Ocd fear of disease
Health Concern OCD - Symptoms and Treatment
What is Health Concern OCD?
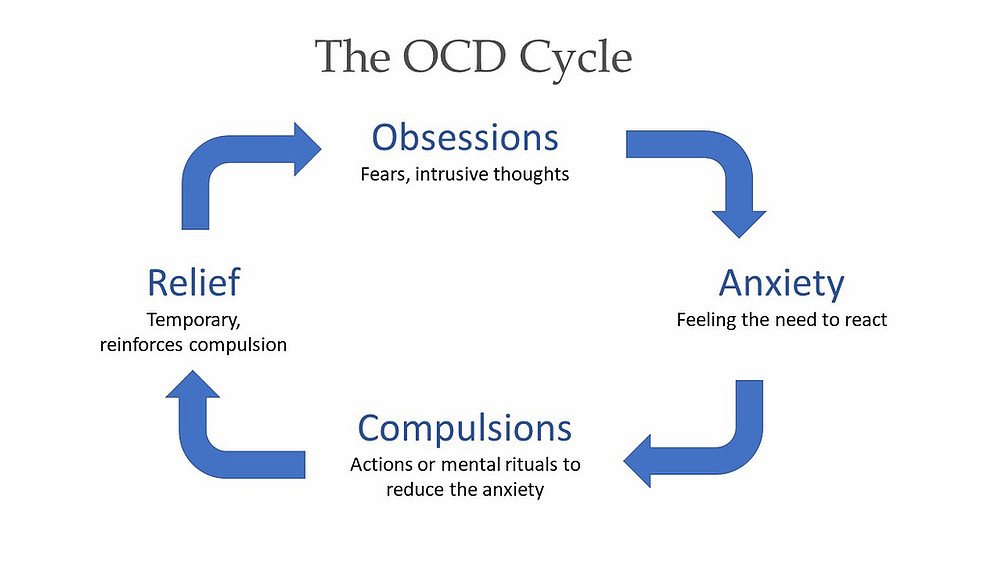
Health Concern Obsessive-Compulsive Disorder is a sub-type of OCD that causes a person to have obsessive thoughts about developing a serious medical condition. The intrusive thoughts that a person with Health Concern OCD experiences are irrational and exaggerated, which create the need to perform compulsions to cope.
Common Symptoms of Health Concern OCD
Typical symptoms of Health Concern OCD are related to obsessions about contracting a life-threatening medical condition. Individuals suffering from Health Concern OCD will ruminate and worry about this fear to an unreasonable and illogical degree. These individuals are also known to seek medical help and get repeated opinions even after receiving conclusive testing. This sub-type of OCD continues to leave doubt and uncertainty about health Concern and illness.
Common Obsessions of Health Concern OCD
The symptoms of Health Concern OCD can vary from person to person but has a theme of health anxiety focused on the fear of getting a disease or developing a dreaded medical condition.
Some example of common obsessions a person may experience with Health Concern OCD include:
- Fear of getting HIV, cancer, or any other life-threatening medical condition
- Obsessing over physical sensations and what kind of medical condition they may related to
- Fears of having brain tumor
- Fear of pneumonia or lung cancer
- Fear of an STD
- Fear of having a heart attack if they feel pain in their left arm or chest
- Fear their appendix is bursting if they have an abdominal cramp
Common Compulsions of Health Concern OCD
Obsessions related to Health Concern OCD can cause varying compulsive behaviors within different people suffering from this type of OCD.
Some common compulsions that are experienced with Health Concern OCD include the following:
- Multiple visits to their doctor’s office or “doctor hopping”
- Repeatedly examining themselves for symptoms
- Creating a habit of looking up their symptoms online
- Repeatedly seeking more advanced testing
- Getting multiple medical examinations for one of their alleged conditions
- Avoiding people, objects, or situations where they may by exposed to diseases
The constant fear of having a serious health condition can cause a person to spend most of their day in a doctor’s office.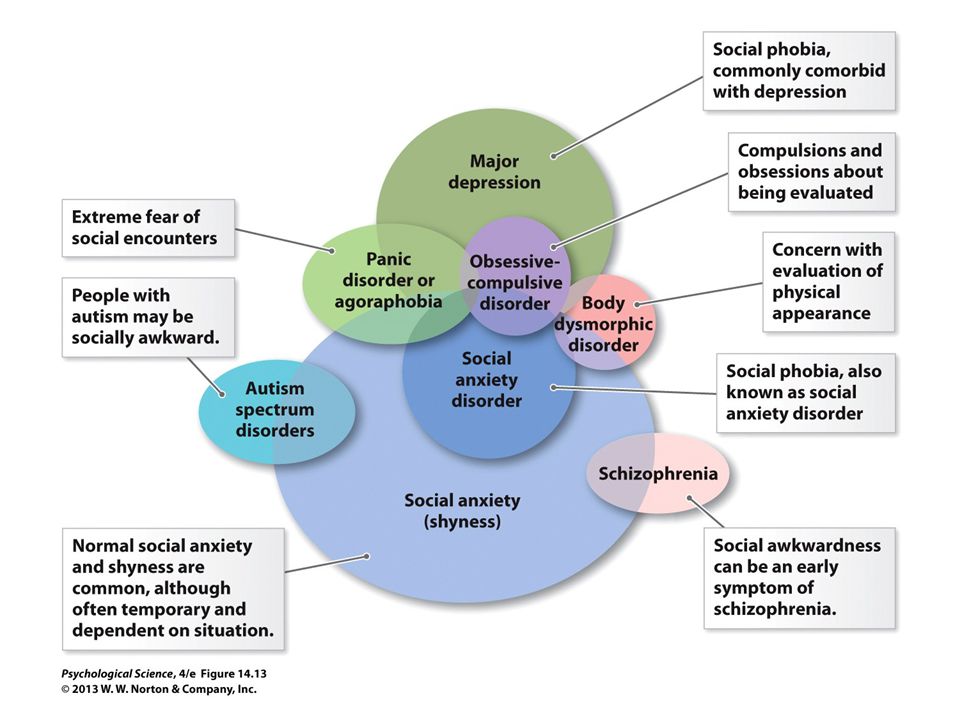 A person with Health Concern OCD is not able to live their lives without thinking they could be terminally ill. Luckily, they are not seriously ill but rather only suffering from this form of OCD.
A person with Health Concern OCD is not able to live their lives without thinking they could be terminally ill. Luckily, they are not seriously ill but rather only suffering from this form of OCD.
Treatment for Health Concern OCD
People suffering from Health Concern OCD are encouraged to seek treatment from a mental health treatment provider that specializes in the treatment of OCD. OCD specialists are equipped and prepared to treat a wide array of OCD subtypes, including Health Concern OCD. Like all types of OCD, Health Concern OCD can be treated with Cognitive-Behavioral Therapy (CBT), specifically with treatment approaches called Exposure with Response Prevention (ERP), and Mindfulness-Based Cognitive-Behavioral Therapy.
Mindful-Based CBT teaches patients that everyone experiences intrusive thoughts. Individuals will also learn that intrusive thoughts have no power over them and that by responding to their thoughts through compulsive behaviors, their thoughts are given more strength and credibility and their fears and obsessions are strengthened and reinforced. Mindfulness-Based CBT is a very effective OCD treatment, especially when combined with ERP.
Mindfulness-Based CBT is a very effective OCD treatment, especially when combined with ERP.
ERP exposes patients to situations related to their intrusive thoughts that cause them anxiety. The goal of this treatment is for the patient to prevent himself or herself from completing their compulsive behaviors when triggered by intrusive thoughts. The situations that are confronted will intensify over time, until the patient can face and overcome their most feared scenario. Once they are able to stop themselves from responding to their intrusive thoughts with compulsive behaviors, they can experience tremendous relief from the symptoms of OCD.
If patients are suffering from severe levels of anxiety due to their OCD, they may benefit from participating in treatment at an Intensive Outpatient (IOP) OCD treatment program, as is offered by The Gateway Institute. The Gateway Institute offers Intensive Outpatient treatment options as well as regular outpatient psychotherapy sessions, and a free, 30 minute face-to-face consultation with one of our experienced and caring clinicians at all three of our beautiful locations in Orange County, Scottsdale, Arizona, and the San Francisco Bay Area. OCD symptoms typically worsen over time and can take over a person’s life, so it is very important to seek OCD treatment as soon as possible with a skilled and dedicated OCD specialist who can provide expertise and support during this journey.
OCD symptoms typically worsen over time and can take over a person’s life, so it is very important to seek OCD treatment as soon as possible with a skilled and dedicated OCD specialist who can provide expertise and support during this journey.
Other Common Sub-Types Of OCD
It is not uncommon for an individual suffering from one OCD sub-type to also suffer from other sub-types. Treating co-occurring sub-types simultaneously is important in finding balance and healing from OCD.
Contamination OCD
Harm OCD
Homosexual (HOCD)
Pure O (Pure Obsessional OCD)
Relationship OCD
Sexual OCD
The Gateway Institute is here to support you in getting the help that you need.
Our Orange County, California, Gateway location is proud to provide anxiety treatment for the cities of Costa Mesa, Fountain Valley, Santa Ana, Garden Grove, Huntington Beach, Newport Beach, Laguna Beach, Fullerton, Irvine, Aliso Viejo, Cypress, Buena Park, Brea, Lake Forest, Tustin, Westminster, Orange and Anaheim.
Our San Francisco Bay Area, California, Gateway location is proud to provide anxiety treatment for the cities of San Francisco, Oakland, Berkeley, Almeda, San Jose, Palo Alto, Fremont, Santa Rosa, Hayward, Sunnyvale, Concord, Santa Clara, Antioch, Richmond, and Fairfield.
Our Maricopa County, Arizona, Gateway location is proud to provide anxiety treatment for the cities of Phoenix, Scottsdale, Glendale, Tempe, Gilbert, Queen Creek, Sun Lakes, Mesa, Chandler, Paradise Valley, Surprise, Cave Creek, Carefree, Fountain Hills, Buckeye, Mesa, Peoria, Sun City, Goodyear, and El Mirage.
Shedding Light on Health Anxiety OCD
Currently you may only know the suffering associated with Health Anxiety OCD, but through the right treatment, there is hope of learning to appreciate the way your mind works.
One of the things I find most heartbreaking about working with some of my OCD clients is that the disorder has ripped from them that which they treasure most and in turn engendered the very life they fear.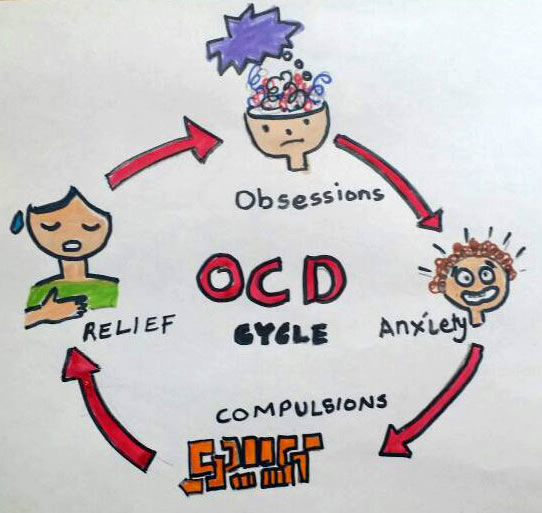 In other words, it makes you become what you fear, just not in the way you’d expect. Those with Harm OCD may fear being rejected after hurting someone, but then they isolate themselves from their families. Those with Pedophile OCD may give up being a parent so there is no chance they will molest their child, but then they live a life not feeling safe around children. Those with Health Anxiety OCD may worry that unidentified or untreated illness will rob them of a fulfilling life, but then they miss out on enjoying the life they always dreamed about having by devoting all their attention to trying to be sure they are not ill. Regardless of the form OCD takes, OCD is the dictator who declares the lengths that must be followed to obtain 100 percent certainty and just as you begin to think you’ve appeased him… the dictator changes the rules.
In other words, it makes you become what you fear, just not in the way you’d expect. Those with Harm OCD may fear being rejected after hurting someone, but then they isolate themselves from their families. Those with Pedophile OCD may give up being a parent so there is no chance they will molest their child, but then they live a life not feeling safe around children. Those with Health Anxiety OCD may worry that unidentified or untreated illness will rob them of a fulfilling life, but then they miss out on enjoying the life they always dreamed about having by devoting all their attention to trying to be sure they are not ill. Regardless of the form OCD takes, OCD is the dictator who declares the lengths that must be followed to obtain 100 percent certainty and just as you begin to think you’ve appeased him… the dictator changes the rules.
Understanding Health Anxiety OCD
Regardless of whether we call it Health Anxiety OCD, Hypochondriasis, Illness Anxiety Disorder, or Somatic Symptom Disorder, this content area is often misunderstood both in the medical profession and the mental health field.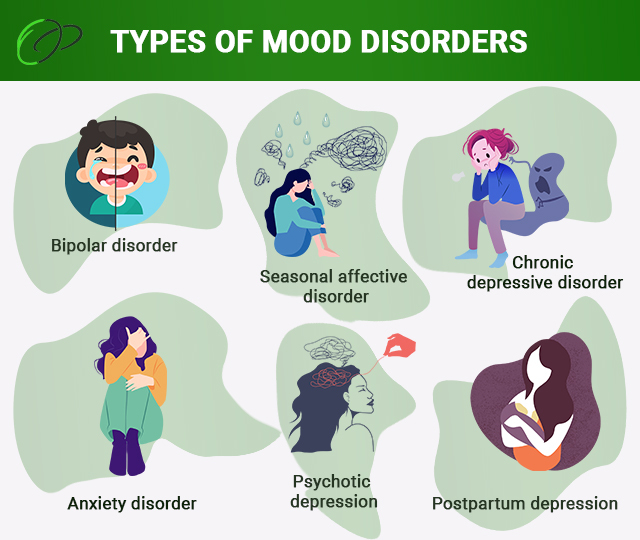 Some of the confusion arises from failing to understand that the diagnosis refers to a person that is chronically anxious about their health, not about whether they are actually sick or not. The fact is, one can be sick and have Health Anxiety OCD.
Some of the confusion arises from failing to understand that the diagnosis refers to a person that is chronically anxious about their health, not about whether they are actually sick or not. The fact is, one can be sick and have Health Anxiety OCD.
As with all content areas of OCD, the real problem is not the content of the obsession, but the process of how you relate to and respond to it. Specifically, the problem is believing that you have to do compulsions in the effort to obtain certainty your fear is untrue. These failed efforts to be certain about one’s health ultimately lead to feeling less certain and more afraid. This being said, the content of all OCD sufferers’ obsessive thoughts always feels and seems important, and this sense of urgency about it distracts from recognizing the process problem. Living with Health Anxiety OCD can feel like you are living on borrowed time, which makes it nearly impossible to enjoy anything. Instead you feel driven to escape what could be a potential death sentence or avert some other tragic misfortune.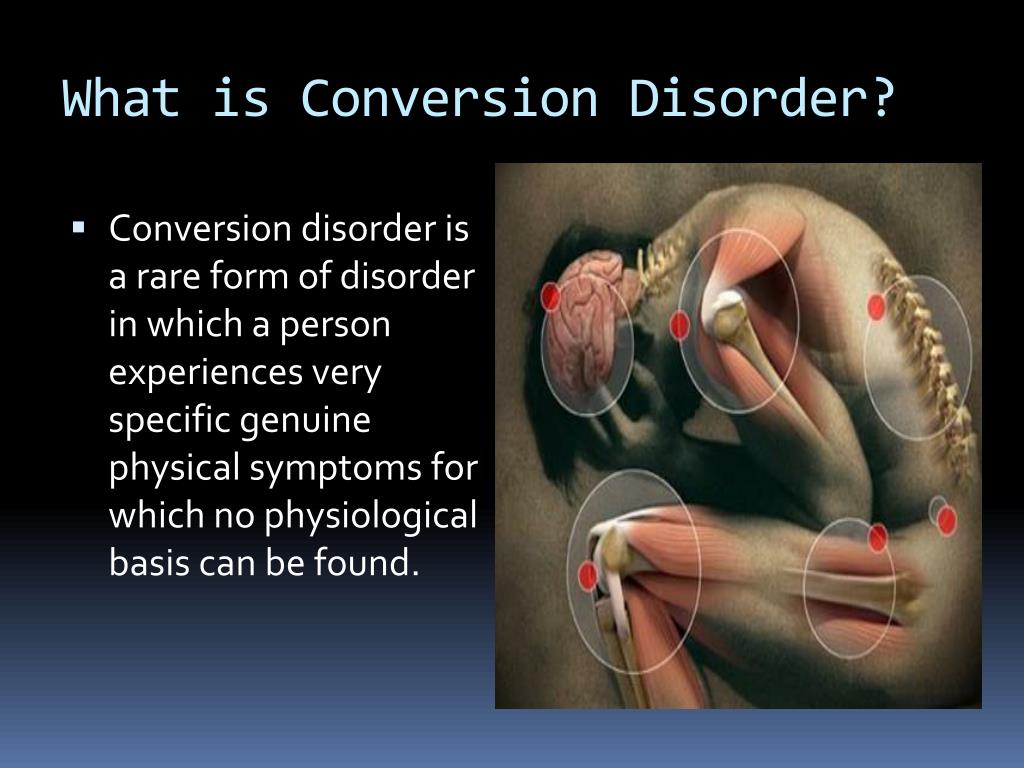 What’s worse, it feels like you alone are responsible for carrying out this mission.
What’s worse, it feels like you alone are responsible for carrying out this mission.
I remember as a child asking my mom what she was always so afraid of, and she said that she was afraid that she would be sick, and that it would be her fault for not being vigilant about watching for signs and symptoms. The look on her face was one of terror and bewilderment as she told me how unbearable it would be to find out she’s sick and to know that it would be all her fault for not having caught it sooner. As a child this made no sense to me but now, as an adult who has lived with OCD (and now specializes in the treatment of OCD) I understand that the terror and fear she felt was real. Her “fight or flight” system had signaled an emergency which she did not know was a false alarm. My mother was afraid of being sick, and everything that comes with being sick, but what really tormented her was the thought that she would be responsible for getting sick due to her failure to have checked enough.
Feared Consequences in Health Anxiety OCD
Feared consequences typically associated with Health Anxiety OCD include fear of dying or suffering from an illness of course, but also fear of permanent suffering, both mentally and physically, fear of abandoning your family because you didn’t take care of yourself, fear of never getting an accurate diagnosis and never finding treatment for your symptoms (real or imagined). This often includes intense pressure not only to figure out what is wrong with you, but also to be sure you are receiving the “right” treatment, for which you also take full responsibility. It is important to recognize when hyper-responsibility is playing a role in your health anxiety, so it can be targeted effectively during treatment.
What Health Anxiety OCD Makes You Feel Responsible For
Here are some ways OCD uses the fear of being irresponsible to keep you stuck in health anxiety.
Responsibility for seeking a diagnosis
- What if I am ill but no one can figure it out because there isn’t a name for it?
- What if this doctor read the results of the tests wrong?
- How do I know that I am not developing an illness that has not been detected?
- What if my failure to find an answer leads to endless suffering due to my awareness of symptoms
Responsibility for being vigilant about monitoring symptoms
- What if this sensation or symptom is a sign of cancer or a chronic illness?
- If I don’t check for signs of illness it could end up being my fault for not checking.

Responsibility for avoiding the potential of contracting an illness
- What if I should not have allowed myself to be around someone who appeared ill?
- What if I have not paid close enough attention to something that could have gotten me ill?
Responsibility for inadvertently causing harm
- What if I have an undetected illness and get someone else sick?
- What if I am currently sick or get sick due to my own lack of vigilance?
Responsibility for reporting symptoms and sensations
- What if I fail to describe my symptoms accurately which results in the wrong diagnosis?
- What if I fail to recognize changes in my symptoms?
Common Compulsions in Health Anxiety OCD
It can be easy to miss when apparent efforts to responsibly take care of your health are actually compulsions that fuel your obsessive thinking. Here are some things to look out for:
- Asking friends or family to examine you for signs of illness
- Repeated visits to multiple doctors
- Requests for unnecessary (and/or repeated) tests
- Excessively checking your own body to look for new symptoms or changes in symptoms
- Reassurance seeking from multiple sources (professional and non-professional)
- Self-reassurance by reviewing behavior to make sure the right precautions were taken or repeating comforting advice already given
- Excessive visits to the Emergency Room
- Avoiding places where one might be exposed to germs or sick people (malls, doctor’s offices, grocery stores, etc.
 )
) - Avoiding objects imagined to cause illness (standing in front of the microwave, holding phone to one’s ear, anything sharp, anything with certain chemicals, etc.)
- Neutralizing bad “sick thoughts” with good “healthy thoughts
The Google Problem
When I was a kid (yes, back then we used encyclopedias) whenever someone was anxious about a potential health concern we went to the bookshelf and consulted a very large medical book. While looking for reassurance from a medical book was still a compulsion which resulted in finding new possibilities and new questions, there was a limit to what information you would find. Plus, it took a fair amount of effort.
Today we have Google, a limitless source of information which can all be obtained with a click. For those with Health Anxiety OCD, Google is often a source of great misery and suffering. It starts with OCD selling you the lie that you could have your answer if you just looked up this one thing and then you could put it aside and carry on with the rest of your day (wouldn’t that be glorious?). However, it never works out this way because with Health Anxiety OCD, Googling itself is a reassurance seeking compulsion which maintains the cycle of OCD. It does this by reinforcing the idea to your brain that not only is your health in question but that you better do something about it fast.
However, it never works out this way because with Health Anxiety OCD, Googling itself is a reassurance seeking compulsion which maintains the cycle of OCD. It does this by reinforcing the idea to your brain that not only is your health in question but that you better do something about it fast.
This is partly what makes Google so problematic because it offers health anxiety sufferers a promise of immediate answers and it never says “No, you have had enough, stop googling”. It feeds you possibility after possibility, mostly negative, which serves to keep you terrified, desperate and even more convinced than before that you are probably very ill. Unlike other addictions where there is an opportunity to pause prior to running out to make a purchase, Google is immediately and readily available at your fingertips. Googling is a common compulsion in many forms of OCD and is usually one of the first compulsions I work with my clients to reduce.
Case Examples
Debbie is a 27-year-old female who initially presented to her doctor with vaginal burning and was concerned she might have an infection! Debbie’s pap smear came back normal and she tested negative for any urinary tract bacterial infections.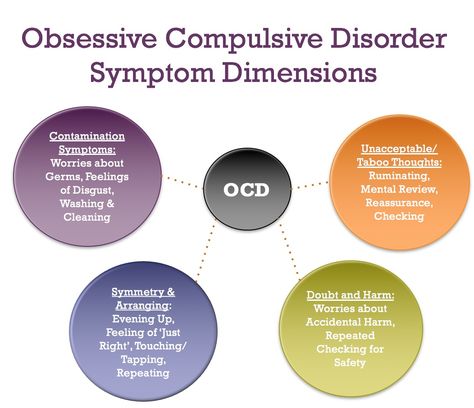 Debbie went home and was fine until she began to feel what seemed like the same sensation of burning she had 2 weeks prior. Debbie became fearful that maybe now she had an infection. Debbie returned to the doctor who again stated that Debbie did not have an infection and maybe she needed to drink more water. This went on for many months. Debbie began to go to different doctors due to feeling embarrassed about going back to the same doctor a second or third time. Debbie was constantly aware of the sensation of burning that seemed to get worse day by day. Debbie was plagued by the following thoughts: What if I have these symptoms forever? What if there is something wrong and nobody can figure it out? What if I have an STD that has been dormant for all these years? Debbie started to Google STD’s and began to worry that maybe she had undiagnosed HPV which could result in cervical cancer. Debbie began to wonder whether she had used protection with every sexual encounter. She began to Google information about how to know if you have HPV which only led her to more questions.
Debbie went home and was fine until she began to feel what seemed like the same sensation of burning she had 2 weeks prior. Debbie became fearful that maybe now she had an infection. Debbie returned to the doctor who again stated that Debbie did not have an infection and maybe she needed to drink more water. This went on for many months. Debbie began to go to different doctors due to feeling embarrassed about going back to the same doctor a second or third time. Debbie was constantly aware of the sensation of burning that seemed to get worse day by day. Debbie was plagued by the following thoughts: What if I have these symptoms forever? What if there is something wrong and nobody can figure it out? What if I have an STD that has been dormant for all these years? Debbie started to Google STD’s and began to worry that maybe she had undiagnosed HPV which could result in cervical cancer. Debbie began to wonder whether she had used protection with every sexual encounter. She began to Google information about how to know if you have HPV which only led her to more questions. She also examined herself daily to look for irritation or signs of an infection. Debbie knew she had OCD but this time her OCD had her focused on the (real) sensations that might indicate an illness instead of the familiar intolerance of uncertainty and discomfort.
She also examined herself daily to look for irritation or signs of an infection. Debbie knew she had OCD but this time her OCD had her focused on the (real) sensations that might indicate an illness instead of the familiar intolerance of uncertainty and discomfort.
Mark is a 52-year-old male who is preoccupied with several moles on his body. Mark has a family history of skin cancer. Mark was diligent with checking the moles on his body to make sure there weren’t any changes in shapes or sizes that could be a sign of melanoma. Every day after showering he would look over the moles before getting dressed. One day he had the thought “how will I know that it didn’t change, and I just didn’t notice” and “what if I have melanoma and it is my fault for not doing a better job of monitoring my body?” The more Mark looked at the moles the more confused he became and wondered what should a mole look like? Mark innocently looked on the internet searching “what does a healthy mole look like”? Mark was immediately bombarded with images of healthy and unhealthy moles. Mark began to frequent the doctor’s office and his dermatologist’s. Both doctors said Mark was fine, but as soon as he left the office he would be plagued by the thought “maybe he didn’t see the one I was talking about.” Mark stared at the moles to look for inconsistencies in shape and color and frequently asked his wife to examine his moles. He began to remember all those summer days in his teens where he had chosen not to wear sunscreen despite his mother’s warnings. Mark’s OCD had him focused on the belief that he was being responsible to monitor changes in his skin when in fact he was on a never-ending quest for certainty driven by an over-inflated sense of responsibility.
Mark began to frequent the doctor’s office and his dermatologist’s. Both doctors said Mark was fine, but as soon as he left the office he would be plagued by the thought “maybe he didn’t see the one I was talking about.” Mark stared at the moles to look for inconsistencies in shape and color and frequently asked his wife to examine his moles. He began to remember all those summer days in his teens where he had chosen not to wear sunscreen despite his mother’s warnings. Mark’s OCD had him focused on the belief that he was being responsible to monitor changes in his skin when in fact he was on a never-ending quest for certainty driven by an over-inflated sense of responsibility.
Inaccurate Beliefs Driving Health Anxiety
In treating any form of OCD, it is important to identify unhelpful ways of framing experiences that drive your belief system and perpetuate you engaging in compulsions. To assist with this process, I often like to talk about fun house mirrors and ask my clients what their experiences have been when looking at their reflection.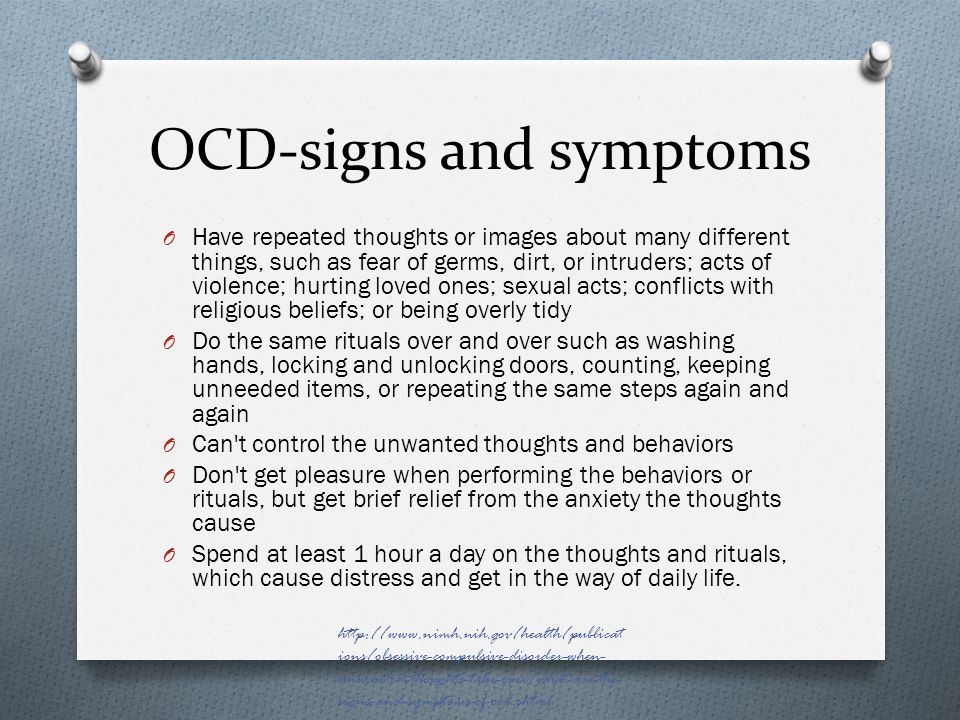 Most of the time they respond by saying they looked fat and short or tall and skinny. I then discuss how if they believed what they saw, they may feel driven to start exercising, to drink daily milkshakes or maybe even to look for work in the circus. I use this to illustrate how mistaken beliefs (or cognitive distortions) drive OCD sufferers to engage in compulsions, leading to more uncertainty and misery.
Most of the time they respond by saying they looked fat and short or tall and skinny. I then discuss how if they believed what they saw, they may feel driven to start exercising, to drink daily milkshakes or maybe even to look for work in the circus. I use this to illustrate how mistaken beliefs (or cognitive distortions) drive OCD sufferers to engage in compulsions, leading to more uncertainty and misery.
Mistaken Belief: You can know the status of your health with absolute certainty: You can never know with 100 percent certainty that you are healthy. Chances are, if you suffer from health anxiety, you know the anguish of going to the doctor’s and immediately upon leaving the office thinking, “What if I didn’t explain my symptoms accurately? What if they misunderstood what I was saying? What if they missed something important?” The truth is that with being human we all run the risk of getting sick or having an illness pop up with no warning. I hate to say it, but we will all die and that may be the result of illness or of old age, but either way our choice is to enjoy our life being present for the things that matter or spend all our time trying to prevent illness and miss out on all the joy that can be found living in the moment.
Mistaken Belief: Symptoms and sensations indicate illness and always have a specific cause that can be determined: This is a fallacy. Sensations happen all the time for many reasons, including for no specific reason. Sometimes sensations and symptoms are related to a specific health concern, sometimes they are indicators of nothing. However, once they are noticed, focused on and resisted, they tend to become more prominent simply because of the hyper-focus on them. To convey this idea with my clients I sometimes like to ask them where they are itchy. At first, they look at me blankly, but then usually identify a place that is itchy. The idea being that when you scan your body for sensations and symptoms you will likely find them. Just because you are aware of these experiences does not mean they are necessarily important or dangerous.
Mistaken Belief: Having the perfect diagnosis will always lead to effective treatment and elimination of all symptoms: While often there are effective treatments for your symptoms, this is not always the case. There are some conditions that even when diagnosed treatment options are limited. This is especially true for some chronic conditions such as Inflammatory Bowel Disease, Headache Disorders, and Musculoskeletal conditions like Fibromyalgia. Your OCD is misleading you to believe that having a diagnosis (i.e. “the Answer”) will lead to relief.
There are some conditions that even when diagnosed treatment options are limited. This is especially true for some chronic conditions such as Inflammatory Bowel Disease, Headache Disorders, and Musculoskeletal conditions like Fibromyalgia. Your OCD is misleading you to believe that having a diagnosis (i.e. “the Answer”) will lead to relief.
Mistaken Belief: You are responsible for taking all possible precautions to avoid illness. The reality is that if you took every precaution you could possibly take to prevent illness, you would never be able to leave your home or have anyone come to your home, including the mail carrier. Even then, you couldn’t be sure that you took all precautions to prevent illness. Most enjoyable things in life inherently come with some risk. If you get out of bed, your risk goes up. Stay in bed too long, and your risk goes up too. But your OCD, not restricted by reason, would have you believe that there is no amount of risk worth taking when it comes to your health.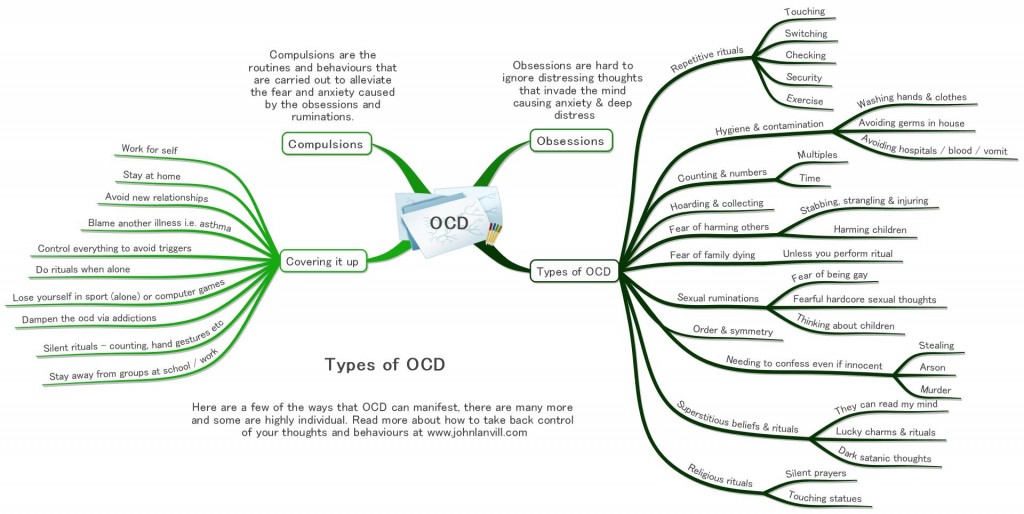
Mindfulness and ERP for Health Anxiety OCD
Exposure and Response Prevention (ERP), simply put, is a process where you confront your fears about your health and refrain from doing compulsions. People often think of mindfulness and ERP as two separate strategies when in fact mindfulness is often a part of ERP. While doing exposure to your fear you are mindfully allowing yourself to both approach and remain in the presence of your fear and mindfully choosing not to engage in compulsions. The purpose of this exercise is to essentially retrain your brain to respond to the obsessive thoughts without doing compulsions which ultimately teaches your brain that these thoughts are irrelevant (or tolerable) and require no response.
Learning to respond differently to these thoughts ultimately results in accepting uncertainty about their meaning. This both reduces your anxiety about the thoughts and increases your willingness to feel whatever anxiety may remain.
Examples of Exposures for Health Anxiety OCD
- Reading articles about people dying from diseases both common and uncommon
- Watching movies or videos about someone with a terminal illness
- Visiting hospitals, nursing homes, or places where you might fear acquiring an illness
- Writing imaginal scripts about being chronically or terminally ill and the consequences that could arise from this
- Writing imaginal scripts about failing to do enough to prevent an illness, failing to take enough precautions or perfectly follow medical advice
For any of the above approaches to work, they must be paired with resisting checking, comparing, reassurance-seeking or other compulsions.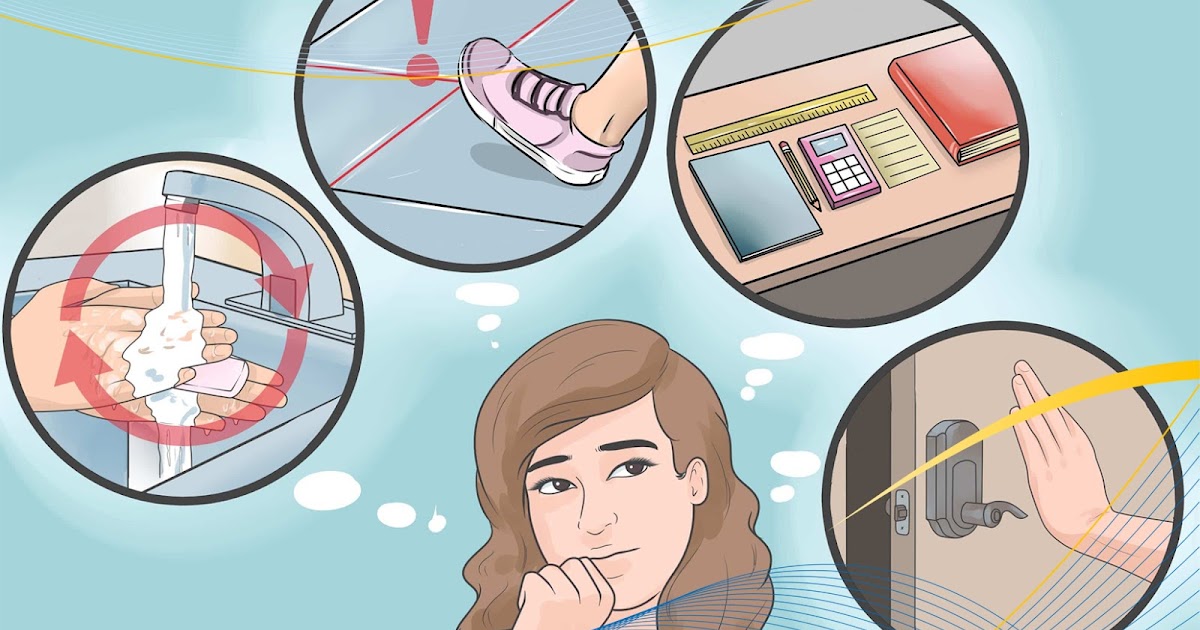 Making contracts/agreements with loved ones to help you resist reassurance-seeking can also be instrumental in your progress.
Making contracts/agreements with loved ones to help you resist reassurance-seeking can also be instrumental in your progress.
Mindful Awareness
With health anxiety, practicing mindful awareness is knowing that you tend to be aware of your body’s symptoms and sensations in every possible way and understanding that simply being aware doesn’t necessarily have to be experienced as aversive. The awareness is experienced as aversive often because of the meaning and judgement subscribed to the experience. Being mindful of physical symptoms and sensations means viewing them from a different standpoint.
I don’t know about you, but I never wake up being greeted by a host of positive thoughts about my day that inspire me to feel good. Instead my brain presents potential pitfalls and disastrous outcomes that if I spend much time thinking about will land me right back into bed. With mindful awareness I can just expect to have these thoughts when I wake up, and instead of trying to make them disappear I make a choice to note them as they arise and just allow myself to get up and move forward. Accepting the presence of unwanted thoughts does not mean accepting the content of the thought as being true.
Accepting the presence of unwanted thoughts does not mean accepting the content of the thought as being true.
For example, I just had the thought …what if I am brewing some kind of cancer at this very moment and am irresponsibly just sitting here doing nothing about it? I could respond by taking the thought as a message or warning of some kind and immediately contact my doctor or I can thank my brain for its creativity and continue to do what I value, which at this moment is to continue to treat and support those with OCD.
Standing Up for Yourself
Sometimes living with Health Anxiety OCD can feel like you are living in your own private hell that never seems to end. On top of the despair you may feel, your OCD condemns and berates you for all the ways you imagine you may have failed, which then leads you to feel more isolated and often depressed. From this standpoint it is difficult to feel motivated or even capable of doing what it requires to get better. This is where self-compassion can be especially helpful. At this point my clients frequently scowl because they assume I am referring to some kind of “give yourself a break type statement” which they often hate. However, self-compassion is simply about viewing yourself as a human being who has challenges like all other human beings. Self-compassion is a way of separating yourself from the nasty voice of OCD and allowing yourself to be honest about the situation without judgement and criticism. From this position you are better equipped to challenge your OCD and actively engage in treatment.
At this point my clients frequently scowl because they assume I am referring to some kind of “give yourself a break type statement” which they often hate. However, self-compassion is simply about viewing yourself as a human being who has challenges like all other human beings. Self-compassion is a way of separating yourself from the nasty voice of OCD and allowing yourself to be honest about the situation without judgement and criticism. From this position you are better equipped to challenge your OCD and actively engage in treatment.
The good news is you are not alone. Currently you may only know the suffering associated with your health anxiety but through the right treatment, there is hope of learning to appreciate the way your mind works. You may even learn to laugh at the ridiculousness of some of the ideas your OCD has you focused on and you may begin to appreciate the creativity it affords you. Above all, you may get to truly enjoy the benefits of the good health your OCD is so protective of.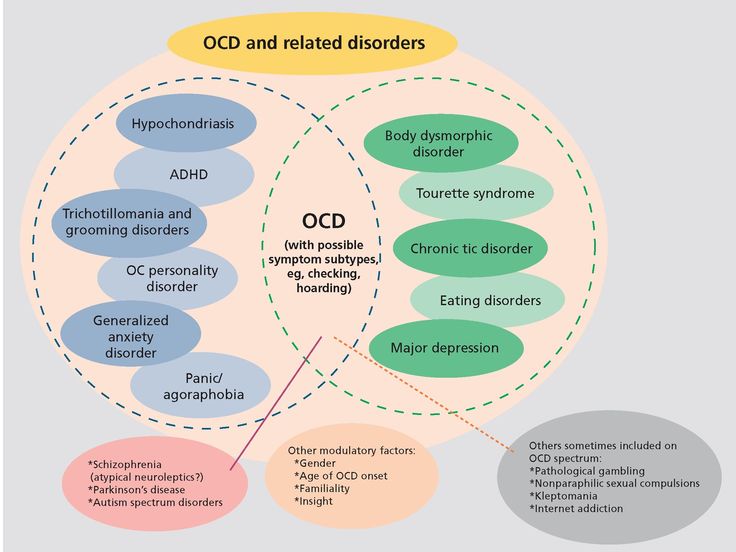
Obsessive-compulsive disorder
A prominent role among mental illnesses is played by syndromes (complexes of symptoms), united in the group of obsessive-compulsive disorder (OCD), which received its name from the Latin terms obsessio and compulsio.
Obsession (lat. obsessio - taxation, siege, blockade).
Compulsions (lat. compello - I force). 1. Obsessive drives, a kind of obsessive phenomena (obsessions). Characterized by irresistible attraction that arises contrary to the mind, will, feelings. Often they are unacceptable to the patient, contrary to his moral and ethical properties. Unlike impulsive drives, compulsions are not realized. These drives are recognized by the patient as wrong and painfully experienced by them, especially since their very appearance, due to its incomprehensibility, often gives rise to a feeling of fear in the patient 2. The term compulsions is also used in a broader sense to refer to any obsessions in the motor sphere, including obsessive rituals.
In domestic psychiatry, obsessive states were understood as psychopathological phenomena, characterized by the fact that phenomena of a certain content repeatedly appear in the mind of the patient, accompanied by a painful feeling of coercion [Zinoviev PM, 193I]. For N.s. characteristic involuntary, even against the will, the emergence of obsessions with clear consciousness. Although the obsessions are alien, extraneous in relation to the patient's psyche, the patient is not able to get rid of them. They are closely related to the emotional sphere, accompanied by depressive reactions, anxiety. Being symptomatic, according to S.L. Sukhanov [1912], "parasitic", they do not affect the course of intellectual activity in general, remain alien to thinking, do not lead to a decrease in its level, although they worsen the efficiency and productivity of the patient's mental activity. Throughout the course of the disease, a critical attitude is maintained towards obsessions. N.s. conditionally divided into obsessions in the intellectual-affective (phobia) and motor (compulsions) spheres, but most often several of their types are combined in the structure of the disease of obsessions. The isolation of obsessions that are abstract, affectively indifferent, indifferent in their content, for example, arrhythmomania, is rarely justified; An analysis of the psychogenesis of a neurosis often makes it possible to see a pronounced affective (depressive) background at the basis of the obsessive account. Along with elementary obsessions, the connection of which with psychogeny is obvious, there are “cryptogenic” ones, when the cause of painful experiences is hidden [Svyadoshch L.M., 1959]. N.s. are observed mainly in individuals with a psychasthenic character. This is where apprehensions are especially characteristic. In addition, N.S. occur within the framework of neurosis-like states with sluggish schizophrenia, endogenous depressions, epilepsy, the consequences of a traumatic brain injury, somatic diseases, mainly hypochondria-phobic or nosophobic syndrome. Some researchers distinguish the so-called. "Neurosis of obsessive states", which is characterized by the predominance of obsessive states in the clinical picture - memories that reproduce a psychogenic traumatic situation, thoughts, fears, actions.
The isolation of obsessions that are abstract, affectively indifferent, indifferent in their content, for example, arrhythmomania, is rarely justified; An analysis of the psychogenesis of a neurosis often makes it possible to see a pronounced affective (depressive) background at the basis of the obsessive account. Along with elementary obsessions, the connection of which with psychogeny is obvious, there are “cryptogenic” ones, when the cause of painful experiences is hidden [Svyadoshch L.M., 1959]. N.s. are observed mainly in individuals with a psychasthenic character. This is where apprehensions are especially characteristic. In addition, N.S. occur within the framework of neurosis-like states with sluggish schizophrenia, endogenous depressions, epilepsy, the consequences of a traumatic brain injury, somatic diseases, mainly hypochondria-phobic or nosophobic syndrome. Some researchers distinguish the so-called. "Neurosis of obsessive states", which is characterized by the predominance of obsessive states in the clinical picture - memories that reproduce a psychogenic traumatic situation, thoughts, fears, actions.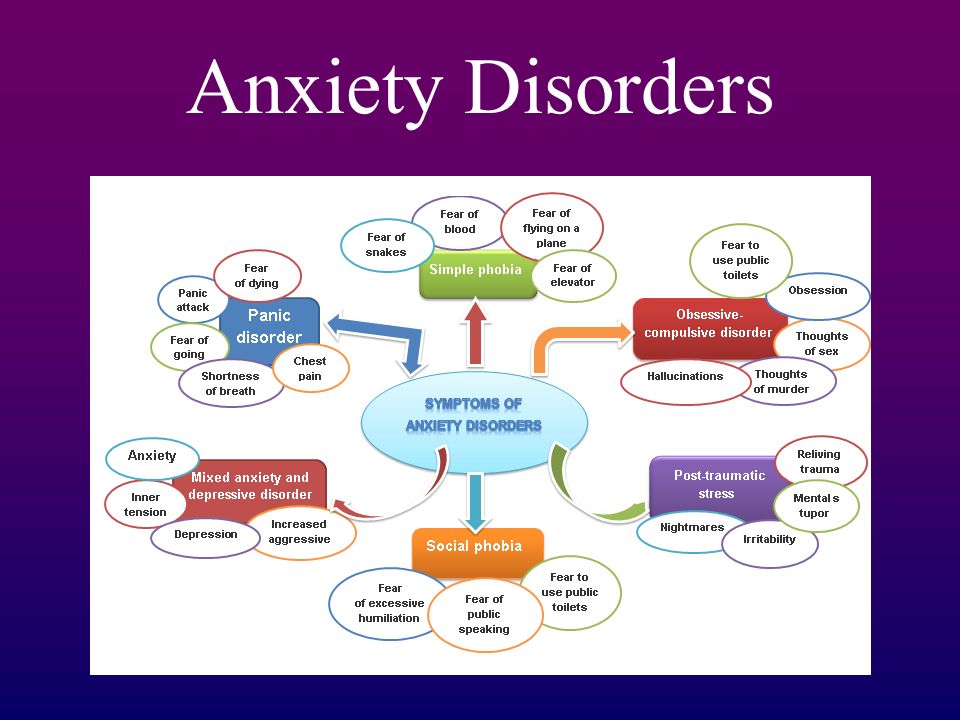 In genesis play a role: mental trauma; conditioned reflex stimuli that have become pathogenic due to their coincidence with others that previously caused a feeling of fear; situations that have become psychogenic due to the confrontation of opposing tendencies [Svyadoshch A.M., 1982]. It should be noted that these same authors emphasize that N.s.c. occurs with various character traits, but most often in psychasthenic personalities.
In genesis play a role: mental trauma; conditioned reflex stimuli that have become pathogenic due to their coincidence with others that previously caused a feeling of fear; situations that have become psychogenic due to the confrontation of opposing tendencies [Svyadoshch A.M., 1982]. It should be noted that these same authors emphasize that N.s.c. occurs with various character traits, but most often in psychasthenic personalities.
Currently, almost all obsessive-compulsive disorders are united in the International Classification of Diseases under the concept of "obsessive-compulsive disorder".
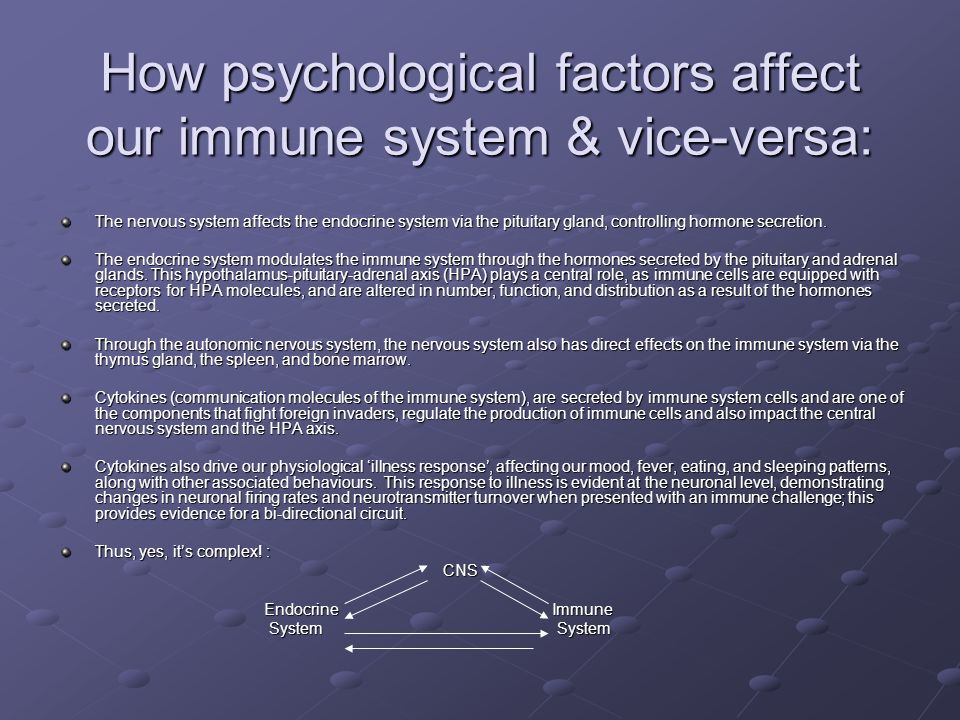
OKR concepts have undergone a fundamental reassessment over the past 15 years. During this time, the clinical and epidemiological significance of OCD has been completely revised. If it was previously thought that this is a rare condition observed in a small number of people, now it is known that OCD is common and causes a high percentage of morbidity, which requires the urgent attention of psychiatrists around the world. Parallel to this, our understanding of the etiology of OCD has broadened: the vaguely formulated psychoanalytic definition of the past two decades has been replaced by a neurochemical paradigm that explores the neurotransmitter disorders that underlie OCD. And most importantly, pharmacological interventions specifically targeting serotonergic neurotransmission have revolutionized the prospects for recovery for millions of OCD patients worldwide.
Parallel to this, our understanding of the etiology of OCD has broadened: the vaguely formulated psychoanalytic definition of the past two decades has been replaced by a neurochemical paradigm that explores the neurotransmitter disorders that underlie OCD. And most importantly, pharmacological interventions specifically targeting serotonergic neurotransmission have revolutionized the prospects for recovery for millions of OCD patients worldwide.
The discovery that intense serotonin reuptake inhibition (SSRI) was the key to effective treatment for OCD was the first step in a revolution and spurred clinical research that showed the efficacy of such selective inhibitors.
As described in ICD-10, the main features of OCD are repetitive intrusive (obsessive) thoughts and compulsive actions (rituals).
In a broad sense, the core of OCD is the syndrome of obsession, which is a condition with a predominance in the clinical picture of feelings, thoughts, fears, memories that arise in addition to the desire of patients, but with awareness of their pain and a critical attitude towards them.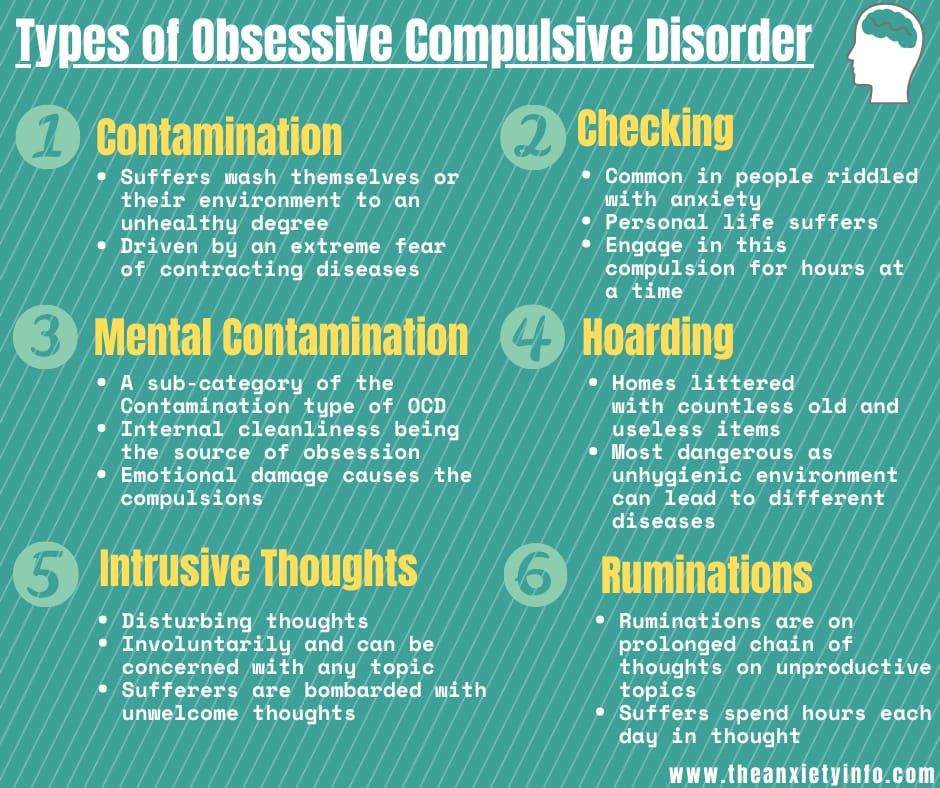 Despite the understanding of the unnaturalness, illogicality of obsessions and states, patients are powerless in their attempts to overcome them. Obsessional impulses or ideas are recognized as alien to the personality, but as if coming from within. Obsessions can be the performance of rituals designed to alleviate anxiety, such as washing hands to combat "pollution" and to prevent "infection". Attempts to drive away unwelcome thoughts or urges can lead to severe internal struggle, accompanied by intense anxiety.
Despite the understanding of the unnaturalness, illogicality of obsessions and states, patients are powerless in their attempts to overcome them. Obsessional impulses or ideas are recognized as alien to the personality, but as if coming from within. Obsessions can be the performance of rituals designed to alleviate anxiety, such as washing hands to combat "pollution" and to prevent "infection". Attempts to drive away unwelcome thoughts or urges can lead to severe internal struggle, accompanied by intense anxiety.
Obsessions in the ICD-10 are included in the group of neurotic disorders.
The prevalence of OCD in the population is quite high. According to some data, it is determined by an indicator of 1.5% (meaning "fresh" cases of diseases) or 2-3%, if episodes of exacerbations observed throughout life are taken into account. Those suffering from obsessive-compulsive disorder make up 1% of all patients receiving treatment in psychiatric institutions. It is believed that men and women are affected approximately equally.
CLINICAL PICTURE
The problem of obsessive-compulsive disorders attracted the attention of clinicians already at the beginning of the 17th century. They were first described by Platter in 1617. In 1621 E. Barton described an obsessive fear of death. Mentions of obsessions are found in the writings of F. Pinel (1829). I. Balinsky proposed the term "obsessive ideas", which took root in Russian psychiatric literature. In 1871, Westphal coined the term "agoraphobia" to refer to the fear of being in public places. M. Legrand de Sol [1875], analyzing the features of the dynamics of OCD in the form of "insanity of doubt with delusions of touch, points to a gradually becoming more complicated clinical picture - obsessive doubts are replaced by ridiculous fears of" touch "to surrounding objects, motor rituals join, the fulfillment of which is subject to the whole life sick. However, only at the turn of the XIX-XX centuries. researchers were able to more or less clearly describe the clinical picture and give syndromic characteristics of obsessive-compulsive disorders. The onset of the disease usually occurs in adolescence and adolescence. The maximum of clinically defined manifestations of obsessive-compulsive disorder is observed in the age range of 10-25 years.
The onset of the disease usually occurs in adolescence and adolescence. The maximum of clinically defined manifestations of obsessive-compulsive disorder is observed in the age range of 10-25 years.
Main clinical manifestations of OCD:
Obsessional thoughts - painful, arising against the will, but recognized by the patient as their own, ideas, beliefs, images, which in a stereotyped form forcibly invade the patient's consciousness and which he tries to resist in some way. It is this combination of an inner sense of compulsive urge and efforts to resist it that characterizes obsessional symptoms, but of the two, the degree of effort exerted is the more variable. Obsessional thoughts may take the form of single words, phrases, or lines of poetry; they are usually unpleasant to the patient and may be obscene, blasphemous, or even shocking.
Obsessional imagery is vivid scenes, often violent or disgusting, including, for example, sexual perversion.
Obsessional impulses are urges to do things that are usually destructive, dangerous or shameful; for example, jumping into the road in front of a moving car, injuring a child, or shouting obscene words while in society.
Obsessional rituals include both mental activities (eg, counting repeatedly in a particular way, or repeating certain words) and repetitive but meaningless acts (eg, washing hands twenty or more times a day). Some of them have an understandable connection with the obsessive thoughts that preceded them, for example, repeated washing of hands - with thoughts of infection. Other rituals (for example, regularly laying out clothes in some complex system before putting them on) do not have such a connection. Some patients feel an irresistible urge to repeat such actions a certain number of times; if that fails, they are forced to start all over again. Patients are invariably aware that their rituals are illogical and usually try to hide them. Some fear that such symptoms are a sign of the onset of insanity. Both obsessive thoughts and rituals inevitably lead to problems in daily activities.
Obsessive rumination (“mental chewing gum”) is an internal debate in which the arguments for and against even the simplest everyday actions are endlessly revised.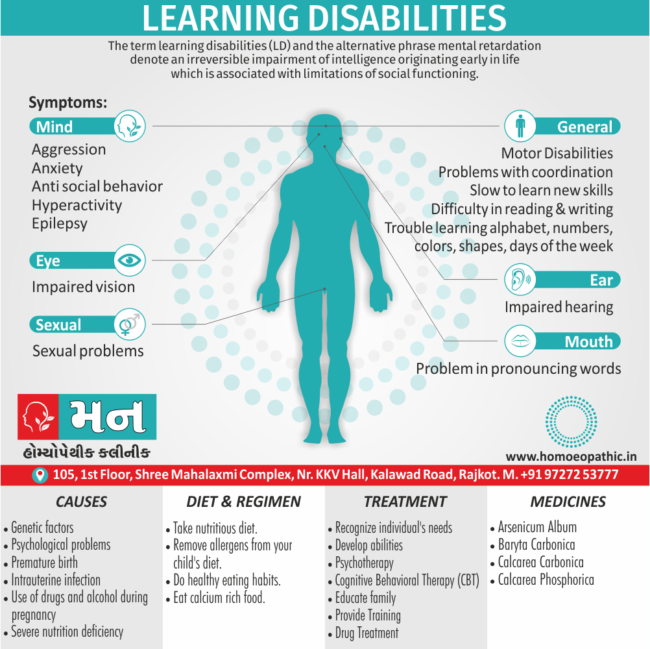 Some obsessive doubts relate to actions that may have been incorrectly performed or not completed, such as turning off the gas stove faucet or locking the door; others concern actions that could harm other people (for example, the possibility of driving past a cyclist in a car, knocking him down). Sometimes doubts are associated with a possible violation of religious prescriptions and rituals - “remorse of conscience”.
Some obsessive doubts relate to actions that may have been incorrectly performed or not completed, such as turning off the gas stove faucet or locking the door; others concern actions that could harm other people (for example, the possibility of driving past a cyclist in a car, knocking him down). Sometimes doubts are associated with a possible violation of religious prescriptions and rituals - “remorse of conscience”.
Compulsive actions - repetitive stereotypical actions, sometimes acquiring the character of protective rituals. The latter are aimed at preventing any objectively unlikely events that are dangerous for the patient or his relatives.
In addition to the above, in a number of obsessive-compulsive disorders, a number of well-defined symptom complexes stand out, and among them are obsessive doubts, contrasting obsessions, obsessive fears - phobias (from the Greek. phobos).
Obsessive thoughts and compulsive rituals may intensify in certain situations; for example, obsessive thoughts about harming other people often become more persistent in the kitchen or some other place where knives are kept. Since patients often avoid such situations, there may be a superficial resemblance to the characteristic avoidance pattern found in phobic anxiety disorder. Anxiety is an important component of obsessive-compulsive disorders. Some rituals reduce anxiety, while after others it increases. Obsessions often develop as part of depression. In some patients, this appears to be a psychologically understandable reaction to obsessive-compulsive symptoms, but in other patients, recurrent episodes of depressive mood occur independently.
Since patients often avoid such situations, there may be a superficial resemblance to the characteristic avoidance pattern found in phobic anxiety disorder. Anxiety is an important component of obsessive-compulsive disorders. Some rituals reduce anxiety, while after others it increases. Obsessions often develop as part of depression. In some patients, this appears to be a psychologically understandable reaction to obsessive-compulsive symptoms, but in other patients, recurrent episodes of depressive mood occur independently.
Obsessions (obsessions) are divided into figurative or sensual, accompanied by the development of affect (often painful) and obsessions of affectively neutral content.
Sensual obsessions include obsessive doubts, memories, ideas, drives, actions, fears, an obsessive feeling of antipathy, an obsessive fear of habitual actions.
Obsessive doubts - intrusively arising contrary to logic and reason, uncertainty about the correctness of committed and committed actions. The content of doubts is different: obsessive everyday fears (whether the door is locked, whether windows or water taps are closed tightly enough, whether gas and electricity are turned off), doubts related to official activities (whether this or that document is written correctly, whether the addresses on business papers are mixed up , whether inaccurate figures are indicated, whether orders are correctly formulated or executed), etc. Despite repeated verification of the committed action, doubts, as a rule, do not disappear, causing psychological discomfort in the person suffering from this kind of obsession.
The content of doubts is different: obsessive everyday fears (whether the door is locked, whether windows or water taps are closed tightly enough, whether gas and electricity are turned off), doubts related to official activities (whether this or that document is written correctly, whether the addresses on business papers are mixed up , whether inaccurate figures are indicated, whether orders are correctly formulated or executed), etc. Despite repeated verification of the committed action, doubts, as a rule, do not disappear, causing psychological discomfort in the person suffering from this kind of obsession.
Obsessive memories include persistent, irresistible painful memories of any sad, unpleasant or shameful events for the patient, accompanied by a sense of shame, remorse. They dominate the mind of the patient, despite the efforts and efforts not to think about them.
Obsessive impulses - urges to commit one or another tough or extremely dangerous action, accompanied by a feeling of horror, fear, confusion with the inability to get rid of it. The patient is seized, for example, by the desire to throw himself under a passing train or push a loved one under it, to kill his wife or child in an extremely cruel way. At the same time, patients are painfully afraid that this or that action will be implemented.
The patient is seized, for example, by the desire to throw himself under a passing train or push a loved one under it, to kill his wife or child in an extremely cruel way. At the same time, patients are painfully afraid that this or that action will be implemented.
Manifestations of obsessive ideas can be different. In some cases, this is a vivid "vision" of the results of obsessive drives, when patients imagine the result of a cruel act committed. In other cases, obsessive ideas, often referred to as mastering, appear in the form of implausible, sometimes absurd situations that patients take for real. An example of obsessive ideas is the patient's conviction that the buried relative was alive, and the patient painfully imagines and experiences the suffering of the deceased in the grave. At the height of obsessive ideas, the consciousness of their absurdity, implausibility disappears and, on the contrary, confidence in their reality appears. As a result, obsessions acquire the character of overvalued formations (dominant ideas that do not correspond to their true meaning), and sometimes delusions.
An obsessive feeling of antipathy (as well as obsessive blasphemous and blasphemous thoughts) - unjustified, driven away by the patient from himself antipathy towards a certain, often close person, cynical, unworthy thoughts and ideas in relation to respected people, in religious persons - in relation to saints or ministers churches.
Obsessive acts are acts done against the wishes of the sick, despite efforts made to restrain them. Some of the obsessive actions burden the patients until they are realized, others are not noticed by the patients themselves. Obsessive actions are painful for patients, especially in those cases when they become the object of attention of others.
Obsessive fears, or phobias, include an obsessive and senseless fear of heights, large streets, open or confined spaces, large crowds of people, the fear of sudden death, the fear of falling ill with one or another incurable disease. Some patients may develop a wide variety of phobias, sometimes acquiring the character of fear of everything (panphobia). And finally, an obsessive fear of the emergence of fears (phobophobia) is possible.
And finally, an obsessive fear of the emergence of fears (phobophobia) is possible.
Hypochondriacal phobias (nosophobia) - an obsessive fear of some serious illness. Most often, cardio-, stroke-, syphilo- and AIDS phobias are observed, as well as the fear of the development of malignant tumors. At the peak of anxiety, patients sometimes lose their critical attitude to their condition - they turn to doctors of the appropriate profile, require examination and treatment. The implementation of hypochondriacal phobias occurs both in connection with psycho- and somatogenic (general non-mental illnesses) provocations, and spontaneously. As a rule, hypochondriacal neurosis develops as a result, accompanied by frequent visits to doctors and unreasonable medication.
Specific (isolated) phobias - obsessive fears limited to a strictly defined situation - fear of heights, nausea, thunderstorms, pets, treatment at the dentist, etc. Since contact with situations that cause fear is accompanied by intense anxiety, the patients tend to avoid them.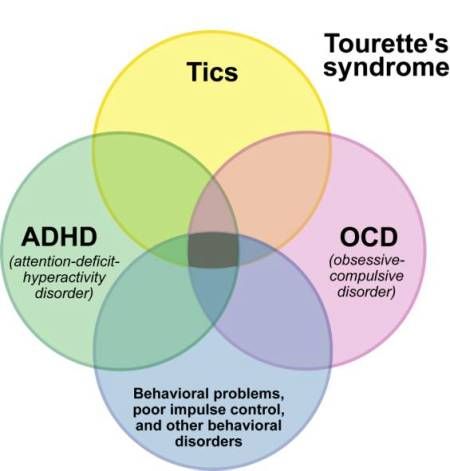
Obsessive fears are often accompanied by the development of rituals - actions that have the meaning of "magic" spells that are performed, despite the critical attitude of the patient to obsession, in order to protect against one or another imaginary misfortune: before starting any important business, the patient must perform some that specific action to eliminate the possibility of failure. Rituals can, for example, be expressed in snapping fingers, playing a melody to the patient or repeating certain phrases, etc. In these cases, even relatives are not aware of the existence of such disorders. Rituals, combined with obsessions, are a fairly stable system that usually exists for many years and even decades.
Obsessions of affectively neutral content - obsessive sophistication, obsessive counting, recalling neutral events, terms, formulations, etc. Despite their neutral content, they burden the patient, interfere with his intellectual activity.
Contrasting obsessions ("aggressive obsessions") - blasphemous, blasphemous thoughts, fear of harming oneself and others. Psychopathological formations of this group refer mainly to figurative obsessions with pronounced affective saturation and ideas that take possession of the consciousness of patients. They are distinguished by a sense of alienation, the absolute lack of motivation of the content, as well as a close combination with obsessive drives and actions. Patients with contrasting obsessions and complain of an irresistible desire to add endings to the replicas they have just heard, giving an unpleasant or threatening meaning to what has been said, to repeat after those around them, but with a touch of irony or malice, phrases of religious content, to shout out cynical words that contradict their own attitudes and generally accepted morality. , they may experience fear of losing control of themselves and possibly committing dangerous or ridiculous actions, injuring themselves or their loved ones. In the latter cases, obsessions are often combined with object phobias (fear of sharp objects - knives, forks, axes, etc.
Psychopathological formations of this group refer mainly to figurative obsessions with pronounced affective saturation and ideas that take possession of the consciousness of patients. They are distinguished by a sense of alienation, the absolute lack of motivation of the content, as well as a close combination with obsessive drives and actions. Patients with contrasting obsessions and complain of an irresistible desire to add endings to the replicas they have just heard, giving an unpleasant or threatening meaning to what has been said, to repeat after those around them, but with a touch of irony or malice, phrases of religious content, to shout out cynical words that contradict their own attitudes and generally accepted morality. , they may experience fear of losing control of themselves and possibly committing dangerous or ridiculous actions, injuring themselves or their loved ones. In the latter cases, obsessions are often combined with object phobias (fear of sharp objects - knives, forks, axes, etc. ). The contrasting group also partially includes obsessions of sexual content (obsessions of the type of forbidden ideas about perverted sexual acts, the objects of which are children, representatives of the same sex, animals).
). The contrasting group also partially includes obsessions of sexual content (obsessions of the type of forbidden ideas about perverted sexual acts, the objects of which are children, representatives of the same sex, animals).
Obsessions of pollution (mysophobia). This group of obsessions includes both the fear of pollution (earth, dust, urine, feces and other impurities), as well as the fear of penetration into the body of harmful and toxic substances (cement, fertilizers, toxic waste), small objects (glass fragments, needles, specific types of dust), microorganisms. In some cases, the fear of contamination can be limited, remain at the preclinical level for many years, manifesting itself only in some features of personal hygiene (frequent change of linen, repeated washing of hands) or in housekeeping (thorough handling of food, daily washing of floors). , "taboo" on pets). This kind of monophobia does not significantly affect the quality of life and is evaluated by others as habits (exaggerated cleanliness, excessive disgust). Clinically manifested variants of mysophobia belong to the group of severe obsessions. In these cases, gradually becoming more complex protective rituals come to the fore: avoiding sources of pollution and touching "unclean" objects, processing things that could get dirty, a certain sequence in the use of detergents and towels, which allows you to maintain "sterility" in the bathroom. Stay outside the apartment is also furnished with a series of protective measures: going out into the street in special clothing that covers the body as much as possible, special processing of wearable items upon returning home. In the later stages of the disease, patients, avoiding pollution, not only do not go out, but do not even leave their own room. In order to avoid contacts and contacts that are dangerous in terms of contamination, patients do not allow even their closest relatives to come near them. Mysophobia is also related to the fear of contracting a disease, which does not belong to the categories of hypochondriacal phobias, since it is not determined by fears that a person suffering from OCD has a particular disease.
Clinically manifested variants of mysophobia belong to the group of severe obsessions. In these cases, gradually becoming more complex protective rituals come to the fore: avoiding sources of pollution and touching "unclean" objects, processing things that could get dirty, a certain sequence in the use of detergents and towels, which allows you to maintain "sterility" in the bathroom. Stay outside the apartment is also furnished with a series of protective measures: going out into the street in special clothing that covers the body as much as possible, special processing of wearable items upon returning home. In the later stages of the disease, patients, avoiding pollution, not only do not go out, but do not even leave their own room. In order to avoid contacts and contacts that are dangerous in terms of contamination, patients do not allow even their closest relatives to come near them. Mysophobia is also related to the fear of contracting a disease, which does not belong to the categories of hypochondriacal phobias, since it is not determined by fears that a person suffering from OCD has a particular disease. In the foreground is the fear of a threat from the outside: the fear of pathogenic bacteria entering the body. Hence the development of appropriate protective actions.
In the foreground is the fear of a threat from the outside: the fear of pathogenic bacteria entering the body. Hence the development of appropriate protective actions.
A special place in the series of obsessions is occupied by obsessive actions in the form of isolated, monosymptomatic movement disorders. Among them, especially in childhood, tics predominate, which, unlike organically conditioned involuntary movements, are much more complex motor acts that have lost their original meaning. Tics sometimes give the impression of exaggerated physiological movements. This is a kind of caricature of certain motor acts, natural gestures. Patients suffering from tics can shake their heads (as if checking whether the hat fits well), make hand movements (as if discarding interfering hair), blink their eyes (as if getting rid of a mote). Along with obsessive tics, pathological habitual actions (lip biting, gnashing of teeth, spitting, etc.) are often observed, which differ from obsessive actions proper in the absence of a subjectively painful sense of persistence and experience them as alien, painful.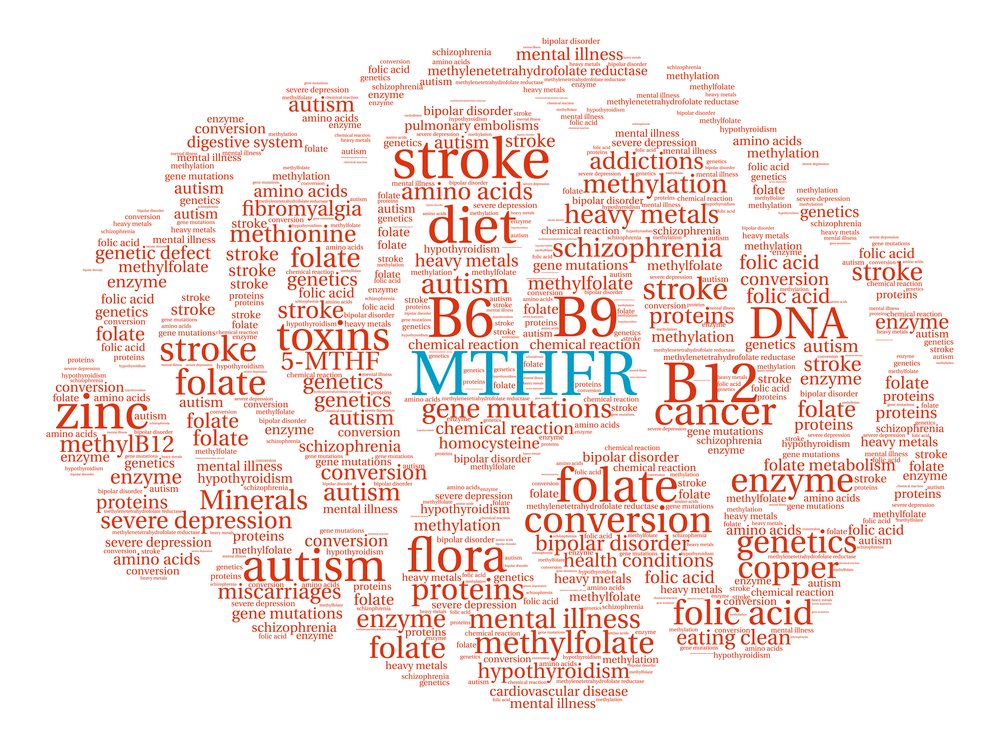 Neurotic states characterized only by obsessive tics usually have a favorable prognosis. Appearing most often in preschool and primary school age, tics usually subside by the end of puberty. However, such disorders can also be more persistent, persist for many years and only partially change in manifestations.
Neurotic states characterized only by obsessive tics usually have a favorable prognosis. Appearing most often in preschool and primary school age, tics usually subside by the end of puberty. However, such disorders can also be more persistent, persist for many years and only partially change in manifestations.
The course of obsessive-compulsive disorder.
Unfortunately, chronization must be indicated as the most characteristic trend in the OCD dynamics. Cases of episodic manifestations of the disease and complete recovery are relatively rare. However, in many patients, especially with the development and preservation of one type of manifestation (agoraphobia, obsessive counting, ritual handwashing, etc.), a long-term stabilization of the condition is possible. In these cases, there is a gradual (usually in the second half of life) mitigation of psychopathological symptoms and social readaptation. For example, patients who experienced fear of traveling on certain types of transport, or public speaking, cease to feel flawed and work along with healthy people.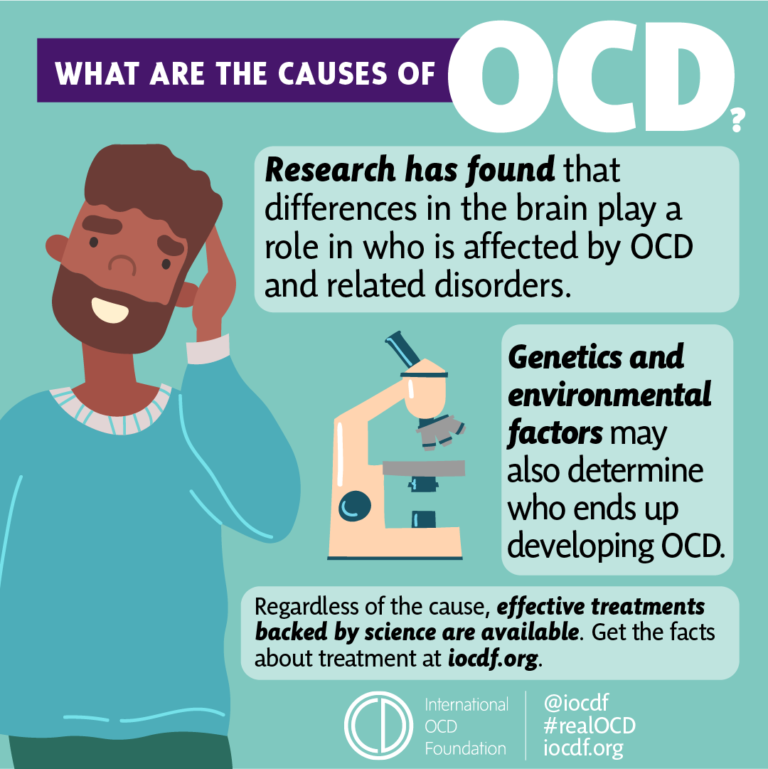 In mild forms of OCD, the disease usually proceeds favorably (on an outpatient basis). The reverse development of symptoms occurs after 1 year - 5 years from the moment of manifestation.
In mild forms of OCD, the disease usually proceeds favorably (on an outpatient basis). The reverse development of symptoms occurs after 1 year - 5 years from the moment of manifestation.
More severe and complex OCDs such as phobias of infection, pollution, sharp objects, contrasting performances, multiple rituals, on the other hand, may become persistent, resistant to treatment, or show a tendency to recur with disorders that persist despite active therapy. Further negative dynamics of these conditions indicates a gradual complication of the clinical picture of the disease as a whole.
DIFFERENTIAL DIAGNOSIS
It is important to distinguish OCD from other disorders that involve compulsions and rituals. In some cases, obsessive-compulsive disorder must be differentiated from schizophrenia, especially when the obsessive thoughts are unusual in content (eg, mixed sexual and blasphemous themes) or the rituals are exceptionally eccentric. The development of a sluggish schizophrenic process cannot be ruled out with the growth of ritual formations, their persistence, the emergence of antagonistic tendencies in mental activity (inconsistency of thinking and actions), and the uniformity of emotional manifestations. Prolonged obsessional states of a complex structure must be distinguished from the manifestations of paroxysmal schizophrenia. Unlike neurotic obsessive states, they are usually accompanied by a sharply increasing anxiety, a significant expansion and systematization of the circle of obsessive associations, which acquire the character of obsessions of "special significance": previously indifferent objects, events, random remarks of others remind patients of the content of phobias, offensive thoughts and thereby acquire in their view a special, menacing significance. In such cases, it is necessary to consult a psychiatrist in order to exclude schizophrenia. It can also be difficult to differentiate between OCD and conditions with a predominance of generalized disorders, known as Gilles de la Tourette's syndrome. Tics in such cases are localized in the face, neck, upper and lower extremities and are accompanied by grimaces, opening the mouth, sticking out the tongue, and intense gesticulation.
Prolonged obsessional states of a complex structure must be distinguished from the manifestations of paroxysmal schizophrenia. Unlike neurotic obsessive states, they are usually accompanied by a sharply increasing anxiety, a significant expansion and systematization of the circle of obsessive associations, which acquire the character of obsessions of "special significance": previously indifferent objects, events, random remarks of others remind patients of the content of phobias, offensive thoughts and thereby acquire in their view a special, menacing significance. In such cases, it is necessary to consult a psychiatrist in order to exclude schizophrenia. It can also be difficult to differentiate between OCD and conditions with a predominance of generalized disorders, known as Gilles de la Tourette's syndrome. Tics in such cases are localized in the face, neck, upper and lower extremities and are accompanied by grimaces, opening the mouth, sticking out the tongue, and intense gesticulation. In these cases, this syndrome can be excluded by the coarseness of movement disorders characteristic of it and more complex in structure and more severe mental disorders.
In these cases, this syndrome can be excluded by the coarseness of movement disorders characteristic of it and more complex in structure and more severe mental disorders.
Genetic factors
Speaking about hereditary predisposition to OCD, it should be noted that obsessive-compulsive disorders are found in approximately 5-7% of parents of patients with such disorders. Although this figure is low, it is higher than in the general population. While the evidence for a hereditary predisposition to OCD is still uncertain, psychasthenic personality traits can be largely explained by genetic factors.
FORECAST
Approximately two-thirds of OCD patients improve within a year, more often by the end of this period. If the disease lasts more than a year, fluctuations are observed during its course - periods of exacerbations are interspersed with periods of improvement in health, lasting from several months to several years. The prognosis is worse if we are talking about a psychasthenic personality with severe symptoms of the disease, or if there are continuous stressful events in the patient's life..jpg) Severe cases can be extremely persistent; for example, a study of hospitalized patients with OCD found that three-quarters of them remained symptom-free 13 to 20 years later.
Severe cases can be extremely persistent; for example, a study of hospitalized patients with OCD found that three-quarters of them remained symptom-free 13 to 20 years later.
TREATMENT: BASIC METHODS AND APPROACHES
Despite the fact that OCD is a complex group of symptom complexes, the principles of treatment for them are the same. The most reliable and effective method of treating OCD is considered to be drug therapy, during which a strictly individual approach to each patient should be manifested, taking into account the characteristics of the manifestation of OCD, age, gender, and the presence of other diseases. In this regard, we must warn patients and their relatives against self-treatment. If any disorders similar to mental ones appear, it is necessary, first of all, to contact the specialists of the psycho-neurological dispensary at the place of residence or other psychiatric medical institutions to establish the correct diagnosis and prescribe competent adequate treatment.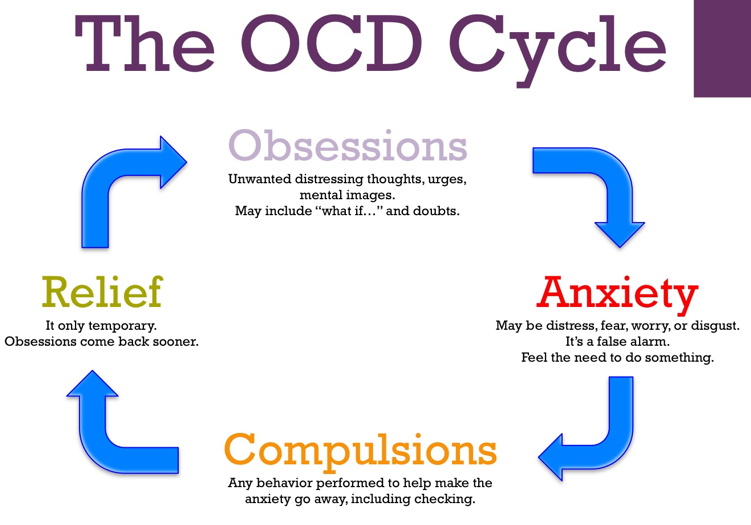 At the same time, it should be remembered that at present a visit to a psychiatrist does not threaten with any negative consequences - the infamous "accounting" was canceled more than 10 years ago and replaced by the concepts of consultative and medical care and dispensary observation.
At the same time, it should be remembered that at present a visit to a psychiatrist does not threaten with any negative consequences - the infamous "accounting" was canceled more than 10 years ago and replaced by the concepts of consultative and medical care and dispensary observation.
When treating, it must be borne in mind that obsessive-compulsive disorders often have a fluctuating course with long periods of remission (improvement). The apparent suffering of the patient often seems to call for vigorous effective treatment, but the natural course of the condition must be kept in mind in order to avoid the typical error of over-intensive therapy. It is also important to consider that OCD is often accompanied by depression, the effective treatment of which often leads to an alleviation of obsessional symptoms.
The treatment of OCD begins with an explanation of the symptoms to the patient and, if necessary, with reassurance that they are the initial manifestation of insanity (a common concern for patients with obsessions).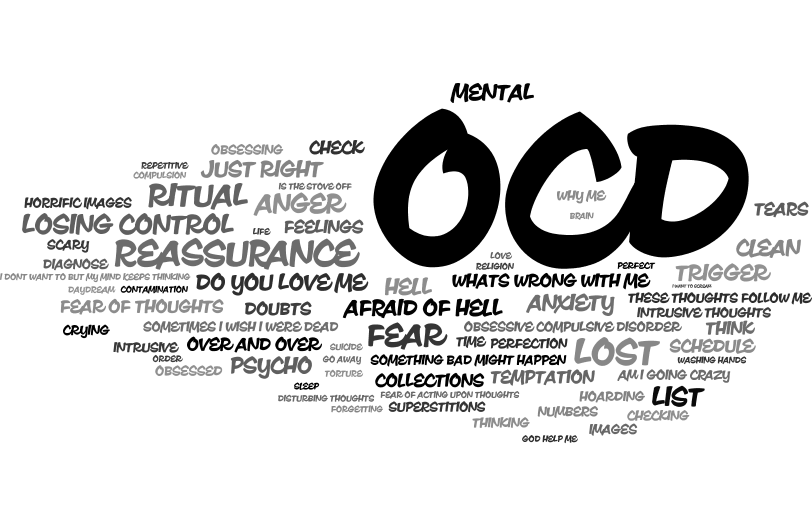 Those suffering from certain obsessions often involve other family members in their rituals, so relatives need to treat the patient firmly, but sympathetically, mitigating the symptoms as much as possible, and not aggravating it by excessive indulgence in the sick fantasies of patients.
Those suffering from certain obsessions often involve other family members in their rituals, so relatives need to treat the patient firmly, but sympathetically, mitigating the symptoms as much as possible, and not aggravating it by excessive indulgence in the sick fantasies of patients.
Drug therapy
The following therapeutic approaches exist for the currently identified types of OCD. Of the pharmacological drugs for OCD, serotonergic antidepressants, anxiolytics (mainly benzodiazepine), beta-blockers (to stop autonomic manifestations), MAO inhibitors (reversible) and triazole benzodiazepines (alprazolam) are most often used. Anxiolytic drugs provide some short-term relief of symptoms, but should not be given for more than a few weeks at a time. If anxiolytic treatment is required for more than one to two months, small doses of tricyclic antidepressants or small antipsychotics sometimes help. The main link in the treatment regimen for OCD, overlapping with negative symptoms or ritualized obsessions, are atypical antipsychotics - risperidone, olanzapine, quetiapine, in combination with either SSRI antidepressants or other antidepressants - moclobemide, tianeptine, or with high-potency benzodiazepine derivatives ( alprazolam, clonazepam, bromazepam).
Any comorbid depressive disorder is treated with antidepressants at an adequate dose. There is evidence that one of the tricyclic antidepressants, clomipramine, has a specific effect on obsessive symptoms, but the results of a controlled clinical trial showed that the effect of this drug is insignificant and occurs only in patients with distinct depressive symptoms.
In cases where obsessive-phobic symptoms are observed within the framework of schizophrenia, intensive psychopharmacotherapy with proportional use of high doses of serotonergic antidepressants (fluoxetine, fluvoxamine, sertraline, paroxetine, citalopram) has the greatest effect. In some cases, it is advisable to connect traditional antipsychotics (small doses of haloperidol, trifluoperazine, fluanxol) and parenteral administration of benzodiazepine derivatives.
Psychotherapy
Behavioral psychotherapy
One of the main tasks of the specialist in the treatment of OCD is to establish fruitful cooperation with the patient. It is necessary to instill in the patient faith in the possibility of recovery, to overcome his prejudice against the "harm" caused by psychotropic drugs, to convey his conviction in the effectiveness of treatment, subject to the systematic observance of the prescribed prescriptions. The patient's faith in the possibility of healing must be supported in every possible way by the relatives of the OCD sufferer. If the patient has rituals, it must be remembered that improvement usually occurs when using a combination of the method of preventing a reaction with placing the patient in conditions that aggravate these rituals. Significant but not complete improvement can be expected in about two-thirds of patients with moderately heavy rituals. If, as a result of such treatment, the severity of rituals decreases, then, as a rule, the accompanying obsessive thoughts also recede. In panphobia, predominantly behavioral techniques are used to reduce sensitivity to phobic stimuli, supplemented by elements of emotionally supportive psychotherapy.
It is necessary to instill in the patient faith in the possibility of recovery, to overcome his prejudice against the "harm" caused by psychotropic drugs, to convey his conviction in the effectiveness of treatment, subject to the systematic observance of the prescribed prescriptions. The patient's faith in the possibility of healing must be supported in every possible way by the relatives of the OCD sufferer. If the patient has rituals, it must be remembered that improvement usually occurs when using a combination of the method of preventing a reaction with placing the patient in conditions that aggravate these rituals. Significant but not complete improvement can be expected in about two-thirds of patients with moderately heavy rituals. If, as a result of such treatment, the severity of rituals decreases, then, as a rule, the accompanying obsessive thoughts also recede. In panphobia, predominantly behavioral techniques are used to reduce sensitivity to phobic stimuli, supplemented by elements of emotionally supportive psychotherapy. In cases where ritualized phobias predominate, along with desensitization, behavioral training is actively used to help overcome avoidant behavior. Behavioral therapy is significantly less effective for obsessive thoughts that are not accompanied by rituals. Thought-stopping has been used by some experts for many years, but its specific effect has not been convincingly proven.
In cases where ritualized phobias predominate, along with desensitization, behavioral training is actively used to help overcome avoidant behavior. Behavioral therapy is significantly less effective for obsessive thoughts that are not accompanied by rituals. Thought-stopping has been used by some experts for many years, but its specific effect has not been convincingly proven.
Social rehabilitation
We have already noted that obsessive-compulsive disorder has a fluctuating (fluctuating) course and over time the patient's condition may improve regardless of which particular methods of treatment were used. Until recovery, patients can benefit from supportive conversations that provide continued hope for recovery. Psychotherapy in the complex of treatment and rehabilitation measures for patients with OCD is aimed at both correcting avoidant behavior and reducing sensitivity to phobic situations (behavioral therapy), as well as family psychotherapy to correct behavioral disorders and improve family relationships. If marital problems aggravate the symptoms, joint interviews with the spouse are indicated. Patients with panphobia (at the stage of the active course of the disease), due to the intensity and pathological persistence of symptoms, need both medical and social and labor rehabilitation. In this regard, it is important to determine adequate terms of treatment - long-term (at least 2 months) therapy in a hospital with subsequent continuation of the course on an outpatient basis, as well as taking measures to restore social ties, professional skills, family relationships. Social rehabilitation is a set of programs for teaching OCD patients how to behave rationally both at home and in a hospital setting. Rehabilitation is aimed at teaching social skills to properly interact with other people, vocational training, as well as skills necessary in everyday life. Psychotherapy helps patients, especially those who experience a sense of their own inferiority, treat themselves better and correctly, master ways to solve everyday problems, and gain confidence in their strength.
If marital problems aggravate the symptoms, joint interviews with the spouse are indicated. Patients with panphobia (at the stage of the active course of the disease), due to the intensity and pathological persistence of symptoms, need both medical and social and labor rehabilitation. In this regard, it is important to determine adequate terms of treatment - long-term (at least 2 months) therapy in a hospital with subsequent continuation of the course on an outpatient basis, as well as taking measures to restore social ties, professional skills, family relationships. Social rehabilitation is a set of programs for teaching OCD patients how to behave rationally both at home and in a hospital setting. Rehabilitation is aimed at teaching social skills to properly interact with other people, vocational training, as well as skills necessary in everyday life. Psychotherapy helps patients, especially those who experience a sense of their own inferiority, treat themselves better and correctly, master ways to solve everyday problems, and gain confidence in their strength.
All of these methods, when used judiciously, can increase the effectiveness of drug therapy, but are not capable of completely replacing drugs. It should be noted that explanatory psychotherapy does not always help, and some patients with OCD even worsen because such procedures encourage them to think painfully and unproductively about the subjects discussed in the course of treatment. Unfortunately, science still does not know how to cure mental illness once and for all. OCD often has a tendency to recur, which requires long-term prophylactic medication.
symptoms, how to get rid of and treat
Olya Selivanova
struggles with obsessive-compulsive disorder
Author profile
Since childhood, I have suffered from obsessive thoughts.
When I was nine years old, I was reading a book, when suddenly the thought occurred to me: “If you don’t finish reading today, your mother will die.” The thought frightened me, I put down the book and cried, but I had to return to reading so that my mother would not die.
From that moment on, the frightening thoughts were different. I could suddenly change the route, because the thought came to my mind: “It is not safe to go further. Get around." There were thoughts to harm loved ones: push, hit, pour over. At such moments, I thought that an evil force had entered into me, and I began to count to myself, imagined how the numbers increased in order in size and knocked bad thoughts out of my head.
By the time I was twelve, it all came to naught, and as a teenager, I decided that it was just childish oddities. But seven years later, the obsessive thoughts returned, and the doctor at the neuropsychiatric dispensary diagnosed me with Obsessive-Compulsive Disorder. I'll tell you how I was treated and how I live now.
Go see a doctor
Our articles are written with love for evidence-based medicine. We refer to authoritative sources and go to doctors with a good reputation for comments. But remember: the responsibility for your health lies with you and your doctor. We don't write prescriptions, we make recommendations. Relying on our point of view or not is up to you.
We don't write prescriptions, we make recommendations. Relying on our point of view or not is up to you.
What is obsessive-compulsive disorder
Obsessive-compulsive disorder is a mental illness in which a person has obsessive thoughts and compulsive actions.
What is Obsessive-Compulsive Disorder - Mayo Clinic
Obsessive thoughts - obsessions - usually revolve around certain topics: fear of harming yourself and others, fear of germs and toxic substances, the need to organize everything. They appear suddenly or are provoked by external circumstances, such as a sharp object or the word "last".
Intrusive thoughts cannot be ignored, they cause anxiety or disgust. In response to them, a person has compulsions - a strong desire to perform certain actions that, according to his feelings, will get rid of such thoughts. Compulsions are difficult to resist: the anxiety will grow until the person gives up.
For example, the obsessive thought that a person will become infected after touching a doorknob will provoke compulsive actions - repeated washing of hands, sometimes for several hours in a row.
/shizofreniya/
How much does it cost to support a relative with a mental disorder
I try not to touch doorknobs in public places and always make sure the door is closed. Do I have OCD?
Sergey Divisenko
psychotherapist
If a person’s condition does not interfere with himself or others, then everything is in order, if it interferes, a disorder can be suspected. In the case of checking the door, one can say that checking if the door is closed once is not a problem, rechecking the door several times in a row and doing it systematically is already a problem.
To understand whether or not there is OCD, the doctor pays attention to how often the patient has obsessive thoughts and compulsive actions and how they affect his life. If symptoms occur more frequently in two weeks than in seven days and interfere with daily activities, it is probably OCD.
In this case, the symptoms should have the following characteristics:
- The person should evaluate them as his own thoughts and desires.

- There must be at least one thought or action that one unsuccessfully resists.
- The thought of a person performing a compulsive action should not in itself be pleasant. The fact that an action will help reduce anxiety is not considered pleasant in this sense.
- Thoughts or actions must be repeated.
How obsessive-compulsive disorder is treated
OCD is considered a lifelong disorder, but with the help of treatment it is possible to achieve remission: to get rid of obsessive thoughts and compulsive actions for a long time or to reduce their number.
Medical treatment. The main drugs for the treatment of OCD are antidepressants of the SSRI group. They increase serotonin levels in the brain, making OCD symptoms less likely to occur.
Treatment options for OCD - NHS
Depending on the course of the disease and symptoms, along with antidepressants, the doctor may prescribe other drugs: tranquilizers, neuroleptics or mood stabilizers.
Cognitive behavioral therapy. This is a type of psychotherapy during which a person learns to control their emotional response to intrusive thoughts. As a result of therapy, obsessive thoughts cease to cause anxiety and compulsive actions.
Cognitive behavioral therapy - NHS
Order of the Ministry of Health of the Russian Federation of September 16, 2003 No. 438 "On psychotherapeutic care"
Psychiatrists, psychotherapists and psychologists are involved in the treatment of OCD in Russia. Psychiatrists prescribe prescription drugs. Psychotherapists and psychologists conduct psychotherapy sessions.
How I was diagnosed
At the age of 19, the development of the disease took a new turn. I was washing the kitchen knife and I had an obsessive thought that I was losing control and could cut myself and the guy who was nearby at that moment. So I began to avoid sharp objects, there was an irresistible desire to hide or throw them away.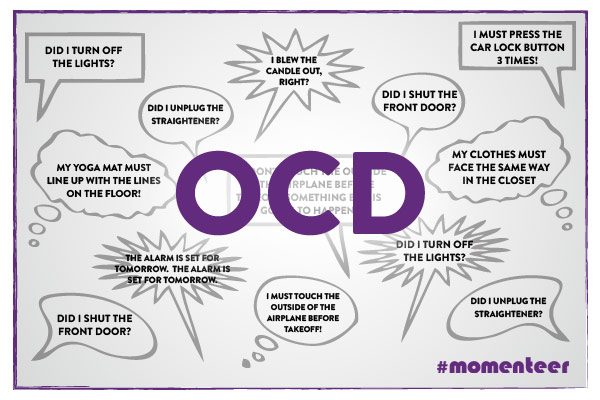
Obsessive thoughts revolved around the topic of death: drinking nail polish remover, bleach, vinegar, throwing yourself under a vehicle or jumping out of a window. Because of this, I removed all dangerous liquids from the house and stayed away from open windows, highways and train station platforms. I didn’t sleep well at night, suffered from anxiety, considered myself crazy and dangerous, and began to move away from everyone.
I also doubted everything. Even if I just performed an action, it seemed to me that it was not completed. I opened the door to make sure that it had been closed before, closed it again, pulled the handle, asked those around me if the door was exactly closed. I could wake up at night and see if the stove was turned on, although before going to bed I went up to it and stared without blinking - so that it would crash into my memory that it was definitely turned off. My young man, seeing all this, insisted that we try to see a psychologist.
In Irkutsk, where I live, psychiatric care can be obtained free of charge at the regional psycho-neurological dispensary. I turned to the psychotherapeutic department of the dispensary for a consultation with a psychologist. At the reception, they brought me a card and said that there was no appointment with a psychologist for the next few days, but I could get to a psychiatrist: there are fewer people who want to see him.
I turned to the psychotherapeutic department of the dispensary for a consultation with a psychologist. At the reception, they brought me a card and said that there was no appointment with a psychologist for the next few days, but I could get to a psychiatrist: there are fewer people who want to see him.
/spravka/
How to get a certificate from PND
At the appointment with the psychiatrist, I told about what was happening to me. The doctor was not surprised and said that it was an obsessive-compulsive disorder. It was the first time I heard my diagnosis, but I didn't believe it. On the Internet, I came across information that OCD is only pedantry, handwashing, fear of germs and perfectionism, and not the creepy things that come to my mind. The psychiatrist said that OCD was treated with antidepressants and offered to write a prescription, but I refused treatment because I thought they were serious drugs that would do more harm than help.
How a visit to a psycho-neurological dispensary with OCD will affect later life
Sergey Divisenko
psychotherapist
The patient could move freely, drive a car, use weapons and work.
With an OCD diagnosis, you can still work in any job, there are no legal barriers to this. With regard to cars and weapons, the situation has changed. In 2014 and 2015, government decrees appeared, according to which OCD became a contraindication for driving and owning weapons.
However, from a psychiatrist's point of view, a person diagnosed with OCD can drive a car and use a weapon. Doctors of the psycho-neurological dispensary still give a certificate about this, but they do it through a medical commission.
Treatment
First hospitalizationMy condition worsened, I tried to ignore obsessive thoughts. But the more I resisted them, the stronger they became. In addition, anger, irritability and constant fatigue appeared.
With new symptoms, I decided to see an endocrinologist, because I heard that this happens with problems with the thyroid gland.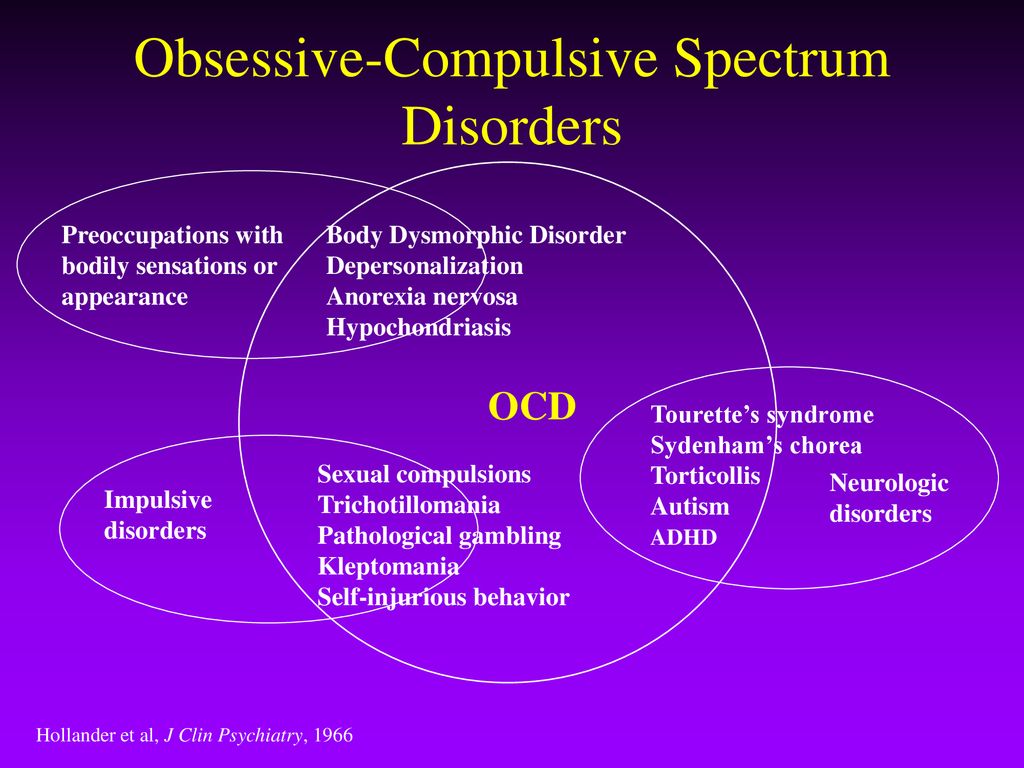 According to the results of ultrasound and hormone tests, the thyroid gland was in order. Then I made an appointment with a neurologist, but he also said that this was not his profile. Both doctors suggested that my constant fatigue, anger and irritability were symptoms of depression and advised me to seek psychiatric help.
According to the results of ultrasound and hormone tests, the thyroid gland was in order. Then I made an appointment with a neurologist, but he also said that this was not his profile. Both doctors suggested that my constant fatigue, anger and irritability were symptoms of depression and advised me to seek psychiatric help.
Symptoms of clinical depression - NHS
I researched information about depression and realized that antidepressants could help, all I had to do was get a prescription. I came to the psychotherapeutic department again, but there was already another psychiatrist there. Since my condition worsened, instead of a prescription, he wrote out a referral for hospitalization in a day hospital. I had prejudices about a psychiatric hospital, so I did not want to visit the hospital. But there was no strength to argue with the psychiatrist.
This is how a referral for hospitalization to a day hospital looks like The next day I was already in the hospital. During the registration, the psychiatrist on duty asked what I was complaining about, measured the pressure and examined whether there were injuries on the body. It turned out to be difficult for me to talk about the symptoms: there was a feeling that they would not believe me, or vice versa, they would believe me so much that they would put me in a round-the-clock hospital. But everything was fine, the psychiatrist wrote down the data on the card, gave it to the orderly, and together with him sent me to the head.
It turned out to be difficult for me to talk about the symptoms: there was a feeling that they would not believe me, or vice versa, they would believe me so much that they would put me in a round-the-clock hospital. But everything was fine, the psychiatrist wrote down the data on the card, gave it to the orderly, and together with him sent me to the head.
The manager looked at the card, confirmed the diagnosis of OCD and depression, and prescribed treatment: an antidepressant, an antipsychotic, a mood stabilizer, tranquilizer tablets, and injections of B vitamins.
/guide/vitamins/
Vitamins: what foods contain and how to take supplements
The routine in the hospital was as follows: I arrived at eight in the morning, had breakfast and took the prescribed pills, took injections, dined and went home. Tablets were issued immediately for one day, but they could also be issued for two days, for example, before the weekend. Once after the injection, I went to an appointment with a clinical psychologist, he gave various tests and questionnaires that tested logic and intelligence.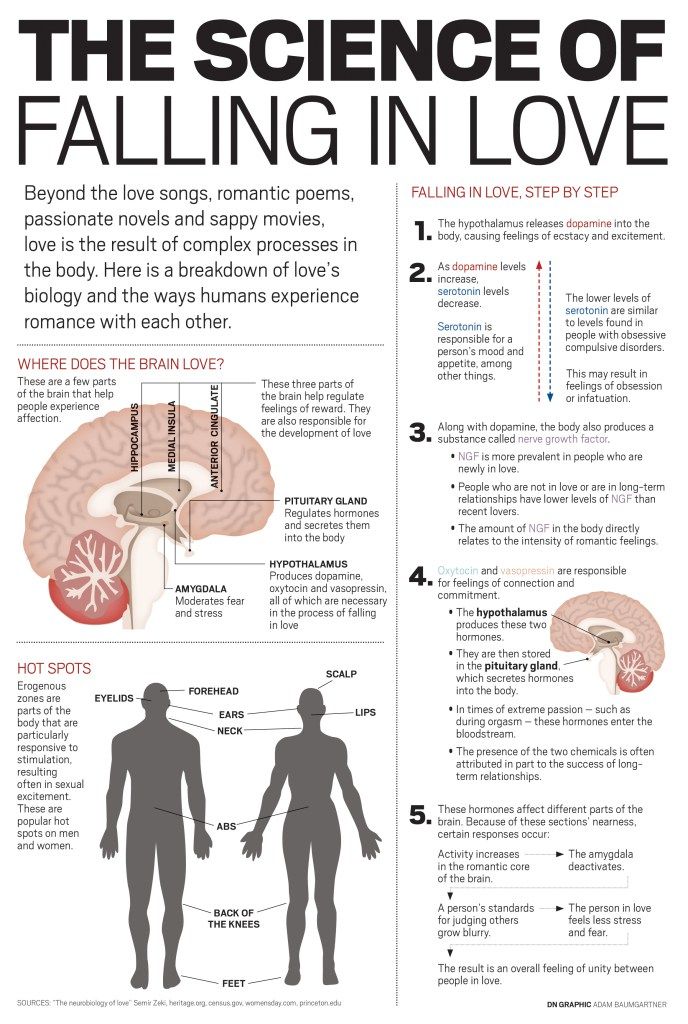
About three times a week I went to see a psychiatrist in the same hospital. I told her about my condition and asked questions. I thought that as soon as I start taking medication, my mood will rise and my anxiety will go away. But this did not happen, so it seemed that everything was in vain and the treatment had to be abandoned. The psychiatrist explained to me that not all drugs begin to act instantly, she assured me that we were on the right track and we had to wait. These conversations made it easier. In my case, antidepressants began to work only on the third month of admission, when I no longer visited the day hospital.
Treatment at the day hospital lasted a month. All medications, medical consultations and meals were free. I spent money only on the road to the hospital and back - 600 R by public transport for the whole time.
/bye-depression/
“It reminded me of a strict regime sanatorium”: how much I spent on treating depression
After treatment, the symptoms of depression remained, but obsessive thoughts began to bother me less often: I stopped being afraid of open windows and was able to ride the escalator. Treatment had to be continued on an outpatient basis. Before I was discharged, the psychiatrist said that she would transfer my data to the psychiatric department. Now I will need to come to the local psychiatrist for prescriptions for medicines, and turn to him if the condition worsens or questions arise.
During the treatment in the hospital, I doubted everything. Even in being sick. Not only the psychiatrist, but also relatives helped to cope. They noticed the changes, but my young man did not let me stop the treatment
They noticed the changes, but my young man did not let me stop the treatment Treatment
Visiting a local psychiatristAfter I was discharged from the hospital, I came to the registration office of the psychiatric department with a passport and I was immediately sent to the district police officer. The doctor did not change the treatment and wrote out a prescription for the same medicines that were given in the day hospital. In the future, a referral to the district police officer was also not required. I just came to the appointment when I needed to update the prescription.
Government Decree of July 30, 1994 No. 890 with a list of categories of beneficiaries who are entitled to free medicines
District psychiatrists were different: some were polite, some were rude and rude. Using the brute force method, I found two normal specialists - when I made an appointment at the reception, I began to ask to be directed to them. Usually the registrar complied with my request.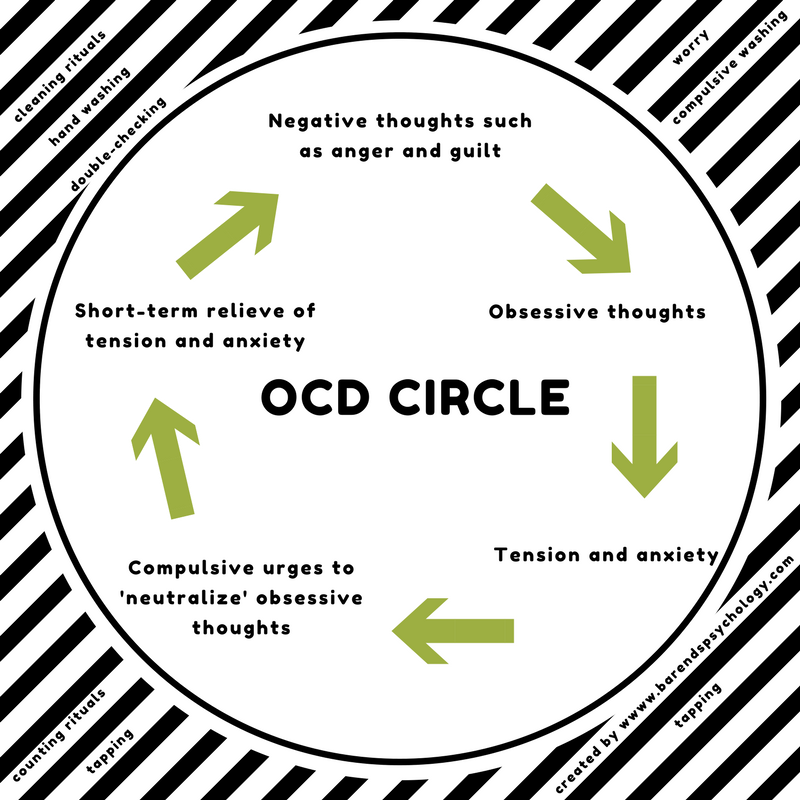
Spent in six months of outpatient treatment — 8895 Р
| Preparation | Spending |
|---|---|
| Antidepressants | 5988 R |
| Normotimics | 2384 R |
| Antipsychotics | 419 R |
| Tranquilizers | 104 R |
Antidepressants
5988 R
Normotimics
2384 R
Neuroleptics
419 419 R
Transquilizers
104 R
Free medicines for the treatment of OCD are provided to certain privileged categories of people. I’m not a beneficiary, so I bought everything with my own money. Pharmacies don’t require a passport, but they put the date of issue of the medicine on the back and don’t sell more than prescribed by prescription. For example, according to a prescription for three months, I was given only three packs of an antidepressant. When I wanted to buy one more to have a supply, the pharmacist refusedTreatment
Second hospitalization and psychotherapy After six months of outpatient treatment, the local psychiatrist recommended to be treated again in the hospital. Antidepressants helped: my mood improved, I got energy and I wanted to live, but I felt a side effect from antipsychotics. I was terribly sleepy, my handwriting changed, it was difficult to write in class and generally follow the train of thought of the teacher. In addition, there were more intrusive thoughts.
Antidepressants helped: my mood improved, I got energy and I wanted to live, but I felt a side effect from antipsychotics. I was terribly sleepy, my handwriting changed, it was difficult to write in class and generally follow the train of thought of the teacher. In addition, there were more intrusive thoughts.
In the day hospital, I was treated by the same psychiatrist as the first time. She adjusted the drug treatment so that I was not bothered by intrusive thoughts. She also said that a psychotherapist had appeared in the hospital and referred me to her for a consultation.
Unlike the psychiatrist's consultations during the first hospitalization, we did not discuss drugs and their effects with the psychotherapist. We talked about what is happening to me and what other methods can be used to combat this, in addition to drugs. At the first appointment, I briefly talked about my lifestyle, obsessive thoughts, compulsive actions, and how I tried to resist them even before the treatment. Then the doctor explained to me what obsessive-compulsive disorder is and how it manifests itself, why my struggle only worsened the condition and led to depression.
Then the doctor explained to me what obsessive-compulsive disorder is and how it manifests itself, why my struggle only worsened the condition and led to depression.
/psychotherapy-search/
How to choose a psychotherapist
We agreed that I would try to keep the number of compulsive actions to a minimum, and I would cope with anxiety from intrusive thoughts with the help of techniques.
Speak key phrases. Thoughts in themselves mean nothing, they can come to mind automatically. We agreed that when I had an obsessive thought, I would simply tell myself that it was a manifestation of OCD. Here are the two phrases that I used: “This is just my thought that…”, “I know that this thought is a manifestation of OCD…” So gradually I stopped identifying myself with my thoughts and realized that thinking about the bad is does not mean to be a bad person.
Separately, we discussed the issue of the materialization of thoughts.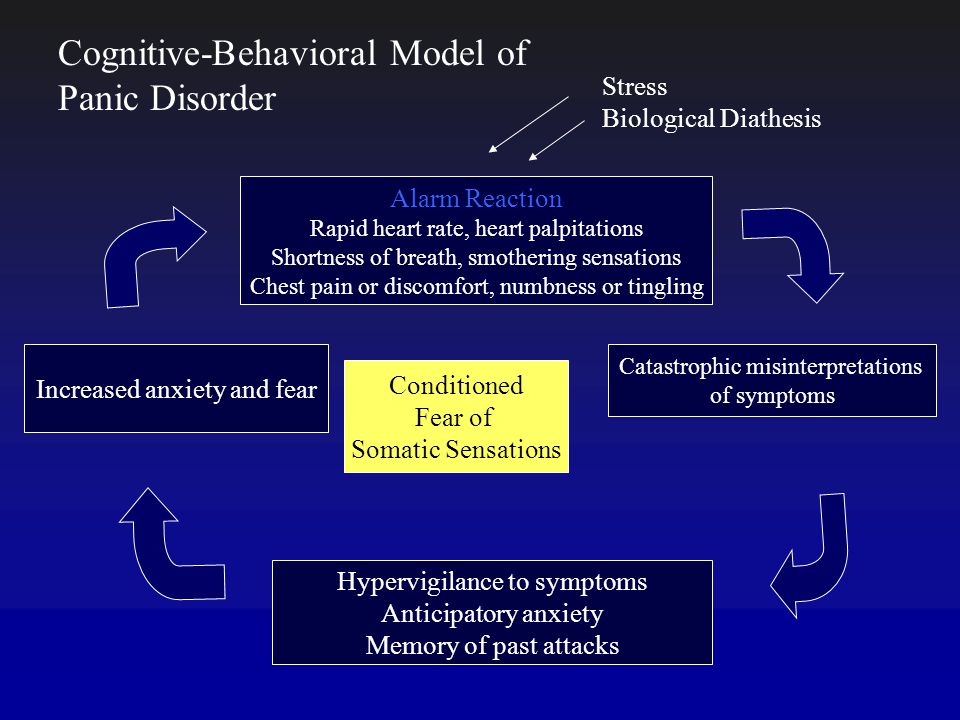 When terrible things are spinning in your head, and you hear from everywhere that thoughts are material, you get very worried. We discussed the fact that thoughts are intangible and you can’t invite trouble with them. This made it easier and the degree of emotions decreased.
When terrible things are spinning in your head, and you hear from everywhere that thoughts are material, you get very worried. We discussed the fact that thoughts are intangible and you can’t invite trouble with them. This made it easier and the degree of emotions decreased.
Observe how the body reacts to anxiety. Every time I had anxiety from obsessive thoughts, I did not run away from it, but watched my body. I was shaking, my heartbeat increased, my breathing quickened, but I continued to live it. The psychotherapist said that I would not die from this. Yes, it is unpleasant and scary, but when you live emotions, you gradually learn to cope with them.
Keep a diary. In the course of the sessions, I became convinced that I cannot control the thoughts themselves - it is impossible, but I can control the reaction to them. So I started keeping a diary.
/psychotherapy/
How psychotherapy works
It was necessary to take notes according to the formula: A - situation, B - my thoughts, C - my emotions. Using such records, it is easier to track the thoughts that cause negative emotions and work them out. For example, when I could not fall asleep for a long time, I began to think that something was going wrong, and this caused anxiety. Then I wrote down the whole situation in a diary and instead of negative thoughts I formulated new ones: "My sleep does not depend on my will, and this is normal." It helped to get rid of anxiety, stop trying to sleep and go about your business. About half an hour later I went to bed and fell asleep peacefully.
Using such records, it is easier to track the thoughts that cause negative emotions and work them out. For example, when I could not fall asleep for a long time, I began to think that something was going wrong, and this caused anxiety. Then I wrote down the whole situation in a diary and instead of negative thoughts I formulated new ones: "My sleep does not depend on my will, and this is normal." It helped to get rid of anxiety, stop trying to sleep and go about your business. About half an hour later I went to bed and fell asleep peacefully.
| I also kept a mood diary. Before treatment, there was no point in monitoring the mood: it always turned out to be bad or indifferent | On antidepressants, I began to make entries in a diary every day and could track what affects my mood |
I also kept a mood diary. Before treatment, there was no point in monitoring the mood: it always turned out to be bad or indifferent. On antidepressants, I began to make entries in a diary every day and could track what affects my mood
Before treatment, there was no point in monitoring the mood: it always turned out to be bad or indifferent. On antidepressants, I began to make entries in a diary every day and could track what affects my mood
In the day hospital, I was treated for a month and a half, during which time I had only five sessions with a psychotherapist. All sessions, meals and drugs, as in the first hospitalization, were free. The only thing I had to spend money on was the road to the hospital and back, as well as the original antidepressant instead of the analogue provided in the dispensary. The doctor recommended the original, it suited me better.
3202 Р
spent on medicines and transport for a month and a half of treatment in the hospital
When I was discharged, the doctor told me that I was in a stable condition, the treatment helped me. I myself felt it: the mood was consistently good, and I quickly coped with obsessive thoughts.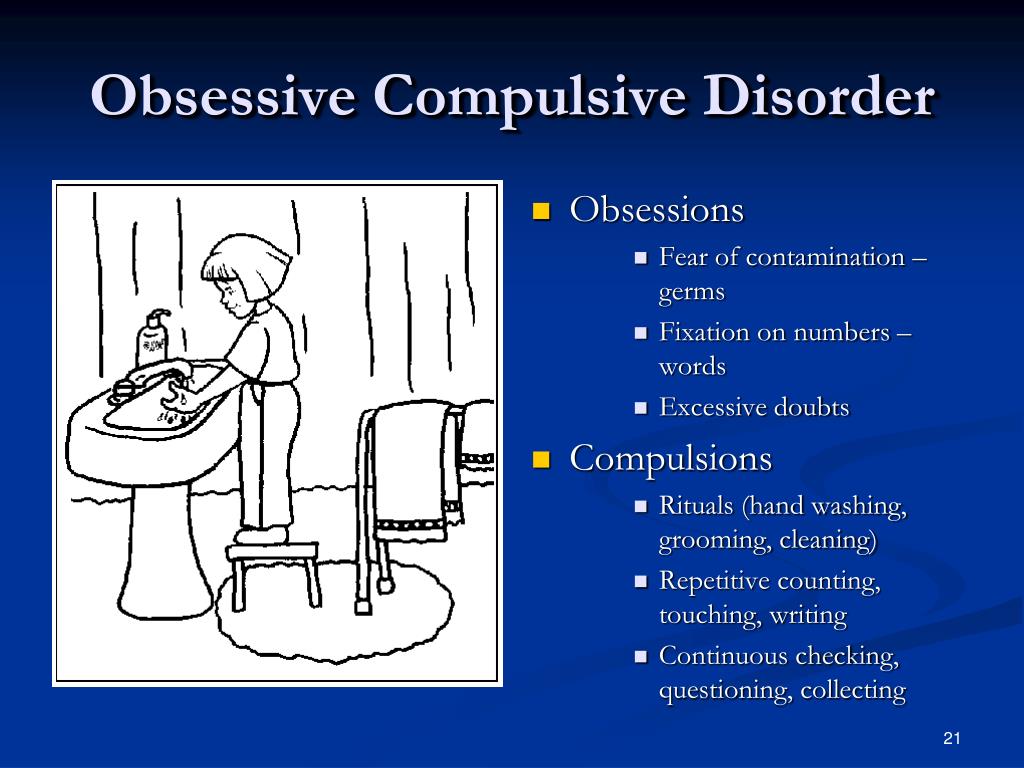 I was canceled all the drugs, except for antidepressants, then I had to continue taking them, be observed by the district psychiatrist and monitor my condition.
I was canceled all the drugs, except for antidepressants, then I had to continue taking them, be observed by the district psychiatrist and monitor my condition.
Spent one and a half months of treatment in a hospital — 3202 Р
| Expenses | Spending |
|---|---|
| Antidepressants | 2422 R |
| Transport | 780 P |
Antidepressants
2422 R
Transport
780 R
How do I feel after treatment
I stopped taking antidepressants a year and a month after discharge I spent another 14,640 R on them. Sometimes I have obsessive thoughts and compulsive actions, but I do not scold myself for this. I know that if I get upset, the symptoms will become more frequent. The psychiatrist warned me that OCD symptoms may appear periodically, but this is normal.
14,640 Р
spent on antidepressants for a year and one month
Coronavirus last spring was a test of strength for me. The condition worsened, compulsive actions resumed, I stopped leaving the house, I began to choke on the street, obsessive thoughts about death appeared. But I managed it on my own with the help of techniques taught to me by the therapist. I kept in my head the idea that if it worked then, it will work now.
The condition worsened, compulsive actions resumed, I stopped leaving the house, I began to choke on the street, obsessive thoughts about death appeared. But I managed it on my own with the help of techniques taught to me by the therapist. I kept in my head the idea that if it worked then, it will work now.
Before treatment, it was difficult for me to talk about my disorder. And now I openly talk about it and I can even joke about random manifestations of OCD. Almost everyone in my circle knows that I was being treated for OCD and depression. They help me notice compulsive actions and stop in time, treat me with understanding when I ask obvious things just in case - for example, did I close the door.
How often do people with OCD need to take drugs for life
Sergey Divisenko
psychotherapist
With the help of treatment, you can achieve remission - for a long time to get rid of the symptoms of OCD or reduce their number. Remission can occur both against the background of taking medications, and without them, against the background of psychotherapy.
Approximately 80% of patients with OCD stop taking medication sooner or later.
How much does OCD treatment cost?
In total, I treated OCD for one year and nine months. Of these, she was treated in a day hospital for two and a half months, and for a year and seven months - on an outpatient basis.
In the hospital, I only spent money on transport to and from the dispensary. Even during the second hospitalization, on the recommendation of the doctor, she bought antidepressants at the pharmacy and took them instead of those given in the hospital. The rest of the drugs, consultations and meals were free.
6 useful services for finding a psychotherapist
Most of the expenses are medicines during outpatient treatment.
Spent on OCD treatment for 1 year and 9 months — 27,337 R
| Expenses | Spending |
|---|---|
| Antidepressants | 23 050 Р |
| Normotimics | 2384 R |
| Antipsychotics | 419 R |
| Tranquilizers | 104 R |
| Transport during hospitalization | 1380 R |
Remember
- Obsessive Compulsive Disorder or OCD is a mental illness in which a person experiences obsessive thoughts and compulsive actions.