Misdiagnosed as schizophrenia
Study Suggests Overdiagnosis of Schizophrenia
In a small study of patients referred to the Johns Hopkins Early Psychosis Intervention Clinic (EPIC), Johns Hopkins Medicine researchers report that about half the people referred to the clinic with a schizophrenia diagnosis didn’t actually have schizophrenia. Schizophrenia is a chronic, severe and disabling disorder marked by disordered thinking, feelings and behavior. People who reported hearing voices or having anxiety were the ones more likely to be misdiagnosed.
In a report of the study in the March issue of the Journal of Psychiatric Practice, the researchers say that therapies can vary widely for people with schizophrenia, bipolar disorder, major depression or other serious types of mental illness, and that misdiagnosis can lead to inappropriate or delayed treatment.
The findings, the researchers say, suggest that second opinions at a specialized schizophrenia clinic after initial diagnosis are wise efforts to reduce the risk of misdiagnosis, and ensure prompt and appropriate patient treatment.
“Because we’ve shined a spotlight in recent years on emerging and early signs of psychosis, diagnosis of schizophrenia is like a new fad, and it’s a problem especially for those who are not schizophrenia specialists because symptoms can be complex and misleading,” says Krista Baker, L.C.P.C., manager of adult outpatient schizophrenia services at Johns Hopkins Medicine. “Diagnostic errors can be devastating for people, particularly the wrong diagnosis of a mental disorder,” she adds.
According to the National Institute of Mental Health, schizophrenia affects an estimated 0.5 percent of the world population, and is more common in men. It typically arises in the late teens, 20s and even as late as the early 30s in women. Symptoms such as disordered thinking, hallucinations, delusions, reduced emotions and unusual behaviors can be disabling, and drug treatments often create difficult side effects.
The new study was prompted in part by anecdotal evidence among health care providers in Baker’s specialty clinic that a fair number of people were being seen who were misdiagnosed. These patients usually had other mental illnesses, such as depression.
These patients usually had other mental illnesses, such as depression.
To see if there was rigorous evidence of such a trend, the researchers looked at patient data from 78 cases referred to EPIC, their specialty clinic at Johns Hopkins Bayview Medical Center, for consultation between February 2011 and July 2017. Patients were an average age of 19, and about 69 percent were men. Seventy-four percent were white, 12 percent African American and 14 percent were another ethnicity. Patients were referred to the clinic by general psychiatrists, outpatient psychiatric centers, primary care physicians, nurse practitioners, neurologists or psychologists.
Each consultation by the clinic took three to four hours, and included interviews with the patient and the family, physical exams, questionnaires, and medical and psychosocial histories.
Of the patients referred to the clinic, 54 people came with a predetermined diagnosis of a schizophrenia spectrum disorder. Of those, 26 received a confirmed diagnosis of a schizophrenia spectrum disorder following their consultation with the EPIC team, which is composed of licensed clinicians and psychiatrists. Fifty-one percent of the 54 cases were rediagnosed by clinic staff as having anxiety or mood disorders. Anxiety symptoms were prominent in 14 of the misdiagnosed patients.
Fifty-one percent of the 54 cases were rediagnosed by clinic staff as having anxiety or mood disorders. Anxiety symptoms were prominent in 14 of the misdiagnosed patients.
One of the other most common symptoms that the researchers believe may have contributed to misdiagnosis of schizophrenia was hearing voices, as almost all incorrectly diagnosed patients reported auditory hallucinations.
“Hearing voices is a symptom of many different conditions, and sometimes it is just a fleeting phenomenon with little significance,” says Russell L. Margolis, M.D., professor of psychiatry and behavioral sciences and the clinical director of the Johns Hopkins Schizophrenia Center at the Johns Hopkins University School of Medicine. “At other times when someone reports ‘hearing voices’ it may be a general statement of distress rather than the literal experience of hearing a voice. The key point is that hearing voices on its own doesn’t mean a diagnosis of schizophrenia.”
In speculating about other reasons why there might be so many misdiagnoses, the researchers say that it could be due to overly simplified application of criteria listed in the Diagnostic Statistical Manual of Mental Disorders, a standard guide to the diagnosis of psychiatric disorders.
“Electronic medical record systems, which often use pull-down diagnostic menus, increase the likelihood of this type of error,” says Margolis, who refers to the problem as “checklist psychiatry.”
“The big take-home message from our study is that careful consultative services by experts are important and likely underutilized in psychiatry,” says Margolis. “Just as a primary care clinician would refer a patient with possible cancer to an oncologist or a patient with possible heart disease to a cardiologist, it’s important for general mental health practitioners to get a second opinion from a psychiatry specialty clinic like ours for patients with confusing, complicated or severe conditions. This may minimize the possibility that a symptom will be missed or overinterpreted.”
Margolis cautioned that the study was limited to patients evaluated in one clinic. Nonetheless, he was encouraged by the willingness of so many patients, their families and their clinicians to ask for a second opinion from the Johns Hopkins clinic. If further study confirms their findings, it would lend support to the belief by the Johns Hopkins team that overdiagnosis may be a national problem, because they see patients from across the country who travel to Johns Hopkins for an opinion. They hope to examine the experience of other specialty consultation clinics in the future.
If further study confirms their findings, it would lend support to the belief by the Johns Hopkins team that overdiagnosis may be a national problem, because they see patients from across the country who travel to Johns Hopkins for an opinion. They hope to examine the experience of other specialty consultation clinics in the future.
Chelsey Coulter of the University of Pittsburgh is also an author on the study.
The study was funded in part by the ABCD Charitable Trust.
Margolis receives grant support from Teva Pharmaceuticals for an unrelated project.
- From Grassroots to EPIC Psychosis Treatment
Patients Are Commonly Misdiagnosed with Schizophrenia
Russell L. Margolis, MD
Schizophrenia may have become a trigger-happy diagnosis.
A retroactive analysis of patients referred to a psychiatry consultation clinic with an initial schizophrenia diagnosis found that about half of all such diagnoses were inaccurate upon further review.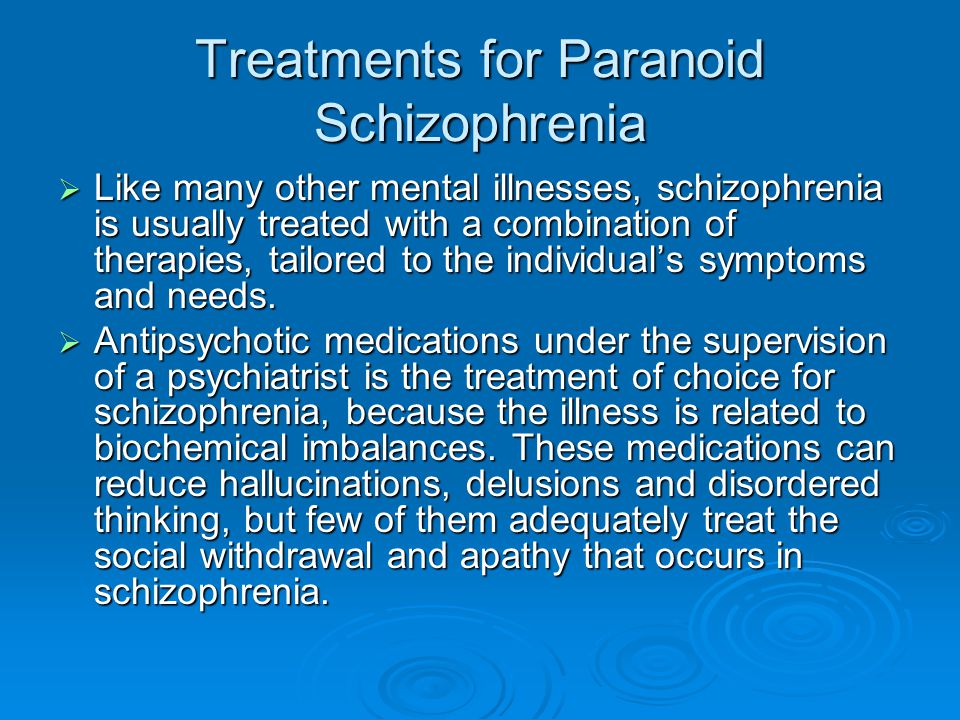
The study, from the Johns Hopkins Early Psychosis Intervention Clinic (EPIC), reported that a multitude of factors may influence a physician too readily diagnosing a patient with schizophrenia—not the least of which being a desire to treat the chronic psychiatric condition with speed and efficacy.
“Early detection of schizophrenia is very important, so the patient can get the correct pharmacologic and non-pharmacologic care they need to stay on the best possible path of their life,” study author Russell L. Margolis, MD, told MD Magazine®.
Margolis, a professor of Psychiatry and Behavioral Sciences, and clinical director of the Johns Hopkins Schizophrenia Center at the Johns Hopkins University School of Medicine, said his team’s findings reflect trends among first-line clinicians, referral psychiatrists, and even flawed electronic medical record (EMR) devices.
The investigators conducted a retroactive chart review of 78 patients who has been referred to EPIC with an early psychosis diagnosis.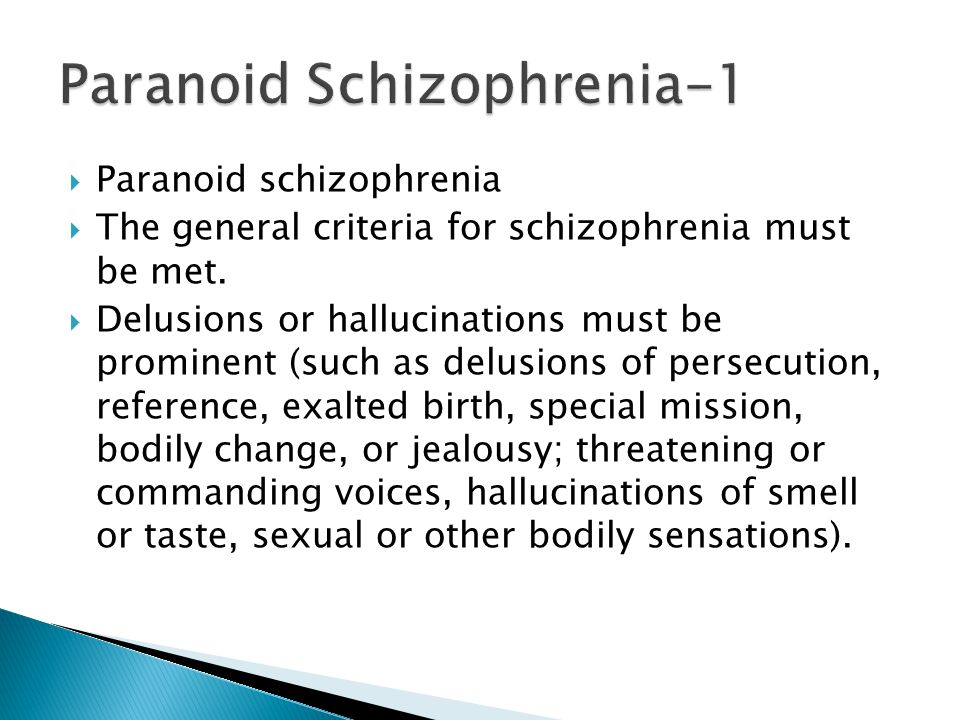 Of the 78 observed patients, 43 (55%) had a primary diagnosis of schizophrenia spectrum disorder at the time of their referral. Among those 43 cases, 22 (51%) concluded with a different diagnosis following the consultation, and 18 (43%) were not diagnosed with any form of primary psychotic disorder.
Of the 78 observed patients, 43 (55%) had a primary diagnosis of schizophrenia spectrum disorder at the time of their referral. Among those 43 cases, 22 (51%) concluded with a different diagnosis following the consultation, and 18 (43%) were not diagnosed with any form of primary psychotic disorder.
The most common patients to be misdiagnosed with schizophrenia were in their teens and 20s with symptoms of anxiety, Margolis said. He explained that these patients could have been the byproduct of what he calls “checklist psychiatry.”
“A patient says he hears voices,” Margolis explained. “It becomes very easy in the EMR to check off them as ‘positive’ for hallucinations. But hearing voices can mean many, many things.”
Having a broad symptom such as hearing voices—which could be a sign of distress in a patient with anxiety issues, or just a fleeting symptom of another psychiatric condition—be assessed in a binary fashion is a disservice to referred patients, Margolis said.
“There can be an overreaction to mental health conditions,” he explained.
That said, the findings equally emphasize the value of specialty consultations as much they do the pitfalls of first-line diagnoses and referrals. While a primary care provider frequently refers patients with cancer to an oncologists and patients with chest pains to a cardiologist, patients presenting with mental health issues are less likely to seek further consultation.
That’s an issue, as psychiatry diagnoses take longer than a routine primary care visit to properly assess, and clinicians are trained to be alert for early-onset psychiatric conditions such as schizophrenia.
“Forty-five minutes is not enough to sort out the care,” Margolis said. “We have to have time to sort out the diagnoses. It’s a great luxury in a consultation clinic like ours, to have hours to spend on a patient at a time.”
Investigators concluded that misdiagnosed patients were more likely to report symptoms of anxiety than they were thought disorder, and that second opinions from specialty clinics could negate the increased rate of false schizophrenia diagnoses.
Margolis said the team is currently examining long-term outcomes and experiences for patients who undergo such specialty consultations, though no data is yet available.
The study, "Specialized Consultation for Suspected Recent-onset Schizophrenia," was published online in Journal of Psychiatric Practice.
Myths about the diagnosis of mental illness
There are a huge number of myths around mental illness and its diagnosis. Including, because modern science is just beginning to learn how the brain works and how the human psyche works, and making a diagnosis does not seem like the most trivial task. Below we refute some misconceptions about the processes and results of diagnosis in modern psychiatry.
To diagnose a mental illness, it is enough to scan the brain. It is a myth. If the best specialist is shown an MRI image and does not provide information about the patient, the specialist will most likely make an erroneous diagnosis.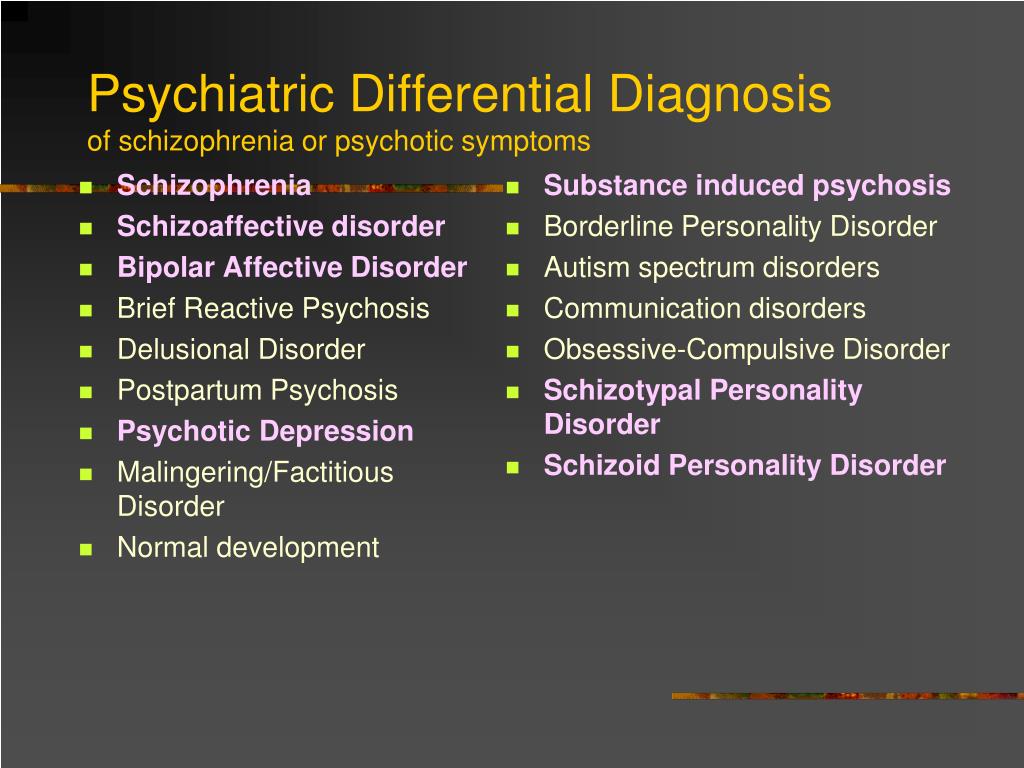 A brain scan may only be effective in making a diagnosis after a clinical interview with a psychiatrist or psychotherapist.
A brain scan may only be effective in making a diagnosis after a clinical interview with a psychiatrist or psychotherapist.
See also
Myths about hypnosis
Schizophrenia can be diagnosed and treated by brain oxygenation. No, it's not. In the early 1990s, the Hebrew University of Jerusalem conducted a study aimed at studying the treatment of schizophrenia using this method. The study did not give concrete results, but became known to the whole world. This has led to the misconception that oxygenation of the brain can diagnose and treat schizophrenia.
A mental disorder can be detected by a blood test. It is a myth. Some time ago, scientists assumed that there are substances in the blood that are inherent in certain psychiatric diseases, such as depression or schizophrenia. However, such studies have not revealed specific relationships between blood elements and mental disorders.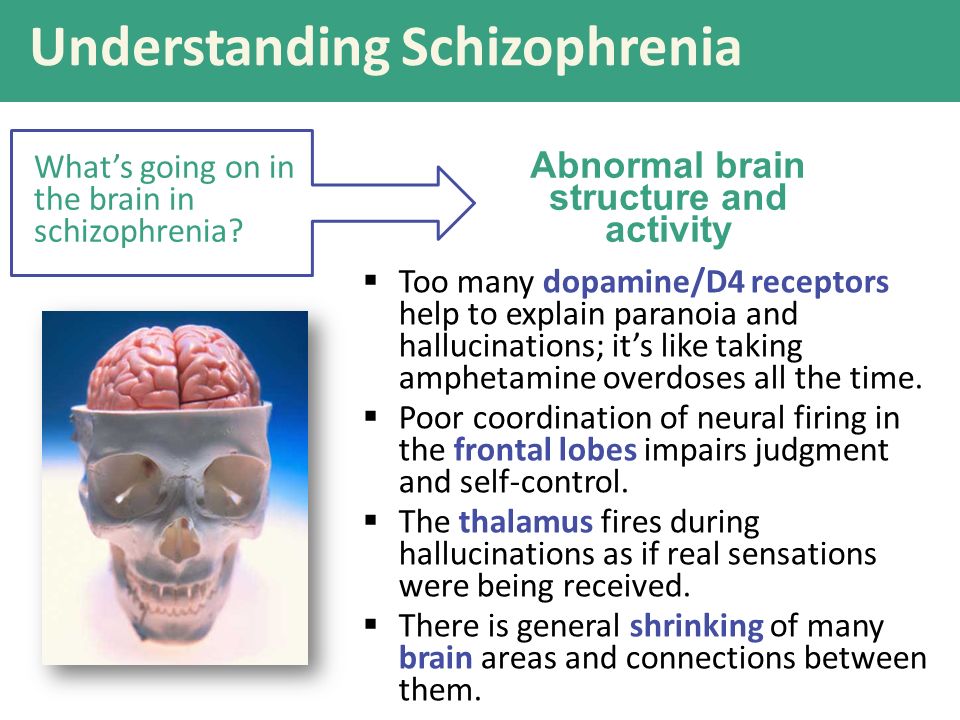
Mental illness can be diagnosed by looking at the human genome. This is not true. Every year, scientists discover more and more new genes, but at the moment, science does not have enough data to diagnose mental illness using genetic tests.
One conversation with a psychiatrist is enough to diagnose the disease. It is not always so. For the diagnosis of major psychiatric diseases, it is enough for the patient to communicate with 1 or 2 specialists. In most cases, this is a psychotherapist and / or a psychiatrist. In more complex cases, you may need the help of a neurologist, endocrinologist, psychologist and other specialists. The more obscure the mental picture, the more specialists are needed to make a diagnosis.
Tests conducted by psychologists to make a diagnosis are not objective. Yes and no. When conducting any psychological test, there is a possibility of obtaining distorted and inaccurate results. However, over the past 20 years, psychologists have greatly improved their test-taking skills and learned how to get the most objective results.
However, over the past 20 years, psychologists have greatly improved their test-taking skills and learned how to get the most objective results.
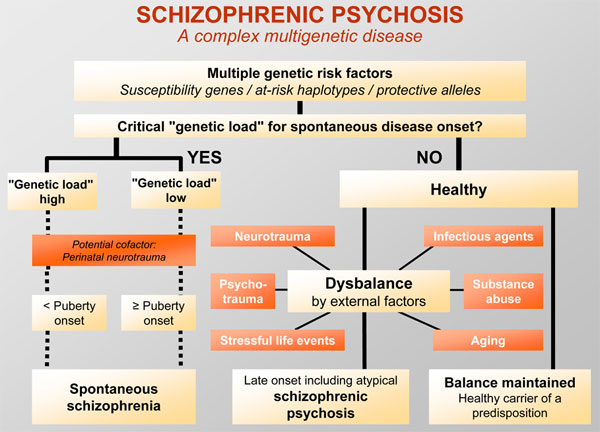
If one of the patient's relatives had a mental illness, it will certainly manifest itself in the patient himself. It's not obligatory. What is inherent in genetics may manifest itself under the influence of external triggers, or it may not manifest itself at all. If a person has the genes for a mental illness, it is not at all necessary that he will be in such social conditions that activate the manifestation of this disease.
See also
Myths about autism
Mental disorder can be identified by the type of person's character. No. If a person has a certain personality structure, it is not at all necessary that he will manifest some kind of mental illness. For example, a schizoid personality type does not guarantee the occurrence of schizophrenia. And even a personality disorder does not necessarily indicate the presence of mental illness.
And even a personality disorder does not necessarily indicate the presence of mental illness.
To date, any mental disorder can only be identified on the basis of a clinical interview - a meeting between a doctor and a patient. No laboratory tests can make a complete diagnosis. At the moment, in psychiatry, it is not possible to make a diagnosis only with the help of MTP, blood tests or genetic testing.
- Diagnosis
Share:
10 questions about schizophrenia - Gazeta.Ru
Are people with schizophrenia dangerous? Are they boisterous? Hear voices? Are they isolated from society? "Gazeta.Ru" answers questions that are formed by common myths about schizophrenia. This material is conceived as an educational program with the aim of destigmatizing the diagnosis of schizophrenia. With its help, we would like to convey the thesis that the diagnosis of schizophrenia is not a final verdict, and ordinary life is possible with it.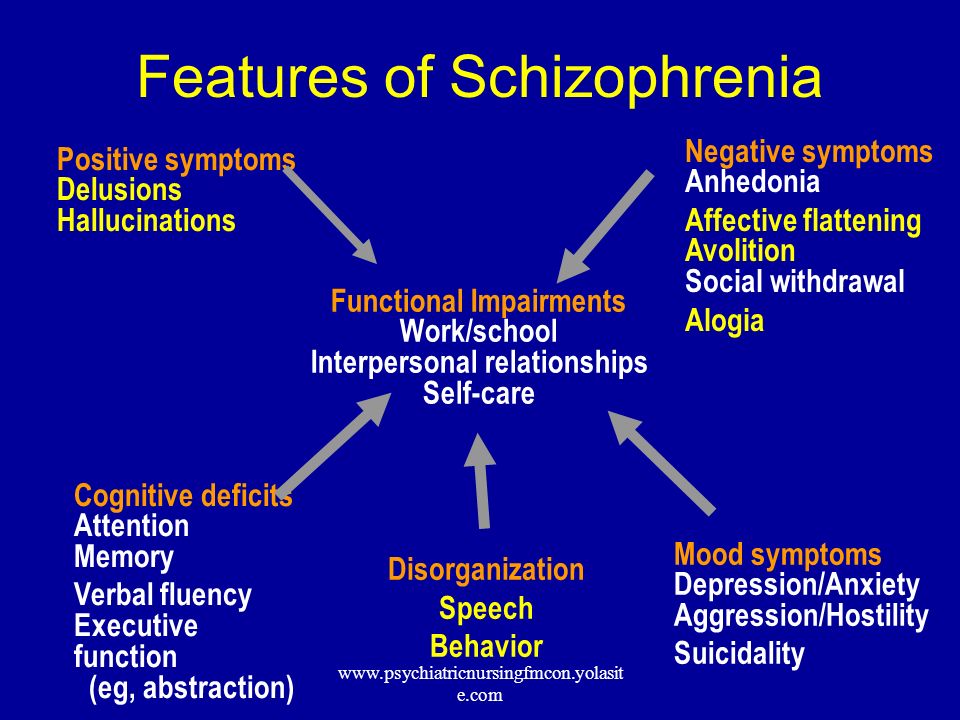
1. Who is to blame if a person develops schizophrenia?
Medicine does not yet know what causes the disorder. It is assumed that this is a coincidence of genetic factors, violations of chemical processes in the brain and environmental influences.
Scientists cannot examine and evaluate the processes that take place in the brain of people diagnosed with schizophrenia. But the studies that are already available have shown that in this disease there are problems in the work of neurotransmitters, mainly dopamine. These are substances through which impulses are transmitted from one nerve cell to another. The brain and central nervous system are also somewhat altered in this disorder. But how these changes affect and when they develop is still unknown.
2. Is there any way I can tell if I or a loved one has schizophrenia?
Diagnosing schizophrenia in oneself is quite difficult: people with a mental disorder most often do not realize that something is wrong with them.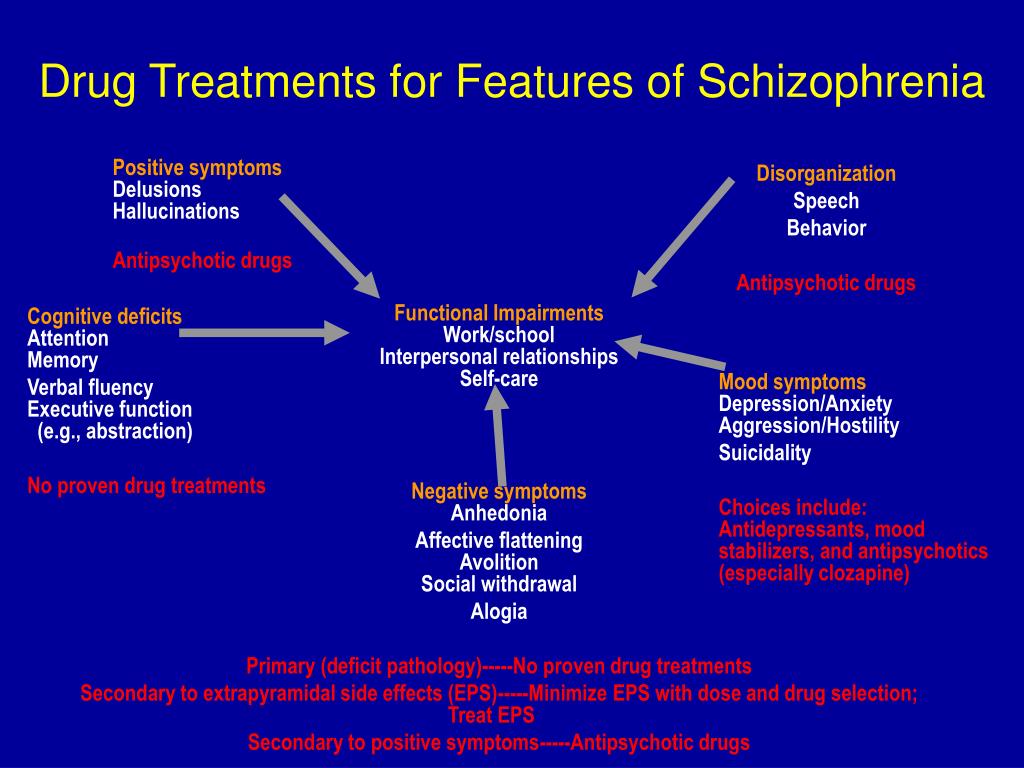 Relatives and friends of the sick person who notice changes in behavior, thinking, habits, and reactions often turn to specialists.
Relatives and friends of the sick person who notice changes in behavior, thinking, habits, and reactions often turn to specialists.
The first signs of the disease can not always be recognized precisely as pathological. A person can joke strangely, move away from people and the professional community. He can talk about unusual feelings and experiences, share unusual ideas and try to implement them. In general terms, his behavior can be described as follows: a closed eccentric, convinced of his inventions. Perhaps this is just a temporary state caused by some kind of experience or stress. But sometimes schizophrenia begins with such non-obvious symptoms.
3. How do people behave when they definitely have schizophrenia?
The disease manifests itself differently in everyone, in different combinations of symptoms and complaints. If relatives or the person himself notice that his (her) condition has signs of a mental disorder, then you need to contact a specialist - only he can diagnose and distinguish one disease from another with similar symptoms.
In general, symptoms of schizophrenia may include:
- Delirium. A person begins to think that something is happening that is related to him or to the world around him: as if someone is watching him, persecuting him, trying to harm him, slander, offend him. It may seem to a patient with schizophrenia that someone has written down thoughts, conversations, texts, tasks in his head and made him think about it, pronounce it, decide it. He is sure that others also hear what is going on in his head, and tries to communicate on this topic. For some, information “appears” that something tragic, dangerous is about to happen in the country, in the world, on Earth. The most important thing is that a person sincerely believes in the reality of all this.
- Hallucinations. These are false auditory, tactile, visual sensations. A person with schizophrenia lives them, for him they are real.
- Negative symptoms. What is listed above is called productive symptoms - they were brought by the disease, this is its product.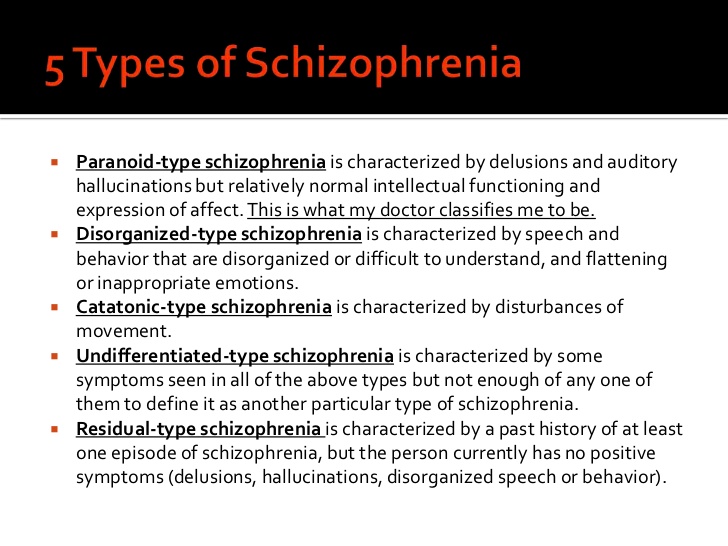 Negative symptoms are those that the disease takes away, minus from the life of the sick person. The liveliness of movements, energy, will, desire to do something, to communicate disappear. A patient with schizophrenia may not want anything, he (she) is not interested in anything, he (she) ceases to take care of himself and observe the simplest hygiene.
Negative symptoms are those that the disease takes away, minus from the life of the sick person. The liveliness of movements, energy, will, desire to do something, to communicate disappear. A patient with schizophrenia may not want anything, he (she) is not interested in anything, he (she) ceases to take care of himself and observe the simplest hygiene.
- Disorders of thinking and speech. For others, they look like a "salad of thoughts and words." The sick person may ask questions to himself or receive them from others, begin to answer and get confused in words.
- Unusual behavior. A person becomes characterized by childishness, antics, frozen postures or, conversely, fussy and meaningless movements, which often do not fit either with the situation, or with the environment, or with the tasks.
4. So, if my friend has these symptoms, then he (she)…?
Not always. Yes, and one symptom from this description, and a combination of several, may indicate schizophrenia, but in the same way they can be disguised as manifestations of a completely different disorder.
close
100%
A non-specialist should not suspect schizophrenia in a person. Even experienced professionals conduct many examinations and tests before making a diagnosis. Therefore, the best tactic in this case is to convince to visit a specialist.
5. It seems that this happened to my loved one. Will he be sent to a psychiatric hospital now?
Optional. Schizophrenia can proceed in different ways, many are successfully treated only at home, on an outpatient basis. If the behavior of your loved one has changed and has become a concern, then do not invent diagnoses, and even more so do not voice the assumption to outsiders. Talk to the person himself, find out what he feels and what worries him. And together with him, sign up with a specialist if you understand that he:
- has become suspicious, listens to something, checks something;
- suddenly loses the thought or thread of the conversation, cuts off speech in mid-sentence or does not complete the matter;
- has problems with social adaptation (cannot perform the simplest actions - for example, buy groceries in a store).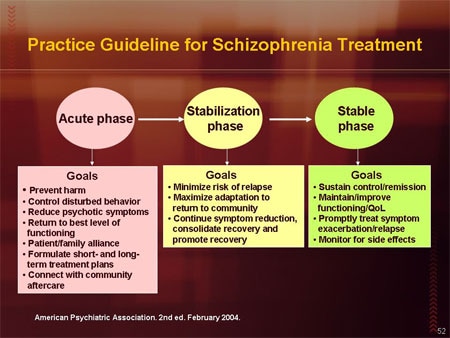
Unfortunately, the circumstances of the disease develop in such a way that from the very beginning the sick person needs help and support from relatives and friends. And it starts with the need to convince him to go to a specialist.
You may have seen the movie A Beautiful Mind. It was created based on the life story of a real-life American mathematician, scientist and Princeton University professor John Nash. He had schizophrenia, which caused his strange behavior, but did not lead to the loss of the ability to think scientifically. The film shows well how the support of loved ones helped John Nash.
This is, of course, an isolated example, but it shows that it is wrong to equate schizophrenia with complete loss of reason. The disease can proceed in different ways, the treatment can be so effective that a person will live almost the same as before.
6. Registration
It's not a shame. This is right and necessary: everyone should receive treatment for their disease. Help for schizophrenia is provided by a specialist, and accounting is a diary of monitoring the course of the disease. It has long been understood abroad that only treatment and control help many people with schizophrenia avoid difficult life situations (vagrancy, alcohol or drug abuse), notice a relapse (return of symptoms) in time, and return to remission.
Help for schizophrenia is provided by a specialist, and accounting is a diary of monitoring the course of the disease. It has long been understood abroad that only treatment and control help many people with schizophrenia avoid difficult life situations (vagrancy, alcohol or drug abuse), notice a relapse (return of symptoms) in time, and return to remission.
7. So now you are on pills all your life?
That would be perfect! If loved ones can convince a person with schizophrenia to take prescribed medications and come to check-ups on time, then symptoms can be controlled and a relapse can be prevented.
8. What does “under control” mean? Don't pills cure?
To control means, with the help of drugs and additional methods (psychotherapy, for example), to make the symptoms of the disease affect life as little as possible. This is called remission. With a favorable course of the disease, remission on medications can be such that a person will remain in society, will live almost the same as before the diagnosis.
close
100%
Some people with this condition manage to take control of their medication and treatment. But still, most need support from loved ones, compassion without obsession and excessive anxiety. In practice, this can be a donated pill box, in which the desired drug is pre-filled. Or creating a calm environment in the house and a joint visit to a psychotherapist. Or daily walks and organizing participation in household chores so that a person does not feel excluded from family life and does not concentrate on experiences.
9. When can a person be considered healthy?
There is no cure for schizophrenia yet. And there are quite a few diseases that can only be brought into remission with the help of drugs: for example, diabetes mellitus or hypertension - people have to take drugs all their lives, but no one considers them defective.
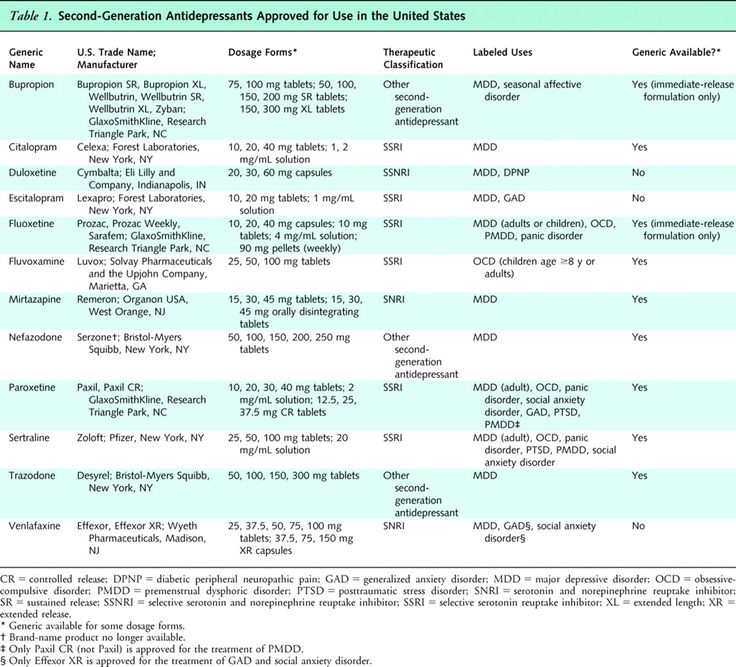
And, of course, the scientific world is looking for, developing, testing drugs that can work as efficiently as possible. For example, in Russia there is a drug from the pharmaceutical company Gideon Richter, which can help fight productive and negative symptoms and make it possible to live more harmoniously in society.
For example, in Russia there is a drug from the pharmaceutical company Gideon Richter, which can help fight productive and negative symptoms and make it possible to live more harmoniously in society.
10. They say that people with this diagnosis can suddenly attack, try to kill, do they become strong like animals?
There are factors that can lead to an outbreak of aggression. But this does not mean that the sick are just waiting for someone to attack. If you had to deal with this, then protect the patient (close the windows, turn off the gas, take away knives and matches, etc.), yourself, family members, animals and call an ambulance, telling what is happening. There is no need to enter into disputes with the patient, mock, demand to calm down or remember the techniques of martial arts. Stay calm, speak in a calm voice.
According to various data obtained by foreign researchers, people with schizophrenia commit 5 to 10% of crimes related to aggression or violence.