Faking an illness
Overview - Munchausen syndrome - NHS
Munchausen syndrome is a psychological condition where someone pretends to be ill or deliberately produces symptoms of illness in themselves.
Their main intention is to assume the "sick role" so that people care for them and they are the centre of attention.
Any practical benefit in pretending to be sick – for example, claiming incapacity benefit – is not the reason for their behaviour.
Munchausen syndrome is named after a German aristocrat, Baron Munchausen, who became famous for telling wild, unbelievable tales about his exploits.
Types of behaviour
People with Munchausen syndrome can behave in a number of different ways, including:
- pretending to have psychological symptoms – for example, claiming to hear voices or claiming to see things that are not really there
- pretending to have physical symptoms – for example, claiming to have chest pain or a stomach ache
- actively trying to get ill – such as deliberately infecting a wound by rubbing dirt into it
Some people with Munchausen syndrome may spend years travelling from hospital to hospital faking a wide range of illnesses. When it's discovered they're lying, they may suddenly leave hospital and move to another area.
People with Munchausen syndrome can be very manipulative and, in the most serious cases, may undergo painful and sometimes life-threatening surgery, even though they know it's unnecessary.
Read more about the signs and symptoms of Munchausen syndrome
What causes Munchausen syndrome?
Munchausen syndrome is complex and poorly understood. Many people refuse psychiatric treatment or psychological profiling, and it's unclear why people with the syndrome behave the way they do.
Several factors have been identified as possible causes of Munchausen syndrome. These include:
- emotional trauma or illness during childhood – this often resulted in extensive medical attention
- a personality disorder – a mental health condition that causes patterns of abnormal thinking and behaviour
- a grudge against authority figures or healthcare professionals
Childhood trauma
Munchausen syndrome may be caused by parental neglect and abandonment, or other childhood trauma.
As a result of this trauma, a person may have unresolved issues with their parents that cause them to fake illness. They may do this because they:
- have a compulsion to punish themselves by making themselves ill because they feel unworthy
- need to feel important and be the centre of attention
- need to pass responsibility for their wellbeing and care on to other people
There's also some evidence to suggest people who have had extensive medical procedures, or received prolonged medical attention during childhood or their teenage years, are more likely to develop Munchausen syndrome when they're older.
This may be because they associate their childhood memories with a sense of being cared for. As they get older, they try to obtain the same feelings of reassurance by pretending to be ill.
Personality disorders
Different personality disorders thought to be linked with Munchausen syndrome include:
- antisocial personality disorder – where a person may take pleasure in manipulating and deceiving doctors, giving them a sense of power and control
- borderline personality disorder – where a person struggles to control their feelings and often swings between positive and negative views of others
- narcissistic personality disorder – where a person often swings between seeing themselves as special and fearing they're worthless
It could be that the person has an unstable sense of their own identity and also has difficulty forming meaningful relationships with others.
Playing the "sick role" allows them to adopt an identity that brings support and acceptance from others with it. Admission to hospital also gives the person a clearly defined place in a social network.
Diagnosing Munchausen syndrome
Diagnosing Munchausen syndrome can be challenging for medical professionals.
People with the syndrome are often very convincing and skilled at manipulating and exploiting doctors.
Investigating claims
If a healthcare professional suspects a person may have Munchausen syndrome, they'll look at the person's health records to check for inconsistencies between their claimed and actual medical history.
Healthcare professionals can also run tests to check for evidence of self-inflicted illness or tampering with clinical tests. For example, the person's blood can be checked for traces of medicine they should not be taking but which could explain their symptoms.
For example, the person's blood can be checked for traces of medicine they should not be taking but which could explain their symptoms.
Doctors will also want to rule out other possible motivations for their behaviour, such as faking illness for financial gain or because they want access to strong painkillers.
Munchausen syndrome can usually be diagnosed if:
- there's clear evidence of fabricating or inducing symptoms
- the person's prime motivation is to be seen as sick
- there's no other likely reason or explanation for their behaviour
Treating Munchausen syndrome
Treating Munchausen syndrome can be difficult because most people with it refuse to admit they have a problem and refuse to co-operate with treatment plans.
Some experts recommend that healthcare professionals should adopt a gentle non-confrontational approach, suggesting the person may benefit from a referral to a psychiatrist.
Others argue that a person with Munchausen syndrome should be confronted directly and asked why they've lied and whether they have stress and anxiety.
People who have Munchausen syndrome have a genuine mental health condition, but will often only admit to having a physical illness.
If a person admits to their behaviour, they can be referred to a psychiatrist for further treatment. If they do not admit to lying, most experts agree the doctor in charge of their care should minimise medical contact with them.
This is because the doctor-patient relationship is based on trust and if there's evidence the patient can no longer be trusted, the doctor is unable to continue treating them.
Psychiatric treatment and CBT
It may be possible to help control the symptoms of Munchausen syndrome if the person admits they have a problem and co-operates with treatment.
There's no standard treatment for Munchausen syndrome, but a combination of psychoanalysis and cognitive behavioural therapy (CBT) has shown some success controlling symptoms.
Psychoanalysis is a type of psychotherapy that attempts to uncover and resolve unconscious beliefs and motivations.
CBT helps a person identify unhelpful and unrealistic beliefs and behavioural patterns. A specially trained therapist teaches the person ways of replacing unrealistic beliefs with more realistic and balanced ones.
Family therapy
People with Munchausen syndrome still in close contact with their family may also benefit from having family therapy.
The person with the syndrome and their close family members discuss how it's affected the family and the positive changes that can be made.
It can also teach family members how to avoid reinforcing the person's abnormal behaviour. For example, this could involve recognising when the person is playing the "sick role" and avoiding showing them concern or offering support.
For example, this could involve recognising when the person is playing the "sick role" and avoiding showing them concern or offering support.
Who's affected by Munchausen syndrome?
There appear to be 2 separate groups of people affected by Munchausen syndrome. They are:
- women who are 20 to 40 years of age, often with a background in healthcare
- unmarried white men who are 30 to 50 years of age
It's unclear why these 2 groups tend to be affected by Munchausen syndrome.
Some experts believe Munchausen syndrome is underdiagnosed because many people succeed in deceiving medical staff. It's also possible cases may be overdiagnosed as the same person could use different identities.
Fabricated or induced illness
Fabricated or induced illness, which used to be known as Munchausen syndrome by proxy, is a related condition.
This is where a person fakes or induces illness in a person under their care, such as their child.
Video: Munchausen syndrome
In this video, an expert discusses Munchausen syndrome and Munchausen by proxy (fabricated or induced illness).
Media last reviewed: 7 December 2021
Media review due: 7 December 2024
Factitious disorder - Symptoms and causes
Overview
Factitious disorder is a serious mental disorder in which someone deceives others by appearing sick, by purposely getting sick or by self-injury. Factitious disorder also can happen when family members or caregivers falsely present others, such as children, as being ill, injured or impaired.
Factitious disorder symptoms can range from mild (slight exaggeration of symptoms) to severe (previously called Munchausen syndrome). The person may make up symptoms or even tamper with medical tests to convince others that treatment, such as high-risk surgery, is needed.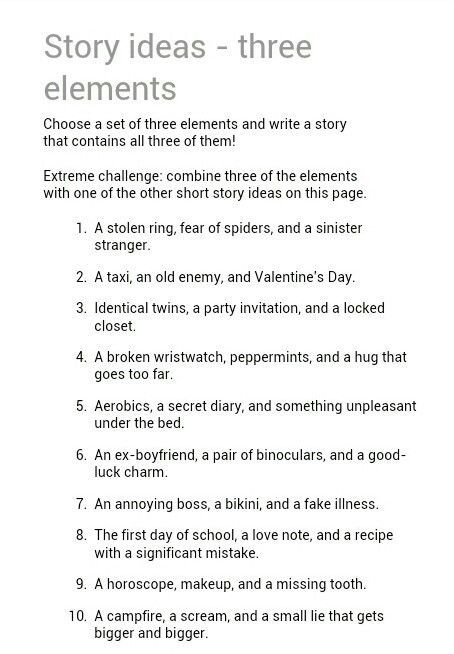
Factitious disorder is not the same as inventing medical problems for practical benefit, such as getting out of work or winning a lawsuit. Although people with factitious disorder know they are causing their symptoms or illnesses, they may not understand the reasons for their behaviors or recognize themselves as having a problem.
Factitious disorder is challenging to identify and hard to treat. However, medical and psychiatric help are critical for preventing serious injury and even death caused by the self-harm typical of this disorder.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms
Factitious disorder symptoms involve mimicking or producing illness or injury or exaggerating symptoms or impairment to deceive others. People with the disorder go to great lengths to hide their deception, so it may be difficult to realize that their symptoms are actually part of a serious mental health disorder. They continue with the deception, even without receiving any visible benefit or reward or when faced with objective evidence that doesn't support their claims.
They continue with the deception, even without receiving any visible benefit or reward or when faced with objective evidence that doesn't support their claims.
Factitious disorder signs and symptoms may include:
Clever and convincing medical or psychological problems
- Extensive knowledge of medical terms and diseases
- Vague or inconsistent symptoms
- Conditions that get worse for no apparent reason
- Conditions that don't respond as expected to standard therapies
- Seeking treatment from many different doctors or hospitals, which may include using a fake name
- Reluctance to allow doctors to talk to family or friends or to other health care professionals
- Frequent stays in the hospital
- Eagerness to have frequent testing or risky operations
- Many surgical scars or evidence of numerous procedures
- Having few visitors when hospitalized
- Arguing with doctors and staff
Factious disorder imposed on another
Factitious disorder imposed on another (previously called Munchausen syndrome by proxy) is when someone falsely claims that another person has physical or psychological signs or symptoms of illness, or causes injury or disease in another person with the intention of deceiving others.
People with this disorder present another person as sick, injured or having problems functioning, claiming that medical attention is needed. Usually this involves a parent harming a child. This form of abuse can put a child in serious danger of injury or unnecessary medical care.
How those with factitious disorder fake illness
Because people with factitious disorder become experts at faking symptoms and diseases or inflicting real injuries upon themselves, it may be hard for health care professionals and loved ones to know if illnesses are real or not.
People with factitious disorder make up symptoms or cause illnesses in several ways, such as:
- Exaggerating existing symptoms. Even when an actual medical or psychological condition exists, they may exaggerate symptoms to appear sicker or more impaired than is true.
- Making up histories. They may give loved ones, health care professionals or support groups a false medical history, such as claiming to have had cancer or AIDS.
 Or they may falsify medical records to indicate an illness.
Or they may falsify medical records to indicate an illness. - Faking symptoms. They may fake symptoms, such as stomach pain, seizures or passing out.
- Causing self-harm. They may make themselves sick, for example, by injecting themselves with bacteria, milk, gasoline or feces. They may injure, cut or burn themselves. They may take medications, such as blood thinners or drugs for diabetes, to mimic diseases. They may also interfere with wound healing, such as reopening or infecting cuts.
- Tampering. They may manipulate medical instruments to skew results, such as heating up thermometers. Or they may tamper with lab tests, such as contaminating their urine samples with blood or other substances.
When to see a doctor
People with factitious disorder may be well aware of the risk of injury or even death as a result of self-harm or the treatment they seek, but they can't control their behaviors and they're unlikely to seek help. Even when confronted with objective proof — such as a videotape — that they're causing their illness, they often deny it and refuse psychiatric help.
Even when confronted with objective proof — such as a videotape — that they're causing their illness, they often deny it and refuse psychiatric help.
If you think a loved one may be exaggerating or faking health problems, it may help to attempt a gentle conversation about your concerns. Try to avoid anger, judgment or confrontation. Also try to reinforce and encourage more healthy, productive activities rather than focusing on dysfunctional beliefs and behaviors. Offer support and caring and, if possible, help in finding treatment.
If your loved one causes self-inflicted injury or attempts suicide, call 911 or emergency medical help or, if you can safely do so, take him or her to an emergency room immediately.
Request an Appointment at Mayo Clinic
Causes
The cause of factitious disorder is unknown. However, the disorder may be caused by a combination of psychological factors and stressful life experiences.
Risk factors
Several factors may increase the risk of developing factitious disorder, including:
- Childhood trauma, such as emotional, physical or sexual abuse
- A serious illness during childhood
- Loss of a loved one through death, illness or abandonment
- Past experiences during a time of sickness and the attention it brought
- A poor sense of identity or self-esteem
- Personality disorders
- Depression
- Desire to be associated with doctors or medical centers
- Work in the health care field
Factitious disorder is considered rare, but it's not known how many people have the disorder. Some people use fake names to avoid detection, some visit many different hospitals and doctors, and some are never identified — all of which make it difficult to get a reliable estimate.
Some people use fake names to avoid detection, some visit many different hospitals and doctors, and some are never identified — all of which make it difficult to get a reliable estimate.
Complications
People with factitious disorder are willing to risk their lives to be seen as sick. They frequently have other mental health disorders as well. As a result, they face many possible complications, including:
- Injury or death from self-inflicted medical conditions
- Severe health problems from infections or unnecessary surgery or other procedures
- Loss of organs or limbs from unnecessary surgery
- Alcohol or other substance abuse
- Significant problems in daily life, relationships and work
- Abuse when the behavior is inflicted on another
Prevention
Because the cause of factitious disorder is unknown, there's currently no known way to prevent it. Early recognition and treatment of factitious disorder may help avoid unnecessary and potentially dangerous tests and treatment.
By Mayo Clinic Staff
Related
Products & Services
Rating of diseases that Russians simulate
Using the Yandex Wordstat tool, Life compiled a rating of symptoms that Russians most often simulate.
Doctors confirm that there are many malingerers.
- Patients with fictitious symptoms come in quite often. Usually they simulate ARVI, a headache,” says Irina Kutuzova, a local therapist at Diagnostic Center No. 5. - ARVI is easy enough to check - you need to measure the temperature, look at the throat. Headaches are more difficult. If, after the examination, I understand that I do not see any symptoms that would indicate a headache, then I refer the patient to a neurologist.
According to the therapist, malingerers usually get what they want.
“They pretend to get sick leave, but for what purposes they need it – not to go to work or something else, I don’t know,” said Irina Kutuzova. — But we usually always go towards patients. It is better to double-check everything, put a person on sick leave and conduct a full examination so as not to miss any serious illness. There are very rude patients. They frankly feign, and when you tell them about it, they also begin to be rude - they say they don’t want to be treated.
It is better to double-check everything, put a person on sick leave and conduct a full examination so as not to miss any serious illness. There are very rude patients. They frankly feign, and when you tell them about it, they also begin to be rude - they say they don’t want to be treated.
Simulators who failed to get sick leave tell their employers that they have poisoned themselves.
- If employees want to "slop down", then most often they complain about poisoning. They say, “Oh, I ate something wrong yesterday, I’ll stay at home today, suddenly poisoning,” said Oksana Rykova, head of the recruitment department at Avtomir.
According to her, such complaints can often be heard before or immediately after a long weekend or vacation. This suggests that employees are simply not averse to extending their vacation at the expense of sick leave.
Lines of malingerers are lining up at the military registration and enlistment offices.
— When I was undergoing a medical examination, on the advice of my acquaintances from medical students, before going to the doctor's office, I squatted many times to increase my pulse, — Muscovite Daniil said. - And when the doctor measured the pressure, I strongly strained my calves - the pressure increased. As a result, in addition to flat feet, I was diagnosed with hypertension, and I did not get into the army.
- And when the doctor measured the pressure, I strongly strained my calves - the pressure increased. As a result, in addition to flat feet, I was diagnosed with hypertension, and I did not get into the army.
Students know the secrets of simulation very well.
“Before an important test or exam, when you are not prepared and your chances of passing are zero, it is always easier to get sick,” says student Daria. - You will be scheduled an exam for the next day, and all classmates will tell you what happened at the exam. It's easier to give up. Here all means are good.
Simulation is learned at school.
“When I was in the fifth grade, my classmates put glue in their noses,” said student Mikhail. - Their snot began to flow, their eyes watered. They went to the nurse and said they had a runny nose. And then they went home.
According to doctors, in such cases, the malingerers can achieve even more success than they expect - that is, actually get sick.
“If you drop glue into your nose, you can completely burn the mucous membrane,” says Irina Kutuzova. - So there may be toxic poisoning and an allergic reaction, up to Quincke's edema.
Other "bad advice" can be found on the Internet. For example, those who are looking for how to simulate a concussion are advised to bang their head against the wall - so that later they can show the doctor a lump or a bruise.
“If you do this, you can get a real concussion, you won’t have to simulate it,” comments Irina Kutuzova.
Faking fainting is more difficult. As Internet sources advise, you need to squat down, hold your breath, and then stand up abruptly. With such an exercise, the head should spin and the coordination of movements should be disturbed.
“If initially there is no pathology with the heart and blood vessels, then such an experiment can pass without consequences,” says Irina Kutuzova. “But it’s not certain that you will faint from it. And if you fall, then do not forget that the lack of oxygen in the brain, even for a short time, can affect its activity. And if you fall, you can get a head injury, even fatal.
And if you fall, you can get a head injury, even fatal.
How to feign an illness (instruction) - In passing ... — LiveJournal
The article is intended for easy lies in order to obtain a sick leave and can hardly be used for another purpose.
Everyone has a situation when they “need sick leave”. Before simulating a disease, it is worth remembering that a doctor is also a person to whom you can explain something, ask, thank, but if there is no other way out, it is worth trying.
What disease to simulate?
You need to decide how many days you need a sick leave, and which specialist in your clinic is most likely to cheat? It should be borne in mind that a visit to the clinic will be necessary to extend the disability and it is unlikely that you will be able to leave somewhere for a month. It is worth enlisting the support of relatives who will be able to confirm your legend and cover up with an unexpected visit to the doctor at home.
It is better to simulate a disease that does not require any serious additional methods of examination, since the chance of detection increases and a lot of time is spent walking around the offices. The therapist is not the best option, because they are trained to recognize left-handed ARIs and have a limit on issuing sick leave. I recommend a neurologist.
The therapist is not the best option, because they are trained to recognize left-handed ARIs and have a limit on issuing sick leave. I recommend a neurologist.
Lumboischealgia (lumbago) for a week
Simulating such a disease is not difficult. The clinic is characterized by a variety of symptoms and comes down to back pain. Entering the office, limping slightly, not sitting down - it hurts. Complaints: pain in the back is constant, severe, I can’t bend over, it gets worse when coughing, laughing (I can’t laugh), it hurts to walk - it radiates to the back, and so on. It is better to choose one sore side, for example, everything happens on the left.
Anamnesis. Yesterday (digging a garden, carrying a piano, raising his wife) and shot like an electric shock. Barely crawled to the bed. Didn't get up. It hurts to roll over. A neighbor brought me to the clinic by car. I drank diclofenac at home (ortofen, voltaren, reopyrin, my wife even gave me Pentalgin) now I feel a little better.
Examination. Shout during palpation of the paravertebral points in the lumbar spine on the side of the lesion (left). It is better to remember the area of pain and say that everything gives back there. No need to replay. Slightly bend over - it hurts further. Understand the leg - slightly raise and further pain. To say that it used to be like this, but on vacation - I lay at home for a week and passed. The maximum examination is radiography, which will not show anything and will not reveal the simulation of the disease. Refuse other methods - CT or MRI (no money). Even though they won't reveal anything.
Concussion for a month
Complaints: headache, dizziness, nausea.
Anamnesis. Yesterday the door in the entrance was hit, I slipped, etc. I don’t remember exactly what happened - my wife said. I don't remember 2-3 minutes before the injury. Do not forget that there must be a hat on the head, otherwise the absence of a bump will be difficult to explain.