Misconception about schizophrenia
Six Common Myths and Misconceptions About Schizophrenia
Split personality. Violent behavior. Never being able to hold onto a job or have a career. Myths abound about schizophrenia, a serious and complex mental disorder currently affecting about 1 percent of American adults.
Patients diagnosed with schizophrenia do not present with a split personality, nor is it common for someone with the disorder to be violent, says Simon Rego, PsyD, chief psychologist at Montefiore Medical Center and Associate Professor of Psychiatry and Behavioral Sciences at Albert Einstein College of Medicine in New York City. And many individuals with schizophrenia are able to work.
Here, experts dispel some of the more common myths about schizophrenia.
#1 Myth: Schizophrenia means you have a split personality.
Reality: “This is a classic myth,” Dr. Rego says. A split personality, also called a Dissociative Identity Disorder or a Multiple Personality Disorder, is extraordinarily rare, he explains. It is quite distinct from schizophrenia, he says. “Schizophrenia is a thought disorder,” he explains, “The myth likely stems from the fact that in schizophrenia there is a breakdown, or split, between thoughts, emotions, and behavior.”
This split results in the person confusing reality and fantasy, Dr. Rego explains. “The person may experience delusions and hallucinations, and emotions may become blunted or inappropriate,” he explains. When most people think of schizophrenia, they think of someone who is seeing things and hearing voices, Dr. Rego points out. “These are what are called positive symptoms, but people with schizophrenia have negative symptoms, too,” he says. Among the common negative symptoms are low motivation, difficulty forming social connections, and a flat, blunted affect, Dr. Rego says. A lack of pleasure in everyday activities, rarely speaking, and difficulty paying attention are also symptoms, according to the American Psychological Association.
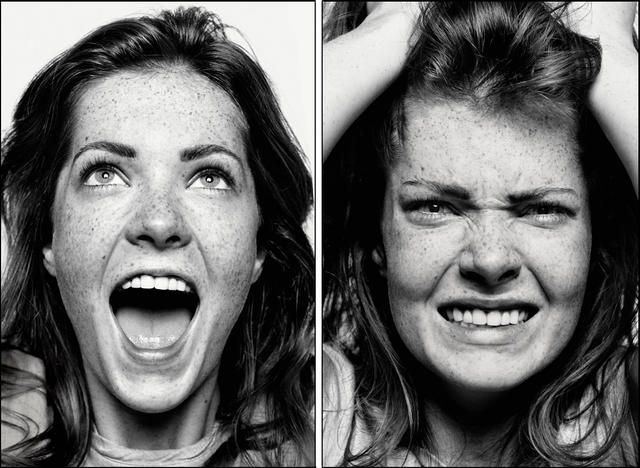
#2 Myth: Violence is common among individuals with schizophrenia.
Reality: It’s actually rare for someone with schizophrenia to be violent, says Dr. Rego. An individual with schizophrenia is much more likely to be the victim of violence rather than the perpetrator, he says. “They tend to struggle more to have the social benefits that most of us have,” Dr. Rego explains. “They may be homeless or staying in a shelter, where they may be singled out and assaulted.”
Some individuals with psychiatric disorders like schizophrenia do become aggressive, says Scott Ira Krakower, DO, assistant unit chief of psychiatry at Zucker Hillside Hospital in Glen Oaks, New York. “However, it is a myth that this is always the case,” he says. “A person can be aggressive and have an anger problem and not have schizophrenia,” he explains. Both medication and counseling can help with any signs of violent behavior, he says.
#3 Myth: People with schizophrenia can’t ever hold down a job.
Reality: Actually, some individuals, when stable, are able to function quite well, Dr. Rego says. “When they are being compliant with their medication and are engaged in some sort of psychosocial treatment, they are often quite functional,” he says. The National Alliance on Mental Illness estimates that as many as half of the two million Americans with schizophrenia can improve significantly or even recover completely if they get treatment. Dr. Rego refers to the “recovery model” of treatment for schizophrenia, and an article in the Current Opinion in Psychiatry.
Rego says. “When they are being compliant with their medication and are engaged in some sort of psychosocial treatment, they are often quite functional,” he says. The National Alliance on Mental Illness estimates that as many as half of the two million Americans with schizophrenia can improve significantly or even recover completely if they get treatment. Dr. Rego refers to the “recovery model” of treatment for schizophrenia, and an article in the Current Opinion in Psychiatry.
“Working appears to help people recover from schizophrenia, and recent advances in vocational rehabilitation have been shown to be effective in countries with differing economies and labor markets. A growing body of research supports the concept that empowerment is an important component of the recovery process,” the authors write.
About a quarter of young people with the disorder recover when treated within six months to two years, reports the American Psychological Association, and another 35 to 40% percent are improved enough after longer-term treatment to live fairly normal lives with only minor symptoms.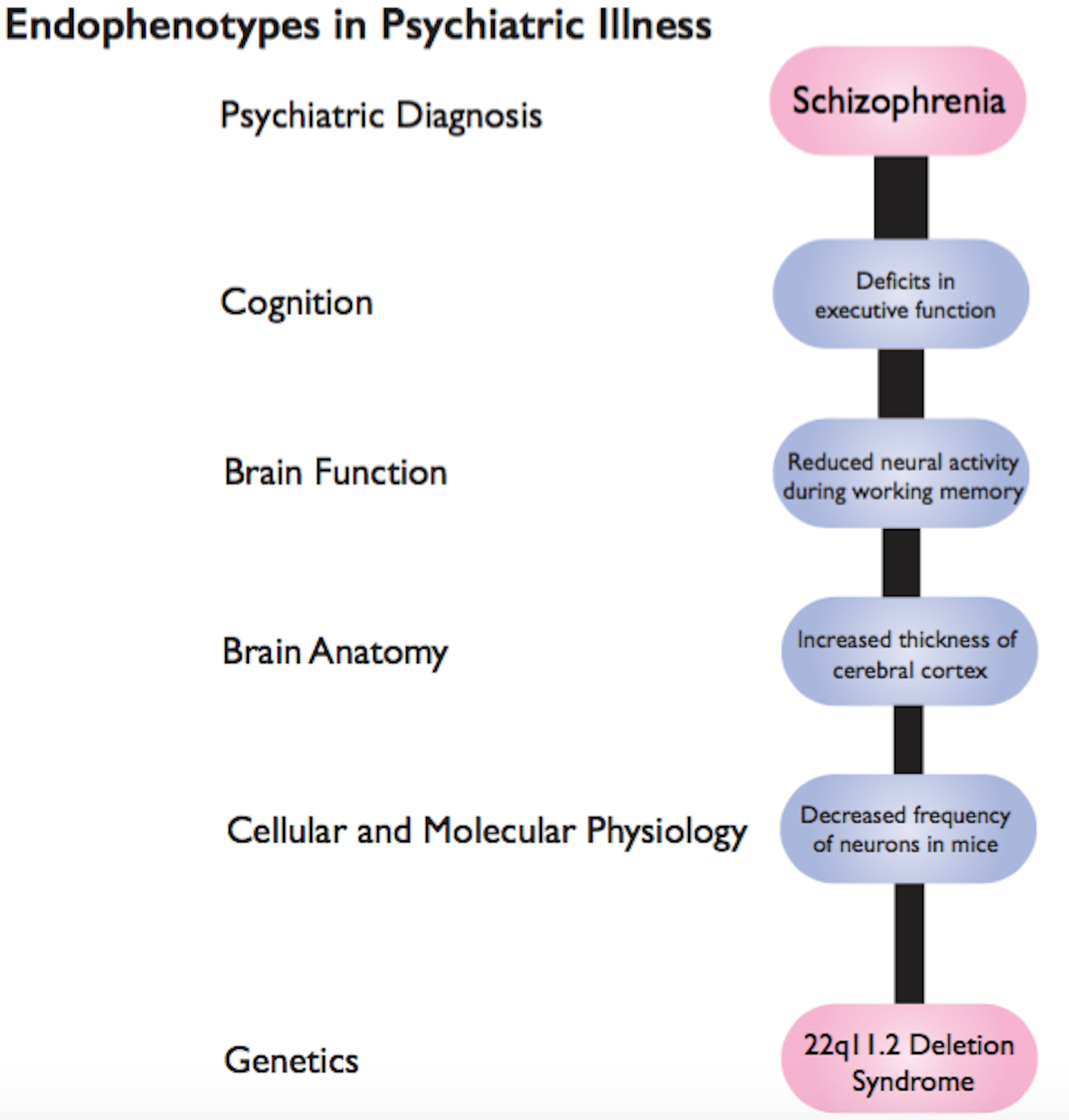 What makes this possible is psychosocial support—psychotherapy, family education, and self-help groups that can help people with schizophrenia cope and regain their lives. Job training and vocational counseling also can be useful. Still, cautions Dr. Krakower, some patients have difficulty holding down a job. “And it’s okay for them to get additional treatment,” he says. “Sometimes they may need to be on disability, and that’s okay, too.”
What makes this possible is psychosocial support—psychotherapy, family education, and self-help groups that can help people with schizophrenia cope and regain their lives. Job training and vocational counseling also can be useful. Still, cautions Dr. Krakower, some patients have difficulty holding down a job. “And it’s okay for them to get additional treatment,” he says. “Sometimes they may need to be on disability, and that’s okay, too.”
#4 Myth: A person with schizophrenia can seem perfectly normal one moment and change into a different person the next.
Reality: A sudden dramatic change of character in individuals with schizophrenia is not the usual scenario, Dr. Rego says. In fact, it’s common for the signs and symptoms of this mental disorder to surface over time. “There are often soft signs that the illness is going to take root,” Dr. Rego says. In the typical progression of the illness, a person may first become flat, isolate more frequently, and decrease their participation in activities.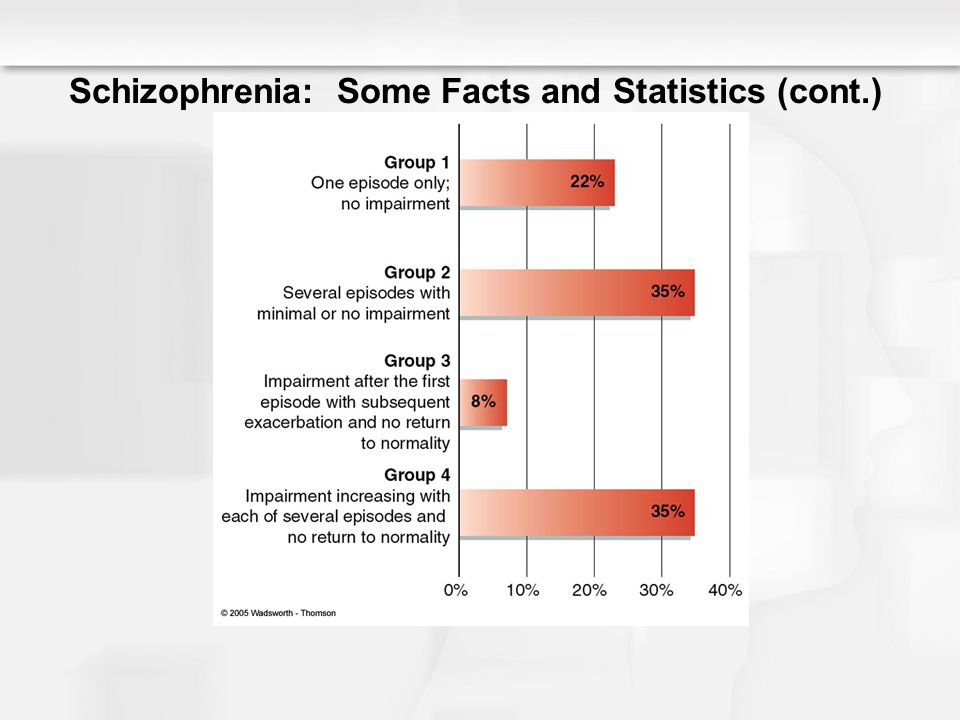 Then a psychotic break could occur—from a stressor such as starting college, Dr. Rego says. “So it is more of a slow progression, with a waxing and waning course that occurs over months and years,” he explains.
Then a psychotic break could occur—from a stressor such as starting college, Dr. Rego says. “So it is more of a slow progression, with a waxing and waning course that occurs over months and years,” he explains.
#5. Myth: People with schizophrenia usually require long-term hospitalization.
Reality: Appropriate treatment today may include a combination of out-patient care, acute hospitalization, and longer-term hospitalization when needed, Dr. Krakower says. And, even when family support and financial resources are available, many patients still need inpatient treatment, he adds.
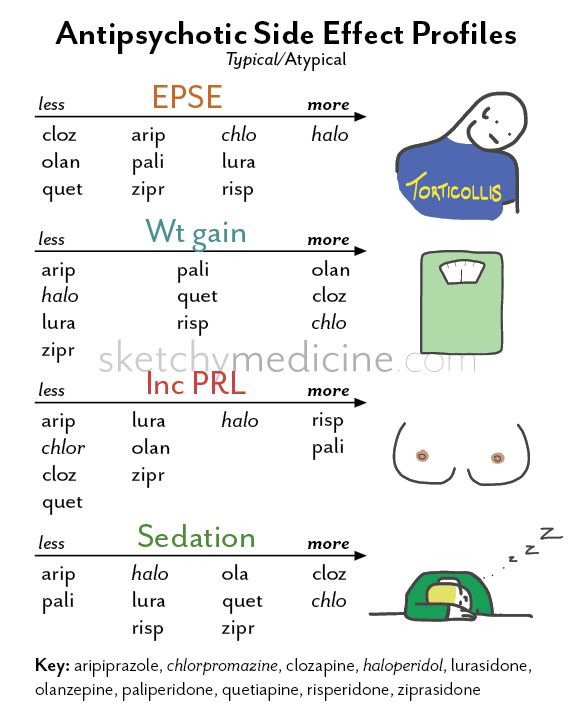
“But the treatment model for schizophrenia is moving away from longer-term hospitalization and toward outpatient treatment,” he says. “At times, individuals may benefit from going to a day program or a partial day hospital, where they can receive daily treatment. Therapy may vary from individual to group therapy and the medication of choice is usually second-generation antipsychotic agents (i.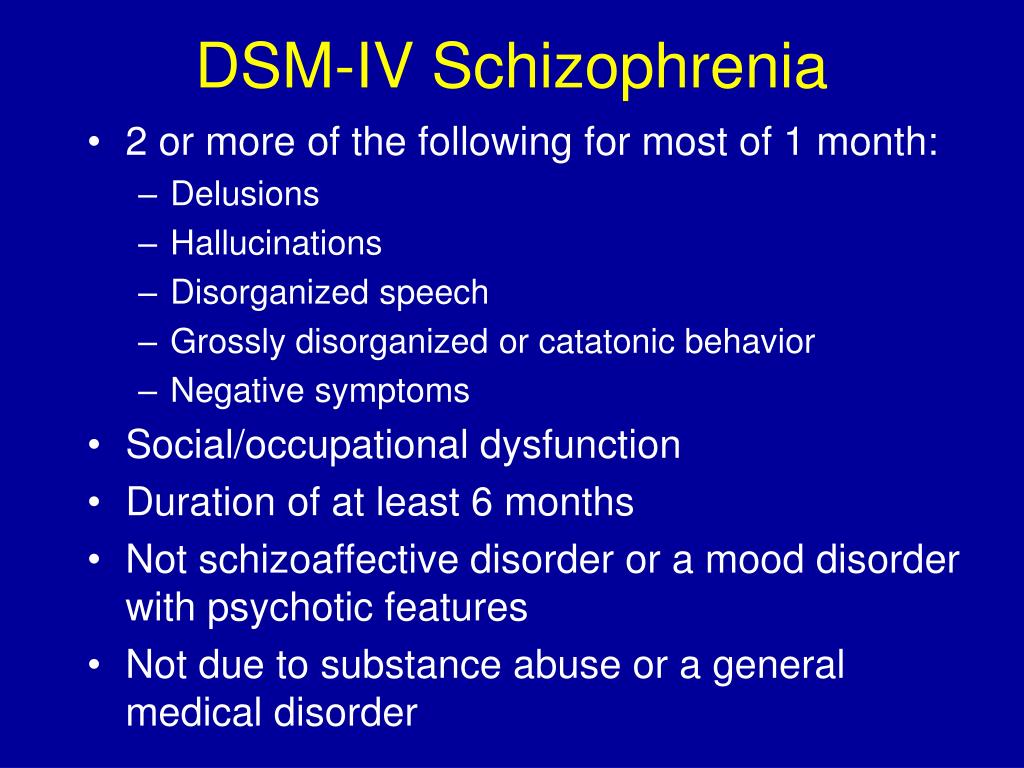 e. aripiprazole, clozapine, and risperidone).”
e. aripiprazole, clozapine, and risperidone).”
In a longer-care setting, the time can vary from weeks to months and depends on how the patient is progressing, Dr. Krakower says.
Long-term hospitalization may also be an indication that the person isn't getting enough support. “In some cases, society has failed them,” says Stephen Ferrando, MD, Director of Psychiatry at Westchester Medical Center Health Network (WMCHealth). “We are not providing enough services for them to succeed.”
#6. Myth: Bad parenting is what causes schizophrenia.
Years ago, it was believed that the mother or both parents were responsible if the child developed schizophrenia, Dr. Rego explains. While there is a genetic susceptibility—the disorder tends to run in families—there is absolutely no evidence that it is caused by how a person is parented, he says.
“Plus, even if your parent has schizophrenia your chances of getting it are less than 25 percent,” Dr. Ferrando explains.
So what does cause it? Rather than a single gene for schizophrenia, it’s likely that various genes, as well as environmental factors, are responsible, according to the American Psychological Association.
Environmental factors that may trigger the onset of schizophrenia can range from extreme academic stress to substance abuse. Dr. Ferrando says. “We know that extreme environmental stress like these situations can trigger the onset of schizophrenia,” he says.
If you or a loved one has been diagnosed with schizophrenia, it may feel scary. Understanding the reality of the disorder not only helps to erase the stigma surrounding the condition but also frees you up to focus on an effective treatment plan.
- “Have you got the wrong impression about schizophrenia?” 18 September 2017. BBC. http://www.bbc.com/news/health-41282282
- “Schizophrenia.” National Institute of Mental Health. Last updated November, 2017. https://www.nimh.nih.gov/health/statistics/schizophrenia.shtml
- "Schizophrenia Attitudes and Awareness." National Alliance on Mental Health. https://www.nami.org/About-NAMI/Publications-Reports/Survey-
- "Recovery from schizophrenia and the recovery model.
 " Current Opinion in Psychiatry. https://www.ncbi.nlm.nih.gov/pubmed/19417668
" Current Opinion in Psychiatry. https://www.ncbi.nlm.nih.gov/pubmed/19417668 - “Schizophrenia treatment.” American Psychological Association. http://www.apa.org/topics/schiz/treatment.aspx
- “Recognizing the signs of schizophrenia.” American Psychological Association. http://www.apa.org/helpcenter/recognizing-schizophrenia.aspx
Notes: This article was originally published March 5, 2018 and most recently updated October 2, 2020.
Rosemary Black
Rosemary Black is a veteran journalist who has written about food, health, fitness, and parenting for more than 25 years. A former senior editor at Everyday Health, she was food editor for the New York Daily News and Parade's Dash magazine. Rosemary, the author of four cookbooks, has written for QualityHealth.com and various other websites and magazines. The mom of 7 lives with her family in Westchester County, New York.
Six Common Myths and Misconceptions About Schizophrenia
Split personality.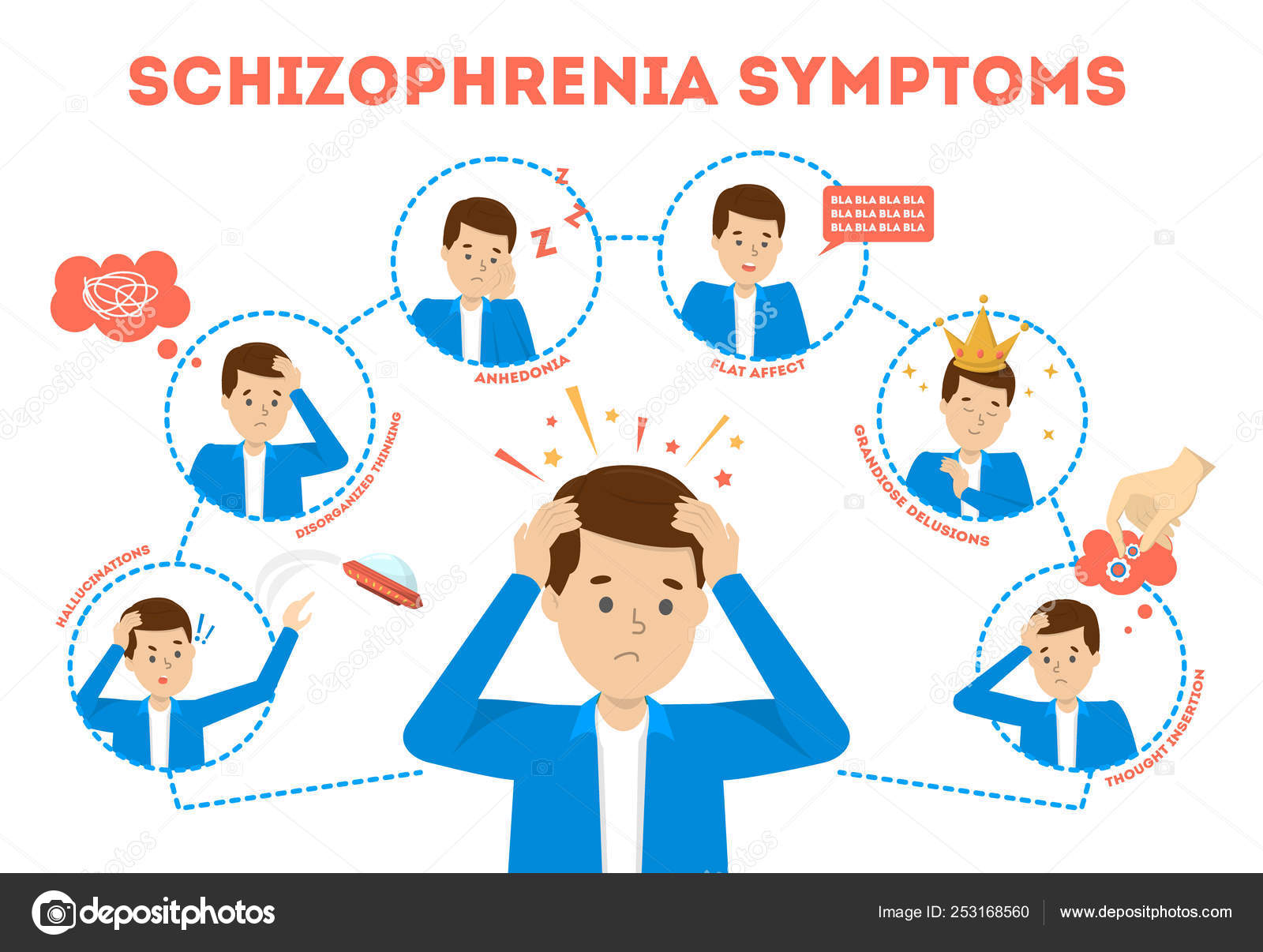 Violent behavior. Never being able to hold onto a job or have a career. Myths abound about schizophrenia, a serious and complex mental disorder currently affecting about 1 percent of American adults.
Violent behavior. Never being able to hold onto a job or have a career. Myths abound about schizophrenia, a serious and complex mental disorder currently affecting about 1 percent of American adults.
Patients diagnosed with schizophrenia do not present with a split personality, nor is it common for someone with the disorder to be violent, says Simon Rego, PsyD, chief psychologist at Montefiore Medical Center and Associate Professor of Psychiatry and Behavioral Sciences at Albert Einstein College of Medicine in New York City. And many individuals with schizophrenia are able to work.
Here, experts dispel some of the more common myths about schizophrenia.
#1 Myth: Schizophrenia means you have a split personality.
Reality: “This is a classic myth,” Dr. Rego says. A split personality, also called a Dissociative Identity Disorder or a Multiple Personality Disorder, is extraordinarily rare, he explains. It is quite distinct from schizophrenia, he says. “Schizophrenia is a thought disorder,” he explains, “The myth likely stems from the fact that in schizophrenia there is a breakdown, or split, between thoughts, emotions, and behavior. ”
”
This split results in the person confusing reality and fantasy, Dr. Rego explains. “The person may experience delusions and hallucinations, and emotions may become blunted or inappropriate,” he explains. When most people think of schizophrenia, they think of someone who is seeing things and hearing voices, Dr. Rego points out. “These are what are called positive symptoms, but people with schizophrenia have negative symptoms, too,” he says. Among the common negative symptoms are low motivation, difficulty forming social connections, and a flat, blunted affect, Dr. Rego says. A lack of pleasure in everyday activities, rarely speaking, and difficulty paying attention are also symptoms, according to the American Psychological Association.
#2 Myth: Violence is common among individuals with schizophrenia.
Reality: It’s actually rare for someone with schizophrenia to be violent, says Dr. Rego. An individual with schizophrenia is much more likely to be the victim of violence rather than the perpetrator, he says.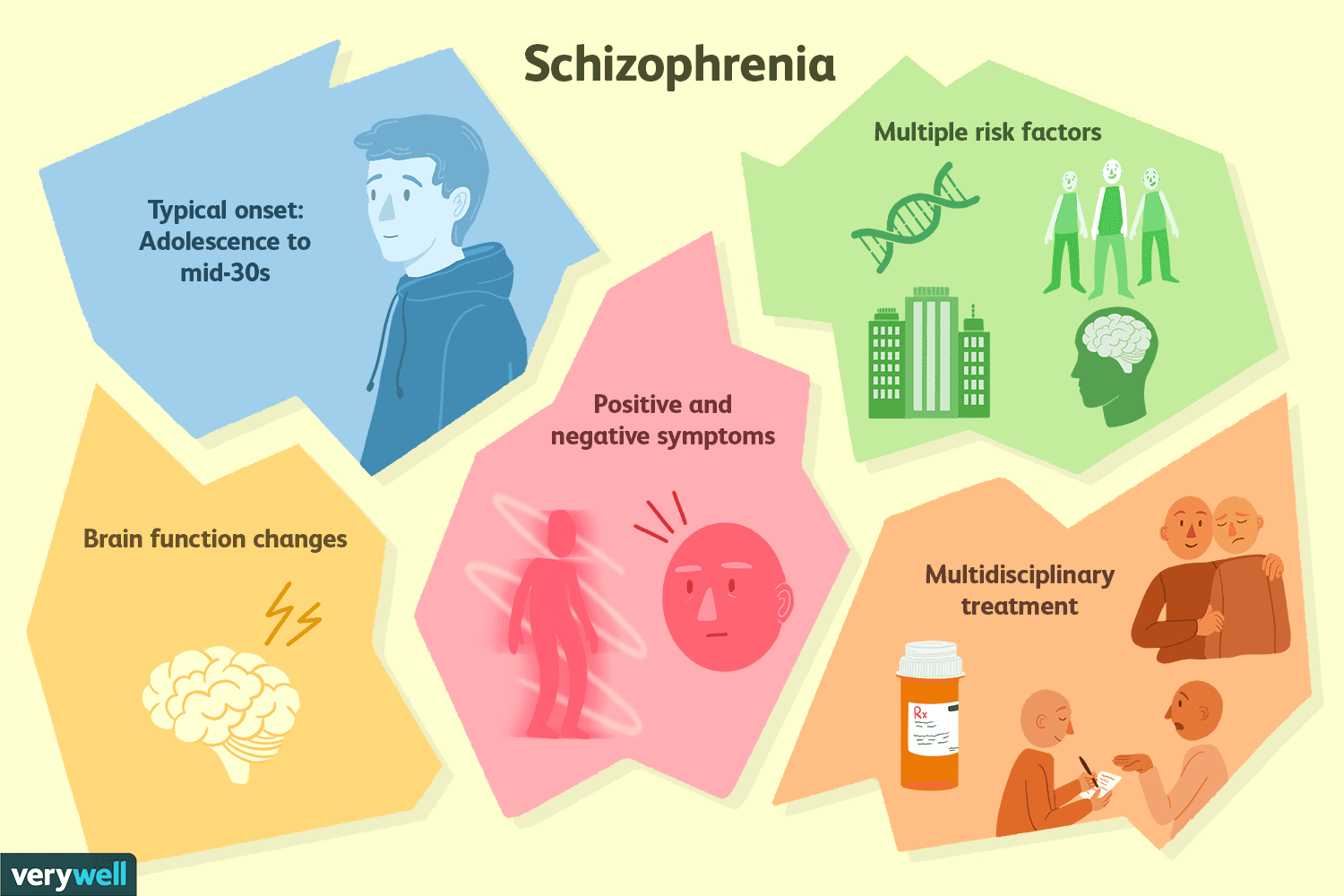 “They tend to struggle more to have the social benefits that most of us have,” Dr. Rego explains. “They may be homeless or staying in a shelter, where they may be singled out and assaulted.”
“They tend to struggle more to have the social benefits that most of us have,” Dr. Rego explains. “They may be homeless or staying in a shelter, where they may be singled out and assaulted.”
Some individuals with psychiatric disorders like schizophrenia do become aggressive, says Scott Ira Krakower, DO, assistant unit chief of psychiatry at Zucker Hillside Hospital in Glen Oaks, New York. “However, it is a myth that this is always the case,” he says. “A person can be aggressive and have an anger problem and not have schizophrenia,” he explains. Both medication and counseling can help with any signs of violent behavior, he says.
#3 Myth: People with schizophrenia can’t ever hold down a job.
Reality: Actually, some individuals, when stable, are able to function quite well, Dr. Rego says. “When they are being compliant with their medication and are engaged in some sort of psychosocial treatment, they are often quite functional,” he says. The National Alliance on Mental Illness estimates that as many as half of the two million Americans with schizophrenia can improve significantly or even recover completely if they get treatment. Dr. Rego refers to the “recovery model” of treatment for schizophrenia, and an article in the Current Opinion in Psychiatry.
Dr. Rego refers to the “recovery model” of treatment for schizophrenia, and an article in the Current Opinion in Psychiatry.
“Working appears to help people recover from schizophrenia, and recent advances in vocational rehabilitation have been shown to be effective in countries with differing economies and labor markets. A growing body of research supports the concept that empowerment is an important component of the recovery process,” the authors write.
About a quarter of young people with the disorder recover when treated within six months to two years, reports the American Psychological Association, and another 35 to 40% percent are improved enough after longer-term treatment to live fairly normal lives with only minor symptoms. What makes this possible is psychosocial support—psychotherapy, family education, and self-help groups that can help people with schizophrenia cope and regain their lives. Job training and vocational counseling also can be useful. Still, cautions Dr. Krakower, some patients have difficulty holding down a job. “And it’s okay for them to get additional treatment,” he says. “Sometimes they may need to be on disability, and that’s okay, too.”
Krakower, some patients have difficulty holding down a job. “And it’s okay for them to get additional treatment,” he says. “Sometimes they may need to be on disability, and that’s okay, too.”
#4 Myth: A person with schizophrenia can seem perfectly normal one moment and change into a different person the next.
Reality: A sudden dramatic change of character in individuals with schizophrenia is not the usual scenario, Dr. Rego says. In fact, it’s common for the signs and symptoms of this mental disorder to surface over time. “There are often soft signs that the illness is going to take root,” Dr. Rego says. In the typical progression of the illness, a person may first become flat, isolate more frequently, and decrease their participation in activities. Then a psychotic break could occur—from a stressor such as starting college, Dr. Rego says. “So it is more of a slow progression, with a waxing and waning course that occurs over months and years,” he explains.
#5.
 Myth: People with schizophrenia usually require long-term hospitalization.
Myth: People with schizophrenia usually require long-term hospitalization.Reality: Appropriate treatment today may include a combination of out-patient care, acute hospitalization, and longer-term hospitalization when needed, Dr. Krakower says. And, even when family support and financial resources are available, many patients still need inpatient treatment, he adds.
“But the treatment model for schizophrenia is moving away from longer-term hospitalization and toward outpatient treatment,” he says. “At times, individuals may benefit from going to a day program or a partial day hospital, where they can receive daily treatment. Therapy may vary from individual to group therapy and the medication of choice is usually second-generation antipsychotic agents (i.e. aripiprazole, clozapine, and risperidone).”
In a longer-care setting, the time can vary from weeks to months and depends on how the patient is progressing, Dr. Krakower says.
Long-term hospitalization may also be an indication that the person isn't getting enough support. “In some cases, society has failed them,” says Stephen Ferrando, MD, Director of Psychiatry at Westchester Medical Center Health Network (WMCHealth). “We are not providing enough services for them to succeed.”
“In some cases, society has failed them,” says Stephen Ferrando, MD, Director of Psychiatry at Westchester Medical Center Health Network (WMCHealth). “We are not providing enough services for them to succeed.”
#6. Myth: Bad parenting is what causes schizophrenia.
Years ago, it was believed that the mother or both parents were responsible if the child developed schizophrenia, Dr. Rego explains. While there is a genetic susceptibility—the disorder tends to run in families—there is absolutely no evidence that it is caused by how a person is parented, he says.
“Plus, even if your parent has schizophrenia your chances of getting it are less than 25 percent,” Dr. Ferrando explains.
So what does cause it? Rather than a single gene for schizophrenia, it’s likely that various genes, as well as environmental factors, are responsible, according to the American Psychological Association.
Environmental factors that may trigger the onset of schizophrenia can range from extreme academic stress to substance abuse. Dr. Ferrando says. “We know that extreme environmental stress like these situations can trigger the onset of schizophrenia,” he says.
Dr. Ferrando says. “We know that extreme environmental stress like these situations can trigger the onset of schizophrenia,” he says.
If you or a loved one has been diagnosed with schizophrenia, it may feel scary. Understanding the reality of the disorder not only helps to erase the stigma surrounding the condition but also frees you up to focus on an effective treatment plan.
- “Have you got the wrong impression about schizophrenia?” 18 September 2017. BBC. http://www.bbc.com/news/health-41282282
- “Schizophrenia.” National Institute of Mental Health. Last updated November, 2017. https://www.nimh.nih.gov/health/statistics/schizophrenia.shtml
- "Schizophrenia Attitudes and Awareness." National Alliance on Mental Health. https://www.nami.org/About-NAMI/Publications-Reports/Survey-
- "Recovery from schizophrenia and the recovery model." Current Opinion in Psychiatry. https://www.ncbi.nlm.nih.gov/pubmed/19417668
- “Schizophrenia treatment.” American Psychological Association.
 http://www.apa.org/topics/schiz/treatment.aspx
http://www.apa.org/topics/schiz/treatment.aspx - “Recognizing the signs of schizophrenia.” American Psychological Association. http://www.apa.org/helpcenter/recognizing-schizophrenia.aspx
Notes: This article was originally published March 5, 2018 and most recently updated October 2, 2020.
Rosemary Black
Rosemary Black is a veteran journalist who has written about food, health, fitness, and parenting for more than 25 years. A former senior editor at Everyday Health, she was food editor for the New York Daily News and Parade's Dash magazine. Rosemary, the author of four cookbooks, has written for QualityHealth.com and various other websites and magazines. The mom of 7 lives with her family in Westchester County, New York.
7 misconceptions about schizophrenia that educated people are ashamed to believe
October 22, 2020 Adviсe
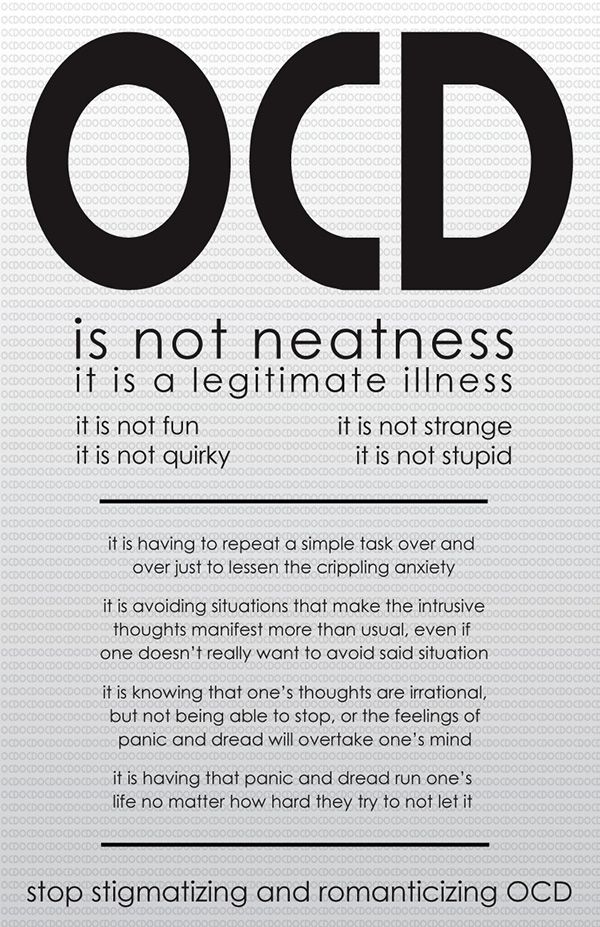
There is a lot of prejudice around any mental disorder, but schizophrenia is not particularly lucky.
What to hide, we are a little afraid of people with this diagnosis, and this is not surprising - the media image of the disease is not very conducive to sympathy. In films, schizophrenia takes its owners away from everyday life into some special world, making people either geniuses or murderers - you won’t understand. Together with the pharmaceutical company Gedeon Richter, we figured out where the truth is and where the delusion is.
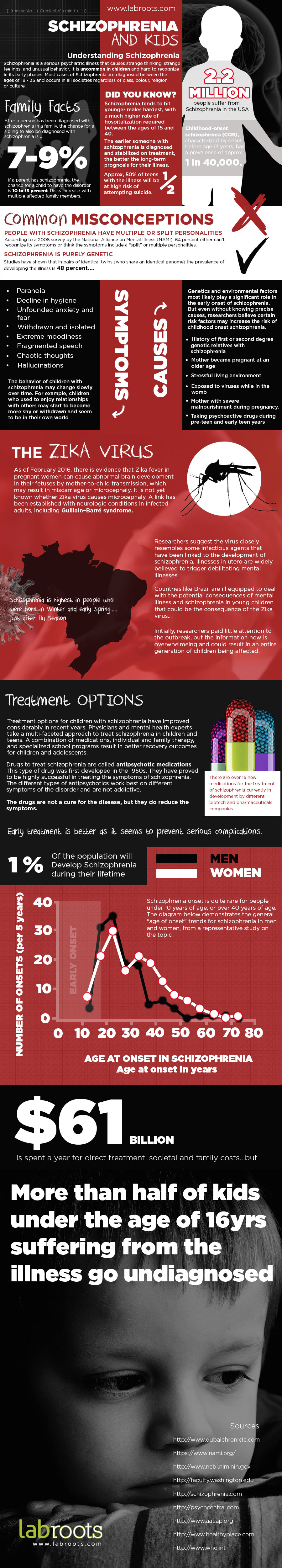
Myth 1. Schizophrenia is a rare disease
Compared to other mental disorders, schizophrenia is actually not that common. It affects 20 million people worldwide, while 264 million people live with depression. But this is not a rare disease. In Russia, there is a list of rare diseases that includes conditions that occur in a maximum of 10 people per 100,000 of the population, and schizophrenia is not on this list. Official statistics with information on how many people in the country live with such a diagnosis cannot be found, but, according to VTsIOM, about 20% of Russians have an acquaintance or relative with schizophrenia.
Myth 2. People with schizophrenia have multiple personalities
People with dissociative disorders “switch” from personality to personality. Schizophrenia has no such symptom. Probably, this myth was born from the meaning of the word schizo, which is translated as "split".
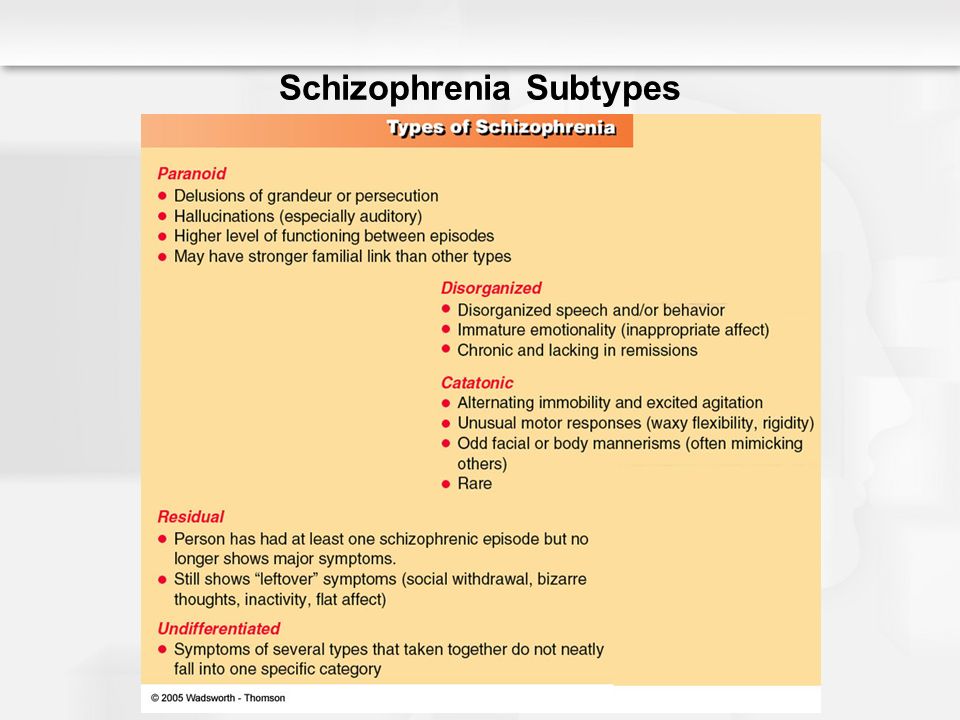
Myth 3. All people with schizophrenia behave in the same way
There are common symptoms (after all, this is a disease). Among them are hallucinations - voices in the head, music, flashes of light and faces that do not exist; crazy ideas - the confidence that you are being watched, thoughts are put into the brain, and hidden messages are sent through the TV; confusion - thoughts scatter, and speech becomes incoherent, so that other people do not understand the essence of the conversation. Symptoms in which the perception of reality is enhanced (a person feels something that does not exist) are called productive, or positive.
But the disease is not limited to this. There are also negative symptoms when feelings are dulled rather than intensified.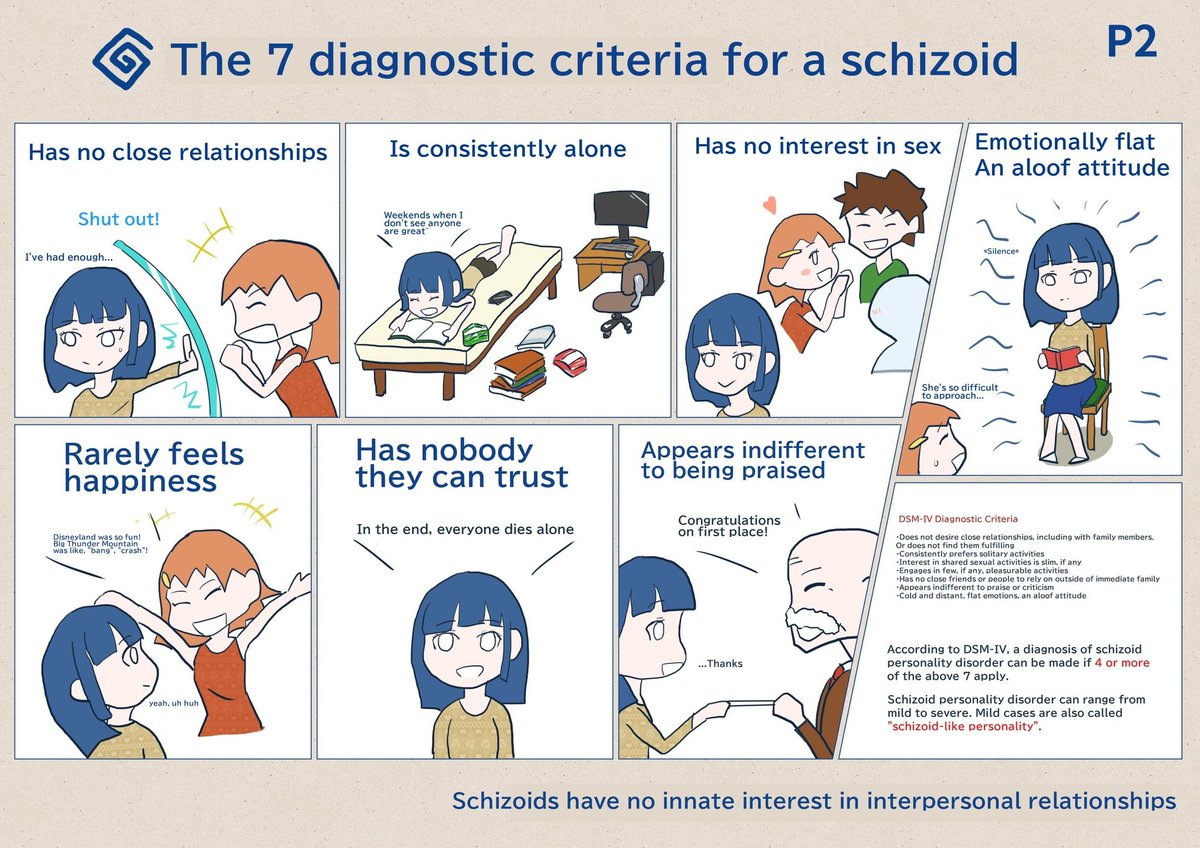 The person becomes withdrawn, seems detached from the rest of the world. Motivation to monitor appearance, communicate and leave the house disappears. Negative manifestations often cause misunderstanding in the family or circle of friends, because they are mistakenly perceived as rudeness or laziness, and not signs of schizophrenia.
The person becomes withdrawn, seems detached from the rest of the world. Motivation to monitor appearance, communicate and leave the house disappears. Negative manifestations often cause misunderstanding in the family or circle of friends, because they are mistakenly perceived as rudeness or laziness, and not signs of schizophrenia.
There are many symptoms, they are combined and expressed in everyone in their own way, so it cannot be said that people with schizophrenia behave in the same way. In addition, everyone has personal qualities of character that are not determined by the disease, but can influence behavior.
Myth 4. People with schizophrenia are dangerous and should be isolated
It is possible that a person with schizophrenia will be prone to aggressive behavior. By the way, it is not necessarily directed at others - usually the patient tries to harm himself. But this does not mean that the diagnosis automatically makes people violent. Most of them are no more dangerous than you and me and have never committed violent crimes.
In 2019, Gedeon Richter, together with VTsIOM, asked the people of Russia what they know and think about schizophrenia. Every fourth respondent believes that the disease makes a person dangerous, so it is better for him to stay away from other people. Even experts sometimes believe in such myths. Due to stigma, people with schizophrenia may be afraid to seek medical help and therefore do not receive proper treatment. Not only in health matters, but also in social life, people face discrimination because of their diagnosis. For example, they may be prohibited from voting in elections, and it may be more difficult to get a job or an education.
MYTH 5. Schizophrenia develops due to childhood trauma
There is a similar myth: "genes are to blame for everything." In fact, the exact cause of the disease is unknown to science. Probably, several factors play their roles at once: heredity, features of the structure and functioning of the brain, stress. But traumatic events, such as violence or the death of a loved one, do not in themselves cause disease.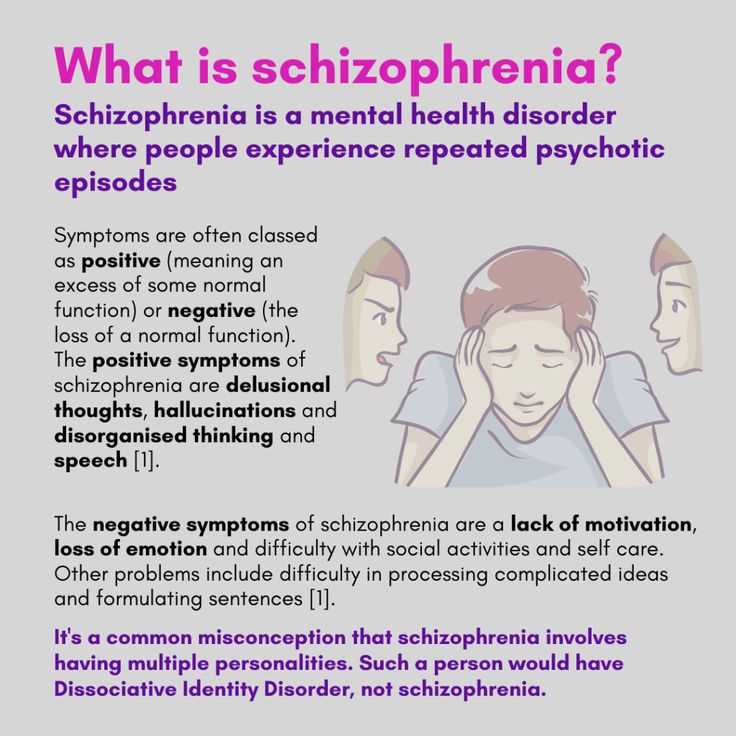 They are more likely to provoke symptoms in those who are genetically predisposed to schizophrenia.
They are more likely to provoke symptoms in those who are genetically predisposed to schizophrenia.
MYTH 6. Schizophrenia is treated with tranquilizers
Schizophrenia is treated with various drugs, but mostly antipsychotics - their goal is not to turn the patient into a vegetable, but to eliminate hallucinations, delusions and other symptoms. So that a person does not delay taking drugs and learns to control the disease, drugs are combined with psychotherapy. Often, family members and the patient themselves need to come to the realization that schizophrenia is not someone else's fault, but a disease that appears for biological reasons. Family and other types of therapy work with this.
First-generation antipsychotics dealt mostly with productive symptoms of schizophrenia like hallucinations, but might not work well enough when patients needed help with negative symptoms such as loss of motivation. Today, modern antipsychotics are available - studies show that they work effectively with both positive and negative symptoms, while they have milder side reactions. Last year, the international pharmaceutical company Gedeon Richter registered a new generation drug in Russia - now specialists can include it in their treatment plan, giving patients the opportunity to lead a more harmonious lifestyle.
Last year, the international pharmaceutical company Gedeon Richter registered a new generation drug in Russia - now specialists can include it in their treatment plan, giving patients the opportunity to lead a more harmonious lifestyle.
Myth 7. People with schizophrenia are disabled for life
Schizophrenia is indeed a lifelong illness, but it can be controlled with medication, support from loved ones and psychotherapy. For many people, the symptoms of schizophrenia can return very rarely, so they live an independent and active life.
Schizophrenia. Signs and symptoms of schizophrenia
Schizophrenia is often referred to as one of the most mysterious diseases. The similarity at first glance of the symptoms of the disease with other mental disorders gives rise to many erroneous judgments.
The image of a person with schizophrenia in society is often associated with aggressiveness, dementia, destructive behavior, inadequacy. And if someone among the relatives had cases of schizophrenia, the stigma of mental illness is almost unconditionally put on his relatives.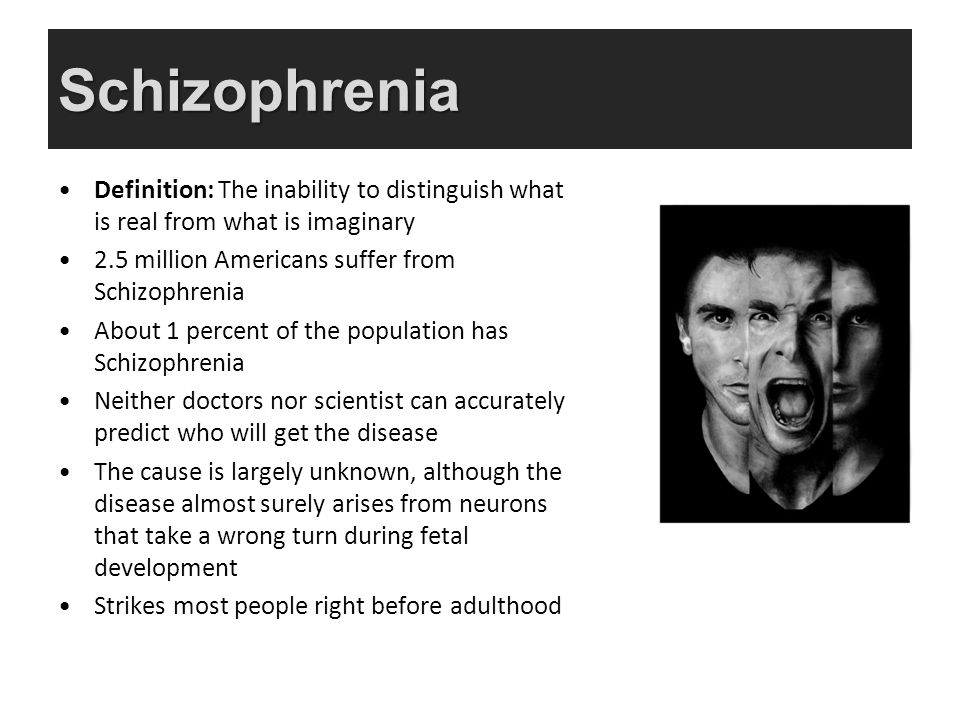 Is it really?
Is it really?
Misconception 1. Schizophrenia = multiple personality
This judgment is completely wrong. The name "schizophrenia" comes from the Greek words "split" and "thinking". With this disease, splitting, disintegration of thought processes and emotional reactions occurs, contact with reality is disturbed.
The most "bright" symptoms of the disease are delirium (false conclusions that cannot be corrected), hallucinations, gross disorganization of speech, behavior and thinking. There may also be negative symptoms - the loss of certain mental functions. For example, the desire to communicate, to make contact with other people, to take care of oneself, to monitor one's appearance disappears.
Multiple personality disorder is a completely different disease . Its essence is that in one person several completely different personalities coexist with their own character traits. Moreover, these personalities do not appear simultaneously: one is completely unaware of the existence of the other.
Misconception 2. Patients with schizophrenia are aggressive and dangerous to society
Such people show aggression no more often than healthy people. However, schizophrenia exacerbates character traits. If a person before the onset of the disease was quick-tempered, prone to aggression, then it is precisely these properties of his temperament that will prevail; if he was soft and calm - the disease will not entail hostility.
In addition, Marina Skugarevskaya added, there are situations when a person hears voices, he has hallucinations, delusional ideas. For example, he believes that he is being followed, persecuted, and spoiled. Since for a person this is a reality, then at some point he can act as it seems logical to him, and therefore in accordance with the plot of delirium.
In situations like this one should remain calm and not try to convince the person with schizophrenia. What he sees and hears, how he interprets what is happening, does not cause him doubts, is true.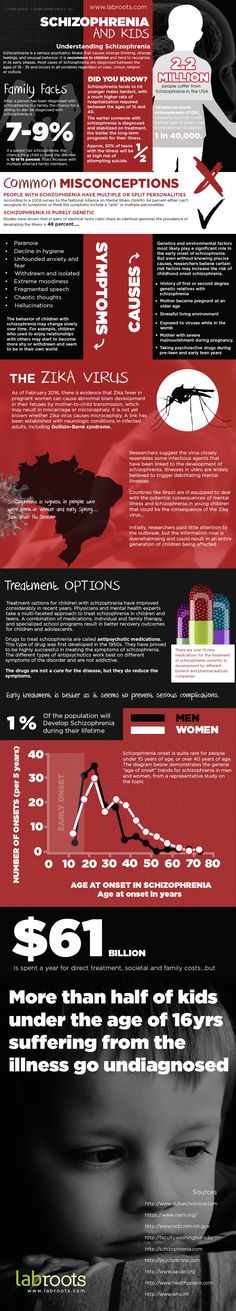 Trying to convince him otherwise or encouraging him, you can provoke aggression. You should speak as calmly, clearly and clearly as possible. It is desirable that someone whom he trusts talks to a person in such situations.
Trying to convince him otherwise or encouraging him, you can provoke aggression. You should speak as calmly, clearly and clearly as possible. It is desirable that someone whom he trusts talks to a person in such situations.
Delusion 3. The worst thing in schizophrenia is hallucinations and delusions
This is not entirely true. Positive symptoms of schizophrenia (such as hallucinations and delusions) are usually easier to treat and correct. While negative symptoms have a greater impact on the quality of life and working capacity, they are more difficult to treat and lead to disability.
It is often said that people with schizophrenia hear only voices. In fact, they may experience both tactile, visual, and olfactory hallucinations. Experts have even revealed a connection between the nature of hallucinations and the characteristics of the environment in which the patient lives. For example, Marina Skugarevskaya said, residents of European countries often experience verbal hallucinations (“hear voices”), while representatives of Eastern countries are more prone to visual hallucinations.
Marina Skugarevskaya: Scientists analyzed records from different years from psychiatric hospitals. So, in the 1930s, the religious theme of hallucinations prevailed, in the 1980s - technogenic.
Misconception 4. Schizophrenia is a genetic disease
Yes and no. The role of genetic factors in the development of the disease is very large. However, the risk of schizophrenia, if one of the parents is sick, increases for the child by about 12%; if a grandmother or grandfather is sick - by 5%. A huge role in the development of the disease is played by the environment of a person, the presence of those factors that can start the disease.
Even identical twins with the same genetic make-up, if one twin has schizophrenia, the other has a 50/50 chance of developing the disease. Genetics gives only a predisposition, the rest depends on external factors - the environment, drug use, stressful situations, prolonged nervous tension, etc.
Delusion 5.