Sertraline withdrawal side effects
Sertraline (Zoloft) | NAMI: National Alliance on Mental Illness
Brand name: Zoloft®
- Tablets: 25 mg, 50 mg, 100 mg
- Liquid: 20 mg/mL
Generic name: sertraline (SER tra leen)
All FDA black box warnings are at the end of this fact sheet. Please review before taking this medication.
What Is Sertraline And What Does It Treat?
Sertraline is an antidepressant medication that works in the brain. It is approved for the treatment of major depressive disorder (MDD), posttraumatic stress disorder (PTSD), premenstrual dysphoric disorder (PMDD), panic disorder, and social anxiety disorder. It is also approved to treat obsessive-compulsive disorder (OCD) in adults, children and adolescents aged 6-17 years.
Symptoms of depression include:
- Depressed mood - feeling sad, empty, or tearful
- Feeling worthless, guilty, hopeless, and helpless
- Loss of interest or pleasure in your usual activities
- Sleep and eat more or less than usual (for most people it is less)
- Low energy, trouble concentrating, or thoughts of death (suicidal thinking)
- Psychomotor agitation (‘nervous energy’)
- Psychomotor retardation (feeling like you are moving and thinking in slow motion)
- Suicidal thoughts or behaviors
PTSD occurs when a person experiences a traumatic event (e. g., assault, combat experience) and then later feels on edge; avoids situations that remind them of the event; and experiences flashbacks or nightmares.
PMDD is a condition where a woman experiences depression, tension, and irritability for a few days prior to menstruation that end when menstruation begins. These symptoms are more severe than those of premenstrual syndrome (PMS).
Panic Disorder occurs when a person experiences unexpected and repeated episodes of intense fear. These episodes have physical symptoms including chest pain, shortness of breath, heart palpitations, sweating, dizziness, and nausea. Fear of future episodes is also part of panic disorder.
Obsessive Compulsive Disorder (OCD) occurs when a person experiences the following symptoms at the same time:
- Obsessions (unwanted, recurrent, and disturbing thoughts)
- Compulsions (repetitive, ritualized behaviors that the person feels driven to perform in order to lessen the anxiety produced by the obsessions)
Social phobia/social anxiety disorder is a fear of situations where one may feel as if they are being judged by others.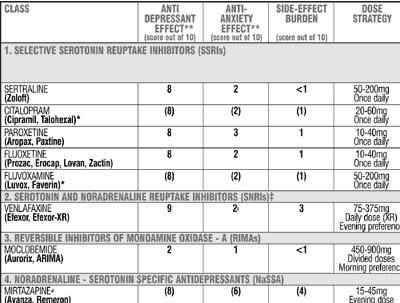 Symptoms include:
Symptoms include:
- Blushing
- Difficulty talking
- Nausea
- Sweating
- Shaking
Sertraline may also be helpful when prescribed “off-label” for binge-eating disorder, bulimia nervosa, and generalized anxiety disorder (GAD). “Off-label” means that it hasn't been approved by the Food and Drug Administration for this condition. Your mental health provider should justify his or her thinking in recommending any “off-label” treatment. They should be clear about the limits of the research around that medication and if there are any other options.
What Is The Most Important Information I Should Know About Sertraline?
Do not stop taking sertraline, even when you feel better. With input from you, your health care provider will assess how long you will need to take the medicine.
Missing doses of sertraline may increase your risk for relapse in your symptoms.
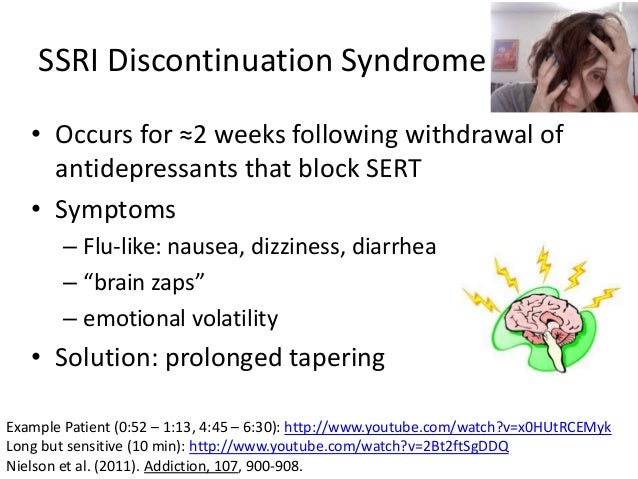
Stopping sertraline abruptly may result in one or more of the following withdrawal symptoms: irritability, nausea, feeling dizzy, vomiting, nightmares, headache, and/or paresthesias (prickling, tingling sensation on the skin).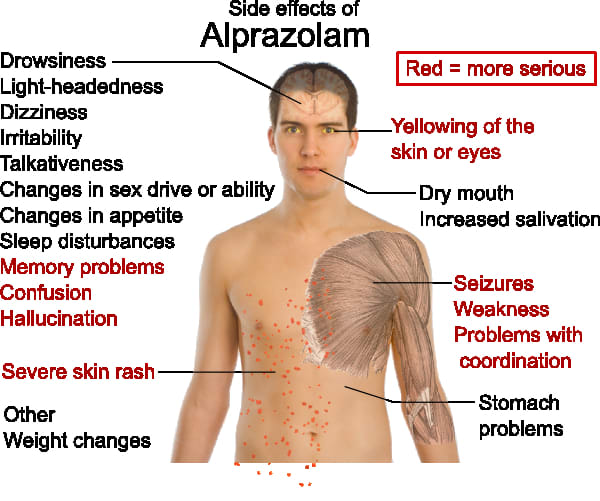
Depression is also a part of bipolar illness. People with bipolar disorder who take antidepressants may be at risk for "switching" from depression into mania. Symptoms of mania include "high" or irritable mood, very high self-esteem, decreased need for sleep, pressure to keep talking, racing thoughts, being easily distracted, frequently involved in activities with a large risk for bad consequences (for example, excessive buying sprees).
Medical attention should be sought if serotonin syndrome is suspected. Please refer to serious side effects for signs/symptoms.
Are There Specific Concerns About Sertraline And Pregnancy?
If you are planning on becoming pregnant, notify your health care provider to best manage your medications. People living with MDD who wish to become pregnant face important decisions. Untreated MDD has risks to the fetus, as well as the mother. It is important to discuss the risks and benefits of treatment with your doctor and caregivers. For women who take antidepressant medications during weeks 13 through the end of their pregnancy (second and third trimesters), there is a risk that the baby can be born before it is fully developed (before 37 weeks).
For mothers who have taken SSRIs during their pregnancy, there appears to be less than a 1% chance of infants developing persistent pulmonary hypertension. This is a potentially fatal condition that is associated with use of the antidepressant in the second half of pregnancy. However, women who discontinued antidepressant therapy were five times more likely to have a depression relapse than those who continued their antidepressant. If you are pregnant, please discuss the risks and benefits of antidepressant use with your health care provider.
Caution is advised with breastfeeding since sertraline does pass into breast milk.
What Should I Discuss With My Health Care Provider Before Taking Sertraline?
- Symptoms of your condition that bother you the most
- If you have thoughts of suicide or harming yourself
- Medications you have taken in the past for your condition, whether they were effective or caused any adverse effects
- If you experience side effects from your medications, discuss them with your provider.
 Some side effects may pass with time, but others may require changes in the medication.
Some side effects may pass with time, but others may require changes in the medication. - Any other psychiatric or medical problems you have, including a history of bipolar disorder
- All other medications you are currently taking (including over the counter products, herbal and nutritional supplements) and any medication allergies you have
- Other non-medication treatment you are receiving, such as talk therapy or substance abuse treatment. Your provider can explain how these different treatments work with the medication.
- If you are pregnant, plan to become pregnant, or are breastfeeding
- If you drink alcohol or use drugs
How Should I Take Sertraline?
Sertraline is usually taken one time per day with or without food.
Typically patients begin at a low dose of medicine and the dose is increased slowly over several weeks.
The dose usually ranges from 50 mg to 200 mg. Only your health care provider can determine the correct dose for you.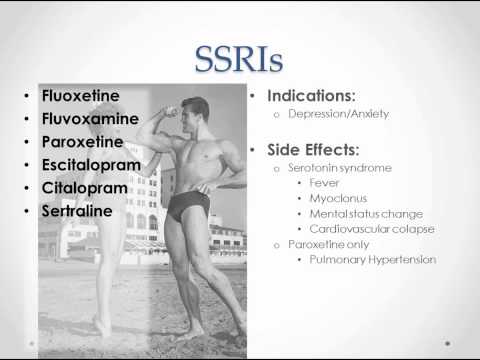
If you are taking it for PMDD, sertraline can be taken once daily (everyday) or intermittently (usually starting 14 days prior to menstruation through the first full day of menses of each cycle).
The liquid should be measured with an oral syringe or dropper which you can get from your pharmacy. It should be added to 4 ounces of water, ginger ale, lemon/lime soda, lemonade, or orange juice immediately prior to taking the medication. It should not be mixed in advance.
Consider using a calendar, pillbox, alarm clock, or cell phone alert to help you remember to take your medication. You may also ask a family member or friend to remind you or check in with you to be sure you are taking your medication.
What Happens If I Miss A Dose Of Sertraline?
If you miss a dose of sertraline, take it as soon as you remember, unless it is closer to the time of your next dose. Discuss this with your health care provider. Do not double your next dose or take more than what is prescribed.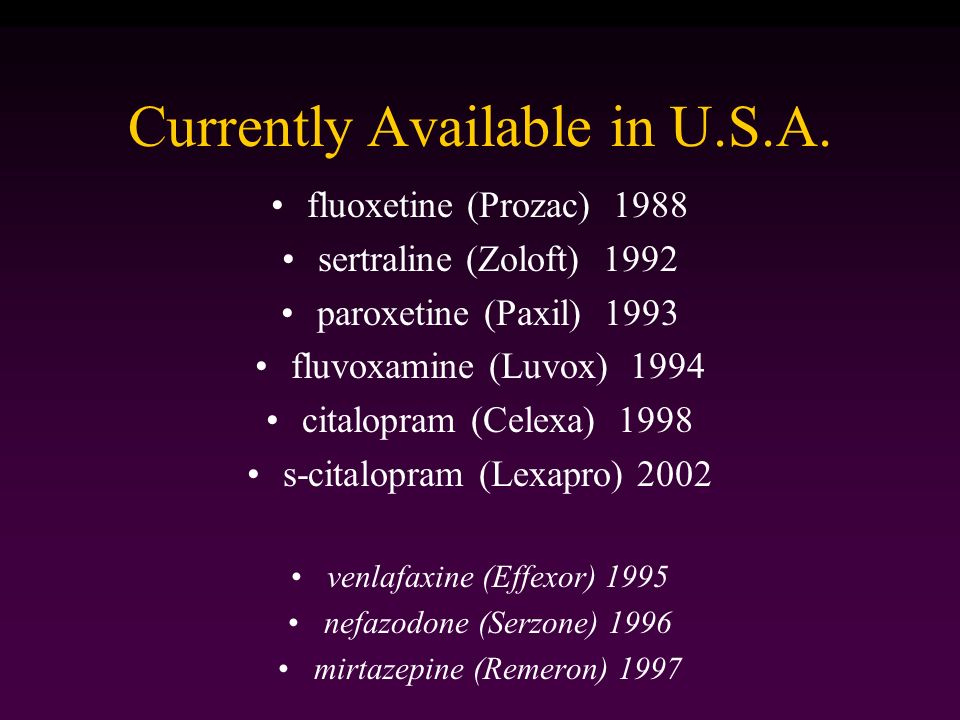
What Should I Avoid While Taking Sertraline?
Avoid drinking alcohol or using illegal drugs while you are taking antidepressant medications. They may decrease the benefits (e.g., worsen your condition) and increase adverse effects (e.g., sedation) of the medication.
What Happens If I Overdose With Sertraline?
If an overdose occurs, call your doctor or 911. You may need urgent medical care. You may also contact the poison control center at 1-800-222-1222.
A specific treatment to reverse the effects of sertraline does not exist.
What Are The Possible Side Effects Of Sertraline?
Common side effects
- Headache, nausea, diarrhea, dry mouth, increased sweating
- Feeling nervous, restless, fatigued, sleepy or having trouble sleeping (insomnia)
These will often improve over the first week or two as you continue to take the medication.
Sexual side effects, such as problems with orgasm or ejaculatory delay often do not diminish over time.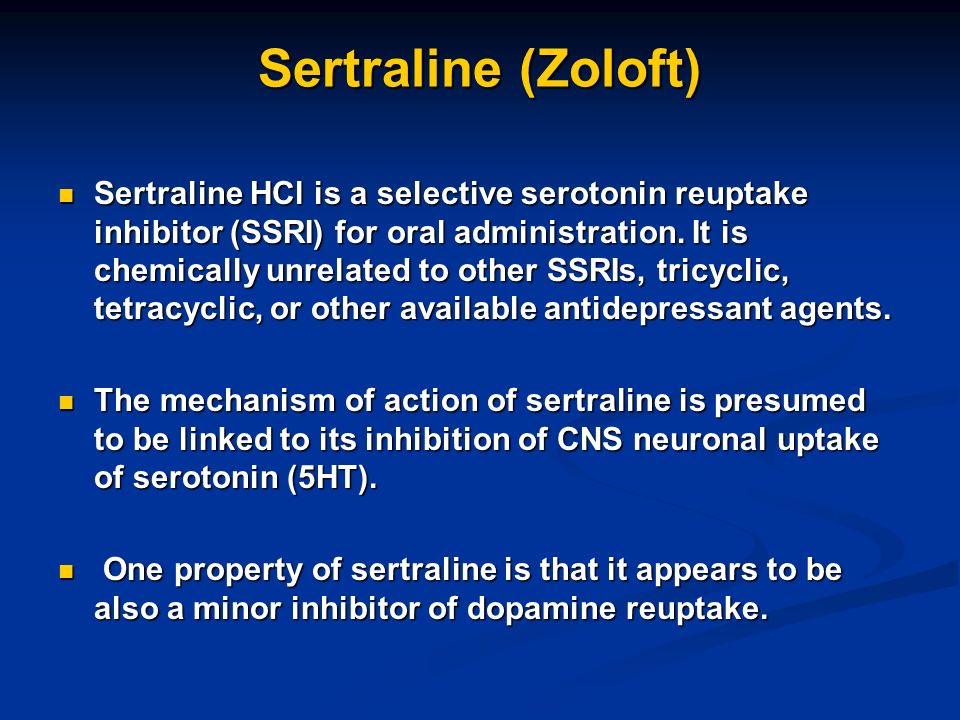
Rare/serious side effects
Low sodium blood levels (symptoms of low sodium levels may include headache, weakness, difficulty concentrating and remembering), teeth grinding, angle closure glaucoma (symptoms of angle closure glaucoma may include eye pain, changes in vision, swelling or redness in or around eye).
Serotonin syndrome (symptoms may include shivering, diarrhea, confusion, severe muscle tightness, fever, seizures, and death), seizure
SSRI antidepressants including sertraline may increase the risk of bleeding events. Combined use of aspirin, nonsteroidal anti-inflammatory drugs (e.g., ibuprofen, naproxen), warfarin, and other anti-coagulants may increase this risk. This may include gums that bleed more easily, nose bleed, or gastrointestinal bleeding. Some cases have been life threatening.
Are There Any Risks For Taking Sertraline For Long Periods Of Time?
To date, there are no known problems associated with long term use of sertraline.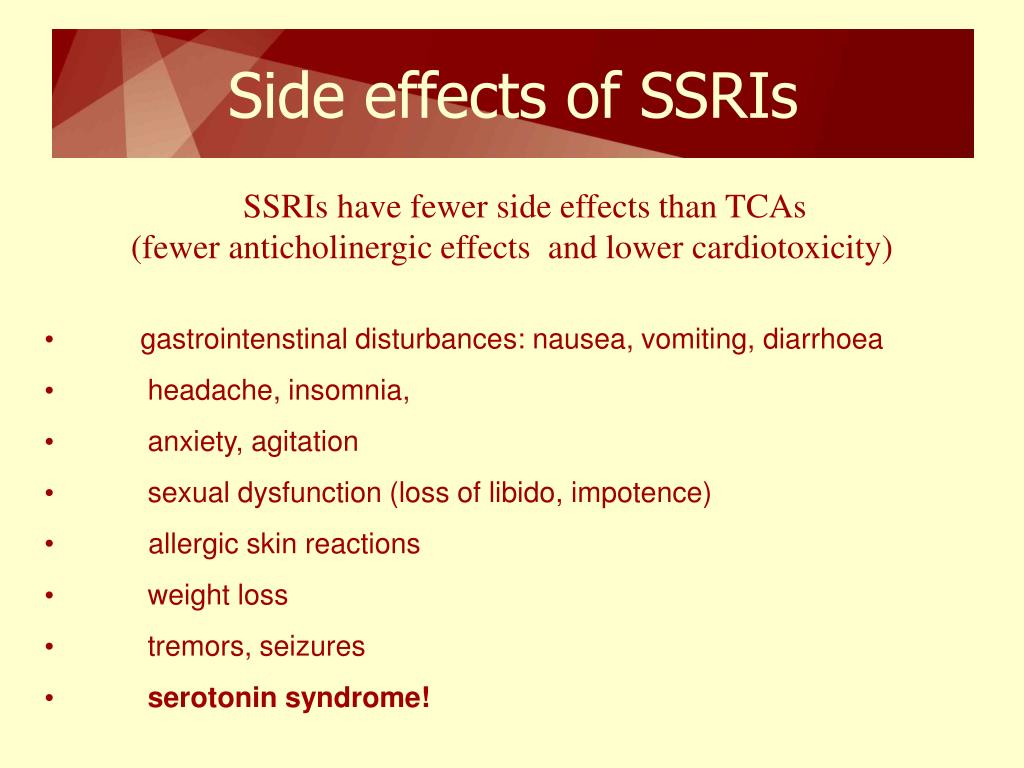 It is a safe and effective medication when used as directed.
It is a safe and effective medication when used as directed.
What Other Medications May Interact With Sertraline?
Sertraline should not be taken with or within two weeks of taking monoamine oxidase inhibitors (MAOIs). These include phenelzine (Nardil®), tranylcypromine (Parnate®), isocarboxazid (Marplan®), rasagiline (Azilect®), and selegiline (Emsam®).
Although rare, there is an increased risk of serotonin syndrome when sertraline is used with other medications that increase serotonin, such as other antidepressants, migraine medications called “triptans” (e.g., Imitrex®), some pain medications (e.g., tramadol (Ultram®)), and the antibiotic linezolid (Zyvox®).
Sertraline should not be taken with pimozide (Orap®).
Sertraline may increase the effects of other medications that can cause bleeding (e.g., ibuprofen (Advil®, Motrin®), warfarin (Coumadin®) and aspirin).
Sertraline liquid should NOT be taken in combination with disulfiram (Antabuse®) due to the alcohol content of the concentrate.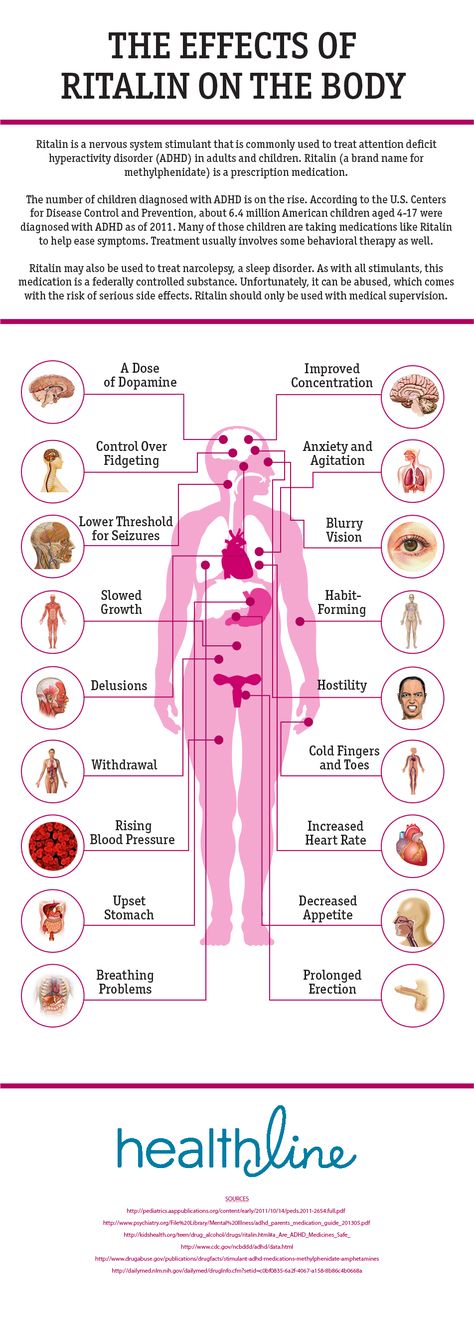
How Long Does It Take For Sertraline To Work?
Sleep, energy, or appetite may show some improvement within the first 1-2 weeks. Improvement in these physical symptoms can be an important early signal that the medication is working. Depressed mood and lack of interest in activities may need up to 6-8 weeks to fully improve.
Summary of FDA Black Box Warnings
Suicidal thoughts or actions in children and adults
Depression and certain other psychiatric disorders are themselves associated with increases in the risk of suicide. Patients with major depressive disorder (MDD), both adult and pediatric, may experience worsening of their depression and/or the emergence of suicidal ideation and behavior (suicidality) or unusual changes in behavior, whether or not they are taking antidepressant medications. This risk may persist until significant remission occurs.
In short-term studies, antidepressants increased the risk of suicidality in children, adolescents, and young adults when compared to placebo.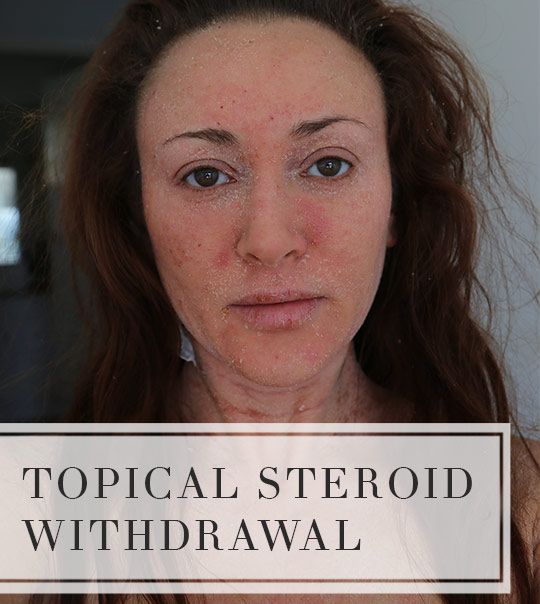 Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24. Adults age 65 and older taking antidepressants have a decreased risk of suicidality. Patients, their families, and caregivers should be alert to the emergence of anxiety, restlessness, irritability, aggressiveness and insomnia. If these symptoms emerge, they should be reported to the patient’s prescriber or health care professional. All patients being treated with antidepressants for any indication should watch for and notify their health care provider for worsening symptoms, suicidality and unusual changes in behavior, especially during the first few months of treatment.
Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24. Adults age 65 and older taking antidepressants have a decreased risk of suicidality. Patients, their families, and caregivers should be alert to the emergence of anxiety, restlessness, irritability, aggressiveness and insomnia. If these symptoms emerge, they should be reported to the patient’s prescriber or health care professional. All patients being treated with antidepressants for any indication should watch for and notify their health care provider for worsening symptoms, suicidality and unusual changes in behavior, especially during the first few months of treatment.
Provided by
(December 2020)
©2020 The College of Psychiatric and Neurologic Pharmacists (CPNP) and the National Alliance on Mental Illness (NAMI). CPNP and NAMI make this document available under the Creative Commons Attribution-No Derivatives 4. 0 International License. Last Updated: January 2016.
0 International License. Last Updated: January 2016.
This information is being provided as a community outreach effort of the College of Psychiatric and Neurologic Pharmacists. This information is for educational and informational purposes only and is not medical advice. This information contains a summary of important points and is not an exhaustive review of information about the medication. Always seek the advice of a physician or other qualified medical professional with any questions you may have regarding medications or medical conditions. Never delay seeking professional medical advice or disregard medical professional advice as a result of any information provided herein. The College of Psychiatric and Neurologic Pharmacists disclaims any and all liability alleged as a result of the information provided herein.
What are the symptoms of Zoloft withdrawal?
Sertraline, which is available under the brand name Zoloft, is an antidepressant belonging to a group of medications known as selective serotonin reuptake inhibitors (SSRIs). When stopping antidepressants such as Zoloft, people may begin to experience withdrawal symptoms.
When stopping antidepressants such as Zoloft, people may begin to experience withdrawal symptoms.
Sertraline is one of the most common antidepressants a doctor may prescribe. When a person is ready to discontinue an antidepressant, they may experience withdrawal symptoms, which a doctor may refer to as discontinuation syndrome.
Some research notes that roughly 20% of people may develop discontinuation symptoms following a reduction in dose. Other sources suggest that up to 80% of people who abruptly stop antidepressants may experience withdrawal symptoms.
Common discontinuation symptoms of stopping sertraline may include nausea, headaches, and tingling skin. For this reason, when a person decides to discontinue sertraline, they should discuss this with their doctor.
The doctor may recommend gradually lowering the dose to reduce or avoid symptoms. It is not advisable for a person to reduce or stop their dosage without their doctor’s approval.
In this article, we will discuss Zoloft withdrawal symptoms, their duration, and when to see a doctor.
Sertraline, which is available under brand names such as Zoloft and Lustral, is a type of SSRI antidepressant. In 1991, the United States approved sertraline to help treat:
- major depressive disorder
- post-traumatic stress disorder
- panic disorder
- social anxiety disorder
- premenstrual dysphoric disorder
- obsessive-compulsive disorder in children, adults, and adolescents 6–17 years old
In some cases, a doctor may also prescribe Zoloft off-label to help treat bulimia nervosa and generalized anxiety disorder.
Similar to many other antidepressants, sertraline has a black box warning. This is the most serious warning from the Food and Drug Administration (FDA). It alerts doctors and patients about potential drug effects, such as suicidal thoughts and behaviors.
It is relatively common for people to experience some withdrawal symptoms when stopping or tapering antidepressants. Some research notes that 46% of people would describe their withdrawal symptoms as severe.
A person may experience withdrawal symptoms due to chemical changes in the brain. The body adjusts to changes that an antidepressant such as Zoloft may cause. Stopping or reducing the antidepressant can throw the brain into a state of imbalance. This can have a physical and mental impact.
The likelihood of developing withdrawal symptoms may relate to the half-life of the antidepressant. The term half-life refers to the amount of time it takes for the body to metabolize 50% of a medication’s active ingredients and eliminate them from the body.
Typically, drugs with a shorter half-life may indicate more potential withdrawal problems. Sertraline has a relatively short half-life of approximately 24 hours and has a moderate risk of causing withdrawal symptoms.
Withdrawal symptoms may occur a few days after a person begins to taper their dose and may last for 1–3 weeks. The severity of symptoms will depend on how long a person has been taking sertraline.
Common symptoms associated with reducing sertraline dose may include:
- nausea
- sweating
- mood changes
- irritability
- dizziness
- brain zaps
- tremors
- anxiety
- confusion
- headache
- lethargy
- insomnia
- tinnitus
- seizures
Typically, antidepressants with shorter half-lives are more likely to cause withdrawal symptoms due to how quickly the body may eliminate them and cause changes in the level of serotonin in the brain.
This also means a person may experience symptoms quicker compared with an antidepressant with a longer half-life. Zoloft has a half-life of roughly 22–35 hours. This rate can vary due to numerous factors, such as the speed of a person’s metabolism.
While tapering Zoloft, people could experience discontinuation symptoms for up to 3 weeks. When stopping antidepressants, some symptoms may persist for up to 6 weeks and occasionally may continue for up to a year.
Always speak with a doctor about any new symptoms that occur when tapering off an antidepressant.
After a person decides they are ready to discontinue Zoloft, a doctor will usually suggest a tapering strategy to wean a person off Zoloft gradually before stopping completely.
The length of time a person has been taking Zoloft will usually determine the length of the tapering strategy. Typically, tapering lasts 4 weeks, but a doctor may suggest tapering the medication over 6–8 weeks to reduce the risk or severity of symptoms.
In other cases, a doctor may suggest switching to another antidepressant that may be easier to wean off or is less likely to cause potential withdrawal symptoms.
In addition to tapering, following self-care tips may also ease the process of weaning off Zoloft. This can include:
- telling family and friends about plans to come off antidepressants
- having a healthy diet
- getting adequate sleep
- getting regular exercise
A doctor may also recommend counseling or therapy if the underlying condition remains after stopping the medication. This may help a person to understand, manage, and overcome the underlying cause of their mood disorder.
Click here to learn more about how to stop antidepressants safely.
Antidepressants such as Zoloft typically include a black box warning as they may worsen symptoms of depression or suicidal ideation and cause unusual changes in behavior.
Caregivers and people taking antidepressants should watch for certain signs and symptoms and talk with a doctor if they occur.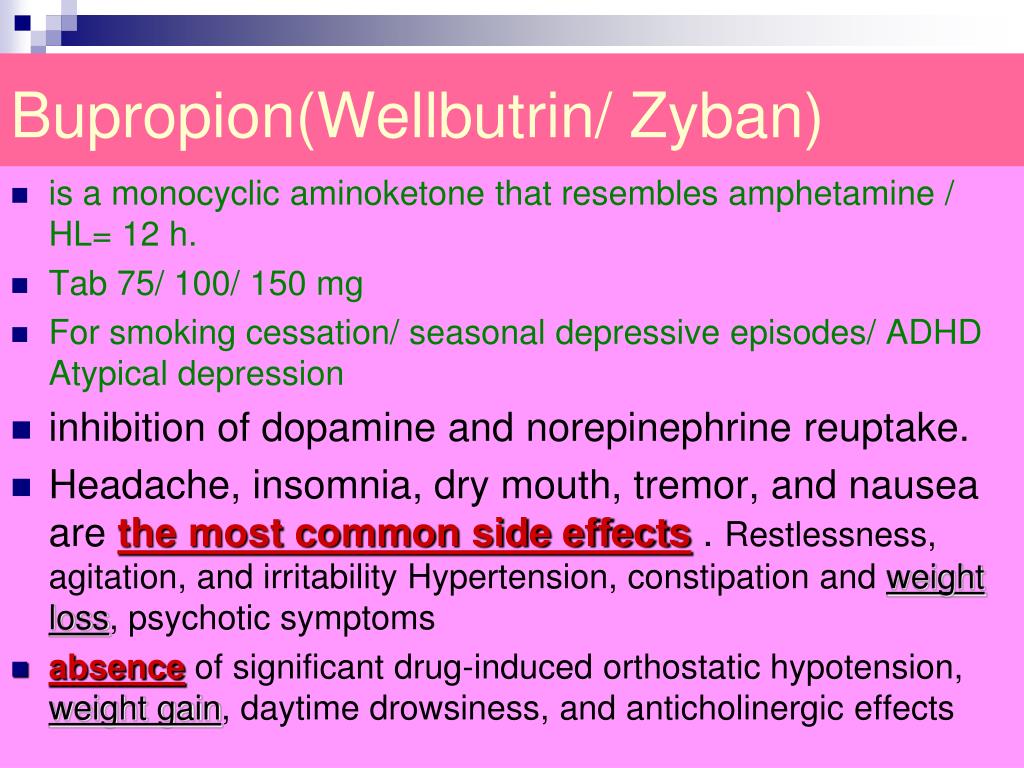 These may include:
These may include:
- anxiety
- restlessness
- irritability
- aggressiveness
- insomnia
Sertraline may also interact with other medications or supplements and increase the risk of having side effects. A person should talk with a doctor before taking sertraline if they are currently taking:
- medications that change their heartbeat
- other medications for depression
- St. John’s wort
Additionally, Zoloft may result in problems if a person:
- has heart problems
- has previously taken other antidepressants
- has glaucoma
- has epilepsy
- has diabetes
- is trying to become pregnant, is pregnant, or breastfeeding
It is not uncommon for people to mistake discontinuation symptoms for symptoms of relapse. This is particularly important to know about antidepressants as discontinuing an antidepressant can increase the risk of relapse for anxiety and depression.
Stopping antidepressants can result in rebound depression, or symptoms returning worse than before.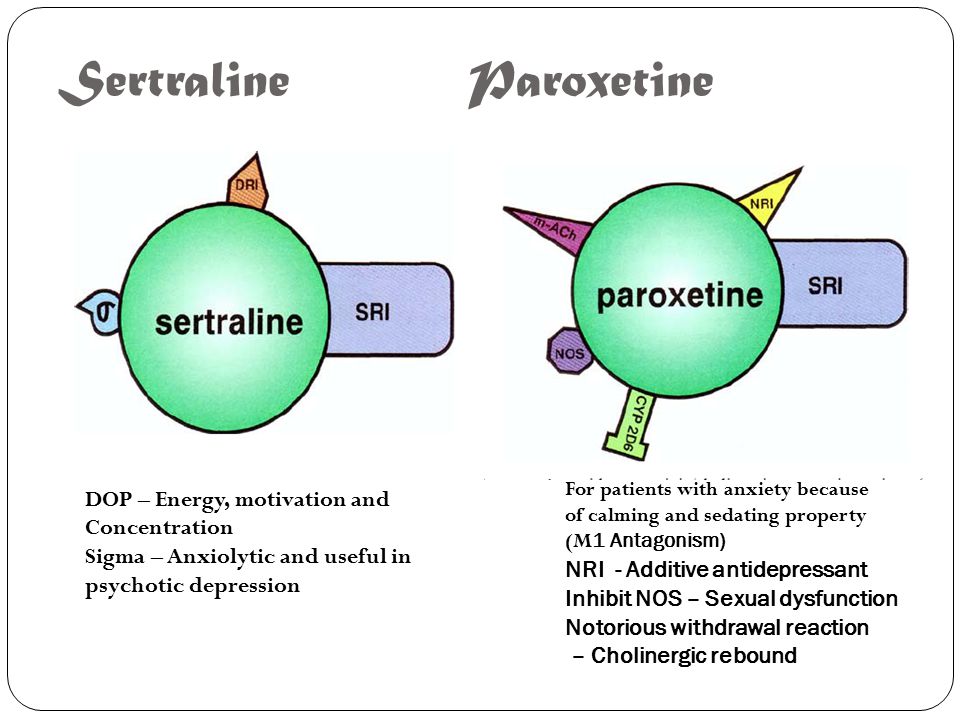 It is important for a doctor to closely monitor and determine the difference to help prevent relapse and treatment failure.
It is important for a doctor to closely monitor and determine the difference to help prevent relapse and treatment failure.
A person should always discuss coming off antidepressants or changing dosages with their doctor before making any changes to their dosage.
It is important to talk with a doctor immediately if withdrawal symptoms are severe, concerning, disabling, or last longer than a few weeks. Additionally, it is important to seek help if a person experiences suicidal thoughts, thoughts of self-harm, or any other unexpected or concerning symptoms.
A person should also seek help if they believe they are presenting symptoms of a relapse.
Sertraline, or Zoloft, is an SSRI antidepressant that doctors frequently prescribe. When a person decides to discontinue an antidepressant such as Zoloft, they should speak with their doctor and follow their advice on discontinuing, such as following a tapering schedule.
There is a moderate risk for people experiencing withdrawal symptoms while reducing their dose of Zoloft.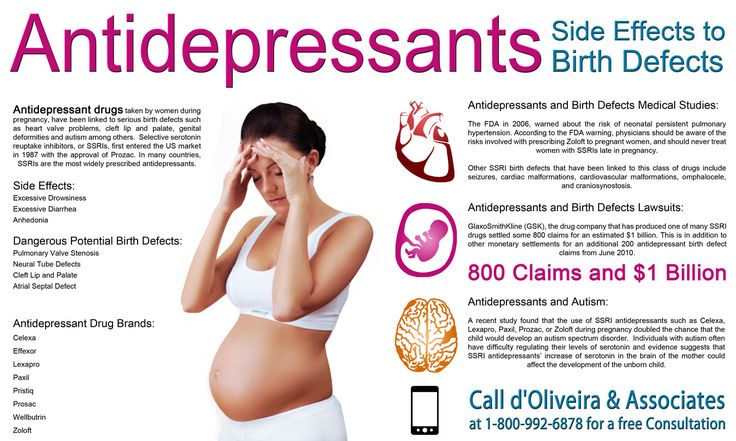 Common symptoms may include agitation, tremors, and headaches.
Common symptoms may include agitation, tremors, and headaches.
In addition to tapering their dose, people can also try self-care tips, such as exercising, getting regular sleep, and having a healthy diet, to reduce potential discontinuation symptoms further.
Zoloft withdrawal syndrome - Center for Healthy Youth
Zoloft - what is this drug? The active substance of the drug is sertraline. It belongs to the pharmacological group of antidepressants and is prescribed to patients with the following symptoms: depression, OCD, panic disorders, PTSD, social phobia. Zoloft is a powerful serotonin reuptake inhibitor in human brain cells.
More than 1/3 of people face the dangerous consequences of abrupt withdrawal of Zoloft. In narcology, this phenomenon is called withdrawal syndrome or withdrawal syndrome. The time of onset of symptoms of withdrawal syndrome when used is directly proportional to the half-life of the drug from the body. A drug such as Zoloft is addictive with systematic irregular use, therefore, there is also a Zoloft withdrawal syndrome, which usually occurs 3-5 days after the last use of the drug. The symptoms of Zoloft withdrawal syndrome are quite difficult to recognize, so people think that the disease has returned and start using the medicine again. nine0003
The symptoms of Zoloft withdrawal syndrome are quite difficult to recognize, so people think that the disease has returned and start using the medicine again. nine0003
-
Can't
persuade
to get treatment?
-
We will help you with motivation for treatment. As a rule, it is difficult for close people to persuade or force an addict to be treated. World experts have developed EFFECTIVE motivation schemes, using which you can lead the addict to the decision to seek help.
8 (800) 333-20-07
How to reduce the dose of Zoloft correctly?
The course of treatment with Zoloft usually lasts no more than 8 weeks (about two months). As with the use of other antidepressants, an unreasonable increase in the duration of its use leads to negative consequences for human health. However, even before the period prescribed by the doctor, it is not recommended to stop taking the drug, since the gradual disappearance of symptoms is not a reason to complete the course.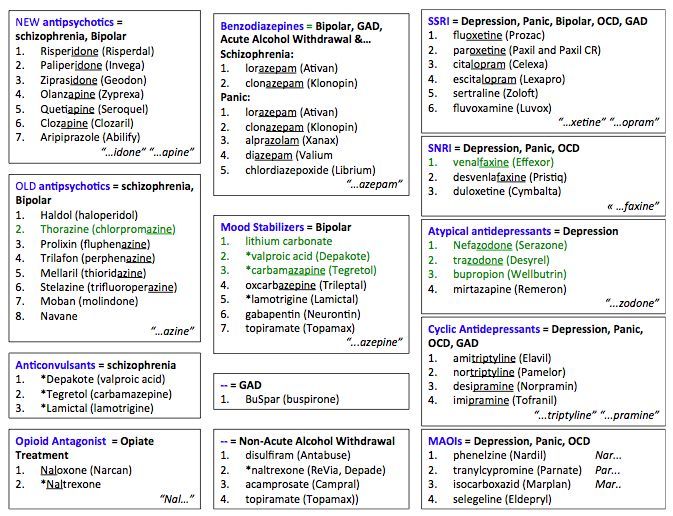 How long can I take Zoloft? nine0003
How long can I take Zoloft? nine0003
How much Zoloft can I take?
Many patients wonder how much Zoloft should be taken? Naturally, the duration of the course is strictly individual. So, how long can you take Zoloft? Only the attending physician, depending on the symptoms present, will be able to tell you how much Zoloft should be taken in your case. A specialist can prescribe a medication for 6-12 months, but this happens in exceptional cases.
The risk of developing withdrawal symptoms is increased in the following cases:
- abrupt drug withdrawal and removal from the body;
- regular intake over two months;
- excessive anxiety;
- Combination with antihypertensives, allergies, and antipsychotics.
Do you want to know the cost of services?
8 (800) 333-20-07 - call our specialist
How to cancel and stop drinking Zoloft?
Zoloft causes a withdrawal syndrome when it is stopped abruptly.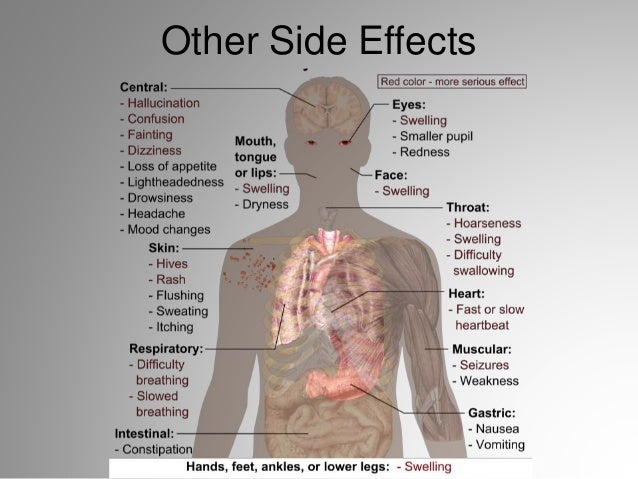 This drug affects the processes occurring in the human brain, so you should take the medicine only with a doctor's prescription. How to stop taking the drug and "get off" from Zoloft? To avoid the withdrawal syndrome, the dosage of the medication according to the medical plan is reduced by 25 mg every 14 days. If a stable remission is achieved after a course of treatment, the doctor will stop taking the drug. However, the specialist will cancel the drug if the patient experiences side effects, insomnia and headache from Zoloft are not uncommon. nine0003
This drug affects the processes occurring in the human brain, so you should take the medicine only with a doctor's prescription. How to stop taking the drug and "get off" from Zoloft? To avoid the withdrawal syndrome, the dosage of the medication according to the medical plan is reduced by 25 mg every 14 days. If a stable remission is achieved after a course of treatment, the doctor will stop taking the drug. However, the specialist will cancel the drug if the patient experiences side effects, insomnia and headache from Zoloft are not uncommon. nine0003
In which case the doctor can cancel the medication:
- the patient has a headache;
- causeless sadness, anxiety;
- feeling of devastation;
- nervousness, irritability;
- weakness;
- suicidal tendencies;
- sleep and appetite disorders;
- decrease in concentration.
If a person has lost their appetite or has regular headaches, the doctor begins a gradual process of reducing the dosage. The therapeutic dose is reduced over several weeks, and sometimes months. nine0003
The therapeutic dose is reduced over several weeks, and sometimes months. nine0003
Symptoms of withdrawal after taking
Is it possible to abruptly stop taking the medicine? Abrupt withdrawal of the drug threatens the occurrence of withdrawal or withdrawal. The human body, accustomed to a certain dose of the drug, will respond without an adaptation period. Most often, a deterioration in the patient's health is noted within 2-4 days after the last use. Depending on the individual characteristics and the state of the central nervous system, withdrawal symptoms may be different.
Symptoms and signs of withdrawal
- nervousness;
- irritability;
- irritability;
- insomnia;
- nausea, vomiting;
- headaches;
- incoordination, balancez.
In some cases, a person will not even feel dangerous signs, and sometimes you may need to call an ambulance for narcological help from the Center for Healthy Youth.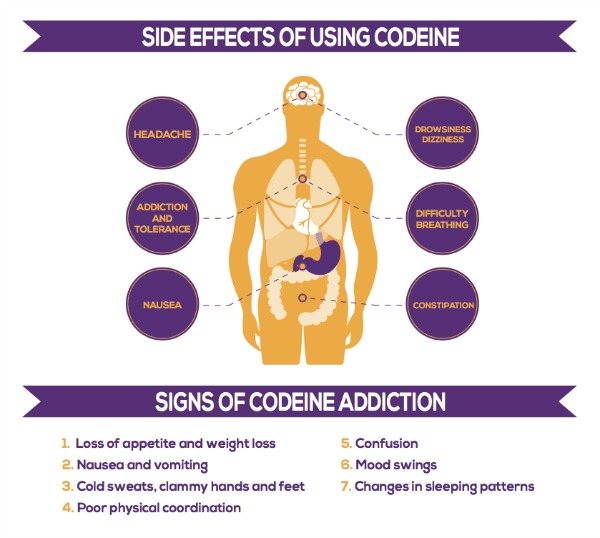 Therefore, if you feel a deterioration in the condition, it is worth contacting a doctor who will help reduce the dose and improve overall well-being. nine0003
Therefore, if you feel a deterioration in the condition, it is worth contacting a doctor who will help reduce the dose and improve overall well-being. nine0003
How long does Zoloft withdrawal last?
Withdrawal symptoms can persist without drug treatment for quite a long time, for several weeks. While taking antidepressants, the activity of neurons changes, so after stopping the drugs, the body needs time to rebuild and adapt to new conditions. The longer the course of treatment was, the longer the rehabilitation period will be. Withdrawal symptoms will not disappear until the active substance of the drug is excreted from the body. If general weakness lasts for a month, you should contact your doctor or specialists from the Healthy Youth Center. nine0003
When does Zoloft start to act and help?
It is important to understand that Zoloft does not begin to act immediately, but after a certain period of time. How long does Zoloft take to work? As a rule, the first positive dynamics begins to be noticeable to the patient only after 2-3 weeks of regular use.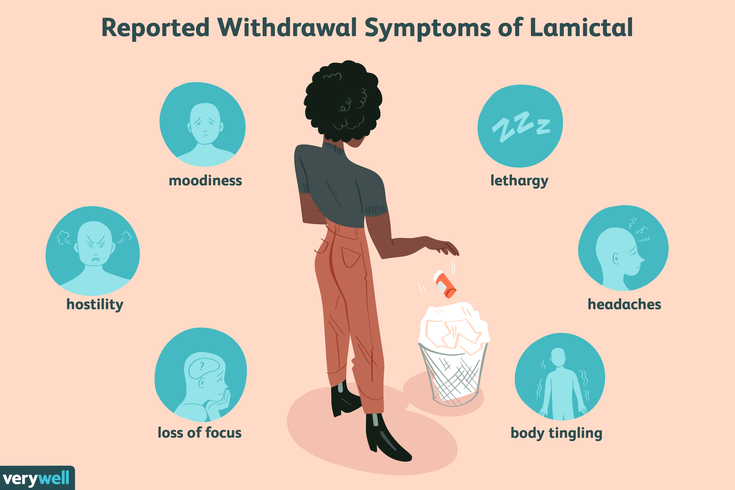 The maximum effect is noticeable after 2-3 months of admission.
The maximum effect is noticeable after 2-3 months of admission.
Discontinuation considerations
When choosing antidepressants, it is important to know which medications the patient has previously taken and which medications they are currently taking. Before prescribing an effective remedy that normalizes the work of the central nervous system, the doctor conducts a number of necessary examinations, identifies existing contraindications and prevents side effects. If Zoloft is not recommended for you, the specialist will offer you a wide range of analogues of this drug, including Cipralex, Prozac, Paxil, Cipramil and other equally effective drugs. The drug Velaksin, Amitriptyline, etc. has a similar effect. nine0003
If you experience withdrawal symptoms after taking Zoloft, contact the Healthy Youth Drug Treatment Center for help. We have been treating addictions for over 15 years.
Video about the treatment of drug addiction and alcoholism in the CCM
Antidepressant discontinuation syndrome: diagnosis, prevention and treatment
04/18/2017
nine0002UP TO ZMISTU NUMBER
Withdrawal symptoms may occur after discontinuation of any class of antidepressants.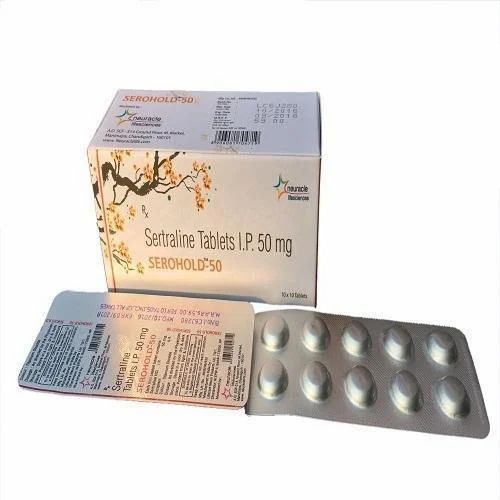 The largest number of publications is devoted to selective serotonin reuptake inhibitors (SSRIs), obviously due to the fact that drugs of this class are most often prescribed for the treatment of depressive disorders. Usually these symptoms are mild and disappear on their own after a while. However, some Patients may need to resume pharmacotherapy. This review briefly discusses the main clinical aspects of the antidepressant discontinuation syndrome.
The largest number of publications is devoted to selective serotonin reuptake inhibitors (SSRIs), obviously due to the fact that drugs of this class are most often prescribed for the treatment of depressive disorders. Usually these symptoms are mild and disappear on their own after a while. However, some Patients may need to resume pharmacotherapy. This review briefly discusses the main clinical aspects of the antidepressant discontinuation syndrome.
This condition is also called antidepressant withdrawal syndrome, although this is not entirely correct. The appearance of symptoms after stopping therapy does not mean that the drug is addictive. Antidepressants do not have addictive potential and do not cause addiction. This is an important positive point that should be communicated to patients, since most people will stop taking the prescribed treatment as soon as possible in case of fear of becoming dependent on the drug.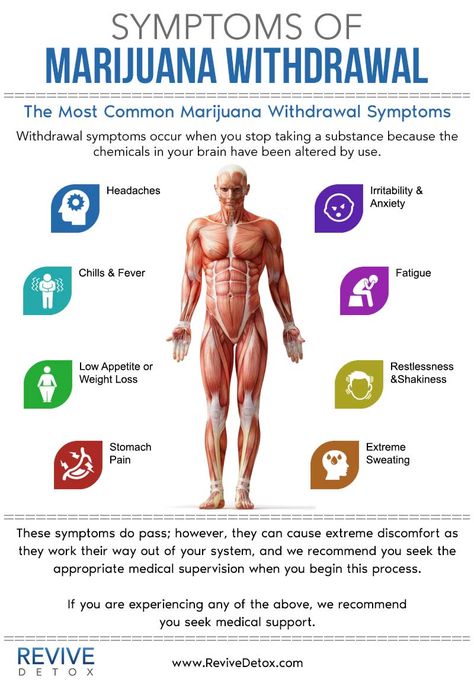 nine0003
nine0003
Why is it important to recognize antidepressant withdrawal syndrome?
There are three reasons: discomfort for the patient, diagnostic problem and possible compliance problems. Although withdrawal symptoms are rarely life-threatening, they are always associated with discomfort and some degree of psychosocial maladjustment. Hence the second problem: having experienced a withdrawal syndrome, the patient hardly agrees to any psychopharmacotherapy in the future. And finally, symptoms that occur in connection with the cessation of the action of an antidepressant can be mistaken for an exacerbation of a depressive disorder, another mental disorder, or a physical illness. nine0009 For example, consider two typical scenarios. Convinced of achieving remission of major depressive disorder, the doctor hurries to please the patient that the antidepressant can be stopped, but forgets to tell how to do it correctly. The patient takes everything literally and the next day forgets about the medicine.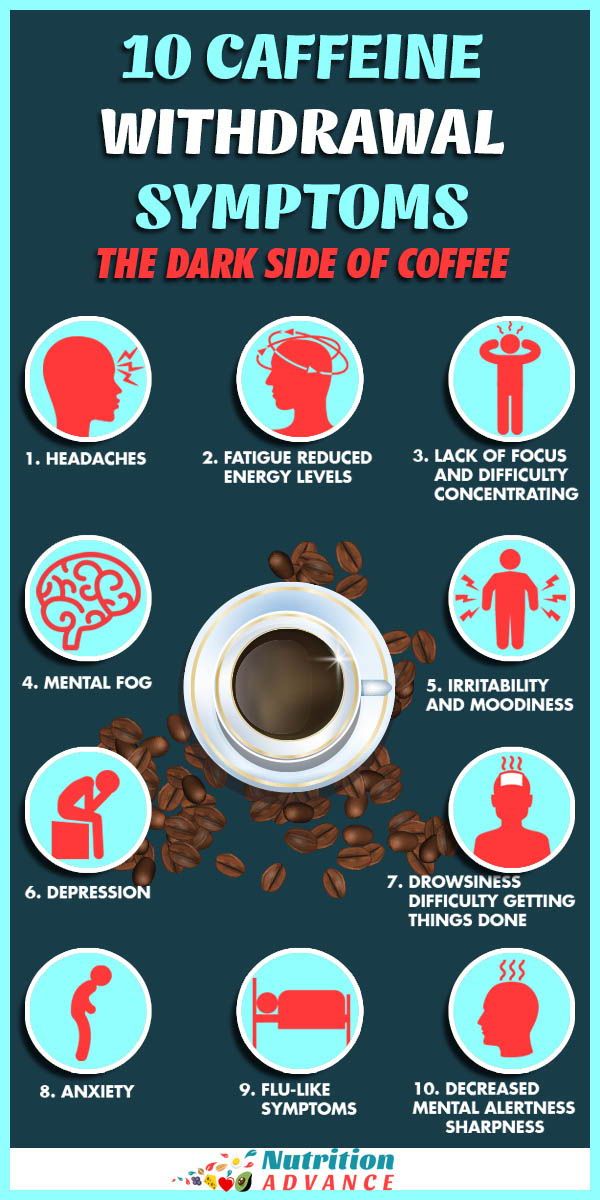 A week later, he develops withdrawal symptoms, and he addresses his complaints to a) the same psychiatrist who forgets to ask how the antidepressant was withdrawn and perceives the symptoms as a relapse of depression; b) to another specialist, for example, a neurologist, to whom he prefers not to report about treatment with a psychiatrist. And the neurologist interprets these non-specific symptoms according to his competence. As a result, unnecessary examinations and possibly even treatment. nine0009 In addition, symptoms can be confused with side effects of a newly prescribed drug after discontinuation of an antidepressant, especially when switching between antidepressants with different mechanisms of action, for example, from paroxetine (SSRI) to bupropion (a dopamine and norepinephrine reuptake inhibitor). This can lead to the erroneous conclusion that the patient does not tolerate the new drug well. Symptoms of discontinuation of therapy may also be perceived as failure of therapy, especially irritability and anxiety.
A week later, he develops withdrawal symptoms, and he addresses his complaints to a) the same psychiatrist who forgets to ask how the antidepressant was withdrawn and perceives the symptoms as a relapse of depression; b) to another specialist, for example, a neurologist, to whom he prefers not to report about treatment with a psychiatrist. And the neurologist interprets these non-specific symptoms according to his competence. As a result, unnecessary examinations and possibly even treatment. nine0009 In addition, symptoms can be confused with side effects of a newly prescribed drug after discontinuation of an antidepressant, especially when switching between antidepressants with different mechanisms of action, for example, from paroxetine (SSRI) to bupropion (a dopamine and norepinephrine reuptake inhibitor). This can lead to the erroneous conclusion that the patient does not tolerate the new drug well. Symptoms of discontinuation of therapy may also be perceived as failure of therapy, especially irritability and anxiety. nine0009 Symptoms of discontinuation of antidepressant therapy can be divided into six categories: sensory symptoms, balance disorders, general somatic, affective, gastrointestinal symptoms, and sleep disorders (Fig.).
nine0009 Symptoms of discontinuation of antidepressant therapy can be divided into six categories: sensory symptoms, balance disorders, general somatic, affective, gastrointestinal symptoms, and sleep disorders (Fig.).
At first, information about the listed manifestations was accumulated from reports of clinical cases. Then this problem was studied in prospective double-blind clinical trials in which patients were specifically randomized to the abolition of antidepressant therapy. nine0009 In English literature, a mnemonic device is used to memorize the spectrum of antidepressant withdrawal syndrome: the main symptoms are encrypted in the word FINISH.
F - from "flu-like" - flu-like symptoms;
I - insomnia;
N - from "nausea" - nausea;
I - from "imbalance" - imbalance;
S - sensory symptoms;
H - from "hyperarousal" - increased excitability, which reflects affective disorders.
It should be noted that the symptoms presented in the figure are mainly associated with discontinuation of SSRIs and serotonin and norepinephrine reuptake inhibitors.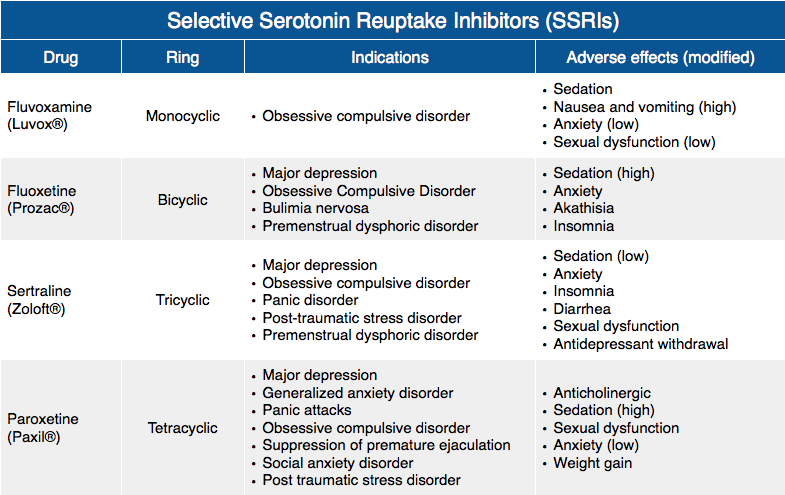 The spectrum of symptoms during withdrawal of monoamine oxidase inhibitors (MAOIs) and tricyclic antidepressants has its own specifics. Thus, in the event of discontinuation of tricyclic antidepressants, sensory symptoms and balance disorders, as a rule, are not observed. With the abolition of MAO inhibitors, symptoms may be more pronounced than after the abolition of SSRIs. Patients may experience a worsening of depressive and anxiety symptoms, an acute impairment of consciousness up to catatonia. nine0003
The spectrum of symptoms during withdrawal of monoamine oxidase inhibitors (MAOIs) and tricyclic antidepressants has its own specifics. Thus, in the event of discontinuation of tricyclic antidepressants, sensory symptoms and balance disorders, as a rule, are not observed. With the abolition of MAO inhibitors, symptoms may be more pronounced than after the abolition of SSRIs. Patients may experience a worsening of depressive and anxiety symptoms, an acute impairment of consciousness up to catatonia. nine0003
When do withdrawal symptoms appear and how long do they last?
They usually appear within the first week after stopping the antidepressant; according to studies, on average on the second day. Spontaneous resolution occurs at different times - from 1 day to 3 weeks, on average, patients continue to experience symptoms for 10 days.
What causes withdrawal syndrome?
The syndrome occurs when antidepressants of all classes are discontinued.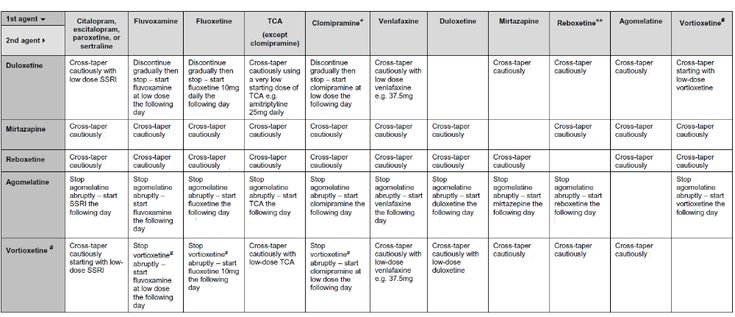 The largest number of reports was recorded for paroxetine. The half-life of the drug from blood plasma is the indicator that correlates more than others with the risk of developing a withdrawal syndrome. In other words, the shorter the residual effect of the drug after the last dose, the higher the likelihood of symptoms. nine0009 For example, fluoxetine has a half-life of 7 days, so this SSRI has the lowest risk of withdrawal. Paroxetine has an average half-life of 24 hours, hence the high risk of withdrawal syndrome, especially when the therapeutic dose is abruptly stopped.
The largest number of reports was recorded for paroxetine. The half-life of the drug from blood plasma is the indicator that correlates more than others with the risk of developing a withdrawal syndrome. In other words, the shorter the residual effect of the drug after the last dose, the higher the likelihood of symptoms. nine0009 For example, fluoxetine has a half-life of 7 days, so this SSRI has the lowest risk of withdrawal. Paroxetine has an average half-life of 24 hours, hence the high risk of withdrawal syndrome, especially when the therapeutic dose is abruptly stopped.
Can antidepressant discontinuation syndrome be distinguished from depression relapse?
Common symptoms include dysphoria, decreased appetite, sleep disturbances and fatigue. But there are also distinctive features—symptoms that are rarely seen in depression, such as sensory phenomena (paresthesias) as well as dizziness, headache, and nausea. In addition, in the case of withdrawal syndrome, a rapid (within 1 day) improvement can be observed when the drug is resumed, while recurrent depression does not respond so quickly to therapy.:max_bytes(150000):strip_icc()/prozac-withdrawal-symptoms-timeline-and-treatment-4766892_final_edit-ddf616fc766d4651afa6b5d804721eea.png) nine0003
nine0003
Who is at risk for developing antidepressant withdrawal syndrome?
Typically, these are patients who begin to feel better after a few weeks of taking an antidepressant and are not sufficiently informed about the need for long-term maintenance therapy. Women who find out they are pregnant during treatment may also abruptly stop taking the antidepressant for safety reasons.
How to stop antidepressants to minimize the risk of withdrawal? nine0014
Patients should be explained in an accessible form the features of the action of the prescribed antidepressant, the rules for increasing and gradually reducing the dose, and warn about a possible deterioration in well-being in the event of an abrupt cessation of therapy. But at the same time, the words "withdrawal syndrome", "addiction", "addiction" should be avoided, since they can be perceived negatively and cause early termination of therapy. Sooner or later, that happy moment comes when it becomes clear that antidepressants can be abandoned.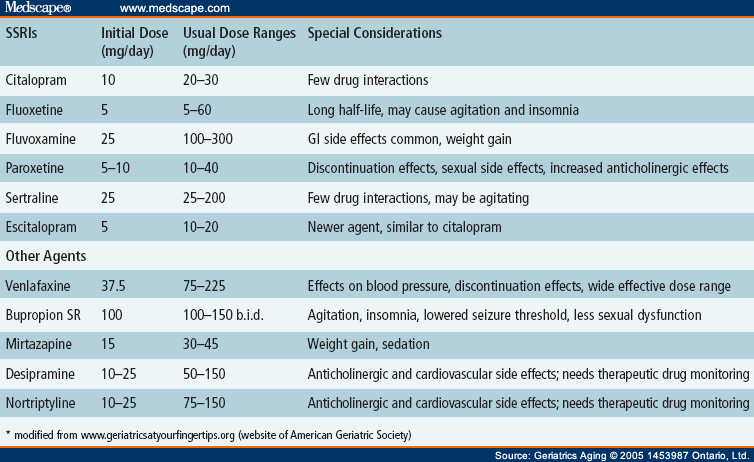 However, the withdrawal process, as a rule, takes several weeks, but in some cases even longer, especially if the patient's health worsens at the first steps of dose reduction. When prescribing fluoxetine, it is possible to cancel the drug without a gradual dose reduction, although it has not been specifically studied in studies. nine0009 If possible, you should also discuss with the patient's relatives the creation of the most favorable conditions for the period of antidepressant withdrawal. Patients with major depressive disorder, as a rule, do not work and are at home, therefore they are not subjected to external psycho-emotional stress. It is optimal if the patient's close environment tries to create a positive atmosphere and tries to involve a family member in some kind of activity in order to distract from the perception of possible withdrawal symptoms. nine0003
However, the withdrawal process, as a rule, takes several weeks, but in some cases even longer, especially if the patient's health worsens at the first steps of dose reduction. When prescribing fluoxetine, it is possible to cancel the drug without a gradual dose reduction, although it has not been specifically studied in studies. nine0009 If possible, you should also discuss with the patient's relatives the creation of the most favorable conditions for the period of antidepressant withdrawal. Patients with major depressive disorder, as a rule, do not work and are at home, therefore they are not subjected to external psycho-emotional stress. It is optimal if the patient's close environment tries to create a positive atmosphere and tries to involve a family member in some kind of activity in order to distract from the perception of possible withdrawal symptoms. nine0003
How to help patients who complain of feeling worse after stopping antidepressants?
If this does happen, explain to the patient that the symptoms are not life-threatening and usually resolve within a few days. If the patient continues to experience symptoms and they reduce quality of life, it is common practice to restart the therapeutic dose of the antidepressant. In the future, you can again try to stop the drug through a very gradual dose reduction. If this does not help, then it is possible to transfer the patient to fluoxetine-SSRI with the lowest risk of withdrawal syndrome, and then cancel it. nine0003
If the patient continues to experience symptoms and they reduce quality of life, it is common practice to restart the therapeutic dose of the antidepressant. In the future, you can again try to stop the drug through a very gradual dose reduction. If this does not help, then it is possible to transfer the patient to fluoxetine-SSRI with the lowest risk of withdrawal syndrome, and then cancel it. nine0003
Literature
1. Haddad P.M., AndersonI.M. (2007). Recognizing and managing antidepressant discontinuation symptoms. Advances in Psychiatric treatment, 13(6): 447-457.
2. Warner C.H., Bobo W., Warner C., Reid S., Rachal J. (2006). Antidepressant discontinuation syndrome. American Family Physician, 74(3): 449-456.
3. Renoir T. (2013). Selective serotonin reuptake inhibitor antidepressant treatment discontinuation syndrome: a review of the clinical evidence and the possible mechanisms involved. Frontiers in Pharmacology, 4.
Prepared by Dmitry Molchanov
- Number:
- Thematic issue "Neurology, Psychiatry, Psychotherapy" No.
 1 (40), March 2017
1 (40), March 2017
12/22/2022 Psychiatry Exchange of alcohol as a strategy for preventing psychosomatic disorder
16.12.2022 PsychiatryStress-induced depression and schizophrenia due to symptoms of depression: why is prevention of dementia necessary?
In the science-practical conference “neurology, psychiatrics, such narcologist at the Council of Svitі: global Vikliki that was the rosvita”, yakuuuuly 6-8 zhovnika 2022 Rock in the online rod.