, you just might start to look at this as YOUR 'time of the month'!
Solution: Be her mother/grandmother for a couple of days. Feed her. Feed her as much as you can. Donuts, coffee, ice cream, pizza, samosas--whatever she's in the mood for, make sure you have a delivery guy ready for each. Do this and she'd never have the #3 kind of PMS.
Edited By:
AtMigration
Published On:
May 24, 2016
How PMS Affects Relationships and Helpful Tips
Open communication and understanding may help minimize challenges of premenstrual syndrome (PMS) on your relationship.
Premenstrual syndrome (PMS) and premenstrual dysphoric disorder (PMDD) are consistent, monthly experiences for many people that may occur alongside a cycle of often uncomfortable emotional and physical sensations.
You may have heard about the ways that PMS or PMDD can almost immobilize an individual experiencing it. But, the symptoms that accompany PMS in an individual may also cause distress in their relationships.
The good news is that there are ways you and your partner can take care of each other during the PMS/PMDD time span.
PMS vs. PMDD
Premenstrual syndrome (PMS) and premenstrual dysphoric disorder (PMDD) are related but not identical.
PMS describes a group of behavioral, emotional, and physical symptoms that a person may experience a week or two before a period. PMDD is a more severe form of PMS that can have a greater impact on your day-to-day life.
According to the Office on Women’s Health of the U.S. Department of Health and Human Services, about 90% of women experience PMS symptoms. Some of those symptoms include:
- fatigue
- irritability
- changes in mood
- decreased sex drive
- tender breasts
- bloating
- cramping
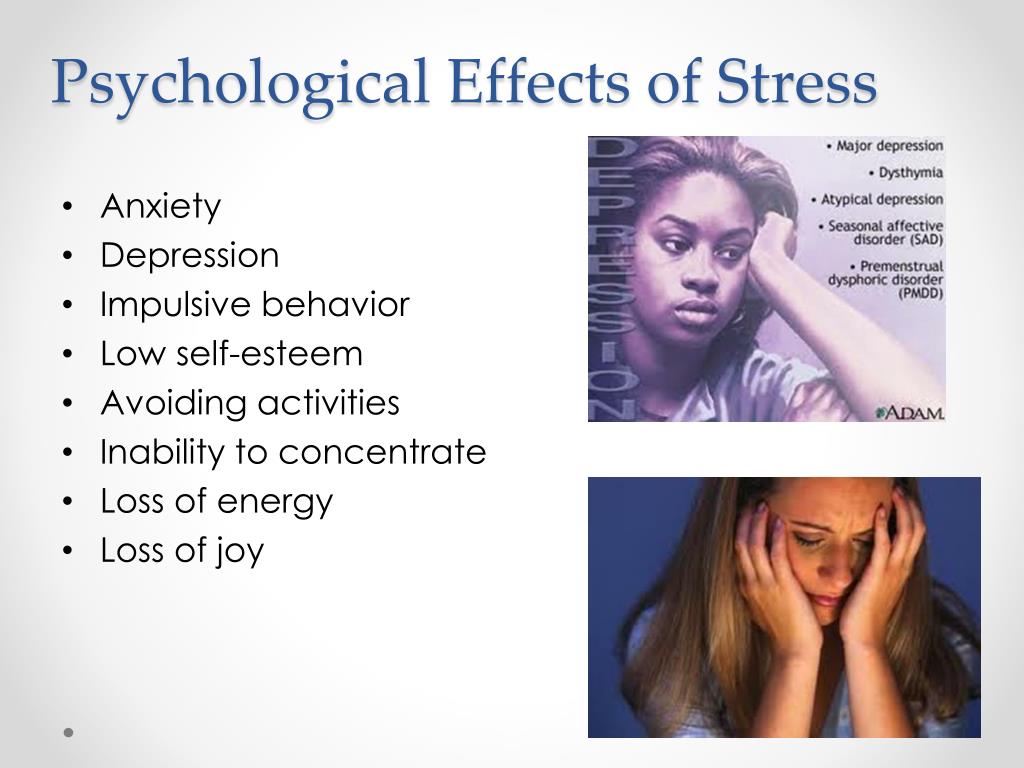
As we mentioned, PMDD is a severe form of PMS, and it affects 3% to 8% of the population. Unlike PMS, healthcare professionals classify PMDD as a depressive disorder. PMDD includes not only physical and behavioral symptoms, but also psychological symptoms like severe irritability, a sense of hopelessness, and even suicidal thoughts. Symptoms appear a week or two before your period.
Unlike PMS, healthcare professionals classify PMDD as a depressive disorder. PMDD includes not only physical and behavioral symptoms, but also psychological symptoms like severe irritability, a sense of hopelessness, and even suicidal thoughts. Symptoms appear a week or two before your period.
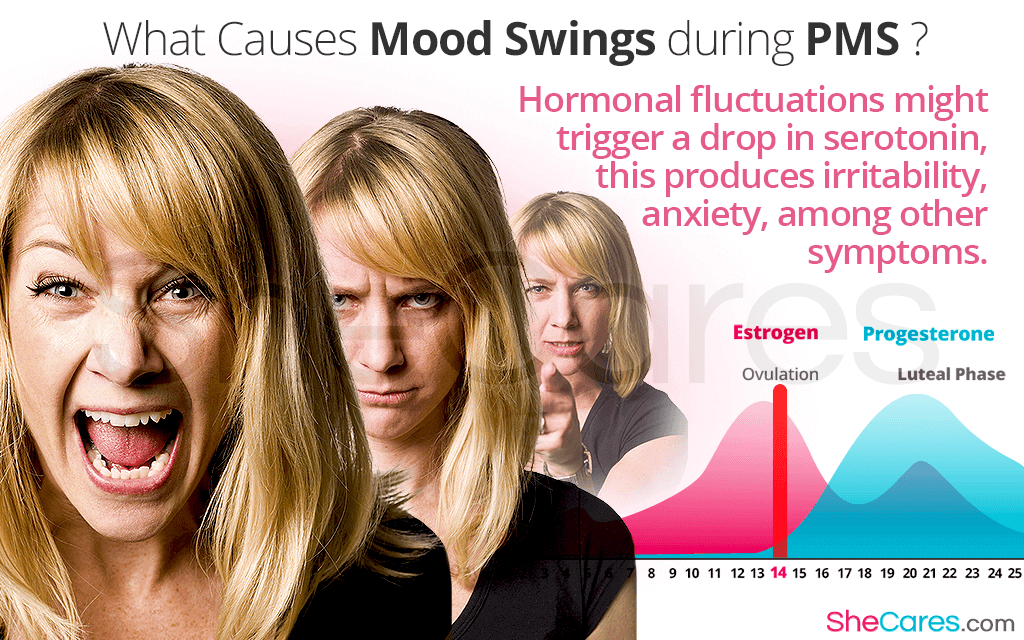
The exact cause of PMS and PMDD remains unknown, but research points to fluctuations in hormones as responsible. Your sensitivity to changes in estrogen and progesterone levels may determine whether you experience PMS. Two other factors that may play a role in whether you experience symptoms are genetics and stress.
Whom do they affect?
PMS and PMDD don’t only affect people who were assigned female at birth; they may also affect trans women, trans men, and nonbinary and gender-expansive individuals. Anyone who still has an ovary/ovaries can have PMS or PMDD because they still have a menstrual cycle. Transgender individuals experiencing PMS or PMDD often don’t receive the support they need.
Someone who was born without ovaries cannot generally experience PMS or PMDD, since there is no menstrual cycle to trigger clinical symptoms. Nonetheless, some transgender women, who were assigned male at birth, report PMS-like symptoms when using hormone therapy, via estrogen and progesterone intake.
Trans men who were assigned female at birth and, thus, may have ovaries, can experience both PMS and PMDD. Research has not found any evidence that testosterone hormone therapy causes a worsening of mental health conditions. In fact, trans men are more likely to experience improvements in social functioning and reduced anxiety and depression once testosterone therapy is begun.
Additionally, there is evidence that women across cultures and ethnicities experience and name PMS symptoms in different ways.
In 2014, researchers published a study exploring PMS in different ethnic groups and observed various differences in how symptoms were perceived and what kind of symptoms were experienced by different groups. For example, compared with African American and white respondents in the United States, Chinese participants in Hong Kong reported fewer pain- and concentration-related PMS symptoms. They also reported significantly lower levels of emotional symptoms.
For example, compared with African American and white respondents in the United States, Chinese participants in Hong Kong reported fewer pain- and concentration-related PMS symptoms. They also reported significantly lower levels of emotional symptoms.
The results of this study indicate that PMS symptoms are interpreted differently by different racial and ethnic groups.
PMS and PMDD don’t only affect the individual experiencing them — they may also impact relationships.
Physical symptoms, as well as anxiety and irritability, are the most severe and widely experienced signs of PMS. These feelings may interrupt your relationship with your family, especially in situations where there are overwhelming demands from a partner or children and the person experiencing PMS may find it more difficult to work through or tolerate negative emotions.
A partner’s response to PMS significantly impacts how a person experiences the premenstrual change.
Research conducted between 1990 and 2001 and summarized in a 2008 study indicates that negative PMS experiences can be a crucial factor in a couple’s relationship satisfaction. For example, women who experience symptoms of PMS are more likely to report difficulties or dissatisfaction in their relationship. On the other hand, women felt less PMS distress if their partnership involved effective communication.
For example, women who experience symptoms of PMS are more likely to report difficulties or dissatisfaction in their relationship. On the other hand, women felt less PMS distress if their partnership involved effective communication.
This indicates that a partner’s response may either improve or worsen the symptoms of PMS a person experiences. Partners should not be dismissive and should offer extra support.
It’s important to know that PMS affects both partners differently.
In lesbian partnerships and relationships between partners who both have an ovary or ovaries, the time during which PMS occurs is reported to be more supportive and understanding. According to older research, this comes from the lesbian partner’s awareness and recognition of premenstrual change, responsiveness to their partner’s needs, willingness for open communication, and general responsibility sharing.
In contrast, a 2013 study found that cis men were unable to understand the premenstrual situation and often suspected that the signs and symptoms reported by their partners were imaginary, or were dismissed and ignored.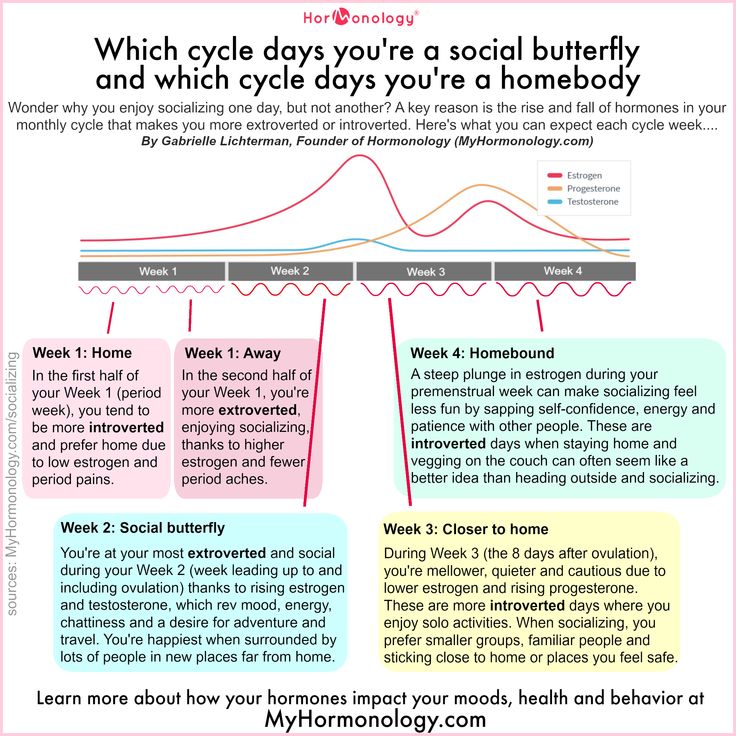 Consequently, this misunderstanding may lead to a lack of emotional and practical support, especially for tasks like domestic duties, from the cis male partner.
Consequently, this misunderstanding may lead to a lack of emotional and practical support, especially for tasks like domestic duties, from the cis male partner.
Women who are straight and experiencing symptoms of PMS show a decrease in shared good experiences with their cis male partner and an increase in relationship conflict during the last week of the cycle. This seems to be the case because while experiencing PMS symptoms, people with ovaries seem to be more sensitive to the unpleasant things in the environment and pay more attention to problems in the relationship than they normally would.
Any partner, regardless of gender, can make a significant positive influence on their partner with PMS, and PMS’s effects on the relationship can be managed.
First, the partner should let the person with ovaries know that they take their PMS or PMDD seriously. The fear that the partner would not take PMS experiences seriously — known as partner dismissal — is one reason why women, particularly those in a heterosexual relationship, may hesitate to give PMS as an explanation for a negative change to mood and behavior.
Communication is critical during this time, and its absence within a couple’s relationship may lead to a higher likelihood of PMS distress. On the contrary, if the partner of someone experiencing PMS responds positively to the other’s open expression of their concerns during this time it is linked to lower rates of premenstrual stress.
During this time period, a partner can show support to the person experiencing PMS by giving them emotional and physical space when needed. Additionally, using patience and acceptance during this time is a helpful way to deal with your partner.
You can also support your partner in practical ways, like doing housework or giving emotional assurance.
In a 2013 study of relationships between cis men and cis women, understanding the women’s experience, and how it differs from that of a cis man, helped men more readily adapt to the woman’s premenstrual changes. It’s also important that the man doesn’t listen to internalized, medicalized concepts and assumptions about PMS, and instead asks directly about his partner’s experience.
Couples-based cognitive behavioral therapy (CBT) is proven to have a greater positive impact on coping behavior, perception of the relationship, and support. For example, one study showed that women who received CBT therapy that included both partners experienced fewer intimate relationship difficulties. On the other hand, women who received individual CBT therapy or no therapy experienced an increase in relationship difficulties.
Aside from your partner or immediate family, social support from friends or your community may also help some people better cope with PMS symptoms.
Lastly, depending on the severity of your symptoms, your doctor may prescribe one or more medications for premenstrual syndrome and may help you find additional ways to relieve symptoms.
Premenstrual syndrome (PMS) and premenstrual dysphoric disorder (PMDD) are normal behavioral, emotional, and physical symptoms that a person may experience a week or two before a period.
These conditions don’t only affect people who were assigned female at birth but may also affect trans women, trans men, and nonbinary and gender-expansive individuals.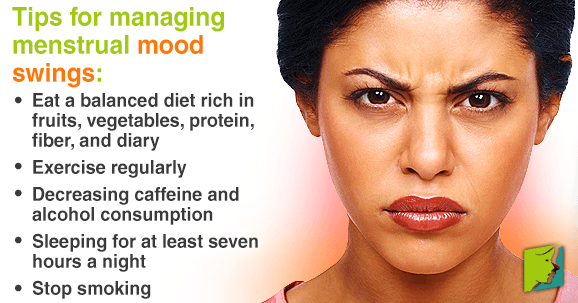 Plus, they may affect not only the individual but also their relationships. A partner’s response significantly affects how a person experiences the premenstrual change.
Plus, they may affect not only the individual but also their relationships. A partner’s response significantly affects how a person experiences the premenstrual change.
We recommend using this time to practice communication, patience, generosity, and sensitivity. If you and your partner have difficulty managing this cycle alone, reaching out to a therapist for CBT couple’s therapy may be helpful. You also may want to consult a doctor about your symptoms to consider medication.
While PMS symptoms can be challenging both for the person experiencing them and their relationships, challenges can be overcome with teamwork and the right tools by your side.
Mood changes suddenly. How to live with a "bipolar"?
Kim Kardashian's husband, rapper Kanye West, spoke well about this disease. On the cover of his album, he wrote: "I hate being bipolar, it's amazing." More precisely, you can’t say. Our expert is a psychiatrist of the highest category, Corresponding Member of the Russian Academy of Sciences, Professor, Head of the Department of Psychiatry and Narcology, Director of the Institute of Electronic Medical Education of the First Moscow State Medical University named after I.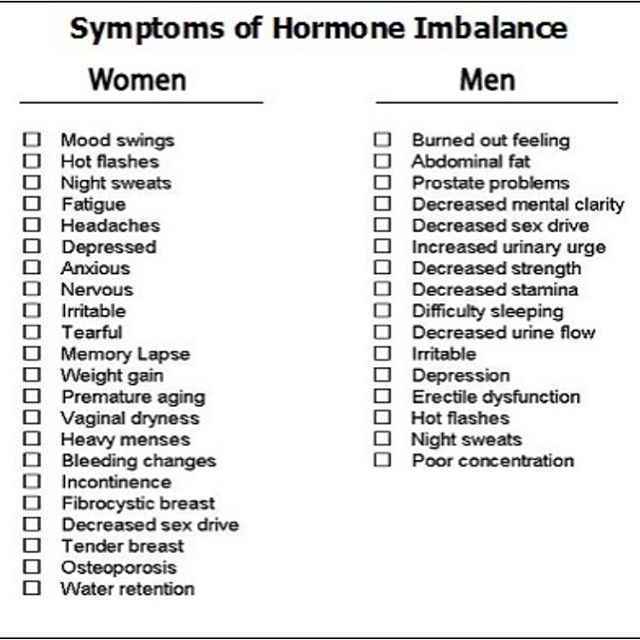 M. Sechenov, Doctor of Medical Sciences Marina Kinkulkina.
M. Sechenov, Doctor of Medical Sciences Marina Kinkulkina.
The essence of mental illness under the abbreviation BAD (bipolar affective disorder) is in radically sharp, causeless mood swings that occur in a person throughout life. Previously, this disease was called manic-depressive psychosis.
Life at different poles
This is not just about successive sadness or fun, as is often the case with emotional people, but about extreme degrees of either despair or euphoria. The change in these moods can take place both gradually and suddenly, and for no apparent reason.
It is believed that many celebrities of the past suffered from bipolar affective disorder. This illness, however, like other mental disorders, is attributed to Byron and Hemingway, Virginia Woolf and Edgar Poe, Van Gogh, Schumann, Vivien Leigh and many others. There is an assumption that even “our everything” suffered from a mild degree of BAD - in any case, contemporaries often mentioned Alexander Sergeevich’s mood swings.
Many modern stars openly admit to having this mental disorder. In particular, Britney Spears, Miley Cyrus, Selena Gomez, Mariah Carey, Mel Gibson and others admitted this.
Genetics or lifestyle?
BAD also affects men, but the weaker sex more often. This violation can appear at any age: both in a teenager and in an elderly person.
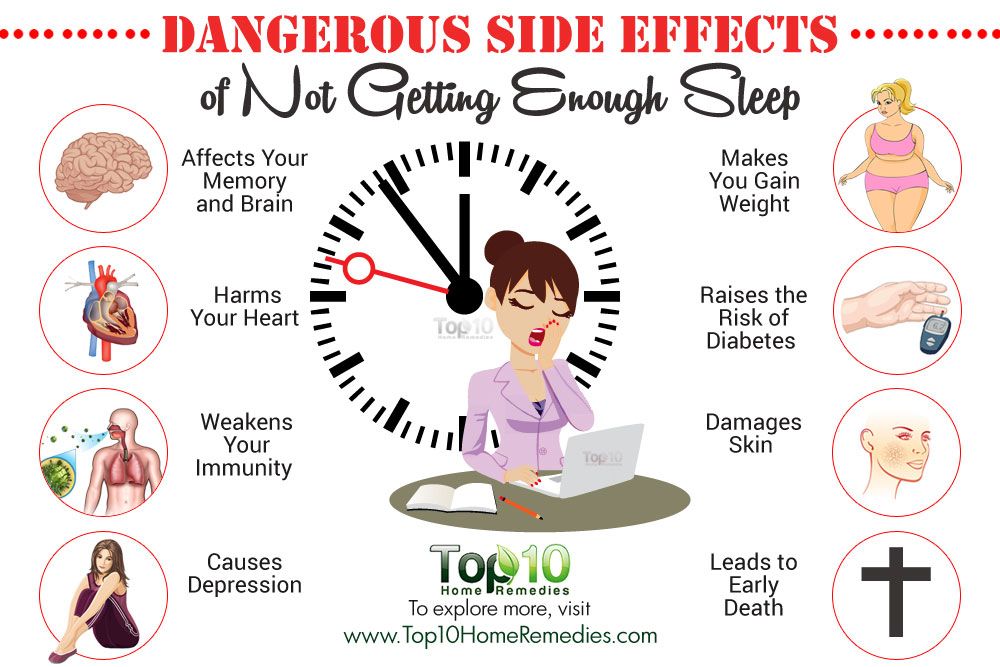
The main risk factor is genetics. However, a specific gene that would be responsible for the development of BAD has not been identified. This is a polygenic disorder, so it does not make sense to take tests to find out how big the risk of getting sick is. Moreover, genetic predisposition is not yet a sentence. This was proven by studies on identical twins, one of whom developed bipolar disorder over the years, while the other did not. There are probably some predisposing factors involved. Some of them are known. It is believed that life at the limit of possibilities, with constant deadlines, stress and chronic sleep deprivation, as well as night shift work, frequent flights with significant change in hourly flights and, of course, the use of psychoactive substances contribute to the development of the disease. Therefore, all this should be avoided. But scientists have yet to find out how the lockdown and pandemic, as well as other stresses of the ill-fated 2020, affect the psyche. Though probably not in the best way.
Therefore, all this should be avoided. But scientists have yet to find out how the lockdown and pandemic, as well as other stresses of the ill-fated 2020, affect the psyche. Though probably not in the best way.
Don't get bored
BAD, according to various estimates, suffer from fractions of a percent to several percent of the population. Recently, the proportion of affective disorders has increased significantly, which can be explained by improved diagnostics (as well as an increase in the number of stresses).
At first glance, the BAR does not look like something scary and dangerous. To many, this disorder even seems attractive - sometimes sad, sometimes fun, in general, you won’t get bored. In addition, being different from everyone else is now fashionable. And then, it is believed that people with BAD have higher intelligence and creativity than the "gray masses". But even if this is true, then none of those who suffer from it will definitely call BAD a pleasant thing. It is especially difficult for those patients who do not seek medical help on time. Without treatment, both phases of bipolar disorder can last for months (although sometimes the disorder occurs with frequently alternating phases). Moreover, it is impossible to say which of the periods of the disease is more difficult - manic or depressive.
It is especially difficult for those patients who do not seek medical help on time. Without treatment, both phases of bipolar disorder can last for months (although sometimes the disorder occurs with frequently alternating phases). Moreover, it is impossible to say which of the periods of the disease is more difficult - manic or depressive.
It's hard when the soul feels bad
Those who have experienced depression say that it is the worst thing that can happen. The whole world appears in black, not only mood, but also self-esteem is greatly reduced, the meaning of existence itself is lost. Life is perceived as a chain of tragic mistakes, the patient constantly blames himself for all the troubles and sins, even those that do not even exist. In addition to mental suffering, physical ones also often arise: a person moves as if in a dream, with difficulty, as if weights are weighed on his feet and hands, or as if he is swimming against the current. In addition, pain and tension are felt throughout the body. With an average degree of depression, the stomach often hurts. On this occasion, people turn to doctors, but the diagnosis cannot be made. And the daily pain continues. Psychiatrists call this somatoform symptomatology. With severe depression, many people have the so-called "precordial longing": pain and heaviness in the chest, "a stone on the heart." But even an in-depth examination does not reveal cardiological problems.
With an average degree of depression, the stomach often hurts. On this occasion, people turn to doctors, but the diagnosis cannot be made. And the daily pain continues. Psychiatrists call this somatoform symptomatology. With severe depression, many people have the so-called "precordial longing": pain and heaviness in the chest, "a stone on the heart." But even an in-depth examination does not reveal cardiological problems.
Often, with depression, patients (especially the elderly) complain of difficulty in thinking, memory impairment. Doctors suspect they have dementia, but in fact, affective disorders do not affect intelligence, and with treatment, when mood stabilizes, mental abilities are restored.
But the worst consequence of depression is suicide. Most suicide attempts are made in this state. Sometimes people in a very pronounced depression, believing that they have done something irreparable, and believing that the consequences of their actions can harm loved ones, decide on extended suicides, in which they settle scores not only with their lives, but also take their loved ones with them ( more often than children).
Bad when too good
The manic stage of BAD is subjectively more pleasant. Patients are in a great mood: they love the whole world and themselves in it. The reflection in the mirror pleases, there is not the slightest doubt about one’s own talents and mind, there is more than enough strength and energy, a bonus is accelerated mental activity. Many patients in this stage sleep for an hour a day, but do not experience fatigue. Sometimes they are on their feet for days - and at least they are cheerful, like an "energizer". It seems to be great. But no. In the mania phase, desires and ideas arise too quickly, so a person grabs at each new business, but, as a rule, does not complete any one. So productivity at this stage is low. But it would be nice if it was just that /
The main danger of mania is that a person has no criticism at this moment and he can do things that he will later regret very much. For example, he can give away all his property to others (sometimes to unfamiliar people or scammers). Or, say, take loans to go on a trip to the other side of the world. Maybe even steal something - for example, to make an expensive gift. Many patients at these moments enter into hasty intimate relationships, mistaking a chance meeting for the love of their lives (while completely “forgetting” that a wife and four children are waiting at home). Finally, often with mania, people, experiencing euphoria, ignore their severe somatic symptoms, as a result, they do not see a doctor for a long time and thus trigger a serious illness (pneumonia, for example, or COVID-19).
Or, say, take loans to go on a trip to the other side of the world. Maybe even steal something - for example, to make an expensive gift. Many patients at these moments enter into hasty intimate relationships, mistaking a chance meeting for the love of their lives (while completely “forgetting” that a wife and four children are waiting at home). Finally, often with mania, people, experiencing euphoria, ignore their severe somatic symptoms, as a result, they do not see a doctor for a long time and thus trigger a serious illness (pneumonia, for example, or COVID-19).
In addition, not all patients in the manic stage are "darlings." Often they show unreasonable aggression if, for example, others do not agree with their "brilliant" ideas. As a result of "angry mania", conflicts and even situations arise that require the intervention of law enforcement agencies and involuntary hospitalization of the patient.
Well Intentioned
The worst thing that relatives and friends of a person with bipolar disorder can do is ignore the problem, devalue suffering, while blaming the patient himself and appealing to his conscience. For example, they call on a depressed person to “pull himself together, not to become limp”, they say that he is “mad with fat” and so on. A patient at the stage of mania is most often accused of immorality, frivolity, irresponsibility, promiscuity in relationships, and so on. However, doing so is like blaming a person with diabetes for not being able to eat sweet cake, or a patient with heart failure for not running a marathon.
For example, they call on a depressed person to “pull himself together, not to become limp”, they say that he is “mad with fat” and so on. A patient at the stage of mania is most often accused of immorality, frivolity, irresponsibility, promiscuity in relationships, and so on. However, doing so is like blaming a person with diabetes for not being able to eat sweet cake, or a patient with heart failure for not running a marathon.
BAD is a disease like many others. And she needs to be treated. The sooner you start the right therapy, the sooner you can stabilize the patient's condition and the better the further prognosis will be.
How to "cure"?
On the Internet, you can not only test yourself for any mental disorder, but also learn how to “cure”. Doctors strongly advise against doing this. The smallest harm of self-treatment is that it will not help, but it can also worsen the condition. For example, inadequate intake of antidepressants in bipolar disorder can plunge a person from a depressive phase into a severe manic state, from which it will then be difficult to get out.
Only a psychiatrist (and not a psychologist, neurologist or doctor of any other profile) can identify bipolar disorder and choose the right treatment. Treatment should be strictly individual, it is selected based on the characteristics of a particular patient and taking into account the moment in the course of the disease. The goal of therapy is not only to level the mood of the patient, but also to prevent repeated episodes.
In the treatment of bipolar disorder, the main role is played by drugs for stabilizing mood - mood stabilizers (lithium salts, some anticonvulsants (anticonvulsants) and antipsychotics of new generations). Modern drugs are much better tolerated than their predecessors, have fewer side effects, as they are designed for long-term use over many years. Against the background of their intake, women can even become pregnant. With depression within this disorder, antidepressants are prescribed only in exceptional cases, given the danger of changing from one phase to another.
BAD cannot be cured once and for all, so you often have to take medication for years (with periodic visits to the doctor). But often, when a patient begins to feel good thanks to the medication (such a state - intermission - is completely indistinguishable from full health), he can stop taking the drugs. This is a big mistake that does not allow to achieve a stable result of treatment. After all, it is the long-term use of the maintenance therapy recommended by the doctor that allows you to achieve a stable state and feel the joy of life for many years.
Link to publication: Arguments and facts
Embed code on the site
Kim Kardashian's husband, rapper Kanye West, spoke well about this disease. On the cover of his album, he wrote: "I hate being bipolar, it's amazing." More precisely, you can’t say. Our expert is a psychiatrist of the highest category, Corresponding Member of the Russian Academy of Sciences, Professor, Head of the Department of Psychiatry and Narcology, Director of the Institute of Electronic Medical Education of the First Moscow State Medical University named after I. M. Sechenov, Doctor of Medical Sciences Marina Kinkulkina.
The essence of mental illness under the abbreviation BAD (bipolar affective disorder) is in radically sharp, causeless mood swings that occur in a person throughout life. Previously, this disease was called manic-depressive psychosis.
Life at different poles
This is not just about successive sadness or fun, as is often the case with emotional people, but about extreme degrees of either despair or euphoria. The change in these moods can take place both gradually and suddenly, and for no apparent reason.
It is believed that many celebrities of the past suffered from bipolar affective disorder. This illness, however, like other mental disorders, is attributed to Byron and Hemingway, Virginia Woolf and Edgar Poe, Van Gogh, Schumann, Vivien Leigh and many others. There is an assumption that even “our everything” suffered from a mild degree of BAD - in any case, contemporaries often mentioned Alexander Sergeevich’s mood swings.
Many modern stars openly admit to having this mental disorder. In particular, Britney Spears, Miley Cyrus, Selena Gomez, Mariah Carey, Mel Gibson and others admitted this.
Genetics or lifestyle?
BAD also affects men, but the weaker sex more often. This violation can appear at any age: both in a teenager and in an elderly person.
The main risk factor is genetics. However, a specific gene that would be responsible for the development of BAD has not been identified. This is a polygenic disorder, so it does not make sense to take tests to find out how big the risk of getting sick is. Moreover, genetic predisposition is not yet a sentence. This was proven by studies on identical twins, one of whom developed bipolar disorder over the years, while the other did not. There are probably some predisposing factors involved. Some of them are known. It is believed that life at the limit of possibilities, with constant deadlines, stress and chronic sleep deprivation, as well as night shift work, frequent flights with significant change in hourly flights and, of course, the use of psychoactive substances contribute to the development of the disease. Therefore, all this should be avoided. But scientists have yet to find out how the lockdown and pandemic, as well as other stresses of the ill-fated 2020, affect the psyche. Though probably not in the best way.
Don't get bored
BAD, according to various estimates, suffer from fractions of a percent to several percent of the population. Recently, the proportion of affective disorders has increased significantly, which can be explained by improved diagnostics (as well as an increase in the number of stresses).
At first glance, the BAR does not look like something scary and dangerous. To many, this disorder even seems attractive - sometimes sad, sometimes fun, in general, you won’t get bored. In addition, being different from everyone else is now fashionable. And then, it is believed that people with BAD have higher intelligence and creativity than the "gray masses". But even if this is true, then none of those who suffer from it will definitely call BAD a pleasant thing. It is especially difficult for those patients who do not seek medical help on time. Without treatment, both phases of bipolar disorder can last for months (although sometimes the disorder occurs with frequently alternating phases). Moreover, it is impossible to say which of the periods of the disease is more difficult - manic or depressive.
It's hard when the soul feels bad
Those who have experienced depression say that it is the worst thing that can happen. The whole world appears in black, not only mood, but also self-esteem is greatly reduced, the meaning of existence itself is lost. Life is perceived as a chain of tragic mistakes, the patient constantly blames himself for all the troubles and sins, even those that do not even exist. In addition to mental suffering, physical ones also often arise: a person moves as if in a dream, with difficulty, as if weights are weighed on his feet and hands, or as if he is swimming against the current. In addition, pain and tension are felt throughout the body. With an average degree of depression, the stomach often hurts. On this occasion, people turn to doctors, but the diagnosis cannot be made. And the daily pain continues. Psychiatrists call this somatoform symptomatology. With severe depression, many people have the so-called "precordial longing": pain and heaviness in the chest, "a stone on the heart." But even an in-depth examination does not reveal cardiological problems.
Often, with depression, patients (especially the elderly) complain of difficulty in thinking, memory impairment. Doctors suspect they have dementia, but in fact, affective disorders do not affect intelligence, and with treatment, when mood stabilizes, mental abilities are restored.
But the worst consequence of depression is suicide. Most suicide attempts are made in this state. Sometimes people in a very pronounced depression, believing that they have done something irreparable, and believing that the consequences of their actions can harm loved ones, decide on extended suicides, in which they settle scores not only with their lives, but also take their loved ones with them ( more often than children).
Bad when too good
The manic stage of BAD is subjectively more pleasant. Patients are in a great mood: they love the whole world and themselves in it. The reflection in the mirror pleases, there is not the slightest doubt about one’s own talents and mind, there is more than enough strength and energy, a bonus is accelerated mental activity. Many patients in this stage sleep for an hour a day, but do not experience fatigue. Sometimes they are on their feet for days - and at least they are cheerful, like an "energizer". It seems to be great. But no. In the mania phase, desires and ideas arise too quickly, so a person grabs at each new business, but, as a rule, does not complete any one. So productivity at this stage is low. But it would be nice if it was just that /
The main danger of mania is that a person has no criticism at this moment and he can do things that he will later regret very much. For example, he can give away all his property to others (sometimes to unfamiliar people or scammers).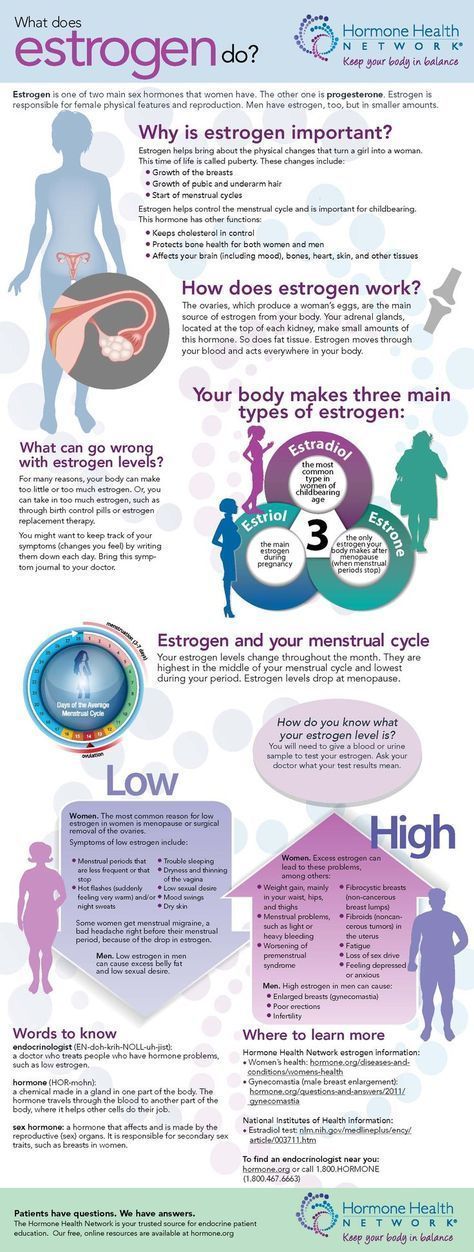 Or, say, take loans to go on a trip to the other side of the world. Maybe even steal something - for example, to make an expensive gift. Many patients at these moments enter into hasty intimate relationships, mistaking a chance meeting for the love of their lives (while completely “forgetting” that a wife and four children are waiting at home). Finally, often with mania, people, experiencing euphoria, ignore their severe somatic symptoms, as a result, they do not see a doctor for a long time and thus trigger a serious illness (pneumonia, for example, or COVID-19).
Or, say, take loans to go on a trip to the other side of the world. Maybe even steal something - for example, to make an expensive gift. Many patients at these moments enter into hasty intimate relationships, mistaking a chance meeting for the love of their lives (while completely “forgetting” that a wife and four children are waiting at home). Finally, often with mania, people, experiencing euphoria, ignore their severe somatic symptoms, as a result, they do not see a doctor for a long time and thus trigger a serious illness (pneumonia, for example, or COVID-19).
In addition, not all patients in the manic stage are "darlings." Often they show unreasonable aggression if, for example, others do not agree with their "brilliant" ideas. As a result of "angry mania", conflicts and even situations arise that require the intervention of law enforcement agencies and involuntary hospitalization of the patient.
Well Intentioned
The worst thing that relatives and friends of a person with bipolar disorder can do is ignore the problem, devalue suffering, while blaming the patient himself and appealing to his conscience. For example, they call on a depressed person to “pull himself together, not to become limp”, they say that he is “mad with fat” and so on. A patient at the stage of mania is most often accused of immorality, frivolity, irresponsibility, promiscuity in relationships, and so on. However, doing so is like blaming a person with diabetes for not being able to eat sweet cake, or a patient with heart failure for not running a marathon.
For example, they call on a depressed person to “pull himself together, not to become limp”, they say that he is “mad with fat” and so on. A patient at the stage of mania is most often accused of immorality, frivolity, irresponsibility, promiscuity in relationships, and so on. However, doing so is like blaming a person with diabetes for not being able to eat sweet cake, or a patient with heart failure for not running a marathon.
BAD is a disease like many others. And she needs to be treated. The sooner you start the right therapy, the sooner you can stabilize the patient's condition and the better the further prognosis will be.
How to "cure"?
On the Internet, you can not only test yourself for any mental disorder, but also learn how to “cure”. Doctors strongly advise against doing this. The smallest harm of self-treatment is that it will not help, but it can also worsen the condition. For example, inadequate intake of antidepressants in bipolar disorder can plunge a person from a depressive phase into a severe manic state, from which it will then be difficult to get out.
Only a psychiatrist (and not a psychologist, neurologist or doctor of any other profile) can identify bipolar disorder and choose the right treatment. Treatment should be strictly individual, it is selected based on the characteristics of a particular patient and taking into account the moment in the course of the disease. The goal of therapy is not only to level the mood of the patient, but also to prevent repeated episodes.
In the treatment of bipolar disorder, the main role is played by drugs for stabilizing mood - mood stabilizers (lithium salts, some anticonvulsants (anticonvulsants) and antipsychotics of new generations). Modern drugs are much better tolerated than their predecessors, have fewer side effects, as they are designed for long-term use over many years. Against the background of their intake, women can even become pregnant. With depression within this disorder, antidepressants are prescribed only in exceptional cases, given the danger of changing from one phase to another.
BAD cannot be cured once and for all, so you often have to take medication for years (with periodic visits to the doctor). But often, when a patient begins to feel good thanks to the medication (such a state - intermission - is completely indistinguishable from full health), he can stop taking the drugs. This is a big mistake that does not allow to achieve a stable result of treatment. After all, it is the long-term use of the maintenance therapy recommended by the doctor that allows you to achieve a stable state and feel the joy of life for many years.
reasons and what to do when treatment is needed
Men make up legends and tell each other jokes about mood swings in women. But in some cases, these are not just whims - everything can be much more serious. Frequent outbursts of anger or emotional swings can be symptoms of illness. Let's try to understand the issue from a medical point of view.
Website editor
Tags:
Alina Titova
Women Health
emotions
How to cheer up
It is not uncommon to hear and read complaints from friends or people you barely know online. Like, a lot of money and time was spent on communicating with psychologists, but in vain. It was not possible to get rid of depression, just as irritability and anxiety did not disappear.
Like, a lot of money and time was spent on communicating with psychologists, but in vain. It was not possible to get rid of depression, just as irritability and anxiety did not disappear.
Sudden mood swings "strain" not only the woman herself, but also the people around her. In fact, sometimes emotions are literally caused by illness. In this case, it is important to contact a therapist, surgeon or endocrinologist in a timely manner.
What causes mood swings
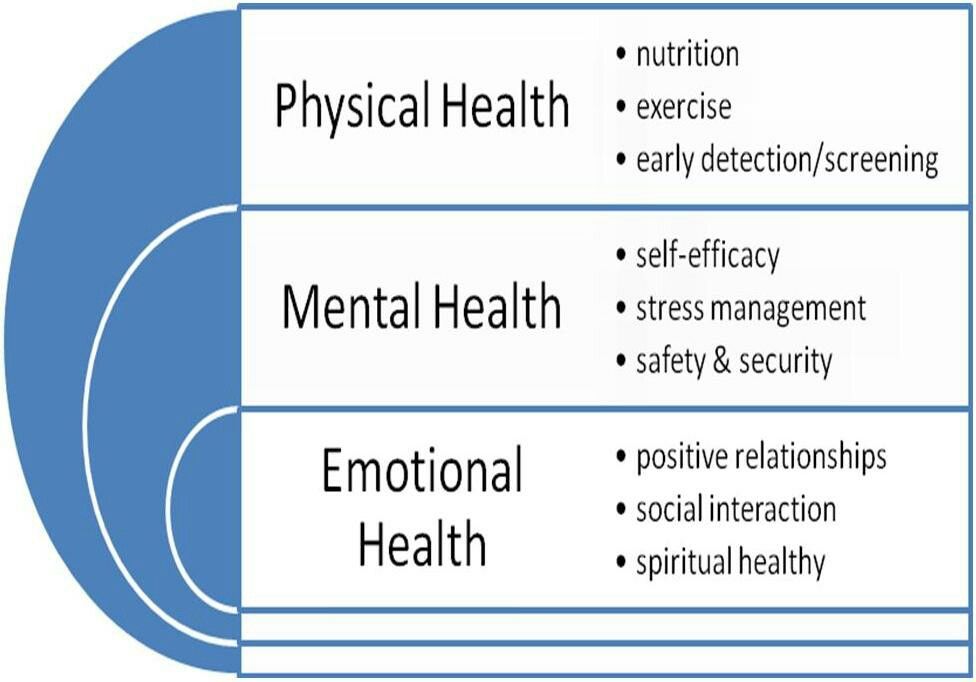
Any emotion, including frequent mood swings, is the result of neurophysiological processes in the brain. But we must remember that experience changes the level of brain activity, controls the endocrine, circulatory and respiratory systems. That is, it is impossible to say unequivocally whether sensory reactions cause physiological changes in the body or are themselves the result of these changes.
Neurologist Sef Kabirsky explains: “Emotions trigger a response in the brain through complex hormonal response pathways. And accordingly, our body reacts physically. For example, fear makes the heart beat faster. Few people have thought about this, but there is also an inverse relationship that affects strong mood swings. Simply put, an increased heartbeat is quite capable of causing a feeling of fear.
And accordingly, our body reacts physically. For example, fear makes the heart beat faster. Few people have thought about this, but there is also an inverse relationship that affects strong mood swings. Simply put, an increased heartbeat is quite capable of causing a feeling of fear.
ADVERTISING - CONTINUED BELOW
Thus, a logical conclusion suggests itself. If physiological changes occur (failure in the hormonal system, problems with metabolism), then they can also cause disturbances in the emotional sphere, become a reason for mood swings in girls and the appearance of unpleasant emotions. But how often do we build such a chain of thought? With constant obsessive thoughts and feelings, at best, we turn to a psychologist. At worst, we start drinking self-prescribed sedatives.
Physiological causes of mood swings
It is difficult to imagine a person who will be disturbed by a constant feeling of joy or happiness. We are more likely to pay attention to manifestations of anger, irritation, sadness, attacks of fear and constant mood swings. The experience of these emotions is quite unpleasant, because they are usually characterized as negative. And even more frightening is the fact that they appeared as if from scratch, without objective reasons.
We are more likely to pay attention to manifestations of anger, irritation, sadness, attacks of fear and constant mood swings. The experience of these emotions is quite unpleasant, because they are usually characterized as negative. And even more frightening is the fact that they appeared as if from scratch, without objective reasons.
Thyroid
Mood swings are most often attributed to thyroid dysfunction. “Hormones have a significant effect on metabolism. Due to the increased production of hormones, all reactions in the body become more intense. As a consequence, the person becomes irritable,” explains Sef Kabirsky.
The troubles of life, which you would not have paid attention to before, are now annoying. And more serious problems can cause tears and even tantrums. In some cases, mood swings lead to aggression and even rage. And vice versa: if the intensity of hormone production decreases, the metabolism slows down.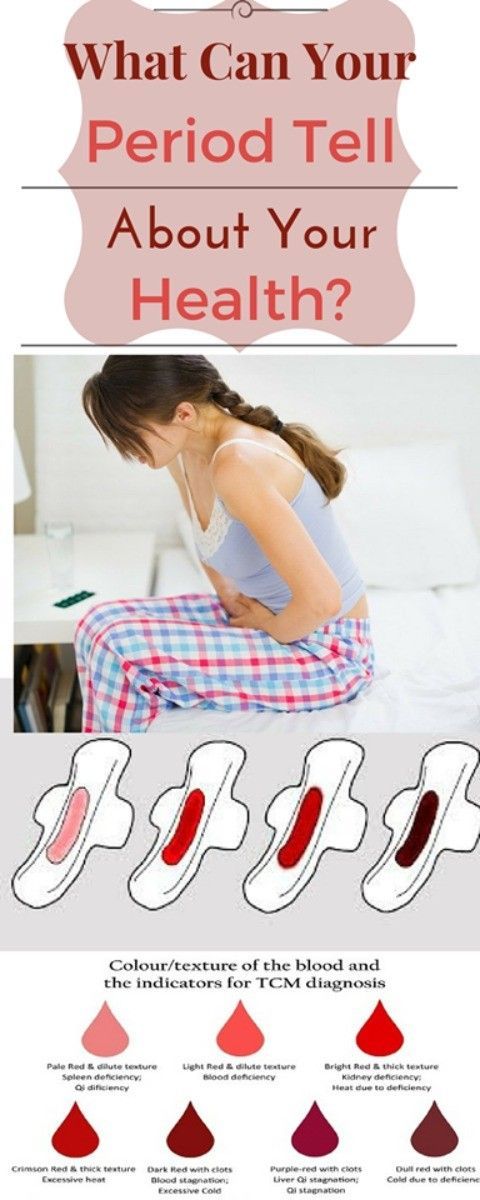 Then the person begins to respond to external stimuli with a delay, becomes lethargic, dull, sad, apathetic. In other words, he begins to believe that he has depression.
Then the person begins to respond to external stimuli with a delay, becomes lethargic, dull, sad, apathetic. In other words, he begins to believe that he has depression.
What to do
The thyroid gland produces hormones that affect all cells and tissues of the body. As studies show, if a failure in her work is expressed only by a sharp change in mood, this is not the worst thing. An endocrinologist will tell you what to do if you are haunted by mood swings, sweating, insomnia, thirst, weight jumps, and so on. You will have to donate blood for hormones and undergo a course of treatment.
Liver and gallbladder
Diseases of the liver and gallbladder also cause mood swings in women. “A spasm of the biliary tract in the liver leads to an increase in the production of norepinephrine, the “hormone of anger,” explains the neurologist. Note that these changes in behavior are usually short-lived. A person quickly starts up, but just as quickly cools down after another outbreak.
A person quickly starts up, but just as quickly cools down after another outbreak.
What to do
Any disease of the internal organs deserves a trip to the specialists. Based on the results of general tests, ultrasound and other diagnostic methods, the doctor will prescribe the appropriate treatment.
Menopause
A new stage in a woman's life can pass quickly and painlessly, or maybe with physical and psychological problems. Many wonder why mood swings are observed during this period. But research explains everything. This is due to hormonal changes that lead to fluctuations in estrogen levels. As a result, during the day the woman manages to cry and laugh. The production of serotonin drops, and it is precisely responsible for good health. Add to this symptoms such as sweating, frequent need to go to the toilet, and the approach of advanced age will cause complete disappointment.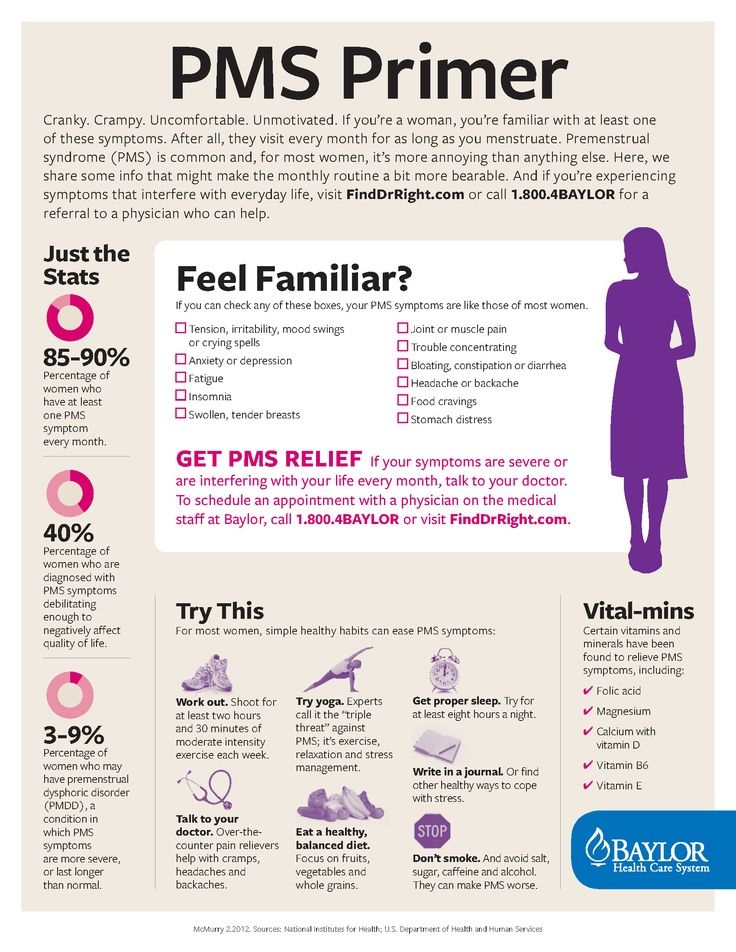
What to do
You can start taking non-hormonal herbal preparations on the advice of a gynecologist in time Like a massage, do yoga, take pine baths. In some cases, antidepressants can help, which should also be recommended by a doctor.
Pregnancy
The hormonal upheaval that occurs in a woman's body will explain the mood swings during pregnancy. Emotional imbalance provokes many questions related to the birth of a child and a huge responsibility. The tendency to dramatization is due not only to the fact that life is divided into "before" and "after" the appearance of the baby. But the body of the expectant mother is also changing, hormones are being rearranged, she feels vulnerable.
Sometimes doctors associate such an exciting period with puberty. Approximately the same mood swings can be observed in adolescents. It is similar to the transition from childhood to adulthood, when the body changes in leaps and bounds, it is not possible to become an adult and formed overnight.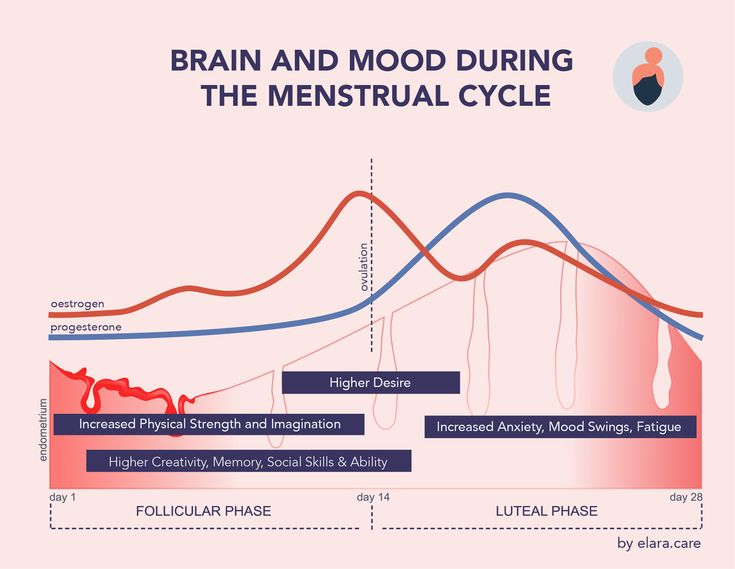 And all this clumsiness drives yesterday's children crazy.
And all this clumsiness drives yesterday's children crazy.
What to do
Future fathers, of course, need to be patient and try to be more attentive to their soul mate than ever. It is important for women to share their fears and doubts in order to feel supported. Sometimes a rational male look is enough to gain confidence.
Mood swings due to psychiatric disorders
It is important to distinguish where the boundary of normal mood changes is. If there was a serious trouble at work or a painful separation from a loved one, sadness is natural. Still, the balance is gradually restored, and you begin to enjoy life. Mental disorders lead to mood swings of a different kind. When for a long time (over two weeks) there is no desire and strength to do something, this is already an occasion to think about the problem that has arisen.
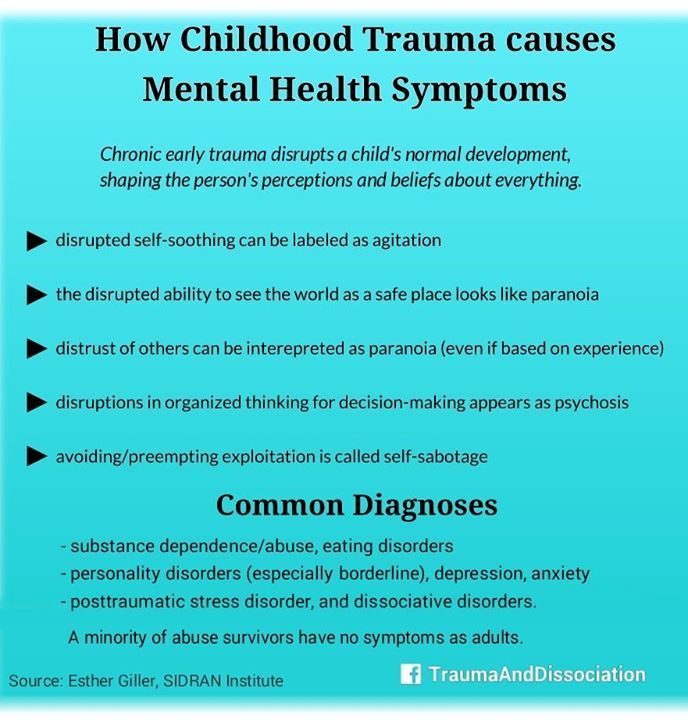
Depression
Refers to affective disorders - mental illness, manifested in pathological mood swings in men and women. Emotions no longer perform the function of evaluating reality. For example, a person in line at a supermarket just looked at you, and it already seems to you that he knows you and is plotting evil. Genetics plays a large role in the occurrence of the disease, as well as social conditions and triggers.
Emotions no longer perform the function of evaluating reality. For example, a person in line at a supermarket just looked at you, and it already seems to you that he knows you and is plotting evil. Genetics plays a large role in the occurrence of the disease, as well as social conditions and triggers.
Inadequate reactions to surrounding people and circumstances make life unbearable and make it impossible to work normally. So, an uncontrolled feeling of fear can provoke problems with the cardiovascular system. Increased blood pressure, heart palpitations cause the production of adrenaline, the hormone responsible for fear. You feel it. Mood swings associated with depression should be treated with the help of a doctor.
Dysthymia
The disease is similar to depression, only it is less severe and more protracted. It is expressed in mood swings in an adult, which lasts at least two years, and in a child and adolescent for at least a year.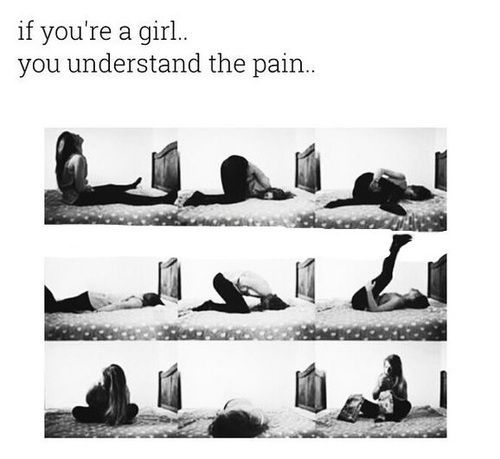 This is not about jumps from a cheerful mood to a sad one, but from a bad mood to a disgusting one. In these cases, those suffering from this disorder perceive their condition as part of their character, because the diagnosis is not established immediately. Depression becomes chronic, life just isn't nice.
This is not about jumps from a cheerful mood to a sad one, but from a bad mood to a disgusting one. In these cases, those suffering from this disorder perceive their condition as part of their character, because the diagnosis is not established immediately. Depression becomes chronic, life just isn't nice.
Bipolar disorder
Severe psychosis, often accompanied by delusions and hallucinations, already makes a person a danger to himself and to society. Once a person has such mood swings, it is already called bipolar disorder. He is no longer just dissatisfied, but ceases to control his actions. He develops suicidal tendencies and mania.
What to do
Mode and psychological comfort are important in the life of any person. And if someone is characterized by mood swings, bipolar disorder has already been encountered in the family, you need to especially carefully approach these moments. Scientists have proven that, first of all, it is necessary to avoid stress, sleep well, distribute rest and load. It is better to stop using alcohol and psychoactive substances. Just don't self-medicate! It is advisable to consult with a psychotherapist or psychiatrist.
Scientists have proven that, first of all, it is necessary to avoid stress, sleep well, distribute rest and load. It is better to stop using alcohol and psychoactive substances. Just don't self-medicate! It is advisable to consult with a psychotherapist or psychiatrist.
Separate mood swings and whims
In order not to treat liver or endocrine diseases with the help of psychoanalysis, and depression with surgical intervention, it is worth understanding what's what.
Psychiatrist, candidate of medical sciences Vlada Titova explains why psychologists cannot be reproached for negligence and unprofessionalism: “A psychologist cannot recognize the symptoms of endocrine or other disorders, focusing only on mood swings, simply because this is not within his competence. Just like endocrinologists are not taught to treat caries, and gynecologists are not taught to save clients from depression. Moreover, without the consent of a doctor, a psychologist does not have the right to make a diagnosis of a mental disorder. After all, he is a psychologist, not a psychiatrist.”
After all, he is a psychologist, not a psychiatrist.”
It often happens that even an experienced psychotherapist or psychiatrist does not immediately recognize the symptoms of diseases associated with sudden mood swings. Because they successfully disguise themselves as emotional or even mental disorders. Of course, there are other signs by which the disease is diagnosed. But often they fade into the background, becoming invisible to the person himself. In the initial stages of diseases, there may simply be no other symptoms other than emotions.
It is clear that it is simply impossible to remember all the signs of physiological diseases that can cause changes in the psychological state. And if, with every mood swing, you look for similar ones in a medical encyclopedia, it’s not far from hypochondria. You need to assess the state of your body as a whole, without separating psychology and physiology.
Recall when you first noticed any emotional changes in your behavior and why mood swings may have occurred.