Leucotomy vs lobotomy
What is a Lobotomy? Risks, History and Why It’s Rare Now
Few medical procedures in history have garnered as much controversy as the lobotomy. Tens of thousands of lobotomies were performed in the United States in the mid-1900s, often leading to devastating outcomes.
A lobotomy, also called a leucotomy, is a type of psychosurgery that was used to treat mental health conditions such as mood disorders and schizophrenia. Psychosurgeries are procedures that involve the physical removal or alteration of part of the brain.
Lobotomies involved separating tissue in an area called the prefrontal cortex in one of two primary ways:
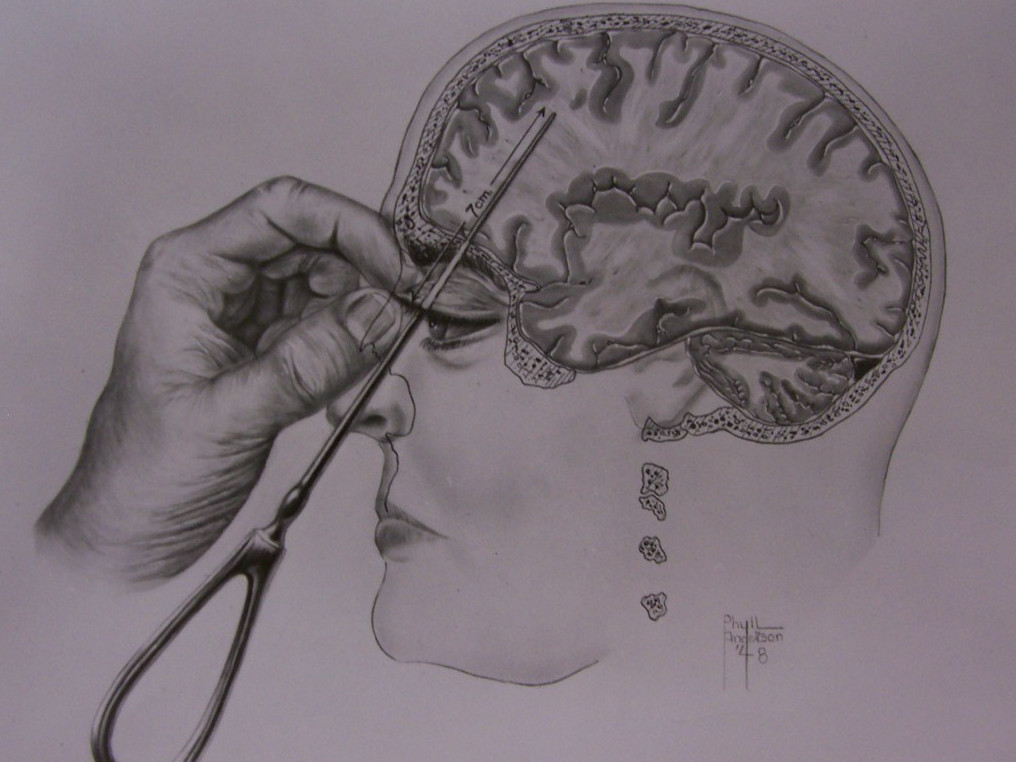
- Frontal lobotomy. A surgeon drilled a hole into each side of the skull and cut through brain tissue with an instrument resembling an ice pick called a leucotome.
- Transorbital lobotomy. A surgeon inserted a leucotome through the eye socket and drove it through a thin layer of bone with a mallet to access the brain.
These procedures are no longer performed in the United States, but some other types of psychosurgery are still performed when other treatments have failed. Read on to learn more about why lobotomies were traditionally performed and why psychosurgery is used today.
Lobotomies are no longer performed in the United States. They began to fall out of favor in the 1950s and 1960s with the development of antipsychotic medications. The last recorded lobotomy in the United States was performed by Dr. Walter Freeman in 1967 and ended in the death of the person on whom it was performed.
In Europe, the Soviet Union banned lobotomies in 1950, a year after inventor Dr. Egas Moniz won the Nobel Prize for medicine. They persisted into the 1970s in the rest of Europe and into the 1980s in Scandinavia.
Some other types of psychosurgeries are still used today, such as:
- cingulotomy
- anterior capsulotomy
- subcaudate tractotomy
- limbic leucotomy
- corpus callosotomy
With advancements in medications, psychosurgeries are rarely performed. Surgery is usually only used when all other treatment options have failed. Surgical techniques still in use today include:
Surgery is usually only used when all other treatment options have failed. Surgical techniques still in use today include:
Cingulotomy
Cingulotomy is the most commonly performed psychosurgery in North America. It’s a type of surgery that involves altering tissue in the anterior cingulate region associated with feeling chronic pain. It’s sometimes used to manage symptoms of:
- chronic and severe anxiety disorders, such as obsessive-compulsive disorder (OCD)
- severe mood disorders, such as treatment-resistance depression or bipolar disorder
- heroin addiction
- chronic pain syndromes that don’t respond to other treatments
- severe schizophrenia with aggressive behavior
Anterior capsulotomy
An anterior capsulotomy is a potential treatment for severe OCD that doesn’t respond to psychotherapy and medications. It involves altering the part of the brain that carries information from the thalamus and brainstem to the prefrontal region.
In a 2019 review, researchers found that of 512 people who received treatment from 1961 to 2018, 73 percent responded to the surgery and 24 percent saw their symptoms resolve.
Subcaudate tractotomy
A subcaudate tractotomy may be used to treat delusions and hallucinations in people with severe schizophrenia with aggressive symptoms. It involves cutting connections between the limbic system and a part of the prefrontal lobe called the orbitofrontal cortex.
Limbic leucotomy
Limbic leucotomy is a combination of the subcaudate tractotomy and cingulotomy. It’s been performed since the 1970s to treat mood disorders and OCD.
Corpus callosotomy
Corpus callosotomy involves severing the corpus callosum, a bundle of nerves that connect your left and right brain hemispheres. In a 2017 study, researchers found that corpus callosotomy is a potentially effective treatment for generalized epilepsy in people with drug-resistant epilepsy.
Lobotomies were considered experimental even at the height of their popularity. Although some people did see improvements in their conditions, many other people experienced life-alternating side effects, or even died.
Although some people did see improvements in their conditions, many other people experienced life-alternating side effects, or even died.
One of the highest-profile cases of a failed lobotomy was that of Rosemary Kennedy, younger sister of John F. Kennedy. After undergoing a lobotomy in 1941 to treat seizures and extreme shifts in mood, she lost her ability to walk or talk. Her personality was permanently altered, and she was left with physical disability.
Risks of psychosurgeries include the risk of death and:
- seizures
- loss of bladder control or bowel control
- changes in appetite
- weakness
- changes in language ability
- brain infection
- cognitive impairment
- changes in personality and emotion
António Egas Moniz and his colleague Almeida Lima are credited with the development of the lobotomy in 1935. They promoted their frontal lobotomy procedure across Europe, despite keeping poor patient records and lacking evidence of effectiveness. The procedure quickly gained popularity, despite thousands of people experiencing severe side effects and outcomes, such as seizures, infections, and death.
The procedure quickly gained popularity, despite thousands of people experiencing severe side effects and outcomes, such as seizures, infections, and death.
American neurologist Walter Freeman and surgeon James Watts championed the procedure in America. Influenced by an Italian colleague, Freeman eventually switched to the transorbital method, in which an icepick-like instrument was inserted through the eye socket to reach the brain. He passionately spread the surgery across North America, despite haphazardly performing surgeries without proper sterilization.
Tens of thousands of lobotomies were performed in the United States between the 1930s and 1960s, often without informed consent. Eventually, lack of evidence supporting the procedure finally caught up with it, and it was largely abandoned once the medication chlorpromazine was developed.
Despite a risk of severe side effects and outcomes, lobotomies were once used to treat many mental health conditions, including schizophrenia, depression, and bipolar disorder. Nowadays, treatment for mental health conditions largely consists of medication and psychotherapy.
Nowadays, treatment for mental health conditions largely consists of medication and psychotherapy.
Antipsychotics and other medications
Antipsychotics are often the initial treatment for acute schizophrenic episodes. They block the effects of the neurotransmitter dopamine on your brain to reduce feelings of anxiety or aggression as well as hallucinations and delusional thoughts.
Many other types of medications are also used to treat mental health conditions, including:
- antidepressants
- anti-anxiety medications
- stimulants
- mood stabilizers
Psychotherapy
Psychotherapy, also called talk therapy, is a common type of mental health treatment. It may be administered alone or in combination with medication. There are many types of psychotherapy used to treat mental health conditions. They include:
- cognitive behavioral therapy
- dialectical behavioral therapy
- interpersonal therapy
- psychodynamic therapy
- psychoanalysis
Hospitalization
Some people with severe mental health conditions may need to be admitted to a medical facility. Laws vary by state, but in most states, a person can be held in facility involuntarily if they pose a danger to themselves or others.
Laws vary by state, but in most states, a person can be held in facility involuntarily if they pose a danger to themselves or others.
Lobotomies were surgeries that involved altering a part of the brain called the prefrontal cortex. Sometimes these surgeries were performed without consent and without proper sterilization, despite a lack of evidence for their effectiveness.
Lobotomies are no longer performed and have largely been replaced by medications. Some other types of psychosurgeries are performed in very rare circumstances to treat conditions such as severe depression or OCD that doesn’t respond to other treatments. These surgeries are considered last resorts.
Lobotomy: Definition, procedure and history
When you purchase through links on our site, we may earn an affiliate commission. Here’s how it works.
(Image credit: mikroman6 via Getty Images)Lobotomy, also known as leucotomy, is a neurosurgical operation that involves permanently damaging parts of the brain's prefrontal lobe, according to the American Association for the Advancement of Science (AAAS). Introduced in the mid-20th century, lobotomies have always been controversial, but were widely performed for more than two decades as treatment for schizophrenia, manic depression and bipolar disorder, among other mental illnesses.
Introduced in the mid-20th century, lobotomies have always been controversial, but were widely performed for more than two decades as treatment for schizophrenia, manic depression and bipolar disorder, among other mental illnesses.
Lobotomy was an umbrella term for a series of different operations that purposely damaged brain tissue in order to treat mental illness, said Dr. Barron Lerner, a medical historian and professor at NYU Langone Medical Center in New York.
"The behaviors [doctors] were trying to fix, they thought, were set down in neurological connections," Lerner told Live Science. "The idea was, if you could damage those connections, you could stop the bad behaviors."
When lobotomy was invented, there were no good ways to treat mental illness, and people were "pretty desperate" for any kind of intervention, Lerner said. Even so, there were always critics of the procedure, he added.
When was the first lobotomy?
Even before the first lobotomy, doctors were manipulating the brain to change behavior. Beginning in the late 1880s, the Swiss physician Gottlieb Burkhardt removed parts of the cortex of the brains of patients with manic agitation, auditory hallucinations and symptoms of schizophrenia. Burkhardt noted in an 1891 paper that the surgery calmed his patients, though some suffered complications such as motor weakness, sensory aphasia (inability to understand speech, writing or tactile symbols) and epilepsy, and one patient died five days after the procedure, researchers reported in 2008 in the Journal of Neurosurgery.
Beginning in the late 1880s, the Swiss physician Gottlieb Burkhardt removed parts of the cortex of the brains of patients with manic agitation, auditory hallucinations and symptoms of schizophrenia. Burkhardt noted in an 1891 paper that the surgery calmed his patients, though some suffered complications such as motor weakness, sensory aphasia (inability to understand speech, writing or tactile symbols) and epilepsy, and one patient died five days after the procedure, researchers reported in 2008 in the Journal of Neurosurgery.
Portuguese neurologist António Egas Moniz is credited with officially inventing the lobotomy in 1935, for which he shared the Nobel Prize for Physiology or Medicine in 1949 (later, a movement was started to revoke the prize, unsuccessfully).
Moniz's breakthrough was inspired by lobotomy-like procedures that Yale neuroscientist John Fulton and his colleague Carlyle Jacobsen performed on chimpanzees. They removed both frontal lobes in a female chimpanzee who had previously displayed anger and frustration if she made a mistake while performing tasks in experiments; after the surgery, the chimp became more cooperative and did not show signs of frustration, scientists wrote in 2014 in the Singapore Medical Journal.
Later that year, Moniz and his colleague Almeida Lima performed the first human lobotomy experiments, operating on 20 people. The doctors targeted the patients' frontal lobes because that brain region is associated with behavior and personality.
Moniz reported the surgeries as a success in treating patients with conditions such as depression, schizophrenia, panic disorder and mania, according to an article published in 2011 in the Journal of Neurosurgery . But the operations had severe side effects, including increased body temperature, vomiting, bladder and bowel incontinence and eye problems, as well as apathy, lethargy and abnormal sensations of hunger, among others. The medical community was initially critical of the procedure, but nevertheless, physicians started using it in countries around the world.
A surgeon using a brace and bit to drill into a patient's skull before performing a lobotomy, at a mental hospital in England, November 1946. (Image credit: Kurt Hutton/Picture Post/Hulton Archive/Getty Images)
How is a lobotomy performed?
Moniz's first lobotomy procedures involved cutting a hole in the skull and injecting ethanol into the brain to destroy the fibers that connected the frontal lobe to other parts of the brain. Later, Moniz developed a surgical instrument called a leucotome, which contains a retractable loop of wire that, when rotated, cuts a circular lesion in brain tissue.
Later, Moniz developed a surgical instrument called a leucotome, which contains a retractable loop of wire that, when rotated, cuts a circular lesion in brain tissue.
Italian and American doctors were early adopters of the lobotomy. American neurosurgeons Walter Freeman and James Watts were the first to perform the procedure in the United States in 1937, making "nine cores in the white matter of each frontal lobe" of a 59-year-old patient, according to a 2015 report in the journal The Lancet. They adapted Moniz's technique to create the "Freeman-Watts technique" or the "Freeman-Watts standard prefrontal lobotomy," in which a surgeon drilled holes in the patient's skull, then inserted and rotated a knife to destroy brain cells, targeting connections between part of the prefrontal lobes and a region in the thalamus, which is a grey-matter structure toward the center of the brain, The New York Times wrote in 1994 in Dr. Watts' obituary.
"Freeman thought psychosis was the result of excessive self-reflection — thoughts that circled back on themselves over and over again," Miriam Posner, assistant professor in the information studies department at UCLA, said in 2019 in the National Library of Medicine's History of Medicine Lecture Series at the National Institutes of Health in Bethesda, Maryland.
"He was being literal when he said lobotomy was a way of cutting those endlessly circling thoughts off within the brain," Posner said.
This skull shows the characteristic marks of transorbital lobotomy, also called, in its time, icepick lobotomy. The small, symmetrical holes in the eye sockets are where a surgical tool perforated the skull. (Image credit: Mütter Museum of The College of Physicians of Philadelphia)
The Italian psychiatrist Amarro Fiamberti developed a procedure that involved accessing the frontal lobes through the eye sockets; that procedure would inspire Freeman to develop the transorbital lobotomy in 1945, a method that would not require a traditional surgeon or operating room, researchers reported in 2019 in the journal Frontiers in Neuroscience. The technique involved using an instrument called an orbitoclast — a long, slender instrument modeled after an ice pick — which the physician would insert through the patient's eye socket using a hammer.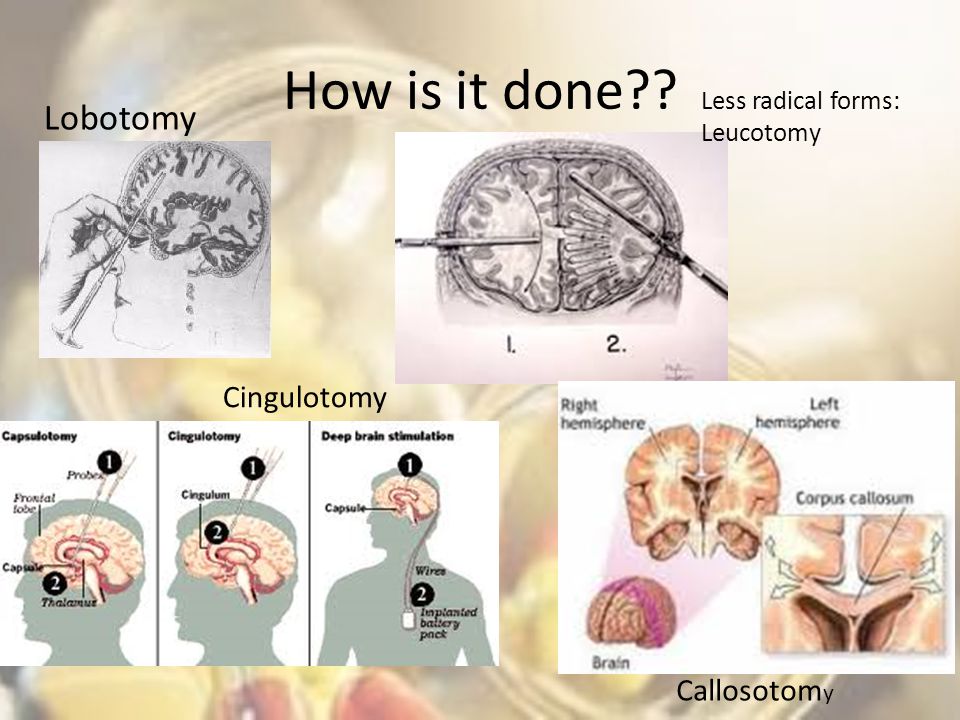 They would then move the instrument side-to-side to separate the frontal lobes from the thalamus, the part of the brain that receives and relays sensory input.
They would then move the instrument side-to-side to separate the frontal lobes from the thalamus, the part of the brain that receives and relays sensory input.
Transorbital lobotomies did not require anesthesia and were quicker to perform than standard lobotomies; consequently, surgeons across Europe and America performed tens of thousands of these procedures over the next two decades, according to the 2019 study. Freeman himself performed at least 3,000, and possibly as many as 5,000 lobotomies, according to the obituary in the Times.
"He traveled around the country, doing multiple lobotomies in a day," Lerner said. "He absolutely did this for way too long." Freeman performed his last lobotomy in 1967; it was his third such procedure on the patient, a woman named Helen Mortensen, NPR reported. She died of a brain hemorrhage soon after, and Freeman was banned from performing surgery, according to NPR.
Dr. Walter Freeman performs a lobotomy using an instrument like an ice pick which he invented for the procedure. Inserting the instrument under the upper eyelid of the patient, Dr. Freeman cuts nerve connections in the front part of the brain. (Image credit: Bettmann/Getty Images)
Inserting the instrument under the upper eyelid of the patient, Dr. Freeman cuts nerve connections in the front part of the brain. (Image credit: Bettmann/Getty Images)
What happens after a lobotomy?
While a small percentage of people supposedly showed improved mental conditions or no change at all, for many patients, lobotomy had negative effects on their personality, initiative, inhibitions, empathy and ability to function on their own, according to Lerner.
"The main long-term side effect was mental dullness," Lerner said. People could no longer live independently, and they lost their personalities, he added.
Mental institutions played a critical role in the prevalence of lobotomy. At the time, there were hundreds of thousands of mental institutions, which were overcrowded and chaotic. By giving unruly patients lobotomies, doctors could maintain control over the institution, Lerner said.
That's exactly what unfolds in the 1962 novel and 1975 film "One Flew Over the Cuckoo's Nest," in which Randle Patrick McMurphy, a violent but sane man who declares himself insane to avoid a prison sentence, is sent to mental hospital and given a lobotomy that leaves him mute, unresponsive and vacant-eyed.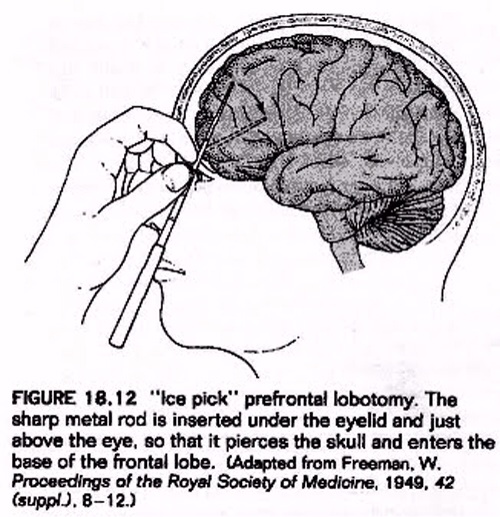
"Usually things in movies are exaggerated," Lerner said. But in this case, it was "disturbingly real," he said.
Photos show a female lobotomy patient before the procedure and one year later, in 1942. (Image credit: Historical Medical Library of The College of Physicians of Philadelphia)
Are lobotomies performed today?
Lobotomies declined in popularity in the 1950s, as their undesirable side effects became more well-known. Criticism of the procedures also grew among medical professionals who said the doctors who performed lobotomies were not neurosurgeons, neglected to report negative outcomes for many of their patients, and overall had "a lack of scientific rigor," according to the Frontiers in Neuroscience study.
"It also became apparent that some institutionalized or incapacitated patients were lobotomized without informed consent, and procedures may have been performed on prisoners to address dysfunctional behavior as opposed to mental illness," the study authors reported.
By the mid-1950s, scientists had developed psychotherapeutic medications such as the antipsychotic chlorpromazine, which was much more effective and safer for treating mental disorders than lobotomy. Nowadays, mental illness is primarily treated with drugs and psychotherapies. In cases where drugs or talk therapy are not effective, people may be treated with electroconvulsive therapy, a procedure that involves passing electrical currents through the brain to trigger a brief seizure, according to the Mayo Clinic.
Lobotomy is rarely, if ever, performed today, and if it is, "it's a much more elegant procedure," Lerner said. "You're not going in with an ice pick and monkeying around." The removal of specific brain areas (psychosurgery) is reserved for treating patients for whom all other treatments have failed.
Additional lobotomy resources
- Nobelprize.org: Controversial Psychosurgery Resulted in a Nobel Prize
- PsychCentral: The Surprising History of the Lobotomy
- NPR: "My Lobotomy": Howard Dully's Journey
This article was updated on Oct. 13, 2021 by Live Science senior writer Mindy Weisberger.
13, 2021 by Live Science senior writer Mindy Weisberger.
Tanya was a staff writer for Live Science from 2013 to 2015, covering a wide array of topics, ranging from neuroscience to robotics to strange/cute animals. She received a graduate certificate in science communication from the University of California, Santa Cruz, and a bachelor of science in biomedical engineering from Brown University. She has previously written for Science News, Wired, The Santa Cruz Sentinel, the radio show Big Picture Science and other places. Tanya has lived on a tropical island, witnessed volcanic eruptions and flown in zero gravity (without losing her lunch!). To find out what her latest project is, you can visit her website.
10 facts about the terrible operation
History remembers many barbaric practices in medicine, but lobotomy is perhaps the most frightening. Today, this operation can only be seen in the cinema, but in the middle of the last century, you could well be forced to undergo a lobotomy for your wayward character.
Alisa Gorbunova
1. Lobotomy, or leucotomy is an operation in which one of the lobes of the brain is separated from the rest of the areas, or completely excised. It was believed that this practice could treat schizophrenia.
2. The method was developed by the Portuguese neurosurgeon Egas Moniz in 1935, and a trial lobotomy took place in 1936 under his supervision. After the first hundred operations, Moniz observed the patients and made a subjective conclusion about the success of his development: the patients calmed down and became surprisingly submissive.
3. The results of the first 20 operations were as follows: 7 patients recovered, 7 patients showed improvement, and 6 people remained with the same illness. But the lobotomy continued to cause disapproval: many of Moniz's contemporaries wrote that the actual result of such an operation was the degradation of the personality.
4. The Nobel Committee considered the lobotomy a discovery that was ahead of its time. Egas Moniz received the Nobel Prize in Physiology and Medicine in 1949. Subsequently, the relatives of some patients requested that the award be canceled, since lobotomy causes irreparable harm to the patient's health and is generally a barbaric practice. But the request was rejected.
5. If Egas Moniz argued that leucotomy is a last resort, then Dr. Walter Freeman considered lobotomy a remedy for all problems, including willfulness and aggressive character. He believed that lobotomy eliminates the emotional component and thereby "improves the behavior" of patients. It was Freeman who introduced the term "lobotomy" in 1945 year. Throughout his life, he operated on about 3,000 people . By the way, this doctor was not a surgeon.
6. Freeman once used an ice pick from his kitchen for an operation. Such a “necessity” arose because the previous instrument, the leukote, could not withstand the load and broke in the skull of patient .
Such a “necessity” arose because the previous instrument, the leukote, could not withstand the load and broke in the skull of patient .
7. Subsequently, Freeman realized that ice pick is great for lobotomy. Therefore, the doctor designed a new medical instrument based on this model. The orbitoclast had a pointed end on one side and a handle on the other. A division was applied to the tip to control the depth of penetration.
8. By the middle of the last century lobotomy had become an incredibly popular procedure : it was practiced in Great Britain, in Japan, in the USA and in many European countries. In the United States alone, about 5,000 operations were performed per year.
9. In the USSR, the new method of treatment was used relatively rarely, but it was improved. The Soviet neurosurgeon Boris Grigoryevich Egorov proposed the use of osteoplastic trepanation instead of access through the orbit. Egorov explained that trepanation would allow more precise orientation in determining the area of surgical intervention.
Egorov explained that trepanation would allow more precise orientation in determining the area of surgical intervention.
10. Lobotomy was practiced in the USSR for 5 years, but was banned at the end of 1950. It is generally accepted that the decision was dictated by ideological considerations , because this method is most widely used in the United States. By the way, in America, lobotomy continued to be practiced until the 70s. However, there is also an opposite point of view: the ban on lobotomy in the USSR was due to the lack of scientific data and the questionable method in general.
consequences of brain lobotomy, history of brain lobotomy operation
Gleb Pospelovo lobotomy— the most famous and darkest of psychosurgical operations
– Oh, yes, after treatment, he will turn into a vegetable! Everyone knows that in psychiatric hospitals people are "zombified", "burned out the brain", "poisoned", "turned into a plant" - in general, they destroy as a person in all possible ways.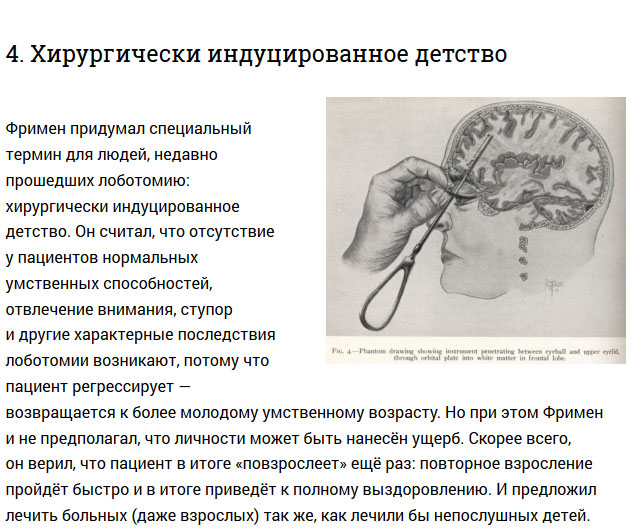
And before the hospital, the patient was just a feast for the eyes, aha!
Actually, this way of thinking has a very scientific name: social stigmatization. In fact, a person who is discharged from a psychiatric hospital is often completely different from what his relatives are used to. Was sociable - became withdrawn, was active, nimble - became inhibited and lethargic. And the media, books, cinema - willingly show exactly how pests in white coats carry out their hellish experiments on people. I will tell you a "secret": if anything turns our patients into "plants", it is not a cure, but a disease. However, this was not always the case…
Do you remember the famous book (or its adaptation) One Flew Over the Cuckoo's Nest and the fate of its main character, McMurphy? Let me remind you: McMurphy was subjected to a lobotomy for violations of the hospital regime. Cheerful, self-confident, groovy rogue-simulant turns into a weak-minded, into a drooling ruin.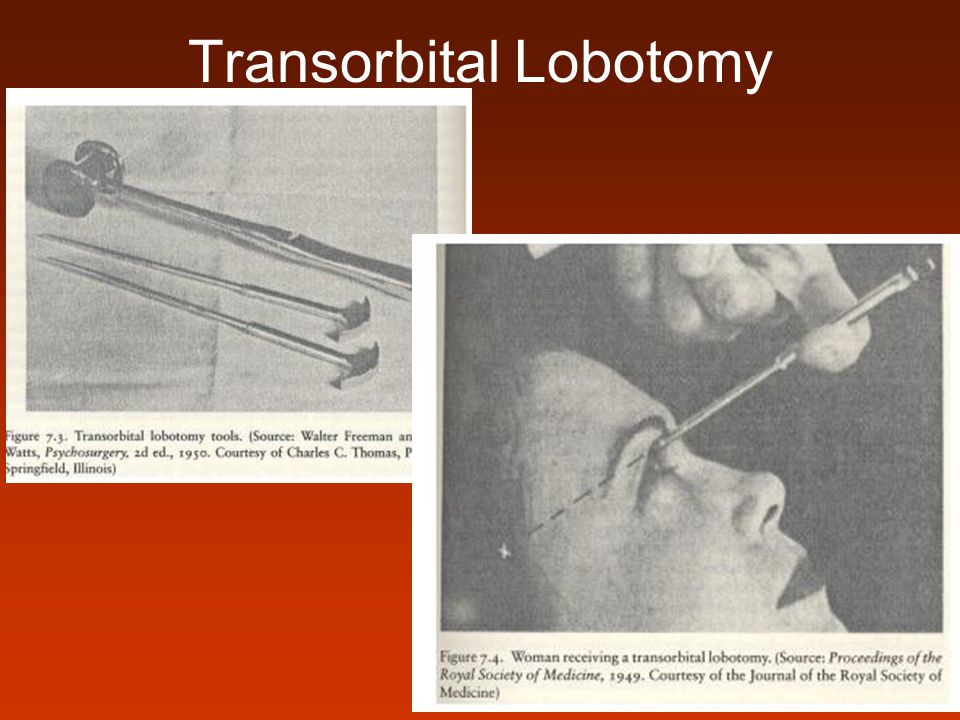 The author of the novel, Ken Kesey, who worked as an orderly in a mental hospital, described the "frontal syndrome" or "frontal lobe syndrome" that developed in people after lobotomy surgery.
The author of the novel, Ken Kesey, who worked as an orderly in a mental hospital, described the "frontal syndrome" or "frontal lobe syndrome" that developed in people after lobotomy surgery.
A bold idea
Brain lobotomy was developed in 1935 by the Portuguese psychiatrist and neurosurgeon Egas Moniz. In 1935, at a conference, he heard a report on the consequences of damage to the prefrontal zone in chimpanzees. Although the focus of this report was on learning difficulties associated with damage to the frontal lobes, Moniz was particularly interested in how one monkey became calmer and more docile after surgery. He hypothesized that the intersection of nerve fibers in the frontal lobe can help in the treatment of mental disorders, in particular - schizophrenia (the nature of which was still very vaguely understood). Moniz believed that the procedure was indicated for patients in serious condition or those whom aggressiveness made socially dangerous. Moniz performed his first operation at 1936 year.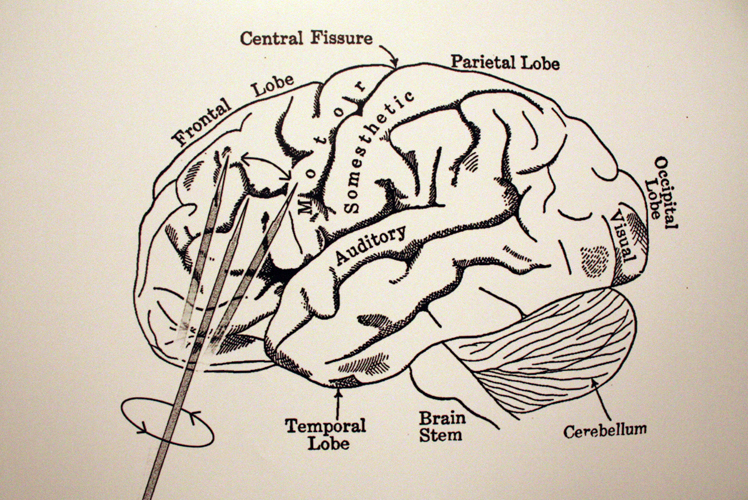 He called it "leukotomy": a loop was inserted into the brain with the help of a guide, and the white matter of the neuronal connections connecting the frontal lobes with other parts of the brain was cut through with rotational movements.
He called it "leukotomy": a loop was inserted into the brain with the help of a guide, and the white matter of the neuronal connections connecting the frontal lobes with other parts of the brain was cut through with rotational movements.
Prefrontal lobotomy, or leucotomy (from other Greek λοβός — share and τομή — cut), — brain surgery, in which the white matter of the frontal lobes of the brain is dissected on one or both sides, the cortex is separated from the lower parts of the brain. The consequence of such an intervention is the exclusion of the influence of the frontal lobes of the brain on the rest of the structures of the central nervous system.
Moniz performed about a hundred of these operations and observed patients. He liked the results, and in 1936 the Portuguese published the results of the surgical treatment of twenty of his first patients: seven of them recovered, seven improved, and six showed no positive dynamics.
Egas Moniz was awarded the Nobel Prize in Physiology or Medicine in 1949 "for his discovery of the therapeutic effects of leucotomy in certain mental illnesses". Since the Monish Prize, leucotomy has become more widely used.
So, Egas Moniz, in his “lobotomy” practice, observed hardly two dozen patients; he never saw most of the others after the operation. Moniz has written several articles and books on lobotomy. Criticism followed: opponents argued that the changes after the operation most of all resemble the consequences of a brain injury and, in fact, represent a degradation of the personality. Many believed that brain mutilation could not improve brain function and damage could lead to the development of meningitis, epilepsy, and brain abscesses. Despite this, Moniz's report (Prefrontal leucotomy. Surgical treatment of certain psychoses, Torino, 1937) led to rapid adoption of the procedure on an experimental basis by individual clinicians in Brazil, Cuba, Italy, Romania, and the United States.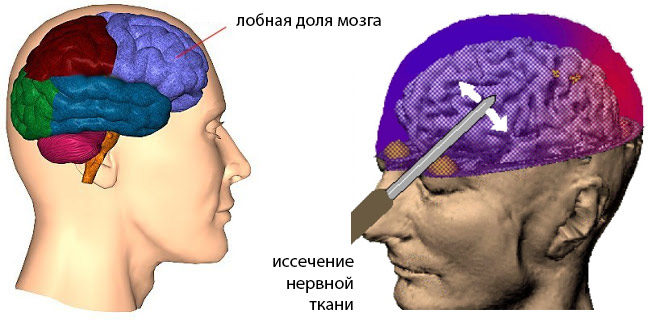
In the Land of Opportunity
American psychiatrist Walter Jay Freeman became the leading promoter of this operation. He developed a new technique that did not require drilling of the patient's skull and called it "transorbital lobotomy". Freeman aimed the narrow end of a surgical instrument, resembling an ice pick, at the eye socket bone, pierced a thin layer of bone with a surgical hammer, and inserted the instrument into the brain. After that, the fibers of the frontal lobes of the brain were cut with the movement of the knife handle. Freeman argued that the procedure would remove the emotional component from the patient's "mental illness". The first operations were carried out with a real ice pick. Subsequently, Freeman developed special instruments for this purpose - the leukotome, and then the orbitoclast.
In the 1940s, lobotomy in the United States became more common for purely economic reasons: the "cheap" method allowed the "treatment" of many thousands of Americans held in closed psychiatric institutions, and could reduce the costs of these institutions by a million dollars a day ! Leading newspapers wrote about the successes of the lobotomy, drawing public attention to it. It is worth noting that at that time there were no effective methods of treating mental disorders, and cases of returning patients from closed institutions to the community were extremely rare.
It is worth noting that at that time there were no effective methods of treating mental disorders, and cases of returning patients from closed institutions to the community were extremely rare.
In the early 1950s, about five thousand lobotomies were performed in the United States a year. Between 1936 and the late 1950s, between 40,000 and 50,000 Americans were lobotomized. The indications were not only schizophrenia, but also severe obsessive-compulsive disorder. Lobotomy was often performed by doctors who had no surgical training. Although not trained as a surgeon, Freeman nevertheless performed about 3,500 of these operations, traveling around the country in his own van, which he called the "lobotomobile".
Lobotomy was widely used not only in the USA, but also in other countries of the world - Great Britain, Finland, Norway, Sweden, Denmark, Japan, the USSR. In European countries, tens of thousands of patients underwent this operation
The result on the face
Already in the late 40s, psychiatrists "saw" that the first studies of lobotomy were carried out without a solid methodology: they operated with incomparable methods on patients with different diagnoses. Whether or not recovery has occurred is a question that has often been decided on the basis of such a criterion as improving the patient's manageability. At 19In the 1950s, more thorough research revealed that, in addition to death, which was observed in 1.5–6% of those operated on, lobotomy can cause seizures, large weight gain, loss of coordination, partial paralysis, urinary incontinence and other problems. Standard tests of intelligence and memory usually did not show any significant deterioration. Patients retained all types of sensitivity and motor activity, they did not experience impairments in recognition, practical skills and speech, but complex forms of mental activity disintegrated. More subtle changes have often been reported in the form of reduced self-control, foresight, creativity, and spontaneous action; selfishness and lack of concern for others. At the same time, criticism of one's own behavior was significantly reduced.
Whether or not recovery has occurred is a question that has often been decided on the basis of such a criterion as improving the patient's manageability. At 19In the 1950s, more thorough research revealed that, in addition to death, which was observed in 1.5–6% of those operated on, lobotomy can cause seizures, large weight gain, loss of coordination, partial paralysis, urinary incontinence and other problems. Standard tests of intelligence and memory usually did not show any significant deterioration. Patients retained all types of sensitivity and motor activity, they did not experience impairments in recognition, practical skills and speech, but complex forms of mental activity disintegrated. More subtle changes have often been reported in the form of reduced self-control, foresight, creativity, and spontaneous action; selfishness and lack of concern for others. At the same time, criticism of one's own behavior was significantly reduced.
Patients could answer ordinary questions or perform habitual actions, but the performance of any complex, meaningful and purposeful acts became impossible. They stopped experiencing their failures, experiencing hesitation, conflicts, and most often were in a state of indifference or euphoria. People who were previously energetic, restless, or aggressive in nature may develop changes towards impulsiveness, rudeness, emotional breakdowns, primitive humor, and unreasonable ambitions.
They stopped experiencing their failures, experiencing hesitation, conflicts, and most often were in a state of indifference or euphoria. People who were previously energetic, restless, or aggressive in nature may develop changes towards impulsiveness, rudeness, emotional breakdowns, primitive humor, and unreasonable ambitions.
In the USSR, special techniques for performing lobotomy were developed - much more accurate in the surgical sense and sparing in relation to the patient. The surgical method was offered only in cases of failure of long-term treatment, which included insulin therapy and electroshock. All patients underwent a general clinical and neurological examination and were carefully studied by psychiatrists. After the operation, both acquisitions in the emotional sphere, behavior and social adequacy, as well as possible losses, were recorded. The lobotomy method itself was recognized as fundamentally acceptable, but only in the hands of experienced neurosurgeons and in cases where the lesion was recognized as irreversible.
With maintenance therapy with nootropics and drugs that correct mental disorders, a significant improvement in the condition was possible, which could last for several years, but the end result still remained unpredictable. As Freeman himself noted, after hundreds of operations performed by him, about a quarter of patients were left to live with the intellectual capabilities of a pet, but "we are quite satisfied with these people ...".
Beginning of end
The decline of lobotomy began in the 1950s after serious neurological complications of the operation became apparent. In the future, lobotomy was prohibited by law in many countries - data have accumulated about the relatively low effectiveness of the operation and its greater danger compared to antipsychotics, which were becoming more and more perfect and actively introduced into psychiatric practice.
In the early 70s, the lobotomy gradually faded away, but in some countries continued to operate until the end of the 80s. In France between 19Between 80 and 1986, 32 lobotomies were performed, during the same period - 70 in Belgium and about 15 at the Massachusetts Hospital; about 15 operations were performed annually in the UK.
In France between 19Between 80 and 1986, 32 lobotomies were performed, during the same period - 70 in Belgium and about 15 at the Massachusetts Hospital; about 15 operations were performed annually in the UK.
In the USSR, lobotomy was officially banned in 1950. And this was not only an ideological underpinning. In the foreground were reasons of a purely scientific nature: the absence of a strictly substantiated theory of lobotomy; lack of strictly developed clinical indications for surgery; severe neurological and mental consequences of the operation, in particular "frontal defect".
“Lobotomy” with a bullet
More than 60 years have passed since the ban on lobotomy in our country. But people continue to get head injuries, get sick with various ailments (Peak's disease, for example), leading to a completely distinct "frontal" symptomatology. I will give a vivid observation of the consequences of the “frontal syndrome” from my own practice.
Two soldiers at the firing range, laughing, began pointing machine guns loaded with live ammunition at each other and shouting something like “Tra-ta-ta!..”. Suddenly he said his "word" and the machine gun ... The result - one had a bullet in the head. The neurosurgeons somehow managed to revive and repair the guy; they inserted several plates into his skull and sent him to us to resolve the issue of further treatment and disability.
During the conversation, the patient made a strange impression. Formally, his mind was not affected, his memory and stock of knowledge were at a normal level; he behaved quite adequately too — at first glance... An unnatural calmness, up to indifference, was striking; the guy indifferently talked about the injury, as if it did not happen to him; made no plans for the future. In the department he was absolutely passive, subordinating; for the most part, he lay on the bed. They invited me to play chess or backgammon, asked me to help the staff - I agreed.