Crisis in psychiatry
Signs, Causes, and How to Get Help
The signs of a mental health crisis differ from person to person. Still, there are ways you can be ready in an emergency.
A mental health crisis is when someone’s behaviors prevent them from functioning or indicate they might harm themselves or others.
A crisis can feel overwhelming, and it might seem as if the coping skills you usually have no longer work.
Psychiatric crises and emergencies are unique to the person, but they can look similar in how a person experiences and behaves during the crisis.
Many people are unable to take care of themselves, have worsened symptoms of preexisting mental health conditions, and threaten or attempt self-harm.
Though untreated mental health conditions can lead to a crisis, it’s a misconception that this is the only time they occur. Things happen — mental health crises can occur in people without a diagnosed mental health condition and in people following a treatment plan.
Are you currently in crisis?
If you feel like you’re having a mental health emergency, you can:
- Call the 988 Suicide and Crisis Lifeline at 988 for English and Spanish
- Chat with professionals at Lifeline Chat
- Text “HOME” to the Crisis Text Line at 741741
- Check out Befrienders Worldwide or Suicide Stop if you’re not in the United States and need to find your country’s crisis hotline
If you decide to call an emergency number like 911, ask the operator to send someone trained in mental health, like Crisis Intervention Training (CIT) officers.
There’s some disagreement over whether there’s a difference between a “mental health emergency” and a “mental health crisis,” but most people use these terms interchangeably.
The National Alliance on Mental Illness (NAMI) uses the terms “crisis” and “emergency” with the same meaning in its detailed guide to navigating a crisis. Many others (including Psych Central) follow suit.
Others define a mental health emergency as a life threatening situation in which someone is a danger to themselves or others, while a crisis is non-life-threatening, but the person is still severely distressed. Some others say an emergency is someone attempting suicide, while a crisis is someone thinking about or planning suicide.
Whether you call it a “mental health emergency,” “crisis,” or “mental breakdown,” people having these experiences need immediate support.
Any threat or attempt of suicide or self-harm is a mental health crisis and a medical emergency.
The reasons for your mental health crisis — just like your mental health — are unique to you.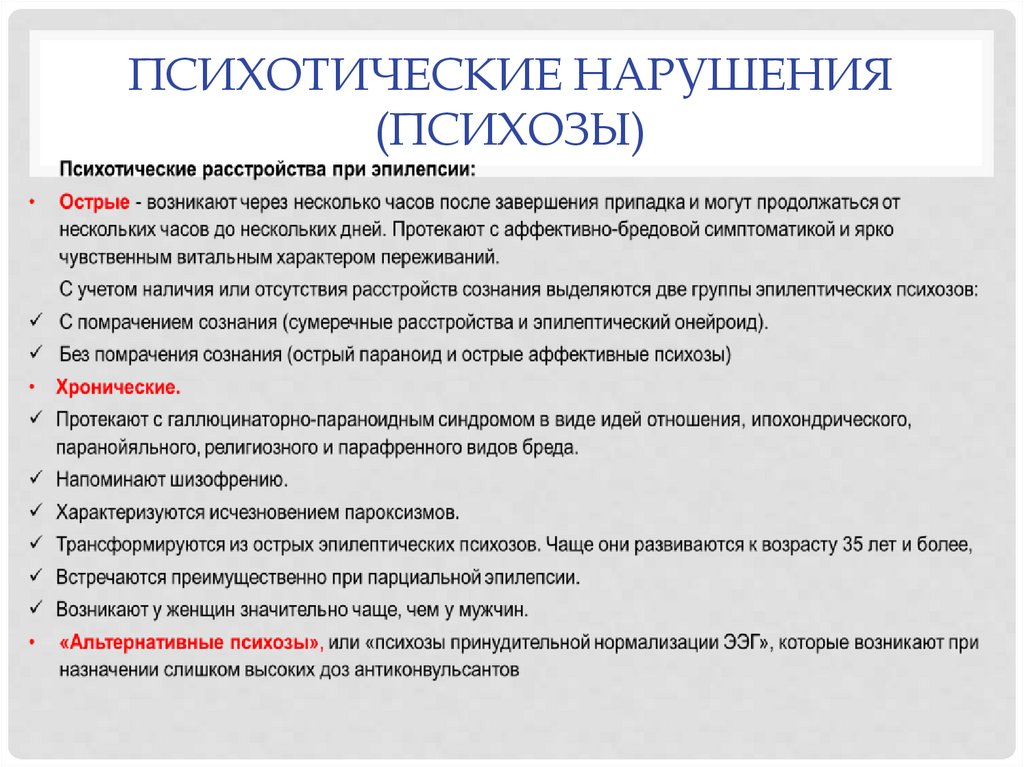 What a crisis is for one person might not be for another.
What a crisis is for one person might not be for another.
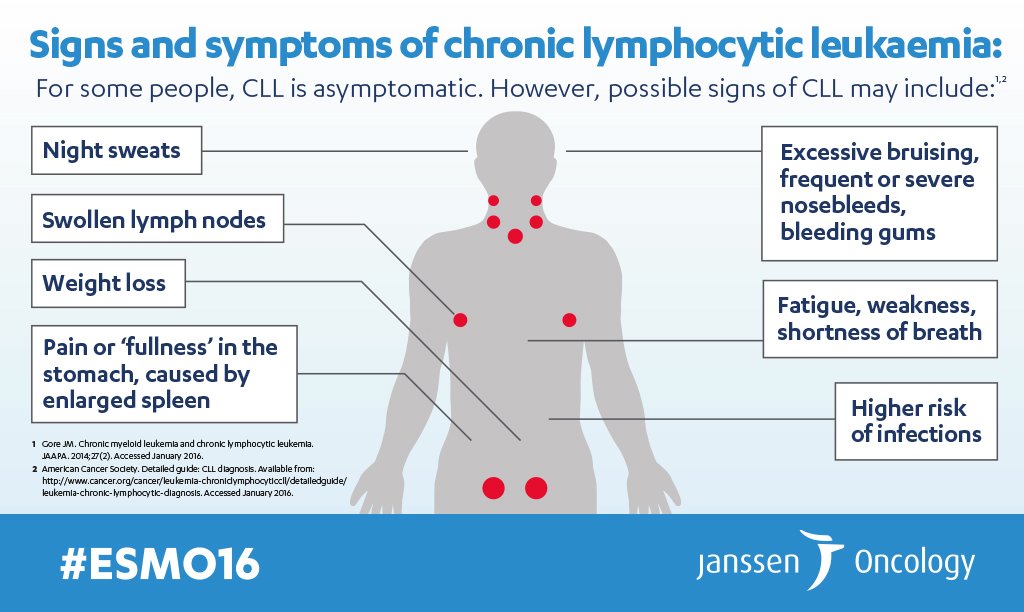
Some signs that you might be having a mental health crisis include:
- difficulty in functioning or being unable to function (e.g., it’s hard to get out of bed, go to work, or do daily tasks)
- having challenges or an inability to take care of your hygiene, such as brushing your teeth, changing clothes, and bathing
- intense or sudden changes in mood
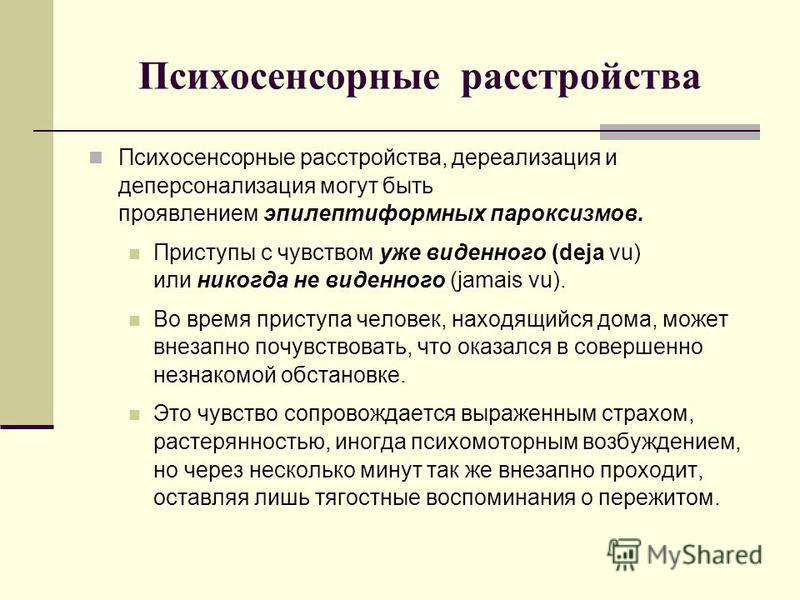
- psychosis such as hallucinations or delusions
- paranoia
- feeling increasingly agitated, angry, or violent
- suicidal thoughts or making plans
- harming yourself or self-medicating
- isolating or withdrawing from others
In most cases, these signs and behavioral changes are severe.
If you already live with a mental health condition, these symptoms could sound like the status quo for you. The key is to figure out what your “normal” is so you can understand what being in a crisis means and when you need to reach out for support.
According to the American Psychological Association (APA), the most common sign of crisis is “a clear and abrupt change in behavior.”
So when your behaviors and moods are not typical for you, that might mean you’re approaching or are in crisis.
Like the signs of a mental health crisis, the causes of a crisis are also unique.
Something that leads to a crisis in one person might not in someone else. This is commonly seen in how different people respond and cope in natural disasters or losing loved ones.
Many potential stressors might contribute to a crisis, including:
- loss
- traumatic event
- changes in relationships (e.g., a divorce or breakup)
- feeling alone or like you don’t have a support system
- switching or stopping mental health treatments
- discrimination
- losing a job or failing a class
- natural disaster, violence, or terrorism
- substance use
- medical diagnosis
According to 2021 research, specific people might be more likely to experience a mental health crisis, including:
- people who’ve had economic losses
- those with preexisting conditions
- people living in crowded environments
A 2015 research review noted that some people with severe mental health conditions might not have strong coping mechanisms. When exposed to excessive stress, the coping tools they have might break down, leading to crisis.
When exposed to excessive stress, the coping tools they have might break down, leading to crisis.
If you believe you’re in crisis — whether or not you’re experiencing thoughts of suicide — you deserve help and support. You’re not a burden. Your mental health matters.
There are many crisis intervention services, but where you live might affect your options.
If you need support right away but aren’t sure about your options, you can call or text a crisis hotline or chat online. You can find a full list of crisis resources here.
You can also:
- go to a walk-in psychiatric urgent care center
- if you have one, call your mental health professional if it’s during their working hours or they have a line for emergencies
- go to an urgent care or emergency room
- call 911 if you believe you or someone else is in immediate danger
If there’s someone you trust to support you, you may also want to call them. They can help you make arrangements or look for services, whether in person or on the phone.
Things to keep in mind
- If you’re worried about being hospitalized, you don’t have to be. While a hospital stay can be helpful for a crisis, some people fear the stigma of being “committed” or fear the financial consequences. People are usually hospitalized if they’re an immediate danger to themselves or others. So if you’re in crisis but not in danger, there are outpatient and telehealth options that can get you support while you remain at home.
- If you call 911, try to be as clear as possible why you’re calling. Unless you know your county has a crisis intervention team, your area may not have professionals trained in handling mental health concerns. If you do need to call 911, you’ll want to tell the operator clearly that it’s a mental health crisis so officers can know to come with deescalation in mind.
What does treatment look like?
Crisis treatments will vary depending on your symptoms, medical history, and even the availability of services. Typically, treatments involve a combination of medication, individual and group therapy, and learning tools and skills to help you support yourself.
Typically, treatments involve a combination of medication, individual and group therapy, and learning tools and skills to help you support yourself.
Where you get treated also depends on your condition and the severity of the crisis. You might get treated at:
- home
- an outpatient facility you go to during the day
- an inpatient psychiatric unit (that may also be called residential care)
- an emergency room
How long you stay in a hospital or program will depend on if your stay is voluntary, involuntary, or part of an emergency hold (typically 72 hours in the United States).
With any crisis intervention, the aim is to set up an aftercare plan that will help you get back to your daily life and prevent a recurrence or crisis situation in the future.
If you believe someone you know is in crisis, you might feel pretty freaked out, depending on the circumstances. It’s important to remain calm (or at least pretend to be for them) and figure out the type of support they need.
You can first start by asking yourself if they’re a danger to themselves or others. This can help you figure out whom to call.
According to NAMI, the goal in a crisis is to de-escalate. There are several techniques you can try:
- Stay calm. Speaking calmly without raising your voice can help avoid inciting further panic. You’ll also want to avoid arguing with them or overreacting. NAMI even recommends that you move slowly.
- Listen. Listening can help you figure out what they need and understand their current symptoms.
- Ask how you can help. Expressing support and concern can help them feel like they’re not alone, especially if you’re not with them in person. See what you can do for them, but understand that they may not be in a state of mind to know what they need, so you may need to be specific. For example, you might ask, “Do you need me to call someone for you?” or “Do you need a ride to the hospital?”
- Offer them options.
 Though you may feel as if you need to take control of the situation, someone might get overwhelmed by that. So instead, you’ll want to offer them options and be patient.
Though you may feel as if you need to take control of the situation, someone might get overwhelmed by that. So instead, you’ll want to offer them options and be patient. - Give them space. You don’t want them to feel trapped or boxed in. You’ll also want to avoid touching them until they give you permission.
If there’s ever a point when you don’t feel safe, it’s important to leave the location immediately. You can still ensure they get the help they need while you remain safe.
The reasons for a mental health crisis can be unique to the person. What a mental health crisis looks like and how it’s treated will also vary from person to person.
According to the World Health Organization, there’s been a 13% increase in mental health conditions in the past decade. In people ages 15 to 29 years old, suicide is the second leading cause of death.
Understanding what mental health emergencies look like and how to seek help can make a difference. You can make a difference.
You can make a difference.
If you want to be prepared, creating a mental health crisis plan to prevent a situation from escalating and having resources within immediate reach can be valuable. Here’s a how-to guide to create your own crisis plan.
What Does a Mental Health Crisis Look Like?
Unfortunately, none of us have to look very far to find someone who has been affected by suicide or mental health crisis. Suicide is the second leading cause of death in the U.S. for adults and the third leading cause of death for teens. The National Alliance on Mental Illness says 1 in 5 youth aged 13-18 experiences a severe mental health condition at some point in their life. That’s 21.4% of youth. The risk of suicide for people with mental health needs is a concern.
Learn about the 5 things every child needs for good mental health here!One of the most common comments we hear at our children’s psychiatric hospitals is that the families and friends of people who are admitted didn’t realize their loved one was going through a crisis. A mental health crisis isn’t something people typically prepare for and they can miss the signs. Here are some ways to recognize when a person is experiencing a mental health crisis and help your loved one get help.
A mental health crisis isn’t something people typically prepare for and they can miss the signs. Here are some ways to recognize when a person is experiencing a mental health crisis and help your loved one get help.
A mental health crisis is any situation in which a person’s actions, feelings, and behaviors can lead to them hurting themselves or others, and/or put them at risk of being unable to care for themselves or function in the community in a healthy manner. Situations that can lead to a mental health crisis can include stress at home like conflicts with loved ones, exposure to trauma, or violence. Stress at work or school and other environmental stress can also contribute to a mental health crisis.
Roberson
Individuals with diagnosed mental illness are at greater risk of experiencing crisis, but too often a crisis occurs before a mental illness has been diagnosed. “We have to remember that mental illness is a physical condition,” said James Roberson, VP of Programs and Innovation at KVC Hospitals. “When crisis strikes it’s not a switch that can be turned off. The body and brain may be working against our own goals and desires. Seeking professional help is the safest way to address the underlying medical issues. Once addressed other therapies and treatment services can be used to prevent future crisis and address underlying issues.”
“When crisis strikes it’s not a switch that can be turned off. The body and brain may be working against our own goals and desires. Seeking professional help is the safest way to address the underlying medical issues. Once addressed other therapies and treatment services can be used to prevent future crisis and address underlying issues.”
A mental health crisis can display in a variety of ways. There is no one indicator that a person is experiencing a mental health emergency or may attempt suicide, but here some signs to look for. The person may be:
- Unable to complete daily tasks like getting dressed, brushing teeth, bathing, etc.
- Verbally saying, writing or insinuating that they’d like to kill themselves and/or talking about death
- Withdrawing from friends, family and their typical social situations
- Showing impulsive or reckless behavior, being aggressive
- Having dramatic shifts in mood, sleeping or eating patterns
According to the National Alliance on Mental Illness, being prepared in advance for a mental health crisis and sharing that plan with your loved one can help to avoid a crisis.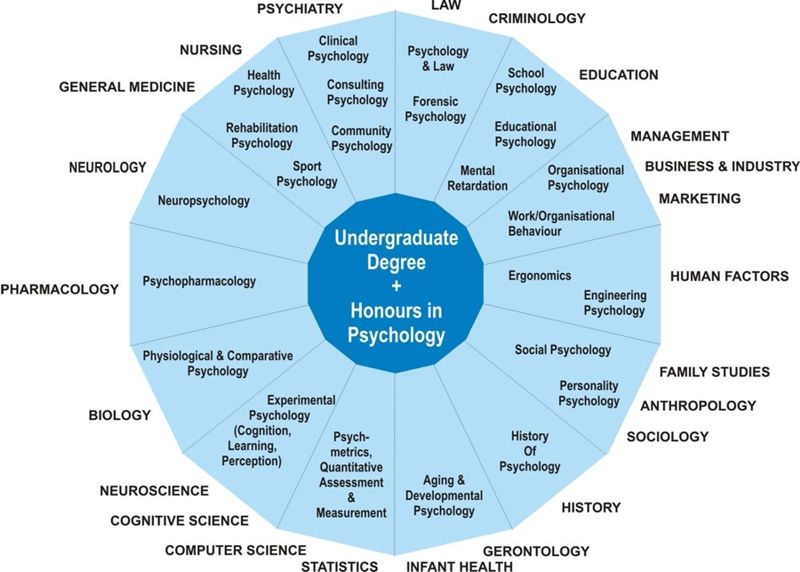 When you suspect a crisis, you’ll need to decide who call to help. If the person is an immediate danger to themselves or someone else, do not hesitate to call 911 and let them know you are with someone experiencing a mental health crisis. If the person is not in immediate danger you can reach out the individual’s therapist, doctor or psychiatrist if they have one. They will be able to provide advice and help with crisis services. You can also go to the local mental health center or emergency room to receive an assessment.
When you suspect a crisis, you’ll need to decide who call to help. If the person is an immediate danger to themselves or someone else, do not hesitate to call 911 and let them know you are with someone experiencing a mental health crisis. If the person is not in immediate danger you can reach out the individual’s therapist, doctor or psychiatrist if they have one. They will be able to provide advice and help with crisis services. You can also go to the local mental health center or emergency room to receive an assessment.
There are also techniques that can help de-escalate a crisis which includes keeping your voice calm, listening to the person, moving slowly and avoiding making judgemental comments. Here are the things you can discuss and information you can gather to create a preparedness plan:
- Know where to go for help. This can be a community mental health center, emergency room or psychiatric treatment facility. The National Suicide Prevention Lifeline is also available 24/7 at 1-800-273-TALK (8255).

- Identify family members and friends who can be available for help and to support the person in crisis.
- Compile the phone numbers and names of the person’s primary care doctor, psychiatrist, therapist and other healthcare providers.
- Compile a list of the medications and diagnoses your loved one has.
- Compile a list of the emotional and verbal triggers that typically affect your loved one.
- Share any history of drug and/or alcohol use you’re aware of, plus any history of psychosis or suicide attempts.
- Consider things that have helped to stabilize and regulate the person in the past.
- Remove weapons, unprescribed medications, and items that can cause risk to their life.
Don’t try to handle the situation alone. If you know someone struggling with depression or experiencing thoughts of self-harm, contact our psychiatric hospitals at (913) 890-7468, or contact the National Suicide Prevention Lifeline at 1-800-273-TALK (8255).
Related Posts:
- How to Talk with Teenagers about Suicide
- Exposing the Connection Between Social Media and Teen Suicide
- 7 Common Myths About Teen Suicide
- Suicide: Preventing the Second Leading Cause of Death for Young People
- Kevin Briggs: The Bridge Between Suicide and Life [TED Talk]
- Therapists Answer Parent’s Questions About Netflix Series “13 Reasons Why”
Posted in Behavioral Healthcare, Parenting, Suicide Prevention | Tags: behavioral health, child mental health, mental health, psychiatric care, psychiatric treatment, suicide, suicide prevention, suicide prevention month
A real crisis in modern psychiatry
MAIN PAGE » PUBLICATIONS CCHR
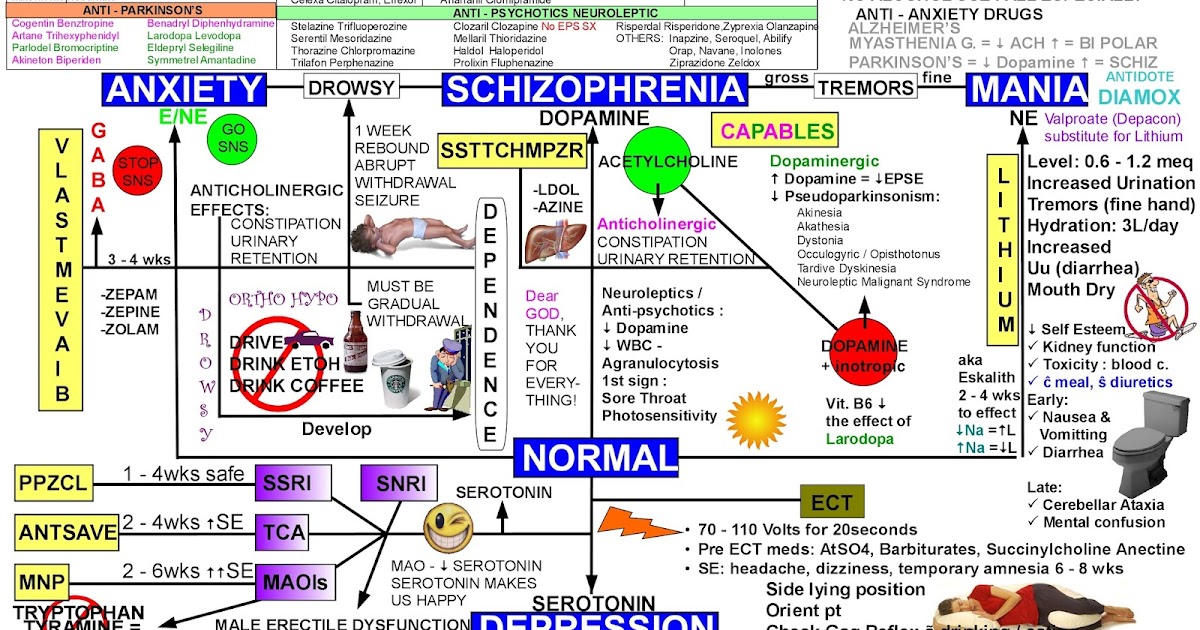
How alarmed should we be that the spread of mental illness has now become a veritable epidemic that affects one in four people in the world? According to alarming reports coming from psychiatric circles, there is a danger that mental illness will soon spread to each of us.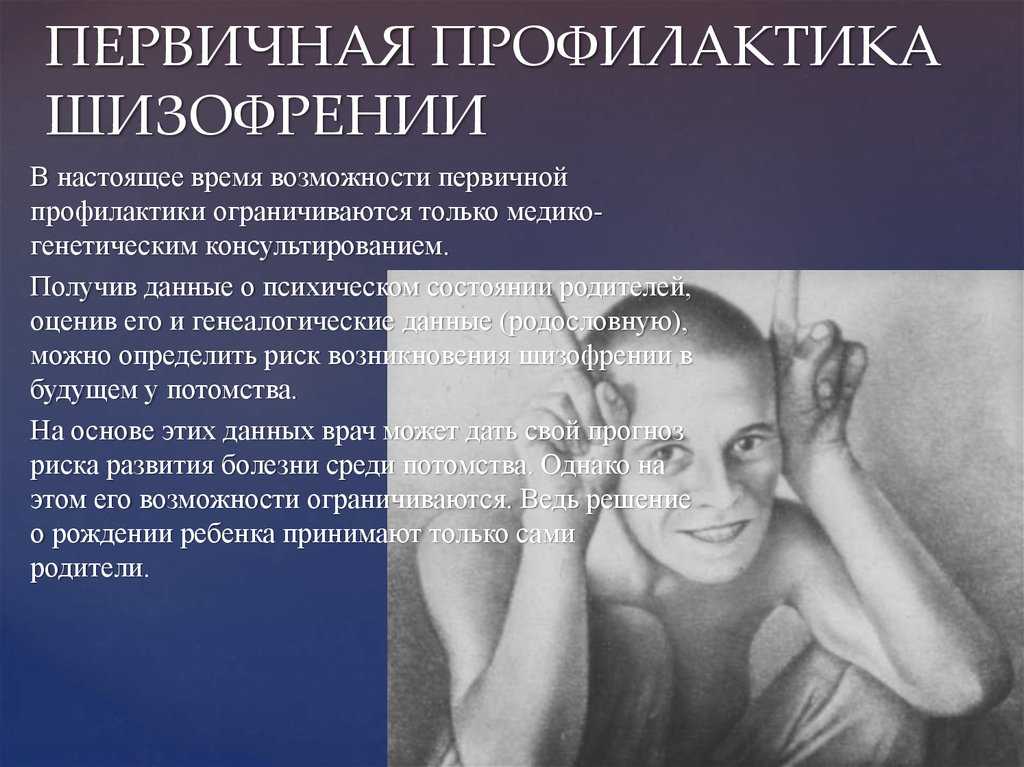 According to these reports, the only thing that can stop this is urgent and large financial investments in the field of psychiatry. They warn of the dire consequences of being denied funding. What psychiatrists never talk about is the diagnostic system that generates these gigantic and therefore alarming statistics of mental disorders. After all, their entire diagnostic system is based on the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) and the chapter on Mental Disorders from the International Classification of Diseases (ICD-10), which they invented. Both of these publications are severely criticized by analysts for their scientific unfoundedness and unreliability, as well as for their one-sided approach to treatment with the help of psychotropic drugs alone.
According to these reports, the only thing that can stop this is urgent and large financial investments in the field of psychiatry. They warn of the dire consequences of being denied funding. What psychiatrists never talk about is the diagnostic system that generates these gigantic and therefore alarming statistics of mental disorders. After all, their entire diagnostic system is based on the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) and the chapter on Mental Disorders from the International Classification of Diseases (ICD-10), which they invented. Both of these publications are severely criticized by analysts for their scientific unfoundedness and unreliability, as well as for their one-sided approach to treatment with the help of psychotropic drugs alone.
Professor Erb Kutchins of the University of Sacramento, California, and New York University professor Stuart Kirk, authors of critical books on the DSM, warn: “Certainly, the creators of DSM harbor too many illusions about it; they are eager to believe that their dreams of scientific excellence and practicality have come true…”
However, the “bitter truth” is that in DSM “too many common human deficiencies are given the character of diseases.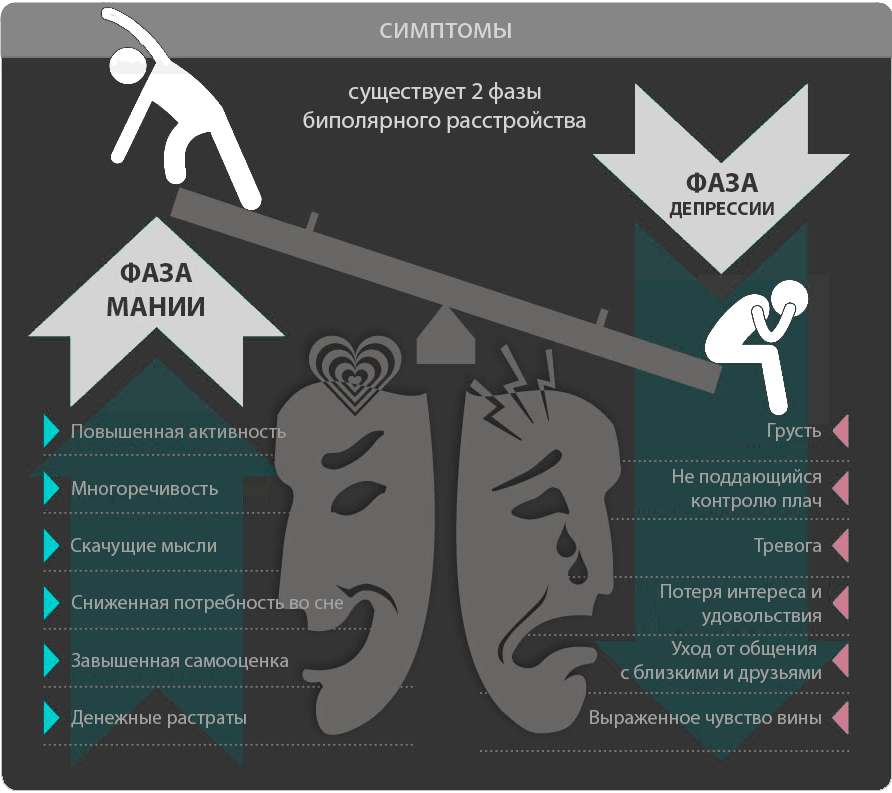 ”
”
Professor Edward Shorter, author of A History of Psychiatry , emphasizes: “Instead of taking a path that leads to a brave new world of science, DSM-IV style psychiatry seems to be definitively heading into the wilderness.”
We have prepared this report and recommendations for government officials responsible for making legislative and administrative decisions in the field of public health. Particularly when decisions are made about the funding of psychiatric programs and insurance against mental illness.
What are the results of the widespread use of DSM by psychiatrists, with its growing by leaps and bounds list of diseases, for each of which a psychiatric drug can be legally prescribed?
- Currently, 20 million schoolchildren worldwide have been diagnosed with a mental disorder and treated with powerful antidepressants or stimulants that are pharmacologically similar to cocaine.
- Worldwide, there is a trend towards a sharp increase in the use and abuse of psychiatric drugs: in 2002, more than 100 million prescriptions for antidepressants alone amounted to 19.
 5 billion dollars.
5 billion dollars. - In France, every seventh prescription is for psychotropic drugs. More than half of the unemployed - and this is 1.8 million people - take psychotropic drugs.
- Over the past 10 years, the growth of mental illness statistics based entirely on the DSM has inflated the global budget for mental health services to incredible proportions.
- Psychiatry spending in the United States today is over $80 billion, up from $33 billion in 1994
- In Switzerland, spending on psychiatry has risen from $73.5 million in 1988 to over $184.8 million in the last 10 years.
- In Germany, the cost of psychiatry is more than 2.6 billion dollars annually.
- In France, the cost of psychiatry has increased so much that in 1996 the country's budget deficit was 400 million dollars.
Despite unprecedented spending, in many countries today there are unheard-of levels of violence, suicide, child abuse, drug addiction, crime - in short, all those very real problems for which psychiatrists have neither solutions nor explanations of the reasons. This means that it is safe to say that cutting funding for psychiatric programs will not exacerbate mental health problems. In reality, reducing funding for dangerous psychiatric treatments and programs will lead to positive changes in the mental health of citizens.
This means that it is safe to say that cutting funding for psychiatric programs will not exacerbate mental health problems. In reality, reducing funding for dangerous psychiatric treatments and programs will lead to positive changes in the mental health of citizens.
The testimonies and data presented in this report come from doctors, lawyers, judges, psychiatrists, parents and others who are involved in one way or another with the issue of mental health. These experts agree that psychiatric requests stemming from the DSM, such as tightening involuntary hospitalization laws or spreading so-called community mental health plans, are devastating to both people and the economy. The same can be said for programs such as screening children in schools for mental disorders.
Claims that only increased funding can improve things in psychiatry have lost all credibility. In the field of science, a theory usually needs to be proven empirically. When the Centers for Disease Control receives funding to fight a dangerous disease, the funding is used to find the biological cause and develop a cure. There are various tests that can show the presence or absence of most physical diseases that have a biological cause. Without questioning the existence of serious mental difficulties that people sometimes experience, nevertheless, it must be stated that in psychiatry there are no objective analyzes or tests with which one could confirm the presence of at least one mental "disease". Diagnosis in psychiatry is completely subjective.
There are various tests that can show the presence or absence of most physical diseases that have a biological cause. Without questioning the existence of serious mental difficulties that people sometimes experience, nevertheless, it must be stated that in psychiatry there are no objective analyzes or tests with which one could confirm the presence of at least one mental "disease". Diagnosis in psychiatry is completely subjective.
The severity of the problems facing modern society reflects the urgent need for effective and humane alternatives to dangerous psychiatric treatments. For your own good, we ask you to explore the alternatives that we deemed it necessary to offer you. We bring this report to your attention in the hope that you will give it due attention and form your own understanding of the current state of the mental health field and the ability or inability of psychiatrists to offer effective solutions to problems in this area.
Rohit Edie, MD
Mary Jo Pagel, MD
Julian Whitaker, MD
Anthony P. Urbanek, MD
Urbanek, MD
Crisis wisely | Big Ideas
Crisis smart | Big Ideas Psychology Julia Fukolova Evgeny DudinHow do stresses and financial crises affect the psyche, why are businessmen at risk, and what does biohacking lead to? This is discussed by the doctor of medical sciences, head of the department of the clinic of psychiatry. S. S. Korsakov at the First Moscow State Medical University named after I. M. Sechenov Dmitry Danilov.
HBR - Russia: How does science define a mentally normal person?
Danilov: There is still no generally accepted medical definition of the state of "mental norm". The most appropriate interpretation is a comfortable perception of a person by himself and his harmonious existence in society.
Yes, but society often rejects non-standard people.
A delicate question. Everyone has heard about the infamous artist Pyotr Pavlensky - he nailed his scrotum to the paving stones on Red Square, and recently set fire to the Bank of France. His actions have no clear purpose. Who is he - a person with a disturbed psyche or just a too bright personality? A whole controversy unfolded among psychiatrists about how to relate to Pavlensky's outrageous acts, and there is no unequivocal opinion on this issue.
Is there a significant relationship between outstanding achievements and mental disabilities?
Among geniuses, the number of mental patients is indeed higher than the average among the population. Outstanding people not only have inclinations in a particular creative field, but also have non-standard thinking, they perceive the world or their inner state differently. A lot of pathographic portraits are devoted to this issue - scientific essays that analyze the features of the psyche of geniuses. Not so long ago, a series of books by the German professor Anton Neumar was published in Russia, dedicated to the peculiarities of the psyche of brilliant artists, outstanding composers and great dictators. For example, Mikhail Vrubel and a number of other brilliant personalities were observed in the university psychiatric clinic, of which I am an employee.
For example, Mikhail Vrubel and a number of other brilliant personalities were observed in the university psychiatric clinic, of which I am an employee.
What about corporate leaders? Many of them have character flaws.
It is unlikely that the leaders of large companies suffer from serious mental illness. Rather, they are dominated by people with a special character, the so-called accentuated personalities. Some of their traits are simply strongly protruded, and with favorable external factors, this gives them the opportunity to take a leading position. I want to emphasize that accentuations are not mental disorders. Just the presence of such personalities helps to overcome the "gray" existence of society and makes our life more interesting.
What issues does modern psychiatry solve?
The main direction is genetic research. Mental illnesses are associated with neurochemical processes in the brain - for example, some substance is not produced (or, conversely, excessively produced). Or, say, there is enough substance, but it is disposed of too quickly or too slowly. Not one, but a variety of genes are responsible for all this, and scientists are trying to figure out which ones. This understanding will enable us to more accurately prescribe treatment.
Or, say, there is enough substance, but it is disposed of too quickly or too slowly. Not one, but a variety of genes are responsible for all this, and scientists are trying to figure out which ones. This understanding will enable us to more accurately prescribe treatment.
The second direction is the search for new drugs that are more effective and safer. But business interests are involved here. For example, in the late 1990s and early 2000s, pharmaceutical companies developed new drugs for the treatment of severe mental disorders, conducted research and declared that these drugs worked better than the old ones. Doctors believed the advertising campaign, but in some cases the hopes were not justified. The new drugs did not work very well and had other side effects, sometimes more severe than before. As a result, many patients suffered: doctors could not slow down the development of the disease while it was possible.
What problems are most often addressed to psychiatrists?
Apart from serious illnesses, people complain of sleep problems, prolonged anxiety, sudden states of panic, various fears, a feeling of gloomy present and hopelessness of the future. The reason for the appeal may be constant fatigue, loss of strength, or, say, discomfort in the body that is not associated with physical illness. All these symptoms make up a picture of neuroses and subdepressions - very mild mental disorders caused by a stressful situation and psychological overload. There is an opinion that such problems usually occur in women or people in an unstable social position, but this is not so. Increasingly, we are approached by successful middle-class men.
The reason for the appeal may be constant fatigue, loss of strength, or, say, discomfort in the body that is not associated with physical illness. All these symptoms make up a picture of neuroses and subdepressions - very mild mental disorders caused by a stressful situation and psychological overload. There is an opinion that such problems usually occur in women or people in an unstable social position, but this is not so. Increasingly, we are approached by successful middle-class men.
Are businessmen at risk?
Modern business means high pace, stress and great responsibility. For individual managers, the problems can be so protracted that it leads to the disorganization of their social life, a decrease in efficiency. Another problem is alcohol abuse. The desire to relieve stress with the help of alcoholic beverages imperceptibly causes the formation of dependence. However, the modern level of culture has led to a decrease in alcoholism, which business representatives often suffered in 1990s
How do financial crises affect mental health?
Researchers have proven that the percentage of seriously mentally ill patients in society is approximately the same and is not associated with social problems. These are the so-called endogenous diseases (for example, schizophrenia), which depend on genetic factors. But the number of psychogenic diseases that occur under the influence of stress increases during crises. People lose their jobs, can't find a new one, their money burns in the banks. Recently, bank employees often apply - many of them were out of work. The head of one bank, whose license was revoked and a criminal case was opened on the fact of fraud, fell into a severe depression, the person even thought about suicide. However, depression and neuroses are successfully treated. We use various non-drug methods or soft drug therapy, and patients return to normal life.
These are the so-called endogenous diseases (for example, schizophrenia), which depend on genetic factors. But the number of psychogenic diseases that occur under the influence of stress increases during crises. People lose their jobs, can't find a new one, their money burns in the banks. Recently, bank employees often apply - many of them were out of work. The head of one bank, whose license was revoked and a criminal case was opened on the fact of fraud, fell into a severe depression, the person even thought about suicide. However, depression and neuroses are successfully treated. We use various non-drug methods or soft drug therapy, and patients return to normal life.
Sudden bankruptcy and other failures can destroy the psyche. And if a person suddenly became rich, this does not happen. Why?
A sharp increase in well-being is also a stress factor, but with a plus sign. It rarely leads to the development of mental pathology, because there is no intrapersonal conflict when expectations do not match reality. Most people dream of catching luck by the tail. However, this stress can cause characterological changes - a person becomes arrogant or, let's say, falls into euphoria, loses the instinct of self-preservation. At 19There were many such cases in the 1990s. The businessman quickly got rich, bought the coolest car, but it all ended in a tragic accident through his fault.
Most people dream of catching luck by the tail. However, this stress can cause characterological changes - a person becomes arrogant or, let's say, falls into euphoria, loses the instinct of self-preservation. At 19There were many such cases in the 1990s. The businessman quickly got rich, bought the coolest car, but it all ended in a tragic accident through his fault.
Some people today are addicted to biohacking and seek to improve the condition of their body and brain in various ways. How to treat it?
The concept of "biohacking" has appeared quite recently. This is a whole range of measures - the correction of nutrition, physical activity, sleep, the internal biological state of the body, productivity, etc. Their goal is to prevent the development of diseases, increase the quality and duration of life. Each new technique causes a stir among consumers, but its effectiveness must first be proven. A healthy lifestyle and physical activity can only be welcomed, as for medicines, I want to upset you - there is no miracle pill.