Lamictal morning or night
How and when to take lamotrigine
Dosage
For epilepsy, the usual dose of lamotrigine is:
- adults and older children (aged 12 years and over) – 100mg to 700mg a day, taken as 1 or 2 doses
- younger children (aged 2 to 11 years) – the dose will vary depending on their weight
For bipolar disorder, the usual dose for adults is:
- between 200mg and 400mg a day, taken as either 1 or 2 doses
Changes to your dose
When you start taking lamotrigine, it's important to increase the dose slowly as this will help reduce or stop side effects.
Once you find a dose that suits you, it'll usually stay the same.
How to take it
You'll usually take lamotrigine once or twice a day. You can take it with or without food.
If you take it twice a day, try to space your doses evenly through the day. For example, take it first thing in the morning and in the evening.
If you're taking standard tablets, swallow them whole with a drink of water. Do not chew them.
If you're taking chewable or dispersible tablets, you can swallow them whole with a drink of water, or chew them or mix them with water or juice to make a drink.
How long to take it for
If you have epilepsy, it's likely that once your condition is under control you'll still need to take lamotrigine for many years.
If you have bipolar disorder, it's likely that you'll take lamotrigine for at least 6 months, but possibly much longer.
Important
Do not stop taking lamotrigine without speaking to your doctor first.
If you forget to take it
If you take lamotrigine once a day and forget your dose, take the missed dose as soon as you remember, unless it's less than 12 hours until your next dose is due. In this case, leave out the missed dose and take your next dose at the usual time.
If you take it twice a day, take the missed dose as soon as you remember, unless it's less than 8 hours before the next dose is due. In this case, leave out the missed dose and take your next dose at the usual time.
Do not take 2 doses at the same time. Never take an extra dose to make up for a forgotten one.
If you have epilepsy, it's important to take this medicine regularly. Missing doses may trigger a seizure.
If you forget to take your tablets for more than 5 days in a row, speak to your doctor, as you'll need to start on a low dose again and gradually increase to your usual dose.
If you forget doses often, it may help to set an alarm to remind you. You could also ask your pharmacist for advice on other ways to help you remember to take your medicine.
If you take too much
Taking too much lamotrigine can lead to symptoms such as:
- rapid, uncontrollable eye movements
- feeling clumsy or losing your balance
- feeling a change in the rhythm of your heartbeat
- having a seizure (fit)
- passing out
Urgent advice: Contact 111 for advice now if:
- you take more than your prescribed dose of lamotrigine
Go to 111.nhs.uk or call 111. If you need advice for a child under the age of 5 years, call 111.
If you have to go to A&E, do not drive yourself. Get someone else to drive you or call for an ambulance.
Get someone else to drive you or call for an ambulance.
Take the lamotrigine packet or the leaflet inside it, plus any remaining medicine, with you.
Stopping lamotrigine
Do not stop taking lamotrigine without talking to your doctor.
If you're taking lamotrigine for epilepsy, stopping it suddenly can cause seizures. Coming off lamotrigine should be done very slowly and might take a few months.
If you're taking lamotrigine for bipolar disorder, it's usually safe to stop taking it without having to reduce your dose first.
If you get a serious side effect, such as a severe skin rash, your doctor may tell you to stop taking lamotrigine straight away, even if you have epilepsy.
Page last reviewed: 20 May 2022
Next review due: 20 May 2025
Lamotrigine | Mood Stabiliser Uses & Side Effects
About lamotrigine
Please note
Thinking about trying medication? Read our guide
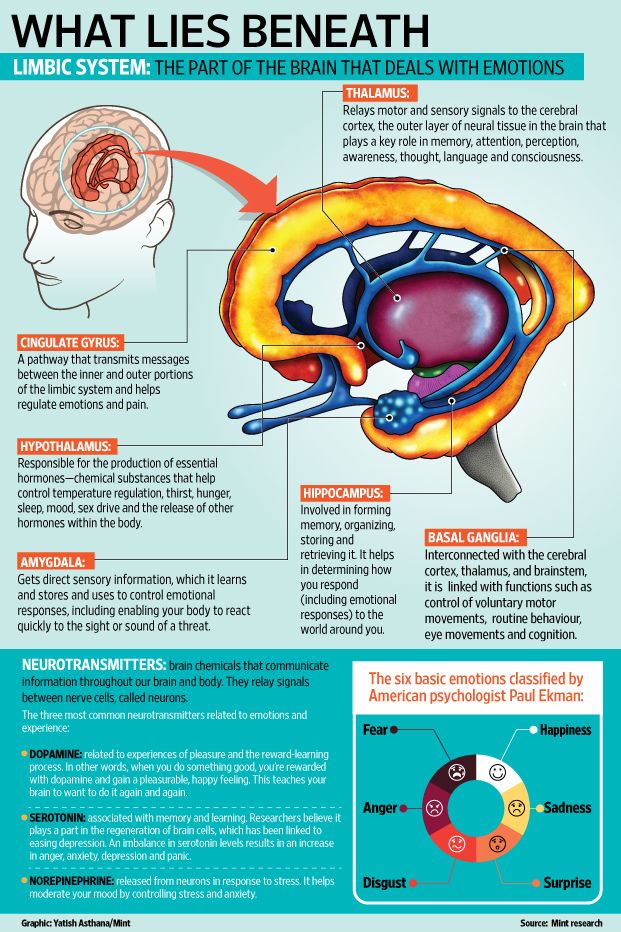
How lamotrigine works
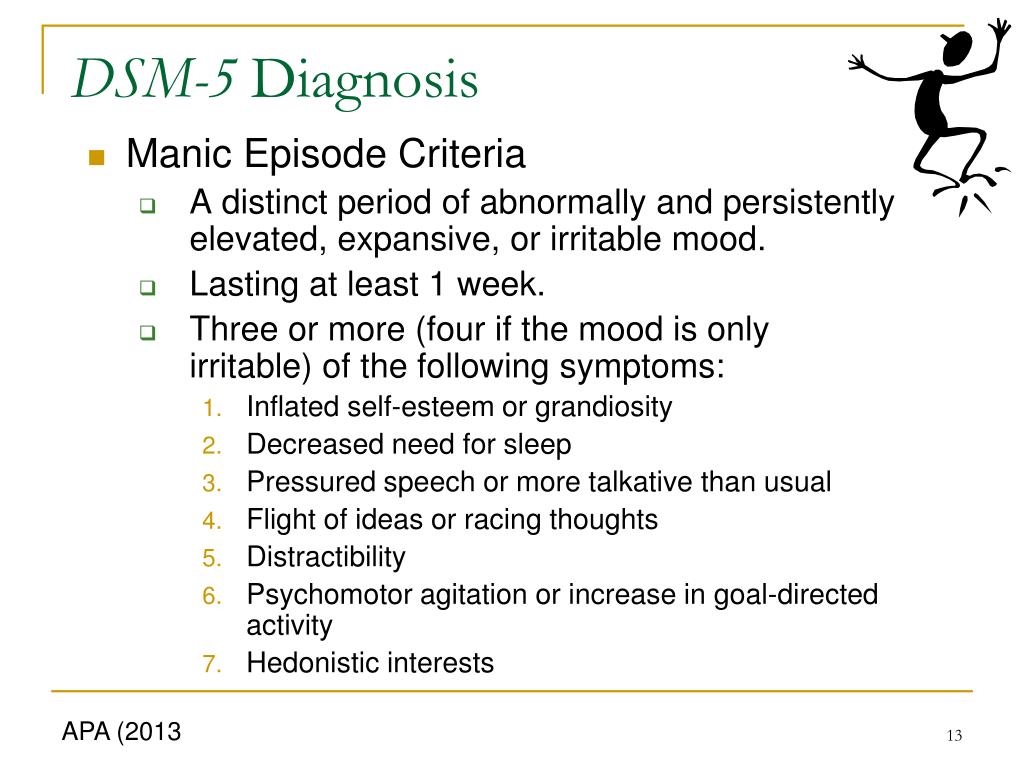
Lamotrigine is a type of medicine called a ‘mood stabiliser’ as it can reduce feelings of excitability and over-activity and reduce mood swings. It tends to work better on the low mood (depression) part of bipolar disorder.
It tends to work better on the low mood (depression) part of bipolar disorder.
It is also taken by some people who have epilepsy, as it increases the effects of the calming transmitter GABA, leading to a reduction in seizures. This is a very separate use but will be covered in any patient leaflets.
Bipolar disorderLamotrigine and everyday life
Frequently asked questions
You may start off at a low dose and gradually increase it every few days or weeks until you and your doctor find the dose that is right for you. It may take up to six weeks to do this, by which time you should be a on a stable, long-term dose and have seen some helpful results from the medication.
It is important not to hurry the dosing timetable as doing so can increase your chances of getting a serious skin reaction.
You may want to let your family and friends know you are taking lamotrigine so they can support you and help you look out for side effects.
For guidance on this, check out our page on getting support with your medication.
Lamotrigine may make you feel very drowsy or sleepy when you start taking it.
It may also make it difficult for you to get to sleep.
If these symptoms carry on for a long time, or if this is difficult for you, talk to your doctor or pharmacist about other medicines you could take.
Alcohol
You can drink alcohol while taking lamotrigine, but it is likely to make you feel sleepier.
Street drugs
We do not know how street drugs affect lamotrigine, but all these drugs affect the way the brain works so they may not mix well.
Lamotrigine can produce a false positive test for phencyclidine (PCP) on a urine drug screen. Talk to your doctor about this if it is a problem for you.
Lamotrigine does not mix well with some other medicines and drugs and may affect the way in which they work. Tell your doctor if you are taking any other medications including over-the-counter medicines for common illnesses and things you put on your skin.
Special information about contraceptive pills containing oestrogen
- When lamotrigine is taken with any type of the Pill (oral contraceptive) containing oestrogen, it lowers the level of lamotrigine that you have in your body.
- If you have a pill-free week, the levels of lamotrigine will then rise, which may give you side effects.
- If you take the Pill without a break, it will make your lamotrigine levels stable. You will not be harmed by not having the break.
- Talk to your doctor or pharmacist before you start taking lamotrigine if you also take the Pill.
- The morning-after pill does not affect the level of lamotrigine in your body as it does not contain oestrogen.
If you have any further questions about this, you should speak to your doctor or pharmacist.
Lamotrigine tablets have lactose in them which may not suit people who have a problem drinking milk or eating certain sugars. Talk to your doctor or pharmacist about this if you think it could be a problem for you.
Do not drive a car or ride a bike just after you start taking lamotrigine.
Taking lamotrigine may make you feel dizzy and may affect your eyesight when you start taking it (possibly causing blurred or double vision).
This could affect you if you drive a car, ride a bike, or do anything else that needs a lot of focus. It might be best to stop doing these things for the first few days, until you know how it affects you.
Do not worry - most people do these things as normal while taking lamotrigine.
Pregnancy
If you become pregnant while you are on lamotrigine, you should carry on taking the medicine and go back to your doctor as soon as possible to discuss whether you should stop or change your medicine.
Studies of over 7,500 women taking lamotrigine showed no increase in problems during the early stages of pregnancy.
Your doctor might also give you extra folic acid to take, which helps prevent any spine problems in your baby.
From month four onwards, you are likely to need a higher dose of lamotrigine to keep the level of the medication in your body constant. After giving birth, your lamotrigine dose will go back to what it was before.
If you are taking lamotrigine for epilepsy, any dose increases may be made based on the results of your blood level tests.
Post-natal
If you and your doctor agree that you will carry on taking lamotrigine throughout your pregnancy, you should tell your midwife that you are taking it before you give birth.
Breastfeeding
Lamotrigine can be passed to the baby in breastmilk, and side effects have been seen in breastfed babies. Usually there is no problem with breastfeeding a healthy baby.
Talk to your midwife or doctor about the benefits and risks of breastfeeding while taking lamotrigine.
There is nothing to suggest that lamotrigine has any effects on fertility.
Lamotrigine is not a banned substance in sport.
It could, however, make you feel dizzy and give you blurred or double vision when you start taking it.
It might be better to delay any sport that needs a lot of focus until you know how it affects you.
Do not worry - most people play sports as normal while taking lamotrigine.
Try not to take lamotrigine for the first time just before your exams, as you may have sleep problems (feeling tired or having difficulty getting to sleep), and some blurred eyesight or double vision when you start taking lamotrigine.
You should talk to your doctor about any future exams if you are starting lamotrigine.
You might decide together to delay starting it until you have done them.
If they are more than a month away, however, you might find that it is better to start lamotrigine to improve your motivation to study.
Do not worry - most people do all these things as normal while taking lamotrigine.
Your doctor should know
Uses, warnings, safety and side effects of lamotrigine
Taking lamotrigine
How long will I need to take lamotrigine for?
You and your doctor should talk about how long you need to take lamotrigine before you begin treatment with this medication.
If you take lamotrigine for bipolar disorder you will probably take it for at least six months (any shorter and your old symptoms can come back). If it works for you, you may take it for much longer than that.
You should only take lamotrigine as agreed with your doctor
Make sure that you know your dose. If it is not written on the label, check with your pharmacist or doctor.
You may have to take lamotrigine once or twice a day.
It doesn’t matter what time you take it each day – choose a time that you can always remember. This could be at mealtimes, or when you brush your teeth. You can take it before or after food.
If you are taking the tablets that you swallow whole, wash them down with a glass of water. Do not try and chew them – they will taste unpleasant.
If you are taking the orodispersible tablets (melts), get a glass of cold water and mix the tablet(s) in at least enough water to cover them. You can stir the drink to help them break up. 'Dispersible' doesn’t mean you will get a totally clear solution - it will look a little cloudy. Drink it all, and then add more water to the glass and drink that in order to make sure you get all the medicine in the tablet.
'Dispersible' doesn’t mean you will get a totally clear solution - it will look a little cloudy. Drink it all, and then add more water to the glass and drink that in order to make sure you get all the medicine in the tablet.
You can also chew the dispersible tablets, but it may help to rinse them down with some cold water.
You can still swallow the dispersible tablets whole with water if you prefer.
What should I do if I miss a dose of lamotrigine?
If you remember later during the day, take it as soon as possible. If you forget to take it by the time of the next dose, just start again with the next dose.
Do not take a double dose.
What will happen if I forget to take my lamotrigine?
If you forget to take your tablets for a few days, you may start getting your old symptoms of low mood back.
Stopping the use of lamotrigine
Although you may not be taking your lamotrigine for seizures (fits), if you stop the medication suddenly, there is a chance you may have a seizure. This is because after taking lamotrigine for some time, your body will have got used to having an anticonvulsant (anti-seizure) medicine on board. Suddenly stopping the use of lamotrigine may therefore cause a seizure. But don't worry - this doesn't mean you are suddenly epileptic.
This is because after taking lamotrigine for some time, your body will have got used to having an anticonvulsant (anti-seizure) medicine on board. Suddenly stopping the use of lamotrigine may therefore cause a seizure. But don't worry - this doesn't mean you are suddenly epileptic.
If you have stopped taking lamotrigine, you need to speak to your doctor so that you can safely start it again and build back up to your dose. It is best to be honest; they will help you get back on track.
If you are thinking of stopping treatment with lamotrigine, talk to your doctor before doing this.
Warnings and safety
Safety headlines
If you have taken more lamotrigine than the dosage recommended by the doctor who prescribed it to you, you must get medical help immediately – even if you do not feel any different.
While taking lamotrigine, some people may think about hurting themselves or taking their own lives. You must go straight to hospital with your medicine if you have any of these thoughts.
Lamotrigine can cause other serious side effects: allergic reactions (difficulty breathing, swelling of your face or throat, itching skin lumps), skin rashes and other serious symptoms. Go to a hospital with your medicine if you get any of these symptoms.
Lamotrigine does not mix well with some other medicines and drugs. The contraceptive Pill can affect the level of lamotrigine in your blood. Talk to your doctor about this if you are on the Pill.
You might feel dizzy or have double vision in the first few days after taking lamotrigine. Do not drive a car, ride a bike or operate machines until you see how this affects you.
Use good contraception while you are taking lamotrigine. If you take it while you are pregnant, it is unlikely to affect the developing baby. However, it can cause symptoms in babies if you breastfeed while taking lamotrigine. Talk to your doctor or midwife about this and get their help.
When to go to the hospital
If you have taken more lamotrigine than the dosage recommended by the doctor who prescribed it to you, you must get medical help immediately – even if you do not feel any different. Go to A&E, and take your medicine with you to show the doctors. Tell them how much you have taken. Get a friend to go with you, if you can, just in case you feel ill on the way.
Go to A&E, and take your medicine with you to show the doctors. Tell them how much you have taken. Get a friend to go with you, if you can, just in case you feel ill on the way.
You might get any of the following symptoms:
- quick, uncontrollable body movements
- clumsiness and lack of co-ordination, causing problems with your balance
- heart rhythm changes
- loss of consciousness, convulsions/seizures (fits) or coma
While taking lamotrigine some people may think about hurting themselves or have thoughts of taking their own lives. This can happen to anyone, including people who are under 25. These thoughts may happen or get worse in the first few weeks of taking the medicine. You must go straight to hospital with your medicine if you have any of these thoughts and tell the doctor that you are taking lamotrigine. There are other medications you can take instead.
You should also go to a doctor or hospital straight away if you get any of the following symptoms:
- skin rashes or redness with blisters and peeling skin around the mouth, nose, eyes and groin/sex organs (genitals)
- peeling of large areas of skin (up to 30% - almost a third – of your body surface)
- ulcers in the mouth, throat, nose or around your groin/sex organs (genitals)
- red or swollen eyes
- a high temperature (fever), flu-like symptoms or drowsiness
- swelling around your face
- swollen glands in your neck, armpit or groin
- unexpected bleeding or bruising
- your fingers turning blue
- a sore throat
- more infections (such as colds) than usual
If these reactions occur, they tend to be during the first eight weeks of taking lamotrigine.
Side effects of lamotrigine
Side effects of lamotrigine
Some side effects that appear should get better after a few days. If they do not, you should go back to your doctor.
Do not stop taking the tablets until you talk to your doctor, or you may get withdrawal symptoms as well.
Very common side effects of taking lamotrigine (affecting more than one in ten people) include:
- headaches
- skin rashes
Common side effects of taking lamotrigine (affecting up to one in ten people) include:
- feeling aggressive, agitated or irritable
- feeling sleepy, tired or drowsy
- insomnia (having difficulty sleeping)
- feeling dizzy
- shaking or tremors
- diarrhoea (loose poo)
- dry mouth
- nausea (feeling sick) or vomiting (being sick)
- having pain in your back or joints, or elsewhere
There are other side effects that you can get when taking this medicine; we have only included the most common ones here.
Please look at the leaflet inside your medicine box, or ask a doctor or pharmacist, if you want to know whether you are getting a side effect from your medicine.
If you do get a side effect, please think about reporting it via the Yellow Card Scheme.
Taking lamotrigine
How long will I need to take lamotrigine for?
You and your doctor should talk about how long you need to take lamotrigine before you begin treatment with this medication.
If you take lamotrigine for bipolar disorder you will probably take it for at least six months (any shorter and your old symptoms can come back). If it works for you, you may take it for much longer than that.
You should only take lamotrigine as agreed with your doctor
Make sure that you know your dose. If it is not written on the label, check with your pharmacist or doctor.
You may have to take lamotrigine once or twice a day.
It doesn’t matter what time you take it each day – choose a time that you can always remember. This could be at mealtimes, or when you brush your teeth. You can take it before or after food.
This could be at mealtimes, or when you brush your teeth. You can take it before or after food.
If you are taking the tablets that you swallow whole, wash them down with a glass of water. Do not try and chew them – they will taste unpleasant.
If you are taking the orodispersible tablets (melts), get a glass of cold water and mix the tablet(s) in at least enough water to cover them. You can stir the drink to help them break up. 'Dispersible' doesn’t mean you will get a totally clear solution - it will look a little cloudy. Drink it all, and then add more water to the glass and drink that in order to make sure you get all the medicine in the tablet.
You can also chew the dispersible tablets, but it may help to rinse them down with some cold water.
You can still swallow the dispersible tablets whole with water if you prefer.
What should I do if I miss a dose of lamotrigine?
If you remember later during the day, take it as soon as possible. If you forget to take it by the time of the next dose, just start again with the next dose.
Do not take a double dose.
What will happen if I forget to take my lamotrigine?
If you forget to take your tablets for a few days, you may start getting your old symptoms of low mood back.
Stopping the use of lamotrigine
Although you may not be taking your lamotrigine for seizures (fits), if you stop the medication suddenly, there is a chance you may have a seizure. This is because after taking lamotrigine for some time, your body will have got used to having an anticonvulsant (anti-seizure) medicine on board. Suddenly stopping the use of lamotrigine may therefore cause a seizure. But don't worry - this doesn't mean you are suddenly epileptic.
If you have stopped taking lamotrigine, you need to speak to your doctor so that you can safely start it again and build back up to your dose. It is best to be honest; they will help you get back on track.
If you are thinking of stopping treatment with lamotrigine, talk to your doctor before doing this.
Warnings and safety
Safety headlines
If you have taken more lamotrigine than the dosage recommended by the doctor who prescribed it to you, you must get medical help immediately – even if you do not feel any different.
While taking lamotrigine, some people may think about hurting themselves or taking their own lives. You must go straight to hospital with your medicine if you have any of these thoughts.
Lamotrigine can cause other serious side effects: allergic reactions (difficulty breathing, swelling of your face or throat, itching skin lumps), skin rashes and other serious symptoms. Go to a hospital with your medicine if you get any of these symptoms.
Lamotrigine does not mix well with some other medicines and drugs. The contraceptive Pill can affect the level of lamotrigine in your blood. Talk to your doctor about this if you are on the Pill.
You might feel dizzy or have double vision in the first few days after taking lamotrigine. Do not drive a car, ride a bike or operate machines until you see how this affects you.
Do not drive a car, ride a bike or operate machines until you see how this affects you.
Use good contraception while you are taking lamotrigine. If you take it while you are pregnant, it is unlikely to affect the developing baby. However, it can cause symptoms in babies if you breastfeed while taking lamotrigine. Talk to your doctor or midwife about this and get their help.
When to go to the hospital
If you have taken more lamotrigine than the dosage recommended by the doctor who prescribed it to you, you must get medical help immediately – even if you do not feel any different. Go to A&E, and take your medicine with you to show the doctors. Tell them how much you have taken. Get a friend to go with you, if you can, just in case you feel ill on the way.
You might get any of the following symptoms:
- quick, uncontrollable body movements
- clumsiness and lack of co-ordination, causing problems with your balance
- heart rhythm changes
- loss of consciousness, convulsions/seizures (fits) or coma
While taking lamotrigine some people may think about hurting themselves or have thoughts of taking their own lives. This can happen to anyone, including people who are under 25. These thoughts may happen or get worse in the first few weeks of taking the medicine. You must go straight to hospital with your medicine if you have any of these thoughts and tell the doctor that you are taking lamotrigine. There are other medications you can take instead.
This can happen to anyone, including people who are under 25. These thoughts may happen or get worse in the first few weeks of taking the medicine. You must go straight to hospital with your medicine if you have any of these thoughts and tell the doctor that you are taking lamotrigine. There are other medications you can take instead.
You should also go to a doctor or hospital straight away if you get any of the following symptoms:
- skin rashes or redness with blisters and peeling skin around the mouth, nose, eyes and groin/sex organs (genitals)
- peeling of large areas of skin (up to 30% - almost a third – of your body surface)
- ulcers in the mouth, throat, nose or around your groin/sex organs (genitals)
- red or swollen eyes
- a high temperature (fever), flu-like symptoms or drowsiness
- swelling around your face
- swollen glands in your neck, armpit or groin
- unexpected bleeding or bruising
- your fingers turning blue
- a sore throat
- more infections (such as colds) than usual
If these reactions occur, they tend to be during the first eight weeks of taking lamotrigine.
Side effects of lamotrigine
Side effects of lamotrigine
Some side effects that appear should get better after a few days. If they do not, you should go back to your doctor.
Do not stop taking the tablets until you talk to your doctor, or you may get withdrawal symptoms as well.
Very common side effects of taking lamotrigine (affecting more than one in ten people) include:
- headaches
- skin rashes
Common side effects of taking lamotrigine (affecting up to one in ten people) include:
- feeling aggressive, agitated or irritable
- feeling sleepy, tired or drowsy
- insomnia (having difficulty sleeping)
- feeling dizzy
- shaking or tremors
- diarrhoea (loose poo)
- dry mouth
- nausea (feeling sick) or vomiting (being sick)
- having pain in your back or joints, or elsewhere
There are other side effects that you can get when taking this medicine; we have only included the most common ones here.
Please look at the leaflet inside your medicine box, or ask a doctor or pharmacist, if you want to know whether you are getting a side effect from your medicine.
If you do get a side effect, please think about reporting it via the Yellow Card Scheme.
The information on this page was reviewed by the College of Mental Health Pharmacy in March 2020.
Visit the CMHP websiteCMHP. College of Mental Health Pharmacy
How to take antiepileptic drugs (AEDs)
home
Services
School of epilepsy
How to take antiepileptic drugs (AEDs)
General
Antiepileptic drugs (AEP) reduce the excessive excitability of brain cells, preventing the development of epileptic seizures. The effect of AEDs depends on their concentration in the blood, so the drugs should be taken daily. Most modern AEDs must be taken twice a day (morning and evening) to keep their blood levels stable. nine0003
How to increase the dose of the drug?
The slower the dose is increased, the lower the risk of side effects. Usually start with ½ or 1 tablet in the evening, after a few days add ½ or 1 tablet in the morning and so on, bringing the dose to therapeutic.
Usually start with ½ or 1 tablet in the evening, after a few days add ½ or 1 tablet in the morning and so on, bringing the dose to therapeutic.
What if I miss a dose?
For such cases, drugs have been developed that must be taken 2 times a day. If you forgot to drink your morning dose and remembered about it a few hours later, feel free to take it. If you remembered the forgotten dose only in the evening, you should not drink the morning + evening dose. Drink only the evening drink and do not forget to take the drug again. nine0003
How do I remember to take my medication?
It is necessary to "attach" the drug intake to regular events in life, for example: after breakfast and after dinner, after morning and evening walks with the dog, after morning and evening washing. You can use reminders on your mobile phone. If the patient suffers from impaired memory and thinking, relatives should monitor the medication. We recommend that you keep a diary of seizures every day and record each medication in it.
How to take medicines: before or after meals?
For modern drugs, this is not important. However, some of the AEDs can irritate the stomach, so we generally recommend taking it after a meal.
How do I change from one drug to another?
The most important rule is to do everything gradually. In most cases, the dose of the "new" drug is gradually increased first, then the dose of the "old" drug is also gradually reduced.
How to replace the drug with its analogue from another manufacturer (after all, the active substance is the same there)? nine0014
The universal rule is that if the body is accustomed to a certain drug of a certain company, then it is better not to change it. However, if there is no other choice (they stopped giving the drug for free and offer its substitute, but there is no money to buy the old drug), then it is necessary to gradually replace the “old” pills with the “new” ones. If you abruptly quit the “old” ones and start drinking the “new” ones, the risk of developing seizures and side effects is higher.
How dangerous are AEDs to health?
Unfortunately, absolutely safe drugs do not exist. In the world, 80% of patients taking AEDs report some side effects. The more modern the drug, the more side effects are indicated in its instructions for use (the manufacturer indicates them so that it cannot be sued). Side effects can be divided into 3 groups: nine0003
A) Idiosyncratic reactions (individual intolerance). They develop in the first months from the start of the medication. Most often - skin rash, jaundice, severe abdominal pain, bleeding, severe vomiting (there may be other manifestations). Idiosyncrasy appears suddenly, it cannot be predicted in advance. At risk are patients who have previously had severe adverse reactions to any drugs. If after the start of taking the medicine there are any serious disorders, you should immediately stop taking it and consult a doctor. nine0003
B) Dose-dependent side effects (they are not on small doses, but they appear on large ones). Typical examples: drowsiness, double vision, unsteadiness when walking, lethargy, trembling in the hands, etc. It is not necessary to immediately cancel the drug, the tactics depend on the severity of the side effects and the effectiveness of the drug (if the side effects are mild and there are no attacks, you will most likely have to put up with them, if the side effects are strong and the attacks still continue, there is no point in taking the drug). Often, over time, the body "gets used" to such side effects and their severity decreases. nine0003
Typical examples: drowsiness, double vision, unsteadiness when walking, lethargy, trembling in the hands, etc. It is not necessary to immediately cancel the drug, the tactics depend on the severity of the side effects and the effectiveness of the drug (if the side effects are mild and there are no attacks, you will most likely have to put up with them, if the side effects are strong and the attacks still continue, there is no point in taking the drug). Often, over time, the body "gets used" to such side effects and their severity decreases. nine0003
C) Chronic side effects - occur with long-term use of AEDs (thickening of the gum mucosa, weight gain or decrease, hormonal disorders, hearing or vision loss, etc.). In some cases, after discontinuation of the drug, these side effects may disappear (for example, weight gain or decrease), in other cases, these side effects are irreversible.
Nevertheless, the prescription of AED is the main method of treatment of epilepsy worldwide, because epileptic seizures in most cases pose a greater threat to health than taking AEDs.
 nine0014
nine0014 Authors: d.m.s. Kotov A.S.; doctor Eliseev Yu.V.
Comparative efficacy of mood stabilizers in the complex therapy of bulimia nervosa
The main forms of eating disorders are anorexia nervosa and bulimia nervosa. There are data in the literature on an increase in the number of patients with this pathology [7–9, 11] over the past decade.
According to ICD-10, for a reliable diagnosis of bulimia nervosa, the following signs are required: a) constant preoccupation with food and an irresistible craving for food, when the patient periodically cannot resist overeating and takes a large amount of food in a short time; b) counteracting the effect of obesity from the food eaten by the patient using one or more methods: inducing vomiting; abuse of laxatives, alternative periods of fasting; use of appetite suppressants, thyroid medications, or diuretics; neglect of insulin therapy by diabetic patients with bulimia; c) the presence in the psychopathological picture of a morbid fear of obesity, when the patient sets for himself a clearly defined limit of body weight - much lower than the premorbid weight, which in the eyes of the doctor represents the optimal or normal weight; frequent history of previous episodes of anorexia nervosa with remissions between the two disorders from several months to several years; the episode preceding bulimia may be symptomatic or mild with moderate weight loss and/or a transient period of amenorrhea. nine0003
nine0003
According to our data [2], patients with bulimia nervosa are characterized by the presence of cyclothymic affective fluctuations, often associated with the season, in combination with increased impulsivity, decreased control over primitive drives and/or severe anxiety disorders, and a tendency to abuse alcohol and drugs and nicotine addiction.
Since affective fluctuations, especially depression, are constantly found in bulimia nervosa, the use of antidepressants and mood stabilizers is justified. The presence of high impulsivity, psychopathic and impulse disorders justify the use of small doses of neuroleptics (behavior correctors). Thus, psychopharmacotherapy in the treatment of bulimia nervosa should be complex. We are talking about a combination of antidepressants and normothymic drugs with low doses of antipsychotics. As normotimics, it is advisable to use carbamazepine and lamotrigine. nine0003
Lamotrigine is an antiepileptic drug that blocks voltage-gated sodium channels in the presynaptic membranes of neurons and inhibits the excessive release of glutamic acid (an amino acid that plays a key role in the development of epileptic seizures). In addition, effects on calcium channels, GABAergic and serotonergic components are described. It is likely that the complex mechanism of action determines the wide spectrum of activity of lamotrigine in epilepsy and a positive effect on mood, which is used in the treatment of bipolar disorders. It should be noted that to date, lamotrigine is the only normotimic, the effectiveness of which, including in patients with "rapid phase change" [5], has been proven in methodologically correctly constructed blind, placebo-controlled studies [3, 4]. Lamotrigine is particularly effective in preventing depressive phases in patients with bipolar affective disorder [6]. nine0003
In addition, effects on calcium channels, GABAergic and serotonergic components are described. It is likely that the complex mechanism of action determines the wide spectrum of activity of lamotrigine in epilepsy and a positive effect on mood, which is used in the treatment of bipolar disorders. It should be noted that to date, lamotrigine is the only normotimic, the effectiveness of which, including in patients with "rapid phase change" [5], has been proven in methodologically correctly constructed blind, placebo-controlled studies [3, 4]. Lamotrigine is particularly effective in preventing depressive phases in patients with bipolar affective disorder [6]. nine0003
Carbamazepine is a derivative of tricyclic iminostilbene containing a carbamoyl group in position 6, which mainly determines the presence of anticonvulsant activity in the drug. Structurally, carbamazepine is close to tricyclic antidepressants of the dibenzoazepine group. The drug has a pronounced anticonvulsant (antiepileptic) and moderately antidepressant (thymoleptic) and normothymic effect. In the mechanism of action of carbamazepine, its GABAergic properties, as well as interaction with central adenosine receptors, play a certain role. In terms of overall effectiveness, carbamazepine is not inferior to lithium carbonate and sodium valproate, however, it has a different spectrum of normothymic action, since its effect is more fully manifested in relation to the reduction of depression compared to mania [1, 12]. The antidepressant effect of carbamazepine is less pronounced than the antimanic effect [10]. nine0003
In the mechanism of action of carbamazepine, its GABAergic properties, as well as interaction with central adenosine receptors, play a certain role. In terms of overall effectiveness, carbamazepine is not inferior to lithium carbonate and sodium valproate, however, it has a different spectrum of normothymic action, since its effect is more fully manifested in relation to the reduction of depression compared to mania [1, 12]. The antidepressant effect of carbamazepine is less pronounced than the antimanic effect [10]. nine0003
The aim of this work was to study the effectiveness of mood stabilizers - carbamazepine and lamotrigine in the complex therapy of bulimia nervosa using an antidepressant.
Fluoxetine, a serotonin reuptake inhibitor, was chosen as the first choice antidepressant for bulimia nervosa. Fluoxetine is a weak antagonist of cholinergic, adreno-, and histamine receptors. Unlike many antidepressants, it does not cause a decrease in the functional activity of postsynaptic β-adrenergic receptors, improves mood, reduces feelings of fear and tension, and reduces dysphoria without the effect of sedation. In average therapeutic concentrations, it practically does not affect the functions of the cardiovascular system. nine0003
In average therapeutic concentrations, it practically does not affect the functions of the cardiovascular system. nine0003
Material and methods
The study included 45 women with various forms of bulimia nervosa. Their mean age was 22.5±4 years; the average duration of the disease is 4.2 years.
Patients included patients (60.9%) with cyclic affective fluctuations in the direction of downward mood and drive disorders and patients with less pronounced cyclic affective fluctuations, characterized by the presence of anxiety, in which there were no or mild drive disorders. nine0003
All patients had premorbid cyclothymic personality traits. 28 (62.2%) people abused alcohol, 23 (51%) - narcotic and other psychoactive substances, 72% of patients smoked; 25 (56%) women were distinguished by sexual disinhibition.
All patients at the time of examination had bulimic symptoms (strong hunger, insatiation, bouts of overeating with possible subsequent induction of artificial vomiting). In order to avoid possible, in their opinion, weight gain after overeating, they engaged in intense physical exercise and limited themselves to food, which was expressed in the use of various low-calorie diets, alternative fasting periods, as well as laxatives and diuretics, cleansing enemas. Almost all patients induced vomiting after bouts of overeating. nine0003
In order to avoid possible, in their opinion, weight gain after overeating, they engaged in intense physical exercise and limited themselves to food, which was expressed in the use of various low-calorie diets, alternative fasting periods, as well as laxatives and diuretics, cleansing enemas. Almost all patients induced vomiting after bouts of overeating. nine0003
Patients were randomized into two groups according to the characteristics of therapy.
In the 1st group (25 patients), patients were prescribed fluoxetine at a dose of 20 mg in the morning and carbamazepine at a dose of 200 mg in 3 doses (50 mg in the morning and afternoon and 100 mg in the evening).
The 2nd group (20 people) was prescribed fluoxetine 20 mg per day in the morning. Lamotrigine was included in therapy according to the scheme: 25 mg per day in the morning and then every 7 days the dose was increased by 25 mg/day up to 100 mg/day.
nine0002 The selected groups did not differ in age and duration of the disease, as well as the features of complex therapy. In all cases, non-drug methods of treatment were used: individual and group psychotherapy, physiotherapy in the form of a circular shower, ultraviolet therapy, respiratory and relaxation therapeutic exercises.
In all cases, non-drug methods of treatment were used: individual and group psychotherapy, physiotherapy in the form of a circular shower, ultraviolet therapy, respiratory and relaxation therapeutic exercises. After discharge from the hospital, all patients continued to take fluoxetine and normothymic for 6 months, and then, after fluoxetine was canceled, they continued to take normothymic for prophylactic purposes for another 3 months. nine0003
The ranking of bulimic symptoms was carried out as follows: no overeating - 0 points; overeating 1-2 times a week (low level) - 1 point; daily bouts of overeating followed by vomiting, no more than 1 time per day (average level) - 2 points; bouts of overeating daily, several times a day with the use of vomiting and gastric lavage (up to clean water), abuse of laxatives, diuretics (high level) - 3 points.
nine0002 The severity of depression was determined on the Hamilton scale (HAM-D), the level of reactive and personal anxiety on the Spielberger self-assessment scale, the degree of asthenia according to subjective criteria with a score on a 5-point scale. In addition, memory functions and other cognitive functions were assessed.
In addition, memory functions and other cognitive functions were assessed. The examination was carried out twice: before the start of pharmacotherapy and after 30 days of inpatient treatment. A year later, a follow-up examination of all patients was carried out.
Results and discussion
Against the background of complex therapy, patients of both groups noted the alignment of mood, a decrease in the frequency and intensity of overeating attacks, vomiting, and the normalization of food intake. As the mood leveled out, the level of fear of weight gain, the intensity of dysmorphophobic experiences, reactive and personal anxiety decreased in most patients.
When quantifying bulimic disorders, the following dynamics was established: before the start of therapy in the 1st group - 2.6 points, after 30 days from the start of therapy - 0.6 points; in the 2nd group before the start of therapy - 2.5 points, after 30 - 0.4 points. nine0003
The level of depression according to HAM-D was determined in the 1st group by an indicator of 15-23 points at the beginning of therapy in both groups, and after 30 days 5-7 points in the 1st group and 0-3 points in the 2nd. According to the Spielberger scale, the level of reactive anxiety before the start of therapy in both groups was high - more than 45 points; after 30 days it decreased to 28-35 points in both groups; averaged 29.6 points in the 1st group and 30.1 points in the 2nd. As for personal anxiety, its indicators changed: 34 points before the start of therapy and 28 points after 30 days, without significant differences between groups. nine0003
According to the Spielberger scale, the level of reactive anxiety before the start of therapy in both groups was high - more than 45 points; after 30 days it decreased to 28-35 points in both groups; averaged 29.6 points in the 1st group and 30.1 points in the 2nd. As for personal anxiety, its indicators changed: 34 points before the start of therapy and 28 points after 30 days, without significant differences between groups. nine0003
The phenomena of asthenia during therapy also decreased: from 5 to 2-3 points in the 1st group and to 0 in the 2nd.
There was also an improvement in cognitive functioning in terms of the ability to memorize and logical construction, the concept of attention, working capacity, the ability to synthesize and analyze the information received.
So, if before the start of the course of treatment, patients memorized from 4 to 6 words spoken aloud and from 3 to 5 geometric figures drawn on paper, then after 30 days of treatment in the 2nd group the number of memorized words increased to 6-9, and geometric shapes - 6-8, in the 1st group the number of memorized words changed little - 5-6 words, and the number of geometric shapes only up to 4-6.
Among the side effects in the 1st group, complaints of drowsiness and lethargy during the day prevailed. In the 2nd group, 3 patients developed skin-allergic reactions in the form of a rash, skin itching. Five patients were excluded from the study: 2 patients from the 1st group due to the severity of side effects and 3 patients from the 2nd group due to allergic reactions. nine0003
A follow-up examination of treated patients in a year gave the following results.
In the 1st group, 8 (34.8%) patients were found to be in stable remission, with no clinical manifestations of bulimia (they had no bouts of overeating for 6 months before the examination, body weight corresponded to a BMI from 18 to 21 points), and social rehabilitation (5 patients continued their studies at a higher educational institution, 3 patients got a job, 2 got married). 12 (46.1%) patients reported a relapse of the disease (overeating rate 2 points) after fluoxetine withdrawal, of which only 2 returned to work. In 3 (13%) patients, clinical manifestations persisted while taking medications (the frequency of vomiting ranged from 1 to 3 points). nine0003
In 3 (13%) patients, clinical manifestations persisted while taking medications (the frequency of vomiting ranged from 1 to 3 points). nine0003
In the 2nd group, 11 (64.7%) patients showed stable remission (for 6 months before the examination, there were no attacks of overeating, body weight corresponded to BMI from 18 to 21 points). At the same time, social rehabilitation was more successful (all 11 patients successfully continued their studies or got a job). 6 (35.2%) patients reported relapse (vomiting frequency 1 to 3 points) after fluoxetine discontinuation, and 1 (5%) patient continued to overeat and vomit.
nine0002 Thus, the combination of fluoxetine and mood stabilizers during 30-day therapy of patients with bulimia nervosa made it possible to achieve a stable improvement in the condition of patients. At the same time, lamotrigine, compared with carbamazepine, caused a slightly greater decrease in the severity of depression. Carbamazepine had little effect on the cognitive functions studied, while the use of lamotrigine significantly improved them.