List of mental health
Types of mental health issues and illnesses
Mental illness is a general term for a group of illnesses that may include symptoms that can affect a person’s thinking, perceptions, mood or behaviour. Mental illness can make it difficult for someone to cope with work, relationships and other demands. The relationship between stress and mental illness is complex, but it is known that stress can worsen an episode of mental illness. Most people can manage their mental illness with medication, counselling or both.This page lists some of the more common mental health issues and mental illnesses.
Anxiety disorders
Anxiety disorders is a group of mental health disorders that includes generalised anxiety disorders, social phobias, specific phobias (for example, agoraphobia and claustrophobia), panic disorders, obsessive compulsive disorder (OCD) and post-traumatic stress disorder. Untreated, anxiety disorders can lead to significant impairment on people’s daily lives.
For more information see: Anxiety disorders.
Behavioural and emotional disorders in children
Common behaviour disorders in children include oppositional defiant disorder (ODD), conduct disorder (CD) and attention deficit hyperactivity disorder (ADHD). Treatment for these mental health disorders can include therapy, education and medication.
For more information see: Behavioural disorders in children.
Bipolar affective disorder
Bipolar affective disorder is a type of mood disorder, previously referred to as ‘manic depression’. A person with bipolar disorder experiences episodes of mania (elation) and depression. The person may or may not experience psychotic symptoms. The exact cause is unknown, but a genetic predisposition has been clearly established. Environmental stressors can also trigger episodes of this mental illness.
For more information see: Bipolar disorder.
Depression
Depression is a mood disorder characterised by lowering of mood, loss of interest and enjoyment, and reduced energy.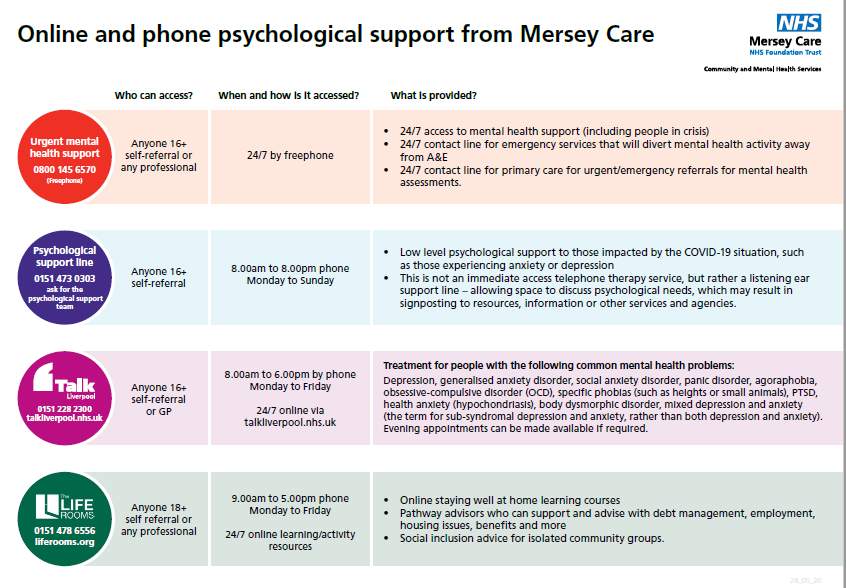 It is not just feeling sad. There are different types and symptoms of depression. There are varying levels of severity and symptoms related to depression. Symptoms of depression can lead to increased risk of suicidal thoughts or behaviours.
It is not just feeling sad. There are different types and symptoms of depression. There are varying levels of severity and symptoms related to depression. Symptoms of depression can lead to increased risk of suicidal thoughts or behaviours.
For more information see: Depression.
Dissociation and dissociative disorders
Dissociation is a mental process where a person disconnects from their thoughts, feelings, memories or sense of identity. Dissociative disorders include dissociative amnesia, dissociative fugue, depersonalisation disorder and dissociative identity disorder.
For more information see: Dissociation and dissociative disorders.
Eating disorders
Eating disorders include anorexia, bulimia nervosa and other binge eating disorders. Eating disorders affect females and males and can have serious psychological and physical consequences.
For more information see: Eating disorders.
Obsessive compulsive disorder
Obsessive compulsive disorder (OCD) is an anxiety disorder. Obsessions are recurrent thoughts, images or impulses that are intrusive and unwanted. Compulsions are time-consuming and distressing repetitive rituals. Treatments include cognitive behaviour therapy (CBT), and medications.
Obsessions are recurrent thoughts, images or impulses that are intrusive and unwanted. Compulsions are time-consuming and distressing repetitive rituals. Treatments include cognitive behaviour therapy (CBT), and medications.
For more information see: Obsessive compulsive disorder.
Paranoia
Paranoia is the irrational and persistent feeling that people are ‘out to get you’. Paranoia may be a symptom of conditions including paranoid personality disorder, delusional (paranoid) disorder and schizophrenia. Treatment for paranoiainclude medications and psychological support.
For more information see: Paranoia.
Post-traumatic stress disorder
Post-traumatic stress disorder (PTSD) is a mental health condition that can develop as a response to people who have experienced any traumatic event. This can be a car or other serious accident, physical or sexual assault, war-related events or torture, or natural disasters such as bushfires or floods.
For more information see: Post-traumatic stress disorder.
Psychosis
People affected by psychosis can experience delusions, hallucinations and confused thinking.. Psychosis can occur in a number of mental illnesses, including drug-induced psychosis, schizophrenia and mood disorders. Medication and psychological support can relieve, or even eliminate, psychotic symptoms.
For more information see: Psychosis.
Schizophrenia
Schizophrenia is a complex psychotic disorder characterised by disruptions to thinking and emotions, and a distorted perception of reality. Symptoms of schizophrenia vary widely but may include hallucinations, delusions, thought disorder, social withdrawal, lack of motivation and impaired thinking and memory. People with schizophrenia have a high risk of suicide. Schizophrenia is not a split personality.
For more information see: Schizophrenia.
Where to get help
- Your GP (doctor)
- Mental health services
Psychosis and mental illness - Better Health Channel
Summary
Read the full fact sheet- People experiencing psychosis are unable to distinguish what is real.
- Psychosis is associated with a number of illnesses that affect the brain.
- Medication and community support can relieve, or even eliminate, psychotic symptoms.
Around three per cent of people will experience a psychotic episode at some point in their life. In any given 12-month period, just under one in every 200 adult Australians will experience a psychotic illness.
The period of time where people experience psychotic symptoms is known as an ‘episode’ of psychosis. Some people only experience a few episodes of psychosis, or a brief episode that lasts for a few days or weeks. Others will experience symptoms more frequently, in association with a longer-term illness such as schizophrenia.
The first episode of psychosis usually occurs in a person's late teens or early 20s.
Symptoms of psychosis
Symptoms of psychosis include:
- confused thinking
- delusions – false beliefs that are not shared by others
- hallucinations – hearing, seeing, smelling or tasting something that isn't there
- changed behaviours and feelings.
Confused thinking and psychosis
During an episode of psychosis a person’s thoughts become confused. Words and ideas lose their meaning or take on meanings that make no sense.
These disturbances in thinking can affect a person's ability to concentrate, remember things and make plans. Confused thinking can continue, even after the psychotic episode has ended.
You may be able to tell that someone is having an episode of psychosis through changes in their speech. These may include:
- speaking very quickly or slowly
- changing topics frequently
- speaking in muddled-up sentences
- using the wrong words to describe things
- making up words.
Delusions and psychosis
Delusions are false beliefs that are not shared by others. Delusions can take various forms, including:
- paranoid delusion – for example, the person believes they are being watched and singled out for some harmful purpose
- grandiose delusion – for example, the person believes they have special powers or that they are an important religious or political figure
- reference delusion – for example, the person believes they are receiving special messages or codes through media such as TV shows, songs or advertising
- control delusion – for example, the person believes their thoughts are being controlled or influenced by outside forces such as aliens, some real or invented group, an individual or something more vague
- somatic delusion – for example, the person believes something has happened to their body – something is wrong with it, some part of it is missing or dead, they have a disease or are infested with parasites
- depressive delusion – for example, the person believes they are guilty of some terrible crime.
Hallucinations and psychosis
A hallucination is when someone hears, sees, smells or tastes something that isn't there. A common form of hallucination is to hear voices that aren't there. Hallucinations can lead to agitation, distress, frustration and even hostility.
Changed behaviour and psychosis
Psychosis can affect a person’s behaviour. A person with psychosis may experience:
- social isolation or becoming withdrawn
- problems with work, social or family life
- problems with motivation
- problems with increased activity
- laughing at inappropriate times or becoming upset without an identifiable cause.
Changed feelings and psychosis
Psychosis can lead to changes in emotions. How a person feels can change for no obvious reason. Examples may include:
•feeling strange and cut off from the world
•mood swings, feeling unusually excited or depressed
•feeling or showing less emotion
•feeling distanced or detached from one's body or thoughts
Types of psychotic illness
There are a number of mental illnesses where psychotic symptoms can be present.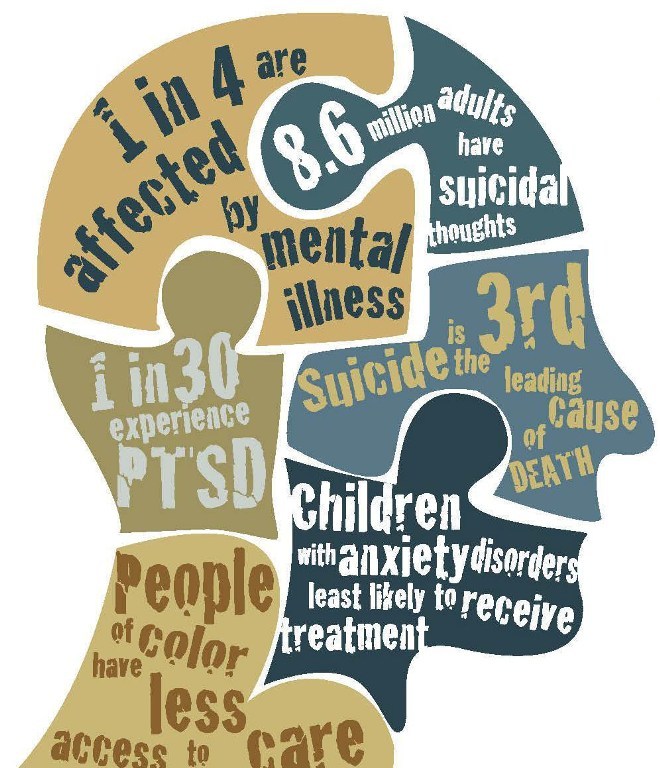 Examples include:
Examples include:
- brief reactive psychosis – psychotic symptoms that arise due to a very stressful event and last less than a month
- drug induced psychosis – caused by drugs such as alcohol, speed, LSD, marijuana, ecstasy or magic mushrooms. The symptoms last until the effects of the drugs wear off (hours or days)
- schizophrenia – most people affected by schizophrenia experience a range of psychotic symptoms and commonly have difficulty organising their thoughts
- bipolar disorder – involves very extreme moods (either very high or very low) that can lead to psychotic symptoms
- psychotic depression – depression can be so intense that it causes psychotic symptoms.
Causes of psychosis
The causes of psychosis are not fully understood. It is likely that psychosis is caused by a number of factors including:
- genetic vulnerability – family history of psychotic disorder
- chemical imbalance in the brain
- substance use, particularly cannabis, speed or ice
- environmental factors
- psychosocial stress – for people who have had an episode of psychosis, significant stress may be a factor in the development of further episodes.
Diagnosis of psychosis
The presence of psychotic symptoms does not automatically mean that someone has a psychotic disorder.
To diagnose a psychotic disorder, a mental health professional will do a comprehensive medical and psychological assessment over time. This can be done either at home or in hospital. They will check for psychosis caused by drugs or other diseases first.
Treatment for psychosis
Treatment can do much to relieve, or even eliminate, the symptoms of psychosis. Treatments include:
- medication – certain medications such as anti-psychotics help the brain to restore its normal chemical balance
- community support programs – ongoing support may be needed to help a person experiencing psychosis to live independently in the community. Support may include help with accommodation, finding suitable work, and the development of social and personal skills
- psychological therapies such as psychotherapy, cognitive-behaviour therapy, family therapy and counselling are aimed at teaching skills and techniques for coping with stress, improving quality of life and helping people to manage their symptoms
- self-help and peer support groups
- lifestyle changes – such as improving general health and reducing stress through activities such as art, music and exercise can support recovery.
 Avoiding drugs and alcohol and getting good sleep can also help.
Avoiding drugs and alcohol and getting good sleep can also help.
Where to get help
- SANE Australia Tel. 1800 18 SANE (7263) Monday to Friday, 10 am – 10 pm
- Need Help? Chat live with a SANE Helpline Advisor (Available Monday-Friday, 10am-10pm AEST).
- SANE Forums are full of people who want to talk to you and offer support.
- Your GP (Doctor)
- Psychosis, SANE Australia, Melbourne.
- Understanding mental health conditions – psychosis, Mind Australia.
- Psychotic disorder assessment and treatment, headspace, National Youth Mental Health Foundation, Australia.
- Psychosis, Orygen, The National Centre of Excellence in Youth Mental Health, Australia.
- Perala J, Suvisaari J, Saarni SI, et al. 2007 ‘Lifetime prevalence of psychotic and bipolar I disorders in a general population’, Archives of General Psychiatry, vol. 64, no. 1, pp. 19–28.
This page has been produced in consultation with and approved by:
Schizophrenia
Schizophrenia- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Data and statistics »
- News bulletin
- The facts are clear
- Publications
- Find Country »
- A
- B
- C
- D
- E
- e
- ё 9000
- x
- C
- h
- Sh
9000 WHO in countries » - Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A
- Developments
- Photo reports
- Questions and answers
- Update
- Emergencies "
- News "
- Disease Outbreak News
- WHO Data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Basic moments "
- About WHO »
- CEO
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center /
- Newsletters/
- Read more/
- Schizophrenia
Key Facts
- Schizophrenia is a severe mental disorder that affects approximately 24 million people, or 1 in 300 people worldwide.

- Schizophrenia causes psychosis, is associated with severe disability, and can negatively affect all areas of life, including personal, family, social, academic and work life.
- People with schizophrenia are often subject to stigma, discrimination and human rights violations.
- Globally, more than two thirds of people with psychosis do not receive specialized mental health care.
- There are a number of effective care options for patients with schizophrenia that can lead to a complete recovery of at least one in three patients.
Symptoms
Schizophrenia is characterized by significant disturbances in perception of reality and behavioral changes such as:
- persistent delusions: the patient has a persistent belief in the truth of certain things, despite evidence to the contrary;
- persistent hallucinations: the patient hears, sees, touches non-existent things and smells non-existent smells;
- sensation of external influence, control or passivity: the presence in the patient of the sensation that his feelings, impulses, actions or thoughts are dictated from outside, put in or disappear from consciousness by someone else's will, or that his thoughts are broadcast to others;
- disorganized thinking, often expressed in incoherent or pointless speech;
- Significant disorganization of behavior, which manifests itself, for example, in the performance by the patient of actions that may seem strange or meaningless, or in an unpredictable or inappropriate emotional reaction that does not give the patient the opportunity to organization of their behavior;
- "negative symptoms" such as extreme poverty of speech, smoothness of emotional reactions, inability to feel interest or pleasure, social autism; and/or
- Extreme agitation or, on the contrary, slowness of movements, freezing in unusual postures.
People with schizophrenia often also experience persistent cognitive or thinking problems that affect memory, attention, or problem-solving skills.
At least one third of patients with schizophrenia experience complete remission of symptoms (1). In some, periods of remission and exacerbation of symptoms follow each other throughout life, in others there is a gradual increase in symptoms.
Scope and impact
Schizophrenia affects approximately 24 million people, or 1 in 300 people (0.32%) worldwide. Among adults, the rate is 1 in 222 (0.45%) (2). Schizophrenia is less common than many other mental disorders. Onset is most common in late adolescence and between the ages of 20 and 30; while women tend to have a later onset of the disease.
Schizophrenia is often accompanied by significant stress and difficulties in personal relationships, family life, social contacts, studies, work or other important areas of life.
Individuals with schizophrenia are 2-3 times more likely to die early than the population average (2). It is often associated with physical illnesses such as cardiovascular disease, metabolic disease, and infectious disease.
It is often associated with physical illnesses such as cardiovascular disease, metabolic disease, and infectious disease.
Patients with schizophrenia often become the object of human rights violations both within the walls of psychiatric institutions and in everyday life. Significant stigmatization of people with this disease is a widespread phenomenon that leads to their social isolation and has a negative impact on their relationships with others, including family and friends. This creates grounds for discrimination, which in turn limits access to health services in general, education, housing and employment.
Humanitarian emergencies and health crises can cause intense stress and fear, disrupt social support mechanisms, lead to isolation and disruption of health services and supply of medicines. All these shocks can have a negative impact on the lives of people with schizophrenia, in particular by exacerbating existing symptoms of the disease. People with schizophrenia are more vulnerable during emergencies to various human rights violations and, in particular, face neglect, abandonment, homelessness, abuse and social exclusion.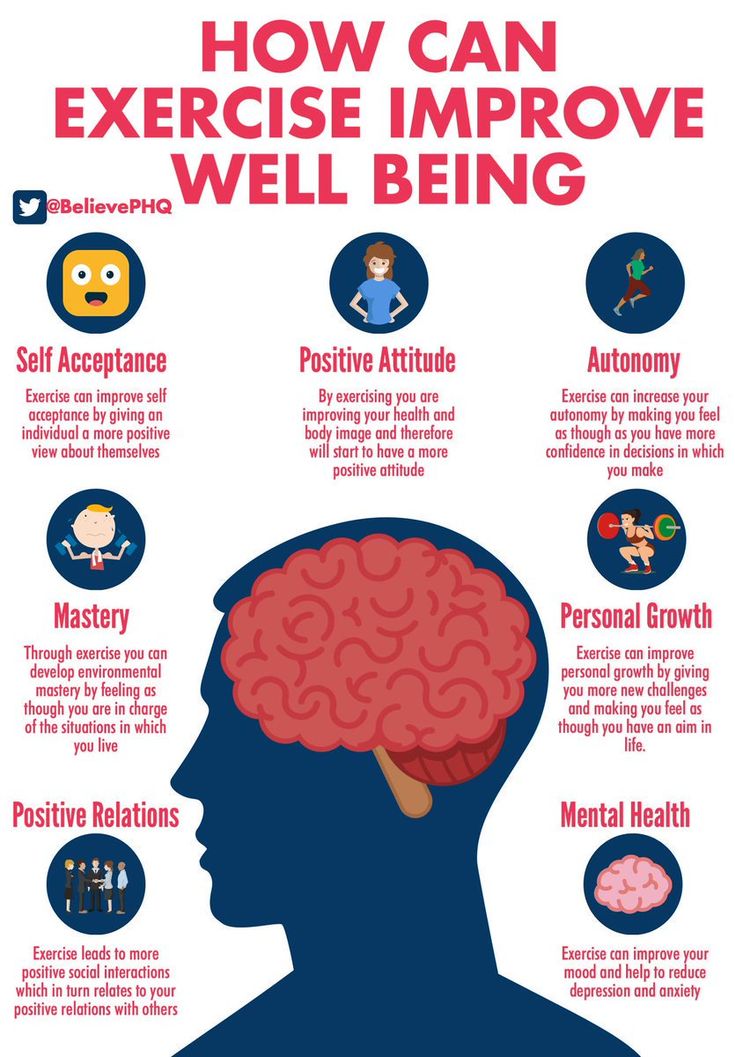
Causes of schizophrenia
Science has not established any one cause of the disease. It is believed that schizophrenia may be the result of the interaction of a number of genetic and environmental factors. Psychosocial factors may also influence the onset and course of schizophrenia. In particular, heavy marijuana abuse is associated with an increased risk of this mental disorder.
Assistance services
At present, the vast majority of people with schizophrenia do not receive mental health care worldwide. Approximately 50% of patients in psychiatric hospitals are diagnosed with schizophrenia (4). Only 31.3% of people with psychosis get specialized mental health care (5). Much of the resources allocated to mental health services are inefficiently spent on the care of patients admitted to psychiatric hospitals.
Available scientific evidence clearly indicates that hospitalization in psychiatric hospitals is not an effective treatment for mental disorders and is regularly associated with the violation of the basic rights of patients with schizophrenia. Therefore, it is necessary to ensure the expansion and acceleration of work on the transfer of functions in the field of mental health care from psychiatric institutions to the level of local communities. Such work should begin with the organization of the provision a wide range of quality community-based mental health services. Options for community-based mental health care include integrating this type of care into primary health care and hospital care. general care, setting up community mental health centres, outpatient care centres, social housing with nursing care and social home care services. Involvement in the care process is essential the patient with schizophrenia, his family members and members of local communities.
Therefore, it is necessary to ensure the expansion and acceleration of work on the transfer of functions in the field of mental health care from psychiatric institutions to the level of local communities. Such work should begin with the organization of the provision a wide range of quality community-based mental health services. Options for community-based mental health care include integrating this type of care into primary health care and hospital care. general care, setting up community mental health centres, outpatient care centres, social housing with nursing care and social home care services. Involvement in the care process is essential the patient with schizophrenia, his family members and members of local communities.
Schizophrenia management and care
There are a number of effective approaches to treating people with schizophrenia, including medication, psychoeducation, family therapy, cognitive behavioral therapy, and psychosocial rehabilitation (eg life skills education).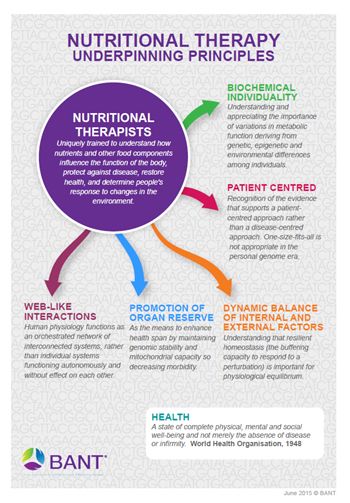 The most important interventions for helping people with schizophrenia are assisted living, special housing and employment assistance. It is extremely important for people with schizophrenia and their families and/or caregivers to a recovery-centered approach that empowers people to participate in decisions about their care.
The most important interventions for helping people with schizophrenia are assisted living, special housing and employment assistance. It is extremely important for people with schizophrenia and their families and/or caregivers to a recovery-centered approach that empowers people to participate in decisions about their care.
WHO activities
steps are in place to ensure that appropriate services are provided to people with mental disorders, including schizophrenia. One of the key recommendations The action plan is to transfer the function of providing assistance from institutions to local communities. WHO Special Mental Health Initiative aims to further progress towards the goals of the Comprehensive Plan mental health action 2013–2030 by ensuring that 100 million more people have access to quality and affordable mental health care.
The WHO Mental Health Gap Action Program (mhGAP) is working to develop evidence-based technical guidelines, tools and training packages to scale up services in countries, especially in low-resource settings. The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in as part of an integrated approach to mental health care at all levels of care. To date, the mhGAP Program has been implemented in more than 100 WHO Member States.
The program focuses on a priority list of mental health disorders, including psychosis, and aims to strengthen the capacity of non-specialized health workers in as part of an integrated approach to mental health care at all levels of care. To date, the mhGAP Program has been implemented in more than 100 WHO Member States.
The WHO QualityRights project aims to improve the quality of care and better protect human rights in mental health and social care settings and to expand opportunities of various organizations and associations to defend the rights of persons with mental disorders and psychosocial disabilities.
The WHO guidelines on community mental health services and human rights-based approaches provide information for all stakeholders who intend to develop or transform mental health systems and services. health in accordance with international human rights standards, including the UN Convention on the Rights of Persons with Disabilities.
Bibliography
(1) Harrison G, Hopper K, Craig T, Laska E, Siegel C, Wanderling J. Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry 2001;178:506-17.
Recovery from psychotic illness: a 15- and 25-year international follow-up study. Br J Psychiatry 2001;178:506-17.
(2) Institute of Health Metrics and Evaluation (IHME). Global Health Data Exchange (GHDx). http://ghdx.healthdata.org/gbd-results-tool?params=gbd-api-2019-permalink/27a7644e8ad28e739382d31e77589dd7 (accessed 25 September 2021)
(3) LaursenTM, Nordentoft M, Mortensen PB. Excess early mortality in schizophrenia. Annual Review of Clinical Psychology , 2014;10, 425-438.
(4) WHO. Mental health systems in selected low- and middle-income countries: a WHO-AIMS cross-national analysis. WHO: Geneva, 2009
(5) Jaeschke K et al. Global estimates of service coverage for severe mental disorders: findings from the WHO Mental Health Atlas 2017 Glob Ment Health 2021;8:e27.
Dementia
Dementia- Popular Topics
- Air pollution
- Coronavirus disease (COVID-19)
- Hepatitis
- Data and statistics »
- News bulletin
- The facts are clear
- Publications
- Find Country »
- A
- B
- C
- D
- D
- E 9000 In
- Ф
- x
- C
- h
- Sh
9000 WHO in countries »- Reporting
- Regions »
- Africa
- America
- Southeast Asia
- Europe
- Eastern Mediterranean
- Western Pacific
- Media Center
- Press releases
- Statements
- Media messages
- Comments
- Reporting
- Online Q&A
- Developments
- Photo reports
- Questions and answers
- Update
- Emergencies "
- News "
- Disease Outbreak News
- WHO Data »
- Dashboards »
- COVID-19 Monitoring Dashboard
- Basic moments "
- About WHO »
- CEO
- About WHO
- WHO activities
- Where does WHO work?
- Governing Bodies »
- World Health Assembly
- Executive committee
- Main page/
- Media Center /
- Newsletters/
- Read more/
- Dementia
Cathy Greenblat
© A photo
Dementia is a syndrome, usually chronic or progressive, in which there is a deterioration in cognitive function (ie the ability to think) to a greater extent than is expected with normal aging. There is a degradation of memory, thinking, understanding, speech and the ability to navigate, count, learn and reason. Dementia does not affect consciousness. Cognitive dysfunction is often accompanied, and sometimes preceded, by a deterioration in emotional control, as well as a degradation in social behavior or motivation.
There is a degradation of memory, thinking, understanding, speech and the ability to navigate, count, learn and reason. Dementia does not affect consciousness. Cognitive dysfunction is often accompanied, and sometimes preceded, by a deterioration in emotional control, as well as a degradation in social behavior or motivation.
Dementia is caused by a variety of illnesses and injuries that primarily or secondarily cause brain damage, such as Alzheimer's disease or stroke.
Dementia is one of the leading causes of disability and addiction among older people worldwide. It can have a profound impact not only on the people who suffer it, but also on their families and caregivers. There is often a lack of awareness and understanding about dementia, leading to stigma and barriers to diagnosis and care. The impact of dementia on caregivers, families and society as a whole can be physical, psychological, social and economic.
Signs and symptoms
Dementia affects people differently, depending on the impact of the disease and on the individual before the disease. The signs and symptoms associated with dementia go through three stages of development.
The signs and symptoms associated with dementia go through three stages of development.
Early stage: The early stage of dementia often goes unnoticed because it develops gradually. Common symptoms include:
- forgetfulness;
- loss of track of time;
- disorientation in a familiar area.
Intermediate: As dementia progresses towards the intermediate stage, the signs and symptoms become more pronounced and increasingly narrowing. They include:
- forgetting about recent events and people's names;
- disorientation at home;
- increasing difficulties in communication;
- need for help with self-care;
- behavioral difficulties, including aimless walking and asking the same questions.
Late stage: In the late stage of dementia, almost complete dependence and inactivity develops. Memory impairment becomes significant, and physical signs and symptoms become more obvious. Symptoms include:
Symptoms include:
- disorientation in time and space;
- difficulty in recognizing relatives and friends;
- increasing need for help with self-care;
- difficulty in moving;
- behavioral changes that may be aggravated and include aggressiveness.
Common forms of dementia
There are many forms of dementia. Alzheimer's disease is the most common form, accounting for 60-70% of all cases. Other common forms include vascular dementia, Lewy body dementia (abnormal protein inclusions that form inside nerve cells), and a group of diseases that contribute to frontotemporal dementia (degeneration of the frontal lobe of the brain). There are no clear boundaries between different forms of dementia, and mixed forms of dementia often coexist.
Dementia rates
There are about 50 million people with dementia worldwide, more than half, almost 60% of them, live in low- and middle-income countries. There are about 10 million new cases of the disease every year.
The proportion of the general population aged 60 years and over with dementia at any point in time is estimated to be between 5% and 8%.
The total number of people with dementia is projected to be around 82 million in 2030 and 152 by 2050. This growth will be driven in large part by an increase in the number of people with dementia in low- and middle-income countries.
Treatment and care
Currently there is no therapy to cure or change the course of dementia. Numerous new drugs are under investigation and are at various stages of clinical trials.
However, much can be done to support and improve the lives of people with dementia, their caregivers and their families. The main goals of medical care for dementia are:\n
- early diagnosis to ensure early and optimal management;
- optimization of physical health, cognitive abilities, activity and well-being;
- detection and treatment of associated physical illness;
- detection and treatment of behavioral and psychological symptoms;
- provide information and long-term support for carers.

Risk factors and prevention
Although age is the most important known risk factor for dementia, it is not an inevitable consequence of aging. What’s more, dementia doesn’t just affect the elderly—early onset of dementia (defined as the onset of symptoms before the age of 65) accounts for up to 9% of all cases of dementia.
Research shows that the risk of dementia can be reduced by exercising regularly, not smoking, avoiding the harmful use of alcohol, controlling your weight, eating well, and maintaining normal blood pressure, cholesterol, and blood sugar levels. Other risk factors include depression, low educational attainment, social isolation, and cognitive inactivity.
Social and economic impact
Dementia has a significant social and economic impact in terms of medical costs, social care costs and informal care. In 2015, total global public spending on dementia was estimated at US$818 billion, corresponding to 1.1% of the world's gross domestic product (GDP).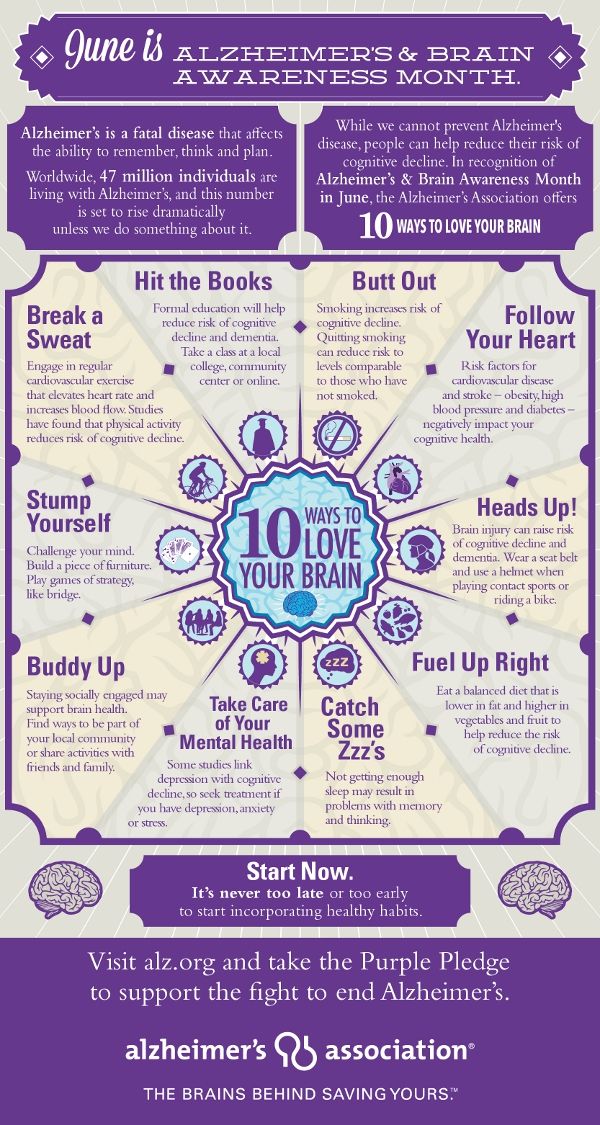 Total spending as a share of GDP ranged from 0.2% in low-income countries to 1.4% in high-income countries.
Total spending as a share of GDP ranged from 0.2% in low-income countries to 1.4% in high-income countries.
Impact on families and caregivers
Dementia can have a profound impact on the families of those affected and their caregivers. The physical, emotional and financial burden can put a lot of stress on families and caregivers, and they need support from the health, social, financial and legal systems.
Human rights
People with dementia are often denied the basic rights and freedoms that other people have. In many countries, physical means and chemicals are widely used in nursing homes and intensive care facilities to retain patients, even though there are regulations in place to protect the human rights to freedom and choice.
Providing high-quality care for people with dementia and their caregivers requires appropriate and supportive legal and regulatory frameworks based on internationally recognized human rights standards.
WHO activities
WHO recognizes dementia as a public health priority.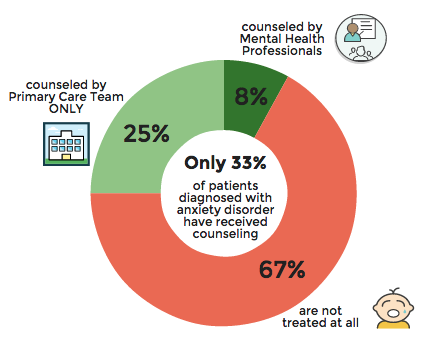 In May 2017, the World Health Assembly approved the Global Health Sector Action Plan for the Response to Dementia 2017-2025. The plan is a comprehensive program of action for policy makers, international, regional and national partners and WHO in the following areas:
In May 2017, the World Health Assembly approved the Global Health Sector Action Plan for the Response to Dementia 2017-2025. The plan is a comprehensive program of action for policy makers, international, regional and national partners and WHO in the following areas:
- taking action on dementia as a public health priority; raising awareness about dementia and creating supportive environment initiatives for people with dementia; reduced risk of developing dementia;
- reduced risk of dementia; diagnosis, treatment and care;
- dementia information systems; support for carers of people with dementia; and
- research and innovation.
An international monitoring platform, the Global Dementia Observatory, has been established for policy makers and researchers to facilitate monitoring and sharing of information on dementia policy, health care, epidemiology and research. WHO is also developing a knowledge-sharing platform to facilitate the sharing of best practices in the field of dementia.
WHO has developed a dementia action plan to help Member States develop and operationalize dementia action plans. This guidance is closely linked to the WHO Global Observatory on Dementia and includes relevant methodologies, such as a checklist, to guide the preparation, development and implementation of action plans for dementia. In addition, this guide can be helpful in identifying stakeholders and setting priorities.
The WHO Guidelines for Reducing the Risk of Cognitive Impairment and Dementia provide evidence-based recommendations for interventions to reduce modifiable risk factors for dementia such as physical inactivity and unhealthy diets, and to manage medical conditions associated with dementia including hypertension and diabetes.
Dementia is also a priority condition under the Mental Health Gap Action Program (mhGAP), which is an important resource for general practitioners, especially in low- and middle-income countries, to use when providing health care first line for psychiatric and neurological problems and disorders caused by the use of psychoactive substances.
WHO has developed the iSupport program to provide caregivers of people with dementia with information and skills. The iSupport web tool is available as a printed manual and is already in use in a number of countries. An online version of "iSupport" will be available soon.
","datePublished":"2022-09-20T12:00:00.0000000+00:00","image":"https://cdn.who.int/media/images/default-source/imported/en -dementia_ce93dcb3-2920-4021-9af5-32cbbee9bf9f.jpg?sfvrsn=1a94c86c_3","publisher":{"@type":"Organization","name":"World Health Organization: WHO","logo":{"@type":"ImageObject"," url":"https://www.who.int/Images/SchemaOrg/schemaOrgLogo.jpg","width":250,"height":60}},"dateModified":"2022-09-20T12:00: 00.0000000+00:00","mainEntityOfPage":"https://www.who.int/ru/news-room/fact-sheets/detail/dementia","@context":"http://schema.org ","@type":"Article"};
Key Facts
- Dementia is a syndrome in which memory, thinking, behavior and ability to perform daily activities deteriorate.
- Dementia mainly affects the elderly, but is not a normal condition of aging.
- There are about 50 million people with dementia worldwide, and almost 10 million new cases occur each year.
- Alzheimer's disease is the most common cause of dementia, accounting for 60-70% of all cases.
- Dementia is one of the leading causes of disability and addiction among older people worldwide.
- Dementia has a physical, psychological, social and economic impact not only on those affected, but also on their caregivers, families and society as a whole.
Dementia
Dementia is a syndrome, usually chronic or progressive, in which cognitive function (i.e., the ability to think) deteriorates to a greater extent than is expected in normal aging. There is a degradation of memory, thinking, understanding, speech and the ability to navigate, count, learn and reason. Dementia does not affect consciousness. Cognitive dysfunction is often accompanied, and sometimes preceded, by a deterioration in emotional control, as well as a degradation in social behavior or motivation.
Dementia is caused by a variety of illnesses and injuries that primarily or secondarily cause brain damage, such as Alzheimer's disease or stroke.
Dementia is one of the leading causes of disability and addiction among older people worldwide. It can have a profound impact not only on the people who suffer it, but also on their families and caregivers. There is often a lack of awareness and understanding about dementia, leading to stigma and barriers to diagnosis and care. The impact of dementia on caregivers, families and society as a whole can be physical, psychological, social and economic.
Signs and symptoms
Dementia affects people differently, depending on the impact of the disease and on the individual before the disease. The signs and symptoms associated with dementia go through three stages of development.
Early stage: The early stage of dementia often goes unnoticed because it develops gradually. Common symptoms include:
- forgetfulness;
- loss of track of time;
- disorientation in a familiar area.

Intermediate: As dementia progresses towards the intermediate stage, the signs and symptoms become more pronounced and increasingly narrowing. They include:
- forgetting about recent events and people's names;
- disorientation at home;
- increasing difficulties in communication;
- need for help with self-care;
- behavioral difficulties, including aimless walking and asking the same questions.
Late stage: In the late stage of dementia, almost complete dependence and inactivity develops. Memory impairment becomes significant, and physical signs and symptoms become more obvious. Symptoms include:
- disorientation in time and space;
- difficulty in recognizing relatives and friends;
- increasing need for help with self-care;
- difficulty in moving;
- behavioral changes that may be aggravated and include aggressiveness.
Common forms of dementia
There are many forms of dementia. Alzheimer's disease is the most common form, accounting for 60-70% of all cases. Other common forms include vascular dementia, Lewy body dementia (abnormal protein inclusions that form inside nerve cells), and a group of diseases that contribute to frontotemporal dementia (degeneration of the frontal lobe of the brain). There are no clear boundaries between different forms of dementia, and mixed forms of dementia often coexist.
Alzheimer's disease is the most common form, accounting for 60-70% of all cases. Other common forms include vascular dementia, Lewy body dementia (abnormal protein inclusions that form inside nerve cells), and a group of diseases that contribute to frontotemporal dementia (degeneration of the frontal lobe of the brain). There are no clear boundaries between different forms of dementia, and mixed forms of dementia often coexist.
Dementia rates
There are about 50 million people with dementia worldwide, more than half, almost 60% of them, live in low- and middle-income countries. There are about 10 million new cases of the disease every year.
The proportion of the general population aged 60 years and over with dementia at any point in time is estimated to be between 5% and 8%.
The total number of people with dementia is projected to be around 82 million in 2030 and 152 by 2050. This growth will be driven in large part by an increase in the number of people with dementia in low- and middle-income countries.
Treatment and care
Currently there is no therapy to cure or change the course of dementia. Numerous new drugs are under investigation and are at various stages of clinical trials.
However, much can be done to support and improve the lives of people with dementia, their caregivers and their families. The main goals of medical care for dementia are:
- early diagnosis to ensure early and optimal management;
- optimization of physical health, cognitive abilities, activity and well-being;
- detection and treatment of associated physical illness;
- detection and treatment of behavioral and psychological symptoms;
- provide information and long-term support for carers.
Risk factors and prevention
Although age is the most important known risk factor for dementia, it is not an inevitable consequence of aging. What’s more, dementia doesn’t just affect the elderly—early onset of dementia (defined as the onset of symptoms before the age of 65) accounts for up to 9% of all cases of dementia.
Research shows that the risk of dementia can be reduced by exercising regularly, not smoking, avoiding the harmful use of alcohol, controlling your weight, eating well, and maintaining normal blood pressure, cholesterol, and blood sugar levels. Other risk factors include depression, low educational attainment, social isolation, and cognitive inactivity.
Social and economic impact
Dementia has a significant social and economic impact in terms of medical costs, social care costs and informal care. In 2015, total global public spending on dementia was estimated at US$818 billion, corresponding to 1.1% of the world's gross domestic product (GDP). Total spending as a share of GDP ranged from 0.2% in low-income countries to 1.4% in high-income countries.
Impact on families and caregivers
Dementia can have a profound impact on the families of those affected and their caregivers. The physical, emotional and financial burden can put a lot of stress on families and caregivers, and they need support from the health, social, financial and legal systems.
Human rights
People with dementia are often denied the basic rights and freedoms that other people have. In many countries, physical means and chemicals are widely used in nursing homes and intensive care facilities to retain patients, even though there are regulations in place to protect the human rights to freedom and choice.
Providing high-quality care for people with dementia and their caregivers requires appropriate and supportive legal and regulatory frameworks based on internationally recognized human rights standards.
WHO activities
WHO recognizes dementia as a public health priority. In May 2017, the World Health Assembly approved the Global Health Sector Action Plan for the Response to Dementia 2017-2025. The plan is a comprehensive program of action for policy makers, international, regional and national partners and WHO in the following areas:
- taking action on dementia as a public health priority; raising awareness about dementia and creating supportive environment initiatives for people with dementia; reduced risk of developing dementia;
- reduced risk of dementia; diagnosis, treatment and care;
- dementia information systems; support for carers of people with dementia; and
- research and innovation.
An international monitoring platform, the Global Dementia Observatory, has been established for policy makers and researchers to facilitate monitoring and sharing of information on dementia policy, health care, epidemiology and research. WHO is also developing a knowledge-sharing platform to facilitate the sharing of best practices in the field of dementia.
WHO has developed a dementia action plan to help Member States develop and operationalize dementia action plans. This guidance is closely linked to the WHO Global Observatory on Dementia and includes relevant methodologies, such as a checklist, to guide the preparation, development and implementation of action plans for dementia. In addition, this guide can be helpful in identifying stakeholders and setting priorities.
The WHO Guidelines for Reducing the Risk of Cognitive Impairment and Dementia provide evidence-based recommendations for interventions to reduce modifiable risk factors for dementia such as physical inactivity and unhealthy diets, and to manage medical conditions associated with dementia including hypertension and diabetes.