Mental health for soldiers
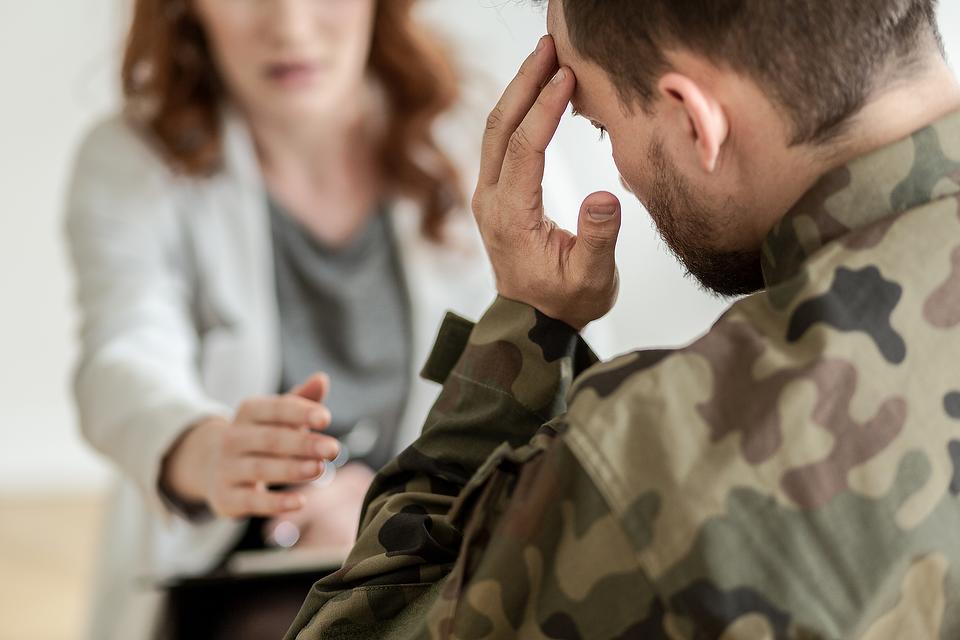
Veterans & Active Duty | NAMI: National Alliance on Mental Illness
Nearly 1 in 4 active duty members showed signs of a mental health condition, according to a 2014 study in JAMA Psychiatry. On this page we focus on questions that military personnel often ask, concerning treatment resources, disclosure and staying healthy during the transition to civilian life. If you are having thoughts of suicide, the Veterans Crisis Line is available 24/7 by dialing 1-800-273-8255 and pressing 1.
NAMI offers information, support and education specifically for veterans, service members and their families. To learn more, visit NAMI Homefront.
Mental Health Concerns
There are three primary mental health concerns that you may encounter serving in the military.
- Postraumtic Stress Disorder (PTSD). Traumatic events, such as military combat, assault, disasters or sexual assault can have long-lasting negative effects such as trouble sleeping, anger, nightmares, being jumpy and alcohol and drug abuse.
When these troubles don't go away, it could be PTSD. The 2014 JAMA Psychiatry study found the rate of PTSD to be 15 times higher than civilians.
- Depression. More than just experiencing sadness, depression doesn't mean you are weak, nor is it something that you can simply "just get over." Depression interferes with daily life and normal functioning and may require treatment. The 2014 JAMA Psychiatry study found the rate of depression to be five times higher than civilians.
- Traumatic Brain Injury (TBI). A traumatic brain injury is usually the result of significant blow to the head or body. Symptoms can include headaches, fatigue or drowsiness, memory problems and mood changes and mood swings.
In the Mental Health Conditions section of our site we discuss these conditions and others and how to recognize the symptoms of mental illness in yourself or someone else.
Who Should I Tell?
Service men and women owe it to their fellow service members to stay in good mental as well as physical health. If you’re concerned about a possible mental health condition—or if you enter the armed forces with a past or present mental health condition—know that the armed forces do not require service members to disclose mental health problems to their chain of command. The responsibility for deciding whether to disclose your condition does fall on the medical officers and care providers you consult. They receive training on military policies concerning the confidentiality of protected health information (PHI). Here are some people to consider speaking with.
If you’re concerned about a possible mental health condition—or if you enter the armed forces with a past or present mental health condition—know that the armed forces do not require service members to disclose mental health problems to their chain of command. The responsibility for deciding whether to disclose your condition does fall on the medical officers and care providers you consult. They receive training on military policies concerning the confidentiality of protected health information (PHI). Here are some people to consider speaking with.
- Confidential counselors are available for service members and their families through Military One Source at 1-800-342-9647. If you’re unsure whether to seek treatment or if you someone you know might need treatment, they are an excellent first stop for information and advice.
- Primary care providers can be helpful for discussing concerns and treatment options.
- Behavioral health care providers
working at primary care clinics are available on many military bases so you can seek a specialist’s advice without leaving base.
 And at some bases, you can find convenient Embedded Behavioral Health teams—clinics separate from traditional medical facilities.
And at some bases, you can find convenient Embedded Behavioral Health teams—clinics separate from traditional medical facilities.
If you or someone you know is struggling or in crisis, help is available. Call or text 988 or chat 988lifeline.org to reach the 988 Suicide & Crisis Lifeline.
How Will Asking for Mental Health Treatment Affect My Career?
Military personnel have always taken care of their physical health, but in today’s armed forces, mental health is equally essential to mission success. The military has changed many of its policies in recent years to encourage better mental health. The Department of Defense acknowledges that untreated mental health conditions pose a greater safety threat than mental health conditions for which you’re seeking treatment.
Under 2014 rules, talking to a doctor about your concerns, asking if you need a diagnosis, or seeking treatment does not affect your career. If your doctor needs to disclose your condition, your career is not at risk from this disclosure.
In addition, with changes to security clearance procedures, you no longer risk losing clearance by consulting a doctor. If you seek help for combat-related issues or receive marital counseling, you do not have to worry about “question 21” regarding treatment for mental or emotional conditions.
The Dangers of Not Disclosing
Untreated mental illness can, however, damage your career. If the symptoms are severe, your commanding officer may require duty limitations or recommend separation from the military for medical reasons.
Military records show that talking to a doctor is a good career move. According to a 2006 study in Military Medicine, 97% of personnel who sought mental health treatment did not experience any negative career impact. The same study showed that it’s risky to ignore a mental health condition. If it worsens, a commanding officer can require a mental health evaluation, which is much more damaging to your career. Among people who had command-directed evaluations, 39% had negative career impact.
Military Policy and Your Privacy
When you seek mental health care, your care provider will inform you that the Department of Defense follows the privacy guidelines set down by HIPAA and the Privacy Act. These guidelines ensure the privacy of your mental health records in most situations. If your care provider discovers that your mental health condition may endanger yourself, others or the mission, however, they are obligated to disclose this information to the chain of command.
Military policy states that care providers can only share certain information and only in those situations involving safety. The precise definition of those circumstances is different for each of the branches of the armed forces.
In the Army, for example, PHI policy states that information can only be released in situations involving an acute threat of harm to self, others or mission; upon admission or discharge from inpatient hospitalization; when entering formal substance abuse treatment; and when enrolling in personnel reliability programs.
If a medical officer or military care provider observes that your health condition poses a danger, the officer will share your medical profile with commanding officers. The information they are allowed to share includes your diagnosis and the medically recommended duty limitations. Unit commanders will decide what duties to assign you until your condition improves.
You can avoid situations requiring disclosure by discussing your concerns with providers when they first arise. Ignoring symptoms may allow them to worsen. A mental health condition may affect only you at first, but if your condition doesn’t improve, your ability to perform your duties may suffer.
If commanders or supervisors observe behaviors that appear to compromise safety or job performance, they can request a command-directed behavioral health evaluation. A command-directed evaluation doesn’t guarantee as much confidentiality as a medical consultation you seek yourself.
How Can I Help a Fellow Warrior?
Strengthening our fighting forces is a group effort. If you’re concerned about a friend or colleague, the most important thing you can do is to ask how they’re doing and to listen without judgment. The symptoms of a mental health condition can sometimes make individuals forget that mission success relies on staying healthy in mind as well as body. They might not realize that their worries are symptoms of mental illness. Listen patiently, offer encouragement and remind them that anyone can develop these symptoms, from privates to generals.
If you’re concerned about a friend or colleague, the most important thing you can do is to ask how they’re doing and to listen without judgment. The symptoms of a mental health condition can sometimes make individuals forget that mission success relies on staying healthy in mind as well as body. They might not realize that their worries are symptoms of mental illness. Listen patiently, offer encouragement and remind them that anyone can develop these symptoms, from privates to generals.
Remind your fellow warrior that the central mission of the armed forces is to maintain a strong fighting force. Share the information here with him or her. Emphasize that talking to a counselor or medical officer won’t hurt career or security clearance, and that every service member has a duty to build resilience by seeking advice and treatment when it’s indicated.
If someone you know tells you about a mental health concern, don’t laugh it off or promise it will get better on its own, even if you want to comfort the person. The stresses of deployment and military life put soldiers at risk for mental illness and make treating them more complicated. The military medical system can’t succeed in its mission to “restore the fighting force” without the help of all personnel to encourage treating mental health conditions swiftly before they can worsen.
The stresses of deployment and military life put soldiers at risk for mental illness and make treating them more complicated. The military medical system can’t succeed in its mission to “restore the fighting force” without the help of all personnel to encourage treating mental health conditions swiftly before they can worsen.
For more advice, recommend that your friend call the completely confidential counselors at Military One Source (1-800-342-9647).
Making a Strong Transition to Civilian Life
Returning to civilian life can be a time of joy, but also a time of emotional upheaval. Your experiences in the service may have changed the way you look at life. You may have new abilities, new friendships or new concerns.
If you were in combat or similarly stressful situations, it’s possible some of the habits that helped you stay strong during traumatic events will be less useful in civilian life. Keeping strong in civilian life might require developing new habits. You may also be at increased risk of PTSD and other symptoms that your brain is recovering from trauma.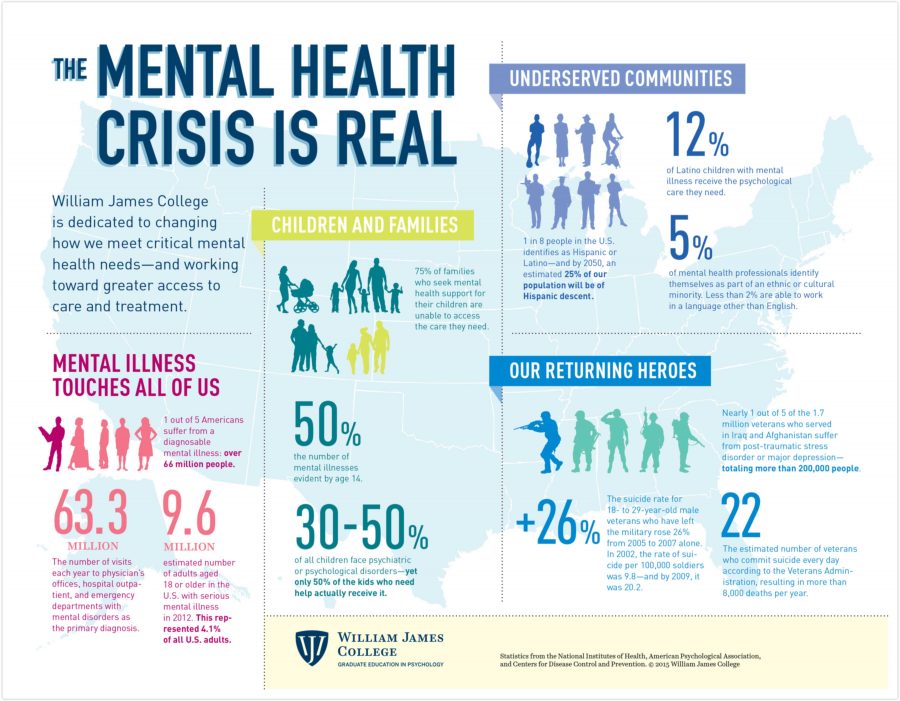
Some veterans find they miss the structure that the military life provides. Some miss feeling a sense of purpose in their daily work. Others may feel isolated because civilians don’t understand the experience of serving. The memories of your experiences also may take time to deal with.
Remember that readjusting takes time. Give yourself opportunities to maintain your physical and mental health during the transition. At NAMI, we understand the questions facing many service members when they return to civilian life. We're here to help. Check out your local NAMI Affiliate to see if it offers a support program for returning vets.
Maintaining a Strong Body and Mind
Here are some important tips and suggestions for maintaining a strong body and mind:
- Reach out to other veterans or veterans’ groups. It's much easier to make the transition when you're not alone. Social support from non-veterans helps as well. Locate a spiritual or religious advisor you enjoy talking to, or a mental health professional.

- Talk to family and friends about your experiences. Even if they don't fully understand what you're going through, it helps them to understand why you may have trouble interacting at times.
- Recognize that others might not understand your military service or your views. If you talk about your experiences and get a negative response, let it go.
- Prepare ahead of time for insensitive questions or topics of conversation. You don’t need to tell anyone about your experiences unless you want to. Practice how to respond or respectfully decline to answer.
- Search the web for information on mental health and transitioning. Identify strategies ahead of time to support your transition. Real Warriors is a great site for all soldiers, whether they be active duty, National Guard or Reserve, or veterans and their families. The information and tools there can help with everything from budgeting and work to insomnia, PTSD and depression.
- Take care of your body and your mind by proactively finding veteran-friendly health services in your area.
 You can obtain information on local services through My HealtheVet, the VA’s online personal health record. This site for veterans, active duty service members, and their families provides access to health records, a personal health journal, online VA prescription refill information and details regarding federal and VA benefits and resources.
You can obtain information on local services through My HealtheVet, the VA’s online personal health record. This site for veterans, active duty service members, and their families provides access to health records, a personal health journal, online VA prescription refill information and details regarding federal and VA benefits and resources. - Take your time reconnecting with family and friends. When you were serving, your role in the family was “distant service member.” Now you and your family are developing a new role for you. Since time has passed, your new role might not be identical to your role before serving. You and your family will adjust and be stronger than before, but don’t expect the adjustments to happen immediately.
- Try to be patient with your civilian coworkers and the civilian work schedule. At times you may feel frustrated that employees in civilian life leave when the work day officially ends, regardless of whether the “mission” for the day is complete.
 They may appear less committed than you're used to, and less interested in team work. You may also find that you and your civilian coworkers have different modes of speech at the office. Military jargon is a complex language and you might feel like you’re having to translate yourself into “civilian English.”
They may appear less committed than you're used to, and less interested in team work. You may also find that you and your civilian coworkers have different modes of speech at the office. Military jargon is a complex language and you might feel like you’re having to translate yourself into “civilian English.” - Recognize that you will feel frustrated sometimes while returning to civilian life, but frustration is normal during this transition. In fact, frustration is a sign that you’re adjusting and growing stronger.
- If you find yourself growing more frustrated or isolated over time, talk to a health professional about whether mental health care can help you increase your resilience. The Department of Defense sponsors coaching and support at In Transition (1-800-424-7877). Medical professionals can help you come out of this transition stronger than before.
The important thing to remember is that you’re not alone. There are many people who want to support you. You can start preparing now, by looking at the VA’s list of common challenges and solutions, or the MilitaryOneSource database of websites offering assistance with the transition to civilian life.
You can start preparing now, by looking at the VA’s list of common challenges and solutions, or the MilitaryOneSource database of websites offering assistance with the transition to civilian life.
Veteran and Military Mental Health Issues
Book
Catarina Inoue 1 , Evan Shawler 2 , Christopher H. Jordan 3 , Christopher A. Jackson 4
In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan.
.
Affiliations
Affiliations
- 1 1st Special Operations Medical Group
- 2 Uniformed Services University of the Health Sciences
- 3 Hurlburt Field Air Force Base
- 4 University of Texas Health Science Center at San Antonio
- PMID: 34283458
- Bookshelf ID: NBK572092
Free Books & Documents
Book
Catarina Inoue et al.
Free Books & Documents
In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan.
.
Authors
Catarina Inoue 1 , Evan Shawler 2 , Christopher H. Jordan 3 , Christopher A. Jackson 4
Affiliations
- 1 1st Special Operations Medical Group
- 2 Uniformed Services University of the Health Sciences
- 3 Hurlburt Field Air Force Base
- 4 University of Texas Health Science Center at San Antonio
- PMID: 34283458
- Bookshelf ID: NBK572092
Excerpt
As the United States faces two decades of continuous war, media and individuals with personal military connections have elevated public and professional concerns for the mental health of veterans and service members. The most publicized mental health challenges facing veterans service members are PTSD and depression. Some research has suggested that approximately 14% to 16% of U.S. service members deployed to Afghanistan and Iraq have PTSD or depression. Although these mental health concerns are highlighted, other issues like suicide, traumatic brain injury (TBI), substance abuse, and interpersonal violence can be equally harmful in this population. The effects of these issues can be wide-reaching and substantially impacts service members and their families. While combat and deployments are linked to increased risks for these mental health conditions, general military service can also lead to difficulties. There is no specified timeline for the presentation of these mental health concerns. Still, there are particularly stressful times for individuals and families, such as in close proximity to combat or when separating from active military service.
The most publicized mental health challenges facing veterans service members are PTSD and depression. Some research has suggested that approximately 14% to 16% of U.S. service members deployed to Afghanistan and Iraq have PTSD or depression. Although these mental health concerns are highlighted, other issues like suicide, traumatic brain injury (TBI), substance abuse, and interpersonal violence can be equally harmful in this population. The effects of these issues can be wide-reaching and substantially impacts service members and their families. While combat and deployments are linked to increased risks for these mental health conditions, general military service can also lead to difficulties. There is no specified timeline for the presentation of these mental health concerns. Still, there are particularly stressful times for individuals and families, such as in close proximity to combat or when separating from active military service.
Current U.S. Census reports estimate roughly 18 million veterans and 2. 1 million active-duty and reserve service members (https://www.census.gov/newsroom/press-releases/2020/veterans-report.html). Since September 11, 2001, there have been 2.8 million active-duty American military personnel deployed to Iraq, Afghanistan, and beyond, leading to increasing numbers of combat veterans amongst the population. More than 6% of the U.S. population have served or are serving in the military. However, this statistic fails to capture the even greater number of family members affected by military service. Understanding military service and its relation to a patient’s physical and mental health can help providers improve their quality of care and potentially help save a patient’s life.
1 million active-duty and reserve service members (https://www.census.gov/newsroom/press-releases/2020/veterans-report.html). Since September 11, 2001, there have been 2.8 million active-duty American military personnel deployed to Iraq, Afghanistan, and beyond, leading to increasing numbers of combat veterans amongst the population. More than 6% of the U.S. population have served or are serving in the military. However, this statistic fails to capture the even greater number of family members affected by military service. Understanding military service and its relation to a patient’s physical and mental health can help providers improve their quality of care and potentially help save a patient’s life.
Post-Traumatic Stress Disorder (PTSD)
Post-traumatic stress disorder (PTSD) was first codified in the Diagnostic and Statistical Manual of Mental Disorders (DSM) 3 in 1980, driven in part by sociopolitical aftereffects of the Vietnam War. It has been alluded to in different forms throughout history, from “soldier’s heart” at the time of the Civil War, “shell shock” in the First World War, or “combat fatigue” around the Vietnam War. DSM criteria remained largely unchanged until the most recent update in 2013, although its classification continues to be debated. It is a complex and evolving biological, psychological, and social entity, making it challenging to study and diagnose. PTSD is often researched in war and disaster survivors but can affect anybody, including children. It is usually seen in survivors of violent events such as assault, disasters, terror attacks, and war, although it is also possible to experience PTSD from secondhand exposure, such as learning that a close friend or family member experienced a violent threat or accident. Many individuals exposed to trauma have transient numbness or heightened emotions, nightmares, anxiety, and hypervigilance but usually overcome symptoms within one month. In roughly 10 to 20% of cases, symptoms become persistent and debilitating.
It has been alluded to in different forms throughout history, from “soldier’s heart” at the time of the Civil War, “shell shock” in the First World War, or “combat fatigue” around the Vietnam War. DSM criteria remained largely unchanged until the most recent update in 2013, although its classification continues to be debated. It is a complex and evolving biological, psychological, and social entity, making it challenging to study and diagnose. PTSD is often researched in war and disaster survivors but can affect anybody, including children. It is usually seen in survivors of violent events such as assault, disasters, terror attacks, and war, although it is also possible to experience PTSD from secondhand exposure, such as learning that a close friend or family member experienced a violent threat or accident. Many individuals exposed to trauma have transient numbness or heightened emotions, nightmares, anxiety, and hypervigilance but usually overcome symptoms within one month. In roughly 10 to 20% of cases, symptoms become persistent and debilitating. PTSD features intrusive thoughts, flashbacks, and nightmares regarding the past trauma, causing avoidance of reminders, hypervigilance, and sleep difficulties. Often, reliving the event can feel as threatening as inciting trauma. Symptoms can interfere with interpersonal and occupational function and manifest in psychological, emotional, physical, behavioral, and cognitive manners. Military personnel can be exposed to an array of potentially traumatizing experiences. Wartime deployments can result in witnessing severe injuries or violent death, sometimes occurring suddenly and not always on expected targets. Apart from the austere environment of deployment, active duty military members are at risk of experiencing non-military-related traumas such as interpersonal violence, physical or sexual abuse. Symptoms related to these traumas can sometimes be exacerbated in the deployed environment.
PTSD features intrusive thoughts, flashbacks, and nightmares regarding the past trauma, causing avoidance of reminders, hypervigilance, and sleep difficulties. Often, reliving the event can feel as threatening as inciting trauma. Symptoms can interfere with interpersonal and occupational function and manifest in psychological, emotional, physical, behavioral, and cognitive manners. Military personnel can be exposed to an array of potentially traumatizing experiences. Wartime deployments can result in witnessing severe injuries or violent death, sometimes occurring suddenly and not always on expected targets. Apart from the austere environment of deployment, active duty military members are at risk of experiencing non-military-related traumas such as interpersonal violence, physical or sexual abuse. Symptoms related to these traumas can sometimes be exacerbated in the deployed environment.
Depression
After two decades of continuous war in Afghanistan, a growing population of veterans with combat and deployment experience is presenting for mental health care. Providers must take into account not only the physical wounds these veterans may have sustained but also the less visible ones such as PTSD, acute stress disorder, and depression. Although the condition does not garner the same attention as PTSD, depression remains one of the leading mental health conditions in the military. In fact, studies show that up to 9% of all appointments in the ambulatory military health network are related to depression. The military environment can act as a catalyst for the development and progression of depression. For example, separation from loved ones and support systems, stressors of combat, and seeing oneself and others in harm’s way are all elements that increase the risk of depression in active duty and veteran populations. Military medical facilities saw an increase from a baseline of 11.4% of members diagnosed with depression to a rate of 15% after deployments to Iraq or Afghanistan. With such a high prevalence, providers must be responsible for identifying active duty and veteran patients who may be suffering from depression.
Providers must take into account not only the physical wounds these veterans may have sustained but also the less visible ones such as PTSD, acute stress disorder, and depression. Although the condition does not garner the same attention as PTSD, depression remains one of the leading mental health conditions in the military. In fact, studies show that up to 9% of all appointments in the ambulatory military health network are related to depression. The military environment can act as a catalyst for the development and progression of depression. For example, separation from loved ones and support systems, stressors of combat, and seeing oneself and others in harm’s way are all elements that increase the risk of depression in active duty and veteran populations. Military medical facilities saw an increase from a baseline of 11.4% of members diagnosed with depression to a rate of 15% after deployments to Iraq or Afghanistan. With such a high prevalence, providers must be responsible for identifying active duty and veteran patients who may be suffering from depression.
Major depression manifests through many symptoms, including depressed mood, loss of interest in activities, insomnia, weight loss or gain, psychomotor retardation, fatigue, decreased ability to concentrate, thoughts of worthlessness, and thoughts of suicide. These symptoms coalesce to significantly impact patients’ abilities to function fully. While the complement of symptoms is readily apparent on paper, a patient’s actual presentation can often be ambiguous. One out of every two depressed patients is not appropriately diagnosed by their general practitioner. Therefore, it is paramount to correctly screen for, identity, and follow through with appropriate treatments, especially in the active duty and veteran military population.
Suicide
Veteran suicide rates are at the highest level in recorded history, with annual deaths by suicide at over 6,000 veterans per year. Overall suicide rates within the United States have increased by 30% between 1999 and 2016. A study involving 27 states estimated 17.8% of these recorded suicides were by veterans. The U.S. Department of Veterans Affairs (VA) published data in 2016 that indicated veteran suicide rates were 1.5 times greater than non-veterans. Research has shown that veterans are at significantly increased risk of suicide during their first year outside of the military. In 2018, a Presidential Executive Order was signed to improve suicide prevention services for veterans during their transition to civilian life. Additionally, the Department of Defense (DoD) and VA have made suicide prevention a major priority because of observed increases in fatal and non-fatal suicide attempts throughout the wars in Iraq and Afghanistan. Within the U.S. Armed Forces, suicide rates doubled between 2000 and 2012, but since 2012 there have been no appreciable changes in the annual rate, with approximately 19.74 deaths per 100,000 service members.
A study involving 27 states estimated 17.8% of these recorded suicides were by veterans. The U.S. Department of Veterans Affairs (VA) published data in 2016 that indicated veteran suicide rates were 1.5 times greater than non-veterans. Research has shown that veterans are at significantly increased risk of suicide during their first year outside of the military. In 2018, a Presidential Executive Order was signed to improve suicide prevention services for veterans during their transition to civilian life. Additionally, the Department of Defense (DoD) and VA have made suicide prevention a major priority because of observed increases in fatal and non-fatal suicide attempts throughout the wars in Iraq and Afghanistan. Within the U.S. Armed Forces, suicide rates doubled between 2000 and 2012, but since 2012 there have been no appreciable changes in the annual rate, with approximately 19.74 deaths per 100,000 service members.
Substance Use Disorders
Despite public attention over recent decades, SUDs, including alcohol use, remains a problem among veterans and military members. In these populations, alcohol use is common and is often used for stress relief and socializing. SUDs are associated with significant adverse medical, psychiatric, interpersonal, and occupational outcomes. One study on military personnel found that approximately 30% of completed suicides and around 20% of deaths due to high-risk behavior were attributable to alcohol or drug use. In the general U.S. population, alcohol is the fourth leading cause of preventable death, and 31% of driving-related fatalities involve alcohol intoxication. The DSM-5 defines SUD as a cluster of behaviors surrounding compulsive drug-seeking. This includes impaired control of, dysfunctional social functioning due to, and physiologic changes caused by drug use. Addiction is the most severe stage, characterized by loss of self-control leading to compulsive drug-seeking despite a desire to quit. Substances include legal drugs such as caffeine, nicotine, and alcohol; prescription medications such as opioids, sedative/hypnotics, and stimulants; and illicit drugs such as marijuana, cocaine, methamphetamines, heroin, hallucinogens, and inhalants.
In these populations, alcohol use is common and is often used for stress relief and socializing. SUDs are associated with significant adverse medical, psychiatric, interpersonal, and occupational outcomes. One study on military personnel found that approximately 30% of completed suicides and around 20% of deaths due to high-risk behavior were attributable to alcohol or drug use. In the general U.S. population, alcohol is the fourth leading cause of preventable death, and 31% of driving-related fatalities involve alcohol intoxication. The DSM-5 defines SUD as a cluster of behaviors surrounding compulsive drug-seeking. This includes impaired control of, dysfunctional social functioning due to, and physiologic changes caused by drug use. Addiction is the most severe stage, characterized by loss of self-control leading to compulsive drug-seeking despite a desire to quit. Substances include legal drugs such as caffeine, nicotine, and alcohol; prescription medications such as opioids, sedative/hypnotics, and stimulants; and illicit drugs such as marijuana, cocaine, methamphetamines, heroin, hallucinogens, and inhalants.
Copyright © 2022, StatPearls Publishing LLC.
Sections
- Continuing Education Activity
- Introduction
- Etiology
- Epidemiology
- History and Physical
- Evaluation
- Treatment / Management
- Differential Diagnosis
- Prognosis
- Complications
- Consultations
- Deterrence and Patient Education
- Enhancing Healthcare Team Outcomes
- Review Questions
- References
Similar articles
-
Suicidal Ideation.

Harmer B, Lee S, Duong TVH, Saadabadi A. Harmer B, et al. 2022 May 18. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. 2022 May 18. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. PMID: 33351435 Free Books & Documents.
-
Prescription of Controlled Substances: Benefits and Risks.
Preuss CV, Kalava A, King KC. Preuss CV, et al. 2022 Sep 21. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. 2022 Sep 21. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. PMID: 30726003 Free Books & Documents.
-
NP Safe Prescribing Of Controlled Substances While Avoiding Drug Diversion.

Dydyk AM, Sizemore DC, Haddad LM, Lindsay L, Porter BR. Dydyk AM, et al. 2022 Oct 9. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. 2022 Oct 9. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. PMID: 33232099 Free Books & Documents.
-
Florida Controlled Substance Prescribing.
Dydyk AM, Sizemore DC, Fariba KA, Sanghavi D, Porter BR. Dydyk AM, et al. 2022 Oct 9. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. 2022 Oct 9. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. PMID: 33428370 Free Books & Documents.
-
Combat duty in Iraq and Afghanistan, mental health problems and barriers to care.

Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Hoge CW, et al. US Army Med Dep J. 2008 Jul-Sep:7-17. US Army Med Dep J. 2008. PMID: 20088060
See all similar articles
References
-
- Deahl MP, Klein S, Alexander DA. The costs of conflict: meeting the mental health needs of serving personnel and service veterans. Int Rev Psychiatry. 2011 Apr;23(2):201-9. - PubMed
-
- Gates MA, Holowka DW, Vasterling JJ, Keane TM, Marx BP, Rosen RC. Posttraumatic stress disorder in veterans and military personnel: epidemiology, screening, and case recognition.
 Psychol Serv. 2012 Nov;9(4):361-82. - PubMed
Psychol Serv. 2012 Nov;9(4):361-82. - PubMed
- Gates MA, Holowka DW, Vasterling JJ, Keane TM, Marx BP, Rosen RC. Posttraumatic stress disorder in veterans and military personnel: epidemiology, screening, and case recognition.
-
- Liu Y, Collins C, Wang K, Xie X, Bie R. The prevalence and trend of depression among veterans in the United States. J Affect Disord. 2019 Feb 15;245:724-727. - PubMed
-
- Sullivan RM, Cozza SJ, Dougherty JG. Children of Military Families. Child Adolesc Psychiatr Clin N Am. 2019 Jul;28(3):337-348. - PubMed
-
- Ravindran C, Morley SW, Stephens BM, Stanley IH, Reger MA.
 Association of Suicide Risk With Transition to Civilian Life Among US Military Service Members. JAMA Netw Open. 2020 Sep 01;3(9):e2016261. - PMC - PubMed
Association of Suicide Risk With Transition to Civilian Life Among US Military Service Members. JAMA Netw Open. 2020 Sep 01;3(9):e2016261. - PMC - PubMed
- Ravindran C, Morley SW, Stephens BM, Stanley IH, Reger MA.
Publication types
The Ministry of Defense will improve the mental health of soldiers and officers
A new order of the Ministry of Defense determines which of the soldiers and officers must undergo medical and psychological rehabilitation, as well as a list of indications for which they can be sent to sanatoriums and dispensaries free of charge. Experts believe that, first of all, these measures will help maintain the mental health of military personnel who are now solving combat missions, including those outside Russia.
In total, the list of military personnel subject to medical and psychological rehabilitation, according to the new order, includes 14 categories. They also include divers who dived to a depth of 60 to 500 meters, submarine crews who performed combat missions for more than 30 days, and astronauts. After 90 days of hard work, military personnel of the aerospace forces and strategic missile forces will be sent for rehabilitation. A separate category includes military personnel of the Main Directorate of the General Staff of the Armed Forces of the Russian Federation, who performed operational and combat missions for more than 30 days.
In a medical institution or rehabilitation center, a serviceman is first of all "passed" through a large-scale psychological and psychiatric diagnostics. With the help of tests and conversations, the specialist must determine whether there are violations in the behavior of the military, whether a person who has been in a hot spot can calmly adapt to civilian life. Often people who have been in a combat zone for a long time suffer from depression and loneliness.
Often people who have been in a combat zone for a long time suffer from depression and loneliness.
In some cases, there may be aggression towards others. Based on this, psychologists and psychiatrists work with military personnel using special methods.
It is believed that military psychologists should be involved in the rehabilitation of servicemen. Unlike civilian specialists, they can more accurately identify risk factors and predict human behavior in combat conditions. Most often, the Russian military undergo rehabilitation in specialized hospitals and sanatoriums of the Ministry of Defense.
The main indications for the medical and psychological rehabilitation of the military are fatigue, overwork and asthenia. Depending on the severity of the person's condition, they can be sent to a sanatorium for 10, 20 or 30 days. But the place of rest, in accordance with the order of the Ministry of Defense, will be determined by commanders on a territorial basis. For example, the military personnel of the Northern Fleet will undergo a rehabilitation course in sanatoriums in the Murmansk region or nearby regions. The officers of the General Staff were not very lucky either, because they will not be sent to resorts either. For their rehabilitation, a special institution has been identified - a military unit in the village of Krasnoye, Podolsky district, Moscow region.
The officers of the General Staff were not very lucky either, because they will not be sent to resorts either. For their rehabilitation, a special institution has been identified - a military unit in the village of Krasnoye, Podolsky district, Moscow region.
Photo: © RIA Novosti/Maxim Blinov
In accordance with the order, rehabilitation for medical and psychological reasons, in particular, military personnel who have been performing tasks to restore constitutional order for more than 30 days, participants in hostilities, as well as performing tasks in a state of emergency or natural disasters.
Employees of the coordinating center for the reconciliation of the warring parties in Syria may well fall into this category. He began work in February 2016 at the Khmeimim airbase. The main tasks of the center include providing humanitarian assistance to the local population and promptly informing about the progress of the reconciliation campaign. The center consists of five divisions, in which more than 50 officers serve.
Specialists from the international mine action center are now also working in Syrian cities - this is a special unit of the Russian engineering troops. The sappers took part in the demining of the territories of eastern Aleppo and historical sites in Palmyra. In addition, according to open sources, two platoons of marines are now guarding the permanent presence of Russian naval vessels at the base in Tarusa. The security of other Russian facilities in Syria has been guarded by the military police since the beginning of 2016. It maintains law and order in cities and controls traffic.
Military sailors will soon go to rest and rehabilitation. In January 2017, Supreme Commander Vladimir Putin ordered a reduction in the grouping of naval forces in the Mediterranean. In accordance with the new order of the Ministry of Defense, medical and psychological rehabilitation is necessary for servicemen of surface ships and headquarters, as well as for technical personnel who participated in campaigns for more than 60 days.
Ships of the Northern Fleet group spent exactly two months in the Mediterranean Sea. On February 8, the heavy nuclear-powered missile cruiser Pyotr Veliky, the heavy aircraft-carrying cruiser Admiral Kuznetsov, as well as two tankers and a tugboat returned to their base in Severomorsk.
A little earlier, an aviation group from these ships returned to their base airfields. Particular emphasis in the document is placed on the military involved in an accident on an airplane, or those who experienced a complete or partial system failure during a parachute jump.
In total, over the previous two months, naval aviation pilots in Syria completed 420 sorties. At this time, the first combat use of Russian carrier-based aircraft in the history of the Russian fleet was recorded. A group of several dozen aircraft attacked the headquarters and command posts of militants, clusters of equipment, firing positions and strongholds of terrorists.
Photo: © RIA Novosti/Vitaly Ankov
At the end of February, the newest frigate "Admiral Grigorovich" set off from Sevastopol to replace the departed ships. It was this ship that carried out launches against targets in Syria last November. The frigate is armed with Caliber-NK cruise missiles, the Shtil self-defense missile system, a 100-mm gun mount, anti-aircraft artillery, a rocket launcher, torpedoes, and can also carry a carrier-based helicopter.
It was this ship that carried out launches against targets in Syria last November. The frigate is armed with Caliber-NK cruise missiles, the Shtil self-defense missile system, a 100-mm gun mount, anti-aircraft artillery, a rocket launcher, torpedoes, and can also carry a carrier-based helicopter.
Special attention to the rehabilitation of servicemen, according to military psychologist Alexei Zakharov, began to be paid in Russia after the participation of our army in the conflicts in Afghanistan and Chechnya. After returning from hot spots, people very often manifested mental disorders and deviations in behavior.
- Stress factors led to the emergence of post-traumatic stress disorders, which "turned off" people from normal life. These things have all been observed. And our doctors, psychologists have worked very hard on this situation,” Zakharov told Life.
The last time the rules for the rehabilitation of military personnel were updated in 2012, the order was signed by the then Minister of Defense Anatoly Serdyukov. Modern adjustments are connected precisely with the combat experience gained by the Russian military in Syria, the expert believes.
Modern adjustments are connected precisely with the combat experience gained by the Russian military in Syria, the expert believes.
- There are fundamental differences (of the modern order from the document of 2012. - Approx. Life ), which relate to the most important factor - combat experience. This experience also applies to the traditional system of data in military psychology and military psychiatry. The imprint was left by work on a completely different, very difficult enemy (terrorists of the ISIS organization banned in Russia. - Note of Life ). This is work in the system of new informational influences on people,” the expert told Life.
Photo: © RIA Novosti
Among the risk factors experienced by the Russian military in Syria, the expert also named a foreign climate, a different language, unfamiliar traditions and a very different value system of local residents.
- The combination of these risk factors seriously affects the military personnel, officers. Naturally, we need to work with them,” Zakharov believes. - Participation in hostilities is associated with serious psychological stress. And sometimes this tension leads to psychological trauma. People working in such a situation should be able to restore their combat capability. People are not machines. They must act consciously.
Naturally, we need to work with them,” Zakharov believes. - Participation in hostilities is associated with serious psychological stress. And sometimes this tension leads to psychological trauma. People working in such a situation should be able to restore their combat capability. People are not machines. They must act consciously.
Military doctors are sounding the alarm: more than half of the conscripts are sick
Some guys who did not complain about their health before the army acquire mental disorders already directly in the units, and there are many reasons for this. But the most unpredictable and sad consequences occur, as a rule, in those cases when the doctors of the VVK do not reveal the deviations and diseases that the conscripts have. As, for example, happened to Alexander Popov (name and surname changed).
The young man was called up for service in May 2002. A year and a half later, Alexander came home on vacation, where he behaved normally, and, according to his mother, she did not notice any changes in his son's behavior. All the worst began when Popov's vacation ended and he returned to the unit. The guy began to withdraw into himself, he did not talk to his colleagues for days. Shortly before his dismissal, he wrote home in letters that something incomprehensible was happening to him: he did not understand those around him and the events that were taking place, he was constantly haunted by a bad mood. “Uncertainty dominates me in all my actions. I myself don’t know where and why I need to go, what and when to do if they don’t tell me something. I don’t know how I will get out of this state ...”
All the worst began when Popov's vacation ended and he returned to the unit. The guy began to withdraw into himself, he did not talk to his colleagues for days. Shortly before his dismissal, he wrote home in letters that something incomprehensible was happening to him: he did not understand those around him and the events that were taking place, he was constantly haunted by a bad mood. “Uncertainty dominates me in all my actions. I myself don’t know where and why I need to go, what and when to do if they don’t tell me something. I don’t know how I will get out of this state ...”
Alevtina Viktorovna Popova, after such messages, took a vacation at her own expense and went to her son's unit. The woman was struck by the change that had taken place in her son: he was gloomy, he imagined enemies and murderers.
Alevtina Viktorovna took her son to the garrison polyclinic and persuaded the psychiatrist to issue a referral to the hospital. But the young man became stubborn: "It is better to commit suicide than go to the hospital. They will point the finger at me and say that I am crazy." The doctor removed him from the outfits, but the commanders took responsibility and continued to put the sick soldier on duty.
They will point the finger at me and say that I am crazy." The doctor removed him from the outfits, but the commanders took responsibility and continued to put the sick soldier on duty.
Mom went home, but a few days after talking with her son on the phone she returned to the unit again. This time, she even more convincingly insisted that Alexander be taken to the hospital and prescribed treatment. In Rostov, doctors discovered a very severe, advanced form of the disease in him and diagnosed him with malignant schizophrenia. After being discharged from the hospital by the VTEK commission, the 20-year-old boy was recognized as a disabled person of the II group.
Alevtina Viktorovna had to quit her job to take care of her sick son. In the Independent Psychiatric Association, which is located in Moscow, experts regarding Popov gave the following conclusion: “The disease is endogenous, that is, external factors could only play a provoking role. condition of a soldier and even opposition to his treatment with a high probability could aggravate the course of the disease.
Psychopaths become in the service
Psychiatrists are increasingly identifying neuropsychiatric diseases in military personnel and the inability to adapt in an army environment. Moreover, deviations are observed not only among conscripts, but also among officers, ensigns, sergeants, as a result of which such sad phenomena arise as escapes from units, insanity, suicide, hazing.
Igor Nikolaevich Orlov, a psychiatrist at the Volgograd garrison polyclinic N 74, through which almost all information about the military personnel of the garrison suffering from neuropsychiatric disorders passes, believes that recently the general mental state of conscripts and military personnel has not been given due attention.
In principle, doctors believe that personality disorders can be found in almost every person, but the degree of their severity depends on how this person manifests himself, for example, in communication with other people.
It turns out that in civilian life such guys are practically healthy and, roughly speaking, they are allergic to the army: they cannot adapt to new, difficult conditions for themselves. Perhaps this is because military service has lost prestige in the minds of most people, today a more "noble" act is in vogue: "mow down" from the army. As a result, a certain layer gets into the service: those who could not "get off", young alcoholics, drug addicts, children from socially disadvantaged families.
- Among them, the percentage of mental disorders is much higher than in the general "population", - says Dr. Igor Orlov. - Such military personnel cannot or do not know how to independently consciously solve interpersonal problems, which exacerbates conflicts in units. To prevent this, future soldiers should check their health, including mental health, even before the army.
Track and cure!
Not only in the Volgograd region, but also in other regions of Russia, physicians have to deal with cases when doctors of military draft commissions do not detect general mental illness among conscripts. As a result, schizophrenics, oligophrenics, patients with epilepsy find themselves in the ranks of the defenders of the Fatherland. The draft boards of the region have found ways to track these diseases. There are two specialized hospitals in the city on the Volga, which have the right to conduct military medical examinations. But military personnel have to face many difficulties in order to get to these hospitals for treatment, and often this leads to the fact that those in need of medical care are dragged out for weeks after the necessary examination.
As a result, schizophrenics, oligophrenics, patients with epilepsy find themselves in the ranks of the defenders of the Fatherland. The draft boards of the region have found ways to track these diseases. There are two specialized hospitals in the city on the Volga, which have the right to conduct military medical examinations. But military personnel have to face many difficulties in order to get to these hospitals for treatment, and often this leads to the fact that those in need of medical care are dragged out for weeks after the necessary examination.
- Often there are cases when some problem of a serviceman can be solved at the level of a psychologist, but commanders do not always express a desire to help a guy with the help of a qualified specialist to understand himself, - says Dr. Igor Orlov.
The medical service of the North Caucasian Military District, after analyzing the available facts, came to the conclusion that about 80 percent of suicides that take place in the military units of the regions of the Southern Federal District are committed by practically healthy people.