Thc for migraines
Can Cannabis or CBD Help?
Written by Susan Bernstein
In this Article
- How Does Pot Ease Pain?
- Does It Work for Migraines?
- What Are the Risks?
- Legal Issues
Migraine headaches can be tough to treat. If your pain, nausea, and sensitivity to light or noise don’t get better with over-the-counter or even prescription drugs, is there another option?
Marijuana might be one under-the-counter remedy for migraine relief. Some research shows that it may help ease migraine symptoms or possibly keep them from starting. But most studies haven't found solid proof of that.
And in some states, it isn’t legal to buy, grow, own, or use marijuana, even for medical reasons. Make sure you find out about your state’s laws before trying it.
How Does Pot Ease Pain?
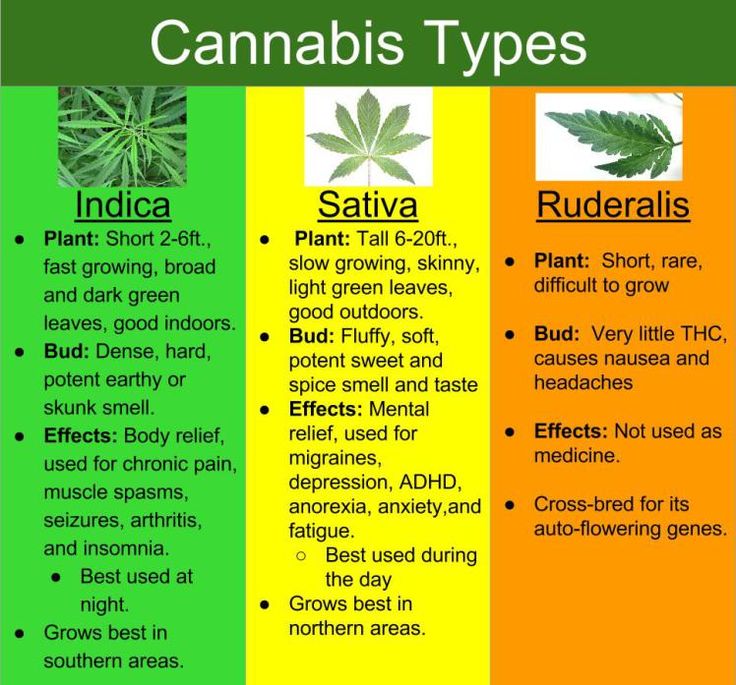
Marijuana is another name for cannabis, a bushy plant that’s used to make paper, rope, and other products.
Inside your brain and other parts of your body, you have a network of cannabinoid receptors. These are tiny loops of protein that affect how you feel pain.
Marijuana has natural compounds called cannabinoids. When you use it, these cannabinoids go into your body and look for the receptors. They change how the receptors work, and they may calm down pain signals.
Cannabinoids may also help with nausea, anxiety, muscle spasms, or other health problems.
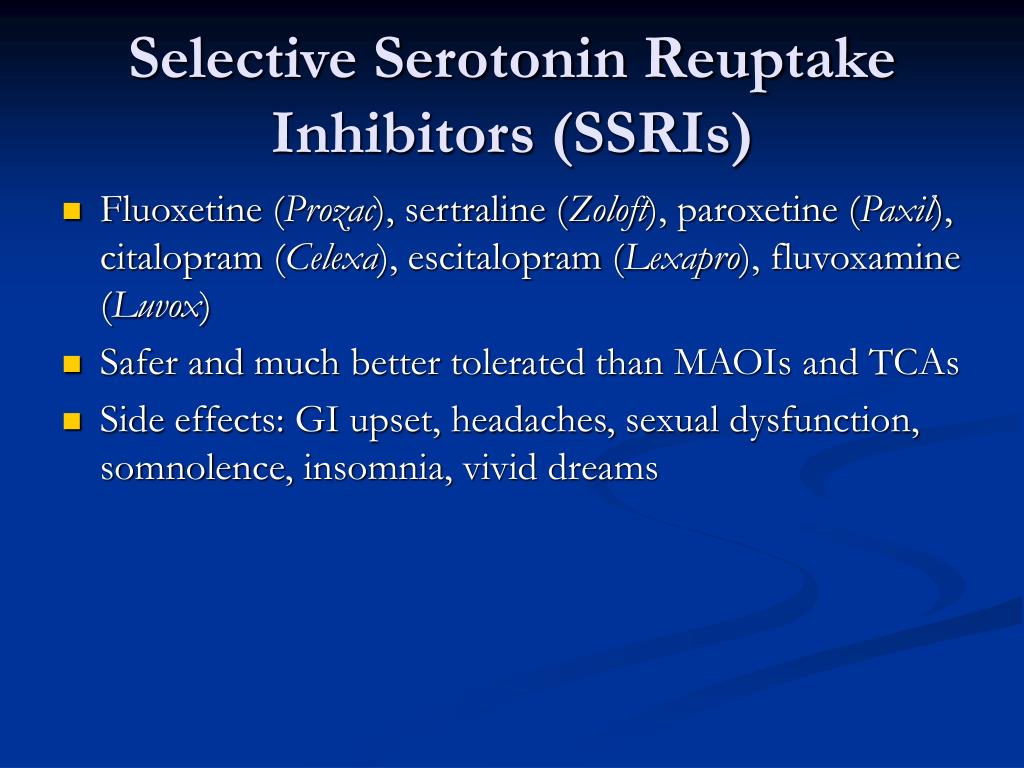
THC is the cannabinoid in marijuana that gets most of the attention. It’s what makes you feel high or relaxed. But another product made from cannabis called cannabidiol (CBD) doesn’t make you feel intoxicated and may help ease pain. Several states have made it legal for CBD to be used for medical reasons.
Does It Work for Migraines?
There’s not a lot of research on this. In a study at the University of Colorado, 121 people who got regular migraine headaches used marijuana daily to prevent attacks. About 40% of them said the number of migraine headaches they got each month was cut in half.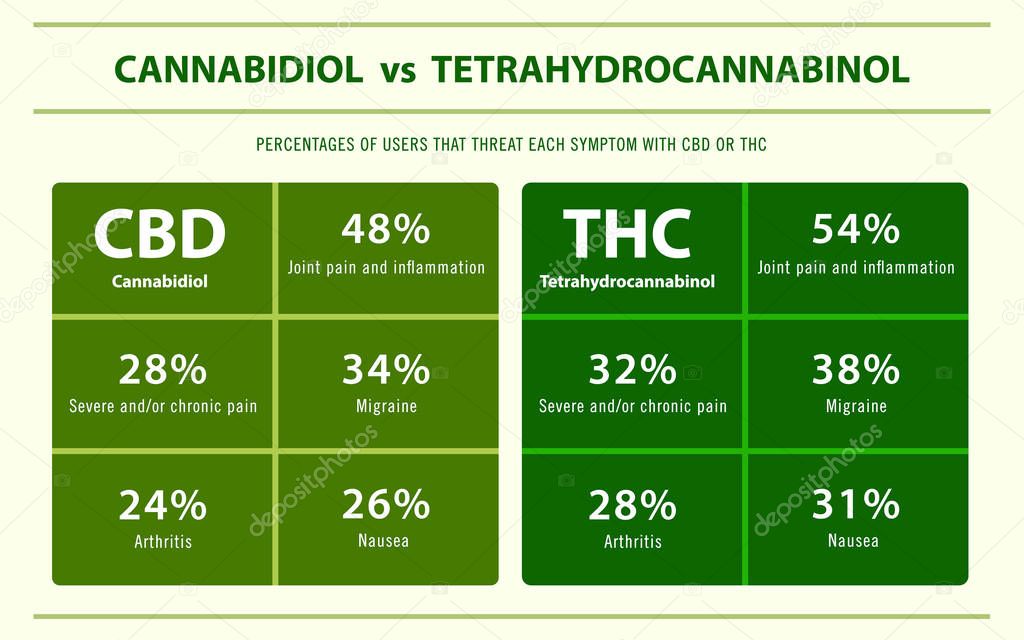
The people used different types of marijuana, but they mostly inhaled it to ease a migraine in progress and some found that it did help stop the pain. Edible products didn’t seem to work as well.
The people who inhaled or smoked marijuana also said it was easier to control the amount of the drug they took in, and they had fewer negative reactions.
What Are the Risks?
If you smoke or eat marijuana, it can make you feel dizzy, weak, confused, sleepy, or moody. And smoking it on a regular basis could harm your heart and lung health over time. Regular use could also lead to addiction and other problems. Short-term use doesn’t seem to be bad for your general health.
Legal Issues
Marijuana is legal for medical use in more than half the states in the U.S. But each state has different laws about how you can buy it or how much you can have. In several states, it’s still illegal to have it even if you have a medical problem that it could treat.
If you have a job, it’s a good idea to know your employer’s rules around drug testing and use, even if it’s legal for medical use in your state. Tests can tell if you have marijuana in your system. And it can stay there up to 30 days after you've used it.
Cannabis for Migraine Pain: What You Need to Know
From triptans to the new calcitonin gene-related peptide (CGRP) inhibitors, there are more and more evidence-based treatments for migraine, a leading cause of disability worldwide.
But migraine treatment is not a one-size-fits-all proposition, and even with the availability of newer, more targeted drugs, as many as 60 percent of people fail to find adequate or consistent relief, according to a report published by Neurology Today in 2020.
No wonder interest in complementary herbal and plant-based therapies, including medical cannabis, is growing.
Nancy Thompson, a 55-year-old Canadian citizen, is one of those people seeking alternatives. Thompson has had migraine attacks since she was a teenager, and once they became frequent (occurring six to seven times weekly), her general practitioner sent her to a neurologist, who prescribed a variety of treatment strategies.
Thompson has had migraine attacks since she was a teenager, and once they became frequent (occurring six to seven times weekly), her general practitioner sent her to a neurologist, who prescribed a variety of treatment strategies.
“We tried a bunch of different things, including an anti-seizure medication and Botox, and for me, they just weren’t doing much of anything. The Botox we considered a success because I would go one day a week without a migraine,” she says.
Desperate for a solution, she and her husband decided, albeit reluctantly, that she should try cannabis.
“I was very apprehensive of it. I had absolutely no idea what would happen,” Thompson says.
Cannabis Use for Headaches Is Not UncommonThompson is not alone in her decision to try cannabis for what has been a lifetime of severe, debilitating headaches. In a survey of U.S. and Canadian adults published in Psychopharmacology in May 2022, as many as 35 percent reported using cannabis to treat their headaches and migraine.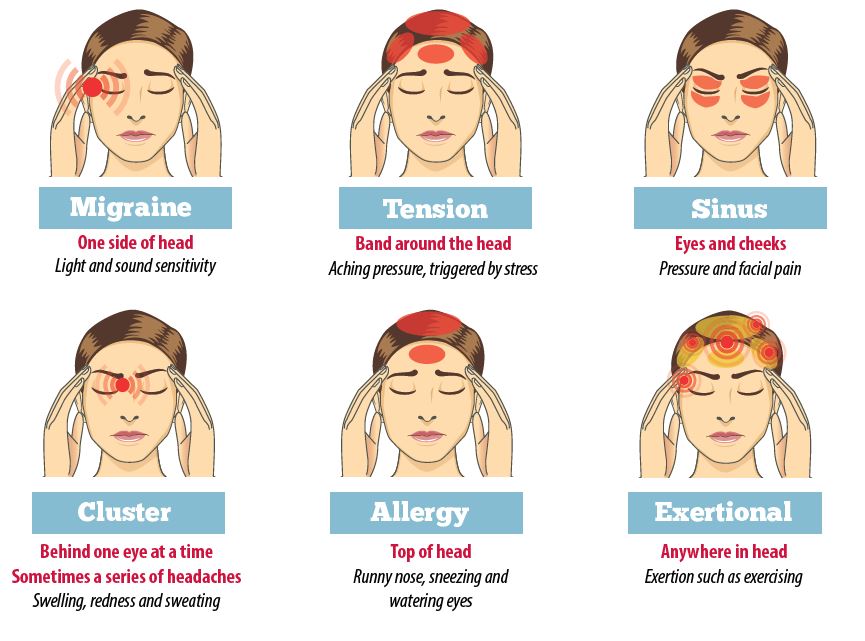
In another survey, published in the Canadian Journal of Neurological Science in September 2021, 34 percent of 200 Canadian patients attending a headache clinic reported using cannabis both for prevention and acute treatment and often at the same time. Sixty percent reported that cannabis reduced the severity of their headaches, while about 30 percent said it prevented their headaches altogether.
Thompson also had a positive experience. With her neurologist’s blessing, a doctor’s prescription, and guidance from a licensed medical cannabis producer, she started vaping cannabis flower. Within three weeks, she went one day without any migraine symptoms, followed by two, and then by three, and then an entire week.
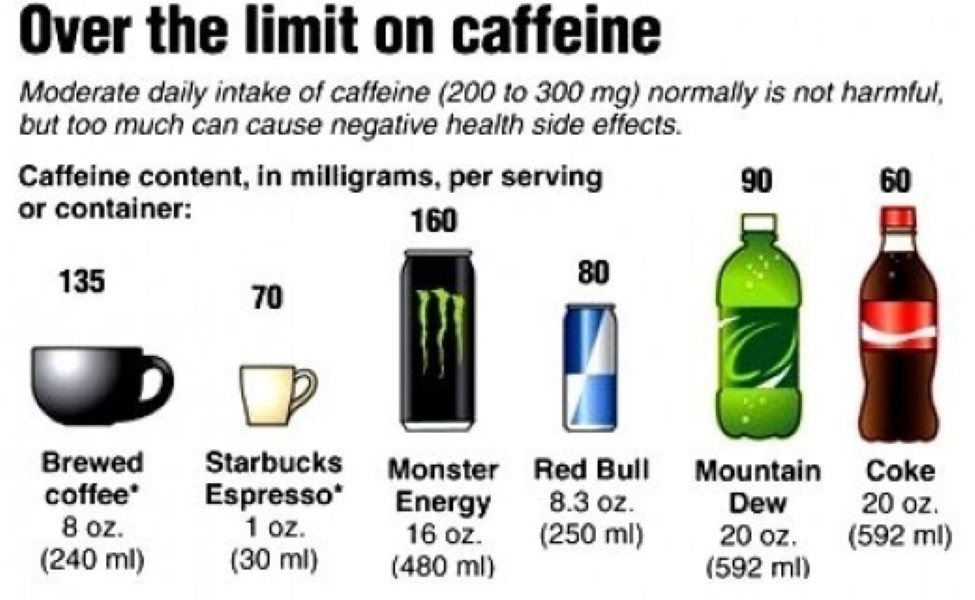
When her migraine symptoms do manage to break through, she says, their duration is slightly shorter. More important, “the pain is nowhere near as bad, that’s for sure, and I can usually get away with just some Tylenol or Advil, go lie down, and within a few hours, I’ll be better,” she says. Thompson also has prescription rescue medication (including a triptan and a buffered aspirin with caffeine) just in case she fails to find relief with cannabis alone.
Thompson also has prescription rescue medication (including a triptan and a buffered aspirin with caffeine) just in case she fails to find relief with cannabis alone.
The link between medical cannabis and migraine is not new. Cannabis has a long history of use in treating severe headache-like pain, with one of the earliest mentions of it dating back to the second millennium B.C. Throughout the centuries that followed, medical cannabis shifted in and out of fashion before regaining its place in modern Western medical toolboxes in the 1840s.
“From 1848 through 1948, cannabis was one of the most commonly used drugs for treatment of migraine,” says Lazlo Mechtler, MD, the medical director of the Dent Neurologic Institute, the Dent Headache Center, and the Cannabis Clinic in Buffalo, New York.
“In the United States, William Osler (the father of modern medicine and a founding member of Johns Hopkins Medical School) used cannabis for treatment of migraines. So did William Gowers, the founding father of neurology in England,” he says.
So did William Gowers, the founding father of neurology in England,” he says.
“Unequivocally, cannabis was one of the drugs of choice back then.”
That is, until the federal government decided to tax and criminalize cannabis in 1937, remove it from the U.S. pharmacopeia in 1942, and then classify it as a Schedule 1 substance in the 1970s (meaning that it had no acceptable medical use and was among the class of drugs having the highest potential for abuse), according to Americans for Safe Access.
Despite ongoing federal limitations, 37 U.S. states have since legalized cannabis for medical or recreational use, which has probably contributed to the renewed interest in its potential effectiveness for treating migraine and other medical conditions.
A Promising but ‘Unproven’ TreatmentBecause of cannabis’s Schedule 1 status, it has been difficult for researchers to obtain special licenses and access the supply of federally endorsed cannabis for their studies. That’s why most of the research examining cannabis in migraine treatment has been observational (meaning that outcomes are measured without introducing a specific treatment or intervention), and why many doctors have been hesitant to recommend cannabis to their patients.
That’s why most of the research examining cannabis in migraine treatment has been observational (meaning that outcomes are measured without introducing a specific treatment or intervention), and why many doctors have been hesitant to recommend cannabis to their patients.
These barriers notwithstanding, observational studies — especially those published within the past few years — have consistently shown benefits of medical cannabis for some people with migraine, including reduced migraine severity or monthly frequency, and have shown that cannabis can be safely substituted for ineffective pharmaceutical drugs.
For example, findings from a study in the 2019 Journal of Pain showed that inhaled cannabis reduced the severity of migraine by almost 50 percent, regardless of the tetrahydrocannabinol (THC) or cannabidiol (CBD) content, formulation, or dose, or how severe the migraine attacks were before the participants tried cannabis. Although many participants developed tolerance, meaning they needed higher doses over time, there did not appear to be an increase in rebound, or medication-overuse, headaches.
Cannabis use reportedly also reduced migraine frequency in as many as 60 percent of Israeli patients with migraine who participated in a questionnaire-based study. Findings, which were published in 2020 in the journal Brain Sciences, showed that compared with people who did not respond to cannabis, those who did experienced 50 percent fewer migraine days per month, significantly lower disability and impact scores, and better sleep quality. When the researchers looked specifically at the chemical components of cannabis being consumed, they found that the majority — 92 percent — were THC-dominant (compared to an even ratio of THC and CBD, or CBD-dominant). In addition, use of medical cannabis tended to result in lower consumption of standard migraine medications, including opioids and triptans.
Similar findings were reported by Canadian researchers in a 2018 survey of chronic pain patients using cannabis that was published in the Journal of Headache Pain. Roughly 45 percent of the 343 participants with probable migraine were able to replace their opioids with cannabis, while 39 percent reported similar substitutions with anti-anxiety and depression medications, and 21 percent with nonsteroidal anti-inflammatory agents (NSAIDs).
Many in the medical community find themselves caught between Schedule 1 and a hard line, seeking answers that are not provided in medical school and that thus far have been lacking in the traditional evidence-based research arena.
“Doctors have never been equipped with scientific information, prospective human data, to be able to educate patients as to what the possible benefits might be from cannabis,” says Nathaniel Schuster, MD, a pain management specialist and headache neurologist at the University of California in San Diego.
Dr. Schuster and his colleagues are hoping to change that.
Schuster is the lead investigator of an ongoing randomized controlled trial assessing the effectiveness of vaporized cannabis treatments in both chronic migraine (defined as more than 15 headache days per month for at least three months) and episodic migraine (defined as 14 or fewer headache days per month).
Participants (who are still being recruited) are blindly randomized to take four puffs of vaporized flower containing THC, a THC-CBD mix, CBD, or placebo as early as possible in the course of a migraine attack.
The primary study goal is to see whether vaping cannabis safely delivers acute headache pain relief within two hours of the treatment. The study will also evaluate whether the treatment eliminates participants’ most bothersome symptom — light sensitivity, sound sensitivity, or nausea — within two hours, as well as what effect it has on symptoms after 24 and 48 hours.
Adding Cannabis to Your Migraine ToolboxWhile the medical community eagerly awaits results of what portends to be an opening for controlled clinical research, what’s the best rule of thumb for people seeking relief now?
Before you consider trying medical cannabis for migraine, it’s important to weigh the potential risks and benefits and ideally (and most importantly) bring a doctor into the conversation.
“Most people who have migraine have it for many years, and most people never talk to a doctor about it, so most are not using the optimal standard of care — evidence-based treatments, which are now much better than they were even a few years ago,” notes Schuster.
“Work with a doctor,” he says. “If you haven’t seen a doctor in the last couple of years, certainly see your doctor again. Migraine is a medical condition that warrants medical treatment.”
An important question to consider when choosing a doctor is whether that person has direct experience in guiding patients on how to use cannabis as migraine treatment.
“Cannabis, or the endocannabinoid system, has not been taught in medical school for years, and only recently have physicians been exposed to that knowledge,” Dr. Mechtler says. “I started a cannabis clinic, so what I’ve done is take cannabis off the streets to a form of medical cannabis under the control of a clinician,” he adds. Thus far, Mechtler says that he’s treated more than 13,000 patients.
Dosing and AdministrationWhile many clinical studies have been conducted using inhaled cannabis, Mechtler does not recommend smoking, noting the risks in people with asthma or lung disease. Instead, people with migraine who wish to try cannabis should consider vaping or tinctures, he says; either formulation quickly delivers cannabis to prevent or stop a migraine early in its tracks, since it bypasses the liver and is directly absorbed into the bloodstream.
The optimal dosing and chemical makeup (chemovars) of medical cannabis varies from person to person, so it’s wise to start low and go slow. Simply, most cannabis formulations contain one of three combinations: chemovar type 1 (THC-dominant), chemovar type 2 (combined THC and CBD), or chemovar type 2 (CBD-dominant). While a majority of observational studies have focused on the THC-dominant approach, the decision is a personal one and should be made with a doctor’s guidance.
“Some people respond to a one-to-one ratio, some people to THC and some people just CBD,” Mechtler says. “But you have to consider age, other medical conditions, type of migraine, frequency, and severity.”
The trial-and-error approach also involves trying a chemovar for a period of time, then returning to the doctor for follow-up, ideally every three months for at least the first year of use. Any discussion should include whether or not medical cannabis is helping to relieve pain, a report of side effects, the frequency and timing of cannabis use, and current dosage (including the need for higher doses to achieve the same effect).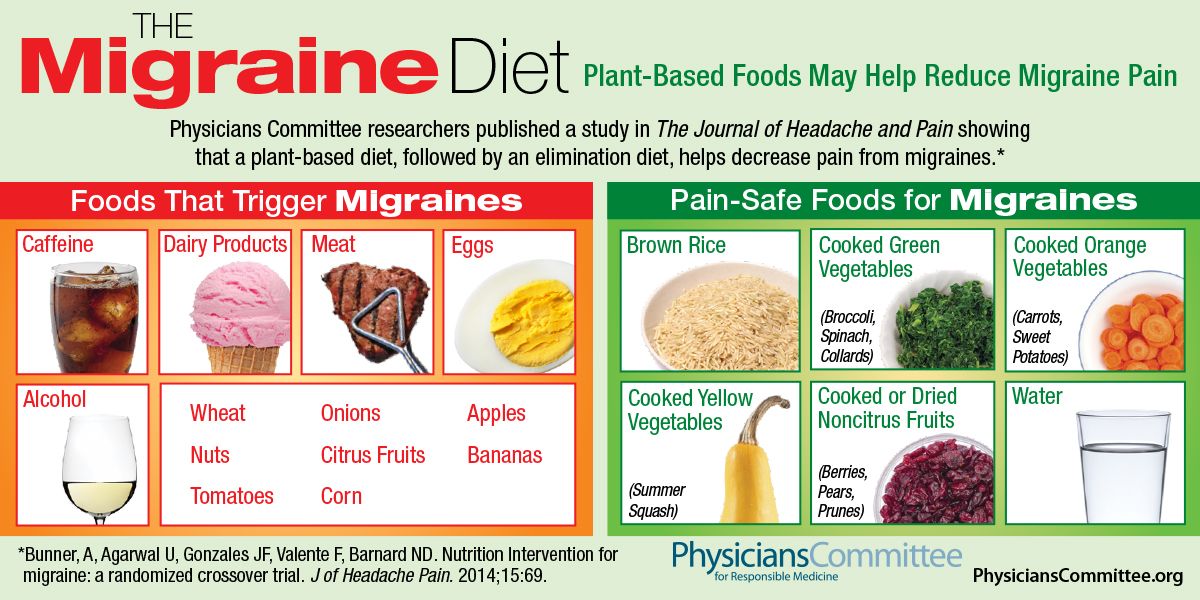 This way, the physician can adjust based on individual outcomes, and in particular, be on the lookout for potential side effects.
This way, the physician can adjust based on individual outcomes, and in particular, be on the lookout for potential side effects.
Overall, most people appear to tolerate cannabis well, but there are a few red flags, according to a review appearing in the May 2019 Clinical Therapeutics and Pharmacology. Although the list is hardly exhaustive, medical cannabis users should be aware of the risk for possible euphoria (“high,” especially with cannabis that is THC-dominant, and often seen in older users who’ve never tried cannabis), anxiety or paranoia, impaired cognition and driving, an increase in cardiovascular activity (including elevated heart rate or blood pressure), eventual tolerance (leading to the need for increasingly higher doses), and medication overuse headache.
Thompson says that since she started using medical cannabis, she has experienced occasional memory lapses (for example, searching for a word while speaking) but that overall, it’s been a life-changer.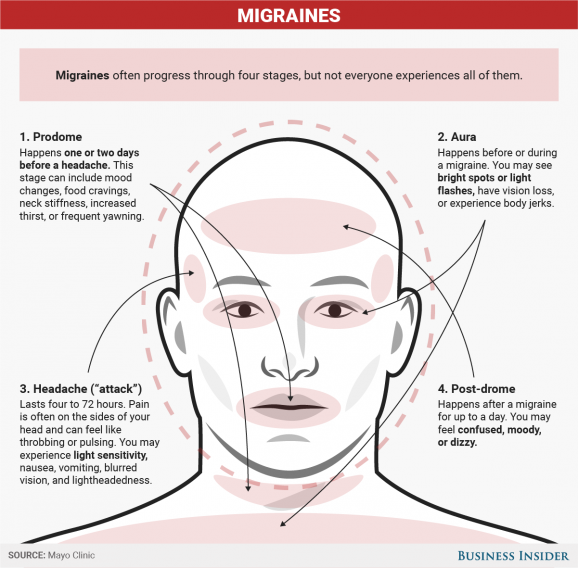
“The difference in my life is so incredible. My kids have their mom back. My husband has his wife back. I’m back in the world, able to work and do things again.”
Keep Your Options OpenFor Thompson, cannabis has been a gateway toward getting her life back on track. But success varies from one person with migraine to another, which is why Mechtler considers it to be just one part of the migraine toolbox.
“I strongly believe that you don’t give patients one option,” he says, “but you have multiple different tools — one for acute migraine, one for nausea, and one could be a cannabis product. That gives power back to the patient.”
9 Top Remedies for Menstrual Migraine
Get an expert’s advice on how best to prevent menstrual and menstrually related migraine.
By Becky Upham
Migraine Diet Modifications: What Really Works?
By emphasizing anti-inflammatory foods in your diet and being aware of potential food triggers, you may be able to reduce the frequency of migraine attacks.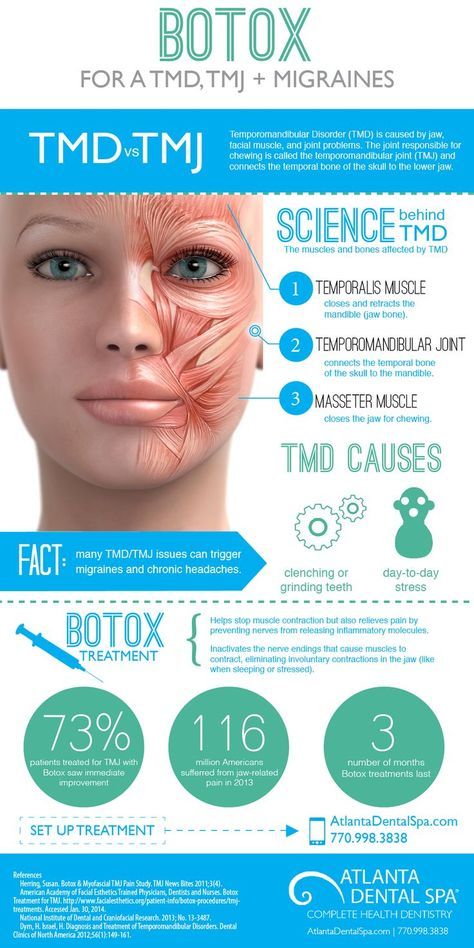 ..
..
By Quinn Phillips
Nerve Stimulation Devices for Migraine Treatment
Devices that deliver electrical or magnetic pulses to specific nerves may reduce migraine episodes or pain intensity.
By Brian P. Dunleavy
Causes and Risk Factors of Migraine
Genetics and other risk factors make you more likely to have migraine. Here are the most common triggers to avoid.
By Becky Upham
Does Migraine Cause Memory Loss?
Migraine’s effects on the brain and memory are complex. Here’s what you need to know.
By Brian P. Dunleavy
What Is Migraine? Symptoms, Causes, Diagnosis, Treatment, and Prevention
By Brian P.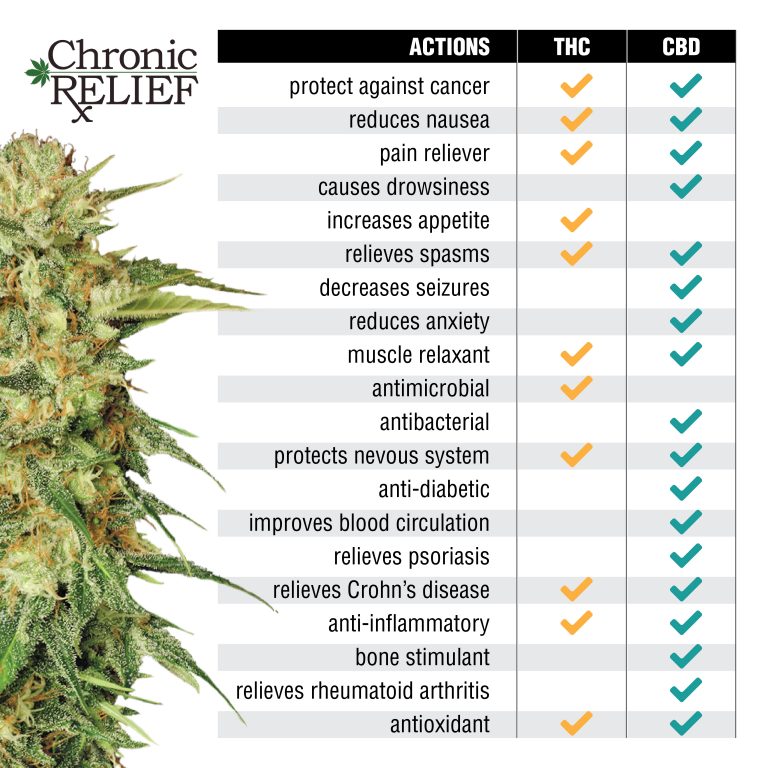 Dunleavy
Dunleavy10 Tips for Taming Migraines While Traveling
Coping with a migraine can put a serious damper on travel plans. Use this advice to stay headache-free and enjoy your trip.
By Jen Laskey
Migraine Signs and Symptoms
By Brian P. DunleavyHow Is Migraine Diagnosed?
Too often, migraine goes undiagnosed. But a correct diagnosis can lead to better treatment and improved quality of life.
By Becky Upham
CBD for migraines | Cannadorra Russia
Almost every tenth person in the world suffers from a migraine or headache. Thousands of people seek professional help or visit a doctor. This disease is very complex, and the question is, can it be cured? And how? Can CBD, a natural dietary supplement, fight migraines?
What is characteristic of migraine?
Migraine is a disease characterized by recurrent attacks of headache with typical accompanying symptoms: nausea, vomiting, dizziness, increased sensitivity to sounds, smells, etc.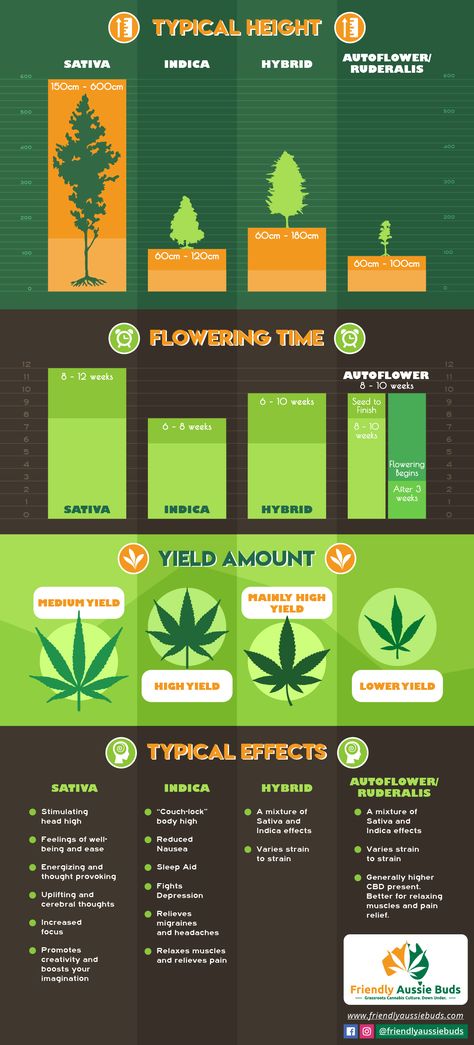 It is more common in women than in men. Migraine headaches are moderate to very severe and can last from a few hours to 3 days. nine0003
It is more common in women than in men. Migraine headaches are moderate to very severe and can last from a few hours to 3 days. nine0003
If migraines are rare and do not have a significant impact on a person's ability to work, then usually medications are prescribed only at the time of the onset of pain. If the attacks are frequent, disrupt the ability to work and are difficult to treat, it makes sense to pay attention to the prevention of migraine attacks. In recent years, many modern methods of combating migraine have appeared, which effectively prevent the development of attacks and minimize the use of drugs. But can CBD help with migraines? nine0003
How can cannabis help with migraines?
As we already know, cannabis interacts with the ECS (endocannabinoid system). The endocannabinoid system regulates the amount of cannabinoids that our body produces on its own and that bind simultaneously to the CB1 and CB2 receptors. The CB1 receptor is located in those parts of the brain and nervous tissue that are responsible for regulating pain signals. Studies have shown that when endocannabinoids activate CB1 receptors, they can block these signals, thereby suppressing pain.
Studies have shown that when endocannabinoids activate CB1 receptors, they can block these signals, thereby suppressing pain.
How can hemp oil with CBD help with migraines?
- Hemp oil can relieve pain and reduce inflammation, and some research suggests that CBD may help treat migraines.
- A growing body of research also shows that CBD can help relieve pain, especially neurological pain associated with various medical conditions.
Low levels of endocannabinoids can lead to reduced pain tolerance. Chronically low cannabinoid levels are believed to play a role in causing hyperalgesia (impaired pain perception) in diseases such as migraine, fibromyalgia, and irritable bowel syndrome. A study on the endocannabinoid anandamide found that people with migraines had significantly less anandamide in their cerebrospinal fluid than those who did not have migraines. This could mean that low levels of endocannabinoids could be causing headaches or migraines. nine0003
nine0003
The use of CBD for headaches is best discussed with your neurologist, but most physicians are willing to let the patient actively use it in their treatment. CBD is a purely natural, non-psychoactive product and you can only "win" by trying it.
What types of hemp CBD can be used for migraines?
Currently the product range is very wide - you can take CBD oil (which we recommend taking in the morning and at any time of the day), CBD capsules (which we recommend taking at night) or CBD vaporization (especially effective for the first symptoms of a migraine). nine0003
Try CBD hemp for migraine and you: take advantage of the promotion until 07/31/2021 - for each CBD liquid vaporizer - CBD liquid as a gift for FREE.
CBD vaporization helps the whole family fight headaches
Unfortunately, my loved ones often suffer from problems associated with headaches - including depression, ... I myself have gone through such a period, and whenever I have a hint of a headache, I vaporize CBD liquid and immediately feel better. The most interesting thing is that the head does not even begin to hurt "for real". nine0003
The most interesting thing is that the head does not even begin to hurt "for real". nine0003
And this is exactly what I recommend to everyone - my mother, my grandmother, my girlfriend - and it really works! I get only positive feedback from them.
Thanks to hemp for being you!
5 / 5
Michaela
Treatment of migraines with marijuana Ukraine - Magaz420
About migraines, or how not to send everything to hell
Continuing the theme of the relationship between mental and physical health, today we want to talk with you about migraines. Unfortunately, this neurological problem is quite common among people of all ages and genders. It can arise due to many factors, having a direct negative impact on all areas of life. nine0003
We would like to point out that people who suffer from headache attacks lose their ability to work and perform daily activities, facing weakness and low levels of concentration. They suffer from debilitating pain sensations, feel mood swings and face a painful reaction to light, up to nausea and dizziness.
They suffer from debilitating pain sensations, feel mood swings and face a painful reaction to light, up to nausea and dizziness.
Also, one should not underestimate the negative impact of migraine on the psychological state of a person, since pain syndromes have an unpleasant effect on the autonomic nervous system, thereby causing anxiety and nervousness, problems with sleep and appetite, which, at times, exacerbates an already rather unpleasant situation . nine0003
In the fight against cancer, marijuana is used to reduce pain.
Based on research by British scientists, approximately 15 people out of 100 are forced to experience migraine attacks at least once a month. That is why those suffering from headaches are used to relying on the help of painkillers, which, unfortunately, are not always able to provide the desired effect. Moreover, these pharmaceutical preparations have negative side effects, which can pose a significant danger to the human body. nine0003
Which, by the way, can't be said about marijuana.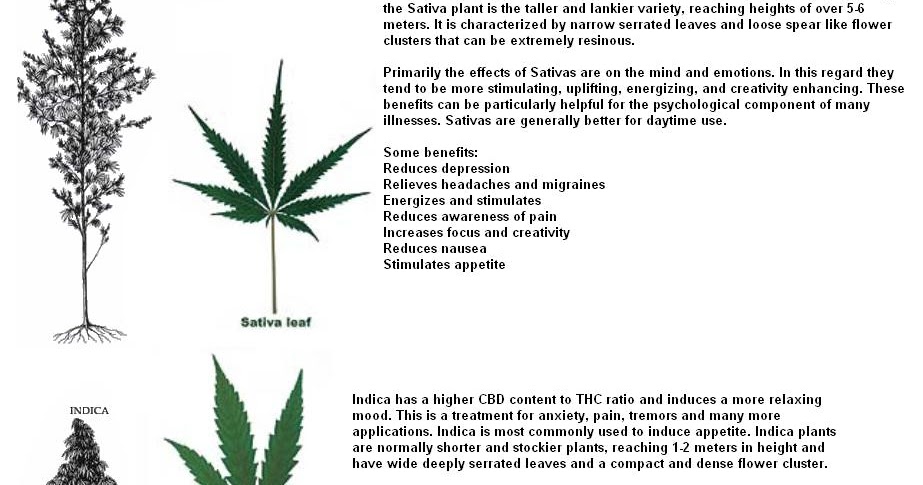
Cannabis cure headaches?
The human body includes many biological systems, one of which is endocannabinoid. It is found in the central nervous system and brain and consists of endocannabinoids and cannabinoid receptors.
So, the endocannabinoid system is important in the functioning of body systems, which includes such functions as pain, digestion, appetite and mood. And in turn, cannabis is really able to relieve pain, by synthesizing (THC and CBD), which can create interaction with certain receptors in the human body. This allows you to regulate the processes in the human body, reducing pain and discomfort. nine0003
Marijuana and Migraine Study
In 2016, a large-scale study of more than 121 adults diagnosed with migraine was published. Scientists say that medical marijuana can reduce the number of attacks of the disease by half.
And another study by Italian scientists, which was published on the website of the Congress of the European Academy of Neurology in 2017, proved that the use of medical marijuana takes place in the treatment and prevention of migraine.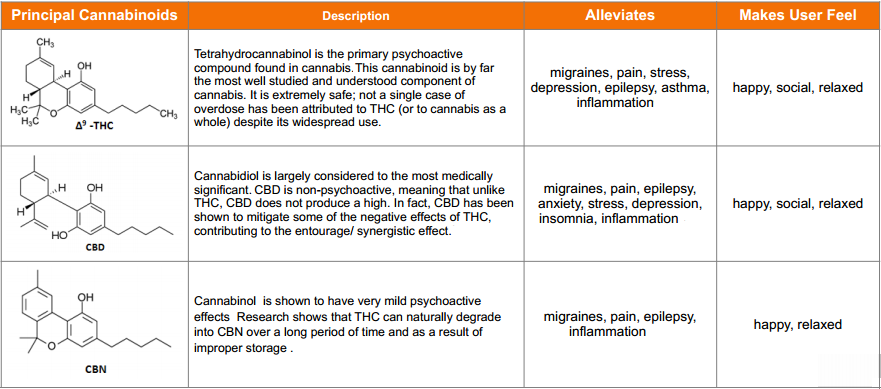 The group, consisting of 48 people, consumed specially calculated dosages of a solution that contained THC and CBD. The result was the discovery of the fact that acute attacks of headaches were reduced by 55% less often than it was just a few weeks ago. nine0003
The group, consisting of 48 people, consumed specially calculated dosages of a solution that contained THC and CBD. The result was the discovery of the fact that acute attacks of headaches were reduced by 55% less often than it was just a few weeks ago. nine0003
A similar effect was found and proven in a 2016 study that showed a 40% reduction in monthly attacks and a 43% reduction in pain intensity.
Patients also noted that in addition to reducing pain, they experienced many more positive changes that related to reducing anxiety, normalizing sleep and relaxing the muscles of the body.
A group of painkillers in the fight against migraine
We cannot exclude and dispute the effectiveness of medicines in the treatment of acute migraine attacks, which, if ignored, can be dangerous not only to health, but also to life. nine0003
But still, as mentioned above, we want to once again note the individual tolerance factor and the presence of some side effects from anesthesia in the form of weakness, problems with stools, increased blood pressure and even impaired coordination.