Paranoid ideation symptoms
Borderline Personality Disorder and Paranoid Ideation – BrightQuest Treatment Centers
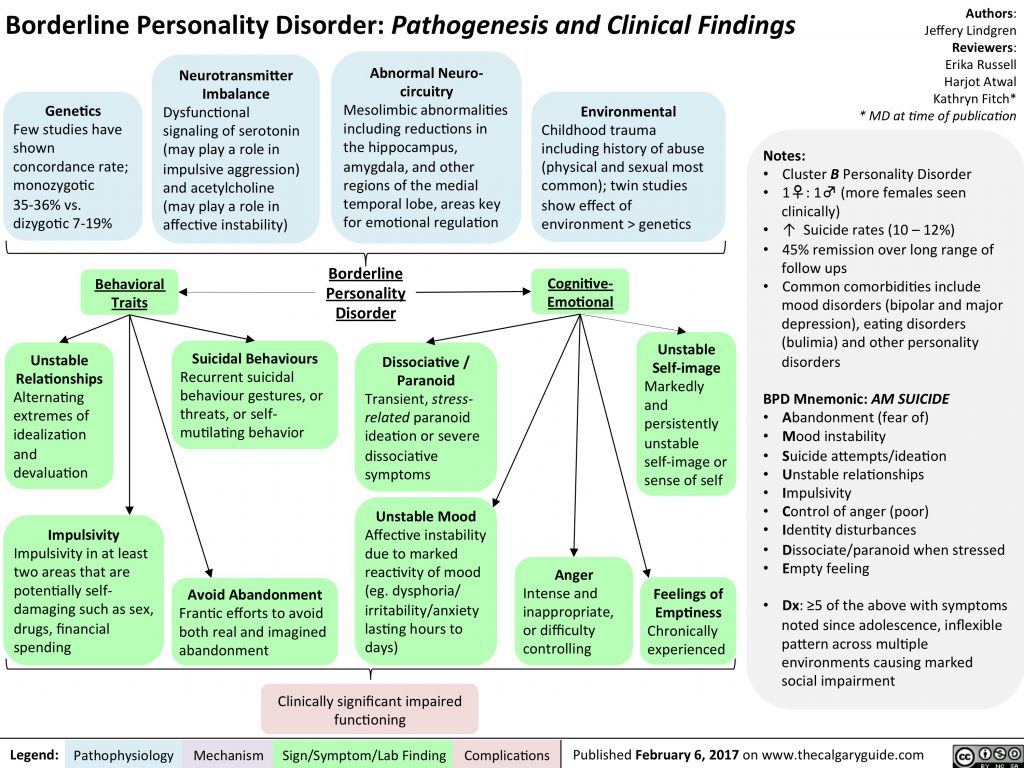
Borderline personality disorder (BPD) can distort thinking and perception, and when people with BPD are under stress they may experience extreme and disconcerting symptoms of paranoia. The proper term for this condition is paranoid ideation, and it is a complication that many men and women with borderline personality disorder will face at some point in their lives. The good news is that borderline personality disorder and paranoid ideation are both amenable to treatment, as long as the commitment to recovery is strong.
People with borderline personality disorder (BPD) struggle to maintain a healthy and consistent self-image. Insecure and unsure of themselves, they experience frequent mood swings and are often mercurial in their behavior. Their inner worlds are frequently filled with turmoil, and they may project their sense of uncertainty onto the outside world.
During times of stress, which may be caused by interpersonal conflict or a lack of self-confidence when facing personal or professional challenges, a person with BPD may suddenly feel surrounded by menace or danger. They may suspect that others—even people they would normally trust—are conspiring against them, or that mysterious forces may somehow be oppressing them.
These feelings of suspiciousness and paranoia may last for just a few days, a few weeks, or indefinitely. Stress-related paranoid ideation is the term chosen by mental health professionals to describe this state of mind, which can cause great misery and consternation among people with borderline personality disorder.
Paranoia as a Symptom of BPD
Stress-related paranoid ideation is one of nine possible diagnostic criteria for borderline personality disorder.
In one comprehensive study of patients receiving mental health services, 87 percent of participants with BPD reported experiencing the symptoms of paranoid ideation. This type of paranoia is classified as “non-delusional,” which separates it from the paranoid delusions associated with psychotic conditions.
This type of paranoia is classified as “non-delusional,” which separates it from the paranoid delusions associated with psychotic conditions.
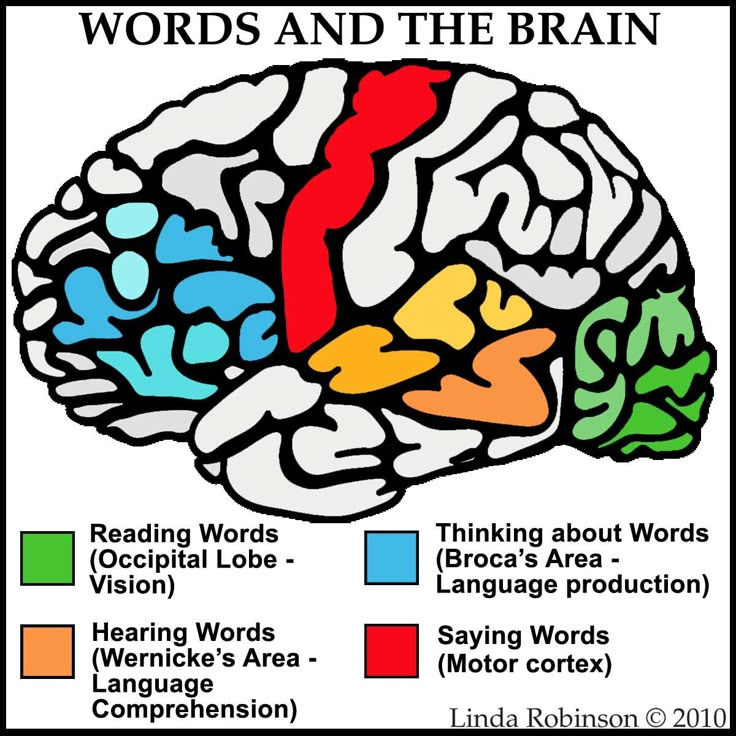
Under the influence of non-delusional paranoia, people with BPD may see signs and symbols of hostile intent everywhere. They may detect hidden meanings in speech, body language, casual glances, and other behaviors that would seem non-threatening or perfectly benign to anyone else. In some instances, their paranoia may center on remote, impersonal forces, like the government or big corporations, that they fear may be spying on or plotting to exploit them.
Unlike people with delusional disorders, men and women experiencing stress-related paranoid ideation are not convinced they have absolute proof that such conspiracies are real. But their fears are powerful, persistent, and difficult to overcome.
Once the stress and anxiety that provokes such feelings is relieved, the person with BPD experiencing paranoid ideation may regain their normal perceptions. But if the source of the stress is chronic and related to enduring life circumstance, their stress-related paranoia may continue indefinitely, at which point treatment may be their only hope for a rapid recovery.
But if the source of the stress is chronic and related to enduring life circumstance, their stress-related paranoia may continue indefinitely, at which point treatment may be their only hope for a rapid recovery.
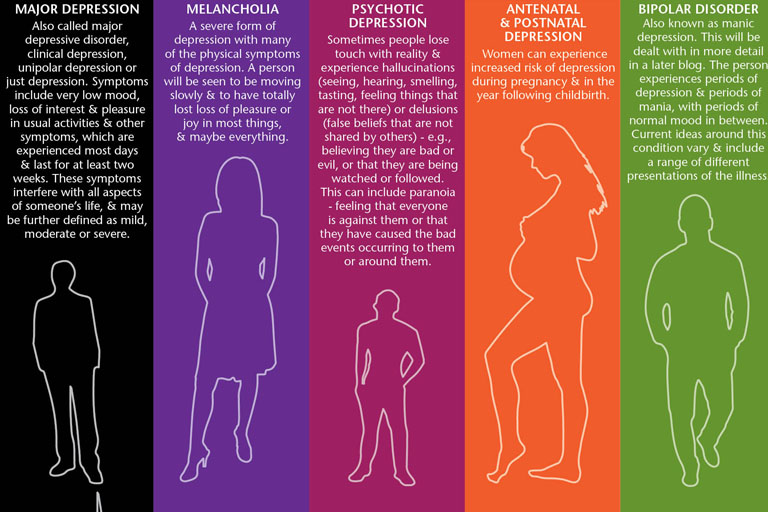
Other Mental Health Disorders That Produce Paranoia
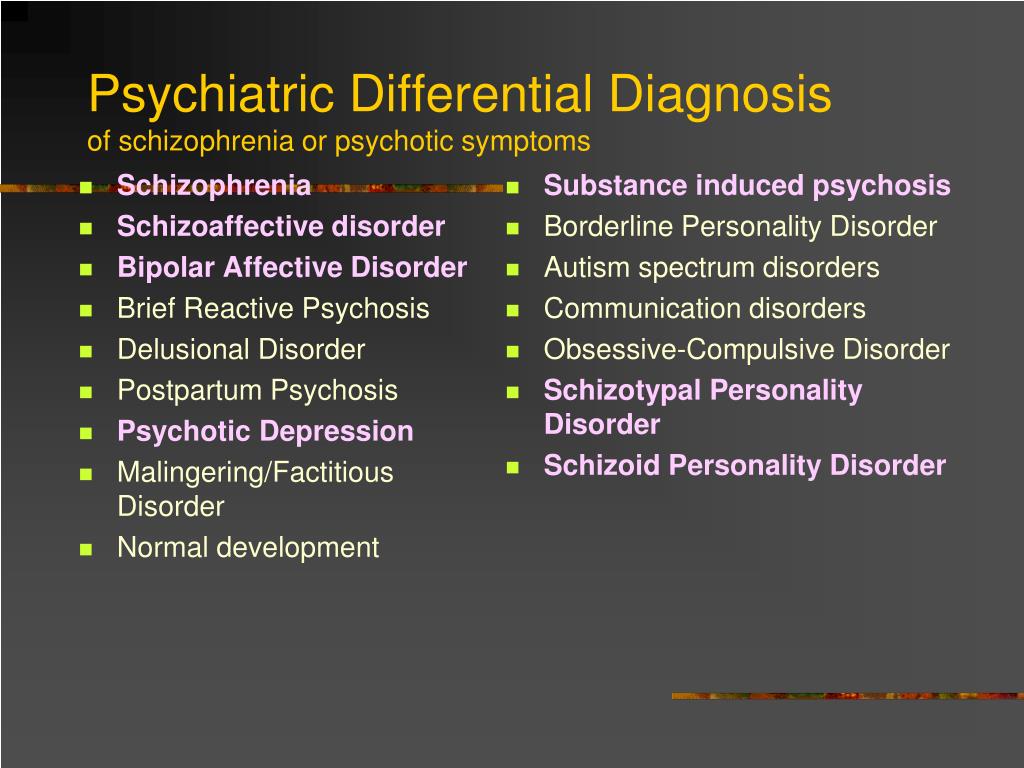
Paranoia is a common complication among people with mental health troubles. Besides borderline personality disorder, the other mental and behavioral health conditions that can produce paranoid symptoms include:
Schizophrenia
Paranoid schizophrenia, or schizophrenia with paranoia, develops in conjunction with delusional psychosis. People with this disorder are convinced they’re the target of hostile plots or campaigns of sabotage, and that hostile actors or agencies are monitoring their every move while actively working to thwart, oppress, or defeat them. They often hear voices (auditory hallucinations) that seem to confirm their worst fears and may need antipsychotic medication to reemerge from their delusional states.
Paranoid personality disorder
While the paranoid ideas and perceptions of people with borderline personality disorder are transient and situational, for people with paranoid personality disorder (PPD) the irrational fears and dark obsessions are constant companions. Paranoia is experienced as a lifestyle, not as an outside invader.
Persecutory or jealous delusional disorders
People with persecutory delusional disorder believe they are being chronically abused, exploited, or plotted against by other people or by sinister organizations (often government agencies). Those who show symptoms of jealous delusional disorder are absolutely convinced their spouses or partners are being unfaithful, and they are immune to any evidence that proves otherwise.
Like schizophrenia, delusional conditions are classified as psychotic disorders based on their ability to produce perceptions and conceptions that seem completely real but are entirely illusory.
Substance-induced disorders
These mental health conditions mimic established forms of mental illness, but they are caused by chronic, untreated substance abuse and addiction. Stimulants like cocaine and methamphetamine can cause frightening and overwhelming feelings of paranoia, and cocaine addiction in particular has long been associated with a paranoia so extreme it can cause violent behavior.
Stimulants like cocaine and methamphetamine can cause frightening and overwhelming feelings of paranoia, and cocaine addiction in particular has long been associated with a paranoia so extreme it can cause violent behavior.
Hallucinogen abuse can also cause paranoid beliefs or perceptions, and many people who report having “bad trips” while under the influence of LSD or other hallucinogens describe being stalked, chased, or persecuted by demons and other types of terrifying monsters.
Begin Your Recovery Journey Today.
619-466-0547Learn About Our Program
How We Treat BPD
Diagnosing Borderline Personality Disorder with Paranoid Ideation
Before borderline personality disorder with stress-related paranoid ideation can be diagnosed, psychotic disorders and substance abuse must be ruled out as causal factors for the symptoms experienced. Psychotic disorders and substance use disorders may be comorbid with BPD in some instances, however, so BPD could still be diagnosed even if alternative explanations for the paranoid ideation are found.
If paranoid symptoms are best explained by the presence of a personality disorder exclusively, it is their duration and context that will determine the diagnosis. Chronic and persistent feelings of paranoia will usually lead to a diagnosis of paranoid personality disorder, while temporary states of paranoid ideation associated with relationship conflicts or other types of stressful situations will make BPD the more likely alternative.
Treating Borderline Personality Disorder and Paranoid Ideation
Despite its persistent nature, borderline personality disorder—and its symptoms, including paranoid ideation—will respond well to mental health treatment, if treatment plans are carefully customized to meet the needs of the individual patient.
Medications are often recommended for people with psychotic disorders that produce paranoid delusions. But in the case of borderline personality disorder and paranoid ideation, psychotherapy is more likely to contribute to long-term recovery.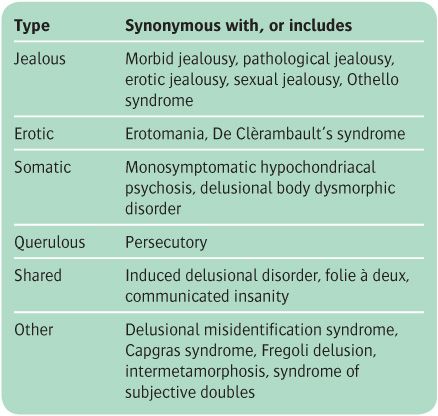
Some of the therapies that have helped people with BPD change their patterns of thinking and reacting include dialectical behavior therapy (DBT), cognitive behavioral therapy (CBT), and psychodynamic therapy, all of which combine practical strategies for self-improvement with the search for greater self-understanding. Holistic healing practices like meditation, biofeedback, Tai Chi, and yoga are also highly recommended for people with transient paranoid ideation, who can benefit greatly from learning more constructive ways to manage stress.
It is never easy to cope with personality disorders, which alter a person’s perspective from a very young age. But with a true commitment to personal growth and psychological development, people who enroll in outpatient or inpatient treatment programs for borderline personality disorder and paranoid ideation can experience dramatic and positive changes in the way they think, behave, and live.
Paranoid Personality Disorder (PPD): Symptoms & Treatment
Overview
What is paranoid personality disorder (PPD)?
Paranoid personality disorder (PPD) is a mental health condition marked by a long-term pattern of distrust and suspicion of others without adequate reason to be suspicious (paranoia). People with PPD often believe that others are trying to demean, harm or threaten them.
People with PPD often believe that others are trying to demean, harm or threaten them.
People with paranoid personality disorder often don’t think their behavior and way of thinking are problematic.
PPD is one of a group of conditions called Cluster A, or eccentric personality disorders. People with these disorders have unusual and eccentric thinking or behavior.
It’s important to note that people with paranoid personality disorder don’t experience delusions or hallucinations with paranoia, as commonly seen in schizophrenia, schizoaffective disorder and severe manic episodes in bipolar disorder.
What age does paranoid personality disorder begin?
People with paranoid personality disorder typically start experiencing symptoms and showing signs of the condition by their late teens or early adult years.
Who does paranoid personality disorder affect?
Overall, research reveals higher rates of paranoid personality disorder (PPD) in people assigned female at birth (AFAB), while samples from hospital records reveal higher rates of PPD in people assigned male at birth (AMAB).
People with PPD are more likely to:
- Live in low-income households.
- Be Black, Native American or Hispanic.
- Be widowed, divorced or separated or never married.
More research is needed to learn more about why these risk factors are associated with PPD and how stress and trauma play a role in its development.
How common is paranoid personality disorder?
Paranoid personality disorder is relatively rare. Researchers estimate that it affects 0.5% to 4.5% of the general U.S. population.
Symptoms and Causes
What are the signs and symptoms of paranoid personality disorder?
People with paranoid personality disorder (PPD) are always on guard, believing that others are constantly trying to demean, harm or threaten them. These generally unfounded beliefs, as well as their habits of blame and distrust, interfere with their ability to form close or even workable relationships. People with PPD severely limit their social lives.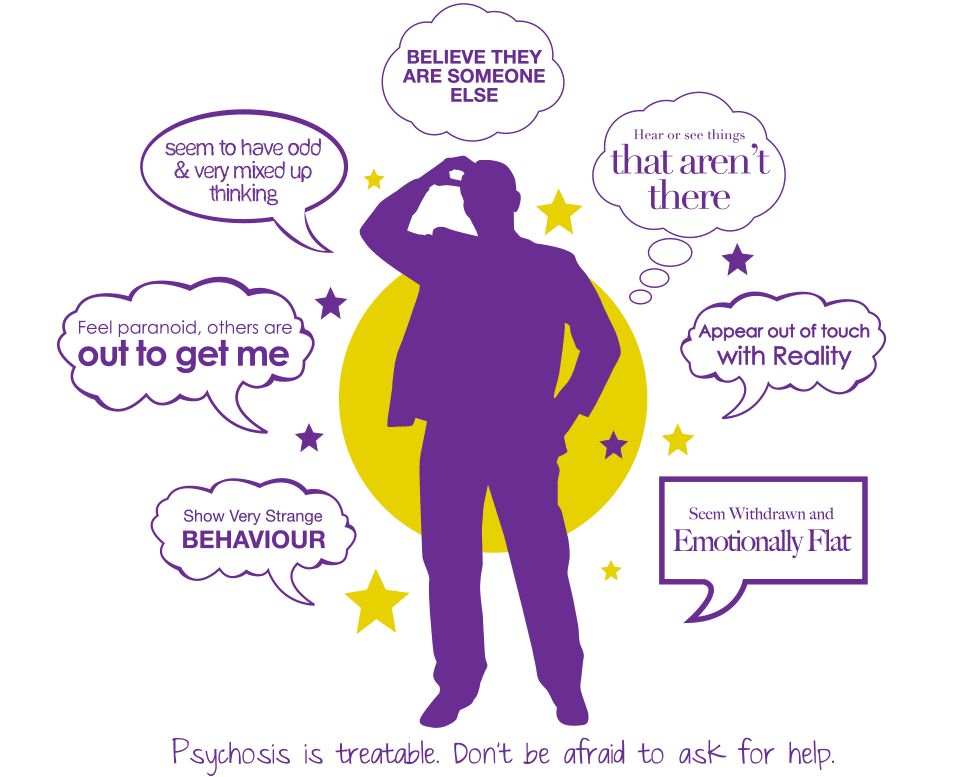
People with PPD may:
- Doubt the commitment, loyalty or trustworthiness of others, believing others are exploiting or deceiving them.
- Be reluctant to confide in others or reveal personal information because they’re afraid the information will be used against them.
- Be unforgiving and hold grudges.
- Be hypersensitive and take criticism poorly.
- Read hidden meanings in the innocent remarks or casual looks of others.
- Perceive attacks on their character that aren’t apparent to others.
- Have persistent suspicions, without justified reason, that their spouses or romantic partners are being unfaithful.
- Be cold and distant in their relationships with others and might become controlling and jealous to avoid being betrayed.
- Not see their role in problems or conflicts, believing they’re always right.
- Have difficulty relaxing.
- Be hostile, stubborn and argumentative.
What causes paranoid personality disorder?
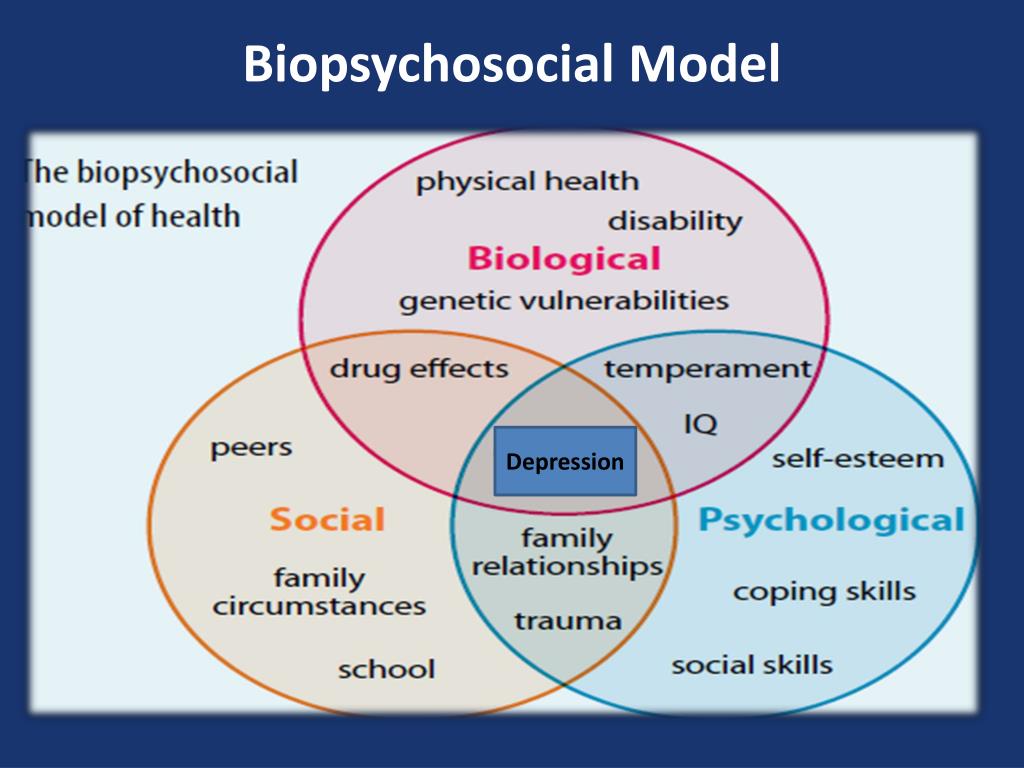
Scientists don’t know the exact cause of paranoid personality disorder (PPD), but it likely involves a combination of environmental and biological factors.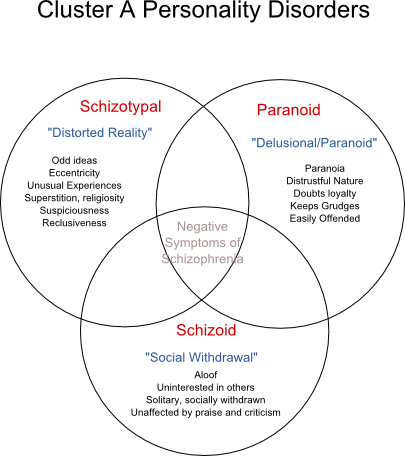
Researchers have found that childhood emotional neglect, physical neglect and supervision neglect play a significant role in the development of PPD in adolescence and early adulthood.
Researchers used to think there was likely a genetic link among schizophrenia, schizotypal personality disorder and PPD, but more studies have revealed that this connection isn’t as strong as they once thought.
Diagnosis and Tests
How is paranoid personality disorder diagnosed?
Personality continues to evolve throughout child and adolescent development. Because of this, healthcare providers don’t typically diagnose someone with paranoid personality disorder (PPD) until after the age of 18.
Personality disorders, including PPD, can be difficult to diagnose, as most people with a personality disorder don’t think there’s a problem with their behavior or way of thinking.
When they do seek help, it’s often related to conditions such as anxiety or depression due to the problems created by their personality disorder, such as divorce or lost relationships, not the disorder itself.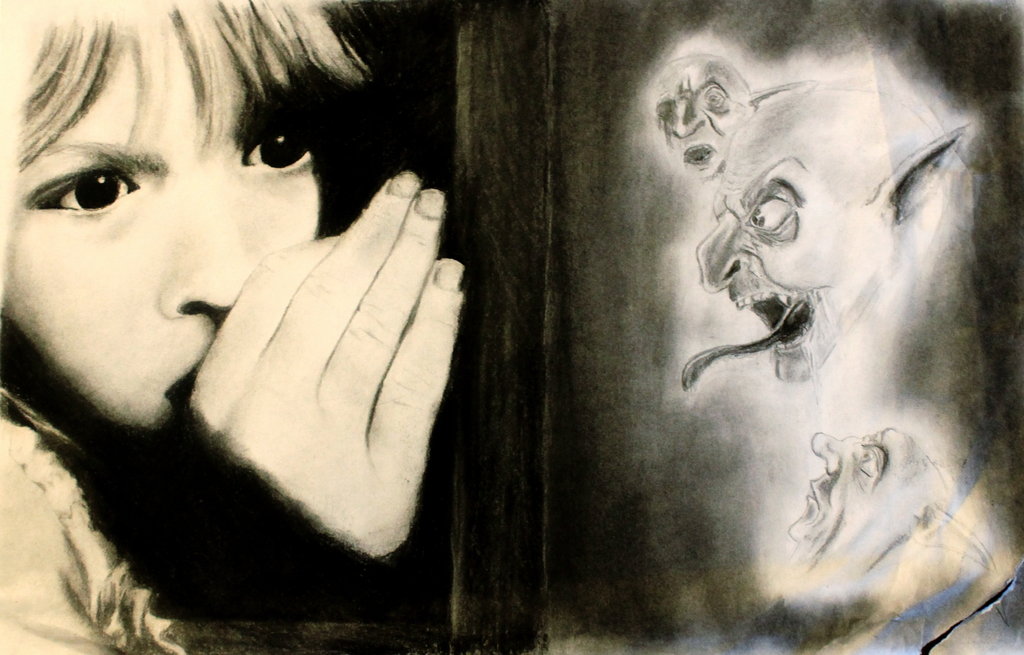
When a mental health professional, such as a psychologist or psychiatrist, suspects someone might have paranoid personality disorder, they often ask broad, general questions that won’t create a defensive response or hostile environment. They ask questions that will shed light on:
- Past history.
- Relationships.
- Previous work history.
- Reality testing.
- Impulse control.
Mental health providers base a diagnosis of paranoid personality disorder on the criteria for the condition in the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders.
Are other medical conditions associated with paranoid personality disorder?
Yes, approximately 75% of people with paranoid personality disorder (PPD) have another personality disorder. The most common personality disorders to co-occur with PPD include:
- Avoidant personality disorder.
- Borderline personality disorder (BPD).
- Antisocial personality disorder (ASPD).
People with PPD are also more likely to have substance use disorder and panic disorder than the general U.S. population.
Management and Treatment
How is paranoid personality disorder treated?
People with paranoid personality disorder (PPD) rarely seek treatment on their own. Family members, coworkers or employers usually refer them.
When someone with PPD does seek treatment, psychotherapy (talk therapy), such as cognitive behavioral therapy (CBT) or dialectical behavior therapy (DBT), is the treatment of choice. Therapy focuses on increasing general coping skills, especially trust and empathy, as well as on improving social interaction, communication and self-esteem.
As people with PPD often distrust others, it poses a challenge for healthcare professionals because trust and rapport-building are important factors of psychotherapy. As a result, many people with PPD may not follow their treatment plan and may even question the motives of the therapist.
Healthcare providers generally don’t prescribe medication to treat PPD. However, medications — such as anti-anxiety, antidepressant or antipsychotic drugs — might be prescribed if the person’s symptoms are extreme or if they have an associated psychological condition, such as anxiety or depression.
Prevention
Can paranoid personality disorder be prevented?
While paranoid personality disorder generally can’t be prevented, treatment can allow someone with PPD to learn more productive ways of dealing with triggering thoughts and situations.
Outlook / Prognosis
What is the prognosis (outlook) for paranoid personality disorder?
The prognosis (outlook) for paranoid personality disorder (PPD) typically depends on whether someone with PPD is willing to accept and commit to treatment. Talk therapy can sometimes reduce paranoia and limit its impact on daily functioning.
Left untreated, PPD can interfere with a person’s ability to form and maintain relationships, as well as their ability to function socially and in work situations. People with PPD are more likely to stop working earlier in their lives than people without personality disorders.
People with PPD are more likely to stop working earlier in their lives than people without personality disorders.
In addition, PPD is one of the strongest predictors of aggressive behavior in a hospital setting. PPD is also associated with stalking and excessive litigation (lawsuits).
A note from Cleveland Clinic
It’s important to remember that paranoid personality disorder (PPD) is a mental health condition. As with all mental health conditions, seeking help as soon as symptoms appear can help decrease disruptions to a person’s life. Mental health professionals can offer treatment plans that can help manage thoughts and behaviors of people with PPD.
Family members of people with paranoid personality disorder often experience stress, depression, grief and isolation. It’s important to take care of your mental health and seek support if you’re experiencing these symptoms.
What is obsession (obsessive thoughts): symptoms, how to get rid of?
- Symptoms of obsession
- What thoughts arise during obsession?
- How a disorder appears
- Classification
- Diagnostics
- How to get rid of obsessive thoughts?
- Treatment
Obsession is a condition in which a person is disturbed by intrusive thoughts.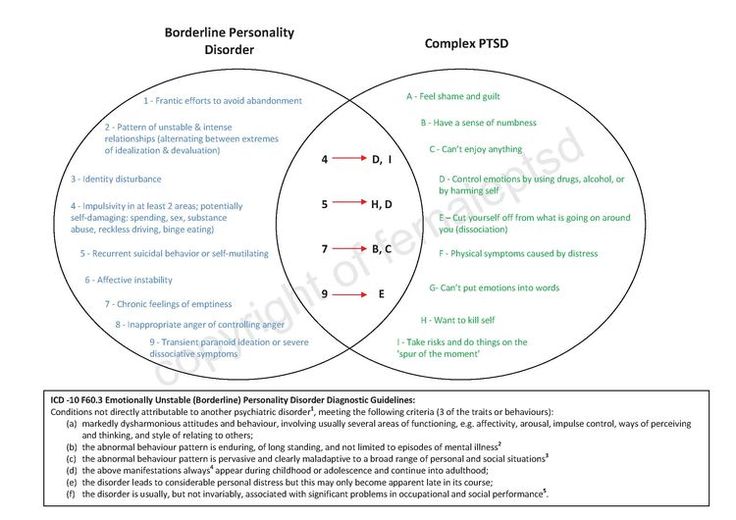 Alien images and urges to certain actions arise involuntarily. A person tries to isolate himself from these ideas, the state causes anxiety and discomfort. If treatment is not done in time, obsession leads to emotional exhaustion, depressive disorder, and the inability to adapt in society.
Alien images and urges to certain actions arise involuntarily. A person tries to isolate himself from these ideas, the state causes anxiety and discomfort. If treatment is not done in time, obsession leads to emotional exhaustion, depressive disorder, and the inability to adapt in society.
Symptoms
Obsessive thoughts accompany a number of psychological illnesses. They develop with neurosis, schizophrenia, depression, obsessive-compulsive disorder (OCD).
Signs that accompany obsession:
-
the inability to influence the appearance of obsessive thoughts, they arise against the will of a person;
-
thoughts are in no way connected with habitual reasoning, the emerging images are alien;
-
by an effort of will it is impossible to drive away these thoughts;
-
accompanied by anxiety, irritability;
-
the clarity of consciousness is preserved, the person adequately perceives what is happening.
Obsessive people have a hard time with intrusive thoughts. Against the background of clarity of consciousness, the patient understands the irrationality of the images that arise, but cannot influence the situation in any way. This is even more worrying.
If seizures occur regularly, the only way out is to consult a psychiatrist.
What thoughts come up when you have an obsession?
Obsessive thoughts during obsession are directed primarily at the person himself, his environment and state of health. The most common ones are:
-
the need for perfect order and symmetry;
-
constant counting of various objects, steps, for example;
-
worries about illness;
-
pollution concerns;
-
thoughts about accidents that should happen to a person or his relatives;
-
concerns about property damage;
-
aggressive, sexual, religious ideas that arise against the will;
-
unwillingness to perform any actions or rejection of any objects, objects.

Obsessive thoughts bring extremely negative emotions. Sometimes there is a desire to follow these ideas, then a person experiences compulsions: he performs actions against his will, in accordance with an obsessive idea. In this state, the patient experiences discomfort, suffering, it interferes with normal life. When an obsessive idea is combined with actions to realize it, obsessive-compulsive disorder (OCD) develops.
Against the background of OCD, a person performs actions that, as it seems to him, will protect him from negative events in life. He may, for example, make it a rule to touch trees, to avoid cracks in the road, because he believes that if he does not do this, irreparable things will happen. The person expects that performing these actions will reduce anxiety and get rid of obsessive thoughts. However, this does not alleviate the condition, the actions turn into a kind of ritual.
How a disorder appears
The cause of the obsessional state has not yet been precisely established. It can be preceded by prolonged stress, experienced psychological trauma, concentration on negative thoughts, and the impact of others. Not all people are prone to developing obsessions. Predisposing factors are:
It can be preceded by prolonged stress, experienced psychological trauma, concentration on negative thoughts, and the impact of others. Not all people are prone to developing obsessions. Predisposing factors are:
-
indecision;
-
restrained reactions with hypersensitivity;
-
self-esteem is reduced or vice versa is too high;
-
suspiciousness;
-
desire to dominate.
People are prone to obsessions, in whose families a high sense of responsibility, perfectionism was instilled. When a child was kept within strict limits, spontaneity was suppressed. The man had to keep his emotions inside. The result was an intrapersonal conflict.
There are different theories regarding the development of obsessions. According to Pavlov's theory, people with a certain type of nervous activity are prone to the condition. When there is a fixation on the processes of excitation along with inactivity. According to Freud's theory, disorder occurs involuntarily and is in no way controlled by consciousness. Occurs against a background of guilt.
According to Freud's theory, disorder occurs involuntarily and is in no way controlled by consciousness. Occurs against a background of guilt.
Classification
According to Jaspers' classification, obsessional disorders are abstract and figurative.
With an abstract form, there is no emotional coloring. Thoughts do not affect the mood of a person in any way, they do not contribute to changes in the psyche. These intrusive thoughts include:
-
Arithmomania. A person constantly counts something (steps, cars, trees), remembers the numbers of telephones and cars. He is constantly busy with digital calculations.
-
Highlighting words. Certain words from the phrases read are decomposed into letters.
-
Memories. The same memory constantly arises in the memory, about which a person tries to tell the largest number of people. Tries to prove the magnitude and importance of this event.
-
Wisdom.
 Regularly there are all sorts of reflections, devoid of any meaning.
Regularly there are all sorts of reflections, devoid of any meaning.
With the development of a figurative form of obsession, the patient experiences severe emotional experiences, mostly of a pessimistic nature:
-
Doubts. Pursues uncertainty about the correctness of the actions taken. The patient will repeatedly check the result. This condition can manifest itself in situations such as returning home to check the turned off iron, gas. If this is not possible, the person experiences strong feelings.
-
Fears. Most often, this condition affects people whose activities may lead to litigation. These are doctors who have doubts about the quality of operations, accountants associated with large financial transactions, and other financially responsible persons in the enterprise. This category of people includes teachers who are responsible for the life and health of the child at school.
-
Experiences.
 Constant thoughts about past events, mostly negative, tragic. Thoughts cause depression, remorse, guilt and regret, shame, tears, fear.
Constant thoughts about past events, mostly negative, tragic. Thoughts cause depression, remorse, guilt and regret, shame, tears, fear. -
attraction. Accompanied by a desire to commit an obscene act: swearing, fighting. Despite the vivid expression of the thought, most often it is not realized in action.
-
Representation. When thoughts arise about the consequences of actions that a person could take. For example, how events will develop if he takes someone's life. Sometimes thoughts are so intrusive that a person ceases to be aware of their irrationality.
-
Antipathy. An unreasonable feeling of hostility towards people, most often close ones. For believers, it may arise in relation to religious figures.
Most often, intrusive thoughts are associated with the following factors:
-
intolerance to the slightest disorder;
-
fear of infection;
-
non-existent danger;
-
obsession of a sexual nature;
-
violence;
-
blasphemy.

There may be complex disorders, when some obsessive thoughts replace others.
Diagnosis
Ideas of an obsessive nature can also appear in other psychological illnesses. Therefore, a qualified specialist who understands the features of the clinical picture should carry out the diagnosis.
Diagnostic measures include:
-
Inspection. Collection of information about complaints, assessment of the clinical picture.
-
Pathopsychological research. Patient observation, interviews and experiments.
-
Surveys. With the help of neurotests and a neurophysiological test system, the severity of the processes is assessed.
How to get rid of obsessive thoughts?
If a person has signs of obsession, thoughts appear that cannot be fenced off, it is necessary to visit a psychiatrist for a consultation. If this is not done in a timely manner, the situation will worsen. Often people with these disorders turn to alcohol or drugs to get away from the problem. However, as a result of taking alcoholic beverages, the symptoms of obsession only increase.
Often people with these disorders turn to alcohol or drugs to get away from the problem. However, as a result of taking alcoholic beverages, the symptoms of obsession only increase.
In addition to the basic therapy prescribed by the doctor, it is necessary to learn self-control. You can reduce the manifestations of obsession by the following actions:
-
learn more about the violation, this will allow you to accept the situation and tune in to the need for treatment;
-
talk about the problem to relatives, parents, spouses or children;
-
do not give up the usual activities;
-
normalize sleep and wakefulness;
-
give up alcohol and drugs;
-
play sports with moderate physical activity;
-
find a hobby that delivers emotional satisfaction;
-
avoid stressful activities.
Treatment
Psychotherapy and drug therapy can reduce the manifestations of the disease or completely get rid of OCD. Psychotherapeutic methods of treatment allow you to learn how to manage manifestations, protect yourself from stress, and avoid fear. As prescribed by the doctor, it is necessary to take drugs that correct neurotic symptoms, relieve fear, anxiety, and control mood. For this purpose, antidepressants, antipsychotics and tranquilizers are prescribed for obsession. After psychotherapy, drug treatment and rehabilitation, the patient returns to normal life, without obsessive thoughts and fears.
Psychotherapeutic methods of treatment allow you to learn how to manage manifestations, protect yourself from stress, and avoid fear. As prescribed by the doctor, it is necessary to take drugs that correct neurotic symptoms, relieve fear, anxiety, and control mood. For this purpose, antidepressants, antipsychotics and tranquilizers are prescribed for obsession. After psychotherapy, drug treatment and rehabilitation, the patient returns to normal life, without obsessive thoughts and fears.
treatment, causes, how to deal with obsessive thoughts
Obsessive thoughts (obsessions) are images or urges that uncontrollably, against the will of a person, invade consciousness. Attempts to get rid of these thoughts lead to outbreaks of anxiety and bring great discomfort. A person experiences constant fears and bad thoughts. If you do not seek help in time, obsessions lead to psychological exhaustion, social isolation and depression.
Obsessive thoughts are found in many diseases: neurosis, depression, obsessive-compulsive disorder (obsessive-compulsive disorder) and even schizophrenia.

Features that distinguish obsessive thoughts syndrome:
- a person cannot influence the appearance of such thoughts, thoughts arise against desire;
- obsessive thoughts are not connected with the usual thoughts of a person - they are separate, alien images;
- the syndrome of obsessive thoughts cannot be overcome by an effort of will;
- the disorder is associated with intense anxiety, irritability;
- clarity of consciousness and critical perception of one's state are usually preserved.
The disorder is extremely difficult to bear. Usually a person realizes what obsessive thoughts mean, understands all the irrationality of the images that arise in the head, but cannot fight them. Attempts to stop the appearance of thoughts and the coercive actions associated with them are unsuccessful and lead to even greater experiences.
It is not difficult to convince people who suffer from this disorder that their obsessive thoughts have no basis. But it doesn't help to get rid of the problem. Situations repeat themselves over and over. A necessary step to get rid of painful conditions is to seek help from a specialist before complications arise.
But it doesn't help to get rid of the problem. Situations repeat themselves over and over. A necessary step to get rid of painful conditions is to seek help from a specialist before complications arise.
What are obsessive thoughts
Obsessive thoughts torment a person, they are unpleasant and disturbing, you want to hide from them, run away. There are all kinds of obsessions.
Here are some examples of intrusive thoughts:
- concerns about pollution and disease;
- pathological need for order and symmetry;
- obsessive and uncontrolled account;
- obsessive thoughts about the bad: a person constantly thinks about accidents that can happen to him, to his relatives, to his property, or even to humanity as a whole;
- groundless and unreasonable avoidance of certain actions or objects;
- thoughts of a religious, sexual, aggressive or any other kind, which are alien to the thinking of the patient and arise against the will.

Constant intrusive thoughts cause unbearable discomfort. Of course, a person has a desire to succumb to these ideas and try to correct the situation. In this case, compulsions appear - actions that a person is forced to periodically perform, even if he does not want to, in order to control what is happening in his head. When obsessive thoughts (obsessions) and obsessive actions (compulsions) are present together, time-consuming, disruptive, and distressing, it indicates the presence of a disease such as obsessive-compulsive disorder (OCD).
A person begins to avoid cracks in the asphalt or touches every tree on the road because alien thoughts “tell” him that if he does not do this, something bad will happen.
Usually compulsions make you do something over and over again, like a ritual. By giving in to coercion, the person hopes that they can prevent or reduce the anxiety that accompanies obsessions. For example, he begins to avoid cracks in the asphalt or touches every tree on the road because alien thoughts "tell" him that if he does not do this, something bad will happen. Unfortunately, such actions do not bring relief and only get worse over time, taking the form of an endless ritual.
Unfortunately, such actions do not bring relief and only get worse over time, taking the form of an endless ritual.
In addition to OCD, there are other diseases in psychiatry that are characterized by different types of obsessive thoughts. Here is some of them:
- phobias,
- neurasthenia,
- schizophrenia.
A phobia is an anxiety disorder characterized by panic and an uncontrollable, irrational fear of certain situations or objects. Strong anxiety can arise even when thinking about a frightening situation, so the patient tries with all his might to avoid a terrible object. All terrible obsessive thoughts and anxieties are associated exclusively with this object.
There are different types of phobias. The most common:
- agoraphobia — fear of open spaces or crowded places;
- social phobia - fear of social interactions. There are other specific phobias that can relate to anything: airplanes, specific animals, the sight of blood.
A phobic disorder may include panic attacks - attacks of fear, which are accompanied by a feeling of impending death and physical sensations: retrosternal pain, interruptions in the heart, dizziness, feeling short of breath, numbness of the extremities, intestinal disorders. All this significantly limits the personal life and performance of a person.
Neurasthenia is a disorder that is associated with exhaustion of the nervous system. It happens after a long illness, physical overload, severe or prolonged stress. Characterized by persistent headache, symptoms of cardiovascular disorders, indigestion and sleep.
Intrusive delusional thoughts may be one of the manifestations of schizophrenia, but the diagnosis is made only in the presence of other signs of schizophrenia.
The disease has three forms-stages that develop one after another. In the hypersthenic form, emotional lability, irritability and intolerance are observed.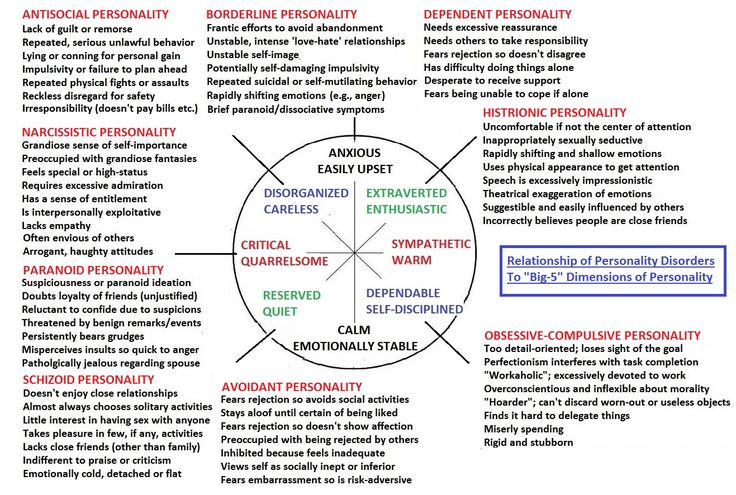 In the second phase, which is called "irritable weakness", aggression and irritation are quickly replaced by emotional exhaustion and impotence. In the third, hyposthenic form, the patient arrives in a state of constant fatigue and bad mood. He focuses on his inner feelings, which depresses him even more. This phase is characterized by obsessive thoughts of a hypochondriacal nature.
In the second phase, which is called "irritable weakness", aggression and irritation are quickly replaced by emotional exhaustion and impotence. In the third, hyposthenic form, the patient arrives in a state of constant fatigue and bad mood. He focuses on his inner feelings, which depresses him even more. This phase is characterized by obsessive thoughts of a hypochondriacal nature.
Schizophrenia is a complex polymorphic mental illness characterized by a fundamental impairment of perception and the breakdown of thought processes. The clinical picture is varied and depends on the form of the disease: hallucinations, delusions, loss of natural mental functions, personality distortion, and much more.
A sick person who suffers from this disease needs full treatment from a psychiatrist. Intrusive delusional thoughts may be one of the manifestations of schizophrenia, but the diagnosis is made only in the presence of other signs that are specific, diagnostically significant criteria for this disorder.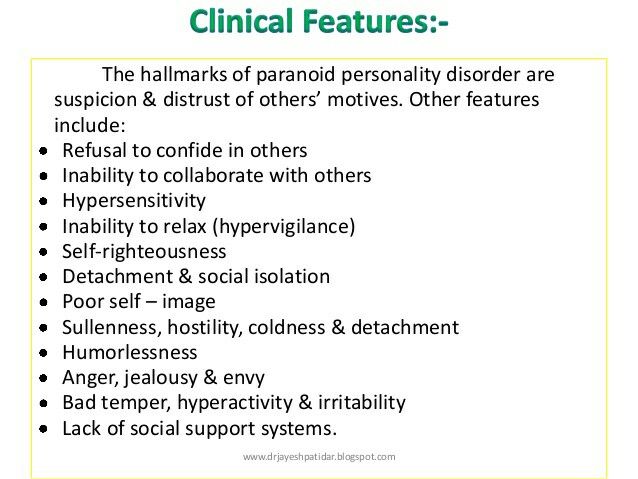
Causes of obsessive thoughts
The occurrence of obsessions is directly related to the underlying disease. For treatment to be effective, an accurate diagnosis is essential. It is not always possible to accurately answer the question of where obsessive thoughts come from. Factors that contribute to the occurrence of this disorder have been identified:
- genetic predisposition;
- brain dysfunction due to organic or biochemical causes, including imbalance of neurotransmitters;
- mental trauma and stress;
- personality traits: people with sensitive and labile temperament;
- The presence of somatic and infectious diseases, disability, pregnancy are predisposing causes of obsessive thoughts.
There are many disorders in which this syndrome occurs, so the diagnosis should be carried out by a highly qualified psychiatrist who can understand the intricacies of the clinical picture and understand why obsessive thoughts arise.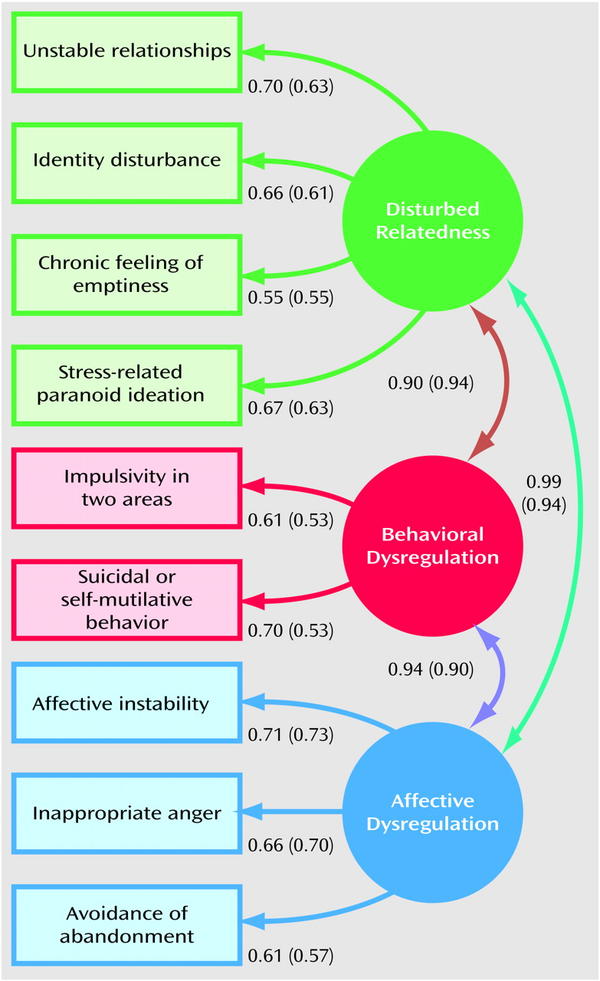 When conducting diagnostics, the following methods are used:
When conducting diagnostics, the following methods are used:
- Psychiatric examination: a specialist will collect an anamnesis, understand the clinical manifestations and personal characteristics of each patient.
- Pathopsychological study: an effective and comfortable technique that, with the help of special experiments, surveys and observations, allows you to conduct a qualitative analysis of mental disorders and understand why obsessive thoughts come.
- Laboratory and instrumental examination: modern diagnostic tests, such as Neurotest and Neurophysiological test system, allow assessing the severity of pathological processes and making an accurate differential diagnosis. Functional methods will help to exclude organic pathology.
How to deal with intrusive thoughts
Mental illnesses that underlie the syndrome in question are a reason to immediately consult a psychiatrist. The symptoms vary greatly, and it is not always easy to notice the distinctive features. Therefore, it is necessary to address the question of what to do with obsessive thoughts to an experienced specialist.
Therefore, it is necessary to address the question of what to do with obsessive thoughts to an experienced specialist.
It happens that a person is afraid to seek help or tries to independently find a way to cope with obsessive thoughts that are so annoying. One of the most common decisions is the use of alcohol and drugs. If a person manages to be distracted, the illusion may be created for a short time that the problem has disappeared. In fact, the situation is only getting worse. You should not try to "kill" intrusive thoughts in this way, because it is likely that obsessions will only intensify when intoxicated.
Talk to someone you trust, such as your parents or friends. A great option is to go to group therapy, in a society of people with similar problems. This will allow you to share experiences and get support.
The consequences of drinking alcohol can be unpredictable. Even if there is a brief relief, thoughts will still arise again, and with even greater force. As a result, new health problems are added, dependence on alcohol or drugs develops, and the disorder worsens. With neurosis of obsessive thoughts, only a specialist will tell you how to get rid of or alleviate the condition.
As a result, new health problems are added, dependence on alcohol or drugs develops, and the disorder worsens. With neurosis of obsessive thoughts, only a specialist will tell you how to get rid of or alleviate the condition.
In addition to the stages of treatment that the doctor will select for you, you need to remember about self-control, rehabilitation and prevention. Here are a few tips beyond basic treatment to help you deal with intrusive thoughts:
- Learn more about your disorder. Learning about your condition will help you quickly accept the problem, calm down and motivate you to better adhere to the treatment plan.
- Talk to someone you trust, such as your parents or friends. A great option is to go to group therapy, in a society of people with similar problems. This will allow you to share experiences and get support.
- Normalization of lifestyle: full sleep, diet, avoidance of alcohol and strong psychotropic substances, moderate physical activity.
- Do not give up your normal activities. Build a career, study, devote time to your favorite hobby. Spend time with family and friends. Don't let illness interfere with your life.
- Avoid Stress: The idea that a strong outburst of emotions will make the fight against obsessive thoughts more effective is false. It will be possible to be distracted only for a short time, but then the nervous system will become even more vulnerable.
Treatment of obsessive thoughts
With the help of modern medicine, it is possible to mitigate the intensity of manifestations, and often completely get rid of obsessions and compulsions.
For obsessive thoughts syndrome, treatment is most effective when combined with psychotherapy and medication. In some cases, one thing is enough. A competent specialist will select an individual program, which will depend on the clinical picture and the severity of the condition.
For obsessive thoughts, treatment may consist of psychotherapy and pharmacotherapy.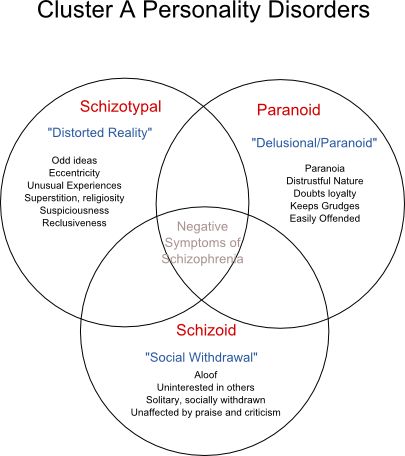
Psychotherapy allows you to fully analyze the situation and work out behavioral, psychological and social problems. Communication with a highly qualified psychotherapist teaches you how to manage symptoms, overcome fears and protect yourself from stress. The arsenal of a modern specialist includes cognitive behavioral therapy, hypno-suggestive techniques, auto-training and other effective approaches. Psychotherapy for obsessive thoughts is a key treatment that will help you understand the problem and deal with it.
Pharmacotherapy. Modern medicines help to correct neurotic symptoms, relieve fear and anxiety, and keep mood under control. Mild antidepressants, antipsychotics and tranquilizers are used.
Fortunately, modern psychiatry knows how to cure obsessive thoughts, reduce or completely eliminate symptoms. Thanks to effective treatment and rehabilitation provided by a competent specialist, patients return to an active life without fears and restrictions.