Ocd rage what to do
Can OCD Make You Angry? Managing Anger and Fear With OCD
Obsessive-compulsive disorder (OCD) is marked by a cycle of unwanted, intrusive thoughts (obsessions) and ritualistic behaviors (compulsions) and can cause a wide range of symptoms in patients. If you or a loved one has OCD, these symptoms likely include bouts of anger or rage. You’re not alone in this: One small study found that 50% of patients with OCD experience anger attacks.
So, is anger a symptom of OCD? Does living with OCD cause one to become angry? There are quite a few reasons why you may experience anger alongside your OCD.
All NOCD Therapists are trained in ERP.
Book a free call to start your journey with a NOCD Therapist
What causes anger in OCD patients?
Some of the most common reasons for anger occurring in people with OCD may include:
- Reactions to medication
- Constant stress and anxiety
- Frustration with living with OCD and its symptoms
- Compulsions being interrupted or done incorrectly
One of the main characteristics of OCD is a seemingly never-ending sense of uncertainty. Compulsions are often performed to gain a sense of control over one’s obsessions and possible foreboding events, but these actions typically only offer temporary relief. Understandably, it can be extremely frustrating to feel a lack of control in life and to feel as if something terrible is always around the corner. This can lead to bouts of anger or rage that can be scary — both for the person experiencing it and their loved ones.
Because someone with OCD often feels like something terrible will happen if they don’t perform their compulsions, they can become extremely fearful if their compulsions aren’t going as expected.
If someone is performing compulsions and is interrupted, this may also trigger an anger attack. In this case, the anger may be directed specifically at the person who caused the interruption, which may put a strain on interpersonal relationships.
Similarly, if you are enacting compulsions and it feels like they are never quite right, that may lead to a bout of intense anger. Because someone with OCD often feels like something terrible will happen if they don’t perform their compulsions, they can become extremely fearful if their compulsions aren’t going as expected. This fear can quickly spiral into rage, even if it doesn’t have a specific target.
Because someone with OCD often feels like something terrible will happen if they don’t perform their compulsions, they can become extremely fearful if their compulsions aren’t going as expected. This fear can quickly spiral into rage, even if it doesn’t have a specific target.
Is OCD anger manageable?
When someone with OCD experiences anger or rage, it can be scary and may make them or their loved ones feel unsafe. These bouts can include screaming, hitting, throwing objects, attacking oneself or others and more. It’s easy to understand why these anger attacks occur, but it’s not as easy to feel like they are manageable.
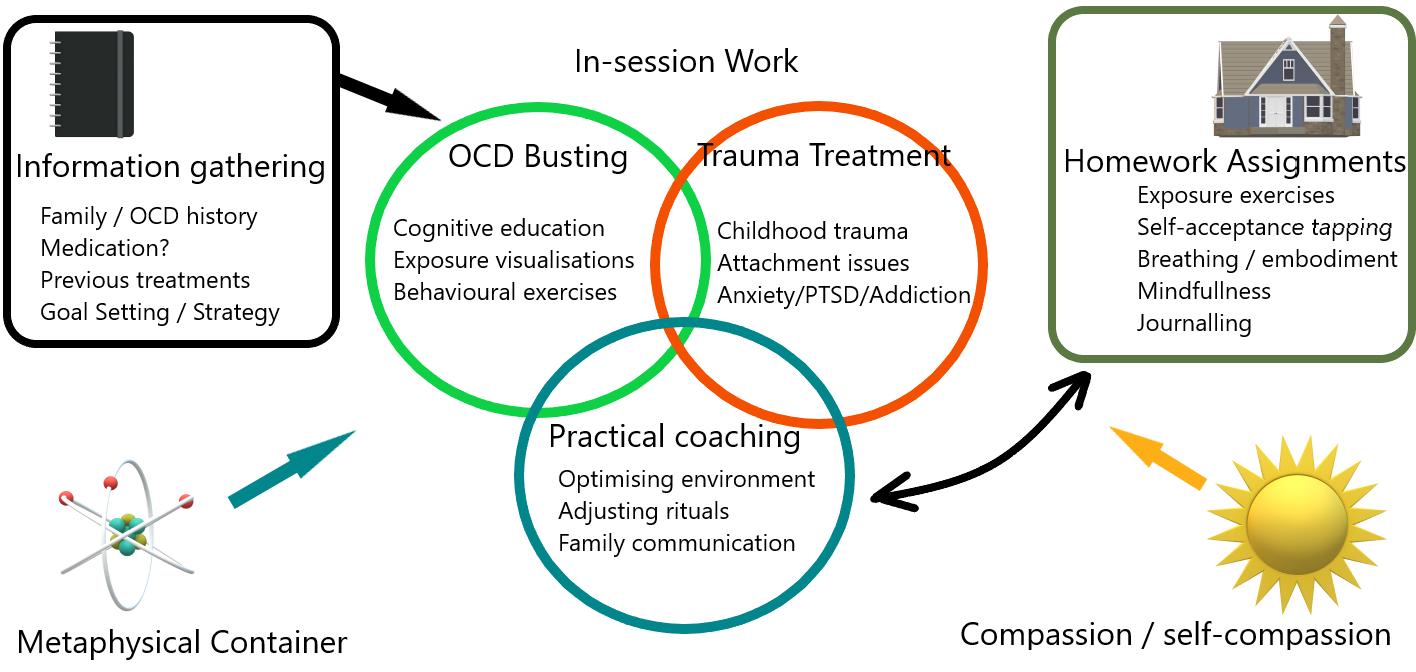
The good news is that anger that coincides with OCD is absolutely manageable through the overall treatment of OCD. In most cases, once the OCD is under better control, the anger will diminish or disappear entirely. If you’re looking for treatment for your OCD — and any related anger you might be experiencing — the best option is a form of cognitive behavioral therapy (CBT) called exposure and response prevention (ERP) therapy.
Commonly referred to as the “gold standard” of treatment for OCD, ERP therapy helps patients become more tolerant of the uncertainty they feel by being exposed to things that trigger their obsessions in a controlled environment. The goal of ERP therapy is to allow for the intrusive thoughts to occur while simultaneously resisting one’s compulsions.
As someone with OCD learns to better endure the uncertainty their disorder causes them, they may feel less overall frustration. Furthermore, as they increase the amount they become more resistant to the urges to engage in compulsions, it can help reduce the occurrence of anger from compulsions being interrupted or going poorly.
If you or a loved one is ready to manage anger associated with OCD, schedule a free call with the NOCD clinical team. Once matched with a therapist, NOCD clients can begin treatment from the comfort of their home through video sessions or phone calls. With ERP-licensed therapists available nationwide, you can be well on your way to finding freedom from the endless cycle of obsessions and compulsions — and any anger you might be experiencing as well — once and for all.
What Should I Do If I Am Struggling With OCD Anger?
Researchers suggest that approximately 51% of OCD sufferers report a reduction in their OCD symptoms, which suggests that this condition can be effectively managed. Managing anger can be tricky for anyone, let alone someone with OCD. And, when an OCD sufferer becomes angry, regardless of the reason, it can be unnerving for the individual and his or her friends, romantic interests or partner, and family members.
In some situations, intense anger can make loved ones feel “unsafe.” OCD anger attacks can include kicking, spitting, hollering, hitting, lashing out, crying, throwing things, biting, name-calling, cursing, bullying others, engaging in self-harm, and/or attacking others. So, while it may be possible to figure out what is causing the anger attacks, trying to figure out how to effectively manage your anger may be a bit more challenging.
According to researchers, when anger is linked to OCD it can be successfully managed with various OCD treatments, such as cognitive-behavioral therapy (CBT), exposure and response prevention (ERP) therapy, acceptance and commitment therapy (ACT), along with other psychotherapies, such as individual counseling, couples or marriage counseling, grief counseling, addiction counseling, group therapy, family therapy, trauma therapy, hypnotherapy (hypnosis) can help you better manage your OCD symptoms
and control your anger.
The universal go-to treatment for OCD is ERP therapy. ERP therapy is beneficial for OCD anger because it helps OCD sufferers become more tolerant of their doubts and the uncertainty they feel. This is accomplished through “exposure” and “desensitization.” More specifically, an ERP therapist “exposes” people with OCD to their OCD triggers, especially the ones that are triggering bouts of anger or rage.
Medications, like SSRI antidepressants, are one of the go-to treatments for OCD. SNRIs, tricyclic antidepressants, MAOIs, beta-blockers, antipsychotics, and/or prescription antihistamines can also be used when SSRIs (i.e., Paxil, Prozac, or Zoloft) and OCD therapies fail to work.
Neurosurgery (brain surgery) and neurosurgical procedures like capsulotomy, cingulotomy, electroconvulsive therapy (ECT), deep brain stimulation, and transcranial magnetic stimulation (TMS) therapy can also be options when other OCD treatments have failed. Note: In 2018, the FDA approved TMS as a possible treatment for OCD.
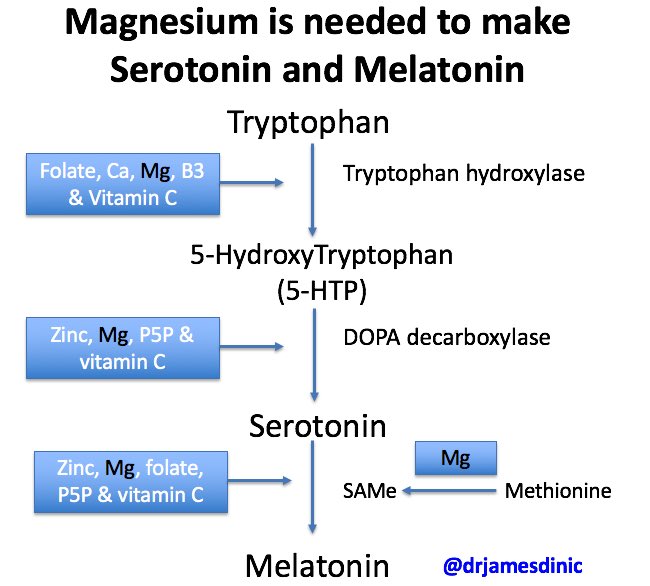
Natural remedies and self-help tools like vitamins and minerals (magnesium, B vitamins, n-acetylcysteine, zinc, etc.), herbs (CBD, St. John’s Wort, kava, borage oil, milk thistle extract, valerian root, Ashwagandha, etc.), acupuncture, light therapy, probiotics, massages, regular exercise, proper sleep, a healthy diet, spending time with friends and family, journaling, practicing yoga and/or mindfulness meditation, music therapy, OCD books, workbooks, and/or apps, OCD forums and support groups, and/or online OCD treatment programs, like Impulse Therapy can be added to your formal OCD treatment plan or used alone.
Once an OCD sufferer learns how to cope with the uncertainty of the condition, they may feel less frustrated, upset, and angry. And, as this individual learns healthy coping skills and strategies, they will become more resistant to the urges to engage in rituals or routines (compulsions). Once this person no longer experiences OCD urges and/or feels compelled to perform certain actions, they will be less likely to become angry.
In other words, once you learn how to resist your impulse to engage in compulsive behaviors, you will be able to more effectively manage your OCD anger. Because you will no longer be engaging in rituals or routines to quell your stress and anxiety and quiet your intrusive thoughts, urges, doubts, uncertainty, mental images, negative emotions, etc. (obsession), you will no longer have the anger risk factor of disrupted or halted compulsions – a possible cause of anger attacks.
Listed below are other ways you can manage your OCD anger:
- Challenge your thoughts and fears.
- Seek OCD help – your anger may dissipate once you have your OCD symptoms under control
- Brainstorm to determine what could be causing your OCD anger.
- Identify your OCD triggers and early warning signs so you can practice stress-management techniques before your anger gets out of control.
- Make a list of ways your friends, partner, and loved ones can support you as you address your anger issues.
- Take a “time-out” when you feel your anger escalating. Only emerge from “time-out” when you feel calmer and more collected.
- Sign-up for an anger management course at a local college.
- Give yourself a break. In other words, be mindful that everyone experiences anger from time to time, it is a natural emotion. Living with OCD can be depressing, anxiety-provoking, exhausting, and overall difficult.
- Pay attention to your accomplishments (big or small), instead of dwelling on what you cannot do.
- Stop being mad at or ashamed of yourself because you have OCD
- Regularly let someone you trust know how you are feeling and what you are experiencing.
- Stop comparing yourself to other people – you are your own person.
- Set boundaries with friends, family members, and romantic interests. Also, do not allow work or social commitments to overwhelm you.
- Set clearly-defined goals for reducing or eliminating your OCD anger
- Be an advocate for yourself.
 In other words, identify what you need to feel safe.
In other words, identify what you need to feel safe.
When combined, these “tools” not only help you manage your OCD symptoms but also help you keep your anger in check. The good news is in most cases, once your OCD symptoms are under control, your anger will likely decline or disappear altogether.
References
- Painuly, N. P., Grover, S., Mattoo, S. K., & Gupta, N. (2011). Anger attacks in obsessive-compulsive disorder. Industrial Psychiatry Journal, 20(2), 115–119. Retrieved from https://doi.org/10.4103/0972-6748.102501
- Burchi, E., Hollander, E., & Pallanti, S. (2018). From treatment response to recovery: A realistic goal in OCD. International Journal of Neuropsychopharmacology, 21(11), 1007–1013. Retrieved from https://doi.org/10.1093/ijnp/pyy079
- U.S. Food and Drug Administration (FDA). (2018). FDA permits the marketing of transcranial magnetic stimulation for the treatment of obsessive-compulsive disorder.
 Retrieved from https://www.fda.gov/news-events/press-announcements/fda-permits-marketing-transcranial-magnetic-stimulation-treatment-obsessive-compulsive-disorder
Retrieved from https://www.fda.gov/news-events/press-announcements/fda-permits-marketing-transcranial-magnetic-stimulation-treatment-obsessive-compulsive-disorder - Painuly, N. P., Grover, S., Mattoo, S. K., & Gupta, N. (2011). Anger attacks in obsessive-compulsive disorder. Industrial Psychiatry Journal, 20(2), 115–119. Retrieved from https://doi.org/10.4103/0972-6748.102501
- Cludius, B., Mannsfeld, A.K., Schmidt, A.F. et al. (2021). Anger and aggressiveness in obsessive-compulsive disorder (OCD) and the mediating role of responsibility, non-acceptance of emotions, and social desirability. Europe Archives Psychiatry Clinical Neuroscience, 271, 1179–1191. Retrieved from https://doi.org/10.1007/s00406-020-01199-8
- Zhang, Y. Y., Gong, H. F., Zhang, X. L., Liu, W. J., Jin, H. Y., Fang, F., Schneider, S., Mcingvale, E., Zhang, C. C., Goodman, W. K., Sun, X. R., & Storch, E. A. (2019). Incidence and clinical correlates of anger attacks in Chinese patients with obsessive-compulsive disorder.
 Journal of Zhejiang University. Science, 20(4), 363–370. Retrieved from https://doi.org/10.1631/jzus.B1800450
Journal of Zhejiang University. Science, 20(4), 363–370. Retrieved from https://doi.org/10.1631/jzus.B1800450 - Johnco, C., Salloum, A., De Nadai, A. S., McBride, N., Crawford, E. A., Lewin, A. B., & Storch, E. A. (2015). Incidence, clinical correlates and treatment effect of rage in anxious children. Psychiatry Research, 229(1-2), 63–69. Retrieved from https://doi.org/10.1016/j.psychres.2015.07.071
- Storch, E. A., Jones, A. M., Lack, C. W., Ale, C. M., Sulkowski, M. L., Lewin, A. B., De Nadai, A. S., & Murphy, T. K. (2012). Rage attacks in pediatric obsessive-compulsive disorder: phenomenology and clinical correlates. Journal of the American Academy of Child and Adolescent Psychiatry, 51(6), 582–592. Retrieved from https://doi.org/10.1016/j.jaac.2012.02.016
- Kawakami, M., & Nakayama, K. (2016). Seishin shinkeigaku zasshi = Psychiatria et neurologia Japonica, 118(7), 484–500. Retrieved from https://pubmed.ncbi.
 nlm.nih.gov/30620492/
nlm.nih.gov/30620492/ - Whiteside, S. P., & Abramowitz, J. S. (2005). The expression of anger and its relationship to symptoms and cognitions in obsessive-compulsive disorder. Depression and Anxiety, 21(3), 106–111. Retrieved from https://doi.org/10.1002/da.20066
symptoms, how to get rid of and treat
Olya Selivanova
struggles with obsessive-compulsive disorder
Author profile
Since childhood, I have suffered from obsessive thoughts.
When I was nine years old, I was reading a book, when suddenly the thought occurred to me: “If you don’t finish reading today, your mother will die.” The thought frightened me, I put down the book and cried, but I had to return to reading so that my mother would not die.
From that moment on, the frightening thoughts were different. I could suddenly change the route, because the thought came to my mind: “It is not safe to go further. Get around. " There were thoughts to harm loved ones: push, hit, pour over. At such moments, I thought that an evil force had entered into me, and I began to count to myself, imagined how the numbers increased in order in size and knocked bad thoughts out of my head.
" There were thoughts to harm loved ones: push, hit, pour over. At such moments, I thought that an evil force had entered into me, and I began to count to myself, imagined how the numbers increased in order in size and knocked bad thoughts out of my head.
By the time I was twelve, it all came to naught, and as a teenager, I decided that it was just childish oddities. But seven years later, the obsessive thoughts returned, and the doctor at the neuropsychiatric dispensary diagnosed me with Obsessive-Compulsive Disorder. I'll tell you how I was treated and how I live now.
Go see a doctor
Our articles are written with love for evidence-based medicine. We refer to authoritative sources and go to doctors with a good reputation for comments. But remember: the responsibility for your health lies with you and your doctor. We don't write prescriptions, we make recommendations. Relying on our point of view or not is up to you.
What is obsessive-compulsive disorder
Obsessive-compulsive disorder is a mental illness in which a person has obsessive thoughts and compulsive actions.
What is Obsessive-Compulsive Disorder - Mayo Clinic
Obsessive thoughts - obsessions - usually revolve around certain topics: fear of harming yourself and others, fear of germs and toxic substances, the need to organize everything. They appear suddenly or are provoked by external circumstances, such as a sharp object or the word "last".
Intrusive thoughts cannot be ignored, they cause anxiety or disgust. In response to them, a person has compulsions - a strong desire to perform certain actions that, according to his feelings, will get rid of such thoughts. Compulsions are difficult to resist: the anxiety will grow until the person gives up.
For example, the obsessive thought that a person will become infected after touching a doorknob will provoke compulsive actions - repeated washing of hands, sometimes for several hours in a row.
/shizofreniya/
How much does it cost to support a relative with a mental disorder
I try not to touch doorknobs in public places and always make sure the door is closed.
 Do I have OCD?
Do I have OCD? Sergey Divisenko
psychotherapist
If a person's condition does not interfere with himself or others, then everything is in order, if it interferes, a disorder can be suspected. In the case of checking the door, one can say that checking if the door is closed once is not a problem, rechecking the door several times in a row and doing it systematically is already a problem.
To understand whether or not there is OCD, the doctor pays attention to how often the patient has obsessive thoughts and compulsive actions and how they affect his life. If symptoms occur more frequently in two weeks than in seven days and interfere with daily activities, it is probably OCD.
In this case, the symptoms should have the following characteristics:
- The person should evaluate them as his own thoughts and desires.
- There must be at least one thought or action that the person unsuccessfully resists.
- The thought of a person performing a compulsive action should not in itself be pleasurable.
 The fact that an action will help reduce anxiety is not considered pleasant in this sense.
The fact that an action will help reduce anxiety is not considered pleasant in this sense. - Thoughts or actions must be repeated.
How obsessive-compulsive disorder is treated
OCD is considered a lifelong disorder, but with treatment it is possible to achieve remission: to get rid of obsessive thoughts and compulsive actions for a long time or to reduce their number.
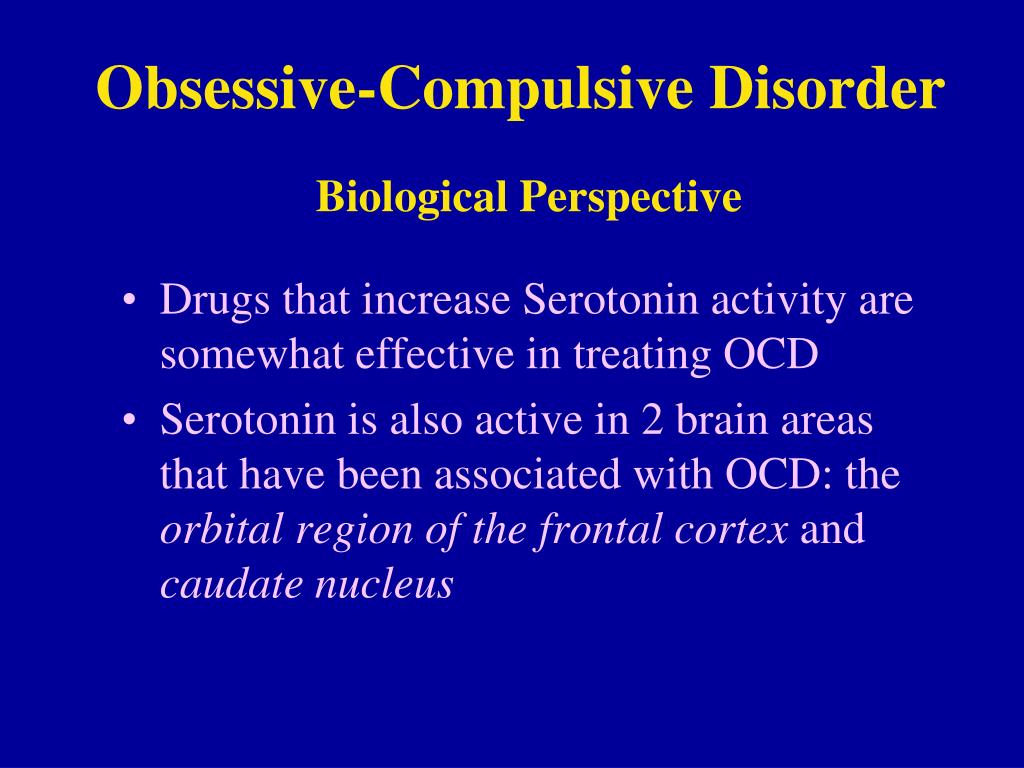
Medical treatment. The main drugs for the treatment of OCD are antidepressants of the SSRI group. They increase serotonin levels in the brain, making OCD symptoms less likely to occur.
Treatment options for OCD - NHS
Depending on the course of the disease and symptoms, along with antidepressants, the doctor may prescribe other drugs: tranquilizers, neuroleptics or mood stabilizers.
Cognitive behavioral therapy. This is a type of psychotherapy during which a person learns to control their emotional response to intrusive thoughts.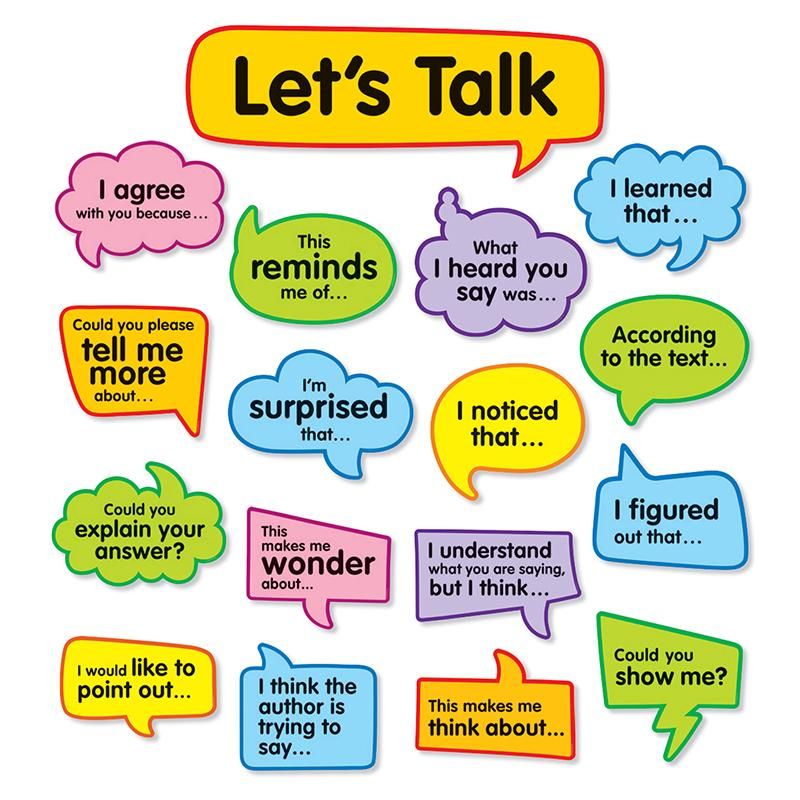 As a result of therapy, obsessive thoughts cease to cause anxiety and compulsive actions.
As a result of therapy, obsessive thoughts cease to cause anxiety and compulsive actions.
Cognitive behavioral therapy - NHS
Order of the Ministry of Health of the Russian Federation of September 16, 2003 No. 438 "On psychotherapeutic care"
Psychiatrists, psychotherapists and psychologists are involved in the treatment of OCD in Russia. Psychiatrists prescribe prescription drugs. Psychotherapists and psychologists conduct psychotherapy sessions.
How I was diagnosed
At the age of 19, the development of the disease took a new turn. I was washing the kitchen knife and I had an obsessive thought that I was losing control and could cut myself and the guy who was nearby at that moment. So I began to avoid sharp objects, there was an irresistible desire to hide or throw them away.
Obsessive thoughts revolved around the topic of death: drinking nail polish remover, bleach, vinegar, throwing yourself under a vehicle or jumping out of a window. Because of this, I removed all dangerous liquids from the house and stayed away from open windows, highways and train station platforms. I didn’t sleep well at night, suffered from anxiety, considered myself crazy and dangerous, and began to move away from everyone.
Because of this, I removed all dangerous liquids from the house and stayed away from open windows, highways and train station platforms. I didn’t sleep well at night, suffered from anxiety, considered myself crazy and dangerous, and began to move away from everyone.
I also doubted everything. Even if I just performed an action, it seemed to me that it was not completed. I opened the door to make sure that it had been closed before, closed it again, pulled the handle, asked those around me if the door was exactly closed. I could wake up at night and see if the stove was turned on, although before going to bed I went up to it and stared without blinking - so that it would crash into my memory that it was definitely turned off. My young man, seeing all this, insisted that we try to see a psychologist.
In Irkutsk, where I live, psychiatric care can be obtained free of charge at the regional psycho-neurological dispensary. I turned to the psychotherapeutic department of the dispensary for a consultation with a psychologist. At the reception, they brought me a card and said that there was no appointment with a psychologist for the next few days, but I could get to a psychiatrist: there are fewer people who want to see him.
At the reception, they brought me a card and said that there was no appointment with a psychologist for the next few days, but I could get to a psychiatrist: there are fewer people who want to see him.
/spravka/
How to get a certificate from the PND
At the appointment with the psychiatrist, I told about what was happening to me. The doctor was not surprised and said that it was an obsessive-compulsive disorder. It was the first time I heard my diagnosis, but I didn't believe it. On the Internet, I came across information that OCD is only pedantry, handwashing, fear of germs and perfectionism, and not the creepy things that come to my mind. The psychiatrist said that OCD was treated with antidepressants and offered to write a prescription, but I refused treatment because I thought they were serious drugs that would do more harm than help.
How a visit to a neuropsychiatric dispensary with OCD will affect later life
Sergey Divisenko
psychotherapist
The patient could move freely, drive a car, use weapons and work.
With an OCD diagnosis, you can still work in any job, there are no legal barriers to this. With regard to cars and weapons, the situation has changed. In 2014 and 2015, government decrees appeared, according to which OCD became a contraindication for driving and owning weapons.
However, from a psychiatrist's point of view, a person diagnosed with OCD can drive a car and use a weapon. Doctors of the psycho-neurological dispensary still give a certificate about this, but they do it through a medical commission.
Treatment
First hospitalizationMy condition worsened, I tried to ignore obsessive thoughts. But the more I resisted them, the stronger they became. In addition, anger, irritability and constant fatigue appeared.
With new symptoms, I decided to see an endocrinologist, because I heard that this happens with problems with the thyroid gland. According to the results of ultrasound and hormone tests, the thyroid gland was in order. Then I made an appointment with a neurologist, but he also said that this was not his profile. Both doctors suggested that my constant fatigue, anger and irritability were symptoms of depression and advised me to seek psychiatric help.
Then I made an appointment with a neurologist, but he also said that this was not his profile. Both doctors suggested that my constant fatigue, anger and irritability were symptoms of depression and advised me to seek psychiatric help.
Symptoms of clinical depression - NHS
I researched information about depression and realized that antidepressants could help, all I had to do was get a prescription. I came to the psychotherapeutic department again, but there was already another psychiatrist there. Since my condition worsened, instead of a prescription, he wrote out a referral for hospitalization in a day hospital. I had prejudices about a psychiatric hospital, so I did not want to visit the hospital. But there was no strength to argue with the psychiatrist.
This is how a referral for hospitalization to a day hospital looks like The next day I was already in the hospital. During the registration, the psychiatrist on duty asked what I was complaining about, measured the pressure and examined whether there were injuries on the body.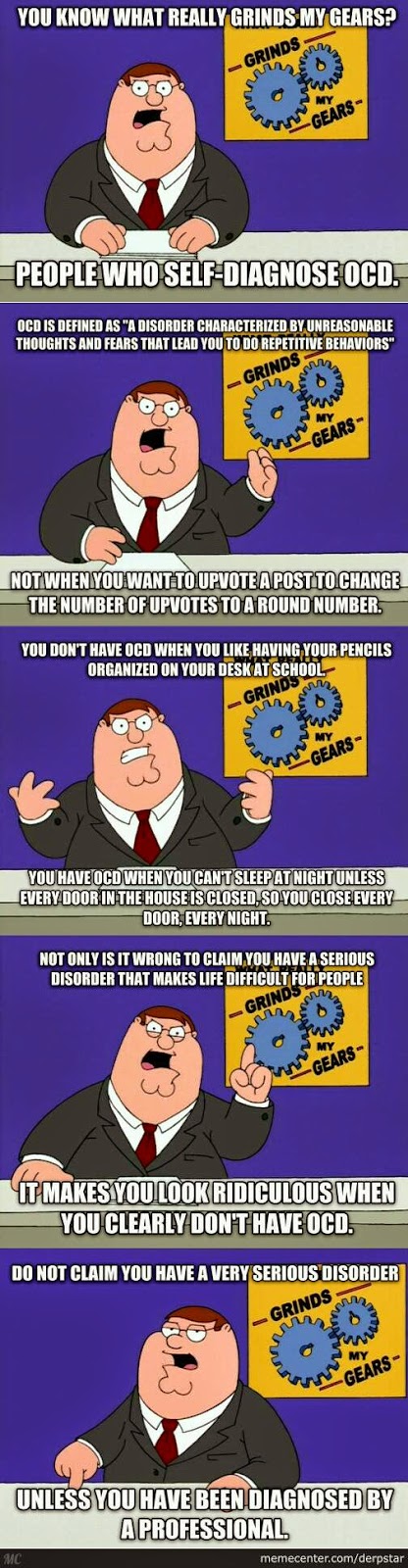 It turned out to be difficult for me to talk about the symptoms: there was a feeling that they would not believe me, or vice versa, they would believe me so much that they would put me in a round-the-clock hospital. But everything was fine, the psychiatrist wrote down the data on the card, gave it to the orderly, and together with him sent me to the head.
It turned out to be difficult for me to talk about the symptoms: there was a feeling that they would not believe me, or vice versa, they would believe me so much that they would put me in a round-the-clock hospital. But everything was fine, the psychiatrist wrote down the data on the card, gave it to the orderly, and together with him sent me to the head.
The manager looked at the card, confirmed the diagnosis of OCD and depression, and prescribed treatment: an antidepressant, an antipsychotic, a mood stabilizer, tranquilizer tablets, and injections of B vitamins.
/guide/vitamins/
Vitamins: what foods contain and how to take supplements
The routine in the hospital was as follows: I arrived at eight in the morning, had breakfast and took the prescribed pills, took injections, dined and went home. Tablets were issued immediately for one day, but they could also be issued for two days, for example, before the weekend. Once after the injection, I went to an appointment with a clinical psychologist, he gave various tests and questionnaires that tested logic and intelligence.
About three times a week I went to see a psychiatrist in the same hospital. I told her about my condition and asked questions. I thought that as soon as I start taking medication, my mood will rise and my anxiety will go away. But this did not happen, so it seemed that everything was in vain and the treatment had to be abandoned. The psychiatrist explained to me that not all drugs begin to act instantly, she assured me that we were on the right track and we had to wait. These conversations made it easier. In my case, antidepressants began to work only on the third month of admission, when I no longer visited the day hospital.
Treatment at the day hospital lasted a month. All medications, medical consultations and meals were free. I spent money only on the road to the hospital and back - 600 R by public transport for the whole time.
/bye-depression/
“It reminded me of a strict regime sanatorium”: how much I spent on treating depression
After treatment, the symptoms of depression remained, but obsessive thoughts began to bother me less often: I stopped being afraid of open windows and was able to ride the escalator. Treatment had to be continued on an outpatient basis. Before I was discharged, the psychiatrist said that she would transfer my data to the psychiatric department. Now I will need to come to the local psychiatrist for prescriptions for medicines, and turn to him if the condition worsens or questions arise.
During the treatment in the hospital, I doubted everything. Even in being sick. Not only the psychiatrist, but also relatives helped to cope.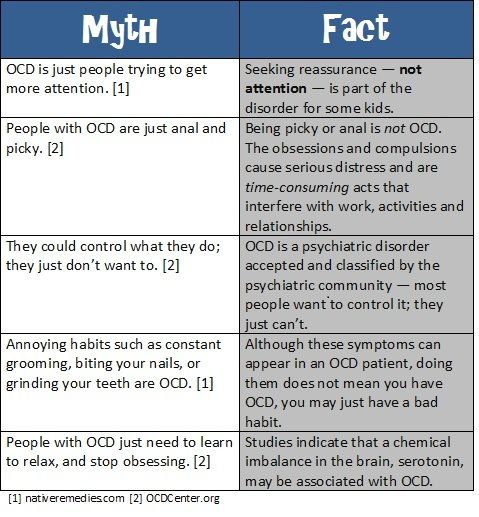 They noticed the changes, but my young man did not let me stop the treatment
They noticed the changes, but my young man did not let me stop the treatment Treatment
Visiting a local psychiatristAfter I was discharged from the hospital, I came to the registration office of the psychiatric department with a passport and I was immediately sent to the district police officer. The doctor did not change the treatment and wrote out a prescription for the same medicines that were given in the day hospital. In the future, a referral to the district police officer was also not required. I just came to the appointment when I needed to update the prescription.
Government Decree of July 30, 1994 No. 890 with a list of categories of beneficiaries who are entitled to free medicines
District psychiatrists were different: some were polite, some were rude and rude. Using the brute force method, I found two normal specialists - when I made an appointment at the reception, I began to ask to be directed to them. Usually the registrar complied with my request.
Spent in six months of outpatient treatment — 8895 Р
| Preparation | Spending |
|---|---|
| Antidepressants | 5988 P |
| Normotimics | 2384 P |
| Antipsychotics | 419 P |
| Tranquilizers | 104 Р |
Antidepressants
5988 R
Normotimics
2384 R
neuroleptics
419 419 p
Transquilizers
104 R
Free medicines for the treatment of OCD are provided to certain privileged categories of people. I’m not a beneficiary, so I bought everything with my own money. Pharmacies don’t require a passport, but they put the date of issue of the medicine on the back and don’t sell more than prescribed by prescription. For example, according to a prescription for three months, I was given only three packs of an antidepressant. When I wanted to buy one more to have a supply, the pharmacist refusedTreatment
Second hospitalization and psychotherapy After six months of outpatient treatment, the district psychiatrist recommended to be treated again in the hospital.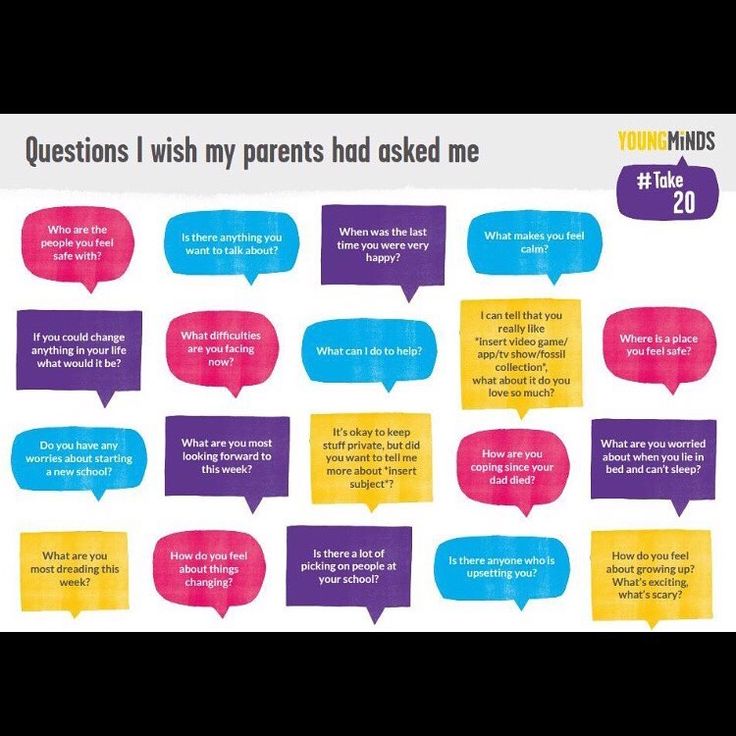 Antidepressants helped: my mood improved, I got energy and I wanted to live, but I felt a side effect from antipsychotics. I was terribly sleepy, my handwriting changed, it was difficult to write in class and generally follow the train of thought of the teacher. In addition, there were more intrusive thoughts.
Antidepressants helped: my mood improved, I got energy and I wanted to live, but I felt a side effect from antipsychotics. I was terribly sleepy, my handwriting changed, it was difficult to write in class and generally follow the train of thought of the teacher. In addition, there were more intrusive thoughts.
In the day hospital, I was treated by the same psychiatrist as the first time. She adjusted the drug treatment so that I was not bothered by intrusive thoughts. She also said that a psychotherapist had appeared in the hospital and referred me to her for a consultation.
Unlike the psychiatrist's consultations during the first hospitalization, we did not discuss drugs and their effects with the psychotherapist. We talked about what is happening to me and what other methods can be used to combat this, in addition to drugs. At the first appointment, I briefly talked about my lifestyle, obsessive thoughts, compulsive actions, and how I tried to resist them even before the treatment.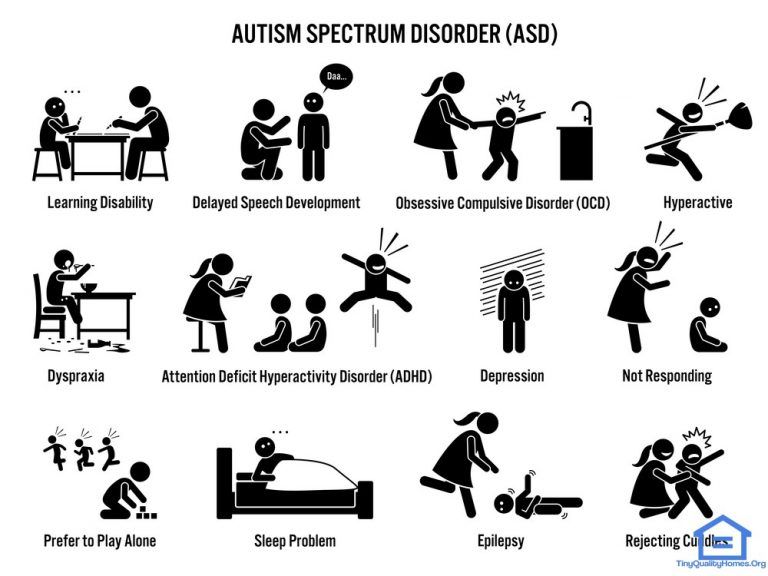 Then the doctor explained to me what obsessive-compulsive disorder is and how it manifests itself, why my struggle only worsened the condition and led to depression.
Then the doctor explained to me what obsessive-compulsive disorder is and how it manifests itself, why my struggle only worsened the condition and led to depression.
/psychotherapy-search/
How to choose a psychotherapist
We agreed that I would try to keep the number of compulsive acts to a minimum, and I would cope with anxiety from intrusive thoughts with the help of techniques.
Speak key phrases. Thoughts in themselves mean nothing, they can come to mind automatically. We agreed that when I had an obsessive thought, I would simply tell myself that it was a manifestation of OCD. Here are the two phrases that I used: “This is just my thought that…”, “I know that this thought is a manifestation of OCD…” So gradually I stopped identifying myself with my thoughts and realized that thinking about the bad is does not mean to be a bad person.
Separately, we discussed the issue of the materialization of thoughts. When terrible things are spinning in your head, and you hear from everywhere that thoughts are material, you get very worried. We discussed the fact that thoughts are intangible and you can’t invite trouble with them. This made it easier and the degree of emotions decreased.
When terrible things are spinning in your head, and you hear from everywhere that thoughts are material, you get very worried. We discussed the fact that thoughts are intangible and you can’t invite trouble with them. This made it easier and the degree of emotions decreased.
Observe how the body reacts to anxiety. Every time I had anxiety from obsessive thoughts, I did not run away from it, but watched my body. I was shaking, my heartbeat increased, my breathing quickened, but I continued to live it. The psychotherapist said that I would not die from this. Yes, it is unpleasant and scary, but when you live emotions, you gradually learn to cope with them.
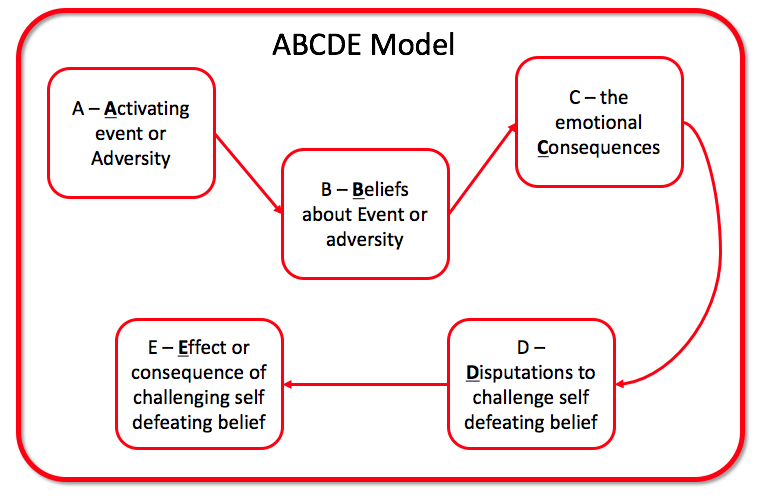
Keep a diary. In the course of the sessions, I became convinced that I cannot control the thoughts themselves - it is impossible, but I can control the reaction to them. So I started keeping a diary.
/psychotherapy/
How psychotherapy works
It was necessary to take notes according to the formula: A - situation, B - my thoughts, C - my emotions. Using such records, it is easier to track the thoughts that cause negative emotions and work them out. For example, when I could not fall asleep for a long time, I began to think that something was going wrong, and this caused anxiety. Then I wrote down the whole situation in a diary and instead of negative thoughts I formulated new ones: "My sleep does not depend on my will, and this is normal." It helped to get rid of anxiety, stop trying to sleep and go about your business. About half an hour later I went to bed and fell asleep peacefully.
Using such records, it is easier to track the thoughts that cause negative emotions and work them out. For example, when I could not fall asleep for a long time, I began to think that something was going wrong, and this caused anxiety. Then I wrote down the whole situation in a diary and instead of negative thoughts I formulated new ones: "My sleep does not depend on my will, and this is normal." It helped to get rid of anxiety, stop trying to sleep and go about your business. About half an hour later I went to bed and fell asleep peacefully.
| I also kept a mood diary. Before treatment, there was no point in monitoring the mood: it always turned out to be bad or indifferent | On antidepressants, I began to make entries in a diary every day and could track what affects my mood |
I also kept a mood diary. Before treatment, there was no point in monitoring the mood: it always turned out to be bad or indifferent. On antidepressants, I began to make entries in a diary every day and could track what affects my mood
Before treatment, there was no point in monitoring the mood: it always turned out to be bad or indifferent. On antidepressants, I began to make entries in a diary every day and could track what affects my mood
In the day hospital, I was treated for a month and a half, during which time I had only five sessions with a psychotherapist. All sessions, meals and drugs, as in the first hospitalization, were free. The only thing I had to spend money on was the road to the hospital and back, as well as the original antidepressant instead of the analogue provided in the dispensary. The doctor recommended the original, it suited me better.
3202 Р
spent on medicines and transport for a month and a half of treatment in the hospital
When I was discharged, the doctor told me that I was in a stable condition, the treatment helped me. I myself felt it: the mood was consistently good, and I quickly coped with obsessive thoughts. I was canceled all the drugs, except for antidepressants, then I had to continue taking them, be observed by the district psychiatrist and monitor my condition.
I was canceled all the drugs, except for antidepressants, then I had to continue taking them, be observed by the district psychiatrist and monitor my condition.
Spent one and a half months of treatment in a hospital — 3202 Р
| Expenditures | Spending |
|---|---|
| Antidepressants | 2422 R |
| Transport | 780 Р |
Antidepressants
2422 R
Transport
780 R
How do I feel after treatment
I stopped taking antidepressants a year and a month after discharge I spent another 14,640 R on them. Sometimes I have obsessive thoughts and compulsive actions, but I do not scold myself for this. I know that if I get upset, the symptoms will become more frequent. The psychiatrist warned me that OCD symptoms may appear periodically, but this is normal.
14,640 Р
spent on antidepressants for a year and one month
Coronavirus last spring was a test of strength for me. The condition worsened, compulsive actions resumed, I stopped leaving the house, I began to choke on the street, obsessive thoughts about death appeared. But I managed it on my own with the help of techniques taught to me by the therapist. I kept in my head the idea that if it worked then, it will work now.
The condition worsened, compulsive actions resumed, I stopped leaving the house, I began to choke on the street, obsessive thoughts about death appeared. But I managed it on my own with the help of techniques taught to me by the therapist. I kept in my head the idea that if it worked then, it will work now.
Before treatment, it was difficult for me to talk about my disorder. And now I openly talk about it and I can even joke about random manifestations of OCD. Almost everyone in my circle knows that I was being treated for OCD and depression. They help me notice compulsive actions and stop in time, treat me with understanding when I ask obvious things just in case - for example, did I close the door.
How often do people with OCD need to take drugs for life
Sergey Divisenko
psychotherapist
With the help of treatment, you can achieve remission - for a long time to get rid of the symptoms of OCD or reduce their number. Remission can occur both against the background of taking medications, and without them, against the background of psychotherapy.
Approximately 80% of patients with OCD stop taking medication sooner or later.
How much does OCD treatment cost?
In total, I treated OCD for one year and nine months. Of these, she was treated in a day hospital for two and a half months, and for a year and seven months - on an outpatient basis.
In the hospital, I only spent money on transport to and from the dispensary. Even during the second hospitalization, on the recommendation of the doctor, she bought antidepressants at the pharmacy and took them instead of those given in the hospital. The rest of the drugs, consultations and meals were free.
6 useful services for finding a psychotherapist
Most of the expenses are medicines during outpatient treatment.
Spent on OCD treatment for 1 year and 9 months — 27,337 R
| Expenditures | Spending |
|---|---|
| Antidepressants | 23 050 Р |
| Normotimics | 2384 P |
| Antipsychotics | 419 P |
| Tranquilizers | 104 Р |
| Transport during hospitalization | 1380 Р |
Save
- Obsessive Compulsive Disorder or OCD is a mental illness in which a person experiences obsessive thoughts and compulsive actions.
- OCD is considered a lifelong disorder, but remission can be achieved with the help of psychotherapy and drugs.
- OCD is treated in Russia by psychiatrists, psychotherapists and psychologists. Psychiatrists prescribe prescription drugs. Psychotherapists and psychologists conduct psychotherapy sessions.
- A visit to a neuropsychiatric dispensary will not prevent people with OCD from moving freely, driving a car, using weapons, or getting a job.
- Patients with OCD can receive care free of charge in state neuropsychiatric dispensaries or at their own expense in private clinics.
Did you also have an illness that affected your lifestyle or attitude? Share your story.
Tell
Treatment of obsessive-compulsive disorder
Treatment of obsessive-compulsive disorder. We will relieve you of obsessive thoughts, movements and rituals. Let's get back to life!
Symptoms of obsessive-compulsive disorder
- Frightening images and drives
- Compulsive acts (rituals)
- Intrusive check of one's own actions
- Fear of trouble, pollution or contamination
- Inexplicable desire to count something
- Excessive organization and pedantry
- Perfectionism in relationships, work and even leisure
- "Stuck", "looping" on one's thoughts
You feel that over time your mood becomes worse: apathy, depression, obsessions increase, and rituals begin to fill all your free time or harm your physical health.
You may have had more than one meeting with psychologists, psychotherapists and psychiatrists. You are not given the "scary" psychiatric diagnoses of Schizophrenia or Bipolar Disorder, but are prescribed medication and psychotherapy nonetheless. However, such treatment cannot be called effective - the symptoms persist and only aggressive pharmacotherapy temporarily reduces anxiety.
What is obsessive-compulsive disorder?
Obsessive-compulsive disorder is a syndrome characterized by the presence of obsessive thoughts (obsessions) to which a person reacts with certain actions (compulsions). The causes of the disorder are rarely superficial. The syndrome is also accompanied by the development of obsessive memories and various pathological phobias. May be chronic, episodic or progressive.
Obsession - obsessive thought, persistent desire for something, uncontrollable and accompanied by anxiety and intense anxiety. In an attempt to cope with such thoughts, a person resorts to committing compulsions.
Compulsion - an irresistible need to perform certain actions (rituals), which can be assessed by the person himself as irrational or meaningless, and the internal need to perform them is forced and is the result of obsessive ideas.
Common examples of OCD manifestations
- An exaggerated sense of danger. Fear of the materiality of thoughts:
- "now I will lose control and hurt my loved ones"
- "something terrible is about to happen, I can feel it"
- "I shouldn't think like that, all this will come true because of me"
- Pathological fear of pollution. Thirst for Purity
- Excessive perfectionism, exaggerated responsibility - "everything must be done perfectly", "everything depends on me, mistakes are unacceptable"
How does this painful algorithm work?
Most people have unwanted or obsessive thoughts quite often, but all sufferers of the disorder greatly exaggerate their importance. Fear of one's own thoughts leads to attempts to neutralize the negative feelings that arise from obsessions, for example by avoiding thought-provoking situations or by engaging in "rituals" of excessive self-cleansing or prayer.
Fear of one's own thoughts leads to attempts to neutralize the negative feelings that arise from obsessions, for example by avoiding thought-provoking situations or by engaging in "rituals" of excessive self-cleansing or prayer.
As we noted earlier, repetitive avoidance behavior can "get stuck", "loop", that is, have a tendency to repeat. The cause of obsessive-compulsive disorder is the interpretation of intrusive thoughts as catastrophic and true.
If you periodically experience over the years:
- Constant or fluctuating anxiety
- The need to perform certain ritualized actions
- A persistent decline in the quality of life due to the need to avoid certain thoughts and actions, places and events
And you are also persecuted:
- Significant problems in studies and career
- Failure to establish a serious relationship
- Constant criticism and pressure from relatives
- Many senseless activities
- Excessive involvement in computer games and the Internet, alcohol
- Loneliness and isolation
We strongly recommend that you do not delay seeking help and that you complete a remedial program.
Consultations and psychotherapeutic sessions according to the program are held several times a week, until the relief of severe symptoms, then the frequency of meetings with specialists is reduced to 2–3 per month. Count on the fact that in the end we will deal with your problem together.
Treatment of obsessive-compulsive disorder in Neuro-Psi
Every day, the specialists of the NEURO-PSI clinic analyze the world practice in the field of psychiatry and psychotherapy. The goal is the impartial selection and implementation of those methods of treatment and psychological assistance, the effectiveness of which has been convincingly proven in independent studies.
We are guided by the principles of evidence-based medicine and use as a basic method of treatment a psychotherapeutic paradigm, the effectiveness of which has been widely recognized by the professional community.
1. What is the essence of the obsessive-compulsive disorder treatment program?
A comprehensive work is carried out with the client, taking into account the main factors that create well-being.
The main emphasis is on teaching the client how to properly respond to his thoughts, emotions, inner feelings and interpretation of external events.
All types of psychotherapeutic and drug treatments serve the same goal: to achieve the best result in the shortest possible time. At the same time, by coordinating the efforts of specialists in various fields, the most complete coverage of all types of mental illnesses, disorders and disorders is possible.
2. What treatments are used
- Priority:
- Cognitive-Behavioral Therapy.
- Schema Therapy.
- Reality Therapy.
- Choice Theory.
- Rational pharmacotherapy.
- Psychopharmacotherapy (if indicated)
- Biofeedback Therapy
- Rational psychocorrection of stress
- Jacobson progressive muscle relaxation.
- Traditional and modern gymnastic systems, relaxation techniques.
- Breathing techniques .

- Stress exposure.
- Self-control training.
- Lifestyle modification
- Work with bad habits.
- Diet correction.
- Professional and social adaptation.
3. How is the treatment under the program
Each treatment program at the NEURO-PSI clinic consists of four stages:
- diagnostics,
- work with disease symptoms,
- work with the causes of the disease,
- consolidation of the achieved results.
Work efficiency is increased by dividing the treatment process into a predetermined number of sessions, at convenient times and without hospitalization. This means that each program is adapted to the problem that the client has addressed.
The treatment method is predictable, time-limited, productive, and most importantly, understandable for the client.
Of course, the treatment takes place in a comfortable mode without interruption from work, study or family. Improvements in well-being and mood (cure) occur in stages: after a decrease in emotional problems, bodily symptoms decrease. Working with the causes (etiology) of obsessive-compulsive disorder helps to avoid relapses in the future.
Improvements in well-being and mood (cure) occur in stages: after a decrease in emotional problems, bodily symptoms decrease. Working with the causes (etiology) of obsessive-compulsive disorder helps to avoid relapses in the future.
4. What are the results and forecast
Upon completion of the program, you get rid of obsessive thoughts and rituals, fear of pollution, unmotivated fears, panic attacks and multiple vegetative symptoms (sudden jumps in blood pressure, heart palpitations, dizziness, nausea).
According to statistics, the effectiveness of the methods used approaches 100% if all recommendations of specialists are followed.
Skills you acquire during the program:
- self-control and self-regulation
- constructive analysis of the state of the body
- understanding one's own mental and emotional sphere
- ability to control one's attention
- ability to act consciously in stressful situations
Significantly improves the emotional and physical condition, gaining self-confidence, in the future.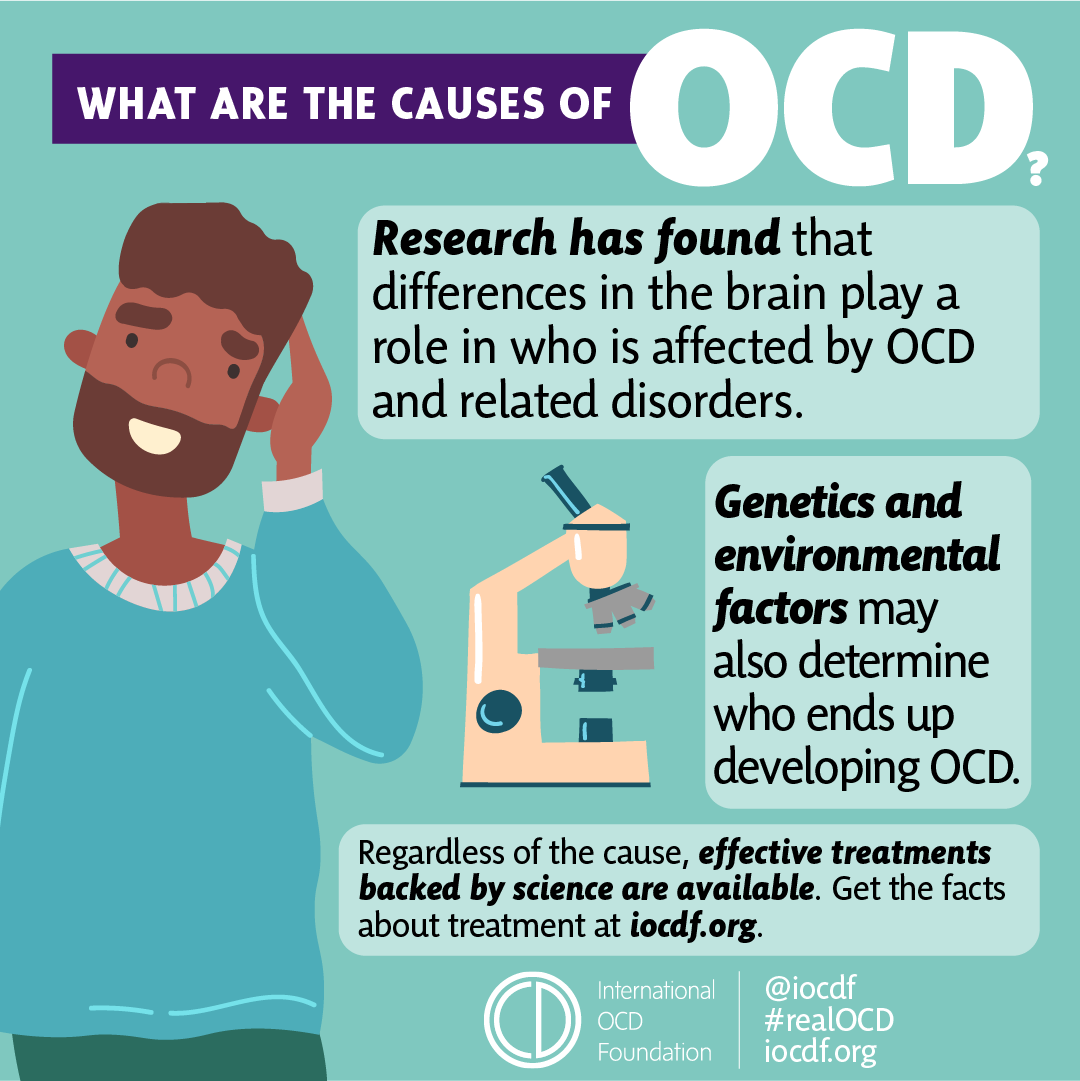 Emotional stress is removed, sleep and appetite are restored. The efficiency is greatly increased.
Emotional stress is removed, sleep and appetite are restored. The efficiency is greatly increased.
Specialists
- Rakhmanov Vladimir Alexandrovich
Psychiatrist, CBT-, ACT- and CFT-psychotherapist.
in the clinic online
Adults (over 18 years old) Elderly (from 60 years old)
Scientific approach. Horizon.
Founder and CEO of the Neuro-Psi network. Psychiatrist and psychotherapist.
As a psychiatrist, Vladimir works strictly in the evidence-based approach (Evidence-based Medicine). As a psychotherapist, he uses modern “rational” methods of psychotherapy (CBT, ACT, CFT, Scheme Therapy)
Vladimir is distinguished by a broad clinical outlook, professional awareness, and a comprehensive understanding of the patient's problem. These qualities are especially important in dealing with complex cases.

Vladimir specializes in working with the following client problems: professional burnout, depressed mood, excessive anxiety, despondency, indecision, regret about missed opportunities, intolerance for uncertainty, loss of meaning and direction in life. Chronic pain, psychosomatic and somatopsychic diseases. Isolation, avoidance of difficulties, loneliness. Does not work with suicidal behavior, addictions of any type, does not conduct outpatient appointments for patients who are hospitalized.
“Difficult tasks, whether it be a health problem or a life catastrophe, require more than perseverance in overcoming. Often a negative course of events changes the intellectual effort - making meaningful decisions based on objective data.
Read more
★9.81 based on 14 reviews
- Chibikova Evgenia Yurievna
Child psychiatrist, adult psychiatrist.
at the clinic online
Children (0-17 years old) Adults (18 to 60 years old)
Concentration.
 Care.
Care. Regularly trains and studies abroad. Thanks to this, he is able to prescribe effective, but at the same time the safest drugs.
Filigree in neurochemistry.
Read more
★9.71 based on 112 reviews
- Kuznetsov Sergey Olegovich
Psychologist. Cognitive behavioral psychotherapist. Family psychotherapist
in the clinic online
Teenagers (16 to 17 years old) Adults (18 to 60 years old)
Clarity. Impartiality.
Outline your problem and steps to fix it. Support on the path of real change. Shows the problem for what it is. Do not embellish and do not add something of their own. Demonstrates an alternative attitude in therapy so that you can live it from your own experience, and not theoretically.
Read more
★9.
 83 based on 52 reviews
83 based on 52 reviews - Dobrovidova Natalya Alexandrovna
Psychologist. Cognitive behavioral psychotherapist. PhD
in the clinic online
Adults (18 to 60 years old) Adolescents (from 14 to 17 years old)
Humanism. Environmental friendliness.
Will teach you how to manage your mental life. She is convinced that "our thoughts are the basis of our mental health and happiness", "and neurosis is a choice." It will help you make a choice in your favor. In fact, it forms a new way of thinking and new habits (which is so difficult to do without help and support). Such changes in the psyche lead to significant changes in life. He believes in every person and considers this the basis of quality therapy.
Read more
★9.64 based on 41 reviews
- Trofimova Marina Ivanovna
Cognitive Behavioral Psychotherapist.
 Sexologist.
Sexologist. in the clinic online
Adults (from 18 to 60 years old)
Non-judgmental. Result.
Can quickly and clearly show the connection between thoughts and emotions that affect life. Teaches you to overestimate the beliefs and attitudes that reduce the quality of life. Helps clients to move towards the goal step by step, respects the choice of the patient, gently and confidently accompanies along the way.
Read more
★9.43 based on 31 reviews
- Vyrikov Artur Igorevich
Clinical psychologist. ACT psychotherapist. Cognitive behavioral psychotherapist
in clinic online
Adults (18 to 55 years old)
Trust. Simplicity.
Creates a friendly atmosphere of understanding and ease, communicates in simple language.
 Easily finds common topics for conversation, tries on situations for himself and asks precise questions "in the case." Helps to quickly understand the essence of the problem and proceed to work on a solution. Works with setting values, finding priorities, and choosing an informed life path.
Easily finds common topics for conversation, tries on situations for himself and asks precise questions "in the case." Helps to quickly understand the essence of the problem and proceed to work on a solution. Works with setting values, finding priorities, and choosing an informed life path. Read more
★9.52 based on 82 reviews
- Yarygin Anton Igorevich
Adult psychiatrist.
in the clinic online
Adults (over 18 years old) Elderly (over 60)
Confidence. Efficiency.
First class and highly organized specialist.
Anton is maximally focused on the healing process. Able to quickly evaluate incoming information, make objective and accurate decisions. Works with full dedication, passionate about the work process.
Competently arranges treatment and brings the case to a positive result.