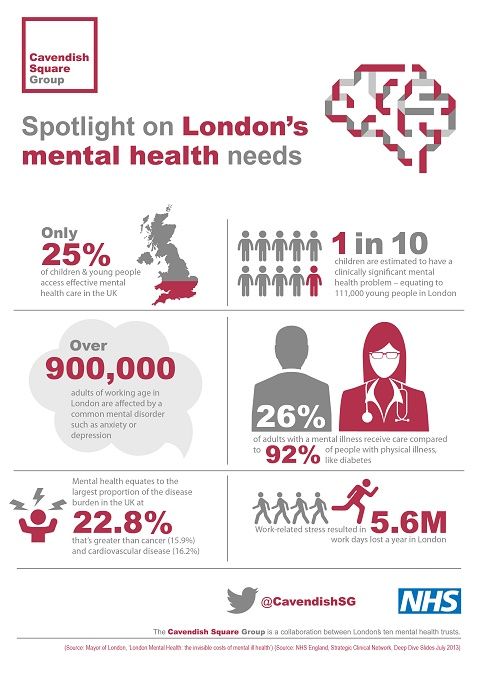
Mental health services in the uk
How to access mental health services
Find out about the different ways to get help with your mental health, the process, and your rights.
Information:
Mental health services are free on the NHS. Your mental health is important and you should get help if you need it.
Find NHS mental health services
Talk to your GP first
You'll need to talk to your GP to use some mental health services. This is known as a GP referral. Your GP can also talk to you about your mental health and help introduce you to the right mental health service for your needs.
Find your local GP surgery
Get help without talking to your GP
There are also some mental health services that you can use without talking to your GP first. This is known as self-referral.
For example, you may be able to refer yourself for help with drug problems and alcohol problems. You can also use self-referral to access talking therapies through a service called Improving Access to Psychological Therapies (IAPT).
NHS psychological therapies services
Get help through your work
If your mental health problem is because of stress at work, your employer might be able to refer you to occupational health services.
You can find out more from the Time to Change website.
Advice on mental health at work from Time to Change
Get help from your school or college
If you're a child or young person, your school or college might be able to refer you directly to a specialist mental health service.
Children and young people's mental health services (CYPMHS)
How mental health referrals work
When you talk to your GP about your mental health they'll listen, give you advice and introduce you to a mental health service they think will be most helpful to you.
These services may come from your GP surgery, a large local health centre, a specialist mental health clinic or a hospital.
Your GP can also refer you to a psychological therapy service or a specialist mental health service for further advice or treatment. The treatment may be provided on a one-to-one basis or in a group with others with similar problems. Therapy can also sometimes involve partners and families.
Your right to choose who helps you
In most cases, you have a right to choose which mental health service provider you go to in England.
You have the legal right to choose which service provider and clinical team you're referred to for your first appointment.
What is a mental health service provider?The NHS works with various organisations to run mental health services across England. They might be charities, private companies or not-for-profit organisations. These are called service providers.
You do not have a legal right to choose if:
- you need urgent or emergency treatment
- you already receive care and treatment for the condition
- the organisation or clinical team you've chosen does not provide the right care for your condition
- you're a prisoner or on temporary release from prison
- you're detained in prescribed accommodation, such as a court, secure children's home, secure training centre, immigration removal centre or young offender institution
- you're detained in a secure hospital setting
- you're a serving member of the armed forces
- you're detained under the Mental Health Act 1983
The NHS Choice Framework on GOV. UK explains all the details of your legal right to choose.
UK explains all the details of your legal right to choose.
Once you've chosen a service provider you also have the right to choose the mental health service team that will be in charge of your treatment.
You'll be seen by the consultant or named professional who leads the mental health team, or by another healthcare professional on the team.
How to book your appointment
Once you've decided on a mental health service provider, you might be able to book your appointment through the NHS e-Referral Service.
There are a few ways to do this:
- your GP can book it while you're at the surgery
- you can book it online yourself, using the appointment request letter your GP gives you
- you can phone the NHS e-Referral Service line on 0345 60 88 88 8, open Monday to Friday, 8am to 8pm, and from 8am to 4pm on weekends and bank holidays
If the service you're being referred to is led by a consultant it will be covered by the NHS's commitment to make sure you're seen within 18 weeks.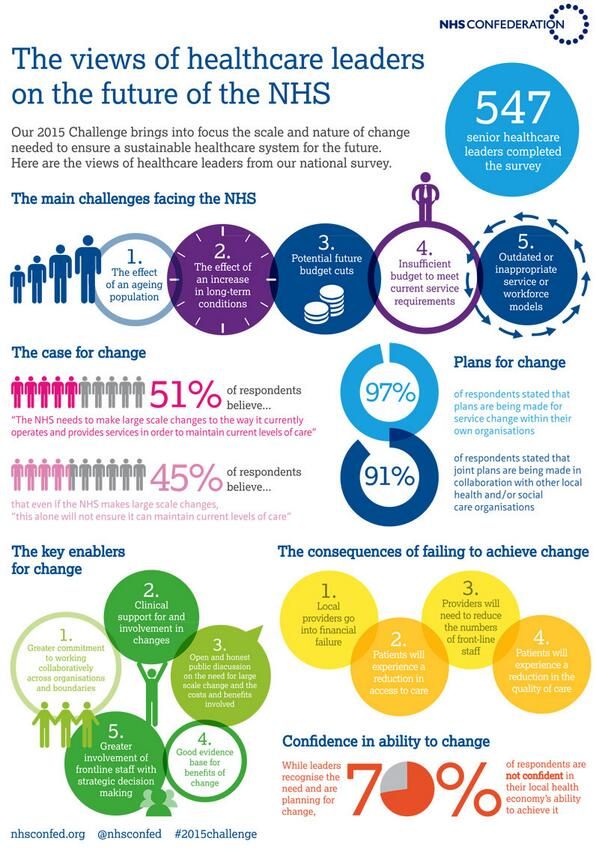
Waiting times for other services will be different depending on where you are in England.
Find out more about waiting times for NHS services
Page last reviewed: 17 February 2022
Next review due: 17 February 2025
NHS England » Community mental health services
Community mental health services play a crucial role in delivering mental health care for adults and older adults with severe mental health needs as close to home as possible.
The NHS Long Term Plan and NHS Mental Health Implementation Plan 2019/20 – 2023/24 set out that the NHS will develop new and integrated models of primary and community mental health care.
A new community-based offer will include access to psychological therapies, improved physical health care, employment support, personalised and trauma informed care, medicines management and support for self-harm and coexisting substance use.
By 2023/24, this will enable at least 370,000 adults and older adults per year nationally to have greater choice and control over their care, and to live well in their communities.
This ambition is supported by an additional £1 billion new Long Term Plan funding per year by 2023/24 to ultimately transform the provision of community mental health care for adults and older adults with severe mental illnesses.
Under the Long Term Plan by 2023/24:
- All Sustainability and Transformation Partnerships (STPs)/Integrated Care Systems (ICSs) will have received funding to develop and begin delivering new models of integrated primary and community care for adults and older adults with severe mental illnesses (SMI).
- These new models of care will span both core community provision and dedicated services, where the evidence supports them. The new models will be built around Primary Care Networks.
- A total of 390,000 people with SMI will receive a physical health check.

- A total of 55,000 people a year will have access to Individual Placement and Support (IPS) services.
- New local funding will also be used to maintain and develop new services for people who have specific or additional needs, including Early Intervention in Psychosis (EIP), complex mental health difficulties associated with a diagnosis of ‘personality disorder’, mental health rehabilitation and adult eating disorders.
We have announced a new transformation fund to support this ambition: in 2019/20 and 2020/21, 12 STPs/ICSs are to receive over £70 million of additional funds to test new models of integrated care and four-week waiting times as part of the Clinically-led Review of NHS Access Standards:
- Cambridgeshire and Peterborough STP
- Cheshire and Merseyside STP
- Frimley Health and Care ICS
- Herefordshire and Worcestershire STP
- Hertfordshire and West Essex STP
- Humber, Coast and Vale Health and Care Partnership
- Lincolnshire STP
- North East London STP
- North West London STP
- Somerset STP
- South Yorkshire and Bassetlaw ICS
- Surrey Heartlands Health and Care Partnership
These early implementer sites will test how the barriers between primary and secondary care can be dissolved. They will lead transformation of community mental health services in England in partnership with Primary Care Networks (PCN) and integrated care systems (ICSs), as well as local authorities and the Voluntary, Community and Social Enterprise sector (VCSE), service users, families and carers, and local communities themselves.
They will lead transformation of community mental health services in England in partnership with Primary Care Networks (PCN) and integrated care systems (ICSs), as well as local authorities and the Voluntary, Community and Social Enterprise sector (VCSE), service users, families and carers, and local communities themselves.
We will use their findings to inform the roll out of new models of integrated primary and community care at the national level, and from 2021/22 to 2023/24, all STPs/ICS will receive a fair share of transformation funding to implement these models locally, in addition to year-on-year increases in baseline funding for all ICSs to bolster community mental health provision starting in 2019/20.
NHS England have also developed a new Framework to support local systems in implementing the Long Term Plan’s vision for transforming community mental health care.
Further resources are being developed to support improved community services for adults with SMI, including on the implementation of increased access to psychological therapies for people with SMI.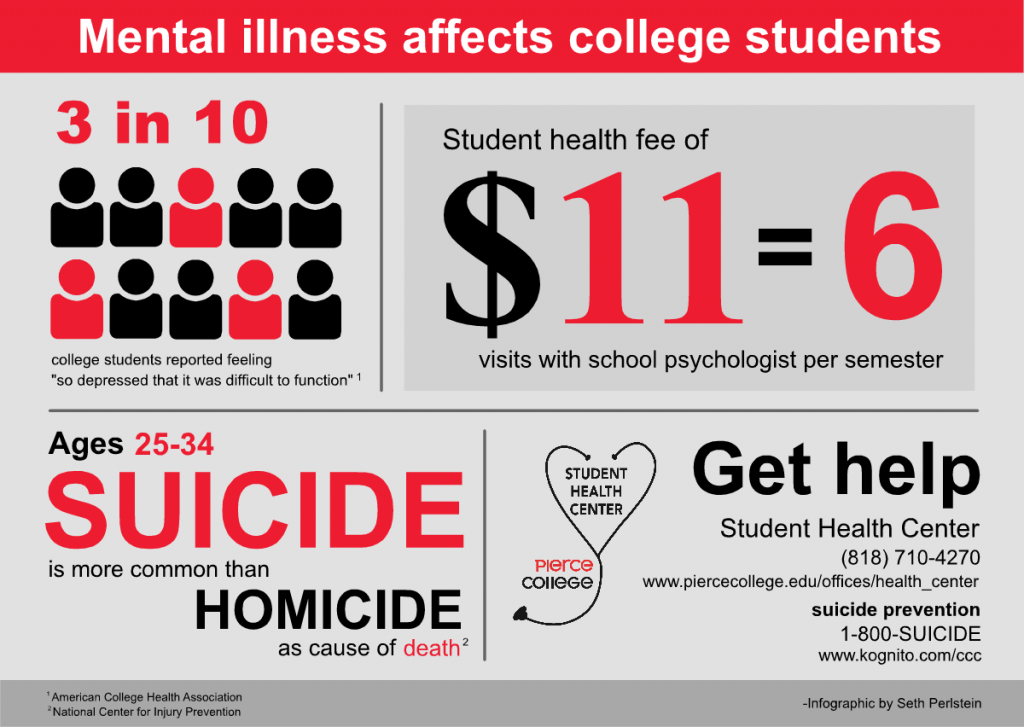
The Community Mental Health Framework for Adults and Older Adults
The new Community Mental Health Framework describes how the Long Term Plan’s vision for a place-based community mental health model can be realised, and how community services should modernise to offer whole-person, whole-population health approaches, aligned with the new Primary Care Networks.
The Framework will be used as the basis for the testing of new integrated primary and community mental health care models across our 12 early implementer sites in 2019/20 and 2020/21.
It is a key resource to inform STPs/ICSs five-year planning process, and to support the effective spend of almost £1 billion new Long Term Plan funding per year by 2023/24.
Care Programme Approach: position statement
The Community mental health framework replaced the Care Programme Approach (CPA) for community mental health services. It enables services to shift away from an inequitable, rigid and arbitrary CPA classification and bring up the standard of care towards a minimum universal standard of high-quality care for everyone in need of community mental healthcare.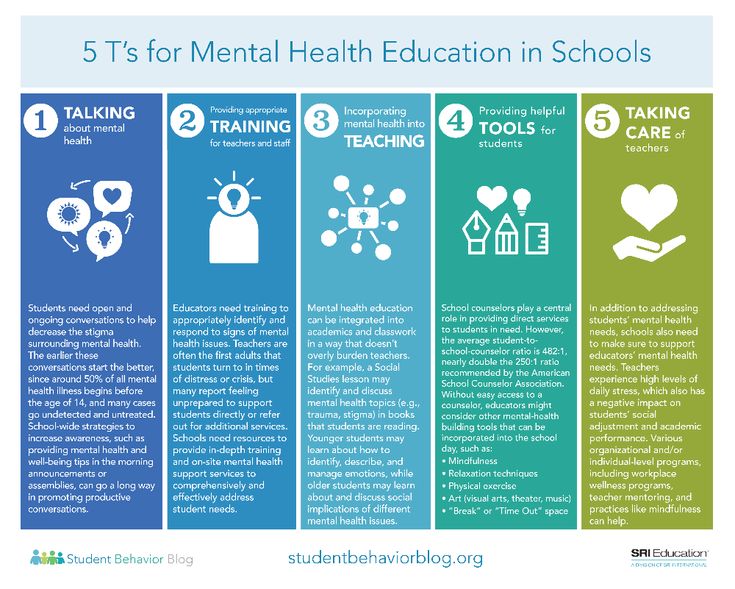
This position statement has been developed in response to queries regarding the national policy position and direction of travel away from the CPA.
Since April 2021, all integrated care systems (ICSs) have received transformation funding to deliver new and integrated models of primary and community mental health care. The position statement will support ICSs to transform, expand and improve community mental health services in line with the framework.
Individual Placement and Support (IPS)
People with severe mental illness (SMI) have low rates of employment (8% vs 75% in the general population). Individual Placement and Support (IPS) is an employment support intervention involving intensive, individual support, a rapid job search followed by placement in paid employment, and in-work support for both the employee and their new employer. It is the best evidence-based approach to help people in this group get and keep a paid job.
As a key commitment in the Five Year Forward View for Mental Health (FYFVMH), NHS England has committed to doubling access to IPS services nationally by 2020/21, enabling more people who experience SMI to find and retain employment, equating to 20,000 people.
The recently published Long Term Plan (LTP) committed the NHS to supporting an additional 35,000 people with severe mental illnesses where this is a personal goal to find and retain employment by 2023/24, a total of 55,000 people per year. This investment will support people to get back into or gain access to employment. It will improve outcomes and recovery for people, meaning they spend less time in hospital and live healthier, happier lives.
To aid the expansion of IPS provision in England, NHS England and NHS Improvement are working with partners Social Finance to deliver IPS Grow, an infrastructure support initiative, which consists of: hands-on implementation support from a network of IPS experts; a workforce development programme; and tools for effective reporting, monitoring and evaluation of services.
A range of IPS Grow resources and guidance has been developed and is available for:
- Commissioners
- IPS Providers
- Individuals looking to begin or develop their career in IPS
For more information on IPS, visit:
- The IPS Grow website
- The Centre for Mental Health website
- Read our case study
Adult Eating Disorders Guidance: Community, Inpatient and Intensive Day Patient Care
As part of work on community based mental health care for adults, alongside work to explore the effectiveness of different approaches to integrated delivery with primary care, NHS England and NHS Improvement are working to improve availability and access to community eating disorder services for adults. Guidance has been published to support commissioners and providers to achieve this.
Guidance has been published to support commissioners and providers to achieve this.
This guidance will support the development and implementation of commissioner, provider and Sustainability and Transformation Partnership/Integrated Care System plans to deliver effective community adult eating disorder services that are integrated with day and/or inpatient care to reduce admissions, length-of-stay and improve outcomes for users, families and carers. This is in line with NHS Long Term Plan ambitions to establish new and integrated models of primary and community mental health care for adults and older adults, including dedicated provision for groups with specific needs such as adults with eating disorders. This guidance also supports the roll-out of the Provider Collaborative (formerly New Care Models) programme to develop NHS-led Provider Collaboratives for adult eating disorder care.
- Adult Eating Disorders Guidance: Community, Inpatient and Intensive Day Patient Care
- Appendices and Helpful Resources for the Adult Eating Disorders Guidance
See also the Children and Young People’s Eating Disorder Guidance.
Early Intervention in Psychosis (EIP)
From April 2016 the early intervention in psychosis standard was introduced. This requires that more than 50 per cent of people experiencing a first episode of psychosis begin treatment with a NICE-approved care package within two weeks of referral.
People who experience psychosis can, and do, recover. The time from onset of psychosis to the provision of evidence-based treatment has a significant influence on long-term outcomes. The sooner people are able to access evidence-based treatment the better the outcomes they achieve.
The EIP standard remains a priority of the NHS and the NHS Long Term Plan and NHS Mental Health Implementation Plan 2019/20 – 2023/24 set out continued commitment to the standard which is included in the Long Term Plan.
Guidance is available to support ongoing local implementation of the standard by commissioners and mental health providers, working with service users and their families, carers and other partners.
NHS England has worked closely with Health Education England in commissioning training places to support delivery of NICE recommended interventions, with a specific focus on cognitive behavioural therapy for psychosis and family interventions.
NHS England has developed helpful resources for commissioners and EIP services to help them meet the EIP standard. Resources includes technical guidance on reporting for the standard, frequently asked questions and good practice examples.
NHS England publishes regular statistics on performance against the waiting time element of the standard.
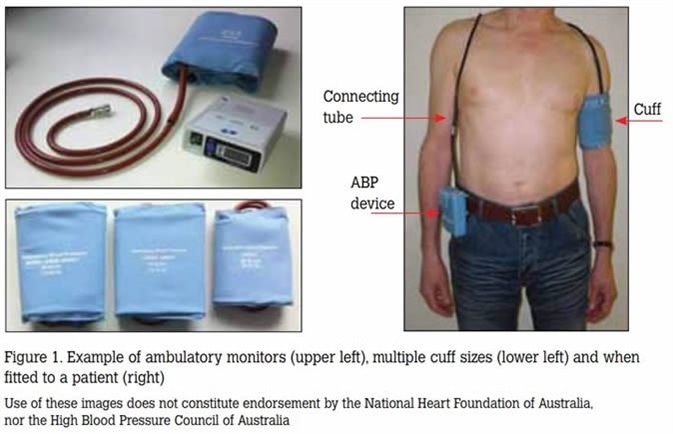
Improving physical health care for people with severe mental illness (SMI)
NHS England is committed to leading work to reduce the premature mortality among people living with severe mental illness (SMI).
People with severe mental illnesses are at higher risk of poor physical health. Compared with the general patient population, patients with severe mental illnesses are at substantially higher risk of obesity, asthma, diabetes, chronic obstructive pulmonary disease (COPD) and cardiovascular disease. People with a long-standing mental health problem are twice as likely to smoke, with the highest rates among people with psychosis or bipolar disorder.
People with a long-standing mental health problem are twice as likely to smoke, with the highest rates among people with psychosis or bipolar disorder.
By 2020/21, the NHS will ensure that at least 280,000 people living with severe mental health problems have their physical health needs met. As set out in the NHS Long Term Plan, by 2023/24, the NHS will further increase the number of people receiving physical health checks to an additional 110,000 people per year, bringing the total to 390,000 checks delivered each year.
Improving Physical Healthcare for People with SMI Guidance for ICSs details the action and collaboration required by commissioners and providers in primary and secondary care to improve access to and the quality of physical health checks and ensure appropriate follow-up care is given. Positive practice examples and tools can be found in the supporting annexes. Public Health England’s report provides more information on physical health inequalities for people with SMI.
NHS England publishes quarterly statistics on the number of people with SMI receiving a full physical health check.
A practical toolkit for mental health trusts and commissioners is also available to help providers and commissioners improve the physical health of patients with serious mental illness in secondary care. The toolkit looks at different approaches to implementing the Lester screening tool.
Download Improving the physical health of patients with serious mental illness – a practical toolkit.
Demonstrating progress and building sustainability
- The Mental Health Five Year Forward View Dashboard outlines how local areas are performing against key areas including the EIP standard.
- The new Mental Health Services Data Set enables the routine capture and reporting of information regarding referral to response, assessment and treatment times, interventions delivered and outcomes.
Suicide prevention
Suicide prevention is a complex system-wide challenge which requires close working between the NHS, public health and partner organisations, tailoring evidence of what works to local need and determinants.
NHS England and Improvement is building on the progress made in the Five Year Forward View, which had already committed to reducing the suicide rate by 10% by the end of 2020/21.
This commitment will be delivered in close partnership with public health and local authorities, Public Health England and Department of Health and Social Care.
By 2023/24, we plan that 100% of Sustainability and Transformation Partnerships STPs will have received investment for a localised suicide reduction programme. This will support locally-led initiatives and there will be significant local autonomy on how it is implemented, as long as it is in line with published guidance.
To support this commitment, NHS England and Improvement has commissioned a national Quality Improvement (QI) offer jointly delivered by The National Confidential Inquiry into Suicide and Safety in Mental Health (NCISH) and The National Collaborating Centre for Mental Health (NCCMH).
Suicide Bereavement Support
For each person who dies, as many as 135 people can be impacted; and in many cases this may be an underestimate.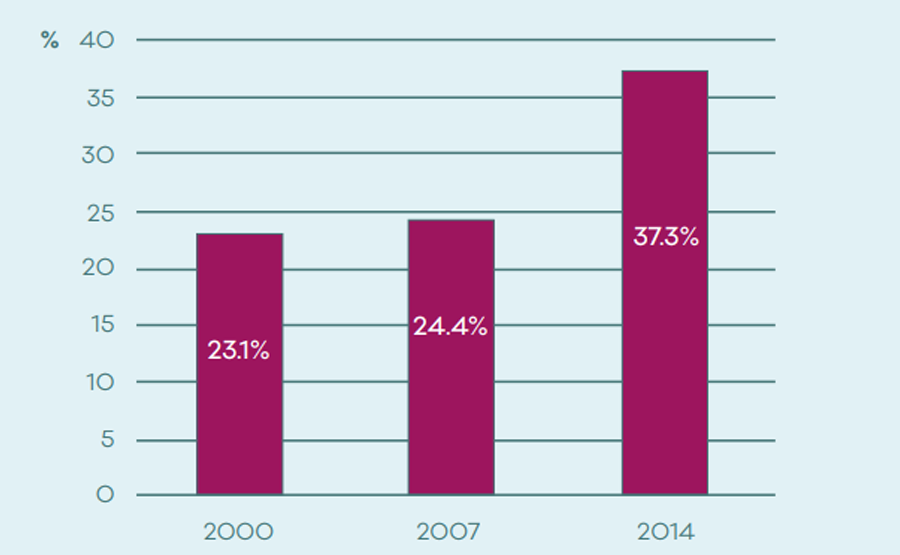 We also know that people who are bereaved by suicide are at risk themselves, which makes it ever so important to support family and friends in the days, weeks, and months, after a bereavement.
We also know that people who are bereaved by suicide are at risk themselves, which makes it ever so important to support family and friends in the days, weeks, and months, after a bereavement.
By 2023/24 we plan that, 100% of STPs will be providing suicide bereavement support services. We are funding local areas to develop their own services for their own population needs. NHS England and Improvement will support local areas with implementation and developing plans for the infrastructure needed to deliver bereavement support.
To enable delivery, we are working with partners Support After Suicide Partnership to deliver postvention bereavement implementation support in addition to a central hub of resources.
National funding profiles
National funding profiles can be found in the following document: NHS Mental Health Implementation Plan 2019/20 – 2023/24
Finding mental health care and therapy in the UK
Talk therapy in the UK is becoming increasingly available on the NHS and is expected to expand over the next few years.
Talk therapy is a broad term that encompasses a variety of therapies designed to help people deal with negative thoughts and feelings and bring about positive change, such as counseling, cognitive behavioral therapy (CBT), and psychotherapy. The Mental Health Foundation (MHF) provides information for anyone who wants to learn more about different types of talking therapy or hear from the experiences of people who have used them. nine0003
Contents
- Mental health care through your family doctor in the UK
- If you would like to try talking therapy, please contact your GP who will be aware of what is available locally.
- Contacting a private specialist
- Charities
- Facing discrimination
- Videos
Mental health care through your family doctor in the UK
It is estimated that about half of the general practitioners' offices in England provide advice and support.
Your therapist's personal views on talking therapy may also affect your access to it. Some therapists are more likely to refer you to therapy than others. According to an online survey conducted by MHF, only 42% of people who visited their therapist for depression received counseling, although 82% of them would be willing to try it. nine0003
If your therapist has personal views on talking therapy, they may refer you for a consultation.
If your therapist does not want to refer you to talking therapy, you may need to find out for yourself what is available in your area and work hard to get it. Or go to another therapist who is willing to refer you.
Access to talk therapy on the NHS will improve over the next few years. Government policy is to make counseling and other treatments, including cognitive behavioral therapy (CBT), more accessible on the NHS. nine0003
The Improved Access to Psychological Therapy (IAPT) Program, launched in 2006, is bringing thousands of new qualified therapists into general practice. This program will provide easy access to NHS talk therapy to anyone who needs it.
This program will provide easy access to NHS talk therapy to anyone who needs it.
If you would like to try talking therapy, please contact your therapist who will be aware of what is available locally.
NHS
Your GP can refer you to free NHS talk therapy. This is usually a short course of counseling or CBT in a general practice counseling service. nine0003
If you have mental health problems, you can see a general practitioner.
If counseling or CBT is not available at the clinic, your GP can refer you to a local counselor or psychotherapist for NHS treatment.
You can also refer yourself for a consultation. Through the IAPT program, a growing number of Primary Care Trusts (PCTs) are implementing self-referral services.
Self-referral to specialists. nine0003
Self-referral means that people who choose not to see their therapist can go directly to a professional psychotherapist. This service is already available in some areas of England.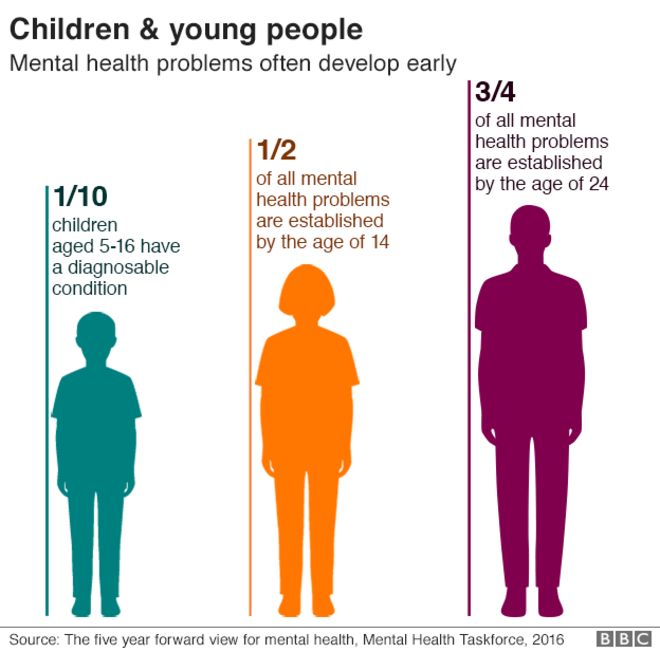 To find out what's available in your area, see our Directory of Psychotherapy Services.
To find out what's available in your area, see our Directory of Psychotherapy Services.
Self-referral means that people prefer to see an occupational therapist directly.
If you have a serious mental illness, such as severe depression, or have experienced trauma or abuse in the past, your PCP can help you decide if you should see another mental health professional, such as a clinical psychologist , a psychotherapist, a psychiatrist, or a member of a local mental health community group. nine0003
See a private specialist
If you can afford it, you can choose paid therapy. The cost of talking therapy varies and a one hour session can cost between £40 and £100.
First, ask your GP if he can recommend a local private GP for you. If you still need help, you can find a private therapist through the Internet, libraries, or the yellow pages
There are no rules governing who can advertise talking therapy, so make sure the therapist is on one of the approved practitioner registries . Talk to several therapists before deciding which one is right for you. nine0003
Talk to several therapists before deciding which one is right for you. nine0003
The following organizations have approved therapists:
- British Association for Behavioral and Cognitive Psychotherapy (BABCP): Cognitive Behavioral Therapists
- Association for Family Therapy (AFT): Family Therapists
- British Association for Counseling and Psychotherapy (BACP): Counselors and Psychotherapists
- British Psychoanalytic Council (BPC): psychoanalytic psychotherapists
- UK Council for Psychotherapy (UKCP): psychotherapists
- British Association for Sexual and Relationship Therapy (BASRT): couples counselors and sex therapists.
Charities
Some charities offer cheap or free talk therapy. These include:
- Cruse - bereavement help,
- Beat - help with eating disorders,
- Mind - mental health issues,
- Relate - relationship counseling. nine0012
Some employers provide counseling for their employees, and many colleges and universities offer free therapy to students who need it.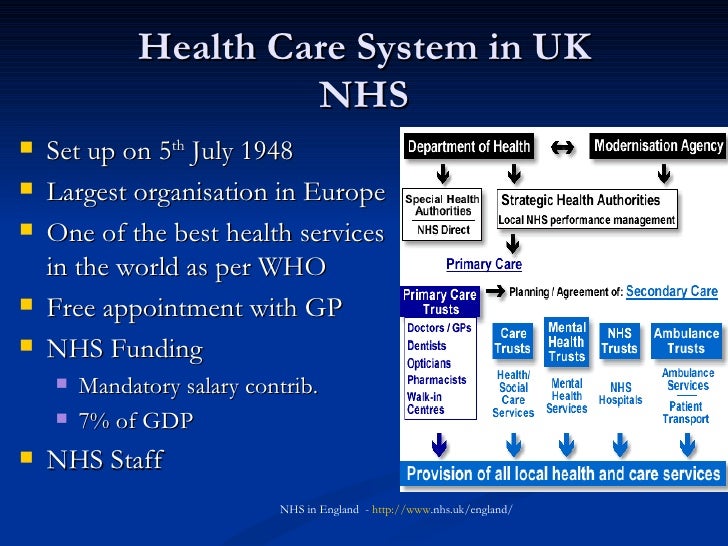
Facing discrimination
Getting NHS treatment can be more difficult for some populations, such as blacks and older people, although they are just as eligible and can benefit as everyone else.
Whatever your origin, like other people. nine0003
Whatever your background, you have the right to be offered talk therapy if that can help you. You can count on the NHS to do everything they can to improve your access to talking therapy. Ask your therapist to refer you to talking therapy if you think it might help.
Video
As a coffee seller driven out of the forest, the national bird of Great Britain and a treasure hunt.
Romantic trip through the canals of Great Britain Monmouthshire and Brecon canal
Marry abroad | Episode 14 | United Kingdom
Program for the admission of refugees from Ukraine to the UK.
UK Wildlife (Part 1) | Documentary film National Geographic
Oddities of Great Britain that await you
Tower of London the story of the most sinister castle in Britain
Questions and myths about going to a psychotherapist. Psychiatrist and clinical psychologist speak
Psychiatrist and clinical psychologist speak
How I became an actor in the UK
Free housing for refugees and SEARCHING FOR A SPONSOR FOR A UK VISA
TOP 5 psychiatric clinics in the UK ▷ prices, doctors and reviews
Your safety is above all! Check out the current border crossing conditions related to COVID-19 on this website and our recommendations on this page.
Check out 5 trusted mental health clinics in the UK
Clinic rating based on 7 visits, 2 patient reviews, prices and information from 5 clinics
#1
Wellington Hospital is the largest private hospital in the UK
Location: Wellington Hospital South Bldg, 8A Wellington Pl, London NW8 9LE
Read all
#2
Royal Brompton & Harvild is the UK's largest center specializing in the diagnosis and treatment of heart and lung diseases. nine0003
Location: Sydney Street, London SW3 6NP
Read all
#3
TrustScore
All reviews have been verified
London Bridge Hospital provides medical services in the following areas: cardiac surgery, kidney and liver transplantation, neurosurgery, skin tuberculosis treatment.
Location: 27 Tooley Street, London SE1 2PR
Read all nine0003
Diseases
ParanoiaWhat is Bookimed?
is a free international platform for finding clinics and arranging treatment for people from anywhere in the world.
Direct prices from clinics Financial policy'>How do we form prices?
Verified clinics Site Selection Policy'>How do we screen clinics?
Free service Financial policy'>Why free?
100% reviews from real patients Feedback policy'>How do we check reviews? nine0003
Trustpilot
Yes, there is No they are in the hospital Examinations not performed
#four
Harley Street Clinic is one of London's first private medical institutions. Harley Street Clinic is a general hospital, but among its priority areas are adult and pediatric oncology and cardiology.
Harley Street Clinic is a general hospital, but among its priority areas are adult and pediatric oncology and cardiology.
The intensive care complex at the clinic was created for the treatment of cardiological diseases, cancer, disorders of the nervous system, spinal injuries. nine0003
Harley Street was the first in the country to offer radiosurgical treatment using the CyberKnife. Thanks to this technology, the clinic performed the world's first operation on an inoperable heart, which gave life to a patient who was considered incurable.
Location: 35 Weymouth Street, London W1G 8BJ
Read all
#five
Princess Grace Hospital is a multidisciplinary private clinic in London. The main areas of the hospital's work: pulmonology, gastroenterology, hepatology, orthopedics, oncology, neurology, nutrition, endocrinology, plastic surgery, spinal surgery, sports medicine, emergency care, urology. nine0003
nine0003
The London Breast Institute operates on the basis of the Princess Grace Hospital, where the best breast oncologists in the UK practice. Location: 42-52 Nottingham Place, London W1U 5NY
Read all
| Procedure | UK | Turkey | Germany | Israel |
|---|---|---|---|---|
| Treatment of schizophrenia | ||||
| Diagnosis and 1 month of complex treatment of schizophrenia | - | - | - | from $9400 |
| Autism treatment | ||||
| Autism diagnosis + 1 month of complex therapy | - | - | - | from 12600$ |
| Treatment for depression |
Need help?
Doctors-coordinators will advise you and help you with the choice. Bookimed services are free of charge for you and do not affect the bill at the clinic.