Medicines to take for a cold
Cold Medicine Options for Cough, Stuffy Nose, Runny Nose, and More
Written by Renee Bacher
In this Article
- Stuffy Nose
- Runny Nose, Watery Eyes, and Sneezing
- Cough
- Fever, Aches, and Sore Throat
- Natural Cold Remedies
Over-the-counter medicines won’t cure your cold, but they might make you feel better, so you can rest as it runs its course. Here's a look at some common products and what they can do for you.
Stuffy Nose
Decongestants can curb swelling inside your nose and sinuses, and help you breathe more easily. If you have nasal or sinus congestion, then a decongestant can be helpful.
Decongestants can make some people hyper or keep them awake.
They can also increase blood pressure and heart rate, and raise the chance of heart attacks and strokes. Pseudoephedrine is the primary oral decongestant available. In general, if your blood pressure is well-controlled with medications, a decongestant shouldn't be a problem as long as you monitor your blood pressure.
This may not be true with certain types of blood pressure drugs. Check with your doctor or pharmacist about what may be best for you.
Nasal decongestants work fast to open breathing passages. But if you use them for more than 3 days in a row, you may have a "rebound effect" and end up more congested than you were at the start. Some doctors suggest using a saline spray instead of a medicated spray. Saline spray works more slowly but has no rebound effect.
Runny Nose, Watery Eyes, and Sneezing
When you have a cold, your body makes chemicals called histamines. That leads to sneezing, a runny nose, and watery eyes.
Over-the-counter antihistamines such as chlorpheniramine and diphenhydramine block this process and can relieve those symptoms. They can also make you sleepy and dry out your eyes, nose, and mouth. Antihistamines can make secretions thick, which can be a problem for people with asthma.
Cough
Can’t stop hacking? You have two main choices in the cold-and-flu aisle:
- Cough suppressants, like dextromethorphan, can provide relief for a short time.
 They work on the part of your brain that controls the process.
They work on the part of your brain that controls the process. - Expectorants, like guaifenesin, can break up congestion in your chest by thinning the mucus in your airways. This way, when you do cough, you can get rid of phlegm more easily. Drink plenty of water if you take this medicine.
An occasional cough may clear the lung of pollutants and excess phlegm and probably shouldn't be treated. But a cough that won’t go away should be diagnosed and treated.
Fever, Aches, and Sore Throat
These symptoms are usually mild with a cold compared to a more serious illness, like the flu. Still, if you feel bad and can’t rest, most experts agree it’s OK to take something to ease pain and lower a fever, like acetaminophen or ibuprofen.
Fever may be a good thing. It helps the body fight off infection by suppressing the growth of bacteria and viruses and activating the immune system. Doctors no longer recommend fighting fever for most people, except perhaps for the very young, the very old, and those with certain medical conditions such as heart disease or lung disease.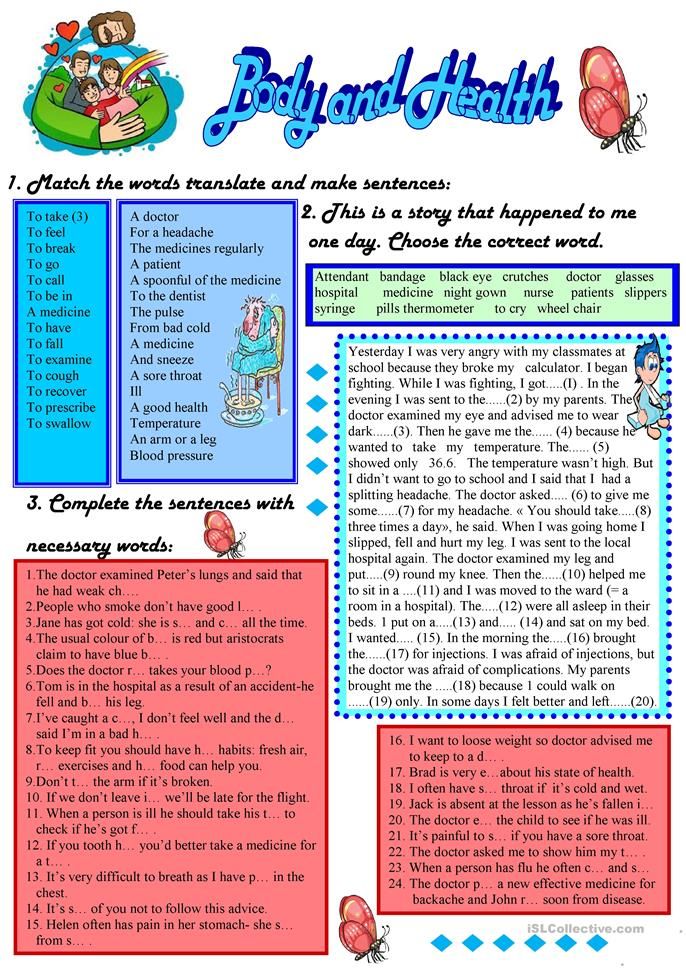 But if you’re uncomfortable, it's fine to take these medications.
But if you’re uncomfortable, it's fine to take these medications.
Young people (including those in their early 20s), however, should avoid aspirin. Acetaminophen (Tylenol) and ibuprofen (Advil) are best. Each type of medicine has risks, so check with your doctor or pharmacist as to which type of pain reliever or fever reducer is best for you.
Drinking lots of fluids and using salt water gargles (made by mixing a cup of warm water and a teaspoon of salt) can often ease the pain of a sore throat. Some oral medications (such as Tylenol) and medicated lozenges and gargles can also temporarily soothe a sore throat. Check with your doctor before using any medications, including over-the-counter drugs, and don't use lozenges or gargles for more than a few days. The drugs could mask signs of strep throat, a bacterial infection that should be treated with antibiotics.
Always check drug labels for side effects, and follow the instructions for taking the medicine. Make sure it won't mix poorly with any other medications you're taking or health problems you have -- ask your doctor or pharmacist if you’re not sure.
Natural Cold Remedies
Maybe you've heard that vitamin C, echinacea, and zinc are good for a cold.
They aren’t cures, but vitamin C and zinc may shorten the length of an illness. Research on echinacea has been mixed. Before you try these products, check with your doctor to make sure they’ll work well with other medicines you’re taking.
Nasal strips can also help you breathe easier, since they can enlarge nasal passages while you wear them.
Other more traditional remedies might help relieve common cold discomfort, too.
- Drink plenty of liquids, including chicken soup. It can make you feel better.
- To relieve a sore throat, gargle with warm salt water, use throat sprays, and suck on ice or lozenges.
- Try a saltwater nasal rinse. These can help with a stuffy or runny nose.
- Use petroleum jelly on your nose if it’s irritated from constant blowing. Facial tissues with added lotions can help prevent, and heal, redness and soreness.
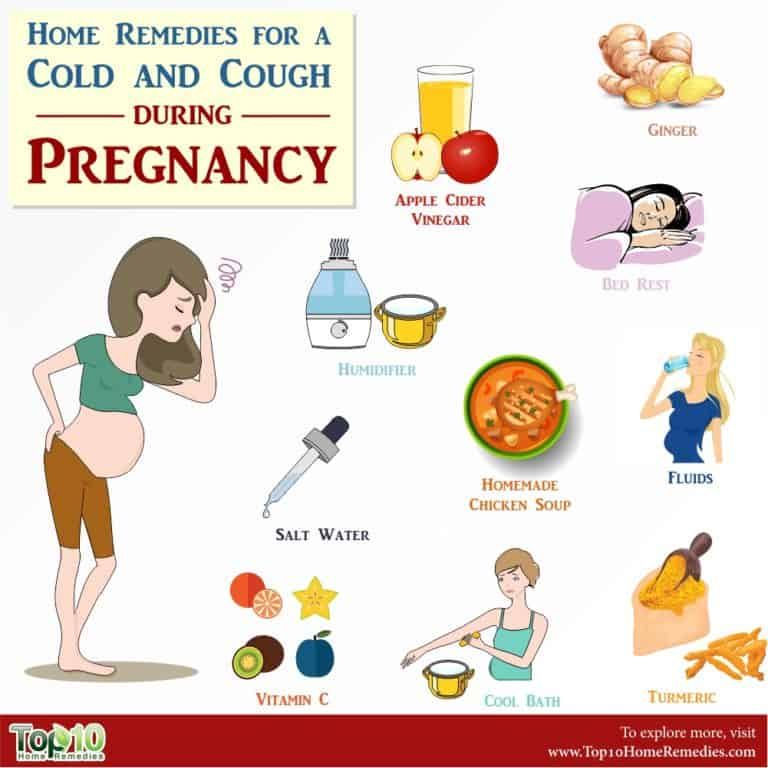
- Use a humidifier to help break up phlegm.
Do what you can to make yourself as comfortable as possible, and rest while your body fights the cold virus.
OTC Medicines for Cough
Written by WebMD Editorial Contributors
In this Article
- All Medicines Aren't the Same
- How to Use Cough Medicine Safely
Is a hacking cough making you feel lousy? Don't grab a random box of cough medicine off the pharmacy shelf. Just a few basics will guide you to an over-the-counter (OTC) medicine for the kind of cough you have.
All Medicines Aren't the Same
The role of cough medicine is to ease symptoms while your body heals.
As a glance at the drugstore shelves will show you, there are many, many brands of OTC cough medicines. But there are only three basic types:
Expectorants help thin mucus, making it easier to cough up. The ingredient guaifenesin is the only expectorant in the U.S., so look for it on the label if you need an expectorant.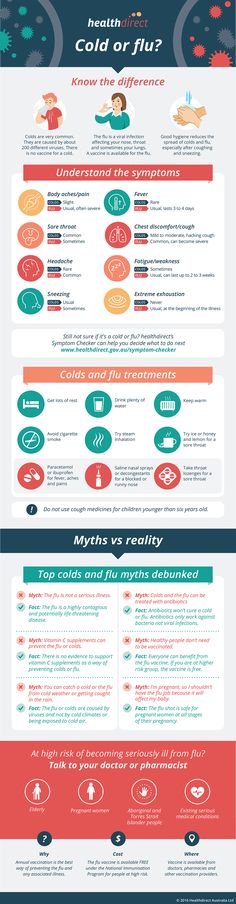
Suppressants help cut the number of times you cough. The active ingredient listed is usually dextromethorphan (DM). Other cough suppressants include camphor, eucalyptus oil, and menthol.
Combination cough products have more than one active ingredient. They have both guaifenesin and dextromethorphan. Cough medicines may also contain ingredients to help coat and soothe the throat.
Combination products may have medicines to ease other symptoms, that may include decongestants for stuffy nose, antihistamines for allergies or a runny nose, or painkillers. Choose a medicine that matches your symptoms.
Cough drops can also help relieve a cough and may ease a sore throat.
How to Use Cough Medicine Safely
- Look at the ingredients. Don't just grab a bottle of anything that says "cough" on it. Check the label. Is it a suppressant or an expectorant? Is it both? Make sure you're getting what you need.
- Don't use medicine for more than 7 days.
 If you do, you could be covering up a more serious problem. See your doctor if your cough is severe or if it doesn't get better after a week.
If you do, you could be covering up a more serious problem. See your doctor if your cough is severe or if it doesn't get better after a week. - Always measure the correct dose. Some people can get too casual about taking OTC cough medicine, slugging it right out of the bottle at times. That's not smart, because even safe medicines in high doses can be very dangerous. High doses of cough medicine can cause serious problems, including brain damage, seizure, or death.
- Be careful with combination medicines. Many OTC cough medicines have multiple ingredients -- expectorants and suppressants along with decongestants, antihistamines, or painkillers. Select products with only the medicines that treat your symptoms. If your symptom is only a cough, for instance, you don't need a decongestant or painkiller. If you need to treat multiple symptoms, check other medicines you take to see if they contain the same ingredients. Don't take two medicines that have the same ingredients.
 If you have any questions, ask your pharmacist or doctor.
If you have any questions, ask your pharmacist or doctor. - Keep away from young children. Make sure to choose the right medicine based on your child's age. Don't give cough and cold medicine to children under age 4. For kids 4 to 6, ask your doctor first. And always make sure to follow the dosing directions on the label.
- Consider doing nothing. Waiting out a cough is the simplest option. Remember that most coughs don't need treatment. You don't have to take any medicine. Give your body a week and your cough will probably go away on its own. If it doesn't, see your doctor.
- Read the label. After you choose the right medicine for you, read the label carefully, so you understand how to take it, common side effects, and any warnings you need to be aware of.
classification, mechanism of action, efficacy, application
If modern medicine has learned to deal with the vast majority of bacterial infections, the situation is different with viral diseases - many of them have to be treated symptomatically.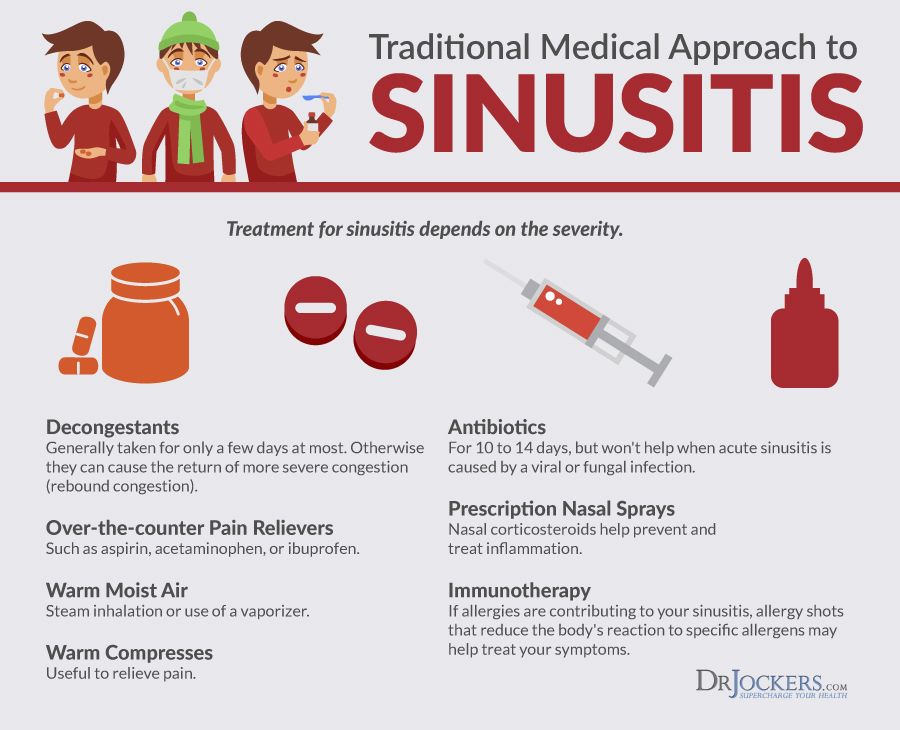 We will tell you which antiviral drugs are effective in treating ARVI, how they work, and in what cases these drugs should be used.
We will tell you which antiviral drugs are effective in treating ARVI, how they work, and in what cases these drugs should be used.
What are antivirals
Viral disease is a difficult task for drug therapy. The fact is that the virus can live and reproduce only inside the host cell, changing its metabolic processes. Therefore, for a long time it was believed that it was impossible to act on viruses without causing significant harm to the body.
Over time, this hypothesis was revised. Since the second half of the last century, scientists have been developing antiviral drugs that act at different stages of the life cycle of the virus - they prevent the virus from attaching to the cell, penetration into and exit of mature viral particles from the cell, and disrupt reproduction (replication).
The effect of these drugs in a therapeutic dose is detrimental to the virus and is practically safe for the body.
Classification of antiviral drugs
All drugs against viruses are divided into the following groups 1 :
● Direct antiviral drugs. They have a strictly defined point of application and suppress the reproduction of a certain type of virus at different stages.
They have a strictly defined point of application and suppress the reproduction of a certain type of virus at different stages.
● Interferons. These are protein compounds that are produced by immune cells in response to an invading virus. They also suppress the activity of viruses by changing a number of processes inside the cell.
● Interferon inducers. These are drugs that stimulate the synthesis of their own protective antiviral substances.
● Immunomodulators. Drugs that affect various parts of the immune defense, they are used only in combination with other antiviral drugs.
According to the method of administration, the listed drugs are divided into systemic and local. The former act on all organs and systems, the latter - locally, in the area of application. Local preparations, as a rule, have a higher concentration of the active substance, work more efficiently, but within a limited superficial focus of infection.
Let us dwell in more detail on the antiviral agents of the listed classes, which are used in ARVI. Many of them not only treat, but also prevent the development of infection.
Many of them not only treat, but also prevent the development of infection.
Direct antivirals
M2 channel blockers
2This class includes the first drug developed in the last century for the chemotherapy of influenza - amantadine. Studies conducted according to the principles of evidence-based medicine have confirmed its effectiveness against influenza viruses type A. In our country, amantadine is not used in the treatment of influenza. Soviet scientists created on its basis a new remedy - rimantadine. This drug has a higher antiviral activity and relatively less toxicity.
How it works. The medicine is taken orally - in the form of tablets, syrup. It penetrates into the blood, and then spreads throughout the body and accumulates in the secretion of the nasal cavity. The active substance binds M2 proteins. This is a kind of "key" in the shell of the virus, which opens the "door" to the cell nucleus through the ion channels in its membrane. The virus enters the cell, but the drug blocks the access of the virus's genetic material to the cell's DNA. Without this, the microorganism cannot reproduce, so the concentration of viruses in the body does not increase. In addition, the drug has an antitoxic effect.
The virus enters the cell, but the drug blocks the access of the virus's genetic material to the cell's DNA. Without this, the microorganism cannot reproduce, so the concentration of viruses in the body does not increase. In addition, the drug has an antitoxic effect.
Application. In order for the medicine to give a good therapeutic effect, the tablets are started to be drunk no later than two days from the onset of the first symptoms of influenza. They are taken twice a day for five days. Children aged 1–14 are given children's syrup.
Contraindications:
● hypersensitivity to the active and auxiliary components of the drug;
● acute liver pathologies;
● acute injury and chronic kidney disease;
● hyperthyroidism;
● pregnancy and breastfeeding;
● Age up to one year.
Side effects. Amantadine often causes a number of negative side effects:
● irritability;
● weakening of concentration;
● sleep disturbance;
● loss of appetite;
● Nausea.
The toxic effect on the central nervous system is enhanced in older people who simultaneously receive antihistamines, anticholinergics (drugs that control bronchial asthma, Parkinson's disease, stop vomiting, and are used in the treatment of chronic obstructive pulmonary disease). Another undesirable effect is the formation of resistance in the infectious agent. Over time, some viruses become resistant to the drug.
Neuraminidase inhibitors
3These include zanamivir (now not used in Russia) and oseltamivir. Both types of antiviral drugs have a similar mechanism of action and indications, are effective against influenza A and B viruses. Compared to the previous group, they are not so toxic, they have a number of contraindications.
How it works. Neuraminidase is one of the main enzymes responsible for the replication of both types of influenza viruses. By blocking it, the medicine temporarily slows down the spread of infection throughout the body. The drug is taken orally. It interacts well with other drugs, often used as part of complex therapy.
The drug is taken orally. It interacts well with other drugs, often used as part of complex therapy.
Application. Tablets (suspension prepared from powder) are recommended to drink from the first symptoms of infection - no later than 48 hours from the initial manifestations, otherwise the use of neuraminidase inhibitors is impractical. The medicine is taken for 5 days, 2 times a day.
Contraindications:
● individual intolerance to any components of the dosage form;
● severe renal and hepatic insufficiency;
● Age up to one year.
Side effects. Most often (in 10-12% of cases) patients complain of nausea and vomiting after the first dose of the drug. Other adverse reactions (in 1-2.5% of patients):
● headaches;
● dizziness;
● weakness;
● insomnia;
● sensation of stuffy nose;
● cough;
● sore throat.
Hemagglutinin inhibitors
4, 5 In Russia, a group of inhibitors is represented by the long-standing domestic drug umifenovir, which acts against viruses of types A and B, and a number of other causative agents of acute respiratory viral infections. However, a study by Russian and British scientists showed that there is a possibility of mutations leading to the emergence of virus strains resistant to umifenovir. Resistance was due to the inability of umifenovir to bind to mutated hemagglutinin. 6 Another drug similar in spectrum is enisamia iodide. This drug is claimed to be highly effective and well tolerated, with no resistant strains.
However, a study by Russian and British scientists showed that there is a possibility of mutations leading to the emergence of virus strains resistant to umifenovir. Resistance was due to the inability of umifenovir to bind to mutated hemagglutinin. 6 Another drug similar in spectrum is enisamia iodide. This drug is claimed to be highly effective and well tolerated, with no resistant strains.
How it works. The drugs act on the hemagglutinin of the virus, a protein that ensures the fusion of its genetic material with cellular DNA. Hemagglutinin inhibitors block infection already at the initial stage, preventing the penetration of the viral particle into the cell.
In addition to the main one, both drugs have additional effects in the fight against the virus: they stimulate the synthesis of interferons, increase the body's resistance to infection. These properties are especially pronounced in enisamium iodide. The drug is rapidly absorbed after oral administration and circulates in the blood for a long time (up to 14 hours), preventing the spread of a viral infection throughout the body.
Application. The drugs are used in the treatment of influenza and other acute respiratory viral infections. Umifenovir is taken orally in the form of capsules, tablets, powder for suspension. The dose and interval, duration of taking the medicine is individually determined by the attending physician. Doctors prescribe enisamia iodide in film-coated tablets, which must be taken orally three times a day for 5-7 days.
In a study conducted by the Illinois Institute of Technology, USA in 2018, it was proved that the administration of enisamium iodide for 4 hours leads to a 100-fold decrease in the concentration of the virus in human bronchial cells. 7 This active ingredient in a dosage of 250 mg and 500 mg is part of the preparations Nobasit ® and Nobasit ® Forte. 8 The drug reduces the risk of complications requiring antibiotics by 4 times and reduces the duration of the disease. 9
Contraindications:
● hypersensitivity to components;
● pregnancy (umifenovir can be used with caution from the second trimester) and breastfeeding;
● Age: use of umifenovir is allowed from the age of 6, enisamia iodide from the age of 12.
In addition, enisamia iodide is not used in case of a tendency to allergic reactions, severe renal and hepatic pathologies.
Side effects. Extremely rarely (less than one case in a thousand), umifenovir can cause allergies - itching, skin rashes, angioedema, and in severe cases - anaphylactic shock. Other side effects were not noted.
Enisamia iodide is generally well tolerated. In some cases, its reception may be accompanied by the following adverse events:
● allergic - itching, skin rash, angioedema;
● unpleasant taste, swelling of the oral mucosa, increased salivation;
● gastrointestinal - heartburn, bloating, nausea and vomiting;
● sore throat, shortness of breath.
Interferons
For the treatment of influenza (including "bird") and other viral respiratory infections, interferon preparations are sometimes used: human leukocyte (mixtures of alpha subtypes) and recombinant (obtained using bacteria) - alpha-2b and gamma.
How it works. Interferon alfa-2b has antiviral and immunomodulatory effects. In intact cells (not infected with a virus), it prevents the virus from entering the cell, and in infected cells, interferon alfa-2b triggers a system of programmed cell death - apoptosis, as a result of which the virus dies along with the cell. The drug also increases the activity of the immune system, enhances phagocytosis and the cytotoxic effect of lymphocytes - protection aimed at eliminating infected cells. Interferon gamma is a powerful immunomodulator. Its main action is the activation of cells responsible for the formation of specific immunity to a primary viral infection and suppression of a secondary bacterial one.
Application. Both types of interferon are used for influenza and SARS in the form of nasal drops. The drug is dripped 2-3 drops 5-6 times a day. Treatment is started as early as possible - before the expiration of three days from the onset of symptoms, otherwise the application will have a preventive effect. Interferon-gamma is also used during the recovery period - within a week.
Interferon-gamma is also used during the recovery period - within a week.
Interferon gamma is not used in hypersensitivity to the drug, pregnancy and under the age of seven years.
Interferon inducers
The list of interferon inducers recommended by the Ministry of Health of the Russian Federation for the treatment of acute respiratory viral infections includes meglumine acridone acetate, tilorone, riamilovir, pentanedioic acid imidazolylethanamide, etc.
Operation principle. All drugs have a similar effect - they contribute to the production of their own interferons of various types, which act universally against many types of viruses.
Application. Preparations are used for ARVI for therapeutic and prophylactic purposes. The dosage regimen is set by the doctor individually for each patient. Common contraindications for most interferon inducers:
● pregnancy;
● breastfeeding;
● Individual intolerance.
● Children's age (restrictions vary depending on the active substance).
Side effects. The most common undesirable effect is the occurrence of an allergic reaction.
Which antiviral drugs are better in the treatment of SARS
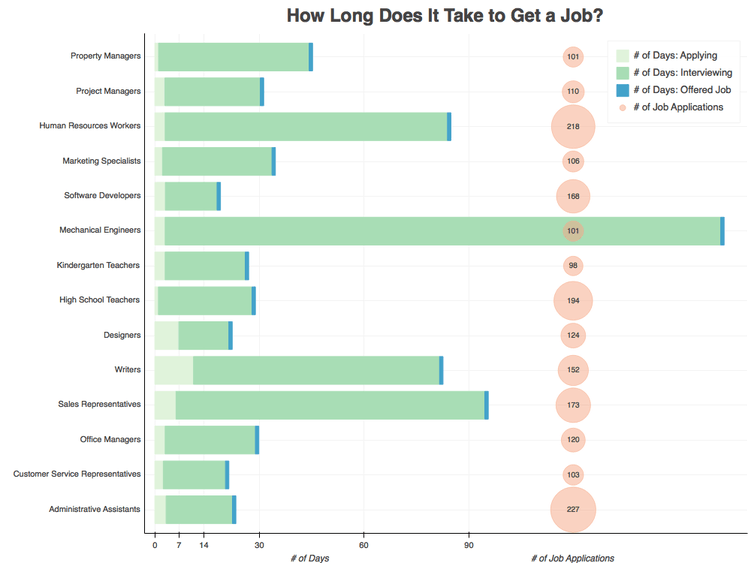
As for SARS and influenza, the table will help to evaluate the effectiveness of antiviral drugs in their therapy in terms of evidence-based medicine. To the right are the scores:
● Strength of Recommendation (RER) from A (most strong) to C.
● Strength of Evidence (CER) of the recommendations given, with 5 being the highest score.
Table 1. Recommendations of the Ministry of Health of the Russian Federation on the use of antiviral drugs of different classes in the treatment of acute respiratory viral infections and influenza. 10, 11
| Medicine | UUR (URD) for influenza | UUR (URD) for SARS |
| Direct antivirals | ||
| Neuraminidase inhibitors | A (1) | Not applicable |
| M2 channel blockers - not recommended for influenza due to rising resistant strains | A (2) | |
| Umifenovir | A (1) | C (2) |
| Enisamia iodide | B (2) | C (2) |
| Interferons | ||
| Alpha 2b or Gamma | B (3) | C (5) |
| Interferon inducers | ||
| Pentandioic acid imidazolylethanamide | B (2) | C (2) |
| Ergoferon | B (2) | C (2) |
| Riamilovir | B (3) | C (1) |
| Kagocel | B (3) | C (3) |
| Tiloron | B (3) | C (3) |
| Meglumine Acridone Acetate | Not applicable | B (1) |
Low scores do not always mean that the drug is not effective - perhaps not all the necessary studies have been carried out with it.
Antivirals for prophylaxis
Many of the drugs listed above are also effective in preventing acute respiratory viral infections - emergency prevention (after contact with the patient) and seasonal. Prophylactic medication during an outbreak is especially necessary for people with reduced immunity - the elderly, suffering from chronic diseases. If taking antiviral drugs does not help prevent the disease, it can make it easier. It is worth remembering that the use of anti-influenza drugs for the purpose of prevention in terms of effectiveness does not replace vaccination.
Essentials at a glance
➢ Antivirals are medicines that directly or indirectly affect the virus.
➢ The most effective drugs with direct antiviral action - they directly affect the virus, its activity, but do not exist for all infections.
➢ Non-specific antivirals—interferons and their inducers—help the immune system defeat the virus and can be used to treat a variety of different infections.
➢ Taking some antivirals can prevent (or alleviate) the disease.
1 Shestakova I.V. Antiviral drugs // Journal for continuing medical education of doctors - https://cyberleninka.ru/article/n/protivovirusnye-preparaty/pdf
2 Khatkhohu M.G. Antiviral drugs: textbook // Maikop State Technological University - 2014 - https://mkgtu.ru/sveden/files/Farmakologiya._Uchebno-metodicheskoe_posobie._Protivovirusnye_sredstva.pdf
3 Hathohu M.G. Antiviral drugs: textbook // Maikop State Technological University - 2014 - https://mkgtu.ru/sveden/files/Farmakologiya._Uchebno-metodicheskoe_posobie._Protivovirusnye_sredstva.pdf
4 Leneva I.A., Pshenichnaya N.Yu. ., Bulgakova V.A. Umifenovir and coronavirus infections: a review of research results and clinical experience // Therapeutic archive - No. 11, 2020 i-opyta-primeneniya-v-klinicheskoy-praktike/pdf
5 Possibilities of etiotropic therapy in reducing the risks of developing severe or complicated ARVI and influenza / Paevskaya E. A. [and other authors] // RMZH - T.27, No. 1-2, 2019.
A. [and other authors] // RMZH - T.27, No. 1-2, 2019.
6 Irina A Leneva, Rupert J Russell, Yury S Boriskin, Alan J Hay. Characteristics of arbidol-resistant mutants of influenza virus: implications for the mechanism of anti-influenza action of arbidol. Antiviral Res. 2009 Feb;81(2):132-40. doi: 10.1016/j.antiviral.2008.10.009. Epub 2008 Nov 24.
7 Boltz D, et al. Activity of enisamium, an isonicotinic acid derivative, against influenza viruses in differentiated normal human bronchial epithelial cells. Antivir Chem Chemother. 2018, , Zubkova T.G., Shakhlanskaya E.V., Evaluation of the effectiveness of the ARVI treatment regimen, including etiotropic (enisamia iodide) and symptomatic therapy // Therapeutic archive No. 3 - 2020.
10 Acute respiratory viral infections (ARVI) in adults: clinical guidelines – https://apicr.minzdrav.gov.ru/api.ashx?op=GetClinrecPdf&id=724_1
11 Influenza in adults: clinical guidelines – https://www.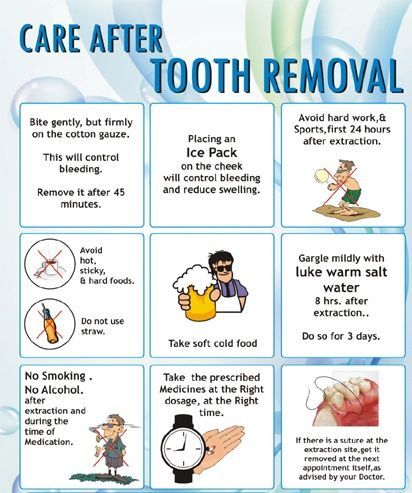 rnmot.ru/public/uploads/RNMOT/clinical/2021/%D0%9A%D0%A0%20%D0%B3%D1%80%D0%B8%D0%BF%D0% BF.pdf
rnmot.ru/public/uploads/RNMOT/clinical/2021/%D0%9A%D0%A0%20%D0%B3%D1%80%D0%B8%D0%BF%D0% BF.pdf
About the product Download instructions
when you can and when you can not take medicine
During the epidemic of colds, everyone is in a hurry to stock up on antibiotics. However, if used incorrectly, they can be harmful to health. In the article, we understand whether antibiotics are needed for colds, why they are prescribed for ARVI and other viral infections, and why self-medication is dangerous.
How antibiotics work
Antibiotics are antibacterial drugs. They affect the metabolic processes of bacteria and disrupt protein synthesis. This prevents reproduction and stops the growth of the colony (bacteriostatic effect) or leads to the death of the pathogenic microbe (bactericidal effect).
Does an antibiotic help with a cold
In medicine, the common cold most often means SARS - respiratory diseases that are caused by viruses. Pathogenic viruses are fundamentally different from bacteria, fungi and other microorganisms. This is a cell-free entity that is not able to carry out metabolism and reproduce on its own.
Pathogenic viruses are fundamentally different from bacteria, fungi and other microorganisms. This is a cell-free entity that is not able to carry out metabolism and reproduce on its own.
The virus is an absolute parasite: it uses host cells for all life processes. Outside a living organism, it is a collection of crystals consisting of protein molecules, which does not show signs of vital activity. And when the viral part (virion) is introduced into a living cell, it begins to replicate, that is, to reproduce many of its own copies.
Since the virus does not synthesize protein on its own, the antibiotic has no effect on it. Therefore, it is useless to use antibacterial drugs for an uncomplicated viral infection. In such cases, antiviral agents are effective - their active substances prevent the penetration of the virus into the cell and replication.
When to take antibiotics
If antibiotics do not help against viruses, why do doctors prescribe them? Such an appointment is justified if:
● A cold has a bacterial nature, for example, a patient has streptococcal tonsillitis 1 .
● Both viruses and bacteria are involved in the infection at the same time - this is called a mixed infection.
● A bacterial infection joins the disease caused by a virus. This process is called superinfection. The protective barrier of the affected tissues is weakened, and they become vulnerable even to opportunistic microbes that are safe for a healthy person. This is a common complication of the common cold - it develops in the range of 4-66% 2 cases.
To accurately determine the pathogen, it is necessary to conduct laboratory tests - PCR analysis and bacteriological culture . But they take time to carry out, and treatment is usually needed now. Therefore, patients with mild ARVI are prescribed antiviral drugs and local antiseptics that act on all microbes, without analysis.
According to the new clinical guidelines of the Ministry of Health of the Russian Federation 3 , published in February 2022, the priority group of drugs for the treatment of acute respiratory viral infections are direct antiviral drugs aimed at the cause of the disease. A new drug of this type is enisamia iodide (Nobazit, Nobazit Forte). The active substance - enisamia iodide - blocks the penetration of the virus into the cell and limits its spread in the body 4 . The results of clinical studies have shown that taking Nobazit reduces the number of complications requiring antibiotic therapy by 4 times. It also reduces the risk of infection spreading to the lower respiratory tract 5 .
A new drug of this type is enisamia iodide (Nobazit, Nobazit Forte). The active substance - enisamia iodide - blocks the penetration of the virus into the cell and limits its spread in the body 4 . The results of clinical studies have shown that taking Nobazit reduces the number of complications requiring antibiotic therapy by 4 times. It also reduces the risk of infection spreading to the lower respiratory tract 5 .
If the patient has purulent discharge or the condition has improved, and then worsened again, then antibacterial agents will be useful. Without analysis, only local forms of antibiotics can be used - as part of nasal drops, sprays.
According to the clinical recommendations of the Ministry of Health, antibiotics for ARVI systemically (in the form of tablets, suspensions, injections) are prescribed only in the following cases :
● The development of acute tonsillitis against the background of a severe or moderate cold.
● Attachment of sinusitis, laryngitis, tracheitis, bronchitis. If the infection is mild, then even if it spreads beyond the upper respiratory tract, it is not recommended to use antibiotics earlier than 10–14 days.
● Development of pneumonia.
In all these cases, it is recommended to first refer the patient for analysis in order to confirm a bacterial infection and select the most effective antibiotic 3 .
What antibiotics to drink for SARS
An antibacterial agent for ARVI is prescribed by a general practitioner, otolaryngologist, pulmonologist. It is better to choose a drug according to the results of the analysis. The best way to find out which antibiotic the causative agent of the infection is most sensitive to is to do a bacteriological culture. The disadvantage of this analysis is a long wait: usually the results are ready only after 3-7 days. PCR is prepared much faster - from 24 hours, but the analysis does not show the sensitivity of a particular infectious agent to drugs.
If it is impossible to perform the analysis or there is no time to wait for the results for a long time, the doctor will prescribe an antibiotic, focusing on the most likely pathogens for a given localization of the infection.
Groups of antibiotics that are most often used for ARVI 6 :
● Semi-synthetic penicillins. For mild acute bacterial infections, amoxicillin is used, for moderate and chronic forms, amoxicillin / clavulanate.
● III-IV generation cephalosporins - ceftriaxone, ceftazidime, cefoperazone, cefepime - are used for chronic moderate and purulent infections.
● Macrolides - azithromycin, clarithromycin. They are used for allergies to penicillins.
● III-IV generation fluoroquinolones - levofloxacin, moxifloxacin. They replace antibiotics of the penicillin group in case of inefficiency.
Most drugs are available in the form of tablets (capsules), powders for suspension and injections. In outpatient practice, tablets and suspensions are more often used.
In outpatient practice, tablets and suspensions are more often used.
Why self-treatment is dangerous
Inappropriate antibiotic treatment can be harmful to health:
● Uncontrolled use of antibiotics increases the resistance of pathogenic microbes to them. If you abuse them for minor infections, they will most likely not help if you have a serious illness.
● Antibiotics often cause allergic reactions up to Quincke's edema.
● A drug that you take without the knowledge of a doctor, in combination with medicines prescribed by a doctor, may give unpredictable results.
● Antibacterial drugs also kill the beneficial microflora of the body, which can lead to digestive disorders and gynecological inflammation.
● An additional unnecessary drug increases the load on the body and delays recovery.
Historical reference
In the middle of the twentieth century, antibiotics made a real revolution in medicine. Translated from Greek, their name means “against life” (“anti” and “bios”), but they only destroy bacteria. During the history of their existence, they have saved millions of new human lives.
Translated from Greek, their name means “against life” (“anti” and “bios”), but they only destroy bacteria. During the history of their existence, they have saved millions of new human lives.
Thanks to antibiotics, people:
● Significantly reduced maternal and child mortality rates in obstetrics, and later successfully introduced assisted reproductive technologies (IVF and others).
● We were able to cure previously incurable fatal and crippling diseases: tuberculosis, leprosy, syphilis and others.
● Learned how to perform the most complex operations without the fear of getting almost inevitable purulent-inflammatory complications.
Introduction of the first antibacterial drugs
Scottish bacteriologist Alexander Fleming is considered the "father" of antibiotics. During the experiments, he noticed: if you place different cultures of microbes next to each other, some begin to actively destroy others. In particular, fungi Penicillium notatum , which accidentally got into a Petri dish with cultures of staphylococci and streptococci, stopped the growth of these harmful bacteria.
The scientist undertook to investigate the mold and in 1929 isolated the first antimicrobial substance from it - penicillin . Animal experiments have shown promising results. Fleming's assistant, who fell ill with purulent sinusitis, voluntarily tested the drug on himself and quickly felt a significant improvement in well-being. However, the scientist failed to develop technologies for the industrial production of the antibiotic.
This was done by the pathologist Howard Florey and the biochemist Ernst Chain. In early 1941, Flory managed to interest industrialists and the US government in the production of a new drug. By the end of 1942, the first large batch was released, marking the beginning of the era of antibiotics. After another 10 years, these drugs became available everywhere, thanks to a significant reduction in the cost of technology and the launch of new production facilities.
The world praised the merits of scientists: in 1945, Fleming, Flory and Chain were awarded the Nobel Prize for the discovery of penicillin and its therapeutic effect against infections. At 19In 1952, the Nobel Prize for the discovery of the anti-tuberculosis antibiotic streptomycin was received by an American microbiologist (formerly our compatriot) Zelman Waksman. 7
At 19In 1952, the Nobel Prize for the discovery of the anti-tuberculosis antibiotic streptomycin was received by an American microbiologist (formerly our compatriot) Zelman Waksman. 7
Modern realities
Today in Russia, about 30 groups of antibiotics are actively used, which include drugs of different origin:
● Natural (biosynthetic) - Derived from fungi or bacteria that are resistant to antibiotics.
● Semi-synthetic - natural substances modified by an enzymatic or chemical method. Such drugs are more effective.
● Synthetic - created artificially in the laboratory.
There are broad-spectrum antibiotics that act on many types of bacteria, and narrow-spectrum antibiotics that selectively destroy a small group of them. Until recently, they worked almost flawlessly. Now a serious global problem is antibiotic resistance - the resistance of microorganisms to drugs. Bacteria, like any living organism, learn to adapt to adverse conditions. 8.9
8.9
Briefly about the main
➢ Antibiotics are antimicrobials that help fight bacterial infections.
➢ Antibacterial drugs are ineffective for any viral infection, including SARS.
➢ Antimicrobial drugs are connected to the treatment of acute respiratory viral infections if a bacterial infection is present along with a viral infection. She can join later.
➢ Take antibiotics only as directed by your doctor. Self-medication leads to unwanted side effects and increases the resistance of microbes to the drug.
1 Maltseva G.S., Grinchuk O.N., Place of antibiotic therapy for streptococcal infection // Medical Council - 2019.
2 Sviryaeva E.N., Korneev K.V., Drutskaya M.S., Kuprash D.V. Mechanisms of restructuring the immune response in viral-bacterial coinfections of the respiratory tract // Biochemistry - V. 81, No. 11, 2016.
3 Clinical guidelines of the Ministry of Health of the Russian Federation: Acute respiratory viral infections (ARVI) in adults
4 Instructions for medical use (Nobasit®, film-coated tablets 250 mg; RU: LP-003508 of 03/16/2016)
5 Lioznov D.