New treatments for ocd
International OCD Foundation | Towards New Medications for Refractory OCD
by Christopher Pittenger, MD, PhD, & Wayne Goodman, MD
This article was initially published in the Summer 2013 edition of the OCD Newsletter.
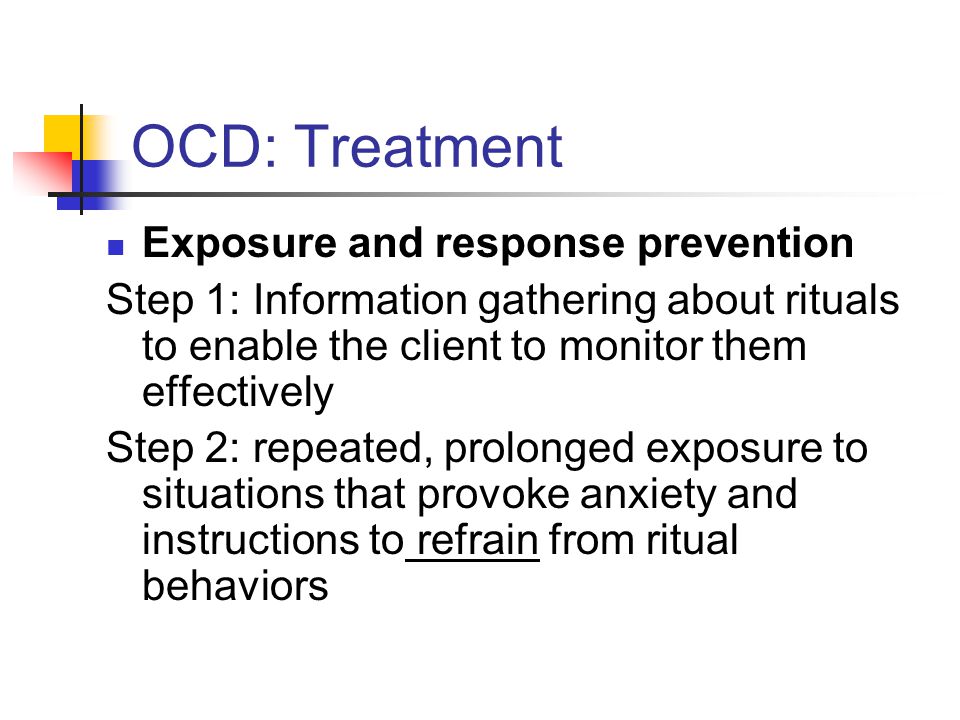
Current psychotherapy and medication treatments for OCD can be of help to many who suffer from the disorder. Unfortunately, as many as a quarter of patients do not experience much benefit from these standard treatments, such as selective serotonin reuptake inhibitors (SSRIs) or Exposure and Response Prevention (ERP), even when they are used well. The development of new treatment options for these individuals is an urgent clinical and research need. This article looks at up-and-coming research on medications that affect the brain’s glutamate system as a strategy for treating refractory OCD (also known as “treatment-resistant” OCD).
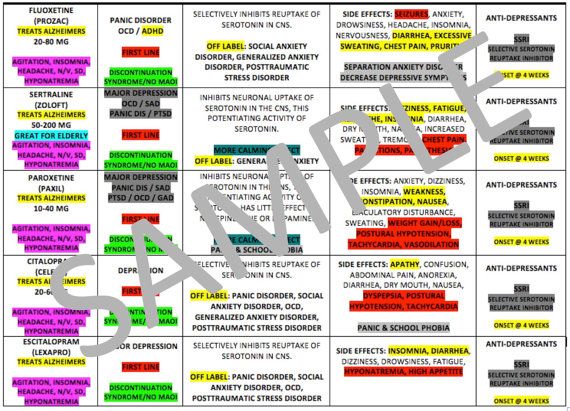
The SSRI antidepressants — fluoxetine (Prozac), fluvoxamine (Luvox), sertraline (Zoloft), paroxetine (Paxil), citalopram (Celexa), and escitalopram (Lexapro) — are the standard “first line” medications used for OCD pharmacotherapy. (The first four of these have been approved by the FDA for the treatment of OCD; the last two have not, but research shows them to be just as effective, and they are often prescribed ‘off label’.) Many patients find that their OCD symptoms get a lot better within 8–12 weeks of taking one of these medications. [For more information about these medications, please visit the IOCDF website page on medication here.] However, some patients do not respond to or tolerate the first medication they are prescribed, and thus may be prescribed a different SSRI or the older antidepressant clomipramine. If this fails, a “second-line” medication may be recommended, such as a low dose “antipsychotic” medication like risperidone.
These first- and second-line medications target the neurotransmitters serotonin and dopamine, and they provide some benefit in a majority of OCD cases. Unfortunately, many patients — up to 30–40% — do not get much benefit. And many of those who are considered ‘responders’ still have significant symptoms, or have difficulty with side effects, especially with the second-line medications.
Because of the clear need to develop treatment options for the many people who do not benefit much from these standard treatments, there has been great interest recently in the use of medications that target other neurotransmitter systems in the brain. In particular, there has been a lot of interest in the neurotransmitter glutamate, an important part of the central nervous system [1]. If glutamate imbalance contributes to OCD, then medications that target the glutamate neurotransmitter system in a variety of ways may hold promise for individuals with otherwise treatment-resistant OCD. This is a major focus of current research, both in academic settings and in the pharmaceutical industry.
Several lines of evidence suggest that changes in glutamate contribute to OCD, in at least some cases. First, genetic abnormalities in a brain protein responsible for maintaining normal glutamate levels have been associated with OCD in numerous studies. While this association has not been proven beyond a doubt and is likely to explain only a minority of OCD cases, it is still the most repeated, and therefore most accepted, genetic finding in OCD to date [2]. Second, examination of cerebrospinal fluid from individuals with OCD has revealed increased levels of glutamate in some of them [3, 4]. Third, some studies using magnetic resonance spectroscopy (MRS), a brain imaging method that makes it possible to measure certain molecules in the brain, have shown changes in normal glutamate levels, with the nature of the change depending on the brain region studied [5]. Less direct evidence for glutamate changes come from findings in animal studies, changes in brain electrical response that are similar to an altered glutamate state, and more [1].
Second, examination of cerebrospinal fluid from individuals with OCD has revealed increased levels of glutamate in some of them [3, 4]. Third, some studies using magnetic resonance spectroscopy (MRS), a brain imaging method that makes it possible to measure certain molecules in the brain, have shown changes in normal glutamate levels, with the nature of the change depending on the brain region studied [5]. Less direct evidence for glutamate changes come from findings in animal studies, changes in brain electrical response that are similar to an altered glutamate state, and more [1].
The theory that glutamate imbalance contributes to OCD has led to studies of a number of drugs and over-the-counter (OTC) supplements that are already widely available, either with or without a prescription. Small studies, most of which have not had a placebo control group, have provided interesting preliminary evidence of benefit from riluzole, memantine, N-acetylcysteine, and topiramate, all of which have an effect on glutamate [1]. In none of these cases is the data strong enough for any of these drugs to be considered part of standard treatment; certainly they are not appropriate in place of a trial of one of the better-proven SSRIs. But in individuals who do not respond to first- and second-line treatments, these other medications are becoming reasonable options. For more information about over-the-counter alternative treatments, please see the article “Title TK” on page TK of this newsletter.
In none of these cases is the data strong enough for any of these drugs to be considered part of standard treatment; certainly they are not appropriate in place of a trial of one of the better-proven SSRIs. But in individuals who do not respond to first- and second-line treatments, these other medications are becoming reasonable options. For more information about over-the-counter alternative treatments, please see the article “Title TK” on page TK of this newsletter.
The way glutamate works in the brain is by attaching to several different receptor proteins, which are essentially the “On/Off” switches for neurons. Thus, glutamate affects electrical communication (or “signaling”) in the brain. One specific receptor, the NMDA receptor, has become a major focus of attention in OCD and other neuropsychiatric conditions, including major depressive disorder. The NMDA receptor is the target of the drug memantine, which is being used by some psychiatrists in refractory cases of OCD. It is also the target of the drug ketamine, which has been shown in recent studies to have a remarkable, rapid antidepressant effect [6]. The effect of ketamine in refractory OCD remains unclear, with one study suggesting that it is not effective (though it can benefit depression in patients who suffer from both conditions), and a more recent one suggesting that it is [7, 8]. This is an interesting and important area of ongoing work.
It is also the target of the drug ketamine, which has been shown in recent studies to have a remarkable, rapid antidepressant effect [6]. The effect of ketamine in refractory OCD remains unclear, with one study suggesting that it is not effective (though it can benefit depression in patients who suffer from both conditions), and a more recent one suggesting that it is [7, 8]. This is an interesting and important area of ongoing work.
There are other, more indirect ways to affect the NMDA receptor, which is a receptor for both glutamate and the related small molecule glycine. Changing brain levels of glycine indirectly adjusts the effects of glutamate; this is an exciting area of recent focus in OCD research. A placebo-controlled trial of glycine itself suggested that it can be of benefit in treatment-resistant OCD. Unfortunately, the very large doses of glycine needed in order to have an effect in the brain resulted in unpleasant side effects, especially nausea [9].
The indirect effect of glycine using sarcosine, which is an amino acid that comes from glycine and is available over the counter, showed some evidence of benefit in an uncontrolled trial [10]. Sarcosine works in the brain by blocking the reuptake of glycine, much as SSRI antidepressants block the reuptake of serotonin, and therefore increasing its levels without the problems associated with taking large amounts of glycine itself. This has led to the idea that a more powerful and specific blocker of glycine reuptake may represent a new frontier in OCD treatment. Such drugs are not yet approved by the FDA or widely available by prescription, but they have been developed by several different pharmaceutical companies for a variety of uses.
Sarcosine works in the brain by blocking the reuptake of glycine, much as SSRI antidepressants block the reuptake of serotonin, and therefore increasing its levels without the problems associated with taking large amounts of glycine itself. This has led to the idea that a more powerful and specific blocker of glycine reuptake may represent a new frontier in OCD treatment. Such drugs are not yet approved by the FDA or widely available by prescription, but they have been developed by several different pharmaceutical companies for a variety of uses.
An investigation of one of these drugs for individuals with refractory OCD, sponsored by the pharmaceutical company F. Hoffman La Roche, Ltd., is currently underway at research sites across the country. The drug, called bitopertin, was originally developed as a new treatment for schizophrenia, especially for “negative symptoms” (when a person is lacking a typical emotional response or thought process) such as reduced motivation [11]; it is completely distinct from traditional antipsychotics like risperidone and haloperidol. While bitopertin is not yet clinically available, it has been used in hundreds of people in earlier studies. This trial is important for the field of OCD research for two reasons. First, it should provide us with important information about a completely new type of medication that may be of benefit to refractory patients. Second, it is the first time since the 1980s that a major trial of a new medication for OCD has been undertaken by the pharmaceutical industry. Collaborations of this sort are very important for turning our growing understanding of the neurobiology underlying OCD symptoms into innovative new treatments.
While bitopertin is not yet clinically available, it has been used in hundreds of people in earlier studies. This trial is important for the field of OCD research for two reasons. First, it should provide us with important information about a completely new type of medication that may be of benefit to refractory patients. Second, it is the first time since the 1980s that a major trial of a new medication for OCD has been undertaken by the pharmaceutical industry. Collaborations of this sort are very important for turning our growing understanding of the neurobiology underlying OCD symptoms into innovative new treatments.
This trial, which goes by the name of Skylyte, is currently looking for individuals with OCD symptoms that have not responded to SSRI treatment to participate.
The needs of OCD sufferers whose symptoms are refractory to the best psychotherapy and pharmacotherapy that we have to offer are great. However, we are in an exciting time for OCD research, and new hope may be on the horizon. The idea that chemicals that have an effect on glutamate can benefit some patients has driven a great deal of research in recent years [1]. And a major treatment trial of a new medication, Skylyte, may indicate new interest by the pharmaceutical industry in the development of new treatment strategies — an interest that has been unfortunately lacking for many years. We are hopeful that these research efforts will lead to new hope in the coming years.
The idea that chemicals that have an effect on glutamate can benefit some patients has driven a great deal of research in recent years [1]. And a major treatment trial of a new medication, Skylyte, may indicate new interest by the pharmaceutical industry in the development of new treatment strategies — an interest that has been unfortunately lacking for many years. We are hopeful that these research efforts will lead to new hope in the coming years.
Acknowledgements & Disclosures: CP is Associate Professor of Psychiatry, Psychology, and in the Child Study Center and Director of the OCD Research Clinic at Yale University in New Haven, Connecticut. His work is funded by the NIMH, the Doris Duke Charitable Foundation, and the State of Connecticut through its support of the Ribicoff Research Facilities at the Connecticut Mental Health Center. WG is Chair of Psychiatry at the Mount Sinai School of Medicine in New York City and is co-founder of the IOCDF.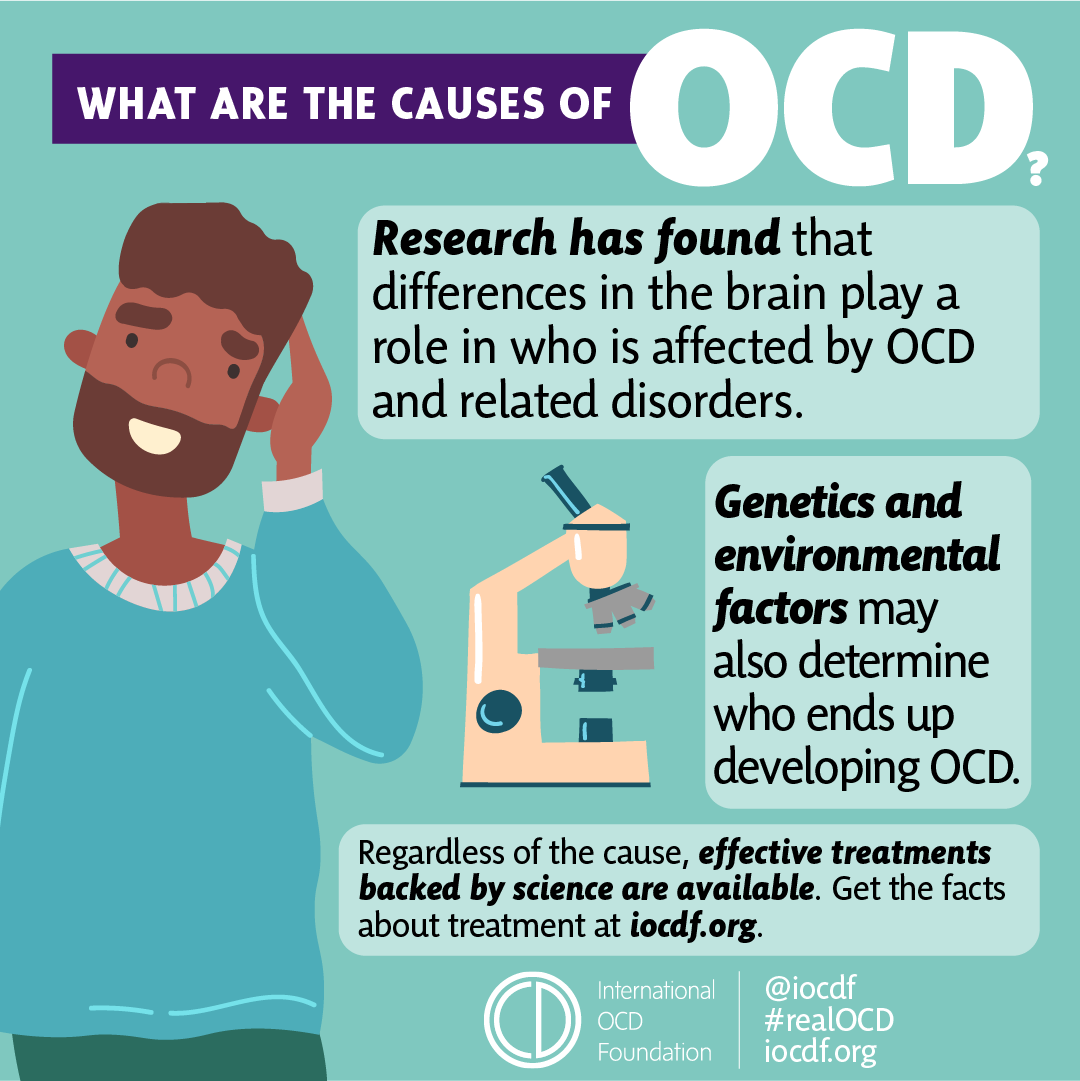 His work is funded by National Institute of Mental Health. Both authors are recruiting patients for the SkyLyte study, funded by F. Hoffman La Roche, Ltd., at their research sites, and have received compensation (< $5000) from Roche for consultative input during the design phases of this trial.
His work is funded by National Institute of Mental Health. Both authors are recruiting patients for the SkyLyte study, funded by F. Hoffman La Roche, Ltd., at their research sites, and have received compensation (< $5000) from Roche for consultative input during the design phases of this trial.
References
- Pittenger, C., Bloch, M.H., & Williams, K. (2011) Glutamate abnormalities in obsessive compulsive disorder: neurobiology, pathophysiology, and treatment. Pharmacol Ther, 132(3), 314–32.
- Stewart, S.E., et al. (2013). Meta-analysis of association between obsessive-compulsive disorder and the 3′ region of neuronal glutamate transporter gene SLC1A1. Am J Med Genet B Neuropsychiatr Genet, 162B(4), 367–79.
- Bhattacharyya, S., et al. (2009). Anti-brain autoantibodies and altered excitatory neurotransmitters in obsessive-compulsive disorder. Neuropsychopharmacology, 34(12), 2489–96.
- Chakrabarty, K., et al.
 (2005). Glutamatergic dysfunction in OCD. Neuropsychopharmacology, 30(9), 1735–40.
(2005). Glutamatergic dysfunction in OCD. Neuropsychopharmacology, 30(9), 1735–40. - Brennan, B.P., et al. (2013). A critical review of magnetic resonance spectroscopy studies of obsessive-compulsive disorder. Biol Psychiatry, 73(1), 24–31.
- Aan Het Rot, M., et al. (2012). Ketamine for depression: where do we go from here? Biol Psychiatry, 72(7), 537–47.
- Bloch, M.H., et al., (2012). Effects of ketamine in treatment-refractory obsessive-compulsive disorder. Biol Psychiatry, 72(11), 964–70.
- Rodriguez, C.I., et al. (2013). Randomized Controlled Crossover Trial of Ketamine in Obsessive-Compulsive Disorder: Proof-of-Concept. Neuropsychopharmacology, ???
- Greenberg, W.M., et al. (2009). Adjunctive glycine in the treatment of obsessive-compulsive disorder in adults. J Psychiatr Res, 43(6), 664–70.
- Wu, P.L., et al. (2011). Sarcosine therapy for obsessive compulsive disorder: a prospective, open-label study.
 J Clin Psychopharmacol, 31(3), 369–74.
J Clin Psychopharmacol, 31(3), 369–74. - Javitt, D.C. (2012). Glycine transport inhibitors in the treatment of schizophrenia. Handb Exp Pharmacol, (213), 367–99.
The New Breakthroughs in OCD Treatment
Certain recent developments in the field of mental health are being closely examined as possible breakthroughs in OCD treatment. Read on to find out more about these cutting-edge advancements.
OCD: Basic Facts and Figures
Obsessive-compulsive disorder (or OCD) is a mental health disorder mainly composed of obsessive thought content and compulsive reactions to them. The more common OCD obsessions are cleanliness and contamination, taboo thoughts and images, catastrophizing (concern over a tragic event befalling the individual or a loved one), and counting and organization. OCD compulsions are much more diverse, holding virtually endless options: it includes variations on checking and rechecking if the lights have been turned off, repeatedly washing one’s hands, tapping the top of the table a set number of times, and more.
Both OCD-related obsessions and OCD-related compulsions enhance one another, causing the severity of the condition to increase. This results in a great deal of stress for the individual experiencing it, who begins to contend with unpleasant, intrusive, and unwanted thoughts throughout the day, in addition to ritualistic and often illogical reactions they feel compelled to carry out. This condition often has detrimental effects on one’s well-being, compromising their social functioning, professional work, academic achievements, and other major aspects of their lives.
2.3% of US adults, as well as 1%-2.3% of US children and adolescents, are diagnosed with OCD. While this condition can develop at any age, symptoms commonly first appear between ten years old and early adulthood. Due to the elusiveness of its symptoms, patients are usually only diagnosed (and only begin to receive treatment) from the ages of 14-17, after previously having their symptoms chalked up to mere eccentricity.
Roughly one third of patients with OCD do not respond to first-line treatments, such as cognitive behavioral therapy (CBT) or selective serotonin reuptake inhibitor medication (SSRIs). The relatively low remission rate has pushed scientists to explore potential alternatives to the more common routes of OCD treatment.
Antibodies to Ward Off Obsession
Recent research has shown that patients with OCD have six times the amount of a protein called Immuno-moodulin, or Imood, compared to individuals who do not contend with OCD. In addition to OCD, Imood was also found to increase symptoms of anxiety and stress, both mental health areas that have already been linked to OCD.
The innovation behind Imood blocking is centered on its potential ability to influence neural activity through a genetic pathway: specifically, it is believed it may be able to influence genes associated with the appearance of OCD symptoms. Indeed, when an antibody to Imood was introduced within a laboratory setting, anxiety levels decreased, leading researchers to pursue similar studies based on the closely related OCD.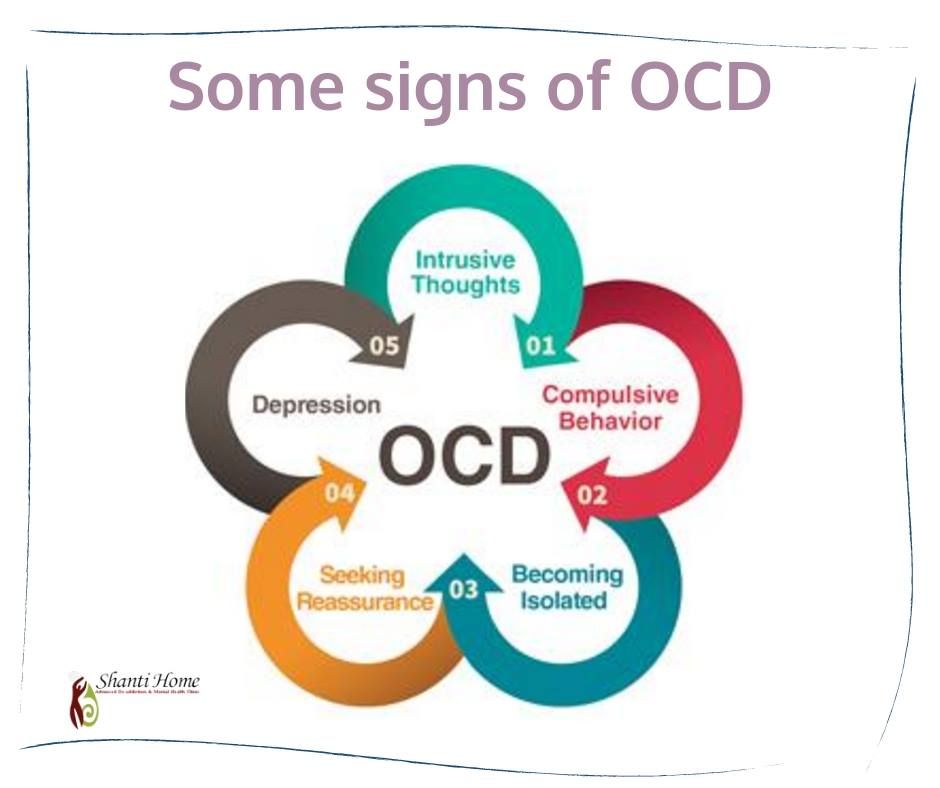
Artificial Intelligence Pinpointing Molecular Efficacy
Artificial intelligence (AI) has been making great strides in the field of depression treatment, and is also showing promising results when it comes to OCD. By relying on algorithmic calculations, AI technology is now allowing researchers to reach empirical conclusions faster and more accurately, thereby increasing the efficacy of manufactured medications.
OCD-focused AI studies have set their sights on discovering which particular protein (or proteins) are involved in the appearance of the condition’s adverse symptoms, and which molecular medication can regulate it. So far, a cell surface protein called 5-HTIA has been implicated: normally, 5-HTIA is activated by the neurotransmitter serotonin, which has already been found to be related to the appearance of this condition. By calculating which molecular drug this protein will respond to, AI research is attempting to effectively decrease OCD severity, even in cases where serotonin activation is below the normal rate.
Glutamate-Focused Medication
While serotonin is still considered the central neurotransmitter involved in the occurrence of OCD, other chemical compounds are being investigated for their role in this condition, particularly the neurotransmitter glutamate. With such a high resistance rate to serotonin-focused SSRI medications, many researchers believe that serotonin alone cannot be called upon to successfully alleviate OCD symptoms. This is why they have turned to additional neurotransmitters, in an effort to better understand the neural pathways involved in this condition. Enter glutamate, the main excitatory neurotransmitter in the brain. Current research suggests that glutamate regulation plays a crucial part in facilitating higher levels of serotonin, thereby enabling a decrease of OCD symptoms.
A newly developed drug called truriluze is believed to be able to regulate glutamate, acting as a modulating agent for the neurotransmitter. Through glutamate’s eventual effect on serotonin, this indirect route to OCD relief is considered a promising step toward more widespread symptom alleviation.
Optogenetics for Accurate Neural Manipulation
The emerging field of optogenetics allows scientists to project light as a way to locate and control the activation of genetically modified neurons. This, in turn, is presently being incorporated into studies on an OCD-related phenomenon—the startle reflex.
The startle reflex is a sudden and unpleasant cognitive overload that occurs due to an alarming and unexpected stimulus. Jumping in one’s seat while watching a scary movie, when they spot the killer about to attack someone, is an example of the startle reflex. Like patients battling anxiety, those contending with OCD were also found to have an overly alert startle reflex.
Optogenetics is providing researchers with the opportunity to examine sensorimotor gating: optogenetic technology is currently able to identify which neural circuits are involved with startle inhibition, which prevent the brain from creating the cognitive overload associated with OCD and anxiety. Scientists focused on sensorimotor gating are hoping to progress their research to eventually reach the ability to not only locate the relevant circuits that prevent OCD symptoms, but also to regulate their activity, thereby inducing such oversight.
Scientists focused on sensorimotor gating are hoping to progress their research to eventually reach the ability to not only locate the relevant circuits that prevent OCD symptoms, but also to regulate their activity, thereby inducing such oversight.
You may also be interested in...
Modern methods of treatment of obsessive compulsive disorder (obsessive-compulsive disorder)
Obsessive-compulsive disorder (obsessive-compulsive disorder) is a disease characterized by obsessive fears and periodically arising ritual stereotyped actions that interfere with the normal course of the patient's life. Obsessions are persistent unwanted ideas, fears, thoughts, images or urges accompanied by muscle tension. Compulsions - syndrome, which is a recurrent obsessive behavior; actions that a person feels compelled to perform. There are simple compulsions (nervous tics, twitching, repeated touching of an object) and complex ones. Complex compulsions, also called “rituals” in psychiatry, are varied and may include the following stereotyped actions: excessive cleansing (washing hands), repetition (repeated repetition of one’s actions: rewriting, rereading, switching on and off), overeating. Compulsive behavior is designed to reduce the level of anxiety caused by obsessive disorder. The patient cannot get rid of obsessive actions and states on his own. They are closely related to the emotional sphere, accompanied by depressive reactions, anxiety. Being symptomatic, according to S.L. Sukhanov [1912], "parasitic", they do not affect the course of intellectual activity in general, although they worsen the efficiency and productivity of the patient's mental activity. Throughout the course of the disease, a critical attitude is maintained towards obsessions. Obsessive states are observed mainly in individuals with a psychasthenic character. Obsessions and compulsions often occur within neurosis-like states in sluggish schizophrenia, endogenous depressions, epilepsy, and the consequences of traumatic brain injury.
Complex compulsions, also called “rituals” in psychiatry, are varied and may include the following stereotyped actions: excessive cleansing (washing hands), repetition (repeated repetition of one’s actions: rewriting, rereading, switching on and off), overeating. Compulsive behavior is designed to reduce the level of anxiety caused by obsessive disorder. The patient cannot get rid of obsessive actions and states on his own. They are closely related to the emotional sphere, accompanied by depressive reactions, anxiety. Being symptomatic, according to S.L. Sukhanov [1912], "parasitic", they do not affect the course of intellectual activity in general, although they worsen the efficiency and productivity of the patient's mental activity. Throughout the course of the disease, a critical attitude is maintained towards obsessions. Obsessive states are observed mainly in individuals with a psychasthenic character. Obsessions and compulsions often occur within neurosis-like states in sluggish schizophrenia, endogenous depressions, epilepsy, and the consequences of traumatic brain injury. Currently, obsessive-compulsive disorders are united in the International Classification of Diseases under the concept of "obsessive-compulsive disorder" (OCD).
Currently, obsessive-compulsive disorders are united in the International Classification of Diseases under the concept of "obsessive-compulsive disorder" (OCD).
The prevalence of OCD in the general population is quite high from 1.5% to 3% (Rasmussen S.A., Eisen J.L., 2007). At the same time, those suffering from obsessive-compulsive disorder make up 1% of all patients receiving treatment in psychiatric institutions. Men and women are affected approximately equally (A. M. Svyadoshch. 1997). Obsessive-compulsive disorder most often begins between the ages of 10 and 30. In this case, the first visit to a psychiatrist usually occurs only between 25 and 35 years. Patients with OCD are most often people with a high level of intelligence, according to various sources, among such patients, the frequency of high IQ is from 12% to 28.53% (Ravizza L., Maina G., 1997).
The cause of OCD is still debatable. Currently, the theory of neurotransmitter disorders is gaining more and more popularity. Pharmacological intervention specifically targeting serotonergic neurotransmission has revolutionized the prospects for recovery for millions of OCD patients worldwide. Today, it is generally accepted that intense serotonin reuptake inhibition (SSRI) is the key to effective treatment of OCD (Rasmussen S.A., Eisen J.L., 2007). For a diagnosis of obsessive-compulsive disorder, obsessions and/or compulsions must occur on more than 50% of days for two consecutive weeks, and they must also be a source of distress and impaired activity.
Pharmacological intervention specifically targeting serotonergic neurotransmission has revolutionized the prospects for recovery for millions of OCD patients worldwide. Today, it is generally accepted that intense serotonin reuptake inhibition (SSRI) is the key to effective treatment of OCD (Rasmussen S.A., Eisen J.L., 2007). For a diagnosis of obsessive-compulsive disorder, obsessions and/or compulsions must occur on more than 50% of days for two consecutive weeks, and they must also be a source of distress and impaired activity.
Obsessive symptoms have the following characteristics:
a) They are regarded as the patient's own thoughts or impulses.
b) There must be at least one thought or action that the patient unsuccessfully resists, even if there are other thoughts and/or actions that the patient no longer resists.
c) The thought of performing a compulsive action should not in itself be pleasurable (simply reducing tension or anxiety is not considered pleasurable in this sense).
d) Thoughts, images or impulses must be unpleasantly repetitive.
Standard treatment for OCD involves a combination of psychotherapy and rational pharmacotherapy. The psychotherapeutic impact is based on a cognitive-behavioral technique, the purpose of which is the patient's awareness and understanding of the disease and step-by-step resistance to its symptoms (Wilson D.T., 2007). In pharmacotherapy, antidepressants from the group of selective serotonin reuptake inhibitors have proven themselves well.
In recent years, the xenon therapy method has been actively introduced into the practice of treating OCD. It is used both in combination with traditional pharmacotherapy (especially if it is not effective enough) or as monotherapy. The use of medical xenon inhalations provides analgesic, sedative, antidepressant and muscle relaxant effects.
Xenon is practically insoluble in body fluids, which ensures rapid exposure and rapid elimination of the drug after the procedure. It potentiates the action of pharmacological drugs, while it does not cause either mental or physical dependence. It is especially important to note the muscle relaxant effect of medical xenon. At the beginning of the last century, the American physiologist and psychiatrist Edmund Jacobson noticed that the synthesis of thoughts is preceded by muscle tension. He deduced the dependence of mental activity on the contraction of skeletal muscles. His main work "You must relax" ("You Must Relax" 1934) is based on the fact that there is a direct relationship between skeletal muscle tone and negative emotional arousal in its various forms (that is, anger, fear, nervousness, irritability). Negative emotions are expressed in muscle contractions and changes in muscle tone, which further leads to the formation of a number of psychosomatic diseases. On this basis, he invented a series of exercises that allow you to relax one or another “stressed” muscle group. This technique involves a long course of exercises.
It potentiates the action of pharmacological drugs, while it does not cause either mental or physical dependence. It is especially important to note the muscle relaxant effect of medical xenon. At the beginning of the last century, the American physiologist and psychiatrist Edmund Jacobson noticed that the synthesis of thoughts is preceded by muscle tension. He deduced the dependence of mental activity on the contraction of skeletal muscles. His main work "You must relax" ("You Must Relax" 1934) is based on the fact that there is a direct relationship between skeletal muscle tone and negative emotional arousal in its various forms (that is, anger, fear, nervousness, irritability). Negative emotions are expressed in muscle contractions and changes in muscle tone, which further leads to the formation of a number of psychosomatic diseases. On this basis, he invented a series of exercises that allow you to relax one or another “stressed” muscle group. This technique involves a long course of exercises. The use of xenon inhalations allows you to achieve good muscle relaxation already in the first session, helping to displace the muscle triggers previously described by Jacobson. It should be noted that exactly muscle tension accompanies the state of obsession and is one of the most painful manifestations of the disease. Thus, by eliminating muscle-tonic manifestations with xenon, we manage to achieve a state of relaxation, calmness and comfort in the patient. This contributes to effective treatment in the shortest possible time.
The use of xenon inhalations allows you to achieve good muscle relaxation already in the first session, helping to displace the muscle triggers previously described by Jacobson. It should be noted that exactly muscle tension accompanies the state of obsession and is one of the most painful manifestations of the disease. Thus, by eliminating muscle-tonic manifestations with xenon, we manage to achieve a state of relaxation, calmness and comfort in the patient. This contributes to effective treatment in the shortest possible time.
The property of xenon to potentiate the action of pharmacological drugs used to treat OCD provides the possibility of a gradual reduction in their dosage up to complete withdrawal. The method of inhalation of medical xenon involves the obligatory conduct of the first three sessions without long breaks (the maximum interval between sessions is 48 hours) for the appearance of a cumulative effect. Later, after assessing the dynamics of the condition, the doctor determines the duration of the required course of treatment, as well as the advisability of changing or adding drug therapy.
Given the rapid muscle relaxant, anxiolytic and antidepressant effect of xenon therapy, as well as pronounced side effects, it seems appropriate to further introduce medical xenon into clinical practice in the complex treatment of patients with obsessive-compulsive disorder.
Obsessive Compulsive Disorder Treatment
Great Thought is an obsessive compulsive disorder treatment program. We will relieve you of obsessive thoughts, movements and rituals. Let's get back to life!
Symptoms of obsessive-compulsive disorder
- Frightening images and drives
- Compulsive acts (rituals)
- Obsessive check of own actions
- Fear of trouble, pollution or contamination
- Inexplicable desire to count something
- Excessive organization and pedantry
- Perfectionism in relationships, work and even leisure
- "Stuck", "looping" on one's thoughts
You feel that over time your mood becomes worse: apathy, depression, obsessions increase, and rituals begin to fill all your free time or harm your physical health.
You may have had more than one meeting with psychologists, psychotherapists and psychiatrists. You are not given the "scary" psychiatric diagnoses of Schizophrenia or Bipolar Disorder, but are prescribed medication and psychotherapy nonetheless. However, such treatment cannot be called effective - the symptoms persist and only aggressive pharmacotherapy temporarily reduces anxiety.
What is obsessive-compulsive disorder?
Obsessive-compulsive disorder is a syndrome characterized by the presence of obsessive thoughts (obsessions) to which a person reacts with certain actions (compulsions). The causes of the disorder are rarely superficial. The syndrome is also accompanied by the development of obsessive memories and various pathological phobias. May be chronic, episodic or progressive.
Obsession - obsessive thought, persistent desire for something, uncontrollable and accompanied by anxiety and intense anxiety. In an attempt to cope with such thoughts, a person resorts to committing compulsions.
Compulsion - an irresistible need to perform certain actions (rituals), which can be assessed by the person himself as irrational or meaningless, and the internal need to perform them is forced and is the result of obsessive ideas.
Common examples of OCD manifestations
- An exaggerated sense of danger. Fear of the materiality of thoughts:
- "now I will lose control and hurt my loved ones"
- "something terrible is about to happen, I can feel it"
- "I shouldn't think like that, all this will come true because of me"
- Pathological fear of pollution. Thirst for Purity
- Excessive perfectionism, exaggerated responsibility - "everything must be done perfectly", "everything depends on me, mistakes are unacceptable"
How does this painful algorithm work?
Most people have unwanted or intrusive thoughts quite often, but all sufferers of the disorder greatly exaggerate their importance. Fear of one's own thoughts leads to attempts to neutralize the negative feelings that arise from obsessions, for example by avoiding thought-provoking situations or by engaging in "rituals" of excessive self-cleansing or prayer.
Fear of one's own thoughts leads to attempts to neutralize the negative feelings that arise from obsessions, for example by avoiding thought-provoking situations or by engaging in "rituals" of excessive self-cleansing or prayer.
As we noted earlier, repetitive avoidance behavior can "get stuck", "loop", i.e. tend to repeat. The cause of obsessive-compulsive disorder is the interpretation of intrusive thoughts as catastrophic and true.
If you periodically experience over the years:
- Constant or fluctuating anxiety
- The need to perform certain ritualized actions
- A persistent decline in the quality of life due to the need to avoid certain thoughts and actions, places and events
And you are also persecuted:
- Significant problems in studies and career
- Failure to establish a serious relationship
- Constant criticism and pressure from relatives
- Many senseless activities
- Excessive involvement in computer games and the Internet, alcohol
- Loneliness and isolation
We strongly recommend that you do not delay seeking help and that you complete a remedial program.
Consultations and psychotherapeutic sessions according to the program are held several times a week, until the relief of severe symptoms, then the frequency of meetings with specialists is reduced to 2–3 per month. Count on the fact that in the end we will deal with your problem together.
Treatment of obsessive-compulsive disorder in Neuro-Psi
Every day, the specialists of the NEURO-PSI clinic analyze the world practice in the field of psychiatry and psychotherapy. The goal is the impartial selection and implementation of those methods of treatment and psychological assistance, the effectiveness of which has been convincingly proven in independent studies.
We are guided by the principles of evidence-based medicine and use as a basic method of treatment a psychotherapeutic paradigm, the effectiveness of which has been widely recognized by the professional community.
1. What is the essence of the obsessive-compulsive disorder treatment program?
A comprehensive work is carried out with the client, taking into account the main factors that create well-being.
The main emphasis is on teaching the client how to properly respond to his thoughts, emotions, inner feelings and interpretation of external events.
All types of psychotherapeutic and drug treatments serve the same goal: to achieve the best result in the shortest possible time. At the same time, by coordinating the efforts of specialists in various fields, the most complete coverage of all types of mental illnesses, disorders and disorders is possible.
2. What treatments are used
- Priority:
- Cognitive-Behavioral Therapy.
- Schema Therapy.
- Reality Therapy.
- Choice Theory.
- Rational pharmacotherapy.
- Psychopharmacotherapy (if indicated)
- Biofeedback Therapy
- Rational psychocorrection of stress
- Jacobson progressive muscle relaxation.
- Traditional and modern gymnastic systems, relaxation techniques.
- Breathing techniques .
- Stress exposure.
- Training in self-control.
- Lifestyle modification
- Work with bad habits.
- Diet correction.
- Professional and social adaptation.
3. How is the treatment under the program
Each treatment program at the NEURO-PSI clinic consists of four stages:
- diagnostics,
- work with disease symptoms,
- work with the causes of the disease,
- consolidation of the achieved results.
Work efficiency is increased by dividing the treatment process into a predetermined number of sessions, at convenient times and without hospitalization. This means that each program is adapted to the problem that the client has addressed.
The program method of treatment is predictable, time-limited, productive, and, most importantly, understandable for the client.
Of course, the treatment takes place in a comfortable mode without interruption from work, study or family. Specialists of various profiles will work with you (team method). This is necessary to minimize the risk of diagnostic errors that could lead to the adoption of a suboptimal treatment plan.
Specialists of various profiles will work with you (team method). This is necessary to minimize the risk of diagnostic errors that could lead to the adoption of a suboptimal treatment plan.
Improvements in well-being and mood (healing) occur in stages: after the decrease in emotional problems, bodily symptoms decrease. Working with the causes (etiology) of obsessive-compulsive disorder helps to avoid relapses in the future.
4. What are the results and prognosis?
Upon completion of the program, you get rid of obsessive thoughts and rituals, fear of pollution, unmotivated fears, panic attacks and multiple vegetative symptoms (sudden jumps in blood pressure, heart palpitations, dizziness, nausea).
According to statistics, the effectiveness of the methods used approaches 100% if all recommendations of specialists are followed.
Skills you acquire during the program:
- self-control and self-regulation
- constructive analysis of the state of the body
- understanding one's own mental and emotional sphere
- ability to control one's attention
- ability to act consciously in stressful situations
Significantly improves emotional and physical condition, gains self-confidence, in the future.