Bipolar disorder aging
Does Bipolar Disorder Get Worse With Age?
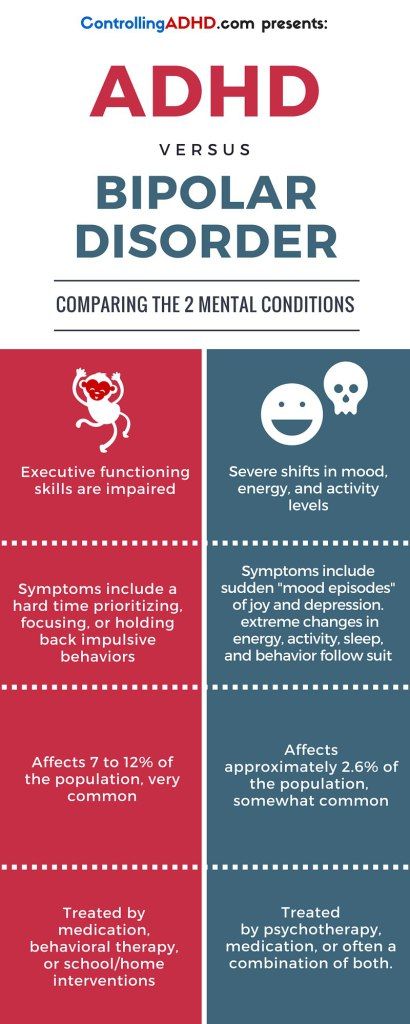
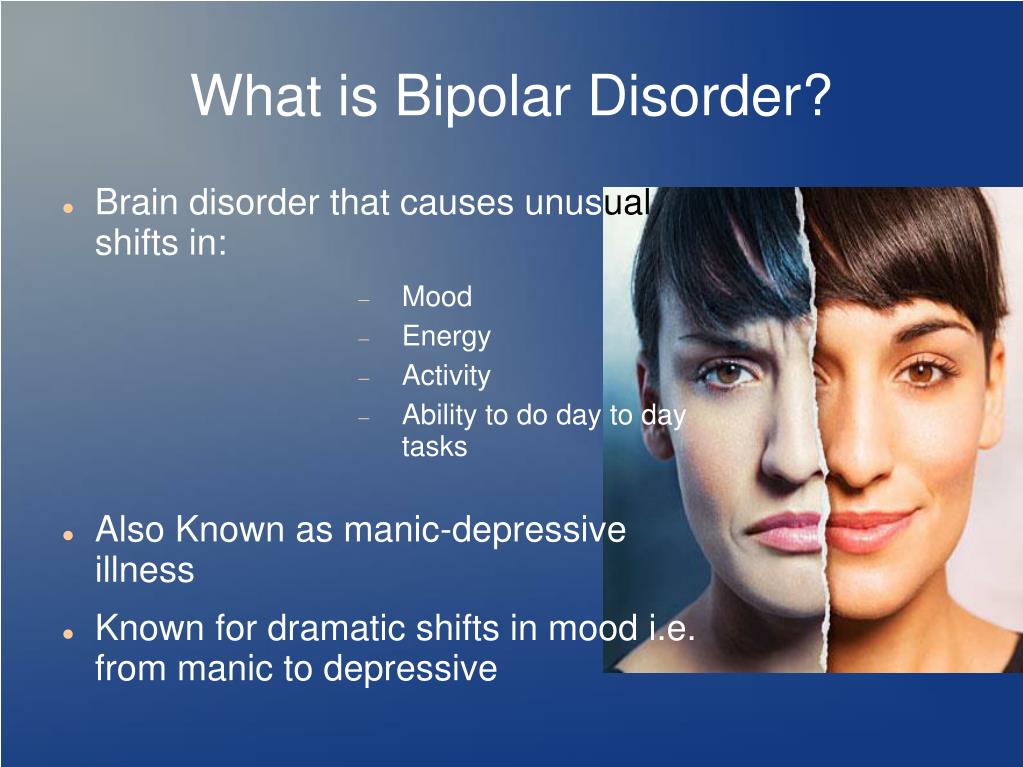
Bipolar disorder is a mental health condition that is characterized by significant shifts in a person’s mood, energy, and concentration.
While the average age of onset for bipolar disorder is 25 years, some people develop the condition much later in life.
About one-quarter of all people with bipolar disorder are 60 years of age or older, and that number is expected to grow to about half by 2030.
While the symptoms of bipolar disorder can vary with age, the frequency, severity, and overall impact of the disorder are generally different in older adults versus younger people.
In this article, we’ll dive into how bipolar disorder changes with age, including how older age can affect symptoms, severity, and overall mental health.
In people living with bipolar disorder, age can affect:
- how symptoms appear
- how severe symptoms are
- how the disorder affects the brain
Although many people with bipolar disorder are diagnosed at an early age, around 5 to 10 percent are ages 50 or older when diagnosed. Only about 0.5 to 1.0 percent of older adults are affected by bipolar I and bipolar II disorders, but the condition accounts for roughly 6 to 10 percent of psychiatric visits in senior communities.
So, how does bipolar disorder appear in older adults versus younger people, and how do the symptoms change as someone ages?
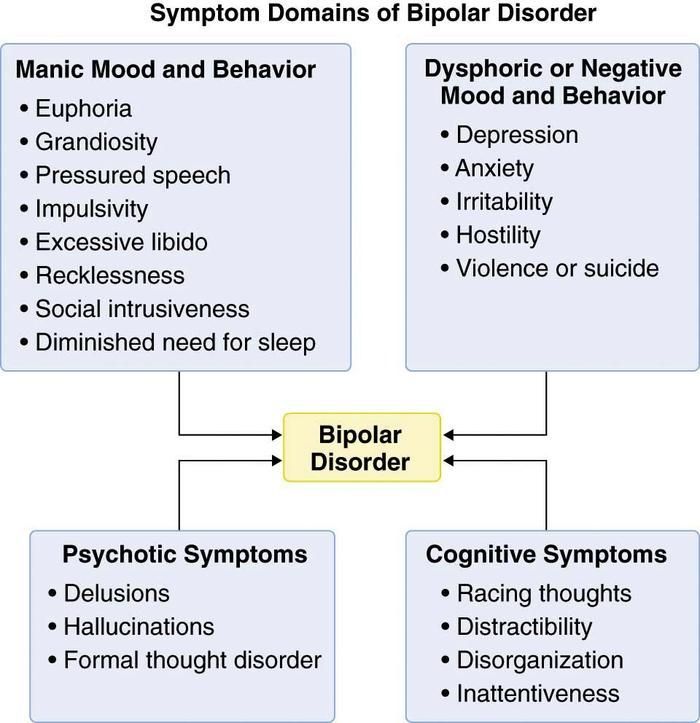
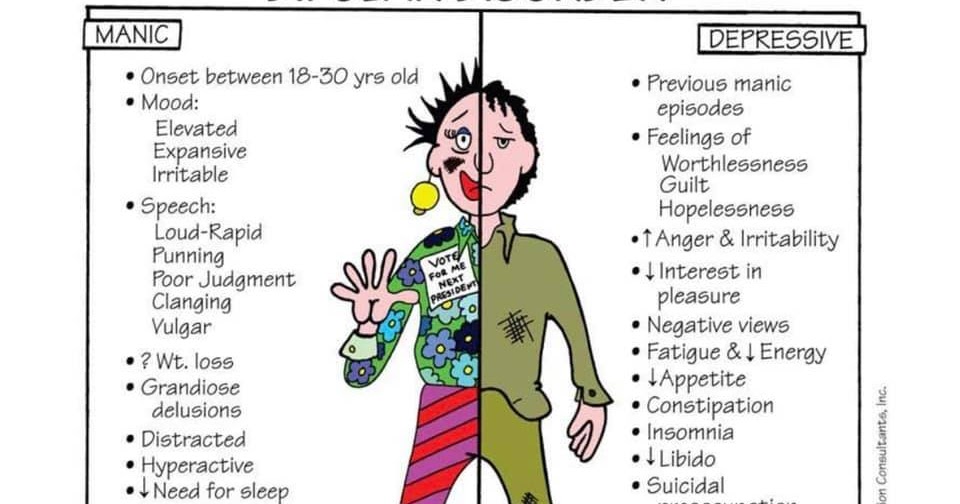
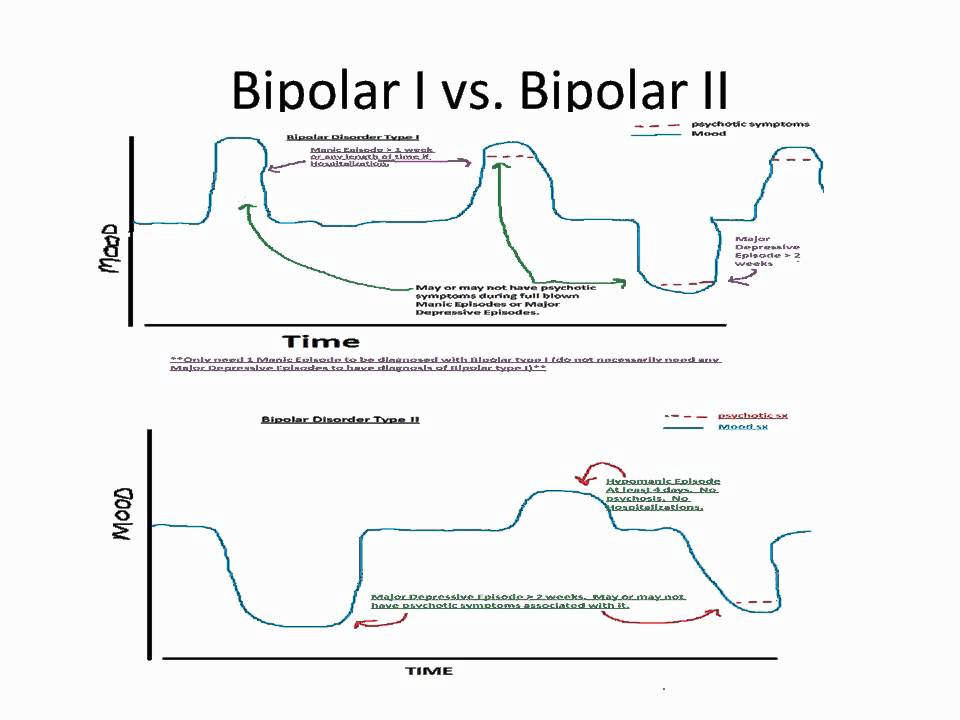
Mood shifts in bipolar disorder lead to distinct episodes that are referred to as:
- Mania: a drastically elevated or “high“ mood
- Hypomania: an elevated state that’s not as extreme as mania
- Depression: a “low“ mood
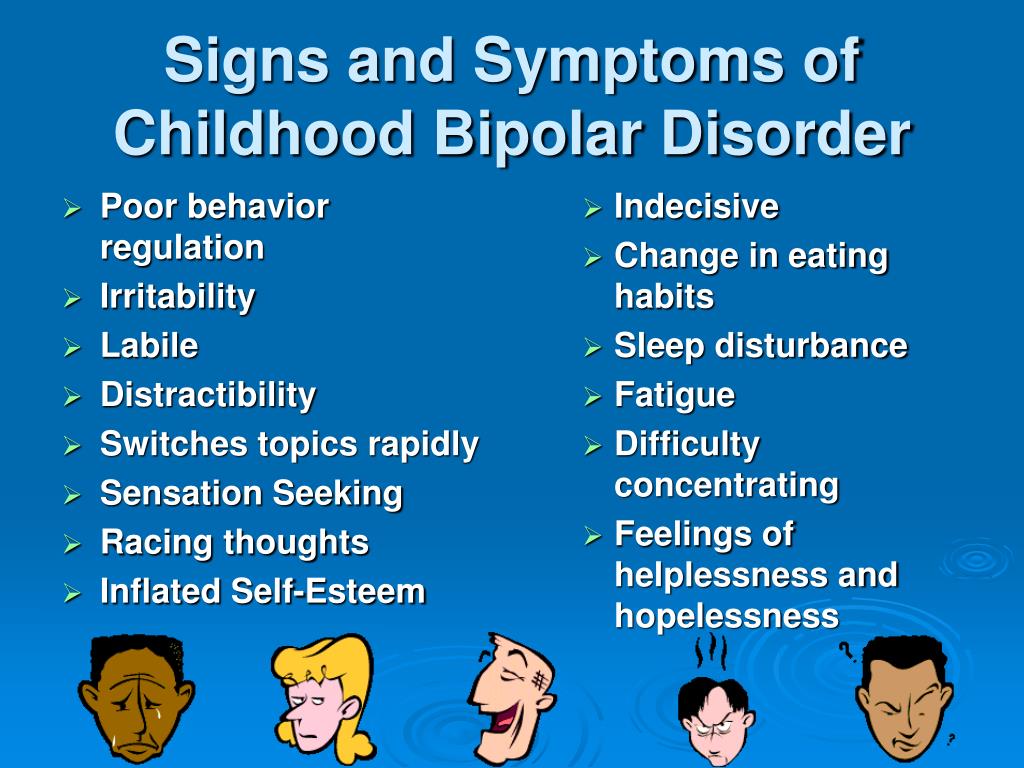
Changes in the frequency and severity of episodes are among the most evident changes in bipolar disorder at an older age. Research suggests that older adults with bipolar disorder often experience:
- more frequent episodes
- more depressive episodes and less time spent in manic or hypomanic states
- less severe manic symptoms and fewer psychotic features with mania
- new symptoms, such as irritability and poor cognition
- lower risk of suicide, although this may be due to survivorship bias
- resistance to treatment options, such as certain medications
Since research on bipolar disorder in older adults is still lacking, it’s difficult to determine exactly how these changes can affect the different types of bipolar disorder.
According to experts, bipolar disorder may speed up aging and contribute to cognitive decline. Older studies have found a link between bipolar disorder and cognitive decline, as well as an increased risk of dementia with each bipolar disorder episode.
While bipolar disorder seems to have a negative effect on executive function and verbal memory in all age groups, older adults are also more likely to be slower at processing information. Because of this, older adults with bipolar disorder may experience lowered neurocognitive ability, which can lead to a much lower quality of life.
Some of these changes may be due to how bipolar disorder affects the tissues within the brain. Many of these neurological changes can also be heightened by a variety of factors, including:
- natural changes of aging
- other medical conditions
- repeated mood episodes
- substance use or misuse
End stage bipolar disorder
Although there is no official classification for end stage bipolar disorder, mild structural changes in the brain that lead to cognitive dysfunction can severely reduce someone’s quality of life, especially toward the end of life.
Research from 2014 shows that older adults with bipolar disorder seem to have much less gray matter in the frontal area of the brain. This area directly contributes to emotional behaviors and emotional regulation. Other studies have also suggested that bipolar disorder may impact other areas of the brain linked to cognition, memory, and more.
So, while many older individuals already experience changes in mood, cognition, and memory as a part of the natural aging process, people with bipolar disorder may experience more intense changes.
Without the right treatment, day-to-day living can be harder, and the overall quality of life may be lower toward the end of life.
If you’ve been diagnosed with bipolar disorder, it’s important to seek treatment for the condition, as it can become progressively worse if left untreated.
Although treatment varies from person to person, doctors usually treat bipolar disorder with both medication and psychotherapy.
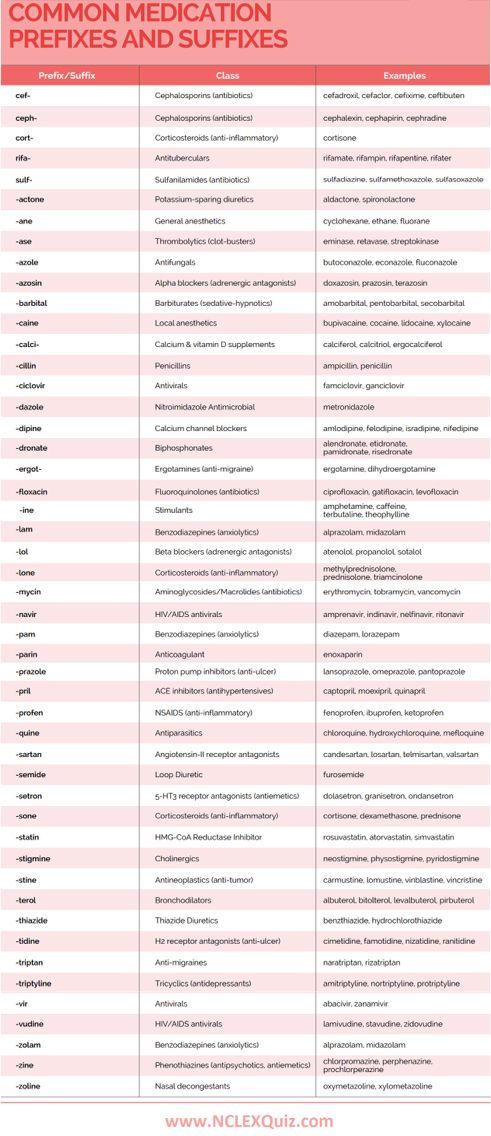
- Medications are often the first-line treatment option for people with bipolar disorder.
 Medications help reduce the chronic (long-term) symptoms of the disorder. Common medication options for bipolar disorder include:
Medications help reduce the chronic (long-term) symptoms of the disorder. Common medication options for bipolar disorder include:- mood stabilizers
- second-generation antipsychotics
- antidepressants
- Psychotherapy is often used along with medication to help reduce the behavioral symptoms of bipolar disorder. Helpful approaches include:
- psychoeducation
- cognitive behavioral therapy (CBT)
- family-focused therapy
As we age, it becomes much more difficult for our bodies to metabolize certain medications. In older adults with bipolar disorder, this can change how traditional mood-stabilizing drugs work.
For example, one study from 2007 found that older participants who were taking lithium or antipsychotic drugs had significantly reduced cognitive functioning. This suggests that older people may be more susceptible to the negative side effects of these medications. With this in mind, it’s important for older adults with bipolar disorder to fully consider the treatment options available to them.
If medication does not help, doctors may suggest electroconvulsive therapy (ECT). During ECT, electrical currents are sent to your brain briefly to stimulate it. It’s usually a last resort to help treat depressive symptoms, but studies have found it effective.
Research from 2015 suggests that older adults with bipolar disorder tend to die 10 years earlier than the general population. This could be because bipolar disorder is often accompanied by other health conditions, such as:
- metabolic syndrome
- hypertension (high blood pressure)
- diabetes
- cardiovascular disease
With the right combination of medication, therapy, and lifestyle changes, people with bipolar disorder might be able to lessen these changes and greatly improve their overall quality of life.
If you’ve been diagnosed with bipolar disorder, it’s important to reach out to a doctor to discuss a treatment plan and find the options that work for you.
Accelerated aging in bipolar disorder: A comprehensive review of molecular findings and their clinical implications
Review
. 2020 May;112:107-116.
2020 May;112:107-116.
doi: 10.1016/j.neubiorev.2020.01.035. Epub 2020 Feb 1.
Gabriel R Fries 1 , Madeline J Zamzow 2 , Taylor Andrews 2 , Omar Pink 2 , Giselli Scaini 2 , Joao Quevedo 3
Affiliations
Affiliations
- 1 Translational Psychiatry Program, Louis A. Faillace, MD, Faillace Department of Psychiatry & Behavioral Sciences, The University of Texas Health Science Center at Houston, 1941 East Rd, 77054 Houston, TX, USA; Center for Precision Health, School of Biomedical Informatics, The University of Texas Health Science Center at Houston.
 7000 Fannin St, 77030 Houston, TX, USA; Neuroscience Graduate Program, The University of Texas MD Anderson Cancer Center UTHealth Graduate School of Biomedical Sciences, Houston, TX, USA. Electronic address: [email protected].
7000 Fannin St, 77030 Houston, TX, USA; Neuroscience Graduate Program, The University of Texas MD Anderson Cancer Center UTHealth Graduate School of Biomedical Sciences, Houston, TX, USA. Electronic address: [email protected]. - 2 Translational Psychiatry Program, Louis A. Faillace, MD, Faillace Department of Psychiatry & Behavioral Sciences, The University of Texas Health Science Center at Houston, 1941 East Rd, 77054 Houston, TX, USA.
- 3 Translational Psychiatry Program, Louis A. Faillace, MD, Faillace Department of Psychiatry & Behavioral Sciences, The University of Texas Health Science Center at Houston, 1941 East Rd, 77054 Houston, TX, USA; Neuroscience Graduate Program, The University of Texas MD Anderson Cancer Center UTHealth Graduate School of Biomedical Sciences, Houston, TX, USA; Translational Psychiatry Laboratory, Graduate Program in Health Sciences, University of Southern Santa Catarina (UNESC), Criciúma, SC, Brazil; Center of Excellence in Mood Disorders, Faillace Department of Psychiatry & Behavioral Sciences, The University of Texas Health Science Center at Houston.
 1941 East Rd, 77054 Houston, TX, USA.
1941 East Rd, 77054 Houston, TX, USA.
- PMID: 32018037
- DOI: 10.1016/j.neubiorev.2020.01.035
Review
Gabriel R Fries et al. Neurosci Biobehav Rev. 2020 May.
. 2020 May;112:107-116.
doi: 10.1016/j.neubiorev.2020.01.035. Epub 2020 Feb 1.
Authors
Gabriel R Fries 1 , Madeline J Zamzow 2 , Taylor Andrews 2 , Omar Pink 2 , Giselli Scaini 2 , Joao Quevedo 3
Affiliations
- 1 Translational Psychiatry Program, Louis A.
 Faillace, MD, Faillace Department of Psychiatry & Behavioral Sciences, The University of Texas Health Science Center at Houston, 1941 East Rd, 77054 Houston, TX, USA; Center for Precision Health, School of Biomedical Informatics, The University of Texas Health Science Center at Houston. 7000 Fannin St, 77030 Houston, TX, USA; Neuroscience Graduate Program, The University of Texas MD Anderson Cancer Center UTHealth Graduate School of Biomedical Sciences, Houston, TX, USA. Electronic address: [email protected].
Faillace, MD, Faillace Department of Psychiatry & Behavioral Sciences, The University of Texas Health Science Center at Houston, 1941 East Rd, 77054 Houston, TX, USA; Center for Precision Health, School of Biomedical Informatics, The University of Texas Health Science Center at Houston. 7000 Fannin St, 77030 Houston, TX, USA; Neuroscience Graduate Program, The University of Texas MD Anderson Cancer Center UTHealth Graduate School of Biomedical Sciences, Houston, TX, USA. Electronic address: [email protected]. - 2 Translational Psychiatry Program, Louis A. Faillace, MD, Faillace Department of Psychiatry & Behavioral Sciences, The University of Texas Health Science Center at Houston, 1941 East Rd, 77054 Houston, TX, USA.
- 3 Translational Psychiatry Program, Louis A. Faillace, MD, Faillace Department of Psychiatry & Behavioral Sciences, The University of Texas Health Science Center at Houston, 1941 East Rd, 77054 Houston, TX, USA; Neuroscience Graduate Program, The University of Texas MD Anderson Cancer Center UTHealth Graduate School of Biomedical Sciences, Houston, TX, USA; Translational Psychiatry Laboratory, Graduate Program in Health Sciences, University of Southern Santa Catarina (UNESC), Criciúma, SC, Brazil; Center of Excellence in Mood Disorders, Faillace Department of Psychiatry & Behavioral Sciences, The University of Texas Health Science Center at Houston.
 1941 East Rd, 77054 Houston, TX, USA.
1941 East Rd, 77054 Houston, TX, USA.
- PMID: 32018037
- DOI: 10.1016/j.neubiorev.2020.01.035
Abstract
Bipolar disorder (BD) has been associated with clinical signs of accelerated aging, which potentially underlies its association with several age-related medical conditions, such as hypertension, metabolic imbalances, dementia, and cancer. This paper aims to comprehensively review evidence of biological aging in BD and explore findings and controversies related to common biological clocks in patients, including telomere length, DNA methylation, mitochondrial DNA copy number, inflammation, and oxidative stress. Our results suggest a complex interplay between biological markers and a potential key role of environmental factors, such as childhood trauma and psychological stress, in determining premature aging in patients.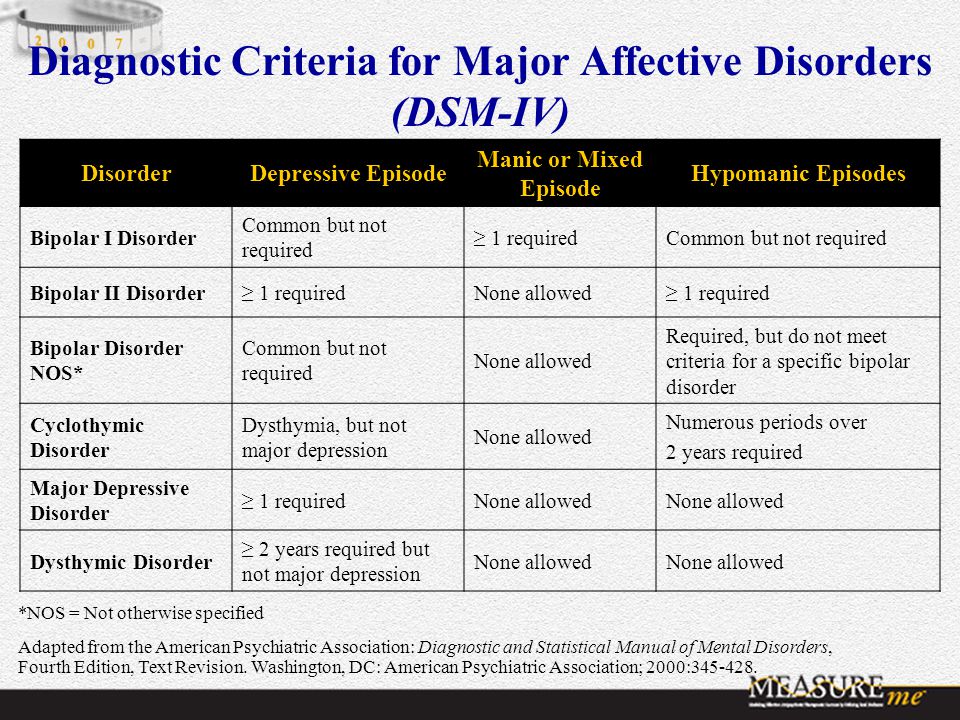 Moreover, given its multifactorial nature, our summary evidences the need for further studies incorporating clinical evidence with biomarkers of accelerated aging in BD. Results of this review strongly suggest BD as an accelerated aging disease seen in both clinical and molecular aspects. Understanding the pathophysiology of aging in BD may ultimately lead to identification of pathways that can be targeted for prevention of premature aging in patients and early onset of aging-related conditions.
Moreover, given its multifactorial nature, our summary evidences the need for further studies incorporating clinical evidence with biomarkers of accelerated aging in BD. Results of this review strongly suggest BD as an accelerated aging disease seen in both clinical and molecular aspects. Understanding the pathophysiology of aging in BD may ultimately lead to identification of pathways that can be targeted for prevention of premature aging in patients and early onset of aging-related conditions.
Keywords: Aging; Bipolar disorder; DNA methylation; Depression; Epigenetics; Inflammation; Mania; Oxidative stress; Telomere length; mtDNA.
Copyright © 2020 Elsevier Ltd. All rights reserved.
Conflict of interest statement
Declaration of Competing Interest None.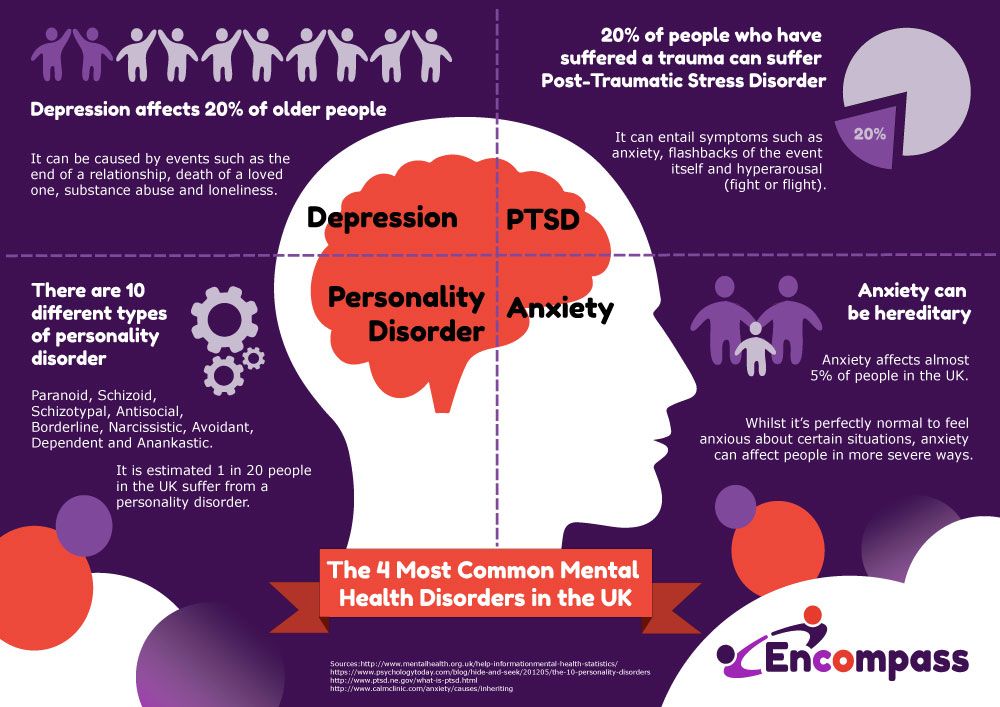
Similar articles
-
Accelerated epigenetic aging and mitochondrial DNA copy number in bipolar disorder.
Fries GR, Bauer IE, Scaini G, Wu MJ, Kazimi IF, Valvassori SS, Zunta-Soares G, Walss-Bass C, Soares JC, Quevedo J. Fries GR, et al. Transl Psychiatry. 2017 Dec 11;7(12):1283. doi: 10.1038/s41398-017-0048-8. Transl Psychiatry. 2017. PMID: 29225347 Free PMC article.
-
The theory of bipolar disorder as an illness of accelerated aging: implications for clinical care and research.
Rizzo LB, Costa LG, Mansur RB, Swardfager W, Belangero SI, Grassi-Oliveira R, McIntyre RS, Bauer ME, Brietzke E. Rizzo LB, et al. Neurosci Biobehav Rev. 2014 May;42:157-69. doi: 10.1016/j.neubiorev.2014.02.004. Epub 2014 Feb 15. Neurosci Biobehav Rev.
 2014. PMID: 24548785 Review.
2014. PMID: 24548785 Review. -
Stress, Telomeres, and Psychopathology: Toward a Deeper Understanding of a Triad of Early Aging.
Epel ES, Prather AA. Epel ES, et al. Annu Rev Clin Psychol. 2018 May 7;14:371-397. doi: 10.1146/annurev-clinpsy-032816-045054. Epub 2018 Mar 1. Annu Rev Clin Psychol. 2018. PMID: 29494257 Free PMC article. Review.
-
Telomere Length, Oxidative Stress, Inflammation and BDNF Levels in Siblings of Patients with Bipolar Disorder: Implications for Accelerated Cellular Aging.
Vasconcelos-Moreno MP, Fries GR, Gubert C, Dos Santos BTMQ, Fijtman A, Sartori J, Ferrari P, Grun LK, Parisi MM, Guma FTCR, Barbé-Tuana FM, Kapczinski F, Rosa AR, Yatham LN, Kauer-Sant'Anna M. Vasconcelos-Moreno MP, et al.
 Int J Neuropsychopharmacol. 2017 Jun 1;20(6):445-454. doi: 10.1093/ijnp/pyx001. Int J Neuropsychopharmacol. 2017. PMID: 28339618 Free PMC article.
Int J Neuropsychopharmacol. 2017 Jun 1;20(6):445-454. doi: 10.1093/ijnp/pyx001. Int J Neuropsychopharmacol. 2017. PMID: 28339618 Free PMC article. -
Shortened telomere length in bipolar disorder: a comparison of the early and late stages of disease.
Barbé-Tuana FM, Parisi MM, Panizzutti BS, Fries GR, Grun LK, Guma FT, Kapczinski F, Berk M, Gama CS, Rosa AR. Barbé-Tuana FM, et al. Braz J Psychiatry. 2016 Oct-Dec;38(4):281-286. doi: 10.1590/1516-4446-2016-1910. Epub 2016 Oct 17. Braz J Psychiatry. 2016. PMID: 27798713 Free PMC article.
See all similar articles
Cited by
-
Lessons from ecology for understanding the heterogeneity of bipolar disorder.
Nunes A, Scott K, Alda M.
 Nunes A, et al. J Psychiatry Neurosci. 2022 Oct 18;47(5):E359-E365. doi: 10.1503/jpn.220172. Print 2022 Sep-Oct. J Psychiatry Neurosci. 2022. PMID: 36257674 Free PMC article. No abstract available.
Nunes A, et al. J Psychiatry Neurosci. 2022 Oct 18;47(5):E359-E365. doi: 10.1503/jpn.220172. Print 2022 Sep-Oct. J Psychiatry Neurosci. 2022. PMID: 36257674 Free PMC article. No abstract available. -
Analysis on in vitro effect of lithium on telomere length in lymphoblastoid cell lines from bipolar disorder patients with different clinical response to long-term lithium treatment.
Squassina A, Meloni A, Congiu D, Bosganas P, Patrinos GP, Lin R, Turecki G, Severino G, Ardau R, Chillotti C, Pisanu C. Squassina A, et al. Hum Genomics. 2022 Oct 17;16(1):45. doi: 10.1186/s40246-022-00418-8. Hum Genomics. 2022. PMID: 36253798 Free PMC article.
-
Neuroimaging Studies of Brain Structure in Older Adults with Bipolar Disorder: A Review.
Rajashekar N, Blumberg HP, Villa LM. Rajashekar N, et al. J Psychiatr Brain Sci. 2022;7(4):e220006. doi: 10.20900/jpbs.20220006. Epub 2022 Aug 25. J Psychiatr Brain Sci. 2022. PMID: 36092855 Free PMC article.
-
Depression, aging, and immunity: implications for COVID-19 vaccine immunogenicity.
Ford BN, Savitz J. Ford BN, et al. Immun Ageing. 2022 Jul 14;19(1):32. doi: 10.1186/s12979-022-00288-7. Immun Ageing. 2022. PMID: 35836263 Free PMC article. Review.
-
Epigenetic GrimAge acceleration and cognitive impairment in bipolar disorder.
Lima CNC, Suchting R, Scaini G, Cuellar VA, Favero-Campbell AD, Walss-Bass C, Soares JC, Quevedo J, Fries GR. Lima CNC, et al. Eur Neuropsychopharmacol.
 2022 Sep;62:10-21. doi: 10.1016/j.euroneuro.2022.06.007. Epub 2022 Jul 8. Eur Neuropsychopharmacol. 2022. PMID: 35810614
2022 Sep;62:10-21. doi: 10.1016/j.euroneuro.2022.06.007. Epub 2022 Jul 8. Eur Neuropsychopharmacol. 2022. PMID: 35810614
See all "Cited by" articles
Publication types
MeSH terms
Bipolar disorder is associated with accelerated aging
Biology, biotechnology
Medicine, physiology, health
+7 926 604 54 63
address
People with bipolar disorder have relatively short telomeres. However, this may not be due to the disease itself, but to the often accompanying unhealthy behaviors (such as tobacco smoking and alcohol abuse).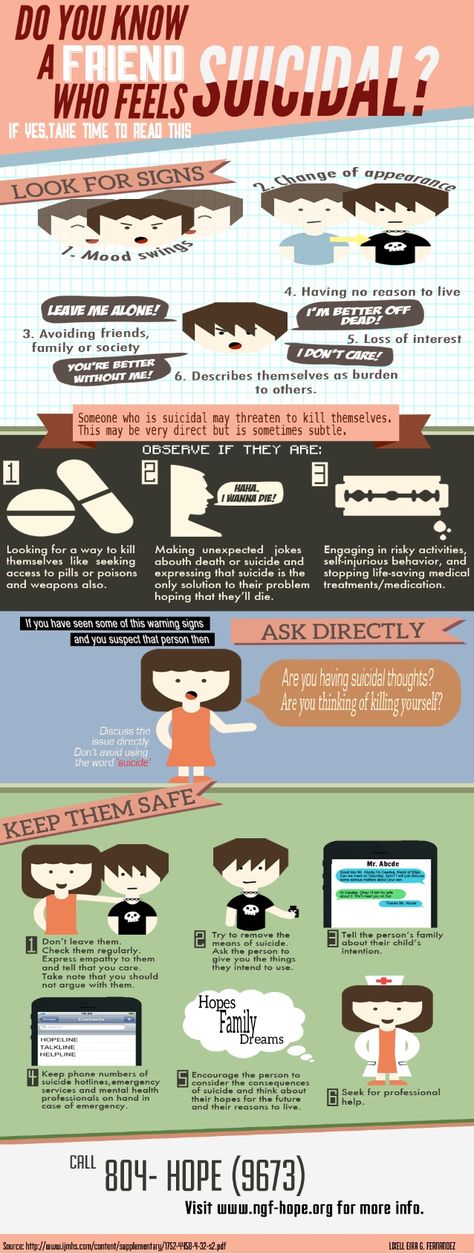
The results of a recently published study show an association between telomere length, a marker of biological aging, and the risk of developing bipolar affective disorder (BAD). This study helps explain why bipolar disorder often accompanies other age-related illnesses.
People with bipolar disorder, also known as manic-depressive illness, experience mood swings, from upbeat and energetic to depressed and depressed. Each year, 2.6% of adults in the United States are diagnosed with this condition. The Russian incidence rates of BAD are significantly lower, but this is most likely due to the lack of a culture of seeking psychiatric help for depression, anxiety disorders, and similar relatively “mild” mental illnesses that are not accompanied by delusions and hallucinations.
In addition to psychological disorders, bipolar disorder is also associated with other diseases that are usually associated with old age: cardiovascular disease, type 2 diabetes, obesity.
Researchers at King's College London and the Icahn School of Medicine at Mount Sinai, New York, decided to investigate this issue in depth.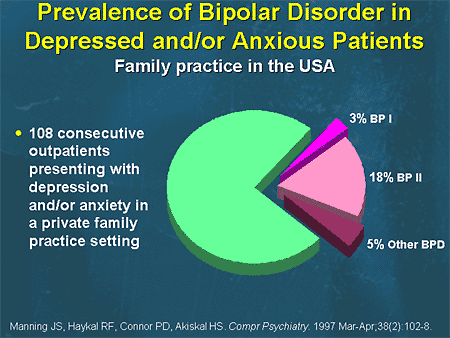 The team was particularly interested in telomeres, the ends of chromosomes that reflect the age of an organism.
The team was particularly interested in telomeres, the ends of chromosomes that reflect the age of an organism.
The results of the work were published in the journal Neuropsychopharmacology .
Telomeres and biological aging
Telomeres are the protective ends of DNA . With each cell division, the telomere shortens until it becomes so short that the cell can no longer divide.
Thus, the length of the telomere can be used to judge biological aging and susceptibility to diseases. Older people tend to have shorter telomeres. However, biological aging is not 100% consistent with chronological aging.
The rate of biological aging is influenced by a variety of factors, from hereditary to environmental factors. This means that two people of the same chronological age can differ significantly in biological.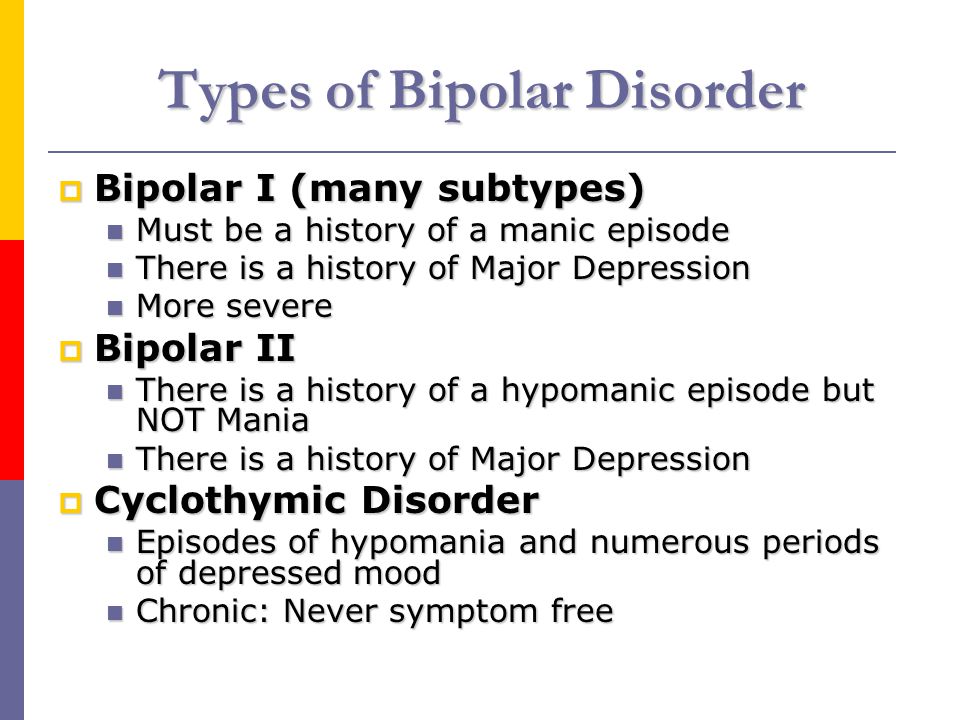
Telomere length is currently being studied as a marker of neuropsychiatric diseases. For example, shortened telomeres have been found in patients with severe depression, schizophrenia, and dementia.
A link has been found between telomere length and the structure of the hippocampus (the area of the brain responsible for memory and regulating mood). Shortened telomeres are also associated with memory impairment.
Lithium slows down aging caused by bipolar disorder
For the study, scientists took DNA samples of from 63 patients with bipolar disorder, 74 first-degree relatives, and 80 healthy non-relatives of the patients. Relatives of patients were included in the study, as it is known that telomere length is a hereditary factor.
First-degree relatives were found to have significantly shorter telomeres than controls. It also turned out that in patients with bipolar disorder, telomere length depends on another factor: lithium.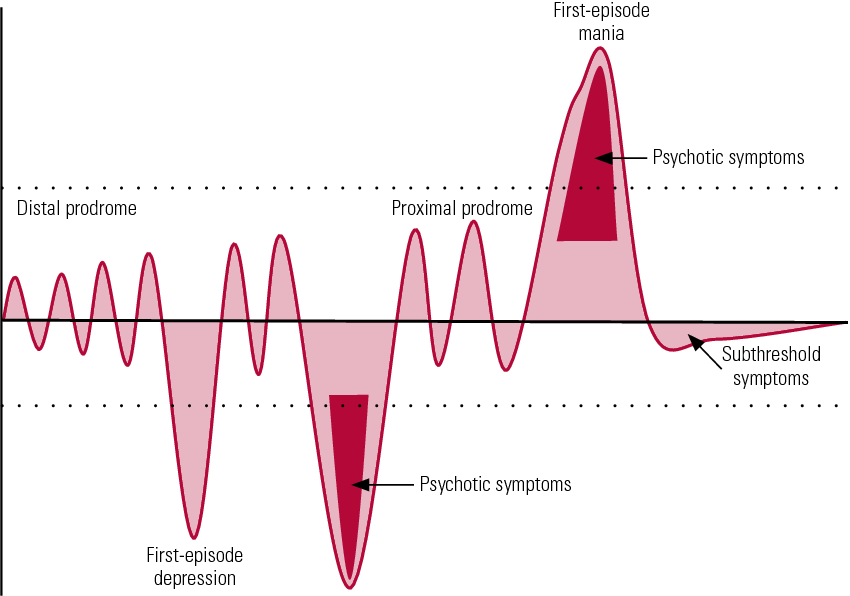
Lithium is often used to treat bipolar disorder. No significant shortening of telomeres was found in patients taking medications with lithium; those who did not take such medicines had the same indicators as their relatives.
This suggests that lithium prevents or significantly slows down premature aging associated with bipolar disorder.
Telomere length and the hippocampus
To study the relationship between telomere length and brain structure, scientists conducted MRI scans of the participants' brains. As predicted, the team found that shortened telomeres were indicative of reduced hippocampal volume.
“The results of our study provide the first evidence that an inherited susceptibility to bipolar disorder is associated with shortened telomeres. This may explain why such patients are more at risk of age-related diseases,” says lead author Dr Timothy Powell of King's College London
. These findings are interesting in their own right, but they also raise new questions. For example, such as Dr. Powell asks: “Are bipolar patients really predisposed to accelerated biological aging? Or are they more prone to activities that cause aging (smoking, unhealthy eating, etc.)? The next important step is to identify those risk factors that can be changed to prevent accelerated aging.”
For example, such as Dr. Powell asks: “Are bipolar patients really predisposed to accelerated biological aging? Or are they more prone to activities that cause aging (smoking, unhealthy eating, etc.)? The next important step is to identify those risk factors that can be changed to prevent accelerated aging.”
The results of the research pave the way for new developments and experiences. Co-leader of the work, Dr. Sophia Frangou, says the results suggest that "patients with bipolar disorder and people with a predisposition to it may benefit from proteins that protect against telomere shortening."
There is a lot of work to be done, but the discovered connection between telomeres, early aging and neuropsychiatric diseases is sure to yield useful and interesting results.
Biology, biotechnology
Medicine, physiology, health
Bipolar disorder shortens life
A recent study has linked bipolar disorder to shortening of telomeres, a major hallmark of cellular aging .
With this, scientists explained why bipolar disorder goes hand in hand with a whole bunch of age-related diseases.
Manic-depressive psychosis, or bipolar affective disorder (BAD) is a common mental disorder characterized by periodic alternation of manic and depressive phases with "light" intervals (interphases). People with bipolar disorder at times experience a burst of energy, become active and energetic, and at times go into a deep depression, lose their joy in life and motivation. About 2.6 million people are diagnosed with bipolar disorder each year in the United States.
In addition to mental health problems, bipolar affective disorder has been linked to an increased risk of age-related diseases such as coronary heart disease, obesity, type II diabetes. The causes of the phenomenon remained a mystery to science.
Now the staff of King's College London and their overseas partners at Icahn School of Medicine in New York have shed light on this issue.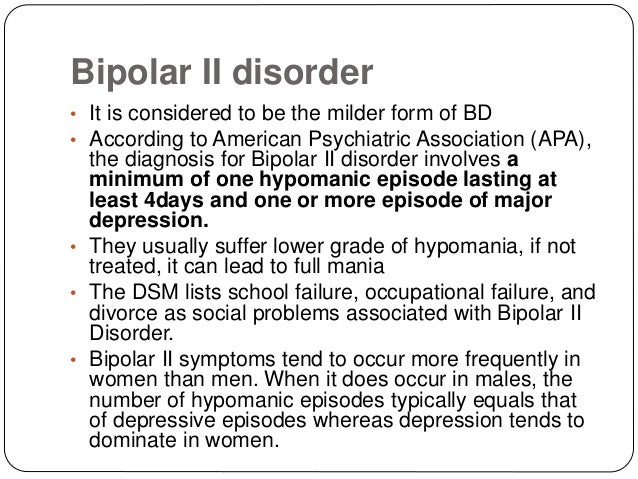 It turned out that BAD is associated with accelerated cellular aging - hence the age-related diseases.
It turned out that BAD is associated with accelerated cellular aging - hence the age-related diseases.
Details of the study published in the journal Neuropsychopharmacology.
Telomeres and human biological aging
Telomeres act as protective "caps" at the ends of chromosomes. With each cell division, telomeres become shorter until the cell loses its ability to reproduce, or becomes sick as a result of accumulated mutations.
It is no coincidence that telomere length is used by scientists as a marker of cell aging and predisposition to age-related diseases. Some telomeres shorten faster, others slower. Accordingly, the biological age of people can differ significantly from the chronological. This process is influenced by numerous internal and external factors. Today, telomere length is increasingly considered as a biomarker of neuropsychiatric diseases - schizophrenia, dementia, major depressive disorder.
A link has recently been found between telomere length and the structure of the hippocampus, a region of the brain involved in mood and memory regulation.
Lithium preparations slow down aging in bipolar disorder
During the study, scientists took DNA samples from 63 patients with bipolar affective disorder, as well as from 74 of their close relatives and 80 random healthy volunteers. Close relatives were chosen because telomere length can be inherited.
It turned out that relatives of sick people had much shorter telomeres compared to random healthy people. Among patients with bipolar disorder, telomere length depended on another factor - lithium preparations.
Lithium is often used in manic-depressive psychosis. Regular intake of lithium somehow helped to slow down the shortening of telomeres. This suggests that drugs are capable of managing cellular aging.
Telomeres and hippocampus
By performing an MRI of the brains of the participants, the scientists made another curious discovery. Telomere shortening was associated with smaller hippocampal volume.