Manic behavior icd 10
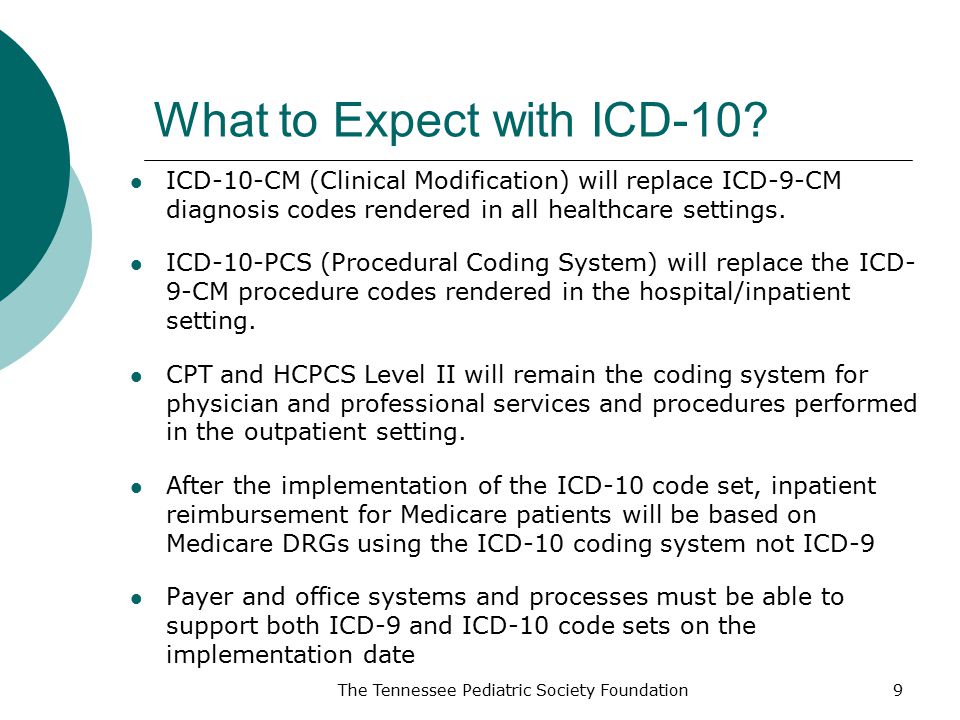
2023 ICD-10-CM Diagnosis Code F30.9: Manic episode, unspecified
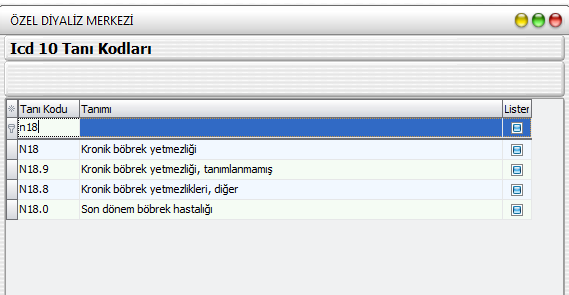
- ICD-10-CM Codes ›
- F01-F99 Mental, Behavioral and Neurodevelopmental disorders ›
- F30-F39 Mood [affective] disorders ›
- F30- Manic episode ›
- 2023 ICD-10-CM Diagnosis Code F30.9
Manic episode, unspecified
- 2016 2017 2018 2019 2020 2021 2022 2023 Billable/Specific Code
- F30.9 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
- The 2023 edition of ICD-10-CM F30.9 became effective on October 1, 2022.
- This is the American ICD-10-CM version of F30.9 - other international versions of ICD-10 F30.
9 may differ.
Applicable To
- Mania NOS
The following code(s) above F30.9 contain annotation back-references
Annotation Back-References
In this context, annotation back-references refer to codes that contain:
- Applicable To annotations, or
- Code Also annotations, or
- Code First annotations, or
- Excludes1 annotations, or
- Excludes2 annotations, or
- Includes annotations, or
- Note annotations, or
- Use Additional annotations
that may be applicable to F30.9:
- F01-F99
2023 ICD-10-CM Range F01-F99
Mental, Behavioral and Neurodevelopmental disorders
Includes
- disorders of psychological development
Type 2 Excludes
- symptoms, signs and abnormal clinical laboratory findings, not elsewhere classified (R00-R99)
- F30
ICD-10-CM Diagnosis Code F30
Manic episode
- 2016 2017 2018 2019 2020 2021 2022 2023 Non-Billable/Non-Specific Code
Includes
- bipolar disorder, single manic episode
- mixed affective episode
Type 1 Excludes
- bipolar disorder (F31.
 -)
-) - major depressive disorder, single episode (F32.-)
- major depressive disorder, recurrent (F33.-)
Approximate Synonyms
- Bipolar 1 disorder, single manic episode
- Bipolar i disorder, single manic episode
- Mania
- Mood disorder of manic type
- Mood disorder w manic features
- Mood disorder with manic feature
Clinical Information
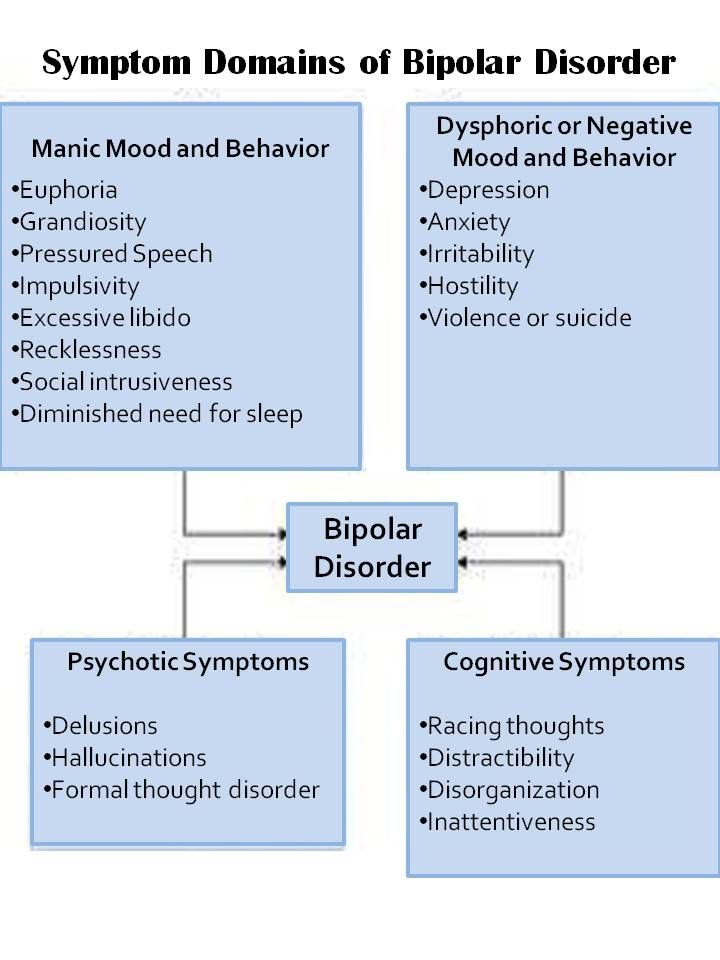
- A disorder characterized by excitement of psychotic proportions manifested by mental and physical hyperactivity, disorganization of behavior and elevation of mood.
- Excitement of psychotic proportions manifested by mental and physical hyperactivity, disorganisation of behaviour and elevation of mood. (on-line medical dictionary)
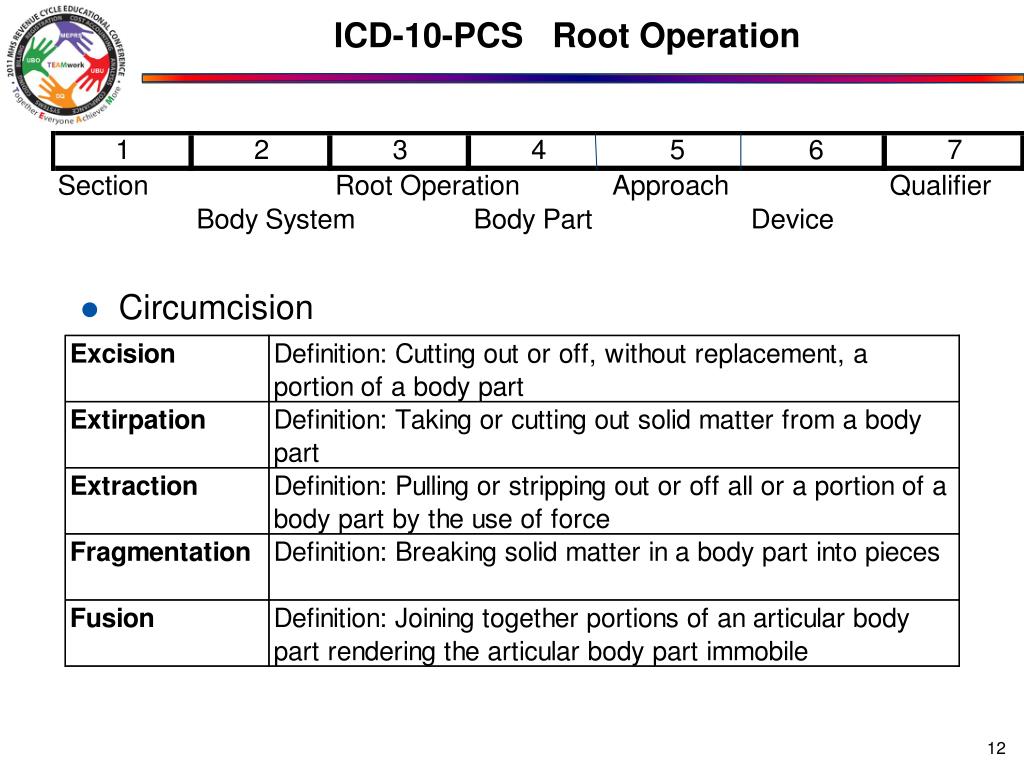
ICD-10-CM F30. 9 is grouped within Diagnostic Related Group(s) (MS-DRG v40.0):
9 is grouped within Diagnostic Related Group(s) (MS-DRG v40.0):
- 885 Psychoses
Convert F30.9 to ICD-9-CM
Code History
- 2016 (effective 10/1/2015): New code (first year of non-draft ICD-10-CM)
- 2017 (effective 10/1/2016): No change
- 2018 (effective 10/1/2017): No change
- 2019 (effective 10/1/2018): No change
- 2020 (effective 10/1/2019): No change
- 2021 (effective 10/1/2020): No change
- 2022 (effective 10/1/2021): No change
- 2023 (effective 10/1/2022): No change
Diagnosis Index entries containing back-references to F30.9:
ICD-10-CM Codes Adjacent To F30. 9
9
F30 Manic episode
F30.1 Manic episode without psychotic symptoms
F30.10 …… unspecified
F30.11 …… mild
F30.12 …… moderate
F30. 13 Manic episode, severe, without psychotic symptoms
13 Manic episode, severe, without psychotic symptoms
F30.2 Manic episode, severe with psychotic symptoms
F30.3 Manic episode in partial remission
F30.4 Manic episode in full remission
F30.8 Other manic episodes
F30. 9
Manic episode, unspecified
9
Manic episode, unspecified
F31 Bipolar disorder
F31.0 Bipolar disorder, current episode hypomanic
F31.1 Bipolar disorder, current episode manic without psychotic features
F31.10 …… unspecified
F31. 11 …… mild
11 …… mild
F31.12 …… moderate
F31.13 …… severe
F31.2 Bipolar disorder, current episode manic severe with psychotic features
F31.3 Bipolar disorder, current episode depressed, mild or moderate severity
F31. 30 …… unspecified
30 …… unspecified
Reimbursement claims with a date of service on or after October 1, 2015 require the use of ICD-10-CM codes.
2023 ICD-10-CM Diagnosis Code F30.8: Other manic episodes
- ICD-10-CM Codes ›
- F01-F99 Mental, Behavioral and Neurodevelopmental disorders ›
- F30-F39 Mood [affective] disorders ›
- F30- Manic episode ›
- 2023 ICD-10-CM Diagnosis Code F30.8
Other manic episodes
- 2016 2017 2018 2019 2020 2021 2022 2023 Billable/Specific Code
- F30.8 is a billable/specific ICD-10-CM code that can be used to indicate a diagnosis for reimbursement purposes.
- The 2023 edition of ICD-10-CM F30.
 8 became effective on October 1, 2022.
8 became effective on October 1, 2022. - This is the American ICD-10-CM version of F30.8 - other international versions of ICD-10 F30.8 may differ.
Applicable To
- Hypomania
The following code(s) above F30.8 contain annotation back-references
Annotation Back-References
In this context, annotation back-references refer to codes that contain:
- Applicable To annotations, or
- Code Also annotations, or
- Code First annotations, or
- Excludes1 annotations, or
- Excludes2 annotations, or
- Includes annotations, or
- Note annotations, or
- Use Additional annotations
that may be applicable to F30.8:
- F01-F99
2023 ICD-10-CM Range F01-F99
Mental, Behavioral and Neurodevelopmental disorders
Includes
- disorders of psychological development
Type 2 Excludes
- symptoms, signs and abnormal clinical laboratory findings, not elsewhere classified (R00-R99)
- F30
ICD-10-CM Diagnosis Code F30
Manic episode
- 2016 2017 2018 2019 2020 2021 2022 2023 Non-Billable/Non-Specific Code
Includes
- bipolar disorder, single manic episode
- mixed affective episode
Type 1 Excludes
- bipolar disorder (F31.
 -)
-) - major depressive disorder, single episode (F32.-)
- major depressive disorder, recurrent (F33.-)
Approximate Synonyms
- Atypical mania
- Atypical manic disorder
- Hypomania
- Manic disorder, atypical
Clinical Information
- A less severe form of mania characterized by elevated mood, hyperactivity, and grandiosity. In contrast to mania, these symptoms do not cause significant impairment of the individual's productivity at work, or social and family relationships.
- Mild form of mania.
ICD-10-CM F30.8 is grouped within Diagnostic Related Group(s) (MS-DRG v40.0):
- 885 Psychoses
Convert F30. 8 to ICD-9-CM
8 to ICD-9-CM
Code History
- 2016 (effective 10/1/2015): New code (first year of non-draft ICD-10-CM)
- 2017 (effective 10/1/2016): No change
- 2018 (effective 10/1/2017): No change
- 2019 (effective 10/1/2018): No change
- 2020 (effective 10/1/2019): No change
- 2021 (effective 10/1/2020): No change
- 2022 (effective 10/1/2021): No change
- 2023 (effective 10/1/2022): No change
Diagnosis Index entries containing back-references to F30.8:
- Bell's
- mania F30.8
- Disorder (of) - see also Disease
- mood F39
ICD-10-CM Diagnosis Code F39
Unspecified mood [affective] disorder
- 2016 2017 2018 2019 2020 2021 2022 2023 Billable/Specific Code
Applicable To
- Affective psychosis NOS
- mood F39
- Episode
- Excitation
- psychogenic F30.
 8
8 - reactive F30.8 (from emotional stress, psychological trauma)
- psychogenic F30.
- Excitement
- hypomanic F30.8
- mental, reactive F30.8 (from emotional stress, psychological trauma)
- state, reactive F30.8 (from emotional stress, psychological trauma)
- Hypomania, hypomanic reaction F30.8
- Mania (monopolar) - see also Disorder, mood, manic episode
- Bell's F30.8
- puerperal F30.8
- Psychosis, psychotic F29
ICD-10-CM Diagnosis Code F29
Unspecified psychosis not due to a substance or known physiological condition
- 2016 2017 2018 2019 2020 2021 2022 2023 Billable/Specific Code
Applicable To
- Psychosis NOS
- Unspecified schizophrenia spectrum and other psychotic disorder
Type 1 Excludes
- mental disorder NOS (F99)
- unspecified mental disorder due to known physiological condition (F09)
- Puerperal, puerperium (complicated by, complications)
- mania F30.
 8
8
- mania F30.
- Reaction - see also Disorder
- hypomanic F30.8
ICD-10-CM Codes Adjacent To F30.8
F29 Unspecified psychosis not due to a substance or known physiological condition
F30 Manic episode
F30.1 Manic episode without psychotic symptoms
F30.10 …… unspecified
F30. 11 …… mild
11 …… mild
F30.12 …… moderate
F30.13 Manic episode, severe, without psychotic symptoms
F30.2 Manic episode, severe with psychotic symptoms
F30.3 Manic episode in partial remission
F30. 4 Manic episode in full remission
4 Manic episode in full remission
F30.8 Other manic episodes
F30.9 Manic episode, unspecified
F31 Bipolar disorder
F31.0 Bipolar disorder, current episode hypomanic
F31. 1 Bipolar disorder, current episode manic without psychotic features
1 Bipolar disorder, current episode manic without psychotic features
F31.10 …… unspecified
F31.11 …… mild
F31.12 …… moderate
F31.13 …… severe
F31. 2 Bipolar disorder, current episode manic severe with psychotic features
2 Bipolar disorder, current episode manic severe with psychotic features
F31.3 Bipolar disorder, current episode depressed, mild or moderate severity
Reimbursement claims with a date of service on or after October 1, 2015 require the use of ICD-10-CM codes.
Manic disorder - Mania signs, classification, treatment
It is impossible to say that borderline personality disorder affects a certain layer of society. It affects both men and women, and adults, and children. It needs to be diagnosed in time, because the statistics of this disease are depressing - 1 out of 10 patients with this disorder commits suicide.
What is borderline personality disorder?
Borderline Personality Disorder (BPD) is a mental disorder in which a person is characterized by emotional instability and low self-control. A patient with this diagnosis is inherent in the fear of loneliness, at the same time he is absolutely not social - it is difficult for him to establish relationships with people, he is afraid of being misunderstood and rejected.
A patient with this diagnosis is inherent in the fear of loneliness, at the same time he is absolutely not social - it is difficult for him to establish relationships with people, he is afraid of being misunderstood and rejected.
In general, abnormal behavior in BPD can be confused with another disorder, but this disease is distinguished by the fact that all the negative emotions of a person are directed at themselves. He does not seek to harm the people around him - they simply scare him. But he also cannot be left alone with himself.
Borderline disorder can be recognized by a non-standard attitude to the outside world: a person is overly impulsive, any failure, even the smallest one, will be perceived as a huge tragedy. For example, a person with BPD who is a couple of minutes late for a meeting will not be able to behave calmly at the event itself - he will be nervous and blame himself for ruining everything. Although, in fact, this is not the case.
The instability of emotions is also inherent in these people - nervousness is felt in all actions, they can react emphatically cheerfully to some positive events, but the reaction is very similar to a simulated one. Negative emotions are also experienced very sharply, others may think that a person with BPD is trying to attract attention to himself.
Negative emotions are also experienced very sharply, others may think that a person with BPD is trying to attract attention to himself.
Always side by side with borderline personality disorder is social maladaptation. People with BPD are very dependent on the opinions of others, they blame themselves for all the troubles, so at some point it becomes easier for them to protect themselves from society, but they cannot be alone either, so a personal collapse occurs. In general, the "border guard" in any society is bored, he cannot find a place for himself in a noisy company.
BPD divides the sufferer's personality in two - constant fluctuations between self-hatred and excessive idealization also distinguish people with this disorder.
According to ICD-10, borderline personality disorder is a subspecies of emotionally unstable personality disorder. The diagnosis is officially recognized by psychiatrists all over the world. Although, a few decades ago, he was stigmatized both in the world of psychiatry and in society. Today the situation has changed, and the attitude towards BPD has become much more conscious and attentive.
Today the situation has changed, and the attitude towards BPD has become much more conscious and attentive.
The term appeared thanks to a group of American psychologists who conducted research in 1968-1980. The result of these works was the recognition of BPD as a separate mental disorder. And borderline personality disorder in the ICD-10 was included by experts.
Any patient with this disorder is very sensitive in relation to other people - he is sensitive to any fluctuations in society, worries about what opinion others build towards him. Due to frequent lifestyle changes and emotional swings, people with BPD feel insecure in life. Often, thinking about their lives, they are overwhelmed with despair, which in most cases leads to depression. It is difficult for people with this disorder to choose their own life path. They are characterized by uncertainty about their personality, which has no core.
Borderline mental personality disorder generates high impulsiveness in a person. This leads to behavior that causes great damage to the patient: many dabble in gambling, may become addicted to alcohol or drugs, become prone to eating disorders, and commit theft. BPD can take many forms. It is characterized by instability, strong and sudden changes in feelings, mood, relationships, self-image and behavior. A person's impulsivity is expressed in affective instability and can manifest itself in at least two areas that, for a person with a borderline mental disorder, are potentially self-damaging: spending money, sex, drug addiction, theft, reckless driving, carousing.
This leads to behavior that causes great damage to the patient: many dabble in gambling, may become addicted to alcohol or drugs, become prone to eating disorders, and commit theft. BPD can take many forms. It is characterized by instability, strong and sudden changes in feelings, mood, relationships, self-image and behavior. A person's impulsivity is expressed in affective instability and can manifest itself in at least two areas that, for a person with a borderline mental disorder, are potentially self-damaging: spending money, sex, drug addiction, theft, reckless driving, carousing.
It is wrong to assume that people with BPD manipulate loved ones with whims and threats of suicide. They thus express their lack of additional support and acceptance. They do not behave this way on purpose, they do not deliberately try to attract attention, to get some kind of benefit. Most often, they try to eradicate these feelings in themselves so that others do not consider such behavior demonstrative.
Borderline personality disorder (ICD code for it with the letter F) causes a person to oscillate between two extremes - "everything is very good" or "everything is very bad." That is how they feel about themselves. Therefore, one of the main researchers of this disorder, A. Stern, introduced the term "narcissism" - this is the idealization that occurs in a person with BPD in the stage of self-love. The scientist also appeals to the concept of "mental bleeding". It correlates with impotence in crisis situations, implies a tendency to compliance.
Borderline disorder, in simple terms, is a mental illness that can take many forms. It is characterized by instability, strong and sudden changes in feelings, mood, relationships, self-image and behavior.
BPD is characterized by recurrent suicidal thoughts in the patient, attempts to injure and mutilate oneself (cuts, cauterization), frequent emotional overreactions, or abrupt mood swings, including depression, irritability, or anxiety. These shifts usually last for several hours, and in some cases from 1 to 2 days. Borderline mental disorders give rise to a feeling of emptiness in a person. Sometimes paranoia can appear - suspicion of other people and a sense of loss of reality.
These shifts usually last for several hours, and in some cases from 1 to 2 days. Borderline mental disorders give rise to a feeling of emptiness in a person. Sometimes paranoia can appear - suspicion of other people and a sense of loss of reality.
The disorder can occur most often in adulthood, statistics indicate a border between 17 and 25 years of age. The first signs of BPD may appear as early as childhood. Due to the fact that the psyche of children has not yet been formed, this disorder is diagnosed not in childhood, but in adolescence.
To fully appreciate the severity of the disease, it would be appropriate to give statistics on the connection between suicide and BPD:
- A third of all suicides are committed by people with borderline psychological disorders.
- The lifetime risk of suicide for people with BPD is as high as 10%.
- The greatest risk of suicide in violation is at a young age (15-30 years).
- Suicide in the disorder can have a particular burden on others: 44% of BPD suicides are committed in the presence of other people, compared with 17% for people with other diagnoses.
The disorder is difficult to diagnose because it can manifest itself in many forms that are often difficult to compare.
The general classification of all types of this type of disorder is as follows:
- The dominant affect is anger.
- Inability to build interpersonal relationships.
- Self rejection.
- One of the main manifestations is depression.
The essence of borderline personality disorder lies in the fact that a person experiences great difficulties with self-identification. This leaves an imprint on his relationship with other people, self-acceptance and creates significant problems in many areas of life.
Symptoms of borderline disorder
The comparison by US psychologist M. Lainen is very true - she said that people with BPD do not have “emotional skin”. And this statement perfectly describes all the symptoms of borderline disorder in the aggregate.
A person can be suspected of having BPD if four or more signs of the disease can be traced in his behavior. It is very important that impulsiveness is clearly expressed. It is also worth watching for stability - if the symptoms make themselves felt every day, then you need to see a specialist.
It is very important that impulsiveness is clearly expressed. It is also worth watching for stability - if the symptoms make themselves felt every day, then you need to see a specialist.
Every potential patient with BPD will experience dramatic emotional swings and mood swings. This is called lability. For example, when a fit of anger and uncontrolled aggression changes dramatically with regret and remorse for one's behavior.
Symptoms of borderline personality disorder:
- Emotional instability, significant mood reactivity.
- Unstable and tense interpersonal relationships with everyone around.
- Impulsiveness.
- Attempts to avoid the real or imagined possibility of being neglected by loved ones.
- Suicidal thoughts and conversations, even attempts are possible, which are repeated from time to time.
- Aggression, hostility.
- Violation of the mental identity of the individual.
- Chronic feeling of spiritual emptiness.
- Transient paranoid ideas associated with stress.
Symptoms and signs of borderline personality disorder also include a pronounced and persistent identity disorder, which manifests itself in insecurity in at least two of the following:
- values;
- sexual orientation;
- ranking friends by preference;
- self-esteem and self-image;
- setting long-term goals.
A person with BPD may be self-limiting, deliberately beating himself up and worrying about his diagnosis. It will seem to him that he is not like everyone else, that the presence of a disease makes him different, special, but this feature has a negative connotation.
The signs of borderline disorder always take on the color of hyperbole - if a person is sad, then this sadness borders on depression, if he is happy, then he does it too emotionally, and negative events can cause aggression.
Why Borderline Disorder Occurs
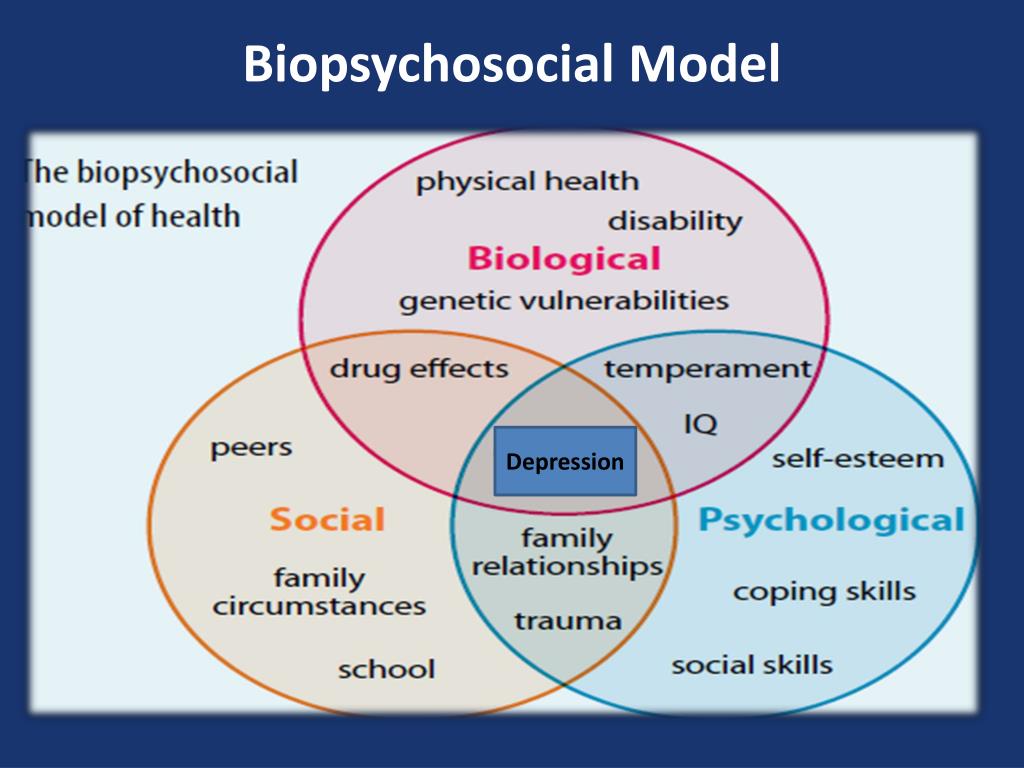
The psychiatric community believes that a person must have certain prerequisites for the development of BPD. That is, it is a disease that occurs as a result of the action of a number of factors.
That is, it is a disease that occurs as a result of the action of a number of factors.
The causes of borderline personality disorder can be different:
- Violation of identity - persistent hostility to one's image, rejection of it.
- The tendency to engage in unstable and polar relationships with people is the idealization of a person or, conversely, his depreciation.
- Impulsivity, which manifests itself in a number of areas and involves self-harm - in addition to suicide, it can be unprotected sex, drug use, overeating.
- Character traits - low self-esteem, increased anxiety, a tendency to pessimistic forecasts, low resistance to stress.
These prerequisites relate rather to the characteristics of the character or type of personality of a person, but there are causes of borderline disorder that do not depend on personality factors:
- genetic predisposition.
- Gender affiliation. Women suffer from BPD more often than men.
People at risk are advised to visit a psychologist periodically in order to prevent the development of BPD and establish a painless connection with the outside world.
Disease pathogenesis
This disease, like many other mental disorders, is considered not fully understood. But one thing is for sure - there is a connection between borderline disorder syndrome and emotional trauma in childhood. This point of view is shared by most researchers. Therefore, less attention is paid to the factors of neurobiology, dysfunction of brain regions and social causes (the influence of the environment in the process of growing up, building communication and interaction with various social groups).
The state of borderline disorder occurs because the amygdala, which is responsible for generating ideas, increases in volume. This provokes an increased manifestation of various states - a person is sad, happy and angry much brighter and more actively than people without a violation.
In the prefrontal cortex, in contrast, there is a decrease in activity during the disorder. It is most concentrated in the right anterior gyrus. This is due to the inability of the "border guards" to regulate their emotions, to stop them. It is the cortex that regulates the degree of arousal, and in the case of BPD, it is less involved. The level of cortisol, which is produced by the hypothalamus, also has a direct effect. This hormone is marked by an overestimated level of indicators in BPD, it provokes increased activity of the hypothalamic-pituitary-adrenal axis, which enters into a state of activity. As a result, there is an increased reaction to stress, and vulnerability to external factors appears.
Stages of borderline disorder
If you do not deal with the treatment of a mental disorder, then it will be aggravated. It is important to identify the symptoms of the disease as soon as possible and consult a doctor. If this is not done, then the signs of a violation will dominate the behavior of a person, he will increasingly move away from his relatives and society, he will begin to develop suicidal tendencies.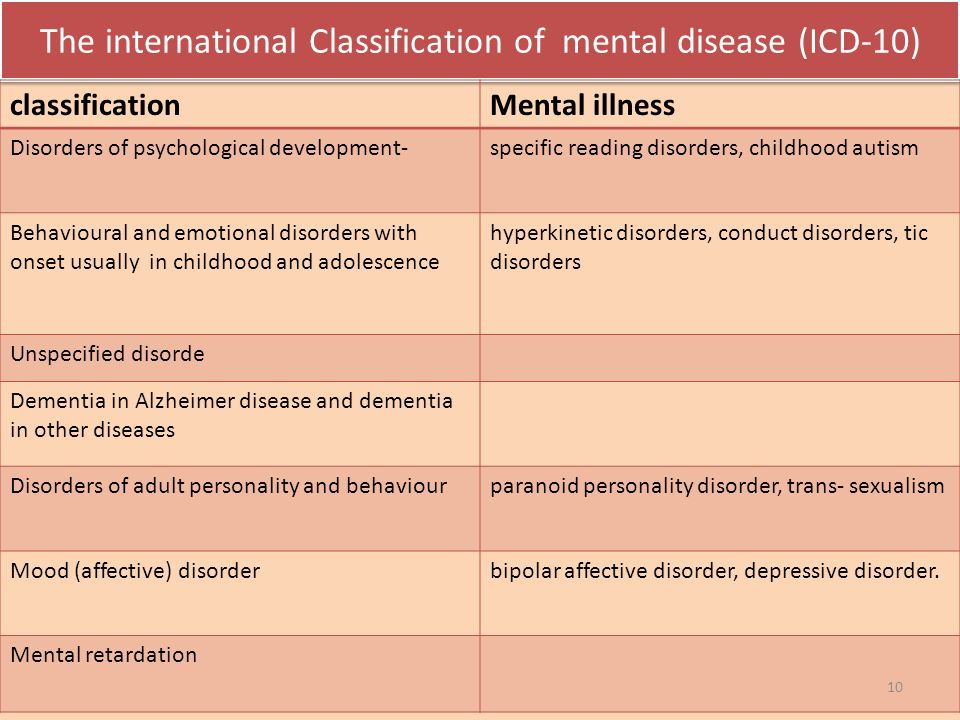
Once an indicator of borderline personality disorder is identified, the disease proceeds according to the following stages:
- interpersonal instability. At this stage, a person tries to avoid abandonment, tries to seem normal, build social relationships, although this is not easy for him. This stage is also marked by the instability of relations - it is difficult for others to understand the "border guard".
- Cognitive disorders, identity disorders. Signs of paranoia begin to appear, a person's idea of himself and his place in the world around him is disturbed.
- Violations of effective and emotional regulation. This is an indicator of borderline disorder of a more severe stage. There is mood instability, unreasonable anger, an inner feeling of emptiness.
- Dysregulation of behavior - the last stage is marked by suicidal tendencies, the desire to injure oneself, uncontrolled emotional outbursts.
How can the disorder be classified
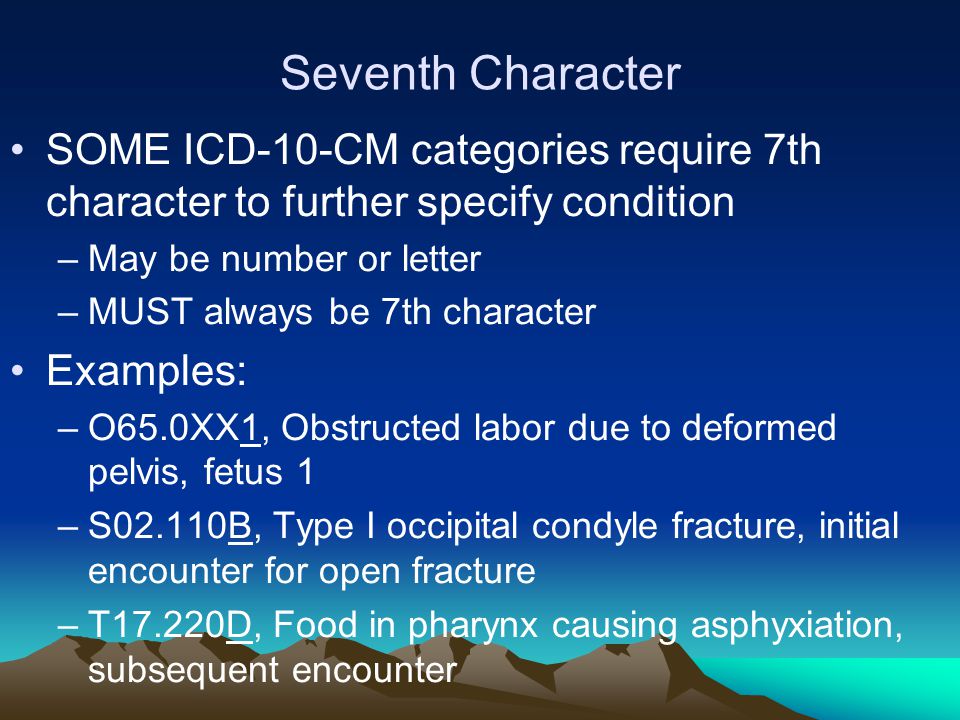
First of all, a classification was adopted in accordance with ICD-10:
- F4 - Neurotic disorders associated with stress and somatoform disorders.
- F5 - Behavioral syndromes associated with physiological disorders and physical factors
- F6 - Personality and behavioral disorders in adulthood.
The types of borderline disorder can be divided into 4 subgroups. They are arranged in order of severity, starting with the least:
- Sad borderline disorder. It is characterized by submissive and compliant behavior. A person behaves very modestly, but inside he experiences helplessness, self-pity, a sense of his own worthlessness. Along with this, there is physical fatigue, unwillingness to do anything.
- Touchy PR. The person is not as malleable as in the dull type. He can express negativity, take everything with hostility. The main distinguishing feature is resentment. A patient with this type is quickly disappointed in everything and everyone.
- Impulsive PR. This is a type of borderline personality disorder in which a person with a disorder is naughty, shows hysterical inclinations, and demonstrates infantilism.
 He is characterized by unreasonable excitement, inability to concentrate, suicidal manifestations are possible.
He is characterized by unreasonable excitement, inability to concentrate, suicidal manifestations are possible. - Self-damaging PR. The most severe of the four subtypes. A person is suicidal and no longer hides his thoughts. He has a clear craving for self-destruction, inflicting damage on himself. In relation to others, he behaves ingratiatingly, but at the same time closed.
Levels of borderline personality disorder can vary and are classified according to severity. There are three in total:
- Easy, when non-standard human behavior is not yet clearly distinguishable. There are difficulties in building relationships with society. And yet the ability to maintain adequate contact is not completely lost. With a mild form, the "border guard" does not express a desire to injure himself or harm others.
- Average, when relationships with relatives and friends become more difficult. A person with a disability transfers these problems to other areas - he believes that everything in his career is compromised against him.
 In this form of borderline, there are threats of ending their lives, but they usually do not come to fruition.
In this form of borderline, there are threats of ending their lives, but they usually do not come to fruition. - Severe, when self-rejection is reflected in absolutely all areas of life, a person feels not accepted by society, ceases to function and try to establish relationships with other people. He is completely immersed in himself, blaming himself for all the failures. There is a high probability of causing bodily harm to yourself. Often it can lead to suicide.
The disease is not divided into gender and age groups. It can be said that borderline disorder is more common in women than in men. But there is no difference in approaches and treatment - a patient of either gender will undergo therapy in accordance with the severity. It is important to pay attention to the type of BPD, the person's genetics, lifestyle and personality characteristics.
What are the possible complications
First of all, the complications of the disease are associated with destructive behavior - the patient, unwittingly, causes negative emotions in those around him, attempts to harm himself begin to appear. During this period, the manifestation of alcohol, drug addiction is possible, which negatively affects the overall health of the body. All organs and systems suffer, great damage is done to the psyche.
During this period, the manifestation of alcohol, drug addiction is possible, which negatively affects the overall health of the body. All organs and systems suffer, great damage is done to the psyche.
A person with BPD may be prone to overeating - hence the violations of the gastrointestinal tract and the corresponding mental disorders (bulimia, anorexia). Attempts to bring yourself physical harm turn into wounds, cuts, burns. During aggression, the patient can harm strangers, although cases of physical harm are very rare - the "border guard" mostly experiences aggression on his own, injuring himself or suffering from internal contradictions.
The worst thing that BPD can turn into is death. Indeed, according to statistics, about 70% of people with this disorder have made at least one suicidal attempt. These attempts can end in failure - due to the deliberate demonstration of suicide or through negligence.
When to see a doctor
The slightest deviation from normal behavior is a reason to visit a specialist. If a person notices any symptoms of BPD, feels lonely, cannot cope with uncontrolled aggression or mood swings, then it is likely that he is diagnosed with borderline disorder.
If a person notices any symptoms of BPD, feels lonely, cannot cope with uncontrolled aggression or mood swings, then it is likely that he is diagnosed with borderline disorder.
It is also important to listen to close people who note changes in the usual state of a person.
Many people with a violation try to cope on their own, as soon as they notice the first signs of a disorder in themselves, but only a professional can provide competent help.
Diagnosis of disorder
How to define borderline disorder? To do this, the doctor fully examines the history and identifies the criteria for BPD:
- a devastating feeling of loneliness;
- sudden impulsivity;
- affective instability and sudden reactions to stressful situations;
- emerging paranoia or severe dissociative symptoms;
- inadequate, unjustified anger, inability to cope with it;
- suicidal thoughts, threats, desire to harm oneself;
- unstable interpersonal relationships;
- violation of one's own identity.
A psychiatrist uses an interview to diagnose borderline personality disorder. It would be useful to conduct an external examination - if scars or scars are found on the skin, then the person is already in the severe stage of BPD.
The generally accepted criteria for making a diagnosis are those set by the American Psychiatric Association.
- Violations that manifest themselves:
- in social functioning - close relationships become unstable, conflicts appear. A person with BPD considers himself abandoned and useless - this leaves an imprint on interaction with people. On the other hand, empathy appears: patients with this disorder are very sensitive and also relate to others, they express sincere sympathy in difficult situations;
- in a personal conflict - a person is characterized by excessive self-criticism, a feeling of instability and constant loneliness. There are no clear goals in life, the patient cannot focus on aspirations, he is removed from career plans.
- hostility to the outside world appears - the patient is irritated, experiences unreasonable anger;
- all emotions are colored negatively - a person is afraid of being rejected, constantly feels anxiety;
- a person is prone to impulsiveness, ready to take risks, and the patient does not think about the consequences of actions.
#PHONEHELP#
BPD treatment
The treatment of borderline disorder primarily takes into account the needs of the person with BPD, to a lesser extent, the doctor relies on generally accepted standards. If the patient has a tendency to depression or increased anxiety, then they resort to drug treatment.
The psychiatric community is more inclined towards outpatient treatment than hospitalization - it has not proven itself as a rational approach to solving this problem.
Currently, there are several approaches to the treatment of borderline disorder, the appropriateness of which in a particular case is determined by the psychotherapist:
- Transfer analysis. This is a type of psychotherapy for which a step-by-step recommendation has been developed that is used in the treatment of BPD.
- Scheme therapy. It combines Gestalt therapy, cognitive behavioral therapy, attachment theory and psychoanalysis. This type of psychotherapy for borderline personality disorder takes into account the patient's childhood, an analysis of the likelihood of traumatic events and abuse. The doctor in this case focuses on the source of experiences, teaches to find ways out and cope with anxiety.
- Dialectical-behavioral therapy. This is a long process that is used to relieve the symptoms of the disease, to save the patient from thoughts of suicide.
- mentalization. Can be done individually or as part of a group. In this technique, the main focus is the level of meaningfulness - a person learns to find the meaning of life, control their emotions and prioritize needs.
- Pharmacotherapy. Studies have proven that there are no effective medications for the treatment of BPD. There are no drugs that can relieve the feeling of emptiness. But the authors of scientific papers came to the conclusion that some drugs can act directionally, that is, get rid of the main symptoms of the disease. Among these drugs, Haloperidol (reduces aggression), Aripiprazole (relieves excessive impulsivity), Valproic acid salts (relieve manifestations of a depressive state) showed the greatest effectiveness.
Disease prevention
It is believed that you can get rid of the violation if you follow all the clinical recommendations for borderline personality disorder. It is not uncommon for patients to completely get rid of all the signs of BPD under the strict guidance of the attending physician.
To date, there are no ways that can prevent this mental disorder. Therefore, it is so important to take all measures to track the disease at an early stage and contact specialists.
References:
- McWilliams N., “Psychoanalytic diagnostics. Understanding Personality Structure in the Clinical Process”
- Ushakov G.K. Borderline neuropsychiatric disorders.-2nd edition-M., Medicine
- Kuzmenok G.F. Collection “Ways of Understanding. Collection of articles for the 15th anniversary of the Society for Psychoanalytic Psychotherapy” - about the combination of therapy and pharmacology.
- Gert Sauer Siberian Lectures on Analytical Psychology
- Churkin A.A., Martyushov A.N. Practical Guide to the Application of the ICD-10 in Psychiatry and Addiction
- Tiganov A.S. Manual of Psychiatry - M. Medicine
- Ukhanovsky A.O., Kutyavin Yu.A., Litvak M.E. General psychopathology
- A.V. Snezhnevsky - Clinical Psychiatry
ICD-10 - codes of diseases - Psychotherapist Sergei Melnikov
To read the contents of the section, click on the title. Clicking again will collapse the section.
Clicking again will collapse the section.
F00-F09 Organic, including symptomatic, psychiatric disorders
F00 Alzheimer's dementia
F00.0 Early-onset Alzheimer's dementia
F00.1 Late-onset Alzheimer's dementia
F00.2 Alzheimer's dementia, atypical or mixed
F00.9 Alzheimer's disease dementia, unspecified
F01 Vascular dementia
F01.0 Acute onset vascular dementia
F01.1 Multi-infarct dementia
F01.2 Subcortical vascular dementia
F01.3 Mixed cortical and subcortical vascular dementia
F01.8 Other vascular dementia
F01.9 Vascular dementia, unspecified
F02
F02.0 Dementia in Pick's disease
F02.1 Dementia in Creutzfeldt-Jakob disease
F02.2 Dementia in Huntington's disease
F02.3 Dementia in Parkinson's disease
F02.4 Dementia in diseases associated with human immunodeficiency virus (HIV)
F02. 8 Dementia in other specified diseases classified elsewhere
8 Dementia in other specified diseases classified elsewhere
F03 Dementia, unspecified
A fifth character may be used to specify dementia in F00-F03:
. x0 without additional symptoms
. x1 with other symptoms, mostly delusional
. x1 with other symptoms, mostly hallucinatory
. x3 with other symptoms, predominantly depressive
. x4 with other mixed symptoms. A sixth character can be used to indicate the severity of dementia:
. xx0 Light
. хх1 Moderate
. хх2 Severe
F04 Organic amnesic syndrome not caused by alcohol or other psychoactive substances
F05 Delirium not caused by alcohol or other psychoactive substances
F05.0 Delirium not associated with dementia
F05.1 Delirium occurring with dementia
F05.8 Other delirium
F05.9 Delirium, unspecified
F06 Other mental disorders due to damage or dysfunction of the brain, or due to physical disease
F06.0 Organic hallucinosis
F06. 1 Organic catatonic disorder
1 Organic catatonic disorder
F06.2 Organic delusional (schizophrenia-like) disorder
F06.3 Organic (affective) disorders
F06.4 Organic anxiety disorder
F06.5 Organic dissociative disorders
F06.5 Organic dissociative disorders 6 Organic emotionally labile (asthenic) disorders
F06.7 Mild cognitive impairment
F06.8 Other specified mental disorders due to damage and dysfunction of the brain and physical illness
F06.9 Unspecified mental disorders due to brain damage and dysfunction and physical disease
F07 Personality and behavioral disorders due to brain damage and dysfunction disease
F07.0 Organic personality disorder
F07.1 Postencephalic syndrome
F07.2 Postconcussion syndrome
F07.8 Other organic disorders of personality and behavior due to disease damage and dysfunction of the brain
F07.9Unspecified mental disorders due to disease damage and dysfunction of the brain
F09 Unspecified organic or symptomatic mental disorders
F10-F19 Mental and behavioral disorders due to the use of psychoactive substances
F10 Mental and behavioral disorders due to alcohol use
F11 Mental and behavioral disorders due to the use of opioids
F12 Mental and behavioral disorders due to the use of cannabinoids
F13 Mental and behavioral disorders due to the use of sedatives or hypnotics
F14 Mental and behavioral disorders due to the use of cocaine
8 Mental and behavioral disorders due to the use of cocaine other stimulants, including caffeine
F16 Mental and behavioral disorders due to the use of hallucinogens
F17 Mental and behavioral disorders due to tobacco use
F18 Mental and behavioral disorders due to the use of volatile solvents
F19 Mental and behavioral disorders due to combined drug use and the use of other psychoactive substances and signs can be used to clarify the clinical condition, and in appropriate cases of acute intoxication and withdrawal states, diagnostic criteria specific to each psychoactive substance are given
F1x.
 0 Acute intoxication
0 Acute intoxication . 00 uncomplicated
. 01 with injury or other bodily injury
. 02 with other medical complications
. 03 with delirium
. 04 with perceptual disorders
. 05 with coma
. 06 with convulsions
. 07 morbid intoxication
F1x.1 Harmful use
F1x.2 Dependency syndrome
. 20 currently abstinence
. 200 Early remission
. 201 Partial remission
. 202 Complete remission
. 21 currently abstinence, but under conditions precluding use
. 22 currently under clinical supervision on maintenance or replacement therapy (controlled addiction)
. 23 currently abstinent but on treatment with aversive or blocking medications
. 24 currently using a psychoactive substance (active addiction)
. 240 without physical symptoms
. 241 with physical symptoms
. 25 episodic use
F1x.3 Cancellation status
. 30 uncomplicated
. 31 with convulsions
F1x.4 State of withdrawal with delirium
.
 40 without seizures
40 without seizures . 41 with convulsions
F1x.5 Psychotic disorder
. 50 schizophrenia-like
. 51 predominantly delusional
. 52 predominantly hallucinatory
. 53 predominantly polymorphic
. 54 predominantly with depressive psychotic symptoms
. 55 predominantly with manic psychotic symptoms
. 56 mixed
F1x.6 Amnestic syndrome
F1x.7 Residual psychotic disorder and late onset psychotic disorder
. 70 reminiscences
. 71 personality or behavioral disorders
. 72 residual affective disorder
. 73 dementia
. 74 other persistent cognitive impairment
. 75 Late onset psychotic disorder
F1x.8 Other mental and behavioral disorders
F1x.9 Unspecified mental and behavioral disorder
. x0 continuous
. x1 episodic with growing defect
. x2 episodic with stable defect
. x3 episodic remitting
. x4 incomplete remission
. x5 complete remission
. x8 other
.
 x9 course unclear, follow-up period too short
x9 course unclear, follow-up period too short F21 Schizotypal disorder
F22 Chronic delusional disorders
F22.0 Delusional disorder
F22.8 Other chronic delusional disorders
F22.9Chronic delusional disorder, unspecified
F23 Acute and transient psychotic disorders
F23.0 Acute polymorphic psychotic disorder without symptoms of schizophrenia
F23.1 Acute polymorphic psychotic disorder with symptoms of schizophrenia
F23.2 Acute schizophrenia-like psychotic disorder predominantly 930138 delusional psychotic disorders
F23.8 Other acute and transient psychotic disorders
F23.9Acute and transient psychotic disorders, unspecified
A fifth character may be used to indicate the presence or absence of acute associated stress:
. x0 without associated acute stress
. x1 with associated acute stress
F24 Induced delusional disorder
F25 Schizoaffective disorders
F25.0 Schizoaffective disorder, manic type
F25. 1 Schizoaffective psychosis
1 Schizoaffective psychosis
F25.2 Schizoaffective disorder, mixed type
F25.8 Other schizoaffective disorders
F25.9 Schizoaffective disorder, unspecified
The following fifth character subtypes may be distinguished:
. x0 simultaneously only affective and schizophrenic symptoms
. x1 both affective and schizophrenic symptoms, plus persistence of schizophrenic symptoms after the disappearance of affective symptoms
F28 Other non-organic psychotic disorders
F29 Unspecified non-organic psychosis
F30-F39 Affective mood disorders
F30 Manic episode
F30.0 Hypomania
F30.1 Mania without psychotic symptoms
F30.2 Mania with psychotic symptoms
. 20 with mood-related psychotic symptoms
. 21 with mood-inappropriate psychotic symptoms
F30.8 Other manic episodes
F30.9 Manic episodes, unspecified
F31 Bipolar affective disorder
F31. 0 Bipolar affective disorder, current hypomanic episode
0 Bipolar affective disorder, current hypomanic episode
F31.1 Bipolar affective disorder, current manic episode without psychotic symptoms
F31.2 Bipolar affective disorder, current manic episode with psychotic symptoms
. 20 with mood-related psychotic symptoms
. 21 with mood-inappropriate psychotic symptoms
F31.3 Bipolar affective disorder, current episode of moderate or mild depression
. 30 without somatic symptoms
. 31 with somatic symptoms
F31.4 Bipolar affective disorder, current episode of severe depression without psychotic symptoms
F31.5 Bipolar affective disorder, current episode of severe depression with psychotic symptoms
. 50 with mood-related psychotic symptoms
. 51 with mood inappropriate psychotic symptoms
F31.6 Bipolar affective disorder, current episode mixed
F31.7 Bipolar affective disorder, remission
F31.8 Other bipolar affective disorders
F31.9 Bipolar affective disorder, unspecified
F32 Depressive episode
F32. 0 Mild depressive episode
0 Mild depressive episode
. 00 without somatic symptoms
. 01 with somatic symptoms
F32.1 Moderate depressive episode
. 10 without somatic symptoms
. 11 with somatic symptoms
F32.2 Major depressive episode without psychotic symptoms
F32.3 Major depressive episode with psychotic symptoms
. 30 with mood-related psychotic symptoms
. 31 with mood-inappropriate psychotic symptoms
F32.8 Other depressive episodes
F32.9 Depressive episodes, unspecified
F33 Recurrent depressive disorder
F33.0 Recurrent depressive disorder, current mild episode
. 00 without somatic symptoms
. 01 with somatic symptoms
F33.1 Recurrent depressive disorder, moderate current episode
. 10 without somatic symptoms
. 11 with somatic symptoms
F33.2 Recurrent depressive disorder, current episode severe without psychotic symptoms
F33.3 Recurrent depressive episode, current episode severe with psychotic symptoms
. 30 with mood-related psychotic symptoms
30 with mood-related psychotic symptoms
. 31 with mood-inappropriate psychotic symptoms
F33.4 Recurrent depressive disorder, in remission
F33.8 Other recurrent depressive disorders
F33.9 Recurrent depressive disorder, unspecified
F34 Chronic (affective) mood disorders
F34.0 Cyclothymia 9016 8 Other chronic affective disordersF34.9 Chronic (affective) mood disorder, unspecified
F38 Other (affective) mood disorders
F38.0 Other single (affective) mood disorders
. 00 mixed affective episode
F38.1 Other recurrent (affective) mood disorders
. 10 recurrent brief depressive disorder
F38.8 Other specified (affective) mood disorders 21
F39 Unspecified (affective) mood disorders
F40-F48 Neurotic, stress-related and somatoform disorders
F40 Anxiety-phobic disorders
F40. 0 Agoraphobia
0 Agoraphobia
. 00 without panic disorder
. 01 with panic disorder
F40.1 Social phobias
F40.2 Specific (isolated) phobias
F40.8 Other phobic anxiety disorders
F40.9 Phobic anxiety disorder, unspecified
F41 Other anxiety disorders
F41.002 Panic disorder (episodic paroxysmal anxiety). 00 Moderate
. 01 Severe
F41.1 Generalized anxiety disorder
F41.2 Mixed anxiety and depressive disorder
F41.3 Other mixed anxiety disorders
F41.8 Other specified anxiety disorders
F41.9 Anxiety disorder, unspecified 6-compulsive disorder F42
F42.0 Predominantly obsessive thoughts or ruminations (mental chewing)
F42.1 Predominantly compulsive acts (obsessional rituals)
F42.2 Mixed obsessive thoughts and actions
F42.8 Other obsessive-compulsive disorders
F42.9 Obsessive-compulsive disorder, unspecified
F43 Reaction to severe stress and adjustment disorders
F43.0 Acute reaction to stress
. 00 Lightweight
00 Lightweight
. 01 Moderate
. 02 Severe
F43.1 Post-traumatic stress disorder
F43.2 Adjustment disorder
. 20 short-term depressive reaction
. 21 prolonged depressive reactions
. 22 mixed anxiety and depressive reaction
. 23 with predominance of disturbance of other emotions
. 24 with a predominance of behavioral disorders
. 25 mixed emotional and behavioral disorder
. 28 other specific predominant symptoms
F43.8 Other reactions to severe stress
F43.9 Reaction to severe stress, unspecified
F44 Dissociative (conversion) disorders
F44.0 Dissociative amnesia
F44.1 Dissociative fugue
F44.2 Dissociative stupor
F44.3 Trances and states of mastery
F44.4 Dissociative motor disorders
F44.5 Dissociative convulsions
F44.6 Dissociative anesthesia and sensory loss
F44.7 Mixed dissociative (conversion) disorders
F44. 8 Other dissociative (conversion) disorders
. 80 Ranser syndrome
80 Ranser syndrome
. 81 multiple personality disorders
. 82 transient dissociative (conversion) disorders occurring in childhood and adolescence
. 33 respiratory system
. 34 urogenital system
. 38 other organ or system
F45.4 Chronic somatoform pain disorder
F45.8 Other somatoform disorders
F45.9 Somatoform disorder, unspecified
F48 Other neurotic disorders
F48.0 Neurasthenia depersonalization
F48.1 Neurasthenia depersonalization
F48.1 .8 Other specific neurotic disorders
F48.9 Neurotic disorder, unspecified
F50-F59 Behavioral syndromes associated with physiological disorders and physical factors
F50 Eating disorders
F50.0 Anorexia nervosa
F50.1 Atypical anorexia nervosa
F50.2 Bulimia nervosa
F50.3 Atypical bulimia nervosa8 Binge eating associated with other disorders
F50. 5 Vomiting associated with other psychological disorders
5 Vomiting associated with other psychological disorders
F50.8 Other eating disorders
F50.9Eating disorder, unspecified
F51 Nonorganic sleep disorders
F51.0 Nonorganic insomnia
F51.1 Nonorganic hypersomnia
F51.2 Nonorganic sleep-wake disorder
F51.3 Sleepwalking (somnambulism)
8 F51.468 Sleep terrors (night terrors)
F51.5 Nightmares
F51.8 Other non-organic sleep disorders
F51.9 Non-organic sleep disorder, unspecified
F52 Sexual dysfunction not due to organic disorder or disease
F52.0 Lack or loss of sexual desire
F52.1 Sexual aversion and lack of sexual satisfaction
. 10 sexual disgust
. 11 lack of sexual satisfaction
F52.2 Absence of genital response
F52.3 Orgasmic dysfunction
F52.4 Premature ejaculation
F52.5 Non-organic vaginismus
F52.6 Non-organic dyspareunia
F52.7 Increased sexual desire
F52.7 Other sexual desire dysfunction not due to an organic disorder or disease
F52. 9 Unspecified sexual dysfunction not due to an organic disorder or disease
9 Unspecified sexual dysfunction not due to an organic disorder or disease
F53 Mental and behavioral disorders associated with the puerperium, not elsewhere classified
F53.0 Mild mental and behavioral disorders associated with the puerperium, not elsewhere classified
F53.1 Severe mental and behavioral disorders associated with the postpartum period, not elsewhere classified
F53.8 Other mental and behavioral disorders associated with the postpartum period, not elsewhere classified
F53.9 Postpartum mental disorder, unspecified
F54 Psychological and behavioral factors associated with disorders or diseases classified elsewhere
F55 Abuse of non-addictive substances
F55.0 Antidepressants
F55.1 Laxatives
F55.2 Analgesics
F55.3 Acid reducers
F55.4 Vitamins
F55.5 Steroids or hormones
F55.6 Specific herbs and folk remedies
F55.8 Other non-addictive substances
F55.9 Unspecified
F59 Unspecified behavioral syndromes associated with physiological disorders and physical factors
F60-F69 Adult personality and behavior disorders
F60 Specific personality disorders
F60. 0 Paranoid personality disorder
0 Paranoid personality disorder
F60.1 Schizoid personality disorder
F60.2 Antisocial personality disorder
F60.3 Emotionally unstable personality disorder
. 30 impulsive type
. 31 borderline type
F60.4 Hysterical personality disorder
F60.5 Anancaste (obsessive-compulsive) personality disorder
F60.6 Anxious (avoidant) personality disorder
F60.7 Dependent personality disorder
F60.8 Other specific personality disorders
F60. 9 Personality disorder, unspecified
F61 Mixed and other personality disorders
F61.0 Mixed personality disorders
F61.1 Disturbing personality changes
F62 Chronic personality changes not associated with brain damage or disease
F62.0 Chronic personality changes after a disaster
F62.1 Chronic personality change after mental illness
F62.8 Other chronic personality changes
F62.9 Chronic personality change, unspecified
F63 Disorders of habits and drives
F63. 0 Pathological gambling
0 Pathological gambling
F63.1 Pathological arson (pyromania)
F63.2 Pathological theft (kleptomania)
F63.3 Trichotilomania
F63.8 Other disorders of habits and168 F63.9 Habit and drive disorder, unspecified
F64 Gender identity disorder
F64.0 Transsexualism
F64.1 Dual role transvestism
F64.2 Gender identity disorder in children
F64.8 Other disorders of gender identity
F64.9 Gender identity disorder, unspecified
F65 Disorders of sexual preference
F65.0 Fetishism
F65.1 Fetish transvestism
F65.2 Exhibitionism F64 Peduidism
F65.3
F65.5 Sadomasochism
F65.6 Multiple disorders of sexual preference
F65.8 Other disorders of sexual preference
F65.9 Sexual preference disorder, unspecified
F66 Psychological and behavioral disorders associated with sexual development and orientation
F66.0 Puberty disorder
F66.1 Ego-dystonic sexual orientation
F66. 2 Sexual relationship disorder
2 Sexual relationship disorder
F66.8 Other disorders of psychosocial development
F66.9 Psychosocial development disorder, unspecified
F68 Other disorders of adult personality and behavior
F68.0 Exaggeration of physical symptoms for psychological reasons
F68.1 Intentionally causing or feigning symptoms or disability, physical or psychological (faking disorder)
F68.8 Other specific disorders of adult personality and behavior
F70-F79 Mental retardation
F70 Mild mental retardation
F71 Moderate mental retardation
F72 Severe mental retardation
F73 Profound mental retardation
F78 Other mental retardation
F79 Unspecified mental retardation
A fourth character may be used to specify the degree of behavioral impairment:
F7x.0 minimal or no behavioral impairment
F7x.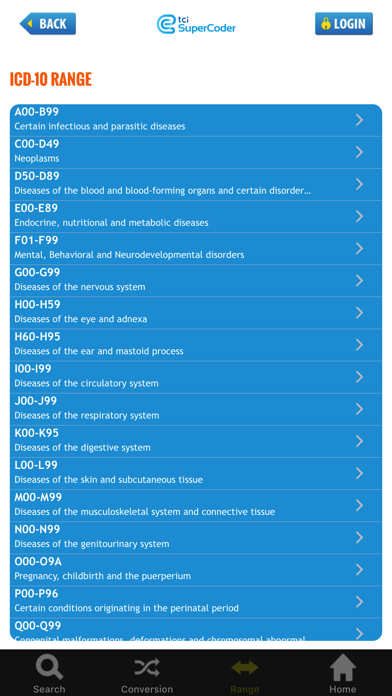 1 significant behavioral impairment requiring attention or treatment
1 significant behavioral impairment requiring attention or treatment
F7x.8 other behavioral impairment
F7x .9 behavioral disorders not identified
F80-F89 Disorders of psychological development
F80 Specific developmental disorders of speech
F80.0 Specific speech articulation disorders
F80.1 Expressive speech disorder
F80.2 Receptive speech disorder
F80.3 Acquired aphasia with epilepsy (Landau-Kleffner syndrome)
F80.8 Other developmental speech disorders
F80.9 Disorder Speech development, unspecified
F81 Specific developmental disorders of school skills
F81.0 Specific reading disorder
F81.1 Specific spelling disorder
F81.2 Specific numeracy disorder
F81.3 Mixed disorder of school skills
F81.8 Other disorders of school skills
F81.9 Developmental disorder of school skills, unspecified
F82 Specific developmental disorder of motor functions
F83 Mixed specific disorders of developmental skills
Other developmental disorders of language 9016 , unspecified
F84 General developmental disorders
F84.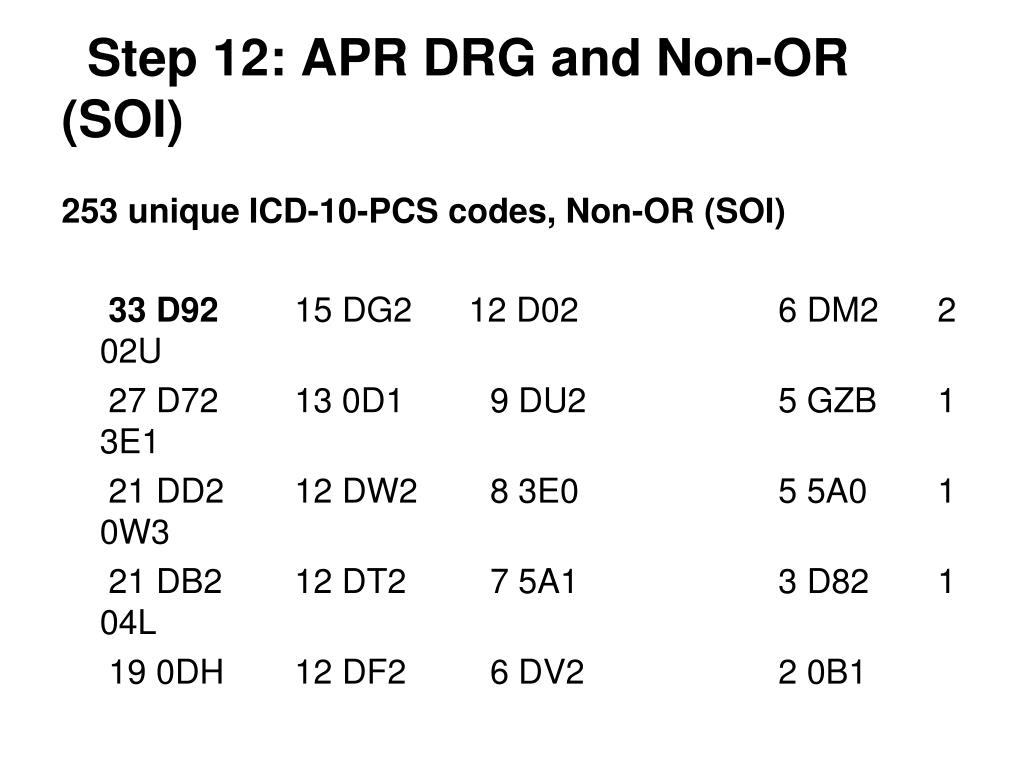 0 Childhood autism
0 Childhood autism
F84.1 Atypical autism
. 10 Atypical at onset
. 11 Atypicality in symptoms
. 12 Atypical in both age of onset and symptomatology
F84.2 Rett's syndrome
F84.3 Other childhood disintegrative disorder
F84.4 Hyperactive disorder associated with mental retardation and stereotypic movements
F84.5 Asperger's syndrome
F84.8 Others general developmental disorders
F84.9 General developmental disorder, unspecified
F88 Other disorders of psychological development
F89 Unspecified developmental disorder
F90-F98 Behavioral and emotional disorders with onset usually in childhood and adolescence
F90 Hyperkinetic disorders
F90.0 Attention disturbance
F90.1 Hyperkinetic conduct disorder
F90.8 Other hyperkinetic disorders
F90.9 Hyperkinetic disorder, unspecified
F91 Conduct disorders
F91.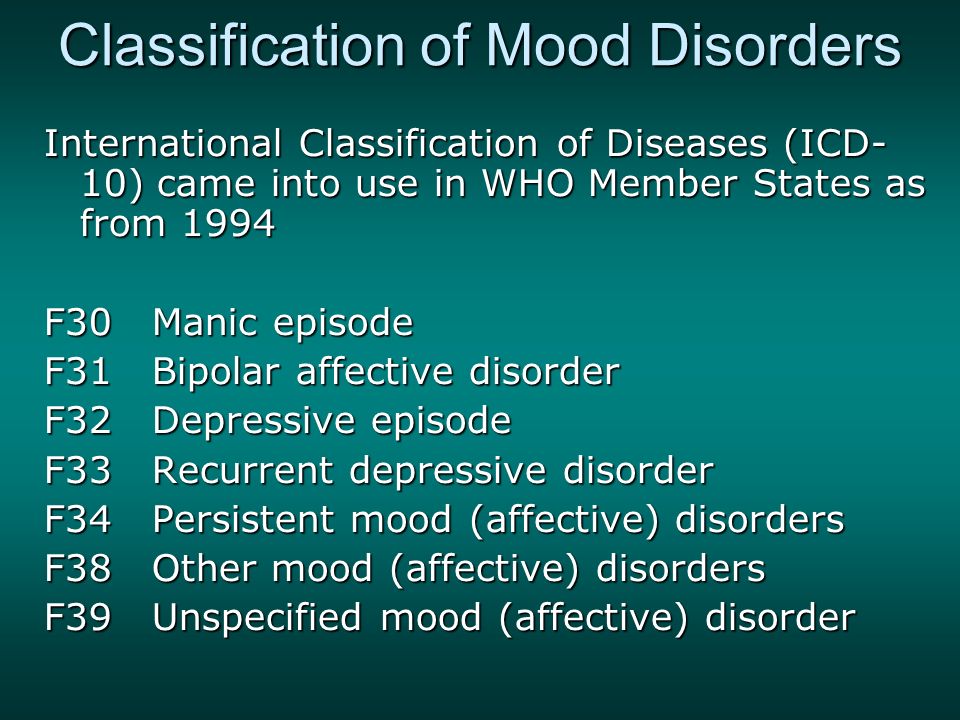 0 Conduct disorder limited to the family
0 Conduct disorder limited to the family
F91.1 Unsocialized conduct disorder
F91.2 Socialized conduct disorder
F91.3 Oppositional defiant disorder
F91.8 Other conduct disorders
F91.9 Conduct disorder, unspecified
3 2 Mixed conduct and emotion disorders
F92.0 Depressive conduct disorder
F92.8 Other mixed conduct and emotion disorders
F92.9 Mixed conduct and emotion disorder, unspecified
F93 Childhood-specific emotional disorders
F93.0 Childhood separation anxiety disorder
F93.1 Childhood phobic anxiety disorder
F93.2 Childhood social anxiety disorder
F93.3 Sibling rivalry disorder
F93.8 Other childhood emotional disorders
80 Childhood generalized anxiety disorder
F93.9 Childhood emotional disorder, unspecified
F94 Disorders of social functioning with onset specific to childhood
F94.0 Selective mutism
F94.1 Reactive attachment disorder of childhood
F94. 2 Disinhibited attachment disorder of childhood
2 Disinhibited attachment disorder of childhood
F94.8 Other childhood social functioning disorders
F94. 9 Childhood social functioning disorder, unspecified
F95 Tic disorders
F95.0 Transient tic disorder
F95.1 Chronic motor or vocal tic disorder
F95.2 Combined vocal and multiple motor tic disorder (de la Tourette syndrome)
F95.8 Other tic disorders
F95.9 Tic disorder, unspecified
F98 Other behavioral and emotional disorders , usually onset in childhood and adolescence
F98.0 Non-organic enuresis
. 00 Nocturnal enuresis only
. 01 Only diurnal enuresis
. 02 Nocturnal and diurnal enuresis
F98.1 Non-organic encopresis
. 10 Failure to acquire physiological bowel control
. 11 Adequate bowel control and defecation at inappropriate sites with normal stool consistency
. 12 Contamination due to liquid stool
F98.2 Eating disorders in infancy
F98.3 Eating inedible (peak) in infancy and childhood
F98.