Mental illness borderline
NIMH » Borderline Personality Disorder
Overview
Borderline personality disorder is a mental illness that severely impacts a person’s ability to regulate their emotions. This loss of emotional control can increase impulsivity, affect how a person feels about themselves, and negatively impact their relationships with others. Effective treatments are available to manage the symptoms of borderline personality disorder.
Signs and Symptoms
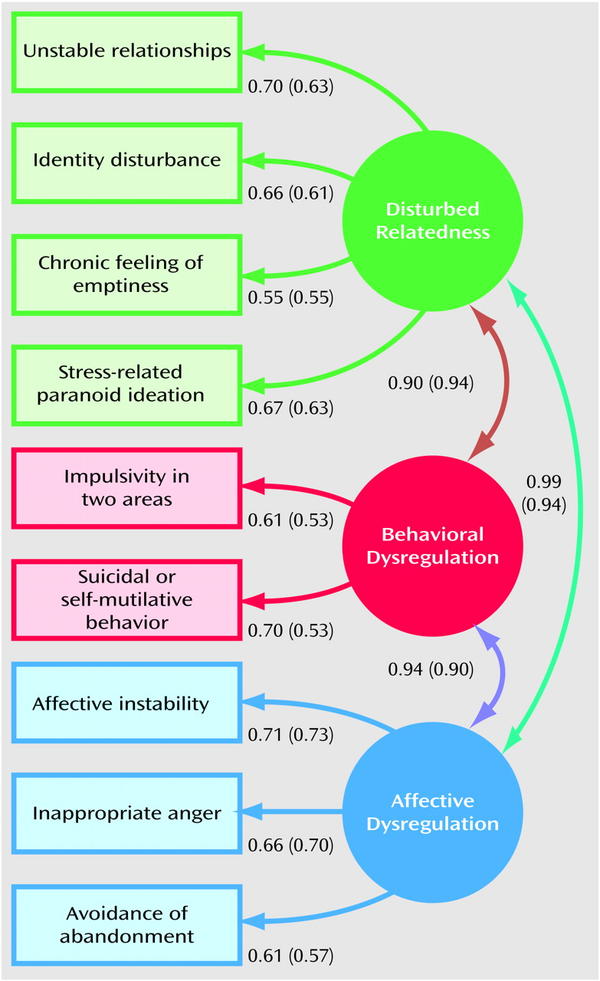
People with borderline personality disorder may experience intense mood swings and feel uncertainty about how they see themselves. Their feelings for others can change quickly, and swing from extreme closeness to extreme dislike. These changing feelings can lead to unstable relationships and emotional pain.
People with borderline personality disorder also tend to view things in extremes, such as all good or all bad. Their interests and values can change quickly, and they may act impulsively or recklessly.
Other signs or symptoms may include:
- Efforts to avoid real or perceived abandonment, such as plunging headfirst into relationships—or ending them just as quickly.
- A pattern of intense and unstable relationships with family, friends, and loved ones.
- A distorted and unstable self-image or sense of self.
- Impulsive and often dangerous behaviors, such as spending sprees, unsafe sex, substance abuse, reckless driving, and binge eating. Please note: If these behaviors happen mostly during times of elevated mood or energy, they may be symptoms of a mood disorder and not borderline personality disorder.
- Self-harming behavior, such as cutting.
- Recurring thoughts of suicidal behaviors or threats.
- Intense and highly variable moods, with episodes lasting from a few hours to a few days.
- Chronic feelings of emptiness.
- Inappropriate, intense anger or problems controlling anger.
- Feelings of dissociation, such as feeling cut off from oneself, observing oneself from outside one’s body, or feelings of unreality.
Not everyone with borderline personality disorder may experience all of these symptoms. The severity, frequency, and duration of symptoms depend on the person and their illness.
People with borderline personality disorder have a significantly higher rate of self-harming and suicidal behavior than the general population.
People with borderline personality disorder who are thinking of harming themselves or attempting suicide need help right away.
If you or someone you know is in immediate distress or is thinking about hurting themselves, call or text the 988 Suicide & Crisis Lifeline at 988 or chat at 988lifeline.org. You can also contact the Crisis Text Line (text HELLO to 741741).
Risk Factors
Researchers aren’t sure what causes borderline personality disorder, but studies suggest that genetic, environmental, and social factors may increase the risk of developing it. These factors may include:
These factors may include:
- Family history: People who have a close family member (such as a parent or sibling) with the illness may be at a higher risk of developing borderline personality disorder.
- Brain structure and function: Research shows that people with borderline personality disorder may have structural and functional changes in the brain, especially in the areas that control impulses and emotion regulation. However, the studies do not demonstrate whether these changes were risk factors for the illness or if such changes were caused by the disorder.
- Environmental, cultural, and social factors: Many people with borderline personality disorder report experiencing traumatic life events, such as abuse, abandonment, or hardship during childhood. Others may have been exposed to unstable, invalidating relationships or conflicts.
Although these factors may increase a person’s risk, it doesn’t mean it is certain that they’ll develop borderline personality disorder.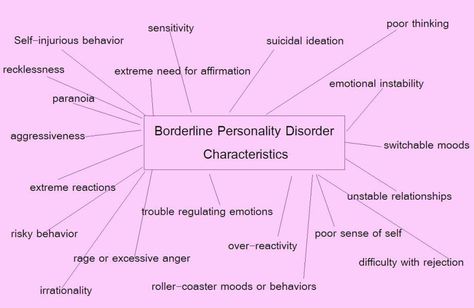 Likewise, people without these risk factors may develop the disorder in their lifetime.
Likewise, people without these risk factors may develop the disorder in their lifetime.
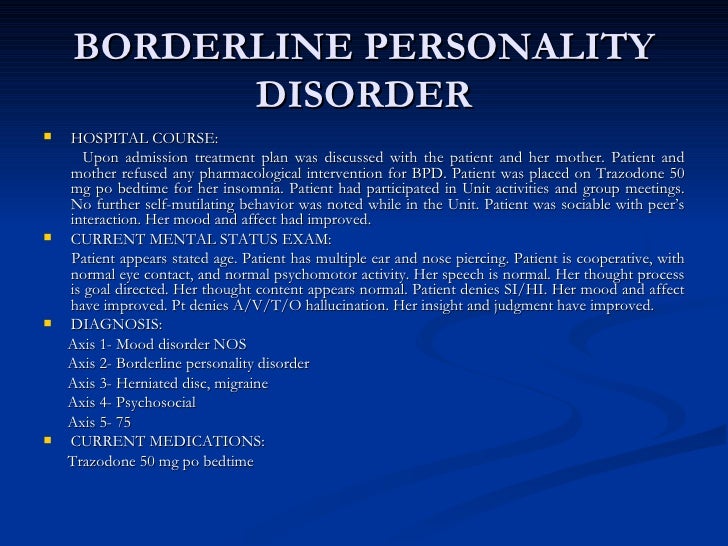
Diagnosis
A licensed mental health professional—such as a psychiatrist, psychologist, or clinical social worker—who is experienced in diagnosing and treating mental disorders can diagnose borderline personality disorder based on a thorough interview and a discussion about symptoms. A careful and thorough medical exam also can help rule out other possible causes of symptoms. In diagnosing the illness, providers will discuss a person’s symptoms and ask about family medical histories, including histories of mental illness.
Borderline personality disorder is usually diagnosed in late adolescence or early adulthood. Occasionally, a person younger than age 18 may be diagnosed with borderline personality disorder if symptoms are significant and last at least a year.
What other illnesses can co-occur with borderline personality disorder?
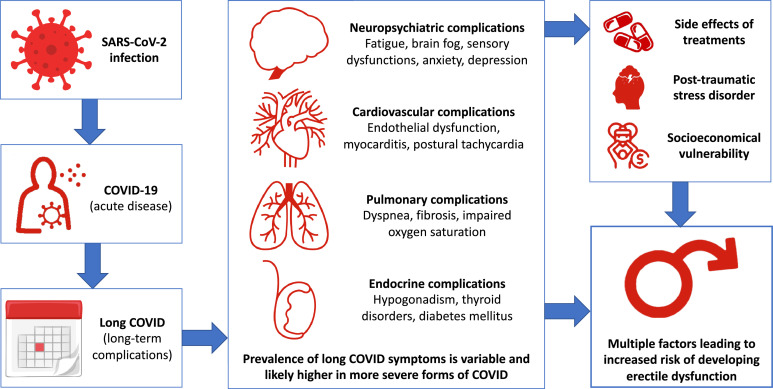
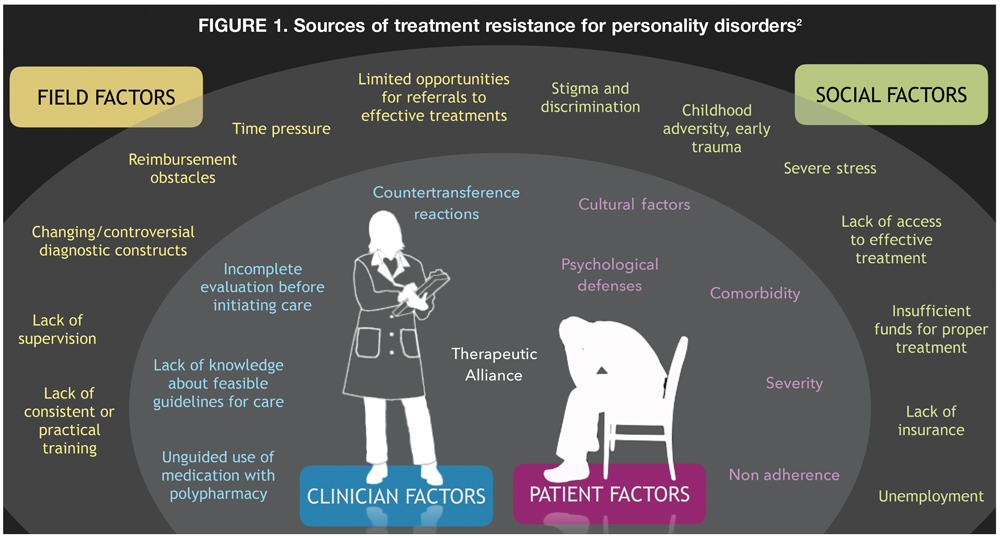
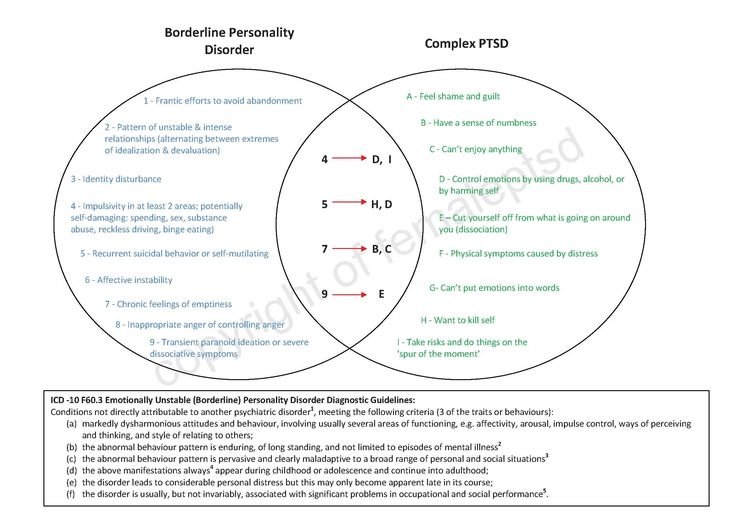
Borderline personality disorder often occurs with other mental illnesses, such as post-traumatic stress disorder (PTSD).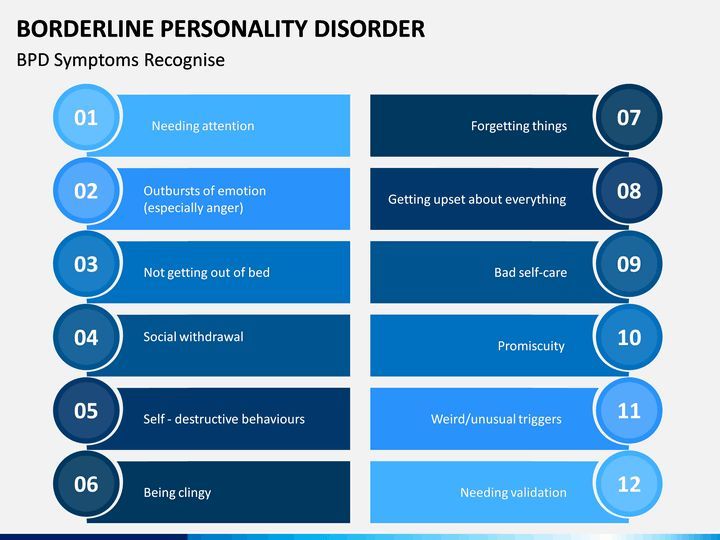 These co-occurring disorders can make it harder to diagnose and treat borderline personality disorder, especially if symptoms of other illnesses overlap with symptoms of the disorder. For example, a person with borderline personality disorder also may be more likely to experience symptoms of major depression, PTSD, bipolar disorder, anxiety disorders, substance abuse, or eating disorders.
These co-occurring disorders can make it harder to diagnose and treat borderline personality disorder, especially if symptoms of other illnesses overlap with symptoms of the disorder. For example, a person with borderline personality disorder also may be more likely to experience symptoms of major depression, PTSD, bipolar disorder, anxiety disorders, substance abuse, or eating disorders.
Treatments and Therapies
Borderline personality disorder historically has been viewed as challenging to treat. But with newer, evidence-based treatment, many people with this disorder experience fewer and less severe symptoms, improved functioning, and better quality of life. It is important for patients with borderline personality disorder to receive treatment from a licensed mental health professional. Other types of treatment, or treatment from a provider who is not appropriately trained, may be ineffective or dangerous.
Many factors affect the length of time it takes for symptoms to improve once treatment begins. It is important for people with borderline personality disorder and their loved ones to be patient and receive support during treatment.
It is important for people with borderline personality disorder and their loved ones to be patient and receive support during treatment.
Seek—and stick with—treatment.
Studies funded by the National Institute of Mental Health (NIMH) indicate that individuals with borderline personality disorder who don’t receive adequate treatment are more likely to develop other chronic medical or mental illnesses and are less likely to make healthy lifestyle choices.
Psychotherapy
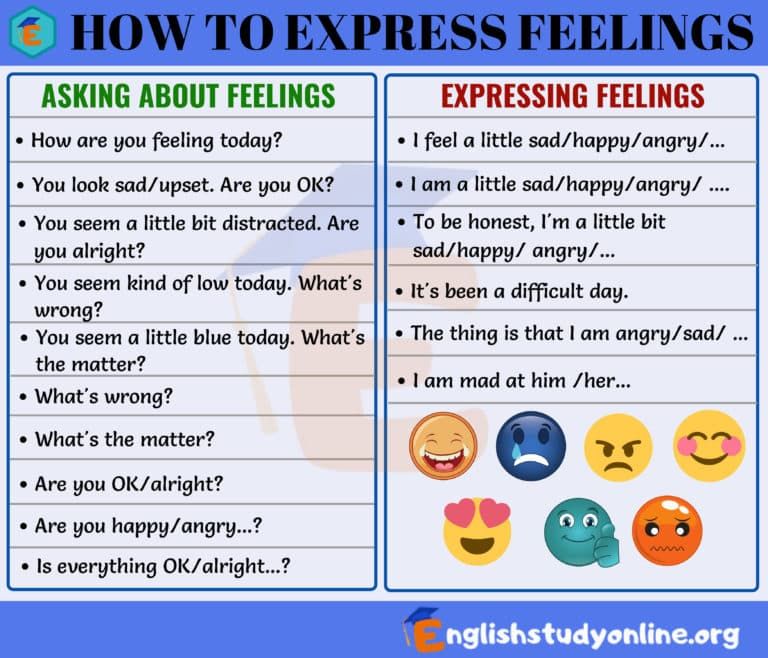
Psychotherapy, sometimes called “talk therapy,” is the first-line treatment for people with borderline personality disorder. Most psychotherapy occurs with a licensed, trained mental health professional in one-on-one sessions or with other individuals in group settings. Group sessions may help teach people with borderline personality disorder to interact with others and express themselves effectively.
Two examples of psychotherapies used to treat borderline personality disorder are:
- Dialectical Behavior Therapy (DBT): This treatment was developed specifically for individuals with borderline personality disorder.
 DBT uses concepts of mindfulness or awareness of one’s present situation and emotional state. DBT also teaches skills to help people control intense emotions, reduce self-destructive behaviors, and improve relationships.
DBT uses concepts of mindfulness or awareness of one’s present situation and emotional state. DBT also teaches skills to help people control intense emotions, reduce self-destructive behaviors, and improve relationships. - Cognitive Behavioral Therapy (CBT): This treatment can help people identify and change core beliefs and behaviors that come from inaccurate perceptions of themselves and others and problems interacting with others. It may help people reduce mood swings and anxiety symptoms and may reduce the number of self-harming or suicidal behaviors.
Read more on NIMH’s Psychotherapies health topic page.
Medications
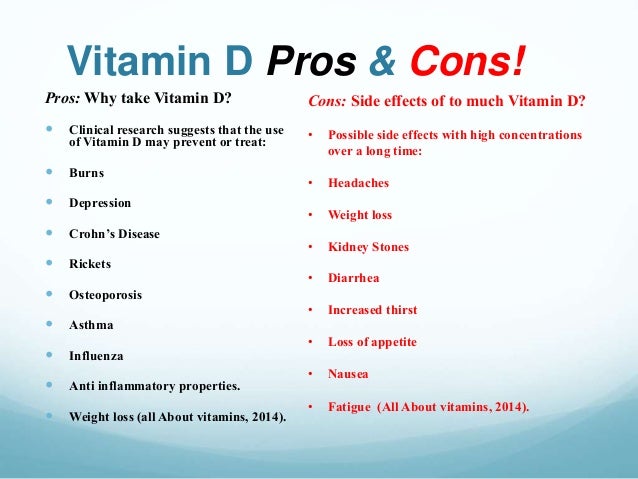
Because the benefits of prescription medication for borderline personality disorder are unclear, medications aren’t typically used as the primary way to treat the illness. However, in some cases, a psychiatrist may recommend medications to treat specific symptoms or co-occurring mental disorders such as mood swings or depression.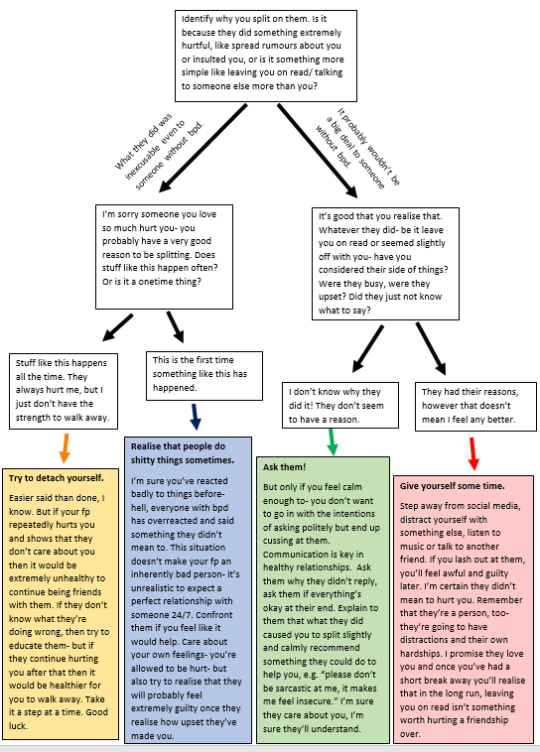 Treatment with medications may require coordinated care from more than one medical professional.
Treatment with medications may require coordinated care from more than one medical professional.
Medications also can sometimes cause side effects in some people. Talk to your provider about what to expect from a particular medication. Read more in NIMH’s Mental Health Medications health topic.
Other Elements of Care
Some people with borderline personality disorder experience severe symptoms and need intensive, often inpatient, care. Others may use some outpatient treatments but never need hospitalization or emergency care.
Therapy for Caregivers and Family Members
Having a relative or loved one with the disorder can be stressful, and family members or caregivers may unintentionally act in ways that can worsen their loved one’s symptoms.
Although more research is needed to determine how well family therapy helps with borderline personality disorder, studies on other mental disorders show that including family members can help support a person’s treatment.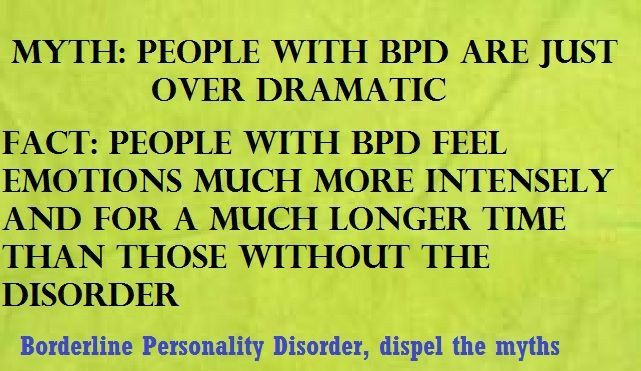 Families and caregivers also can benefit from therapy.
Families and caregivers also can benefit from therapy.
Family therapy helps by:
- Allowing the relative or loved one to develop skills to understand and support a person with borderline personality disorder.
- Focusing on the needs of family members to help them understand the obstacles and strategies for caring for someone with the disorder.
Finding Help
If you’re not sure where to get help, a health care provider can refer you to a licensed mental health professional, such as a psychiatrist or psychologist with experience treating borderline personality disorder. If you need help starting the conversation, check out the Tips for Talking With Your Health Care Provider fact sheet.
Other resources include:
- Substance Abuse and Mental Health Services Administration’s Behavioral Health Treatment Services Locator, a tool for finding mental health services in your area
- NIMH’s Help for Mental Illnesses webpage
- Agency for Healthcare Research and Quality’s website
Tips for Family and Caregivers
Here are some ways to help a friend or relative with the disorder:
- Take time to learn about the illness to understand what your friend or relative is experiencing.
- Offer emotional support, understanding, patience, and encouragement. Change can be difficult and frightening to people with borderline personality disorder, but things can improve over time.
- Encourage your loved one in treatment for borderline personality disorder to ask about family therapy.
- Seek counseling for yourself. Choose a different therapist than the one your relative is seeing.
Join a Study
Clinical trials are research studies that look at new ways to prevent, detect, or treat diseases and conditions. The goal of clinical trials is to determine if a new test or treatment works and is safe. Although individuals may benefit from being part of a clinical trial, participants should be aware that the primary purpose of a clinical trial is to gain new scientific knowledge so that others may be better helped in the future.
Researchers at NIMH and around the country conduct many studies with patients and healthy volunteers.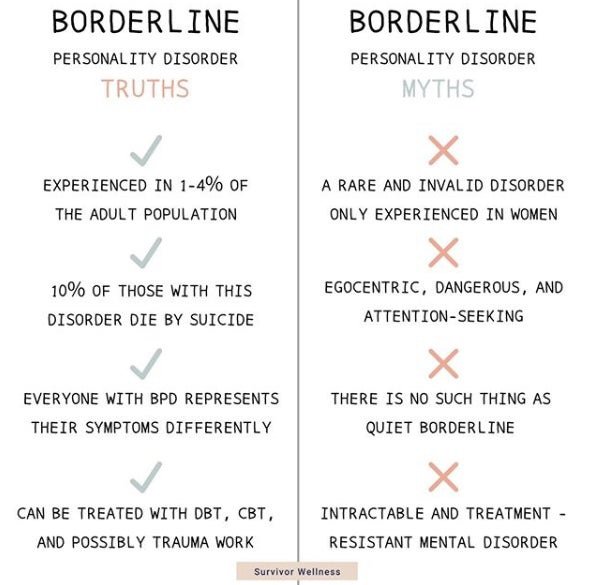 We have new and better treatment options today because of what clinical trials uncovered years ago. Be part of tomorrow’s medical breakthroughs. Talk to your health care provider about clinical trials, their benefits and risks, and whether one is right for you.
We have new and better treatment options today because of what clinical trials uncovered years ago. Be part of tomorrow’s medical breakthroughs. Talk to your health care provider about clinical trials, their benefits and risks, and whether one is right for you.
To learn more or find a study, visit:
- NIMH’s Clinical Trials webpage: Information about participating in clinical trials
- Clinicaltrials.gov: Current Studies on Borderline Personality Disorders: List of clinical trials funded by the National Institutes of Health (NIH) being conducted across the country
Health Hotlines
- 988 Suicide & Crisis Lifeline: The Lifeline provides 24-hour, confidential support to anyone in suicidal crisis or emotional distress. Call or text 988 to connect with a trained crisis counselor. Support is also available via live chat. Para ayuda en español, llame al 988.
- Disaster Distress Hotline: People affected by any disaster or tragedy can call this helpline, sponsored by the Substance Abuse and Mental Health Services Administration, to receive immediate counseling.
 Call or text 1-800-985-5990 to connect with a trained professional from the closest crisis counseling center within the network.
Call or text 1-800-985-5990 to connect with a trained professional from the closest crisis counseling center within the network. - Veterans Crisis Line: This helpline is a free, confidential resource for Veterans of all ages and circumstances. Call 1-800-273-8255, press "1"; text 838255; or chat online to connect with 24/7 support.
- Crisis Text Line: Text HELLO to 741741 for free and confidential support 24 hours a day throughout the U.S.
- More NIH Information Lines
Learn More
Free Brochures and Shareable Resources
- Borderline Personality Disorder: A brochure that offers basic information about borderline personality disorder, including signs and symptoms, treatment, and finding help. Also available en español.
- 5 Action Steps for Helping Someone in Emotional Pain: Infographic presenting five steps for helping someone in emotional pain to prevent suicide.
 Also available en español.
Also available en español. - Suicide in America: Frequently Asked Questions: Fact sheet can help you, or a friend or family member, learn about the signs and symptoms, risk factors and warning signs, and ongoing research about suicide and suicide prevention. Also available en español.
- Warning Signs of Suicide: An infographic presenting behaviors and feelings that may be warnings signs that someone is thinking about suicide. Also available en español.
- Shareable Resources on Borderline Personality Disorder: Help support borderline personality disorder awareness and education in your community. Use these digital resources, including graphics and messages, to spread the word about borderline personality disorder.
Multimedia
- Experts Discuss Borderline Personality Disorder: Learn the signs, symptoms, diagnosis, treatments, and the latest research on borderline personality disorder.
Federal Resources
- Borderline Personality Disorder (MedlinePlus Medical Encyclopedia)
- Introduction to Co-Occurring Borderline Personality Disorder and Substance Use Disorders (Substance Abuse and Mental Health Services Administration)
- Personality Disorders (MedlinePlus - also en español)
Research and Statistics
- Journal Articles: References and abstracts from MEDLINE/PubMed (National Library of Medicine).
- Statistics: Personality Disorders: Webpage listing information on the prevalence of personality disorder among adults.
Last Reviewed: April 2022
Unless otherwise specified, NIMH information and publications are in the public domain and available for use free of charge. Citation of NIMH is appreciated. Please see our Citing NIMH Information and Publications page for more information.
Borderline personality disorder | NAMI: National Alliance on Mental Illness
- Overview
- Treatment
- Support
- Discuss
Borderline Personality Disorder (BPD) is a condition characterized by difficulties regulating emotion. This means that people who experience BPD feel emotions intensely and for extended periods of time, and it is harder for them to return to a stable baseline after an emotionally triggering event.
This difficulty can lead to impulsivity, poor self-image, stormy relationships and intense emotional responses to stressors. Struggling with self-regulation can also result in dangerous behaviors such as self-harm (e.g. cutting).
It’s estimated that 1.4% of the adult U.S. population experiences BPD. Nearly 75% of people diagnosed with BPD are women. Recent research suggests that men may be equally affected by BPD, but are commonly misdiagnosed with PTSD or depression.
Symptoms
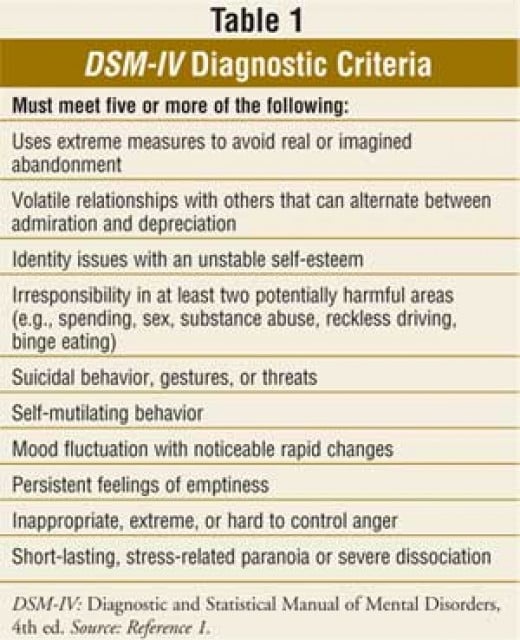
People with BPD experience wide mood swings and can feel a great sense of instability and insecurity.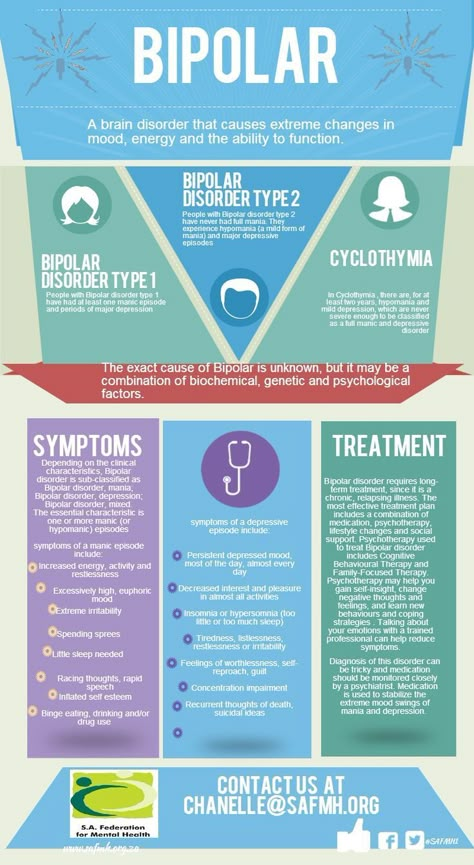 According to the Diagnostic and Statistical Manual diagnostic framework, some key signs and symptoms may include:
According to the Diagnostic and Statistical Manual diagnostic framework, some key signs and symptoms may include:
- Frantic efforts to avoid real or imagined abandonment by friends and family.
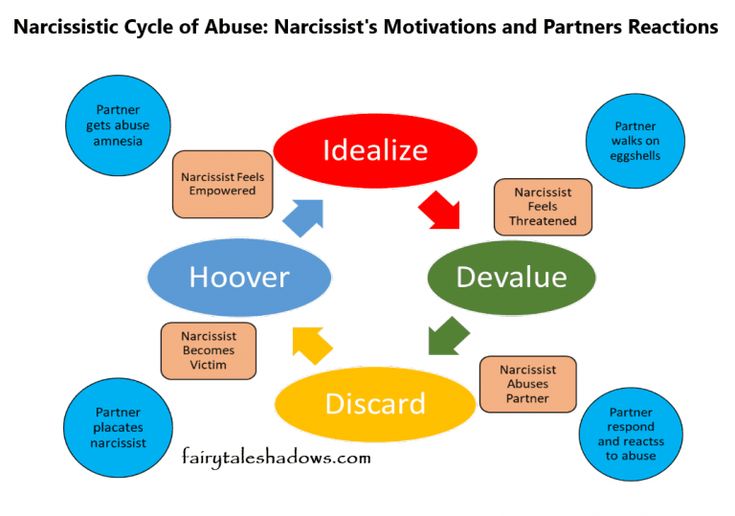
- Unstable personal relationships that alternate between idealization (“I’m so in love!”) and devaluation (“I hate her”). This is also sometimes known as "splitting."
- Distorted and unstable self-image, which affects moods, values, opinions, goals and relationships.
- Impulsive behaviors that can have dangerous outcomes, such as excessive spending, unsafe sex, reckless driving, or misuse or overuse of substances.
- Self-harming behavior including suicidal threats or attempts.
- Periods of intense depressed mood, irritability or anxiety lasting a few hours to a few days.
- Chronic feelings of boredom or emptiness.
- Inappropriate, intense or uncontrollable anger—often followed by shame and guilt.
- Dissociative feelings—disconnecting from your thoughts or sense of identity or “out of body” type of feelings—and stress-related paranoid thoughts.
 Severe cases of stress can also lead to brief psychotic episodes.
Severe cases of stress can also lead to brief psychotic episodes.
Causes
The causes of BPD are not fully understood, but scientists agree that it is the result of a combination of factors, including:
- Genetics. While no specific gene or gene profile has been shown to directly cause BPD, research suggests that people who have a close family member with BPD may be at a higher risk of developing the disorder.
- Environmental factors. People who experience traumatic life events—such as physical or sexual abuse during childhood or neglect and separation from parents—are at increased risk of developing BPD.
- Brain function. The emotional regulation system may be different in people with BPD, suggesting that there is a neurological basis for some of the symptoms. Specifically, the portions of the brain that control emotions and decision-making/judgment may not communicate optimally with one another.
Diagnosis
There is no definitive medical test to diagnose BPD, and a diagnosis is not based on one specific sign or symptom. BPD is best diagnosed by a mental health professional following a comprehensive clinical interview that may include talking with previous clinicians, reviewing previous medical evaluations and, when appropriate, interviews with friends and family.
Treatment
An effective treatment plan should include your preferences while also addressing any other co-existing conditions you may have. Examples of treatment options include psychotherapy; medications; and group, peer and family support. The overarching goal of treatment is for a person with BPD to increasingly self-direct their own treatment plan as they learn what works and what doesn’t.
- Psychotherapy—such as dialectical behavioral therapy (DBT), cognitive behavioral therapy (CBT) and psychodynamic psychotherapy—is the first line of choice for BPD. Learning ways to cope with emotional dysregulation in a therapeutic setting is often the key to long-term improvement for those experiencing BPD.
- Medications may be instrumental to a treatment plan, but there is no one medication specifically made to treat the core symptoms of BPD. Rather, several medications can be used off-label to treat various symptoms. For example, mood stabilizers and antidepressants help with mood swings and dysphoria. And for some, low-dose antipsychotic medication may help control symptoms such as disorganized thinking.
- Short-term hospitalization may be necessary during times of extreme stress, and/or impulsive or suicidal behavior to ensure safety.
Related Conditions
BPD can be difficult to diagnose and treat, and successful treatment includes addressing any other conditions a person might have. Many with BPD also experience additional conditions like:
- Anxiety Disorders
- Posttraumatic Stress Disorder
- Bipolar Disorder
- Depression
- Eating Disorders (notably bulimia nervosa)
- Substance Use Disorders / Dual Diagnosis
Reviewed December 2017
Borderline personality disorder
Borderline personality disorder is associated with unstable mood and behavior that has a significant impact on a person's daily life
Borderline personality disorder is a type of personality disorder in which a person experiences periods of tension, unstable moods and behaviors, and an altered "feeling of self".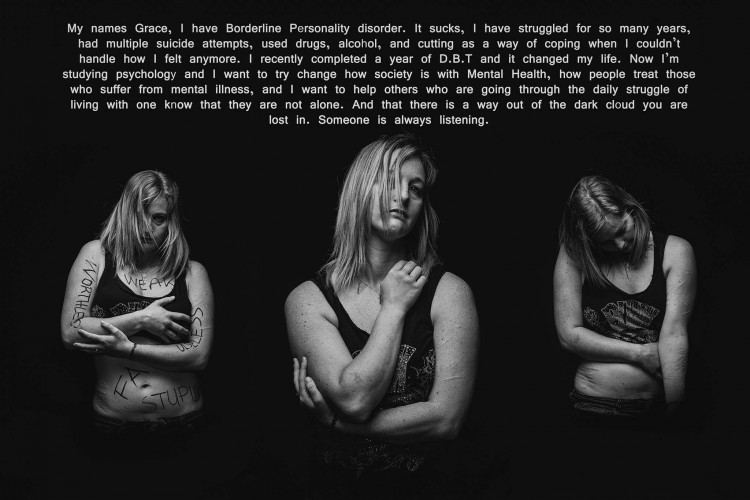 1 All of these can result in impulsive actions and relationship problems with friends and family members, impairing the person's ability to cope with everyday life. 1.2
1 All of these can result in impulsive actions and relationship problems with friends and family members, impairing the person's ability to cope with everyday life. 1.2
Borderline personality disorder is a serious illness associated with self-harm and suicidal attempts. One in ten patients complete suicide. 2
Facts About Borderline Personality Disorder
Borderline personality disorder is a type of personality disorder in which a person experiences periods of tension, unstable mood and behavior, and an altered sense of self. 1
One in ten patients complete suicide. 2
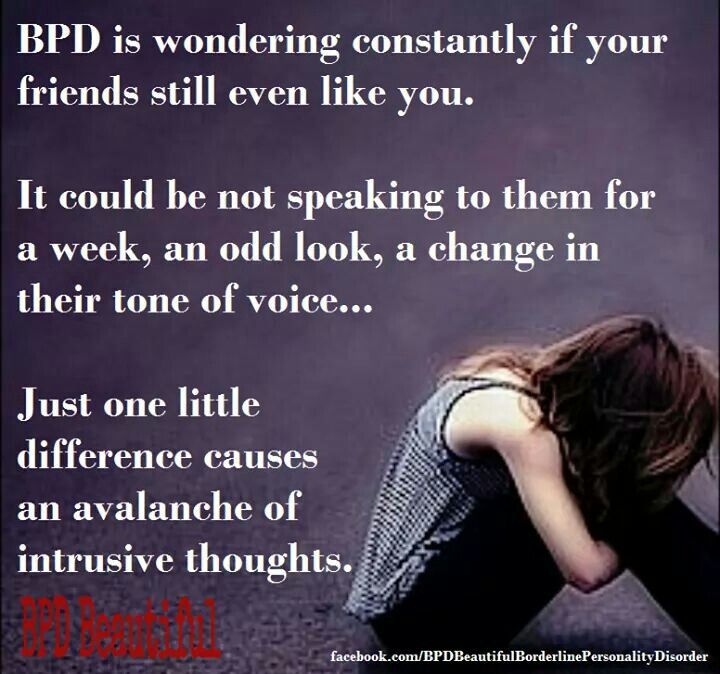
Patients with borderline personality disorder are very sensitive to changes in their environment, and may respond inappropriately and acutely to such changes. They may, for example, be afraid of being abandoned by a loved one. 2 If the person whom patient
2 If the person whom patient
is expecting arrives late, the patient easily changes the feeling of attachment to dislike or anger.1,2 This reflects the extreme perception of the world by the patient, who sees everything and everyone - including oneself – either good or bad.1,2
People with borderline personality disorder are often insecure, may suddenly change their life goals and views on career, life values and friends. .2 They may develop intense unwarranted anger or feelings of emptiness, and are prone to self-harm.2 Patients with borderline personality disorder may also experience depression and anxiety.1,2
Facts about Borderline Personality Disorder
Estimates of the proportion of people who have borderline personality disorder vary from less than 1% to around 6%. 2-4
Borderline personality disorder affects a roughly equal number of men and women, but appears to be more disabling in women the same frequency in men and women, but in women it is more severe. 3
3
Symptoms of borderline personality disorder most often first appear during adolescence.4 The disease is most severe and problematic in young adults and tends to improve with age.2 Symptoms may persist throughout life, but most patients with borderline personality disorder by the age of 30-40 have a stable job and a home.2
People with borderline personality disorder are emotionally and functionally unstable, which places a significant burden on their families.5 Mood swings are a source of stress for both the patient and his/her others, which can lead to the development of mental disorders in the latter.1,5
People who are concerned that they – or their loved ones – are experiencing symptoms of borderline personality disorder should see their doctor for help and advice.
Borderline personality disorder is diagnosed by a mental health professional using interviews and discussions about symptoms and medical history. 1
1
Psychotherapy can help people with borderline personality disorder by, for example, teaching them how to interact with others and to express their thoughts and feelings more clearly. 1 It may also be beneficial for caregivers and family members of those affected to receive therapy and guidance on how best to care for a person with borderline personality disorder. 1 There is currently no cure, but one study showed that, after 10 years, 50% of people with borderline personality disorder had recovered, being able to function at work and maintain personal relationships. 6
- National Institute of Mental Health. borderline personality disorder. NIH publication number QF 17-4928. Available from: https://www.nimh.nih.gov/health/publications/borderline-personality-disorder/index.shtml [accessed 30 September 2019].
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders.
 5th ed. Arlington, VA: American Psychiatric Association; 2013.
5th ed. Arlington, VA: American Psychiatric Association; 2013. - Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2008;69(4):533–545.
- National Institute for Health and Clinical Excellence. Borderline personality disorder: recognition and management. 2009. Available from: https://www.nice.org.uk/guidance/cg78/resources/borderline-personality-disorder-recognition-and-management-pdf-975635141317 [accessed 30 September 2019].
- Bailey RC, Grenyer BFS. Burden and support needs of carers of persons with borderline personality disorder: a systematic review. Harv Rev Psychiatry. 2013;21(5):248–258.
- Zanarini MC, Frankenburg FR, Reich DB, Fitzmaurice G. Time to attainment of recovery from borderline personality disorder and stability of recovery: a 10-year prospective follow-up study.
Am J Psychiatry. 2010;167(6):663–667.
1. National Institute of Mental Health. borderline personality disorder. NIH publication number QF 17-4928. Available from: https://www.nimh.nih.gov/health/publications/borderline-personality-disorder/index.shtml [accessed 30 September 2019].
2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013.
3. Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2008;69(4):533–545.
4. National Institute for Health and Clinical Excellence. Borderline personality disorder: recognition and management. 2009. Available from: https://www.nice.org.uk/guidance/cg78/resources/borderline-personality-disorder-recognition-and-management-pdf-975635141317 [accessed 30 September 2019].
Access to Brain Health
We are dedicated to improving access to brain health in accordance with WHO.
Our Science
Lundbeck has developed some of the world’s most widely prescribed therapies.
This is Lundbeck
A specialized pharmaceutical company focused exclusively on brain diseases.
Borderline personality disorder: what it is, symptoms and signs of BPD
Borderline personality disorder is characterized by emotional instability, impulsive behavior and low self-control. Forbes Life figured out what causes this disease, how to diagnose borderline personality disorder and how to help people who have experienced it
Mental personality disorders differ from other types of disorders in their intensity. They cannot be treated like an ordinary illness, as a temporary mental disorder, because personality disorders affect a set of personal characteristics formed in childhood. There are a number of problems with diagnosing such diseases: their symptoms are quite individual, although there are a number of common signs. For borderline personality disorder (BPD), these may include difficulties with self-image, extreme mood swings, risky behavior, and self-harm. The good news is that personality disorders can still be managed—there is a cure.
Finished reading here
Now officially: BPD is a diagnosis
Borderline personality disorder is one of ten types of personality disorders in modern psychotherapy, which is expressed in problems of awareness and formation of personal identity. Psychologist, Gestalt therapist Valentin Oskin notes that this mental illness is associated with strong, uncontrollable and often painful emotions that lead to a distorted sense of self and unstable interpersonal relationships.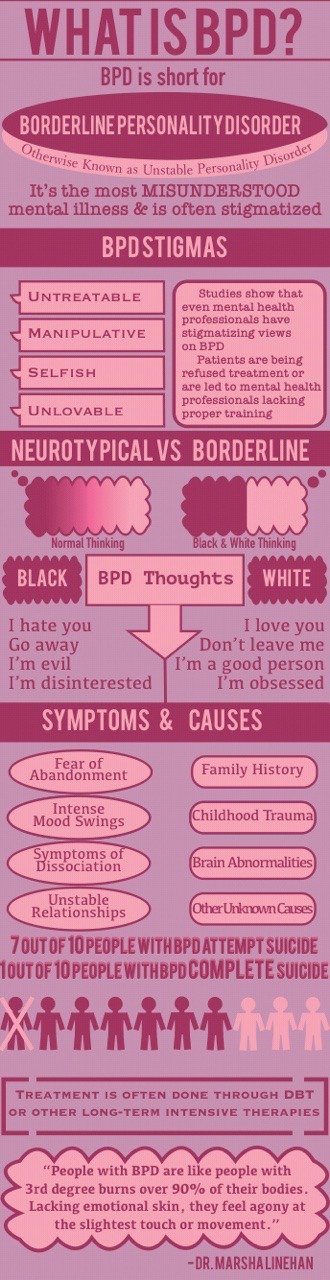
People with BPD are reverse solipsists: they are convinced of the inviolability of the world around them, but doubt the reality of their own existence - their image of the inner “I” is so mobile and unstable. In addition to depersonalization, "borderguards" are characterized by impulsiveness, dependence on other people, unstable behavior, a tendency to a chaotic life, and even a need to harm themselves and injure themselves. "Border guards" are characterized by chronic suicidality: 75% of people with BPD try to commit suicide, of which about 10% die as a result of suicide. Moreover, a third of all completed suicides were committed by those suffering from borderline personality disorder.
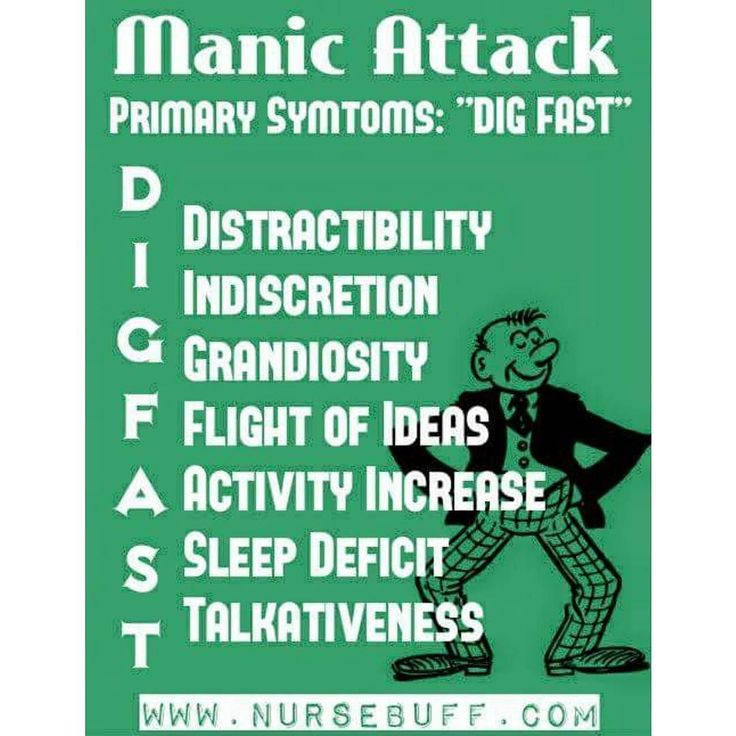
Despite the statistics, until 2022 the diagnosis of BPD in Russia could not be officially diagnosed - borderline personality disorder in psychiatry was defined as a disease only in foreign classifications of diseases. It was often called impulsive personality disorder or generally diagnosed as sluggish schizophrenia: the diseases are similar in symptoms, among the signs of BPD there are no hallucinations and delusions. BPD also resembles bipolar affective disorder (up to 40% of "border guards" get an erroneous diagnosis of bipolar disorder), only periods of depressive and elated mood are replaced with bipolar disorder less often. The transition to the International Classification of Diseases of the 11th revision will finally allow doctors to make an accurate diagnosis for Russian citizens and prescribe the appropriate treatment.
It was often called impulsive personality disorder or generally diagnosed as sluggish schizophrenia: the diseases are similar in symptoms, among the signs of BPD there are no hallucinations and delusions. BPD also resembles bipolar affective disorder (up to 40% of "border guards" get an erroneous diagnosis of bipolar disorder), only periods of depressive and elated mood are replaced with bipolar disorder less often. The transition to the International Classification of Diseases of the 11th revision will finally allow doctors to make an accurate diagnosis for Russian citizens and prescribe the appropriate treatment.
Diagnosis is not a sentence, the boundary between normal and pathological is very flexible: “Each of us has borderline responses. For some, they are deeply hidden and appear only in crises, traumas, stressful situations. And for some, life as such is stressful, and therefore the ways of responding turn into what psychologists could call the borderline organization of the personality,” notes Irina Mlodik, Candidate of Psychological Sciences, in the book “House of Cards. Psychotherapeutic assistance to clients with borderline disorders.
Psychotherapeutic assistance to clients with borderline disorders.
Related material
Ghost hints
Most people with BPD are unaware of their diagnosis and do not seek medical attention. And it's not just that BPD in psychology does not have a clear definition. The disease does not allow you to objectively assess your mental state and understand that the indomitable monster inside is raging not because of the permanent retrograde Mercury and the fatal force of circumstances. The absence of obvious mental abnormalities like hallucinations makes it possible to attribute emotional behavior to character traits. Colleagues, friends and relatives often believe that behind the disgusting behavior of such a person is hysteria and selfishness. Therefore, systematic treatment of borderline personality disorder begins in most cases after a suicide attempt.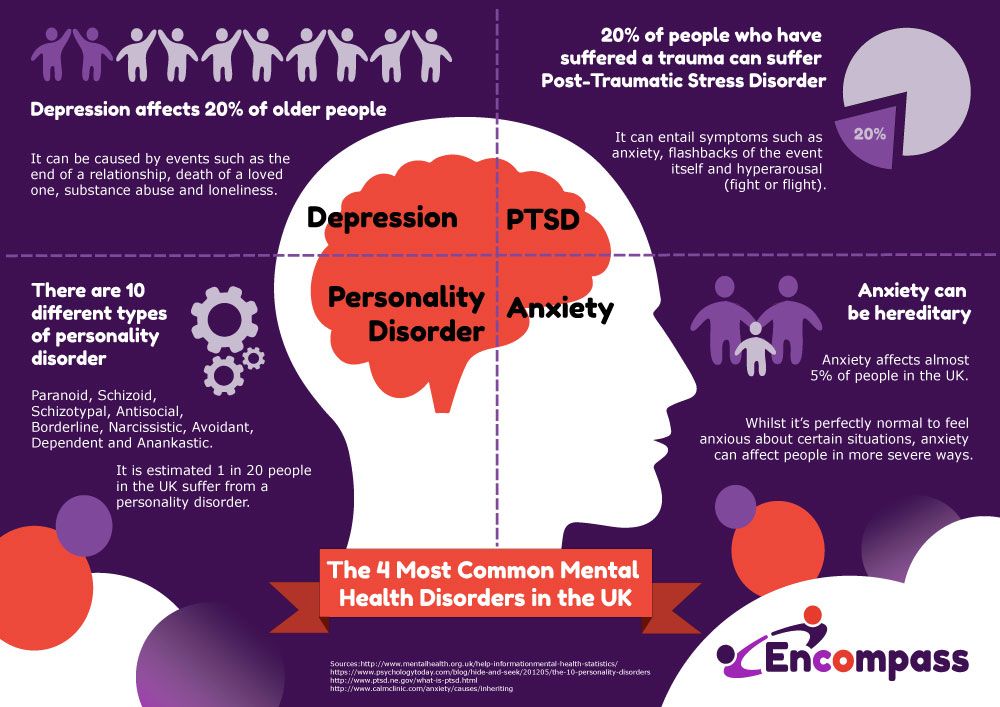
The most striking and obvious sign of borderline personality disorder is a craving for auto-aggression, or self-harm. This is not only the infliction of bodily harm (cuts, blows or burns), but also the intention to deprive oneself of sleep, nutrition. This practice is not necessarily a consequence of suicidal behavior: physical pain serves as a way to drown out inner pain, to switch attention from uncontrollable emotions to those that have become the result of an effort of will. The problem is that self-harm is either carefully hidden by people with BPD because it is not normal in our culture, or they perceive it as controlled behavior (eg, exhausting workouts in the gym, striving to do work tasks in their free time).
Borderline personality disorder may be accompanied by alcohol, drug, gambling and a number of other diseases. “For example, depression, anxiety disorders, eating disorders are common in people with BPD. Often, a history of PTSD or CPTSD is found, ”notes Valentin Oskin. That is, constant panic attacks or overeating in the evenings can be a sign of more serious mental disorders than just a reaction to stress.
Often, a history of PTSD or CPTSD is found, ”notes Valentin Oskin. That is, constant panic attacks or overeating in the evenings can be a sign of more serious mental disorders than just a reaction to stress.
Mind, a British mental health resource, highlights the following symptoms that may indicate borderline personality disorder. If they last long enough and have a negative impact on your life, it makes sense to consult a psychotherapist or psychiatrist:
- Fear of being alone. You constantly worry about people leaving you and are ready to do everything to prevent this from happening.
- Impulsivity and affectivity. You are overcome by strong emotions that last from several hours to several days and can change quickly (for example, from feelings of happiness and confidence to sudden depression and sadness). This is especially evident in a state of anger, which is difficult to control.
 In a state of severe stress, you may also experience paranoia or dissociation (as if everything is not happening to you, but to someone else).
In a state of severe stress, you may also experience paranoia or dissociation (as if everything is not happening to you, but to someone else). - Depersonalization. There is no clear idea of who you really are: the sense of self and behavior changes radically depending on where and with whom you are. As an option - a constant feeling of emptiness inside, boredom, misunderstanding of one's true desires and values.
- Communication problems. It is very difficult for you to create and maintain stable relationships, you are prone to masochistic communication, cyclically idealize and devalue even the closest people, and do not always correctly interpret the motives of the actions of others.
“Borderline personality disorder can manifest itself in a wide range of signs,” says Valentin Oskin, “the symptoms of borderline personality disorder are most fully described in the DSM-5 and ICD-11 reference books.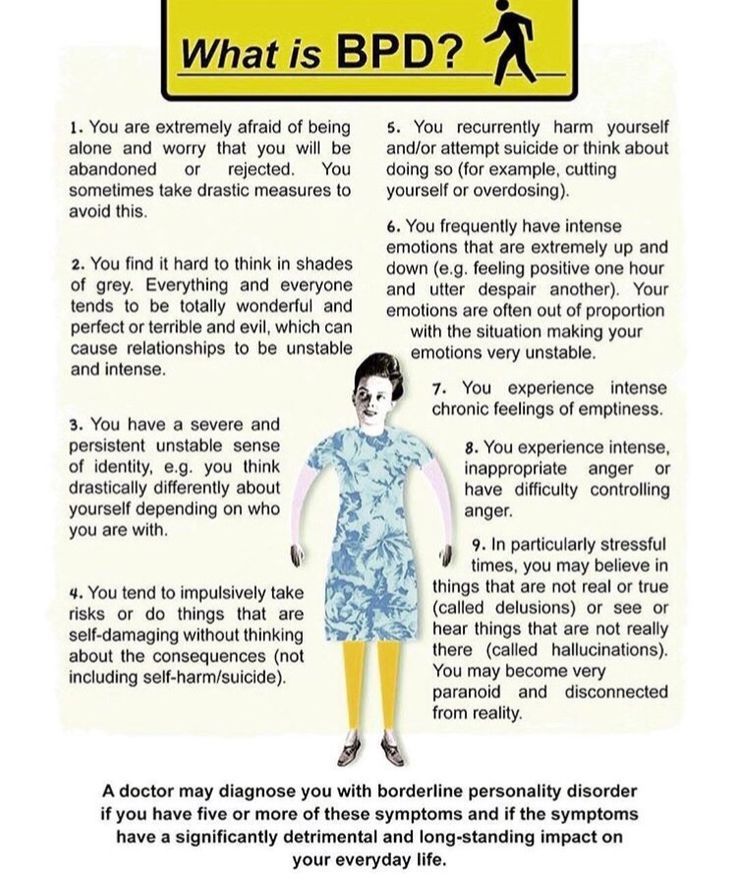 If grouped together, the symptoms will reflect a lack of control in the emotional, behavioral, cognitive spheres, as well as a distortion of the sense of self and a violation of interpersonal relationships. According to the psychologist, it is extremely difficult for people with BPD to break off relationships, even those that need to be broken off. Instead, they may go to great lengths to keep the people who matter to them around them.
If grouped together, the symptoms will reflect a lack of control in the emotional, behavioral, cognitive spheres, as well as a distortion of the sense of self and a violation of interpersonal relationships. According to the psychologist, it is extremely difficult for people with BPD to break off relationships, even those that need to be broken off. Instead, they may go to great lengths to keep the people who matter to them around them.
At the same time, “border guards” tend to involuntarily throw out their emotions on those who are dear to them: “Often this ends with interruption of communication, because not everyone is able to endure such a bolt from the blue. And even more so if this thunder rumbles once every couple of months, ”Ksenia Ivanenko notes in her Telegram channel, where she describes her personal experience in dealing with BPD.
Related material
To determine if you are at risk, you can take several tests for borderline personality disorder that are publicly available. It is important to understand that the result obtained is not a final diagnosis, it can only be made by a qualified doctor after analyzing the symptoms.
It is important to understand that the result obtained is not a final diagnosis, it can only be made by a qualified doctor after analyzing the symptoms.
The Root of the Problem: What Causes Borderline Personality Disorder
Effective treatment for most mental illnesses requires identifying the cause. Borderline personality disorder is problematic in that it arises from a number of factors and affects the basic components of the personality. That is, there is simply no specific reason that triggers the PRL processes. “While BPD is one of the most researched personality disorders, there is no consensus on what exactly causes it. Severe stresses experienced by children and adolescents, such as neglect, prolonged painful separation, loss of a parent, violence, are common in people with BPD. There is also evidence of a genetic predisposition: among first-line relatives of a person with borderline disorder, the likelihood of developing a similar disorder is 3-5 times higher when compared with the general population,” notes Valentin Oskin.
Any person can be at risk, especially if he is going through a difficult stressful situation. It is known that this diagnosis is made more often in women than in men, and that in almost all cases of BPD it is driven by a deep emotional shock. Most researchers agree that the development of BPD is promoted by a combination of two groups of factors:
- Stress and traumatic life situations. For example, sexual, physical, or emotional abuse, persistent feelings of fear or abandonment during childhood, family problems, repressed feelings of anger, anxiety, and sadness. Stress or trauma in adulthood can trigger the onset of borderline personality disorder.
- Genetic predisposition and environmental influences. The disease can be inherited, but more often borderline occurs as a pattern of behavior unconsciously borrowed from parents or close people, reactions to external stimuli.
Related material
No reason to break ties
If there is a “border guard” in your environment, you can build constructive communication with him, although this will require a lot of effort. “It is important to understand that a person with borderline personality disorder takes criticism extremely hard, for him it sounds like rejection, which he is terribly afraid of. At the same time, emotional jumps do not allow him to get the desired intimacy. Relations with such a person are usually like a swing between the poles "I love you, don't leave me - I hate you, I'll leave you." It is important to understand that with borderline personality disorder it is impossible to consciously change your behavior, thinking, emotional reactions and response patterns to certain situations, ”says Valentin Oskin.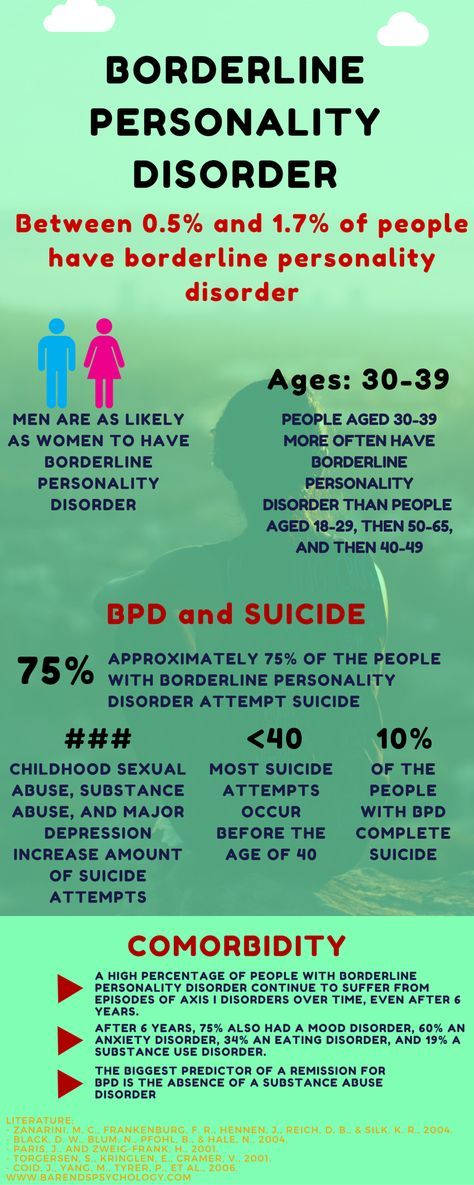
Many "border guards" live with a constant oppressive feeling of guilt, they feel broken, bad and unworthy of normal communication, which they badly need. They are unable to correctly read the reactions of others and the motives of their actions. This determines their strange behavior and repels potential partners and friends. Often, people with borderline personality disorder have a Favorite Person - a person on whom the "borderguard" is extremely dependent and who replaces not only everyone around him, but also himself. If this person is busy or there is a conflict with him, the “border guard” literally collapses the world: he drowns in a storm of emotions, reflects on death and looks for thousands of reasons why he was rejected.
There are a number of rules that psychologists have developed for those who seek to communicate as "border guards", minimizing chaos, conflicts and the possibility of a tragic denouement: could end in disaster.
Related material
How to get rid of BPD
The main way to deal with borderline personality disorder is psychotherapy, in which work is done on the accompanying manifestations of an unstable mental state (depression, addictions, eating disorders, etc. ) and syndromes (it is often necessary to treat alcohol withdrawal symptoms) syndrome). This is a long and complicated process, but statistics show that 70% of the “border guards” get rid of the main symptoms during therapy within six years, and remission occurs in a third of patients after two years.
) and syndromes (it is often necessary to treat alcohol withdrawal symptoms) syndrome). This is a long and complicated process, but statistics show that 70% of the “border guards” get rid of the main symptoms during therapy within six years, and remission occurs in a third of patients after two years.
“In therapy, people with BPD are primarily trained in emotional control, responsibility, and interpersonal skills. Dialectico-behavioral psychotherapy, a specially developed method for the treatment of BPD based on cognitive behavioral therapy, is well suited for this. No less effective is schema therapy, which also has special developments for the treatment of BPD. In the course of treatment, pharmacotherapy can also be prescribed, for example, for the treatment of associated depression or anxiety disorder, ”says Valentin Oskin.
Comprehensive treatment may include the following therapies:
- Dialectical Behavioral Therapy (DBT).