Missing a dose of lithium
NAMI: National Alliance on Mental Illness
Download PDF
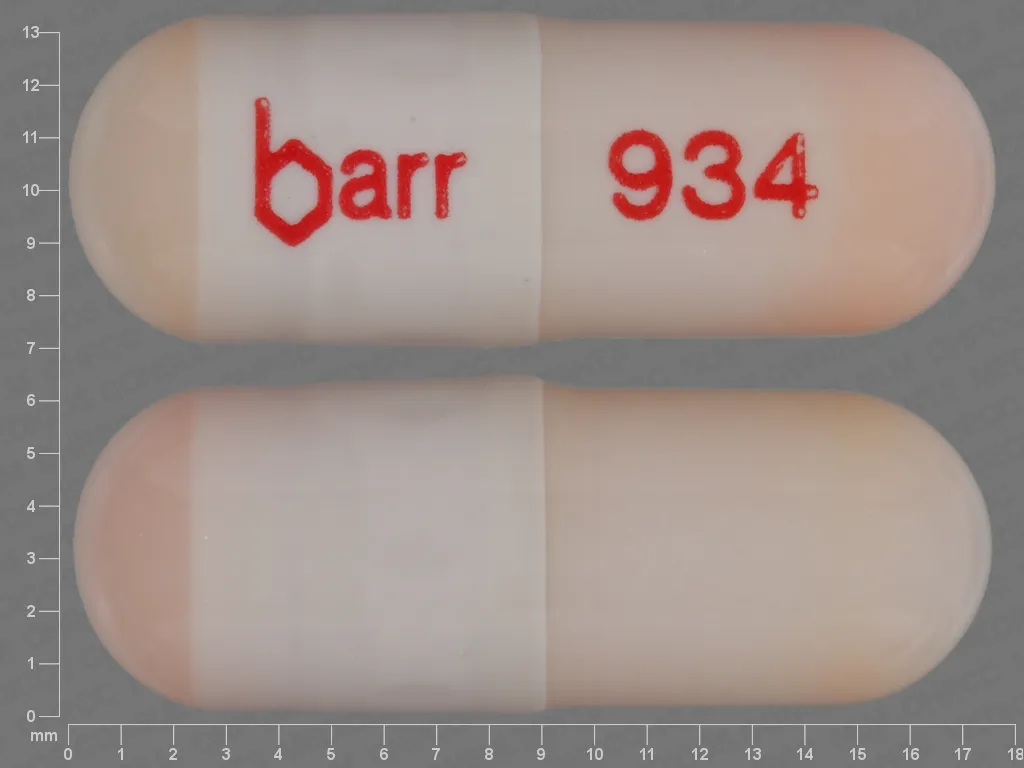
Generic name: lithium (LITH ee um)
- Tablets: 300 mg
- Capsules: 150 mg, 300 mg, 600 mg
- Extended-release tablets: 300 mg, 450 mg
- Oral lithium citrate solution (liquid): 8 mEq/5 mL
Brand names:
- Lithobid®
- Extended-release tablets: 300 mg, 450 mg
- Eskalith®, Eskalith CR®: discontinued
All FDA black box warnings are at the end of this fact sheet. Please review before taking this medication.
What Is Lithium And What Does It Treat?
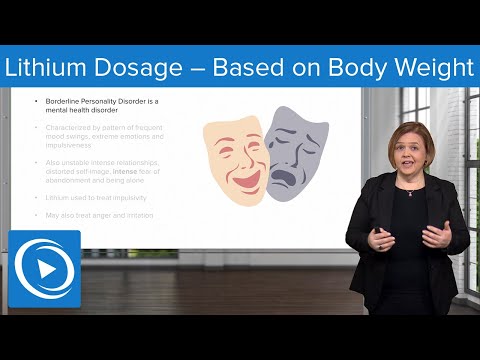
Lithium is a mood stabilizer medication that works in the brain. It is approved for the treatment of bipolar disorder (also known as manic depression). Bipolar disorder involves episodes of depression and/or mania.
Symptoms of depression include:
- Depressed mood — feeling sad, empty, or tearful
- Feeling worthless, guilty, hopeless, or helpless
- Loss of interest or pleasure in normal activities
- Sleep and eat more or less than usual (for most people it is less)
- Low energy, trouble concentrating, or thoughts of death (suicidal thinking)
- Psychomotor agitation (‘nervous energy’)
- Psychomotor retardation (feeling like you are moving in slow motion)
Symptoms of mania include:
- Feeling irritable or “high”
- Having increased self esteem
- Feeling like you don’t need to sleep
- Feeling the need to continue to talk
- Feeling like your thoughts are too quick (racing thoughts)
- Feeling distracted
- Getting involved in activities that are risky or could have bad consequences (e.
g., excessive spending)
Lithium may also be helpful when prescribed “off-label” for depression, especially when combined with antidepressant medications. “Off-label” means that it hasn’t been approved by the Food and Drug Administration for this condition. Your mental health provider should justify his or her thinking in recommending an “off-label” treatment. They should be clear about the limits of the research around that medication and if there are any other options.
What Is The Most Important Information I Should Know About Lithium?
Bipolar disorder requires long-term treatment. Do not stop taking lithium, even when you feel better. With input from you, your health care provider will assess how long you will need to take the medication. Missing doses of lithium may increase your risk for a relapse in your mood symptoms.
Do not stop taking lithium or change your dose without talking to with your health care provider first.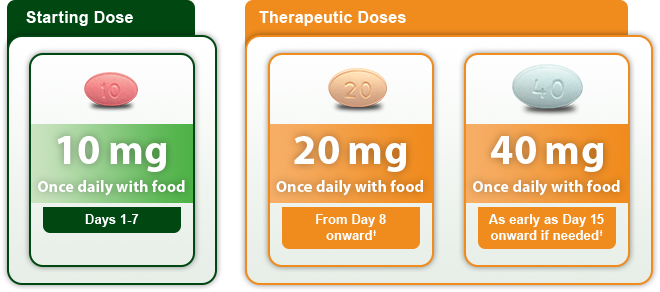
In order for lithium to work properly, it should be taken every day as ordered by your health care provider.
Periodically, your health care provider may ask you to provide a blood sample to make sure the appropriate level of medication is in your body and to assess for side effects, such as changes in blood cell counts or kidney function.
Are There Specific Concerns About Lithium And Pregnancy?
If you are planning on becoming pregnant, notify your health care provider so that he/she can best manage your medications. People living with bipolar disorder who wish to become pregnant face important decisions. It is important to discuss the risks and benefits of treatment with your doctor and caregivers.
Lithium has been associated with an increased risk of Ebstein’s anomaly, a heart valve defect. Even though data suggest that the risk of Ebstein’s anomaly from first trimester use of lithium is very low, an ultrasound of the heart is recommended at 16 to 20 weeks of gestation. Lithium levels should be monitored monthly in early pregnancy and weekly near delivery. Do not stop taking lithium without first speaking to your health care provider. Discontinuing mood stabilizer medications during pregnancy has been associated with a significant increase in symptom relapse.
Lithium levels should be monitored monthly in early pregnancy and weekly near delivery. Do not stop taking lithium without first speaking to your health care provider. Discontinuing mood stabilizer medications during pregnancy has been associated with a significant increase in symptom relapse.
Regarding breastfeeding, caution is advised since lithium does pass into breast milk. In general, breastfeeding is not recommended while taking lithium.
What Should I Discuss With My Health Care Provider Before Taking Lithium?
- Symptoms of your condition that bother you the most
- If you have thoughts of suicide or harming yourself
- Medications you have taken in the past for your condition, whether they were effective or caused any adverse effects
- If you experience side effects from your medications, discuss them with your provider. Some side effects may pass with time, but others may require changes in the medication.
- Any other psychiatric or medical problems you have
- All other medications you are currently taking (including over the counter products, herbal and nutritional supplements) and any medication allergies you have
- Other non-medication treatment you are receiving, such as talk therapy or substance abuse treatment.
 Your provider can explain how these different treatments work with the medication.
Your provider can explain how these different treatments work with the medication. - If you are pregnant, plan to become pregnant, or are breastfeeding
- If you drink alcohol or use illegal drugs
How Should I Take Lithium?
Lithium is usually taken 1-3 times per day with or without food.
Typically patients begin at a low dose of medication and the dose is increased slowly over several weeks.
The dose usually ranges from 600 mg to 1200 mg daily, but some people may require higher doses depending on weight or symptoms. Only your health care provider can determine the correct dose for you.
Extended release tablets: Swallow the tablet whole. Do not crush or chew extended release tablets.
Liquid: Measure with a dosing spoon or oral syringe, which you can get from your pharmacy.
Use a calendar, pillbox, alarm clock, or cell phone alert to help you remember to take your medication. You may also ask a family member a friend to remind you or check in with you to be sure you are taking your medication.
What Happens If I Miss A Dose Of Lithium?
If you miss a dose of lithium, take it as soon as you remember, unless it is closer to the time of your next dose. Discuss this with your healthcare provider. Do not double your dose or take more than what is prescribed.
What Should I Avoid While Taking Lithium?
Avoid drinking alcohol or using illegal drugs while you are taking lithium. They may decrease the benefits (e.g., worsen your condition) and increase adverse effects (e.g., sedation) of the medication.
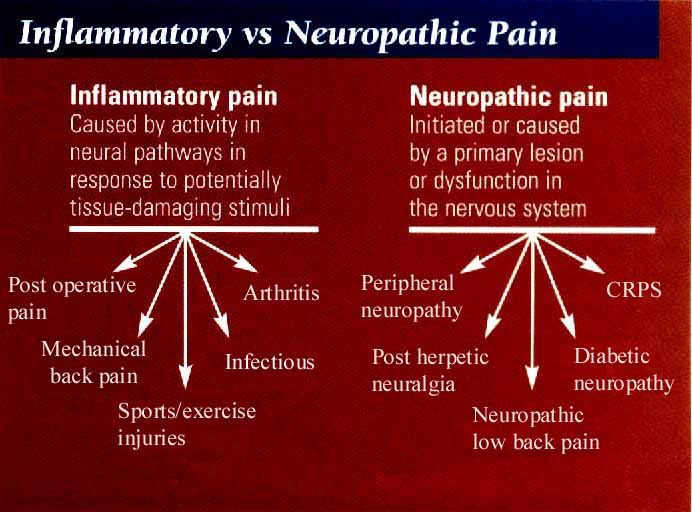
Avoid low sodium diets and dehydration because this can increase the risk of lithium toxicity.
Avoid over the counter and prescription pain medications that contain nonsteroidal anti-inflammatory medications (NSAIDS) such as ibuprofen (Motrin®, Advil®) or naproxen (Aleve®, Naprosyn®) because these medications can increase the risk of toxicity from lithium.
Avoid excessive intake of caffeinated beverages, such as coffee, tea, cola or energy drinks, since these may decrease levels of lithium and decrease effectiveness of the medication. Discontinuing caffeine use may increase lithium levels. Consult your health care provider before reducing or stopping caffeine use.
Discontinuing caffeine use may increase lithium levels. Consult your health care provider before reducing or stopping caffeine use.
What Happens If I Overdose With Lithium?
If an overdose occurs call your doctor or 911. You may need urgent medical care. You may also contact the poison control center at 1-800-222-1222.
A specific treatment to reverse the effects of lithium does not exist, but there are treatments to decrease the effects of the medication. Only a doctor can determine if you require treatment.
What are the possible side effects of lithium?
Common side effects
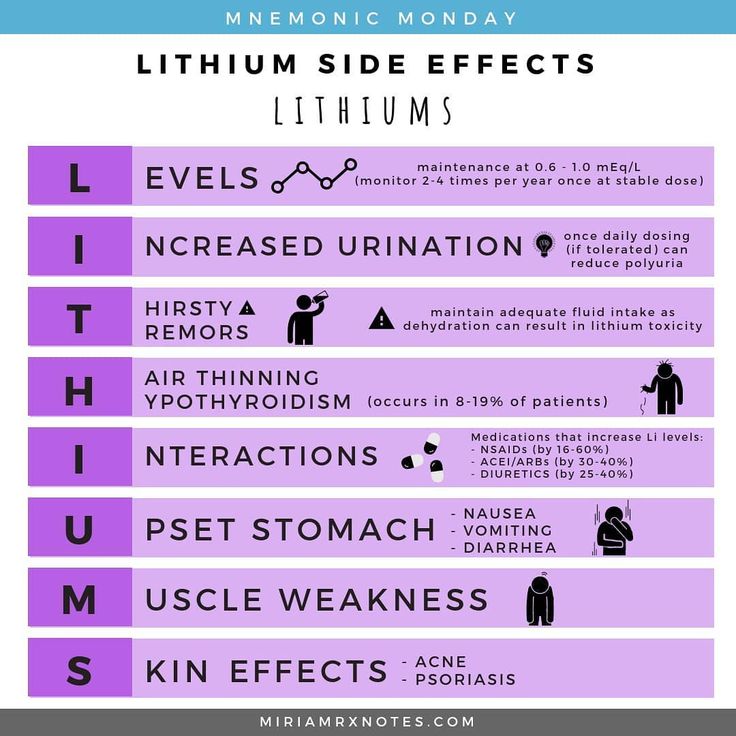
- Headache
- Nausea or vomiting
- Diarrhea
- Dizziness or drowsiness
- Changes in appetite
- Hand tremors
- Dry mouth
- Increased thirst
- Increased urination
- Thinning of hair or hair loss
- Acne-like rash
Rare/serious side effects
Signs of lithium toxicity include severe nausea and vomiting, severe hand tremors, confusion, vision changes, and unsteadiness while standing or walking. These symptoms need to be addressed immediately with a medical doctor to ensure your lithium level is not dangerously high.
These symptoms need to be addressed immediately with a medical doctor to ensure your lithium level is not dangerously high.
In rare cases, lithium may lead to a reversible condition known as diabetes insipidus. If this occurs you would notice a significant increase in thirst and how much fluid you drink and how much you urinate. Talk to your doctor if you notice you are urinating more frequently than usual.
Are There Any Risks For Taking Lithium For Long Periods Of Time?
Hypothyroidism (low levels of thyroid hormone) may occur with long-term lithium use.
Rare kidney problems have been associated with long-term use of lithium. The risk increases with high levels of lithium. Your doctor will monitor your kidney function at routine check-ups to ensure this does not occur.
What Other Medications May Interact With Lithium?
The following medications can increase the levels and effects of lithium:
- Diuretics, such as: hydrochlorothiazide (Microzide®), furosemide (Lasix®), bumetanide (Bumex®), torsemide (Demadex®), acetazolamide (Diamox®), chlorthiazide (Diuril®), and chlorthalidone (Thalitone®)
- Non-steroidal anti-inflammatory medications (NSAIDs) including: Ibuprofen (Advil®, Motrin®), naproxen (Naprosyn®), celecoxib (Celebrex®), diclofenac (Voltaren®), and nabumetone (Relafen®)
- Certain blood pressure medications, called angiotensin receptor blockers or angiotensin converting enzyme inhibitors.

- Angiotensin receptor blockers (ARBs): valsartan (Diovan®), olmesartan (Benicar®), candesartan (Atacand®), losartan (Cozaar®)
- Angiotensin converting enzyme (ACE) inhibitors: enalapril (Vasotec®), captopril (Capoten®), benazepril (Lotensin®), fosinopril (Monopril®)
- Certain antidepressants, known as monoamine oxidase inhibitors (MAOIs). Examples include phenelzine (Nardil®), tranylcypromine (Parnate®), selegiline (Eldepryl®, Emsam®), and isocarboxazid (Marplan®)
The following medications may decrease the levels and effect of lithium:
- Caffeine
- Sodium chloride (table salt)
- A medication used to treat breathing problems called theophylline (Theo–Dur®, Slo–Bid®)
How Long Does It Take For Lithium To Work?
It is very important to tell your doctor how you feel things are going during the first few weeks after you start taking lithium. It will probably take several weeks to see big enough changes in your symptoms to decide if lithium is the right medication for you.
Mood stabilizer treatment is generally needed lifelong for persons with bipolar disorder. Your doctor can best discuss the duration of treatment you need based on your symptoms and illness.
Summary of Black Box Warnings
Lithium toxicity
Lithium toxicity is closely related to lithium blood levels and can occur at doses close to therapeutic levels; lithium levels should be monitored closely when starting the medication or if individuals experience side effects of the medication.
Provided by
(January 2023)
©2022 The American Association of Psychiatric Pharmacists (AAPP) and the National Alliance on Mental Illness (NAMI). AAPP and NAMI make this document available under the Creative Commons Attribution-No Derivatives 4.0 International License. Last Updated: January 2016.
This information is being provided as a community outreach effort of the American Association of Psychiatric Pharmacists. This information is for educational and informational purposes only and is not medical advice. This information contains a summary of important points and is not an exhaustive review of information about the medication. Always seek the advice of a physician or other qualified medical professional with any questions you may have regarding medications or medical conditions. Never delay seeking professional medical advice or disregard medical professional advice as a result of any information provided herein. The American Association of Psychiatric Pharmacists disclaims any and all liability alleged as a result of the information provided herein.
This information is for educational and informational purposes only and is not medical advice. This information contains a summary of important points and is not an exhaustive review of information about the medication. Always seek the advice of a physician or other qualified medical professional with any questions you may have regarding medications or medical conditions. Never delay seeking professional medical advice or disregard medical professional advice as a result of any information provided herein. The American Association of Psychiatric Pharmacists disclaims any and all liability alleged as a result of the information provided herein.
I've Missed a Dose; What Should I Do?
Published: May 2003
Information on this subject has been updated. Read the most recent information.
Prescriber Update 24(1): 14
May 2003
Andrew Gilbert, Libby Roughead and Lloyd Sansom, Quality Use of Medicines and Pharmacy Research Centre, University of South Australia, Adelaide
Reprinted from Australian
Prescriber 2002;25(1):16-18 with permission.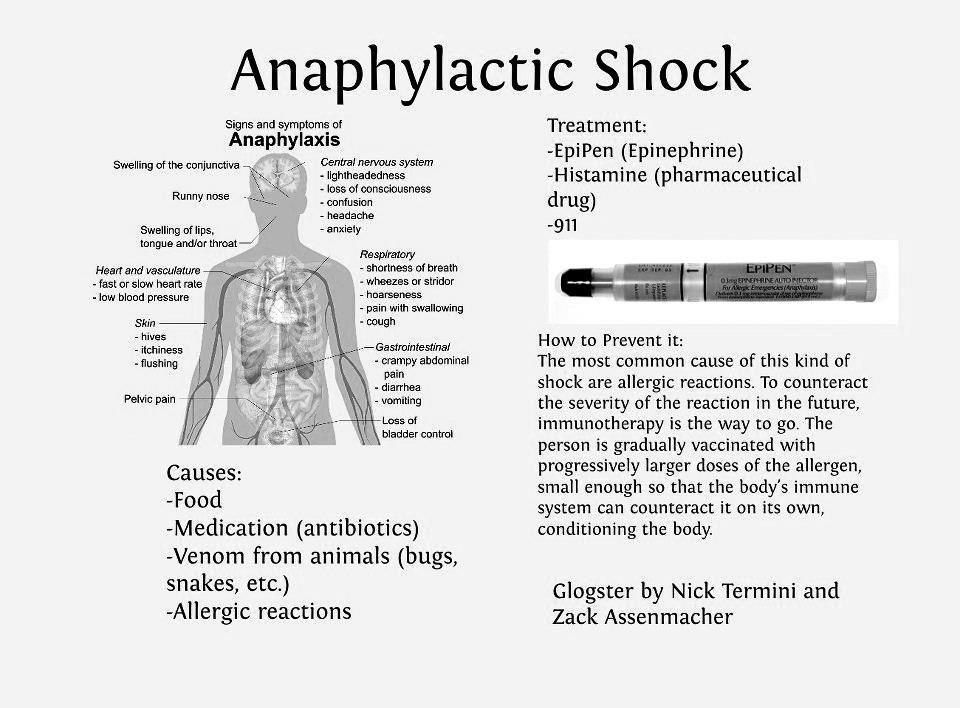
More than 80% of patients occasionally miss a dose of their medication. Health practitioners ought to plan with their patients what to do if a dose is missed. Patients believe that this plan should be a required part of the information received when a medication is prescribed and dispensed. Consumer Medicine Information sheets, which are available for most commonly prescribed medications, contain a section on what to do if a dose is missed. The routine use of these sheets or similar advice may help patients to know what to do when they miss a dose.
Introduction
Why don't consumers know what to do when they miss a
dose of their medication? As health professionals we know that the
vast majority of patients occasionally miss a dose of their medication.
This unintentional non-compliance, and request for advice after the event,
is very common in practice. In a study of 205 people, 90% rated having information
on 'what to do if a dose is missed' as very important or important and only
1.5% did not want information on this topic.1
A USA study2 found that less than 50% of patients
received this information.
In a study of 205 people, 90% rated having information
on 'what to do if a dose is missed' as very important or important and only
1.5% did not want information on this topic.1
A USA study2 found that less than 50% of patients
received this information.
Given our understanding of the difficulties around compliance with medication regimens, it must be our expectation that many patients will miss doses. Informing them about what to do about a missed dose at the time of prescribing, dispensing and administration would seem to be a logical step towards improved compliance.
Pre-emptive advice
Missed doses could be viewed within the framework of patient non-compliance,
however the problems which arise often result because health professionals
do not give enough information to allow the patient to safely use the medication.
Teaching a patient what to do if a dose is missed and providing strategies
to minimise the number of missed doses appears a sensible approach. 3
Providing written information, that includes what to do if a dose is missed,
improves people's self-administration of medicines, including corrective
action when a dose is missed.4
3
Providing written information, that includes what to do if a dose is missed,
improves people's self-administration of medicines, including corrective
action when a dose is missed.4
In practice, giving information on what to do if a dose is missed should not be too onerous a task for medical practitioners or pharmacists. Most of the commonly prescribed medications in Australia come with, or have available, a Consumer Medicine Information (CMI) sheet.a All CMI sheets have a section entitled 'What to do if you miss a dose'. Giving patients a CMI sheet the first time they receive a medication, and using this material in discussion with patients at the time of prescribing and dispensing would prepare them for this eventuality.
Assessing the importance of a missed dose (Table 1)
The severity of the patient's condition, whether clinically significant
breakthrough effects are likely to be observed, and the characteristics
of the medication should be considered when deciding the most appropriate
strategy following a missed dose. Vulnerable patients are easily recognisable
in any practice and include those on medications of low therapeutic index,b
or suffering from conditions which require constant maintenance of therapeutic
concentrations (for example epilepsy and thromboembolic diseases requiring
anticoagulation). On the other hand, for most people with hypertension
or hypercholesterolaemia a single missed dose will be of little consequence.
Vulnerable patients are easily recognisable
in any practice and include those on medications of low therapeutic index,b
or suffering from conditions which require constant maintenance of therapeutic
concentrations (for example epilepsy and thromboembolic diseases requiring
anticoagulation). On the other hand, for most people with hypertension
or hypercholesterolaemia a single missed dose will be of little consequence.
The patients should be informed at the time of prescribing and dispensing, of strategies to minimise missed doses and to redeem the situation when a dose is missed. Highlighting the strategy as it appears on the CMI or writing out an action plan as a reminder to the patient may prove very useful.
While a pre-emptive approach is ideal it is recognised that requests
for information about missed doses are common. Knowledge of a drug's
half-life, a major determinant of the fluctuation in interdose concentrations
at steady state, is useful for making recommendations on what to do if a
dose is missed. Upon cessation of therapy, it takes four to five half-lives
for the drug to be completely eliminated.
Upon cessation of therapy, it takes four to five half-lives
for the drug to be completely eliminated.
In general, medications, or their active metabolites, with a long half-life tend to create less problems when a dose is missed than medications with a short half-life. However, the clinical effect of some drugs is not related to the half-life. This usually occurs when the drug is acting via an irreversible mechanism (for example aspirin's effect on platelets), via an indirect mechanism (for example the effect of warfarin on blood coagulation), when the drug is a pro-drug (in which case it is the half-life of the active species that is important) or when the drug is converted to an active metabolite which has a long half-life.5
Missing several consecutive doses raises additional problems. For
example, for drugs with long half-lives it can take a significant time to
re-establish therapeutic concentrations when regular dosing resumes unless
loading doses are given (for example digoxin). Drugs with short half-lives
will lose therapeutic effect rapidly. Further, drugs with first-dose
effects, for example an ACE inhibitor in combination with diuretics, may
also present clinical problems when normal dosing is resumed. Overall,
surprisingly few studies have examined the clinical significance of a missed
dose.
Drugs with short half-lives
will lose therapeutic effect rapidly. Further, drugs with first-dose
effects, for example an ACE inhibitor in combination with diuretics, may
also present clinical problems when normal dosing is resumed. Overall,
surprisingly few studies have examined the clinical significance of a missed
dose.
Missed doses of the oral contraceptive pill have been well studied.
Women taking the pill need to be aware of the risk associated with missed
doses and of what to do when a dose is missed (Table
1). Given the complexity of this information, and the risk of
an unwanted pregnancy, it is important that any verbal counselling is supported
with appropriate written material. Where a CMI sheet is available
this can be used during the consultation. If no CMI sheet is available
for the prescribed product, written notes based on the recommendations in
the Australian Medicines Handbook are useful. 6
6
Conclusion
For the vast majority of patients an occasional missed dose will have little impact on the outcome of therapy. Most CMI sheets include statements such as:
- If you forget to take one or more doses: take your next dose at the normal time and in the normal amount. Do not take any more than your doctor prescribed.
- If you miss one dose, skip it and continue with your normal schedule.
Having this knowledge when starting therapy may be a simple way to alleviate much patient anxiety and in some cases avoid unwanted clinical consequences.
a In New Zealand, CMI fact sheets are available for some medicines. These CMI can be freely accessed from the Medsafe web site: www.medsafe.govt.nz/Medicines/infoSearch.asp
b The therapeutic index reflects the range of concentrations
between the drug concentration which produces toxic effects and the drug
concentration required for therapeutic effects. A narrow therapeutic
index means only small increases in concentration can cause toxicity and
small decreases in concentration can result in loss of efficacy.
A narrow therapeutic
index means only small increases in concentration can cause toxicity and
small decreases in concentration can result in loss of efficacy.
Conflict of interest: none declared
References
- Howard J, Wildman K, Blain J, Wills S, Brown D. The importance of drug information from a patient perspective. J Soc Admin Pharm 1999;16:115-26.
- Lyons RF, Rumore MM, Merola MR. An analysis of drug information desired by the patient. J Clin Pharm Ther 1996;21:221-8.
- Zind R, Furlong C, Stebbins M. Educating patients about missed medication doses. J Psychosoc Nurs Ment Health Serv 1992;30:10-4.
- Paulson PT, Bauch R, Paulson ML, Zilz DA. Medication data sheets - an aid to patient education. Drug Intell Clin Pharm 1976;10:448-53.
- Sansom L, editor. Australian Pharmaceutical Formulary
and Handbook.
 17th ed. Canberra: Pharmaceutical Society of Australia;
2000.
17th ed. Canberra: Pharmaceutical Society of Australia;
2000. - Australian Medicines Handbook 2000. 2nd ed. Adelaide: Australian Medicines Handbook Pty Ltd.; 2000. p. 17-9.
Table 1
Examples of medications for which missed doses may be clinically important, and information for patients on what to do if a dose is missed
| Medication | Information for consumers |
|---|---|
| Oral contraceptives | |
| Combined oral contraceptives | If one or more tablets are missed from the inactive tablets,
no additional contraceptive precautions are necessary, and tablet
taking should be recommenced ignoring the missed tablet or tablets. However, if all the inactive tablets are missed and then the next pack is not started on time, start as soon as it is remembered. 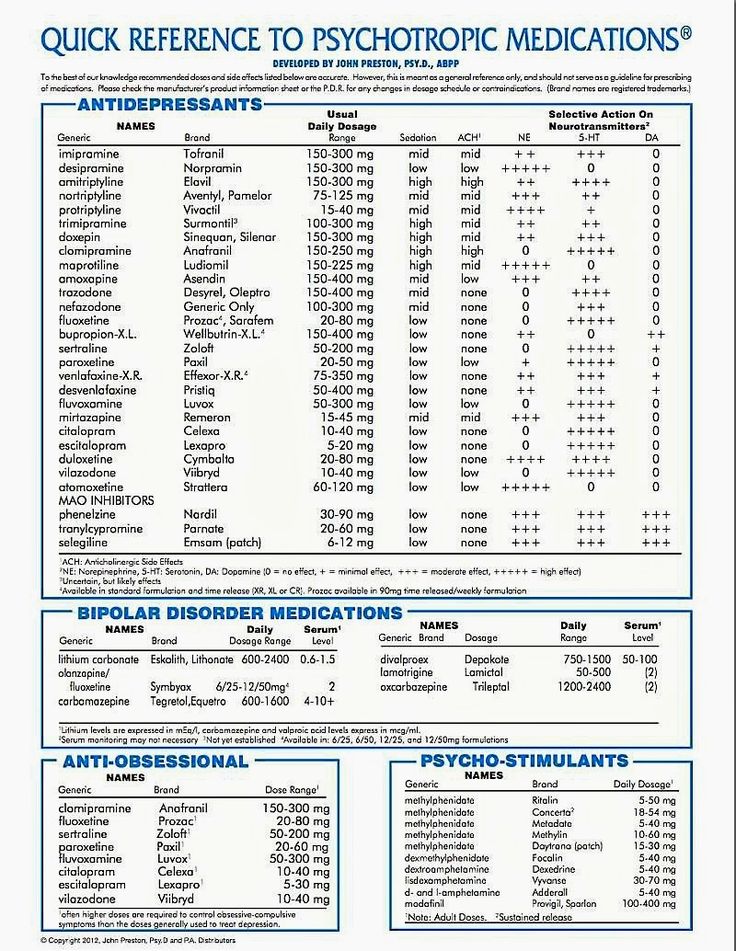 Additional contraception (such as a condom or a diaphragm) must
be used for the next 7 days.
Additional contraception (such as a condom or a diaphragm) must
be used for the next 7 days.If an active tablet is forgotten take it as soon as it is remembered, within 12 hours after the time that it is normally taken. Then take the next and subsequent tablets at the usual time. If there is a delay of more than 12 hours after the time that the tablet is normally taken, contraceptive protection in this cycle may be reduced. There is more risk in becoming pregnant if tablets are missed during the first week, or at the end of the current pack. Take the missed tablet as soon as it is remembered, even if this means taking two tablets at the same time. Any earlier missed tablets are left in the pack. Continue taking a daily tablet as usual, and use additional contraceptive precautions (except for the rhythm or temperature method) for the next 7 days.  If these 7 days extend
into the inactive section, skip the inactive section and start a
new pack in the active area on the next day instead If these 7 days extend
into the inactive section, skip the inactive section and start a
new pack in the active area on the next day instead |
| Progestogen-only oral contraceptives | For women using the progestogen-only pill the recommendation for the use of other methods of contraception is extended to 14 days if the dose is delayed by three hours or more. |
| Anticonvulsants | |
| Acetazolamide Carbamazepine Ethosuximide Phenytoin Tiagabine Topiramate Vigabatrin |
If it is almost time for next dose (within 4 hours), skip the
missed dose and take the next dose when it is due. Otherwise, take
it as soon as it is remembered, and then go back to taking the medicine
as usual. Do not take a double dose to make up for the missed dose. This may increase the chance of you getting an unwanted adverse
effect.
This may increase the chance of you getting an unwanted adverse
effect. |
| Lamotrigine Sodium valproate |
Do not take a double dose to make up for the dose that you missed. (This drug has a long half-life.) |
| Digoxin Warfarin |
If it is almost time for the next dose, skip the missed dose and take the next dose when it is due. Otherwise, take it as soon as it is remembered, and then go back to taking the medicine as usual. Do not take a double dose to make up for the dose that you missed. |
| Psychotropics | |
| Lithium | If it is almost time for the next dose (within 2 hours), skip
the missed dose and take the next dose when it is due. Otherwise,
take it as soon as it is remembered, and then go back to taking
the medicine as usual. Do not take a double dose to make up for
the dose that you missed. Do not take a double dose to make up for
the dose that you missed. |
| Antidepressants other than monoamine oxidase
inhibitors Monoamine oxidase inhibitors |
If it is almost time for the next dose, skip the missed dose and take the next dose when it is due. Otherwise, take it as soon as it is remembered, and then go back to taking the medicine as usual. Do not take a double dose to make up for the dose that you missed. |
| Phenelzine Tranylcypromine | Do not take an extra dose. Wait until the next day and take the normal dose then. |
Memorial Sloan Kettering Cancer Center
Adult Medication
Share Provided by Lexicomp ® , this document contains all the information you need to know about this medicine, including indications, directions for use, side effects, and when your healthcare provider should be contacted.
Trade names: USA
Lithobid
Brand names: Canada
APO-Lithium Carbonate; Carbolith; DOM-Lithium Carbonate; Lithane; Lithmax; PMS-Lithium Carbonate
Warning
- This drug in doses close to standard doses can cause serious side effects. In rare cases, this may include death. Do not exceed the prescribed dosage of the drug. You will need to have blood tests to measure the level of this drug in your blood. There are many symptoms of elevated lithium levels in the blood. Please read carefully the section of this leaflet that tells you which situations require you to see a doctor.
What is this drug used for?
- This medicine is used to treat bipolar disorder.
- This drug may also be used for other indications. Consult your doctor.
What should I tell my doctor BEFORE taking this drug?
- If you have an allergy to this drug, any of its ingredients, other drugs, foods or substances.
 Tell your doctor about your allergies and how they have manifested.
Tell your doctor about your allergies and how they have manifested. - If you have any of the following health problems: dehydration, heart disease, kidney disease, low blood salt levels, or severe weakness or illness.
- If you have a certain heart disorder called Brugada syndrome or have ever fainted for no reason.
- If a member of your family has Brugada Syndrome, or someone in your family has died suddenly before the age of 45.
- If you are taking medicines to control your blood pressure or heart problems. You may need to take blood samples for a more thorough analysis.
This list of drugs and conditions that may interact with this drug is not exhaustive.
Tell your doctor and pharmacist about all medicines you take (prescription and over-the-counter, natural products and vitamins) and any health problems you have. You need to make sure that this drug is safe for your conditions and in combination with other drugs you are already taking. Do not start or stop taking any drug or change the dosage without your doctor's advice.
Do not start or stop taking any drug or change the dosage without your doctor's advice.
What do I need to know or do while taking this drug?
- Tell all your health care workers that you are taking this drug. These are doctors, nurses, pharmacists and dentists.
- Perform blood tests as directed by your doctor. Consult with your doctor.
- Avoid driving and other activities that require increased attention until you see how this drug affects you.
- If you are starting a low-salt diet, tell your doctor. Changes the metabolism of lithium in the body.
- Consult your doctor before drinking alcohol.
- An increase in body temperature, infection, vomiting, diarrhea or increased sweating can lead to a change in the concentration of the drug in the blood. If any of these symptoms occur, consult your doctor.
- Caution should be exercised in hot weather and during vigorous activity. Drink plenty of fluids to prevent dehydration.

- Report symptoms of high blood sugar to your healthcare provider, such as confusion, drowsiness, unusual feeling of thirst or hunger, increased urination, flushing, rapid breathing, and fruity breath.
- Some people who take this drug have a certain heart disorder (Brugada syndrome). These people had the disorder before but were unaware of it. People with Brugada syndrome have abnormal heart rhythms and are at risk of sudden death. Consult your doctor.
- People who take this drug with some other drugs, such as haloperidol, have rarely had brain problems. Sometimes these brain disorders have led to long-term brain damage. Consult your doctor.
- A severe and sometimes deadly complication called serotonin syndrome can occur. This risk may be increased if certain other drugs are taken at the same time. Call your doctor right away if you experience agitation, balance problems, confusion, hallucinations, high fever, tachycardia or abnormal heart rhythms, flushing, muscle twitching or stiffness, seizures, tremors or tremors, excessive sweating, severe diarrhea, nausea or vomiting , a very severe headache.

- This drug has been associated with increased intracranial pressure and eye inflammation. This can lead to visual disturbances, such as loss of vision. Call your doctor right away if you have a very severe headache, ringing in the ears, or visual disturbances such as blurred vision, double vision, or loss of vision.
- If you develop symptoms of kidney problems such as difficulty urinating, changes in the amount of urine you produce, bloody, brown or foamy urine, shortness of breath or cough, puffiness or swelling of your face, feet or hands, call your doctor right away.
- If you are 65 years of age or older, use this drug with caution. You may experience more side effects.
- Possible adverse effects of this drug on the fetus. You may need to take a pregnancy test before you start taking this drug to make sure you are NOT pregnant.
- If you are pregnant or become pregnant while taking this drug, call your doctor right away.
- If you are breastfeeding or planning to breastfeed, tell your doctor.
 This drug passes into breast milk and may harm your baby.
This drug passes into breast milk and may harm your baby.
What side effects should I report to my doctor immediately?
WARNING. In rare cases, this drug can cause serious and sometimes deadly side effects in some patients. Contact your doctor or seek medical attention right away if you have any of the following signs or symptoms that may be associated with serious side effects:
- Signs of an allergic reaction, such as rash, hives, itching, red and swollen skin with blisters or peeling, possibly accompanied by fever, wheezing or wheezing, tightness in the chest or throat, difficulty breathing, swallowing or speaking, unusual hoarseness, swelling in the mouth, face, lips, tongue or throat.
- Symptoms of increased acidity in the blood (acidosis), such as confusion, rapid breathing, tachycardia, irregular heartbeat, very severe abdominal pain, nausea or vomiting, severe drowsiness, shortness of breath, increased fatigue or weakness.
- Thyroid symptoms such as weight changes, nervousness, agitation, anxiety, weakness, thinning hair, depression, swelling in the eyes or neck, difficulty concentrating, temperature control problems, menstrual changes, tremors, or sweating.
- Signs of fluid and electrolyte imbalances such as mood changes, confusion, muscle pain or weakness, fast or irregular heart rate, severe dizziness or loss of consciousness, extreme thirst, seizures, feeling very tired or weak, decreased appetite, inability to urinate or change in the amount of urine produced, dry mouth, dry eyes, severe nausea or vomiting.
- Bloating.
- Diarrhea.
- Dizziness.
- Difficulties with walking.
- Uncontrolled body movements, jerky movements, balance problems, difficulty swallowing or speaking.
- Muscle weakness.
- Feeling sluggish.
- Loss of control over eye movements.
- Mood changes.
- Heat.

- Hallucinations (a person sees or hears something that is not in reality).
- Impairment or loss of memory.
- Anxiety.
- Shortness of breath, sudden weight gain, or swelling of the arms or legs.
- Unexplained fluctuations in weight.
- Inability to control the bladder.
- Loss of control over bowel movements.
- Violation of sexual function.
What are some other side effects of this drug?
Any medicine can have side effects. However, for many people, side effects are either minor or non-existent. Talk to your doctor or get medical help if these or any other side effects bother you or don't go away:
- Feeling dizzy, drowsy, tired or weak.
- Nausea.
- Decreased appetite.
- Pain in the intestines.
- Increased salivation.
- Gas formation.
- Dry mouth.
- Headache.
- Dry or thin hair.

- Hair loss.
- Change in the ability to perceive taste.
- Joint pain.
This list of possible side effects is not exhaustive. If you have any questions about side effects, please contact your doctor. Talk to your doctor about side effects.
You can report side effects to the National Health Board.
You can report side effects to the FDA at 1-800-332-1088. You can also report side effects at https://www.fda.gov/medwatch.
What is the best way to take this drug?
Use this drug as directed by your doctor. Read all the information provided to you. Strictly follow all instructions.
All forms:
- Take with or without food. Take with food if medicine causes nausea.
- You should keep the amount of salt consumed daily at the same level.
- Follow your doctor's instructions for recommended types and amounts of fluids to drink while taking this drug.
Liquid (solution):
- Liquid doses should be measured with caution.
 Use the dispenser that comes with the medication. If the dispenser is not provided in the package, ask the pharmacist for a dosing agent for this drug.
Use the dispenser that comes with the medication. If the dispenser is not provided in the package, ask the pharmacist for a dosing agent for this drug.
Modified release tablets:
- Swallow whole. Don't chew or crumble.
What if I miss a dose of a drug?
- Take the missed dose as soon as you can.
- If it's time for your next dose, don't take the missed dose and then go back to your regular dosing schedule.
- Do not take 2 doses or an additional dose at the same time.
- If you miss a dose and are not sure what to do, contact your doctor.
How do I store and/or discard this drug?
- Store at room temperature in a dry place. Do not store in the bathroom.
- Keep all medicines in a safe place. Keep all medicines out of the reach of children and pets.
- Dispose of unused or expired drugs. Do not empty into a toilet or sewer unless instructed to do so.
 If you have any questions about disposing of medicines, ask your pharmacist. Drug disposal programs may be in place in your area.
If you have any questions about disposing of medicines, ask your pharmacist. Drug disposal programs may be in place in your area.
General information about medicines
- If your health does not improve or even worsens, see your doctor.
- Do not give your medicine to anyone and do not take other people's medicines.
- Some medicines may come with other patient information leaflets. If you have questions about this drug, talk with your doctor, nurse, pharmacist, or other health care professional.
- A separate instruction for patients is attached to the drug. Please read this information carefully. Reread it each time you refill your supply. If you have any questions about this drug, ask your doctor, pharmacist, or other health care professional.
- If you think you have overdosed, call a poison control center or get medical help right away. Be prepared to tell or show what drug you took, how much, and when it happened.
Consumer Use of Information and Limitation of Liability
This summary information includes a summary of the diagnosis, treatment, and/or drug product. It is not intended to be a comprehensive source of data and should be used as a tool to help the user understand and/or evaluate potential diagnostic and treatment options. It does NOT include all information about conditions, treatments, medications, side effects, or risks that may apply to a particular patient. It should not be considered medical advice or a substitute for medical advice, diagnosis or treatment provided by a physician based on a medical examination and assessment of the patient's specific and unique circumstances. Patients should consult with their physician for full information about their health, medical issues, and treatment options, including any risks or benefits regarding the use of medications. This information is not a guarantee that a treatment or drug is safe, effective, or approved for a particular patient. UpToDate, Inc. and its subsidiaries disclaim any warranties or liabilities related to this information or its use. The use of this information is subject to the Terms of Use found at https://www.wolterskluwer.com/en/know/clinical-effectiveness-terms.
UpToDate, Inc. and its subsidiaries disclaim any warranties or liabilities related to this information or its use. The use of this information is subject to the Terms of Use found at https://www.wolterskluwer.com/en/know/clinical-effectiveness-terms.
Last revision date
2021-11-08
Copyright
© UpToDate, Inc. and its affiliates and/or licensors, 2023. All rights reserved.
Date last updated
Monday, December 12, 2022
Experts have changed the way adults treat depression » Medvestnik
The National Institute for Health and Care Excellence (NICE) has updated guidelines for treating adults with depression. The changes affected the tactics of treating the disease, the possibility of intensifying antidepressant therapy, and ways to cancel drug therapy.
Definition
Depression is a mental disorder characterized by an inability to experience positive emotions (loss of interest in and enjoyment of ordinary things and activities), depressed mood, and a wide range of associated emotional, cognitive, somatic, and behavioral symptoms, according to the NICE document .
Principles of Case Management
In caring for a patient with depression, the professional should strive to build a relationship of trust. It is necessary to communicate with the patient openly, without judging him, avoiding stigmatization and discrimination, respecting confidentiality, privacy and respect for his personality. The patient must be given full access to up-to-date, evidence-based recommendations for the treatment of depression, as well as information about local self-help groups.
At the first meeting with the patient, it is necessary to clarify the history of the disease, concomitant mental and somatic pathology, the presence of episodes of elevated mood (for differential diagnosis with bipolar disorder), previous therapy and response to it. It is important to know the patient's strengths, personal resources, difficulties in relationships, lifestyle (eg, diet, physical activity, sleep), the presence of stressful or traumatic life events, current or past (divorce, loss of a loved one, trauma), conditions life, whether he has drug or alcohol abuse. A patient with depression should definitely ask about the presence of suicidal thoughts and intentions.
A patient with depression should definitely ask about the presence of suicidal thoughts and intentions.
If suicidal risk is identified, the patient should be referred to a psychiatrist immediately.
Periods of high risk
When working with depressed patients, special care should be taken during periods of high risk: when starting and changing therapy, with increased stress. It is necessary to advise the patient and his relatives to pay attention to mood swings, anxiety, negative feelings and a sense of hopelessness, the appearance of suicidal thoughts.
It should be remembered that high doses of antidepressants can be toxic, so patients with suicidal risk should limit the amount of medication dispensed at one time on their hands.
The risk of suicidal thoughts, the likelihood of self-harm and suicide increase in the first weeks of antidepressant therapy.
Treatment
For subthreshold and mild depression, antidepressant therapy should not be the first choice.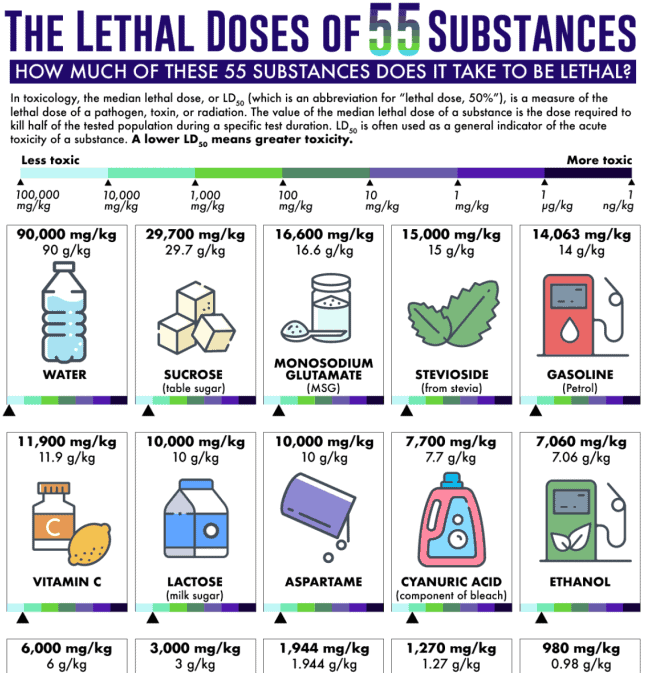 The patient can be offered a wide range of therapeutic techniques: self-help groups, cognitive behavioral therapy, behavioral activation, interpersonal psychotherapy, short-term psychodynamic psychotherapy, group physical education classes specially designed for patients with depression, mindfulness-based cognitive therapy and meditation.
The patient can be offered a wide range of therapeutic techniques: self-help groups, cognitive behavioral therapy, behavioral activation, interpersonal psychotherapy, short-term psychodynamic psychotherapy, group physical education classes specially designed for patients with depression, mindfulness-based cognitive therapy and meditation.
When working with patients with depressive disorders moderate and severe , antidepressant therapy may be required in addition to non-pharmacological methods.
When suggesting drug therapy to a patient, the reasons for prescribing the drug, possible drugs, dosage and options for changing it, expected improvements in therapy, possible side effects and withdrawal should be discussed.
When prescribing an antidepressant, the physician should explain to the patient the possible effects at the start of treatment, the timing of response to therapy (usually 4 weeks), and the need to take drugs for at least 6 months after the onset of remission.
A follow-up appointment should be scheduled after 2 weeks or after 1 week if there is a risk of suicide or if the patient is between 18 and 25 years of age.
Principles of Antidepressant Withdrawal and Dose Reduction
The patient should be aware that antidepressant withdrawal is gradual, gradual and successful in most cases. Abrupt discontinuation of therapy, skipping a dose, or taking an incomplete dose may cause a withdrawal syndrome: dizziness, sensory disturbances (eg, tingling sensation), mental changes (irritability, anxiety, anxiety, low mood, tearfulness, panic attacks, fears, confusion, occasionally suicidal thoughts), sleep disturbance, sweating, gastrointestinal disturbances (eg, nausea), palpitations, fatigue, headaches, joint and muscle pain.
Most often, the withdrawal syndrome is mild and lasts from 1 to 2 weeks, sometimes it can be more severe and last for several weeks, in rare cases - months. Occasionally, the withdrawal syndrome can be severe, especially with abrupt withdrawal of therapy.
When antidepressants are discontinued, the dose should be reduced in stages, for example by 50%. After that, reduce by another 25%, when small doses are reached, a transition to liquid forms of drugs is possible.
Before each step, you should make sure that there is no or minimal manifestations of the withdrawal syndrome.
Drugs with a short half-life should be discontinued more slowly. Cancellation of fluoxetine, given its prolonged action, can be performed with the transition to taking the drug every other day.
Successful withdrawal of antidepressants can take weeks to months. In severe withdrawal symptoms, the antidepressant should be resumed at full dose and tapered more slowly after symptoms resolve.
Augmentation therapy
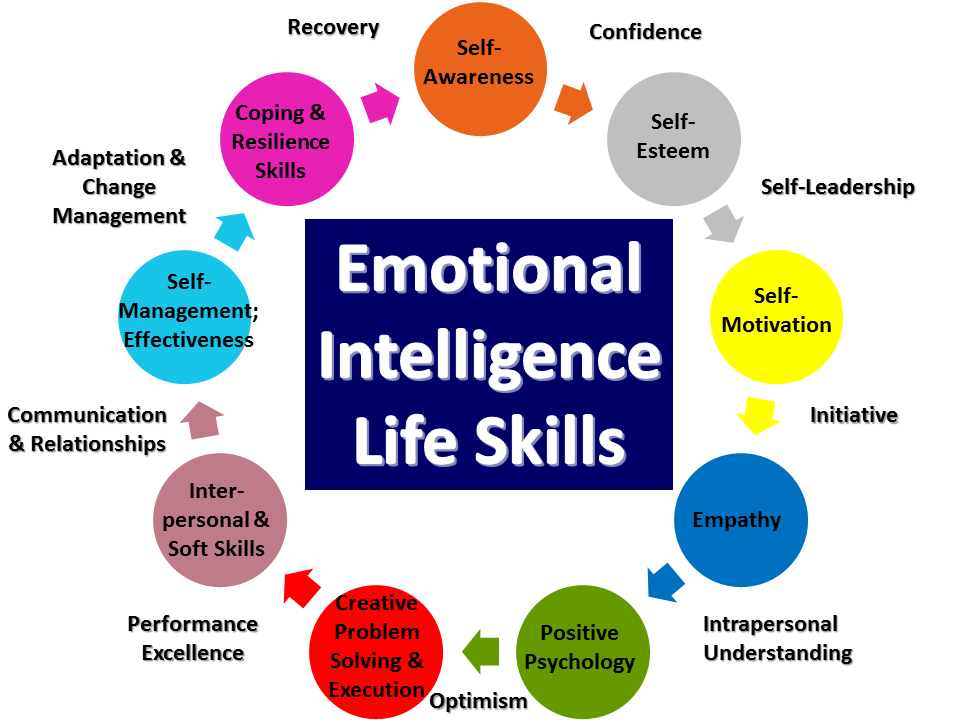
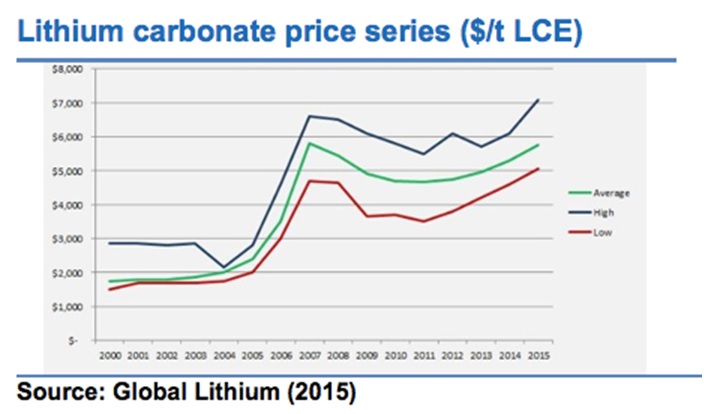
Lithium may be used as augmentation therapy for depression. After the appointment and then every 6 months, it is necessary to perform weight control, evaluate the function of the kidneys and thyroid gland, and the level of calcium.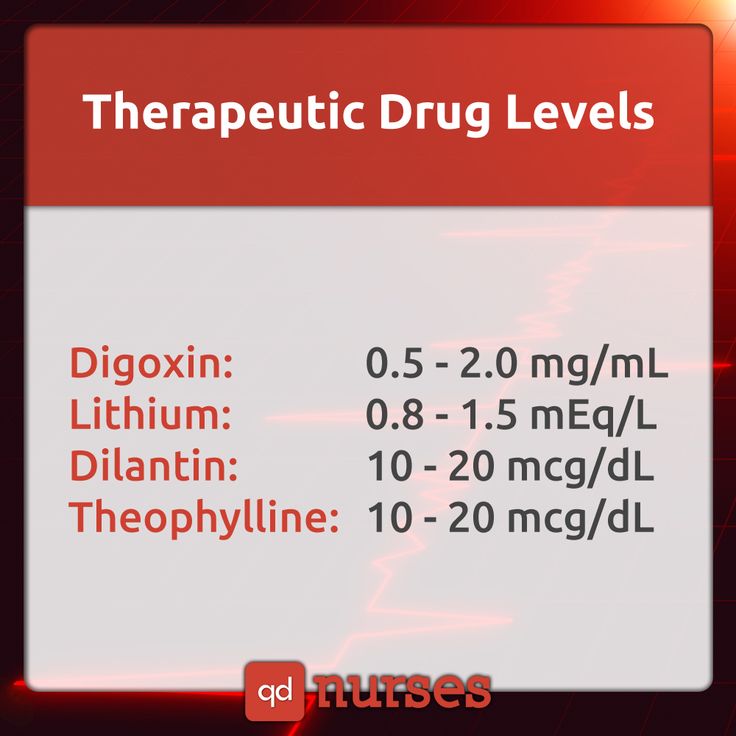
Plasma lithium levels should be assessed 12 hours after the first dose, then 1 week later, and 1 week after each dosage change; further drug monitoring is carried out every 3-6 months, depending on the patient's health status.
The concentration of lithium in the blood plasma should not exceed 1.0 mmol / l (the level required to achieve a therapeutic effect is from 0.4 mmol / l). Cancellation of lithium is carried out within 1-3 months under the supervision of a psychiatrist.
Antipsychotics may also be used to augment therapy, with attention to potential side effects (eg, extrapyramidal symptoms [eg, tremor, parkinsonism], elevated plasma prolactin levels).
When prescribing antipsychotics, it is necessary to monitor the clinical analysis of blood and urine, the concentration of electrolytes, prolactin, glucose and liver enzymes in the blood after 6, 12 weeks and 1 year from the start of therapy, and then annually, and also perform ECG monitoring.