Obsessions and autism
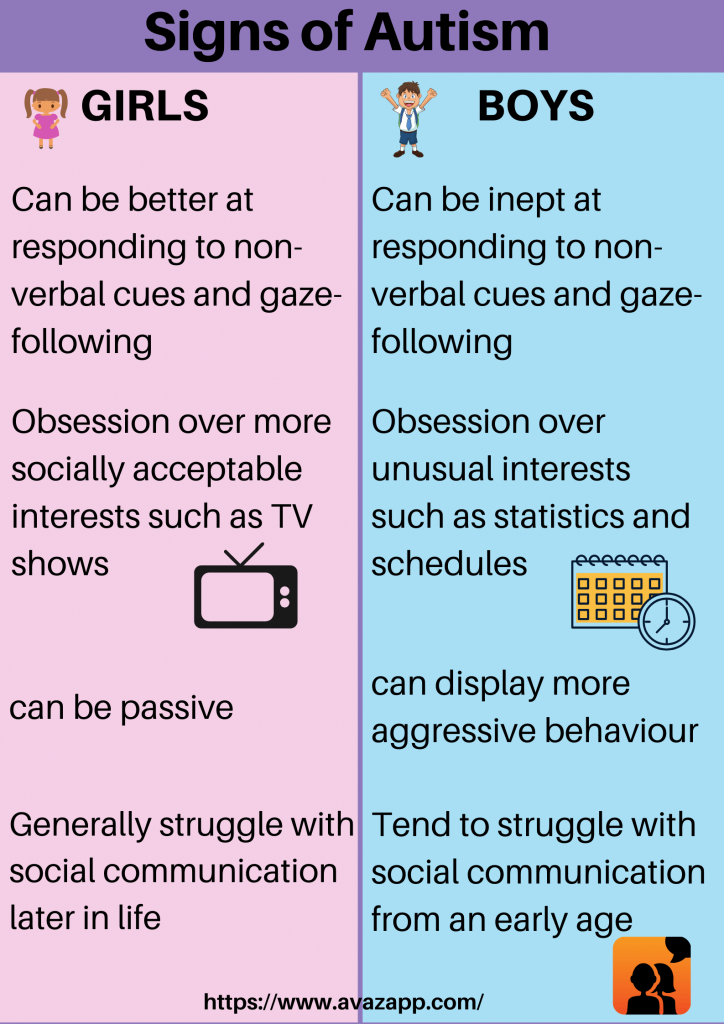
Obsessions and repetitive behaviour - a guide for all audiences
Intense interests and repetitive behaviour can be a source of enjoyment for autistic people and a way of coping with everyday life. But they may be obsessions and limit people's involvement in other activities and cause distress or anxiety. Find out what you can do to help.
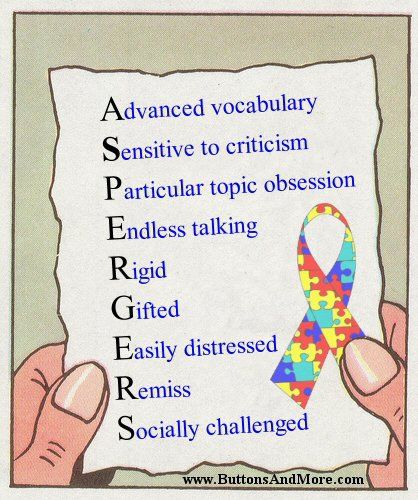
Intense interests
“My mind was constantly whirring with thoughts, worries and concerns. The time spent with my intense interest was the only time in which I had a clear mind – it gave me that much sought-after relaxation.” Autistic young person
Many autistic people have intense and highly-focused interests, often from a fairly young age. These can change over time or be lifelong. It can be art, music, gardening, animals, postcodes or numbers. For many younger children it's Thomas the Tank Engine, dinosaurs or particular cartoon characters.
Autistic people might also become attached to objects (or parts of objects), such as toys, figurines or model cars – or more unusual objects like milk bottle tops, stones or shoes. An interest in collecting is also quite common.
Autistic people often report that the pursuit of such interests is fundamental to their wellbeing and happiness, and many channel their interest into studying, paid work, volunteering, or other meaningful occupations. The interest can:
- provide structure, order and predictability, and help people manage the uncertainties of daily life
- give someone a way to start conversations and feel more self-assured in social situations
- help someone to relax and feel happy.
Is it an obsession or a hobby?
It is the intensity and duration of a person's interest in a particular topic, object, or collection that marks it out as an obsession.
- Is the person unable to stop the activity/interest independently?
- Is the interest impacting on the person's learning?
- Is the interest limiting the person's social opportunities?
- Is the interest causing significant disruption to other people, eg parents, carers and family?
If your answer to any of the questions above is 'yes', then their interest may have become an obsession which is affecting them, you and/or other people in their life.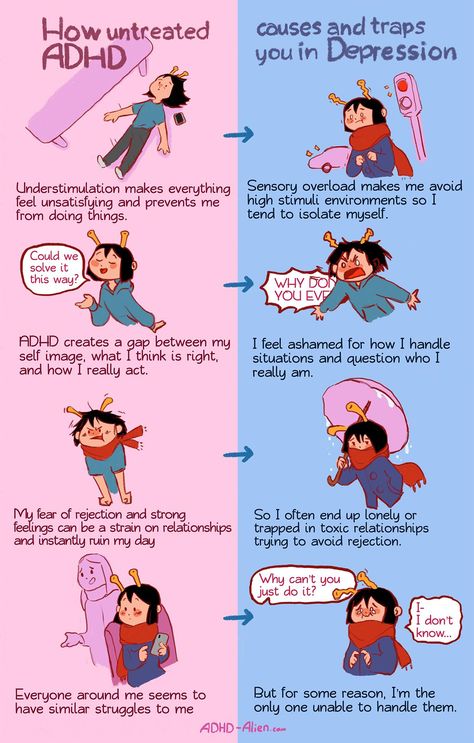
Repetitive behaviour
Repetitive behaviour may include arm or hand-flapping, finger-flicking, rocking, jumping, spinning or twirling, head-banging and complex body movements. This is known as 'stimming' or self-stimulating behaviour.
The reasons behind it include:
- for enjoyment
- an attempt to gain sensory input, eg rocking may be a way to stimulate the balance (vestibular) system; hand-flapping may provide visual stimulation
- an attempt to reduce sensory input, eg focusing on one particular sound may reduce the impact of a loud, distressing environment; this may particularly be seen in social situations
- to deal with stress and anxiety and to block out uncertainty.
Ask yourself if the repetitive behaviour restricts the person's opportunities, causes distress or discomfort, or impacts on learning?
For instance, a behaviour that is perhaps acceptable in a young child may not be appropriate as they get older, eg stroking other people's hair, copying people's accents, or collecting shiny things - meaning they collect change that people leave around. If it is causing difficulties, or is in some way unsafe, they may need support to stop or change the behaviour, or reduce their reliance on it.
Strategies to use
Understand the function of the behaviour
Think about the function of the repetitive behaviour or obsession.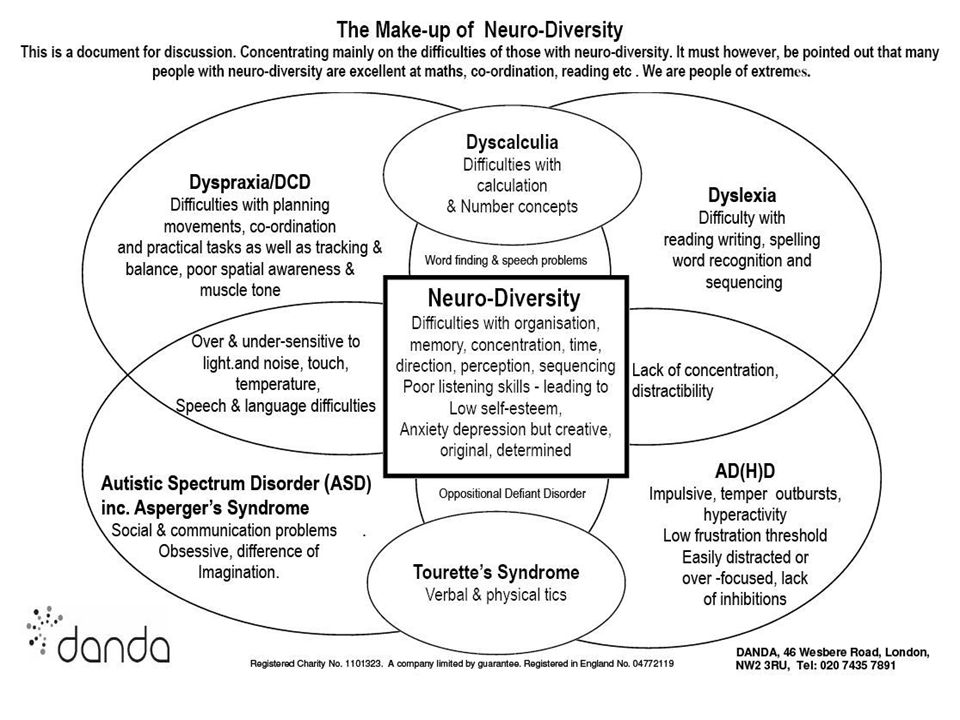 What does the person get out of it? Does it reduce anxiety, or block out noise?
What does the person get out of it? Does it reduce anxiety, or block out noise?
Modify the environment
Does the person always seem to find a particular place like a classroom, hard to cope with? Is it too bright? You might find that modifying the environment (eg turning off strip lighting) can help to reduce sensory discomfort. If the behaviour is a way of getting sensory input, look for alternative ways of achieving the same sensation.
Increase structure
Make the world a more structured and predictable place. A more structured environment could reduce boredom, which is sometimes a reason for repetitive behaviour. You might prepare a range of enjoyable or calming activities to re-direct the person to if they seem bored or stressed.
Try using visual supports (such as daily timetables), social stories™, or pre-plan strategies to prepare for change or events that might be stressful, or daily transition times. Egg timers or time timers can help someone to understand abstract concepts like time, plan what they need to do, in what order, and understand the concept of waiting.
Find product suppliers and picture symbols in our Autism Services Directory or find out about apps that you can use to structure time or build social stories™.
Learn more about how you can help with change, sequencing, transition and school break times.
Manage anxiety
Self-regulation skills are any activities that help a person to manage their own emotions and behaviour.
If you can help the person to identify when they are feeling stressed or anxious and help them learn alternative strategies to use, you may, in time, see less repetitive and obsessively habitual behaviour. Strategies to consider might be relaxation techniques such as taking 10 deep breaths or squeezing a stress ball, as well as finding ways to communicate their need for support either verbally or, if that is too difficult, by showing a red card or writing a note.
Many autistic people have difficulty with abstract concepts such as emotions, but there are ways to turn emotions into more 'concrete' concepts, eg stress scales.
You can use a traffic light system, visual thermometer, or a scale of 1-5 to present emotions as colours or numbers. For example, a green traffic light or a number 1 can mean 'I am calm'; a red traffic light or a number 5, 'I am angry'.
Develop other strategies to manage anxiety, such as the Brain in Hand digital self-management support system. Consider contacting a counsellor experienced in working with autistic people.
Intervene early
Repetitive behaviours and obsessions are generally harder to change the longer they continue. Behaviour that is perhaps acceptable in a young child may not be appropriate as they get older, eg obsession with stroking other people's hair. Autistic people should be encouraged to reduce or stop the behaviour before they reach an age where it’s not acceptable.
Set boundaries
If you need to, set clear, consistent limits - for example, ration an object, the time a person should spend talking about a subject, or the places where they can carry out a particular behaviour. Behavioural change is most likely to be successful and the person less likely to be distressed if you start small and go slowly. Increase time restrictions and introduce other limits gradually.
Behavioural change is most likely to be successful and the person less likely to be distressed if you start small and go slowly. Increase time restrictions and introduce other limits gradually.
Decide together a realistic target and put together a plan to reach that target over a period of time. It is important to set small, realistic goals to help build on success and increase confidence.
Think about whether the person would find it easier to engage in the interest for shorter periods throughout the day or for longer periods but less often.
Consider what needs to be changed. Are they unable to stop doing the activity? Work on reducing the time spent on it. Is the issue that they constantly start the activity throughout the day even when they are trying to focus on other things? Work on reducing the frequency. If it is a mixture of both, focus on one aspect to change at first, to increase the chance of success and reduce anxiety.
If it is a mixture of both, focus on one aspect to change at first, to increase the chance of success and reduce anxiety.
Example
- Week 1: decide on the plan and target, creating a visual support explaining the change.
- Week 2: Jane is allowed to talk about her favourite TV programme for 15 mins, every hour.
- Week 3: Jane is allowed to talk about her favourite TV programme for 10 mins, every hour.
- Week 4: Jane is allowed to talk about her favourite TV programme for 10 mins every two hours.
Continue in this way until you meet the goal, which is to find a balance between enjoying the interest and doing other activities.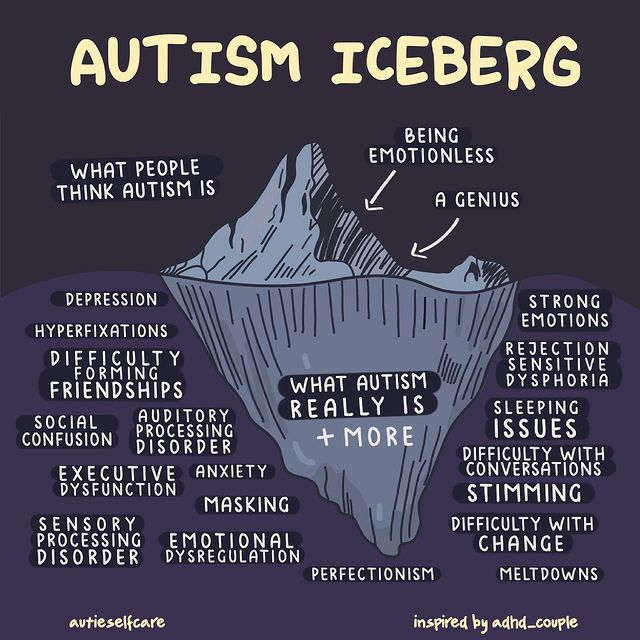
Provide alternatives
Think of alternative activities the person could do. For example, if they have spoken to family about their interest for the set amount of time that day, consider directing them to record their thoughts on their phone or write them down in an interest book. While the family are no longer engaging in the activity, the thoughts are still expressed, hopefully meeting the person’s need and therefore lowering their anxiety. If they want to express their thoughts about their interest again before their next allotted time, they could write things down and let them know you will talk to them about their notebook thoughts later. You could use visual supports to explain these additional activities.
It might be possible for the person to engage in their interest in new ways, perhaps joining a club or group, or studying or working in a related area.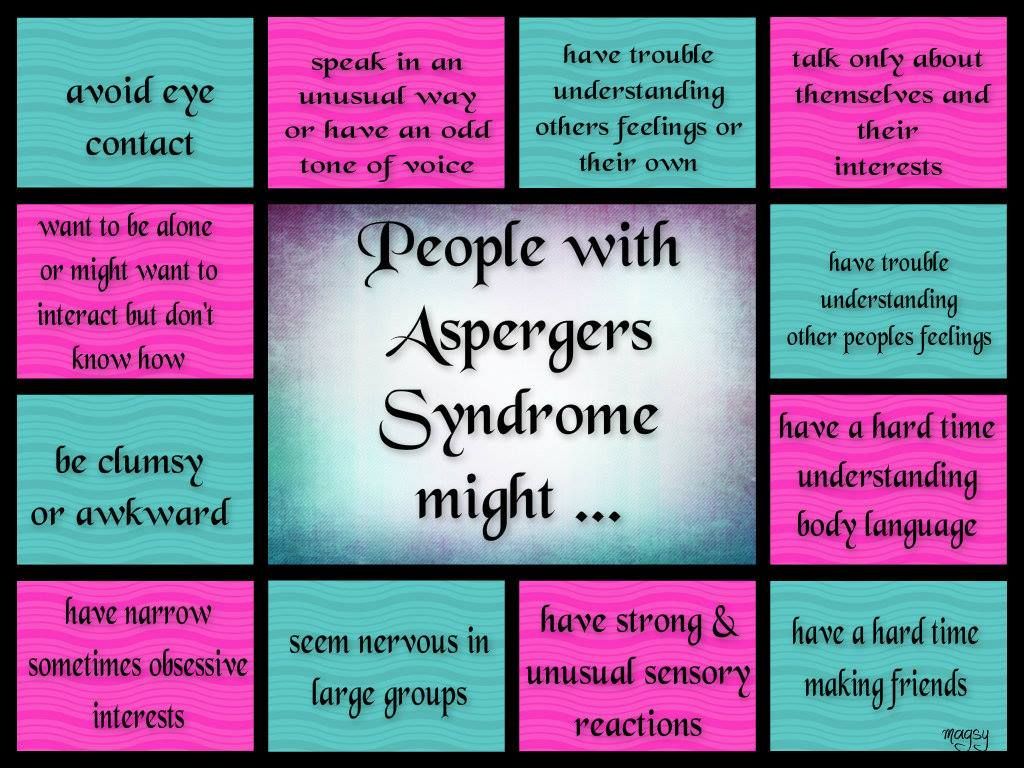
Where the activity relates to sensory needs, provide an alternative activity that has the same function, eg:
- someone who puts inedible objects in their mouth could have a bag with edible alternatives (that provide similar sensory experiences) such as raw pasta or spaghetti, or seeds and nuts
- a person who smears their poo could have a bag with play dough in it to use instead.
More from our charity
- Online Community
- Parent to Parent service
- Use our Autism Services Directory to find counsellors experienced in working with autistic people.

Obsessions, routines, rituals & autism
Obsessions, rituals, routines and autistic children and teenagers
Many autistic children and teenagers have obsessions, routines or rituals. Some children have all of these things, and others have only one or two.
Obsessions
Autistic children and teenagers can be very intense and focused about favourite toys, activities and topics of conversation.
For example, younger children might collect things like twigs or balls or want to know the birthday of everyone they meet. They might open and close doors over and over again, or rush into each new place to find and flush the toilet. Older children might have very narrow interests or preoccupations, like needing to know everything possible about trains.
Some children move from one interest or obsession to another, and the interests last for weeks or months before they change. Others develop an interest – for example, in trains – in early childhood and continue this interest through adolescence and into adulthood.
Rituals
Some autistic children and teenagers have rituals. For example, some children might keep favourite objects in specific places, like the bottom corner of a drawer in the bedroom. They might have to get their objects out and touch them before bed. Or they might drink only from particular cups, or ask the same questions and always need specific answers.
Routines
Routines are often important to autistic children and teenagers. They can find change and transitions difficult to cope with. They might like to eat, sleep or leave the house in the same way every time. For example, children might go to bed happily if you follow their regular bedtime routines, but won’t settle if the routines are broken. They might get very upset if their route to preschool is changed, or they might insist on putting their clothes on in the same order each morning.
How obsessions, routines and rituals help autistic children and teenagers
We don’t know what causes obsessive behaviour or the need for routines and rituals. The cause might not be the same for everyone.
The cause might not be the same for everyone.
For young autistic children who have limited play skills, special interests can be something they enjoy.
Also, obsessions, routines and rituals help some autistic children manage stress and anxiety. When they feel stressed because they don’t understand what’s going on around them, obsessions and rituals let them take some control of their surroundings.
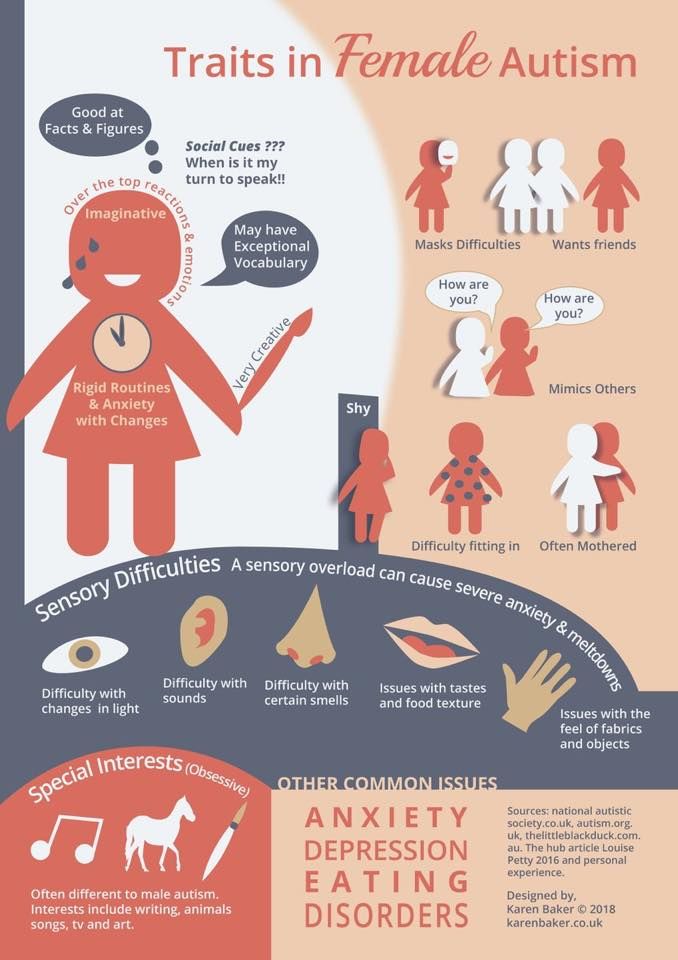
Sensory sensitivities can lead to some autistic children developing obsessions and rituals. For example, children might stroke people’s hair whenever they can because they enjoy the sensation or it helps them feel calm.
And some autistic children have trouble with planning, so having a rigid routine or ritual helps comfort them and relieves feelings of stress and anxiety.
You can use your child’s obsessions and special interests as rewards and motivators to help teach them new skills and behaviour.
Handling autistic children’s obsessions, routines and rituals
Some autistic children – and their families – can live with daily obsessive behaviour, routines and rituals. Others might want to find ways to handle the habits differently.
Others might want to find ways to handle the habits differently.
If you’re thinking about doing things differently, it can help to ask some questions about the habit and how it affects your child and family. For example:
- Is your child’s behaviour affecting their ability to learn?
- Is your child’s behaviour affecting their social life?
- Is your child’s behaviour affecting your family’s ability to carry out day-to-day activities, or to go on holidays or trips?
- How would you feel if this behaviour is the same in a few years?
- Is your child’s behaviour causing harm to themselves or others?
Your answers to these questions might help you decide whether it’s worth trying to change things. And if you decide you want to work on your child’s obsessions and routines, your answers might help you work out what to focus on.
Before you develop a plan to manage your child’s obsessions, rituals and routines, it’s a good idea to think about your child’s developmental level and communication skills. For example, does your child have the communication skills to understand your instructions?
For example, does your child have the communication skills to understand your instructions?
Working out what’s causing your child’s behaviour might also guide your next steps. Is it sensory? Or does your child feel anxious when faced with the unknown? You might be able to manage the sensory issues or the anxiety, which could lead to a decrease in the behaviour.
If your child’s behaviour isn’t affecting their life or other people in a negative way, but you still want to decrease it, you could consider setting some limits on the behaviour. For example, you could allow your child to talk about their special interest subject for half an hour after school. After that, they need to switch to a new activity.
You might also be able to find a positive outlet for an obsessive interest. For example, if your child has an interest in dinosaurs, keeping a scrapbook might work well.
Autistic children can get upset when they can’t do their obsessive behaviour, routines or rituals. Strategies for making changes to routines and managing difficult behaviour can help you and your family manage these situations.
Strategies for making changes to routines and managing difficult behaviour can help you and your family manage these situations.
Getting professional help with obsessions, routines and rituals
An experienced professional can help you understand and manage your child’s obsessive behaviour, routines or rituals.
A good first step is talking with your child’s paediatrician, psychologist, another health professional working with your child, or school support staff.
Obsessive-compulsive disorder (OCD) and autism
03/05/19
Autism and obsessive-compulsive disorder (OCD) often coexist, scientists are trying to study both disorders in order to better differentiate them and determine more effective treatment
Author Daisy Yuhas
Source: Spectrum News
Steve Slavin was 48 years old when a visit to a psychologist forced him to dramatically change his ideas about his own life. He had a very difficult year. Slavin began to suffer from anxiety, which manifested itself in negative thoughts and repetitive actions, and this was not the first time he suffered from them. nine0003
He had a very difficult year. Slavin began to suffer from anxiety, which manifested itself in negative thoughts and repetitive actions, and this was not the first time he suffered from them. nine0003
As a child, he could not enter a room unless he had swallowed an even number of times beforehand, and he had to swallow and count to four, six, or eight with one foot up before stepping on a stone in the pavement. As an adult, he often experienced a lot of stress around other people, and he washed his hands again and again because he was terrified of catching something from other people. He also often suffered from depression, due to which he began to avoid acquaintances and friends.
This time his depression and anxiety got worse and his doctor referred him to a psychologist. “I spent weeks, if not months, trying to get an appointment with him,” he recalls. However, within the first 10 minutes of the meeting, the psychologist suddenly stopped asking him about his childhood and current mental health issues, and instead asked him what he knew about autism. nine0003
nine0003
Coincidentally, a relative had spoken to Slavin about autism just two days earlier, suggesting that this might explain his dislike of social situations. Slavin knew almost nothing about autism, but suggested that it was possible. By the end of the consultation, the psychologist was practically certain that “I either have high-functioning autism or some kind of brain damage,” Slavin recalls, chuckling. Only a few years later, the doctor gave him an official diagnosis - obsessive-compulsive disorder (OCD). He was also confirmed to have autism. nine0003
At first glance, autism and obsessive-compulsive disorder seem to have nothing in common. However, doctors and researchers talk about the intersection of these two disorders. Research data indicate that up to 84% of autistic people suffer from some type of anxiety disorder, and up to 17% of people with autism have OCD. And according to one 2017 study, even more people with OCD have undiagnosed autism.
Part of this overlap may be due to misdiagnosis: OCD-induced rituals may resemble repetitive behaviors in autism, and vice versa. However, there is growing evidence that many people, like Slavin, have both disorders. A 2015 study that analyzed the health records of 3.4 million Danish people over 18 years found that as adults, people with autism are twice as likely to be diagnosed with OCD than people without autism. Similarly, the same study found that people with OCD were four times more likely to be diagnosed with autism as adults than people without OCD. nine0003
However, there is growing evidence that many people, like Slavin, have both disorders. A 2015 study that analyzed the health records of 3.4 million Danish people over 18 years found that as adults, people with autism are twice as likely to be diagnosed with OCD than people without autism. Similarly, the same study found that people with OCD were four times more likely to be diagnosed with autism as adults than people without OCD. nine0003
Over the past ten years, researchers have begun to study the combination, interaction, and differences between these two disorders. Understanding these differences is important not only for making a correct diagnosis, but also for choosing an effective treatment. It appears that the experience of people with OCD and autism is unique, different from that of people with one of these disorders. And for these people, standard OCD treatments, such as cognitive behavioral therapy (CBT), may not be effective.
Missed diagnoses
Anyone can develop obsessive thoughts (obsessions) or obsessive actions (compulsions).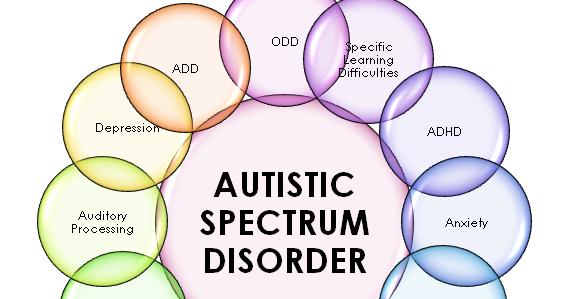 Many people start worrying about not turning off the stove at home, or checking again that they took their keys with them. "It's part of a normal life experience," says Ailsa Russell, a clinical psychologist at the University of Bath in the UK.
Many people start worrying about not turning off the stove at home, or checking again that they took their keys with them. "It's part of a normal life experience," says Ailsa Russell, a clinical psychologist at the University of Bath in the UK.
Most people can get over these unpleasant obsessions and go on with their normal lives. However, with obsessive-compulsive disorder, such anxiety becomes stronger and begins to interfere with normal daily functioning. nine0003
Some people with OCD, like Slavin, count steps or breaths or perform other meaningless actions because they feel that without these actions, something terrible is bound to happen. Other people call themselves "inspectors" - they check again and again that they have done a task correctly, and this prevents them from doing other things. Other people with OCD are constantly bathing or scrubbing because they are afraid of dirt or contamination.
"Typically, people with OCD are aware that their fears and behavior are irrational," says Russell, despite this OCD sufferer is trapped in intense anxiety and compulsive rituals.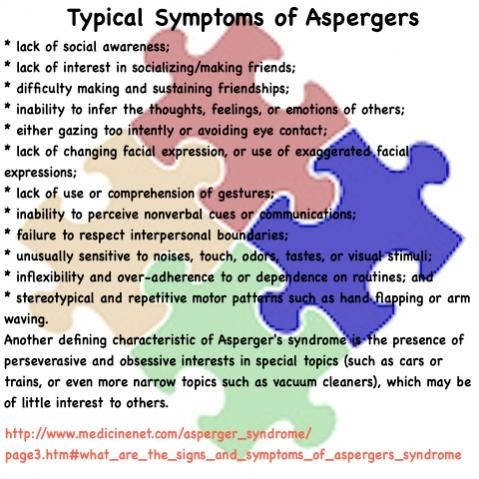 nine0003
nine0003
The intersection between OCD and autism is still poorly understood. According to a 2015 analysis, people with both disorders are characterized by non-standard sensory responses. For some autistic people, sensory overload is the main source of stress and anxiety. For example, Slavin is terrified of police sirens and doorbells, he says that for his nervous system they are like bomb explosions.
Some researchers say that the social problems of people with autism can increase their anxiety, which in turn can lead to OCD. Failure to interpret social cues can lead to social isolation or bullying by others, which increases anxiety. “Separating anxiety from autism is extremely difficult,” says Roma Vasa, director of mental health services at the Kennedy Krieger Institute in Baltimore, USA. nine0003
These commonalities can make it difficult to distinguish between symptoms of autism and OCD. Even for an experienced clinician, OCD compulsions can resemble the “sameness seeking” or repetitive behaviors of autistic people, which may include tapping, lining up objects, or striving to always walk in the same path. Separating the two states can be a daunting task.
Separating the two states can be a daunting task.
As the 2015 analysis showed, the key difference is that obsessive thoughts (obsessions) lead to obsessive actions (compulsions), but not to autistic symptoms. Another feature is that people with OCD cannot, in principle, replace their rituals with other actions. In Vasa's words: "They need to do everything in a certain way, otherwise they experience anxiety and discomfort." nine0003
At the same time, autistic people tend to have a repertoire of different repetitive behaviors that serve a similar function and from which to choose. “They just go for any behavior that helps them calm down, it doesn’t really matter to them any particular action,” says Jeremy Winstra-Vanderviel, professor of psychiatry at Columbia University, USA.
Thus, doctors need to determine why a person performs a particular action. But this task becomes difficult if it is difficult for the patient to describe his experience in words. Autistic people may have speech, communication, or intellectual impairments and often have significant difficulty identifying and understanding their inner experience.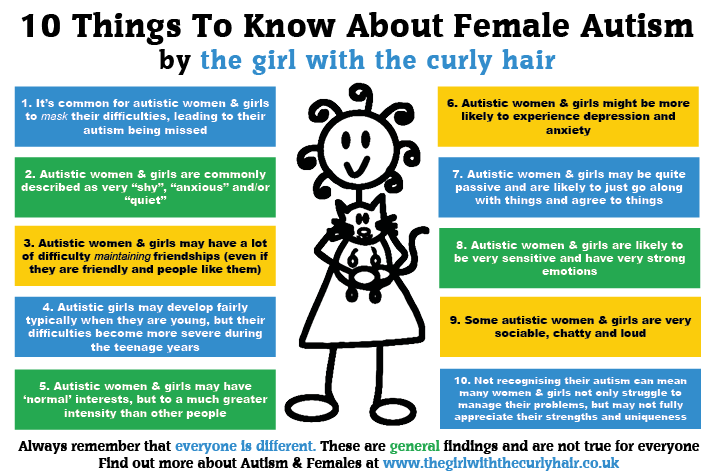 This can lead to misdiagnosis, as happened in the case of Slavin. nine0003
This can lead to misdiagnosis, as happened in the case of Slavin. nine0003
As a child, Slavin often visited a psychologist's office in the suburbs of London. However, the experts who examined him missed both OCD and autism. Slavin did not speak until the age of 6. According to him, his first childhood memories are classes with a speech therapist and a child psychologist. Even after he started talking, he avoided other people and didn't like making eye contact. He suffered from severe anxiety and abdominal pain.
At about 11 years of age, he was diagnosed with "childhood schizophrenia" and was prescribed Valium and lithium. Doctors warned his parents that he might need a lifelong stay in a medical facility. Instead, he was able to attend a prestigious high school, get a degree and become, in his words, a "slightly more functional" person, and thanks to his passion for music, he was able to launch a career as a professional composer. nine0003
Being diagnosed with autism many years later brought him great relief, but it was also associated with new problems. During conversations with specialists, for example, they began to attribute any of his complexities to autism, including problems with the perception of auditory information. “Once you get this diagnosis, the doctors start saying, ‘Well, it’s because of autism,’ they don’t pay attention to the nuances,” he says. Slavin found that no one can say for sure whether a particular behavior is the result of OCD or autism, or what exactly can be done about it. nine0003
During conversations with specialists, for example, they began to attribute any of his complexities to autism, including problems with the perception of auditory information. “Once you get this diagnosis, the doctors start saying, ‘Well, it’s because of autism,’ they don’t pay attention to the nuances,” he says. Slavin found that no one can say for sure whether a particular behavior is the result of OCD or autism, or what exactly can be done about it. nine0003
General Biology
Slavin's questions may be answered soon as more researchers look at the combination of autism and OCD. Until 10 years ago, research on this topic was practically non-existent, says Suma Jacob, a professor of psychiatry at the University of Minnesota, USA. When she said she was interested in studying the two disorders, "the main experts in the field said to pick one disorder," she says. This situation is starting to change, in part because researchers have begun to realize how common it is to combine autism and OCD. nine0003
nine0003
Jacob and colleagues have been tracking repetitive behaviors (which may be associated with autism or OCD) in thousands of children as young as 3 years old. “From a brain perspective, all these disorders are connected,” she says.
In fact, scientists have found that the same brain regions and neural pathways play an important role in both autism and OCD. Brain scans point to a special role for the striatum, an area of the brain that is associated with motor functions and rewards. Some research suggests that in people with autism and people with OCD, one structure within the striatum, the caudate nucleus, is larger than normal. nine0003
Animal models also suggest a role for the striatum. Winstra-Vanderwil studies autism and OCD with repetitive behavior rodents. He and other scientists found that in both disorders, the animals show abnormalities in the neural circuitry that runs through the striatum and plays a key role in how we start and stop behavior, as well as influencing habit formation.
Another area of research is related to interneurons, which often suppress impulses between cells. If the interneurons in the striatum of mice are disrupted, this leads to twitching, anxiety, and repetitive behavior that resembles OCD and Tourette's syndrome. nine0003
In male mice, the impact on the functioning of interneurons also leads to a sharp decrease in sociability, which, to some extent, may resemble autism. "Unexpectedly, mice also developed social deficits identical to those we see in animal models of autism," says Christopher Pittenger, director of the OCD Research Clinic at Yale University, who led the work. For this reason, he says, interneurons could be a target for both OCD and autism treatments. nine0003
This connection at the level of neural pathways may reflect common genetic causes. A 2015 Danish study found that people with autism were more likely to have relatives with OCD than people in a control group. However, genetic comparisons of the two disorders have shown conflicting results at this stage, which may be due to the fact that very little is known about genetic factors in OCD.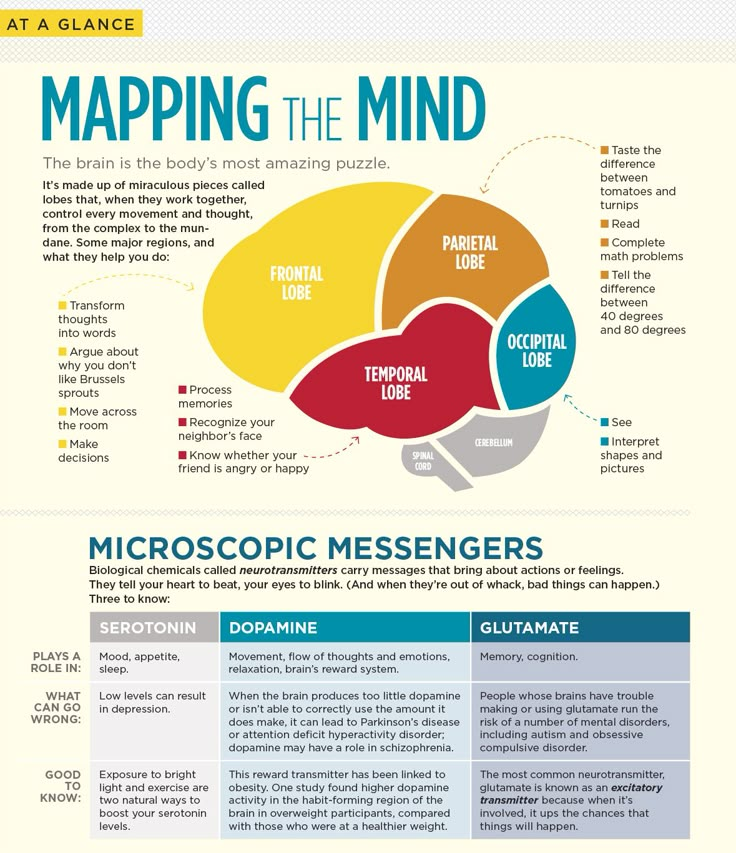 “As embarrassing as it is to admit, we know a lot more about the genetics of autism than we do about the genetics of OCD,” says Pittenger. A similar gap may explain why a 2018 meta-analysis of genome studies of more than 200,000 people with 25 disorders, including autism and OCD, found no common gene variants for OCD and autism. nine0003
“As embarrassing as it is to admit, we know a lot more about the genetics of autism than we do about the genetics of OCD,” says Pittenger. A similar gap may explain why a 2018 meta-analysis of genome studies of more than 200,000 people with 25 disorders, including autism and OCD, found no common gene variants for OCD and autism. nine0003
Unpublished work by another research group suggests that rare “de novo mutations,” that is, spontaneous mutations that neither parent has, significantly increase the risk of autism and OCD. Some of the genes that researchers have linked to both diagnoses are related to the immune system. This suggests that interactions between environmental factors and the immune system may play a role. Another gene from the general list, CHD8, regulates gene expression. nine0003
Treatment adaptation
Until scientists can combine all the data from the preliminary studies, no new drugs can be expected. But there are other methods that can help people with both disorders.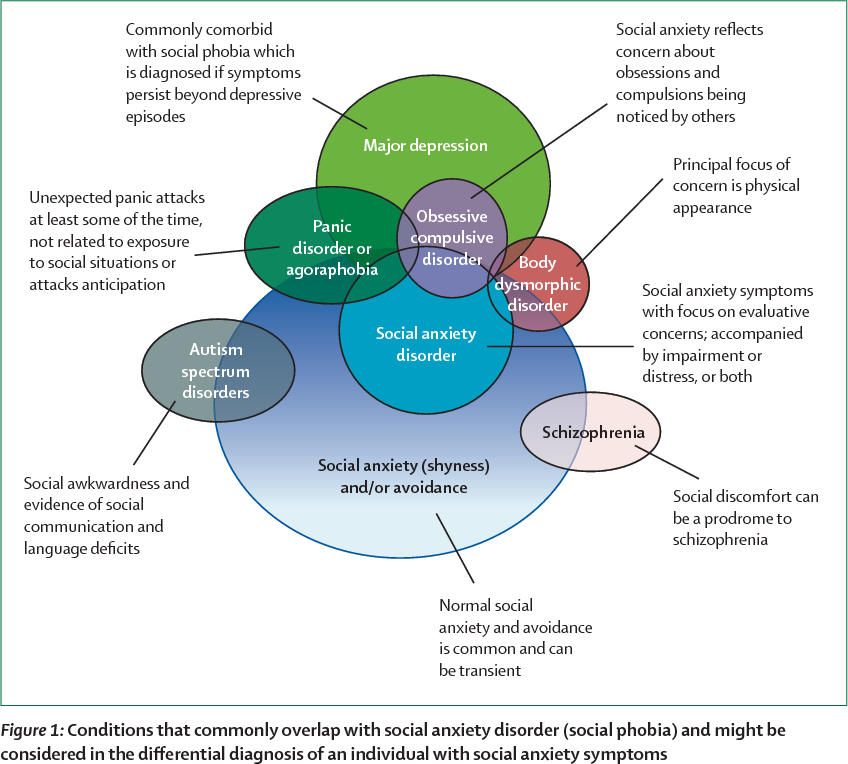
On a chilly December evening, people from all over the UK join the OCD & Autism Support Group, a monthly online conference organized by OCD Action, a British charity that helps people with OCD. The number of group members varies greatly during each meeting, but this evening, a few days before Christmas, only four people called. nine0003
During the meeting, a woman named Michelle (only given names in the group) explains that she cannot leave the house unless she makes sure all the lights and appliances are turned off. Thomas spends several hours a day showering. Both of them talk about social difficulties and how they make them anxious. They often worry about what other people think of them, and whether others find their behavior related to OCD or autism strange.
Like most support groups, calling together helps participants feel they are not alone. They also share new information and tips, such as how to use a timer to reduce the time spent washing your hands. Three of the participants mention cognitive behavioral therapy (CBT), which can help people better understand and manage their obsessive thoughts and actions. As with other forms of psychotherapy that rely on dialogue, it may not be effective for people with autism. For example, such psychotherapy did not help Slavin. nine0003
As with other forms of psychotherapy that rely on dialogue, it may not be effective for people with autism. For example, such psychotherapy did not help Slavin. nine0003
He suspects that he was unable to follow the therapist's methods because of his difficulty with listening to speech and lack of mental flexibility, which he attributes to autism. “Many people on the autism spectrum find it difficult to imagine the situation and how it could lead to a different outcome, so traditional CBT doesn't always work,” he says. Instead, Slavin controls OCD with varying degrees of success with antidepressants.
Some researchers are trying to adapt CBT for people with autism, such as "making sure everyone can see and appreciate their own emotional state," says Russell. Together with her colleagues at King's College London, Russell found in a preliminary study that modified methods may help some adults with autism and OCD manage their anxiety. In January of this year, she and her colleagues, building on the success of the subsequent larger study, developed a clinical guideline. nine0003
nine0003
People with autism and OCD can also benefit from a more personalized approach to cognitive behavioral therapy. For example, possible schemes might include parent participation in counseling, language facilitation according to the person's language ability, use of visual support and rewards. One clinical trial compared this adapted therapy with standard CBT in more than 160 children with autism and OCD. As yet unpublished results suggest that standard CBT may be beneficial, but an individualized approach works best. nine0003
It seems to Slavin that a more individual approach to treatment can be successful, but he himself has not tried such approaches. Working with organizations that help people with OCD and people with autism, he began to appreciate the diversity of people with both disorders. “It feels like every single person needs their own diagnosis, their own category, because everyone is so different,” he says.
Ten years after being diagnosed with autism, Slavin wants to share his experience, also in order to combat the lack of resources he has faced. In 2010, he opened a website and started a YouTube channel where he talks about what he has learned about living with autism. nine0003
In 2010, he opened a website and started a YouTube channel where he talks about what he has learned about living with autism. nine0003
“I just think of autism as a certain set of circumstances that you can use to your advantage and say, 'OK, I'm going to forgive myself if I don't quite understand how other people act,'” says Slavin. “You can even find joy in your oddities and differences from others ... But OCD, there is nothing good about it at all.”
In October he published a book on his progress. So far, the title of the book sounds like "The search for the norm."
We hope that the information on our website will be useful or interesting for you. You can support people with autism in Russia and contribute to the work of the Foundation by clicking on the "Help" button. nine0003
Research, Psychiatry, Comorbidities
Obsessive Compulsive Disorder or "Just Autism"?
05/18/14
Psychiatrist on differential diagnosis of obsessive-compulsive disorder in autism
Source: Autism Speaks
for children with an autistic spectrum of typical, or something, or something is the same. preoccupation with some object, toy, video, task, and so on. Sometimes it is difficult for parents to determine whether such preoccupation is a manifestation of autism or whether it is behavior associated with obsessive-compulsive disorder (OCD). Children with autism can also be diagnosed with OCD. Below, Dr. Judy Riven explains how you can find out if your child needs to be tested for this disorder. nine0126
preoccupation with some object, toy, video, task, and so on. Sometimes it is difficult for parents to determine whether such preoccupation is a manifestation of autism or whether it is behavior associated with obsessive-compulsive disorder (OCD). Children with autism can also be diagnosed with OCD. Below, Dr. Judy Riven explains how you can find out if your child needs to be tested for this disorder. nine0126
Several psychological disorders, including obsessive compulsive disorder or OCD, are common in autism. However, on the other hand, some of the symptoms of autism resemble those of other disorders, including OCD. So it can be difficult to separate the manifestations of autism in a given patient from the symptoms of another disorder.
As the name suggests, OCD includes obsessions (unwanted, intrusive thoughts), compulsions (unwanted, compulsive actions), or both. Obsessions are involuntary thoughts appearing at regular intervals that are both intrusive and undesirable for a person. Obsessions cause very strong stress, but at the same time a person cannot ignore them. Very often, people suffering from obsessional thoughts try to reduce the discomfort they cause by performing a specific action (often ritualistic). Such actions, which allow temporary relief of obsession, are called compulsive actions. Compulsions are repetitive, repetitive actions that take a person a considerable amount of time, but the person feels that he “must” perform this or that action in response to an unpleasant intrusive thought, even if from the outside this behavior seems meaningless. nine0003
Obsessions cause very strong stress, but at the same time a person cannot ignore them. Very often, people suffering from obsessional thoughts try to reduce the discomfort they cause by performing a specific action (often ritualistic). Such actions, which allow temporary relief of obsession, are called compulsive actions. Compulsions are repetitive, repetitive actions that take a person a considerable amount of time, but the person feels that he “must” perform this or that action in response to an unpleasant intrusive thought, even if from the outside this behavior seems meaningless. nine0003
Obsessions or special interests?
OCD is often confused with special interests or repetitive activities that are a feature of autism. However, the symptoms of these conditions are actually very different. Obsessive interests in autism, as a rule, bring joy and pleasure to a person. OCD is more of a behavior that a person engages in just to reduce overwhelming stress or anxiety.
It is impossible to understand what exactly is happening to a person without a complete examination. Not too long ago, I had a conversation with the mother of a 25-year-old young man with autism who was worried about her son. She told me that although her son has always had repetitive behaviors, lately he constantly wants to redo different tasks, such as dressing again or taking a shower, even if he just took it. He also insists that their car be turned back if they just drove down a different street. I noticed two features that led me to believe that she was describing possible symptoms of OCD. nine0003
Not too long ago, I had a conversation with the mother of a 25-year-old young man with autism who was worried about her son. She told me that although her son has always had repetitive behaviors, lately he constantly wants to redo different tasks, such as dressing again or taking a shower, even if he just took it. He also insists that their car be turned back if they just drove down a different street. I noticed two features that led me to believe that she was describing possible symptoms of OCD. nine0003
First, she noted that this behavior was significantly different from her child's past behavior that was associated with autism. Second, she described an increase in the severity of his symptoms. Finally, the description of her son's behavior matched the typical OCD symptom of getting stuck on something because it feels "wrong." In order to “fix” something, a person with OCD has to “re-do” something. For example, in this young man's case, he felt compelled to re-shower or re-dress.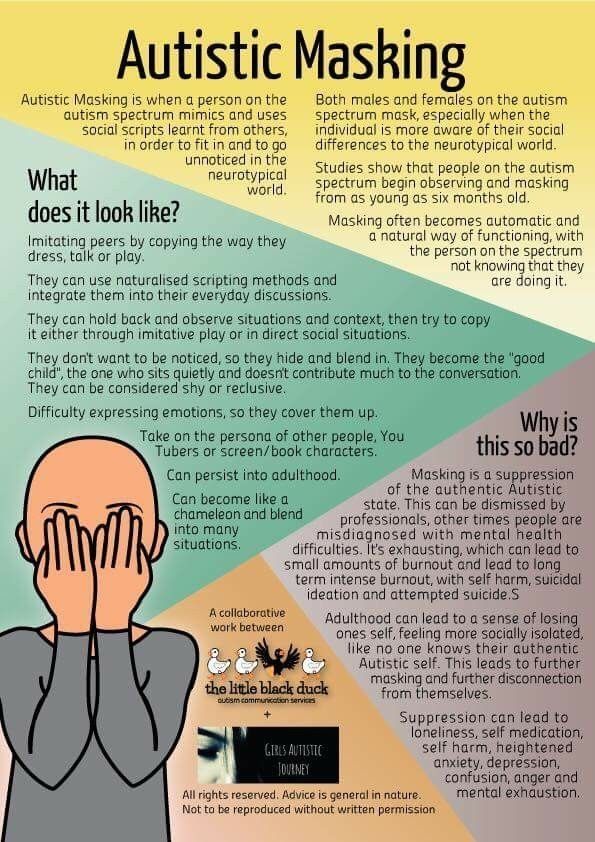 It also suited his need to drive the "right" way. nine0003
It also suited his need to drive the "right" way. nine0003
We have effective therapy!
If the new symptoms meet the criteria for an official diagnosis of OCD, the person may benefit from special treatment. In particular, a vast body of research has shown that cognitive behavioral therapy can help people with autism manage OCD symptoms. (Editor's note: Dr. Riven is one of the first practitioners to adapt cognitive behavioral therapy for people with autism.)
This psychotherapy involves helping the person become aware of their obsessive thoughts and compulsive behaviors and identify them as such. For example, a person can learn to recognize the physical symptoms of stress associated with obsessions. In CBT, we explain that thoughts can affect physical well-being and vice versa. nine0003
More importantly, we provide the patient with useful tools for managing problematic symptoms. This may include deep breathing and repeating positive affirmations, such as, “It's just OCD.