Borderline personality verbal abuse
Building Your Case: How to Document Abuse
Search Close
Leave this site safely
You can quickly leave this website by clicking the “X” in the top right or by pressing the Escape key twice.
To browse this site safely, be sure to regularly clear your browser history.
Got it
Security Alert
Internet usage can be monitored and is impossible to erase completely. If you’re concerned your internet usage might be monitored, call us at 800.799.SAFE (7233). Learn more about digital security and remember to clear your browser history after visiting this website.
Click the red “X” in the upper-right corner or “Escape” button on your keyboard twice at any time to leave TheHotline.org immediately.
OK
If you are in an abusive relationship and are in the process of taking (or deciding to take) legal action against your abusive partner, documenting the abusive behaviors of your partner can be an important component of building your case.
It’s worth noting that each state has different laws about what evidence and documentation can be used in court. Speaking with a legal advocate in your state might better prepare you for your unique situation (our advocates at the Hotline can help locate a legal advocate near you). According to WomensLaw, in most states evidence can include (but is not limited to) the following:
- Verbal testimony from you or your witnesses
- Medical reports of injuries from the abuse
- Pictures (dated) of any injuries
- Police reports of when you or a witness called the police
- Household objects torn or broken by the abuser
- Pictures of your household in disarray after a violent episode
- Pictures of weapons used by the abuser against you
- A personal diary or calendar in which you documented the abuse as it happened
Below are a few actions you can take to create documentation, if you are able to or feel safe doing so:
- Visit the doctor.
-
More and more, doctors and gynecologists are trained to recognize signs of abuse. Your health care provider could also be a safe resource for disclosing the abuse. If you’re visiting a doctor for an injury, ask them about safe ways they can make notes about the abuse — ex. Some can write “cause of an injury” without it having to go to the police.
- Consider outside documentation.
-
Do you have a trusted friend, coworker or family member who knows what’s going on and would be willing to help? There are many ways they can help document the abuse — whether that’s a coworker making note of times your partner calls you at the office, or a friend holding your journal at her house.
- Create a stalking log.
-
If your partner is stalking you, creating a stalking log can be very helpful to your case.
 The National Center for Victims of Crime’s Stalking Resource Center has examples of stalking logs (in PDF and Word formats) as well as additional information on stalking.
The National Center for Victims of Crime’s Stalking Resource Center has examples of stalking logs (in PDF and Word formats) as well as additional information on stalking. - Learn more about police reports.
-
ex. Like filing about a lost bike. Ask, “Hypothetically, if there was something that was happening that I would want to report…”
Always ask questions. Call your local police department’s non-emergency number and find out about the protocols and procedures of filing a police report.
This can help you prepare for filing a police report if you need to, which creates a paper trail of the abuse.
- Take pictures.
-
A digital camera or your phone camera may not always be safe. Consider getting a disposable camera. Another option is for someone else to take the pictures and keep them for you.
- Let it go to voicemail.
-
Is your partner calling over and over? Let it go to voicemail once and save the voicemail.
- Save digital evidence.
-
Do you have a smartphone? Most have the “take a screenshot” option. Thirty missed calls from your abusive partner? Take a screenshot of that. Threatening texts? Instead of responding to them, take a screenshot of them. These screen shots get saved in your images folder, so remember to send them on to a friend and delete them. If your partner sends threatening emails, don’t respond to them, but consider saving them in a folder in your inbox.
If you’re not sure if documenting your abuse would be safe, always go with your gut. It’s very important to keep in mind that you are the expert on your situation, and what works for one person may not be a safe idea for another person.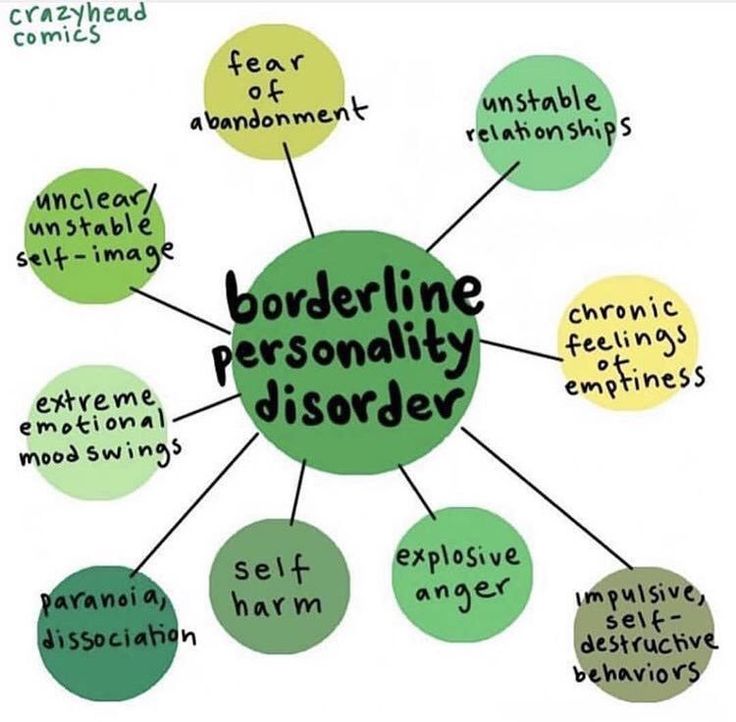
We are not legal advocates at the Hotline, but we are able to offer support and refer you to the local or state resources that might be helpful to you.
Answers shouldn’t be hard to find.
We're here to help!
- Call 1.800.799.SAFE (7233)
- Chat live now
- Text "START" to 88788
Visit our page for Privacy Policy. Msg&DataRatesMayApply. Text STOP to opt out.
Borderline Personality and The Hidden Abuse of Non Borderlines
Posted by A.J. Mahari and Reviewed by Ryan House, PsyD Clinical Psychologist
Borderline Personality Disorder (BPD) is highly associated with verbal abuse, emotional abuse, psychological abuse, physical abuse, and/or domestic violence often suffered by those who are non-borderline.
Recent findings suggest that further research is necessary to better understand the association and differentiation between psychological dysfunction and trauma processing, emotional regulation, distress tolerance, and interpersonal sensitivity of individuals diagnosed with BPD.
The propensity for abusiveness in those with BPD can be instigated by the narcissistic injury that is at the heart of the core wound of abandonment.
Borderline Personality And Abuse
Those diagnosed with Borderline Personality Disorder (BPD) or those with BPD who may not even know they have it, are more likely than the general population to be verbally, emotionally/psychologically, physically abusive.
But what is behind the connection between Borderline Personality and abuse?
The reality of this is such because borderlines lack a known, consistent self, and they struggle with abandonment fears and abandonment depression that stem directly from a primal core wound of abandonment that arrests their emotional and psychological development in the very first few months of life.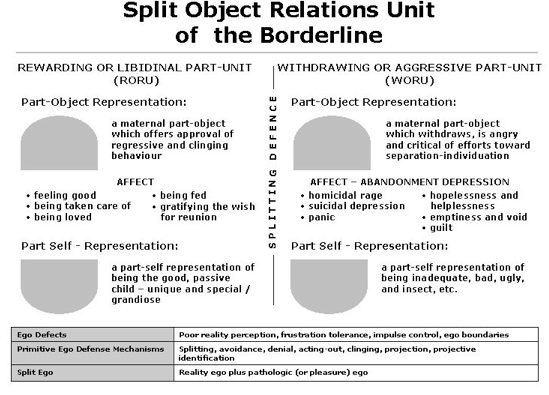
This arrested development impacts most, if not all, areas of relating and leaves borderlines unable to interact in age-appropriate healthy ways.
Ways of relating that unfold in the present and that aren’t layered with deep intra-psychic pain – pain that is unresolved.
Intra-Psychic Pain Is The Root
The roots of abuse in BPD, particularly in intimate significant other relationships with Non-Borderlines have their genesis in the borderline’s re-living of this deep intra-psychic pain.
Pain that is triggered through attempts to be emotionally intimate with someone else. The intimacy that non-personality-disordered people enjoy is stressful and overwhelming to the borderline.
It enlivens the borderline’s worst nightmare – the unresolved pain of the core wound of abandonment.
It arouses all the maladaptive defenses of the borderline because he/she re-experiences the terror and panic of either his/her past experience of feeling annihilated or engulfed and/or his/her fear of being annihilated or engulfed, often alternately when trying to be close to someone one else.
Approach-Avoidance Conflict
This sets up an approach-avoidance conflict, a “get-away-closer” style of trying to relate that has its roots in the “I hate-you-don’t-leave-me” struggle of the borderline who experiences any withdrawal of intense, close, (albeit also threatening) intimacy, attachment or bond as a threat to his or her safety at best, and entire existence (psychologically) at worst.
Add to this that when there is any distancing or break in the intensity and symbiotic-like closeness (if in fact closeness is ultimately achieved) the borderline then fears, and/or feels abandoned.
This conflict of fearing or re-experiencing annihilation versus engulfment and then the re-experiencing of the fear of or actual feelings of abandonment that the borderline experiences, often subconsciously, in trying to be in relationship to other, causes the borderline to be triggered back to his/her original core wound of abandonment feelings in such a way as to trigger the primal feelings of helplessness, loss of control, needs equaling survival, thwarted needs being akin with the death of the lost self.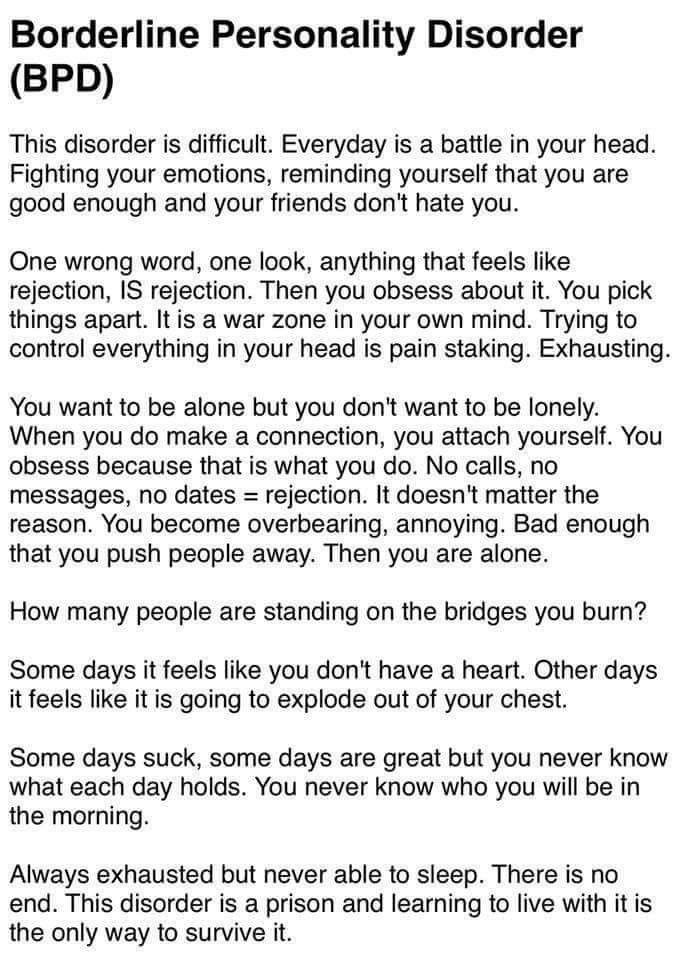
This whirlwind of unregulated emotion meeting with fear and distrust generates the original feelings of rage that this core wound of abandonment aroused in the first place.
A Wound of Abandonment Can Feel Like Psychological Death
The core wound of abandonment, when one is very young and experiences it, is the experience of psychological death. It is intense and arouses the borderline to fight for survival while they experience the sheer terror of feeling like they might actually just die or be killed by what they are feeling.
This heightened state of arousal is both psychological and biological – it is physiological. It is a strong drive to survive and rage is at its core.
Borderline Rage
Rage is the most primal feeling generated and the most protective defense that a young infant can muster to try to have the caregiver return to once again provide some sense of being for the infant.
Feelings and reactions of rage are experienced by those who go on to develop BPD so early in life that they precede cognitive and verbal development.
This is what makes borderline rage so primal, so intense, and in the case of the borderline so raw and unmanageable in terms of often triggered dysregulated emotion of those with BPD.
It is pain that has long-since been dissociated from and abandoned by the borderline. This abandoned pain of BPD is the ignition switch that needs only the hint or flicker of an emotional flame to ignite a combustible, all-too-often abusive rage like no other.
This is what the borderline regresses to.
When the borderline is in a regressed and to varying degrees dissociated experience, the non-borderline partner is experienced by the borderline as that withdrawing or abandoning caretaker from the past that was needed for literal physical and psychological survival.
Issues That Trigger Rage
When the non-borderline partner, living, On The Other Side of BPD isn’t focusing 100% of his or her attention on the borderline (especially if you have actually attained closeness) and there is any experienced or even perceived break in the symbiotic connection that enables the borderline to feel somewhat secure (like the not having to attend to a child, or go to the washroom or any simple thing) – even when stressed by the closeness – and already beginning to cycle to the fear of the loss of it – the borderline will often react from this cesspool of ever-churning rage which is the protection for the very vulnerable and young abandoned pain of the borderline. This ends in a lashing out by the borderline personality, abuse is often the end result.
This ends in a lashing out by the borderline personality, abuse is often the end result.
Different Expressions of Borderline Rage
All rage is not expressed the same way. All borderlines do not abuse in the same ways.
As you will see in my next article, there are many different forms that the abuse generated by this narcissistic woundedness takes. Some borderlines rage, literally, they scream and yell and throw things or hit people.
While other borderlines (known as quiet or “acting in” borderlines) may rage in such passive-aggressive ways that the non-borderline might not realize that the borderline is raging.
Rage is Always Smoldering
This inherent free-floating, always-at-the-ready rage, if you will, is the root source of a lot of the varying types and styles of abuse that non-borderlines are bombarded with.
It can often be sudden and seem to come out of nowhere because the source of it is deep inside the psyche of the borderline.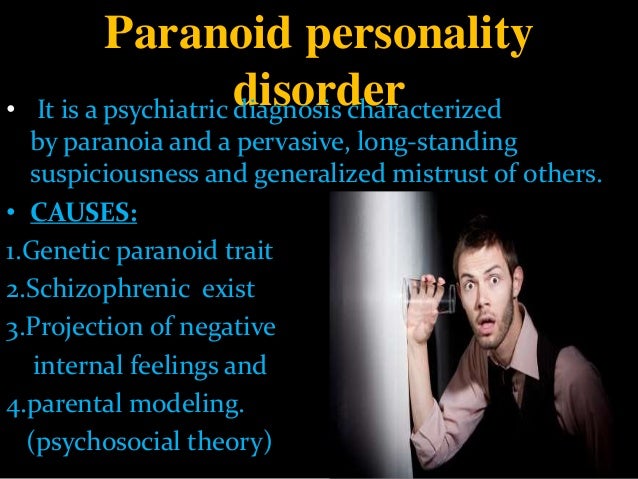
Emotional And Psychological Arrest
Borderlines lack a known self. They have not been able to emotionally or psychologically mature beyond a very early stage of emotional developmental arrest.
An emotional/psychological arrest that takes place when the developing authentic self essentially experiences a death, is lost to the borderline and is then supplanted by the false self.
Why Life Can Seem Constantly Painful
Life, for those with BPD, is, to say the least, one devastatingly painful experience of trying to live and exist in the absence of a known self in the fragmented pieces of the blurred experience of the here and now enmeshed with the past.
It is one perpetual separation-individuation crisis void of the big picture until and unless it can be resolved.
Current Feelings Trigger Past Wounds
Borderlines do not learn how to cope with the feelings that they have in the here and now, that trigger past intense unresolved feelings of the actual loss of the psychological self.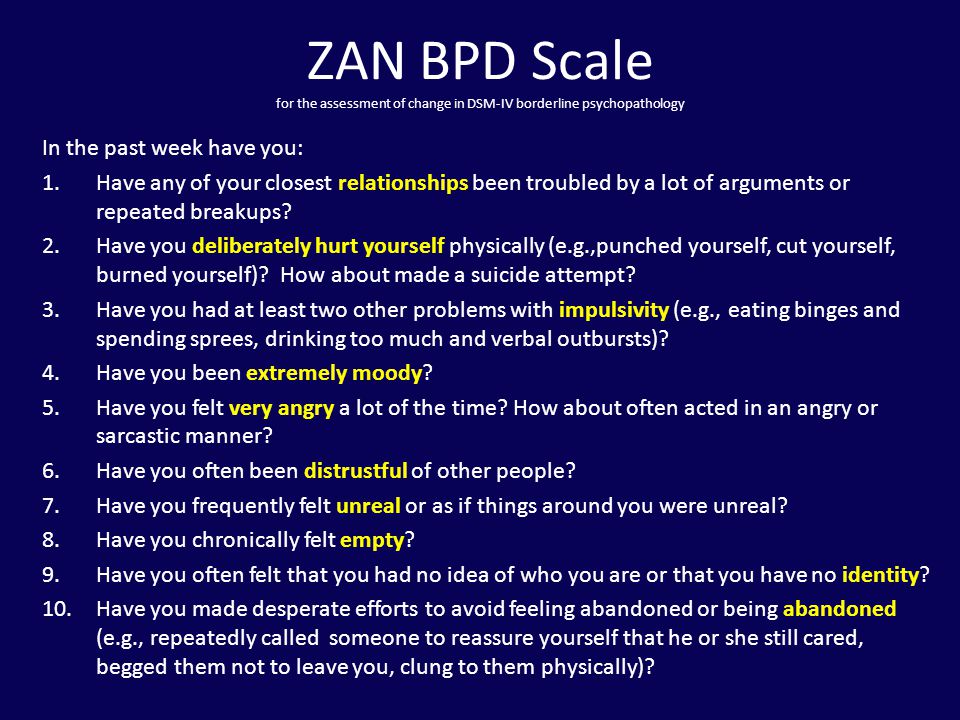
Lack of Object Constancy
Borderlines lack the ability to hold in any consistent or congruent way object constancy.
They experience relatedness as being as fragile as out of sight out of mind.
A bond that a non-borderline feels exists between him/herself and the borderline whether he/she is in the presence of the borderline or not is not something that the borderline can psychologically remember, trust, or believe.
Object constancy or any connectedness or attachment that could be defined as “secure” is fleeting for the borderline who has not been able to develop object constancy.
The fleeting nature of this inability on the part of those with BPD to hold object constancy in any consistent or congruent way leaves those with BPD in a very painful place – literally between a rock and a hard place in what is the classic relational no-win of an untreated person with BPD.
Loss of Authentic Self
This loss of the authentic psychological self is re-experienced over and over again and the fear of it and the fear of the pain of it grows each and every time one is triggered back to it.
The Cycle Continues
This builds both anger and a continually proliferating inability to cope with it in any constructive way.
Anything short of intense symbiotic connection that is uninterrupted will once again send the borderline cycling back around the re-experiencing of everything associated with the core wound of abandonment.
As the borderline cycles back to this enraging and vulnerable – which isn’t tolerable – place of abandonment depression (Masterson) and abandonment trauma so too begins the apex of the likelihood of abuse.
Along with abuse of all sorts, the result of this cycle is often a punishing talionic impulse acted on in the heat of the triggered-dissociated moment by the borderline in what are known as repetition compulsions.
Borderline Personality And Abuse AwarenessMost borderlines, until and unless they have substantial and successful therapy are not consciously aware of what I am describing here.
- Some are totally oblivious to their behavior.
- Some see their behavior as a means to an end and take little to no responsibility for it or any of its consequences.
- Others understand that they have acted poorly again, pissed someone off, have once again made real the threat of and/or fear abandonment and loss, but they do not understand why they’ve done it.
- Similarly, they have no clue how to stop it.
- Others project it out onto the non-borderline and think that everything that has come from them was actually done to them by the non-borderline.
This can be a crazy-making experience for the non-borderline. This is of little consolation to the non-borderline, however. It does not, at all, justify the abuse.
Will a Person With BPD Ever Change?
However, clearly I write about this here to say that if a borderline is not getting treatment, and I mean for real, not just going through the motions type of treatment, there is no logical reason to even begin to believe that the abuse that any borderline in your life is perpetrating upon you will stop.
The very thing that you most want from your borderline (or wanted if you’ve left the relationship) in terms of what it means to have a relationship and to relate was not ever even on the table because the borderline is not an emotionally/psychologically mature being.
BPD’s Immature Relational Ability
The borderline is still a very wounded and very young child, emotionally, in terms of the ability or understanding of how to actually relate to others.
This is the case because what borderlines do is not relate to others for who they are but as an extension of the borderline – and more to the point – as an extension of the parent (usually mother) that most failed them or by whom the borderline most feels abandoned, for whatever reason(s).
No Concept of The Real Self
The borderline has no idea who he/she really is. He/she often feels as if he/she does not exist.
This is especially true if the borderline does not have an other to project all of his/her feelings out onto and an other from whom they then require the mirroring back of an identity of what is a painful lack of known self.
In her book, The Narcissistic/Borderline Couple, Joan Lachkar, Ph.D., writes,
“For the borderline, the focus is primarily on bonding and attachment issues. Borderlines often form addictive love relationships (including normal dependency), they form parasitic relationships, and project their needs in hostile, threatening ways. Because their defenses and demands are excessive, borderlines tend to remain in the dance, rarely achieving their aims.”
The dance that Lachkar refers to, in my past, for me, as I look back now many years into recovery when I was borderline, was one of seeking to re-invent, re-experience, re-do, the ruptured relationship with my mother.
This wound caused me to lose my authentic self to the defensive and manipulative abusive narcissistic defenses of the borderline false self in such a way that would once and for all satiate the developmental needs arrested at the time of my core wound of abandonment and teach me how to actually bond without feeling like it would kill me.
The dance, for me, was one of seeking to recreate and recapture that symbiotic relationship that I never had the chance to have with my mother, through others, in an end-justifies-the-means kind of way, that was, at times, very abusive to others in my life, in the past, on my part.
That dance was a complicated punishing and unforgiving dance of codependency through which I sought to resolve what for years seemed like the unresolvable woundedness that was the source of my rage and the abuse that I perpetrated against others in the name of trying to actually be psychologically born which is necessary in order to get on and stay on the road to recovery.
RELATED ARTICLE: Borderline Personality and Abuse
Narcissistic Defense Mechanisms
Most, if not all borderlines, have, as a result of this core wound of abandonment, a well-developed defense mechanism of narcissism and also have varying degrees of narcissistic injury that manifests in the and through the false self.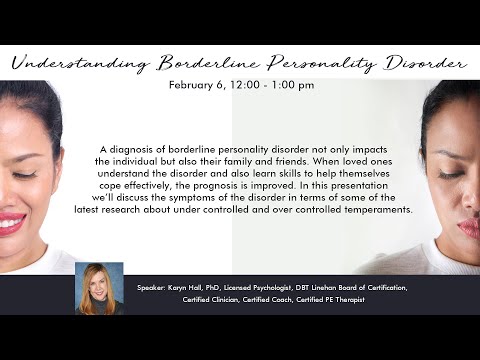
This narcissistic injury or wound and its subsequent usage as a defense mechanism along with the narcissism seen in the false self of those with BPD are not to be lumped together with Narcissistic Personality Disorder – they are not one and the same at all.
Incapable of Adult Intimacy
Borderlines who live from a false self and who do not have an active and keen awareness of their own core wound of abandonment and their abandoned pain are not capable of age-appropriate adult intimacy or relating.
It is from the core of this emotional dysfunction that borderlines end up abusing either themselves, others, or both. Non-borderlines, are often on the receiving end of many types of abuse.
The Pain Of Borderline Relating
The very nature of borderline relating makes for a dysfunctional and toxic relational style that non-borderlines will benefit greatly from learning more about so that they can deepen their understanding of BPD and also take care of themselves.
Many non-borderlines come to realize that they want and/or need to break free from the puzzling and painful maze that is borderline relating. Relating that is more often than not abusive.
What Non-Borderline’s Need To Do
If you are a non-borderline and you are being abused by someone with BPD, you need to take care of yourself. It won’t do you or the borderline any good to deny or excuse his or her abuse and think that having a personality disorder justifies it in any way – it does not.
You cannot control what a person with BPD does, but, you can make choices about what you will and what you will not live with. Once you make that choice you need to identify and make known boundaries that are firmly explained and firmly enforced consistently.
Many non-borderlines do not realize that the sane choice for them if the borderline in their lives is not getting help and/or cannot take personal responsibility and stop and change any and all abusive behavior and/or relating, is to leave, break free and take care of themselves.
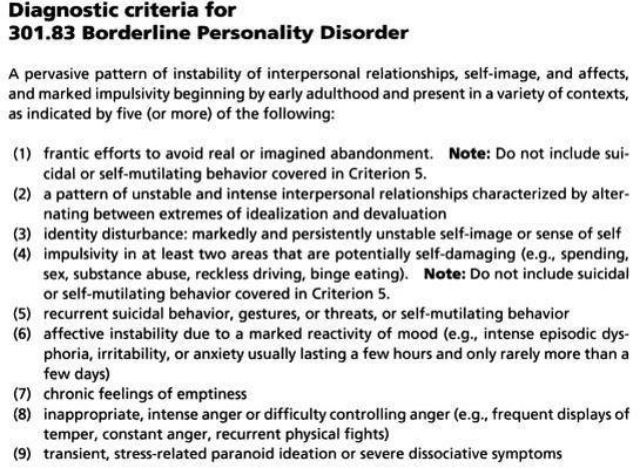
Borderline personality disorder: what it is, symptoms and signs of BPD
Borderline personality disorder is characterized by emotional instability, impulsive behavior and low self-control. Forbes Life figured out what causes this disease, how to diagnose borderline personality disorder and how to help people who have experienced it
Mental personality disorders differ from other types of disorders in their intensity. They cannot be treated like an ordinary illness, as a temporary mental disorder, because personality disorders affect a set of personal characteristics formed in childhood. There are a number of problems with diagnosing such diseases: their symptoms are quite individual, although there are a number of common signs. For borderline personality disorder (BPD), these may include difficulties with self-image, extreme mood swings, risky behavior, and self-harm. The good news is that personality disorders can still be managed—there is a cure.
The good news is that personality disorders can still be managed—there is a cure.
Now officially: BPD is a diagnosis
Borderline personality disorder is one of the ten types of personality disorders in modern psychotherapy, which is expressed in problems of awareness and formation of personal identity. Psychologist, Gestalt therapist Valentin Oskin notes that this mental illness is associated with strong, uncontrollable and often painful emotions that lead to a distorted sense of self and unstable interpersonal relationships.
People with BPD are reverse solipsists: they are convinced of the inviolability of the world around them, but doubt the reality of their own existence - their image of the inner “I” is so mobile and unstable. In addition to depersonalization, "borderguards" are characterized by impulsiveness, dependence on other people, unstable behavior, a tendency to a chaotic life, and even a need to harm themselves and injure themselves.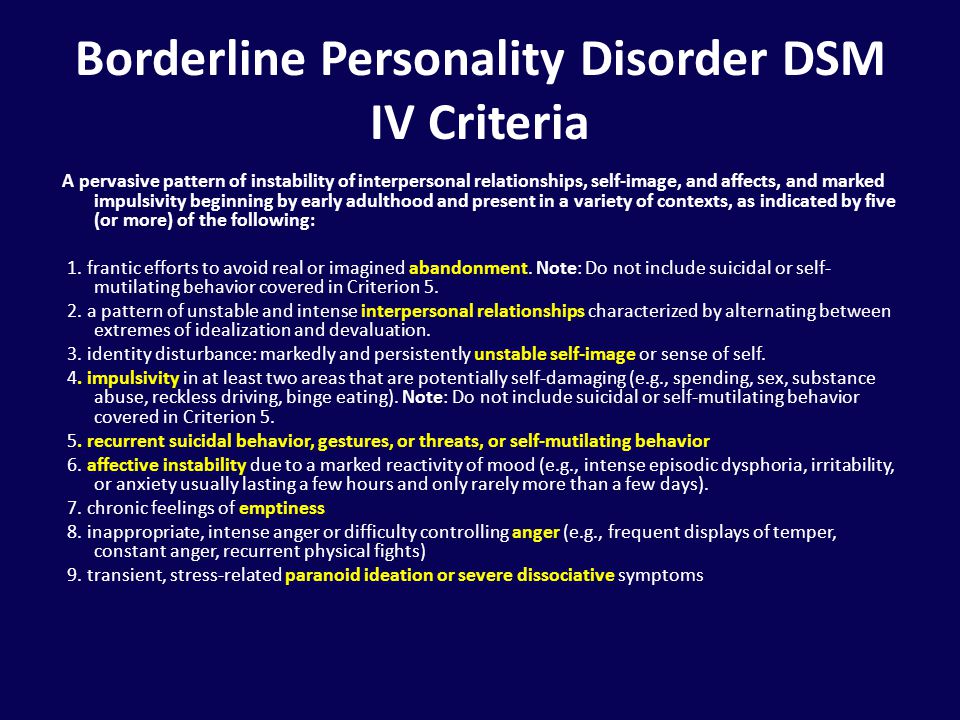 "Border guards" are characterized by chronic suicidality: 75% of people with BPD try to commit suicide, of which about 10% die as a result of suicide. Moreover, a third of all completed suicides were committed by those suffering from borderline personality disorder.
"Border guards" are characterized by chronic suicidality: 75% of people with BPD try to commit suicide, of which about 10% die as a result of suicide. Moreover, a third of all completed suicides were committed by those suffering from borderline personality disorder.
Despite the statistics, until 2022 the diagnosis of BPD in Russia could not be officially diagnosed - borderline personality disorder in psychiatry was defined as a disease only in foreign classifications of diseases. It was often called impulsive personality disorder or generally diagnosed as sluggish schizophrenia: the diseases are similar in symptoms, among the signs of BPD there are no hallucinations and delusions. BPD also resembles bipolar affective disorder (up to 40% of "border guards" get an erroneous diagnosis of bipolar disorder), only periods of depressive and elated mood are replaced with bipolar disorder less often. The transition to the International Classification of Diseases of the 11th revision will finally allow doctors to make an accurate diagnosis for Russian citizens and prescribe the appropriate treatment.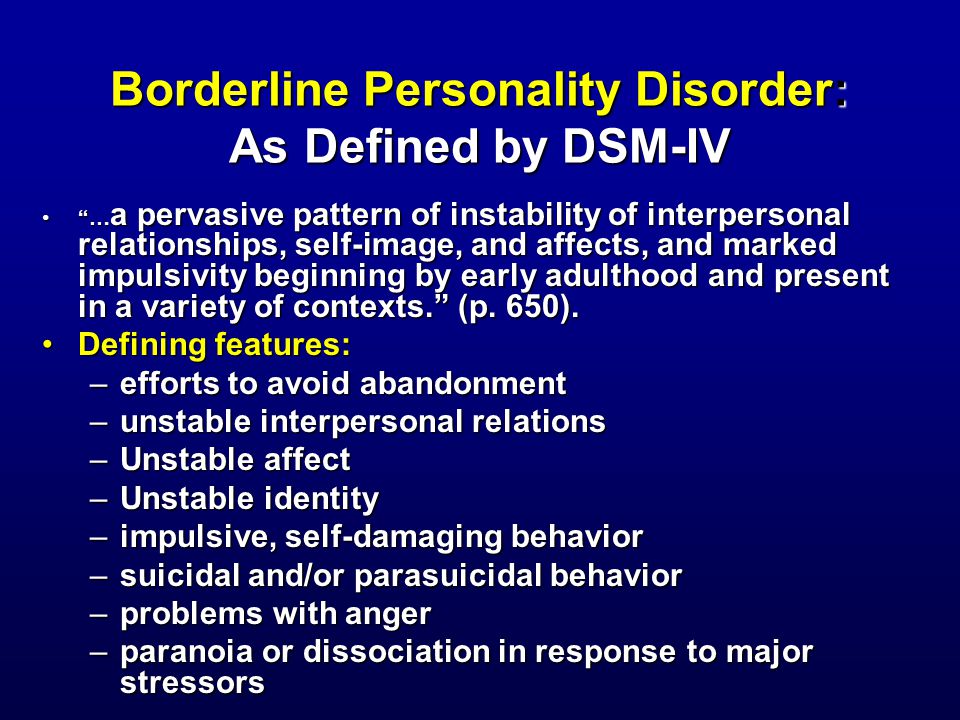
Diagnosis is not a sentence, the boundary between the norm and pathology is very flexible: “Each of us has borderline responses. For some, they are deeply hidden and appear only in crises, traumas, stressful situations. And for some, life as such is stressful, and therefore the ways of responding turn into what psychologists could call the borderline organization of the personality,” notes Irina Mlodik, Candidate of Psychological Sciences, in the book “House of Cards. Psychotherapeutic assistance to clients with borderline disorders.
Related material
Ghost hints
Most people with BPD are unaware of their diagnosis and do not seek medical attention. And it's not just that BPD in psychology does not have a clear definition. The disease does not allow you to objectively assess your mental state and understand that the indomitable monster inside is raging not because of the permanent retrograde Mercury and the fatal force of circumstances. The absence of obvious mental abnormalities like hallucinations makes it possible to attribute emotional behavior to character traits. Colleagues, friends and relatives often believe that behind the disgusting behavior of such a person is hysteria and selfishness. Therefore, systematic treatment of borderline personality disorder begins in most cases after a suicide attempt.
The absence of obvious mental abnormalities like hallucinations makes it possible to attribute emotional behavior to character traits. Colleagues, friends and relatives often believe that behind the disgusting behavior of such a person is hysteria and selfishness. Therefore, systematic treatment of borderline personality disorder begins in most cases after a suicide attempt.
The most striking and obvious sign of borderline personality disorder is a craving for auto-aggression, or self-harm. This is not only the infliction of bodily harm (cuts, blows or burns), but also the intention to deprive oneself of sleep, nutrition. This practice is not necessarily a consequence of suicidal behavior: physical pain serves as a way to drown out inner pain, to switch attention from uncontrollable emotions to those that have become the result of an effort of will. The problem is that self-harm is either carefully hidden by people with BPD because it is not normal in our culture, or they perceive it as controlled behavior (eg, exhausting workouts in the gym, striving to do work tasks in their free time).
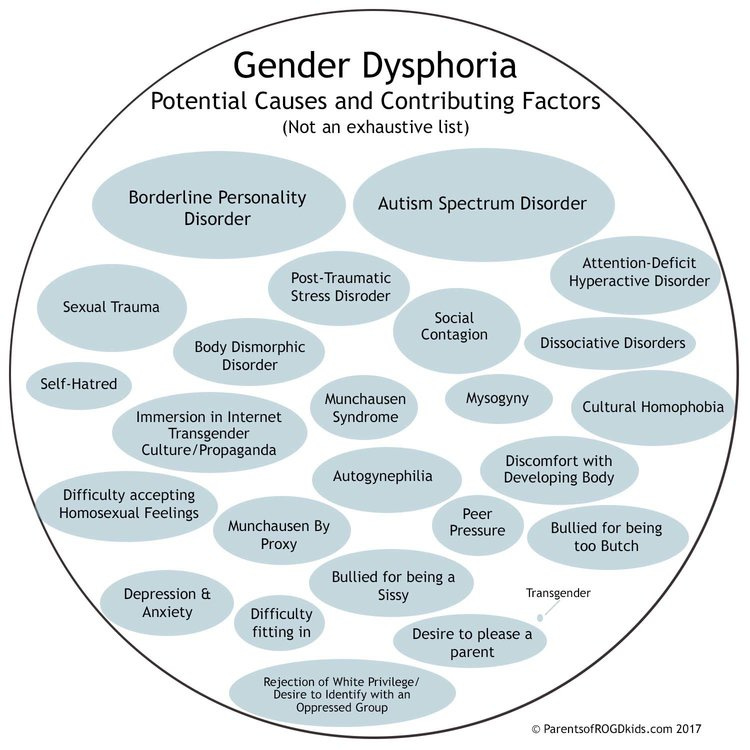
Borderline personality disorder can be accompanied by alcohol, drug, gambling addiction and a number of other diseases. “For example, depression, anxiety disorders, eating disorders are common in people with BPD. Often, a history of PTSD or CPTSD is found, ”notes Valentin Oskin. That is, constant panic attacks or overeating in the evenings can be a sign of more serious mental disorders than just a reaction to stress.
Mind, a British mental health information resource, highlights the following symptoms that may indicate borderline personality disorder. If they last long enough and have a negative impact on your life, it makes sense to consult a psychotherapist or psychiatrist:
- Fear of being alone. You constantly worry about people leaving you and are ready to do everything to prevent this from happening.
- Impulsivity and affectivity. You are overcome by strong emotions that last from several hours to several days and can change quickly (for example, from feelings of happiness and confidence to sudden depression and sadness). This is especially evident in a state of anger, which is difficult to control. In a state of severe stress, you may also experience paranoia or dissociation (as if everything is not happening to you, but to someone else).
- Depersonalization. There is no clear idea of who you really are: the sense of self and behavior changes radically depending on where and with whom you are. As an option - a constant feeling of emptiness inside, boredom, misunderstanding of one's true desires and values.
- Communication problems. It is very difficult for you to create and maintain stable relationships, you are prone to masochistic communication, cyclically idealize and devalue even the closest people, and do not always correctly interpret the motives of the actions of others.

“Borderline personality disorder can manifest itself in a wide range of signs,” says Valentin Oskin, “the symptoms of borderline personality disorder are most fully described in the DSM-5 and ICD-11 reference books. If grouped together, the symptoms will reflect a lack of control in the emotional, behavioral, cognitive spheres, as well as a distortion of the sense of self and a violation of interpersonal relationships. According to the psychologist, it is extremely difficult for people with BPD to break off relationships, even those that need to be broken off. Instead, they may go to great lengths to keep the people who matter to them around them.
At the same time, “border guards” tend to involuntarily throw out their emotions on those who are dear to them: “Often this ends with an interruption in communication, because not everyone is able to endure such a bolt from the blue. And even more so if this thunder rumbles once every couple of months, ”Ksenia Ivanenko notes in her Telegram channel, where she describes her personal experience in dealing with BPD.
And even more so if this thunder rumbles once every couple of months, ”Ksenia Ivanenko notes in her Telegram channel, where she describes her personal experience in dealing with BPD.
Related material
To determine if you are at risk, you can take several tests for borderline personality disorder that are publicly available. It is important to understand that the result obtained is not a final diagnosis, it can only be made by a qualified doctor after analyzing the symptoms.
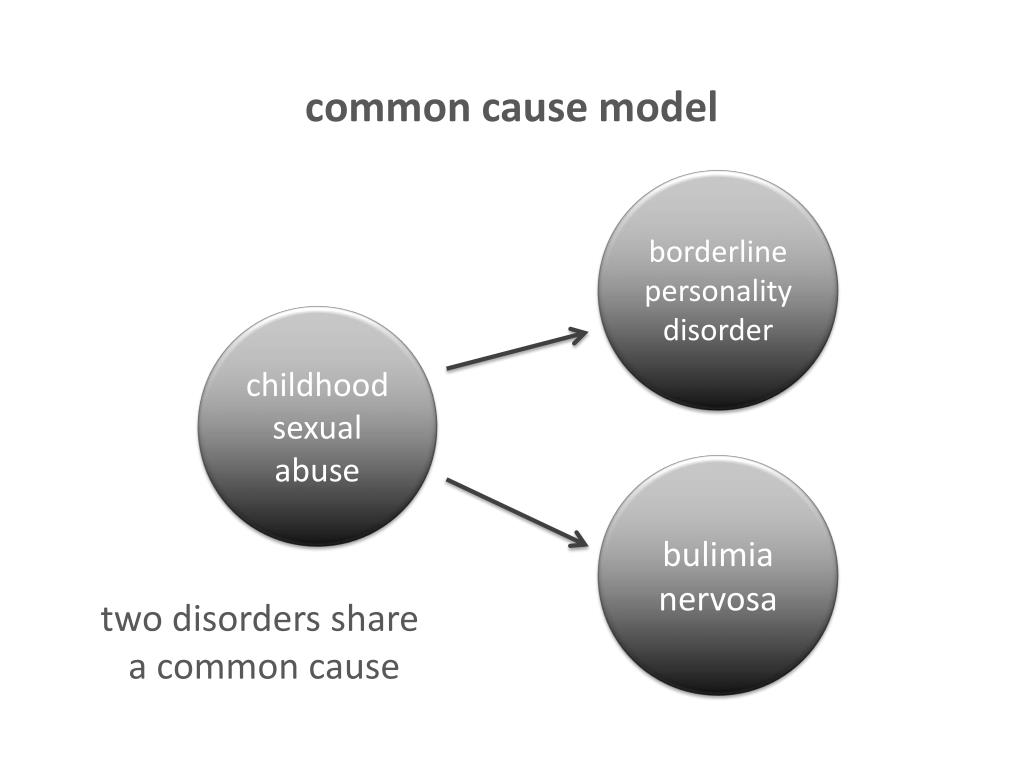
The Root of the Problem: What Causes Borderline Personality Disorder
Effective treatment for most mental illnesses requires identifying the cause. Borderline personality disorder is problematic in that it arises from a number of factors and affects the basic components of the personality. That is, there is simply no specific reason that triggers the PRL processes. “While BPD is one of the most researched personality disorders, there is no consensus on what exactly causes it. Severe stresses experienced by children and adolescents, such as neglect, prolonged painful separation, loss of a parent, violence, are common in people with BPD. There is also evidence of a genetic predisposition: among first-line relatives of a person with borderline disorder, the likelihood of developing a similar disorder is 3-5 times higher when compared with the general population,” notes Valentin Oskin.
That is, there is simply no specific reason that triggers the PRL processes. “While BPD is one of the most researched personality disorders, there is no consensus on what exactly causes it. Severe stresses experienced by children and adolescents, such as neglect, prolonged painful separation, loss of a parent, violence, are common in people with BPD. There is also evidence of a genetic predisposition: among first-line relatives of a person with borderline disorder, the likelihood of developing a similar disorder is 3-5 times higher when compared with the general population,” notes Valentin Oskin.
Any person can be at risk, especially if he is going through a difficult stressful situation. It is known that this diagnosis is made more often in women than in men, and that in almost all cases of BPD it is driven by a deep emotional shock. Most researchers agree that the development of BPD is promoted by a combination of two groups of factors:
- Stress and traumatic life situations.
 For example, sexual, physical or emotional abuse, persistent feelings of fear or abandonment in childhood, family problems, repressed feelings of anger, anxiety, and sadness. Stress or trauma in adulthood can trigger the onset of borderline personality disorder.
For example, sexual, physical or emotional abuse, persistent feelings of fear or abandonment in childhood, family problems, repressed feelings of anger, anxiety, and sadness. Stress or trauma in adulthood can trigger the onset of borderline personality disorder. - Genetic predisposition and environmental influences. The disease can be inherited, but more often borderline occurs as a pattern of behavior unconsciously borrowed from parents or close people, reactions to external stimuli.
Related material
No reason to break ties
If there is a “border guard” in your environment, you can build constructive communication with him, although this will require a lot of effort. “It is important to understand that a person with borderline personality disorder takes criticism extremely hard, for him it sounds like rejection, which he is terribly afraid of. At the same time, emotional jumps do not allow him to get the desired intimacy. Relations with such a person are usually like a swing between the poles "I love you, don't leave me - I hate you, I'll leave you." It is important to understand that with borderline personality disorder it is impossible to consciously change your behavior, thinking, emotional reactions and response patterns to certain situations, ”says Valentin Oskin.
At the same time, emotional jumps do not allow him to get the desired intimacy. Relations with such a person are usually like a swing between the poles "I love you, don't leave me - I hate you, I'll leave you." It is important to understand that with borderline personality disorder it is impossible to consciously change your behavior, thinking, emotional reactions and response patterns to certain situations, ”says Valentin Oskin.
Many "border guards" live with a constant oppressive feeling of guilt, they feel broken, bad and unworthy of normal communication, which they badly need. They are unable to correctly read the reactions of others and the motives of their actions. This determines their strange behavior and repels potential partners and friends. Often, people with borderline personality disorder have a Favorite Person - a person on whom the "borderguard" is extremely dependent and who replaces not only everyone around him, but also himself.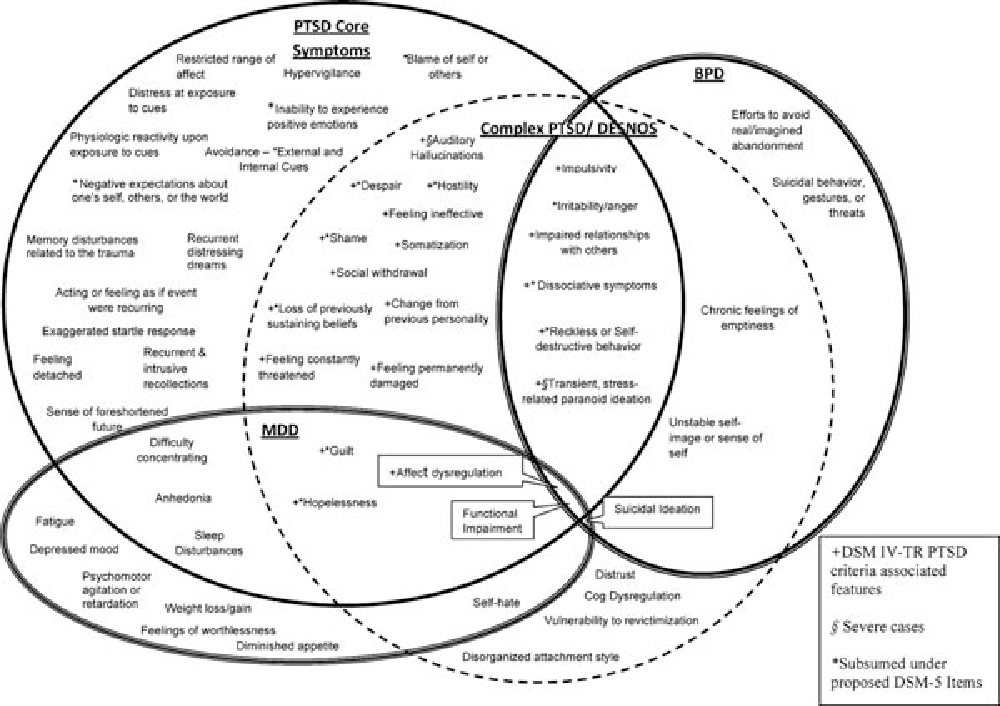 If this person is busy or there is a conflict with him, the “border guard” literally collapses the world: he drowns in a storm of emotions, reflects on death and looks for thousands of reasons why he was rejected.
If this person is busy or there is a conflict with him, the “border guard” literally collapses the world: he drowns in a storm of emotions, reflects on death and looks for thousands of reasons why he was rejected.
There are a number of rules that psychologists have developed for those who seek to communicate as "border guards", minimizing chaos, conflicts and the possibility of a tragic denouement: could end in disaster.
 Take care of yourself: specify the time you spend separately, and try to logically explain why you are doing this or that and do not intend to devalue or leave the “border guard”.
Take care of yourself: specify the time you spend separately, and try to logically explain why you are doing this or that and do not intend to devalue or leave the “border guard”. Related material
How to get rid of BPD
The main way to deal with borderline personality disorder is psychotherapy, in which work is done on the accompanying manifestations of an unstable mental state (depression, addictions, eating disorders, etc.) and syndromes (it is often necessary to treat alcohol withdrawal symptoms). syndrome). This is a long and complicated process, but statistics show that 70% of the “border guards” get rid of the main symptoms during therapy within six years, and remission occurs in a third of patients after two years.
“In therapy, people with BPD are primarily trained in emotional control, responsibility, and interpersonal skills.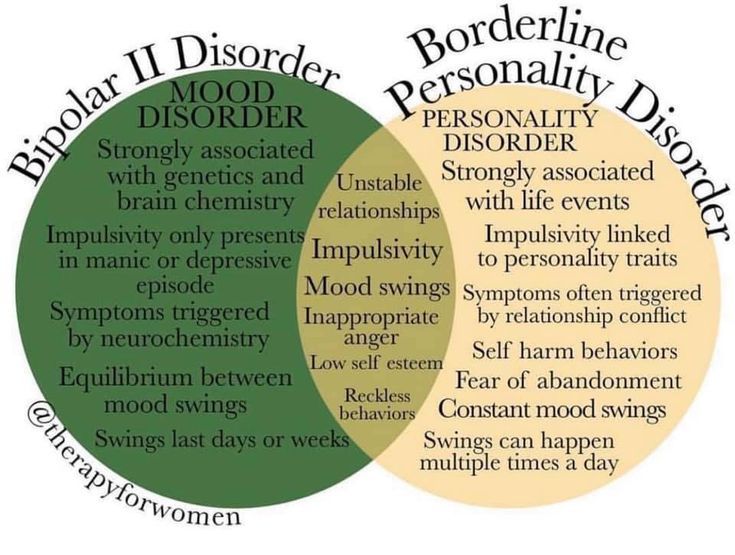 Dialectico-behavioral psychotherapy, a specially developed method for the treatment of BPD based on cognitive behavioral therapy, is well suited for this. No less effective is schema therapy, which also has special developments for the treatment of BPD. In the course of treatment, pharmacotherapy can also be prescribed, for example, for the treatment of associated depression or anxiety disorder, ”says Valentin Oskin.
Dialectico-behavioral psychotherapy, a specially developed method for the treatment of BPD based on cognitive behavioral therapy, is well suited for this. No less effective is schema therapy, which also has special developments for the treatment of BPD. In the course of treatment, pharmacotherapy can also be prescribed, for example, for the treatment of associated depression or anxiety disorder, ”says Valentin Oskin.
Comprehensive treatment may include the following therapies:
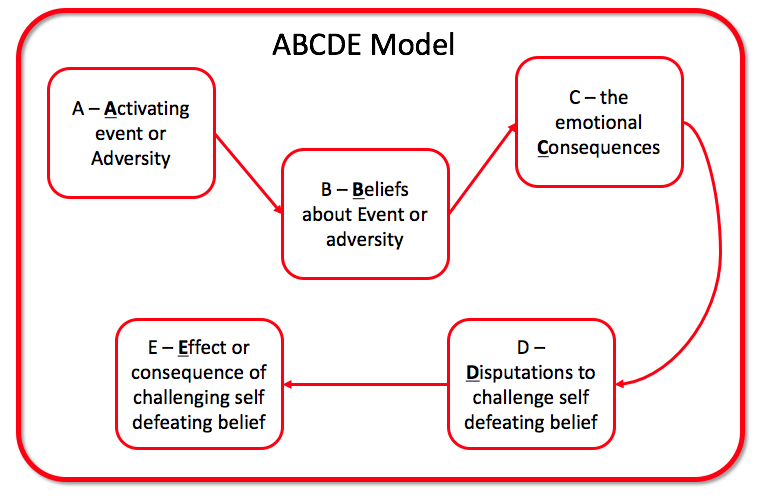
- Dialectical Behavioral Therapy (DBT). Allows the "border guard" to realize that problems can be viewed from different angles, eliminates black and white thinking.
- Mentalization (MBT). It helps to explain to oneself the behavior of other people, logically argue their motives and work to improve interpersonal interaction.
- Transference Psychotherapy (TFP) teaches to perceive positive and negative qualities simultaneously, to get out of the "deification/devaluation" paradigm.
- Cognitive Behavioral Therapy helps to change the way of thinking, reactions to stress and correct affective patterns of behavior.
- Schematic therapy is a complex treatment based on psychoanalysis and gestalt therapy. It changes the behavioral patterns laid down in childhood or adolescence.
- Self help. It consists in tracking the dynamics of emotions, asking yourself questions like “how do I feel now?”, “What does he (a) specifically want from me?”, “Is this reality or my fiction?”.
To improve their inner state, people with BPD are advised to start meditating, exercising, walking more often in the fresh air, trying to rationalize their own mood swings, learning self-soothing techniques and training willpower in order to stop emotional breakdowns in time.
Related material
Borderline personality disorder: what is its cause?
Know Yourself
- Photo
- Getty Images
If a film were made about Anna, a single mother of three daughters, the average viewer would most likely consider what they saw was too much and a collection of movie clichés.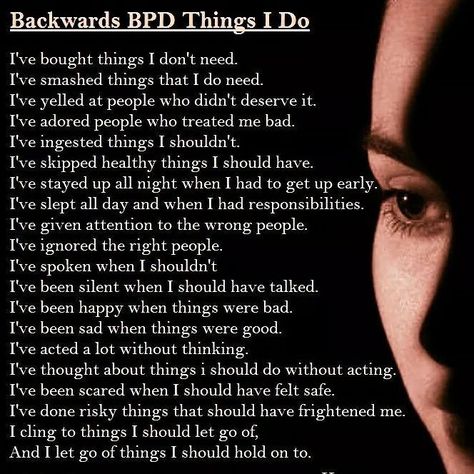
Anna is in her forties, born and raised in East Germany, an hour from Berlin, and spent her childhood surrounded by alcoholics. The father and mother abused the girl, both emotionally and physically. As a teenager, she was raped several times, and she also lost a close friend - she became pregnant and was killed by her own father.
Now Anna recalls that the behavior of her parents hurt her most of all of the above - it seemed that they simply did not care about her. For example, when Anna told her mother about the rape, she replied that the girl herself was to blame, and her father, in front of whom her daughter had once been hit by a car, only hurried her on: “It's okay, get up, you'll be late for work.”
It is not surprising that Anna, according to her own recollections, grew up embittered and aggressive, did not know how to control emotions, and in her teenage years she tried to commit suicide twice.
As an adult, she continued to behave “on the edge”: she drove too fast and engaged in self-harm, she cut herself do something with yourself.
"
Anna is currently being treated for both post-traumatic stress disorder (PTSD) and borderline personality disorder (BPD), a condition characterized by intense, unstable emotions that affect a person's self-image and relationships, and is often accompanied by self-harm and suicidal behavior.
PTSD and BPD are similar in many ways: patients with these diagnoses have the same difficulty in controlling their emotions, and they also have a disturbed sense of their own "I". The key difference is that trauma has always been considered the cause of the development of PTSD, while the roots of borderline personality disorder were not clear to psychologists and psychiatrists for a long time.
Research, however, shows that between 30 and 80% of people with BPD have also experienced a major trauma that may have caused their disorder.
Perhaps the problem for a long time lay in the fact that specialists understood the concept of "trauma" too narrowly
What does it change? At a minimum, the treatment of patients with borderline personality disorder - even doctors have long considered them "difficult", prone to manipulation and resistant to treatment.
But the fact that it may not be about a personality disorder, but about a condition caused by a serious injury, can fundamentally change everything. However, first things first.
BLURED BORDERS
When Bohus, now a successful psychiatrist in his early 60s, was practicing in a psychiatric clinic in Germany, he saw a woman sitting on the floor, drawing blood from self-inflicted wounds on the wall. After telling the senior psychiatrist about the patient, Bohus heard in response: “Oh, she’s just a“ border guard ”, do not pay attention. You can't help her anyway. And no, people like her never commit suicide. It's just an attempt to get attention."
Bohus did as his senior comrade told him to. Soon the woman took her own life.
The psychiatrist blames the conservative and paternalistic attitude towards patients that existed in those days for what happened. Especially to the "border guards".
The term itself, by the way, was coined back in the 1930s by the German-born American psychiatrist Adolf Stern: this is how he described a condition on the border between neurosis (a mental illness like depression or anxiety that is not accompanied by hallucinations or delusions) and psychosis, in which patients lose touch with reality.
Working with border guards using the usual psychotherapeutic methods, according to Stern, was extremely difficult.
Borderline personality disorder, however, was only officially diagnosed in the 1970s. Psychiatrist John Gunderson, after studying patients who were falsely diagnosed with schizophrenia, identified six distinctive features of the "new" disorder: psychosis,
chaotic relationships with others,
illogical thinking,
ability to maintain the appearance of "normality".
Shortly thereafter, in 1980, the disorder was included in the Diagnostic and Statistical Manual of Mental Disease, the main document that guided psychologists and psychiatrists of the time, and this allowed them to finally start looking for suitable treatments (in addition, Gunderson with colleagues just proved that the healing of people with such a diagnosis is possible).
Women are most commonly diagnosed with this disorder
Although there is good reason to believe that both sexes are equally affected, it is simply that women are more likely to seek help.

The controversy around this pathology still does not subside: some experts consider it unique and associated with the patient's trauma, others - only one of the variations of a personality disorder, still others adhere to an intermediate explanation. For example, clinical psychologist Julian Ford believes that “there is ample evidence that trauma plays a role in the formation of almost any personality disorder, but exactly what role remains to be seen.”
PEOPLE WITHOUT "EMOTIONAL SKIN"
Bohus recalls that in his youth, patients with BPD were treated in different ways: some doctors preferred to isolate them from the rest and drug them with undisguised suspicion and even hostility; others were supportive, warm, allowed to interact with other patients, and taught how to deal with stress. According to Bohus, such patients showed significant signs of improvement.
Alas, clinical psychologist Marsha Linehan fell into the first category: shortly after graduating from high school, the girl was diagnosed with BPD.
She was sent to a psychiatric clinic, where she inflicted numerous injuries on herself - banging her head against the walls, extinguishing cigarettes with her hands and cutting them. Her doctors tried a lot: strong drugs, electric shock and cold therapy (the girl was fixed on the bed and covered with ice sheets), but all this, according to Linehan, harmed rather than helped.
The experience, which the woman describes as "a living hell," motivated her to dedicate her life to helping others. “Borderline patients can be compared to third-degree burns: they just don't have 'emotional skin'. Even the slightest touch can cause them unbearable pain, leading to a state of despair, rage or shame.
Linehan developed a new system of therapy called Dialectical Behavioral Therapy (DBT). It is based on the desire to simultaneously accept the patient and help him change his destructive behavior. Clinical studies have shown that this approach significantly reduces the key manifestations of borderline personality disorder, such that treated patients are less likely to end up in hospitals and injure themselves.
Although the approach has proved to be extremely effective, it does not work with one important aspect - all with the same injury.
CAPITAL TRAUMA
It wasn't until 1980 that the diagnosis of PTSD was formalized as the first disorder unequivocally caused by external causes. Although the cases of post-traumatic stress disorder themselves have been known since the First World War.
In the early 1990s, Harvard psychiatrist Judith Herman, after reviewing a wealth of literature on trauma survivors, came up with a new diagnosis: complex PTSD. Such a diagnosis, in her opinion, should be made to patients who have experienced stress due to being at the mercy of other people: both in camps and prisons, and in especially destructive families. Such patients have difficulty managing their emotions, are prone to self-harm, their self-image is severely damaged, and relationships with others are highly unstable.
And again a heated discussion ensued: many were confused by the fact that Herman's listed symptoms intersected with signs of BPD
Experts divided into two camps: some argued that PTSD was unfairly pathologised, equating it to personality disorders, while others believed that, although many people with BPD have actually experienced trauma, this does not explain their behavior in general.
The main question that appeared on the agenda: what can be considered an injury? Although some patients, including Anna, mentioned at the beginning of the material, did have a traumatic experience, nothing like this happened to others.
In the fifth and current version of the Diagnostic and Statistical Manual of Mental Illness, trauma refers to cases in which a person directly experienced or witnessed a life or health threatening event, or was a victim or eyewitness of sexual violence. This means that those who witness domestic violence, and, for example, police officers who regularly encounter the cruelty of this world, experience trauma.
Although the official definition appeared, it still did not become clearer, and many suggest that everything described above be considered Trauma with a capital letter, and cases of verbal abuse, neglect, bullying and poverty should simply be called trauma. This makes sense: trauma (with a small “t”) is, alas, extremely common: a study in the United States shows that two-thirds of American adults have had some kind of traumatic experience.
At the same time, even “less serious” injuries, especially those inflicted in childhood, leave a tangible mark on the human brain
wording problems. In addition, trauma causes shrinkage of the hippocampus (a structure associated with memory and learning), increased activity in the amygdala (the center of emotional regulation), and disruption of connections between these and other areas of the brain.
Scientists have found that both patients with BPD and those who have experienced trauma (with a large or small "t"), there are common neurobiological changes: structural and functional abnormalities in the limbic system, which just includes the amygdala and hippocampus . One of their constructive suggestions is to help patients "train" the amygdala by learning to control their brain activity in real time.
Some researchers, however, advise not to forget about other causes of the development of the disorder, in addition to trauma, for example, about hereditary factors (their influence is clinically confirmed).
Perhaps a child with a "bad" heredity is more likely to encounter traumatic events, and due to his "genetic inheritance" and cope with them with difficulty.
A kind of vicious circle is formed: a sensitive person reacts impulsively to situations in which he is hurt, and, as a result, remains misunderstood; for his reaction, he is rejected or attempts are made to "change" or control him.
It is also still not fully understood why some children develop borderline personality disorder or PTSD or depression as a result of exposure to traumatic events, while others do not. What makes us resilient or vulnerable?
In search of an answer to this question, a group of researchers led by Martin Teicher studied subjects who experienced something really bad in childhood, but who grew up into mentally healthy adults. It turned out that, in general, their brain is very similar to the brain of patients with diagnoses, with the exception of the amygdala, which is different.
Another interesting point.
Bohus and colleagues studied women who had been sexually abused at a young age. It turned out that those of them, whose traumatic experience was not devalued by others, but provided support, were able to subsequently build healthy relationships with partners, while the rest developed certain disorders.
Anna also believes that the root of her problems lies in her lack of support from her parents: “I don’t love myself because I was told all my childhood that I was unworthy of love.” And this alone, by the way, in itself draws on trauma - and, perhaps, can lead to the formation of borderline personality disorder.
BREAKING THE CIRCLE
But there is definitely light at the end of the tunnel: right now, several groups of researchers are working to develop an approach that will focus on trauma when working with patients with borderline personality disorder. At the moment, the most progressive specialists are already combining the dialectical-behavioral approach with trauma-focused therapy.

One of the main goals of this approach is to help patients connect past traumatic events with what they are experiencing in the present.
“The trick is to get the brain to believe that certain stimuli are no longer a threat,” Bohus explains. “With DBT, we teach patients to recognize, name and regulate their emotions, and therefore control their behavior.” This approach has already proved to be effective. Bohus' team is now modifying the approach to work with patients without a history of trauma with a capital T.
After several months in the clinic, Anna switched to outpatient treatment. She has not fully worked through old traumas, but she copes with her emotions much better. In a sense, she was very lucky: despite everything she had experienced, she was able to find careful and experienced doctors who helped her.
And this is perhaps the main lesson to learn from this whole story: no matter what your past was, how difficult it is for you now, and what diagnosis is on your medical record, never settle for a dismissive attitude towards yourself.