Obsessive compulsive personality treatment
Obsessive Compulsive Personality Disorder (OCPD)
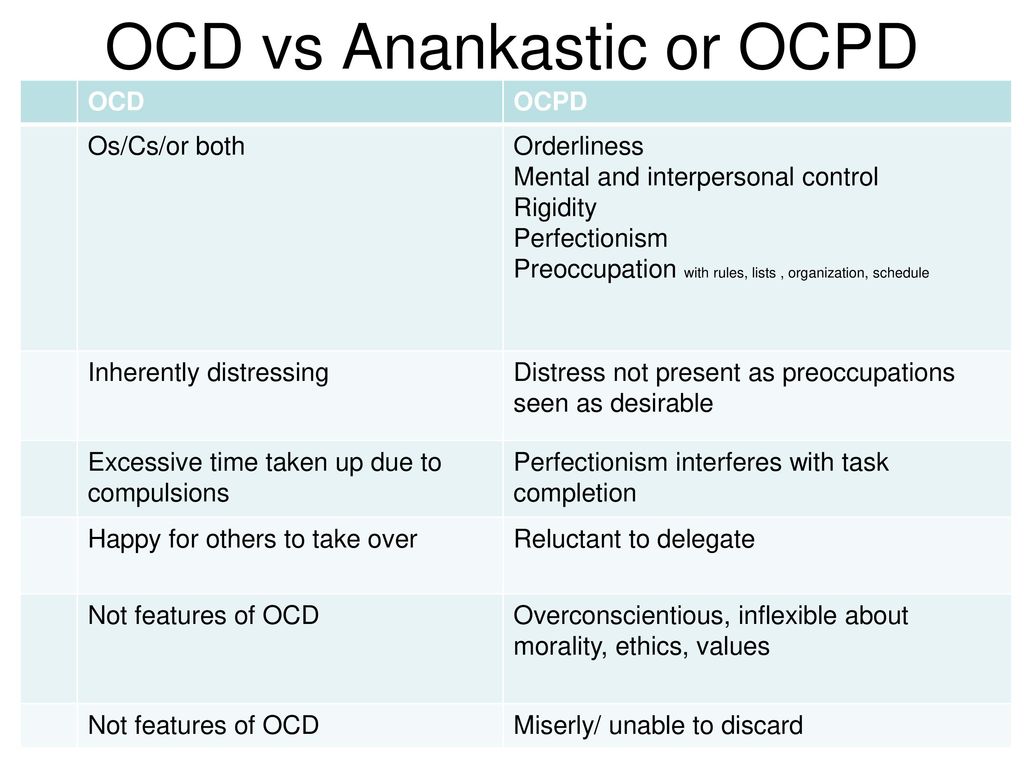
Obsessive-Compulsive Personality Disorder (OCPD) and Obsessive-Compulsive Disorder (OCD) sound the same, and are often confused and mistakenly interchanged as being the same illness, but not withstanding similar names, they are in fact two separate conditions.
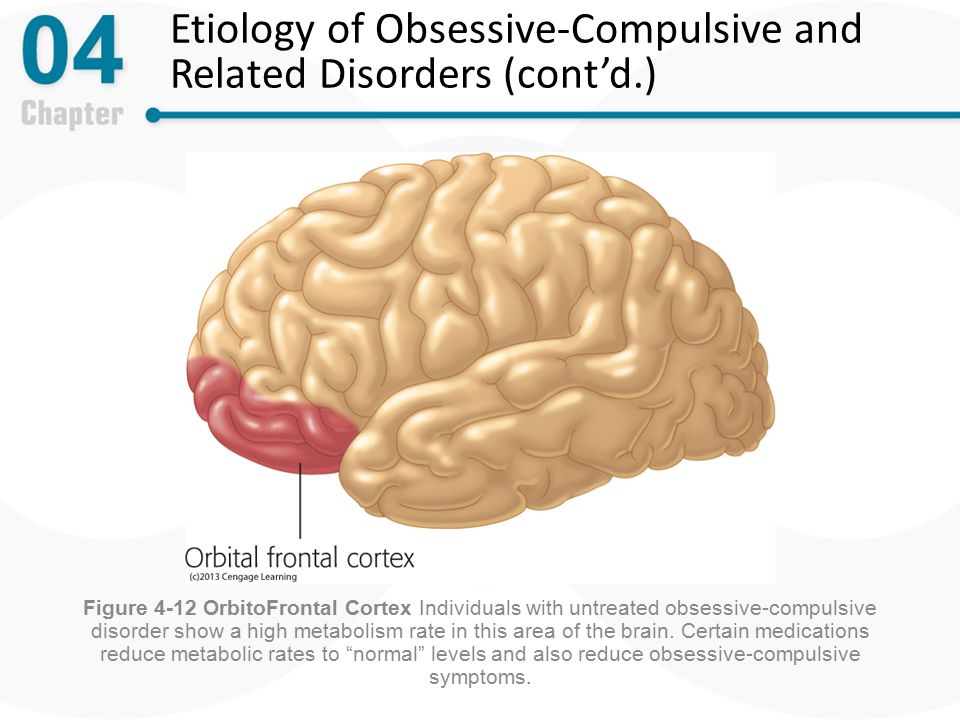
Whilst OCD is considered an anxiety disorder, OCPD, as the name suggests, is actually a personality disorder. It’s also possible to suffer from both OCD and OCPD simultaneously.
So what is OCPD?
Section Contents
- Obsessive Compulsive Personality Disorder (OCPD)
- Clinical Classification of OCPD
The World Health Organization’s International Classification of Diseases (ICD) uses the term Anankastic Personality Disorder to code and describe OCPD. The word ‘anankastic’ is derived from the Greek word anankastikos meaning ‘compulsion’.
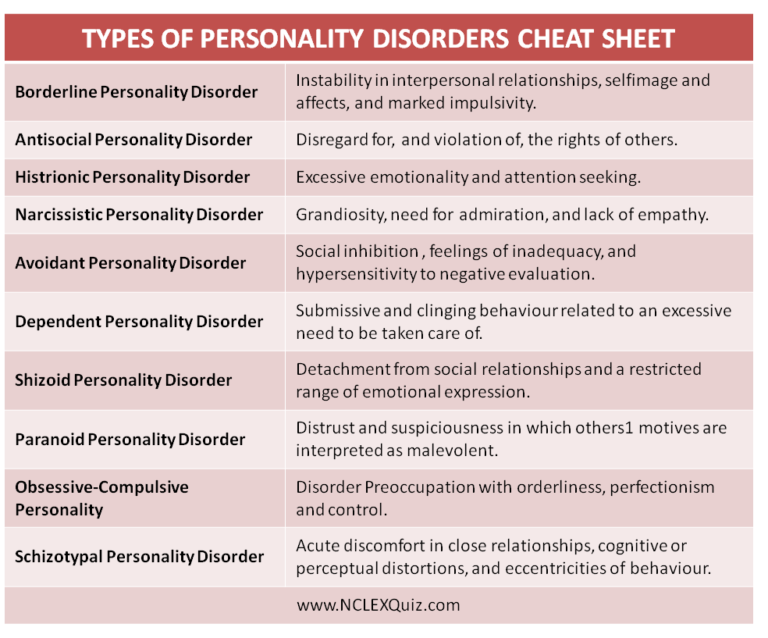
The main features of Obsessive Compulsive Personality Disorder (OCPD) is a preoccupation with orderliness, perfectionism (around anything from cleanliness to order) at the expense of flexibility, openness, and efficiency, regardless of the impact on others.
Individuals with OCPD attempt to maintain control with painstaking attention to rules, trivial details, lists and procedures to the extent that the major point of the activity is often lost, often becoming inflexible. They become oblivious to the fact that other people will often become annoyed at the extent they perform tasks and the delays caused, often believing the other person may be wrong for not working to the same perceived standard.
The inflexibility can also impact on areas of morality, ethics and values, forcing themselves and others to follow very rigid moral principles.
OCPD is one of the most prevalent personality disorders in the general population, with estimated prevalence ranging from 2% to 8%. Some studies suggest that Obsessive-Compulsive Personality Disorder is more common in males.
How does OCPD differ from OCD?
Individuals with anxiety disorders like OCD, may have an increased likelihood of having a personality that meets some criteria for Obsessive-Compulsive Personality Disorder. Despite this individuals with OCD do not have a pattern of behaviour that would usually meet the criteria for OCPD.
Despite this individuals with OCD do not have a pattern of behaviour that would usually meet the criteria for OCPD.
The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) specifies the following difference in diagnosing OCD and/or OCPD:
Despite the similarity in names, OCD is usually easily distinguished from obsessive-compulsive personality disorder by the presence of true obsessions and compulsions in OCD. When criteria for both obsessive-compulsive personality disorder and OCD are met, both diagnoses should be recorded.
Much of the difference is based around how much insight the person suffering has. Whilst people with OCD usually have sufficient insight that OCD is causing their behaviour, and accept they need to change, people with OCPD usually have little, if any, insight into their behaviours, rituals and thinking needing to change. Typically, people with OCD know they need help and will usually want treatment, but people with OCPD typically believe they don’t require treatment.
Significantly, whereas with OCD, the thoughts, beliefs and behaviours (obsessions and compulsions) are because of feared consequences that feel very real; which often interfere in several areas of the person’s life including work, social and/or family life. With OCPD, the problem is much more about rigidity around rules rather than perceived consequences and will usually interfere with certain tasks. Interpersonal relationships will often suffer, with co-workers, or even employer relationships becoming strained because of set rules having to be adhered to at work. Equally at home, family members of people with OCPD can often feel extremely criticised and controlled which can be frustrating and upsetting and often lead to conflict.
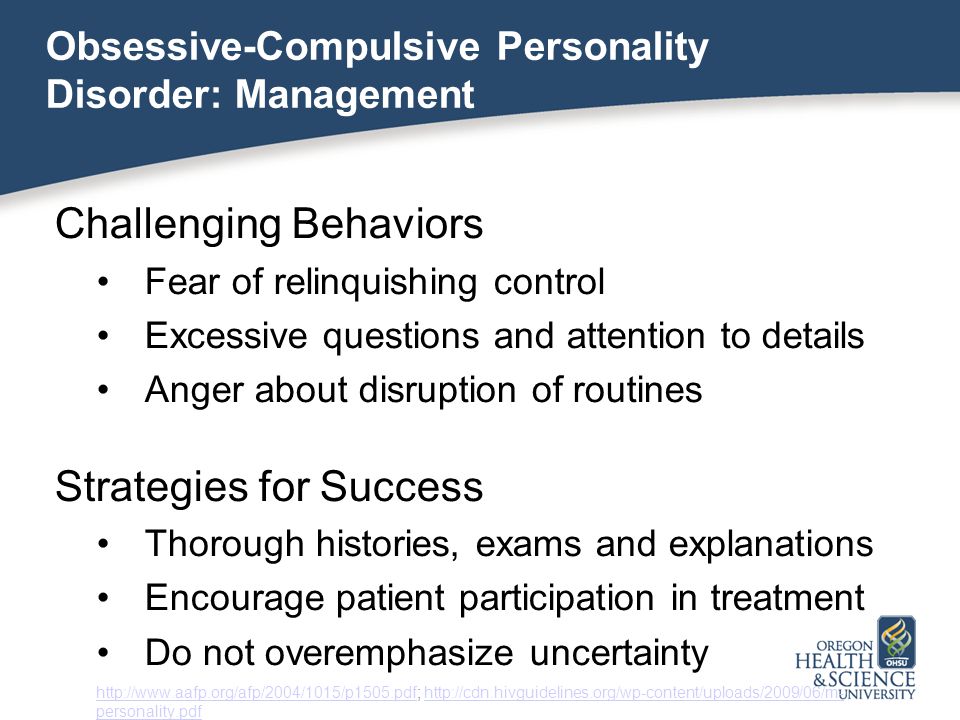
Treating Obsessive Compulsive Personality Disorder
It’s not easy to treat OCPD, even when the person is prepared to seek help, but if the person is willing to seek and accept help, then treatment can be effective. It has been suggested that sometimes those with OCPD may respond better to treatment because of rigid adherence to therapy tasks set by the therapist.
The treatments for OCPD are very similar to those for OCD, with the treatment found to be the most effective being a talking therapy called Cognitive Behavioural Therapy (CBT). Some people find they also need the additional support of medications.
What to read next:
Depression
OCPD Clinical Classification
Page information and additional reading
[lastreviewed]
[nextreviewed]
Additional Reading:
Disclaimer: This article is for information only and should not be used for the diagnosis or treatment of Obsessive-Compulsive Disorder or any other medical condition. OCD-UK have taken all reasonable care in compiling this information, but always recommend consulting a doctor or other suitably qualified health professional for diagnosis and treatment of Obsessive-Compulsive Disorder or any other medical condition.
Obsessive-Compulsive Personality Disorder (OCPD) - HelpGuide.org
What is obsessive-compulsive personality disorder (OCPD)?
It's not unusual for someone to be diligent, orderly, or stubborn. In some cases, those personality traits can even come in handy. However, when those traits are taken to an extreme, they can reduce the quality of a person's physical, emotional, and social well-being.
People with obsessive-compulsive personality disorder (OCPD) have a fixation with perfection, control, and orderliness. Their preoccupation is severe enough to lead to impairment. Picture a student who is so focused on small details that they fail to complete an assignment. Or imagine someone whose moral code is so inflexible that they have trouble seeing things from another person's perspective.
A person with OCPD may not be aware of their condition or see a need for change. In fact, they may believe that other people are the ones who should change.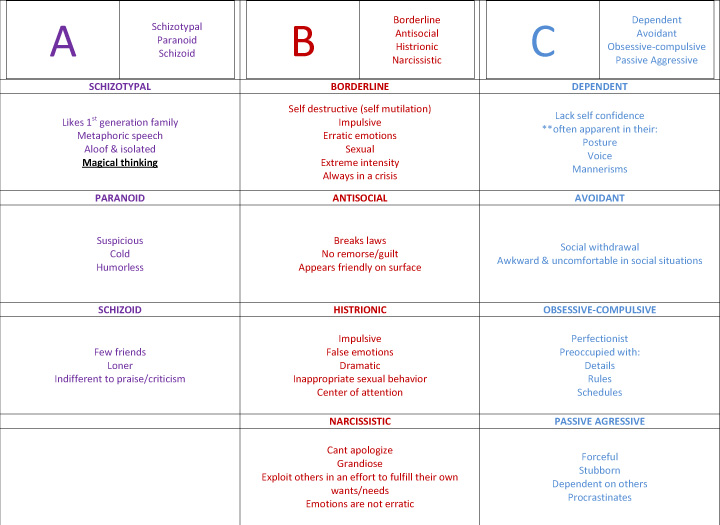
People with OCPD have a tendency to impose their high standards on others. For example, a husband with OCPD might refuse to let his wife help plant a garden unless the wife agrees to follow a strict methodology. If his partner deviates at all from the rules, the husband can become overly critical.
Unsurprisingly, this rigid approach to life can lead to difficulty maintaining relationships or adapting to new circumstances. Loneliness and depression may develop as relationships deteriorate. The person with OCPD may avoid or quit activities they don't immediately excel in, limiting their potential. In addition, an intense focus on perfectionism can lead to anxiety, eating disorders, and other physical and mental problems.
Do you think you recognize these symptoms in yourself or someone you love? Learn more about the specific signs of OCPD as well as self-help tips that can help manage the disorder.
Causes and symptoms of OCPD
OCPD is one of the most common personality disorders.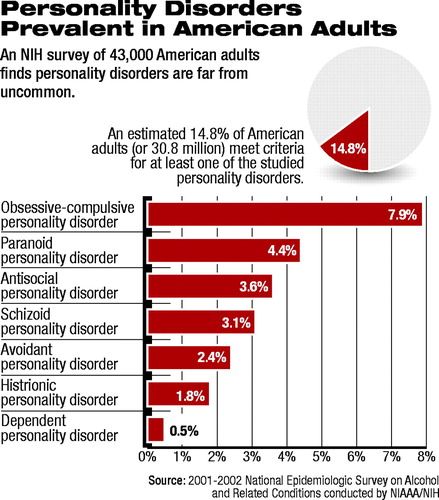 Research indicates that somewhere between 3 to 8 percent of the population has OCPD, and it's most common in older people. This personality disorder involves a persistent pattern of behavior that often starts when the person is a teenager or young adult.
Research indicates that somewhere between 3 to 8 percent of the population has OCPD, and it's most common in older people. This personality disorder involves a persistent pattern of behavior that often starts when the person is a teenager or young adult.
Experts haven't identified one exact cause of OCPD. However, research suggests that a person's upbringing may play a role. For example, being raised in an environment that has strict rules and harsh punishments may lead a person to obsess over doing things “the right way.” OCPD may also have a genetic component, meaning that it might be inherited.
Signs and symptoms of OCPD include:
- Perfectionism that gets in the way of finishing tasks.
- Fixation with using lists, rules, and schedules to maintain order.
- Unwillingness to delegate work to someone who may take a different approach to the task.
- Devotion to work that leads to neglect of relationships.
- Hoarding money for future disasters.
- Overly conscientious of ethics, morality, and values.
- Inability to get rid of worthless items, such as worn-out shoes, despite the lack of sentimental value.
- Overly stubborn and rigid disposition.
Diagnosis
For an OCPD diagnosis, a person must show at least four of the eight signs listed above. The symptoms must be part of a long-term pattern that was formed by early adulthood.
The diagnosis process will likely involve screening questionnaires, which allow the person to self-report on their own behavior. The screening is followed by an interview. In addition to self-reported details, information gathered from friends, family, and peers can also help a mental health expert make an accurate diagnosis.
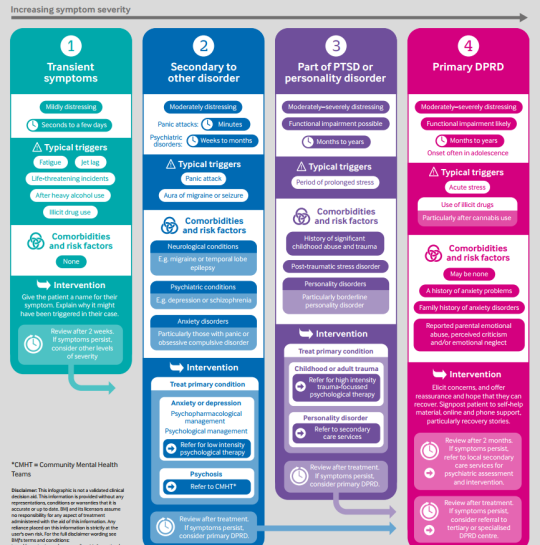
A mental health expert will need to rule out other possible explanations for the behavior. For example, obsessive-compulsive disorder (OCD) is a separate condition that can also involve a preoccupation with orderliness and hoarding.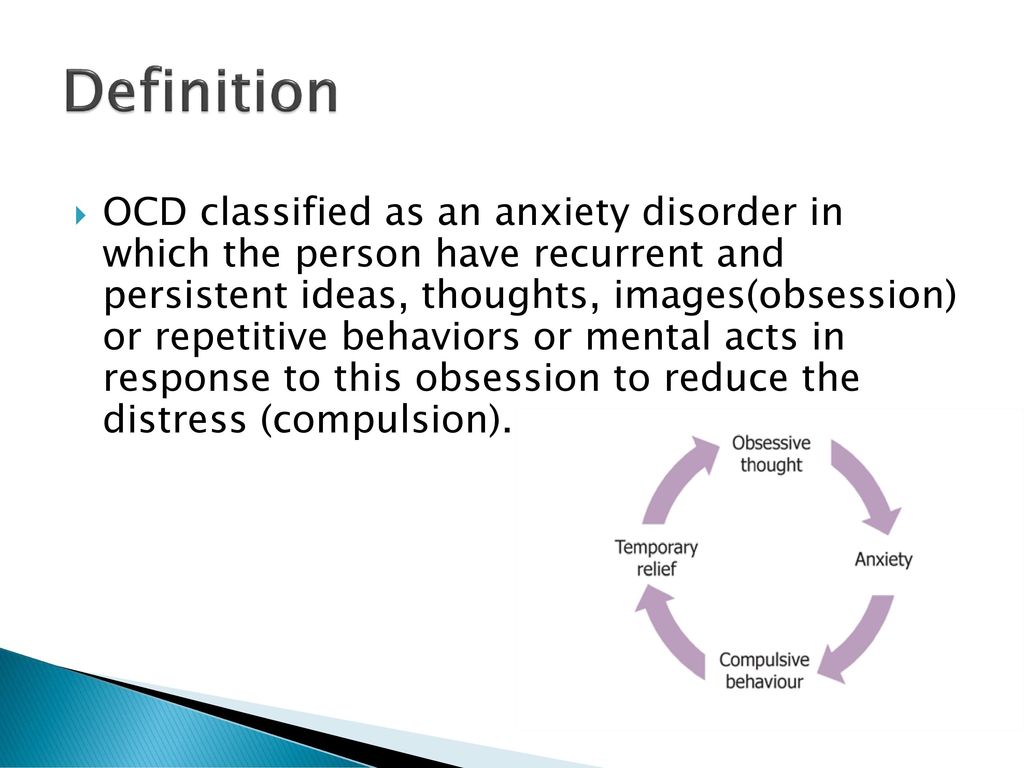
It can also be tricky to distinguish OCPD behavior from “conventional” behavior. Some questions to consider:
- Is the person overly devoted to work? Or are they just trying to earn higher pay for financial stability?
- Is the person a perfectionist? Or are they just detail-oriented and willing to cut corners when necessary?
- Is the person obsessed with control? Or do they just want a practical amount of orderliness in their home?
- Is the person having a hard time getting rid of items due to sentimental value?
If you suspect you have OCPD, you may feel hesitant to seek a diagnosis. Perhaps you feel as though your approach to life is more helpful than harmful. In many cases, people with OCPD who seek a diagnosis do so at the request of a loved one. So, if your approach to life seems to be damaging your relationships, a formal diagnosis may offer insight and a path forward.
Speak to a Licensed Therapist
The world's largest therapy service.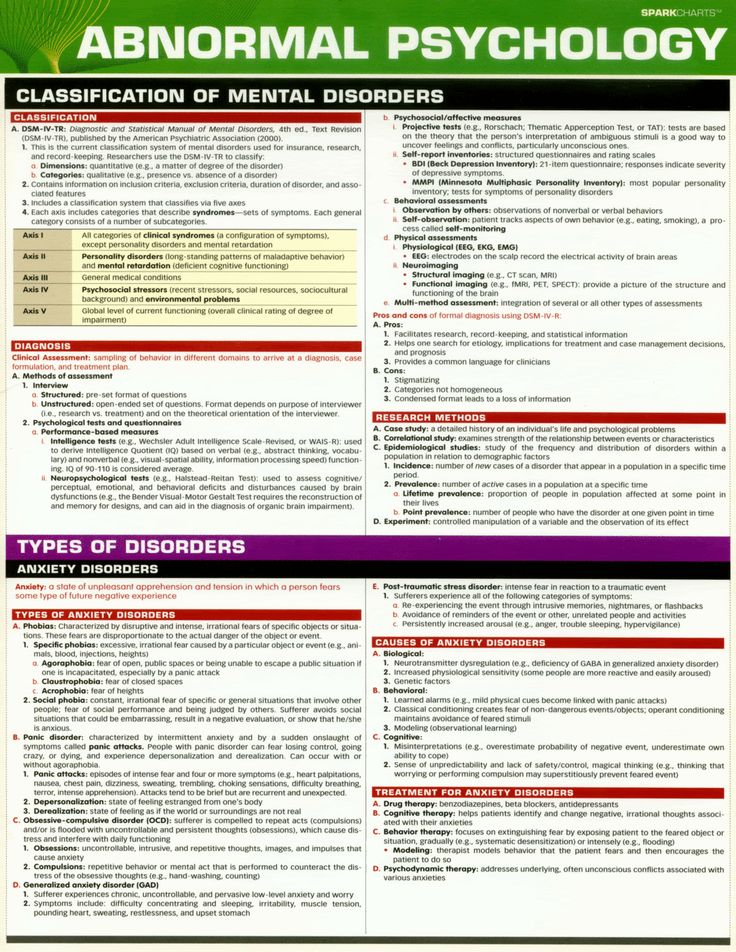 100% online. Get matched with a professional, licensed, and vetted therapist in less than 48 hours.
100% online. Get matched with a professional, licensed, and vetted therapist in less than 48 hours.
Get 20% off
Professional online therapy and tools based on proven CBT strategies. Get instant help, along with your own personalized therapy toolbox.
Get 20% off
Affiliate Disclosure
Co-occurring disorders
People with OCPD often struggle with other physical and mental health conditions. When multiple disorders are present, it's important to address all of the issues simultaneously, as they may affect one another. Some of these co-occurring disorders include:
Eating disorders. Perfectionism can motivate people with OCPD to reach for unrealistic standards, even at the cost of their own health. That degree of perfectionism is also found in people with eating disorders, such as anorexia and bulimia nervosa, so these conditions may co-occur with OCPD.
[Read: Eating Disorder Treatment and Recovery]
Mood disorders. Research shows that OCPD is associated with mood disorders, including depression. Workplace burnout, difficulty with social interactions, and failure to live up to their own high expectations may contribute to depressive symptoms. OCPD traits have also been linked to suicidal ideation.
Research shows that OCPD is associated with mood disorders, including depression. Workplace burnout, difficulty with social interactions, and failure to live up to their own high expectations may contribute to depressive symptoms. OCPD traits have also been linked to suicidal ideation.
Physical problems. One study found that OCPD traits are linked to cardiovascular health conditions, such as hypertension. Other research seems to indicate an association between OCPD and stroke and arthritis.Avoidant Personality Disorder (AVPD)
Other personality disorders. A person can struggle with overlapping personality disorders. People with OCPD may also be diagnosed with dependent, histrionic, borderline, avoidant, or narcissistic personality disorders.
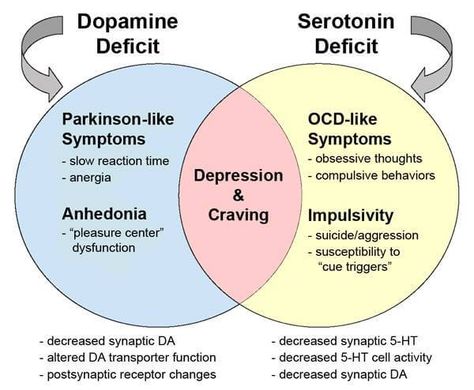
Anxiety disorders. As people with OCPD are striving to maintain order and achieve perfection, they may also be plagued by anxiety. Anxiety disorders, such as generalized anxiety disorder and panic disorder, may co-occur with OCPD. OCD is another anxiety disorder that may co-occur with OCPD, and the two conditions are commonly mistaken for each other.
OCD is another anxiety disorder that may co-occur with OCPD, and the two conditions are commonly mistaken for each other.
OCPD vs. OCD
Despite similarities in their names, OCPD and obsessive-compulsive disorder (OCD) have key differences.
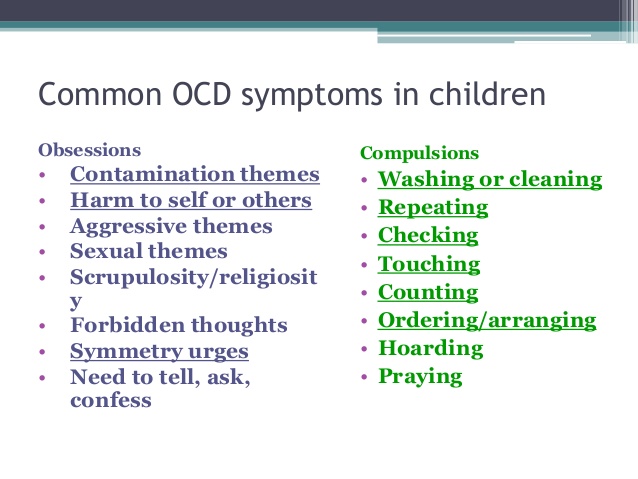
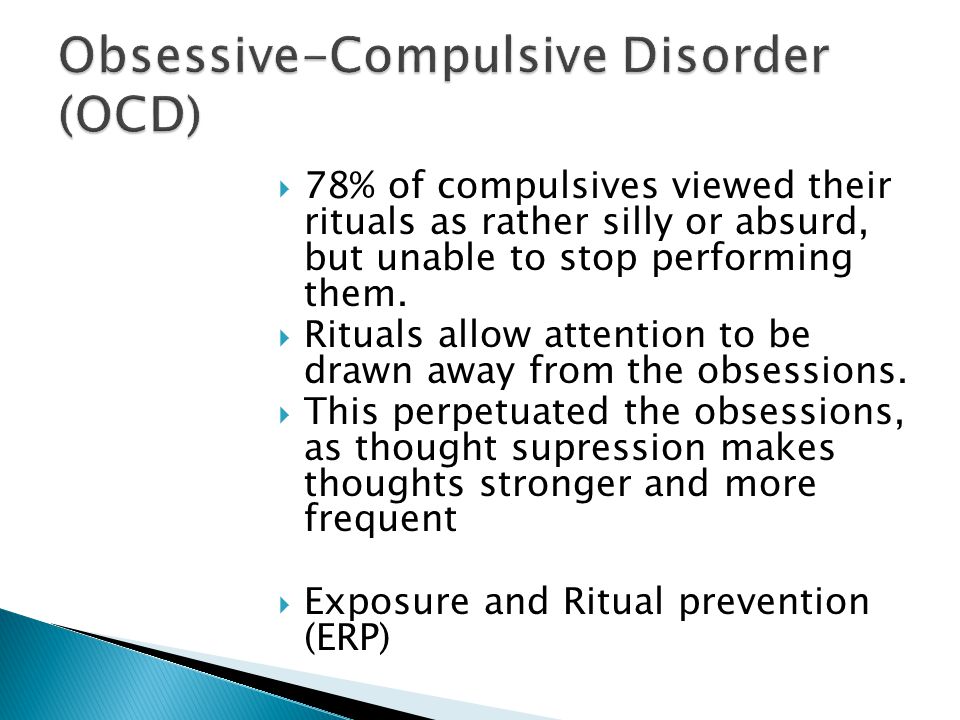
People with OCD struggle with unwanted, anxious thoughts (obsessions) and feel compelled to perform ritualized actions to reduce their anxiety. For example, a fear of germs may lead a person with OCD to continually wash their hands. The person is often aware that their fears and urges are irrational.
[Read: Obsessive-Compulsive Disorder (OCD)]
People with OCPD are less likely to recognize their disorder than people with OCD. They typically aren’t driven by obsessive thoughts or specific repetitive actions. Instead, they have a more general desire for order and perfection, which they see as part of their own fixed values. Research also shows that people with OCPD are less impulsive and more willing to delay rewards than people OCD.
| OCD traits vs. OCPD traits | |
| OCD traits | OCPD traits |
| You keep wiping down the kitchen counter because you have anxious, intrusive thoughts about food contamination. You’re aware this is a time-consuming activity, and the irrationality of it causes you distress. | You frequently clean the kitchen counter because you want it to look spotless. The activity is inconvenient for everyone else in your family, but you believe the kitchen needs to remain neat and orderly. |
| You keep checking and rearranging luggage items, trying to ease the fear of something being damaged, lost, or left behind. | You create a detailed list of what you want to pack and in which suitcase. You become so fixated on writing the list you no longer have time to pack. |
| You keep asking if you’ve insulted someone. You're experiencing intrusive thoughts about accidentally offending other people. | You take a long time to speak so your words avoid misinterpretation. In your mind, everyone should be this careful when speaking. |
OCPD is more common than OCD, but about 15 to 28 percent of people with OCD may also have OCPD. Someone with both disorders may experience more severe symptoms, as well as higher distress. Due to the stubborn nature of people with OCPD, they may be less willing to accept treatment. However, when they do accept treatment, their preoccupation with perfectionism may be beneficial. For example, they may be more thorough in following their self-help practices.
Self-help for OCPD
If you or a loved one have OCPD, there are many steps you can take to limit some of the more negative aspects of the disorder. Many of these strategies involve easing the strong desire to control every circumstance and perfect every task.
OCPD self-help tip 1: Manage stress
People with OCPD often feel they have a lot of tasks on their schedule and believe those tasks need to be done well. On top of that, crippling fear of failure can lead to procrastination. This can make for stressful days and outbursts of frustration.
Relaxation techniques can help you manage stress and improve your mood. They might also help you reflect on and accept matters that are beyond your control. Here are a few practices that may help:
Experiment with mindful breathing. This simple form of meditation involves focusing on your inhales and exhales. Long, deep breaths can decrease your stress response and keep you grounded in the present moment.
[Listen: Mindful Breathing Meditation]
Exercise regularly. Physical activity releases endorphins, hormones that promote a feeling of well-being. Activities such as yoga and tai chi can be especially helpful, as they combine physical activity with mindful breathing.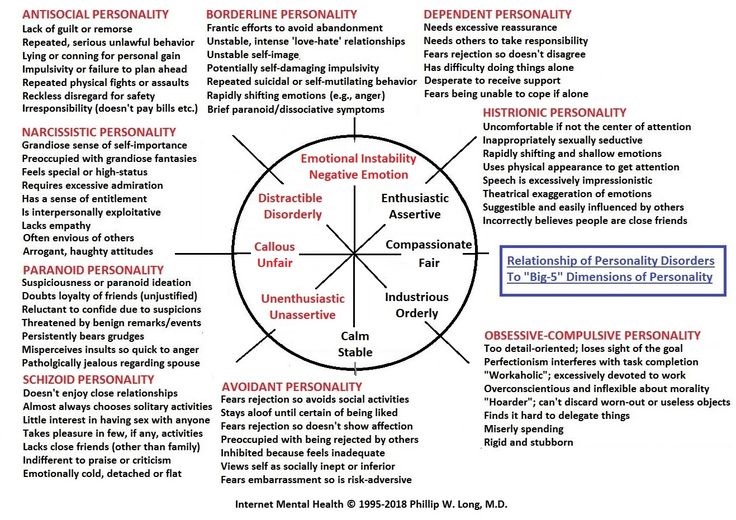
Get enough rest. Even if you think of yourself as a workaholic, it's important to get enough sleep every night. Lack of sleep not only raises your stress levels, it can also hinder your work performance.
Eat healthy meals. Poor eating habits can leave your body more susceptible to stress. Think of healthy meals as a high priority as you plan your daily schedule.
Helping someone with OCPD manage stress
If you're living with someone with OCPD and want to encourage them to try the practices listed above, remind them that everyone can benefit from stress management. Frame it as a team activity that can improve both your lives, rather than an activity that is only meant to “fix” them. Take the time to meditate with them or join them in exercising and eating healthy.
Tip 2: Practice self-compassion
If you have OCPD, there's no doubt that you have high expectations for yourself. When those expectations aren't met, you might take your frustrations out on yourself as well as friends and family members.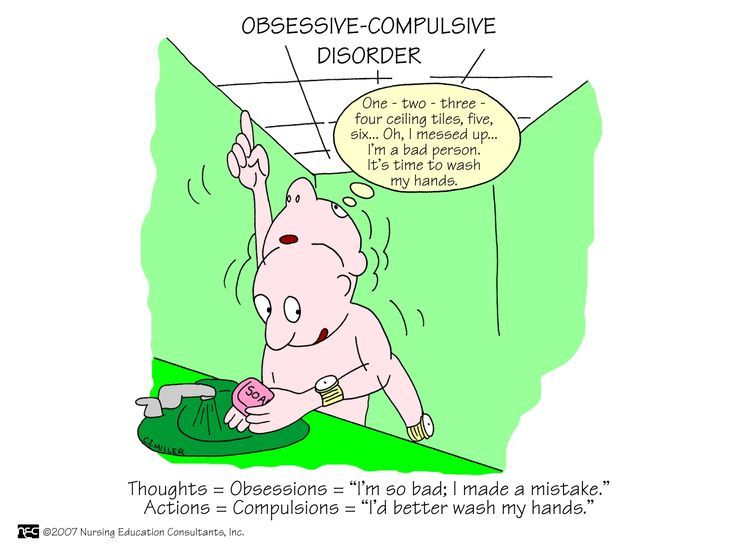 You might also have a tendency to overinflate the flaws you see in yourself and others.
You might also have a tendency to overinflate the flaws you see in yourself and others.
Self-compassion starts with accepting that you (and those around you) have limits. Despite your best efforts, you'll make mistakes and overlook things. Don't think of those shortcomings as evidence that you're a failure. Look at them as opportunities to grow and remember to forgive yourself rather than allow self-hatred to build.
Adjusting self-talk
Another step toward self-compassion involves paying attention to your self-talk. When you engage in negative self-talk, you use disparaging inner monologue such as, “I'm not good enough” or “I'm such an idiot.” These kinds of thoughts can lead you to depression and warp your perception of reality.
Try to notice when you're using negative self-talk and challenge those negative statements with neutral or positive self-talk.
| Self-talk examples | |
| Negative self-talk | Neutral or positive self-talk |
“I'm stupid for forgetting to do my taxes. ” ” | “I forgot to do my taxes because I was busy with other things. This mistake doesn't make me a bad person.” |
| “My friends secretly hate the way I act.” | “I'm grateful I have supportive friends, and I can take steps to strengthen those friendships.” |
| “My relationship is falling apart, but therapy would be a waste of my time.” | “There's still time to repair my relationship. Therapy might help me grow.” |
| “I skipped my workout, which means that I'm lazy and unhealthy.” | “I didn't have the time or motivation to exercise today. I can do it some other time and let my body rest today.” |
Use self-talk to encourage yourself rather than tear yourself down. Talk to yourself as if you're trying to comfort or empower a loved one.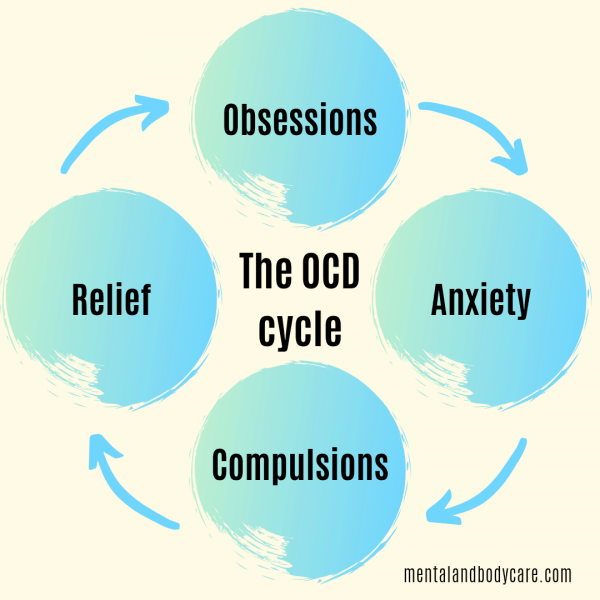
Helping someone with OCPD practice self-compassion
If you live with someone with OCPD, offer them praise to counter their negative self judgments. For example, if they didn't break their own jogging record, remind them that their current record is extremely impressive. Let them know that there is always time for growth. This may help steer them away from “all or nothing” thinking and remind them to be self-compassionate.
You can also encourage them to join you in meditation practices that focus specifically on self-kindness. Try our audio guide Being Kind to Yourself: A Meditation.
Tip 3: Manage emotions
A 2015 study that investigated emotional functioning in people with OCPD found that the disorder is associated with high levels of negative emotions, such as frustration, as well as difficulties identifying and accepting their own emotions.
So, if you have OCPD, it's not unusual to want to hide back certain emotions, especially negative ones like shame, anger, or fear.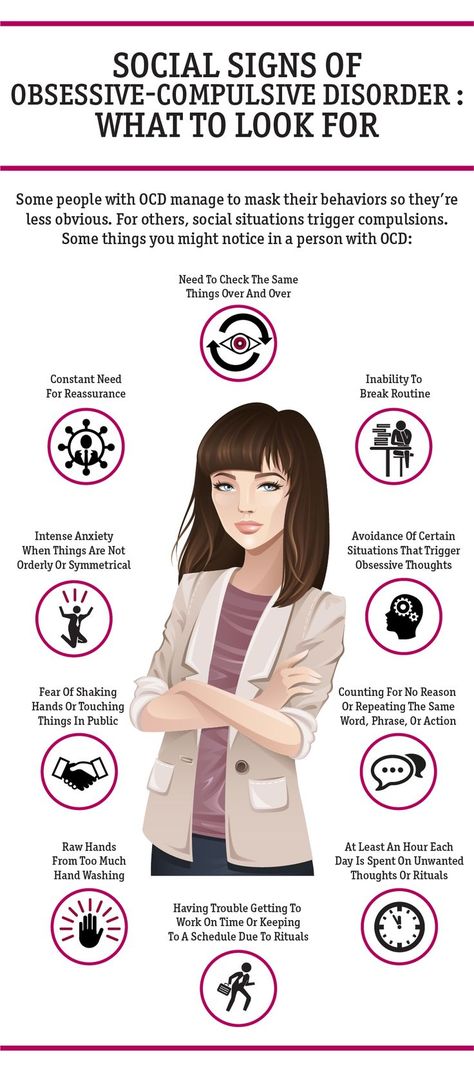 You might even feel uncomfortable when other people express those emotions. However, suppressing your emotions can also lead to issues over time, such as angry outbursts and depressive episodes. Here are a few ways to better manage your emotions:
You might even feel uncomfortable when other people express those emotions. However, suppressing your emotions can also lead to issues over time, such as angry outbursts and depressive episodes. Here are a few ways to better manage your emotions:
Identify your emotions. Learn to identify your emotions instead of denying what you're feeling. You might begin by learning to notice physical signs of your emotions. Maybe when you're angry you feel your jaw tighten, or perhaps when you're sad you feel yourself droop.
Accept your emotions. This can be difficult, especially if you pride yourself on keeping a level head. Just know that everyone experiences a range of emotions, and it's normal to feel everything from sadness to anger to shame. Having these emotions doesn't make you a weak person.
Problem solve. Identify what's bothering you. Maybe you made a mistake at work and feel angry at yourself for overlooking details. Is there anything you can do to address the root cause of the issue? Or maybe an argument with your partner has left you feeling tired and depressed.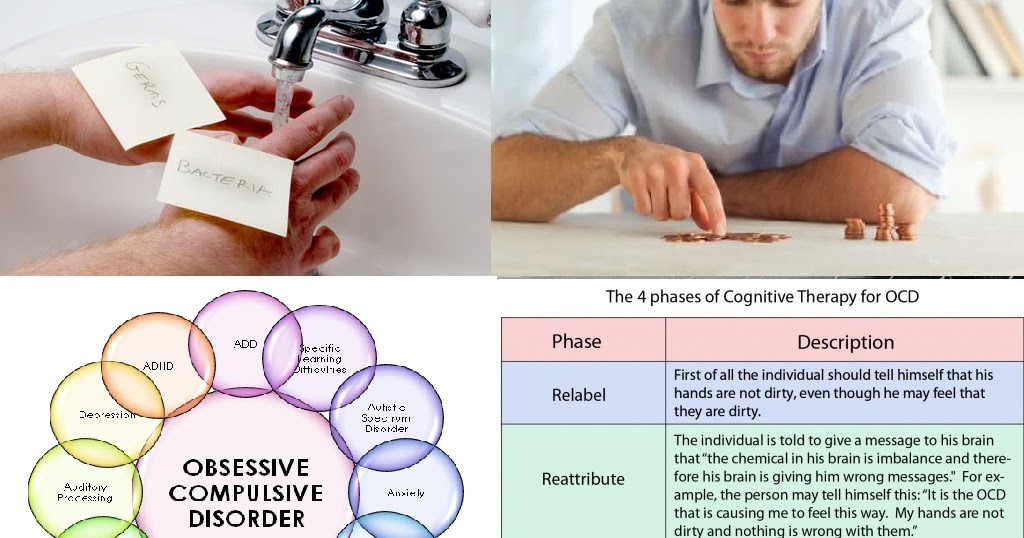 What can be done to repair the rift between the two of you?
What can be done to repair the rift between the two of you?
Reevaluate the situation. Not every problem has a solution. In some cases, you may simply need to accept and reevaluate the situation. Imagine that you've fallen behind schedule and now you have no time for your daily run. In the grand scheme of things, does it matter that you've missed this workout? Perhaps your body needed the rest anyway. Reappraising matters can help put them in perspective and steer you away from catastrophizing.
A powerful tool to help you manage your emotions
HelpGuide’s free Emotional Intelligence Toolkit can help you learn how to identify and manage difficult emotions in healthier ways. Over time, it can make a huge difference in your ability to manage stress, balance your moods and emotions, and take back control of your life.
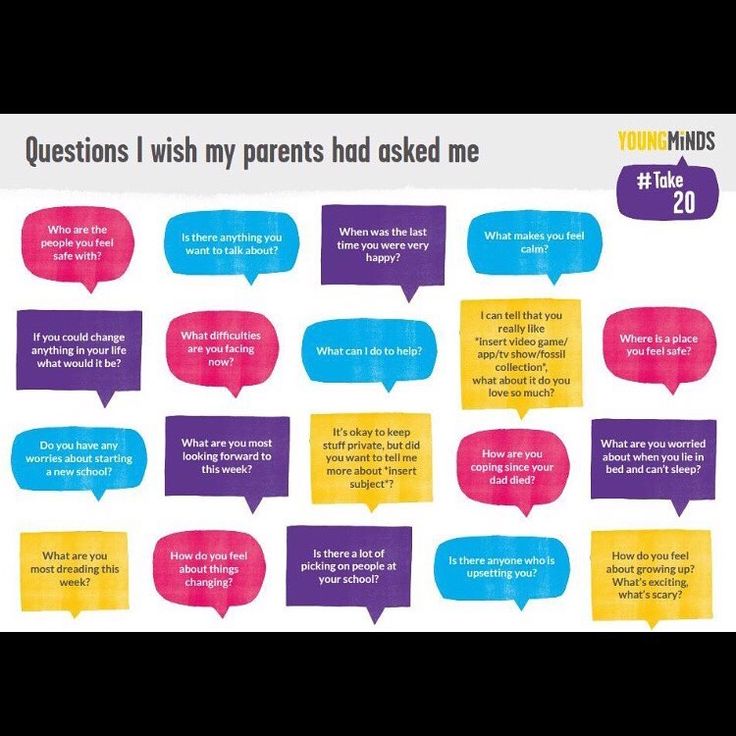
Helping someone with OCPD manage emotions
You can encourage your loved one to use the steps above, but you can also go further and make them feel comfortable venting to you. Be an engaged listener by asking questions and empathizing with them. You shouldn't try to write off their concerns as “no big deal,” but you can gently move them along in reevaluating the situation.
Be an engaged listener by asking questions and empathizing with them. You shouldn't try to write off their concerns as “no big deal,” but you can gently move them along in reevaluating the situation.
Tip 4: Reach out for help
If you have OCPD, be willing to accept two potentially uncomfortable truths: You can't do everything alone and you have blind spots. Get in contact with self-help groups or online forums where people share their OCPD experiences. This can help you learn more about how the disorder affects people in different ways. You'll also learn how others cope with the negative aspects of OCPD.
Encouraging someone with OCPD to reach out for help
If you're close to someone with OCPD, be prepared for them to push back on the idea that they need to change or improve at all. However, gently encouraging them to join OCPD self-help groups may lead them to self-reflection. They may be more willing to hear from people who have similar preoccupations with perfectionism and orderliness.
Another strategy is to point to depression, work burnout, anxiety, or irritability as a reason to seek out help rather than place the emphasis on OCPD. Appeal to the person logically, citing concrete examples of how certain traits impact your relationship.
How OCPD affects relationships
If you're in a relationship with someone with OCPD, you might struggle with your friend or partner's persistent need for control. Maybe they always insist on planning out every detail of your vacation. Or perhaps they demand that every room in the house be cleaned in a specific way and according to a specific schedule. You may have grown accustomed to walking away from arguments or feeling like their work life takes priority over you.
And if you're the one with OCPD, you might feel frustrated that the people around you have different standards. Maybe your spouse or roommate doesn't keep things as tidy as you'd like. Or perhaps they aren't as punctual or frugal as you.
Despite all of these potential frustrations, it's possible for people with OCPD to have long and healthy relationships with others. Whether you or your loved one has OCPD, use the following strategies to keep the peace:
Don't fixate on winning
This can be particularly challenging for a person with OCPD, who may feel a strong desire to be right. However, even those without OCPD may struggle with this. Do your best to put your ego aside during arguments, and look to resolve conflicts rather than “win” them.
Be respectful and thoughtful in communicating, even if you both need to take an occasional pause to clear your heads. Use “I” statements to express your perspective. Avoid using “you” statements to assign blame. Don't hesitate to apologize when necessary.
Appreciate each other
Sometimes it's easy for a person with OCPD to fall into a routine of being overly critical. And the person without OCPD may fall into a similar pattern, focusing only on their friend or partner's rigidity and negative aspects.
Remember to be vocal about what traits you appreciate in each other, such as work ethic and reliability. Tell the person how they've improved your life, whether that includes their emotional support or their contributions to the household. This helps create a sense of security.
See the good in your partner
Despite a tendency to be controlling, people with OCPD often have good intentions. And when they show annoyance or frustration, they're likely grappling with feelings of anxiety or helplessness. Recognize those feelings, and ask what you can do to help.
If you have OCPD, it's also important to recognize the other person's good intentions. Their drive toward perfection may not be as strong as yours, but, in the end, neither of you can ever be flawless.
Take care of yourself
Having a relationship with someone with OCPD may require you to be more assertive. Be clear about what expectations are too high. For example, if you believe their cleanliness demands are unreasonable, let your loved one know.
Try to compromise on a solution, and don't feel the need to overextend yourself. Recognize that your way of doing things doesn't have to match their way of doing things.
If a romantic relationship isn't working, couple's therapy can be helpful. However, if your partner is abusive or unwilling to change, you may need to accept that the relationship won't work at this time.
[Read: Dealing with a Breakup or Divorce]
Professional treatment for OCPD
When self-help treatments offer little relief from negative OCPD symptoms, professional treatments are the next step. Again, many people with OCPD may not see the need to treat symptoms, much less visit a professional. You may need to be patient and present evidence that intervention is needed.
Therapy
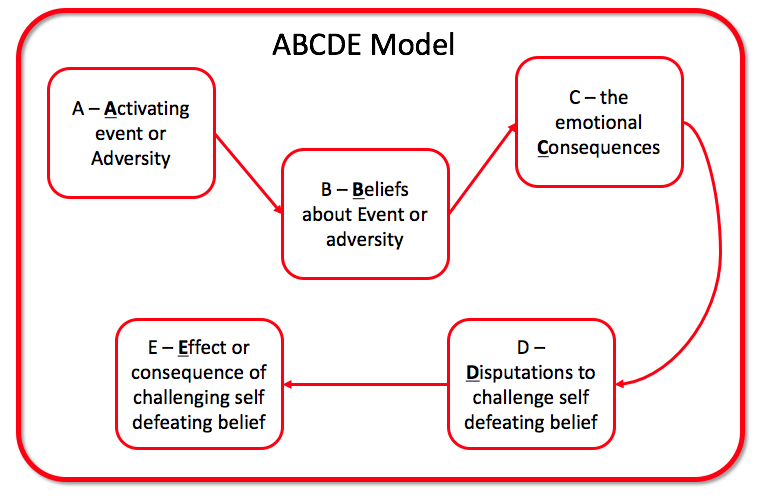
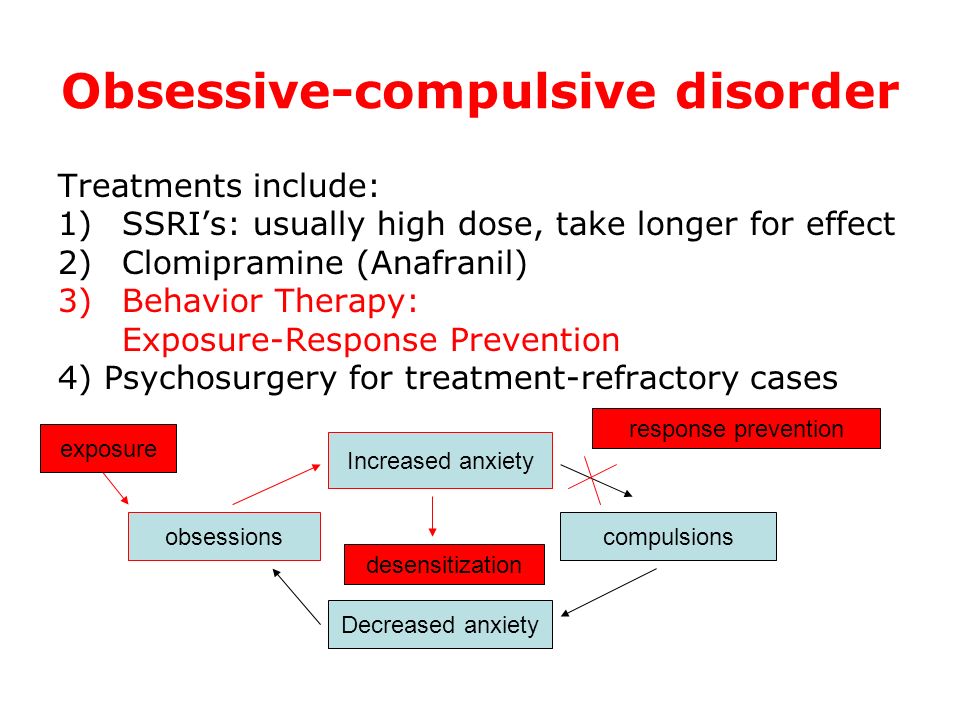
Two common approaches to therapy for OCPD include cognitive behavioral therapy (CBT) and psychodynamic therapy.
During CBT, a therapist may draw the person's attention to how their core beliefs can be detrimental to their mental health, physical health, and relationships. For example, a therapist might challenge a person's core belief of, “I need to create lists and plan things out to feel comfortable.” CBT can also help a person find constructive ways to express emotions such as frustration.
For example, a therapist might challenge a person's core belief of, “I need to create lists and plan things out to feel comfortable.” CBT can also help a person find constructive ways to express emotions such as frustration.
Psychodynamic therapy helps a person with OCPD connect present-day traits with past experiences. A person with OCPD might find that their need for control and order is rooted in childhood experiences with overly critical parents.
[Read: Online Therapy: Is it Right for You?]
Other potential therapy interventions may include:
- Dialectical behavioral therapy (DBT), which may improve emotional regulation.
- Nidotherapy, which focuses on making environmental changes to improve the person's mental health.
Medication
You won't find a single type of medication for treating the entire spectrum of OCPD symptoms. However, certain medication can be prescribed to treat specific aspects of OCPD and its co-occurring disorders. A few examples include:
A few examples include:
- Selective serotonin reuptake inhibitors (SSRIs), types of antidepressants, may be used to decrease the person's over fixation on details.
- Benzodiazepines and other anti-anxiety drugs may help a person with OCPD who is also experiencing an anxiety disorder, such as OCD.
- Anticonvulsant medications may be used to reduce irritability and stabilize mood.
Finding the right mix of medication and therapy may require some trial and error. In the meantime, a focus on accepting imperfections and managing negative emotions may lead to noticeable changes.
Helplines and support
- In the U.S.
Call the NAMI HelpLine at 1-800-950-6264.
- UKIndia
Call the SANEline at 07984 967 708.
- Australia
Call the Sane Helpline at 1800 187 263.
- Canada
Visit Mood Disorders Society of Canada for links to provincial helplines.
- India
Call the Vandrevala Foundation Helpline at 1860 2662 345.
- Online
Find links to forums and support groups at The OCPD Foundation.

Last updated or reviewed on March 1, 2023
Treatment of obsessive-compulsive disorder
Treatment of obsessive-compulsive disorder. We will relieve you of obsessive thoughts, movements and rituals. Let's get back to life!
Symptoms of obsessive-compulsive disorder
- Frightening images and drives
- Compulsive acts (rituals)
- Intrusive check of one's own actions
- Fear of trouble, pollution or contamination
- Inexplicable desire to count something
- Excessive organization and pedantry
- Perfectionism in relationships, work and even leisure
- "Stuck", "looping" on one's thoughts
You feel that over time your mood becomes worse: apathy, depression, obsessions increase, and rituals begin to fill all your free time or harm your physical health.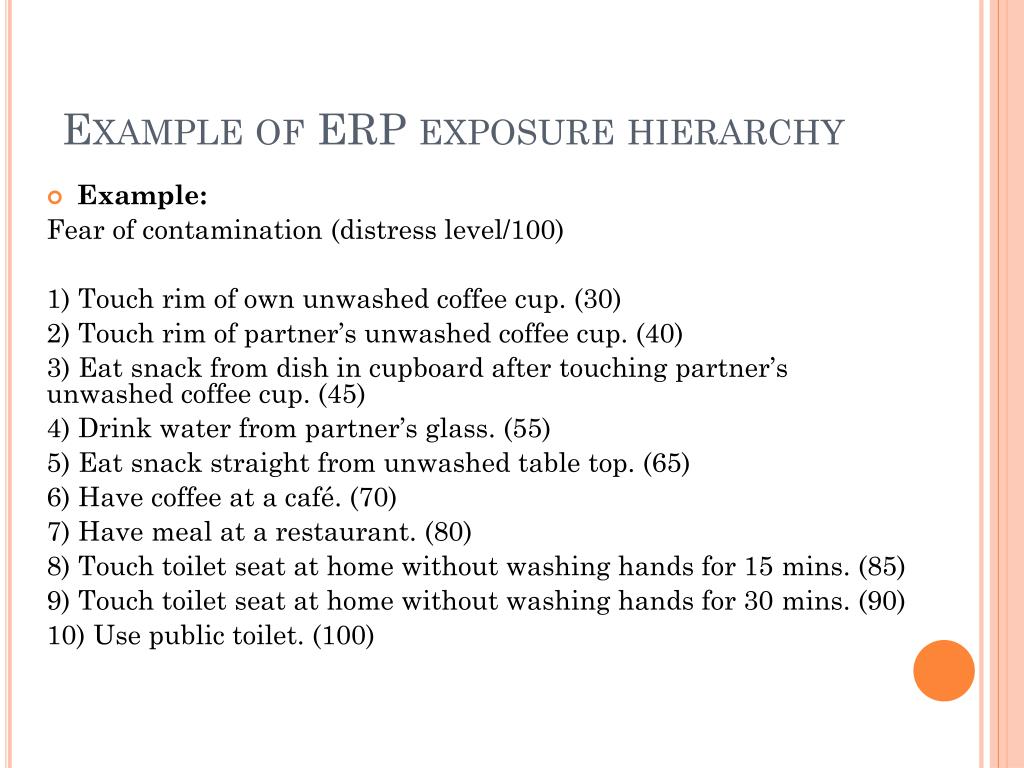
You may have had more than one meeting with psychologists, psychotherapists and psychiatrists. You are not given the "scary" psychiatric diagnoses of Schizophrenia or Bipolar Disorder, but are prescribed medication and psychotherapy nonetheless. However, such treatment cannot be called effective - the symptoms persist and only aggressive pharmacotherapy temporarily reduces anxiety.
What is obsessive-compulsive disorder?
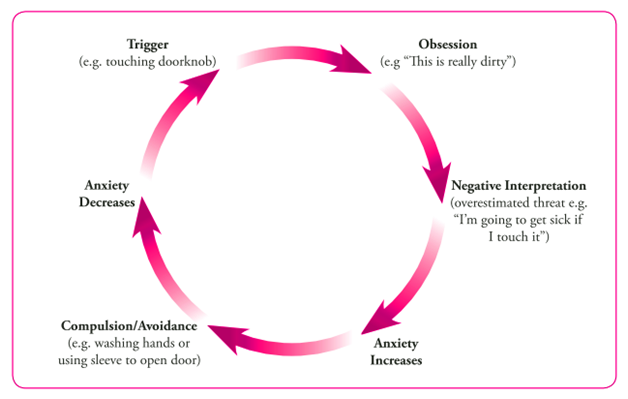
Obsessive-compulsive disorder is a syndrome characterized by the presence of obsessive thoughts (obsessions) to which a person reacts with certain actions (compulsions). The causes of the disorder are rarely superficial. The syndrome is also accompanied by the development of obsessive memories and various pathological phobias. May be chronic, episodic or progressive.
Obsession - obsessive thought, persistent desire for something, uncontrollable and accompanied by anxiety and intense anxiety. In an attempt to cope with such thoughts, a person resorts to committing compulsions.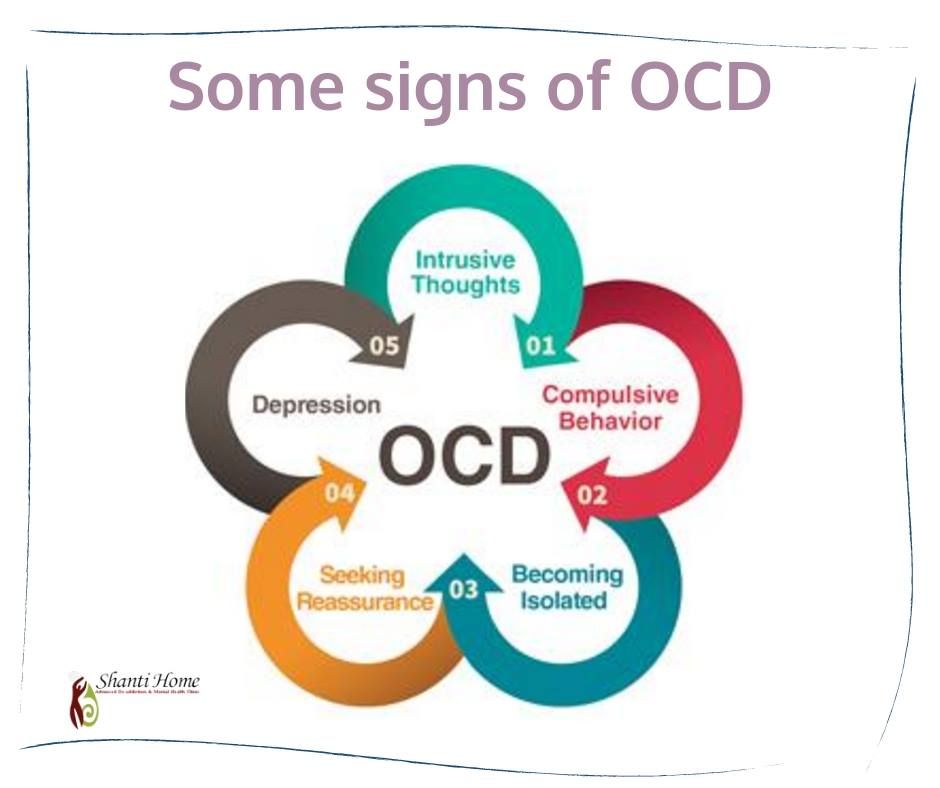
Compulsion - an irresistible need to perform certain actions (rituals), which can be assessed by the person himself as irrational or meaningless, and the internal need to perform them is forced and is the result of obsessive ideas.
Common examples of OCD manifestations
- An exaggerated sense of danger. Fear of the materiality of thoughts:
- "now I will lose control and hurt my loved ones"
- "something terrible is about to happen, I can feel it"
- "I shouldn't think like that, all this will come true because of me"
- Pathological fear of pollution. Thirst for Purity
- Excessive perfectionism, exaggerated responsibility - "everything must be done perfectly", "everything depends on me, mistakes are unacceptable"
How does this painful algorithm work?
Most people have unwanted or obsessive thoughts quite often, but all sufferers of the disorder greatly exaggerate their importance. Fear of one's own thoughts leads to attempts to neutralize the negative feelings that arise from obsessions, for example by avoiding thought-provoking situations or by engaging in "rituals" of excessive self-cleansing or prayer.
Fear of one's own thoughts leads to attempts to neutralize the negative feelings that arise from obsessions, for example by avoiding thought-provoking situations or by engaging in "rituals" of excessive self-cleansing or prayer.
As we noted earlier, repetitive avoidance behavior can "get stuck", "loop", that is, have a tendency to repeat. The cause of obsessive-compulsive disorder is the interpretation of intrusive thoughts as catastrophic and true.
If you periodically experience over the years:
- Constant or fluctuating anxiety
- The need to perform certain ritualized actions
- A persistent decline in the quality of life due to the need to avoid certain thoughts and actions, places and events
And you are also persecuted:
- Significant problems in studies and career
- Failure to establish a serious relationship
- Constant criticism and pressure from relatives
- Many senseless activities
- Excessive involvement in computer games and the Internet, alcohol
- Loneliness and isolation
We strongly recommend that you do not delay seeking help and that you complete a remedial program.
Consultations and psychotherapeutic sessions according to the program are held several times a week, until the relief of severe symptoms, then the frequency of meetings with specialists is reduced to 2–3 per month. Count on the fact that in the end we will deal with your problem together.
Treatment of obsessive-compulsive disorder in Neuro-Psi
Every day, the specialists of the NEURO-PSI clinic analyze the world practice in the field of psychiatry and psychotherapy. The goal is the impartial selection and implementation of those methods of treatment and psychological assistance, the effectiveness of which has been convincingly proven in independent studies.
We are guided by the principles of evidence-based medicine and use as a basic method of treatment a psychotherapeutic paradigm, the effectiveness of which has been widely recognized by the professional community.
1. What is the essence of the obsessive-compulsive disorder treatment program
Since obsessive thoughts, rituals and conditions are only symptoms of mental dysfunction, the root cause must be treated in order to achieve a stable result. A comprehensive work is carried out with the client, taking into account the main factors that create well-being.
A comprehensive work is carried out with the client, taking into account the main factors that create well-being.
The main emphasis is on teaching the client how to properly respond to his thoughts, emotions, inner feelings and interpretation of external events.
All types of psychotherapeutic and drug treatments serve the same goal: to achieve the best result in the shortest possible time. At the same time, by coordinating the efforts of specialists in various fields, the most complete coverage of all types of mental illnesses, disorders and disorders is possible.
2. What treatments are used
- Priority:
- Cognitive-Behavioral Therapy.
- Schema Therapy.
- Reality Therapy.
- Choice Theory.
- Rational pharmacotherapy.
- Psychopharmacotherapy (if indicated)
- Biofeedback Therapy
- Rational psychocorrection of stress
- Jacobson progressive muscle relaxation.
- Traditional and modern gymnastic systems, relaxation techniques.
- Breathing techniques .
- Stress exposure.
- Self-control training.
- Jacobson progressive muscle relaxation.
- Lifestyle modification
- Work with bad habits.
- Diet correction.
- Professional and social adaptation.
3. How is the treatment under the program
Each treatment program at the NEURO-PSI clinic consists of four stages:
- diagnostics,
- work with disease symptoms,
- work with the causes of the disease,
- consolidation of the achieved results.
Work efficiency is increased by dividing the treatment process into a predetermined number of sessions, at convenient times and without hospitalization. This means that each program is adapted to the problem that the client has addressed.
The treatment method is predictable, time-limited, productive, and most importantly, understandable for the client.
Of course, the treatment takes place in a comfortable mode without interruption from work, study or family. Improvements in well-being and mood (cure) occur in stages: after a decrease in emotional problems, bodily symptoms decrease. Working with the causes (etiology) of obsessive-compulsive disorder helps to avoid relapses in the future.
4. What are the results and forecast
Upon completion of the program, you get rid of obsessive thoughts and rituals, fear of pollution, unmotivated fears, panic attacks and multiple vegetative symptoms (sudden jumps in blood pressure, rapid heartbeat, dizziness, nausea).
According to statistics, the effectiveness of the methods used approaches 100% if all recommendations of specialists are followed.
Skills you acquire during the program:
- self-control and self-regulation
- constructive analysis of the state of the body
- understanding one's own mental and emotional sphere
- ability to control one's attention
- ability to act consciously in stressful situations
Significantly improves the emotional and physical condition, gains self-confidence, in the future. Emotional stress is removed, sleep and appetite are restored. The efficiency is greatly increased.
Emotional stress is removed, sleep and appetite are restored. The efficiency is greatly increased.
Specialists
- Rakhmanov Vladimir Alexandrovich
Psychiatrist, CBT-, ACT- and CFT-psychotherapist.
in the clinic online
Adults (over 18 years old) Elderly (from 60 years old)
Scientific approach. Horizon.
Founder and CEO of the Neuro-Psi network. Psychiatrist and psychotherapist.
As a psychiatrist, Vladimir works strictly in the evidence-based approach (Evidence-based Medicine). As a psychotherapist, he uses modern “rational” methods of psychotherapy (CBT, ACT, CFT, Scheme Therapy)
Vladimir is distinguished by a broad clinical outlook, professional awareness, and a comprehensive understanding of the patient's problem. These qualities are especially important in dealing with complex cases.

Vladimir specializes in working with the following client problems: professional burnout, depressed mood, excessive anxiety, despondency, indecision, regret about missed opportunities, intolerance for uncertainty, loss of meaning and direction in life. Chronic pain, psychosomatic and somatopsychic diseases. Isolation, avoidance of difficulties, loneliness. Does not work with suicidal behavior, addictions of any type, does not conduct outpatient appointments for patients who are hospitalized.
“Difficult tasks, whether it be a health problem or a life catastrophe, require not only perseverance in overcoming. Often a negative course of events changes the intellectual effort - making meaningful decisions based on objective data.
Read more
★9.81 based on 14 reviews
- Chibikova Evgenia Yurievna
Child psychiatrist, adult psychiatrist.
at the clinic online
Children (0-17 years old) Adults (18 to 60 years old)
Concentration.
 Care.
Care. Regularly trains and studies abroad. Thanks to this, he is able to prescribe effective, but at the same time the safest drugs.
Filigree in neurochemistry.
Read more
★9.71 based on 112 reviews
- Kuznetsov Sergey Olegovich
Psychologist. Cognitive behavioral psychotherapist. Family psychotherapist
in the clinic online
Teenagers (16 to 17 years old) Adults (18 to 60 years old)
Clarity. Impartiality.
Outline your problem and steps to fix it. Support on the path of real change. Shows the problem for what it is. Do not embellish and do not add something of their own. Demonstrates an alternative attitude in therapy so that you can live it from your own experience, and not theoretically.
Read more
★9.
 83 based on 52 reviews
83 based on 52 reviews - Dobrovidova Natalya Alexandrovna
Psychologist. Cognitive behavioral psychotherapist. PhD
in the clinic online
Adults (18 to 60 years old) Adolescents (from 14 to 17 years old)
Humanism. Environmental friendliness.
Will teach you how to manage your mental life. She is convinced that "our thoughts are the basis of our mental health and happiness", "and neurosis is a choice." It will help you make a choice in your favor. In fact, it forms a new way of thinking and new habits (which is so difficult to do without help and support). Such changes in the psyche lead to significant changes in life. He believes in every person and considers this the basis of quality therapy.
Read more
★9.64 based on 41 reviews
- Trofimova Marina Ivanovna
Cognitive Behavioral Psychotherapist.
 Sexologist.
Sexologist. in the clinic online
Adults (from 18 to 60 years old)
Non-judgmental. Result.
Can quickly and clearly show the connection between thoughts and emotions that affect life. Teaches you to overestimate the beliefs and attitudes that reduce the quality of life. Helps clients to move towards the goal step by step, respects the choice of the patient, gently and confidently accompanies along the way.
Read more
★9.43 based on 31 reviews
- Vyrikov Artur Igorevich
Clinical psychologist. ACT psychotherapist. Cognitive behavioral psychotherapist
in clinic online
Adults (18 to 55 years old)
Trust. Simplicity.
Creates a friendly atmosphere of understanding and ease, communicates in simple language.
 Easily finds common topics for conversation, tries on situations for himself and asks precise questions "in the case." Helps to quickly understand the essence of the problem and proceed to work on a solution. Works with setting values, finding priorities, and choosing an informed life path.
Easily finds common topics for conversation, tries on situations for himself and asks precise questions "in the case." Helps to quickly understand the essence of the problem and proceed to work on a solution. Works with setting values, finding priorities, and choosing an informed life path. Read more
★9.52 based on 82 reviews
- Yarygin Anton Igorevich
Adult psychiatrist.
in the clinic online
Adults (over 18 years old) Elderly (over 60)
Confidence. Efficiency.
First class and highly organized specialist.
Anton is maximally focused on the healing process. Able to quickly evaluate incoming information, make objective and accurate decisions. Works with full dedication, passionate about the work process.
Competently arranges treatment and brings the case to a positive result.
Read more
★9.27 based on 37 reviews
- Shlyapnikov Sergei Anatolievich
Psychiatrist.
in the clinic online
Adults (18-60) Elderly (from 60 years old) Adolescents (16 to 17 years old)
Perseverance. Result.
Strengths. An incredibly empathetic psychiatrist who works effectively with patients of all ages. He specializes in working with anxiety, panic, depression, obsessions and, in general, working with neurotic disorders.
“I am convinced that psychiatry is one of the most interesting branches of medicine. Seeing the patient feel better is priceless.”
Able to smooth out sharp corners in a humorous way. Sense of humor.
More details
★8.
 23 based on 13 reviews
23 based on 13 reviews
Treatment of obsessive-compulsive disorder
Treatment of obsessive-compulsive disorder. We will relieve you of obsessive thoughts, movements and rituals. Let's get back to life!
Symptoms of obsessive-compulsive disorder
- Frightening images and drives
- Compulsive acts (rituals)
- Intrusive check of one's own actions
- Fear of trouble, pollution or contamination
- Inexplicable desire to count something
- Excessive organization and pedantry
- Perfectionism in relationships, work and even leisure
- "Stuck", "looping" on one's thoughts
You feel that over time your mood becomes worse: apathy, depression, obsessions increase, and rituals begin to fill all your free time or harm your physical health.
You may have had more than one meeting with psychologists, psychotherapists and psychiatrists. You are not given the "scary" psychiatric diagnoses of Schizophrenia or Bipolar Disorder, but are prescribed medication and psychotherapy nonetheless.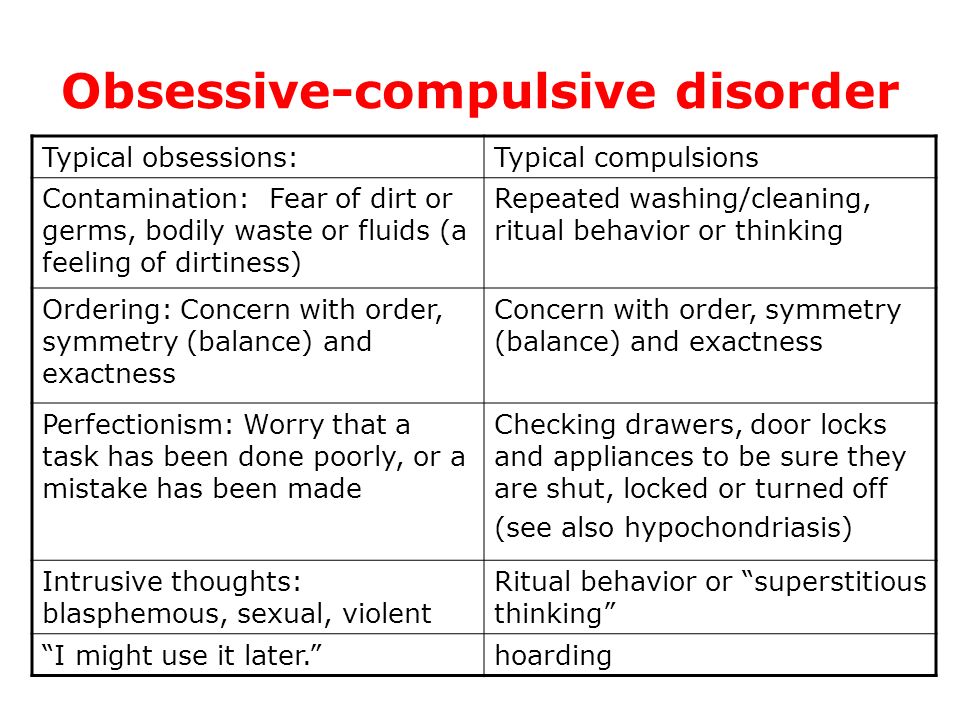 However, such treatment cannot be called effective - the symptoms persist and only aggressive pharmacotherapy temporarily reduces anxiety.
However, such treatment cannot be called effective - the symptoms persist and only aggressive pharmacotherapy temporarily reduces anxiety.
What is obsessive-compulsive disorder?
Obsessive-compulsive disorder is a syndrome characterized by the presence of obsessive thoughts (obsessions) to which a person reacts with certain actions (compulsions). The causes of the disorder are rarely superficial. The syndrome is also accompanied by the development of obsessive memories and various pathological phobias. May be chronic, episodic or progressive.
Obsession - obsessive thought, persistent desire for something, uncontrollable and accompanied by anxiety and intense anxiety. In an attempt to cope with such thoughts, a person resorts to committing compulsions.
Compulsion - an irresistible need to perform certain actions (rituals), which can be assessed by the person himself as irrational or meaningless, and the internal need to perform them is forced and is the result of obsessive ideas.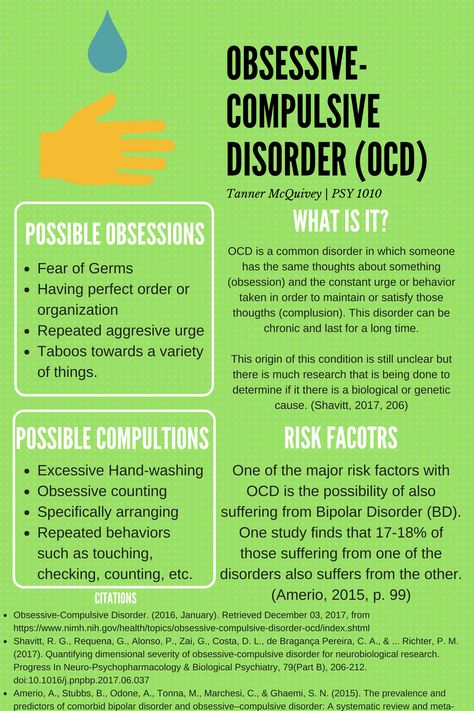
Common examples of OCD manifestations
- An exaggerated sense of danger. Fear of the materiality of thoughts:
- "now I will lose control and hurt my loved ones"
- "something terrible is about to happen, I can feel it"
- "I shouldn't think like that, all this will come true because of me"
- Pathological fear of pollution. Thirst for Purity
- Excessive perfectionism, exaggerated responsibility - "everything must be done perfectly", "everything depends on me, mistakes are unacceptable"
How does this painful algorithm work?
Most people have unwanted or obsessive thoughts quite often, but all sufferers of the disorder greatly exaggerate their importance. Fear of one's own thoughts leads to attempts to neutralize the negative feelings that arise from obsessions, for example by avoiding thought-provoking situations or by engaging in "rituals" of excessive self-cleansing or prayer.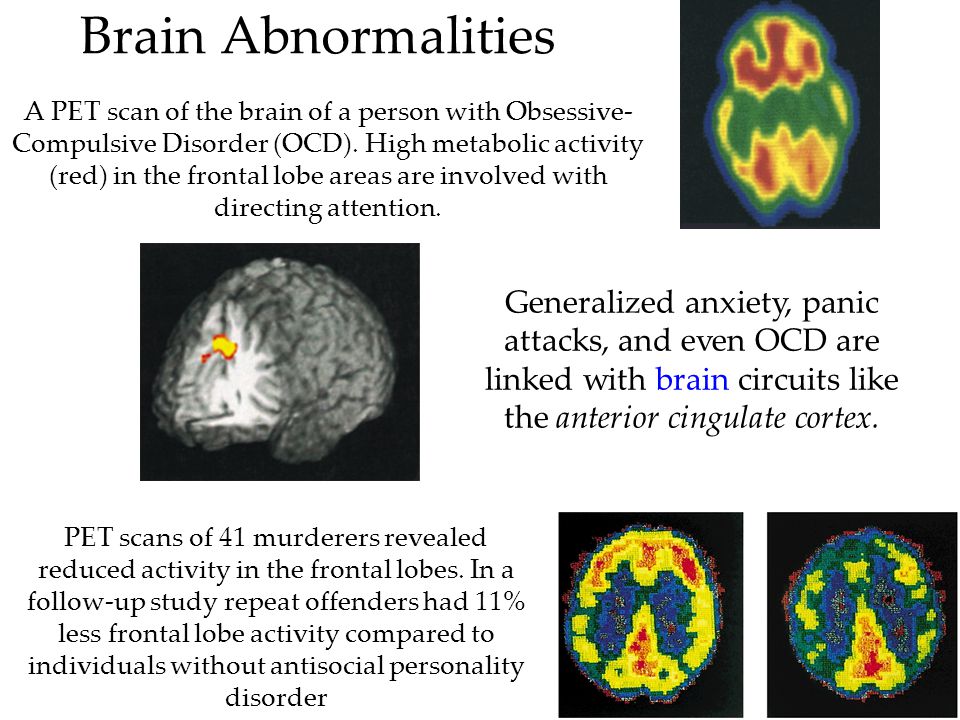
As we noted earlier, repetitive avoidance behavior can "get stuck", "loop", that is, have a tendency to repeat. The cause of obsessive-compulsive disorder is the interpretation of intrusive thoughts as catastrophic and true.
If you periodically experience over the years:
- Constant or fluctuating anxiety
- The need to perform certain ritualized actions
- A persistent decline in the quality of life due to the need to avoid certain thoughts and actions, places and events
And you are also persecuted:
- Significant problems in studies and career
- Failure to establish a serious relationship
- Constant criticism and pressure from relatives
- Many senseless activities
- Excessive involvement in computer games and the Internet, alcohol
- Loneliness and isolation
We strongly recommend that you do not delay seeking help and that you complete a remedial program.
Consultations and psychotherapeutic sessions according to the program are held several times a week, until the relief of severe symptoms, then the frequency of meetings with specialists is reduced to 2–3 per month. Count on the fact that in the end we will deal with your problem together.
Treatment of obsessive-compulsive disorder in Neuro-Psi
Every day, the specialists of the NEURO-PSI clinic analyze the world practice in the field of psychiatry and psychotherapy. The goal is the impartial selection and implementation of those methods of treatment and psychological assistance, the effectiveness of which has been convincingly proven in independent studies.
We are guided by the principles of evidence-based medicine and use as a basic method of treatment a psychotherapeutic paradigm, the effectiveness of which has been widely recognized by the professional community.
1. What is the essence of the obsessive-compulsive disorder treatment program
Since obsessive thoughts, rituals and conditions are only symptoms of mental dysfunction, the root cause must be treated in order to achieve a stable result. A comprehensive work is carried out with the client, taking into account the main factors that create well-being.
A comprehensive work is carried out with the client, taking into account the main factors that create well-being.
The main emphasis is on teaching the client how to properly respond to his thoughts, emotions, inner feelings and interpretation of external events.
All types of psychotherapeutic and drug treatments serve the same goal: to achieve the best result in the shortest possible time. At the same time, by coordinating the efforts of specialists in various fields, the most complete coverage of all types of mental illnesses, disorders and disorders is possible.
2. What treatments are used
- Priority:
- Cognitive-Behavioral Therapy.
- Schema Therapy.
- Reality Therapy.
- Choice Theory.
- Rational pharmacotherapy.
- Psychopharmacotherapy (if indicated)
- Biofeedback Therapy
- Rational psychocorrection of stress
- Jacobson progressive muscle relaxation.

- Traditional and modern gymnastic systems, relaxation techniques.
- Breathing techniques .
- Stress exposure.
- Self-control training.
- Jacobson progressive muscle relaxation.
- Lifestyle modification
- Work with bad habits.
- Diet correction.
- Professional and social adaptation.
3. How is the treatment under the program
Each treatment program at the NEURO-PSI clinic consists of four stages:
- diagnostics,
- work with disease symptoms,
- work with the causes of the disease,
- consolidation of the achieved results.
Work efficiency is increased by dividing the treatment process into a predetermined number of sessions, at convenient times and without hospitalization. This means that each program is adapted to the problem that the client has addressed.
The treatment method is predictable, time-limited, productive, and most importantly, understandable for the client.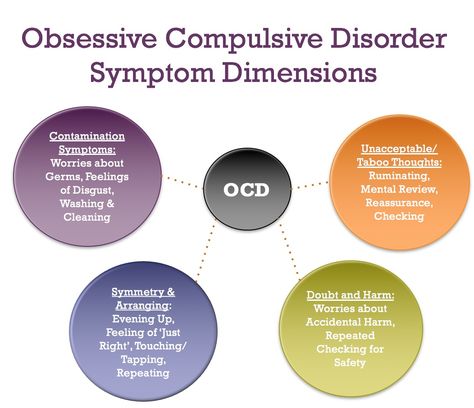
Of course, the treatment takes place in a comfortable mode without interruption from work, study or family. Improvements in well-being and mood (cure) occur in stages: after a decrease in emotional problems, bodily symptoms decrease. Working with the causes (etiology) of obsessive-compulsive disorder helps to avoid relapses in the future.
4. What are the results and forecast
Upon completion of the program, you get rid of obsessive thoughts and rituals, fear of pollution, unmotivated fears, panic attacks and multiple vegetative symptoms (sudden jumps in blood pressure, rapid heartbeat, dizziness, nausea).
According to statistics, the effectiveness of the methods used approaches 100% if all recommendations of specialists are followed.
Skills you acquire during the program:
- self-control and self-regulation
- constructive analysis of the state of the body
- understanding one's own mental and emotional sphere
- ability to control one's attention
- ability to act consciously in stressful situations
Significantly improves the emotional and physical condition, gains self-confidence, in the future.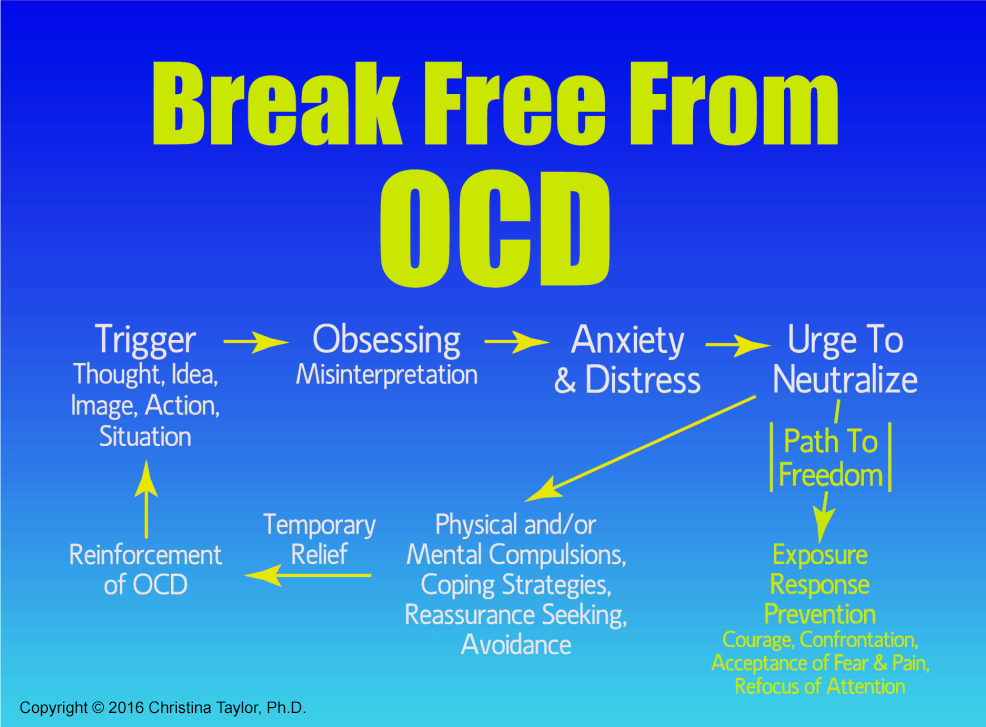 Emotional stress is removed, sleep and appetite are restored. The efficiency is greatly increased.
Emotional stress is removed, sleep and appetite are restored. The efficiency is greatly increased.
Specialists
- Ruzanov Leonid Timofeevich
Head of the Moscow branch. Cognitive behavioral psychotherapist. Family psychotherapist
in the clinic online
Adults (18 to 55 years old)
Energy. Optimism.
Leading specialist of the clinic. It will help to cope where it seemed impossible. Changes the thinking pattern from self-critical to supportive. It teaches you to treat yourself with deep compassion and sincere sympathy, which gives an experience of acceptance (the absence of which, very often, is the root of the problem). A master of generating insights and understanding in clients.
Read more
★9.79 based on 46 reviews
- Pantsov Oleg Vyacheslavovich
Psychologist.
 Family psychotherapist. Child-parent psychologist. Adolescent psychologist
Family psychotherapist. Child-parent psychologist. Adolescent psychologist Online only
Adults (18+) Teenagers (from 14 to 17 years old)
Harmony. Professionalism.
Online reception only.
A holistic specialist who owns the most modern techniques of family psychotherapy. He knows how to look at the situation from different points of view and find the best solution.
Will teach you how to build a dialogue with your partner and with yourself in a new way. Comprehensive approach to overcoming individual and family crises. He adheres to a systematic approach in his work, which combines a clear structure with a careful and attentive attitude.
Read more
★9.76 based on 43 reviews
- Trushkina (Savostina) Anastasia Dmitrievna
Psychologist, Cognitive behavioral therapist, EMDR psychologist.
Online only
Adults (18+) Adolescents (14 to 17 years old)
Flexibility.
 Result.
Result. Online reception only.
Adheres to evidence-based therapies only. It will help to correctly identify the causes of problems and outline a plan for solving them in a short time. Builds partner-equal relationships with clients, accepts and treats each client without judgment. Has her experience of continuous personal therapy for five years.
Read more
★9.89 based on 34 reviews
- Kortunova Irina Alexandrovna
Systemic family psychotherapist, Child-parent psychologist, Emotionally focused therapist, Emdr-psychologist
in clinic online
Adults (18 to 60 years old) Adolescents (11 to 17 years old)
Support. Creation.
Will help to overcome family crises, establish mutual understanding in a couple, cope with naughty children.
 Hear each family member and teach to hear each other. He will give clear recommendations and help you find new working strategies to solve difficult situations.
Hear each family member and teach to hear each other. He will give clear recommendations and help you find new working strategies to solve difficult situations. Believes that each person can do much more than he does, and even more than he thinks. It will help to reveal one's potential, removing fears, fears, anxieties. He knows how to create a warm, trusting atmosphere at the session, he feels the client subtly.
Read more
★9.69 based on 14 reviews
- Strepetova Olesya Vladimirovna
Psychologist, Systemic Family Therapist, Emotionally Focused Therapist, Emdr Psychologist.
in the clinic online
Teenagers (14 to 17 years old) Adults (18 to 50 years old)
Acceptance. Rationality.
Professional and understanding psychologist, sensitive to the individual characteristics of clients, their needs and difficulties.
 He will find a special approach to everyone, he knows various techniques of systemic therapy: short-term strategic therapy, ORCT, EFT, etc., as well as techniques for working with trauma.
He will find a special approach to everyone, he knows various techniques of systemic therapy: short-term strategic therapy, ORCT, EFT, etc., as well as techniques for working with trauma. Will provide support on personal and family issues, help to overcome the crisis in a couple's relationship, cope with difficult situations and get out of them in a resourceful state. I am convinced that the quality of our life directly depends on how we live it “here and now”.
Read more
★9.57 based on 12 reviews
- Sotskaya Gulnara Mizkhatovna
Adolescent Psychologist, Child-Parent Psychologist, Child Psychologist, Neuropsychologist, CBT Therapist.
in the clinic online
Adults (19 to 30 years old) Children (from 2 to 17 years old)
Acceptance.
 Support.
Support. Professional in expert diagnostics and psycho-correctional work with children and adolescents with various disorders (ADHD, ADHD and ADD), emotional disorders, peer problems and crisis conditions.
Competently solves the problems of child-parent relationships: skillfully selects the "key" to the child and teaches parents to use this "key". Conducts EPI (Experimental Psychological Research).
More
★9.98 based on 7 reviews
- Samarina Olga Evgenievna
Child psychiatrist
Clinic only
Children (0-15 years old)
Peace of mind. Confidence.
Olga is a young and competent child psychiatrist. Like most modern doctors working in a scientific-evidence-based approach, Olga continuously studies foreign sources and literature, knows how to find an approach to each little patient. Olga does not work with adults.
Interested in the profession and has an endless love for children.
Learn more