Lyme disease and mental illness
Lyme disease: a neuropsychiatric illness
Save citation to file
Format: Summary (text)PubMedPMIDAbstract (text)CSV
Add to Collections
- Create a new collection
- Add to an existing collection
Name your collection:
Name must be less than 100 characters
Choose a collection:
Unable to load your collection due to an error
Please try again
Add to My Bibliography
- My Bibliography
Unable to load your delegates due to an error
Please try again
Your saved search
Name of saved search:
Search terms:
Test search terms
Email: (change)
Which day? The first SundayThe first MondayThe first TuesdayThe first WednesdayThe first ThursdayThe first FridayThe first SaturdayThe first dayThe first weekday
Which day? SundayMondayTuesdayWednesdayThursdayFridaySaturday
Report format: SummarySummary (text)AbstractAbstract (text)PubMed
Send at most: 1 item5 items10 items20 items50 items100 items200 items
Send even when there aren't any new results
Optional text in email:
Create a file for external citation management software
Full text links
Atypon
Full text links
Review
. 1994 Nov;151(11):1571-83.
doi: 10.1176/ajp.151.11.1571.
B A Fallon 1 , J A Nields
Affiliations
Affiliation
- 1 Department of Psychiatry, College of Physicians and Surgeons, Columbia University, New York.
- PMID: 7943444
- DOI: 10.1176/ajp.151.11.1571
Review
B A Fallon et al. Am J Psychiatry. 1994 Nov.
. 1994 Nov;151(11):1571-83.
doi: 10.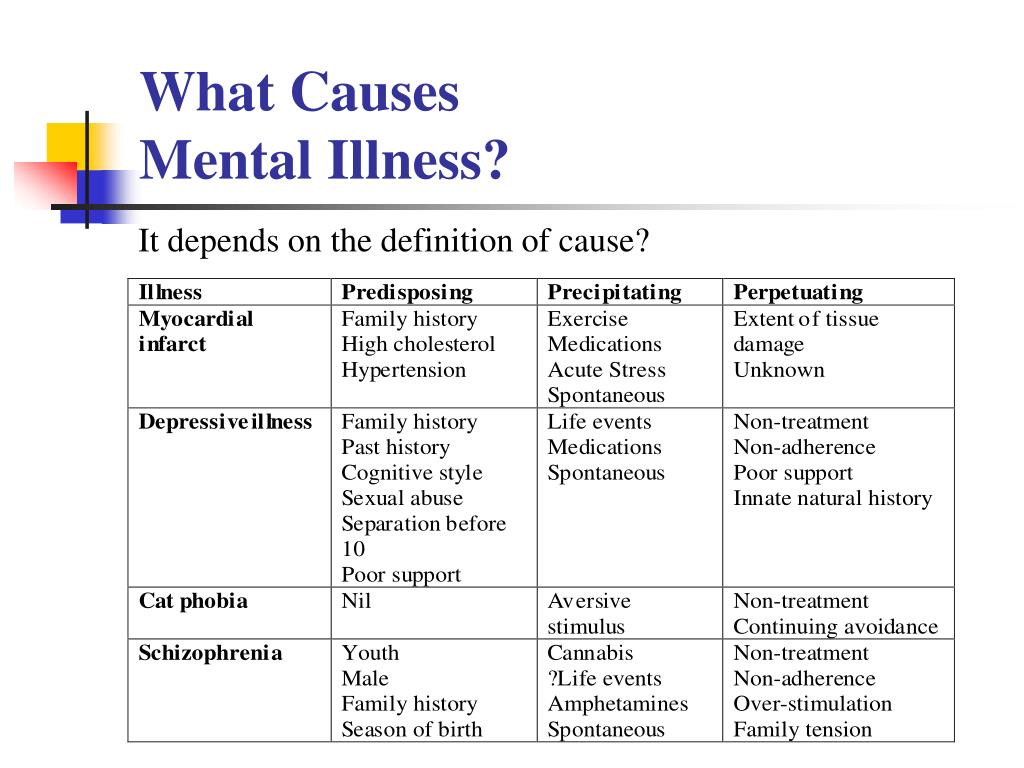 1176/ajp.151.11.1571.
1176/ajp.151.11.1571.
Authors
B A Fallon 1 , J A Nields
Affiliation
- 1 Department of Psychiatry, College of Physicians and Surgeons, Columbia University, New York.
- PMID: 7943444
- DOI: 10.1176/ajp.151.11.1571
Abstract
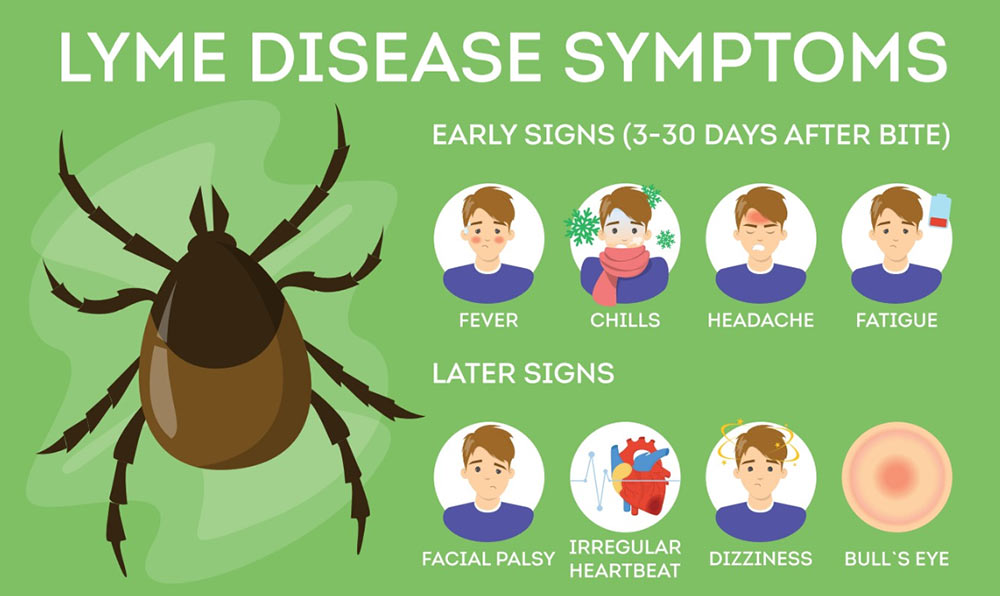
Objective: Lyme disease is a multisystemic illness that can affect the central nervous system (CNS), causing neurologic and psychiatric symptoms. The goal of this article is to familiarize psychiatrists with this spirochetal illness.
Method: Relevant books, articles, and abstracts from academic conferences were perused, and additional articles were located through computerized searches and reference sections from published articles.
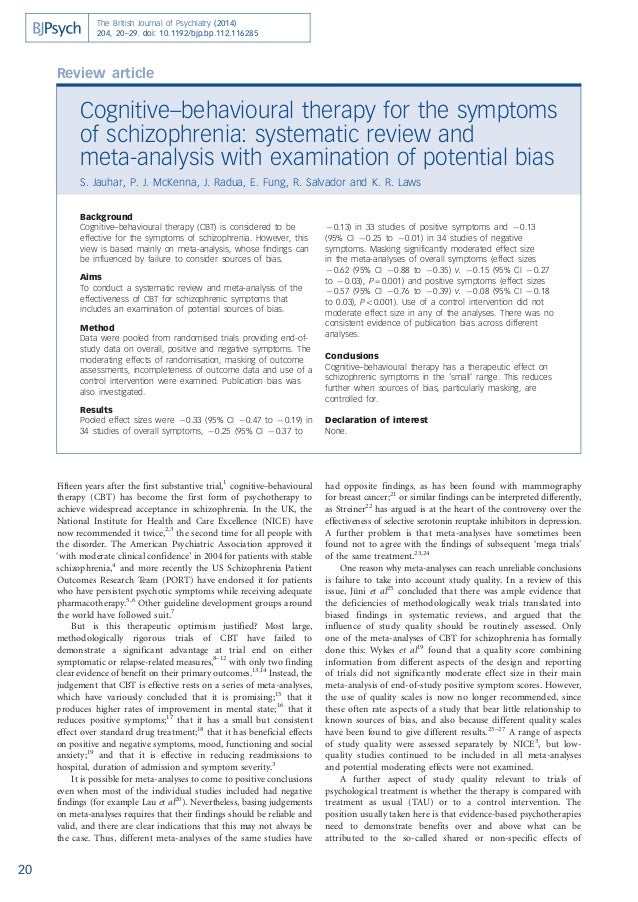
Results: Up to 40% of patients with Lyme disease develop neurologic involvement of either the peripheral or central nervous system. Dissemination to the CNS can occur within the first few weeks after skin infection. Like syphilis, Lyme disease may have a latency period of months to years before symptoms of late infection emerge. Early signs include meningitis, encephalitis, cranial neuritis, and radiculoneuropathies. Later, encephalomyelitis and encephalopathy may occur. A broad range of psychiatric reactions have been associated with Lyme disease including paranoia, dementia, schizophrenia, bipolar disorder, panic attacks, major depression, anorexia nervosa, and obsessive-compulsive disorder.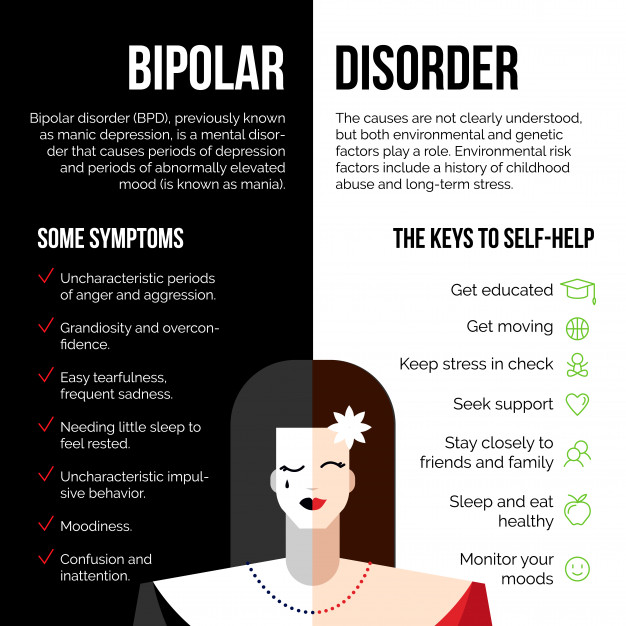 Depressive states among patients with late Lyme disease are fairly common, ranging across studies from 26% to 66%. The microbiology of Borrelia burgdorferi sheds light on why Lyme disease can be relapsing and remitting and why it can be refractory to normal immune surveillance and standard antibiotic regimens.
Depressive states among patients with late Lyme disease are fairly common, ranging across studies from 26% to 66%. The microbiology of Borrelia burgdorferi sheds light on why Lyme disease can be relapsing and remitting and why it can be refractory to normal immune surveillance and standard antibiotic regimens.
Conclusions: Psychiatrists who work in endemic areas need to include Lyme disease in the differential diagnosis of any atypical psychiatric disorder. Further research is needed to identify better laboratory tests and to determine the appropriate manner (intravenous or oral) and length (weeks or months) of treatment among patients with neuropsychiatric involvement.
Similar articles
-
[Signs and significance of a tick-bite: psychiatric disorders associated with Lyme disease].
Sno HN.
 Sno HN. Tijdschr Psychiatr. 2012;54(3):235-43. Tijdschr Psychiatr. 2012. PMID: 22422416 Review. Dutch.
Sno HN. Tijdschr Psychiatr. 2012;54(3):235-43. Tijdschr Psychiatr. 2012. PMID: 22422416 Review. Dutch. -
Nervous system Lyme disease.
Halperin JJ. Halperin JJ. Vector Borne Zoonotic Dis. 2002 Winter;2(4):241-7. doi: 10.1089/153036602321653824. Vector Borne Zoonotic Dis. 2002. PMID: 12804165 Review.
-
Psychiatric manifestations of Lyme borreliosis.
Fallon BA, Nields JA, Parsons B, Liebowitz MR, Klein DF. Fallon BA, et al. J Clin Psychiatry. 1993 Jul;54(7):263-8. J Clin Psychiatry. 1993. PMID: 8335653
-
Borrelia burgdorferi in the nervous system: the new "great imitator".
Pachner AR. Pachner AR. Ann N Y Acad Sci. 1988;539:56-64. doi: 10.1111/j.1749-6632.1988.tb31838.x. Ann N Y Acad Sci. 1988. PMID: 3190104
-
Neuro-ophthalmic manifestations of Lyme disease.
Balcer LJ, Winterkorn JM, Galetta SL. Balcer LJ, et al. J Neuroophthalmol. 1997 Jun;17(2):108-21. J Neuroophthalmol. 1997. PMID: 9176782 Review.
See all similar articles
Cited by
-
Neurological Pain, Psychological Symptoms, and Diagnostic Struggles among Patients with Tick-Borne Diseases.
Maxwell SP, Brooks C, McNeely CL, Thomas KC. Maxwell SP, et al. Healthcare (Basel). 2022 Jun 23;10(7):1178. doi: 10.3390/healthcare10071178. Healthcare (Basel).
 2022. PMID: 35885705 Free PMC article.
2022. PMID: 35885705 Free PMC article. -
Lyme Neuroborreliosis Presenting as Multiple Cranial Neuropathies.
Sriram A, Lessen S, Hsu K, Zhang C. Sriram A, et al. Neuroophthalmology. 2021 Jul 23;46(2):131-135. doi: 10.1080/01658107.2021.1951769. eCollection 2022. Neuroophthalmology. 2021. PMID: 35273419 Free PMC article.
-
Borrelia burgdorferi Co-Localizing with Amyloid Markers in Alzheimer's Disease Brain Tissues.
Senejani AG, Maghsoudlou J, El-Zohiry D, Gaur G, Wawrzeniak K, Caravaglia C, Khatri VA, MacDonald A, Sapi E. Senejani AG, et al. J Alzheimers Dis. 2022;85(2):889-903. doi: 10.3233/JAD-215398. J Alzheimers Dis. 2022. PMID: 34897095 Free PMC article.
-
Anorexia Nervosa Caused by Polymicrobial Tick-Borne Infections: A Case Study.
Kinderlehrer DA. Kinderlehrer DA. Int Med Case Rep J. 2021 May 10;14:279-287. doi: 10.2147/IMCRJ.S311516. eCollection 2021. Int Med Case Rep J. 2021. PMID: 34007219 Free PMC article.
-
Symptom heterogeneity and patient subgroup classification among US patients with post-treatment Lyme disease: an observational study.
Rebman AW, Yang T, Aucott JN. Rebman AW, et al. BMJ Open. 2021 Jan 13;11(1):e040399. doi: 10.1136/bmjopen-2020-040399. BMJ Open. 2021. PMID: 33441353 Free PMC article.
See all "Cited by" articles
Publication types
MeSH terms
Full text links
Atypon
Cite
Format: AMA APA MLA NLM
Add to Collections
- Create a new collection
- Add to an existing collection
Name your collection:
Name must be less than 100 characters
Choose a collection:
Unable to load your collection due to an error
Please try again
Send To
Lyme Disease Heightens Risk of Mental Disorders, Suicidality
A Columbia-led study advises physicians and patients be aware of psychiatric symptoms, particularly the first year after diagnosisIn a new study, U.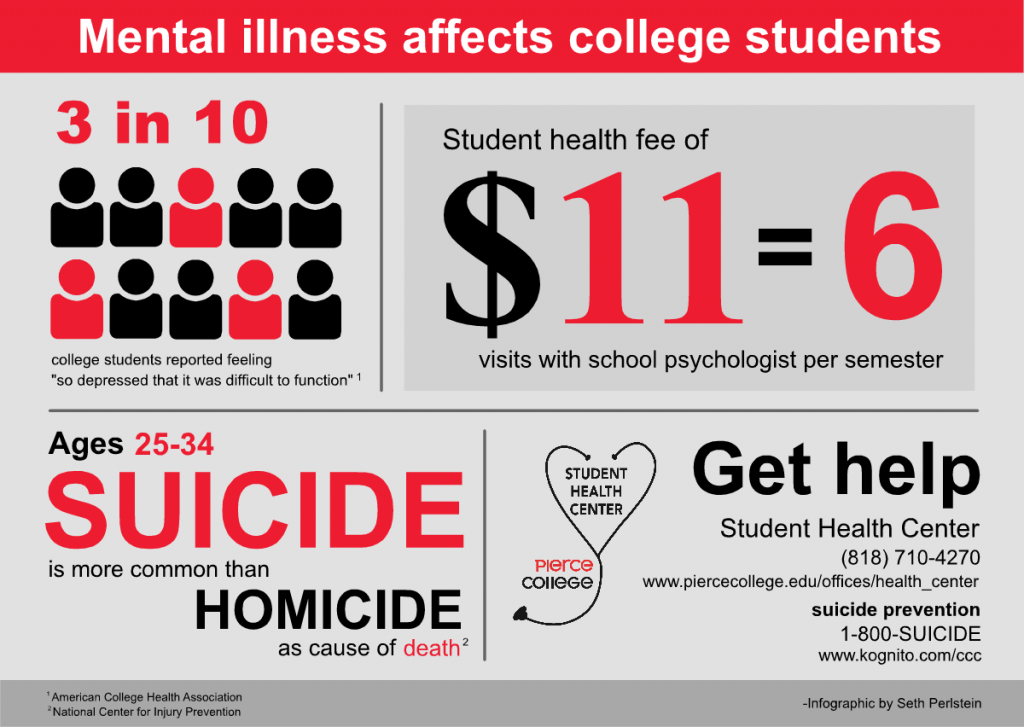 S. and Danish researchers report that patients who received a hospital diagnosis of Lyme disease—inpatient, outpatient, or at the ER—had a 28 percent higher rate of mental disorders and were twice as likely to have attempted suicide post-infection, compared to individuals without the diagnosis.
S. and Danish researchers report that patients who received a hospital diagnosis of Lyme disease—inpatient, outpatient, or at the ER—had a 28 percent higher rate of mental disorders and were twice as likely to have attempted suicide post-infection, compared to individuals without the diagnosis.
The study, a collaboration of Columbia University and the Copenhagen Research Centre for Mental Health, is believed to be the first large, population-based study examining the relationship between Lyme disease and psychiatric outcomes.
The research appears in the July 28 online edition of the American Journal of Psychiatry.
“It is time to move beyond thinking of Lyme disease as a simple illness that only causes a rash,” said Brian Fallon, MD, MPH, a psychiatrist with the New York State Psychiatric Institute and Columbia University who is the lead author of the paper. “In addition to the risk of severe cardiac, rheumatologic, and neurologic problems, Lyme disease can cause severe mental health problems as well.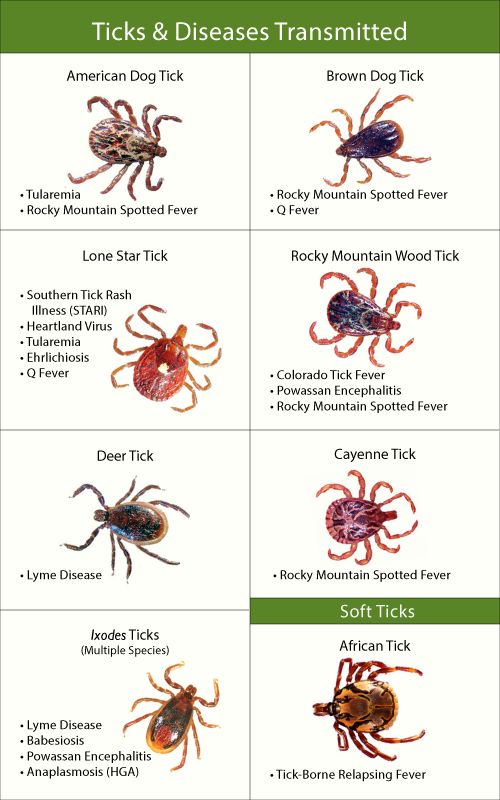 ”
”
Dr. Fallon, one of the foremost researchers of the neuropsychiatric effects of Lyme disease, is director of the Lyme and Tick-borne Diseases Research Center at Columbia. The team of investigators on the study includes Michael Benros MD, PhD, principal investigator; Trine Madsen, PhD, co-first author; and Annette Erlangsen, PhD, all psychiatric epidemiologists at the Research Centre for Mental Health.
Higher Rate of Death by Suicide
To conduct their study, the researchers analyzed the medical record diagnoses of nearly 7 million people living in Denmark over a 22-year period, comparing the mental health data of individuals after a hospital-based diagnosis of Lyme disease to the rest of the Danish population who had never had a Lyme diagnosis recorded in the national medical register.
Patients who had a history of mental disorder or suicidality prior to the Lyme disease diagnosis were excluded from the analysis.
The analysis revealed that in addition to patients with Lyme disease being at greater risk of mental disorders and suicide attempts, they also had a 42 percent higher rate of affective disorders, such as depression and bipolar disorder, and a 75 percent higher rate of death by suicide than those without the diagnosis.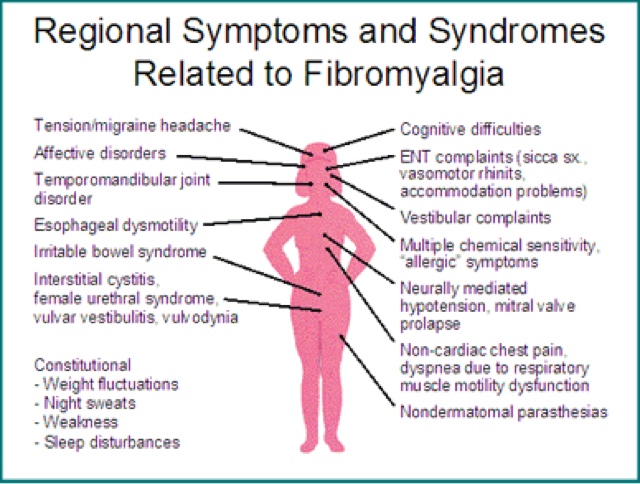
Additionally, having more than one episode of Lyme disease was associated with a higher rate of mental disorders, affective disorders, and suicide attempts.
Half a Million People Treated for Lyme Disease Each Year
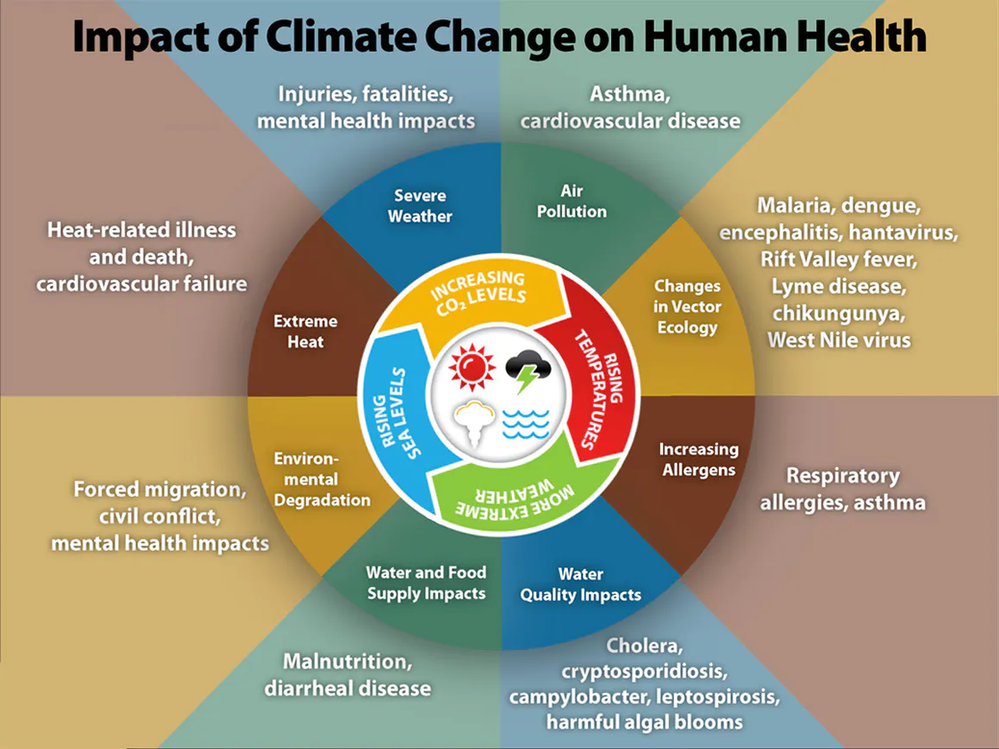
Each year nearly half a million people in the United States are diagnosed and treated for Lyme disease, also known as Lyme borreliosis, caused by a bacterium carried by deer ticks and transmitted to humans through their bite. The majority of cases have been reported in the northeastern, mid-Atlantic, and north-central states, but the geographic range where ticks and tick-borne diseases are found continues to expand.
Although most cases can be cured with a two- to four-week course of oral antibiotics, 10-20 percent of patients may suffer with symptoms of pain, fatigue, or difficulty thinking that last for months to years after treatment.
Several studies have pointed to a connection between Lyme disease and cognitive disorders months to years after antibiotic therapy or in people with untreated infections. In severe cases, individuals with late-stage Lyme disease may experience impaired concentration, irritability, memory and sleep disorders, and painful nerve dysfunction.
In severe cases, individuals with late-stage Lyme disease may experience impaired concentration, irritability, memory and sleep disorders, and painful nerve dysfunction.
Dr. Michael Benros emphasizes that most people do not develop severe mental health issues after Lyme borreliosis. During the study period, only 7 percent of the nearly 13,000 individuals with a hospital diagnosis of Lyme disease followed up with hospital clinicians complaining of symptoms subsequently diagnosed as mental disorders.
Clinicians and Patients Should Be Aware of Risk
But findings of the study, the researchers said, are emblematic of a trend in Lyme disease cases that should not be overlooked. The Danish medical registry includes only psychiatric diagnosis made in a hospital setting – not by clinicians in communities – and it is likely that the number of individuals with new onset mental health problems following infection is much higher.
“This nationwide study confirms the association between Lyme disease and psychiatric disorders,” Dr.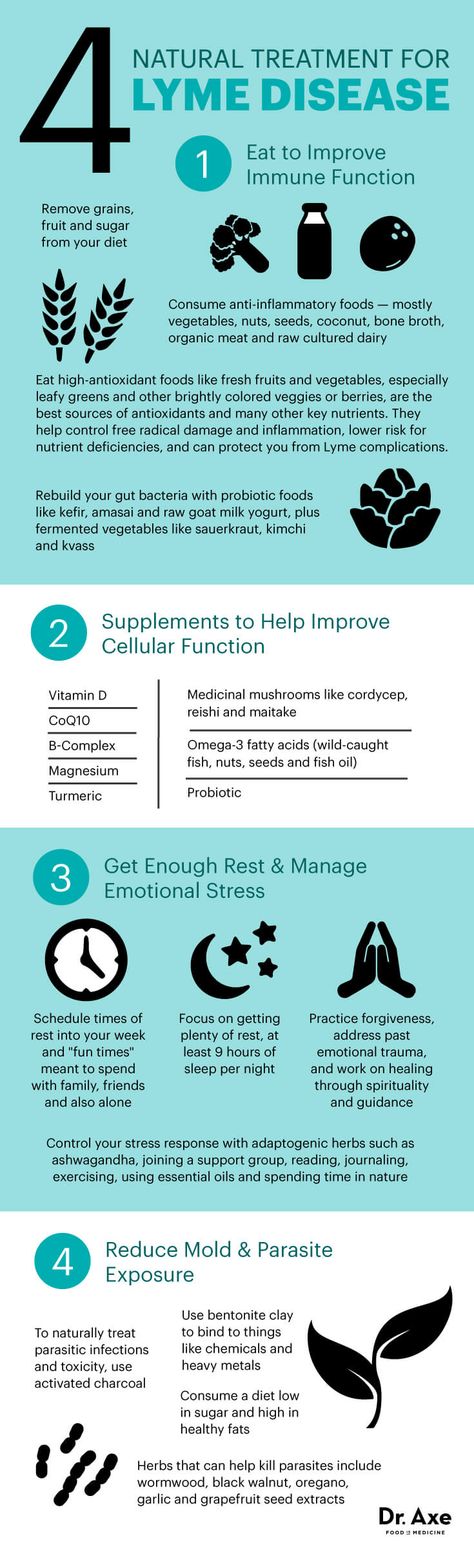 Benros said. “Treating clinicians and patients should be aware of an increased risk of mental health problems, particularly during the first year after a severe Lyme disease infection, and if mental health issues arise, patients should seek treatment and guidance. "
Benros said. “Treating clinicians and patients should be aware of an increased risk of mental health problems, particularly during the first year after a severe Lyme disease infection, and if mental health issues arise, patients should seek treatment and guidance. "
The study, “Lyme Borreliosis and Associations with Mental Disorders and Suicidal Behavior: A Nationwide Danish Cohort Study,” was funded by the Global Lyme Alliance, Inc.
– Carla Cantor
90,000 named the consequences of the mental bite for the psyche / HB- Opinions
- Business
- Podkasta
- Life
- Exclusions NV
Support Support
17 August, 2021, 14:02 9002, 14:02 9002, 14:02 9002, 14:02, 14:02, 14:02, 14:02, 14:02, 14:000 : Anton Khodorenko
American and Danish researchers report that patients who were diagnosed with Lyme disease had a 28% higher rate of mental disorders.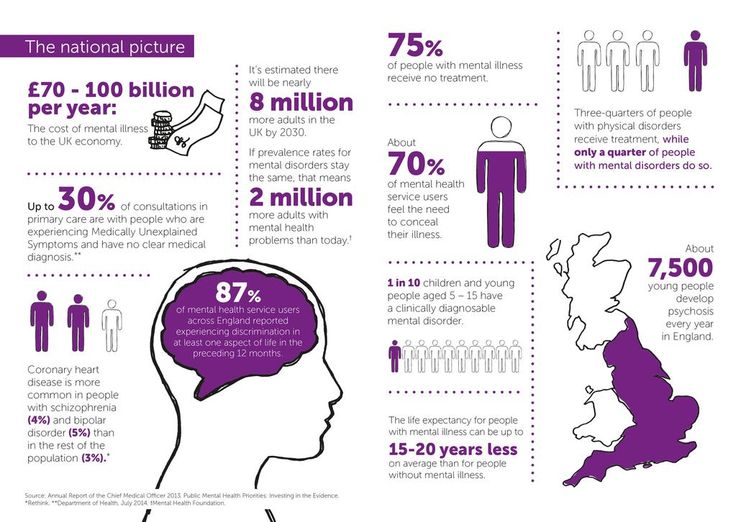
In addition, these people were twice as likely to attempt suicide after surgery compared to people without a diagnosis, according to the new study.
This study, a collaboration between Columbia University and the Copenhagen Mental Health Research Center, is considered the first large population-based study to investigate the relationship between Lyme disease and psychiatric problems.
Video of the Day
only causes a rash. In addition to the risk of serious heart, rheumatological, and neurological problems, Lyme disease can also cause serious mental health problems,” said Brian Fallon, MD, MPH, psychiatrist at the New York State Psychiatric Institute and Columbia University, who is the lead author of the paper. .
Dr. Fallon, one of the leading researchers on the neuropsychiatric effects of Lyme disease, is director of the Lyme and Tick Research Center at Columbia University.
To conduct their study, the authors analyzed the medical records of the diagnoses of almost 7 million people living in Denmark over a 22-year period, comparing the mental health data of people after a hospital diagnosis of Lyme disease with that of a population who had never had a Lyme diagnosis recorded.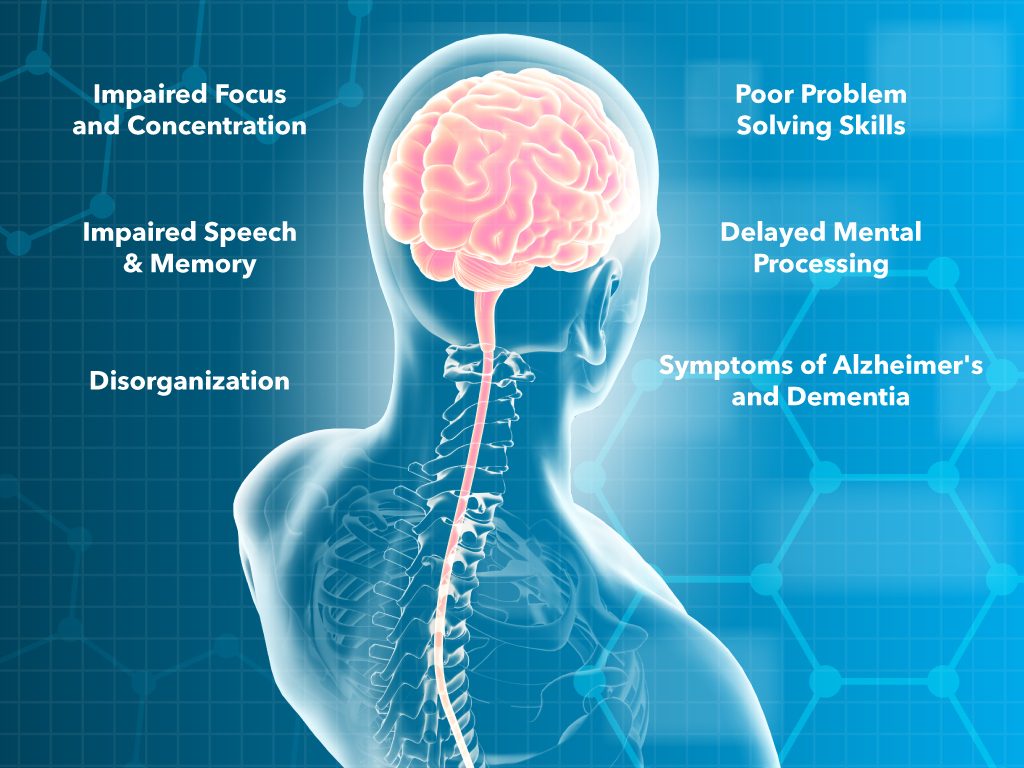 in the national medical register.
in the national medical register.
Patients with a history of psychiatric disorders or suicidal tendencies prior to the diagnosis of Lyme disease were excluded from the analysis.
The analysis showed that patients with Lyme disease, in addition to a higher risk of mental disorders and suicide attempts, also have a 42% higher rate of affective disorders such as depression and bipolar disorder, and a 75% higher rate of death from suicide than those without a diagnosis.
In addition, having more than one episode of Lyme disease was associated with higher rates of psychiatric disorders, affective disorders, and suicide attempts.
Each year, nearly half a million people in the United States are diagnosed and treated for Lyme disease, also known as Lyme borreliosis, caused by bacteria carried by ticks and transmitted to humans through tick bites.
Although most cases can be cured with a two to four week course of oral antibiotics, 10 to 20 percent of patients may experience symptoms of pain, fatigue, or difficulty thinking that persist for months or years after treatment.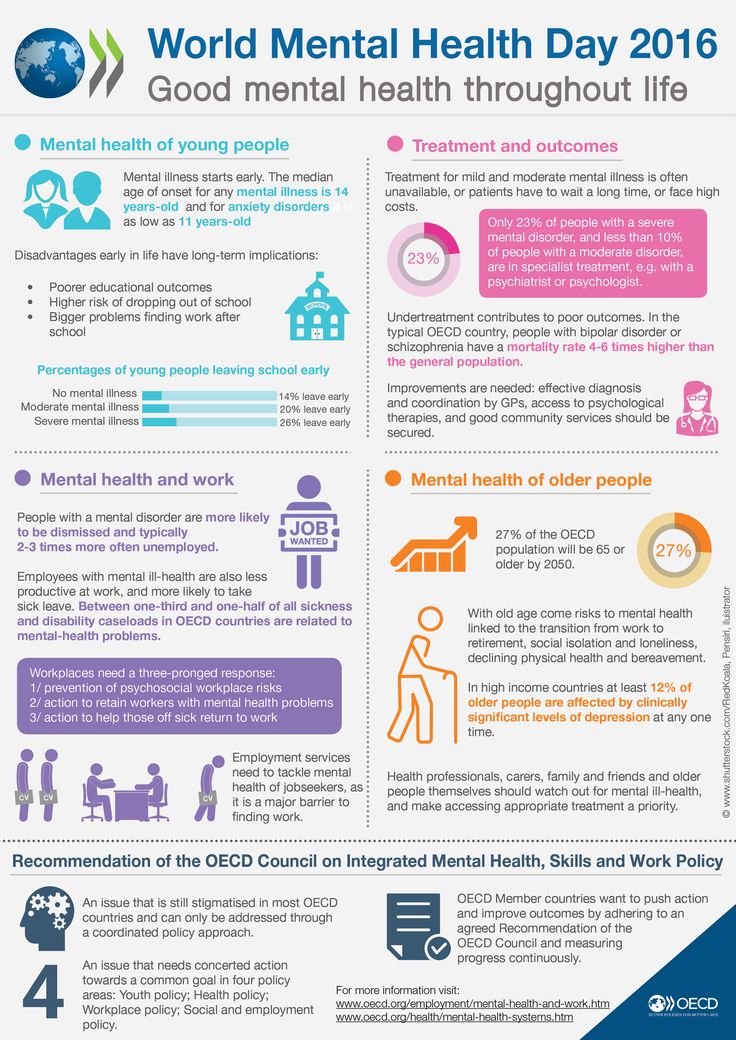
Several studies have shown an association between Lyme disease and cognitive impairment months or years after antibiotic therapy or in people with untreated infections. In severe cases, people with advanced Lyme disease may experience impaired concentration, irritability, memory and sleep disturbances, and painful nerve dysfunction.
Top News Digest
Free email newsletter of only the best content from HB 9 editors0020
Emailed Monday through Friday
Dr. Michael Benros, co-author of the paper, emphasizes that most people with Lyme borreliosis do not develop serious mental health problems. During the study period, only 7 percent of nearly 13,000 people with a hospital diagnosis of Lyme disease presented to hospital clinicians with symptoms that were later diagnosed as psychiatric disorders.
But the results of the study show a trend in Lyme cases that should not be overlooked. The Danish medical registry only includes psychiatric diagnoses made in a hospital setting and not by doctors in the community, and it is likely that the number of people with new mental health problems after infection is much higher.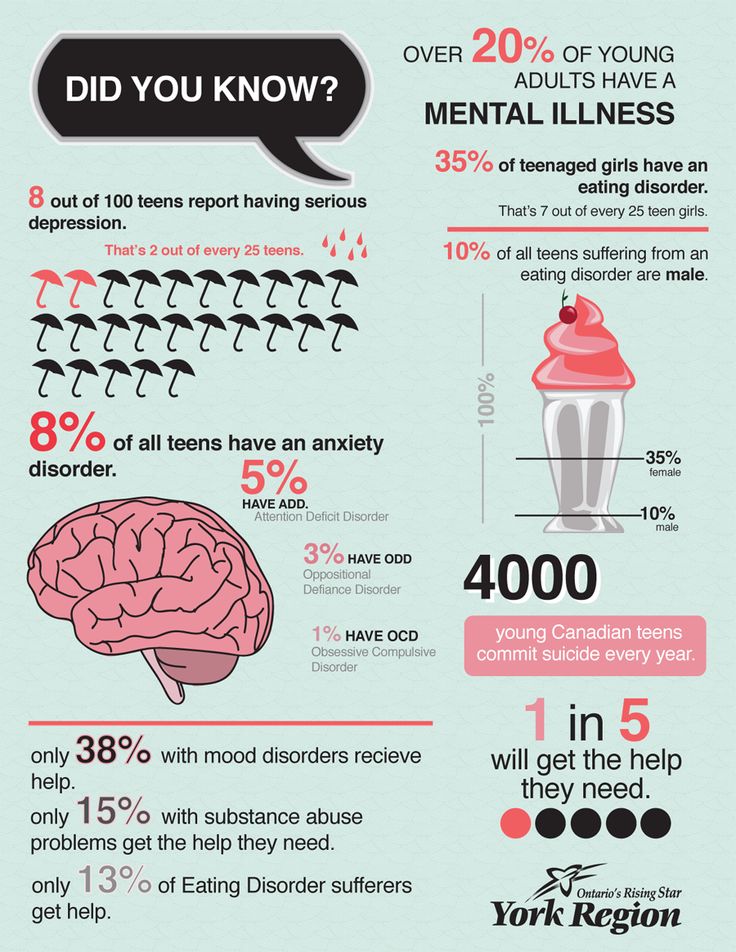
Previously HB wrote that in 2019 the first case of acute psychotic disorder was diagnosed in the UK, which was provoked by stress caused in the patient by the results of the Brexit referendum.
Due to Brexit concerns, his mental health began to deteriorate rapidly after the referendum results were announced, the article says. At first, the patient began to spend more time posting his thoughts on Brexit on social media.
It became difficult for him to come to terms with the ongoing political events and became increasingly worried about incidents of a racist nature. The man also began to sleep worse.
He went to the attending physician, who prescribed him an antidepressant and sleeping pills. This treatment did not help. The patient developed paranoia and illusions (he believed that the two different women he saw were the same person). The man became more and more worried, and when he began to scatter things at home, he was hospitalized.
Legal information. This article is for general reference only and should not be taken as a substitute for medical advice. HB is not responsible for any diagnosis made by the reader based on the materials of the site. HB is also not responsible for the content of other Internet resources, links to which are present in this article. If you are concerned about your health, see your doctor.
This article is for general reference only and should not be taken as a substitute for medical advice. HB is not responsible for any diagnosis made by the reader based on the materials of the site. HB is also not responsible for the content of other Internet resources, links to which are present in this article. If you are concerned about your health, see your doctor.
Tags: Psychiatry Suicide Lyme disease tick bite
Show more news
About the use of cookies
By continuing to browse NV.ua you confirm that you have read the Terms of Use of the site and agree to the use of cookies
About cookies
Lyme disease - QBQVET
Lyme disease Borreliosis is a bacterial infection carried by ixodid ticks. Until now, there is an opinion that you can get Lyme disease only on the east coast of the United States, however, at present, the habitat of ixodid ticks and, as a result, the geography of infection with Lyme disease has expanded significantly.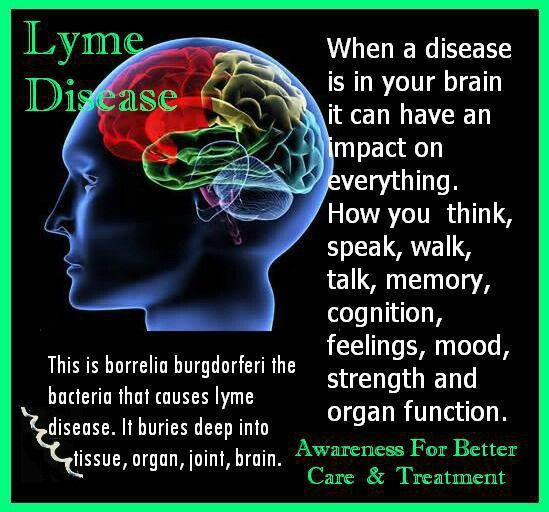 Today, Lyme disease occurs in more than 60 countries around the world.
Today, Lyme disease occurs in more than 60 countries around the world.
Here are some numbers. The US Centers for Disease Control and Prevention estimates that about 300,000 patients are diagnosed with Lyme disease every year. At the same time, it must be borne in mind that often the disease is latent, so it is quite difficult to diagnose it. Thus, many doctors are of the opinion that the real number of patients is much higher. For comparison, here are the statistics for Russia. According to official data, about 10,000 cases of borreliosis infection were detected in the previous year. Naturally, the number of undetected cases is many times greater.
Lyme disease affects everyone, regardless of age. The risk group includes children, the elderly and those whose profession is somehow connected with being outdoors in places where ticks are found.
What is Lyme disease?
The causative agent of borreliosis is a spirochete - a spiral bacterium Borrelia burgdorferi. A feature of the disease is that at first it proceeds without symptoms or disguises itself as other diseases. The disease can affect any of the organs, incl. on the brain and nervous system, muscles and joints, heart.
A feature of the disease is that at first it proceeds without symptoms or disguises itself as other diseases. The disease can affect any of the organs, incl. on the brain and nervous system, muscles and joints, heart.
Patients with chronic Lyme disease often present with symptoms such as chronic fatigue, fibromyalgia, multiple sclerosis, and a range of mental illnesses, including depression.
Mechanisms of infection.
Lyme disease is transmitted to most people by the bite of a nymph tick (the growth stage of the tick between larva and adult).
After a tick bite, it can remain attached for several days, and the longer it remains on the body, the more likely it is to transmit borreliosis and other pathogens.
In case of infection during pregnancy, transmission of the disease to the child is possible. Other mechanisms of transmission of the disease from person to person are not yet known.
Distribution area of the disease.
Currently, Lyme disease occurs on every continent except Antarctica. The world's largest focus of the disease is located in the northeastern United States, in Russia the main focus is the Tomsk region. However, a sharp increase in the incidence is recorded in the Leningrad, Kostroma, Yaroslavl, Vologda, Kirov, Perm, Sverdlovsk regions, the Komi-Permyatsk Autonomous Okrug, the Republic of Mari El, and Udmurtia
The world's largest focus of the disease is located in the northeastern United States, in Russia the main focus is the Tomsk region. However, a sharp increase in the incidence is recorded in the Leningrad, Kostroma, Yaroslavl, Vologda, Kirov, Perm, Sverdlovsk regions, the Komi-Permyatsk Autonomous Okrug, the Republic of Mari El, and Udmurtia
Not all ticks carry Lyme disease. In the same areas, studies of different samples of ticks show infection rates from 0% to 70%. Because of this, it is quite difficult to determine the actual number of infected ticks and, as a result, to predict the risk of morbidity.
How to minimize the risk of infection.
If possible, try to refrain from walking in the forest in regions where ticks are most common during the period of their greatest activity, namely in April-June.
Treat clothes with acaricide before going out. In order to protect your pets, use special drops from ticks. Take a good look at yourself after the walk.