Ocd tics examples
Obsessive-Compulsive Disorder (OCD) | Chestnut Health Systems
What is OCD?
Obsessive-Compulsive Disorder (OCD) is a common, chronic and long-lasting disorder in which a person has uncontrollable, reoccurring thoughts (obsessions) and behaviors (compulsions) that he or she feels the urge to repeat over and over.
What are the signs and symptoms of OCD?
People with OCD may have symptoms of obsessions, compulsions, or both. These symptoms can interfere with all aspects of life, such as work, school, and personal relationships.
Obsessions are repeated thoughts, urges, or mental images that cause anxiety. Common symptoms include:
- Fear of germs or contamination
- Unwanted forbidden or taboo thoughts involving sex, religion, and harm
- Aggressive thoughts towards others or self
- Having things symmetrical or in a perfect order
Compulsions are repetitive behaviors that a person with OCD feels the urge to do in response to an obsessive thought. Common compulsions include:
- Excessive cleaning and/or handwashing
- Ordering and arranging things in a particular, precise way
- Repeatedly checking on things, such as repeatedly checking to see if the door is locked or that the oven is off
- Compulsive counting
Not all rituals or habits are compulsions. Everyone double checks things sometimes. But a person with OCD generally:
- Can't control his or her thoughts or behaviors, even when those thoughts or behaviors are recognized as excessive
- Spends at least 1 hour a day on these thoughts or behaviors
- Doesn’t get pleasure when performing the behaviors or rituals, but may feel brief relief from the anxiety the thoughts cause
- Experiences significant problems in their daily life due to these thoughts or behaviors
Some individuals with OCD also have a tic disorder. Motor tics are sudden, brief, repetitive movements, such as eye blinking and other eye movements, facial grimacing, shoulder shrugging, and head or shoulder jerking.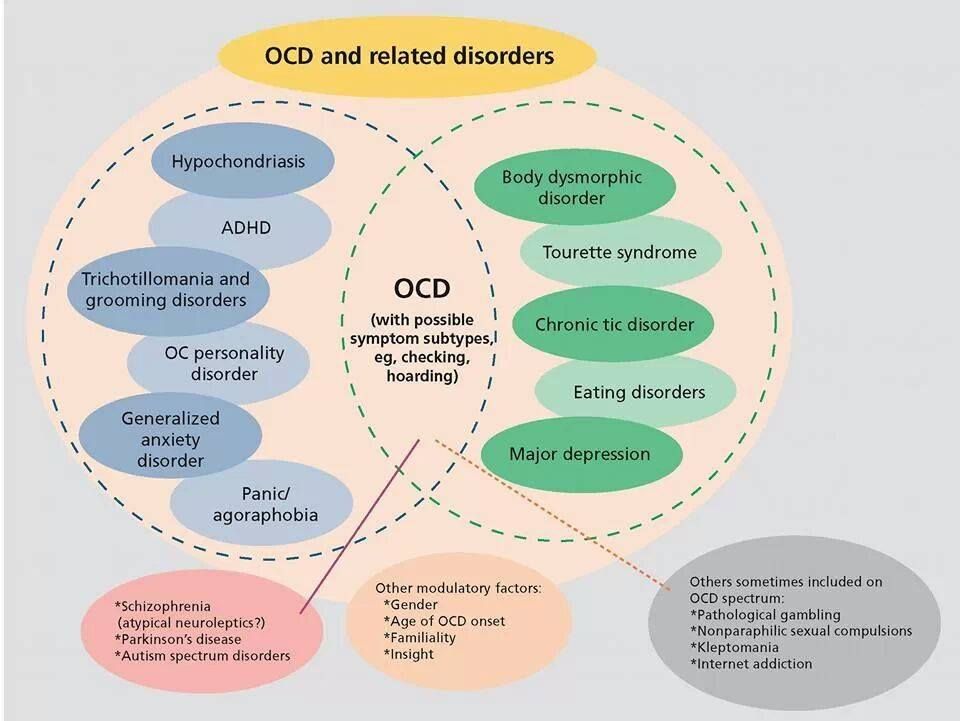 Common vocal tics include repetitive throat-clearing, sniffing, or grunting sounds.
Common vocal tics include repetitive throat-clearing, sniffing, or grunting sounds.
Symptoms may come and go, ease over time, or worsen. People with OCD may try to help themselves by avoiding situations that trigger their obsessions, or they may use alcohol or drugs to calm themselves. Although most adults with OCD recognize that what they are doing doesn’t make sense, some adults and most children may not realize that their behavior is out of the ordinary. Parents or teachers typically recognize OCD symptoms in children.
If you think you have OCD, talk to your doctor about your symptoms. If left untreated, OCD can interfere in all aspects of life.
What are the risk factors for OCD?
OCD is a common disorder that affects adults, adolescents, and children all over the world. Most people are diagnosed by about age 19, typically with an earlier age of onset in boys than in girls, but onset after age 35 does happen.
The causes of OCD are unknown, but risk factors include:
Genetics
Twin and family studies have shown that people with first-degree relatives (such as a parent, sibling, or child) who have OCD are at a higher risk for developing OCD themselves. The risk is higher if the first-degree relative developed OCD as a child or teen. Ongoing research continues to explore the connection between genetics and OCD and may help improve OCD diagnosis and treatment.
The risk is higher if the first-degree relative developed OCD as a child or teen. Ongoing research continues to explore the connection between genetics and OCD and may help improve OCD diagnosis and treatment.
Brain Structure and Functioning
Imaging studies have shown differences in the frontal cortex and subcortical structures of the brain in patients with OCD. There appears to be a connection between the OCD symptoms and abnormalities in certain areas of the brain, but that connection is not clear. Research is still underway. Understanding the causes will help determine specific, personalized treatments to treat OCD.
Environment
People who have experienced abuse (physical or sexual) in childhood or other trauma are at an increased risk for developing OCD.
In some cases, children may develop OCD or symptoms following a streptococcal infection—this is called Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections (PANDAS). For more information, please read this fact sheet on PANDAS.
For more information, please read this fact sheet on PANDAS.
What types of treatments and therapies are available?
OCD is typically treated with medication, psychotherapy or a combination of the two. Although most patients with OCD respond to treatment, some patients continue to experience symptoms.
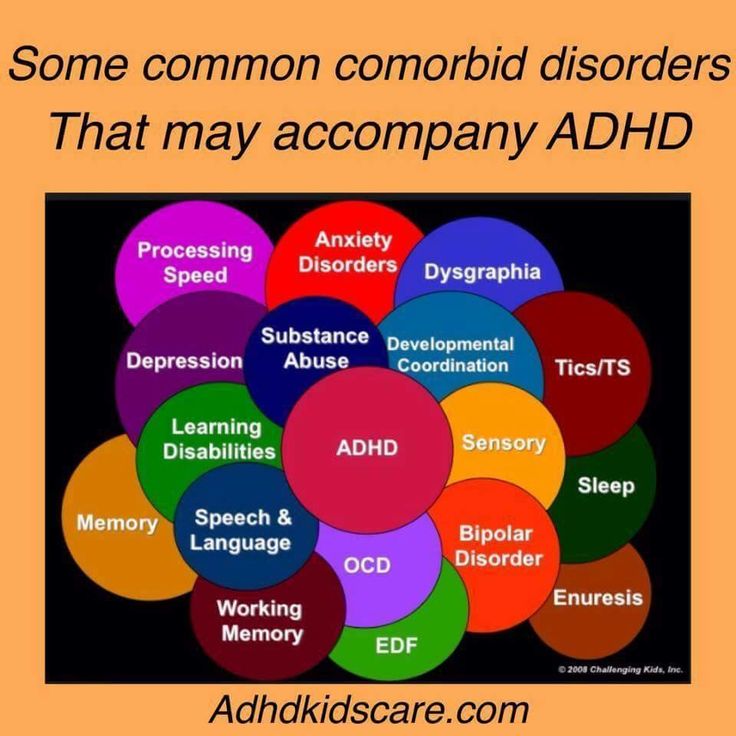
Sometimes people with OCD also have other mental disorders, such as anxiety, depression, and body dysmorphic disorder, a disorder in which someone mistakenly believes that a part of their body is abnormal. It is important to consider these other disorders when making decisions about treatment.
Medication
Serotonin reuptake inhibitors (SRIs) and selective serotonin reuptake inhibitors (SSRIs) are used to help reduce OCD symptoms. Examples of medications that have been proven effective in both adults and children with OCD include clomipramine, which is a member of an older class of “tricyclic” antidepressants, and several newer “selective serotonin reuptake inhibitors” (SSRIs), including:
- fluoxetine
- fluvoxamine
- sertraline
SRIs often require higher daily doses in the treatment of OCD than of depression and may take 8 to 12 weeks to start working, but some patients experience more rapid improvement.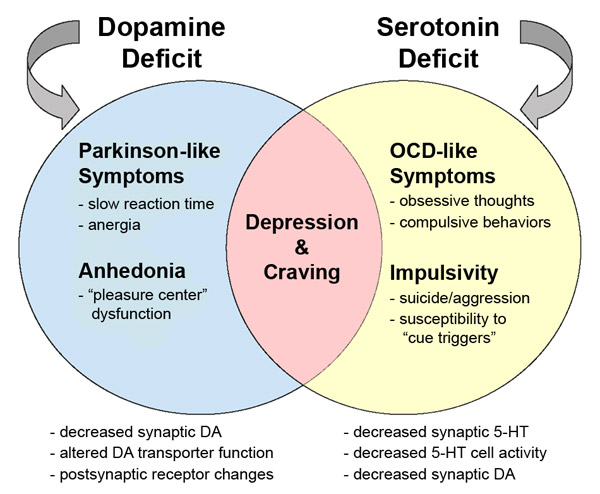
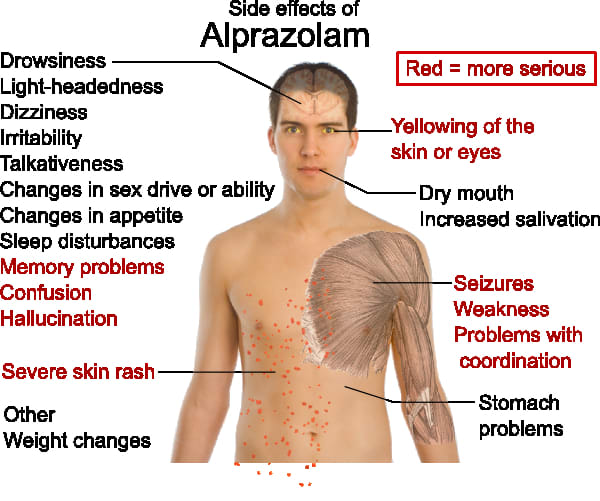
If symptoms do not improve with these types of medications, research shows that some patients may respond well to an antipsychotic medication (such as risperidone). Although research shows that an antipsychotic medication may be helpful in managing symptoms for people who have both OCD and a tic disorder, research on the effectiveness of antipsychotics to treat OCD is mixed.
If you are prescribed a medication, be sure you:
- Talk with your doctor or a pharmacist to make sure you understand the risks and benefits of the medications you're taking.
- Do not stop taking a medication without talking to your doctor first. Suddenly stopping a medication may lead to "rebound" or worsening of OCD symptoms. Other uncomfortable or potentially dangerous withdrawal effects are also possible.
- Report any concerns about side effects to your doctor right away. You may need a change in the dose or a different medication.
- Report serious side effects to the U.
 S. Food and Drug Administration (FDA) MedWatch Adverse Event Reporting program online at http://www.fda.gov/Safety/MedWatch or by phone at 1-800-332-1088. You or your doctor may send a report.
S. Food and Drug Administration (FDA) MedWatch Adverse Event Reporting program online at http://www.fda.gov/Safety/MedWatch or by phone at 1-800-332-1088. You or your doctor may send a report.
Other medications have been used to treat OCD, but more research is needed to show the benefit for these options. For basic information about these medications, you can visit the National Institute of Mental Health (NIMH) Mental Health Medications web page. For the most up-to-date information on medications, side effects, and warnings, visit the FDA website.
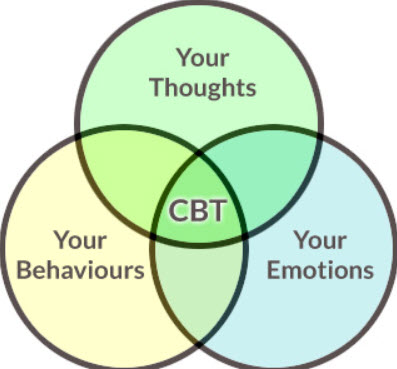
Psychotherapy
Psychotherapy can be an effective treatment for adults and children with OCD. Research shows that certain types of psychotherapy, including cognitive behavior therapy (CBT) and other related therapies (e.g., habit reversal training) can be as effective as medication for many individuals. Research also shows that a type of CBT called Exposure and Response Prevention (EX/RP) is effective in reducing compulsive behaviors in OCD, even in people who did not respond well to SRI medication. For many patients EX/RP is the add-on treatment of choice when SRIs or SSRIs medication does not effectively treat OCD symptoms.
For many patients EX/RP is the add-on treatment of choice when SRIs or SSRIs medication does not effectively treat OCD symptoms.
Other Treatment Options
NIMH is supporting research into new treatment approaches for people whose OCD does not respond well to the usual therapies. These new approaches include combination and add-on (augmentation) treatments, as well as novel techniques such as deep brain stimulation (DBS). You can learn more about brain stimulation therapies on the NIMH website.
National Institute of Mental Health (2019). Obsessive-Compulsive Disorder. Retrieved June 10, 2019, from https://www.nimh.nih.gov/health/topics/obsessive-compulsive-disorder-ocd/index.shtml.
Sign Up For Our Newsletter
x
OCD, Tics, Tourette's, & Related Disorders | Mount Sinai
If you or a loved one is struggling with obsessive-compulsive disorder (OCD), Tourette's disorder, or other related disorders, Mount Sinai can help. Our team of highly trained and experienced specialists offers empathetic and personalized care to patients of all ages. We recognize that many who are affected by these disorders may also have other conditions, such as attention-deficit/hyperactivity disorder (ADHD), autism, trichotillomania (repetitive pulling or twisting hair), or body-focused repetitive behaviors (nail-biting or skin-picking).
Our team of highly trained and experienced specialists offers empathetic and personalized care to patients of all ages. We recognize that many who are affected by these disorders may also have other conditions, such as attention-deficit/hyperactivity disorder (ADHD), autism, trichotillomania (repetitive pulling or twisting hair), or body-focused repetitive behaviors (nail-biting or skin-picking).
To address the needs of our patients, our team works closely with other specialists, within our program and the larger Mount Sinai Health System, to provide comprehensive and developmentally-appropriate evaluations and treatment.
About Obsessive-compulsive Disorder (OCD)
Individuals affected by obsessive-compulsive disorder (OCD) experience recurrent, unwanted, and distressing thoughts and fears (obsessions). These obsessions can occur out of the blue or in response to triggers in a person’s day-to-day life. Obsessions often lead to the performance of rituals or repetitive behaviors (compulsions) that temporarily reduce the anxiety generated by obsessions.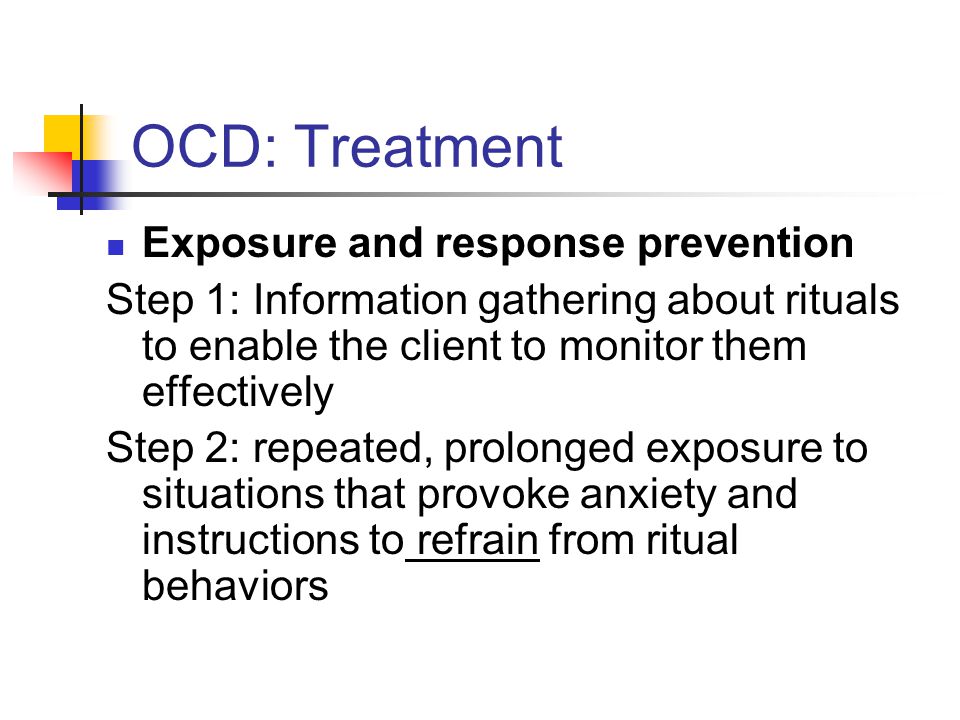 Compulsions interfere with daily life and can be very time-consuming. In addition, avoiding situations that trigger obsessions or compulsions can impact individual’s personal life, family life, and functioning at home, school, or work. OCD symptoms may begin during childhood but symptoms can start at any point over the lifespan.
Compulsions interfere with daily life and can be very time-consuming. In addition, avoiding situations that trigger obsessions or compulsions can impact individual’s personal life, family life, and functioning at home, school, or work. OCD symptoms may begin during childhood but symptoms can start at any point over the lifespan.
Getting effective treatment can be difficult: patients who present for help may be misunderstood or misdiagnosed. Too often, years go by before a patient or a loved one seeks help or gets an accurate diagnosis. Some who have OCD also have other conditions. Tic, Tourette's disorder, ADHD, and autism symptoms all occur at higher rates in those affected by OCD compared to those who do not have OCD. It is also important to identify any other anxiety or mood disorders and social or learning difficulties in order to understand the difficulties and challenges our patients are facing. At Mount Sinai, we take all your symptoms and concerns into account as we develop a treatment plan to address your current emotional and psychiatric needs.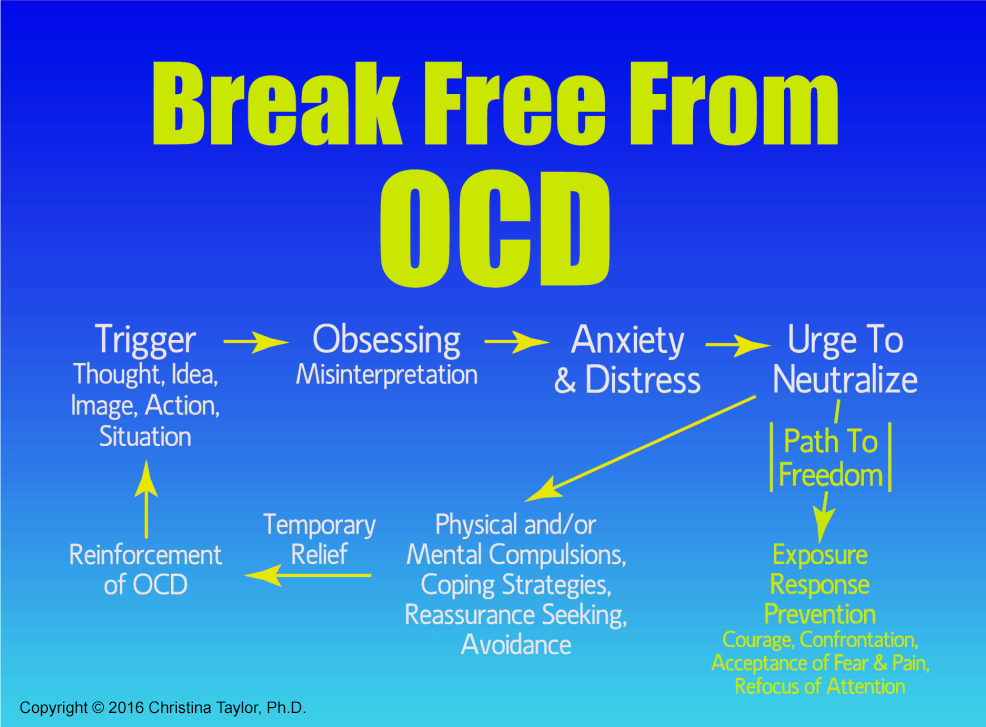
About Tourette's and Tic Disorders
Tics are sudden, rapid, recurrent involuntary movements or sounds. Tics typically begin during childhood, often around the ages of four to six. Occasional or isolated tics are not uncommon, and about 15 percent of school-age children may have some tics at one time or another. However, tic disorders in which multiple tics are present for more than a year are less common but they can cause significant interference, distress, or impairment.
Tourette's disorder is the most complex tic disorder and involves multiple motor tics and at least one vocal tic that persist, more often than not, for at least 12 months. Motor tics often begin in the head and neck area, and examples include eye blinking, eye widening, nose movements, and grimacing. However, any part of the body can be involved (for example, finger movements, abdominal tensing, and certain postures). Verbal tics also come in many forms, ranging from sniffing, throat-clearing, and small noises to repeating syllables, words, or sentences.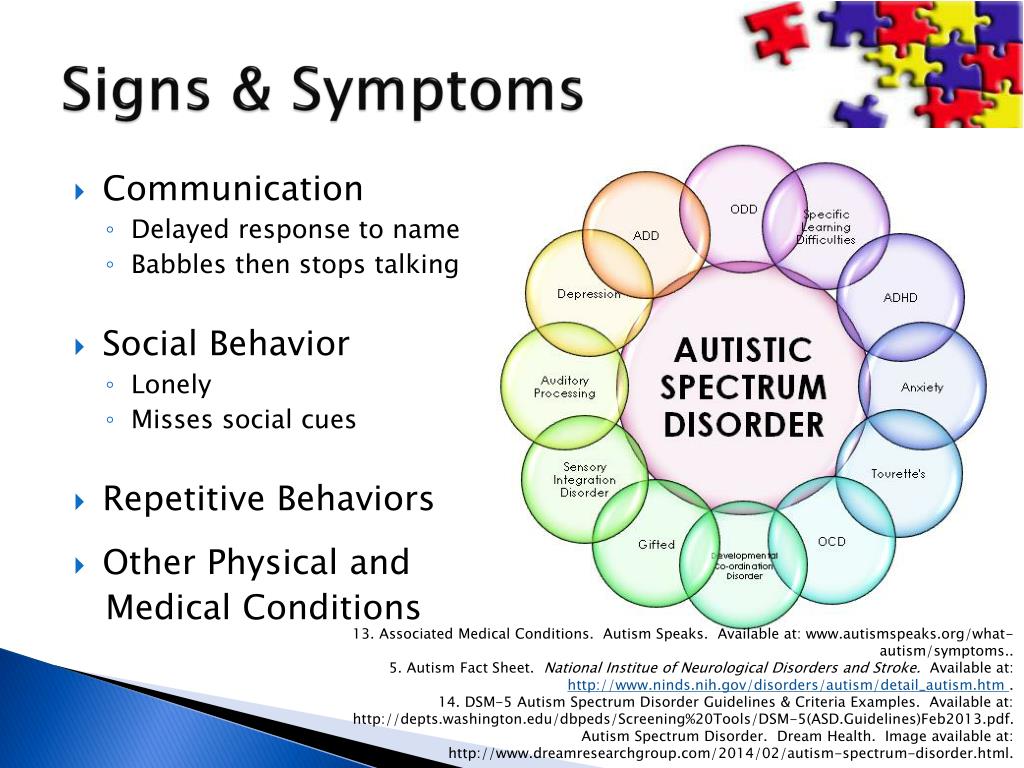 Individuals affected by Tourette's disorder may also have OCD or OCD-like symptoms (for example, needing to touch, tap, rub things, or performing actions repeatedly until they feel at peace). Anxiety or mood symptoms, attention-deficit/hyperactivity disorder (ADHD) symptoms, autism, and/or social or learning problems may also be present. We provide a comprehensive evaluation in order to devise a developmentally-appropriate treatment plan to address active and interfering tic symptoms.
Individuals affected by Tourette's disorder may also have OCD or OCD-like symptoms (for example, needing to touch, tap, rub things, or performing actions repeatedly until they feel at peace). Anxiety or mood symptoms, attention-deficit/hyperactivity disorder (ADHD) symptoms, autism, and/or social or learning problems may also be present. We provide a comprehensive evaluation in order to devise a developmentally-appropriate treatment plan to address active and interfering tic symptoms.
Our Philosophy
At Mount Sinai, we have adult psychiatrists, child and adolescent psychiatrists, psychologists, and neuropsychologists who use the latest approaches in the evaluation and treatment of OCD, Tourette's disorder, and related disorders. We embrace a team approach to meet each patient’s individual needs. When appropriate, we work with other doctors or specialists. Our goal is to help our patients live their lives free from interfering and distressing symptoms.
Our companion research program is focused on projects that relate to the neurobiology and genetics of OCD and tic disorders and an improved understanding of factors that influence risk and severity of these conditions in order to develop innovative and effective treatments.
Hyperkinesis and tics in children - diagnosis and treatment in Moscow
Tics are sudden, involuntary, violent, stereotyped, repeated, non-rhythmic, short-term movements of one muscle, muscle group or body parts. Tics can also manifest as sound abnormalities, expressed as shouting out of a sound, syllable, or word.
Tics appear in childhood, mostly between five and ten years of age, more common in boys, but also in girls (although much less frequently). In most cases, they can be corrected and disappear by the age of fifteen. Tics are not always completely involuntary and unconscious, sometimes they can be slowed down or weakened by an effort of will. nine0003
There are a lot of varieties of tics - from the simplest to the very complex. They may not bother the child at all, he may not even notice his involuntary movements, freely communicate with peers (these may be single blinks or other simple motor tics). But tics can also have a pronounced form - it is very difficult for a child with such tics to be among people, and they noticeably complicate his life. He cannot express thoughts without interference, perform some actions.
He cannot express thoughts without interference, perform some actions.
The treatment of tics is a very difficult task, the solution of which is primarily based on a correctly identified cause. With tics, there is often an undulation of the course of the disease - periods of exacerbations and remissions. During periods of exacerbation of tics, it is especially important to observe the child by a neurologist.
At the Center for Speech Neurology "DoctorNeuro" you will undergo a complete examination under the supervision of an experienced neurologist. Based on the results of the examination, the doctor will determine the cause of tics, depending on this, prescribe drug therapy, and, if necessary, decide on the introduction of additional (non-drug) methods of correction and will monitor the course of treatment. nine0003
The task of a qualified neurologist is to strike a balance between how much tics affect quality of life, and the side harm that therapy can cause.
And decide in favor of the patient
Krivtsova Julianna Pavlovna,
Neurologist
Doctor of the first category
Examination
Neurologist
under the ticks must be carried out a detailed neurological examination, including a norrosa, ostens. and neck, sometimes - MRI of the brain. The scope of the necessary examination is determined by the neurologist. As a result of the examination, the neurologist determines the cause of the disease and prescribes treatment. nine0003
EEG
An electroencephalogram is performed to make a differential diagnosis with epileptic conditions, as well as to assess the level of bioelectrical activity of the brain.
Laboratory examination
If an infectious cause of tics is suspected, a biochemical blood test for inflammatory markers (acute phase proteins) may be ordered.
Immunologist
For the same reason, consultation with an immunologist and an additional immunological examination may also be necessary. nine0003
nine0003
Neuropsychologist
Neuropsychologist assesses the state of the child's higher mental functions (memory, thinking, motor sphere, perception, etc.), as well as an assessment of the emotional-volitional sphere.
In the course of neuropsychological diagnostics in children suffering from tics, disorders of attention, visual and auditory perception, speech, and motor skills are most often noted. For example, when examining the preservation of the motor functions of a child, insufficient smoothness of movements, slowness of movements, and a violation of the correct sequence of the motor program are noted. Also, such children often have difficulties in self-organization, impulsivity, programming difficulties, regulation and control of their own behavior. nine0003
TREATMENT
After determining the cause, the neurologist prescribes the necessary therapy. In some cases, anti-inflammatory and immunomodulatory therapy is additionally prescribed for sedative therapy (if the cause of tics is an infectious agent).
There are no standard treatment regimens for tics. The choice of therapy is always an individual process. The range of sedatives used ranges from the most "weak", mainly of plant origin, to "serious" drugs from the group of antipsychotics. A neurologist always weighs the effectiveness of the therapy used and the possible side effects and applies a treatment strategy “from weak drugs to strong ones”. That is why the process of treating tics always requires intermediate observations by a neurologist, the doctor must monitor the results of his therapy. Depending on the dynamics and severity of tics, the interval for visiting a neurologist can be several days, several weeks, or several months. Sometimes it takes a long time to take drugs, several months, and sometimes even years. It all depends on the severity of the course of the disease. nine0003
ADDITIONAL (NON-DRUG) TREATMENT
Often, a neurologist can prescribe additional (non-drug) treatments: massage of the cervical-collar zone, electrosleep, osteopathic treatment.
If necessary, the neurologist can also prescribe a course of sessions with a child neuropsychologist and a child neuropsychiatrist, whose help is especially effective if the tics were provoked by a stressful situation.
Transcranial magnetic stimulation (TMS) is an effective new treatment method. This is a unique modern non-invasive technique for the treatment of neurological disorders. To date, both in domestic and foreign scientific literature, there is a fairly large number of studies on the treatment of tics with the help of TMS. The principle of action of TMS lies in the painless and safe effect of short-term magnetic impulses on the nerve cells of the cerebral cortex. In the case of the treatment of tics, an “inhibiting” excessive activity of neurons is used. nine0003
The experience of using the TMS technique in our Center has a sufficient number of examples of the treatment of tics with a positive result.
Exacerbation of tics
As a rule, the onset and exacerbation of tics occur at two age periods of hormonal adjustment and active growth of the child's body - 6-7 years (elementary school) and puberty (adolescence) period, which in recent years tends to earlier manifestation at 10-11 years.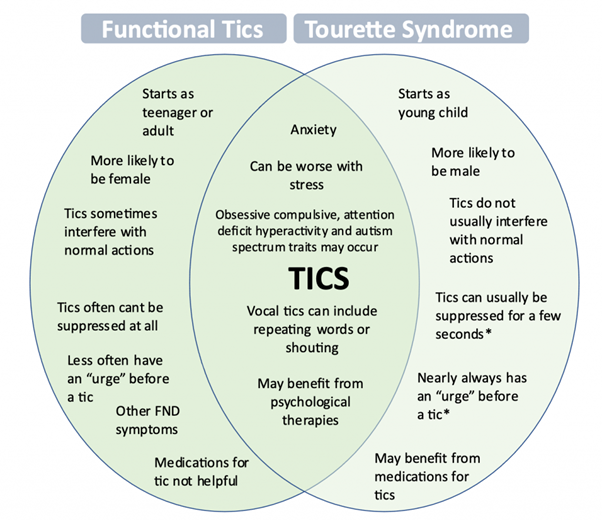
Exacerbations of tics often occur against the background of past infections, as well as stress, fright, and a traumatic situation. nine0003
Types of tics
According to the nature of clinical manifestations, tics are divided into motor (motor) and sound (vocal).
The most common motor tics are blinking, nose movements, various grimaces, head tilts, torso tilts and turns, bouncing. Vocal tics are manifested as separate sounds (it can even be a cough or bark), and shouting out whole words.
According to the severity of tics, there are simple tics (single), multiple common (when several types of tics are noted) and generalized (when both motor and vocal tics are present, almost all groups of the facial and trunk muscles are involved). nine0003
Causes
The causes of tics can be different. The main causes include:
Hereditary cause - in the family, tics are noted in relatives, in parents. The severity of hereditary tics can be different - from single blinks to a severe form of tics, manifested by multiple motor and sound phenomena, up to coprolalia (this severe form of tics is called Gilles de la Tourette's disease, after the name of the doctor who described this hereditary disease).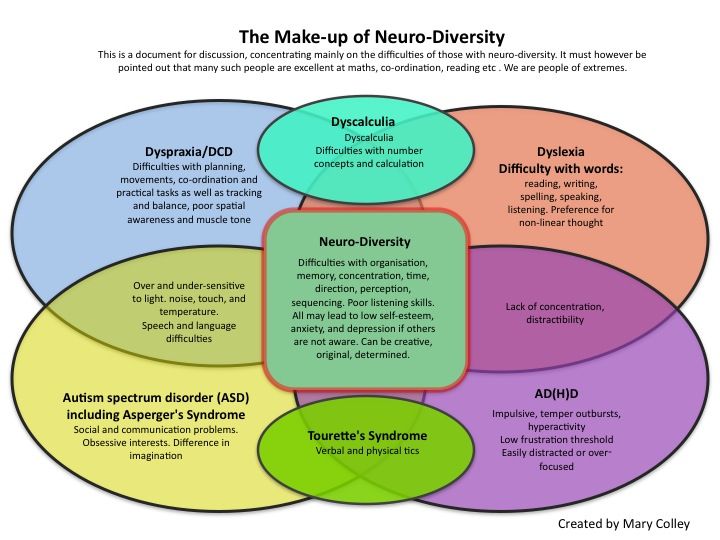 nine0003
nine0003
Tics can be caused by stress, fear, or a traumatic situation. As a rule, such children have increased anxiety, sleep disturbances, emotional instability, disorders of the neurotic circle.
In children, tics often occur after an infection. It often happens that the child seems to have already recovered from a cold, the tests returned to normal, but his cough persists. Pediatricians treat him for a long time and unsuccessfully, and in the end it turns out that the cough is a vocal tic. This example, in particular, convincingly demonstrates the need for a thorough examination in order to make a correct diagnosis. Motor tics are also often the result of an infection. There is a separate group of tics that have arisen after a streptococcal infection. They are symptoms of a complex autoimmune syndrome caused by streptococcus. nine0003
The basis of the mechanism of development of tics is a violation of the metabolism of certain substances (neurotransmitters) involved in the transmission of nerve impulses. The subcortical formations of the brain are affected - this is the part of the brain that is normally controlled by the cortex. With tics, it begins to function independently, which is why involuntary movements occur.
The subcortical formations of the brain are affected - this is the part of the brain that is normally controlled by the cortex. With tics, it begins to function independently, which is why involuntary movements occur.
Nervous tic. Causes and treatment
A tic is an accelerated, repetitive contraction of certain muscles, most commonly the face or arms. A nervous tic may look like a normal purposeful human movement, but in this case they are absolutely devoid of practical need. A nervous tic occurs without the "permission" of a person, only in the waking state and can rarely be suppressed by the will of the owner. Nervous tics are chaotic. nine0003
Automation of our movements without the participation of the cerebral cortex is handled by the extrapyramidal system of the brain. Excessive excitement in this area leads to the appearance of a tick, as one of the symptoms of an increase in the activity of the extrapyramidal system.
Most often, nervous tics appear in the mimic muscles of the face, for example, in twitching of the eyelids.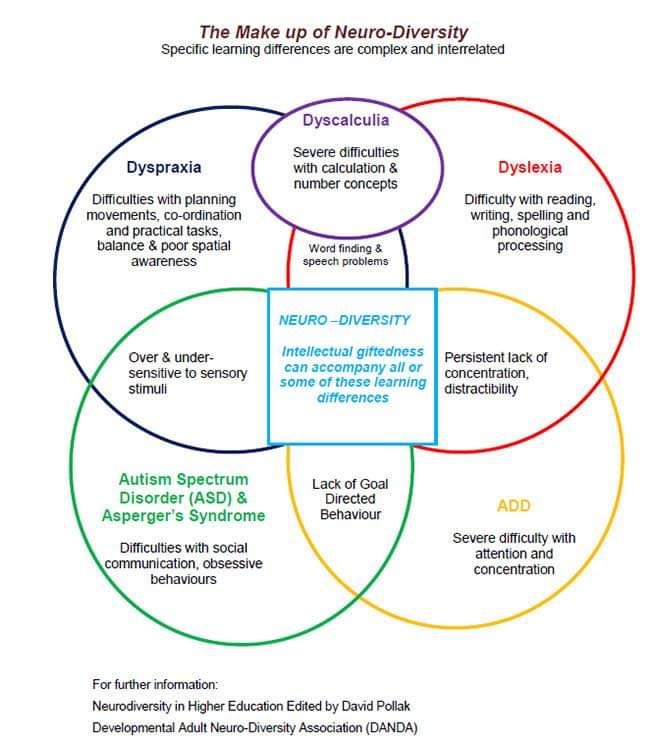 Almost every person who has experienced psycho-emotional stress is familiar with this symptom. In this case, a person can be absolutely healthy. A separate group prone to the appearance of tics is children aged 2-10 years. nine0003
Almost every person who has experienced psycho-emotional stress is familiar with this symptom. In this case, a person can be absolutely healthy. A separate group prone to the appearance of tics is children aged 2-10 years. nine0003
Nervous tics may be primary (pass as quickly as they started without medical intervention). The main causes of primary nervous tics in adults are frequent severe stress, exhaustion of the nervous system, and chronic fatigue.
There are many more reasons for the appearance of secondary nervous tics. These are (neuro-circulatory) dystonia, diabetes mellitus, kidney and liver diseases, brain tumors, injuries received during childbirth, trigeminal neuralgia, mental illness. This also includes past infectious diseases, the result of taking medications, carbon monoxide poisoning, etc. nine0003
Hereditary nervous tics are called Terett's disease. It affects children whose parents suffer from this pathology. The probability of transmission of the disease is 50%, while the severity of the course can be different and weaken with age.
In the reproduction of nervous tics, one muscle group or several may take part, in which case they are called complex. In addition, a nervous tic can begin in one location, and then affect more and more muscles incrementally. Such a nervous tic is called generalized. nine0003
The most common are mimic nervous tics: blinking, blinking, twitching of the nose, head, tongue sticking out, licking.
Motor nervous tics - involuntary movement of limbs: shrugging shoulders, throwing legs forward, clenching fists, etc.
Vocal tics: whistling, squeaking, clattering tongue, coughing, clearing throat, grunting, etc.
With sensory tics, a person feels discomfort in some part of the body and, as a result, makes involuntary movements. nine0003
Complicated nervous tics include: repetition of gestures, snapping fingers, rubbing certain places, jumping, repetition of abuse, simple, already said own or other people's words.
Diagnosis of nervous tics includes a blood test to detect inflammatory changes in the body.