Am i having a psychotic break
Early Psychosis and Psychosis | NAMI: National Alliance on Mental Illness
In this 2-part podcast series, NAMI Chief Medical Officer Dr. Ken Duckworth guides discussions on early psychosis that offer insights from individuals, family members and mental health professionals. Read the transcript.
Note: Content includes discussions on topics such as suicide attempts and may be triggering.
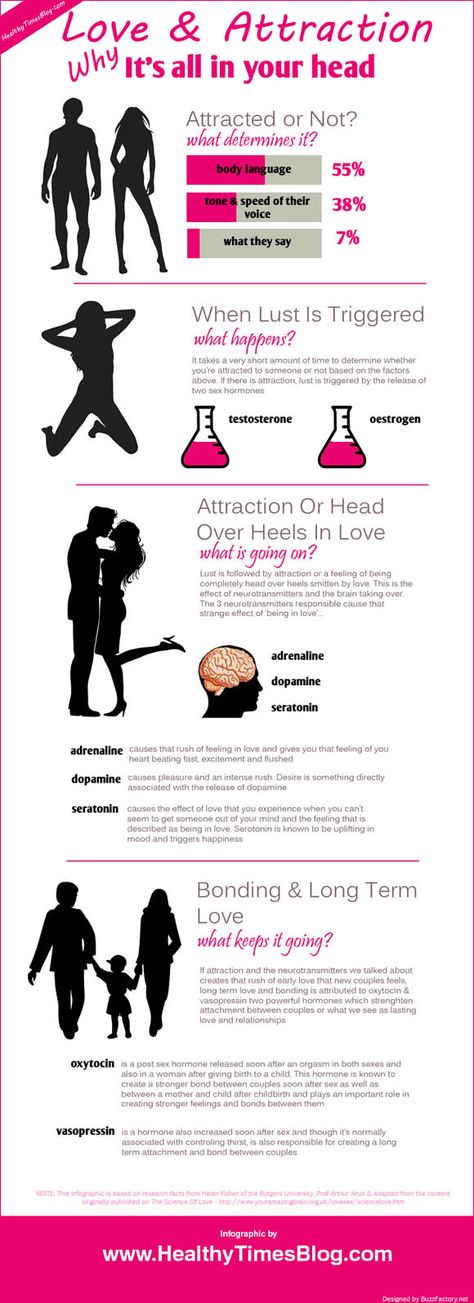
Most people think of psychosis as a break with reality. In a way it is. Psychosis is characterized as disruptions to a person’s thoughts and perceptions that make it difficult for them to recognize what is real and what isn’t. These disruptions are often experienced as seeing, hearing and believing things that aren’t real or having strange, persistent thoughts, behaviors and emotions. While everyone’s experience is different, most people say psychosis is frightening and confusing.
Psychosis is a symptom, not an illness, and it is more common than you may think. In the U.S., approximately 100,000 young people experience psychosis each year. As many as 3 in 100 people will have an episode at some point in their lives.
Early or first-episode psychosis (FEP) refers to when a person first shows signs of beginning to lose contact with reality. Acting quickly to connect a person with the right treatment during early psychosis or FEP can be life-changing and radically alter that person’s future. Don’t wait to take the first step and prepare yourself with information by reviewing these tip sheets:
What is Early and First-Episode Psychosis?
Early Psychosis: What's Going on and What Can You Do?
Encouraging People to Seek Help for Early Psychosis
Early Intervention: Tips for School Staff and Coaches
Symptoms
Early warning signs before psychosis
Early psychosis or FEP rarely comes suddenly. Usually, a person has gradual, non-specific changes in thoughts and perceptions, but doesn't understand what's going on. Early warning signs can be difficult to distinguish from typical teen or young adult behavior. While such signs should not be cause for alarm, they may indicate the need to get an assessment from a doctor.
Early warning signs can be difficult to distinguish from typical teen or young adult behavior. While such signs should not be cause for alarm, they may indicate the need to get an assessment from a doctor.
Encouraging people to seek help for early psychosis is important. Families are often the first to see early signs of psychosis and the first to address the issue of seeking treatment. However, a person's willingness to accept help is often complicated by delusions, fears, stigma and feeling unsettled. In this case, families can find the situation extremely difficult, but there are engagement strategies to help encourage a person to seek help.
It's important to get help quickly since early treatment provides the best hope of recovery by slowing, stopping and possibly reversing the effects of psychosis. Early warning signs include the following:
- A worrisome drop in grades or job performance
- Trouble thinking clearly or concentrating
- Suspiciousness or uneasiness with others
- A decline in self-care or personal hygiene
- Spending a lot more time alone than usual
- Strong, inappropriate emotions or having no feelings at all
Signs of early or first-episode psychosis
Determining exactly when the first episode of psychosis begins can be hard, but these signs and symptoms strongly indicate an episode of psychosis:
- Hearing, seeing, tasting or believing things that others don’t
- Persistent, unusual thoughts or beliefs that can’t be set aside regardless of what others believe
- Strong and inappropriate emotions or no emotions at all
- Withdrawing from family or friends
- A sudden decline in self-care
- Trouble thinking clearly or concentrating
Such warning signs often point to a person’s deteriorating health, and a physical and neurological evaluation can help find the problem.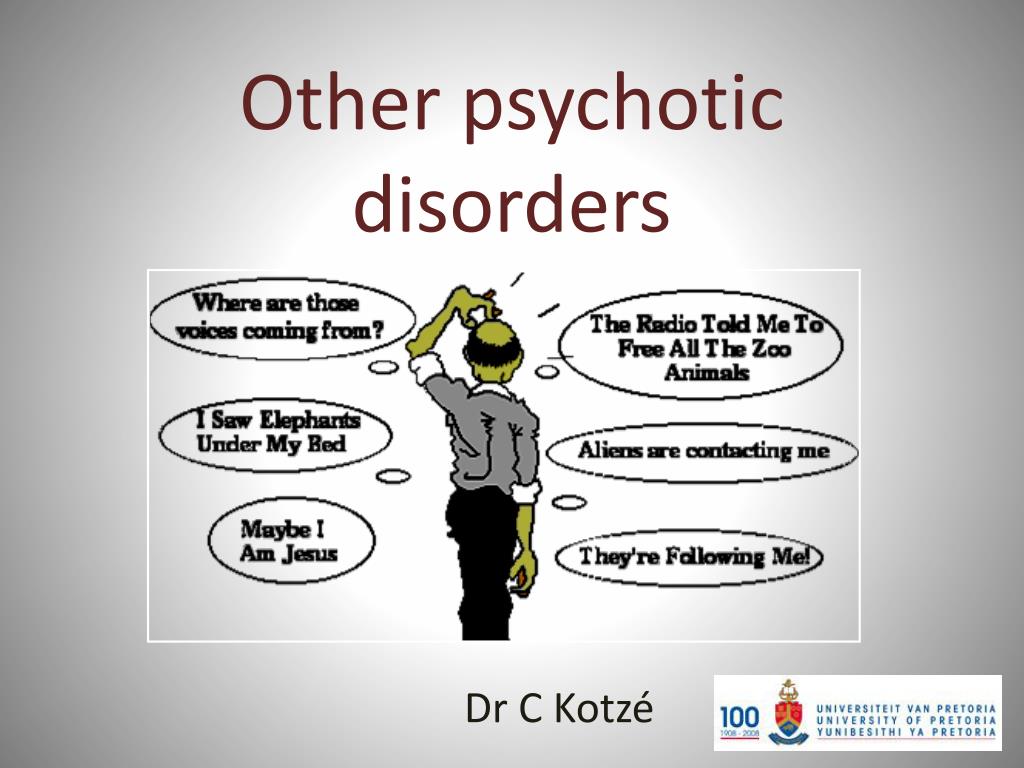 A mental health professional performing a psychological evaluation can determine if a mental health condition is involved and discuss next steps. If the psychosis is a symptom of a mental health condition, early action helps to keep lives on track.
A mental health professional performing a psychological evaluation can determine if a mental health condition is involved and discuss next steps. If the psychosis is a symptom of a mental health condition, early action helps to keep lives on track.
Psychosis
Psychosis includes a range of symptoms but typically involves one of these two major experiences:
Hallucinations are seeing, hearing or feeling things that aren’t there, such as the following:
- Hearing voices (auditory hallucinations)
- Strange sensations or unexplainable feelings
- Seeing glimpses of objects or people that are not there or distortions
Delusions are strong beliefs that are not consistent with the person’s culture, are unlikely to be true and may seem irrational to others, such as the following:
- Believing external forces are controlling thoughts, feelings and behaviors
- Believing that trivial remarks, events or objects have personal meaning or significance
- Thinking you have special powers, are on a special mission or even that you are God.

Causes
We are still learning about how and why psychosis develops, but several factors are likely involved. We do know that teenagers and young adults are at increased risk of experiencing an episode of psychosis because of hormonal changes in their brain during puberty.
Several factors that can contribute to psychosis:
- Genetics. Many genes can contribute to the development of psychosis, but just because a person has a gene doesn’t mean they will experience psychosis. Ongoing studies will help us better understand which genes play a role in psychosis.
- Trauma. A traumatic event such as a death, war or sexual assault can trigger a psychotic episode. The type of trauma—and a person’s age—affects whether a traumatic event will result in psychosis.
- Substance use. The use of marijuana, LSD, amphetamines and other substances can increase the risk of psychosis in people who are already vulnerable.
- Physical illness or injury. Traumatic brain injuries, brain tumors, strokes, HIV and some brain diseases such as Parkinson’s, Alzheimer’s and dementia can sometimes cause psychosis.
- Mental health conditions. Sometimes psychosis is a symptom of a condition like schizophrenia, schizoaffective disorder, bipolar disorder or depression.
Diagnosis
A diagnosis identifies an illness; symptoms are components of an illness. Health care providers draw on information from medical and family history and a physical examination to diagnose someone. If causes such as a brain tumor, infection or epilepsy are ruled out, a mental illness might be the reason.
If the cause is related to a mental health condition, early diagnosis and treatment provide the best hope of recovery. Research shows that the earlier people experiencing psychosis receive treatment, the better their long-term quality of life.
Treatment
Early or first-episode psychosis
Early treatment of psychosis, especially during the first episode, leads to the best outcomes.
Research has shown significant success using a treatment approach called Coordinated Specialty Care (CSC). CSC uses a team of health professionals and specialists who work with a person to create a personal treatment plan based on life goals while involving family members as much as possible.
CSC has the following key components:
- Case management
- Family support and education
- Psychotherapy
- Medication management
- Supported education and employment
- Peer support
SAMHSA maintains an Early Serious Mental Illness (ESMI) Treatment Locator as a source of information for family members who are seeking CSC programs in the US. Portions of their website are available in Spanish.
Psychosis treatment
Traditional treatment for psychosis involves psychotherapy and medication. Several types of therapy have successfully helped individuals learn to manage their condition. In addition, medication targets symptoms and helps reduce their impact.
Related Conditions
Psychosis can be related to several mental health conditions:
- Bipolar Disorder
- Schizoaffective Disorder
- Schizophrenia
- Substance use disorders / Dual Diagnosis
Substance Abuse and Trauma Treatment Facilities
7 Warning Signs of a Psychotic Episode: EXIS Recovery Inc.: Substance Abuse and Trauma Treatment FacilitiesPsychosis is a disrupted mental state that causes a loss of contact with reality. For someone who’s in the midst of a psychotic episode, it’s hard to tell the difference between what’s real and what’s only in their minds.
Psychosis usually begins during adolescence or early adulthood. Every year in the United States, roughly 100,000 teens and young adults experience first-episode psychosis (FEP). All told, about three in 100 people go through a psychotic episode at some point in their lives.
Here at EXIS Recovery in West Los Angeles, we know that early treatment makes a world of difference to someone who’s having a psychotic episode. Let’s explore the phases of psychosis, including common warning signs of an acute psychotic episode.
Let’s explore the phases of psychosis, including common warning signs of an acute psychotic episode.
Phases of psychosis
Psychosis isn’t a condition unto itself. It’s a symptom of an underlying health problem. While it’s most commonly a feature of a mental illness like schizophrenia, bipolar disorder, or major depression, psychosis can also be triggered by trauma, substance abuse, brain disease or injury, and even extreme sleep deprivation.
Although psychosis is a highly individual experience, a typical psychotic episode progresses through three distinct stages: the prodromal phase, the acute phase, and recovery.
We discussed the prodromal phase at length in a recent blog post about how to recognize the early signs of a psychotic disorder. This initial stage of psychosis, which is marked by gradual changes in a person’s thoughts, feelings, or behaviors, can last for several months to a year or longer.
During the prodromal phase, a person may find it difficult to focus, understand what others are saying, or keep track of their own thoughts. As a result, they may feel irritable, disconnected, overloaded, or suspicious.
As a result, they may feel irritable, disconnected, overloaded, or suspicious.
Signs of acute psychosis
Eventually, the prodromal phase of psychosis gives way to the acute phase, or what you might recognize as a psychotic episode. It’s during this phase that the characteristic signs of psychosis, including hallucinations and delusions, emerge and become obvious.
Common warning signs of a psychotic episode include:
Hallucinations
A hallucination is sensing something that isn’t real. A person may see objects or people that aren’t there, hear voices or sounds that don’t exist, feel imagined touch sensations, smell odors that no one else can smell, or experience taste when there’s nothing in their mouth.
Delusions
A delusion is an unshakeable belief that’s unlikely to be true and seems irrational to others. A person who suffers from delusions may believe that external forces control their thoughts and behaviors or that a person or institution is out to get them. Delusions of grandeur can make a person feel all-powerful or even god-like.
Delusions of grandeur can make a person feel all-powerful or even god-like.
Confused speech
Acute psychosis can cause disturbed thought patterns that make it hard to stay focused. This can take the form of rapid-fire or continuous speech, disrupted speech that switches from one topic to the next mid-sentence, or frequent speech pauses from a lost train of thought.
Mood changes
A psychotic episode can also give rise to dramatic mood swings, particularly for those whose symptoms are a result of a mental health condition like schizophrenia or bipolar disorder. In such cases, a person may experience a high, elated mood (mania) followed in relatively quick succession by a low, withdrawn mood (depression).
Improper behavior
Socially inappropriate behavior is another hallmark sign of acute psychosis. This may take the form of childish or regressive behavior, inappropriate affection, or excessive dependency. This aspect of psychosis can be especially distressing for caregivers, family, and friends.
Severe anxiety
Losing touch with reality during a psychotic episode can be scary and confusing, and many people become extremely anxious as a result. Persistent feelings of anxiety can lead to disrupted sleep patterns, a lack of motivation, diminished self-care, and difficulty functioning overall.
Social withdrawal
Living in an alternate reality can be incredibly isolating, particularly when it becomes clear that others aren’t having the same experience. This deep sense of isolation causes many people to turn inward and withdraw from family and friends.
Treatment and recovery
That a person will transition into the final phase of psychosis, recovery, isn’t a foregone conclusion — it’s entirely dependent on timely intervention and care. People who suffer from psychosis are more likely to recover fully if they receive early treatment, preferably soon after psychotic symptoms are observed.
Understanding the kinds of gradual changes that occur before a psychotic episode, as well as being able to recognize the most common signs of acute psychosis, can give you a head start in helping a friend or loved one get the care they need when they need it.
As mental health experts who specialize in psychotic disorders, the team at EXIS combines evidence-based practices and treatments with a coordinated care approach to help patients successfully transition from acute psychosis to complete recovery.
Call 424-244-3513 to reach our West Los Angeles office today, or use the easy online booking tool to schedule an appointment with one of our trusted mental health experts any time.
Treating Your Opioid Addiction with Medication-Assisted Treatment (MAT)
Medication-assisted treatment (MAT) uses FDA-approved medications to diminish physical dependency and reduce or prevent withdrawal symptoms. Here’s how it can help you detox safely, relieve cravings, reduce relapse, and sustain recovery.
EMDR for Substance Abuse: What to Expect
Unprocessed trauma and substance abuse have a close, interconnected relationship for nearly half of those who struggle with addiction. Learn how EMDR therapy helps flip the switch on trauma to support a healthy recovery.
Learn how EMDR therapy helps flip the switch on trauma to support a healthy recovery.
5 Steps to Take to Manage Your Fear of Flying
If the thought of getting on an airplane leaves you feeling anxious and full of dread, you’re not alone: Aerophobia, or fear of flying, affects about 25 million Americans. Here are five effective ways to gain the upper hand over your fear.
How to Encourage Your ADHD Child’s Strengths
ADHD can make it harder for your child to pay attention, follow directions, sit still, and control their impulses. But instead of focusing on what may be “wrong” with your child, ask yourself what’s right and encourage their strengths. Here’s how.
How Depression Affects Your Sleep (and What to Do About It)
There’s a two-way, circular path between depression and sleep disturbance: Each can give rise to the other and actively perpetuate one another. Luckily, you can break the vicious cycle between disrupted sleep and depression — here’s how.
Luckily, you can break the vicious cycle between disrupted sleep and depression — here’s how.
Getting the Support You Need After a Traumatic Loss
When the loss of a loved one is traumatic — whether it’s sudden, unexpected, connected to violence, or all the above — your grief reaction can be complex and overwhelming. Here’s why getting the right support matters.
Nervous breakdown - what it is, causes, symptoms, treatment
Everyone faces stress, but for some people it can develop into a nervous breakdown. What is a nervous breakdown, why does it occur and how does it manifest itself? Especially for Forbes Life, clinical psychologist, co-founder of the YouTalk service Anna Krymskaya talks about the causes, symptoms and consequences of this condition
What is a nervous breakdown
In the past, the term "nervous breakdown" was often used to refer to various mental disorders, but today such a diagnosis in there is no medicine, and a nervous breakdown is not considered a mental illness. The terms “nervous breakdown”, “nervous breakdown” or “emotional breakdown” often describe a condition where a person cannot cope with stress, anxiety and anxiety on their own, cannot function normally in everyday life.
The terms “nervous breakdown”, “nervous breakdown” or “emotional breakdown” often describe a condition where a person cannot cope with stress, anxiety and anxiety on their own, cannot function normally in everyday life.
Causes of a nervous breakdown
Although a breakdown is not a mental illness, any other disorder such as PTSD, depression, borderline personality disorder, or etc.), can provoke a breakdown.
Chronic stress can also cause a nervous breakdown, for example, caused by a series of financial difficulties, problems at work and in personal relationships. At risk are people who do not have stress tolerance skills and reliable social support.
You can prevent stress from developing into a nervous breakdown if you “catch” your condition a few weeks before the crisis point
How to understand that you have a nervous breakdown
The signs of a nervous breakdown vary from person to person and depend on the cause. Each organism reacts in its own way. Some symptoms are related to mental state, well-being and changes in behavior. However, physical symptoms are also possible.
Each organism reacts in its own way. Some symptoms are related to mental state, well-being and changes in behavior. However, physical symptoms are also possible.
Psychological symptoms of a nervous breakdown can manifest themselves as:
- acute anxiety that the person cannot cope with on their own;
- a feeling of detachment and disinterest in communicating with friends and relatives, doing the usual things;
- inability to focus and make decisions;
- mood swings - feeling of depression, emotional burnout, outbursts of uncontrollable anger and fear, feeling of helplessness, sobbing and hysteria;
- depersonalization - a state when a person does not feel himself;
- isolation from reality — a person does not distinguish between reality and imagination;
- as well as hallucinations, paranoia (the feeling that someone is watching you), suicidal thoughts and self-harm attempts.

Related material
Physical symptoms include insomnia and restless sleep, fatigue and exhaustion up to the inability to do even normal daily activities, frequent colds, digestive disorders. As well as such physiological manifestations as heart palpitations, discomfort in the chest, a feeling of a coma in the throat, which seems to make it harder to breathe - that is, signs of a panic attack. Some of the symptoms of a nervous breakdown are similar to those of burnout, a state of mental and emotional exhaustion that is often the result of chronic workplace stress.
Photo by Mikhail Nilov PexelsTreatment of a nervous breakdown
There is no universal answer to the question of how to treat a nervous breakdown. Depending on the situation and diagnosis, both a psychiatrist and a psychologist will help to cope with a nervous breakdown - these specialists have a different profile of work, often in the event of a nervous breakdown, the support of both is needed.
A psychiatrist specializes in diagnosing depression, generalized anxiety disorder, post-traumatic stress disorder and other conditions. If some mental disorder has become the basis for a nervous breakdown, medications can help treat it. Antidepressants and anti-anxiety medications are usually prescribed, but other medication options are available depending on the condition.
Diet, physical activity, and some simple habits can help you through stressful times.
In terms of psychological help, cognitive behavioral therapy (CBT) is considered the most effective treatment for nervous disorders. This approach helps to identify errors and false attitudes in thinking and interpreting life events, it works effectively for a specific task and in short-term therapy, for example, within 20 sessions. CBT is an important mechanism for the treatment of anxiety disorders of various nature. For a nervous breakdown, cognitive behavioral therapy may include homework, journaling to analyze experiences that occur during the day, refocusing, relaxation, and mindfulness techniques, as well as exposure (intentional encounters with frightening situations in order to reduce fear) and rational-emotive role-playing games. A psychologist should be able to ask open-ended questions correctly, show empathy and give a person the necessary tools that will help them to help themselves in the future.
CBT is an important mechanism for the treatment of anxiety disorders of various nature. For a nervous breakdown, cognitive behavioral therapy may include homework, journaling to analyze experiences that occur during the day, refocusing, relaxation, and mindfulness techniques, as well as exposure (intentional encounters with frightening situations in order to reduce fear) and rational-emotive role-playing games. A psychologist should be able to ask open-ended questions correctly, show empathy and give a person the necessary tools that will help them to help themselves in the future.
What to do to avoid a nervous breakdown
You can prevent stress from developing into a nervous breakdown if you “catch” your condition a few weeks before the crisis point. Try not to overload yourself, find time to replenish resources and slow down.
Some simple habits can help you through stressful times. All of them are quite simple, but proven effective. Try to eat a balanced diet that energizes. The diet should be varied, it is worth removing coffee, alcohol and other stimulants from the diet to reduce anxiety and improve sleep. Do not forget about regular physical activity - it can even be small daily walks.
All of them are quite simple, but proven effective. Try to eat a balanced diet that energizes. The diet should be varied, it is worth removing coffee, alcohol and other stimulants from the diet to reduce anxiety and improve sleep. Do not forget about regular physical activity - it can even be small daily walks.
Related material
Relaxation techniques and breathing practices also show high efficiency in the fight against stress. For example, you can use a visualization technique where you create a mental image of a place that calms you, or muscle relaxation, where you first tense and then relax different muscle groups. Try focusing on deep, slow breathing: inhale through your nose for 4 seconds, hold your breath for 7 seconds, and exhale through your mouth for 8 seconds.
If you have a nervous breakdown, you are in a critical condition and urgently need help, you can contact one of these organizations:
+7 (800) 2000-122 - a helpline for children, adolescents and their parents.
+7 (499) 216-50-50 - emergency psychological assistance.
+7 (499) 901-02-01 - assistance to survivors of sexual violence.
+7 (495) 916-30-00 - assistance to survivors of domestic violence (the Violence.net Center is recognized in Russia as a foreign agent).
+7 (800) 101-65-47 - hotline for men.
a nervous breakdown - how to recognize, overcome and prevent it - Personal experience on vc.ru
These questions are answered by the Reminder edition together with the online school of psychological professions "Psychodemia".
2788 views
Image generated by Stable Diffusion neural network through DreamStudio
Sometimes we lose control of ourselves - we start to hysteria, scream or cry, we experience strong anger, we cannot even do simple routine things, continue to “take out”, sometimes we experience strong inner feelings, background anxiety and insomnia. We call such moments a nervous breakdown - but medicine does not know such a diagnosis. What is a nervous breakdown, what factors provoke it, what effect does it have on the body and how to deal with it? Reminder answers these questions together with the online school of psychological professions "Psychodemia".
We call such moments a nervous breakdown - but medicine does not know such a diagnosis. What is a nervous breakdown, what factors provoke it, what effect does it have on the body and how to deal with it? Reminder answers these questions together with the online school of psychological professions "Psychodemia".
What is a nervous breakdown
"Nervous breakdown" is commonly referred to as a person's acute reaction to stress; a state when the psyche cannot withstand the amount of stress and fails. A breakdown manifests itself as a more vivid or atypical emotional reaction for a particular person, a loss of emotional control by him.
There is no clear definition of "nervous breakdown" in modern science: psychologists call this a certain state - exacerbation, the peak of one of the disorders associated with anxiety and stress. "Nervous breakdown" is not a medical term, does not indicate a specific mental illness, but it is not a normal or healthy response to stress, explains Dr.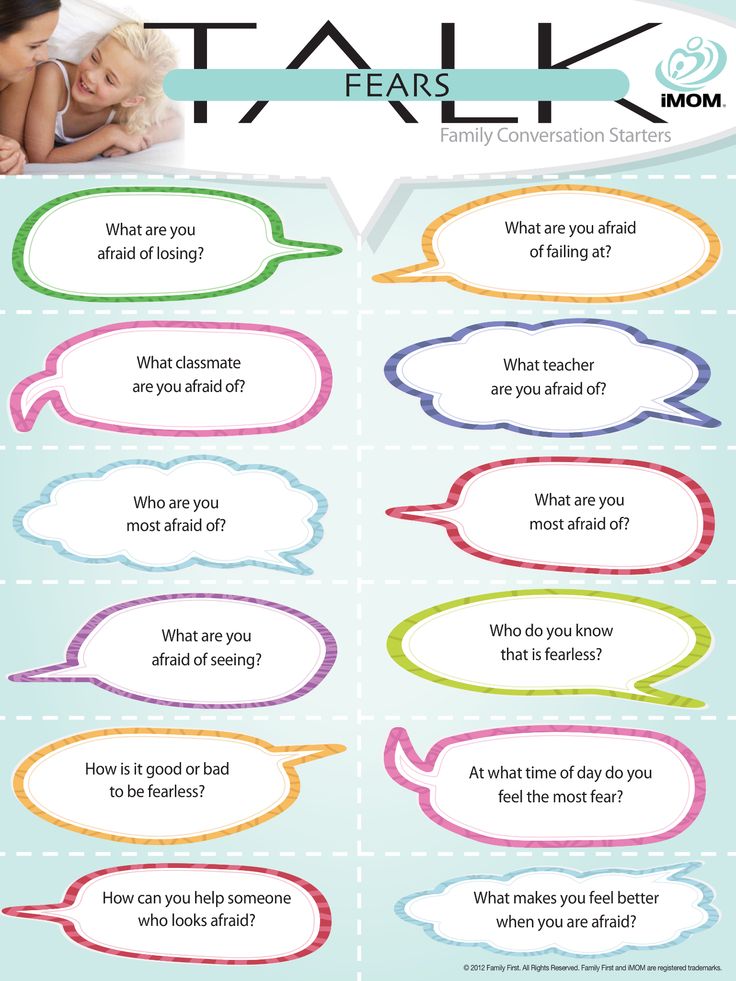 Daniel Hall-Flavin of the American Mayo Clinic. According to him, patients usually use this term to describe a stressful situation in which they are temporarily unable to function normally, respond emotionally and physically to life's challenges.
Daniel Hall-Flavin of the American Mayo Clinic. According to him, patients usually use this term to describe a stressful situation in which they are temporarily unable to function normally, respond emotionally and physically to life's challenges.
“If we were cars, a nervous breakdown is a complete tire blowout that sends us to the side of the road,” writes Chris Curtis of the Huntsman Institute of Mental Health at the University of Utah Health Sciences.
What does a nervous breakdown feel like
The signs and symptoms of a nervous breakdown can vary depending on both the underlying cause and the person's physical and mental condition. Here are some common signs:
- The person cannot control himself, behaves impulsively.
- Experiencing complex emotions: guilt, fear, rage, resentment.
- Feels powerless, afraid that he will not be able to cope with his affairs and duties.
- Experiences sleep disturbances, difficulty falling asleep and waking up.
- Loses appetite, meals may become irregular and chaotic.
- It is difficult to do ordinary things: wash your face, brush your teeth, do the cleaning.
- Difficulty focusing, feeling depressed and tired.
- Do not want to leave the house or communicate with other people.
People can call "nervous breakdown" very different things. “A person with an anxiety disorder may mistakenly refer to a panic attack as a relapse, a person with BAD (Bipolar Affective Disorder) or BPD (Borderline Personality Disorder) may refer to self-injurious behavior as a relapse. In any case, a breakdown can become a signal for a person, after which he will begin to realize the severity of his condition and seek help, ”says Maria Danina, founder of Psychodemia, Candidate of Psychological Sciences.
Comorbid psychiatric disorders may change the pattern of the breakdown itself: People with panic disorder were more likely to complain of trouble breathing or a panic-like build-up of fear during their breakdown. And people with an affective disorder experienced much more intense anger and a greater tendency to yell and aggressive behavior than people without comorbid disorders.
And people with an affective disorder experienced much more intense anger and a greater tendency to yell and aggressive behavior than people without comorbid disorders.
Important : a nervous breakdown must be distinguished from a psychotic breakdown or psychosis, a much more dangerous condition. These conditions have a number of similar symptoms, but there is a main and key difference: the adequacy of the person. During a nervous breakdown, a person feels unable to function normally, but is fully and adequately aware of what is happening to him and around him. And during a psychotic break, a person cannot adequately assess the situation, loses touch with reality, he may begin auditory or visual hallucinations, strange and delusional ideas, thoughts about harming himself or others. If in the case of a nervous breakdown, the help of specialists is desirable, then in the case of psychosis, a person needs mandatory and immediate psychiatric help.
What causes a nervous breakdown
Here are the most common reasons:
- Difficult life situations.
 For example, the death of a loved one, serious financial problems, divorce, loss of housing, business, and other difficult external problems.
For example, the death of a loved one, serious financial problems, divorce, loss of housing, business, and other difficult external problems. - Severe emaciation of the body. This leads to an accelerated pace of life, strict diets, super-intense workouts, prolonged lack of sleep and good rest.
- Mental disorders associated with stress. Adjustment disorder or post-traumatic stress disorder (PTSD).
- Anxiety disorders associated with stress. For example, generalized anxiety disorder, in which a person experiences tension and anxiety without any objective reasons.
- Mood disorders, bipolar or depressive disorder and others.
But this is the explanation of modern scientists, and when the term “nervous breakdown” appeared, its main cause was considered to be an acute deficiency of a special “energy”, which led to the fact that your nerves stopped working (in English, a “nervous breakdown” sounds like a nervous breakdown, which can be translated as "breakdown of nerves").
How did the term "nervous breakdown" come about
It was proposed at the very beginning of the 20th century by the American neurologist George Miller Beard; at the end of the 19th century, he was the first to describe and introduce into circulation the term "neurasthenia", by which he understood "deficiency or lack of nervous force."
Dr. Beard believed that every person is born with a certain, finite supply of "nerve capital" that cannot be calculated or measured. Nerve capital is expended during life in much the same way as the charge of an electric battery. Beard considered the main reason for the too rapid expenditure of nervous capital to be modern civilization, which differs from the ancients in five characteristics that cause nervous exhaustion in people: steam engines, periodicals, the telegraph, sciences, and the mental activity of women.
In 1901, Beard published the book Nervous Breakdown (full title: "Nervous Breakdown. Associated Vices, Prevention, and Treatment. Proper Life Technique for Knowledge Workers"). It is neurasthenia that leads to a nervous breakdown, which can be translated both as “breakdown of nerves” and as “nervous bankruptcy,” Beard believed. He called the immediate cause of this breakdown "mental overwork": for obvious reasons, it is more common in people engaged in mental work, who also drink too much alcohol, coffee and tea, eat poorly and sleep little.
Proper Life Technique for Knowledge Workers"). It is neurasthenia that leads to a nervous breakdown, which can be translated both as “breakdown of nerves” and as “nervous bankruptcy,” Beard believed. He called the immediate cause of this breakdown "mental overwork": for obvious reasons, it is more common in people engaged in mental work, who also drink too much alcohol, coffee and tea, eat poorly and sleep little.
Beard's ideas were very advanced: at that time, people who went to doctors with symptoms of a nervous breakdown were often recognized as imaginary patients, hypochondriacs, experiencing an unfounded fear of a non-existent disease. “There are many people who suffer from vague symptoms for no apparent reason,” Beard wrote in the introduction to the book, “They have no evidence of poor health, relatives and friends do not sympathize with them, suggesting that they go to work or exert more willpower, many doctors find physically healthy and they say, 'You're just nervous, you're fine. '" Beard, on the other hand, argued that neurasthenia and nervous breakdowns are "real" disorders that need to be treated because they cause depression, sexual disorders and indigestion; people can become irritable, lose sleep, memory, and even begin to fear for their minds.
'" Beard, on the other hand, argued that neurasthenia and nervous breakdowns are "real" disorders that need to be treated because they cause depression, sexual disorders and indigestion; people can become irritable, lose sleep, memory, and even begin to fear for their minds.
Russian illustrated guide to Western European resorts, sea bathing, hospitals and cities. 1909
Beard recommended to treat nervous breakdowns primarily with sleep - "a natural restorer of a weary brain." And he called physical activities - hunting, playing golf or riding a bicycle - "pumping out blood" from an overstressed brain and distributing it throughout the body as the best sleep stimulants. But he categorically advised to avoid overwork: it, like mental overwork, wastes the finite supply of nervous energy in vain. Beard also advised patients to worry less ("It's not work that kills, it's worry") and more rest, avoiding mental stress. And for doctors, if necessary, use massage, hypnosis, treatment with water and electricity (Bird recommends static electricity as an almost indispensable remedy for insomnia and very useful for brain overstrain and alcoholism).
Neurasthenia was considered a disease of businessmen, intellectuals, writers and other members of the upper classes. Especially women from the upper classes: it was believed that they were more vulnerable due to "a weaker nervous system." Silas Weir Mitchell, one of Beard's supporters, generally believed that only two groups of people are susceptible to neurasthenia: businessmen working in a very competitive environment and socially active women.
Mitchell proposed a "rest cure", intended mainly for women, which eventually became the best known treatment for neurasthenia. For 6-8 weeks they were kept in bed, massaged and fed fatty foods; it was believed that the body needed "fat and blood" to produce nerve energy. But there were also more active methods of treatment: men and women were sent to forest boarding houses or ranches, where they ate fried meat, walked a lot and breathed fresh air. For those who could not afford a long and expensive vacation, temporary relief was offered through electric shock treatment in the doctor's office.
Russian illustrated guide to Western European resorts, sea bathing, hospitals and cities. 1909
At the same time, most of the largest and publicly accessible national parks in the United States were opened precisely in those years when neurasthenia became a "fashionable disease": they were considered excellent places for solitude and relaxation for neurasthenics. And the explosive growth in popularity of cycling, travel, and sports leagues was also largely due to people's belief that physical activity helps to avoid nervous exhaustion. But already at 19In the 1920s, the popularity of neurasthenia began to decline.
Much of the medical establishment has always been skeptical about this diagnosis: the idea of an immeasurable "nerve capital" seemed dubious to many. And by the end of the 1930s, the medical paradigm changed completely: doctors practically stopped diagnosing "neurasthenia", and its symptoms began to be considered as mental. Neurasthenia finally disappeared as a diagnosis after the Second World War. And in the 1960s, a sharp rise in accessible and mass psychiatry began, new drugs for the treatment of mental disorders appeared, and “nerve capital” and its depletion were no longer remembered.
And in the 1960s, a sharp rise in accessible and mass psychiatry began, new drugs for the treatment of mental disorders appeared, and “nerve capital” and its depletion were no longer remembered.
But, of course, people have not stopped having nervous breakdowns.
Why nervous breakdowns are needed
At its core, a nervous breakdown is a protective reaction to the mental stress that a person experiences, a kind of fuse. With the help of this state, the body relieves stress - often through tears, screams, aggression. And the tension really goes away - and this could even be called a plus of a nervous breakdown. But everything is more complicated: this defensive reaction works only in the moment, and if a person after a breakdown returns to the same environment or continues to experience the same stress, there is a high probability that breakdowns will be repeated.
Is it possible to avoid a nervous breakdown
Yes, in most cases a nervous breakdown can be prevented. In the life of a modern person, as a rule, an increased level of stress, but this does not make a breakdown inevitable. If you have time to relax, replenish resources and thus regularly reduce the level of tension, this will help prevent stress from developing into a nervous breakdown.
In the life of a modern person, as a rule, an increased level of stress, but this does not make a breakdown inevitable. If you have time to relax, replenish resources and thus regularly reduce the level of tension, this will help prevent stress from developing into a nervous breakdown.
Here are some preventive measures:
- Give yourself a full day off.
- Control the balance between work and leisure.
- Watch your diet so that it is regular and complete.
- Do whatever physical activity you can.
- Take regular walks in the fresh air.
- Interact with animals: play with cats and dogs, watch birds or even aquarium fish.
You may have your own methods to help you recover and return to a calm state - go for a massage or sauna, do active sports, light candles or an aromatic lamp, solve a puzzle or paint a picture by numbers. Use whatever works effectively and doesn't harm you.
Use whatever works effectively and doesn't harm you.
But what to do if a nervous breakdown does happen?
How to get out of a nervous breakdown
First of all, it is necessary to reduce the level of stress. You can be helped by simple and effective methods that are used to inhibit the sympathetic nervous system, which is activated during times of stress.
- Physical activity. Try running, doing some squats or push-ups. Do not overwork yourself: do physical exercises until you feel a little tired.
- Muscle tension and relaxation. Try to squeeze your hand tightly into a fist, and then relax it as much as possible. Do the same with the other hand, then try to alternately tense and relax different parts of the body.
- Cold water. You can wash your face with it or briefly apply ice to your face.
- Written or oral account. Start subtracting from a hundred by three or by seven, or write down a few examples that you can devote five to seven minutes of your time to.

- Breathing exercises. Deep breathing triggers the parasympathetic nervous system, which is responsible for reducing emotional and physical arousal. There are several techniques that work to help you deal with stress quickly.
If you think that you have had a nervous breakdown, you need to give yourself a break and reduce all stress: like after an illness, the body needs time to recover. Reduce all loads for a while; take a vacation or time off from work; postpone all non-urgent matters; get enough sleep.
It is advisable to consult a psychologist: psychotherapy will not only help reduce stress levels, but also speed up the process of overcoming a nervous breakdown. Methods such as cognitive behavioral therapy or emotional effectiveness therapy are recommended for quick recovery. Sometimes medications may be needed.
How to recover from a nervous breakdown
Find its causes . A nervous breakdown is an alarm signal with which the body makes it clear that the load on the psyche was excessive. If the causes of the breakdown are not removed, it may recur, but each time the psyche will be depleted and it will be worse to adapt to new stress. It is important to analyze the causes and check them for relevance.
If the causes of the breakdown are not removed, it may recur, but each time the psyche will be depleted and it will be worse to adapt to new stress. It is important to analyze the causes and check them for relevance.
Cognitive-behavioral psychologist and Psychodemic expert Alexandra Titareva recommends dividing all possible causes of stress into three groups:
- Problems you can deal with.
- Issues you can't do anything about.
- Problems that do not require your active participation.
Pay more attention to the first group: solving problems gives us satisfaction and confidence, this will reduce stress levels. And by focusing on issues that we have no control over, we will feel helpless.
Take care of yourself . The recommendations here will be very similar to the breakdown prevention measures listed above, with a greater focus on relaxation and "lazy" ways to rest. Sleep more, walk more, spend time with loved ones, take vacations if possible, don't demand too much from yourself.
Sleep more, walk more, spend time with loved ones, take vacations if possible, don't demand too much from yourself.
Clinical psychologist Ilya Gavin notes that a person gets used to tension in the body and stops feeling it. Even now, reading this text, you may not notice how tense your shoulders are until you pay attention to them. The tension that a person experiences before and during a nervous breakdown weakens his sense of the body and attention to it, the tension becomes his norm. It is important to pay attention to the sensations in the body, notice the physical tension and relax. Body practices and mindfulness practices will help with this.
Reduce (at least temporarily) your consumption of information. Alexandra Titareva notes that the excessive flow of information directly affects the decrease in emotional stability. Check if you spend too much time on the Internet or in front of the TV. Try to allocate small time slots for reading the main news of the day and stick to this schedule.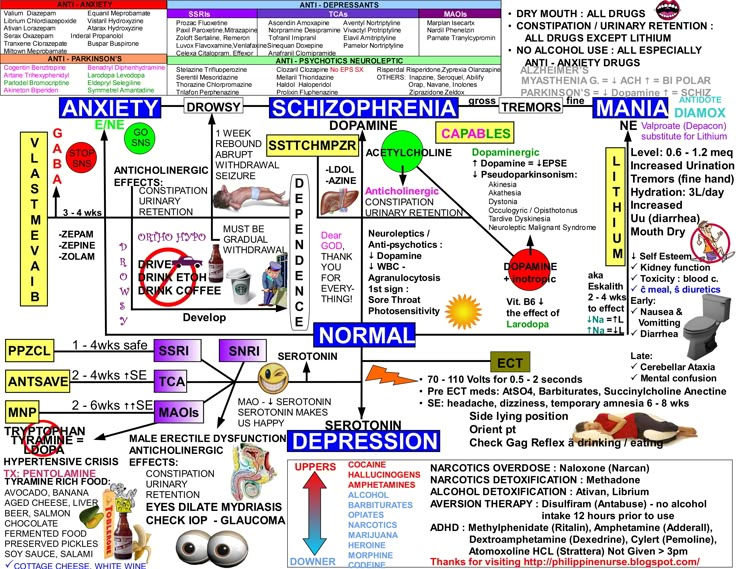
Curiously, most of the advice of Dr. Beard, who also disliked the press, is still relevant: doctors today recommend that people after a nervous breakdown avoid alcohol, coffee and other stimulants, eat better, sleep more and engage in physical activity for better sleep, but not moderately, to a slight pleasant fatigue.
Check your health . The stress that precedes a nervous breakdown in itself has a bad effect on health, and the consequences of a nervous breakdown can be manifested by a decrease in immunity, performance, cognitive functions, pain of unknown origin, and, in the presence of additional factors, strokes and heart attacks. After a little rest after a breakdown, make a health check: visit the main doctors, take basic tests, if you know your “weak points” in advance, check them.
What to read and listen to about how to deal with nervous breakdowns
- Free Psychodemic mini-course "How to live this fucking life".
- Article "How to distinguish 'normal anxiety' from an anxiety disorder.