Paralysis sleeping disorder
Sleep Paralysis - Causes, Symptoms, Treatment, and Prevention
Written by Beth Roybal
Is Sleep Paralysis a Symptom of a Serious Problem?
Sleep researchers conclude that, in most cases, sleep paralysis is simply a sign that your body is not moving smoothly through the stages of sleep. Rarely is sleep paralysis linked to deep underlying psychiatric problems.
Over the centuries, symptoms of sleep paralysis have been described in many ways and often attributed to an "evil" presence: unseen night demons in ancient times, the old hag in Shakespeare's Romeo and Juliet, and alien abductors. Almost every culture throughout history has had stories of shadowy evil creatures that terrify helpless humans at night. People have long sought explanations for this mysterious sleep-time paralysis and the accompanying feelings of terror.
What Is Sleep Paralysis?
Sleep paralysis is a feeling of being conscious but unable to move. It occurs when a person passes between stages of wakefulness and sleep. During these transitions, you may be unable to move or speak for a few seconds up to a few minutes. Some people may also feel pressure or a sense of choking. Sleep paralysis may accompany other sleep disorders such as narcolepsy. Narcolepsy is an overpowering need to sleep caused by a problem with the brain's ability to regulate sleep.
When Does Sleep Paralysis Usually Occur?
Sleep paralysis usually occurs at one of two times. If it occurs while you are falling asleep, it's called hypnagogic or predormital sleep paralysis. If it happens as you are waking up, it's called hypnopompic or postdormital sleep paralysis.
What Happens With Hypnagogic Sleep Paralysis?
As you fall asleep, your body slowly relaxes. Usually you become less aware, so you do not notice the change. However, if you remain or become aware while falling asleep, you may notice that you cannot move or speak.
What Happens With Hypnopompic Sleep Paralysis?
During sleep, your body alternates between REM (rapid eye movement) and NREM (non-rapid eye movement) sleep. One cycle of REM and NREM sleep lasts about 90 minutes. NREM sleep occurs first and takes up to 75% of your overall sleep time. During NREM sleep, your body relaxes and restores itself. At the end of NREM, your sleep shifts to REM. Your eyes move quickly and dreams occur, but the rest of your body remains very relaxed. Your muscles are "turned off" during REM sleep. If you become aware before the REM cycle has finished, you may notice that you cannot move or speak.
One cycle of REM and NREM sleep lasts about 90 minutes. NREM sleep occurs first and takes up to 75% of your overall sleep time. During NREM sleep, your body relaxes and restores itself. At the end of NREM, your sleep shifts to REM. Your eyes move quickly and dreams occur, but the rest of your body remains very relaxed. Your muscles are "turned off" during REM sleep. If you become aware before the REM cycle has finished, you may notice that you cannot move or speak.
Who Develops Sleep Paralysis?
Up to as many as four out of every 10 people may have sleep paralysis. This common condition is often first noticed in the teen years. But men and women of any age can have it. Sleep paralysis may run in families. Other factors that may be linked to sleep paralysis include:
- Lack of sleep
- Sleep schedule that changes
- Mental conditions such as stress or bipolar disorder
- Sleeping on the back
- Other sleep problems such as narcolepsy or nighttime leg cramps
- Use of certain medications, such as those for ADHD
- Substance abuse
How Is Sleep Paralysis Diagnosed?
If you find yourself unable to move or speak for a few seconds or minutes when falling asleep or waking up, then it is likely you have isolated recurrent sleep paralysis. Often there is no need to treat this condition.
Often there is no need to treat this condition.
Check with your doctor if you have any of these concerns:
- You feel anxious about your symptoms
- Your symptoms leave you very tired during the day
- Your symptoms keep you up during the night
Your doctor may want to gather more information about your sleep health by doing any of the following:
- Ask you to describe your symptoms and keep a sleep diary for a few weeks
- Discuss your health history, including any known sleep disorders or any family history of sleep disorders
- Refer you to a sleep specialist for further evaluation
- Conduct overnight sleep studies or daytime nap studies to make sure you do not have another sleep disorder
How Is Sleep Paralysis Treated?
Most people need no treatment for sleep paralysis. Treating any underlying conditions such as narcolepsy may help if you are anxious or unable to sleep well. These treatments may include the following:
- Improving sleep habits -- such as making sure you get six to eight hours of sleep each night
- Using antidepressant medication if it is prescribed to help regulate sleep cycles
- Treating any mental health problems that may contribute to sleep paralysis
- Treating any other sleep disorders, such as narcolepsy or leg cramps
What Can I Do About Sleep Paralysis?
There's no need to fear nighttime demons or alien abductors. If you have occasional sleep paralysis, you can take steps at home to control this disorder. Start by making sure you get enough sleep. Do what you can to relieve stress in your life -- especially just before bedtime. Try new sleeping positions if you sleep on your back. And be sure to see your doctor if sleep paralysis routinely prevents you from getting a good night's sleep.
If you have occasional sleep paralysis, you can take steps at home to control this disorder. Start by making sure you get enough sleep. Do what you can to relieve stress in your life -- especially just before bedtime. Try new sleeping positions if you sleep on your back. And be sure to see your doctor if sleep paralysis routinely prevents you from getting a good night's sleep.
What is Sleep Paralysis? | Sleep Foundation
While we usually think of being asleep or awake as clearly defined and distinct, conditions like sleep paralysis challenge these fixed boundaries.
Sleep paralysis is a temporary inability to move that occurs right after falling asleep or waking up. Individuals remain aware during episodes, which frequently involve troubling hallucinations and a sensation of suffocation.
These episodes of sleep paralysis involve elements of both sleep and wakefulness, which is part of why they can give rise to distressing symptoms.
While much is still unknown about sleep paralysis, a review of its types, symptoms, causes, impacts, and treatment can enable a better understanding of the condition and how to try to prevent it.
What Is Sleep Paralysis?
Sleep paralysis is a condition identified by a brief loss of muscle control, known as atonia, that happens just after falling asleep or waking up. In addition to atonia, people often have hallucinations during episodes of sleep paralysis.
Sleep paralysis is categorized as a type of parasomnia. Parasomnias are abnormal behaviors during sleep. Because it is connected to the rapid eye movement (REM) stage of the sleep cycle, sleep paralysis is considered to be a REM parasomnia.
Standard REM sleep involves vivid dreaming as well as atonia, which helps prevent acting out dreams. However, under normal circumstances, atonia ends upon waking up, so a person never becomes conscious of this inability to move.
As a result, researchers believe that sleep paralysis involves a mixed state of consciousness that blends both wakefulness and REM sleep. In effect, the atonia and mental imagery of REM sleep seems to persist even into a state of being aware and awake.
What Are the Types of Sleep Paralysis?
In the medical literature, two terms are commonly used to categorize cases of sleep paralysis.
- Isolated sleep paralysis is when the episodes are not connected to an underlying diagnosis of narcolepsy, a neurological disorder that prevents the brain from properly controlling wakefulness and often leads to sleep paralysis.
- Recurrent sleep paralysis involves multiple episodes over time.
In many cases, these two defining characteristics are combined to describe a condition of recurrent isolated sleep paralysis (RISP), which involves ongoing instances of sleep paralysis in someone who does not have narcolepsy.
What Does Sleep Paralysis Feel Like?
The fundamental symptom of sleep paralysis is atonia or the inability to move the body. It occurs shortly after falling asleep or waking up, and during an episode, a person feels awake and is aware of this loss of muscle control.
An estimated 75% of sleep paralysis episodes involve hallucinations that are distinct from typical dreams. As with atonia, these can occur when falling asleep (hypnagogic hallucinations) or waking up (hypnopompic hallucinations).
As with atonia, these can occur when falling asleep (hypnagogic hallucinations) or waking up (hypnopompic hallucinations).
Hallucinations during sleep paralysis fall into three categories:
- Intruder hallucinations, which involve the perception of a dangerous person or presence in the room.
- Chest pressure hallucinations, also called incubus hallucinations, that can incite a feeling of suffocation. These frequently occur along with intruder hallucinations.
- Vestibular-motor (V-M) hallucinations, which can include feelings of movement (such as flying) or out-of-body sensations.
Atonia is often distressing, and troubling hallucinations can make sleep paralysis episodes even more bothersome. For this reason, around 90% of episodes are associated with fear while only the minority have more pleasant or even blissful hallucinations. The perception of these episodes has been found to vary significantly based on a person’s cultural context.
Episodes can last from a few seconds to around 20 minutes, and the average length is between six and seven minutes. In most cases, episodes end on their own but occasionally are interrupted by another person’s touch or voice or by an intense effort to move that overcomes atonia.
How Common Is Sleep Paralysis?
Estimates vary, but researchers believe that about 8% of people experience sleep paralysis at some point in their life. Among these people, there is little data about how often episodes recur.
Sleep paralysis can occur at any age, but first symptoms often show up in childhood, adolescence, or young adulthood (ages 7 to 25). After starting in the teenage years, episodes may occur more frequently in the 20s and 30s.
What Causes Sleep Paralysis?
The exact cause of sleep paralysis is unknown. Studies have examined data to see what is associated with a higher risk of sleep paralysis and have found mixed results. Based on that research, researchers believe that multiple factors are involved in provoking sleep paralysis.
Sleep disorders and other sleeping problems have shown some of the strongest correlations with isolated sleep paralysis. Higher rates of sleep paralysis — 38% in one study — are reported by people with obstructive sleep apnea (OSA), a sleep disorder of repeated lapses in breathing. Sleep paralysis also has been found to be more common in people with nighttime leg cramps.
Insomnia symptoms like having a hard time falling asleep and excessive daytime sleepiness have been found to be associated with sleep paralysis. People whose circadian rhythms are not aligned with their local day-night cycle, such as people with jet lag and shift workers, may also be at higher risk of sleep paralysis.
Certain mental health conditions have shown a connection with sleep paralysis. People with anxiety disorders, including panic disorder, appear to be more likely to experience the condition. Some of the strongest associations are in people with post-traumatic stress disorder (PTSD) and others who have had exposure to childhood sexual abuse or other types of physical and emotional distress. Stopping alcohol or antidepressants can also lead to REM rebound, which may cause sleep paralysis too.
Stopping alcohol or antidepressants can also lead to REM rebound, which may cause sleep paralysis too.
Studies have found a higher risk in people with a family history of sleep paralysis, but no specific genetic basis has been identified.
Some studies have found that people who show traits of imaginativeness and disassociating from their immediate environment, such as with daydreaming, are more likely to experience sleep paralysis. There may be a link as well between sleep paralysis and vivid nightmares and/or lucid dreaming.
With all of these correlations, it is unknown whether there is any causation, and if so, whether sleep paralysis is the cause, effect, or if the relationship is bidirectional. Further research is necessary to investigate these correlations and better understand the numerous potential causes of sleep paralysis.
Is Sleep Paralysis a Serious Problem?
For most people, sleep paralysis is not a serious problem. It is classified as a benign condition and usually does not happen frequently enough to cause significant health problems.
However, an estimated 10% of people have more recurrent or bothersome episodes that make sleep paralysis especially distressing. As a result, they may develop negative thoughts about going to bed, reducing time allotted for sleep or provoking anxiety around bedtime that makes it harder to fall asleep. Sleep deprivation can lead to excessive sleepiness and numerous other consequences for a person’s overall health.
Treatments for Sleep Paralysis
A first step in treating sleep paralysis is to talk with a doctor in order to identify and address underlying problems that may be contributing to the frequency or severity of episodes. For example, this could involve treatment for narcolepsy or steps to better manage sleep apnea.
Overall, there is limited scientific evidence about the optimal treatment for sleep paralysis. Many people don’t know that the condition is relatively common and thus see themselves as crazy or shameful after episodes. As a result, even just the acknowledgement and normalization of their symptoms by a doctor can be beneficial.
Because of the connection between sleep paralysis and general sleeping problems, improving sleep hygiene is a common focus in preventing sleep paralysis. Sleep hygiene refers to a person’s bedroom setting and daily habits that influence sleep quality.
Examples of healthy sleep tips that can contribute to better sleep hygiene and more consistent nightly rest include:
- Following the same schedule for going to bed and waking up every day, including on weekends.
- Keeping a set pre-bed routine that helps you get comfortable and relaxed.
- Outfitting your bed with the best mattress and best pillow for your needs.
- Setting up your bedroom to have limited intrusion from light or noise.
- Reducing consumption of alcohol and caffeine, especially in the evening.
- Putting away electronic devices, including cell phones, for at least a half-hour before bed.
Improving sleep hygiene is frequently incorporated into cognitive behavioral therapy for insomnia (CBT-I), a type of talk therapy that works to reframe negative thoughts and emotions that detract from sleep.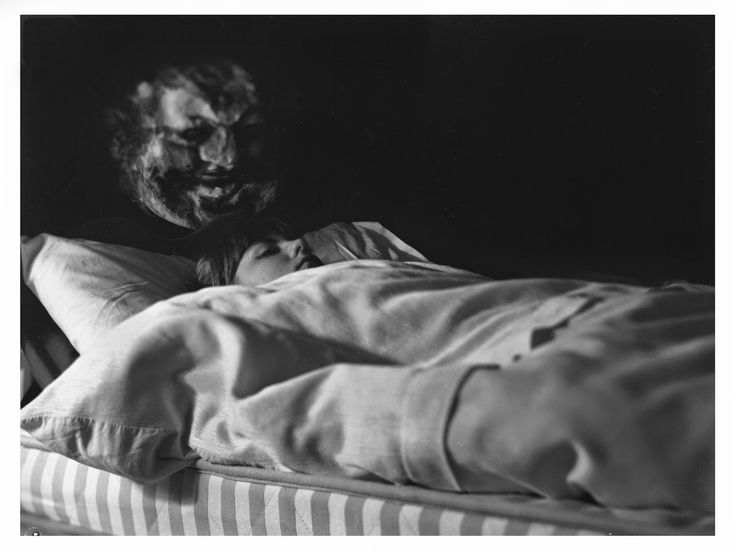
A specific form of CBT has been developed for sleep paralysis, but more research is needed to validate its effectiveness. CBT has an established track record in addressing mental health conditions like anxiety and PTSD that may be factors influencing the risk of sleep paralysis.
Some medications are known to suppress REM sleep, and these may help to stop sleep paralysis. These medications can have side effects, though, and may cause a rebound in REM sleep when someone stops taking them. For these reasons, it’s important to talk with a doctor before taking any medication in order to discuss its potential benefits and downsides.
- Was this article helpful?
- YesNo
References
+12 Sources
-
1.
Brooks, P., & Peever, J. (2008, November 1). Unraveling the mechanisms of REM sleep atonia. Nature and Science of Sleep, 10, 355-367. https://pubmed.ncbi.nlm.nih.gov/19226735/
-
2.

Denis D. (2018). Relationships between sleep paralysis and sleep quality: Current insights. Nature and Science of Sleep, 10, 355–367. https://pubmed.ncbi.nlm.nih.gov/30464663/
-
3.
Denis, D., French, C. C., & Gregory, A. M. (2018). A systematic review of variables associated with sleep paralysis. Sleep Medicine Reviews, 38, 141–157. https://pubmed.ncbi.nlm.nih.gov/28735779/
-
4.
Olunu, E., Kimo, R., Onigbinde, E.O., Akpanobong, M.A.U., Enang, I.E., Osanakpo, M., Monday, I.T., Otohinoyi, D.A., & Fakoya A.O. Sleep paralysis, a medical condition with a diverse cultural interpretation. International Journal of Applied & Basic Medical Research, 8(3), 137–142. https://pubmed.ncbi.nlm.nih.gov/30123741/
-
5.
Sharpless B. A. (2016). A clinician's guide to recurrent isolated sleep paralysis. Neuropsychiatric Disease and Treatment, 12, 1761–1767. https://pubmed.ncbi.nlm.nih.gov/27486325/
-
6.
National Institute of Neurological Disorders and Stroke.
 Narcolepsy fact sheet. (2020, March 16). Retrieved August 05, 2020, from https://www.ninds.nih.gov/disorders/patient-caregiver-education/fact-sheets/narcolepsy-fact-sheet
Narcolepsy fact sheet. (2020, March 16). Retrieved August 05, 2020, from https://www.ninds.nih.gov/disorders/patient-caregiver-education/fact-sheets/narcolepsy-fact-sheet -
7.
Hsieh, S. W., Lai, C. L., Liu, C. K., Lan, S. H., & Hsu, C. Y. (2010). Isolated sleep paralysis linked to impaired nocturnal sleep quality and health-related quality of life in Chinese-Taiwanese patients with obstructive sleep apnea. Quality of Life Research, 19(9), 1265–1272. https://pubmed.ncbi.nlm.nih.gov/20577906/
-
8.
Singh, S., Kaur, H., Singh, S., & Khawaja, I. (2018). Parasomnias: A comprehensive review. Cureus, 10(12), e3807. https://pubmed.ncbi.nlm.nih.gov/30868021/
-
9.
Denis, D., & Poerio, G. L. (2017). Terror and bliss? Commonalities and distinctions between sleep paralysis, lucid dreaming, and their associations with waking life experiences. Journal of Sleep Research, 26(1), 38–47. https://pubmed.ncbi.nlm.nih.gov/27460633/
-
10.

Denis, D., French, C. C., Schneider, M. N., & Gregory, A. M. (2018). Subjective sleep-related variables in those who have and have not experienced sleep paralysis. Journal of Sleep Research, 27(5), e12650. https://pubmed.ncbi.nlm.nih.gov/29280229/
-
11.
Kaczkurkin, A. N., & Foa, E. B. (2015). Cognitive-behavioral therapy for anxiety disorders: an update on the empirical evidence. Dialogues in Clinical Neuroscience, 17(3), 337–346. https://pubmed.ncbi.nlm.nih.gov/26487814/
-
12.
A.D.A.M. Medical Encyclopedia. (2021, April 19). Sleep paralysis. MedlinePlus. Retrieved June 23, 2022, from https://medlineplus.gov/ency/article/000801.htm
See More
Sleep paralysis: causes, symptoms, treatment
Summary. Knowledge of the mechanisms of the development of the disease can help to overcome it
Sleep paralysis (sleep stupor) - a condition characterized by temporary paralysis with preserved consciousness; usually occurs when falling asleep or at the moment of awakening.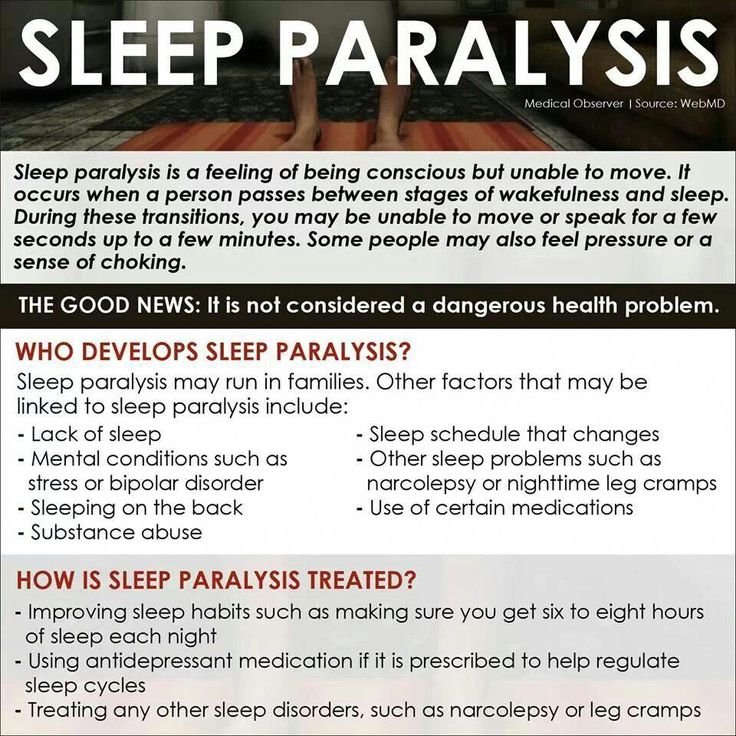 This pathology is often accompanied by complex hallucinations and intense fear. The phenomenon of sleep paralysis occurs in 5-40% of people aged 12-30 years, most common among people with narcolepsy. Sleep stupor is considered to be physically harmless, but misunderstanding of the essence with its regular experience is a significant psychological trauma.
This pathology is often accompanied by complex hallucinations and intense fear. The phenomenon of sleep paralysis occurs in 5-40% of people aged 12-30 years, most common among people with narcolepsy. Sleep stupor is considered to be physically harmless, but misunderstanding of the essence with its regular experience is a significant psychological trauma.
Sleep paralysis is mentioned in different cultures. Among the Slavic peoples, it is associated with mara (kikimora), a nightlight (demon), which jumps on its chest in the middle of the night to warn of good or bad. In Mexico they say “the corpse climbed on me”, in Newfoundland (Canada) they call this state “the old witch”, in the Muslim tradition, sleep paralysis is attributed to the tricks of genies.
This pathology was the basis of the series of works of the Swiss-English artist Henry Fuseli "Nightmare". In four paintings, the artist depicted a sleeping woman with an incubus (in medieval legends, a dissolute demon) on her chest, the embodiment of unconscious fears.
Signs and symptoms of sleep paralysis:
- inability to move, lasting from a few seconds to a few minutes;
- preservation of consciousness;
- inability to speak;
- hallucinations and frightening sensations;
- feeling of pressure on the chest, bed moving, doors opening;
- inability to separate reality from fiction;
- feeling of impending death;
- intense perspiration;
- headache and muscle pain;
- paranoia.
Sleep paralysis usually occurs when a person sleeps on their back. The predisposing factors of the pathology are excessive tension, overexcitation, jet lag after a long flight, changes in sleep patterns, and associated panic disorders. This pathology can be a symptom of other diseases: depression, migraine, narcolepsy, obstructive sleep apnea syndrome, arterial hypertension and anxiety disorders.
The hypnotic episodes characteristic of sleep paralysis are of 3 types:
- sensations of the presence of an "intruder": opening doors, shuffling feet, a person in the shadows, a humanoid, a foreigner, etc.
 ;
; - incubus: feeling of pressure on the chest, difficulty in breathing, suffocation, sexual violence;
- vestibulo-motor hallucinations: sensation of falling, swimming, flying, hovering over one's body.
Sleep paralysis is based on desynchronization of brain and muscle activity during REM sleep. So, during this period, the parts of the brain responsible for identifying situations that threaten a person are in a state of increased sensitivity, perceiving everyday sounds and other stimuli, usually ignored by the brain, as a potential danger.
Since sleep paralysis often occurs against the background of uncontrolled chronic stress and sleep disturbances, the correction of this condition is primarily associated with the elimination of these factors.
Doctors advise:
- even on weekends and holidays, adhere to the same sleep-wake schedule;
- create favorable conditions for sleep: comfortable mattress, bedding and underwear, as well as a clean, dark, cool bedroom;
- reduce the brightness of the lighting in the evening hours, as well as provide a dim night lighting;
- intense daylight;
- avoid naps after 3 pm, limit nap duration to ≤90 min;
- do not eat 2 hours before bedtime, refrain from evening alcohol and caffeine;
- daily exercise, but no later than 2 hours before bedtime;
- create a ritual with soothing activities before bed, such as listening to soothing music, reading, etc.
 ;
; - avoid email at least 1 hour before bedtime.
Doctors also recommend reducing stimulant use, meditating or praying regularly, learning to control depression or anxiety, and avoiding sleeping on your back.
Survivors of sleep paralysis are advised not to withdraw into themselves, to discuss the problem with relatives and friends, to seek help from a specialist.
Anna Antonyuk
Sleep paralysis: causes, types, mechanism of occurrence
Sleep paralysis is a violation of the processes of falling asleep, awakening. It is characterized by complete muscular atony against the background of wakefulness of consciousness. The vast majority develops at the time of awakening. Accompanied by hallucinations, fear, inability to move.
Causes of sleep paralysis
Sleep paralysis occurs most often in the supine position. Provoking factors can be overexertion, overexcitation, disruption of biorhythms, panic disorders.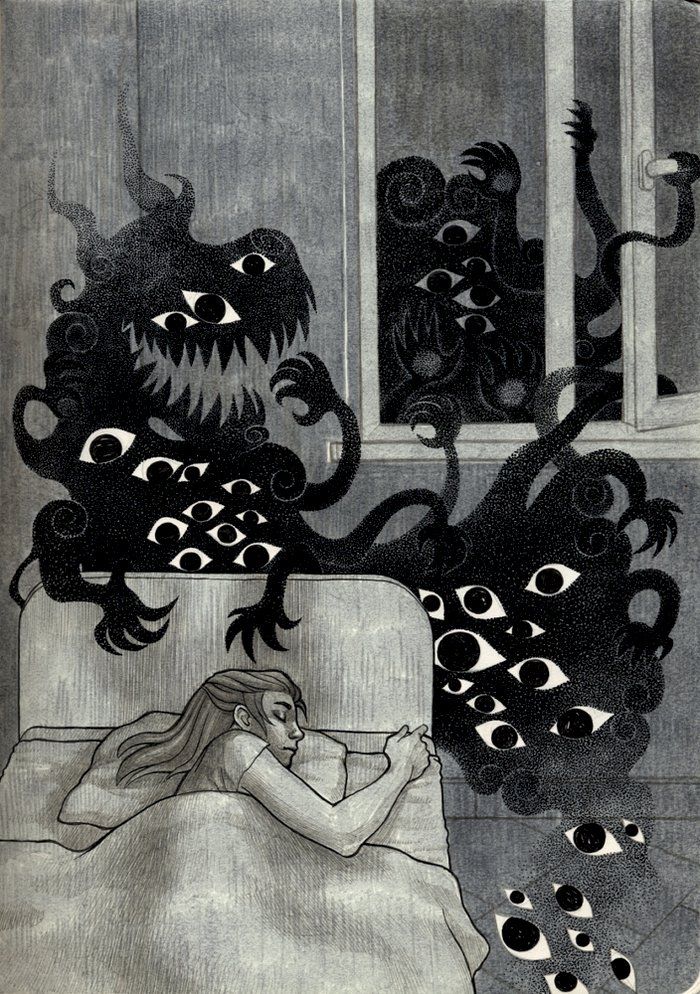 Paralytic sleep can be a symptom of the following diseases:
Paralytic sleep can be a symptom of the following diseases:
- narcolepsy;
- migraine;
- sleepwalking;
- arterial hypertension;
- anxiety disorders;
- depression;
- obstructive sleep apnea syndrome.
Important! Sleep paralysis can occur in a healthy person if the sleep pattern is disturbed. Rarely, this condition occurs in the position on the side or on the stomach - mainly when the person lies on his back.
Why sleep paralysis happens
Sleep begins with a slow phase and moves into a fast one. The latter is characterized by a decrease in muscle tone except for the respiratory ones. The rhythm of breathing is accelerated, the breath is short. The activity of the brain becomes as in wakefulness. During sleep paralysis, the sequence of processes is disrupted. Consciousness wakes up before muscle tone is restored. As a result, there is a state of immobility, which is called sleep paralysis. It can occur when falling asleep, when the phase of REM sleep begins, and consciousness is still awake.
It can occur when falling asleep, when the phase of REM sleep begins, and consciousness is still awake.
In the fast phase of sleep, a reflex setting of breathing occurs. If the awakened person tries to take a deep breath, he will not succeed. This causes a feeling of tightness in the chest. The inability to make movements is perceived by the brain as a threat. Large amounts of neurotransmitters are released. It is they who give rise to fear, hallucinations, panic. The vestibular apparatus is also active. But due to the lack of movement, he does not receive signals, there is a feeling of flight.
Sleep paralysis symptoms
The pathological condition resembles a stroke, paralysis. A person is not able to perform actions, move. This condition is accompanied by the following symptoms:
- fear;
- panic;
- auditory and visual hallucinations.
Patients report that they see hostile creatures, dark figures, hear hum, noise, squeak. There is an illusion of flight, soaring, circling.
There is an illusion of flight, soaring, circling.
The main complaints are:
- feeling of tightness in the chest;
- suffocation;
- inability to breathe.
Paralytic sleep lasts from 2 seconds to 3 minutes. In the post-attack state, neurological symptoms are absent. The frequency of attacks varies from one to three per night. There are no complications, serious asphyxia, life-threatening. Therefore, it is not possible to die from sleep paralysis. However, getting out of it on your own is quite problematic.
Book an online consultation if you are concerned about sleep paralysis. Our neurologists will sort out the causes, psychiatrists will provide psychological support, draw up a plan for further actions, and will be in touch at any time of the day.
Types of sleep paralysis
The classification is based on the belonging of seizures to the period of falling asleep or awakening. There are the following types of parasomnia:
There are the following types of parasomnia:
| Name | Description |
| hypnopompic | Characteristic for the period of waking up. Doesn't happen often. Patients complain that they feel immobile before falling asleep |
| hypnagogic | Occurs during the transition to sleep. A pronounced clinical picture is characteristic |
Example A man came tired from work and decided to rest. Darkness, but his feelings remained. It seemed to him that he was drunk and falling somewhere. Then someone's steps were heard. At that moment, the man woke up and heard that someone was walking around the apartment. He couldn't move at all. Then he felt as if someone sat on his feet. And then began to rise higher on his body. It feels like a press has fallen on his chest. Breathing is difficult, a whisper is heard in the ear, hot breathing. The man understood what was happening to him. Gathered all the will into a fist to withstand another 30 seconds of this horror.
Breathing is difficult, a whisper is heard in the ear, hot breathing. The man understood what was happening to him. Gathered all the will into a fist to withstand another 30 seconds of this horror.
Pathology diagnostics
Night paralysis is diagnosed according to the clinical picture. Specific examinations are carried out with frequently recurring episodes. This allows you to exclude psychological, neurological pathology:
- examination by a neurologist;
- polysomnography captures a paralytic episode;
- electroencephalopathy makes it possible to differentiate sleep paralysis from epileptic paroxysms;
- The MSLT test is done to check for narcolepsy;
- work with a psychiatrist.
Differential diagnosis is carried out with apnea, somnambulism, narcolepsy, mental illness.
Night paralysis treatment
You can get rid of this condition by working with a psychotherapist, a neurologist. Measures are being taken to normalize sleep, psychological relaxation before going to bed. It is possible to fight sleep paralysis with the help of medications in cases of mental illness. neurological disorders. You can avoid night attacks if you follow the general recommendations:
Measures are being taken to normalize sleep, psychological relaxation before going to bed. It is possible to fight sleep paralysis with the help of medications in cases of mental illness. neurological disorders. You can avoid night attacks if you follow the general recommendations:
- avoid physical. mental overload;
- set a time for going to bed and stick to it;
- before going to bed, give up gadgets, TV;
- try to relax before bed. It can be massage, aromatherapy, scented salt baths;
- you should wake up on an alarm clock, since parasomnias are most often recorded during self-awakening.
Sign up for an online consultation if you are worried about sleep fears, you are afraid of sleep paralysis. Our psychologists and neurologists will take a comprehensive approach to solving your problem: they will provide psychological assistance, teach you how to control emotions, work through fears, select analogues of drugs if necessary, and advise clinics for examination.
Complications of sleep paralysis
Sleep numbness in itself is not dangerous to human health. Undesirable consequences arise from the psychological side. A person begins to be afraid to fall asleep, tries to drink more coffee, energy drinks. Stupor can provoke neurological, psychological problems, which will subsequently need to be treated and corrected.
Another danger is obsession with what is happening. A person begins to believe that he has an incurable disease, which will lead to neurosis. Sleep paralysis brings the greatest harm to people who associate it with otherworldly forces, evil, and mysticism.
Is it possible to cause sleep paralysis when falling asleep
Despite the fact that this state is not a pleasant one, there are those who wish to experience sleep paralysis for themselves. Its appearance for them is associated with the ability to move around in the worlds, to see hallucinations, to fly, to predict the future.![]()
Such people can lie still, completely relaxed, day or night. First the eyes are open, then they lie closed. Auditory hallucinations and vibrations may appear. The intensification and duration of these sensations depend on the degree of fatigue and the environment. Increased vibrations will indicate tactile hypnagogic hallucinations. They are possible only during the period of falling asleep and sleep paralysis occurs.
Important! It is possible to induce numbness in sleep. But you shouldn't do it. This is an abnormal state of the body in which no predictions occur, since hallucinations are a figment of the imagination.
FAQ
What do you see with sleep paralysis?
+
Moving shadows, ugly people, evil creatures, dead relatives - all this is seen by a person with sleep parasomnia. However, visual hallucinations may not be - only auditory.
How to avoid sleep paralysis?
+
Try to establish a daily routine, abstract from stress, do not overload. This is where sleep paralysis can be hidden. In addition, it is necessary to be able to combine work and rest. If paralysis nevertheless happened, it is important to remember that this is only a delusion of the imagination and it can be cured.
This is where sleep paralysis can be hidden. In addition, it is necessary to be able to combine work and rest. If paralysis nevertheless happened, it is important to remember that this is only a delusion of the imagination and it can be cured.
How long does sleep paralysis last?
+
Sometimes sleep paralysis lasts up to 20 minutes. For patients, this time seems like an eternity and is experienced quite hard due to auditory, visual hallucinations. There can be up to three such attacks per night.
Who gets sleep paralysis?
+
It occurs between the ages of 7 and 25. It occurs in 8-10 percent of the population. The average duration of an attack is up to 4 minutes. However, it does not depend on the gender of the person.
Expert opinion
Sleep when you cannot move is called sleep paralysis. From the outside, it looks like a person has woken up, but at the same time he does not make movements, he cannot say anything. At this moment, he can hear sounds, noises, voices, see different creatures. A feeling of fear and panic sets in. Many patients complained about the inability to take a deep breath, heaviness in the chest. It is impossible to die from this condition, but it is possible to get psychological and neurological problems because of the fear of falling asleep and experiences from what you see.
At this moment, he can hear sounds, noises, voices, see different creatures. A feeling of fear and panic sets in. Many patients complained about the inability to take a deep breath, heaviness in the chest. It is impossible to die from this condition, but it is possible to get psychological and neurological problems because of the fear of falling asleep and experiences from what you see.
We publish only verified information
Article author
Agishev Damir Adgemovich doctor - neurologist
Experience 35 years
Consultations 1121
Articles 130
Specialist with many years of experience working with patients.