Lists of mental disorders and symptoms
Types of mental health issues and illnesses
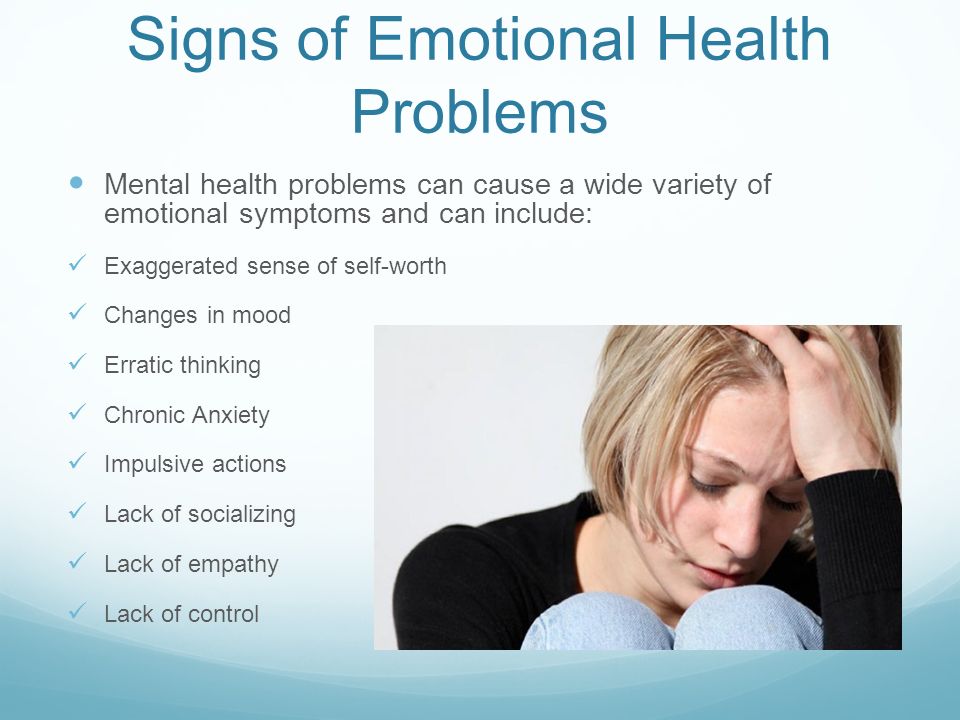
Mental illness is a general term for a group of illnesses that may include symptoms that can affect a person’s thinking, perceptions, mood or behaviour. Mental illness can make it difficult for someone to cope with work, relationships and other demands.
The relationship between stress and mental illness is complex, but it is known that stress can worsen an episode of mental illness. Most people can manage their mental illness with medication, counselling or both. This page lists some of the more common mental health issues and mental illnesses.
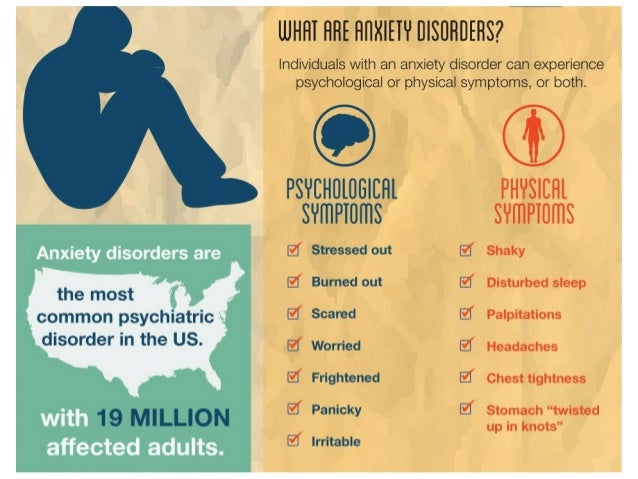
Anxiety disorders
Anxiety disorders are a group of mental health disorders that includes:
- generalised anxiety disorders
- social phobias
- specific phobias (for example, agoraphobia and claustrophobia)
- panic disorders
- obsessive compulsive disorder (OCD)
- post-traumatic stress disorder (PTSD).
Untreated, anxiety disorders can lead to significant impairment on people’s daily lives.
For more information see: Anxiety disorders.
Behavioural and emotional disorders in children
Common behaviour disorders in children include:
- oppositional defiant disorder (ODD)
- conduct disorder (CD)
- attention deficit hyperactivity disorder (ADHD).
Treatment for these mental health disorders can include therapy, education and medication.
For more information see: Behavioural disorders in children.
Bipolar affective disorder
Bipolar affective disorder is a type of mood disorder, previously referred to as ‘manic depression’. A person with bipolar disorder experiences episodes of mania (elation) and depression. The person may or may not experience psychotic symptoms. The exact cause is unknown, but a genetic predisposition has been clearly established. Environmental stressors can also trigger episodes of this mental illness.
For more information see: Bipolar disorder.
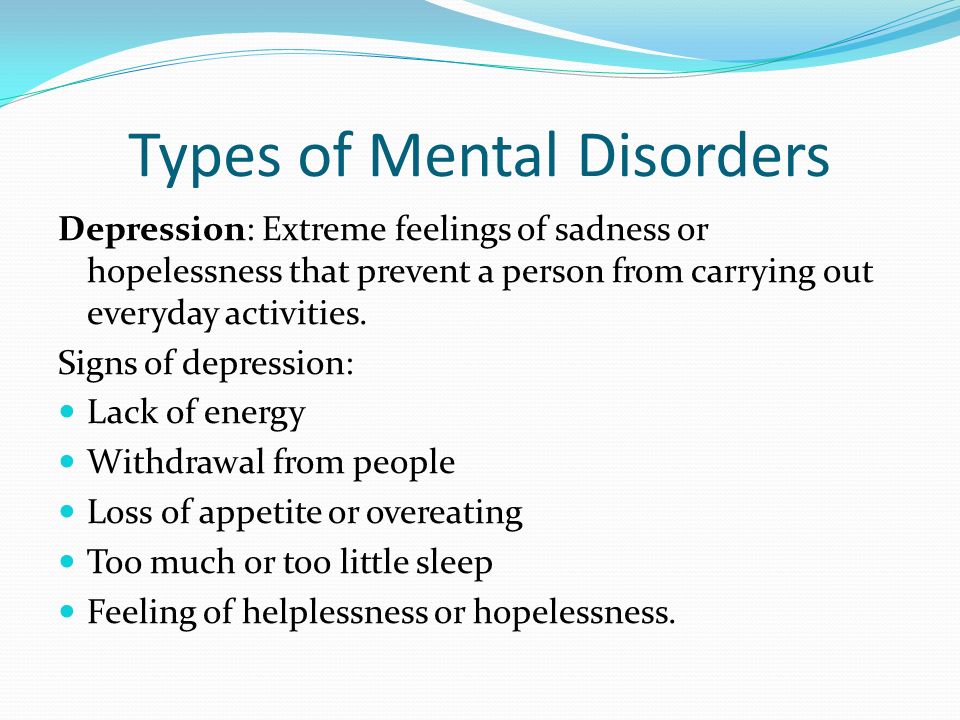
Depression
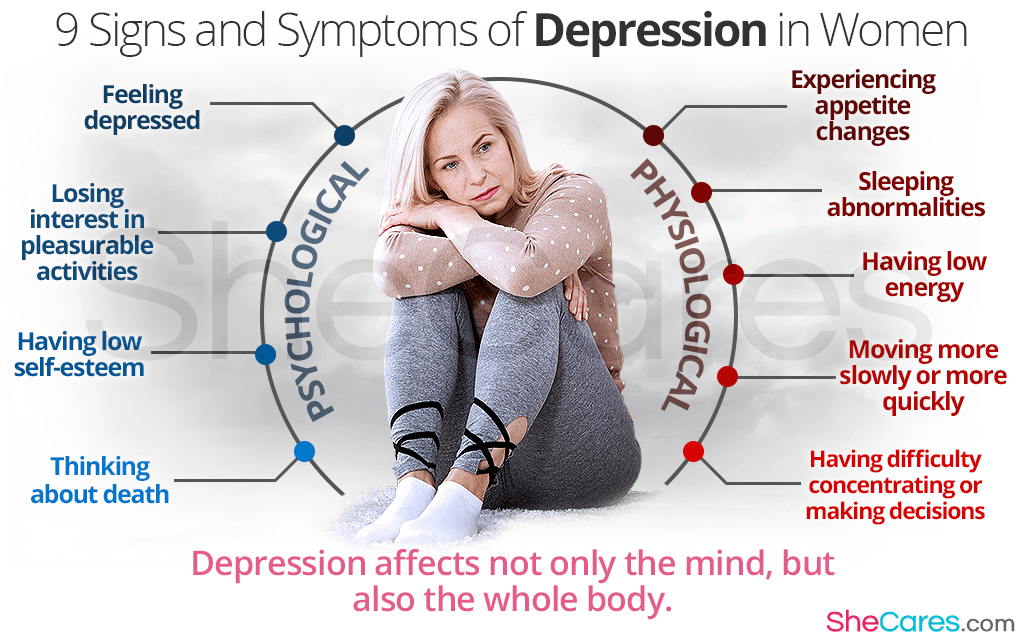
Depression is a mood disorder characterised by lowering of mood, loss of interest and enjoyment, and reduced energy.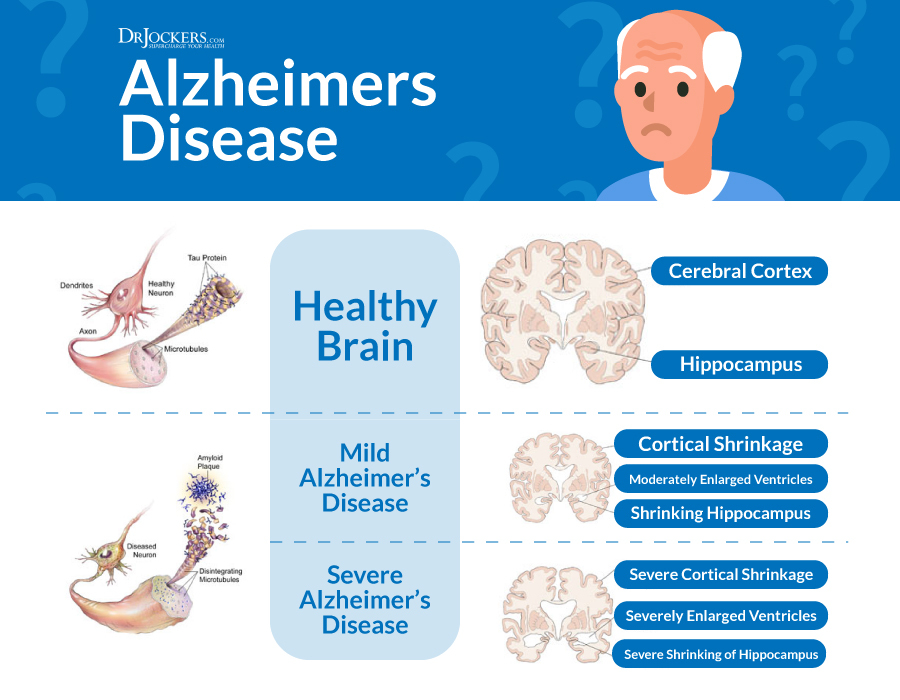 It is not just feeling sad. There are different types and symptoms of depression. There are varying levels of severity and symptoms related to depression. Symptoms of depression can lead to increased risk of suicidal thoughts or behaviours.
It is not just feeling sad. There are different types and symptoms of depression. There are varying levels of severity and symptoms related to depression. Symptoms of depression can lead to increased risk of suicidal thoughts or behaviours.
For more information see: Depression.
Dissociation and dissociative disorders
Dissociation is a mental process where a person disconnects from their thoughts, feelings, memories or sense of identity. Dissociative disorders include dissociative amnesia, depersonalisation disorder and dissociative identity disorder.
For more information see: Dissociation and dissociative disorders.
Eating disorders
Eating disorders include anorexia, bulimia nervosa and other binge eating disorders. Eating disorders can affect people of all ages and genders, and can have serious psychological and physical consequences.
For more information see: Eating disorders.
Obsessive compulsive disorder
Obsessive compulsive disorder (OCD) is an anxiety disorder.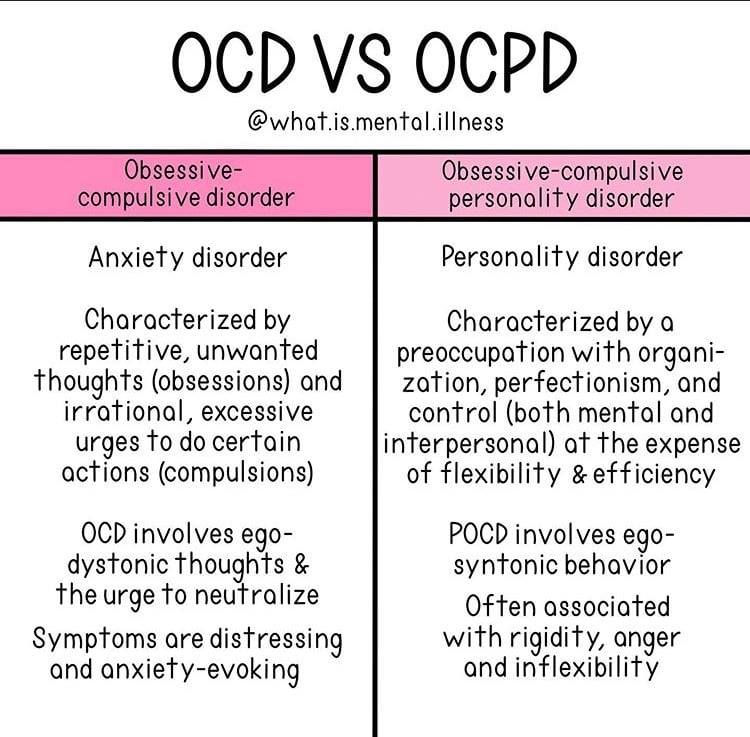 Obsessions are recurrent thoughts, images or impulses that are intrusive and unwanted. Compulsions are time-consuming and distressing repetitive rituals.
Obsessions are recurrent thoughts, images or impulses that are intrusive and unwanted. Compulsions are time-consuming and distressing repetitive rituals.
Treatments include cognitive behaviour therapy (CBT) and medications.
For more information see: Obsessive compulsive disorder.
Paranoia
Paranoia is the irrational and persistent feeling that people are ‘out to get you’. Paranoia may be a symptom of conditions including paranoid personality disorder, delusional (paranoid) disorder and schizophrenia.
Treatment for paranoia includes medications and psychological support.
For more information see: Paranoia.
Post-traumatic stress disorder
Post-traumatic stress disorder (PTSD) is a mental health condition that can develop as a response to people who have experienced any traumatic event. This can be a car or other serious accident, physical or sexual assault, war-related events or torture, or natural disasters such as bushfires or floods.
For more information see: Post-traumatic stress disorder (PTSD).
Psychosis
People affected by psychosis can experience delusions, hallucinations and confused thinking. Psychosis can occur in a number of mental illnesses, including drug-induced psychosis, schizophrenia and mood disorders. Medication and psychological support can relieve, or even eliminate, psychotic symptoms.
For more information see: Psychosis.
Schizophrenia
Schizophrenia is a complex psychotic disorder characterised by disruptions to thinking and emotions, and a distorted perception of reality. Symptoms of schizophrenia vary widely but may include hallucinations, delusions, thought disorder, social withdrawal, lack of motivation and impaired thinking and memory.
People with schizophrenia have a high risk of suicide. Schizophrenia is not a split personality.
For more information see: Schizophrenia.
Where to get help
- In an emergency, always call triple zero (000)
- Your GP (doctor)
- Psychiatrist
- Psychologist
- LifelineExternal Link Tel.
 13 11 14 – Australia-wide crisis support and prevention service
13 11 14 – Australia-wide crisis support and prevention service - beyondblueExternal Link Tel. 1300 22 4636 – support for issues relating to anxiety and depression
- SANE AustraliaExternal Link Tel. 1800 18 SANE (7263)
- Mental Health Foundation of Australia (Victoria)External Link Tel. (03) 9427 0406
- Anxiety Recovery Centre VictoriaExternal Link Tel. (03) 9830 0533 or 1300 ANXIETY (1300 269 438)
- Kids HelplineExternal Link Tel. 1800 55 1800 – free counselling for young people between the ages of 5 and 25
Psychosis and mental illness - Better Health Channel
Summary
Read the full fact sheet- People experiencing psychosis are unable to distinguish what is real.
- Psychosis is associated with a number of illnesses that affect the brain.
- Medication and community support can relieve, or even eliminate, psychotic symptoms.
Around three per cent of people will experience a psychotic episode at some point in their life. In any given 12-month period, just under one in every 200 adult Australians will experience a psychotic illness.
The period of time where people experience psychotic symptoms is known as an ‘episode’ of psychosis. Some people only experience a few episodes of psychosis, or a brief episode that lasts for a few days or weeks. Others will experience symptoms more frequently, in association with a longer-term illness such as schizophrenia.
The first episode of psychosis usually occurs in a person's late teens or early 20s.
Symptoms of psychosis
Symptoms of psychosis include:
- confused thinking
- delusions – false beliefs that are not shared by others
- hallucinations – hearing, seeing, smelling or tasting something that isn't there
- changed behaviours and feelings.
Confused thinking and psychosis
During an episode of psychosis a person’s thoughts become confused. Words and ideas lose their meaning or take on meanings that make no sense.
Words and ideas lose their meaning or take on meanings that make no sense.
These disturbances in thinking can affect a person's ability to concentrate, remember things and make plans. Confused thinking can continue, even after the psychotic episode has ended.
You may be able to tell that someone is having an episode of psychosis through changes in their speech. These may include:
- speaking very quickly or slowly
- changing topics frequently
- speaking in muddled-up sentences
- using the wrong words to describe things
- making up words.
Delusions and psychosis
Delusions are false beliefs that are not shared by others. Delusions can take various forms, including:
- paranoid delusion – for example, the person believes they are being watched and singled out for some harmful purpose
- grandiose delusion – for example, the person believes they have special powers or that they are an important religious or political figure
- reference delusion – for example, the person believes they are receiving special messages or codes through media such as TV shows, songs or advertising
- control delusion – for example, the person believes their thoughts are being controlled or influenced by outside forces such as aliens, some real or invented group, an individual or something more vague
- somatic delusion – for example, the person believes something has happened to their body – something is wrong with it, some part of it is missing or dead, they have a disease or are infested with parasites
- depressive delusion – for example, the person believes they are guilty of some terrible crime.
Hallucinations and psychosis
A hallucination is when someone hears, sees, smells or tastes something that isn't there. A common form of hallucination is to hear voices that aren't there. Hallucinations can lead to agitation, distress, frustration and even hostility.
Changed behaviour and psychosis
Psychosis can affect a person’s behaviour. A person with psychosis may experience:
- social isolation or becoming withdrawn
- problems with work, social or family life
- problems with motivation
- problems with increased activity
- laughing at inappropriate times or becoming upset without an identifiable cause.
Changed feelings and psychosis
Psychosis can lead to changes in emotions. How a person feels can change for no obvious reason. Examples may include:
•feeling strange and cut off from the world
•mood swings, feeling unusually excited or depressed
•feeling or showing less emotion
•feeling distanced or detached from one's body or thoughts
Types of psychotic illness
There are a number of mental illnesses where psychotic symptoms can be present. Examples include:
Examples include:
- brief reactive psychosis – psychotic symptoms that arise due to a very stressful event and last less than a month
- drug induced psychosis – caused by drugs such as alcohol, speed, LSD, marijuana, ecstasy or magic mushrooms. The symptoms last until the effects of the drugs wear off (hours or days)
- schizophrenia – most people affected by schizophrenia experience a range of psychotic symptoms and commonly have difficulty organising their thoughts
- bipolar disorder – involves very extreme moods (either very high or very low) that can lead to psychotic symptoms
- psychotic depression – depression can be so intense that it causes psychotic symptoms.
Causes of psychosis
The causes of psychosis are not fully understood. It is likely that psychosis is caused by a number of factors including:
- genetic vulnerability – family history of psychotic disorder
- chemical imbalance in the brain
- substance use, particularly cannabis, speed or ice
- environmental factors
- psychosocial stress – for people who have had an episode of psychosis, significant stress may be a factor in the development of further episodes.

Diagnosis of psychosis
The presence of psychotic symptoms does not automatically mean that someone has a psychotic disorder.
To diagnose a psychotic disorder, a mental health professional will do a comprehensive medical and psychological assessment over time. This can be done either at home or in hospital. They will check for psychosis caused by drugs or other diseases first.
Treatment for psychosis
Treatment can do much to relieve, or even eliminate, the symptoms of psychosis. Treatments include:
- medication – certain medications such as anti-psychotics help the brain to restore its normal chemical balance
- community support programs – ongoing support may be needed to help a person experiencing psychosis to live independently in the community. Support may include help with accommodation, finding suitable work, and the development of social and personal skills
- psychological therapies such as psychotherapy, cognitive-behaviour therapy, family therapy and counselling are aimed at teaching skills and techniques for coping with stress, improving quality of life and helping people to manage their symptoms
- self-help and peer support groups
- lifestyle changes – such as improving general health and reducing stress through activities such as art, music and exercise can support recovery.
 Avoiding drugs and alcohol and getting good sleep can also help.
Avoiding drugs and alcohol and getting good sleep can also help.
Where to get help
- Your GP (doctor)
- Psychiatrist
- Your local mental health service
- SANE AustraliaExternal Link Tel. 1800 18 SANE (7263) Monday to Friday, 10 am – 10 pm
- Need Help? Chat live with a SANE Helpline AdvisorExternal Link (Available Monday-Friday, 10am-10pm AEST).
- SANE ForumsExternal Link are full of people who want to talk to you and offer support.
- PsychosisExternal Link, SANE Australia, Melbourne.
- Understanding mental health conditions – psychosisExternal Link, Mind Australia.
- Psychotic disorder assessment and treatmentExternal Link, headspace, National Youth Mental Health Foundation, Australia.
- PsychosisExternal Link, Orygen, The National Centre of Excellence in Youth Mental Health, Australia.
- Perala J, Suvisaari J, Saarni SI, et al. 2007 ‘Lifetime prevalence of psychotic and bipolar I disorders in a general populationExternal Link’, Archives of General Psychiatry, vol.
 64, no. 1, pp. 19–28.
64, no. 1, pp. 19–28.
This page has been produced in consultation with and approved by:
Types of mental disorders
Call us
Make an appointment
- Main page
- Psychiatry
- Types of mental disorders
- Types of mental disorders
Aggressive behavior
accompanies many mental illnesses. Manifested in hostility, threats and attacks. If these symptoms arose in a person for the first time and are generally not characteristic of him, most likely, he needs to immediately consult a psychiatrist. In other cases of aggressive behavior (especially - unreasonable) consultation with a psychiatrist is also desirable.
Apathy of the mentally ill
state of indifference, detachment, loss of interest and desire to do something. It is often a manifestation of depression, while it is painfully experienced. If apathy does not burden the patient, then this may be a manifestation of another mental or neurological disease.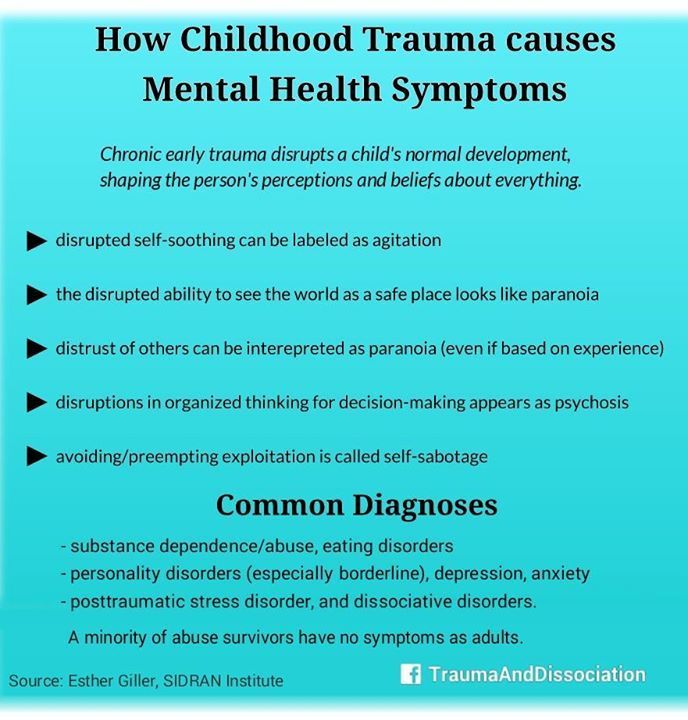
Autism
Autism is a condition in which a person lives in an internal or unreal (virtual) world, and not in real events. Close such a person is seen as closed, uninterested in what is happening around, closed. The world of fantasy overlaps reality, and therefore a person with autism is cold and indifferent to the people around him, including those close to him. An autistic person is often not burdened by the difficulties of social interaction and communication disorders. Autism occurs both in childhood and in adulthood, and in adults it can be not only a “continuation” of childhood autism, but also a consequence of a developed mental disorder.
Delirium tremens (delirium)
occurs mainly in patients with alcoholism, at the second or third stage of the disease. It is important to note that delirium occurs more often not in intoxication, but on the 2nd-3rd day of abstinence from alcohol after drinking (at the peak of the withdrawal syndrome). It is characterized by confusion, increased body temperature, disorientation, agitation, vision of various hallucinatory images. For patients with delirium tremens, hallucinatory images of moving animals (running rats, cockroaches, gnomes, etc.) are characteristic. Patients attract attention to themselves by their behavior: they are agitated, excited, try to catch hallucinatory images or brush them off, shake them off themselves, often talk to them.
For patients with delirium tremens, hallucinatory images of moving animals (running rats, cockroaches, gnomes, etc.) are characteristic. Patients attract attention to themselves by their behavior: they are agitated, excited, try to catch hallucinatory images or brush them off, shake them off themselves, often talk to them.
Delirium tremens is also possible in non-drinkers, especially in children and the elderly with diseases that occur with a high temperature. Thus, delirium tremens is a sign of intoxication of the body.
Insomnia
in chronically current mental disorders is an indicator of deterioration in mental well-being, since it often appears before all other symptoms.
Crazy ideas (strange judgments, delirium)
are most often perceived by close and surrounding people as strange judgments that do not correspond to reality. At the same time, a person with delusions cannot be persuaded, even if he does not know what to object to attempts to persuade him.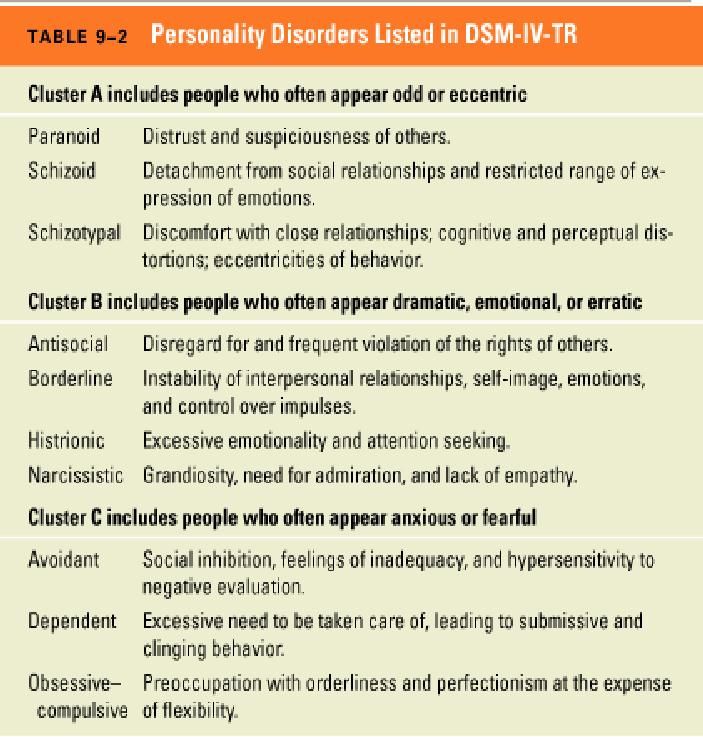 Crazy ideas don't need proof. It is rather "knowledge", conviction. Because of this, the behavior of a person with delusional ideas is determined by the content of these ideas. According to the content, the main forms of delusions can be divided into delusions of persecution (what is popularly called “persecution mania”: the patient is pursued by special services or other organizations, they try to poison or rob relatives or neighbors; people on the street somehow in a special way, look unfriendly and whisper about him), delusions of grandeur (the patient is the heir to the royal family, the inventor of the time machine or the law of immortality, the ruler of the world, sometimes the messenger of God or God himself, or the devil, etc.) and delusions of self-abasement (accusing oneself of sins, numerous errors, delirium of a physical defect). A patient with delusional judgments needs to be treated by a psychiatrist.
Crazy ideas don't need proof. It is rather "knowledge", conviction. Because of this, the behavior of a person with delusional ideas is determined by the content of these ideas. According to the content, the main forms of delusions can be divided into delusions of persecution (what is popularly called “persecution mania”: the patient is pursued by special services or other organizations, they try to poison or rob relatives or neighbors; people on the street somehow in a special way, look unfriendly and whisper about him), delusions of grandeur (the patient is the heir to the royal family, the inventor of the time machine or the law of immortality, the ruler of the world, sometimes the messenger of God or God himself, or the devil, etc.) and delusions of self-abasement (accusing oneself of sins, numerous errors, delirium of a physical defect). A patient with delusional judgments needs to be treated by a psychiatrist.
Excitement or agitation
frequent and rather dangerous signs of mental disorders. Accompany anxiety, depression, psychotic states. With motor arousal in depressed patients, one should be on the alert: suicidal actions are possible. You should also be especially attentive to patients with psychotic arousal: impulsive (unpredictable), including aggressive actions are frequent, which can be dangerous both for the patient and for his environment.
Accompany anxiety, depression, psychotic states. With motor arousal in depressed patients, one should be on the alert: suicidal actions are possible. You should also be especially attentive to patients with psychotic arousal: impulsive (unpredictable), including aggressive actions are frequent, which can be dangerous both for the patient and for his environment.
Hallucinations
perception of something that is not really there. Hallucinations are:
- visual (a person "sees" something that is not there: animals running around the house, people, paintings, sometimes whole panoramas: landscapes, battles),
- auditory (a person "hears" extraneous sounds - music, rustles , voices; at the same time, sounds can be localized both in external space: from the corner of the room, behind the wall, from the street, and inside the head, less often - another part of the body),
- olfactory (perception of foreign odors, more often - unpleasant)
- gustatory (strange, often unpleasant taste sensations)
- tactile (for example, sensation on the skin of "crawling" insects; accompanied by scratching, is a sign of serious intoxication)
Dementia (dementia)
, deterioration in the ability to judge and infer.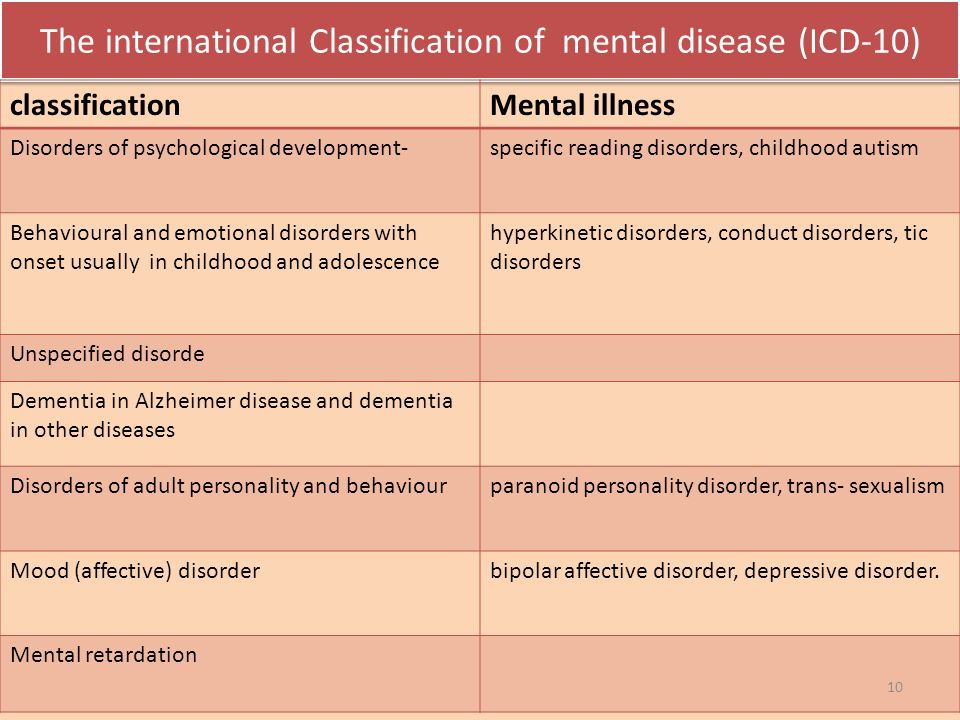 It usually occurs in old age. It can begin imperceptibly: with difficulty remembering words, narrowing the scope of attention, a slight change in mood (quick transitions from tearfulness to joy and back). The character gradually changes: the person becomes more stubborn, but at the same time more suggestible. The vocabulary is depleted, the stock of knowledge is depleted. The most common cause of dementia is damage to the cerebral vessels by an atherosclerotic process, as a result of which the vessels become narrower and blood flow to the brain tissues worsens. Having noticed in time, such changes can be stopped by properly selected therapy (which will also be the prevention of strokes). However, you should be careful if someone close to you has such changes in adulthood and unfolds very quickly: this may be a more complex disease (for example, Alzheimer's disease).
It usually occurs in old age. It can begin imperceptibly: with difficulty remembering words, narrowing the scope of attention, a slight change in mood (quick transitions from tearfulness to joy and back). The character gradually changes: the person becomes more stubborn, but at the same time more suggestible. The vocabulary is depleted, the stock of knowledge is depleted. The most common cause of dementia is damage to the cerebral vessels by an atherosclerotic process, as a result of which the vessels become narrower and blood flow to the brain tissues worsens. Having noticed in time, such changes can be stopped by properly selected therapy (which will also be the prevention of strokes). However, you should be careful if someone close to you has such changes in adulthood and unfolds very quickly: this may be a more complex disease (for example, Alzheimer's disease).
Dysmorphophobia / dysmorphomania
experiences, the content of which is the belief in one's own physical inferiority: a cosmetic defect, overweight, bad smell, in a word, a repulsive appearance. If a defect in appearance really does take place, and in a person’s life this circumstance is predominant, then we are talking about dysmorphophobia (a neurotic level of disorder). If there is actually no defect in appearance, or it is, but not so significant, and at the same time the person is downright convinced of his own ugliness, is seized by ideas of a physical defect, goes to doctors and even undergoes surgery with plastic surgeons, or falls into anorexia ( when convinced of excessive fullness), then here we are talking about dysmorphomania (delusional level of disorders).
If a defect in appearance really does take place, and in a person’s life this circumstance is predominant, then we are talking about dysmorphophobia (a neurotic level of disorder). If there is actually no defect in appearance, or it is, but not so significant, and at the same time the person is downright convinced of his own ugliness, is seized by ideas of a physical defect, goes to doctors and even undergoes surgery with plastic surgeons, or falls into anorexia ( when convinced of excessive fullness), then here we are talking about dysmorphomania (delusional level of disorders).
Hypochondria
state of increased concern about one's health. In this case, the disease of the body may or may not be present. A person suffering from hypochondria, as a rule, is afraid of a specific disease, but can also "generally" feel sick and "find" various diseases in himself (Moliere's "imaginary patient"). He constantly listens to his inner feelings and cannot experience pleasure simply from the process of life.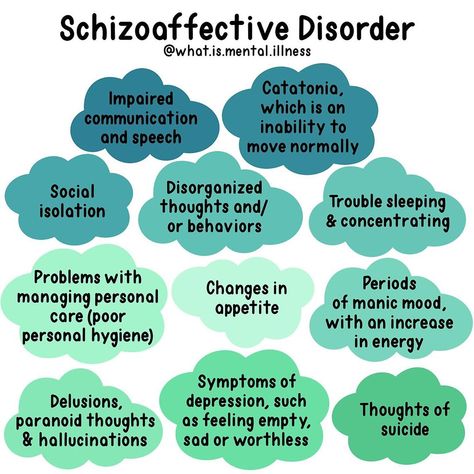 In general, hypochondria can be described as "the experience of Illness."
In general, hypochondria can be described as "the experience of Illness."
Treatment of anorexia
stubborn desire to limit oneself in food intake in order to lose weight. Often accompanied by the induction of artificial vomiting after eating, overly active physical exercises, taking large doses of laxatives. It occurs both with increased and with normal body weight. It is observed more often in girls. It is important to note that at first, anorexic behavior is carefully hidden from others, and is recognized by loved ones already at the stage of severe exhaustion.
Treatment of bulimia
How do you know if a person has bulimia? Often a person does not admit to the last that he overeats, tries to keep his addiction a secret. He is sure that he can solve the problem of nutrition on his own, by an effort of will. Signs of bulimia. Wolf hunger is a condition in which there is an uncontrolled intake of a huge amount of food. The lack of selectivity in food is characteristic, while saturation is not felt. As a rule, it occurs after a period of strict food abstinence, and, in fact, is the “back side” of anorexia.
As a rule, it occurs after a period of strict food abstinence, and, in fact, is the “back side” of anorexia.
Treatment of chronic depression
Not all depression can be cured by psychotherapy alone. Sometimes a temporary intake of specially selected drugs is required. Signs of the severity of depression are: suicidal tendencies, a feeling of despair, self-accusatory statements, anxious arousal, a feeling of general bodily change, physically experienced longing, as well as a painful loss of emotions (love, joy, compassion).
Persecution mania
without good reason are signs of a mental disorder. Such patients often hide their experiences, and then these disorders can be suspected by their behavior: a wary look, anxiety, fearfulness, absent-mindedness, window coverings, listening to something.
Unexplained somatic complaints
It happens (and more often lately) that a person feels physically ill, but no doctor finds a pathology in him. In this case, consultation with a psychiatrist is necessary: depression, neurosis, and an unresolved internal conflict may be hidden behind inexplicable somatic complaints.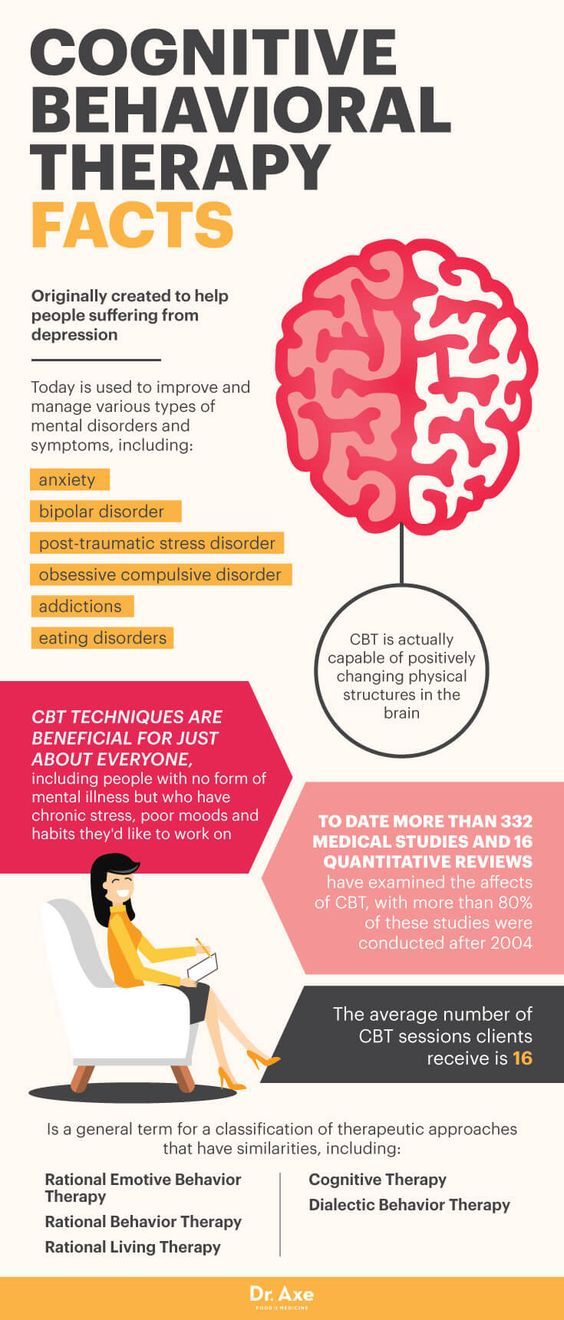
Sloppiness (neglect of hygiene)
occurs in patients with depression, psychosis, as well as chronically ongoing mental illness (schizophrenia, progressive dementia).
Fatigue
Fatigue can be a sign of both physical illness and mental illness. It is often noted in disorders of the depressive circle, while the patient may not feel a noticeable decrease in mood, but feels increasing lethargy, fatigue, inability to cope with the usual stress.
Loss of memory
is typical for the elderly, as well as those who have suffered severe traumatic brain injury, patients with alcoholism. It is a sign of a brain disease (vascular damage by atherosclerosis, atrophic processes in the cerebral cortex, past brain injuries, alcohol intoxication).
In vascular diseases in the elderly, forgetfulness of current and recent events and facts is characteristic, inability to learn new things. At the same time, the memory of long-standing events can remain intact for a very long time.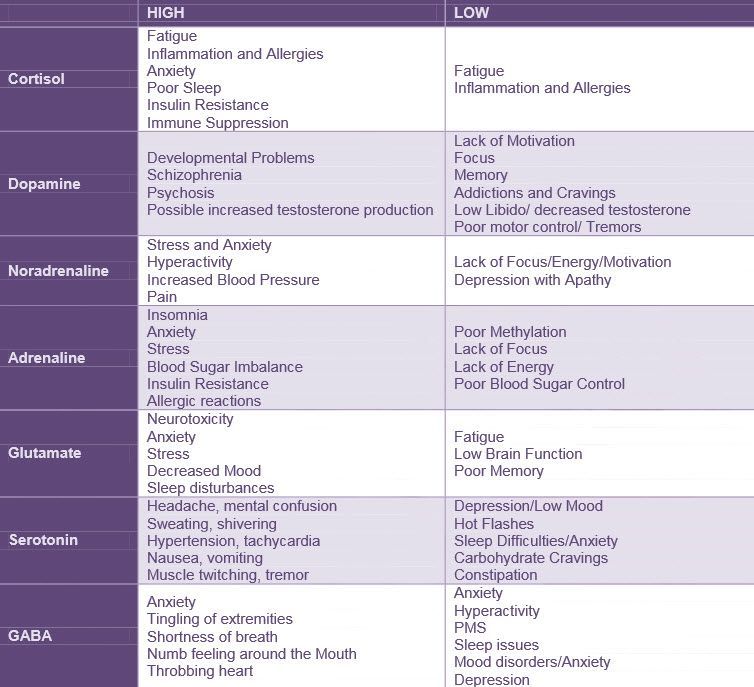
With atrophic processes in the brain, memory loss can be very rapid and abrupt. In this case, the onset of the disease in adulthood (45-55 years) is possible. In such cases, you should not delay contacting a specialist.
Psychosis
is a rather severe disorder of mental activity, the treatment of which is carried out mainly by medication. Family members of the affected person may seek help for unexplained behavioral changes, including bizarre or threatening behavior (withdrawal, suspicion, threats). Signs that should alert in terms of the development of a psychotic state: hallucinations (false or imagined sensations, for example, perceiving voices when no one is around), delusions (uncorrectable deliberately false beliefs, for example, the patient may be sure that he is being poisoned neighbors, that he receives messages from television or that he is being watched in a special way), agitation or unusual behavior, strange statements, sudden changes or instability of the emotional state. It should be noted that upon leaving the psychotic state, patients need psychotherapeutic assistance aimed at forming a critical attitude towards their disorders, improving socialization, and learning to recognize the first signs of a deterioration in mental well-being (prevention of recurrent psychosis).
It should be noted that upon leaving the psychotic state, patients need psychotherapeutic assistance aimed at forming a critical attitude towards their disorders, improving socialization, and learning to recognize the first signs of a deterioration in mental well-being (prevention of recurrent psychosis).
Hidden depression
acts not as a distinct depression of mood and other mental functions, but as an internal bodily ill-being affecting various organs, functions, systems. Thus, depression can disguise itself as diseases of the cardiovascular, gastrointestinal, respiratory, and nervous systems. The well-known “pain of unclear etiology” (a diagnosis often encountered in the practice of therapists) often has the same nature.
Anguish
an oppressive painful feeling, which is often experienced as a "constriction", heaviness in the chest. Longing is much more intense than such worldly emotions as sadness or sadness. It often happens with depression and can occur without a significant reason.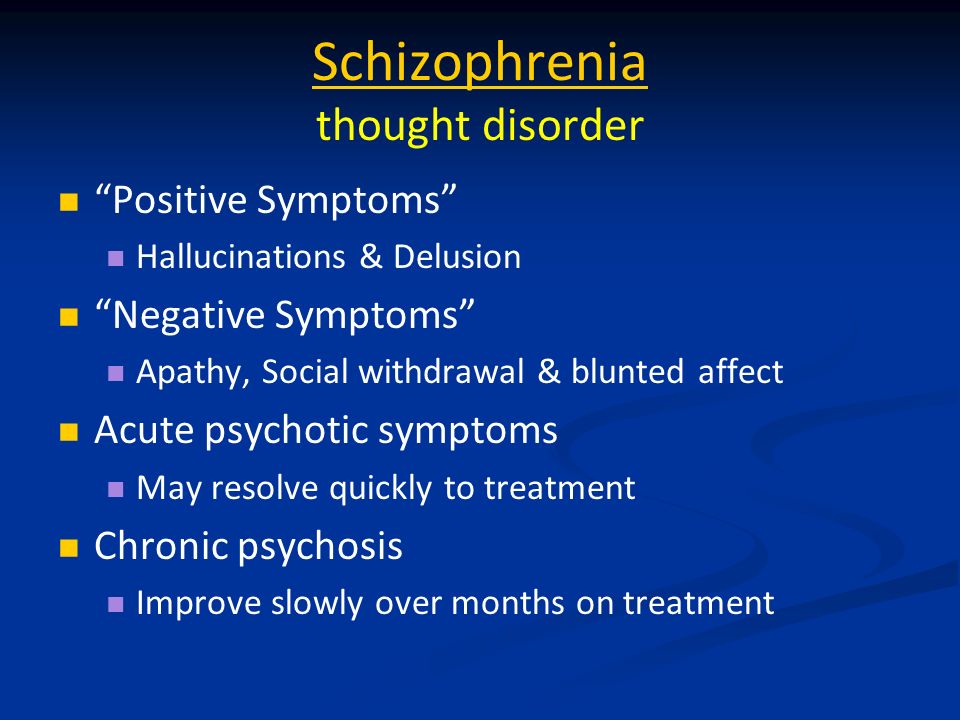
Anxiety in psychiatry
Uncertainty, suspense, feeling that something is about to happen. In other words, it is an emotional experience characterized by discomfort from the uncertainty of perspective. This is the most important human emotion, closely related to the need for security. Anxiety is sometimes felt bodily, like itching, excitement in the chest, internal trembling, and is often combined with motor excitement.
Epileptic seizure
in its most typical form is characterized by an abrupt onset: a person screams, loses consciousness, falls, then sharply strains, sometimes turns blue, followed by convulsions. After a seizure, a person is usually lethargic, lethargic and drowsy. This is the so-called convulsive seizure. However, often epileptic seizures are non-convulsive in nature, occur without a fall and may escape the attention of the patient's relatives. Signals indicating the need to see a doctor are:
- any sharp falls with loss of consciousness (even without convulsions),
- a tendency to suddenly “freeze” and “turn off” (sometimes for seconds, while stereotypical movements of the arms, head, facial muscles of the face are possible; this feature can be observed during a conversation , performing everyday activities),
- loss of memory of some events, facts when a person was not drunk, could walk, perform some actions, which he cannot remember anything about later.
It should be noted that the presence of epileptic seizures does not always indicate epilepsy as a disease. Convulsive and non-convulsive seizures can be a consequence of brain damage (traumatic brain injury, consequences of alcohol intoxication, and in young children, convulsions are the only non-specific response of the body to many stimuli, in particular, an increase in body temperature).
- About psychiatry
- Types of psychiatric disorders
- Severe mental disorders
- Symptoms of disorders
- Psychiatric diseases
- Expert opinion
- Manic disorders
- Anorexia
- Child psychiatry
- Autism treatment
- Treatment of paranoia
8 most common mental disorders that people attribute to themselves //Psychological newspaper
In recent years, it has become somewhat fashionable to have this or that mental disorder. An important role in this was played by the fact that in recent years, as a whole, they have begun to talk more about mental disorders, the topic has ceased to be taboo, and mental illness itself is something shameful in the public mind.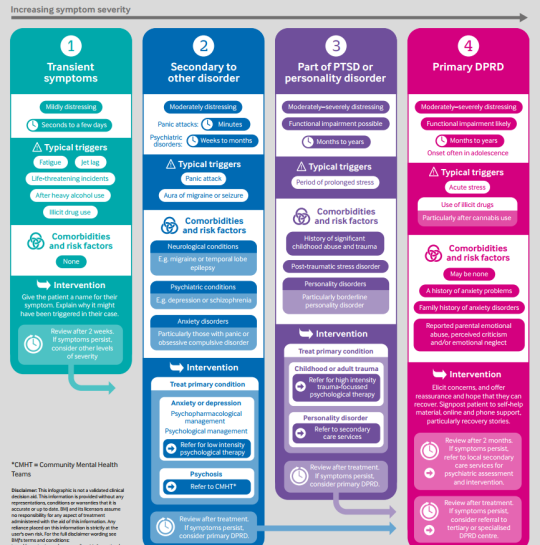
“This trend is especially noticeable among adolescents, since in adolescence there is a formation of personality and a search for one’s own uniqueness, and mental disorders seem to young people as something unusual and even mysterious, something that distinguishes them from other people,” the psychiatrist explains. Irina Korobkova . “In addition, teenagers are often very impressionable, they are greatly influenced by what they may have read or seen in books, films or real life, and they are more likely to compare and “transfer” what they see or hear to themselves.
Most often, people attribute the following mental disorders to themselves.
1. Depression
“This is one of the most common mental disorders, and for many years it has been in first place in the ranking of “fashionable” disorders,” says Irina Korobkova. - This is a unique state, because it affects our feelings, thoughts, behavior, physical condition, intellectual abilities, perception of ourselves, the surrounding reality and our own perspectives.
Feature of depression
The key manifestations of depression are persistently depressed mood and the loss of the ability to experience positive emotions. It is literally impossible to distract a depressed person from painful experiences at least for a while. The patient has impaired metabolism of a number of neurotransmitters in the brain.
Depression very often takes a chronic course and in one way or another worries a person throughout life, at times increases the risk of serious cardiovascular diseases and suicide, that is, one can literally die from depression. With depression, there is often a hereditary burden.
Just a bad mood, a grief reaction, emotional burnout - all this is not depression, although it has some manifestations similar to it.
About depression in an article by Doctor of Medical Sciences Tatyana Arturovna Karavaeva.
2. Bipolar affective disorder (BAD)
- A disease in which depressive and manic phases alternate.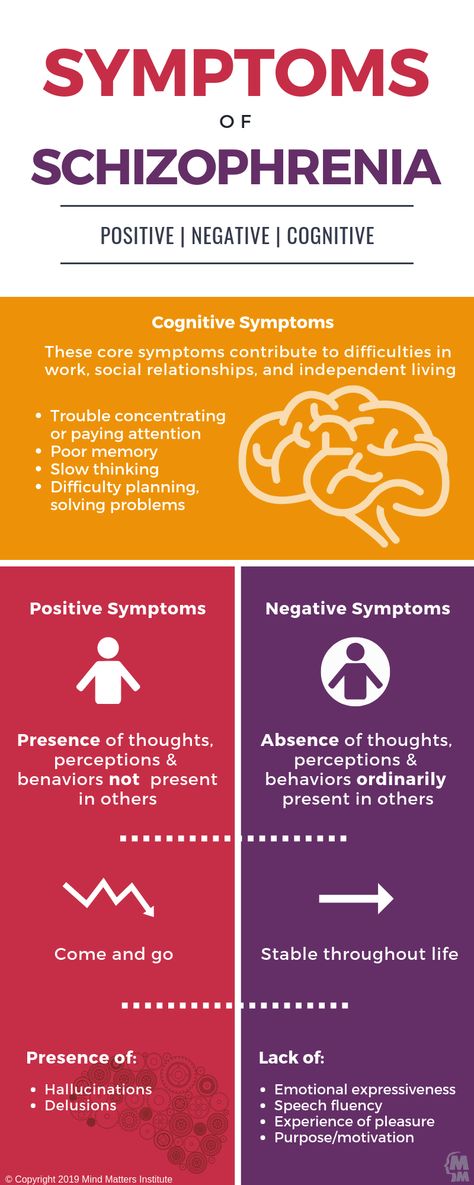 Mania (emphasis on "I") is the exact opposite of depression, the doctor explains. — It may seem that this is a wonderful state in which a person is always satisfied and happy, but in fact, mania is a serious mental disorder, and patients with bipolar disorder with a long history of the disease are much more afraid of mania than depression.
Mania (emphasis on "I") is the exact opposite of depression, the doctor explains. — It may seem that this is a wonderful state in which a person is always satisfied and happy, but in fact, mania is a serious mental disorder, and patients with bipolar disorder with a long history of the disease are much more afraid of mania than depression.
Feature of BAR
This state is dangerous because, due to the overestimation of their own capabilities, people do things that are not characteristic of them and inadequate: they take loans for large amounts of money, enter into intimate relationships with strangers, get involved in dubious adventures, the doctor explains.
With a particularly severe course of bipolar disorder, people can almost constantly lie in psychiatric hospitals, since mood disorders do not allow them to fully integrate into society.
- With bipolar disorder, the risk of suicide is significantly higher than with unipolar depression. With bipolar disorder, constant drug therapy is required, - Irina Korobkova draws attention.
Just because you are a "mood person" does not mean that you are "bipolar".
3. Borderline Personality Disorder (BPD)
“In my subjective opinion, this is the most “fashionable” diagnosis of the last 3-4 years,” says the psychiatrist. — BPD is a persistent personality disorder that is manifested by impulsivity, low self-control, emotional instability, high anxiety, significant difficulties in social interaction, and often self-damaging behavior.
Feature PRL
In the development of BPD, the role of heredity is great. Often develop depression, alcohol and drug addiction, eating disorders. BPD patients often die by suicide. BPD is a personality disorder, that is, a pathological change in a person's character.
It is impossible to make a diagnosis of BPD based on one or two symptoms. A comprehensive assessment of all manifestations and monitoring of the development of the condition over time is important.
4. Panic attacks (PA)
“Like depression, PA is an “eternal classic” of psychiatry,” explains Irina Korobkova. “Modern life is very conducive to anxiety disorders in general and panic attacks in particular, because the dynamic rhythm, high demands and standards, multitasking mode - all this forces us to live at the limit of our capabilities.
“Modern life is very conducive to anxiety disorders in general and panic attacks in particular, because the dynamic rhythm, high demands and standards, multitasking mode - all this forces us to live at the limit of our capabilities.
Panic attack feature
This is a pronounced anxiety-vegetative attack, in which a variety of autonomic symptoms unfold against the background of anxiety (strong and / or rapid heartbeat, interruptions in the work of the heart, lack of air, fever or chills, feeling of sinking in the chest, sweating, lump in the throat, nausea, fainting, a sharp urge to urinate and / or defecate, etc.), as well as a fear of death and / or fear of going crazy.
Further, the fear of a recurrence of such an attack and the avoidance of certain places in which they occur can be added. Panic attacks are not a disease, but a syndrome, and they occur with a variety of mental disorders. Treatment usually responds very well.
However, panic attacks are often called something that they are not at all.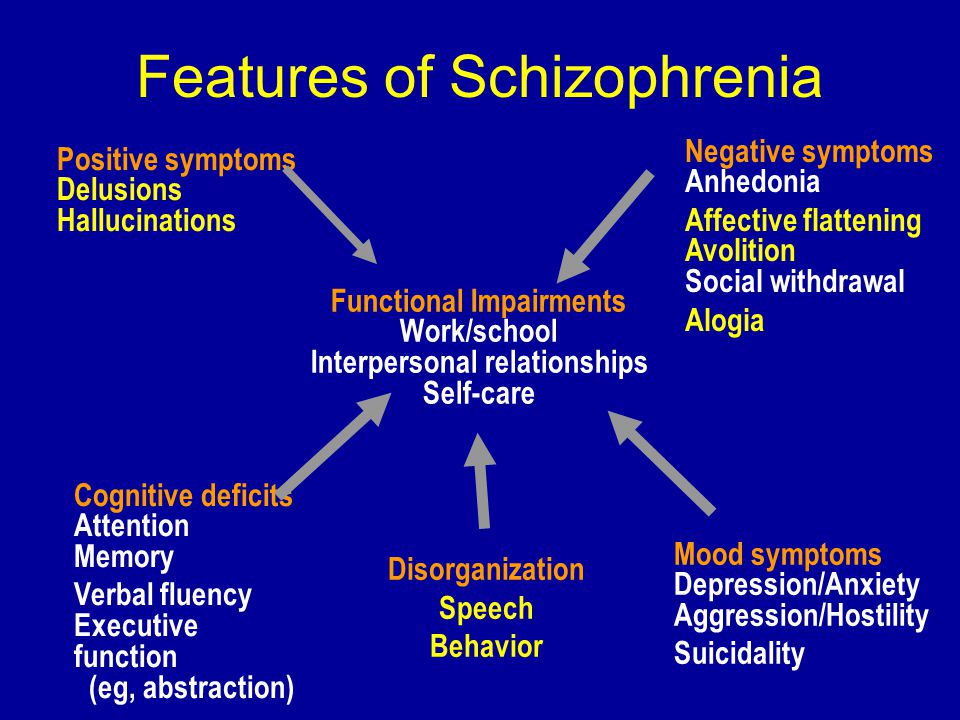 Severe anxiety, anxiety, inner tension, or fear is not a panic attack.
Severe anxiety, anxiety, inner tension, or fear is not a panic attack.
5. Anorexia
- An eating disorder (EDD), which is manifested by the fear of weight gain, deliberate pronounced dietary restrictions and, as a rule (but not always!), Significant weight loss below the biological norm, - this is how Irina Korobkova describes the disease.
The expert notes that the fashion for thinness itself appeared in the era of supermodels of the 1990-2000s. Later, the promotion of unhealthy thinness became even more widespread, many Internet publics appeared that approved of the unhealthy desire for excessive thinness and called for it.
Anorexia Feature
Anorexia is primarily a genetic disease. The influence of heredity in anorexia is up to 80%.
Young girls dream of getting anorexic in order to be thin, easily endure food restrictions and “not break into goodies.” But they should know that it is the mental disorder with the highest mortality rate.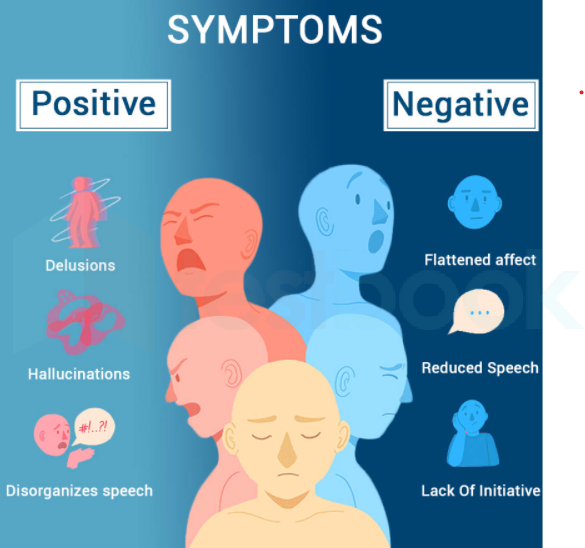
About anorexia in an article by psychiatrist and psychotherapist Tatyana Leonidovna Kharaburova.
6. Social phobia
“Now it has become fashionable to associate any feature of one’s character or temperament with a mental disorder, and introverted people who are prone to solitude and do not need a large number of social contacts have begun to call themselves social phobes,” says the psychiatrist.
Features of social phobia
In fact, social phobia is a painful disorder when a person wants to be in a circle of people and express himself in society, but cannot do this due to the large amount of anxiety and shame associated with social interaction.
The percentage of errors as a result of "self-diagnosis" is very high. Therefore, leave questions of diagnosis and treatment to doctors.
7. Autism
And especially its most functional variant (with intact intelligence) is Asperger's syndrome.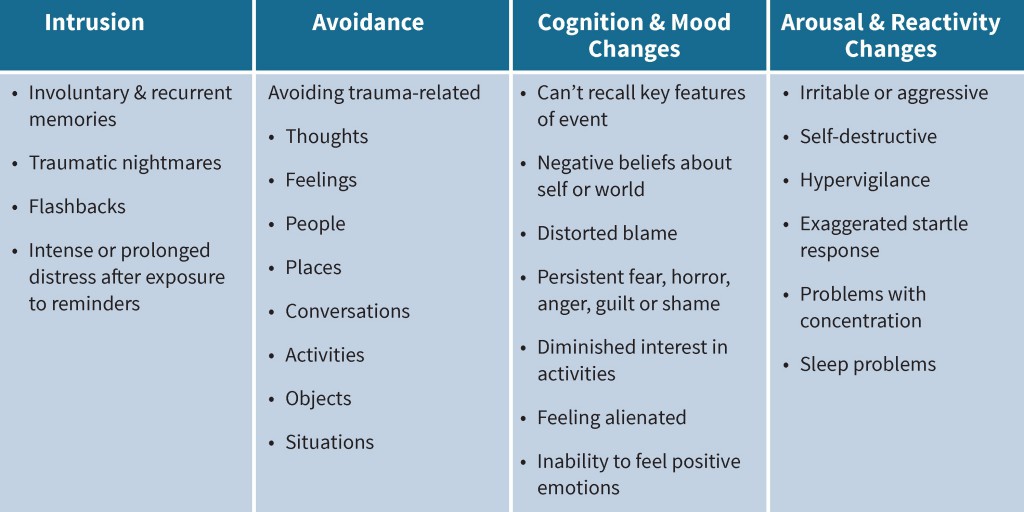
“People often imagine autistic people as unusual people with superpowers, such as they are shown in the film “Rain Man” and the series “The Good Doctor,” explains Irina Korobkova. But films are always fiction to one degree or another.
Feature of autism
In fact, autism is a severe mental disorder associated with impaired development of the central nervous system. As a result of such a violation, a person reacts sharply to some stimuli and is completely indifferent to others. People with autism move away from reality, are immersed in the world of their own experiences and cannot socialize normally.
Among medical students there is a concept of "third-year syndrome". This is how they designate a situation when students - future doctors, who do not yet have enough special knowledge and developed clinical thinking, read about the symptoms of various diseases and find all of them in themselves. What can we say about people who have nothing to do with medicine at all.
8. ADHD - Attention Deficit Hyperactivity Disorder
“Often, people, having experienced minimal difficulty concentrating in the process of studying or working, decide that they have ADHD,” the doctor draws attention. - In fact, in an adult, such problems in the overwhelming majority of cases are due to a violation of the regime and lifestyle (lack of sleep, lack of rest, an excessive number of tasks per unit of time) or disorders of the anxiety-depressive circle.
Features ADHD
This is a childhood disorder that by adulthood either smooths out or passes, or “outgrows” into other forms of psychopathology.
At the same time, children with ADHD literally cannot sit still for a second, they experience great difficulties with learning and establishing social contacts.
“Only a psychiatrist should be engaged in the diagnosis of mental illness,” recalls Irina Korobkova. - If you are worried about your psycho-emotional state, the first thing to do is to make an appointment with a psychiatrist, and not engage in self-diagnosis.