Natural narcolepsy treatment
Natural Tips to Stay Alert With Narcolepsy
Medically Reviewed by Carol DerSarkissian, MD on October 01, 2022
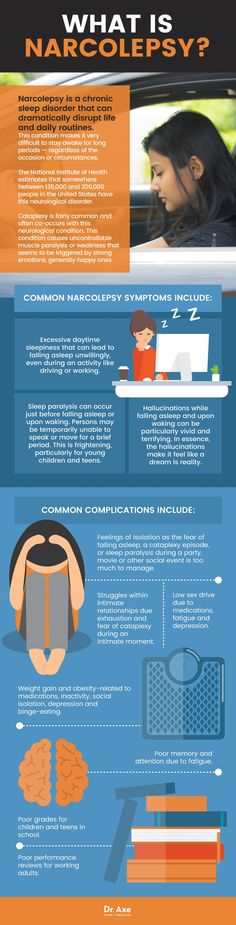
The world narcolepsy was coined in 1880s to mean “seized by somnolence,” or sleepiness. Just staying awake through the daylight hours can be difficult or impossible. Prescription drugs are often the go-to therapy for this brain disorder. But changes to your diet, habits, and environment also can help keep you alert without the side effects from medications.
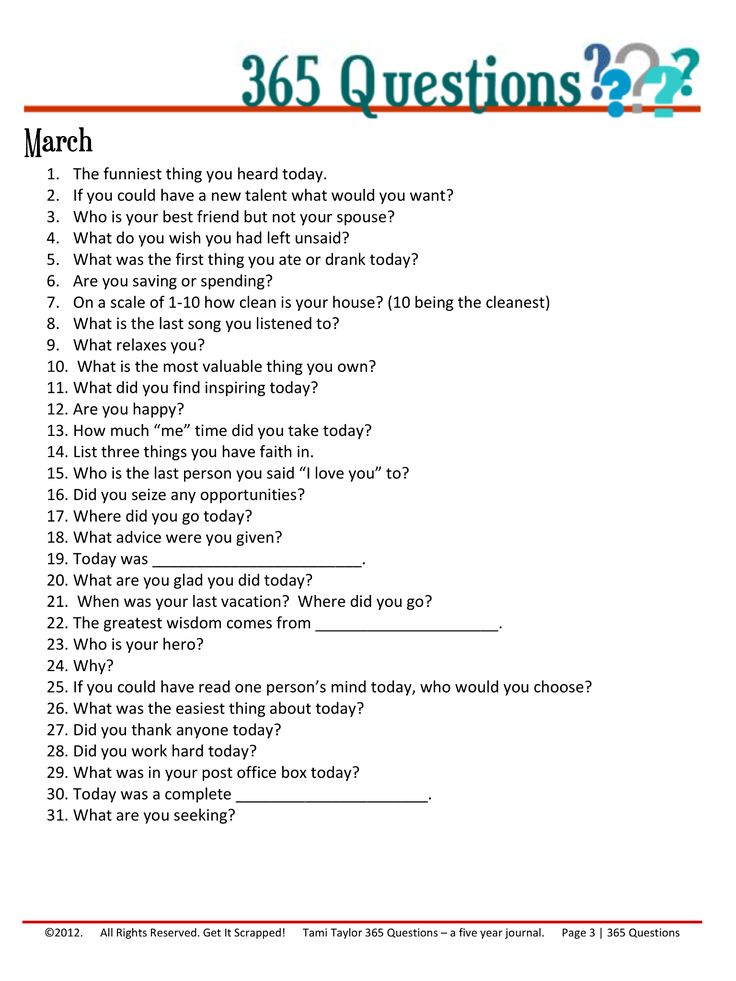
It’s called “strategic napping.” Try to take several cat naps of about 15-20 minutes every day. But cap your dozes to no more than 30 minutes. Sleeping longer can make you more tired. If you have a job, the Americans With Disabilities Act requires your employer to make arrangements for you. For example, you might use your office, nursing lounge, or a wellness room to sneak quick rests.
Many people with narcolepsy sleep restlessly at night. Your body then needs to make the shortfall during the day. Try these tips to pack more quality ZZZs during your normal bedtime hours:
- Relax before turning in. Avoid alcohol close to bedtime.
- Try to go to bed at the same time each night.
- If you wake up during the night, avoid reaching for your phone or other electronics. Screens stimulate, not relax, you.
If you have a more severe type of condition called narcolepsy with cataplexy, you may be low on a hormone called hypocretin that helps you stay alert. The good news is that many foods contain hypocretin. They include sourdough bread, dark leafy greens, kimchi and other fermented vegetables, and salmon and other foods rich in omega-3 fatty acids.
Lots of people feel drowsy after a big meal. That can be especially true if you have narcolepsy. Limit sugar and other carbs to stay more alert. Eat smaller meals and snack on nuts, berries, and other nutritious foods in between.
Walk around every 20 minutes or so to stay alert. If you work at a desk, get up and visit the break room. Climb a flight of stairs and back. Other ideas to sneak in blood-flowing moments include:
Climb a flight of stairs and back. Other ideas to sneak in blood-flowing moments include:
- Pace while talking on the phone.
- Stand up when you read emails and texts.
- Walk to the bathroom even if you don’t need to go.
Those golden rays not only help you stay awake, they spark your brain to make feel-good chemicals. Sunshine helps your skin make vitamin D, a key nutrient in treating narcolepsy. Low vitamin D levels have been linked with poor sleep quality. Pair morning strolls with whole grains, scrambled eggs, and other foods that help put pep in your step.
Cold feet may help keep you awake. One study found that people with narcolepsy tend to have warmer skin temperatures in their fingers and toes. Cooler hands and feet made the people in the study more alert. You can dial down your body warmth with special cooling clothing, by avoiding warm drinks or meals, or using fans to keep your hands and feet chilled.
Coffee, tea, or other caffeine-fueled eye-openers may help prevent drowsiness. But take care if you take stimulant medications such as armodafinil (Nuvigil) or modafinil (Provigil) for your narcolepsy. Mixing them with caffeine can make your heart race or trigger jitters and anxiety. Avoid caffeine after 4 p.m.
But take care if you take stimulant medications such as armodafinil (Nuvigil) or modafinil (Provigil) for your narcolepsy. Mixing them with caffeine can make your heart race or trigger jitters and anxiety. Avoid caffeine after 4 p.m.
Regular physical activity ramps up your metabolism but also may help you rest better at night. Find something you can enjoy and stick with at least 20 minutes per day. Think tai chi, dancing, weight training, gardening, swimming, or tennis. Finish your workouts at least 3 hours before bedtime so you can wind down for restful slumber.
In a small survey, smokers who had narcolepsy all reported nicotine helped fight daytime sleepiness. There was a dangerous downside, though. One-third of the respondents said they’d fallen asleep while smoking, and many others had come close. Lit smoking materials led to burn injuries and property damage, and even larger fires. And it can be tough to quit because nicotine withdrawal causes drowsiness.
IMAGES PROVIDED BY:
1) Sanja Radin / Getty Images
2) fizkes / Getty Images
3) jacoblund / Getty Images
4) (Clockwise from top left) clubfoto / Getty Images, billnoll / Getty Images, naito8 / Getty Images, 4kodiak / Getty Images
5) Neydtstock / Getty Images
6) LL28 / Getty Images
7) adamkaz / Getty Images
8) Rike_ / Getty Images
9) Gregor Schuster / Photographer's Choice RR
10) PixelsEffect / Getty Images
11) alejandrophotography / Getty Images
SOURCES:
Progress in Neurobiology: “Challenges in the development of therapeutics for narcolepsy.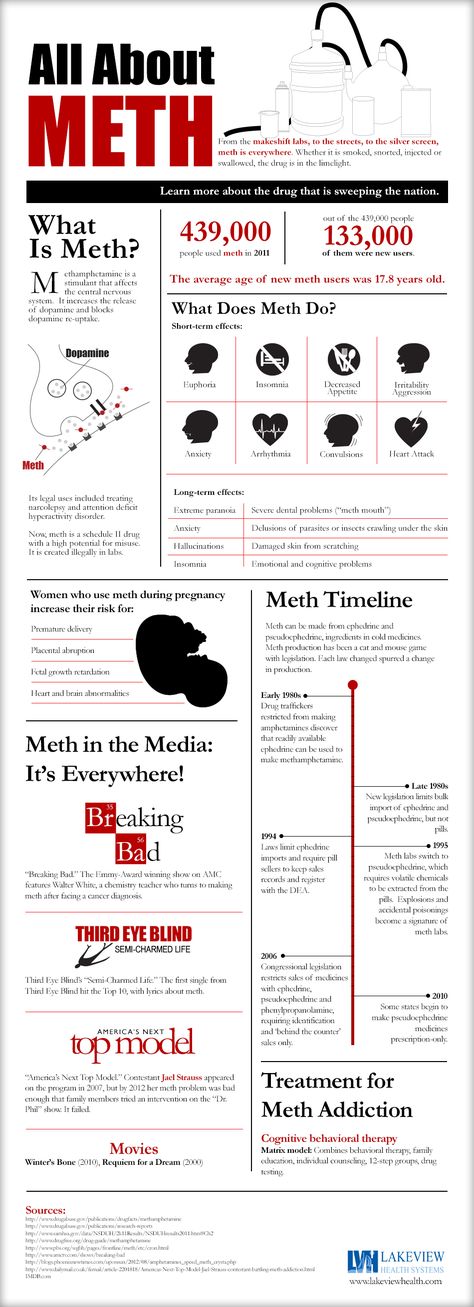 ”
”
Division of Sleep Medicine at Harvard Medical School: “Medications for Treating Daytime Sleepiness in Narcolepsy,” “Understanding Narcolepsy,” “Narcolepsy: Medications,” “Narcolepsy,” “Narcolepsy: At Work.”
Sleep Science: “Current and Future Treatment Options for Narcolepsy: A Review.”
Narcolepsy Network: “For Employees,” “Narcolepsy and Wakefulness: What’s the Connection?” “Lifestyle Adjustments.”
Sleep Foundation: “What Causes Narcolepsy?” “Cataplexy,” “Diet, Alcohol, Exercise, and Narcolepsy.”
Nutrients: “The Association Between Vitamin D Deficiency and Sleep Disorders: A Systematic Review and Meta-Analysis.”
Cleveland Clinic: “Narcolepsy: Management and Treatment.”
Journal of Clinical Sleep Medicine: “Narcoleptic Patients' Perceptions of Nicotine.”
© 2022 WebMD, LLC. All rights reserved. View privacy policy and trust info
Narcolepsy: Complementary and Alternative Treatments
Narcolepsy is a chronic sleep disorder that disrupts your wake-sleep pattern and brings about overwhelming drowsiness and periods of sudden sleep attacks during the daytime.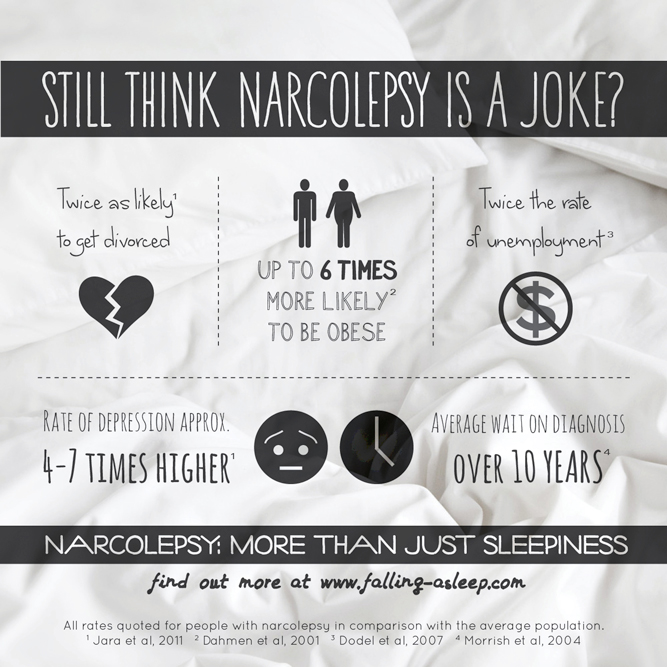 The complex, lifelong condition affects 1 in 2,000 people but it often goes undiagnosed. There’s no cure for narcolepsy but medications and certain lifestyle changes may help manage the symptoms.
The complex, lifelong condition affects 1 in 2,000 people but it often goes undiagnosed. There’s no cure for narcolepsy but medications and certain lifestyle changes may help manage the symptoms.
For some people with narcolepsy, conventional Western medication alone may not be enough to ease the day-to-day symptoms, which can take a toll on quality of life. Some choose to include complementary medicine or turn to alternative medicine to manage their condition.
Complementary medicine includes approaches that you take along with traditional Western medicine. While alternative medicine focuses on approaches you may take instead of conventional medicine your doctor uses. In some cases, your doctor may choose to combine different approaches to get the best results. This is called integrative medicine.
For narcolepsy, this can range from lifestyle changes, melatonin supplements, and natural herbal extracts to trying yoga or acupuncture for a better wake-sleep cycle.
Searching for an Alternative
For Gina Dennis, 49, intense sleepiness was something she struggled with since she was a teenager. Getting out of bed each morning was an ordeal. It was something she shared in common with her mother. When her mother got diagnosed with narcolepsy later in life, Dennis decided to get checked out as well. Soon after, Dennis who was in her late 30s by then, was also diagnosed with narcolepsy.
Getting out of bed each morning was an ordeal. It was something she shared in common with her mother. When her mother got diagnosed with narcolepsy later in life, Dennis decided to get checked out as well. Soon after, Dennis who was in her late 30s by then, was also diagnosed with narcolepsy.
Her doctor put her on a regimen of drugs to help her stay awake through the day. But the drugs didn’t work as well as the Dallas native had hoped. But when her teenage son started to show symptoms, she came to find out that narcolepsy ran in her family. Turns out, her son and ex-husband also had the same sleeping disorder.
“It was breaking my heart, so we eventually got [my son] diagnosed. But here he is, a teenager, and he’s looking at a lifetime of medications. It just didn't seem good enough for me. So, I started to do some research,” Dennis says.
She went down the internet rabbit hole and stumbled upon another blogger who suggested the ketogenic diet to curb the daytime sleepiness. She decided to give it a try. In the ketogenic diet, the idea is to focus on getting your calories from high fat and moderate amounts of protein foods and cut back on most carbohydrates like sugar, bread, and pasta. It can be quite restrictive.
She decided to give it a try. In the ketogenic diet, the idea is to focus on getting your calories from high fat and moderate amounts of protein foods and cut back on most carbohydrates like sugar, bread, and pasta. It can be quite restrictive.
Dennis says she saw changes within a week. “I had a level of wakefulness that I had never had before, not even with the medication, it was cleaner, it didn't feel a buzz as some of the medications I had been taking,” Dennis says. In fact, over time, she stopped taking her medications altogether.
It’s been about 10 years since Dennis and her family started making dietary changes. While it’s helped bring a lot of the symptoms under control, she’s quick to add that it’s not a cure-all.
“I'm not saying I don't have symptoms because I do. But what I found through this entire journey is that diet is one component, the other component is some lifestyle changes.”
Alternative and Complementary Treatments
If you’re looking to try out or take on complementary or alternative approaches to manage your day-to-day narcolepsy symptoms, there are a few ways to go about it.
Yoga and meditation. A few studies point out that certain yoga positions can bring about relaxation, ease anxiety, and help with sleep issues. This may be because of its meditative properties such as breathing in and out and taking in the moment.
However, not all types of yoga are beneficial, says Rubin Naiman, PhD, a psychologist, sleep and dream specialist and clinical assistant professor of medicine at the University of Arizona Center for Integrative Medicine.
“I think yoga is helpful for anybody and everybody, because it really helps refashion our relationship with the body,” Naiman says. “There are 10 ways to do yoga, and not all are helpful. But when it’s done right, it’s almost like a friendly dialogue with our body.”
If you’re looking to try yoga to help you relax and sleep better at night, keep these things in mind:
- Find the right style of yoga. Hot yoga or vinyasa yoga require movements that will raise your heart rate. Doing this before bed will make your sleep worse.
 Instead, choose a relaxing technique.
Instead, choose a relaxing technique. - Set the scene for yoga and meditation. You can dim the light, put on soft, soothing music, and find a space to stretch out in comfy clothes.
- Focus on breathing. Pay attention to taking your breath in and out through your nose and mouth. This can be therapeutic and help you de-stress before you get to bed.
- Don’t push yourself too hard. Do only what you physically tolerate. You can work your way up over time.
Herbal remedies. Research shows that certain herbs can induce or regulate sleep. You can add them to beverages like tea or take them as supplements. For example, chamomile flower used in teas may help with poor sleep issues. The flower has several chemical compounds like apigenin that can have a mild tranquilizing effect. However, there needs to be more research done on chamomile’s effectiveness for conditions like narcolepsy. Some people are allergic to chamomile so it’s best to try in small amounts first.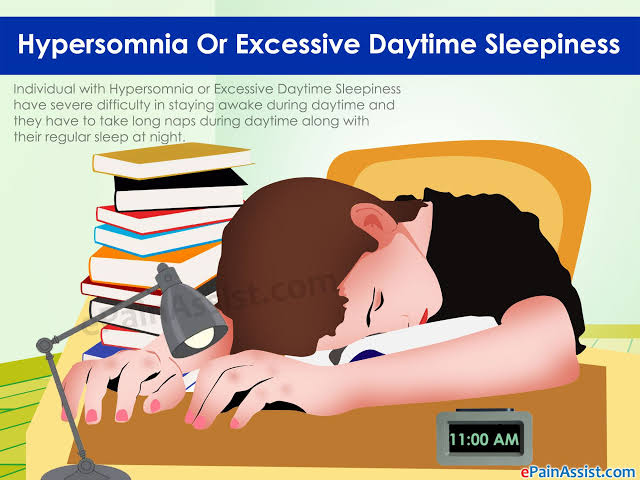
Valerian root has natural sedative properties and has long been used as a sleep aid to help ease issues like stress, anxiety or headaches that disrupt your sleep cycle. But clinical trials on valerian root’s effects have had inconsistent results. Experts aren’t sure what effects long-term use may have on your body.
Other herbs used to improve sleep problems include passion flower, kava, red ginseng, lemon balm, and hops. If you’re taking prescription drugs, it’s important to note that certain herbs can interact with other drugs or cause side effects. It’s always a good idea to tell your doctor before you try any herbal remedies or supplements.
Melatonin. Your body naturally makes melatonin around 4 hours before you got to sleep. It’s triggered when your body’s exposure to light reduces naturally at night. But if you have narcolepsy, your sleep/wake cycle may not be properly regulated. Research shows that taking melatonin supplements can help regulate and induce sleep, increase rapid eye movement (REM) sleep time, and improve sleep quality. You can buy melatonin in pill form over the counter. If you’re not sure how much you take, ask the pharmacist or your doctor.
You can buy melatonin in pill form over the counter. If you’re not sure how much you take, ask the pharmacist or your doctor.
Lifestyle changes. When you have narcolepsy, one of the symptoms includes falling asleep or feeling excessively drowsy involuntarily during the day. This can be dangerous if you’re driving or out and about in public. To reduce the intense sleepiness during the day and sleep better at night, you can:
- Schedule small, regular naps during the day.
- Stick to a bedtime routine. Try to go to bed at the same time each night and wake up at the same time, too.
- Reduce any distractions in the room where you sleep at night.
- Avoid alcohol, smoking, and caffeine before bedtime.
- Don’t eat large meals for dinner before sleep.
- Exercise regularly to help you stay awake and alert during the day. But don’t work out or push yourself too much 2 hours before you go to bed.
Cognitive behavioral therapy (CBT). This type of psychological treatment attempts to change your thinking patterns. This may help you cope with symptoms for several health conditions, including narcolepsy. Naiman says it’s especially helpful for people who have cataplexy, a core symptom in which you may have a sudden muscle weakness and collapse. It can be triggered by emotions like laughter, surprise, or negative things like stress and anxiety.
This type of psychological treatment attempts to change your thinking patterns. This may help you cope with symptoms for several health conditions, including narcolepsy. Naiman says it’s especially helpful for people who have cataplexy, a core symptom in which you may have a sudden muscle weakness and collapse. It can be triggered by emotions like laughter, surprise, or negative things like stress and anxiety.
“When people begin to have symptoms of cataplexy, there is a reaction of anxiety like, ‘oh God, I’m about to fall off,’ and then the anxiety spirals into this adversarial relationship with narcolepsy,” Naiman says. “With CBT, we talk about meeting cataplexy in a mindful way. It’s about understanding that if I tense up each time, it makes the cataplexy worse.”
For some patients, Naiman says he uses CBT to help them consciously work through a narcolepsy episode when it comes on. This helps them learn skills to handle it better the next time they have a sudden episode.
CBT may include learning other strategies like:
- Learning how to use problem-solving skills to manage difficult situations
- Evaluating thoughts and experiences in a realistic way
- Developing confidence
If you plan to try CBT, ask your doctor or a psychologist if it’s right for you.
Acupuncture. As part of traditional Chinese medicine, acupuncture practitioners insert thin needles at specific points on your body. The idea is for the needles to stimulate certain pressure points that bring about pain relief and reduce narcolepsy symptoms like headache. However, researchers say there’s not enough evidence to know if it helps with sleep problems.
Acupuncture is relatively safe if it’s done by someone who’s experienced. However, if it’s done incorrectly, nonsterile needles can cause infections or other dangerous health problems. If you’re going to try acupuncture, make sure to visit an experienced acupuncturist.
Emotional freedom technique (EFT). Similar to acupuncture, EFT is a simple, self-therapeutic manual tapping therapy used to relieve stress and anxiety. To do it, you have to tap certain meridian points on your face and body while saying out loud whatever is concerning you to work through distressing situations or the onset of anxiety or depression. It combines other psychological therapies like talk therapies, exposure therapy, and cognitive behavioral therapy. It promotes self-acceptance.
Similar to acupuncture, EFT is a simple, self-therapeutic manual tapping therapy used to relieve stress and anxiety. To do it, you have to tap certain meridian points on your face and body while saying out loud whatever is concerning you to work through distressing situations or the onset of anxiety or depression. It combines other psychological therapies like talk therapies, exposure therapy, and cognitive behavioral therapy. It promotes self-acceptance.
It was founded in the 1995 and the idea behind the tapping is that it stimulates the pressure points to signal the brain and the central nervous system to release chemicals to ease stress or fear.
While there are few studies that show EFT’s effects and benefits psychologically, there is limited evidence if it positively impacts physical health to improve conditions like narcolepsy and others. But EFT is safe, harmless, and a cheap, affordable option you can use anywhere if you want to calm your emotions and center yourself.
Things to Be Aware of Before You Try Complementary or Alternative Medicine
Most complementary and alternative treatments like yoga or EFT are safe to use and harmless. But not all alternative medicine options, particularly herbal remedies, products, and supplements, are safe even if they are “natural.”
Many herbs or over-the-counter supplements may interact or suppress prescription medication you may be taking and may cause dangerous side effects. The FDA does not regulate dietary supplements like it oversees and regulates prescription drugs.
Thinking about trying a complementary or alternative medicine or product for narcolepsy?
- Talk to your doctor about it. Ask if it will affect or interact with any drugs you may be taking for narcolepsy or other conditions you may have. Tell them if you’re planning to use a certain product or technique. This will help them get a full picture of your health and medical history when they treat you.
- Look up potential side effects or safety for long-term use before you try any herbs.
 If you’re not sure, ask your doctor about it.
If you’re not sure, ask your doctor about it. - If you’re pregnant or planning to get pregnant, ask your doctor before trying something new.
- Ask your health insurance provider if they cover complementary or alternative treatment options like CBT or acupuncture. This may help avoid any surprise bills or expenses.
- Talk to your doctor before you cut back or stop taking your prescription drugs or treatments.
If you experience side effects or an allergic reaction from certain products or supplements, get medical attention as soon as possible or tell your doctor about it.
what is it, symptoms, treatment, causes of daytime sleepiness
Font size Color scheme Images
x
Make an appointment
Name* Phone* Adult Child (under 18)x
Sign up for analysis
Name* Telephone* ☆ st. Malaya Balkanskaya, 23 (m.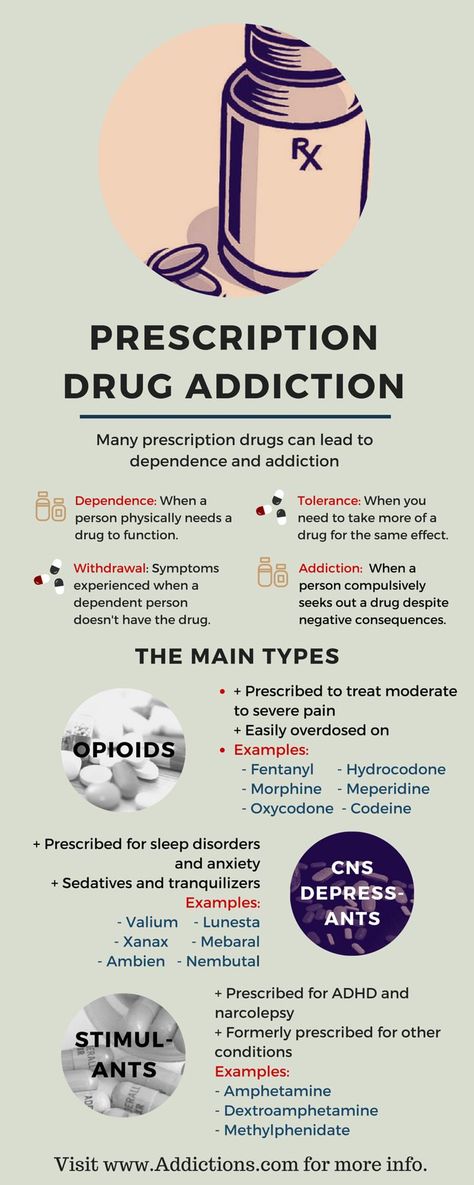 Kupchino)
Kupchino)
Dunaisky ave., 47 (m. Dunaiskaya)
Udarnikov ave., 19 (m. Ladozhskaya)
st. Marshala Zakharova, 20 (metro station Leninskiy pr-t)
Vyborgskoe shosse, 17 (metro Prospect of Enlightenment)
- Call
435 55 55 -
Make an appointment
This disease is treated by Somnologist
The information provided on this page should not be used for self-treatment or self-diagnosis. If you suspect a disease, you should seek help from a qualified specialist. Only your doctor can diagnose and prescribe treatment.
Article content:
- Causes
- Symptoms of narcolepsy
- Diagnostics
- Narcolepsy treatment
- Prognosis and prevention
What is narcolepsy?
Narcolepsy is a pathological condition characterized by an inability to control sleep and wakefulness. Sudden onset of excessive daytime sleepiness and other symptoms of narcolepsy can occur at any time, even in situations that require extreme concentration, such as driving. The risk group for the development of narcolepsy is men, the frequency of cases is 1 in 2 thousand people. But there is an opinion that the prevalence is higher due to the fact that not all patients do not seek medical help and treatment. Narcolepsy Source:
The risk group for the development of narcolepsy is men, the frequency of cases is 1 in 2 thousand people. But there is an opinion that the prevalence is higher due to the fact that not all patients do not seek medical help and treatment. Narcolepsy Source:
description of the clinical observation. Remizevich R.S., Kurasov E.S. Bulletin of the National Medical and Surgical Center. N. I. Pirogova, Volume 8, No. 4, 2013. pp. 141-145 - not a fatal pathology, but accidents still happen during attacks.
Causes
The exact causes of narcolepsy are unknown, although it has been established that heredity plays a role, as well as a lack of the neurotransmitter orexin, which is responsible for wakefulness.
REM sleep literally invades the periods of wakefulness and the transition to sleep. Symptoms of narcolepsy are associated with a sharp loss of muscle tone, the appearance of vivid visions, which are just characteristic of the phase of REM sleep. nine0003
It was not possible to establish the exact reasons for the decrease in the production of the neurotransmitter, but the predisposing factors for the development of the pathology were identified:
- serious craniocerebral injuries and their consequences;
- infectious diseases affecting the nervous system Source:
Autonomic disorders in narcolepsy (review of foreign literature). Golokov V.A., Nikolaeva T.Ya., Schneider N.A., Kantimirova E.A. Medical Almanac No. 5(45), 2016. pp. 165-168;
Golokov V.A., Nikolaeva T.Ya., Schneider N.A., Kantimirova E.A. Medical Almanac No. 5(45), 2016. pp. 165-168; - pronounced hormonal changes; nine0025
- autoimmune diseases;
- chronic stress and severe emotional upheavals;
- nervous and physical exhaustion.
As a rule, the development of a disease requires the combined action of several factors at once. Great importance in the mechanism of the development of the state is given to the work of immunity. An immune response is triggered, as a result of which its own cells are mistakenly destroyed, which leads to the onset of symptoms.
Symptoms of narcolepsy
The most common symptom is excessive daytime sleepiness, as well as persistent sleep disturbances at night. This creates inconvenience, spoils the quality of life, affects success in work and social relations.
Over time, the clinical picture changes, other signs join:
- The first and most common symptom is sudden falling asleep during the day.
 Drowsiness is severe, patients fall asleep against their will, even in unsuitable surroundings. But after waking up, they feel a surge of strength, there is no drowsiness. This state can be deceptive - after a short time they fall asleep again. At the same time, waking up the patient is no more difficult than during normal sleep. nine0025
Drowsiness is severe, patients fall asleep against their will, even in unsuitable surroundings. But after waking up, they feel a surge of strength, there is no drowsiness. This state can be deceptive - after a short time they fall asleep again. At the same time, waking up the patient is no more difficult than during normal sleep. nine0025 - Cataplexy Source:
Narcolepsy with prepubertal onset cataplexy. Gromova D.O., Zinovieva O.E., Rogovina E.G., Poluektov M.G. Neurological journal No. 4, 2012. pp. 22-27 - sudden muscle weakness after strong emotional outbursts. The resulting weakness can be explained by a sharp loss of muscle tone, which often ends in injuries associated with a fall. The duration of the attack varies and lasts up to several minutes, followed by falling asleep. nine0025 - Hallucinations on falling asleep and waking up. They are characterized as vivid acoustic or visual visions that correspond to REM sleep. This state is sometimes called "waking sleep", and the patient himself does not realize that he is sleeping and dreaming.
 This is a dangerous condition that creates confusion between reality and dream.
This is a dangerous condition that creates confusion between reality and dream. - Sleep paralysis is a condition characterized by the inability to move after waking up, but the ability to breathe and blink remains. The patient is conscious, understands where he is. Most often, sleep paralysis is formed in the morning, less often in the evening and at night. Sleep paralysis is aggravated by hallucinations without the ability to move. The condition goes away after a few minutes. nine0025
Only 10% of patients present with all symptoms at once. Usually first appear in young people, with no previous diseases. Although they can be associated with strong emotional upheavals or chronic stress. After the first onset of symptoms, narcolepsy is permanent, but does not affect life expectancy.
In clinical practice, it is customary to distinguish 2 types of narcolepsy:
- the first occurs due to orexin deficiency, the appearance of cataplexy is characteristic Source:
Narcolepsy-cataplexy. Vasilchenko T.S., Gabdrakipova A.A. Bulletin of Science and Education No. 24(78), 2020. pp. 53-55;
Vasilchenko T.S., Gabdrakipova A.A. Bulletin of Science and Education No. 24(78), 2020. pp. 53-55; - the second is characterized by a normal level of the neurotransmitter and cataplexy does not occur.
Diagnostics
The main thing is to detect the pathology in time to prevent risks to the patient's physical health and harm to others. The patient cannot control narcolepsy, attacks occur even at the time of hard work and maximum concentration of attention, as well as performing tasks that involve risks to health and even life. nine0003
When visiting a doctor, the symptoms that characterize the diagnosis are studied in detail. The doctor is interested in:
- the patient's complaints, when the attack first occurred and how long it lasted, what symptoms are present;
- neurological examination data, some tests;
- results of additional examination methods to confirm the diagnosis.
These include polysomnography. Source:
Source:
Problems in the differential diagnosis of epileptic seizures and narcolepsy (clinical observation). Dmitrenko D.V., Alekseeva O.V., Sapronova M.R., Usoltseva A.A., Areshkina I.G. Bulletin of the North-Eastern Federal University. M. K. Ammosov. Series: Medical Sciences No. 4(13), 2018. pp. 44-51 with EEG data. This method of examination allows you to objectively assess the activity of the brain and sleep phases. The survey continues throughout the night. Electrodes are placed on the patient's head, which fix the indicators and give them out in the form of curves - the doctor analyzes the data. nine0003
Additionally, CT and MRI are recommended to assess brain function and condition. In some cases, it may be necessary to analyze the cerebrospinal fluid, which is aimed at determining the concentration of orexin.
Treatment tactics are determined by the data obtained during the examination. This takes into account the severity of concomitant pathology, acquired diseases.
Treatment of narcolepsy
Drug treatment prescribed by specialists is constant, but the number of drugs depends on the clinical picture and the characteristics of the manifestation of the disease. Doctors usually prescribe:
- stimulants;
- sleeping pills to help normalize night sleep;
- antidepressants;
- means to combat daytime sleepiness.
Other recommendations are added to medications - lifestyle changes that help control symptoms. Patients with narcolepsy are recommended to:
- strictly follow the daily routine: go to bed and get up at the same time, regardless of holidays and weekends; nine0025
- give up alcohol completely and stop smoking;
- Minimize your intake of coffee, sugary sodas, energy drinks, and junk food;
- introduce a short daytime nap into your schedule;
- lead an active lifestyle, play sports, for example, exercise therapy, yoga.
Prognosis and prevention
Unfortunately, there is no cure for narcolepsy. All treatment is aimed at controlling and maximizing symptom relief. After the course of treatment, the patient returns to his usual way of life, although there are still some restrictions. nine0003
All treatment is aimed at controlling and maximizing symptom relief. After the course of treatment, the patient returns to his usual way of life, although there are still some restrictions. nine0003
There are some prohibitions for all narcolepsy patients. They are forbidden to drive a car, as well as to occupy positions related to hazardous industries, for example, to work with machine tools, in large factories, etc. After all, an attack can happen at any moment, regardless of what a person is doing.
- Narcolepsy-cataplexy. Vasilchenko T.S., Gabdrakipova A.A. Bulletin of Science and Education No. 24(78), 2020. p.53-55
- Narcolepsy with cataplexy with onset in prepubertal age. Gromova D.O., Zinovieva O.E., Rogovina E.G., Poluektov M.G. Neurological journal №4, 2012. pp.22-27
- Modern concepts of narcolepsy with a description of clinical observation. Remizevich R.S., Kurasov E.S. Bulletin of the National Medical and Surgical Center. N. I. Pirogova, Volume 8, No.
 4, 2013. p.141-145
4, 2013. p.141-145 - Autonomic disorders in narcolepsy (review of foreign literature). Golokov V.A., Nikolaeva T.Ya., Schneider N.A., Kantimirova E.A. Medical Almanac No. 5(45), 2016. p.165-168
- Problems of differential diagnosis of epileptic seizures and narcolepsy (clinical observation). Dmitrenko D.V., Alekseeva O.V., Sapronova M.R., Usoltseva A.A., Areshkina I.G. Bulletin of the North-Eastern Federal University. M. K. Ammosov. Series: Medical Sciences No. 4(13), 2018. p.44-51
Article published : 31/05/2017
Last updated : 30/11/2022
See also
Nightmares
Sleep disorders
Snoring treatment
Licenses
Medicom LLC
(Udarnikov Avenue)
Medicom LLC
(Vyborgskoye Highway)
Medi Len LLC
(Marshal Zakharov St.)
MediProf LLC
avenue)
Medi Prof LLC
(Malaya Balkanskaya St.)
Go to the license section Go to the legal information section
record from website DISCOUNT 10%
Enrollment is only possible through the contact center.
To register, fill out the form below and you will be contacted.
By clicking on the button, you consent to the processing of your personal data by
nine0003
You are enrolling:
Clinic: {{department}}
Specialty: {{specialty}}
Doctor: {{doctor}}
Date and time: {{form.date | setTime(form.time) | dateTimeFormatted}}
Date of birth: {{age | dateFormatted}}
{{appointmentReply}}
By clicking "Sign up", I accept the terms of the user agreement, the provisions on the protection of personal data and give my consent to the processing of personal data. nine0003
In order to pass the mandatory registration, you must come to the registration desk 10 minutes before your appointment with your passport.
If the patient is a minor (children under 18), it is mandatory to be accompanied by one of the parents with the presentation of his passport and birth certificate of the child.
Relatives and third parties accompanying a minor must have a notarized consent of the parents or legal representatives.
If you have booked an appointment with a coloproctologist, please read the information about preparing for an appointment
The price of the consultation includes:
History taking, preliminary diagnosis and examination appointment. All additional doctor's manipulations at the appointment are paid according to the price list.
If you change your mind, please unsubscribe from the appointment by phone +7 (812) 435-55-55
The price of the consultation includes:
History taking, preliminary diagnosis and examination appointment. All additional doctor's manipulations at the appointment are paid according to the price list. nine0003
If you change your mind, please unsubscribe from the appointment using your Personal Account or by phone +7 (812) 435-55-55.
Are you sure you want to stop recording?
If you have any questions, call us at +7 (812) 435-55-55
Are you sure you want to change the current entry?
If you have any questions, call us at +7 (812) 435-55-55
You are subject to some restrictions on online booking. nine0003
nine0003
Appointment possible via contact center.
You can sign up by phone +7 (812) 435-55-55
The specialist does not see patients of the specified age. To register please fill out the form below and you will be contacted.
Make an appointment
Would you like us to call you
?
Name Telephone
By clicking on the button, you consent
to process their personal data
You will be contacted to confirm your application.
Making an appointment
Preliminary appointment through the site
Our employee will contact you to confirm the appointment with a specialist
By clicking on the button, you consent to the processing of your personal data by
Learn more about quality assurance of medical services
Would you like us to call you
?
By clicking on the button, you consent to the processing of your personal data by
Leave a request and our specialist
will select a convenient time for a communication session with a doctor
By clicking on the button, you consent to the processing of your personal data by
Screenshot of a review from Yandex. Maps*
Maps*
By clicking on the button, you consent to the processing of your personal data by
Sign up
for a consultation
Choose a clinic 1st. Marshal Zakharov, house 20Vyborg highway, house 17, bldg. 1
By clicking on the button, you consent
to process their personal data
Learn more about the quality assurance of medical services
Appointment for tests
Preliminary appointment through the site
Our employee will contact you to confirm the appointment with a specialist
By clicking on the button, you consent to the processing of your personal data by
Write to manager
customer support services SM-Clinic
By clicking on the button, you consent to the processing of your personal data by
We use cookies.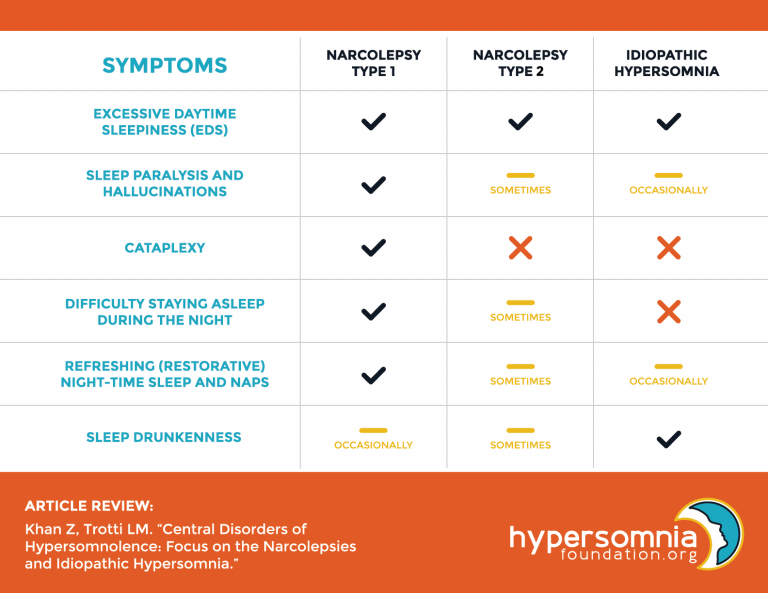 This allows us to analyze the interaction of visitors with the site and make it better. By continuing to use the site, you agree to the use of cookies.
This allows us to analyze the interaction of visitors with the site and make it better. By continuing to use the site, you agree to the use of cookies.
To accept
Migraine and sleep
Migraine is a chronic disease with a long course of many years, which is associated with a significant burden of this disease. According to data from the Burden of Most Common Diseases study, migraine ranks sixth in terms of the number of years lived with maladaptation [1]. At the same time, in combination with other common headaches (tension headache — TTH, drug-induced headache), it already ranks third in this indicator [1]. The burden of this disease is due not only to episodic seizures, but also to disorders closely associated with this disease, many of which are considered comorbid and are of independent importance in terms of both clinical symptom formation and the choice of treatment strategies. nine0003
Among the disorders associated with migraine, sleep disturbances are among the most common. Sleep disorders and migraine are very common conditions in the population, but their relationship is undoubtedly closer than their random occurrence in one patient.
Sleep disorders and migraine are very common conditions in the population, but their relationship is undoubtedly closer than their random occurrence in one patient.
The close relationship between migraine headache and sleep has long been discussed. One of the first descriptions of the connection between migraine attacks and sleep belongs to the English doctor E. Liveing [2], who in 1873 first described the effect of sleep on headache relief. Observations of patients show that in most of them, a violation of the usual sleep pattern (insufficient or excessive sleep duration, jet lag) can provoke a headache. For example, excessive sleep on certain days is naturally accompanied by a severe migraine attack - a phenomenon known as "weekend migraine" [3]. nine0003
Long-term sleep disorders significantly affect the course of migraine. For example, the study of the factors leading to the transformation of episodic migraine into a chronic form revealed that the presence of long-term sleep disorders and subjective dissatisfaction with nighttime sleep are the most important factors responsible for the chronicity of migraine [4].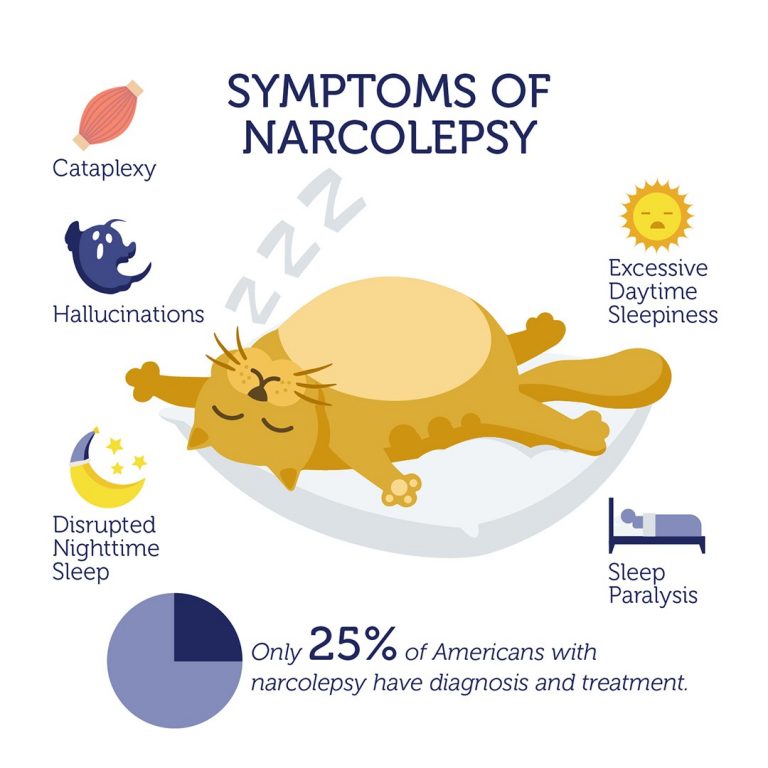 At the same time, adequate treatment of insomnia in such patients, including the use of sleep hygiene strategies, can contribute to the reverse transformation of chronic migraine into episodic. It is known that migraine and sleep disorders are often accompanied by anxiety and depression and are naturally provoked by stress factors. Among patients with migraine, 24–42% experience migraine attacks, almost exclusively associated with sleep or upon awakening, which determines many of the features of the manifestations of the disease in this category of patients [5]. nine0003
At the same time, adequate treatment of insomnia in such patients, including the use of sleep hygiene strategies, can contribute to the reverse transformation of chronic migraine into episodic. It is known that migraine and sleep disorders are often accompanied by anxiety and depression and are naturally provoked by stress factors. Among patients with migraine, 24–42% experience migraine attacks, almost exclusively associated with sleep or upon awakening, which determines many of the features of the manifestations of the disease in this category of patients [5]. nine0003
Among the sleep disorders associated with migraine headache, the most common in clinical practice are insomnia, parasomnia, restless legs syndrome (RLS), and bruxism. Despite the existence of data on reciprocal relationships between migraine and most of these disorders [6], their nature remains not fully understood.
Migraine and insomnia
Almost 1/3 of the world's population complains of insomnia [7]. According to the International Classification of Sleep Disorders II (ICSD-II, 2006), insomnia is a clinical syndrome characterized by recurring disturbances in the initiation, duration, consolidation, or quality of sleep that occur despite sufficient time and conditions for sleep and are manifested by disruption of daytime activities [ 7]. The absolute duration (number of hours) of sleep is not critical, since the normal (sufficient) duration of sleep can vary greatly from person to person. The causes of insomnia can be different: severe overwork, too bright and noisy rooms, poor sleep hygiene, somatic diseases, acute and chronic pain syndromes, anxiety, depression and other mental disorders. In some cases, the idiopathic nature of insomnia is considered, possibly associated with the presence of a genetic predisposition. Shift work and jet lag also have a negative impact on sleep patterns. Clinical observations of patients with migraine show that complaints of difficulty falling asleep, frequent awakenings in the middle of the night and superficial sleep are very common, especially in patients with a long course of the disease.
According to the International Classification of Sleep Disorders II (ICSD-II, 2006), insomnia is a clinical syndrome characterized by recurring disturbances in the initiation, duration, consolidation, or quality of sleep that occur despite sufficient time and conditions for sleep and are manifested by disruption of daytime activities [ 7]. The absolute duration (number of hours) of sleep is not critical, since the normal (sufficient) duration of sleep can vary greatly from person to person. The causes of insomnia can be different: severe overwork, too bright and noisy rooms, poor sleep hygiene, somatic diseases, acute and chronic pain syndromes, anxiety, depression and other mental disorders. In some cases, the idiopathic nature of insomnia is considered, possibly associated with the presence of a genetic predisposition. Shift work and jet lag also have a negative impact on sleep patterns. Clinical observations of patients with migraine show that complaints of difficulty falling asleep, frequent awakenings in the middle of the night and superficial sleep are very common, especially in patients with a long course of the disease. On the other hand, there is evidence that highlights the apparent impact of the sleep-wake cycle on the course of migraine. So, M. Peres et al. [8] conducted a study evaluating the course of episodic and chronic migraine in 200 patients, which revealed that in 46.5% of cases there was a regular occurrence of migraine attacks after a change in sleep patterns. At the same time, migraine attacks on the background of sleep disturbances developed significantly more often in patients with a chronic variant of the course of the disease. nine0003
On the other hand, there is evidence that highlights the apparent impact of the sleep-wake cycle on the course of migraine. So, M. Peres et al. [8] conducted a study evaluating the course of episodic and chronic migraine in 200 patients, which revealed that in 46.5% of cases there was a regular occurrence of migraine attacks after a change in sleep patterns. At the same time, migraine attacks on the background of sleep disturbances developed significantly more often in patients with a chronic variant of the course of the disease. nine0003
The prevalence of insomnia in patients with migraine, according to different authors, varies from 21 to 69% [7]. In a population study by I. Morgan et al. [9] used the Pittsburgh Sleep Quality Index (PSQI) and the WHO Quality of Life Questionnaire in patients with migraine compared with controls. The study showed that approximately 14% of patients experienced migraine attacks. Among them, 42.8% had insufficient sleep duration (less than 7 hours), 28. 3% had prolonged episodes of daytime falling asleep (more than 30 minutes), 393% complained of increased daytime sleepiness and 42.8% noted low sleep efficiency (less than 65%), which significantly distinguished them from healthy controls.
3% had prolonged episodes of daytime falling asleep (more than 30 minutes), 393% complained of increased daytime sleepiness and 42.8% noted low sleep efficiency (less than 65%), which significantly distinguished them from healthy controls.
Many researchers note that, in general, patients suffering from migraine have a significantly reduced quality of life. S. Seidel et al. [10] surveyed 500 patients with migraine and their families as part of a large population-based PAMINA study. All participants in the study had no neurological disorders and changes on MRI and CT of the brain. Sleep quality (PSQI) and daytime sleepiness were assessed using the Epworth Sleepiness Scale (ESS), and data from the Depression and Anxiety Scale were analyzed. The results of the study showed that patients with prolonged migraine headaches experience sleep disturbances, including insufficient sleep duration, the duration of falling asleep, sleep dissatisfaction, the presence of daytime sleepiness, nightmares, compared with the control group. Among these disorders, one of the most severe is the decrease in the level of wakefulness during the daytime. Complaints about daytime sleepiness are often noted by patients with Parkinson's disease, epilepsy, emotional and affective disorders, with depression this figure reaches 57.1% [11]. Excessive daytime sleepiness maladjusts patients, affecting their quality of life, often episodes of drowsiness are imperative and are combined with attention deficit. The prevalence of daytime sleepiness in the general population ranges from 10–20% [12]. It is known that about 25% of migraine patients experience severe drowsiness in various phases of an attack [12]. Excessive daytime sleep is also characteristic of patients with chronic migraine and serves as a factor in its chronicity [13]. In a study by J. Kim et al. [14] analyzed 2695 patients aged 19 to 69 years, among whom 143 (5.3%) experienced migraine attacks. The patients were followed up for a year. Excessive daytime sleepiness predominated in the migraine group (19.
Among these disorders, one of the most severe is the decrease in the level of wakefulness during the daytime. Complaints about daytime sleepiness are often noted by patients with Parkinson's disease, epilepsy, emotional and affective disorders, with depression this figure reaches 57.1% [11]. Excessive daytime sleepiness maladjusts patients, affecting their quality of life, often episodes of drowsiness are imperative and are combined with attention deficit. The prevalence of daytime sleepiness in the general population ranges from 10–20% [12]. It is known that about 25% of migraine patients experience severe drowsiness in various phases of an attack [12]. Excessive daytime sleep is also characteristic of patients with chronic migraine and serves as a factor in its chronicity [13]. In a study by J. Kim et al. [14] analyzed 2695 patients aged 19 to 69 years, among whom 143 (5.3%) experienced migraine attacks. The patients were followed up for a year. Excessive daytime sleepiness predominated in the migraine group (19. 6%), with a prevalence of 13.4% in the non-migraine headache group and 9.4% in the control group. After analyzing the results of the study, the authors concluded that patients with migraine are more likely than in the control group to have poor sleep quality, impaired sleep initiation, a decrease in its duration, as well as excessive daytime sleepiness, especially in the subgroup with high (more than 10 once a month) frequency of migraine attacks and higher intensity (visual analogue scale) headache. nine0003
6%), with a prevalence of 13.4% in the non-migraine headache group and 9.4% in the control group. After analyzing the results of the study, the authors concluded that patients with migraine are more likely than in the control group to have poor sleep quality, impaired sleep initiation, a decrease in its duration, as well as excessive daytime sleepiness, especially in the subgroup with high (more than 10 once a month) frequency of migraine attacks and higher intensity (visual analogue scale) headache. nine0003
According to the results of the study [15], patients who had migraine attacks occurred predominantly at night differed in a number of clinical signs from patients who experienced predominantly daytime attacks. When analyzing the polysomnographic characteristics of patients with migraine, a characteristic pattern was revealed — often the onset of headache attacks coincided with the REM sleep phase (REM) or with the transition from REM to non-REM sleep [16]. Along with this, such patients showed a decrease in the duration of FBS in general and especially on the night preceding the morning development of a migraine attack. The pattern of polysomnographic characteristics in different phases of the disease is also interesting. R. Goder et al. [17] showed a significant decrease in the number of nocturnal awakenings and motor activity, a reduction in the power of the beta rhythm in deep sleep and the alpha rhythm in the first phase of FBS in the pre-attack period. Many authors interpret the results obtained as neurophysiological correlates of a decrease in cortical activity on the night before a migraine attack. In the post-attack period, patients with migraine often have vivid, dramatic dreams, which are often frightening in nature, although it is known that dreams with such plots do not serve as triggers for migraine attacks. nine0003
The pattern of polysomnographic characteristics in different phases of the disease is also interesting. R. Goder et al. [17] showed a significant decrease in the number of nocturnal awakenings and motor activity, a reduction in the power of the beta rhythm in deep sleep and the alpha rhythm in the first phase of FBS in the pre-attack period. Many authors interpret the results obtained as neurophysiological correlates of a decrease in cortical activity on the night before a migraine attack. In the post-attack period, patients with migraine often have vivid, dramatic dreams, which are often frightening in nature, although it is known that dreams with such plots do not serve as triggers for migraine attacks. nine0003
Migraine and parasomnias
Parasomnias are unusual forms of behavior or sensations that occur during sleep (from Greek para - about; Lat. somnus - sleep) [7]. The International Classification of Sleep Disorders [18] identifies three groups of parasomnias: those associated with slow sleep (sleepwalking, night terrors, night eating syndrome), associated with REM sleep (sleep paralysis, nightmares, REM sleep behavior disorders) and others (syndrome " exploding head" - SVG, sleep hallucinations, nocturnal enuresis).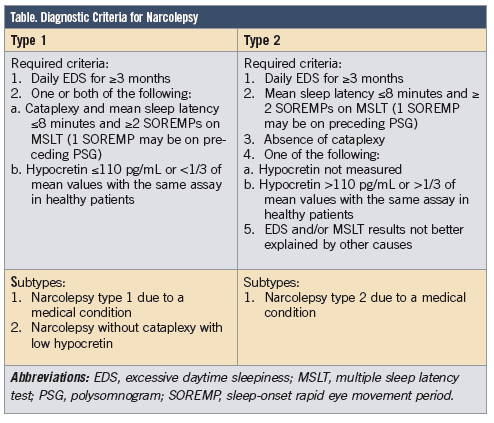 In patients with migraine cephalgia as a whole, more often than in the population, cases of enuresis, sleep-talking, sleepwalking, night terrors are detected. These patterns are shown in prospective observations of children in specialized headache clinics. O. Bruni et al. [nineteen] revealed that in patients with migraine, phenomena such as sleep-talking, snoring and nightmares are significantly more common than in the control group.
In patients with migraine cephalgia as a whole, more often than in the population, cases of enuresis, sleep-talking, sleepwalking, night terrors are detected. These patterns are shown in prospective observations of children in specialized headache clinics. O. Bruni et al. [nineteen] revealed that in patients with migraine, phenomena such as sleep-talking, snoring and nightmares are significantly more common than in the control group.
U. Isik et al. [20] conducted a population-based study among schoolchildren aged 6–13 years, the results of which fully confirmed that among children with migraine, the most common types of parasomnias are snoring, nightmares, somnabulism, sleep talking and vocalization in sleep. In the study by M. Zarowski et al. [21] examined 150 children with episodic migraine, 150 with episodic TTH, and 284 without complaints of headaches (control group). After analyzing the results, the authors came to the conclusion that parasomnias are much more common in the group with headache compared to healthy people, while there was no significant difference in groups with migraine and TTH. nine0003
nine0003
SVG is one of the rather rare forms of parasomnia, characterized by the sensation of a loud noise in the head before going to sleep. For the first time, the nocturnal phenomenon was described in 1920 as a noise similar to a strong explosion emanating from the head, due to which in 1988 in the work of J. Pearse [22], where 50 clinical cases were described in patients with similar nocturnal conditions, the syndrome received the appropriate name. SVG is characterized by the appearance of loud noises during the transitions of various stages of sleep and upon awakening. Although the episodes do not pose a threat to the health of the patient, this frightening phenomenon can lead to clinical consequences. In some cases, CHD is mild, but more often, episodes of CHD cause patients to be very anxious and fearful, as many regard them as a sign of a stroke. In a number of clinical cases described, the noises were characterized as “shotgun shots” or “bomb explosions”, when, along with a loud sound, patients described flashes of bright light, which immediately caused awakening. nine0003
nine0003
The occurrence of attacks of SVH can occur in a series over several nights, then for several weeks or months this condition does not bother, and the patient does not feel any consequences. Seizures may be characterized by muscle twitches or convulsions. Usually, all these sensations are not painful, but in some cases, patients report an acute attack of pain in the head area. The study by R. Evans [23] describes the occurrence of SVH attacks on the night preceding a typical migraine attack, which in this case was regarded by the author as a migraine aura. Currently, there are no clear data on the prevalence of the disease and the frequency of episodes in the population. It was previously thought that CVS is rare, mainly in patients older than 50 years, predominantly in women [22]. And although large-scale population studies have not been conducted, B. Sharpless [24] analyzed the prevalence of CVS among students. 211 verified cases of SVH were identified, which accounted for 18. 0% of the study population. In these patients, episodes of head bloating were accompanied by severe fear, although it was clinically significant only in 2.80% of cases. This study showed that CVS is significantly more common than previously thought, and even at a young age. nine0003
0% of the study population. In these patients, episodes of head bloating were accompanied by severe fear, although it was clinically significant only in 2.80% of cases. This study showed that CVS is significantly more common than previously thought, and even at a young age. nine0003
Migraine and sleep movement disorders
One of the most challenging aspects of migraine comorbidity is its association with temporomandibular joint dysfunction (TMJD). TMD is an umbrella term that summarizes various clinical syndromes involving the muscles of mastication, the temporomandibular joint, and related structures. Among these syndromes, sleep bruxism plays a special role in migraine, especially in childhood. Bruxism is regarded as an important factor in the initiation and persistence of pain in TMD [25]. It is usually divided into bruxism sleep and wakefulness. nine0003
Sleep bruxism is defined as masticatory muscle activity accompanied by clenching of teeth and characteristic grinding that occurs predominantly during non-REM sleep. The prevalence of sleep bruxism reaches 14% in children, 8% in middle-aged adults, and only 3% in the elderly [26]. In 2/3 of cases, sleep bruxism, which begins in childhood, persists in adults. It is assumed that various factors may be involved in its origin: stressful life events, personality traits, the presence of anxiety, frequent awakenings in a dream, genetic predisposition, changes in dopaminergic and serotonergic neurotransmission, as well as recreational factors (smoking, coffee abuse). Bruxism that occurs without specific causes is called primary or idiopathic. Forms of bruxism associated with other diseases (for example, Parkinson's disease), with the use of psychotropic drugs (antidepressants of the group of selective serotonin reuptake inhibitors or neuroleptics), are defined as secondary bruxism. nine0003
The prevalence of sleep bruxism reaches 14% in children, 8% in middle-aged adults, and only 3% in the elderly [26]. In 2/3 of cases, sleep bruxism, which begins in childhood, persists in adults. It is assumed that various factors may be involved in its origin: stressful life events, personality traits, the presence of anxiety, frequent awakenings in a dream, genetic predisposition, changes in dopaminergic and serotonergic neurotransmission, as well as recreational factors (smoking, coffee abuse). Bruxism that occurs without specific causes is called primary or idiopathic. Forms of bruxism associated with other diseases (for example, Parkinson's disease), with the use of psychotropic drugs (antidepressants of the group of selective serotonin reuptake inhibitors or neuroleptics), are defined as secondary bruxism. nine0003
Teeth grinding during sleep can lead to abrasion of tooth enamel, grinding of teeth, malocclusion, dysfunction and pain in the joint area, hypertrophy of masticatory muscles and their soreness. Pain is usually bilateral, symmetrical and localized in 84.3% of cases in the face, in 67.1% of patients in the frontotemporal region of the head [25]. Sleep bruxism is most common in children with a history of episodic migraine attacks. The prevalence of craniomandibular pain is about 66% in patients with sleep bruxism [25]. In 2014, in a study conducted by A. Masuko et al. [27], found a high prevalence of sleep bruxism in children with episodic migraine compared with the control group (25% versus 0%). Sleep bruxism and migraine are periodic conditions, and their comorbidity may be due to common pathophysiological mechanisms, in particular autonomic dysfunction with sympathetic activation and a decrease in the activity of the dopaminergic system, which is characteristic of both conditions [27]. nine0003
Pain is usually bilateral, symmetrical and localized in 84.3% of cases in the face, in 67.1% of patients in the frontotemporal region of the head [25]. Sleep bruxism is most common in children with a history of episodic migraine attacks. The prevalence of craniomandibular pain is about 66% in patients with sleep bruxism [25]. In 2014, in a study conducted by A. Masuko et al. [27], found a high prevalence of sleep bruxism in children with episodic migraine compared with the control group (25% versus 0%). Sleep bruxism and migraine are periodic conditions, and their comorbidity may be due to common pathophysiological mechanisms, in particular autonomic dysfunction with sympathetic activation and a decrease in the activity of the dopaminergic system, which is characteristic of both conditions [27]. nine0003
The term "restless leg syndrome" (RLS) was introduced by K. Ekbom in 1954 [28] to describe a sensorimotor disorder characterized by a strong, poorly controlled need to move the limbs. Unpleasant sensations in the extremities appear with a long stay in immobility, for example, in bed, in a sitting position. A characteristic feature of the RLS is the confinement to the evening and night time. Such unpleasant sensations force the patient to make relief movements and often lead to sleep disturbance and social disadaptation, affecting the quality of life in general [29].]. Sleep disturbances associated with this phenomenon in the form of difficulty falling asleep and frequent awakenings in the middle of the night are extremely pronounced in patients with RLS. Violation of the quality of night sleep is accompanied by drowsiness and fatigue in the daytime. Despite the fact that the name of the syndrome includes the lower extremities, in 21–57% of cases, similar sensations are described in the hands [29]. The prevalence of episodic RLS in the general population is 5–10%, with women suffering twice as often as men [29]. In certain categories of patients, the prevalence of RLS is even higher.
Unpleasant sensations in the extremities appear with a long stay in immobility, for example, in bed, in a sitting position. A characteristic feature of the RLS is the confinement to the evening and night time. Such unpleasant sensations force the patient to make relief movements and often lead to sleep disturbance and social disadaptation, affecting the quality of life in general [29].]. Sleep disturbances associated with this phenomenon in the form of difficulty falling asleep and frequent awakenings in the middle of the night are extremely pronounced in patients with RLS. Violation of the quality of night sleep is accompanied by drowsiness and fatigue in the daytime. Despite the fact that the name of the syndrome includes the lower extremities, in 21–57% of cases, similar sensations are described in the hands [29]. The prevalence of episodic RLS in the general population is 5–10%, with women suffering twice as often as men [29]. In certain categories of patients, the prevalence of RLS is even higher.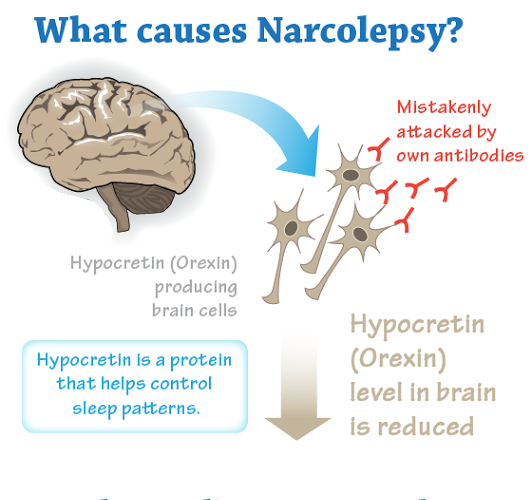 Among pregnant women, RLS occurs 2-3 times more often than in the general population, and in patients with renal insufficiency - 2-4 times more often. The disease usually begins in the 4th or 5th decade of life. The occurrence of RLS in the elderly is characterized by a high rate of progression and a more severe course of the disease. nine0003
Among pregnant women, RLS occurs 2-3 times more often than in the general population, and in patients with renal insufficiency - 2-4 times more often. The disease usually begins in the 4th or 5th decade of life. The occurrence of RLS in the elderly is characterized by a high rate of progression and a more severe course of the disease. nine0003
Several epidemiological studies have shown a strong association of RLS with migraine compared not only with the general population, but also with prevalence among patients with other primary headaches [30–32]. At the same time, there is a clear relationship between the severity of RLS symptoms, the frequency of migraine attacks and the quality of sleep in these patients, which was demonstrated in a special study by P. Chen et al. [32]. Based on the results of clinical observations and experimental studies, a point of view was expressed about the existence of a possible pathogenetic relationship between RLS and migraine. Thus, it is known that iron deficiency is an established cause of secondary RLS, the severity of which decreases with replenishment of iron levels. Special MRI techniques demonstrate a decrease in the iron content in the substantia nigra in patients with early onset RLS, the degree of which correlates with the severity of the disease [32]. On the other hand, there are data indicating that iron metabolism disorders may underlie the pathogenesis of migraine, which was demonstrated in a neuroimaging study by M. Kruit et al. [33]. nine0003
Special MRI techniques demonstrate a decrease in the iron content in the substantia nigra in patients with early onset RLS, the degree of which correlates with the severity of the disease [32]. On the other hand, there are data indicating that iron metabolism disorders may underlie the pathogenesis of migraine, which was demonstrated in a neuroimaging study by M. Kruit et al. [33]. nine0003
Pathophysiology of the relationship between migraine and sleep disorders
The problem of the relationship between migraine and sleep disorders is becoming increasingly important, given the results of recent studies that have revealed new aspects of this association [34-36]. Although basic research in this area is preliminary, there is clear clinical evidence linking the mechanisms of initiation and maintenance of sleep and headaches, including migraine, cluster headache, hypnic headache, obstructive sleep apnea syndrome headache, and some other forms of cephalalgia. nine0003
nine0003
Discussion of the neurobiological basis of the relationship between migraine and sleep disorders involves considering both the neuroanatomical commonality of the mechanisms of trigeminal noci- and antinociception and the functioning of somnogenic systems, but also the role of neurotransmitter and neurohormonal systems in the formation of a close association of migraine headache with sleep disorders.
The processes of sleep formation and the trigeminal nociceptive system share some common mechanisms regarding neurotransmission and the functions of various brain regions. Trigeminal afferents in the first branch of the trigeminal nerve innervate the intracranial vessels and dura and converge on the trigeminal caudal nucleus (TCN) in the brain stem. Another important system that has projections to the TCO is the posteromedial thalamus, and some afferents from the TCO project to the limbic and insular regions of the brain. These systems play a key role in the formation of migraine headache. All of these afferents from the TCO travel through the midbrain and interact closely with nuclei in the brain stem and midbrain. In addition, TCO also has direct connections to the hypothalamus via specific neurons. There are also collaterals to the nuclei of the solitary tract and parabrachial nuclei. These structures are the main control centers of viscerosensory and are involved in cardiovascular, respiratory and gastrointestinal processes. They interact through these collaterals with other autonomic functions such as sleep, wakefulness, sympathetic and parasympathetic (eg pupillary responses, secretory functions) and neuroendocrine functions. Based on these neuroanatomical premises, it becomes clear that pain processing can be modulated through these circuits through autonomic/autonomic symptoms and reflex mechanisms. Therefore, changes in autonomic homeostasis (for example, during sleep) can alleviate or suppress pain at these levels, including in migraine [37]. nine0003
All of these afferents from the TCO travel through the midbrain and interact closely with nuclei in the brain stem and midbrain. In addition, TCO also has direct connections to the hypothalamus via specific neurons. There are also collaterals to the nuclei of the solitary tract and parabrachial nuclei. These structures are the main control centers of viscerosensory and are involved in cardiovascular, respiratory and gastrointestinal processes. They interact through these collaterals with other autonomic functions such as sleep, wakefulness, sympathetic and parasympathetic (eg pupillary responses, secretory functions) and neuroendocrine functions. Based on these neuroanatomical premises, it becomes clear that pain processing can be modulated through these circuits through autonomic/autonomic symptoms and reflex mechanisms. Therefore, changes in autonomic homeostasis (for example, during sleep) can alleviate or suppress pain at these levels, including in migraine [37]. nine0003
The antinociceptive system (ie the descending pain control system) plays a very important role in the complex relationship between pain and sleep. In the lower parts of the trunk at the level of the bridge, three structures can be identified that project, for example, to the posterior horn and reduce pain activation at the spinal level and the level of TCO: 1) rostroventromedial medulla oblongata; 2) serotonergic raphe nuclei; 3) noradrenergic blue spot [38]. The other most important antinociceptive structure is the periaqueductal gray matter (PGR), which is associated with the previously mentioned antinociceptive structures. OSV is involved not only in nociception, but also in the regulation of autonomic functions such as blood pressure and heart rate. The ventrolateral part of the SSV is perhaps the most important anatomical region that can be considered as a link between migraine headache and somnogenic systems. The ventrolateral OSV is activated by the orexin system and can cause REM sleep to be turned off. Moreover, orexins can stimulate neurons in the ventrolateral part of the SV that inhibit antinociceptive activity in the TCO (i.
In the lower parts of the trunk at the level of the bridge, three structures can be identified that project, for example, to the posterior horn and reduce pain activation at the spinal level and the level of TCO: 1) rostroventromedial medulla oblongata; 2) serotonergic raphe nuclei; 3) noradrenergic blue spot [38]. The other most important antinociceptive structure is the periaqueductal gray matter (PGR), which is associated with the previously mentioned antinociceptive structures. OSV is involved not only in nociception, but also in the regulation of autonomic functions such as blood pressure and heart rate. The ventrolateral part of the SSV is perhaps the most important anatomical region that can be considered as a link between migraine headache and somnogenic systems. The ventrolateral OSV is activated by the orexin system and can cause REM sleep to be turned off. Moreover, orexins can stimulate neurons in the ventrolateral part of the SV that inhibit antinociceptive activity in the TCO (i. e., facilitate trigeminal nociception) [39]. These findings are consistent with clinical observational data on the onset of migraine-like headaches upon stimulation of SSV [38].
e., facilitate trigeminal nociception) [39]. These findings are consistent with clinical observational data on the onset of migraine-like headaches upon stimulation of SSV [38].
The hypothalamus, containing orexinergic neurons, is the central structure involved in the mechanisms of both the formation of migraine headache and the generation and maintenance of sleep. These neurons have projections to the RCB and may also be an anatomical and physiological substrate for the association between headache and sleep. The hypothalamus is considered as a complex structure that regulates the activity of the underlying centers that perform homeostatic functions. But the most important part of the hypothalamus involved in nociception is its ventrolateral part. It is known that the application of opioids to this part of the hypothalamus can cause deep analgesia [40], therefore, neurostimulation of this area is useful for alleviating cluster headache [41]. The posterior hypothalamus and areas adjacent to the hypothalamus are surrounded by neurons containing orexins [42]. These neurons are involved in both antinociception processes and mechanisms of sleep disorders such as narcolepsy. In general, it can be assumed that dysfunction of the hypothalamic systems contributes not only to impaired sleep-wake function, but also to impaired pain processing through orexinergic neurons. nine0003
These neurons are involved in both antinociception processes and mechanisms of sleep disorders such as narcolepsy. In general, it can be assumed that dysfunction of the hypothalamic systems contributes not only to impaired sleep-wake function, but also to impaired pain processing through orexinergic neurons. nine0003
Orexins, A and B are neuropeptides synthesized exclusively in the hypothalamus [43]. It has been suggested that orexins are involved in the transition from episodic to chronic migraine, as they regulate numerous neuroendocrine functions and autonomic processes such as obesity, as well as drug abuse and other forms of addictive behavior [43]. Moreover, orexinergic activity in the ventrolateral SSV can be blocked by a 5-HT1B/1D receptor antagonist and provoke migraine attacks. On the other hand, this suggests that it is possible that triptans may influence the sleep-wake cycle and autonomic functions that are regulated by orexins. Sleep is mainly induced by the suppression of the activity of the above structures. The main component of this system is projections from the ventrolateral preoptic hypothalamus to the raphe nuclei and the locus coeruleus. Inhibitory transmitters such as GABA and galanin act in these projections [44]. The main sleep-inducing molecule is adenosine, which accumulates during the day and activates the ventrolateral preoptic hypothalamus [45]. This mechanism is called the homeostatic sleep drive. Another mechanism that induces sleep is the endogenous circadian sleep drive, which occurs in the suprachiasmatic nucleus (SCN) of the hypothalamus and is modulated by retinal currents during the day and melatonin production by the pineal gland at night [3]. SCN is indirectly related to other sleep-regulating centers in the hypothalamus. Moreover, SCN is also associated with hypothalamic control centers for autonomic functions such as thermoregulation and endogenous steroid homeostasis [3]. nine0003
The main component of this system is projections from the ventrolateral preoptic hypothalamus to the raphe nuclei and the locus coeruleus. Inhibitory transmitters such as GABA and galanin act in these projections [44]. The main sleep-inducing molecule is adenosine, which accumulates during the day and activates the ventrolateral preoptic hypothalamus [45]. This mechanism is called the homeostatic sleep drive. Another mechanism that induces sleep is the endogenous circadian sleep drive, which occurs in the suprachiasmatic nucleus (SCN) of the hypothalamus and is modulated by retinal currents during the day and melatonin production by the pineal gland at night [3]. SCN is indirectly related to other sleep-regulating centers in the hypothalamus. Moreover, SCN is also associated with hypothalamic control centers for autonomic functions such as thermoregulation and endogenous steroid homeostasis [3]. nine0003
Melatonin is a specific hormone synthesized from serotonin in the pineal gland. In some chronobiological conditions accompanied by headache, changes in melatonin secretion have been found. For example, in cluster headache, a decrease in both peak and mean levels of melatonin secretion has been shown. These changes are more pronounced during pain bundles [3]. Similar changes have also been found in patients with migraine [46]. In addition, melatonin secretion in migraine patients is more sensitive to light than in the control group [46]. The role of melatonin is confirmed by data from studies of its effectiveness [47]. nine0003
In some chronobiological conditions accompanied by headache, changes in melatonin secretion have been found. For example, in cluster headache, a decrease in both peak and mean levels of melatonin secretion has been shown. These changes are more pronounced during pain bundles [3]. Similar changes have also been found in patients with migraine [46]. In addition, melatonin secretion in migraine patients is more sensitive to light than in the control group [46]. The role of melatonin is confirmed by data from studies of its effectiveness [47]. nine0003
Talk
Thus, although the neurobiological relationship between sleep and migraine headache has not yet been fully elucidated and there is no single concept explaining the patterns of their coexistence, it nevertheless seems possible to discuss several important mechanisms. One of the key factors of this concept is the proximity and functional unity of the structures and systems that provide both the processes of initiation and maintenance of sleep, and the trigeminal noci- and antinociception systems that implement migraine headache.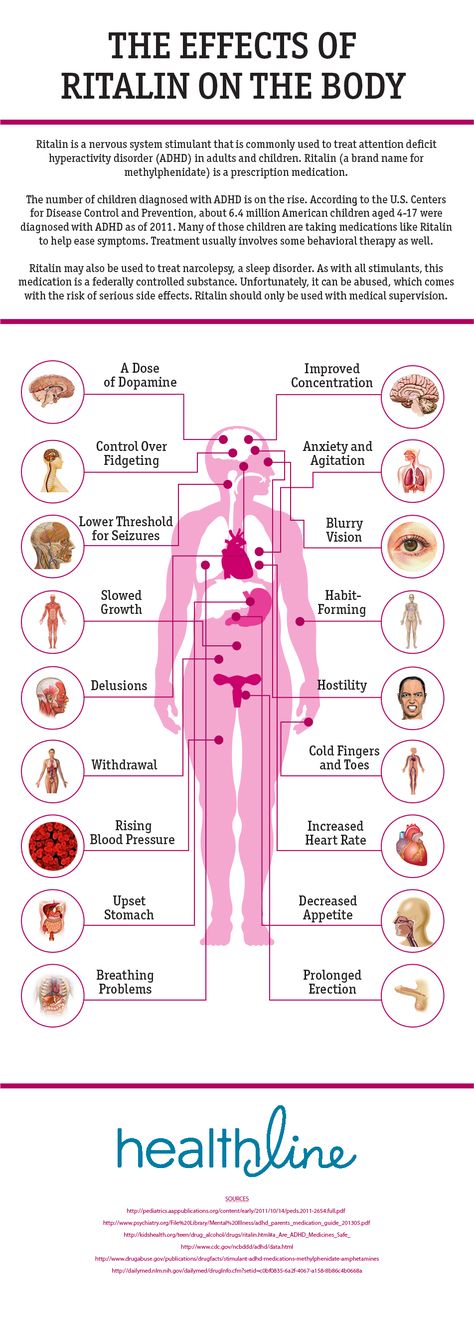 The second important mechanism is a complex of neurotransmitter and neurohormonal systems, which include serotonergic, dopaminergic, noradrenergic, melatonergic, orexinergic, opioidergic mechanisms, etc.
The second important mechanism is a complex of neurotransmitter and neurohormonal systems, which include serotonergic, dopaminergic, noradrenergic, melatonergic, orexinergic, opioidergic mechanisms, etc.
The need to study the pathophysiology of these relationships is dictated by the needs of clinical practice. It is known that sleep disorders and migraine, being comorbid conditions, significantly increase the risk of each other [19, 37]. The coexistence of sleep disorders and headaches not only manifests itself by overlapping clinical manifestations, but also largely determines their natural course and prognosis. High comorbidity with sleep disorders contributes to the transformation of episodic migraine into a chronic, persistent condition, often resistant to modern methods of treatment. To date, there are no specific evidence-based recommendations for the management of these complex patients. Nevertheless, it is clear that patients with migraine complaining of sleep disturbances need, first of all, an adequate diagnosis of the type of headaches in accordance with standard criteria. In case of detection of migraine headache, it is necessary to apply classical approaches to its prevention and relief of attacks. It is extremely important to identify chronic forms of migraine, since the correction of sleep disorders in these cases is an effective treatment strategy and most often allows chronic cephalgia to regress to an episodic form. nine0003
In case of detection of migraine headache, it is necessary to apply classical approaches to its prevention and relief of attacks. It is extremely important to identify chronic forms of migraine, since the correction of sleep disorders in these cases is an effective treatment strategy and most often allows chronic cephalgia to regress to an episodic form. nine0003
Screening questionnaires may be useful for diagnosing sleep disorders, including for the detection of sleep apnea syndrome, which requires specific treatment and avoidance of the use of sedatives and hypnotics. In these patients, it is mandatory to comply with sleep hygiene measures, which is important, among other things, to maintain the individual chronobiological pattern of the sleep-wake cycle, which protects against the effects of factors provoking migraine attacks. Finally, in patients with migraine and persistent complaints of sleep disturbance, clinical assessment of anxiety and depression is important, given the high risk of psychiatric diseases in this category of patients.