Levels of migraines
What are the stages of a migraine?
Speaking of Health
Topics in this Post
- Headache
- Family Medicine
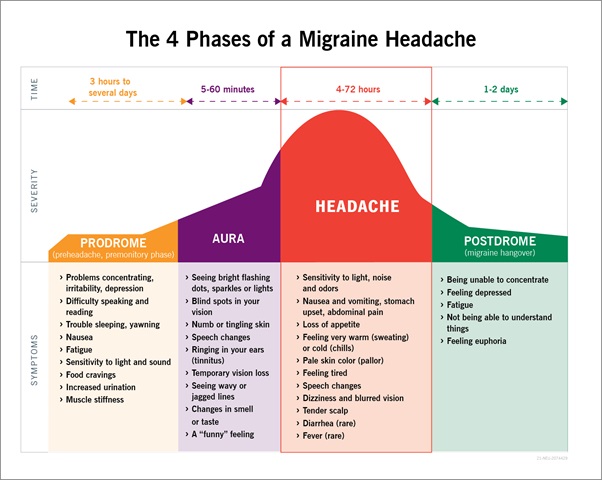
Migraines are a common condition with about 15% of U.S. adults reporting a migraine or severe headache in the previous three months, according to the Centers for Disease Control and Prevention. Migraines, which often begin in childhood, adolescence or early adulthood, can progress through four stages: prodrome, aura, attack and post-drome. Not everyone who has migraines goes through all stages.
Learn more about each stage of a migraine:
1. Prodrome
One or two days before a migraine, you might notice subtle changes that warn of an upcoming migraine, including constipation, mood changes from depression to euphoria, food cravings, neck stiffness, increased thirst and urination or frequent yawning.
2. Aura
For some people, aura might occur before or during migraines. Auras are reversible symptoms of the nervous system. They're usually visual, but they also can include other disturbances. Each symptom usually begins gradually, builds up over several minutes and lasts 20 minutes to one hour.
Examples of auras include:
- Visual phenomena, such as seeing various shapes, bright spots or flashes of light
- Vision loss
- "Pins-and-needles" sensations in an arm or leg
- Weakness or numbness in the face, or one side of the body
- Difficulty speaking
- Hearing noises or music
- Uncontrollable jerking or other movements
3. Attack
A migraine usually lasts from four to 72 hours if untreated, and the frequency varies by the person. Migraines might occur rarely or strike several times a month.
During a migraine, you might have:
- Pain, usually on one side of your head, but often on both sides
- Pain that throbs or pulses
- Sensitivity to light, sound, and sometimes smell and touch
- Nausea and vomiting
4.
 Post-drome
Post-dromeAfter a migraine attack, you might feel drained, confused and washed out for up to a day. Some people report feeling elated. Sudden head movement might bring on pain again briefly.
Migraines are often undiagnosed and untreated. If you regularly have signs and symptoms of migraines, keep a record of your attacks and how you treated them. Then make an appointment with your health care provider to discuss your headaches.
Learn more about headaches:
- Get 6 tips for headache relief.
- Get the facts about headache medication.
- Learn about Botox as a chronic migraine treatment.
- Read common questions about headaches and get answers.
Nancy Erickson, M.D., is a Family Medicine physician in Onalaska, Wisconsin.
For the safety of our patients, staff and visitors, Mayo Clinic has strict masking policies in place. Anyone shown without a mask was either recorded prior to COVID-19 or recorded in a non-patient care area where social distancing and other safety protocols were followed.
Topics in this Post
- Headache
- Family Medicine
Common questions about headaches
Tips to help ease anxiety
Easing the fear of nightmares
Which Type Do You Have?
Written by WebMD Editorial Contributors
In this Article
- With or Without Aura?
- With Brainstem Aura
- Episodic
- Chronic
- Hemiplegic
- Migraine Without Headache (Silent Migraine)
- Abdominal Migraine
- Menstrual
- Ocular (or Retinal)
- Vestibular
- Status Migrainosus
- Ophthalmoplegic Migraine
- When to Call the Doctor
Almost 38 million Americans get migraine attacks. They usually feel like pulsing or throbbing on one side of the head. They can also cause nausea, vomiting, and sensitivity to light and sound.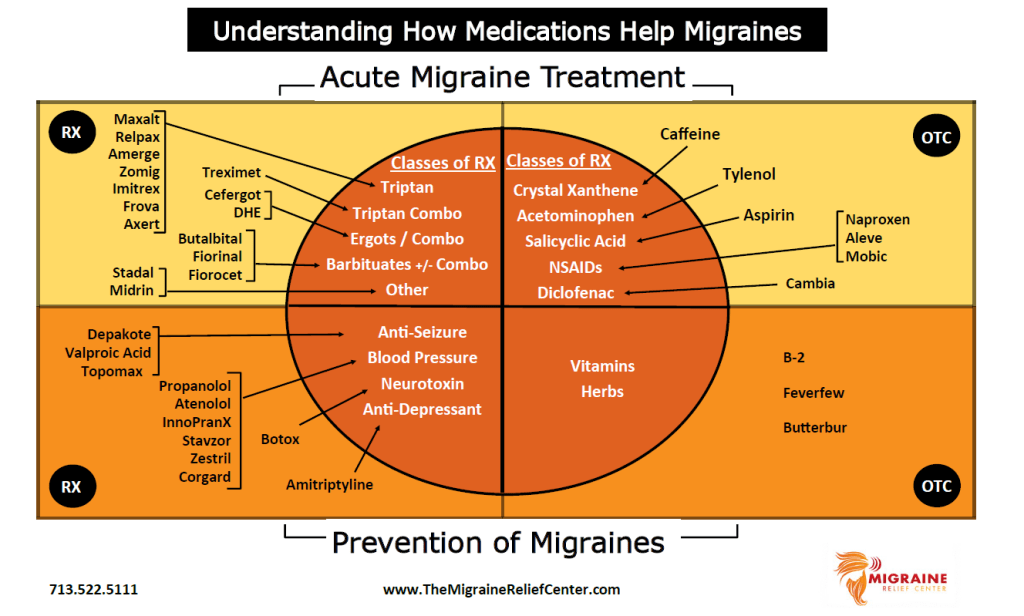 And they can be much more severe than other headaches.
And they can be much more severe than other headaches.
But migraine attacks aren’t all alike. Yours might be very different from someone else’s.
With or Without Aura?
The two major categories are migraine with aura (once called "classical migraines”) and migraine without aura (formerly known as "common migraines”).
"Aura" usually includes visual symptoms like lines, shapes, or flashes. You may even lose some of your vision for 10 to 30 minutes. You could also feel tingling in your arms and legs. Auras can even affect smell, taste, touch, or speech.
Aura happens to about 1 in 4 people who get migraine headaches. It usually starts before the head pain begins and lasts up to an hour.
There are also several migraine subtypes.
With Brainstem Aura
This used to be called basilar type migraine. It includes visual, sensory, or speech or language symptoms and at least two of the following: slurred speech, vertigo (a sensation of spinning or dizziness), tinnitus (ringing in the ears), double vision, unsteadiness, and a severe sensitivity to sound.
Episodic
This is the general pattern for most people with migraine. It means you get migraine attacks from time to time – up to about 7 days out of the month. In general, if you have a headache or migraine attack on more than 7 days out of the month, you may have a more serious form of migraine like high-frequency episodic migraine or chronic migraine (see below).
High-frequency episodic
This pattern of migraine means you have 8 to 14 headache days per month with at least some migraine symptoms. It also makes you more likely than others to develop chronic migraine.
Chronic
This is a headache that happens 15 or more days a month for more than 3 months. It includes migraine symptoms on at least 8 of those days each month.
Hemiplegic
This word means "paralysis on one side of the body." The aura that comes along with these headaches causes temporary (less than 72 hours) weakness on one side of the body. The aura symptoms usually go away within 24 hours.
The symptoms are very similar to a stroke but cause no lasting nerve damage.
Still, don't diagnose yourself! If you have symptoms of hemiplegic migraine, get medical help right away to rule out a stroke.
Migraine Without Headache (Silent Migraine)
Yes, you can have a migraine without head pain. It's often called a "silent" migraine.
Aura is usually the main warning sign of this type of migraine. But you may also have nausea and other migraine symptoms. It usually lasts only about 20-30 minutes.
Abdominal Migraine
An abdominal migraine affects your belly instead of your head. The symptoms include:
- Stomach pain
- Nausea
- Appetite loss
- Vomiting
Adults can get abdominal migraines. But they usually affect children who also have regular migraines, or who have relatives with migraines.
Doctors don't know what causes them. But they share some of the same triggers as regular migraines. And migraine medications can work to treat them.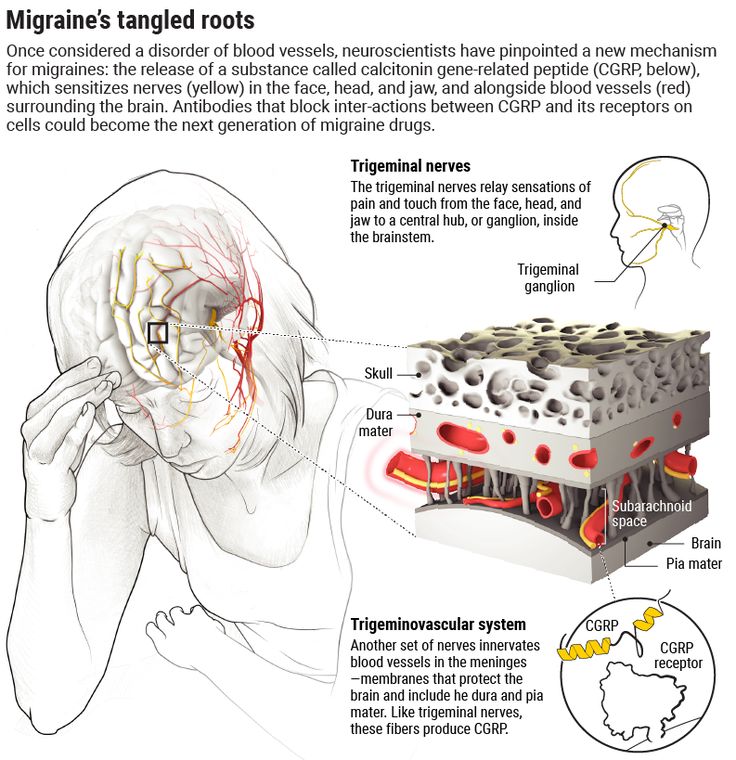
Menstrual
These usually happen 2 days before the start of a woman’s period and last through 3 days after. Women who get these may also have other kinds of migraine headaches at other times of the month, but the migraine around menstruation is usually without aura.
Ocular (or Retinal)
This form of migraine is very rare. It involves seeing colors, flashing lights, or other visual changes, including the loss of some or all vision in one eye. The visual loss should last less than an hour and be followed by a typical migraine headache. However, other serious conditions can cause sudden loss of vision in one eye, so go to a doctor right away if you have vision changes.
Vestibular
With this type of migraine, you also get vertigo. The spinning sensation usually lasts a few minutes to hours.
Status Migrainosus
Ongoing pain -- lasting longer than 3 days -- is a trait of status migrainosus. It can be caused by some medications or medication withdrawal.
The pain and nausea from this type of migraine can be so intense that you need hospital care. Get help right away if so.
Ophthalmoplegic Migraine
If you have pain and weakness around your eye, you need medical help right away. Rare symptoms like these may be due to ophthalmoplegic migraine -- what's now known as a neuralgia -- or a more serious condition. Ophthalmoplegic migraines often last a week and may cause a droopy eyelid, double vision, and other eye changes.
When to Call the Doctor
Call your doctor right away if you have:
- A change in migraine features, how often a migraine happens, or how severe it is
- A headache that lasts days, getting worse as it goes
- A headache brought on by coughing, sneezing, bearing down, or straining while on the toilet
Call 911 or go to the emergency room if you have:
- The worst headache you’ve ever had, especially if it started very quickly
- Headache after a head injury
- Head injury with loss of consciousness
- Fever or stiff neck with a headache
- Confusion or lack of consciousness
- Paralysis or weakness
- Seizure
- Change in vision
- Vision loss
Immunology of headache
The assumption about the participation of cells of the immune system in the pathogenesis of headache (HA) has been found in the works of scientists since the 70s [1, 2]. Despite the ambiguity of the results obtained in the course of numerous experiments, all researchers agree on one thing: the immune system plays a key role in the development and chronicity of G.B. The analysis of numerous data made it possible to identify the main neuroimmunological mechanisms of the primary forms of this pathology.
Despite the ambiguity of the results obtained in the course of numerous experiments, all researchers agree on one thing: the immune system plays a key role in the development and chronicity of G.B. The analysis of numerous data made it possible to identify the main neuroimmunological mechanisms of the primary forms of this pathology.
Allergic mechanism GB
Based on clinical observations, it was initially hypothesized that an allergic mechanism is involved in the pathophysiology of migraine. The high comorbidity of migraine and atopic diseases such as eczema and asthma has come to be considered as the main argument in favor of a presumed dysfunction of the immune system in patients with migraine [1]. Seasonal allergies are one of the commonly identified migraine triggers. So, according to the results of the study by M.I. Karpova [3], allergic diseases account for 15% of all identified somatic disorders in patients with tension headache (THE), regardless of the course of cephalalgia, 16% in episodic migraine, and 18% in chronic. In one study, when measuring serum histamine and total IgE levels in 70 patients with migraine without aura, the following values were obtained: 48.2 ng / ml and 38.3 IU / ml in the control group, 105.0 ng / ml and 79.1 IU/ml for migraine without allergy and 159.1 ng/ml and 303.3 IU/ml for migraine and allergy, respectively. It was concluded that the relationship between allergy and migraine may be based on an IgE-mediated mechanism and histamine release. However, if allergic reactions are involved in the development of HD, this cannot explain the increased frequency of migraine in conditions where mast cell activation occurs in the absence of high serum IgE titers, such as in eczema, interstitial cystitis, or irritable bowel syndrome. In addition, histamine receptor antagonists are ineffective in the treatment of migraine, therefore, the pathophysiological mechanisms of migraine development are more complex and are not limited to an increase in the level of plasma histamine [4].
In one study, when measuring serum histamine and total IgE levels in 70 patients with migraine without aura, the following values were obtained: 48.2 ng / ml and 38.3 IU / ml in the control group, 105.0 ng / ml and 79.1 IU/ml for migraine without allergy and 159.1 ng/ml and 303.3 IU/ml for migraine and allergy, respectively. It was concluded that the relationship between allergy and migraine may be based on an IgE-mediated mechanism and histamine release. However, if allergic reactions are involved in the development of HD, this cannot explain the increased frequency of migraine in conditions where mast cell activation occurs in the absence of high serum IgE titers, such as in eczema, interstitial cystitis, or irritable bowel syndrome. In addition, histamine receptor antagonists are ineffective in the treatment of migraine, therefore, the pathophysiological mechanisms of migraine development are more complex and are not limited to an increase in the level of plasma histamine [4].
Study by V.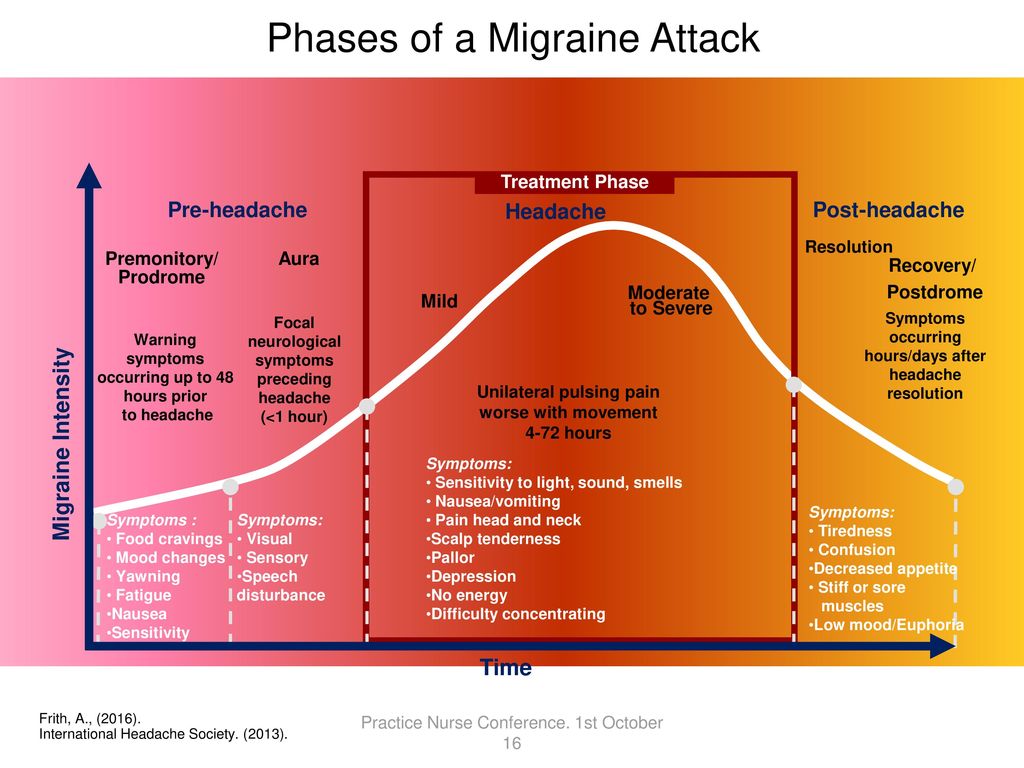 Martin et al. [4] shows that the association of allergy with migraine depends on age, the degree of allergic sensitization, and the use of immunotherapy. A low "grade of atopy" was associated with less frequent and disabling migraine attacks in younger people, while higher grades were associated with more frequent attacks. As a result of immunotherapy of allergic rhinitis, the frequency and severity of HA decreased in younger people [5].
Martin et al. [4] shows that the association of allergy with migraine depends on age, the degree of allergic sensitization, and the use of immunotherapy. A low "grade of atopy" was associated with less frequent and disabling migraine attacks in younger people, while higher grades were associated with more frequent attacks. As a result of immunotherapy of allergic rhinitis, the frequency and severity of HA decreased in younger people [5].
Infections and HD
An association between GB and infectious processes has also been found. The ninth section of the International Classification of Headaches (ICHD-3 beta version) is assigned to a special type of secondary headaches associated with the direct impact of infectious processes - "Headaches associated with infections" [6], while in this article we are talking about primary headaches. B. A high frequency of subclinical and clinical infections has been found in patients with migraine, which indirectly supports the idea that the immune system is involved in the mechanisms of the development of this disease. Patients note that infections not only precede migraine attacks, but also increase the intensity of GB. Based on the obtained clinical, anamnestic and laboratory data, D.V. Maltsev [7] substantiated the relationship between the existing active herpes infection, identified immune disorders and GB attacks in patients with severe migraine without aura, on the basis of which he identified an immune-dependent form of migraine without aura and developed a method for the preventive treatment of severe migraine without aura using immunotropic drugs . Other scientists have found a link between infection with virus Varicella zoster and the occurrence of short-term unilateral neuralgic headache with conjunctival injection and lacrimation [8] and nummular headache [9]. A number of scientists [12, 13] found a connection between migraine and infections Toxoplasma gondii [10, 11], Chlamydia pneumoniae .
Patients note that infections not only precede migraine attacks, but also increase the intensity of GB. Based on the obtained clinical, anamnestic and laboratory data, D.V. Maltsev [7] substantiated the relationship between the existing active herpes infection, identified immune disorders and GB attacks in patients with severe migraine without aura, on the basis of which he identified an immune-dependent form of migraine without aura and developed a method for the preventive treatment of severe migraine without aura using immunotropic drugs . Other scientists have found a link between infection with virus Varicella zoster and the occurrence of short-term unilateral neuralgic headache with conjunctival injection and lacrimation [8] and nummular headache [9]. A number of scientists [12, 13] found a connection between migraine and infections Toxoplasma gondii [10, 11], Chlamydia pneumoniae .
The focus of many scientists is the connection between GB and Helicobacter pylori infection.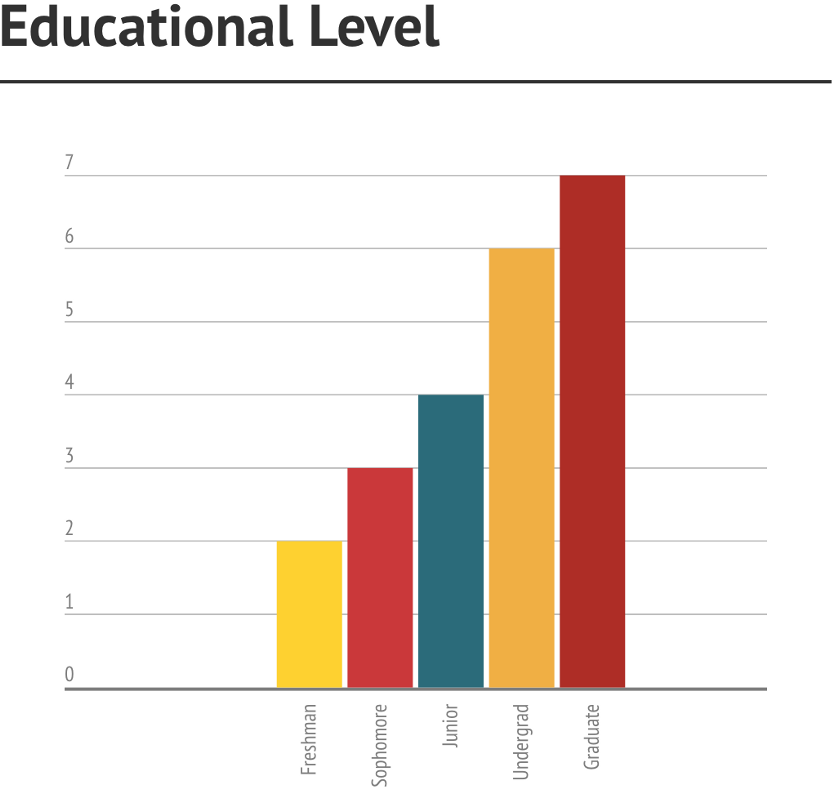 M. Hosseinzadeh et al. [16] in patients with migraine ( n = 70) and healthy ( n = 70) the following indicators were assessed: IgG and IgM antibody titer to Helicobacter pylori , age, profession, the presence of diseases of the gastrointestinal tract (GIT), mode and characteristics of nutrition, intake medications, sleep disturbances, the effects of stress, environmental and other factors. The highest prevalence of migraine was among housewives (40%), who had a high association of headache attacks and menstruation (69.5%). In 75.7% of patients with migraine, gastrointestinal diseases were diagnosed: gastroesophageal reflux (47.1%), gastric ulcer (17.1%), gastritis (4.3%). These data are consistent with the results of other studies [14, 15], confirming a significant correlation between migraine and digestive disorders. The average value of the optical density of IgG and IgM antibodies to H. p ylori were 60.08±7.7 and 32.1±8.7 respectively in the migraine group and 21.
M. Hosseinzadeh et al. [16] in patients with migraine ( n = 70) and healthy ( n = 70) the following indicators were assessed: IgG and IgM antibody titer to Helicobacter pylori , age, profession, the presence of diseases of the gastrointestinal tract (GIT), mode and characteristics of nutrition, intake medications, sleep disturbances, the effects of stress, environmental and other factors. The highest prevalence of migraine was among housewives (40%), who had a high association of headache attacks and menstruation (69.5%). In 75.7% of patients with migraine, gastrointestinal diseases were diagnosed: gastroesophageal reflux (47.1%), gastric ulcer (17.1%), gastritis (4.3%). These data are consistent with the results of other studies [14, 15], confirming a significant correlation between migraine and digestive disorders. The average value of the optical density of IgG and IgM antibodies to H. p ylori were 60.08±7.7 and 32.1±8.7 respectively in the migraine group and 21.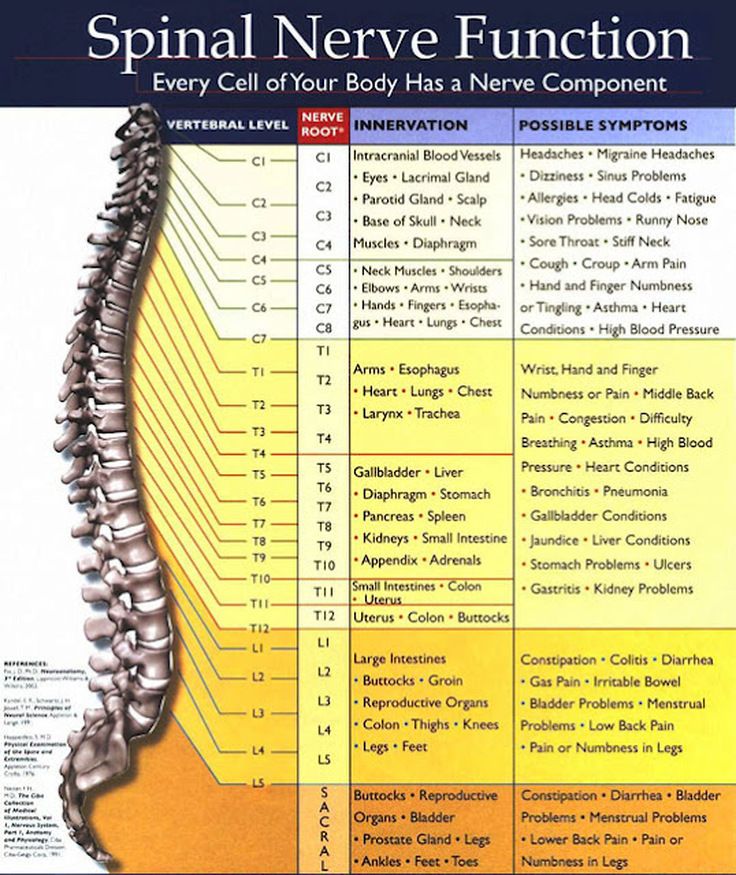 82±6.2 and 17.6±9.4 in the control group group. The prevalence of migraine and IgG and IgM titers to H. p ylori were significantly correlated using independent Student's T-test ( p ≡0.048 and p ≡0.03, respectively). In 71.4% of cases, the main stimulus for the onset of GB was stress, while 91.4% of patients noted the onset of anxiety after an attack. In addition, 72.9% of patients had sleep disorders. About 48.6% of patients noted a particular relationship between the occurrence and severity of a migraine attack and the consumption of certain foods, especially cheese (17.1%), fatty foods (12.9%) and spices (11.4%). Thus, the results of the study showed a strong correlation between migraine and H. pylori infection, gastrointestinal diseases, stress, social class, nutrition and sleep quality. Based on the data obtained, scientists propose to consider Helicobacter pylori infection as an etiological factor in migraine. In addition, according to the literature [17–19], as a result of aimed at eliminating the infection H .
82±6.2 and 17.6±9.4 in the control group group. The prevalence of migraine and IgG and IgM titers to H. p ylori were significantly correlated using independent Student's T-test ( p ≡0.048 and p ≡0.03, respectively). In 71.4% of cases, the main stimulus for the onset of GB was stress, while 91.4% of patients noted the onset of anxiety after an attack. In addition, 72.9% of patients had sleep disorders. About 48.6% of patients noted a particular relationship between the occurrence and severity of a migraine attack and the consumption of certain foods, especially cheese (17.1%), fatty foods (12.9%) and spices (11.4%). Thus, the results of the study showed a strong correlation between migraine and H. pylori infection, gastrointestinal diseases, stress, social class, nutrition and sleep quality. Based on the data obtained, scientists propose to consider Helicobacter pylori infection as an etiological factor in migraine. In addition, according to the literature [17–19], as a result of aimed at eliminating the infection H . pylori treatment reduces the frequency, intensity and duration of migraine attacks.
pylori treatment reduces the frequency, intensity and duration of migraine attacks.
In the study of M.I. Karpova [3] found that in the chronic course of HDN significantly more often than in episodic cases, frequent acute respiratory viral infections (ARVI), chronic inflammatory infectious diseases of the throat and nose were diagnosed. Chronic migraine compared to episodic migraine is characterized by a higher incidence of acute respiratory viral infections, allergic urticaria, chronic infections of the urinary system and diseases associated with H . pylori . Chronic recurrent infectious and inflammatory diseases, which, despite the variety of clinical manifestations, are based on an immunodeficiency state, occupied 35% in the structure of episodic TTH and 51% in chronic. In patients with episodic migraine, this figure was 43%, with chronic - 46%. Based on the data of scientific publications, it can be concluded that secondary immunodeficiency, characterized by the development of chronic recurrent infectious diseases, has a negative impact on the clinical manifestations of HDN and migraine, being one of the leading factors in their progression [3].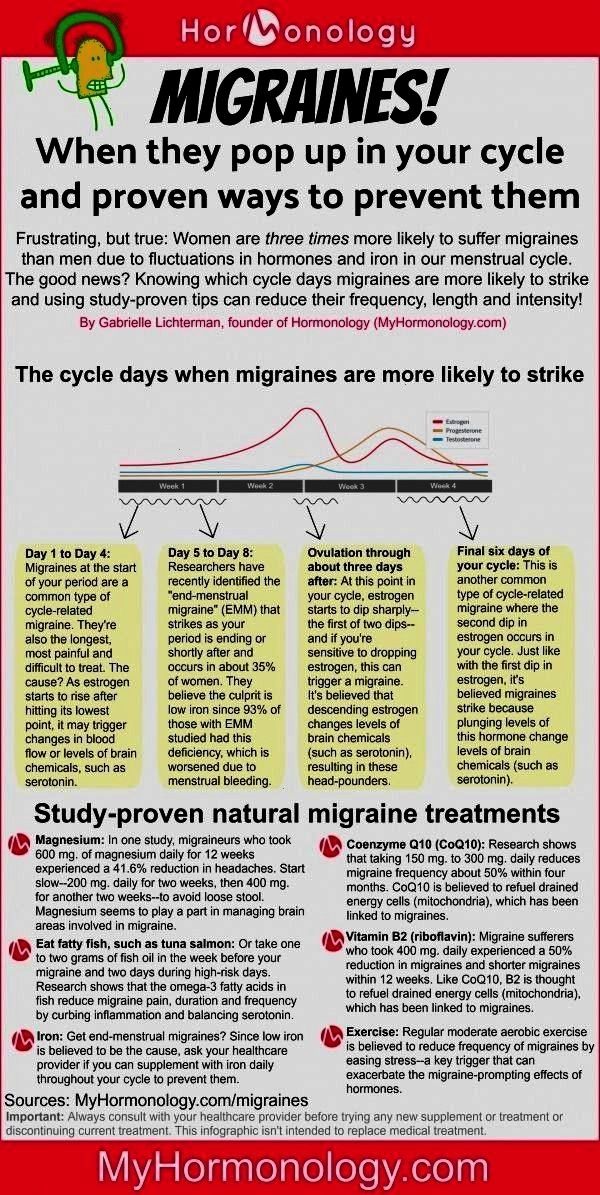
Of interest is the high prevalence of HD in patients with chronic fatigue syndrome (CFS) and fibromyalgia, the development of which is associated with stress, decreased immunity, and infections [20, 21]. Thus, in the study by M. Ravindran [22], migraine was diagnosed in 84% of patients with CFS, HDN — in 81%, in the control group — in 5 and 45%, respectively. At the same time, patients with CFS suffering from migraine without aura had a higher prevalence of fibromyalgia (47%) compared with the control group (0%). Scientists concluded that there are similar pathophysiological mechanisms for the development of these diseases. In 2011, employees of the Research Clinic for Functional Disorders and Psychosomatics at the Aarhus University Hospital (Denmark) introduced the concept of "Bodily Distress Syndrome", the typical symptoms of which are headache, back pain, muscle pain, joint pain, gastrointestinal disorders, shortness of breath, fatigue. Scientists suggest using this diagnosis if the listed symptoms cannot be explained by a specific disease. Recent studies have shown that, despite the similarity of symptoms, patients are given different diagnoses: "fibromyalgia", "chronic fatigue syndrome", "irritable bowel syndrome", various chronic pain syndromes, "somatoform disorder", "multiple chemical sensitivity". According to the authors of [23], different diagnoses are subtypes of the same disorder.
Recent studies have shown that, despite the similarity of symptoms, patients are given different diagnoses: "fibromyalgia", "chronic fatigue syndrome", "irritable bowel syndrome", various chronic pain syndromes, "somatoform disorder", "multiple chemical sensitivity". According to the authors of [23], different diagnoses are subtypes of the same disorder.
Scientific data indicate the presence of changes in the serum levels of various immunocompetent cells in patients with migraine and TTH. Below is a detailed analysis of the involvement of immune system components in the development and progression of HD.
Immunocompetent cells - clinical markers of HD
In the first works on the relationship between the immune system and the HD clinic, attention was focused on the influence of mast cells on the spreading cortical depression in migraine. The suggestion that activation of mast cells in the dura mater may be a pathophysiological mechanism for the development of HD is also based on the results of studies showing that the level of histamine in the serum of patients with cluster HD due to it increases. In addition, biopsy of the temporal artery on the painful side of patients suffering from cluster HA revealed degranulated mast cells [24].
In addition, biopsy of the temporal artery on the painful side of patients suffering from cluster HA revealed degranulated mast cells [24].
In addition to vasodilating molecules, mast cells secrete various pro-inflammatory mediators: kinins, prostaglandins, and numerous cytokines, including IL-6 and TNF-α [24, 25]. Mast cell cytokines are involved in the development of neuropsychiatric disorders. Mast cell secretion is stimulated by IgE and antigens, anaphylotoxins, cytokines, hormones, and neuropeptides. The latter include substance P, somatostatin, neurotensin, parathyroid hormone, a peptide that activates pituitary adenylate cyclase, and a peptide associated with the calcitonin gene, which is localized with substance P and serotonin receptors in trigeminal ganglion neurons. Mast cells are able to selectively and locally release some mediators: serotonin, eicosanoids, and IL-6, substances involved to some extent in the pathogenesis of HD [24].
Mast cells in the brain can regulate the permeability of blood vessels in it.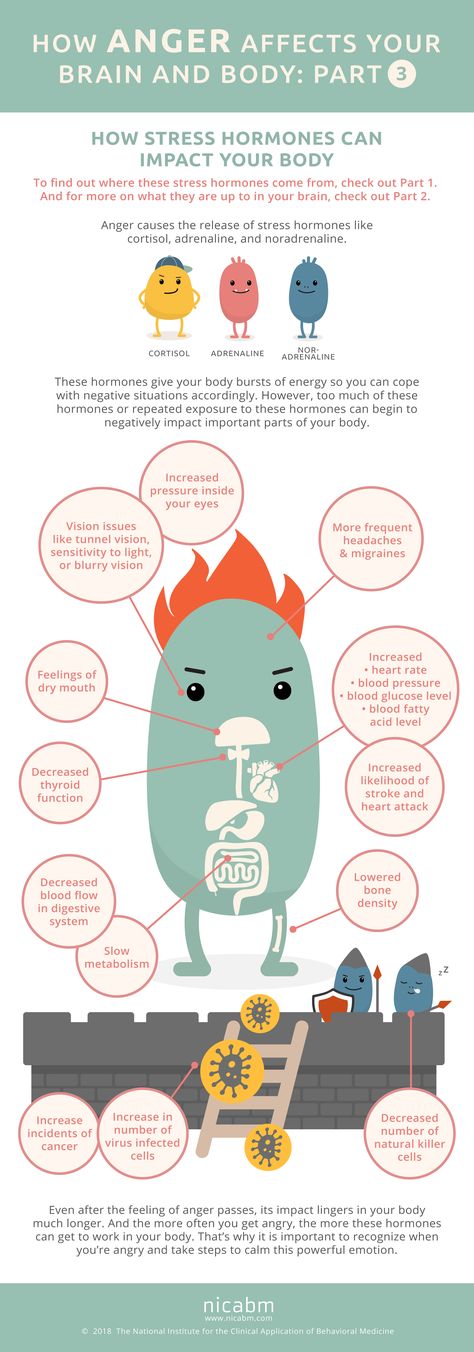 Their vasodilating molecules include histamine, nitric oxide (NO), vasoactive intestinal peptide, and vascular endothelial growth factor, which may be responsible for the vasodilation phase associated with throbbing migraine pain. For example, histamine release does not induce severe headache, while NO is considered by many scientists [24] to be a key molecule in the pathophysiology of migraine. Other scientists [26] suggest that mast cells contribute to the development of migraine through the activation of the renin-angiotensin system due to the ability to release renin and increase the local production of angiotensin II. This hypothesis may explain the association between migraine and cardiovascular disease, as well as the effectiveness of antihypertensive drugs in migraine prevention.
Their vasodilating molecules include histamine, nitric oxide (NO), vasoactive intestinal peptide, and vascular endothelial growth factor, which may be responsible for the vasodilation phase associated with throbbing migraine pain. For example, histamine release does not induce severe headache, while NO is considered by many scientists [24] to be a key molecule in the pathophysiology of migraine. Other scientists [26] suggest that mast cells contribute to the development of migraine through the activation of the renin-angiotensin system due to the ability to release renin and increase the local production of angiotensin II. This hypothesis may explain the association between migraine and cardiovascular disease, as well as the effectiveness of antihypertensive drugs in migraine prevention.
Interaction of qualitative and quantitative characteristics of leukocytes in the GB clinic
In a number of studies, during a migraine attack, an increase in the number of rosette-forming cells, NK cells (natural killers), monocyte chemotaxis and a positive phagocytic response, a decrease in the content of T-lymphocytes, a deficiency of phagocytes and their cytotoxic activity was noted compared with the interictal period and control [27 , 28].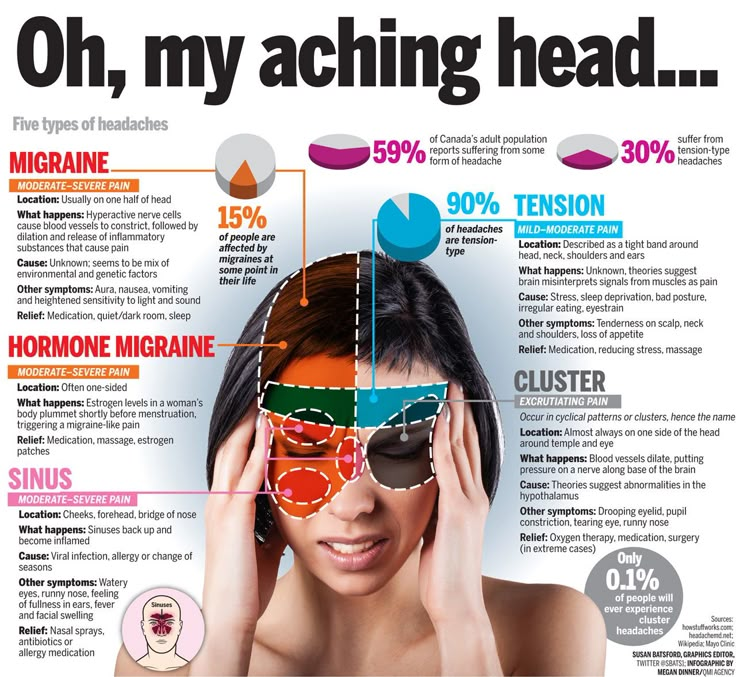 In the work of G. Stirparo et al. [29] showed an increase in the number of monocytes and NK cells in the peripheral blood in cluster GB. At the same time, no changes in the function of monocytes were detected in episodic or chronic TTH.
In the work of G. Stirparo et al. [29] showed an increase in the number of monocytes and NK cells in the peripheral blood in cluster GB. At the same time, no changes in the function of monocytes were detected in episodic or chronic TTH.
Other scientists have reported that activated macrophages contribute to pain conditions. They can release a variety of inflammatory mediators, in particular the pro-inflammatory cytokines TNF-α and interleukin-1β (IL-1β)), nerve growth factor (NGF), NO, and prostaglandins. In the experimental deficit of macrophages in peripheral tissues, they greatly contribute to the inflammatory pain that is produced by zymosan and the irritating acetic acid. In addition, it is assumed [30] that the activation of macrophages has a marked effect on the subsequent recruitment and activation of other types of cells (eg, neutrophils) at the site of inflammation.
A.V. Maltsev [7] described the characteristic changes in the blood count in patients with severe migraine without aura in the period between attacks, which consisted in a pronounced imbalance in the levels of granulo- and agranulocytes due to absolute lymphocytosis (in 53% of patients) against the background of a high proportion of leuko- (in 34 %) and neutropenia (in 35%).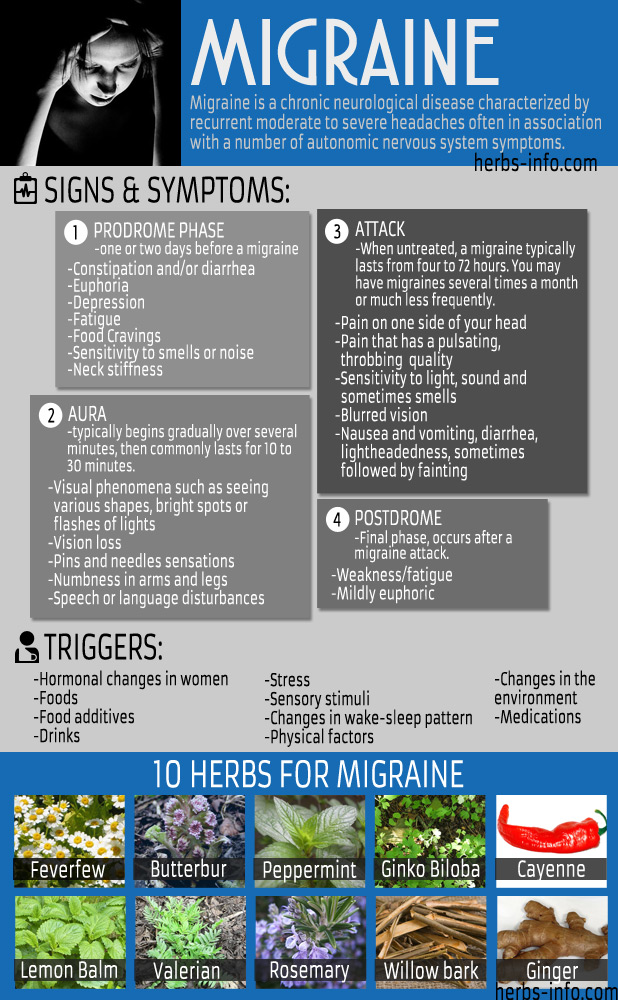 In patients with migraine without aura in the interictal period, insufficiency of the cellular component of innate immunity was revealed, which consisted in a pronounced decrease in the level of large granular lymphocytes and CD3-CD16+CD56+ cells (natural killers), as well as a low level of phagocytic activity of neutrophils. A significant decrease in the average level of the immunoregulatory index and a significant increase in the number of CD3 + CD8 + cytotoxic (killer-suppressor) lymphocytes were also found, which indicated dysfunction of the immune system in patients with migraine. Such changes in the immune status indicate the presence of chronic viral, bacterial, protozoal infections.
In patients with migraine without aura in the interictal period, insufficiency of the cellular component of innate immunity was revealed, which consisted in a pronounced decrease in the level of large granular lymphocytes and CD3-CD16+CD56+ cells (natural killers), as well as a low level of phagocytic activity of neutrophils. A significant decrease in the average level of the immunoregulatory index and a significant increase in the number of CD3 + CD8 + cytotoxic (killer-suppressor) lymphocytes were also found, which indicated dysfunction of the immune system in patients with migraine. Such changes in the immune status indicate the presence of chronic viral, bacterial, protozoal infections.
M.I. Karpova [3] found that in patients with episodic and chronic migraine, as well as in patients with chronic TTH, there was a decrease in the relative number of CD3+ (an integral indicator of the cellular link of immunity), CD11b+ (a subpopulation of prekillers) of lymphocytes, which indicates a lack of cellular effector link of immunity. In addition, in chronic migraine, a decrease in the relative number of CD4+ (T-helpers), the ratio of CD4+/CD8+ (immune regulatory index) was registered, in chronic TTH — a decrease in the percentage of CD4+. A decrease in the level of the main regulatory cells of the immune response indicates the inability of the body to resist infections. It is CD4+ cells that infect the human immunodeficiency virus (HIV). There are two subpopulations of helper T-cells - CD4+ - Th2 and Th3, which differ in the set of synthesized cytokines. A decrease in their total number indicates an imbalance of pro- and anti-inflammatory cytokines, as well as a decrease in the formation of antibodies, especially IgE. Thus, both the direction of the unfolding of the immune response and its effectiveness depend on the activity of T-helpers.
In addition, in chronic migraine, a decrease in the relative number of CD4+ (T-helpers), the ratio of CD4+/CD8+ (immune regulatory index) was registered, in chronic TTH — a decrease in the percentage of CD4+. A decrease in the level of the main regulatory cells of the immune response indicates the inability of the body to resist infections. It is CD4+ cells that infect the human immunodeficiency virus (HIV). There are two subpopulations of helper T-cells - CD4+ - Th2 and Th3, which differ in the set of synthesized cytokines. A decrease in their total number indicates an imbalance of pro- and anti-inflammatory cytokines, as well as a decrease in the formation of antibodies, especially IgE. Thus, both the direction of the unfolding of the immune response and its effectiveness depend on the activity of T-helpers.
A recent study by M. Arumugam and V. Parthasarathy [31] also confirms that immunoregulatory disorders may be involved in the pathophysiology of migraine. Scientists found an increase in the level of CD4+ T-helpers and a decrease in T-cytotoxic CD8+ and immunoregulatory CD4+CD25+ lymphocytes.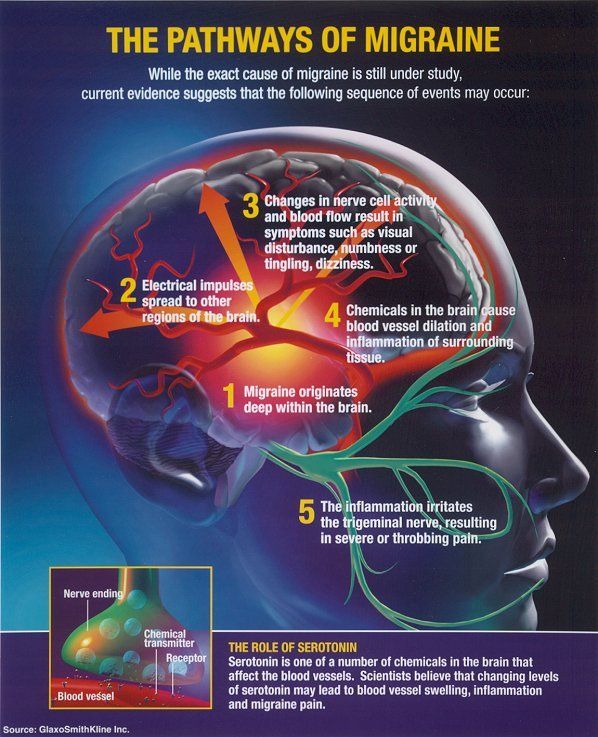
The role of cell and intercellular adhesion molecules in the pathogenesis of HD
According to the trigeminal-vascular theory, aseptic neurogenic inflammation activates the nociceptive terminals of the afferent fibers of the trigeminal nerve located in the vascular wall, leading to the formation of GB [32]. According to scientists, selectins, cell adhesion molecules, play an important role in the process of leukocyte transmigration to the site of damage during an inflammatory response stimulated by pro-inflammatory cytokines. P. Sarchielli et al. [33] determined the content of soluble forms of cell adhesion molecules - sL- and sE-selectins, intercellular adhesion sICAM-1 and vascular cell adhesion sVCAM-1 in serial samples of internal jugular venous blood taken from patients with migraine without aura during attacks, in correlation with the level of pro-inflammatory cytokines TNF-α, IL-1β and IL-6. Lymphocytes obtained from jugular venous blood were also evaluated for the expression of leukocyte function antigen (LFA-1) and very late activation antigen (VLA-4), involved in the recruitment and adhesion of leukocytes at the site of inflammation. A decrease in their expression was manifested by recurrent bacterial infections and impaired functional adhesion of leukocytes. During the study, a simultaneous transient increase in sICAM-1, TNF-α and IL-6 was noted in the first 2 hours after the onset of an attack and the moment of catheter placement ( p <0.0001; p <0.001 and p <0.003, respectively). There was a progressive decrease in LFA-1 expression by CD4+ and CD8+ T cells with significantly lower percentages at 2 and 4 hours after the onset of an attack ( p <0.01 and p <0.022, respectively). Variations in the percentage of VLA-4 expressing cells were not observed. Probably, a short-term increase in sICAM-1 and TNF-α in the blood of the internal jugular vein of patients with migraine without aura can be caused by sensory neuropeptides released from activated trigeminal endings. Thus, the inflammatory component of the pathogenesis of migraine was experimentally confirmed, in which cellular and intercellular adhesion molecules produced under the action of pro-inflammatory cytokines take part.
A decrease in their expression was manifested by recurrent bacterial infections and impaired functional adhesion of leukocytes. During the study, a simultaneous transient increase in sICAM-1, TNF-α and IL-6 was noted in the first 2 hours after the onset of an attack and the moment of catheter placement ( p <0.0001; p <0.001 and p <0.003, respectively). There was a progressive decrease in LFA-1 expression by CD4+ and CD8+ T cells with significantly lower percentages at 2 and 4 hours after the onset of an attack ( p <0.01 and p <0.022, respectively). Variations in the percentage of VLA-4 expressing cells were not observed. Probably, a short-term increase in sICAM-1 and TNF-α in the blood of the internal jugular vein of patients with migraine without aura can be caused by sensory neuropeptides released from activated trigeminal endings. Thus, the inflammatory component of the pathogenesis of migraine was experimentally confirmed, in which cellular and intercellular adhesion molecules produced under the action of pro-inflammatory cytokines take part.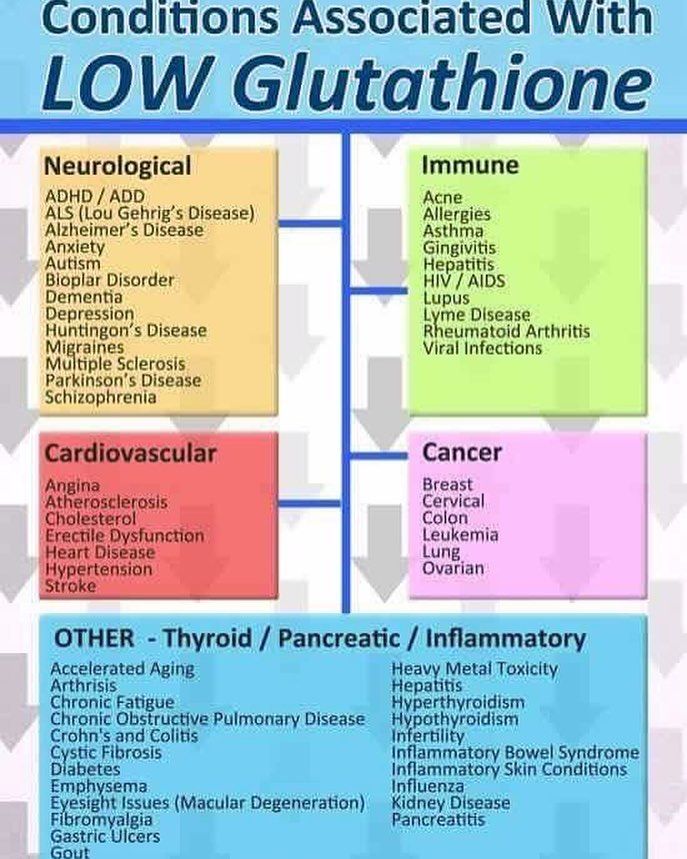
Adiponectin - a link between obesity and HD
Obesity is known to be a significant risk factor for the development of chronic migraine. It has been established that metabolically and hormonally active adipose tissue secretes more than 30 different regulatory substances - adipokines or adipocytokines. Among the latter, adiponectin (A) attracts special attention, which can probably modulate the action of inflammatory mediators involved in the pathogenesis of migraine. It increases tissue sensitivity to insulin and glucose tolerance, reduces lipid content in cells, has an anti-atherogenic effect, and also has an anti-inflammatory effect by inhibiting the production of IL-6 and TNF cytokines and inducing the production of the cytokine IL-10. Adiponectin reduces migraine symptoms. A large amount of adipose tissue leads to a decrease in the secretion of adiponectin, and consequently, to an increase in inflammatory reactions and increased headache. At the same time, a sharp increase in the level of adiponectin also leads to a deterioration in the general condition in HD [34].
At the same time, a sharp increase in the level of adiponectin also leads to a deterioration in the general condition in HD [34].
Results of recent clinical trials by B. Marics et al. [35] also point to a link between obesity and migraine. Experiments in rats fed a diet high in fat and sucrose found an increase in the basal level of the TRPA1 agonist-induced release calcitonin gene-related peptide (CGRP) receptor from trigeminal afferent fibers in rats suffering from obesity and insulin resistance, and a reduced release of CGRP in response to potassium chloride. These rats also showed additional vasodilation of the meningeal arteries after dural administration of acrolein, a TRPA1 receptor agonist, a decrease in TRPA1 protein expression in the trigeminal ganglion, and an increase in the level of circulating pro-inflammatory cytokines - IL-1 and IL-6, in addition to an increase in the blood concentration of insulin and fasting glucose. TRPA1 is an ankyrin receptor that is expressed to a greater extent in small-diameter nociceptors located in the trigeminal, nodose, and jugular ganglia, as well as in the posterior roots of the spinal cord, and directly perceives pain stimuli and inflammatory mediators. Thus, trigeminal nerve sensitization can be considered as a mechanism for the development of HD in obese individuals.
Thus, trigeminal nerve sensitization can be considered as a mechanism for the development of HD in obese individuals.
Cytokines - regulators of the interaction of the immune and nervous systems
The interaction between immune cells is regulated by several mechanisms, including the action of cytokines, which play an important role in modulating the quality and intensity of the immune response. The hypothesis that cytokines are possible mediators of pain explains the potential mechanism for its generation in migraine and TTH. A growing body of evidence suggests that pain and inflammation are related, and related publications [36, 37] often use the term “neurogenic inflammation”. This theory is supported by the effectiveness of the use of non-steroidal anti-inflammatory drugs in the treatment of these pathologies. It is likely that cytokines play a role in mediating neurovascular inflammation in migraine. Activation and sensitization of meningeal nociceptors leads to afferent signaling, which, according to many researchers [38, 39], contributes to the occurrence of G. B. Recent data [40] also indicate that the formation of drug-induced GB is based on the activation of Toll-like receptors-4 located on glial cells, which leads to the synthesis of pro-inflammatory cytokines, adhesion molecules, costimulatory molecules, followed by activation of adaptive immunity structures.
B. Recent data [40] also indicate that the formation of drug-induced GB is based on the activation of Toll-like receptors-4 located on glial cells, which leads to the synthesis of pro-inflammatory cytokines, adhesion molecules, costimulatory molecules, followed by activation of adaptive immunity structures.
However, the role of cytokines in the pathophysiology of HD remains unclear. Thus, some authors point to an increase in the level of pro-inflammatory cytokines in various types of AH, while others note the absence of changes in their plasma levels [41, 42].
Pro- (TNF-α, IL-1b, IL-6) and anti-inflammatory (IL-10, IL-4, IL-3 and IL-2) cytokines play an important role in modulating pain threshold and may promote sensitization of trigeminal fibers [43]. It has been proven that hyperalgesia can be induced by administration of IL-1 or TNF-α. The key role of pro-inflammatory cytokines in the development of hyperalgesia becomes apparent when one considers that it can be blocked by an IL-1 receptor antagonist or TNF-binding protein [44].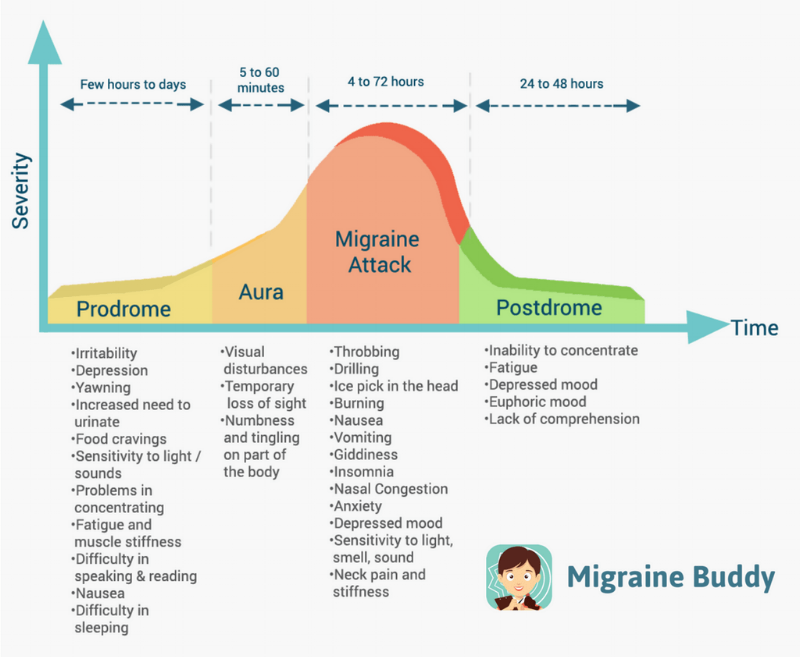
L. Boćkowski et al. [41] found an increase in the levels of pro-inflammatory cytokines (IL-1, sTNF-RI and TNF-α) in children with migraine and HDN, and also that the level of IL-1β in patients with migraine with aura is significantly higher than in children with migraine with aura. migraine without aura. The investigators further analyzed plasma concentrations of anti-inflammatory cytokines (IL-4, IL-10, and IL-13) in children and adolescents with migraine and TTH during attacks and between attacks. An increase in the level of IL-4 was found in 17.1% of patients with migraine and 28.6% with TTH, IL-13 - in 17.1 and 15.2%, respectively, an increase in the concentration of IL-10 - only in 3 (4 .4%) of 68 patients. Pro-inflammatory cytokines are involved in the pathogenesis of migraine attacks, but fluctuations in cytokine levels in children may differ from those in adults.
In the work of M.I. Karpova [3] also stated an increase in the concentration of pro-inflammatory cytokines - IL-1α and TNF-α in patients suffering from migraine and chronic TTH compared with the control group.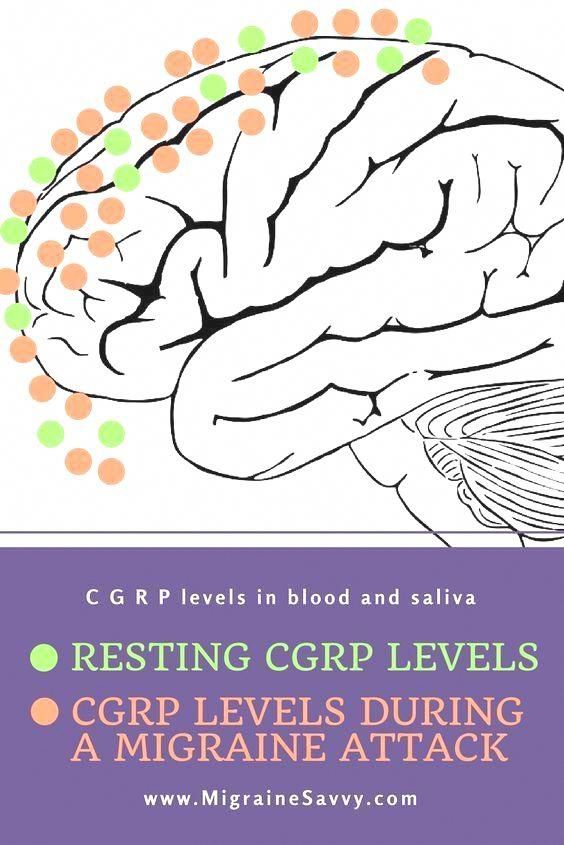 A positive correlation was found between the frequency of pain days and the serum levels of IL-1α and TNF-α in tension-type headache and migraine.
A positive correlation was found between the frequency of pain days and the serum levels of IL-1α and TNF-α in tension-type headache and migraine.
When measuring the levels of anti-inflammatory cytokines IL-4 and IL-10, it was found that during a migraine attack in adults there is a decrease in the level of IL-4, while the level of IL-10, on the contrary, increases. In a study [41], researchers noted that in 12 (52.2%) of 23 patients with migraine, plasma levels of IL-10 were significantly higher than in healthy controls. An increase in plasma levels of IL-4 was observed in 12 (37.5%), and IL-5 - in 27 (84.3%) patients with migraine. An increase in the level of IL-4 in blood plasma was found in 62.5% of cases in the interictal period.
Imbalance of Th2/Th3 cytokines produced by CD4+ T-helpers in the pathogenesis of HD
An important role in the development of migraine pain is played by an imbalance between Th2/Th3 cytokines. Th2 cytokines (IFN-γ, TNF-β, IL-2 and IL-3) affect cellular immunity, while Th3 cytokines (IL-4, IL-5, IL-6, IL-9, IL-10, IL-13 and granulocyte-macrophage colony-stimulating factor - GM-CSF) stimulate the development of B-cells, secretion of antibodies and provide a humoral response of the body. It was also shown that the Th2 subpopulation was reduced in patients with migraine without aura compared with the control group, while the serum IL-4 level was higher in the former. In migraine with aura, peripheral monocytes spontaneously release detectable in vitro large amounts of NO, and these patients have significantly higher serum NO levels than controls. It is assumed that NO may be involved not only in the modulation of the Th2/Th3 balance, but also in the activation of type 2 cyclooxygenase, which is responsible for the synthesis of prostaglandins. In turn, most pro-inflammatory cytokines (IFN-γ, IL-1β and TNF-α) are powerful inducers of NO release by monocytes. It has recently been found [45] that an increase in NO production by monocytes in patients with migraine without aura may be the result of activation of INOS expression secondary to a transient increase in NFkB activity.
Th2 cytokines (IFN-γ, TNF-β, IL-2 and IL-3) affect cellular immunity, while Th3 cytokines (IL-4, IL-5, IL-6, IL-9, IL-10, IL-13 and granulocyte-macrophage colony-stimulating factor - GM-CSF) stimulate the development of B-cells, secretion of antibodies and provide a humoral response of the body. It was also shown that the Th2 subpopulation was reduced in patients with migraine without aura compared with the control group, while the serum IL-4 level was higher in the former. In migraine with aura, peripheral monocytes spontaneously release detectable in vitro large amounts of NO, and these patients have significantly higher serum NO levels than controls. It is assumed that NO may be involved not only in the modulation of the Th2/Th3 balance, but also in the activation of type 2 cyclooxygenase, which is responsible for the synthesis of prostaglandins. In turn, most pro-inflammatory cytokines (IFN-γ, IL-1β and TNF-α) are powerful inducers of NO release by monocytes. It has recently been found [45] that an increase in NO production by monocytes in patients with migraine without aura may be the result of activation of INOS expression secondary to a transient increase in NFkB activity.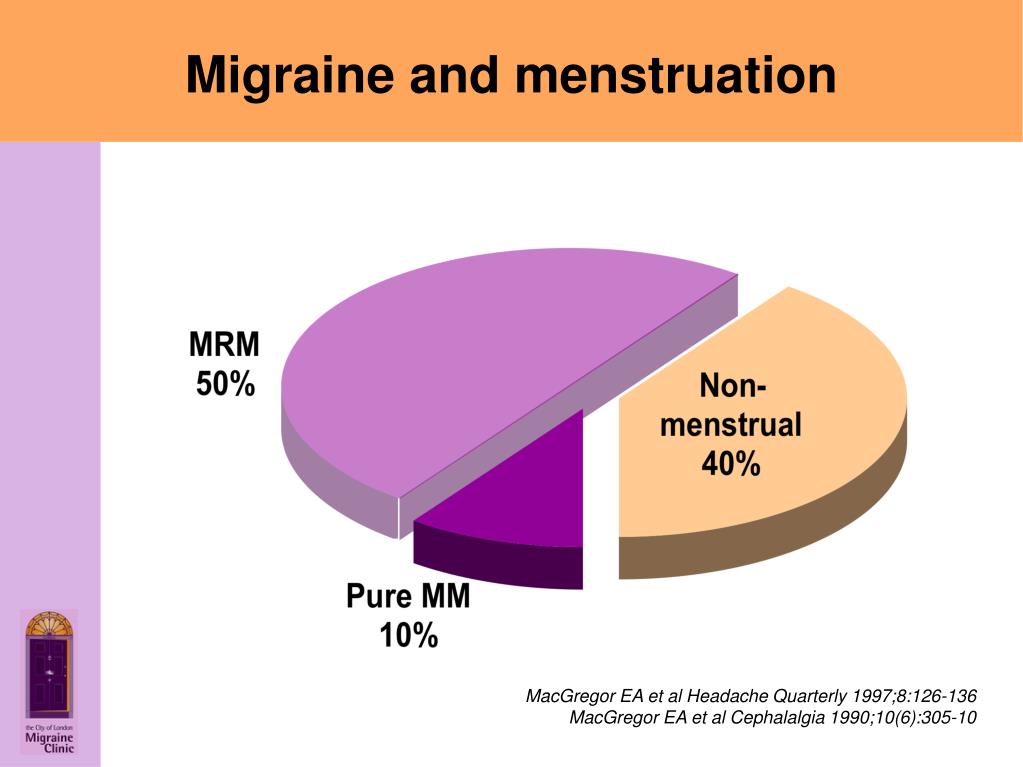 This observation is extremely important: in fact, NF-KB activation is associated with the induction of genes encoding pro-inflammatory cytokines (IL-1β, IL-6 and TNF-α) and cyclooxygenase expression.
This observation is extremely important: in fact, NF-KB activation is associated with the induction of genes encoding pro-inflammatory cytokines (IL-1β, IL-6 and TNF-α) and cyclooxygenase expression.
Violations of the humoral link of immunity in HD
There are few scientific works in the literature devoted to the study of changes in humoral immunity in G.B. Back in 1977, G. Lord et al. [46] noted a significant decrease in the content of C3 and C4 complement fractions in blood plasma during a migraine attack. T. Shimomura et al. [47] noted a significant increase in the total concentration of immunoglobulins of class A, M, G and CEC in blood plasma in patients suffering from migraine and HDN, compared with the control. According to other researchers [38], during the period of cluster HA, there is a significant decrease in the level of IgA, C3 fraction of complement, while the level of IgG, M and C4 fraction of complement did not differ from the control.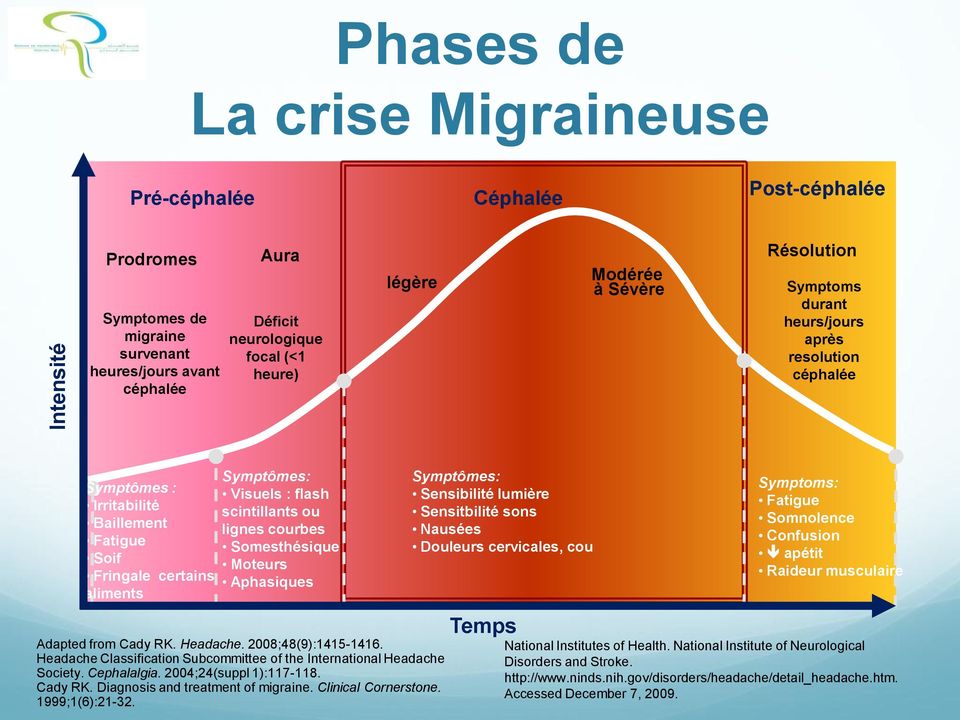
In 2014, J. Hanly et al. [48] published the results of a large international study involving 1732 patients diagnosed with systemic lupus erythematosus (SLE). The work was devoted to studying the characteristics of GB and the frequency of its occurrence in such patients. Despite the rather high incidence of GB detection (in 17.8% of patients, including migraine [60.7%], TTH [38.6%], nonspecific GB [7.1%], cluster GB [2.6%] and intracranial hypertension [1.0%]), the researchers did not reveal any relationship between the development of one or another type of HD, SLE activity, therapy, and the titer of SLE-specific antibodies (ANF, antibodies to nDNA, Sm-antigen, Ro / SS- A, antigen La/SS-B, to RNP, AKL).
The aim of the study L. Stojanovich et al. [49] studied non-thrombotic neurological manifestations in antiphospholipid syndrome depending on the type and level of antiphospholipid antibodies detected. It was found that chorea, migraine and epilepsy were more often diagnosed in secondary antiphospholipid syndrome (SAPS), other types of hypertension and depression were diagnosed in primary (PAPS). Note that when migraine was detected, a statistically significant increase in the level of antibodies to cardiolipin (aCL IgM) and lupus anticoagulant (LA) was noted. These data are also consistent with the strong correlation between migraine and SLE found in a number of studies [50–53]. A. Eggers [54] found a relationship between the presence of migraine in patients with SLE and the severity and rate of development of the disease. The authors explain this by the fact that migraine is often accompanied by systemic platelet activation and a brief but intense oxidative burst of platelets, which leads to an increase in the extracellular level of hydrogen peroxide (H 2 O 2 ) enough to turn off T cell regulatory function via the CD28 cascade. Passive diffusion H 2 O 2 mimics the effect of H 2 O 2 formation caused by CD28 ligation. This eliminates the immunosuppressive effect of immunoregulatory T cells on self-reactive ones, and the development or exacerbation of an autoimmune disease occurs spontaneously.
Note that when migraine was detected, a statistically significant increase in the level of antibodies to cardiolipin (aCL IgM) and lupus anticoagulant (LA) was noted. These data are also consistent with the strong correlation between migraine and SLE found in a number of studies [50–53]. A. Eggers [54] found a relationship between the presence of migraine in patients with SLE and the severity and rate of development of the disease. The authors explain this by the fact that migraine is often accompanied by systemic platelet activation and a brief but intense oxidative burst of platelets, which leads to an increase in the extracellular level of hydrogen peroxide (H 2 O 2 ) enough to turn off T cell regulatory function via the CD28 cascade. Passive diffusion H 2 O 2 mimics the effect of H 2 O 2 formation caused by CD28 ligation. This eliminates the immunosuppressive effect of immunoregulatory T cells on self-reactive ones, and the development or exacerbation of an autoimmune disease occurs spontaneously.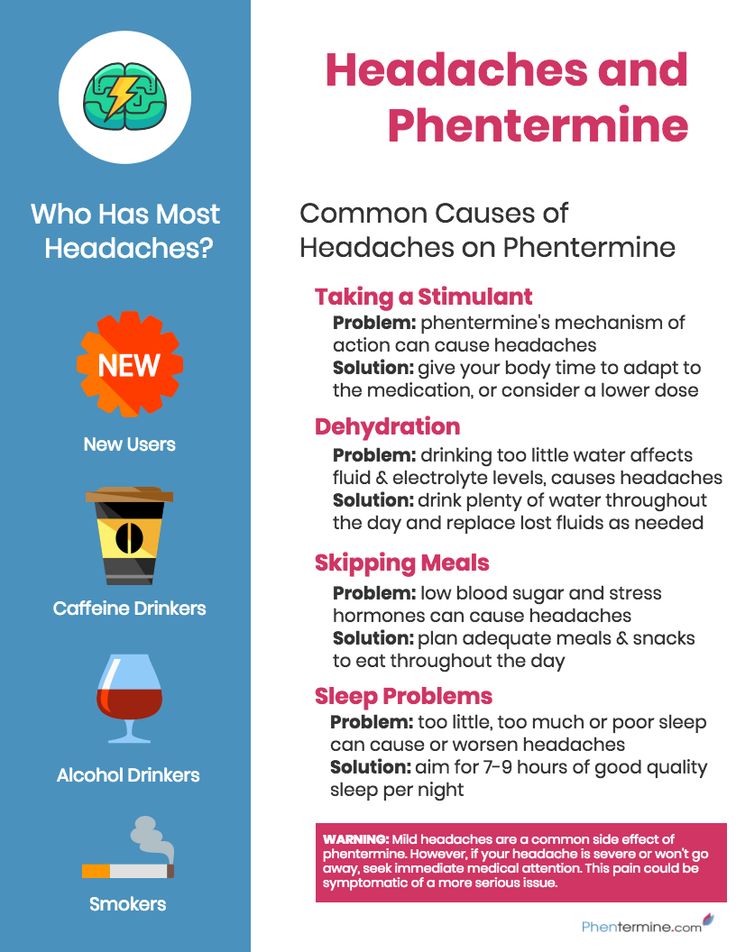
However, in a number of studies [55], the relationship between migraine and the presence of antiphospholipid antibodies in the blood has been refuted. So, R. Rajan et al. [56], who studied prothrombotic conditions in migraine, did not find a statistically significant increase in the level of lupus anticoagulant, antibodies to cardiolipin and β2-glycoprotein-1 compared with the control group.
A similar diagnostic examination has been performed in patients with lenticular headache, the etiopathogenesis of which remains unclear. W. Chen et al. [57] suggested that it is autoimmune disorders that underlie this disease. The results of the study confirm their theory: in 16 (69.6%) of 23 patients, abnormalities were detected at the autoimmune level: in 8 patients, antibodies to the antinuclear factor were found, in 6 - to SSA / La, in 2 - to SSB / Ro, 4 — rheumatoid factor, 1 — antibodies to ds-DNA. An abnormal increase in the blood titer of antibodies to β-glycoprotein-1 was observed in 4 patients, lupus anticoagulant - in 1.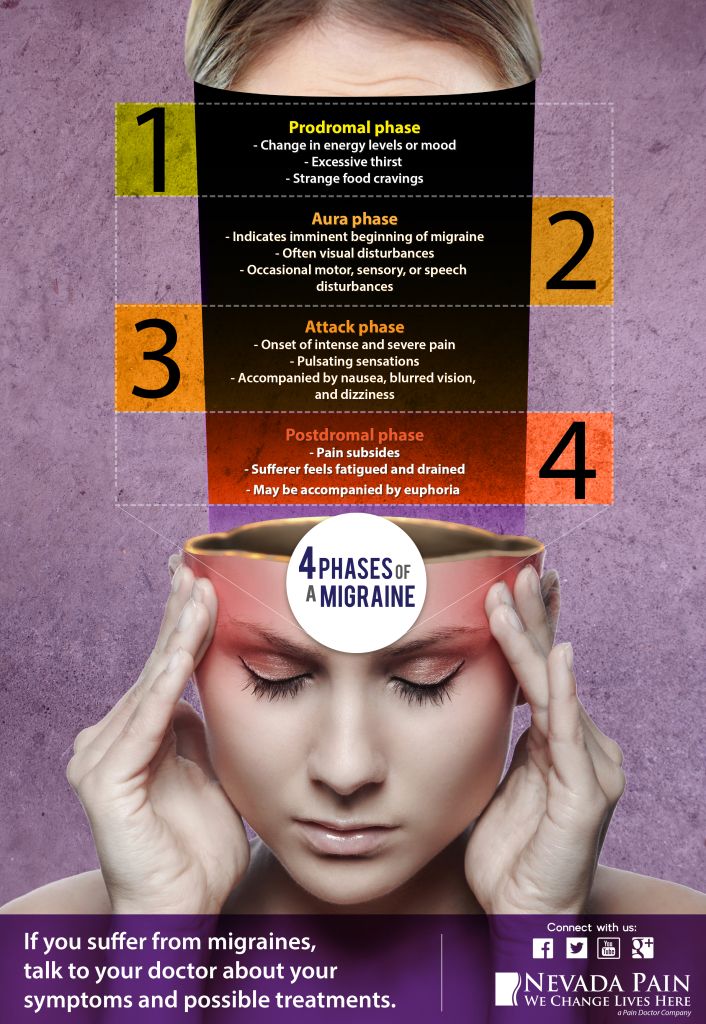 Based on these data, 15 (65%) patients were diagnosed with Sjogren's syndrome, rheumatoid arthritis or antiphospholipid syndrome" (AFS).
Based on these data, 15 (65%) patients were diagnosed with Sjogren's syndrome, rheumatoid arthritis or antiphospholipid syndrome" (AFS).
A group of scientists from Lebanon, England, and the United Arab Emirates analyzed the reports on the study of GB in APS, published from 1969 to 2015. patients with APS. In July 2016, it was proposed to introduce migraine into the new International criteria for the diagnosis of APS [58].
On MRI, migraine may appear as multiple foci of ischemic origin. And in 2011 R. Türkoğlu et al. [59] conducted a study aimed at studying the immunological factors associated with these lesions. To study the relationship between lesions detected by MRI and the level of antinuclear antibodies (Hu (ANNA 1), Yo-1 (PCA1), CV2, Ma2, Ri (ANNA2), amphiphysin), patients with migraine and white matter lesions (WML) were examined. ) brain; with migraine without PMB; multiple sclerosis patients with PMB but no history of HD, and 20 healthy controls. A higher frequency of detection of antinuclear antibodies was in patients with migraine and PMS compared with patients without PMS (12/17 and 2/19respectively, p = 0. 0004). At the same time, antinuclear antibodies were not detected in patients with multiple sclerosis. Based on the results obtained, scientists suggest the involvement of inflammation in the pathogenesis of migraine.
0004). At the same time, antinuclear antibodies were not detected in patients with multiple sclerosis. Based on the results obtained, scientists suggest the involvement of inflammation in the pathogenesis of migraine.
The results of the analyzed studies on the study of the humoral link of immunity, and the comorbidity of HD and infectious processes described above, testify in favor of the presence of autoimmune disorders in the pathophysiology of HD.
These data confirm the importance of immunological disorders in the pathogenesis of various types of GB. The development of ways to control the elements of the immune system seems to be a promising direction in the search for new methods of treatment.
M. Youssof et al. [60] examined 50 patients diagnosed with migraine and 45 healthy ones. The migraine group included 21 men and 29 women, whose mean age was 25.82±9.7 years (8-45 years). Serum levels of pro- (TNF-α and IL-6) and anti-inflammatory (IL-2 and IL-10) cytokines were studied to assess the role of cytokines in the pathophysiology of migraine, as well as to determine the relationship between them and the clinical response after prophylactic therapy with one of four drugs or their combination. As a result, patients with migraine had significantly higher concentrations of TNF-α and IL-6 compared to controls (for TNF-α: 1.78 ± 0.92 during an attack and 1.06±0.50 pg/ml in the period between attacks versus 0.64±0.60 pg/ml, p = 0.003 and p = 0.008, respectively; for IL-6: 2.23 ± 0.60 during an attack and 1.17 ± 0.49 pg / ml in the interictal period vs. 0.57 ± 0.51 pg / ml, p = 0.000 and p =0.004 respectively). The mean levels of IL-10 were significantly lower in migraine (3.20±1.14 pg/ml during an attack and 3.41±1.08 pg/ml in the period between attacks) than in controls (5.92±1. 19 pg/ml) ( p = 0.008 and p \u003d 0.005). Based on the data obtained, the scientists put forward the idea that one of the potential mechanisms of action of drug prevention of migraine may be their effect on various cytokines. After 4 months of treatment with drugs used alone or in combination, there was a decrease in the levels of TNF-α and IL-6 without a significant effect on the levels of IL-2 or IL-10.
As a result, patients with migraine had significantly higher concentrations of TNF-α and IL-6 compared to controls (for TNF-α: 1.78 ± 0.92 during an attack and 1.06±0.50 pg/ml in the period between attacks versus 0.64±0.60 pg/ml, p = 0.003 and p = 0.008, respectively; for IL-6: 2.23 ± 0.60 during an attack and 1.17 ± 0.49 pg / ml in the interictal period vs. 0.57 ± 0.51 pg / ml, p = 0.000 and p =0.004 respectively). The mean levels of IL-10 were significantly lower in migraine (3.20±1.14 pg/ml during an attack and 3.41±1.08 pg/ml in the period between attacks) than in controls (5.92±1. 19 pg/ml) ( p = 0.008 and p \u003d 0.005). Based on the data obtained, the scientists put forward the idea that one of the potential mechanisms of action of drug prevention of migraine may be their effect on various cytokines. After 4 months of treatment with drugs used alone or in combination, there was a decrease in the levels of TNF-α and IL-6 without a significant effect on the levels of IL-2 or IL-10.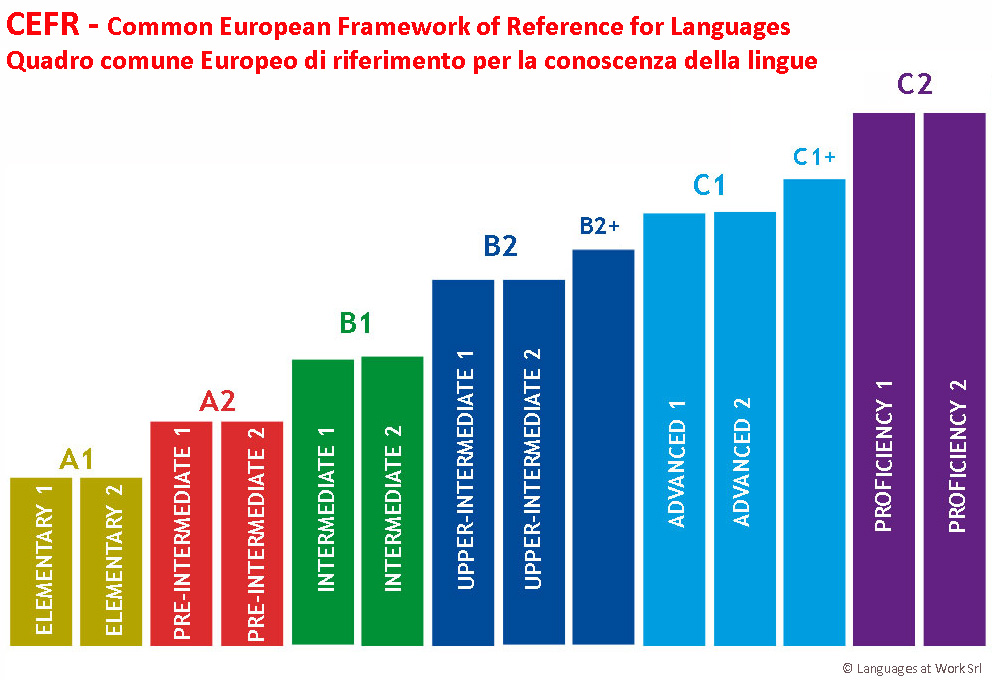 The prophylactic effect on the cytokine profile of the most widely used drugs in the treatment of migraine in children: cyproheptadine (an antihistamine and antiserotonergic drug), amitriptyline (a tricyclic antidepressant), propranolol (a beta-adrenergic receptor blocker) and topiramate (an antiepileptic drug) was studied. As a result, when using all the drugs used alone or in combination, there was a significant decrease in the levels of TNF-α and IL-6.
The prophylactic effect on the cytokine profile of the most widely used drugs in the treatment of migraine in children: cyproheptadine (an antihistamine and antiserotonergic drug), amitriptyline (a tricyclic antidepressant), propranolol (a beta-adrenergic receptor blocker) and topiramate (an antiepileptic drug) was studied. As a result, when using all the drugs used alone or in combination, there was a significant decrease in the levels of TNF-α and IL-6.
R. Vallejo et al. [61] evaluated the efficacy of cyproheptadine, amitriptyline, propranolol, and flunarizine in preventing migraine in 77 children by measuring levels of cytokines, including TNF-α, IL-1β, and IL-6, and leptin before and 4 months after treatment. Each drug reduced not only the frequency and duration of seizures, but also the severity of GB according to the PedMIDAS scale. During the experiment, there were no significant differences in the decrease in the level of cytokines among the drugs used ( p > 0.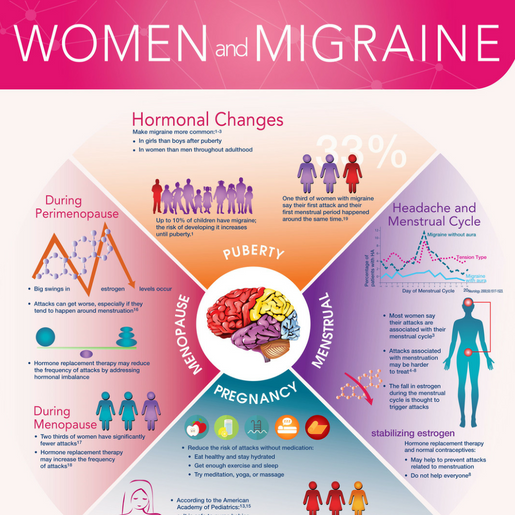 05). However, leptin levels have increased with cyproheptadine ( p <0.05), which was not reported with amitriptyline and propranolol. It was concluded that the measurement of levels of cytokines correlated with clinical manifestations could be a way to objectively assess the effectiveness of treatment for migraine. Serum IL-6 levels were measured in 66 patients with migraine. Of these patients, 23 (34.9%) received topiramate prophylactically. Mean IL-6 levels in patients with migraine taking topiramate were higher than in patients who did not take it: 67.06±92.09 and 44.09±59.19 pg/ml, respectively ( p >0.05). The level of IL-6 in the control group of healthy people was 8.60±7.36 pg/ml, which was significantly lower than in the group of patients with migraine ( p = 0.001). This proves the involvement of IL-6 in the induction of pain and inflammatory mechanisms of migraine attacks, and, according to the authors of the study, it can also serve as a marker of the effectiveness of treating HD.
05). However, leptin levels have increased with cyproheptadine ( p <0.05), which was not reported with amitriptyline and propranolol. It was concluded that the measurement of levels of cytokines correlated with clinical manifestations could be a way to objectively assess the effectiveness of treatment for migraine. Serum IL-6 levels were measured in 66 patients with migraine. Of these patients, 23 (34.9%) received topiramate prophylactically. Mean IL-6 levels in patients with migraine taking topiramate were higher than in patients who did not take it: 67.06±92.09 and 44.09±59.19 pg/ml, respectively ( p >0.05). The level of IL-6 in the control group of healthy people was 8.60±7.36 pg/ml, which was significantly lower than in the group of patients with migraine ( p = 0.001). This proves the involvement of IL-6 in the induction of pain and inflammatory mechanisms of migraine attacks, and, according to the authors of the study, it can also serve as a marker of the effectiveness of treating HD.
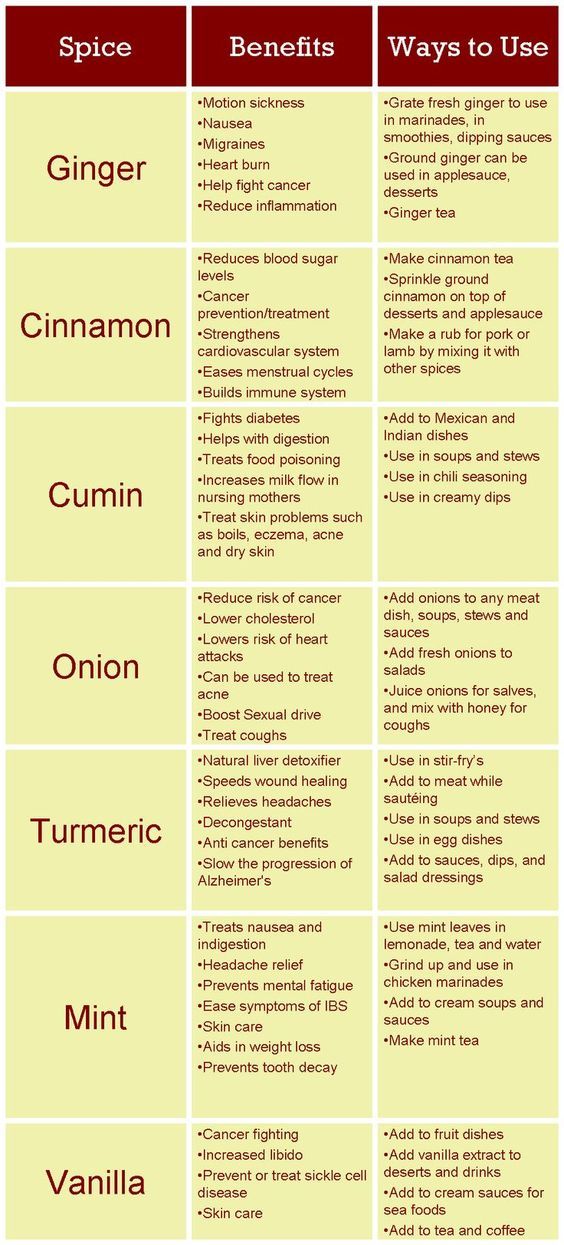
The search for new directions in the treatment of HD is not limited to the study of cytokine profile indicators. Gradually, the practice of a neurologist includes the identification of migraine triggers using immunological tests for IgG and IgE to food allergens [62]. Thus, J. Pascual and A. Oterino [63] diagnosed food intolerance in 56 patients suffering from migraine that did not respond to traditional drug therapy. In all patients, specific IgG immunoglobulins to food allergens were identified, in the control group - only in 15 (26%) people. The highest allergic reaction was observed to such products as eggs, cheese, cow's milk, yeast, wheat, tomatoes, pork and beans, in the control group - cow's milk, cheese and eggs. Then the patients followed an individual diet for 6 months, excluding products in accordance with the results of the analyzes. At the end of the diet, 43 patients did not have a single migraine attack, 4 had a decrease in the intensity and frequency of attacks, 9- there were no significant changes in the clinical picture of the disease.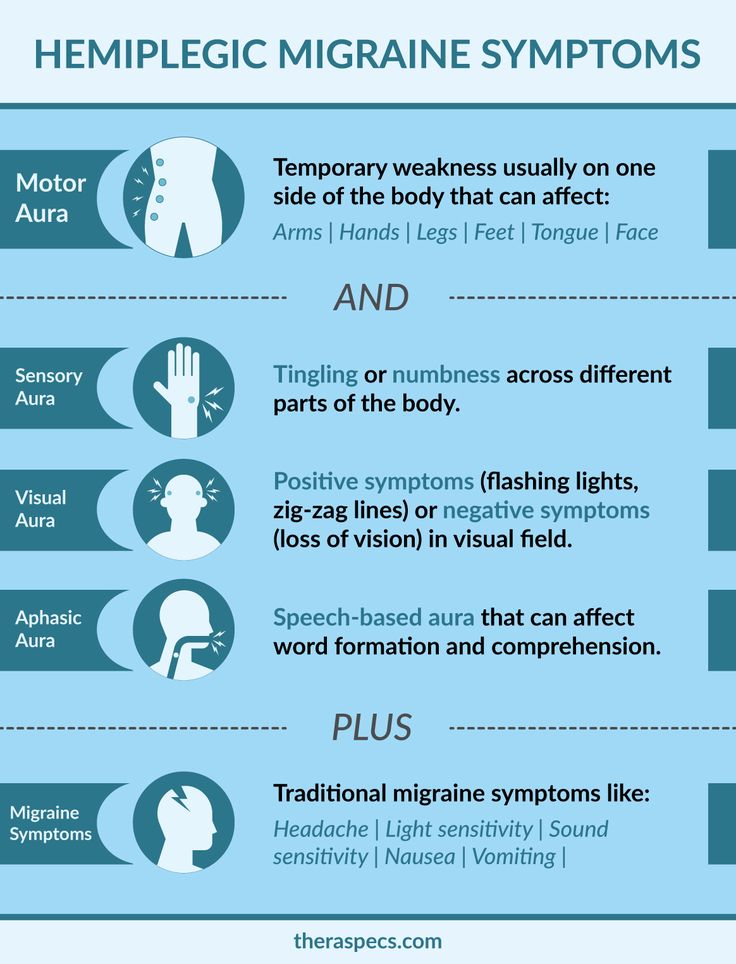 The assertion that dietary adherence is critical in the prevention of HD is supported by the fact that migraine attacks returned a few days after the patient began to eat food.
The assertion that dietary adherence is critical in the prevention of HD is supported by the fact that migraine attacks returned a few days after the patient began to eat food.
Causes of migraine - Health Clinic 365 Yekaterinburg
Although the causes of migraine are not fully understood, genetics and environmental factors seem to play a role.
Migraine attacks can be caused by changes in the structures of the brain and their interactions with the trigeminal nerve, the main pathway of pain impulses.
In addition, their development may be affected by existing imbalances of brain chemicals, including serotonin, which plays an important role in pain regulation. Researchers are still studying the role of serotonin in migraine, however, it is already known that serotonin levels decrease during migraine attacks. This can lead to the release of neuropeptides, including calcitonin gene-related peptide (CGRP). It is known that the peptide encoded by the calcitonin gene (CGRP) plays a key role in the mechanism of development of migraine headache.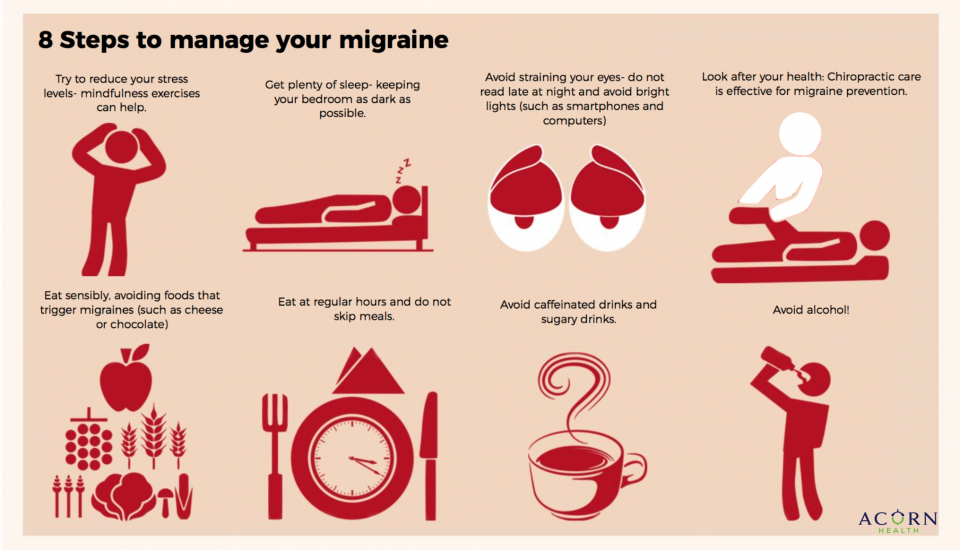 During a migraine attack, this neuropeptide is released from the neurons of the trigeminal nerve and binding to its receptor causes vasodilation of the brain and neurogenic inflammation of the vascular wall. This inflammation activates the pain mechanisms of the trigeminal nerve fibers located in the vascular wall, which act on the lining of the brain, causing pain. The more the calcitonin-related peptide gene (CGRP) is released, the stronger and more painful the headache.
During a migraine attack, this neuropeptide is released from the neurons of the trigeminal nerve and binding to its receptor causes vasodilation of the brain and neurogenic inflammation of the vascular wall. This inflammation activates the pain mechanisms of the trigeminal nerve fibers located in the vascular wall, which act on the lining of the brain, causing pain. The more the calcitonin-related peptide gene (CGRP) is released, the stronger and more painful the headache.
Migraine triggers
A number of factors can trigger migraines, including:
- Hormonal changes in women. Fluctuating levels of estrogen seem to cause headaches in many women. Migraine sufferers often report headaches just before or during their period, when they experience a significant drop in estrogen. Other women note that pregnancy or menopause contributed to the development of migraine. Hormonal medications, such as oral contraceptives and hormone replacement therapy, can also increase the frequency and severity of migraine attacks.
 Some women, however, find that their migraine flares less frequently when they take these drugs.
Some women, however, find that their migraine flares less frequently when they take these drugs. - Products. Certain types of cheese, salty foods, and some others can cause migraines. Irregular eating or fasting can also trigger attacks.
- Food additives. The sweetener aspartame and the preservative monosodium glutamate (MSG), found in many foods, can trigger migraines.
- Drinks. Alcohol, especially wine and drinks high in caffeine, can trigger migraines.
- Stress. Stress at work or at home can trigger migraines.
- Sensory stimuli. Bright lights, sun glare, and loud noises can trigger migraines. Strong odors - including perfume, paint thinner, secondhand smoke, and others - can trigger migraines in some people.
- Sleep. Lack of sleep or too much sleep can trigger a migraine attack in some people.
- Physical factors. Intense physical exertion, including sexual activity, can trigger a migraine.
- Changes in the environment.
 Changes in the weather or barometric pressure can trigger a migraine.
Changes in the weather or barometric pressure can trigger a migraine. - Medicinal preparations. Oral contraceptives and vasodilators such as nitroglycerin can make migraines worse.
Risk factors
Several factors make you more prone to migraine, including:
- Heredity.
- Age. Migraine can begin at any age, most often migraine debuts in adolescence. Migraine attacks tend to become more frequent and worse in people around the age of 30 and then gradually become less intense and less frequent over the following decades.
- Pos. Women are three times more likely to suffer from migraines. Headaches tend to bother boys more than girls during childhood, but this changes by the time of puberty.
- Hormonal changes. If you are a woman who has a migraine, you may find that the headache starts just before and shortly after the onset of your period. The frequency and intensity of seizures can also change during pregnancy or menopause.
 Migraines usually improve after menopause.
Migraines usually improve after menopause.
Where the service is provided
Clinic on st. Kuznechnaya, 83 Clinic on the street. Union, 2 Clinic on the street. Stepan Razin, 122
Our specialists
Clinic on the street. Bazhova, 137
Bandurina Tatyana Viktorovna
Deputy chief physician for clinical and expert work, neurologist, highest category
Clinic on the street. Bazhova, 137
Semenikhina Olga Alekseevna
Neurologist, highest category
Clinic on the street. Soyuznaya, 2
Sazonova Yuliya Alexandrovna
Neurologist, chiropractor
Clinic on the street. Stepana Razina, 122
Antropov Andrey Gennadievich
Neurologist, the highest category, Ph.D.
Center for periodic and preliminary medical examinations
Where the service is provided
Clinic on st. Kuznechnaya, 83 Clinic on the street. Union, 2 Clinic on the street.