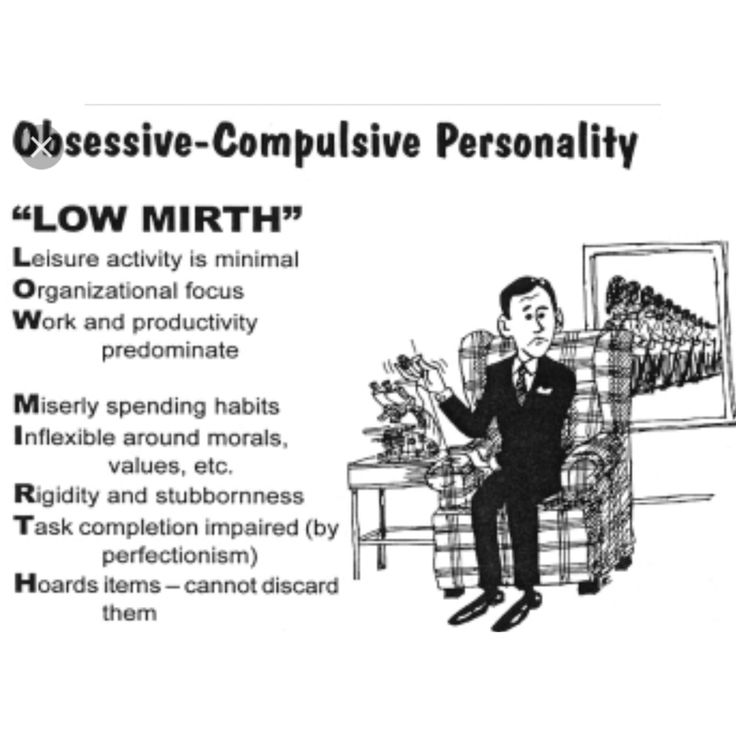
Obsessive compulsive disorder psychology definition
NIMH » Obsessive-Compulsive Disorder
Overview
Obsessive-compulsive disorder (OCD) is a common, chronic, and long-lasting disorder in which a person has uncontrollable, reoccurring thoughts ("obsessions") and/or behaviors ("compulsions") that he or she feels the urge to repeat over and over.
Signs and Symptoms
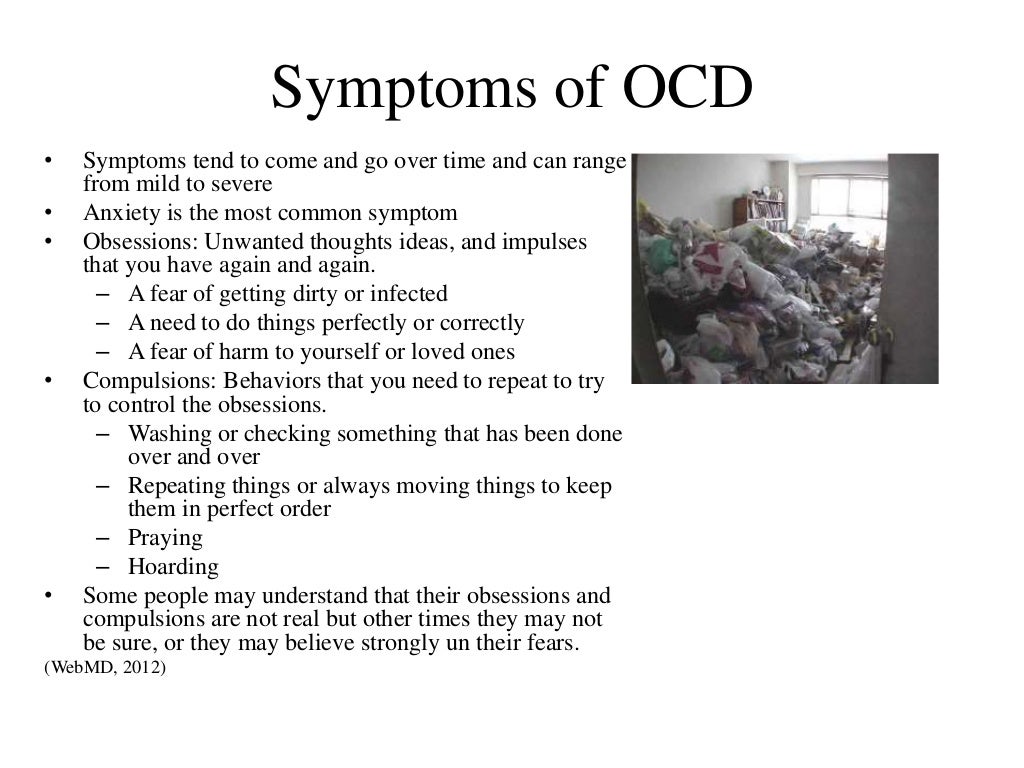
People with OCD may have symptoms of obsessions, compulsions, or both. These symptoms can interfere with all aspects of life, such as work, school, and personal relationships.
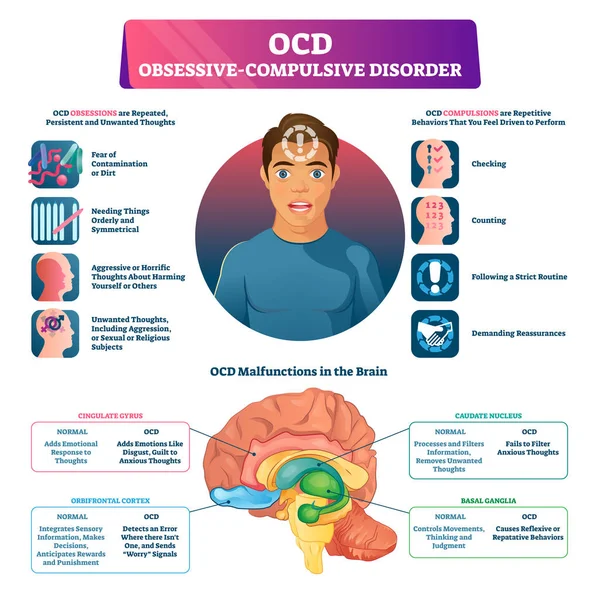
Obsessions are repeated thoughts, urges, or mental images that cause anxiety. Common symptoms include:
- Fear of germs or contamination
- Unwanted forbidden or taboo thoughts involving sex, religion, or harm
- Aggressive thoughts towards others or self
- Having things symmetrical or in a perfect order
Compulsions are repetitive behaviors that a person with OCD feels the urge to do in response to an obsessive thought. Common compulsions include:
- Excessive cleaning and/or handwashing
- Ordering and arranging things in a particular, precise way
- Repeatedly checking on things, such as repeatedly checking to see if the door is locked or that the oven is off
- Compulsive counting
Not all rituals or habits are compulsions. Everyone double checks things sometimes. But a person with OCD generally:
- Can't control his or her thoughts or behaviors, even when those thoughts or behaviors are recognized as excessive
- Spends at least 1 hour a day on these thoughts or behaviors
- Doesn’t get pleasure when performing the behaviors or rituals, but may feel brief relief from the anxiety the thoughts cause
- Experiences significant problems in their daily life due to these thoughts or behaviors
Some individuals with OCD also have a tic disorder. Motor tics are sudden, brief, repetitive movements, such as eye blinking and other eye movements, facial grimacing, shoulder shrugging, and head or shoulder jerking. Common vocal tics include repetitive throat-clearing, sniffing, or grunting sounds.
Common vocal tics include repetitive throat-clearing, sniffing, or grunting sounds.
Symptoms may come and go, ease over time, or worsen. People with OCD may try to help themselves by avoiding situations that trigger their obsessions, or they may use alcohol or drugs to calm themselves. Although most adults with OCD recognize that what they are doing doesn’t make sense, some adults and most children may not realize that their behavior is out of the ordinary. Parents or teachers typically recognize OCD symptoms in children.
If you think you have OCD, talk to your health care provider about your symptoms. If left untreated, OCD can interfere in all aspects of life.
Risk Factors
OCD is a common disorder that affects adults, adolescents, and children all over the world. Most people are diagnosed by about age 19, typically with an earlier age of onset in boys than in girls, but onset after age 35 does happen. For statistics on OCD in adults, please see the NIMH Obsessive-Compulsive Disorder webpage.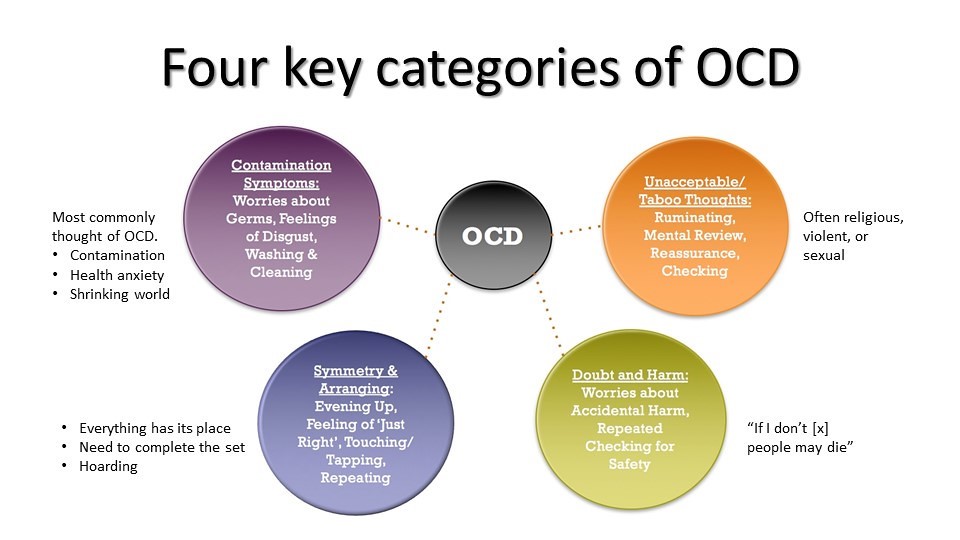
The causes of OCD are unknown, but risk factors include:
Genetics
Twin and family studies have shown that people with first-degree relatives (such as a parent, sibling, or child) who have OCD are at a higher risk for developing OCD themselves. The risk is higher if the first-degree relative developed OCD as a child or teen. Ongoing research continues to explore the connection between genetics and OCD and may help improve OCD diagnosis and treatment.
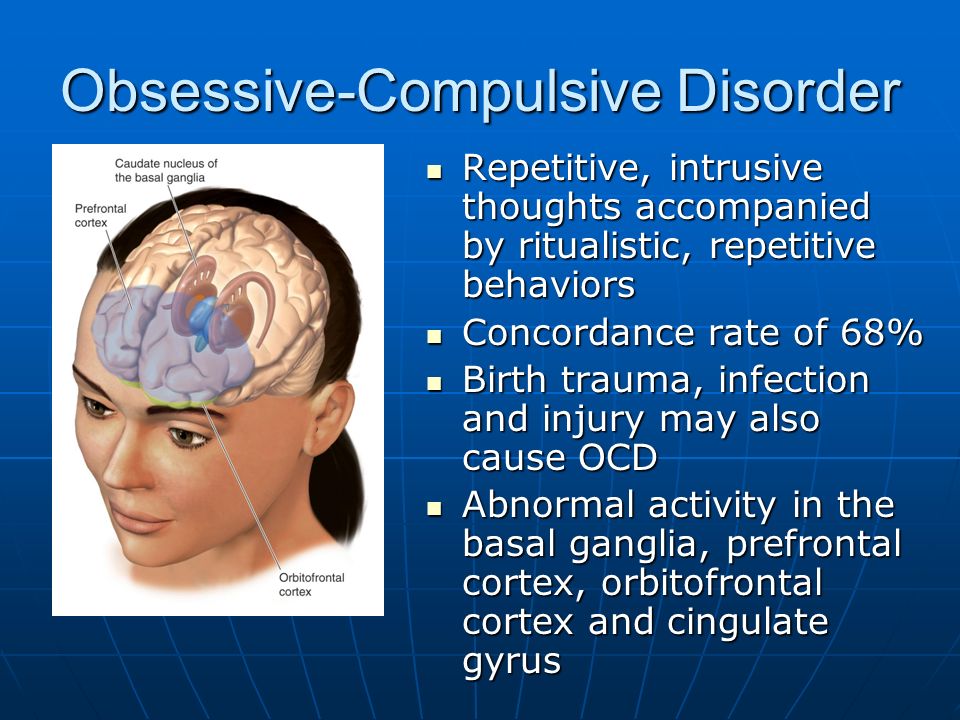
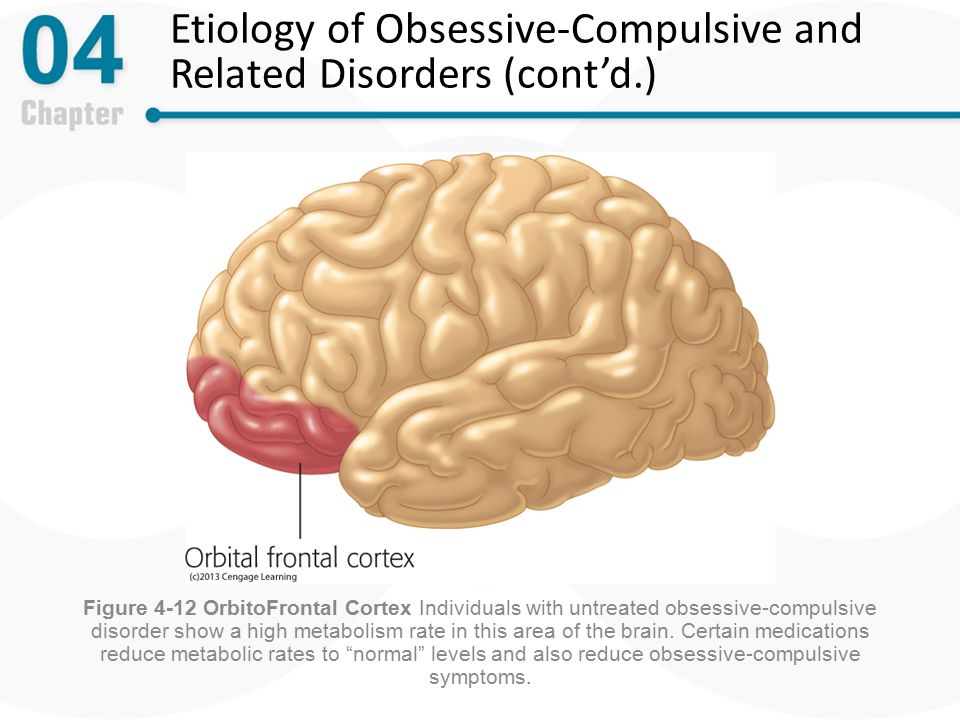
Brain Structure and Functioning
Imaging studies have shown differences in the frontal cortex and subcortical structures of the brain in patients with OCD. There appears to be a connection between the OCD symptoms and abnormalities in certain areas of the brain, but that connection is not clear. Research is still underway. Understanding the causes will help determine specific, personalized treatments to treat OCD.
Environment
An association between childhood trauma and obsessive-compulsive symptoms has been reported in some studies. More research is needed to understand this relationship better.
More research is needed to understand this relationship better.
In some cases, children may develop OCD or OCD symptoms following a streptococcal infection—this is called Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections (PANDAS). For more information, please read NIMH's fact sheet on PANDAS.
Treatments and Therapies
OCD is typically treated with medication, psychotherapy, or a combination of the two. Although most patients with OCD respond to treatment, some patients continue to experience symptoms.
Sometimes people with OCD also have other mental disorders, such as anxiety, depression, and body dysmorphic disorder, a disorder in which someone mistakenly believes that a part of their body is abnormal. It is important to consider these other disorders when making decisions about treatment.
Medication
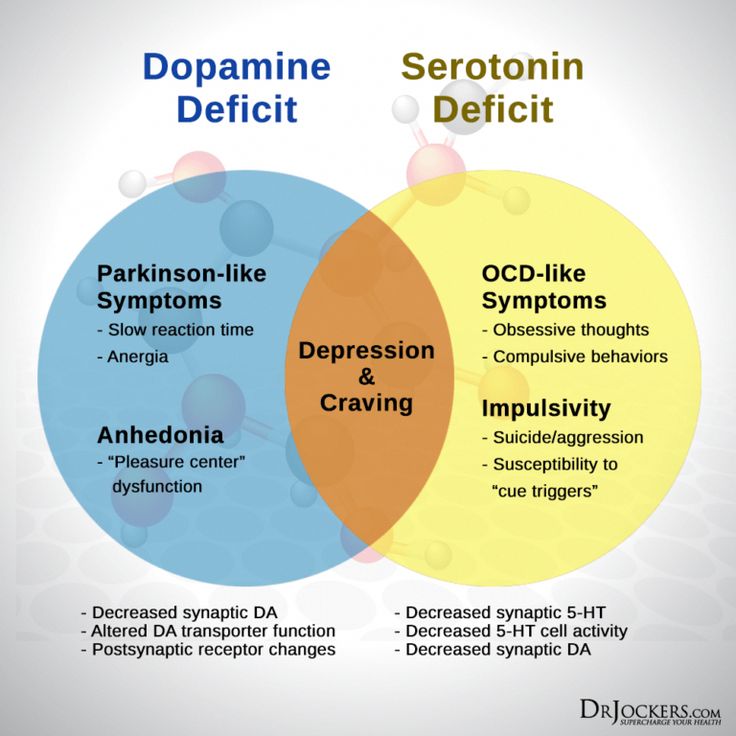
Serotonin reuptake inhibitors (SRIs), which include selective serotonin reuptake inhibitors (SSRIs) are used to help reduce OCD symptoms.
SRIs often require higher daily doses in the treatment of OCD than of depression and may take 8 to 12 weeks to start working, but some patients experience more rapid improvement.
If symptoms do not improve with these types of medications, research shows that some patients may respond well to an antipsychotic medication. Although research shows that an antipsychotic medication may help manage symptoms for people who have both OCD and a tic disorder, research on the effectiveness of antipsychotics to treat OCD is mixed.
If you are prescribed a medication, be sure you:
- Talk with your health care provider or a pharmacist to make sure you understand the risks and benefits of the medications you're taking.
- Do not stop taking a medication without talking to your health care provider first. Suddenly stopping a medication may lead to "rebound" or worsening of OCD symptoms. Other uncomfortable or potentially dangerous withdrawal effects are also possible.
- Report any concerns about side effects to your health care provider right away.
 You may need a change in the dose or a different medication.
You may need a change in the dose or a different medication. - Report serious side effects to the U.S. Food and Drug Administration (FDA) MedWatch Adverse Event Reporting program online or by phone at 1-800-332-1088. You or your health care provider may send a report.
Other medications have been used to treat OCD, but more research is needed to show the benefit of these options. For basic information about these medications, you can visit the NIMH Mental Health Medications webpage. For the most up-to-date information on medications, side effects, and warnings, visit the FDA website.
Psychotherapy
Psychotherapy can be an effective treatment for adults and children with OCD. Research shows that certain types of psychotherapy, including cognitive behavior therapy (CBT) and other related therapies (e.g., habit reversal training) can be as effective as medication for many individuals. Research also shows that a type of CBT called Exposure and Response Prevention (EX/RP)—spending time in the very situation that triggers compulsions (e.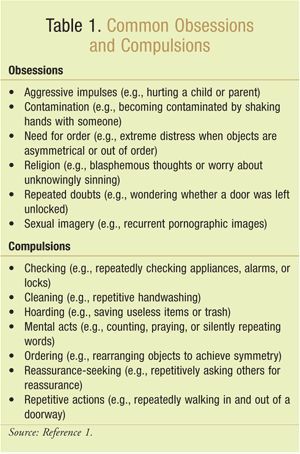 g. touching dirty objects) but then being prevented from undertaking the usual resulting compulsion (e.g. handwashing)—is effective in reducing compulsive behaviors in OCD, even in people who did not respond well to SRI medication.
g. touching dirty objects) but then being prevented from undertaking the usual resulting compulsion (e.g. handwashing)—is effective in reducing compulsive behaviors in OCD, even in people who did not respond well to SRI medication.
As with most mental disorders, treatment is usually personalized and might begin with either medication or psychotherapy, or with a combination of both. For many patients, EX/RP is the add-on treatment of choice when SRIs or SSRIs medication does not effectively treat OCD symptoms or vice versa for individuals who begin treatment with psychotherapy.
Other Treatment Options
In 2018, the FDA approved Transcranial Magnetic Stimulation (TMS) as an adjunct in the treatment of OCD in adults.
NIMH is supporting research into other new treatment approaches for people whose OCD does not respond well to the usual therapies. These new approaches include combination and add-on (augmentation) treatments, as well as novel techniques such as deep brain stimulation. You can learn more about brain stimulation therapies on the NIMH website.
You can learn more about brain stimulation therapies on the NIMH website.
Finding Treatment
For general information on mental health and to locate treatment services in your area, call the Substance Abuse and Mental Health Services Administration (SAMHSA) Treatment Referral Helpline at 1-800-662-HELP (4357). SAMHSA also has a Behavioral Health Treatment Locator on its website that can be searched by location. You can also visit the NIMH’s Help for Mental Illnesses page for more information and resources.
Join a Study
Clinical trials are research studies that look at new ways to prevent, detect, or treat diseases and conditions. The goal of clinical trials is to determine if a new test or treatment works and is safe. Although individuals may benefit from being part of a clinical trial, participants should be aware that the primary purpose of a clinical trial is to gain new scientific knowledge so that others may be better helped in the future.
Researchers at NIMH and around the country conduct many studies with patients and healthy volunteers. We have new and better treatment options today because of what clinical trials uncovered years ago. Be part of tomorrow’s medical breakthroughs. Talk to your health care provider about clinical trials, their benefits and risks, and whether one is right for you.
We have new and better treatment options today because of what clinical trials uncovered years ago. Be part of tomorrow’s medical breakthroughs. Talk to your health care provider about clinical trials, their benefits and risks, and whether one is right for you.
To learn more or find a study, visit:
- NIMH’s Clinical Trials webpage: Information about participating in clinical trials
- Clinicaltrials.gov: Current Studies on OCD: List of clinical trials funded by the National Institutes of Health (NIH) being conducted across the country
Learn More
Free Booklets and Brochures
- Obsessive-Compulsive Disorder: When Unwanted Thoughts Take Over: This brochure provides information on OCD including signs and symptoms, causes, and treatment options such as psychotherapy and medication. Also available en español.
Federal Resources
- Obsessive-Compulsive Disorder (MedlinePlus – also en español)
Research and Statistics
- Journal Articles: This webpage provides information on references and abstracts from MEDLINE/PubMed (National Library of Medicine).

- OCD Statistics: Adults: This webpage lists information on the prevalence of OCD among adults.
Last Reviewed: September 2022
Unless otherwise specified, NIMH information and publications are in the public domain and available for use free of charge. Citation of NIMH is appreciated. Please see our Citing NIMH Information and Publications page for more information.
Obsessive-compulsive disorder (OCD) - Symptoms and causes
Overview
Obsessive-compulsive disorder (OCD) features a pattern of unwanted thoughts and fears (obsessions) that lead you to do repetitive behaviors (compulsions). These obsessions and compulsions interfere with daily activities and cause significant distress.
You may try to ignore or stop your obsessions, but that only increases your distress and anxiety. Ultimately, you feel driven to perform compulsive acts to try to ease your stress. Despite efforts to ignore or get rid of bothersome thoughts or urges, they keep coming back.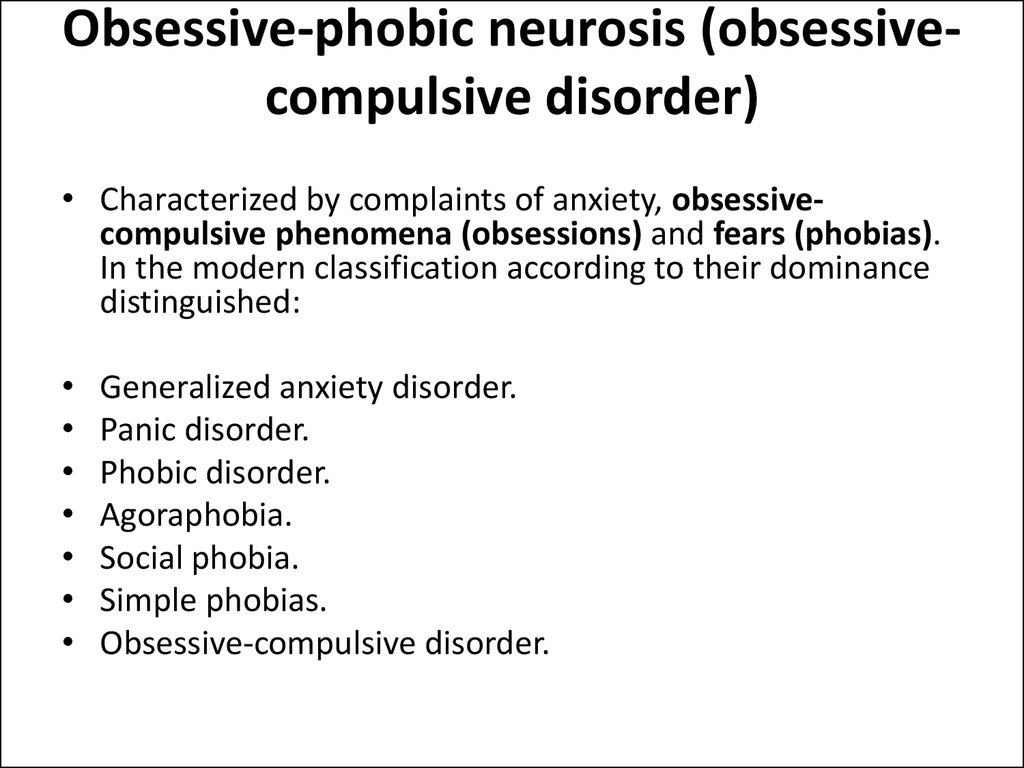 This leads to more ritualistic behavior — the vicious cycle of OCD.
This leads to more ritualistic behavior — the vicious cycle of OCD.
OCD often centers around certain themes — for example, an excessive fear of getting contaminated by germs. To ease your contamination fears, you may compulsively wash your hands until they're sore and chapped.
If you have OCD, you may be ashamed and embarrassed about the condition, but treatment can be effective.
Symptoms
Obsessive-compulsive disorder usually includes both obsessions and compulsions. But it's also possible to have only obsession symptoms or only compulsion symptoms. You may or may not realize that your obsessions and compulsions are excessive or unreasonable, but they take up a great deal of time and interfere with your daily routine and social, school or work functioning.
Obsession symptoms
OCD obsessions are repeated, persistent and unwanted thoughts, urges or images that are intrusive and cause distress or anxiety. You might try to ignore them or get rid of them by performing a compulsive behavior or ritual. These obsessions typically intrude when you're trying to think of or do other things.
You might try to ignore them or get rid of them by performing a compulsive behavior or ritual. These obsessions typically intrude when you're trying to think of or do other things.
Obsessions often have themes to them, such as:
- Fear of contamination or dirt
- Doubting and having difficulty tolerating uncertainty
- Needing things orderly and symmetrical
- Aggressive or horrific thoughts about losing control and harming yourself or others
- Unwanted thoughts, including aggression, or sexual or religious subjects
Examples of obsession signs and symptoms include:
- Fear of being contaminated by touching objects others have touched
- Doubts that you've locked the door or turned off the stove
- Intense stress when objects aren't orderly or facing a certain way
- Images of driving your car into a crowd of people
- Thoughts about shouting obscenities or acting inappropriately in public
- Unpleasant sexual images
- Avoidance of situations that can trigger obsessions, such as shaking hands
Compulsion symptoms
OCD compulsions are repetitive behaviors that you feel driven to perform.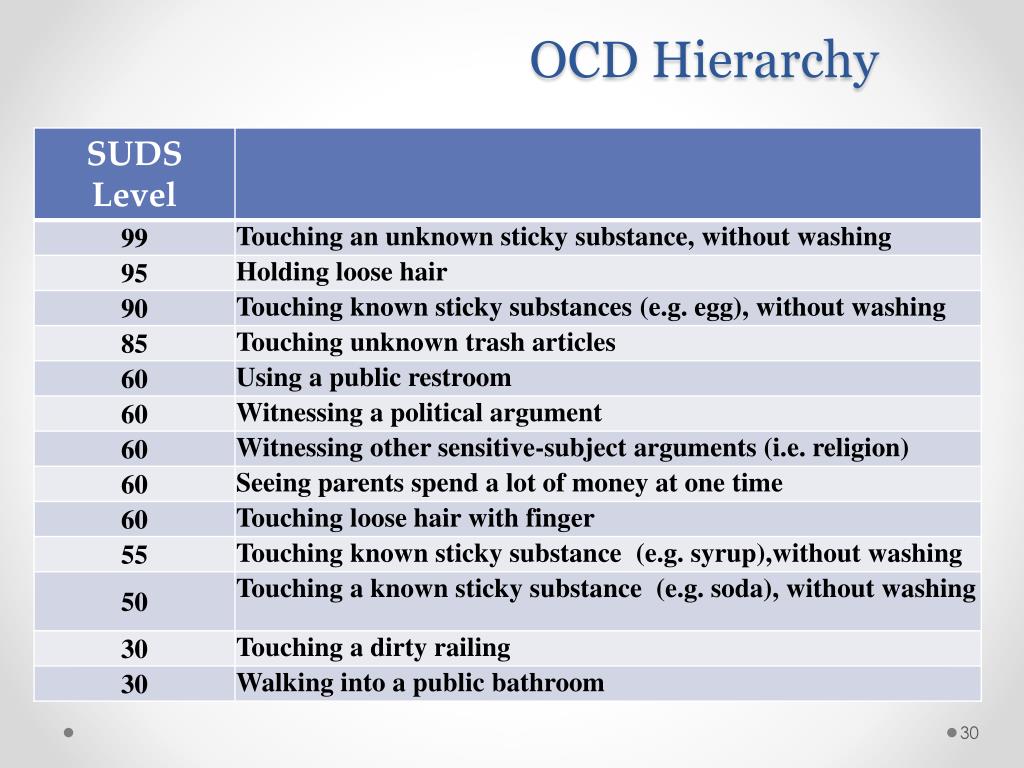 These repetitive behaviors or mental acts are meant to reduce anxiety related to your obsessions or prevent something bad from happening. However, engaging in the compulsions brings no pleasure and may offer only a temporary relief from anxiety.
These repetitive behaviors or mental acts are meant to reduce anxiety related to your obsessions or prevent something bad from happening. However, engaging in the compulsions brings no pleasure and may offer only a temporary relief from anxiety.
You may make up rules or rituals to follow that help control your anxiety when you're having obsessive thoughts. These compulsions are excessive and often are not realistically related to the problem they're intended to fix.
As with obsessions, compulsions typically have themes, such as:
- Washing and cleaning
- Checking
- Counting
- Orderliness
- Following a strict routine
- Demanding reassurance
Examples of compulsion signs and symptoms include:
- Hand-washing until your skin becomes raw
- Checking doors repeatedly to make sure they're locked
- Checking the stove repeatedly to make sure it's off
- Counting in certain patterns
- Silently repeating a prayer, word or phrase
- Arranging your canned goods to face the same way
Severity varies
OCD usually begins in the teen or young adult years, but it can start in childhood. Symptoms usually begin gradually and tend to vary in severity throughout life. The types of obsessions and compulsions you experience can also change over time. Symptoms generally worsen when you experience greater stress. OCD, usually considered a lifelong disorder, can have mild to moderate symptoms or be so severe and time-consuming that it becomes disabling.
Symptoms usually begin gradually and tend to vary in severity throughout life. The types of obsessions and compulsions you experience can also change over time. Symptoms generally worsen when you experience greater stress. OCD, usually considered a lifelong disorder, can have mild to moderate symptoms or be so severe and time-consuming that it becomes disabling.
When to see a doctor
There's a difference between being a perfectionist — someone who requires flawless results or performance, for example — and having OCD. OCD thoughts aren't simply excessive worries about real problems in your life or liking to have things clean or arranged in a specific way.
If your obsessions and compulsions are affecting your quality of life, see your doctor or mental health professional.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.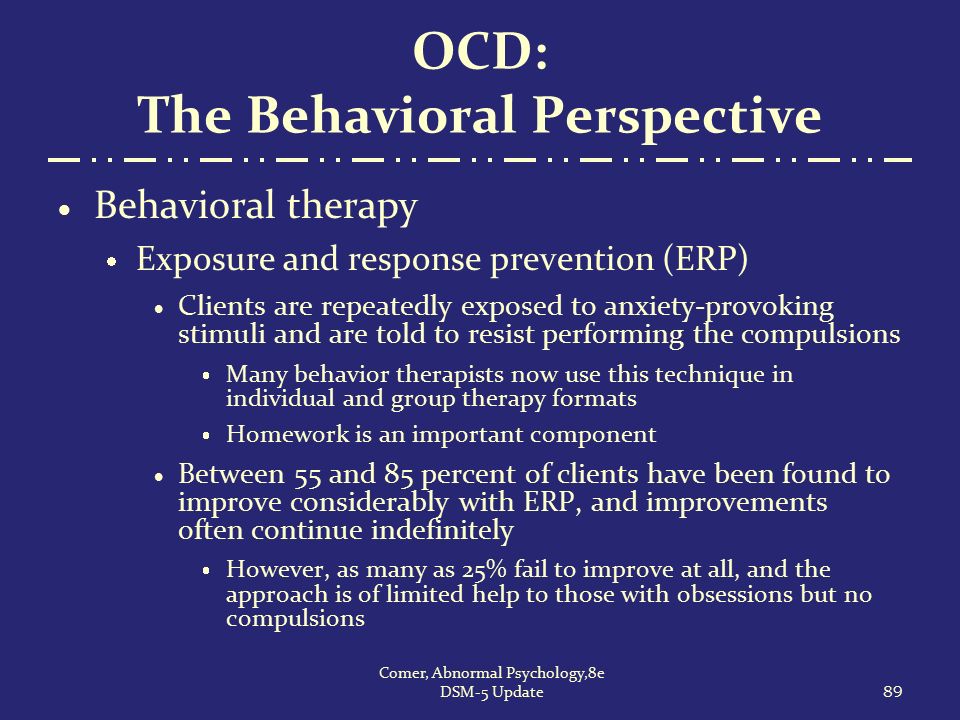
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Causes
The cause of obsessive-compulsive disorder isn't fully understood. Main theories include:
- Biology.
 OCD may be a result of changes in your body's own natural chemistry or brain functions.
OCD may be a result of changes in your body's own natural chemistry or brain functions. - Genetics. OCD may have a genetic component, but specific genes have yet to be identified.
- Learning. Obsessive fears and compulsive behaviors can be learned from watching family members or gradually learned over time.
Risk factors
Factors that may increase the risk of developing or triggering obsessive-compulsive disorder include:
- Family history. Having parents or other family members with the disorder can increase your risk of developing OCD.
- Stressful life events. If you've experienced traumatic or stressful events, your risk may increase. This reaction may, for some reason, trigger the intrusive thoughts, rituals and emotional distress characteristic of OCD.

- Other mental health disorders. OCD may be related to other mental health disorders, such as anxiety disorders, depression, substance abuse or tic disorders.
Complications
Problems resulting from obsessive-compulsive disorder may include, among others:
- Excessive time spent engaging in ritualistic behaviors
- Health issues, such as contact dermatitis from frequent hand-washing
- Difficulty attending work, school or social activities
- Troubled relationships
- Overall poor quality of life
- Suicidal thoughts and behavior
Prevention
There's no sure way to prevent obsessive-compulsive disorder. However, getting treatment as soon as possible may help prevent OCD from worsening and disrupting activities and your daily routine.
By Mayo Clinic Staff
Related
Associated Procedures
Obsessive Compulsive Disorder (OCD): what it is, symptoms, treatment, advice from a doctor Some people develop symptoms during adolescence, although they are usually diagnosed in adults.
 Obsessive-compulsive disorder can significantly interfere with a fulfilling life, but treatment can help keep it under control.
Obsessive-compulsive disorder can significantly interfere with a fulfilling life, but treatment can help keep it under control. Let's figure out together with experts what are the causes of OCD, what therapeutic and drug methods are used by doctors, and how to behave relatives of a person who has been diagnosed with this disorder.
Contents
- What it is
- Signs and symptoms
- Causes
- Diagnosis
- How to treat
- Advice for relatives 902 support groups
- obsessions - persistent thoughts or impulses, intrusive and unacceptable, causing anxiety;
- compulsions are rituals that are built into the thoughts of a person, he considers it necessary to perform them in response to an obsession.
- present daily;
- are uncontrollable;
- are not enjoyable;
- affect work and social life.
- Checks if the door is locked, if the iron and oven are switched off.
- Unreasonably suspects undiagnosed health conditions such as pregnancy or schizophrenia.
- Afraid of germs, things that can be dirty, constantly cleaning.
- Strives for excessive symmetry and order, feels the need to arrange things in a certain way: by size, colors or alphabet.
- Cannot drive obsessive thoughts and ideas away from himself. Some of them can be violent or disturbing.
- Genetics. If you have OCD in your next of kin—father, mother, brother, and sister—the chances are high that you have it too.
- Structure and function of the brain. In the brain of OCD sufferers, increased activity is recorded in the region of the cortico-striatal-thalamo-cortical loop [5].
- Environment. High levels of stress, increased anxiety can also be a trigger for the development of obsessive-compulsive disorder.
- Concomitant diseases. OCD is often diagnosed in parallel with eating disorders and depression [6].
- Traumatic events. The disorder can be the result of difficult circumstances experienced: psychological and sexual abuse, physical trauma, loss of loved ones.
- Infections. Occasionally, OCD is found in children who have had a streptococcal infection.
 This is called pediatric autoimmune neuropsychiatric disorders.
This is called pediatric autoimmune neuropsychiatric disorders. - Do you experience obsessive thoughts about possible tragic events, death, serious illnesses, fires, accidents?
- Are you concerned about the possibility of contamination with germs and chemicals?
- Do you unnecessarily re-read emails or text messages before or after sending them?
- Are you obsessed with keeping everything in order (cataloging books, perfect stacks of clothes in your closet, sized pencils on your desk)?
- Do you repeat routine activities such as opening a door, putting on your shoes, or getting into bed over and over again until you feel like you've done it "right"?
- Do you have recurring inappropriate thoughts (often of a religious, violent, or sexual nature) that seem intrusive and out of control?
- Do you feel the need to constantly seek confirmation of what you have said or done?
- Do you follow ritualized washing, cleaning or personal grooming habits (eg washing your hands five times in a row)?
- Do you avoid certain colors or numbers because you consider them "unlucky"?
- Do you check your trash before throwing it away to make sure it's clean?
- Do you worry about doing something out of a senseless urge, like pushing a stranger or hitting a loved one?
- Do you check oven handles, door locks and car brakes over and over again in a short period of time?
- Anxiety and Depression Association of America (ADAA) - mental health resources, including conferences of the International OCD Foundation.
 There are online support groups for those with the disorder.
There are online support groups for those with the disorder. - OCD Peers - Virtual support groups (6-10 members) using a HIPAA compliant platform. Video conferences with group mentor, open discussions and agenda. All groups are paid.
- 7 cups - on the platform you can find a volunteer who will be in touch and ready to listen to the problem. This is not a qualified professional, but sometimes speaking out to an attentive listener is just as important as working through a problem with a licensed psychotherapist.
- Support Groups - A free resource with several hundred support groups on a variety of topics, including those for OCD sufferers. Groups are moderated to avoid bullying and inappropriate user reactions.
- HealthUnlocked - literally "health unlocked" - a resource with forums to support people with various diseases. The ROC topic is moderated not only by the portal administrators, but also by representatives of the International ROC Foundation.

- Frightening images and drives
- Compulsive acts (rituals)
- Obsessive Self Check
- Fear of trouble, pollution or contamination
- Inexplicable desire to count something
- Excessive organization and pedantry
- Perfectionism in relationships, work and even leisure
- "Stuck", "looping" on one's thoughts
- An exaggerated sense of danger. Fear of the materiality of thoughts:
- "now I will lose control and hurt my loved ones"
- "something terrible is about to happen, I can feel it"
- "I shouldn't think like that, all this will come true because of me"
- Pathological fear of pollution. Thirst for Purity
- Excessive perfectionism, exaggerated responsibility - "everything must be done perfectly", "everything depends on me, mistakes are unacceptable"
- Constant or fluctuating anxiety
- The need to perform certain ritualized actions
- Persistent decline in quality of life due to the need to avoid certain thoughts and actions, places and events
- Significant problems in studies and career
- Failure to establish a serious relationship
- Constant criticism and pressure from relatives
- Many senseless activities
- Excessive involvement in computer games and the Internet, alcohol
- Loneliness and isolation
- Priority:
- Cognitive-Behavioral Therapy.
- Schema Therapy.
- Reality Therapy.
- Choice Theory.
- Rational pharmacotherapy.
- Psychopharmacotherapy (by indications)
- Biofeedback Therapy
- Rational psychocorrection of stress
- Jacobson Progressive Muscle Relaxation.
- Traditional and modern gymnastic systems, relaxation techniques.
- Breathing techniques .
- Stress exposure.
- Self-control training.
- Lifestyle modification
- Working with bad habits.
- Diet correction.
- Professional and social adaptation.
- diagnostics,
- work with disease symptoms,
- work with the causes of the disease,
- consolidation of the achieved results.
- self-control and self-regulation
- constructive body analysis
- understanding one's own mental and emotional sphere
- ability to control one's attention
- ability to act consciously in stressful situations
What is obsessive-compulsive disorder?
Unsplash
Obsessive-compulsive disorder is a common chronic and long-term condition in which a person has uncontrollable repetitive, obsessive thoughts (ideas) and/or actions (behaviors) [1]. OCD is diagnosed in 1.3% of the world's population [2].
Many people confuse OCD with nail biting or negative thinking. Both can be a sign of the disease, but other diagnostic criteria must be taken into account. The obsession is often that a person considers certain numbers or colors to be "good" or "bad". It happens that the habit with OCD is washing your hands repeatedly after touching something that is considered dirty, infected, dangerous. Although the person does not want to think or do it, he is unable to stop [3].
The obsession is often that a person considers certain numbers or colors to be "good" or "bad". It happens that the habit with OCD is washing your hands repeatedly after touching something that is considered dirty, infected, dangerous. Although the person does not want to think or do it, he is unable to stop [3].
Vladimir BelovMedical psychologist, child psychologist, consultant suicidologist, leading specialist of the Semeynaya clinic network
“Obsessive Compulsive Disorder is a neuropsychological disorder that always includes two components:
The most common connection between these components is that compulsions are actions whose purpose is to neutralize or reduce the distress caused by obsessions.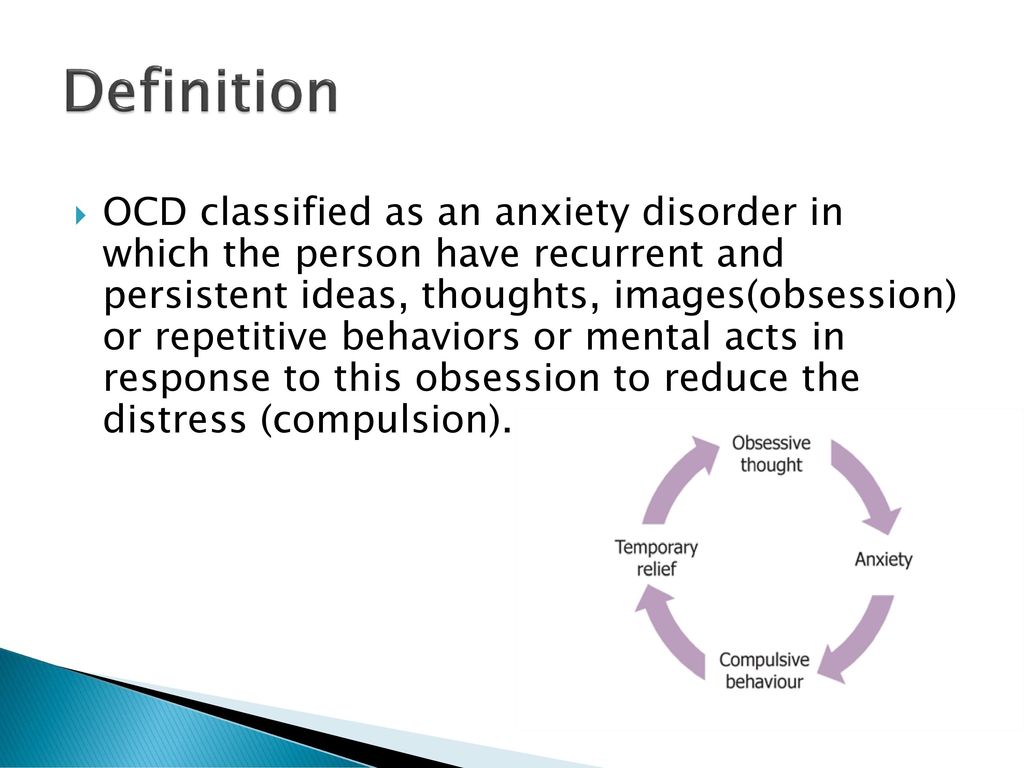 Rituals include such processes as endless washing of hands, double-checking one's own actions or the state of some objects. For some people, these are specific prayers, rituals when going to work, when returning to an apartment, while waiting for transport.
Rituals include such processes as endless washing of hands, double-checking one's own actions or the state of some objects. For some people, these are specific prayers, rituals when going to work, when returning to an apartment, while waiting for transport.
Signs and symptoms of obsessive-compulsive disorder
Unsplash
Obsessions - involuntary thoughts and ideas: "I shook hands with a person and now I can get infected with something." This rumination in itself is perfectly normal, but the person with OCD will wash their hands again and again, unable to get rid of it. This is already a compulsion - an obsessive behavior, an individual unstoppable ritual. In the short term, it reduces anxiety, but the thought returns and the action must be repeated. A person feels that he must do it, while he cannot stop. Everyone has recurring habits or thoughts that recur frequently. But in the case of OCD they are:
It's not unusual to wonder if the curling iron is unplugged. It’s worth worrying if this thought haunts you every day, makes you return home halfway from work and check (more than once, even if you just made sure that the device is not turned on). Obsessive-compulsive disorder comes in many forms, but most cases fall into at least one of the four main categories. The symptoms of OCD are rooted in the person's obsessive behavior. For example, he:
Anastasia AfanasyevaPsychiatrist, psychotherapist, clinical director of the psychological platform Alter
“Intrusive thoughts can occur as part of a variety of disorders, from psychosis to anxiety. To understand what disease these thoughts can be associated with, experts look at how a person treats them. For example, a person in psychosis may not even have a shadow of doubt and discomfort from the fact that the obsessive thought “you can harm your child” is spinning in his head. A person with OCD cannot have this, he will be frightened by such thoughts, and he will try to do everything to prevent this from happening, for example, remove all sharp objects away from him or not approach the child. Discomfort and the feeling that these thoughts are "inadequate", "wrong" will be an important identifying factor that this is OCD.
To understand what disease these thoughts can be associated with, experts look at how a person treats them. For example, a person in psychosis may not even have a shadow of doubt and discomfort from the fact that the obsessive thought “you can harm your child” is spinning in his head. A person with OCD cannot have this, he will be frightened by such thoughts, and he will try to do everything to prevent this from happening, for example, remove all sharp objects away from him or not approach the child. Discomfort and the feeling that these thoughts are "inadequate", "wrong" will be an important identifying factor that this is OCD.
People without disorders can also have obsessive thoughts, but normally we quickly cope with them and they do not disturb life, forcing us to rebuild it for ourselves: the thought appeared - the person brushed it off and moved on.
Causes of OCD
Unsplash
Doctors do not give a specific explanation of the causes of the onset and development of OCD.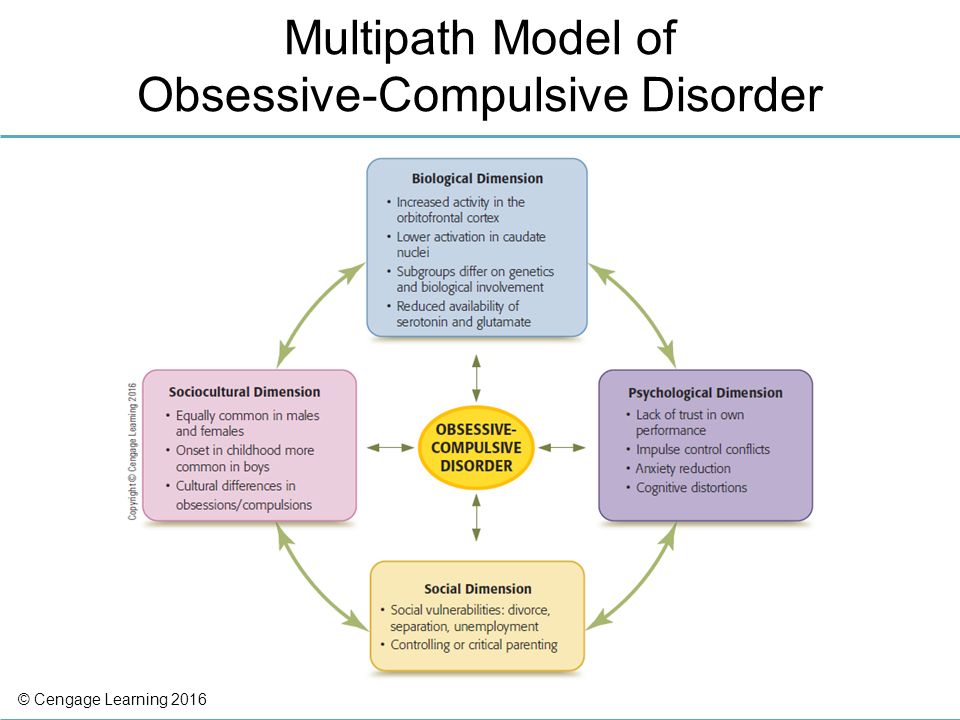 It is most often diagnosed in adolescence and adulthood, with women 1.6 times more likely than men [4]. The factors for the development of the disease include:
It is most often diagnosed in adolescence and adulthood, with women 1.6 times more likely than men [4]. The factors for the development of the disease include:
There is a hypothesis that disturbing deviations developed and persisted in the course of evolution [7]. When people did not have access to modern advances in medicine and hygiene, those who had less contact with a possible source of infection and were constantly on the alert, assessing possible risks and double-checking the safety of food and housing, survived.
Obsessive Compulsive Disorder Diagnostics
Unsplash
All people from time to time find themselves in stressful situations, many people find it helpful to put things in order at home or in the closet, everyone at least once caught himself thinking that he had not turned off the coffee maker in a hurry to a meeting. It doesn't mean you have OCD. Only a doctor can make an accurate diagnosis. Contact a specialist if the above symptoms directly affect your relationship with yourself and others, steal time, do not allow you to relax and enjoy life.![]()
In society, the attitude towards OCD is often superficial and not serious. It is often perceived as a funny feature of a person. But the worsening symptoms cannot be controlled by willpower alone. OCD can be expressed in varying degrees of obsession, and for many it really does not interfere (and may help maintain cleanliness and keep processes under control), but for others it poses a real threat to normal life [8].
There are specialized tests for obsessive-compulsive disorder. Try to answer several questions in the format "often", "rarely", "never", "always":
If most of the described thoughts and situations appear suspiciously often in your daily life, you should consult a general practitioner.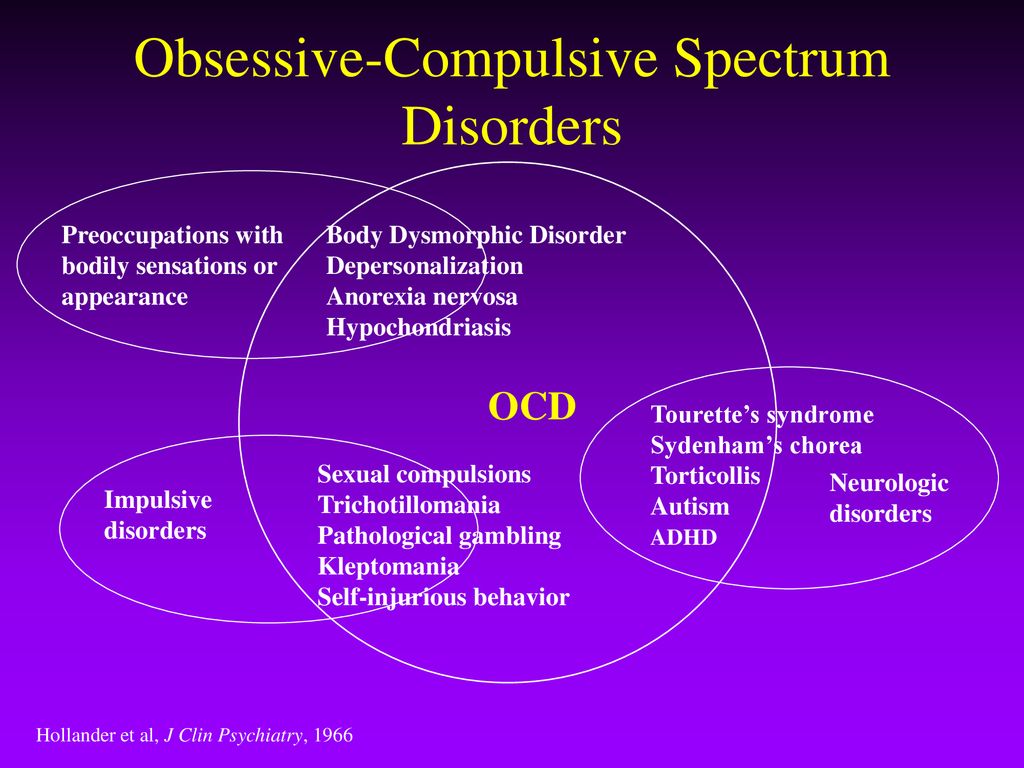 He will conduct a physical examination and order blood tests to make sure that the symptoms are not caused by something else. If OCD is suspected, work with a therapist or psychiatrist to talk about life circumstances, feelings, thoughts, and habits.
He will conduct a physical examination and order blood tests to make sure that the symptoms are not caused by something else. If OCD is suspected, work with a therapist or psychiatrist to talk about life circumstances, feelings, thoughts, and habits.
How to treat obsessive-compulsive disorder
Shutterstock
There is no specific drug that can completely eliminate the symptoms of OCD. But medication support and additional psychological techniques for working on oneself help to work through this problem and keep it under control.
Psychotherapy
Cognitive Behavioral Therapy allows you to change your thinking patterns. Anastasia Afanasyeva believes that one of the most important techniques when working with OCD is distancing, exposing and challenging thoughts: “Distancing is a group of techniques in which we teach a person with OCD to notice intrusive thoughts, realize their ineffectiveness and switch from thinking about them to current ones. affairs. It is important here not to try to start controlling and “not thinking” these thoughts, as this is unrealistic and causes even more anxiety. Instead, for example, we can imagine that thoughts are like an annoying radio broadcast that cannot be turned off, but is not worth listening to.
affairs. It is important here not to try to start controlling and “not thinking” these thoughts, as this is unrealistic and causes even more anxiety. Instead, for example, we can imagine that thoughts are like an annoying radio broadcast that cannot be turned off, but is not worth listening to.
Exposure is the conscious exposure to uncomfortable situations in order to gradually learn to endure stress and stop using rituals that reduce anxiety in the moment, such as double-checking, washing hands, avoiding sharp objects.
Challenging and checking the reality of thoughts helps to understand that often a thought is just a thought and not every thought that comes to mind is worth believing. To assess how true this idea is, you can write it down on a piece of paper and give facts for and against its correctness.
Relaxation
Anxiety and obsessive thoughts are inevitably associated with tension in the body. Available meditation techniques, as well as massage and yoga classes, help to consciously look at the circumstances and cope with stress.
Anastasia Afanasyeva:
“In general, working with anxiety disorders always involves homework, as people learn to cope with their anxiety not only in the psychologist's office, but also in situations that arise in everyday life. Mostly it's working with thoughts and changing behavioral strategies that support OCD or reduce anxiety for only a short time.
The most common treatment for OCD involves individual sessions with a psychotherapist. There are practically no therapy protocols with proven efficacy for groups.”
Medicines
When taking drugs, you can achieve a stable remission. The timing of drug treatment will be determined by the attending physician. Do not stop taking antidepressants at the first sign of improvement.
Vladimir Belov:
“First of all, we need both a psychiatrist and a medical psychologist/psychotherapist. Because, on the one hand, cognitive-behavioral therapy is used, which is quite effective and has a lot of scientific evidence: exposure and prevention of reactions and rituals.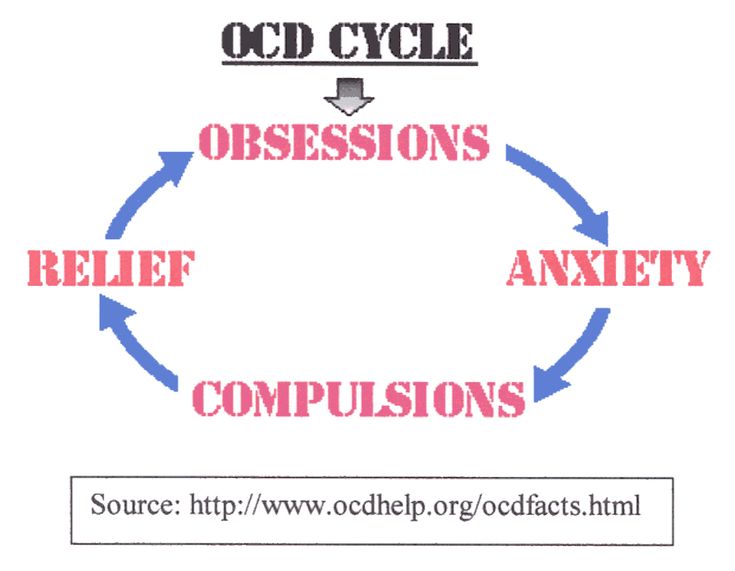 This program goes on for several months and is combined with drugs. First of all, these are antidepressants - selective serotonin reuptake inhibitors and atypical antipsychotic drugs. Much depends on the condition of the patient and the severity of the process in which he is.
This program goes on for several months and is combined with drugs. First of all, these are antidepressants - selective serotonin reuptake inhibitors and atypical antipsychotic drugs. Much depends on the condition of the patient and the severity of the process in which he is.
What to do for relatives of an OCD patient
Unsplash
People who live near a person with OCD often find themselves in difficult conditions. They want to help by interrupting the compulsive manifestations of a loved one, which can create an even more stressful situation for him. But it is also not worth closing your eyes to the disease. Psychologists advise updating it, pronouncing the problem. Develop the emotional intelligence of a loved one: let's understand that he can safely talk to you about any of his feelings. Emphasize that you are always ready to listen and help: “I am with you, we will deal with this problem together.”
Anastasia Afanasyeva:
“If someone in your family suffers from OCD, one of the important tasks that you face is to stay out of the anxiety maintenance cycle. For example, one should not encourage the desire for excessive cleanliness, endless washing of clothes, washing hands, constant fruitless visits to doctors, one should not participate in rechecking any facts. You need to understand that this does not help a loved one cope with anxiety, but reinforces a non-working pattern of behavior and serves as proof that such behavior and thoughts are justified.
For example, one should not encourage the desire for excessive cleanliness, endless washing of clothes, washing hands, constant fruitless visits to doctors, one should not participate in rechecking any facts. You need to understand that this does not help a loved one cope with anxiety, but reinforces a non-working pattern of behavior and serves as proof that such behavior and thoughts are justified.
Forums, support groups for people with OCD
Unsplash
The best option is to contact a trusted doctor and treat according to his recommendations. In addition to medicines and work with a specialist, the fulfillment of independent tasks plays an important role. It is important for people with OCD to talk about the problem and see the support of others. Like-minded forums often help. You can join thematic groups on social networks or contact volunteers:
Share
Materials for Article
Authors
Tags
Irina Rudevich
Treatment of obsessive-compulsive disorder
"Excellent thought" - a program for the treatment of obsessive-compulsive disorder. We will relieve you of obsessive thoughts, movements and rituals. Let's get back to life!
Symptoms of obsessive-compulsive disorder
You feel that over time your mood becomes worse: apathy, depression, obsessions increase, and rituals begin to fill all your free time or harm your physical health.
You may have had more than one meeting with psychologists, psychotherapists and psychiatrists. You are not given the "scary" psychiatric diagnoses of Schizophrenia or Bipolar Disorder, but are prescribed medication and psychotherapy nonetheless. However, such treatment cannot be called effective - the symptoms persist and only aggressive pharmacotherapy temporarily reduces anxiety.
You are not given the "scary" psychiatric diagnoses of Schizophrenia or Bipolar Disorder, but are prescribed medication and psychotherapy nonetheless. However, such treatment cannot be called effective - the symptoms persist and only aggressive pharmacotherapy temporarily reduces anxiety.
What is obsessive-compulsive disorder?
Obsessive-compulsive disorder is a syndrome characterized by the presence of obsessive thoughts (obsessions) to which a person reacts with certain actions (compulsions). The causes of the disorder are rarely superficial. The syndrome is also accompanied by the development of obsessive memories and various pathological phobias. May be chronic, episodic or progressive.
Obsession - obsessive thought, persistent desire for something, uncontrollable and accompanied by anxiety and intense anxiety. In an attempt to cope with such thoughts, a person resorts to committing compulsions.
Compulsion - an irresistible need to perform certain actions (rituals), which can be assessed by the person himself as irrational or meaningless, and the internal need to perform them is forced and is the result of obsessive ideas.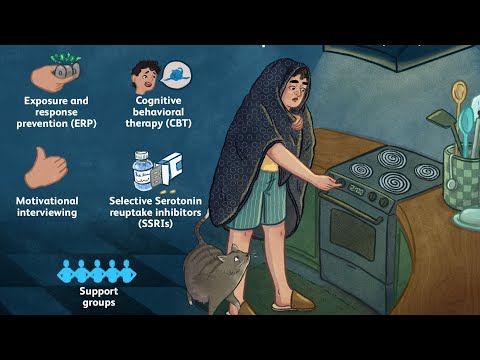
Common examples of OCD
How does this painful algorithm work?
Most people have unwanted or obsessive thoughts quite often, but all sufferers of the disorder greatly exaggerate their importance. Fear of one's own thoughts leads to attempts to neutralize the negative feelings that arise from obsessions, for example by avoiding thought-provoking situations or by engaging in "rituals" of excessive self-cleansing or prayer.
As we noted earlier, repetitive avoidance behavior can "get stuck", "loop", that is, have a tendency to repeat.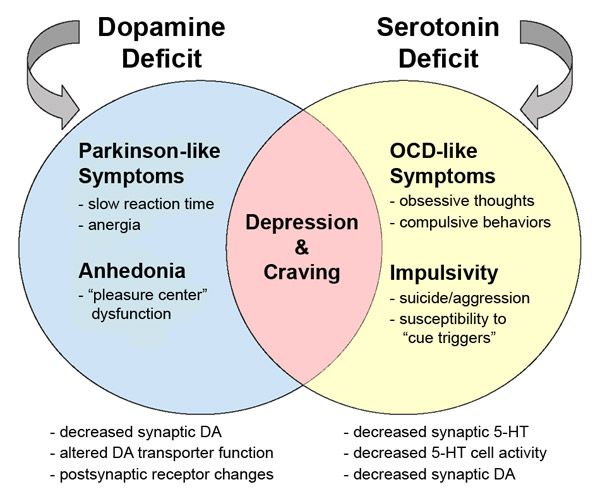 The cause of obsessive-compulsive disorder is the interpretation of intrusive thoughts as catastrophic and true.
The cause of obsessive-compulsive disorder is the interpretation of intrusive thoughts as catastrophic and true.
If you experience periodically over the years:
And you are also persecuted:
We strongly recommend that you do not delay seeking help and that you complete a remedial program. Consultations and psychotherapeutic sessions according to the program are held several times a week, until the relief of severe symptoms, then the frequency of meetings with specialists is reduced to 2–3 per month.
Count on the fact that in the end we will deal with your problem together.
Treatment of obsessive-compulsive disorder in Neuro-Psi
Every day, specialists of the Neuro-Psi clinic analyze the world practice in the field of psychiatry and psychotherapy. The goal is the impartial selection and implementation of those methods of treatment and psychological assistance, the effectiveness of which has been convincingly proven in independent studies.
We are guided by the principles of evidence-based medicine and use as a basic method of treatment a psychotherapeutic paradigm, the effectiveness of which has been widely recognized by the professional community.
1. What is the essence of the obsessive-compulsive disorder treatment program
Since obsessive thoughts, rituals and conditions are only symptoms of mental dysfunction, the root cause must be treated in order to achieve a stable result. A comprehensive work is carried out with the client, taking into account the main factors that create well-being.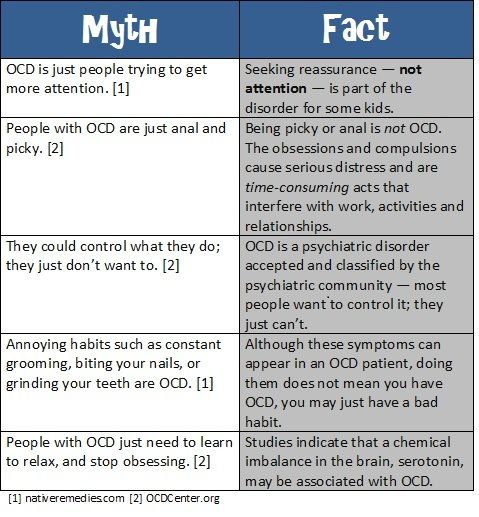
The main emphasis is on teaching the client how to properly respond to his thoughts, emotions, inner feelings and interpretation of external events.
All types of psychotherapeutic and drug treatments serve the same goal: to achieve the best result in the shortest possible time. At the same time, by coordinating the efforts of specialists in various fields, the most complete coverage of all types of mental illnesses, disorders and disorders is possible.
2. What treatments are used
3. How is the treatment under the program
Each treatment program at the NEURO-PSI clinic consists of four stages:
Work efficiency is increased by dividing the treatment process into a predetermined number of sessions, at convenient times and without hospitalization. This means that each program is adapted to the problem that the client has addressed.
The program method of treatment is predictable, time-limited, productive, and, most importantly, understandable for the client.
Of course, the treatment takes place in a comfortable mode without interruption from work, study or family. Specialists of various profiles will work with you (team method). This is necessary to minimize the risk of diagnostic errors that could lead to the adoption of a suboptimal treatment plan.
Specialists of various profiles will work with you (team method). This is necessary to minimize the risk of diagnostic errors that could lead to the adoption of a suboptimal treatment plan.
Improvements in well-being and mood (healing) occur in stages: after the decrease in emotional problems, bodily symptoms decrease. Working with the causes (etiology) of obsessive-compulsive disorder helps to avoid relapses in the future.
4. What are the results and prognosis?
Upon completion of the program, you get rid of obsessive thoughts and rituals, fear of pollution, unmotivated fears, panic attacks and multiple vegetative symptoms (sudden jumps in blood pressure, heart palpitations, dizziness, nausea).
According to statistics, the effectiveness of the methods used approaches 100% if all recommendations of specialists are followed.
Skills you acquire during the program:
Significantly improves the emotional and physical condition, gaining self-confidence, in the future.