Liquid anti depressants
Which antidepressants come in liquid forms?
Many, but not all, antidepressants are available as liquid formulations, which include oral solutions or oral concentrates. These are useful in many situations—for children, those with trouble swallowing, when fine titration is required, and so on.
The following are the liquid preparations of antidepressants that are available in the US as of May 2022.
SSRIs
Citalopram (generic) 10 mg/5 mL (150 mL, 200 mL, 225 mL, 240 mL, 300 mL)
Escitalopram oral solution (generic) 5 mg/5 mL (150 mL, 240 mL, 300 mL, 450 mL, 600 mL). The escitalopram oral solution may be mixed with other liquids like water, orange juice, or apple juice (source).
Fluoxetine (generic) 20 mg/5 mL (120 mL)
Paroxetine (generic) 10 mg/5mL (250 mL)
Sertraline (generic) 20 mg/mL (60 mL). Note: Sertraline is available as an “oral concentrate”, which is not the same as an oral solution. Sertraline oral concentrate contains 20 mg per mL and it must be diluted before it is taken.
Fluvoxamine (not available as a liquid)
SNRIs
None of them is available as a liquid (desvenlafaxine ER, duloxetine, levomilnacipran, milnacipran, venlafaxine/venlafaxine ER).
Tricyclic antidepressants
Nortriptyline 10 mg/5 mL (75 mL, 115 mL, 150 mL, 300 mL, 473 mL)
MAO inhibitors
None of them is available as a liquid (phenelzine, tranylcypromine, isocarboxazid).
Other antidepressants
Bupropion/ bupropion SR/ bupropion XL—not available as a liquid
Mirtazapine—not available as a liquid
Summary
SSRIs: As of May 2022, liquid formulations are available in the US for all but one of the six SSRIs—for citalopram, escitalopram, fluoxetine, paroxetine, and sertraline, but not for fluvoxamine.
TCAs: A liquid formulation is available for nortriptyline.
Other antidepressants: A liquid formulation is NOT available for any of the serotonin-norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants other than nortriptyline, or any of the MAO inhibitors.
Related Pages
How to manage patients who are “sensitive to medications”
Antidepressants: What are the alternatives to the oral route?
Sometimes, a medication may be given rectally
Can patients who are NPO not take medications orally?
Medication formulations and their contents
Do sustained-release preparations have fewer adverse effects?
Extended-release preparations of psychotropic medications
Which extended-release capsule can be opened and how?
Two patients where opening medication capsules was helpful
Why, when, and how to split medication tablets
Recommended pill cutters and pill crushers
Which tablets are actually extended-release formulations and so should not be cut?
Orally disintegrating tablets (ODTs) can be useful
Psychotropic medications are sometimes given sublingually
Gluten in medications
Can lactose in medication pills cause intolerance?
Medication cost, generics, pharmacies
How to find out the price of medications, compare prices, and get the lowest possible price
Tips on reducing the cost of medications by using higher strength pills
Medications from Canadian pharmacies?
Using a Canadian pharmacy can reduce the cost of some medications
Should we encourage patients to use independent pharmacies?
Medication prices on Costco.
 com versus on Goodrx.com
com versus on Goodrx.comA simple way to significantly reduce the cost of l-methylfolate (Deplin®)
How can I know in advance whether the insurance will cover this medication?
Prior authorization for medications
Pharmacy benefit managers
Are generic medications really equivalent to brand-name medications?
Which manufacturers of generic versions of psychotropic medications are better or worse?
Treatments: Main menu
Copyright © 2017 to 2022, Simple and Practical Medical Education, LLC. All rights reserved. May not be reproduced in any form without express written permission.
Disclaimer: The content on this website is provided as general education for medical professionals. It is not intended or recommended for patients or other laypersons or as a substitute for medical advice, diagnosis, or treatment. Patients must always consult a qualified health care professional regarding their diagnosis and treatment. Healthcare professionals should always check this website for the most recently updated information.
Healthcare professionals should always check this website for the most recently updated information.
Overview - Antidepressants - NHS
Antidepressants are a type of medicine used to treat clinical depression.
They can also be used to treat a number of other conditions, including:
- obsessive compulsive disorder (OCD)
- generalised anxiety disorder
- post-traumatic stress disorder (PTSD)
Antidepressants are also sometimes used to treat people with long-term (chronic) pain.
Read more about when antidepressants are used.
How antidepressants work
It's not known exactly how antidepressants work.
It's thought they work by increasing levels of chemicals in the brain called neurotransmitters. Certain neurotransmitters, such as serotonin and noradrenaline, are linked to mood and emotion.
Certain neurotransmitters, such as serotonin and noradrenaline, are linked to mood and emotion.
Neurotransmitters may also affect pain signals sent by nerves, which may explain why some antidepressants can help relieve long-term pain.
While antidepressants can treat the symptoms of depression, they do not always address its causes. This is why they're usually used in combination with therapy to treat more severe depression or other mental health conditions.
How effective are antidepressants?
Research suggests that antidepressants can be helpful for people with moderate or severe depression.
They're not usually recommended for mild depression, unless other treatments like talking therapy have not helped.
Doses and duration of treatment
Antidepressants are usually taken in tablet form. When they're prescribed, you'll start on the lowest possible dose thought necessary to improve your symptoms.
When they're prescribed, you'll start on the lowest possible dose thought necessary to improve your symptoms.
Antidepressants usually need to be taken for 1 or 2 weeks (without missing a dose) before the benefit starts to be felt. It's important not to stop taking them if you get some mild side effects early on, as these effects usually wear off quickly.
If you take an antidepressant for 4 weeks without feeling any benefit, speak to your GP or mental health specialist. They may recommend increasing your dose or trying a different medicine.
A course of treatment usually lasts for at least 6 months after you start to feel better. Some people with recurrent depression may be advised to take them indefinitely.
Read more about antidepressant dosages.
Side effects
Different antidepressants can have a range of different side effects. Always check the information leaflet that comes with your medicine to see what the possible side effects are.
Always check the information leaflet that comes with your medicine to see what the possible side effects are.
The most common side effects of antidepressants are usually mild. Side effects should improve within a few days or weeks of treatment, as the body gets used to the medicine.
Read more about:
- possible side effects of antidepressants
- cautions and interactions of antidepressants
Coming off antidepressants
Talk to your doctor before you stop taking antidepressants. It's important that you do not stop taking antidepressants suddenly.
Once you're ready to come off antidepressants, your doctor will probably recommend reducing your dose gradually over several weeks – or longer, if you have been taking them for a long time.
This is to help prevent any withdrawal symptoms you might get as a reaction to coming off the medicine.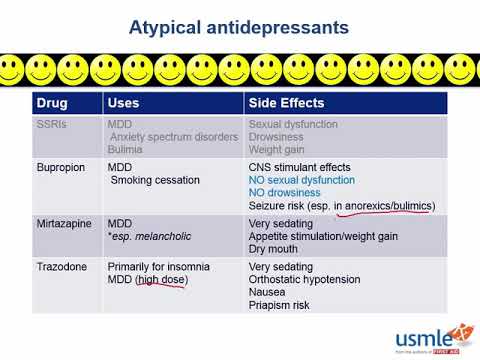
Read more about stopping or coming off antidepressants.
Types of antidepressants
There are several different types of antidepressants.
Selective serotonin reuptake inhibitors (SSRIs)
SSRIs are the most widely prescribed type of antidepressants. They're usually preferred over other antidepressants, as they cause fewer side effects. An overdose is also less likely to be serious.
Fluoxetine is probably the best known SSRI (sold under the brand name Prozac). Other SSRIs include citalopram (Cipramil), escitalopram (Cipralex), paroxetine (Seroxat) and sertraline (Lustral).
Serotonin-noradrenaline reuptake inhibitors (SNRIs)
SNRIs are similar to SSRIs. They were designed to be a more effective antidepressant than SSRIs. However, the evidence that SNRIs are more effective in treating depression is uncertain. It seems that some people respond better to SSRIs, while others respond better to SNRIs.
However, the evidence that SNRIs are more effective in treating depression is uncertain. It seems that some people respond better to SSRIs, while others respond better to SNRIs.
Examples of SNRIs include duloxetine (Cymbalta and Yentreve) and venlafaxine (Efexor).
Noradrenaline and specific serotonergic antidepressants (NASSAs)
NASSAs may be effective for some people who are unable to take SSRIs. The side effects of NASSAs are similar to those of SSRIs, but they're thought to cause fewer sexual problems. However, they may also cause more drowsiness at first.
The main NASSA prescribed in the UK is mirtazapine (Zispin).
Tricyclic antidepressants (TCAs)
TCAs are an older type of antidepressant. They're no longer usually recommended as the first treatment for depression because they can be more dangerous if an overdose is taken. They also cause more unpleasant side effects than SSRIs and SNRIs.
They also cause more unpleasant side effects than SSRIs and SNRIs.
Exceptions are sometimes made for people with severe depression that fail to respond to other treatments. TCAs may also be recommended for other mental health conditions, such as OCD and bipolar disorder.
Examples of TCAs include amitriptyline, clomipramine, dosulepin, imipramine, lofepramine and nortriptyline.
Some types of TCAs, such as amitriptyline, can also be used to treat chronic nerve pain.
Serotonin antagonists and reuptake inhibitors (SARIs)
SARIs are not usually the first choice of antidepressant, but they may be prescribed if other antidepressants have not worked or have caused side effects.
The main SARI prescribed in the UK is trazodone (Molipaxin).
Monoamine oxidase inhibitors (MAOIs)
MAOIs are an older type of antidepressant that are rarely used nowadays.
They can cause potentially serious side effects so should only be prescribed by a specialist doctor.
Examples of MAOIs include tranylcypromine, phenelzine and isocarboxazid.
Other treatments for depression
Other treatments for depression include talking therapies such as cognitive behavioural therapy (CBT).
People with moderate to severe depression are usually treated using a combination of antidepressants and CBT. Antidepressants work quickly in reducing symptoms, whereas CBT takes time to deal with causes of depression and ways of overcoming it.
Regular exercise has also been shown to be useful for those with mild depression.
Read more about alternatives to antidepressants.
Yellow Card Scheme
The Yellow Card Scheme allows you to report suspected side effects from any type of medicine you're taking. It's run by a medicines safety watchdog called the Medicines and Healthcare products Regulatory Agency (MHRA).
It's run by a medicines safety watchdog called the Medicines and Healthcare products Regulatory Agency (MHRA).
See the Yellow Card Scheme website for more information.
Community content from HealthUnlockedFGBNU NTsPZ. ‹‹Depression in General Medicine: A Guide for Physicians››
One of the main arguments in favor of the use of first-line antidepressants in the treatment of affective disorders in general medical practice is the minimal (compared to second-line drugs) severity of side effects.
Differences in the complications of thymoanaleptic therapy are clearly seen when comparing the main manifestations of the undesirable effect of representatives of first-line antidepressants (SSRIs, SSOZS) and TCAs, which is clearly demonstrated by the data given in Table. fourteen. nine0003
Nevertheless, it is impossible to completely exclude complications even when using sparing psychotropic drugs. The greatest likelihood of developing side effects of psychopharmacotherapy occurs in patients with somatic diseases, as well as in elderly people who show hypersensitivity to psychotropic drugs; in these contingents, even with careful dose titration, in addition to the main thymoanaleptic effect, side effects may also occur. nine0003
The greatest likelihood of developing side effects of psychopharmacotherapy occurs in patients with somatic diseases, as well as in elderly people who show hypersensitivity to psychotropic drugs; in these contingents, even with careful dose titration, in addition to the main thymoanaleptic effect, side effects may also occur. nine0003
The main side effects of antidepressants include anticholinergic disorders of the central and autonomic nervous system, cardiovascular system, complications from the hematopoietic organs, metabolic and endocrine disorders (weight changes, sexual dysfunction, allergic reactions).
Side effects often appear in the initial stages of treatment (in the first 2 weeks) and sometimes persist for 3-4 weeks of therapy, and then reverse development. For more persistent and at the same time severe disorders, dose reduction is indicated, and, if necessary, therapy is discontinued. nine0003
Treatment with tianeptine (SSOZS) is accompanied by a minimum of undesirable effects.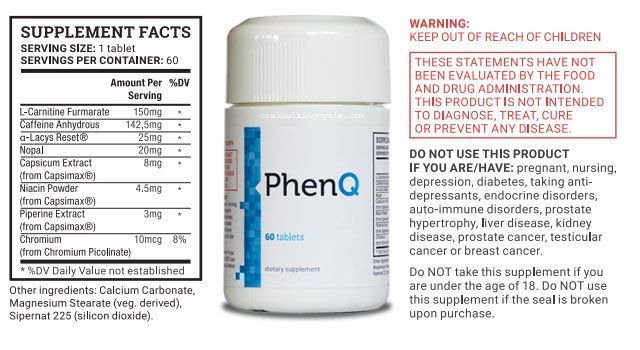 Side effects of the drug are most often limited to complaints of dry mouth, nausea, and drowsiness during the day. Only in some cases, phenomena of transient orthostatic hypotension, dizziness, headaches, skin allergic reactions are also observed. The most common side effects of SSRIs are:
Side effects of the drug are most often limited to complaints of dry mouth, nausea, and drowsiness during the day. Only in some cases, phenomena of transient orthostatic hypotension, dizziness, headaches, skin allergic reactions are also observed. The most common side effects of SSRIs are:
- nausea,
- dry mouth
- loss of appetite, nine0003
- vomit,
- diarrhea,
- constipation.
Along with this, undesirable effects from the autonomic and central nervous system are possible:
- dizziness,
headaches (citalopram)
- insomnia,
- increase (or appearance) of anxiety,
- nervousness
- a sense of inner tension.
The latter appear in the first weeks of treatment or with increasing doses. nine0003
There are transient extrapyramidal disorders in the form of tremor. As for other disorders (parkinsonism, akathisia, dyskinesias), judging by the data of a number of publications, they are recorded only in individual cases. The use of fluoxetine and paroxetine may be accompanied by increased bleeding and even bleeding.
The use of fluoxetine and paroxetine may be accompanied by increased bleeding and even bleeding.
During SSRI therapy, neurotoxic reactions (serotonin syndrome) affecting the gastrointestinal tract and nervous system (colic in the abdomen , flatulence, loose stools, nausea, vomiting; tremor, dysarthria, muscle hypertonicity, hyperreflexia, myoclonic twitching, ataxia) are possible. In more severe cases, hyperthermia, confusion, symptoms of disorientation join [Malin D.I., 2000]. nine0003
Severe complications often occur in the process of drug interaction with combined use:
- SSRIs and MAOIs,
- SSRIs and OIMAO-A (moclobemide),
- TCA (anafranil) and OIMAO-A.
Along with side effects, the effects of antidepressants associated with overdose are of great importance (especially in the context of a general medical network). The risk of deliberately taking large amounts of drugs for suicidal purposes poses a safety advantage to first-line antidepressants. This is evidenced by comparative data on the safety of some first-line and second-line antidepressants, presented in Table. fifteen. nine0003
This is evidenced by comparative data on the safety of some first-line and second-line antidepressants, presented in Table. fifteen. nine0003
The safety of first-line drugs is indicated by the data of C. Las-mier et al. (1991) in relation to tianeptine. Taking large doses of this drug (from 12 to 60 tablets) (12 cases of suicidal use of tianeptine are summarized) does not lead to death and is not accompanied by significant (compared with the norm) deviations of the clinical and electrocardiological parameters of the cardiovascular system.
Table 15. Safety of antidepressants [based on R. Priest, D. Baldwin, 1994]
| Preparations | Hazard measure (number of deaths from overdose per 1 million prescriptions) | Degree of danger |
| First line antidepressants | ||
| Fluoxetine (Prozac) Fluvoxamine (Fevarin) Mianserin (Lerivon) | Less than 10 | Relatively dangerous |
| Second line antidepressants | ||
| Clomipramine (Anafranil) Maprotiline (Ludiomil) Trazadone (Tritgiko) | More than 10 | Potentially dangerous |
| Imipramine (Melipramine) Phenelzine (Nardil) | Over 20 | Dangerous |
| Amitriptyline Trianylcypramine (transamine) | Over 40 | Very dangerous |
With an overdose of milnacipran (ixel), vomiting, hyperventilation, and tachycardia are observed. However, even taking excessively high daily amounts of the drug (1900-2800 mg) does not lead to severe complications and results in complete recovery [Montgomery S. A. et at, 1996].
However, even taking excessively high daily amounts of the drug (1900-2800 mg) does not lead to severe complications and results in complete recovery [Montgomery S. A. et at, 1996].
Taking mirtazapine (Remeron) in excessive doses (up to 315 mg - 4 observations) is accompanied only by transient somnolence without impaired respiratory and cardiovascular functions [Montgomery S.A., 1995].
Experts have changed the way adults treat depression » Medvestnik
The National Institute for Health and Care Excellence (NICE) has updated guidelines for treating adults with depression. The changes affected the tactics of treating the disease, the possibility of intensifying antidepressant therapy, and ways to cancel drug therapy.
Definition
Depression is a mental disorder characterized by an inability to experience positive emotions (loss of interest in and enjoyment of ordinary things and activities), depressed mood, and a wide range of associated emotional, cognitive, physical, and behavioral symptoms, according to the NICE document . nine0003
nine0003
Principles of Case Management
In caring for a patient with depression, the professional should strive to build trust. It is necessary to communicate with the patient openly, without judging him, avoiding stigmatization and discrimination, respecting confidentiality, privacy and respect for his personality. The patient must be given full access to up-to-date, evidence-based recommendations for the treatment of depression, as well as information about local self-help groups.
At the first meeting with the patient, it is necessary to clarify the history of the disease, concomitant mental and somatic pathology, the presence of episodes of elevated mood (for differential diagnosis with bipolar disorder), previous therapy and response to it. It is important to know the patient's strengths, personal resources, difficulties in relationships, lifestyle (eg, diet, physical activity, sleep), the presence of stressful or traumatic life events, current or past (divorce, loss of a loved one, trauma), conditions life, whether he has drug or alcohol abuse. A patient with depression should definitely ask about the presence of suicidal thoughts and intentions. nine0003
A patient with depression should definitely ask about the presence of suicidal thoughts and intentions. nine0003
If suicidal risk is identified, the patient should be referred to a psychiatrist immediately.
Periods of high risk
When working with depressed patients, special care should be taken during periods of high risk: when starting and changing therapy, with increased stress. It is necessary to advise the patient and his relatives to pay attention to mood swings, anxiety, negative feelings and a sense of hopelessness, the appearance of suicidal thoughts.
It should be remembered that high doses of antidepressants can be toxic, so patients with suicidal risk should limit the amount of medication dispensed at one time on their hands. nine0003
The risk of suicidal thoughts, the likelihood of self-harm and suicide increase in the first weeks of antidepressant therapy.
Treatment
For subthreshold and mild depression, antidepressant therapy should not be the first choice. Patients with moderate and severe depressive disorders may require antidepressant therapy in addition to non-pharmacological treatments. When suggesting drug therapy to a patient, the reasons for prescribing the drug, possible drugs, dosage and options for changing it, expected improvements in therapy, possible side effects and withdrawal should be discussed. When prescribing an antidepressant, the physician should explain to the patient the possible effects at the start of treatment, the timing of response to therapy (usually 4 weeks), and the need to take drugs for at least 6 months after the onset of remission. A follow-up appointment should be scheduled after 2 weeks or after 1 week if there is a risk of suicide or if the patient is between 18 and 25 years of age. The patient should be aware that antidepressant withdrawal is gradual, gradual and successful in most cases. Abrupt discontinuation of therapy, skipping a dose, or taking an incomplete dose may cause a withdrawal syndrome: dizziness, sensory disturbances (eg, tingling sensation), mental changes (irritability, anxiety, anxiety, low mood, tearfulness, panic attacks, fears, confusion, occasionally suicidal thoughts), sleep disturbance, sweating, gastrointestinal disturbances (eg, nausea), palpitations, fatigue, headaches, joint and muscle pain. nine0003 Most often, the withdrawal syndrome is mild and lasts from 1 to 2 weeks, sometimes it can be more severe and last for several weeks, in rare cases - months. Occasionally, the withdrawal syndrome can be severe, especially with abrupt withdrawal of therapy. When antidepressants are discontinued, the dose should be reduced in stages, for example by 50%. After that, reduce by another 25%, when small doses are reached, a transition to liquid forms of drugs is possible. Before each step, you should make sure that there is no or minimal manifestations of the withdrawal syndrome. nine0003 Drugs with a short half-life should be discontinued more slowly. Cancellation of fluoxetine, given its prolonged action, can be performed with the transition to taking the drug every other day. Successful withdrawal of antidepressants can take weeks to months. In severe withdrawal symptoms, the antidepressant should be resumed at full dose and tapered more slowly after symptoms resolve. Lithium may be used as augmentation therapy for depression. After the appointment and then every 6 months, it is necessary to perform weight control, evaluate the function of the kidneys and thyroid gland, and the level of calcium. Plasma lithium levels should be assessed 12 hours after the first dose, then 1 week later, and 1 week after each dosage change; further drug monitoring is carried out every 3-6 months, depending on the patient's health status. nine0003 The concentration of lithium in the blood plasma should not exceed 1.0 mmol / l (the level required to achieve a therapeutic effect is from 0.4 mmol / l). Cancellation of lithium is carried out within 1-3 months under the supervision of a psychiatrist. Antipsychotics may also be used to augment therapy, with attention to potential side effects (eg, extrapyramidal symptoms [eg, tremor, parkinsonism], elevated plasma prolactin levels). nine0003 When prescribing antipsychotics, it is necessary to monitor the clinical analysis of blood and urine, the concentration of electrolytes, prolactin, glucose and liver enzymes in the blood after 6, 12 weeks and 1 year from the start of therapy, and then annually, and also perform ECG monitoring. The patient can be offered a wide range of therapeutic techniques: self-help groups, cognitive behavioral therapy, behavioral activation, interpersonal psychotherapy, short-term psychodynamic psychotherapy, group physical education classes specially designed for patients with depression, mindfulness-based cognitive therapy and meditation. nine0003
The patient can be offered a wide range of therapeutic techniques: self-help groups, cognitive behavioral therapy, behavioral activation, interpersonal psychotherapy, short-term psychodynamic psychotherapy, group physical education classes specially designed for patients with depression, mindfulness-based cognitive therapy and meditation. nine0003
 nine0003
nine0003 Principles of Antidepressant Withdrawal and Dose Reduction

Augmentation therapy


Learn more