Dsm 5 criteria for agoraphobia
Agoraphobia - Psychiatric Disorders - Merck Manuals Professional Edition
By
John W. Barnhill
, MD, New York-Presbyterian Hospital
Last review/revision Apr 2020 | Modified Sep 2022
View Patient Education
Topic Resources
Agoraphobia is fear of and anxiety about being in situations or places without a way to escape easily or in which help might not be available if intense anxiety develops.
(See also Overview of Anxiety Disorders Overview of Anxiety Disorders Everyone periodically experiences fear and anxiety. Fear is an emotional, physical, and behavioral response to an immediately recognizable external threat (eg, an intruder, a car spinning on.
.. read more .)
The situations are avoided, or they may be endured but with substantial anxiety. About 30 to 50% of people with agoraphobia also have panic disorder Panic Attacks and Panic Disorder A panic attack is the sudden onset of a discrete, brief period of intense discomfort, anxiety, or fear accompanied by somatic and/or cognitive symptoms. Panic disorder is occurrence of repeated... read more .
Agoraphobia without panic disorder affects about 2% of women and 1% of men during any 12-month period. Peak age at onset is the early 20s; first appearance after age 40 is unusual.
Common examples of situations or places that create fear and anxiety include standing in line at a bank or at a supermarket checkout, sitting in the middle of a long row in a theater or classroom, and using public transportation, such as a bus or an airplane. Some people develop agoraphobia after a panic attack in a typical agoraphobic situation. Others simply feel uncomfortable in such a situation and may never or only later have panic attacks there.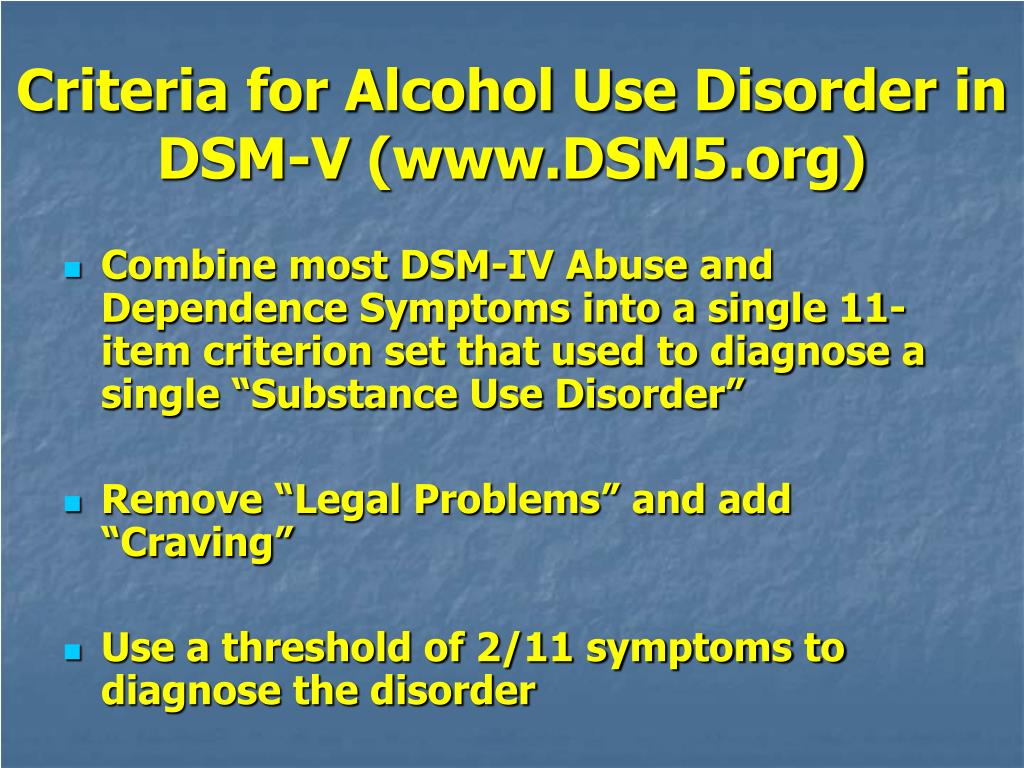 Agoraphobia often interferes with function and, if severe enough, can cause people to become housebound.
Agoraphobia often interferes with function and, if severe enough, can cause people to become housebound.
Clinical criteria
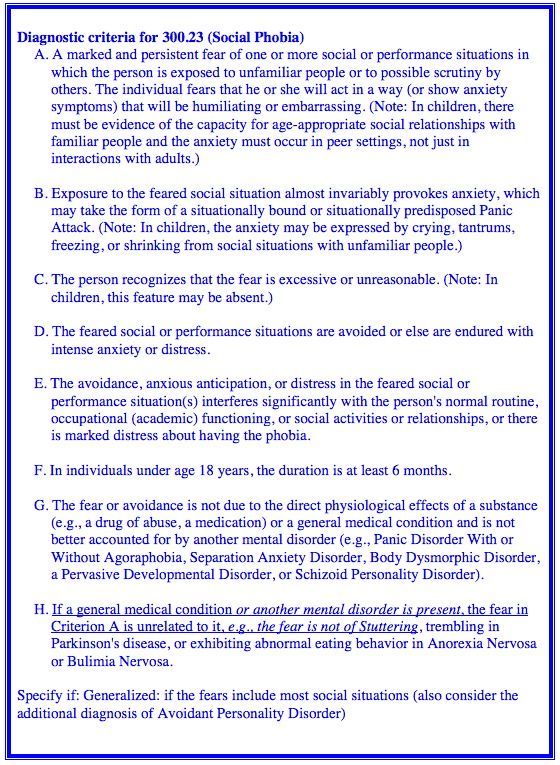
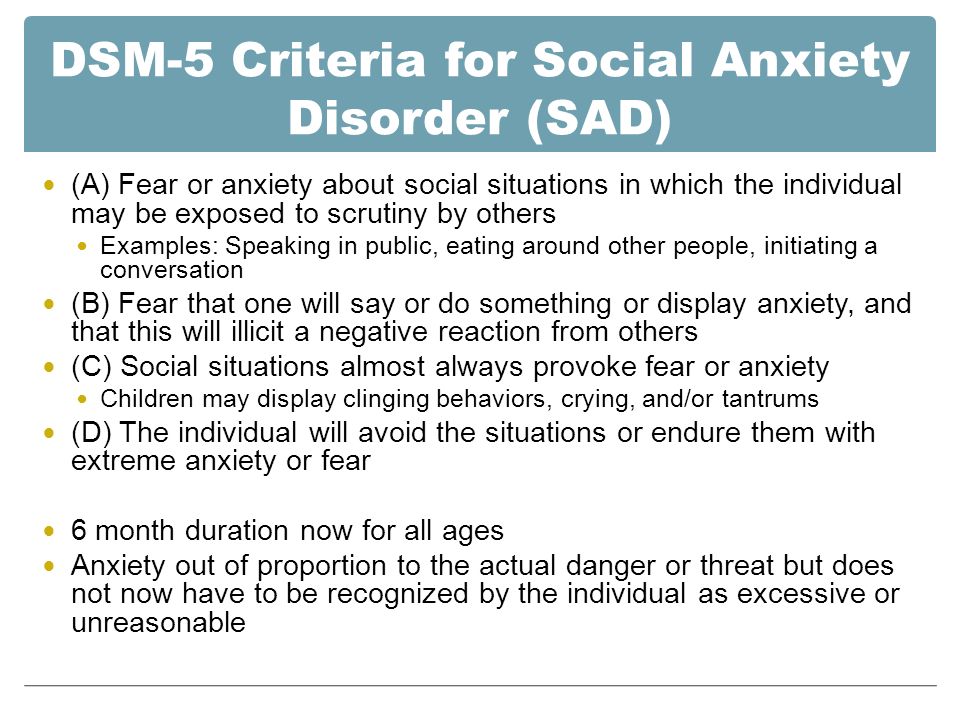
Diagnosis is clinical based on criteria in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5).
To meet the DSM-5 criteria for diagnosis, patients must have marked, persistent (≥ 6 months) fear of or anxiety about ≥ 2 of the following situations:
Using public transportation
Being in open spaces (eg, parking lot, marketplace)
Being in an enclosed place (eg, shop, theater)
Standing in line or being in a crowd
Being alone outside the home
Fear must involve thoughts that escape from the situation might be difficult or that patients would receive no help if they became incapacitated by fear or a panic attack. In addition, all of the following should be present:
The same situations nearly always trigger fear or anxiety.
Patients actively avoid the situation and/or require the presence of a companion.
The fear or anxiety is out of proportion to the actual threat (taking into account sociocultural norms).
The fear, anxiety, and/or avoidance cause significant distress or significantly impair social or occupational functioning.
Also, the fear and anxiety cannot be more correctly characterized as a different mental disorder (eg, social anxiety disorder Social Phobia Social phobia is fear of and anxiety about being exposed to certain social or performance situations. These situations are avoided or endured with substantial anxiety. Phobias are a type of... read more , body dysmorphic disorder Body Dysmorphic Disorder Body dysmorphic disorder is characterized by preoccupation with ≥ 1 perceived defects in physical appearance that are not apparent or appear only slight to other people. The preoccupation with... read more ).
VIDEO
If untreated, agoraphobia usually waxes and wanes in severity.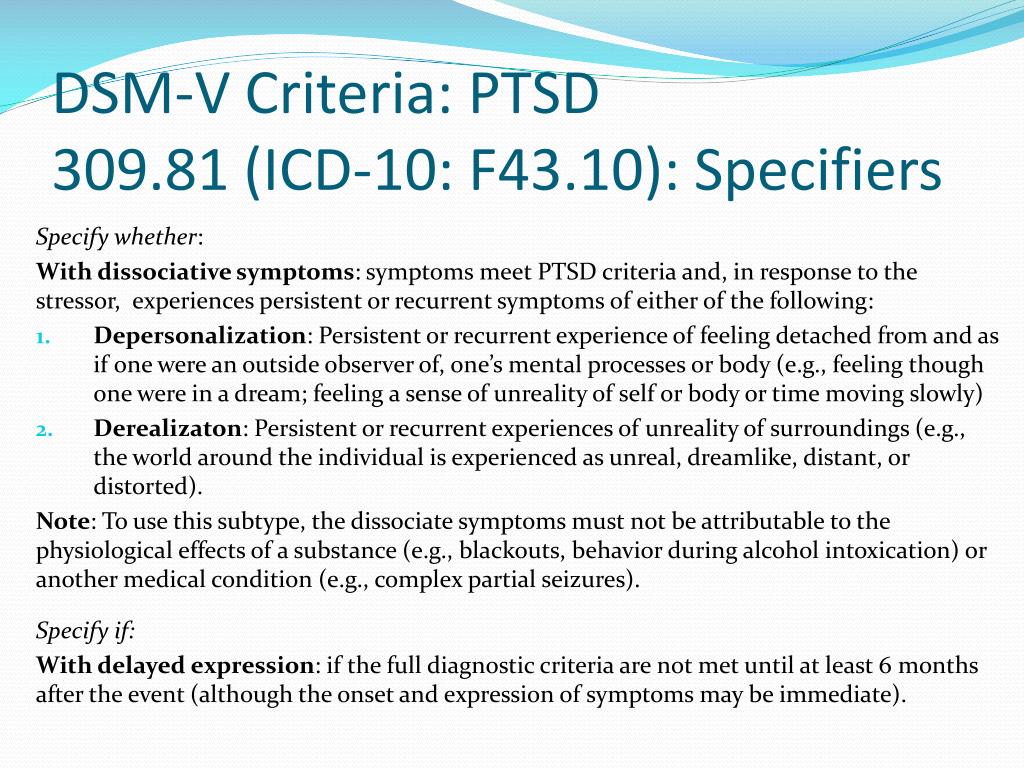 Agoraphobia may disappear without formal treatment, possibly because some affected people conduct their own form of exposure therapy. But if agoraphobia interferes with functioning, treatment is needed.
Agoraphobia may disappear without formal treatment, possibly because some affected people conduct their own form of exposure therapy. But if agoraphobia interferes with functioning, treatment is needed.
Cognitive-behavioral therapy is effective for agoraphobia. Cognitive-behavioral therapy involves teaching patients to recognize and control their distorted thinking and false beliefs as well as instructing them on exposure therapy Exposure therapy Specific phobic disorders consist of persistent, unreasonable, intense fears (phobias) of specific situations, circumstances, or objects. The fears provoke anxiety and avoidance. The causes... read more .
Many patients with agoraphobia benefit from drug therapy with an SSRI.
NOTE: This is the Professional Version. CONSUMERS: View Consumer Version
Copyright © 2023 Merck & Co. , Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
, Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
Test your knowledge
Take a Quiz!Agoraphobia - PsychDB
Table of Contents
Agoraphobia
Primer
DSM-IV to DSM 5 Change
DSM-5 Diagnostic Criteria
Signs and Symptoms
Screening and Rating Scales
Pathophysiology
Differential Diagnosis
Investigations
Physical Exam
Treatment
Guidelines
Resources
Primer
Agoraphobia is an anxiety disorder where an individual has intense fears about at least two different types of situations, with the fear being that escape may be difficult or help may be unavailable if panic-like symptoms occur.
Epidemiology
The annual prevalence of agoraphobia is about 1.
 7%.
7%.The incidence peaks in late adolescence and early adulthood.
Females are twice as likely as males to experience agoraphobia.
Prognosis
The course of agoraphobia is usually persistent and chronic.
If untreated, the remission rate is around 10%.
More than 33% of individuals with agoraphobia are homebound and unable have gainful employment.
Comorbidity
Other anxiety disorders such as specific phobias, panic disorder, and social anxiety disorder are common.
Major depressive disorder, PTSD, and alcohol use disorder are also common as well, typically as a secondary result of agoraphobia.
Risk Factors
Anxiety disorders, depressive disorders, substance use disorders, and personality disorders, can be comorbid with agoraphobia.
Temperamental factors such as anxiety sensitivity (belief that anxiety symptoms are harmful)
Environmental factors such as reduced warmth and increased overprotection by parental figures, and adverse childhood events are risk factors.
The heritability for agoraphobia is is 61%., and has the most genetic association of the phobias.
Cultural
What counts as avoidance is difficult to judge aross cultures and sociocultural contexts (e.g. - it may be socioculturally appropriate for orthodox Muslim women to avoid leaving the house alone, and this is not indicative of agoraphobia).
DSM-IV to DSM 5 Change
The DSM-5 created agoraphobia as a separate diagnosis, whereas in the previous version, DSM-IV, panic disorder could be diagnosed as “panic disorder with agoraphobia” or “panic disorder without agoraphobia.” Thus, much of the research on agoraphobia is based on the DSM-IV definition.
DSM-5 Diagnostic Criteria
Criterion A
Marked fear or anxiety about at least 2 of the following 5 situations:
Public transportation (e.g. - automobiles, buses, trains, ships, planes)
Open spaces (e.
 g. - parking lots, malls, marketplaces, bridges)
g. - parking lots, malls, marketplaces, bridges)Enclosed places (e.g. - rooms, shops, theatres, cinemas)
Crowds or standing in line
Being outside of home alone
Criterion B
The individual fears or avoids these situations because of thoughts that:
Escape might be difficult, or
Help might not be available in the event of developing panic-like symptoms or other incapacitating or embarrassing symptoms (e.g. - fear of falling or fear of incontinence in the elderly).
Criterion C
The agoraphobic situations almost always provoke fear or anxiety.
Criterion D
The agoraphobic situations are actively avoided, require the presence of a companion, or are endured with intense fear or anxiety.
Criterion E
The fear or anxiety is out of proportion to the actual danger posed by the agoraphobic situations and to the sociocultural context.
Criterion F
The fear, anxiety, or avoidance is persistent, typically lasting for 6 months or more.
Criterion G
The fear, anxiety, or avoidance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning.
Criterion H
If another medical condition (e.g. - inflammatory bowel disease, Parkinson’s disease) is present, the fear, anxiety, or avoidance is clearly excessive.
Criterion I
The fear, anxiety, or avoidance is not better explained by the symptoms of another mental disorder:
The symptoms are not confined to a specific phobia, situational type
Do not involve only social situations (social anxiety disorder)
Do not relate exclusively to obsessions (obsessive-compulsive disorder)
Do not relate to defects or flaws in physical appearance (body dysmorphic disorder)
Do not relate to reminders of traumatic events (post-traumatic stress disorder)
Do not relate to fear of separation (separation anxiety disorder).

Note: Agoraphobia is diagnosed irrespective of the presence of panic disorder. If an individual’s presentation meets criteria for panic disorder and agoraphobia, both diagnoses should be assigned.
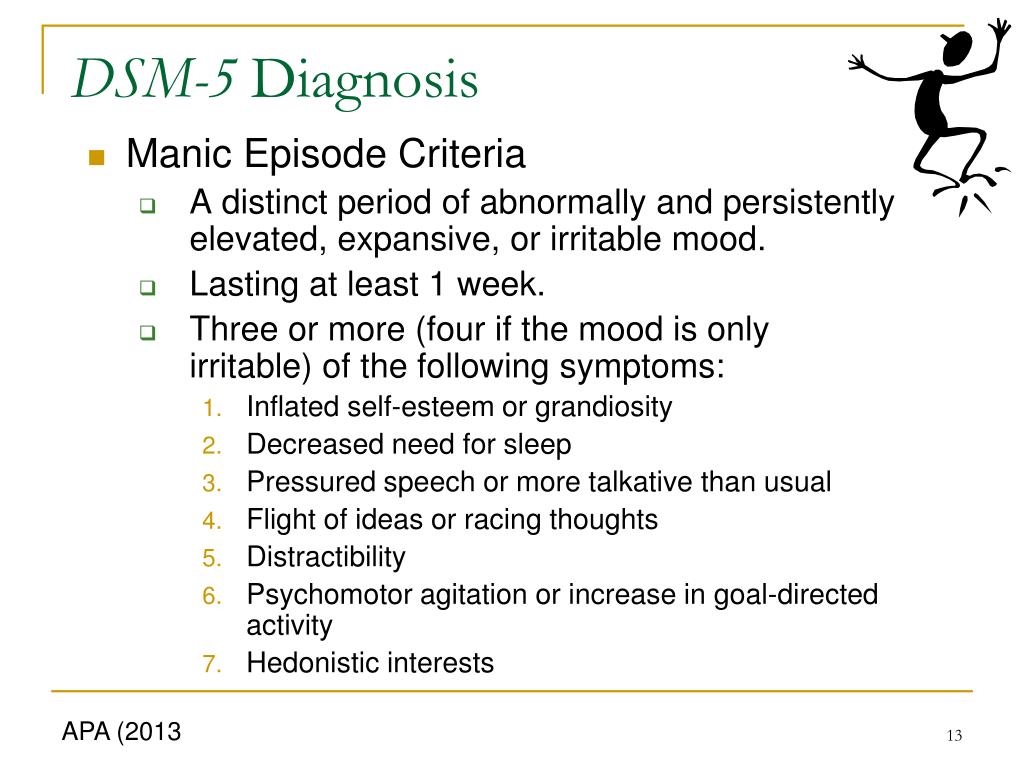
Panic Attack Specifier
Specify if:
Sweating
Trembling or shaking
Unsteady, dizziness, light-headed, or faint
Derealization (feelings of unreality) or depersonalization (being detached from one self)
Excessive/accelerated heart rate, palpitations, or pounding heart
Nausea or abdominal distress
Tingling, numbness, parathesesias
Shortness of breath
Fear of losing control or “going crazy”
Fear of dying
Choking feelings
Chest pain or discomfort
Chills or heat sensations
Note: The symptoms presented in this specifier are for the purpose of identifying a panic attack. However, panic attacks are not a mental disorder. Panic attacks can occur in the context of any anxiety disorder as well as other mental disorders (e.g. - depressive disorders, posttraumatic stress disorder, substance use disorders) and some medical conditions (e.g. - cardiac, respiratory, vestibular, gastrointestinal). When the presence of a panic attack is identified, it should be noted as a specifier (e.g. - “social anxiety disorder with panic attacks”). For panic disorder, the presence of panic attack is contained within the criteria for the disorder and panic attack is not used as a specifier.
However, panic attacks are not a mental disorder. Panic attacks can occur in the context of any anxiety disorder as well as other mental disorders (e.g. - depressive disorders, posttraumatic stress disorder, substance use disorders) and some medical conditions (e.g. - cardiac, respiratory, vestibular, gastrointestinal). When the presence of a panic attack is identified, it should be noted as a specifier (e.g. - “social anxiety disorder with panic attacks”). For panic disorder, the presence of panic attack is contained within the criteria for the disorder and panic attack is not used as a specifier.
Note: Culture-specific symptoms (e.g. - tinnitus, neck soreness, headache, uncontrollable screaming or crying) may be seen. Such symptoms should not count as one of the four required symptoms.
Signs and Symptoms
Individuals with agoraphobia frequently believe that escape from such their feared situations might be difficult (e.
 g. - “I won't be able to get out of here”) or that help might be unavailable (e.g. - “There will be nobody there to help me”) when the panic-like symptoms or other incapacitating or embarrassing symptoms occur.
g. - “I won't be able to get out of here”) or that help might be unavailable (e.g. - “There will be nobody there to help me”) when the panic-like symptoms or other incapacitating or embarrassing symptoms occur.Beyond the panic attack symptoms (see above), other incapacitating or embarrassing symptoms include symptoms such as:
Vomiting and inflammatory bowel symptoms
In older adults, a fear of falling
In children, a sense of disorientation and getting lost
It is important to recognize that the fear or anxiety is evoked nearly every time the individual comes into contact with the feared situation.
The avoidance can become so impairing that the person is completely homebound and refuses to leave.
Screening and Rating Scales
Pathophysiology
See also article: Panic Disorder: Pathophysiology
Differential Diagnosis
When diagnostic criteria for agoraphobia and another disorder are fully met, both diagnoses should be assigned, unless the fear, anxiety, or avoidance of agoraphobia is attributable to the other disorder. Weighting of criteria and clinical judgment may be helpful in some cases.
Weighting of criteria and clinical judgment may be helpful in some cases.
Specific phobia, situational type
Differentiating agoraphobia from situational specific phobia can be challenging in some cases, because these conditions share similar symptoms.
Specific phobia, situational type, should be diagnosed instead of agoraphobia if the fear, anxiety, or avoidance is limited to just
1of the agoraphobic situations.If there are fears from
2or more agoraphobic situations, a diagnosis of agoraphobia is warranted. Thus, if the situation is feared for reasons other than panic-like symptoms or other incapacitating or embarrassing symptoms (e.g. - fears of being directly harmed by the situation itself, such as fear of being bitten by a dog), then the diagnosis of specific phobia is more appropriate.
Separation anxiety disorder
In separation anxiety disorder, the thoughts are about be away from significant others and the home environment (i.
 e. - parents or other attachment figures). Contrast this with agoraphobia, where the focus is on panic-like symptoms or other incapacitating or embarrassing symptoms in the two or more feared situations.
e. - parents or other attachment figures). Contrast this with agoraphobia, where the focus is on panic-like symptoms or other incapacitating or embarrassing symptoms in the two or more feared situations.
Social anxiety disorder (social phobia)
In social anxiety disorder, the focus is on fear of being negatively evaluated.
Panic disorder
Acute stress disorder and posttraumatic stress disorder (PTSD)
Acute stress disorder and PTSD can be differentiated from agoraphobia by asking whether the fear, anxiety, or avoidance is related only to situations that remind the individual of a traumatic event.
If the fear, anxiety, or avoidance is restricted to reminders of trauma, and if the avoidance behavior does not extend to two or more agoraphobic situations, then agoraphobia should not be diagnosed.
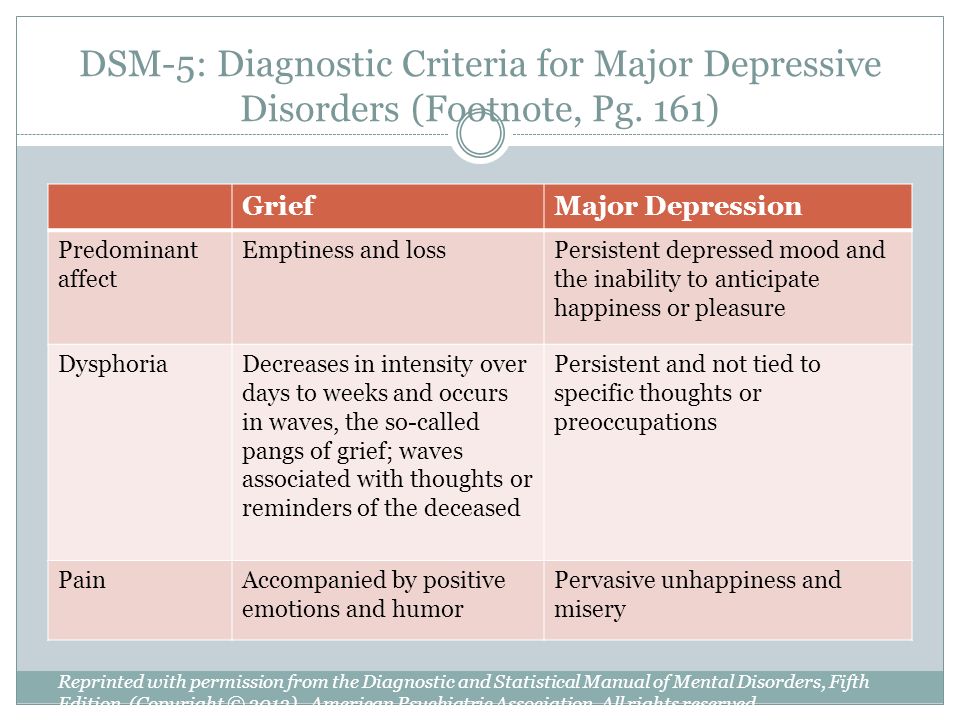
Major depressive disorder
In major depressive disorder, the individual may avoid leaving the home because of apathy, loss of energy, low self-esteem, and anhedonia.
 If the avoidance is unrelated to fears of panic-like or other incapacitating or embarrassing symptoms, then agoraphobia should not be diagnosed.
If the avoidance is unrelated to fears of panic-like or other incapacitating or embarrassing symptoms, then agoraphobia should not be diagnosed.
Other medical conditions
Agoraphobia is not diagnosed if the avoidance of situations is due to a physiological consequence of a medical condition, based on history, laboratory findings, and a physical examination. This includes medical conditions such as neurodegenerative disorders with motor symptoms (e.g. - Parkinson's disease, multiple sclerosis) and cardiovascular disorders.
Individuals with some medical conditions may avoid situations due to realistic concerns about being incapacitated (e.g. - fainting in transient ischemic attacks) or being embarrassed (e.g. - diarrhea in Crohn's disease). Thus, the diagnosis of agoraphobia should be given only when the fear or avoidance is clearly in excess of that usually associated with these medical conditions.
Investigations
Depending on the initial presenting symptoms (e.
 g. - dizziness, tachycardia), potential investigations can include: CBC, fasting glucose, fasting lipid profiles, electrolytes, liver enzymes, serum bilirubin, serum creatinine, urinalysis, urine toxicology for substance use, thyroid stimulating hormone (TSH).
g. - dizziness, tachycardia), potential investigations can include: CBC, fasting glucose, fasting lipid profiles, electrolytes, liver enzymes, serum bilirubin, serum creatinine, urinalysis, urine toxicology for substance use, thyroid stimulating hormone (TSH).An ECG and beta-HCG should be ordered if relevant.
Physical Exam
Treatment
See main article: Panic Disorder: Treatment
The treatment for agoraphobia is similar to treatment for panic disorder, as most studies have been done under the DSM-IV criteria (and agoraphobia was a subtype in panic disorder).
Guidelines
See also: Psychiatry Clinical Practice Guidelines (CPGs)
Resources
For Patients
AnxietyCanada: Patient Resources
For Providers
Articles
Research
References
1) American Psychiatric Association.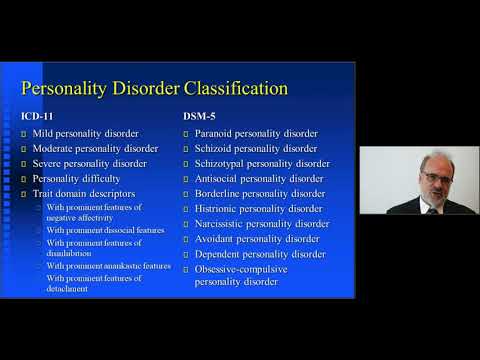 (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Arlington, VA.
(2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Arlington, VA.
2) American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Arlington, VA.
3) American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Arlington, VA.
4) American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Arlington, VA.
5) American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Arlington, VA.
6)Katzman, M. A., Bleau, P., Blier, P., Chokka, P., Kjernisted, K., & Van Ameringen, M. (2014). Canadian clinical practice guidelines for the management of anxiety, posttraumatic stress and obsessive-compulsive disorders. BMC psychiatry, 14(1), 1-83.
7)Bandelow, B.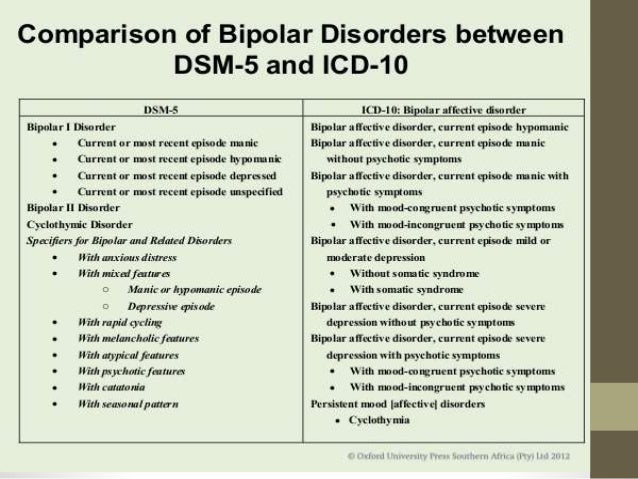 , Brunner, E., Broocks, A., Beinroth, D., Hajak, G., Pralle, L., & Rüther, E. (1998). The use of the Panic and Agoraphobia Scale in a clinical trial. Psychiatry Research, 77(1), 43-49.
, Brunner, E., Broocks, A., Beinroth, D., Hajak, G., Pralle, L., & Rüther, E. (1998). The use of the Panic and Agoraphobia Scale in a clinical trial. Psychiatry Research, 77(1), 43-49.
8)Katzman, M. A., Bleau, P., Blier, P., Chokka, P., Kjernisted, K., & Van Ameringen, M. (2014). Canadian clinical practice guidelines for the management of anxiety, posttraumatic stress and obsessive-compulsive disorders. BMC psychiatry, 14(1), 1-83.
Agoraphobia
Agoraphobia is a type of anxiety disorder. In essence, agoraphobia is the fear of being in public places, in open spaces where the person who has it assesses the situation as difficult to escape. For some people, it may be difficult to even leave the house, making everyday life difficult. While this mental illness can significantly impair quality of life, there is a positive side to it - diagnostic and treatment options are available. Read on if you want to know more about agoraphobia - what it is, what its potential causes are, how it's diagnosed, and what are the treatment options for this condition.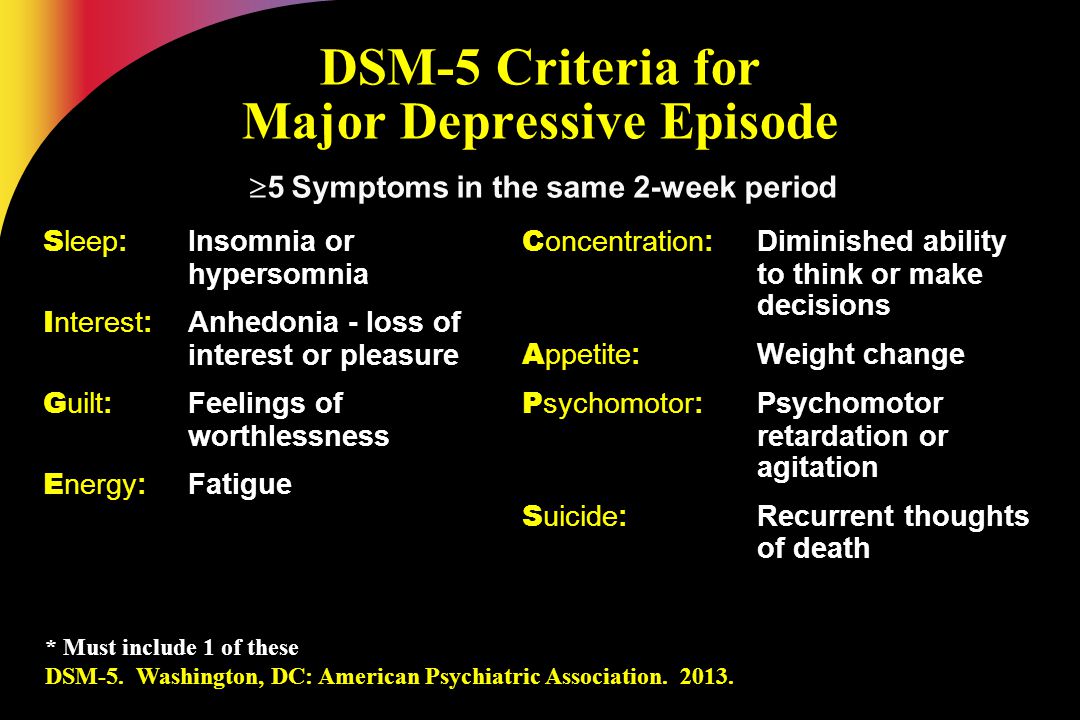 nine0003
nine0003
Definition of agoraphobia
Meaning of agoraphobia. The term "agoraphobia" comes from the Greek language, which means fear of the market. This means that the person suffering from agoraphobia is afraid to be in an open and crowded place (for example, in shops, crowds, restaurants, buses or trains, etc.).
Psychology of the definition of agoraphobia. According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), people with agoraphobia experience intense fear or anxiety caused by exposure to certain situations (anxiety can also be anticipatory). These situations can range from being in an open space such as a market, a bridge, a parking lot, to being on a bus, train, restaurant, cinema, theater, crowd anywhere, or even alone outside the home. Fear and anxiety then trigger other symptoms, such as irrational thoughts about getting trapped or avoiding certain situations.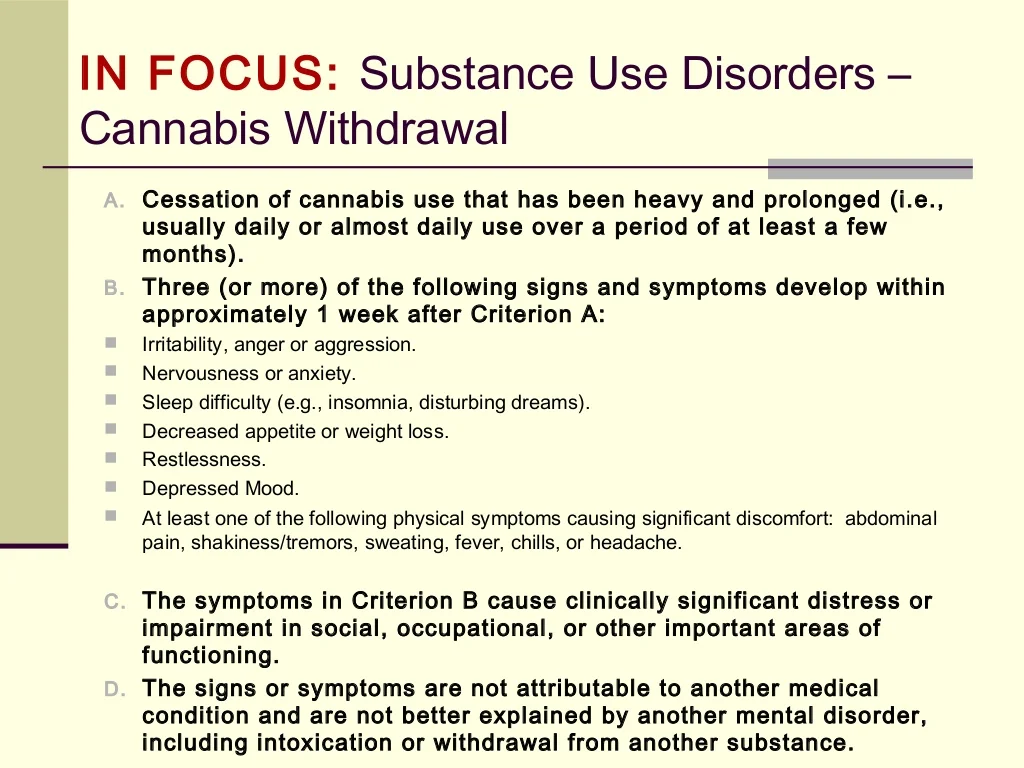 Simply put, agoraphobia is the fear of being alone in public places (the fear of agoraphobia). nine0003
Simply put, agoraphobia is the fear of being alone in public places (the fear of agoraphobia). nine0003
Before we delve into the topic of agoraphobia, let's first analyze what phobias are.
What is a phobia?
Phobias are strong irrational fear reactions. This means that a person suffering from a phobia (or multiple phobia) experiences a sense of panic when confronted with the source of their fear. This "trigger" can be a place, a situation, or a specific object (hence the diagnosis of a specific phobia noted in the DSM). Phobias share some similarities with generalized anxiety disorder, but the main difference is that phobias are always associated with a specific trigger or phobic object. nine0003
The fact that this irrational fear can be caused by something specific makes it difficult for people living with phobias to perform certain daily activities. This fear can vary in intensity and can go from annoying to actually turning off.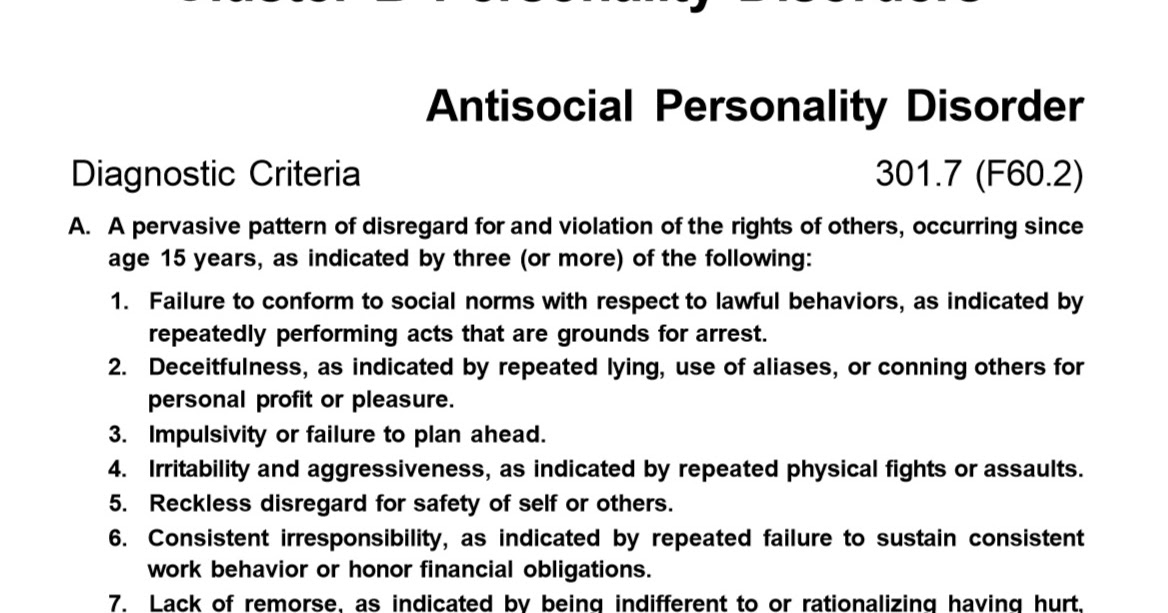
What causes a phobia?
This is the question that concerns everyone when they talk about phobias. We know that a phobia means a strong irrational fear when confronted with a phobic object, but when exactly does a needle, insect, public place, etc. become a trigger that can wreak havoc on someone's life? Apparently, there are some genetic and environmental factors that can lead to phobias. First, one of them may be a family member with an anxiety disorder. Experiencing stressful and/or traumatic events (such as drowning, being bitten by an insect, etc.) can also lead to a phobia. Exposure to certain environmental conditions, such as excessive height or small spaces, can also cause phobias (such as fear of heights or claustrophobia). Moreover, people with other psychiatric disorders, such as depressive disorders or substance use disorders, may be more likely to develop different types of phobias. nine0003
What are the symptoms of a phobia?
The main symptom of any phobia is fear and everything that fear entails in someone's nervous system.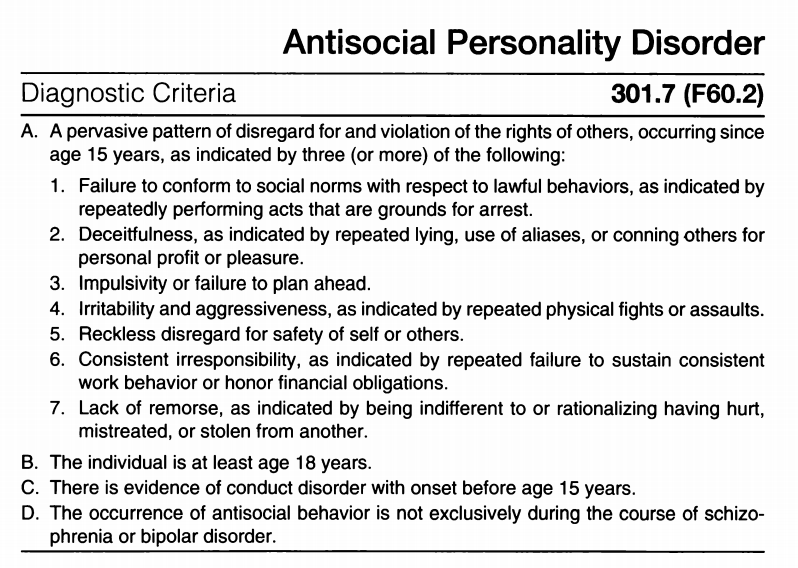 The most intense and common symptom of phobias is a panic attack, which will be detailed later in this article.
The most intense and common symptom of phobias is a panic attack, which will be detailed later in this article.
Types of phobia
There are many different types of phobias that correspond to the phobic object. Here are some of the most common:
- agoraphobia; nine0012
- social phobia - also known as social anxiety disorder; it is the fear of social interactions that may lead a person to self-isolate in order to avoid any social situation that may cause him to panic;
- glossophobia - fear experienced by someone speaking to an audience;
- claustrophobia - fear of close, enclosed, small spaces;
- acrophobia - fear of heights; nine0050
- homophobia - fear of injury or blood;
- arachnophobia - fear of spiders;
- cynophobia - fear of dogs;
- nyctophobia - fear of darkness or night (typical in childhood, but if it persists into adulthood, it is considered a phobia).
Although all of these can have a huge impact on a person's daily activities, agoraphobia remains a serious phobia that needs to be dealt with on your own. The fact that the DSM classification of anxiety disorders describes agoraphobia separately from specific phobias is a good indicator of the importance and severity of this mental health condition. nine0003
Symptoms of agoraphobia
People with agoraphobia tend to avoid situations or places that may cause them fear, anxiety, panic, helplessness or entrapment. Sometimes they may experience panic attacks. So what are the exact symptoms of agoraphobia? Some of these symptoms include:
- anxiety and fear;
- separation from others;
- fear of being alone or leaving the house;
- fear of being in difficult situations (for example, in a bus or elevator). nine0050
As we mentioned earlier, the symptoms caused by agoraphobia can also be accompanied by panic attacks.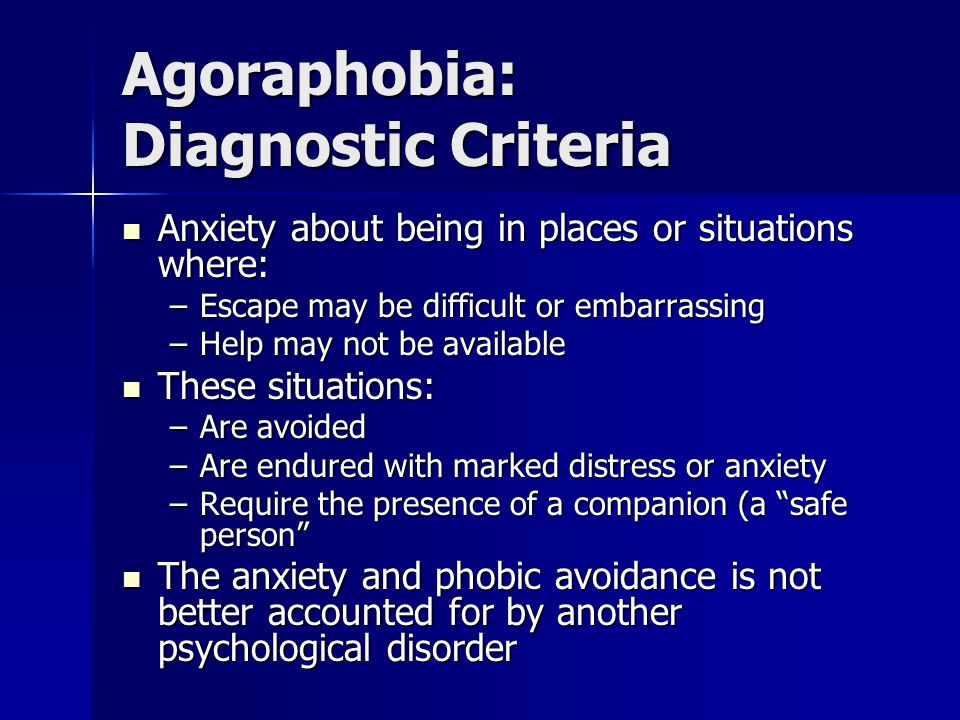 But what are panic attacks and why do we hear the term so often lately? Read on for answers to these questions.
But what are panic attacks and why do we hear the term so often lately? Read on for answers to these questions.
Panic attacks
What are panic attacks?
Panic attacks are episodes of sudden and intense fear when there is no real or even obvious danger that could justify a reaction. Some people experience only one or a few panic attacks in their lives, but others may have recurring episodes that can lead to panic disorder over time (we'll talk about this later in the article). It is also important to note that the intensity of a panic attack can be so high that people who experience it may develop a preemptive fear of panic attacks, meaning that they start avoiding certain situations or places just because they are afraid of provoking them. nine0003
What triggers a panic attack?
Although in most cases no specific cause of the panic attack has been found, in some other cases these episodes may be associated with other mental health conditions, meaning that they may be either a symptom or a consequence of them. Some of these conditions can be agoraphobia, other types of phobias, panic disorder, post-traumatic stress disorder (PTSD), or obsessive-compulsive disorder (OCD). nine0003
Some of these conditions can be agoraphobia, other types of phobias, panic disorder, post-traumatic stress disorder (PTSD), or obsessive-compulsive disorder (OCD). nine0003
What are the symptoms of a panic attack?
A panic attack occurs suddenly and without much warning. This means that in a person who experiences them, the nervous system of certain symptoms is suddenly excited, which correspond to the reaction of the body to danger. You've probably heard of the fight-flight-freeze reaction, right? Well, this is a prime example of such a response. The main thing to consider is that in the case of panic attacks, the threat is not obvious.
The symptoms of a panic attack come on gradually and reach their peak intensity about ten minutes after onset. Some of the most common symptoms of panic attacks include chest pain, difficulty breathing, hyperventilation, rapid heart rate (which is why many people think they are having a heart attack and may even seek medical attention), shaking, nausea, abdominal pain, dizziness , numbness, and a strong feeling that they are losing control or about to die. nine0003
Panic attacks are not medically life-threatening. However, they can mask really serious health problems, and given the similarity of symptoms to other serious illnesses (such as heart attacks), it's still important to see a doctor who can confirm that you don't really have a heart attack.
Who gets panic attacks?
As we mentioned earlier, panic attacks can sometimes occur on their own or they can be associated with an underlying mental illness, which means that people with a depressive disorder, an anxiety disorder, or a substance use disorder may also experience panic attacks. Women suffer more from panic attacks (this is also due to the fact that the prevalence of most of the disorders listed above is higher among women). In rare cases, children experience panic attacks, the frequency of which increases during puberty. In addition, prevalence is declining among the elderly. nine0003
Can panic attacks be cured?
Basically it all depends on the cause of your panic attacks. Whether they are related to another mental illness (such as agoraphobia, panic disorder, post-traumatic stress disorder, or OCD) or are isolated episodes, a healthcare professional will recommend a combination of psychotherapy, medication, and lifestyle changes. If left untreated and dealt with, panic attacks can lead to a strong anticipation of potential panic attacks and even a strong sense of fear experienced while in public places (i.e. Agoraphobia). Therefore, if you are experiencing panic attacks, do not hesitate to seek professional help to help you overcome your fears. nine0003
Now that we have briefly looked at one of the symptoms of agoraphobia, let's go back to this condition and begin to understand it more deeply.
Causes of agoraphobia
Unfortunately, the true cause of agoraphobia is not yet known. However, while agoraphobia can occur on its own, in most cases it is associated with an underlying mental illness.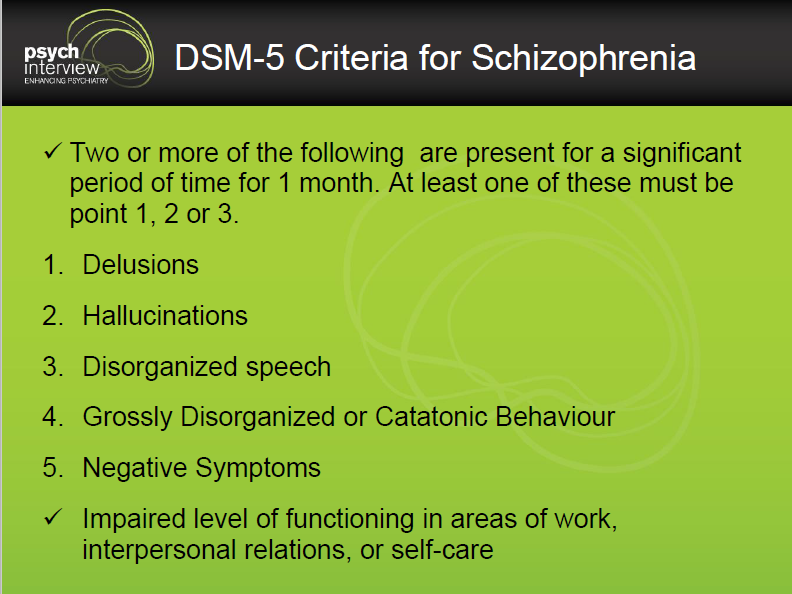 Some additional diagnoses for comorbidity with agoraphobia are anxiety disorders (eg, panic disorder, other phobias, social anxiety disorder), major depressive disorder, post-traumatic stress disorder, or substance use disorder (particularly alcohol). It is important to know that in the case of anxiety disorders, agoraphobia is more of a consequence or "later" addition to the list of symptoms, while in the case of depressive disorder and substance use disorder, agoraphobia is already present when the diagnosis is made. nine0003
Some additional diagnoses for comorbidity with agoraphobia are anxiety disorders (eg, panic disorder, other phobias, social anxiety disorder), major depressive disorder, post-traumatic stress disorder, or substance use disorder (particularly alcohol). It is important to know that in the case of anxiety disorders, agoraphobia is more of a consequence or "later" addition to the list of symptoms, while in the case of depressive disorder and substance use disorder, agoraphobia is already present when the diagnosis is made. nine0003
It is probably clear by now that agoraphobia is often associated with other underlying mental illnesses, the most common of which is panic disorder. You might be wondering what is panic disorder?
Agoraphobia with panic disorder.
According to the DSM, most people diagnosed with panic disorder report symptoms of agoraphobia before the onset of panic disorder. Panic disorder is a mental health condition that involves having recurring and unexpected panic attacks.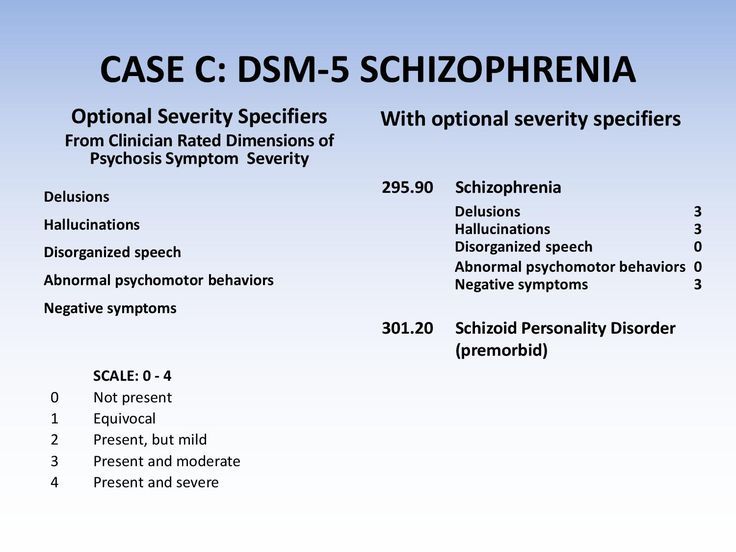 This means that a person who experiences more than one panic attack in a given period of time, and these attacks occur when there is no obvious trigger (such as when the person is trying to sleep - in which case they are called nocturnal panic attacks), then that person is amenable to diagnosis panic disorder. nine0003
This means that a person who experiences more than one panic attack in a given period of time, and these attacks occur when there is no obvious trigger (such as when the person is trying to sleep - in which case they are called nocturnal panic attacks), then that person is amenable to diagnosis panic disorder. nine0003
The frequency of panic attacks can vary greatly. This means that someone may have one panic attack per week for several months, or one panic attack every day for some time, followed by periods without panic attacks, or even two panic attacks per month for several years. Otherwise, the symptoms are very similar, but can also vary in intensity.
Given that panic disorder is basically multiple panic attacks occurring over a period of time, the exact cause of this disorder is not known. Some researchers have found genetic links, others have not. However, there is one aspect about which there seems to be some consensus, and that is that major life changes can cause panic attacks.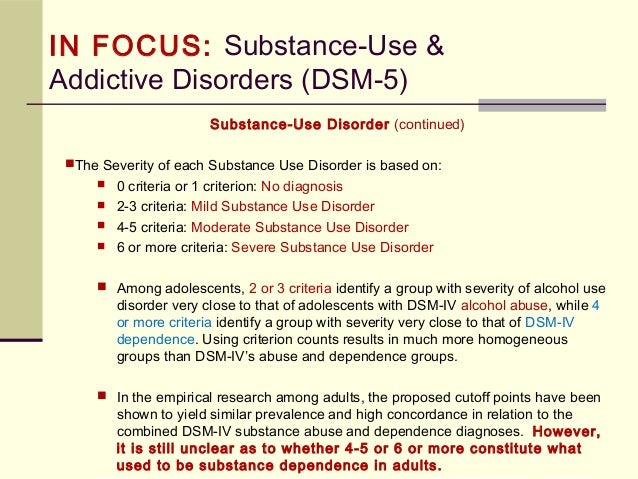 In terms of treatment options, psychotherapy, medications, and lifestyle changes can improve the outcome for a person with panic disorder. nine0003
In terms of treatment options, psychotherapy, medications, and lifestyle changes can improve the outcome for a person with panic disorder. nine0003
Risk factors for agoraphobia
There are some individual and environmental risk factors for agoraphobia. Some of them:
Pre-existing panic attacks or other types of phobias;
- high level of neuroticism;
- also testing anxiety hypersensitivity, that is, the belief that anxiety symptoms can harm oneself;
- experiencing stressful and/or traumatic events in childhood; nine0050
- development of a child in a strict or, on the contrary, overprotective family environment;
- having a family member with agoraphobia (agoraphobia is inherited in about 60% of cases).
Agoraphobia prevalence
Agoraphobia is more common in women than in men. Every year, this diagnosis is made in 1-2% of adolescents and adults. Although agoraphobia can also occur in childhood, it is rare and peaks in incidence are reached during adolescence and early adulthood—usually before age 35. nine0003
Although agoraphobia can also occur in childhood, it is rare and peaks in incidence are reached during adolescence and early adulthood—usually before age 35. nine0003
Diagnosis of agoraphobia
If you suspect that you meet the criteria for a diagnosis of agoraphobia, a psychiatrist will be the doctor who can further evaluate this. If your symptoms make it too difficult for you to go to a counseling session in person, you should know that there are doctors who can provide mental health counseling online so that they can adjust to your needs.
During a psychiatric consultation, the doctor will ask you about your symptoms: when they first appeared, how often they occur, how intense they are and in what situations they occur. In addition, they will also ask you about the medical history of you and your family. Considering the intensity of the physical symptoms of agoraphobia, your doctor may also indicate the need for blood tests and regular medical consultation to rule out any physical conditions that may be causing your symptoms.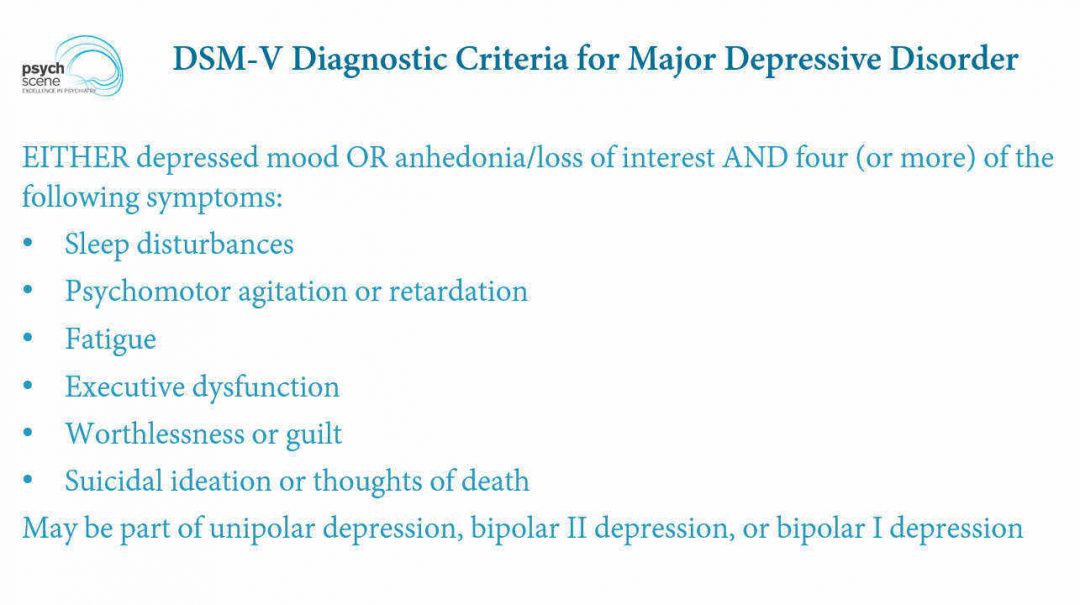 nine0003
nine0003
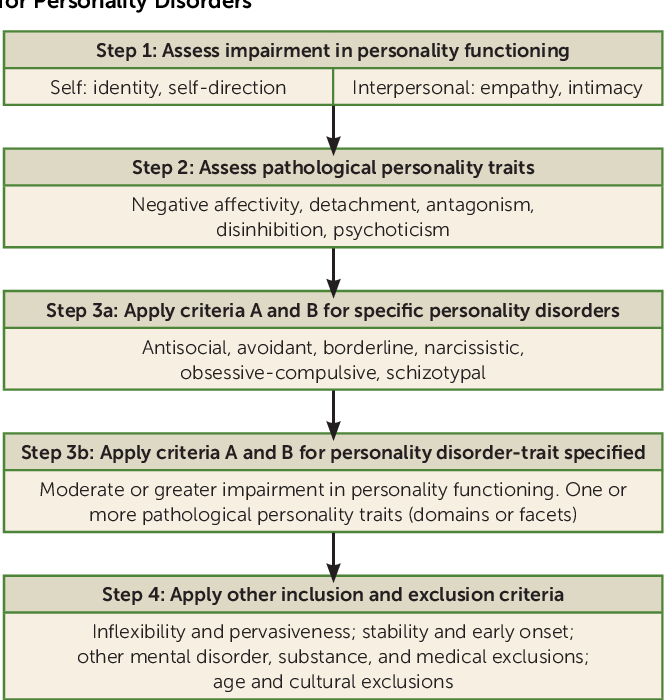
To make a diagnosis of agoraphobia, the DSM provides a list of criteria that you need to check. The DSM is a guideline for diagnosing a mental health condition written by the American Psychiatric Association, so it is mainly used in the US and some other countries. There is another guide, ICD - International Classification of Diseases, developed by the World Health Organization, which can also offer criteria for diagnosing agoraphobia. In this article, we will focus on the criteria listed by the American Psychiatric Association in the DSM for diagnosing agoraphobia. nine0003
According to the DSM, in order to be diagnosed with agoraphobia, you must first experience extreme anxiety and fear in two or more of these situations: using public transportation (such as a bus), being in an open space (such as a market), being in enclosed spaces (such as in an elevator), being in a crowd, or being alone outside the home. The next criterion states that the person in question avoids public and open spaces due to the irrational thought that he will not be helped to escape if something happens to him.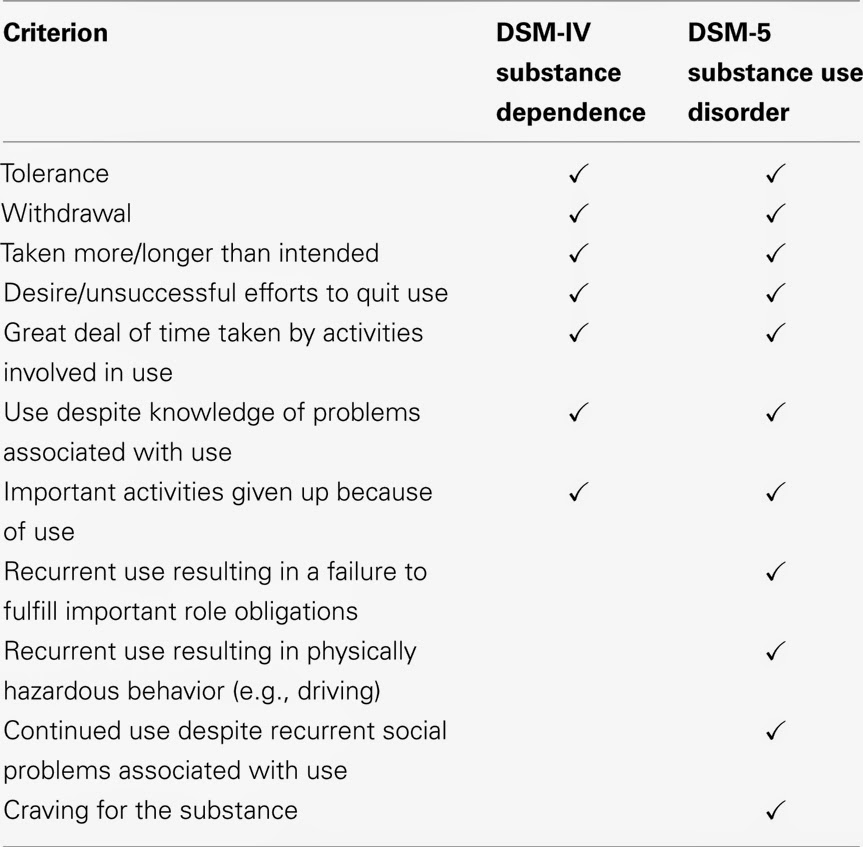 In addition, a person may require someone to accompany him in public places, and his fear cannot be justified by a real, obvious threat or danger. Moreover, this fear must be present for at least six months. nine0003
In addition, a person may require someone to accompany him in public places, and his fear cannot be justified by a real, obvious threat or danger. Moreover, this fear must be present for at least six months. nine0003
We also talked a lot about agoraphobia with panic disorder. It is important to know that although one of the symptoms of agoraphobia is panic attacks, and this condition can be combined with panic disorder, they can also occur individually. Therefore, whoever sets the criteria for both conditions should receive a dual diagnosis and receive a treatment plan according to their symptoms and signs.
As for the tests that can be used to detect agoraphobia, they are not as well studied as we would like. However, there are several tests that can measure the intensity of your symptoms that may be helpful to your doctor in deciding the best course of action. However, be aware that tests found on the Internet are not reliable and that a good test must be tested on different populations before it can give a good, credible result (agoraphobia test).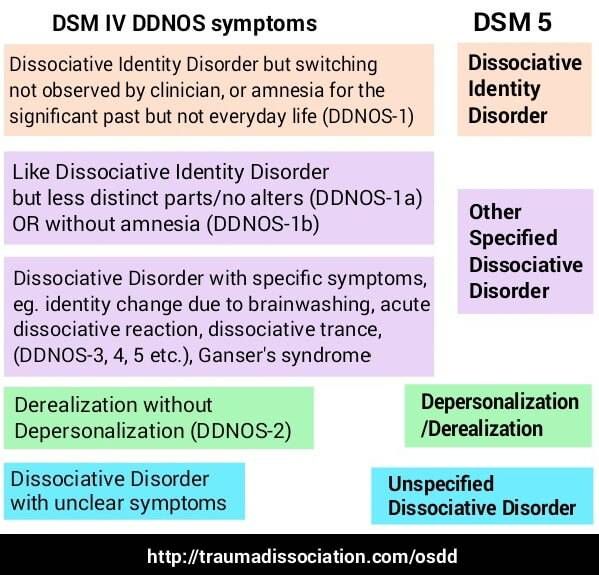 Therefore, if you suspect that you have agoraphobia, it is better to make an appointment with a professional than to take an online survey that cannot fully assess your situation. nine0003
Therefore, if you suspect that you have agoraphobia, it is better to make an appointment with a professional than to take an online survey that cannot fully assess your situation. nine0003
Treatment of agoraphobia
As with panic attacks, agoraphobia can be treated with psychotherapy, medication and lifestyle changes. However, it is likely that you will get the most benefit from their combination. Let's take a look at what these treatment options can do.
- Psychotherapy. This requires regular sessions with a psychotherapist who can help you better manage your symptoms as well as better understand their causes. For best results, therapy is usually recommended at the same time as prescription medications. In terms of different types of psychotherapy, cognitive behavioral therapy (CBT) has proven to be the most effective in treating phobias, and thus agoraphobia. The point of this type of therapy is to help you understand the thoughts and feelings you are experiencing and then seek to improve your symptoms by changing your perspective on the disorder itself.
 Basically, it takes your disordered, distorted thoughts and turns them into healthy and constructive thoughts that help you regain control. Another type of therapy used in the treatment of phobias is exposure therapy, which means that you will gradually be exposed to situations and places that you fear. This can be done in the presence of a therapist and with his help. However, this can be quite difficult for some people, which is why some avoid this type of therapy. Ideally, if the therapy (and medication) works, exposure will eventually become a way to regain control of your life. nine0050
Basically, it takes your disordered, distorted thoughts and turns them into healthy and constructive thoughts that help you regain control. Another type of therapy used in the treatment of phobias is exposure therapy, which means that you will gradually be exposed to situations and places that you fear. This can be done in the presence of a therapist and with his help. However, this can be quite difficult for some people, which is why some avoid this type of therapy. Ideally, if the therapy (and medication) works, exposure will eventually become a way to regain control of your life. nine0050 - Medicines. SSRIs (Selective Serotonin Reuptake Inhibitors) such as Prozac or antidepressants and anti-anxiety medications (eg Xanax) are usually prescribed in this case. They are intended to relieve the symptoms of agoraphobia and especially panic attacks. It is important to remember that drugs do not eliminate the cause of the disorder, but eliminate its symptoms, while therapy can help with the cause.
- Lifestyle changes. Although they do not cure agoraphobia, they can help create a more relaxing environment in which you feel more comfortable and less anxious. Physical exercise, a good and healthy diet, and the practice of meditation can improve your overall well-being. nine0050
Conclusion
Agoraphobia is a mental health condition that can seriously impair the quality of life. Somatic symptoms as well as cognitive symptoms can interfere with the daily activities of a person with this type of phobia. Luckily, there are treatment options and professionals available to help anyone in need, so if you suspect you have agoraphobia (or any other mental illness), feel free to research and ask for help from a healthcare professional. The best thing you can do is take care of yourself, and sometimes that means asking for help. nine0003
Clinical features of the combination of agoraphobia and non-psychotic mental disorders | Kovalev
Introduction
Russian and English articles were searched in the databases ELibrary.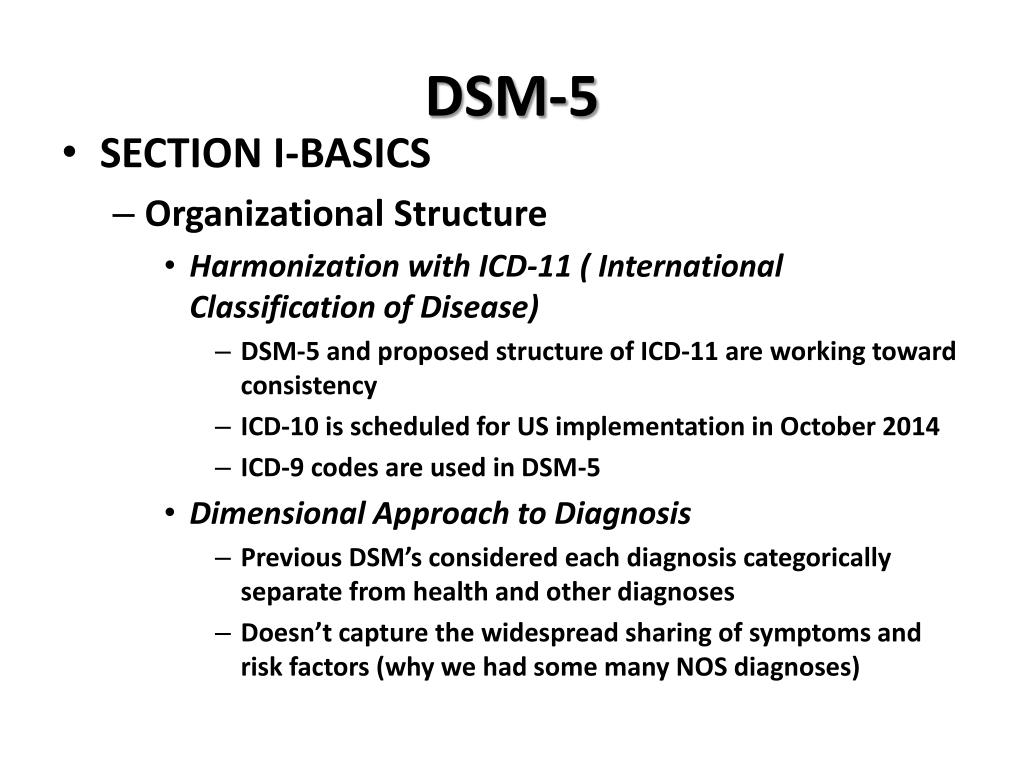 ru, Web of Science, Scopus, Clinical Case, PubMed, Cochrane Database of Systematic Reviews. Articles were searched using the keywords "agoraphobia", "anxiety disorders", "borderline mental disorders". Inclusion criteria — full-text articles in Russian and English, original research, Cochrane reviews, clinical observations, publication date from 1994 to 2020 Exclusion criteria - abstracts, abstracts, publication date before 1994. A total of 734 publications were found. 43 publications met the inclusion/exclusion criteria.
ru, Web of Science, Scopus, Clinical Case, PubMed, Cochrane Database of Systematic Reviews. Articles were searched using the keywords "agoraphobia", "anxiety disorders", "borderline mental disorders". Inclusion criteria — full-text articles in Russian and English, original research, Cochrane reviews, clinical observations, publication date from 1994 to 2020 Exclusion criteria - abstracts, abstracts, publication date before 1994. A total of 734 publications were found. 43 publications met the inclusion/exclusion criteria.
Agoraphobia is a disorder characterized by the appearance of fear when the patient is in open space or in crowded places (shops, bus stops) with the subsequent formation of behavior to avoid situations that caused fear. According to the classification given in the ICD-10, it can be divided into two groups: agoraphobia without anamnestic data for panic disorder and panic disorder with agoraphobia (ICD-10). Some researchers distinguish agoraphobia with early and late (after 65 years) onset [1].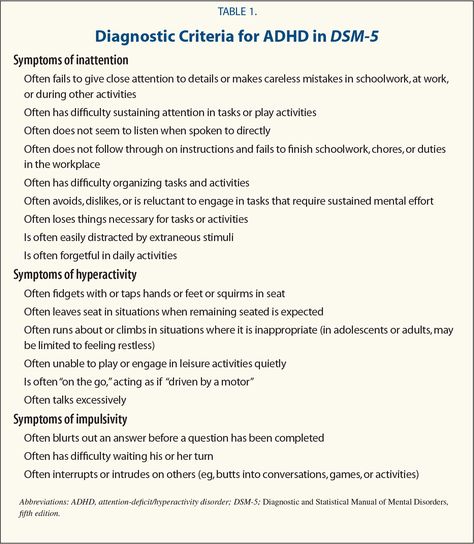 nine0003
nine0003
The prevalence of panic disorder is estimated at about 2% of the population per year, or about 2–5% of the population during a lifetime [2][3]. Among these patients, one-third to one-half have agoraphobic symptoms, although the percentage is even higher in clinical samples [4]. Such a fairly high percentage of agoraphobia in the population makes this topic relevant for research.
The results of recent studies show a comorbidity between agoraphobia and other anxiety spectrum disorders. In particular, agoraphobia occurs in 0.8% of people who have had a panic attack, in 1.1% with panic disorder [2]. It has also been shown that a third of patients with panic disorder and major depressive disorder develop agoraphobia [5]. nine0003
It is important to note that comorbidity increases the severity of the disease and reduces the effectiveness of the treatment. The nosologies listed above are combined into a group of borderline mental disorders that have a high percentage of occurrence in the population [6]. Some of them, in particular PTSD (post-traumatic stress disorder), may be factors that shape the development of agoraphobia, so it is important to strive to reduce the prevalence of these nosologies [7].
Some of them, in particular PTSD (post-traumatic stress disorder), may be factors that shape the development of agoraphobia, so it is important to strive to reduce the prevalence of these nosologies [7].
Another factor in the importance of work in this direction is the fact that agoraphobia significantly aggravates the course of panic disorder and worsens the quality of life of patients, assessed on the SF-36 scale [8]. nine0003
Taking into account the prevalence of the disease and the decrease in the quality of life in patients, the selection of effective therapy for panic-agoraphobic states plays an important role [9][10].
Panic attacks and panic disorder as the basis for the formation of agoraphobic symptoms
It can be said that the position of agoraphobia as a separate nosology was very "shaky" for a long time. In particular, there was a question about the secondary formation of agoraphobia in relation to panic disorder. Or is it a separate nosological unit, as it was originally indicated in the ICD? nine0258 ) .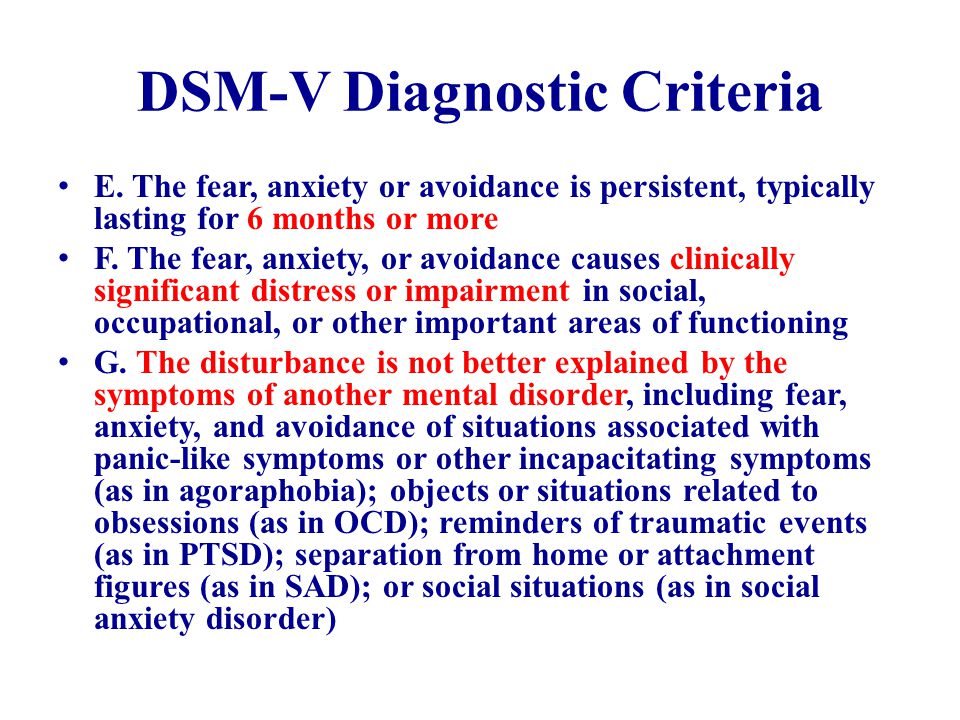 Subsequently, agoraphobia was included in the ICD-9 as an independent syndrome, manifested by multiple fears, and in the ICD-10 it occupies the same status (ICD-10, 1995).
Subsequently, agoraphobia was included in the ICD-9 as an independent syndrome, manifested by multiple fears, and in the ICD-10 it occupies the same status (ICD-10, 1995).
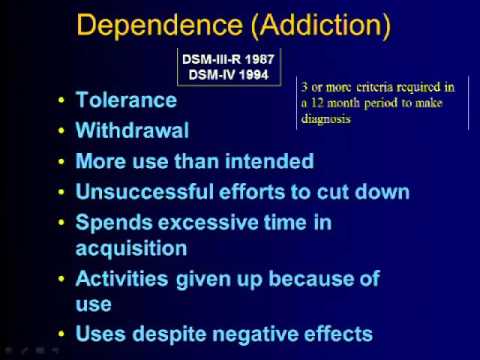
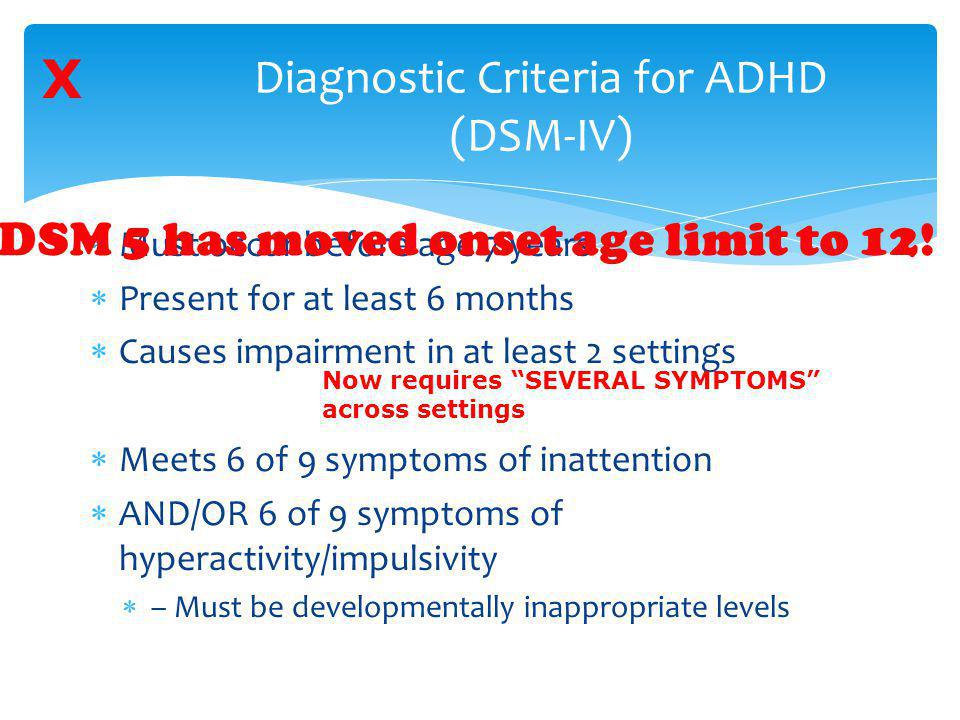
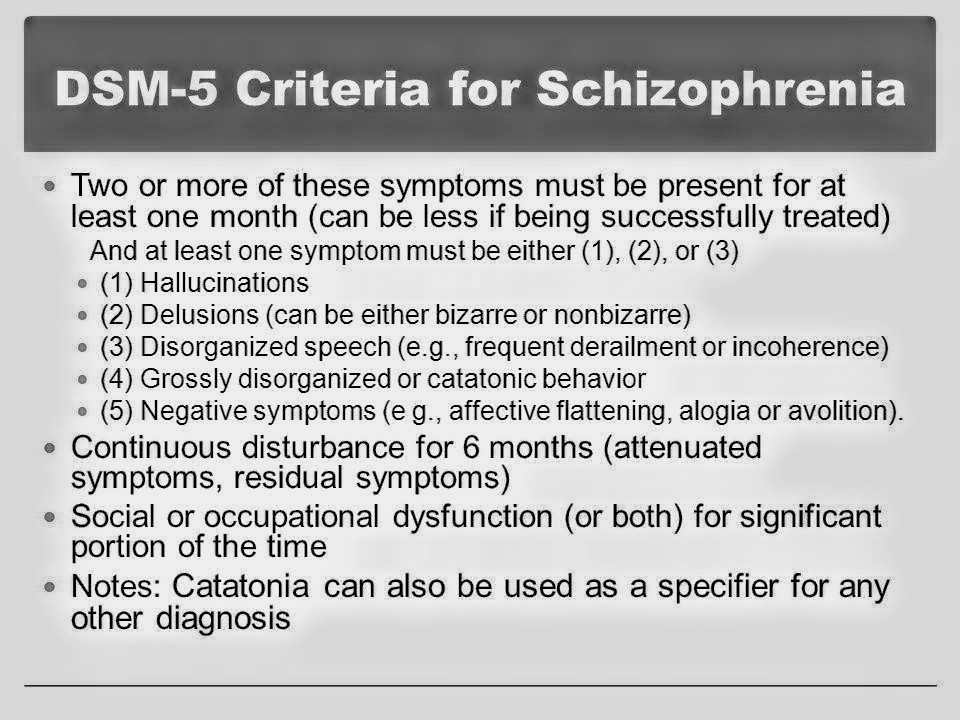
In the United States, where the DSM is the main system for classifying mental disorders, agoraphobia is defined as “a feeling of fear with avoidant behavior that develops when one or among people is in places from which it is difficult to get out or get medical help in an emergency situation.” It can be said that this definition is similar to the definition of panic disorder and the definition of agoraphobia given in ICD-10. However, the DSM definition of agoraphobia is closer to panic disorder than to phobias. Agoraphobia with panic attacks should be coded as its initial phase, when there are recurrent panic attacks, which in turn leads to the development of fear of such an attack and, accordingly, the avoidance of situations and places that can provoke such an attack. If there is no history of panic attacks, then the diagnosis is agoraphobia without panic attacks, but according to the DSM, avoidance behavior is required to be the result of anxiety about the development of a panic attack, that is, in any case, an association is indicated between a panic disorder or attack and agoraphobia , which is the difference between this classification and ICD-10.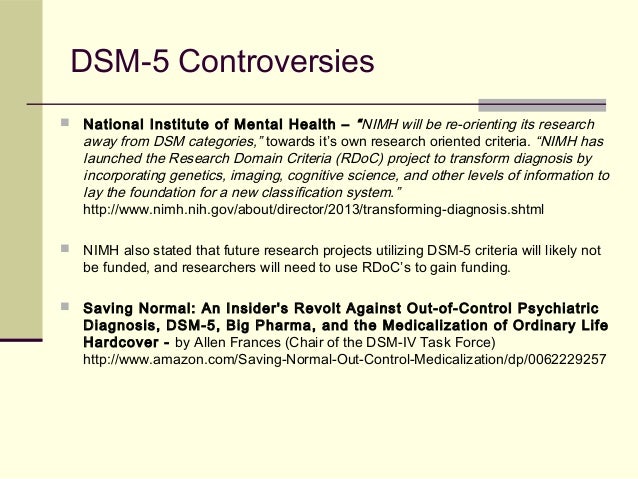 Thus, with the DSM-III-R, agoraphobia was defined as a response to situations in which a panic attack occurred. However, the evolution of subsequent revisions of the DSM has been towards greater acceptance of agoraphobia outside of the construct of panic attacks or panic disorder. The DSM-V classification, released in 2013, has undergone significant changes to the heading of anxiety disorders, including agoraphobia and panic disorder. In particular, they were divided into two separate diagnoses, that is, when formulating a diagnosis, two different codes should be used. It can be said that the diagnostic criteria for agoraphobia have undergone only minor changes. In particular, it is necessary to confirm the occurrence of fear in two or more situations in order to exclude other phobias (APA, 2013). nine0003
Thus, with the DSM-III-R, agoraphobia was defined as a response to situations in which a panic attack occurred. However, the evolution of subsequent revisions of the DSM has been towards greater acceptance of agoraphobia outside of the construct of panic attacks or panic disorder. The DSM-V classification, released in 2013, has undergone significant changes to the heading of anxiety disorders, including agoraphobia and panic disorder. In particular, they were divided into two separate diagnoses, that is, when formulating a diagnosis, two different codes should be used. It can be said that the diagnostic criteria for agoraphobia have undergone only minor changes. In particular, it is necessary to confirm the occurrence of fear in two or more situations in order to exclude other phobias (APA, 2013). nine0003
Panic disorder is a chronic disease, resulting in patients requiring long-term therapy [11]. At the same time, agoraphobia has been shown to be a predictor of poor outcome in individuals with panic disorder [11].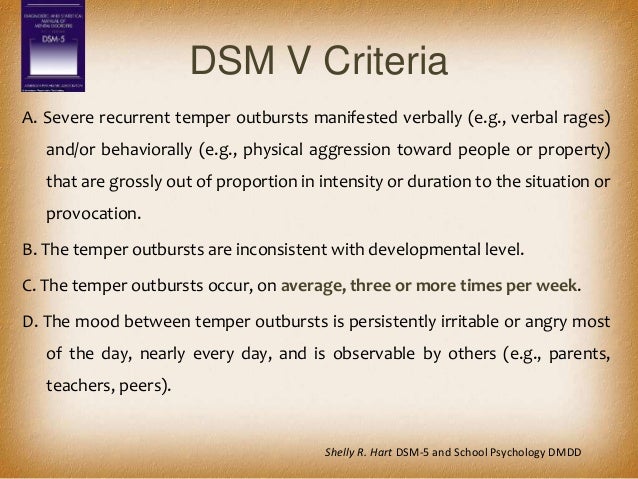 The presence of agoraphobia in such patients exacerbates the clinical course of panic disorder and increases the likelihood of having one or more comorbid psychiatric disorders compared with patients with panic disorder but without agoraphobia. It has been shown that after a panic attack, 37% of patients exhibit moderate avoidance behavior, with 81% of these patients developing such behavior in less than a year [12]. Researchers have identified risk factors that increase the risk of developing agoraphobic symptoms, such as early age at onset of panic attacks [13], female gender [14], and belonging of the underlying disease to the anxiety spectrum group [12]. According to the data of domestic researchers, the predominant sex of patients with panic disorder and agoraphobia is female, and the age of the onset of the disease is 21–30 (32.4%) and 31–40 (35.3%) years, which corresponds to the data of foreign scientists [15 ]. nine0003
The presence of agoraphobia in such patients exacerbates the clinical course of panic disorder and increases the likelihood of having one or more comorbid psychiatric disorders compared with patients with panic disorder but without agoraphobia. It has been shown that after a panic attack, 37% of patients exhibit moderate avoidance behavior, with 81% of these patients developing such behavior in less than a year [12]. Researchers have identified risk factors that increase the risk of developing agoraphobic symptoms, such as early age at onset of panic attacks [13], female gender [14], and belonging of the underlying disease to the anxiety spectrum group [12]. According to the data of domestic researchers, the predominant sex of patients with panic disorder and agoraphobia is female, and the age of the onset of the disease is 21–30 (32.4%) and 31–40 (35.3%) years, which corresponds to the data of foreign scientists [15 ]. nine0003
Features of the clinical picture of anxiety spectrum disorders in combination with agoraphobia
Generalized anxiety disorder is a mental pathology that demonstrates a high degree of comorbidity with other nosologies. In particular, it has been shown that the lifetime incidence of major depressive disorder in generalized anxiety disorder is 62.4%, agoraphobia is 25.7%, and panic disorder is 23.5% [16]. nine0003
In particular, it has been shown that the lifetime incidence of major depressive disorder in generalized anxiety disorder is 62.4%, agoraphobia is 25.7%, and panic disorder is 23.5% [16]. nine0003
Domestic studies have shown the comorbidity of agoraphobia and somato-vegetative type of generalized anxiety disorder, which is manifested by short-term somatized anxiety reactions during the day 1 . Among other disorders that are comorbid with anxiety disorder, of interest is irritable bowel syndrome, which leads to the development of agoraphobia. This is due to the fact that patients are afraid to experience the manifestations of this syndrome in public, which forms avoidant behavior [17]. nine0003
The impact of agoraphobia on the course of depressive disorders
Studies have shown that the comorbidity of depression and panic disorder with agoraphobia is associated with increased anxiety, hypochondria, feelings of “inadequacy”, social isolation, as well as with treatment failure, difficulties in psychosocial rehabilitation, and an increase in the frequency of hospitalization [ eighteen]. Also, the severity of depressive symptoms (feelings of guilt, hopelessness) increases in the presence of panic disorder with agoraphobia [19]. Sareen J. et al., 2005 [20] showed that panic disorder with agoraphobia is associated with a history of suicide attempts. This is very important because a history of a suicide attempt is regarded as a predictor of further suicide attempts. Some researchers believed that the presence of a suicide attempt in patients suffering from major depressive disorder is not associated with the presence of panic disorder, since the presence of anxiety, hypochondria was regarded as a protective factor against suicidal behavior, since these patients were more afraid of death [21]. Other researchers believed that there is a link between psychomotor agitation and suicidal ideation, which contradicts the hypothesis of anxiety as a protective factor against suicide [22]. The key point in these hypotheses is the existence of a link between depressive and anxiety spectrum disorders.
Also, the severity of depressive symptoms (feelings of guilt, hopelessness) increases in the presence of panic disorder with agoraphobia [19]. Sareen J. et al., 2005 [20] showed that panic disorder with agoraphobia is associated with a history of suicide attempts. This is very important because a history of a suicide attempt is regarded as a predictor of further suicide attempts. Some researchers believed that the presence of a suicide attempt in patients suffering from major depressive disorder is not associated with the presence of panic disorder, since the presence of anxiety, hypochondria was regarded as a protective factor against suicidal behavior, since these patients were more afraid of death [21]. Other researchers believed that there is a link between psychomotor agitation and suicidal ideation, which contradicts the hypothesis of anxiety as a protective factor against suicide [22]. The key point in these hypotheses is the existence of a link between depressive and anxiety spectrum disorders. nine0003
nine0003
It has been studied for a long time what factors associated with panic-agoraphobic symptoms can lead to an increased risk of suicidal behavior, in addition to the influence of depression. Patients with comorbidity of anxiety and depression may commit suicide more often than patients without anxiety, as this is a way to get rid of the symptoms that worry them [20]. Panic attacks during depression significantly impair social functioning, which in turn can lead to suicidal ideation. nine0003
It should be noted that there is an inverse effect of depression on agoraphobia, in particular, there is an increase in the severity of phobic symptoms [23].
Thus, there is a complex pathogenetic relationship between panic-agoraphobic symptoms and depression. In this regard, the study of this issue is very important, as it will help reduce the likelihood of suicidal behavior.
PTSD as an etiological factor in agoraphobia
Studies have shown a high comorbidity between panic disorder and PTSD.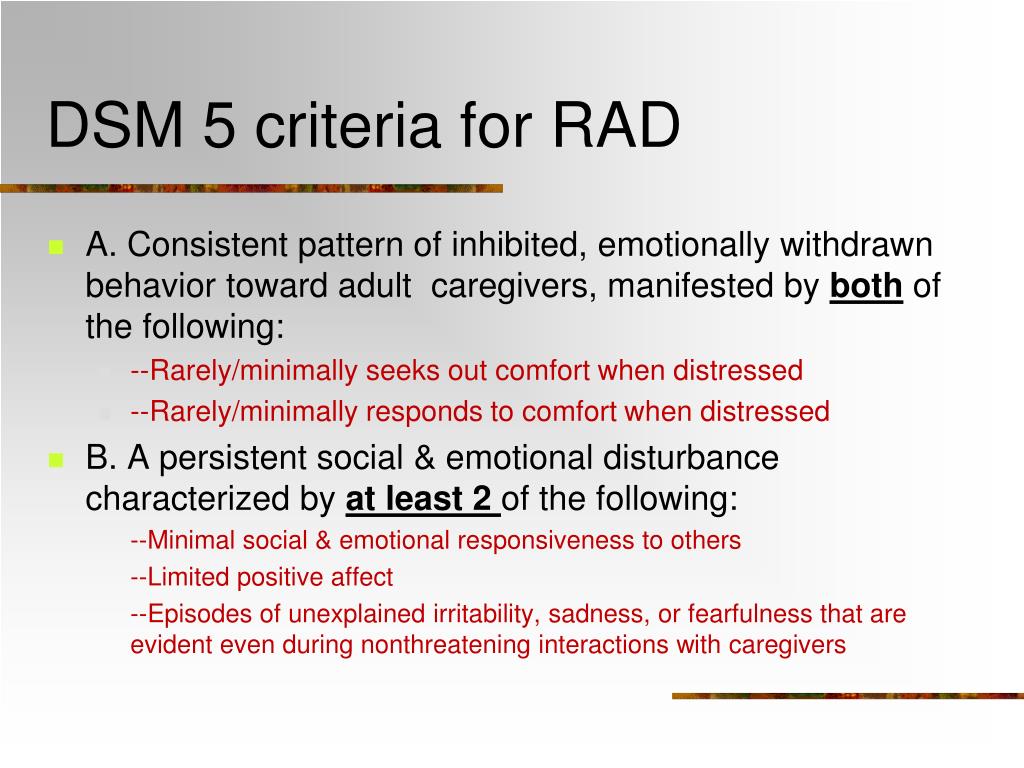 Thus, panic disorder occurs in 7.3-18.6% of men and 12.6-17.5% of women suffering from PTSD [24]. More recent studies have shown that 35% of patients with PTSD experienced panic attacks within a year, leading to increased comorbidity with other anxiety spectrum disorders and impaired social functioning [25]. nine0003
Thus, panic disorder occurs in 7.3-18.6% of men and 12.6-17.5% of women suffering from PTSD [24]. More recent studies have shown that 35% of patients with PTSD experienced panic attacks within a year, leading to increased comorbidity with other anxiety spectrum disorders and impaired social functioning [25]. nine0003
The relationship between PTSD and panic disorder is emphasized in connection with the emergence of a circular model of the development of fear, which postulates a similar etiology of anxiety disorders based on this emotion [26]. Applying this hypothesis to PTSD and panic disorder, we can say that in a situation that triggers a reminder of a physical threat, a person experiences tachypnea, heart pain and fear of death. The hypothesis of the circular formation of a feeling of fear is in good agreement with the assumption that panic during a traumatic event becomes part of a conditioned reflex that can start at a certain moment, demonstrating the above symptoms [27]. In this case, agoraphobic symptoms can form, when patients avoid those places that cause a panic attack and experience anxiety about its likely development [13].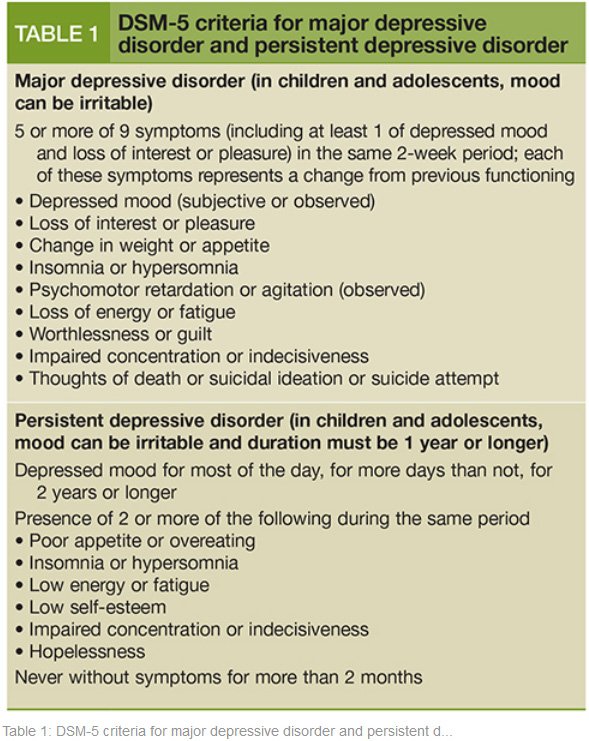 nine0003
nine0003
The influence of personality disorders on the clinical picture of agoraphobia
Understanding how personality traits are associated with the onset of panic disorder and agoraphobia is an important step in understanding the etiology of the latter. Researchers have shown that cluster C (“anxiety” group) of psychopathy, especially avoidant and dependent, are associated with anxiety disorders, in particular with panic disorder and agoraphobia [28]. It should be noted that some researchers dispute the view that these types of personality disorders are predisposing factors for panic disorder and agoraphobia, based on retrospective data on the premorbid personality structure of patients with anxiety disorders. Other researchers believe that in the early stages of the course of a panic disorder, the symptoms of the disease cannot affect the deformation of the personality [29]. This point of view can be supported by the fact that effective treatment of panic disorder and agoraphobia can neutralize pathocharacterological personality traits [30].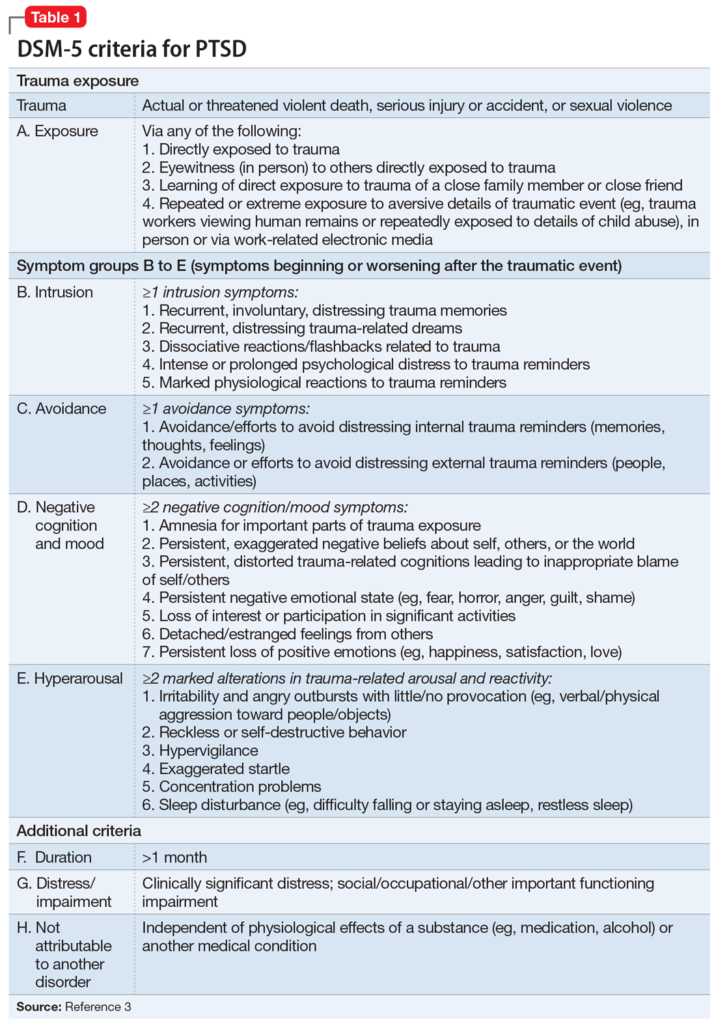
It is known that the personal characteristics of patients can have a significant impact on the prognosis of therapy. Thus, in the study by M. Ozkan and A. Altindag, 2005 [31] it was shown that those patients in whom characterological features reach the severity of psychopathic, panic disorder is characterized by a more severe course, agoraphobic symptoms are more often associated, and the risk of suicide is higher. nine0003
Among the factors that form personality, in addition to genetically determined personality traits, education plays an important role. Domestic researchers have shown that a disharmonious type of upbringing was very often applied to patients with agoraphobia. The most common style is “hyperresponsibility and hyperprotection” (50.98%), which correlates with social anxiety and social phobia. The next most common (24.11%) parenting style was "Cinderella", as a result of which patients have a complex of guilt and addiction, and the ban on the manifestation of negative emotions led to somatization of anxiety 2 .
Influence of the type of hypochondria on the dynamics of agoraphobia
After a panic attack, patients often develop anxiety in anticipation of a second attack, which is updated if it is necessary to stay in a situation that can trigger a phobic reaction (anxiety, a feeling of tension in the body, tachycardia, shortness of breath). These manifestations could be accompanied by the development of hypochondriacal disorders. Fear for health was in the nature of obsessive hypochondria with an understanding of the morbidity and groundlessness of the phobia and the fight against it, but sometimes hypochondria can take on the character of overvalued. The latter option is distinguished by the absence of a critical attitude to one's condition [18]. nine0003
In the work of I. B. Poze 3 it was also found that all patients suffering from agoraphobia have comorbidity with hypochondriacal disorders: from the degree of fixation to obsessive nature. Neurotic hypochondria was characterized by the specificity of nosophobia with somato-vegetative manifestations. The clinical picture was characterized by a change of syndromes, such as hypochondriacal manifestations and pathocharacteristic changes in personality overlapped the picture of phobia. Subsequently, the clinic of neurotic development was determined by a complex obsessive-phobic and hypochondriacal complex. Interestingly, according to the results of this work, it was revealed that the overvalued type of hypochondriacal disorders was formed in patients with personality disorders. So, in anxiety, anancaste and dependent personality disorders, hypochondriacal development was revealed with an accentuation of perfectionism, a change in priorities and values, and a “break in the life curve”. The hysterical personality showed a more favorable course. There was a partial reduction of hypochondria with the restoration of the previous level of functioning. Thus, we can say that the presence of a hysterical radical in the personality structure is prognostically favorable, while an anacastic, anxious and dependent one is unfavorable.
The clinical picture was characterized by a change of syndromes, such as hypochondriacal manifestations and pathocharacteristic changes in personality overlapped the picture of phobia. Subsequently, the clinic of neurotic development was determined by a complex obsessive-phobic and hypochondriacal complex. Interestingly, according to the results of this work, it was revealed that the overvalued type of hypochondriacal disorders was formed in patients with personality disorders. So, in anxiety, anancaste and dependent personality disorders, hypochondriacal development was revealed with an accentuation of perfectionism, a change in priorities and values, and a “break in the life curve”. The hysterical personality showed a more favorable course. There was a partial reduction of hypochondria with the restoration of the previous level of functioning. Thus, we can say that the presence of a hysterical radical in the personality structure is prognostically favorable, while an anacastic, anxious and dependent one is unfavorable. At the same time, the clinical picture of hypochondria determines the dynamics of the course of agoraphobia. With neurotic hypochondria, long-term remissions without psychopathological disorders were observed, and with overvalued hypochondria, a continuous course with generalization and complication of the clinical picture due to the formation of comorbid relationships was observed. nine0003
At the same time, the clinical picture of hypochondria determines the dynamics of the course of agoraphobia. With neurotic hypochondria, long-term remissions without psychopathological disorders were observed, and with overvalued hypochondria, a continuous course with generalization and complication of the clinical picture due to the formation of comorbid relationships was observed. nine0003
Research in this direction abroad took place in the eighties. Hypochondria was seen as a somatic manifestation of a violation of self-perception, and agoraphobia as a defensive reaction and an attempt to restore a disturbed self-perception. It has also been shown that patients can endure panic attacks earlier without understanding their psychological etiology, but that they may be the key moment in the formation of hypochondria or an anxious temperament.
Agoraphobia as part of sluggish schizophrenia
Although most of the study of the comorbidity of anxiety disorders and schizophrenia dates back to the early years of the nosological approach in psychiatry, for a long time this topic was ignored by both clinicians and researchers [32].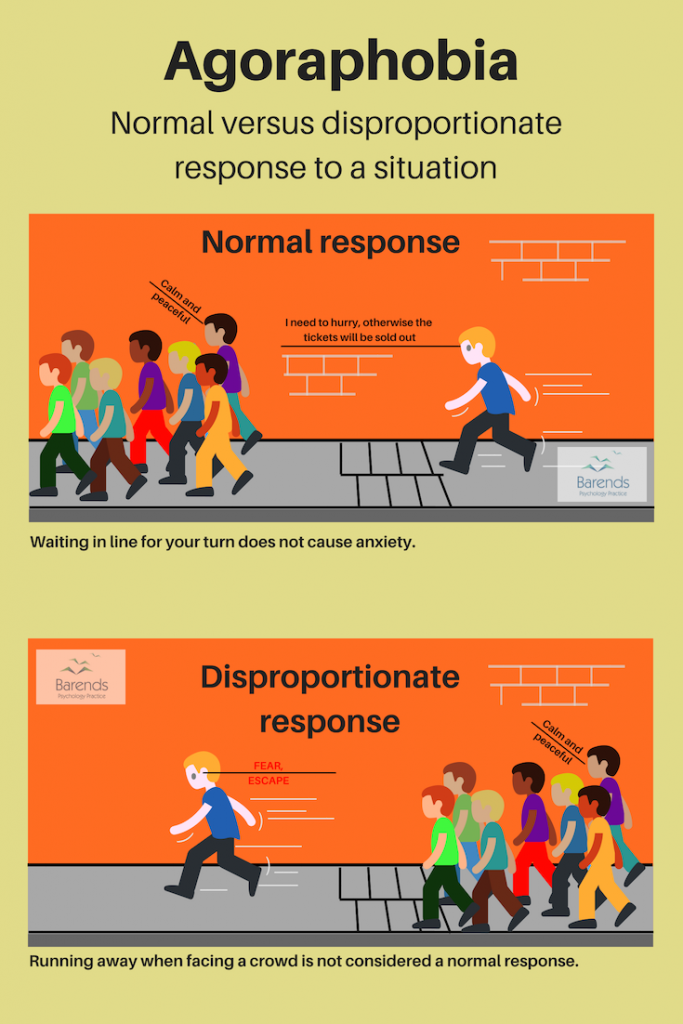 This was probably due to the fact that for a long time in the DSM diagnostic criteria it was indicated that an anxiety spectrum disorder can be diagnosed if there is no connection with the disorder of the first axis, in particular schizophrenia, which led to a low diagnosis of this nosology in patients with schizophrenia. [33]. However, with the advent of the DSM-III-R, the diagnosis of comorbid anxiety disorder was allowed if its manifestations were not associated with an underlying mental illness. The second reason for the increased interest in this problem at the moment is that the presence of a comorbid anxiety disorder negatively affects the rehabilitation of patients and their degree of functioning [34]. Thus, the treatment of anxiety spectrum disorders in patients with schizophrenia is necessary, as it increases the likelihood of achieving a favorable outcome [35]. In a meta-analytic study by A. M. Achim et al., 2009, which included 52 studies with a total of 4,032 patients, examined the frequency of anxiety spectrum disorders in patients with schizophrenia.
This was probably due to the fact that for a long time in the DSM diagnostic criteria it was indicated that an anxiety spectrum disorder can be diagnosed if there is no connection with the disorder of the first axis, in particular schizophrenia, which led to a low diagnosis of this nosology in patients with schizophrenia. [33]. However, with the advent of the DSM-III-R, the diagnosis of comorbid anxiety disorder was allowed if its manifestations were not associated with an underlying mental illness. The second reason for the increased interest in this problem at the moment is that the presence of a comorbid anxiety disorder negatively affects the rehabilitation of patients and their degree of functioning [34]. Thus, the treatment of anxiety spectrum disorders in patients with schizophrenia is necessary, as it increases the likelihood of achieving a favorable outcome [35]. In a meta-analytic study by A. M. Achim et al., 2009, which included 52 studies with a total of 4,032 patients, examined the frequency of anxiety spectrum disorders in patients with schizophrenia.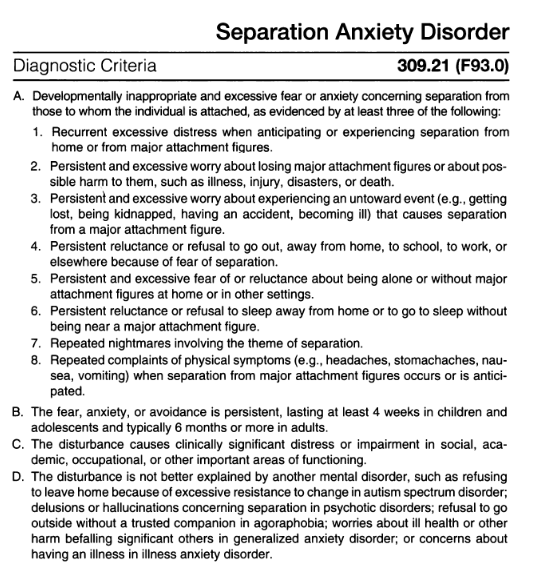 The authors showed that the average prevalence of agoraphobia in this cohort of patients is 5.4%, 95% confidence interval lies in the range from 0.2% to 10.6% [36].
The authors showed that the average prevalence of agoraphobia in this cohort of patients is 5.4%, 95% confidence interval lies in the range from 0.2% to 10.6% [36].
In the Russian school of psychiatry, it is customary to single out a sluggish type of schizophrenic process, which in the American school is regarded as a schizotypal personality type. The endogenous process in this case is characterized by the absence of pronounced positive symptoms, but against the background of a “delayed” course [37]. Some researchers consider agoraphobia as part of a defect formed as a result of a sluggish process 4 [40].
According to Russian studies, the onset of agoraphobia in patients with schizophrenia occurs in adulthood. The main plot of the phobia is the fear of being alone in a confined space and the fear of independent movement on the street. Interestingly, agoraphobic symptoms were formed not only against the background of panic disorder, but also in patients with synesthesia [38].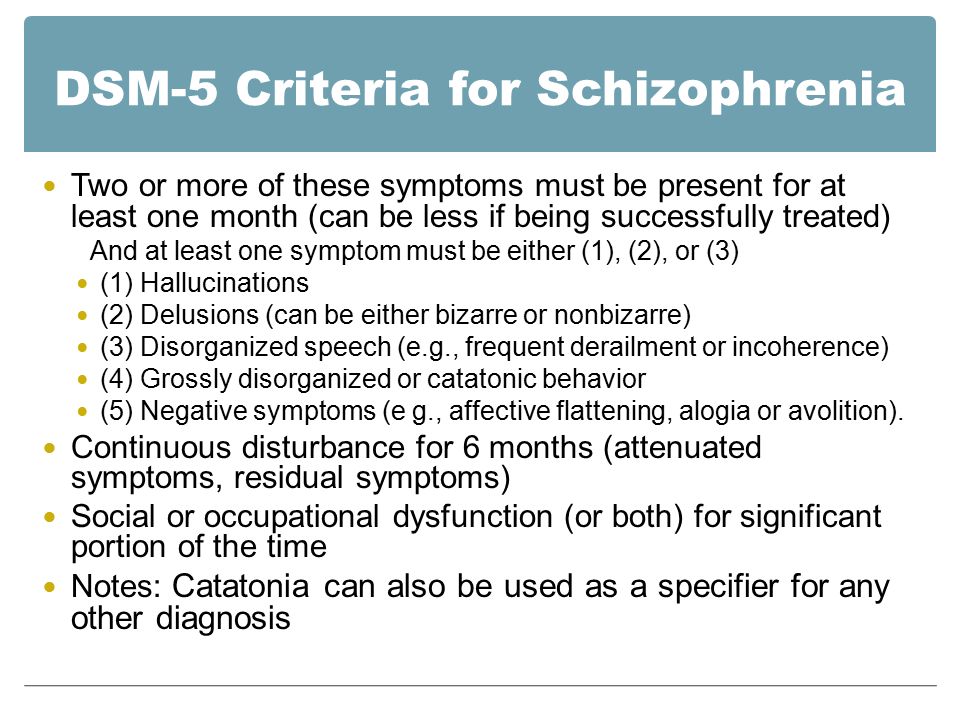
The influence of agoraphobia on the clinical picture of chronic alcoholism
In Germany, U. Schneider and A. Altman, 2001 conducted a large retrospective epidemiological study MUCPA (Multicentre Study of Psychiatric Comorbidity in Alcoholics - Multicenter Study of Comorbidity with Psychiatric Diseases among Alcoholics), the purpose of which was to determine the prevalence of comorbid psychiatric disorders among people suffering from alcoholism . The study included 556 patients suffering from alcoholism (patients who also used other psychoactive substances were excluded from the study). Anxiety disorders were found in 42.3% of those surveyed. Generalized anxiety disorder was diagnosed in 42.3%, agoraphobia in 12.9%.%, social phobia — in 13.1%, panic disorder — in 13.7% of the examined [39].
According to K. Tomasson and P. Vaglum (1996), in the presence of agoraphobia/panic disorder, the risk of re-treatment for alcoholism after detoxification is 6 times higher in individuals with less than two previous visits [40].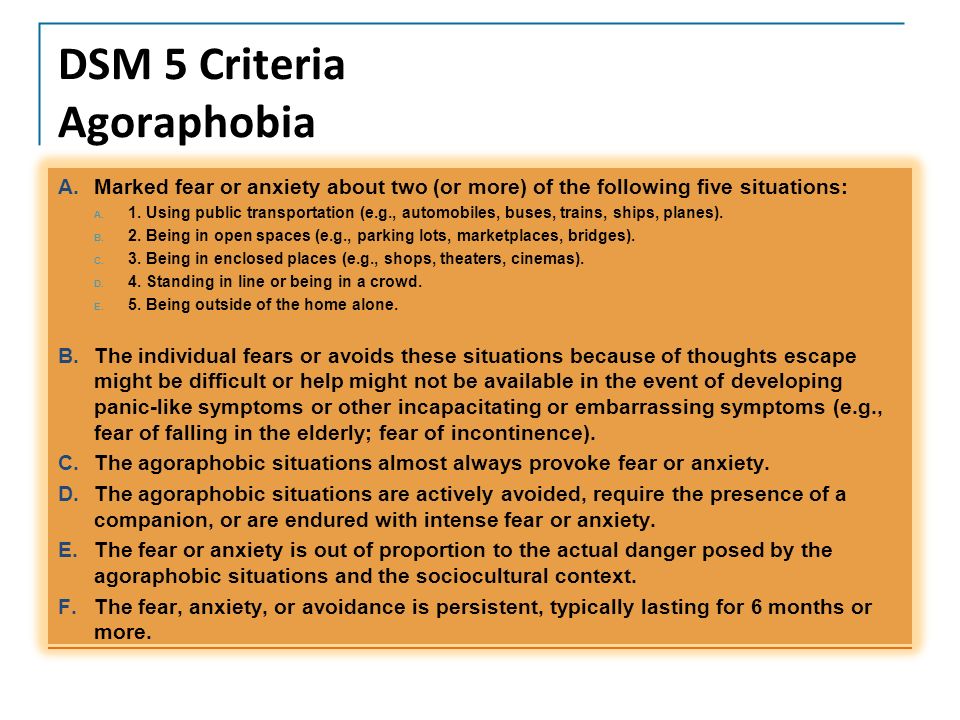
Domestic studies have shown that the picture of panic disorder with agoraphobia worsens if the patient has chronic alcoholism (in particular, the frequency of attacks increases), while the presence of agoraphobic symptoms leads to a relapse of alcoholic disease, which is explained by the use of alcohol to alleviate symptoms [35 ]. The same authors showed that in the presence of chronic alcoholism, agoraphobic symptoms in panic disorder develop faster, and the quality of remission is significantly lower than in patients without alcohol dependence. nine0003
Domestic researchers have revealed a high incidence of dependence on tranquilizers, while this phenomenon is more common in people with an unfavorable course of agoraphobia 5 .
Conclusion
Summarizing the above, it can be noted that agoraphobia is still an urgent problem for both the clinician and the researcher. An analysis of the literature showed that, probably due to the dominance of "American" views on this nosology, it was inextricably considered secondary to panic disorder.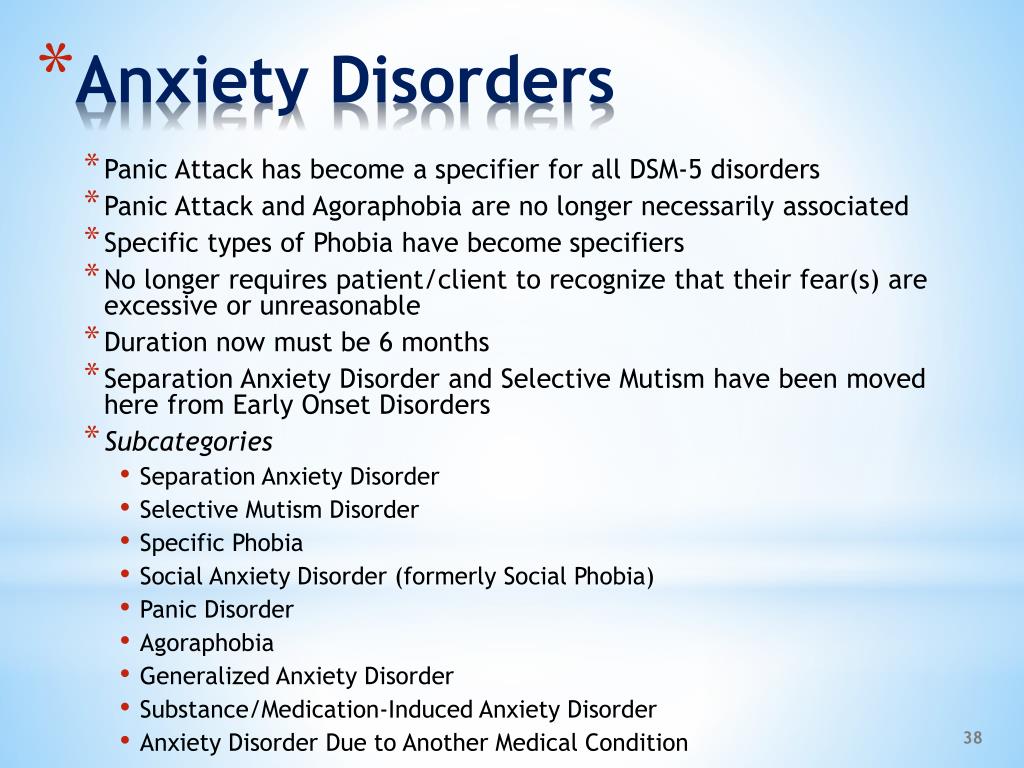 In turn, this has led to a lack of data on agoraphobic symptoms. However, even from this material it is clear that this disorder is a serious problem for a psychiatrist due to the fact that it is not rare, while it aggravates the clinical picture of other mental illnesses. In particular, as mentioned above, it increases the risk of suicidal behavior in depression, reduces the effectiveness of therapy for schizophrenia spectrum disorders and the quality of life of patients, leads to a relapse of chronic alcoholism, and also increases the likelihood of developing dependence on tranquilizers. nine0003
In turn, this has led to a lack of data on agoraphobic symptoms. However, even from this material it is clear that this disorder is a serious problem for a psychiatrist due to the fact that it is not rare, while it aggravates the clinical picture of other mental illnesses. In particular, as mentioned above, it increases the risk of suicidal behavior in depression, reduces the effectiveness of therapy for schizophrenia spectrum disorders and the quality of life of patients, leads to a relapse of chronic alcoholism, and also increases the likelihood of developing dependence on tranquilizers. nine0003
1. Less Yu.E. Typology of generalized anxiety disorder (clinic, comorbidity): Abstract of the thesis. dis. for the degree of Ph.D. GNTSSSP named after V.P. Serbian. Moscow, 2008. 123 p.
2. Pose. I.B. Clinical and psychological predictors of an unfavorable course of agoraphobia with panic disorder: Abstract of the thesis. dis. for the degree of Ph.D. Moscow State Medical University named after A.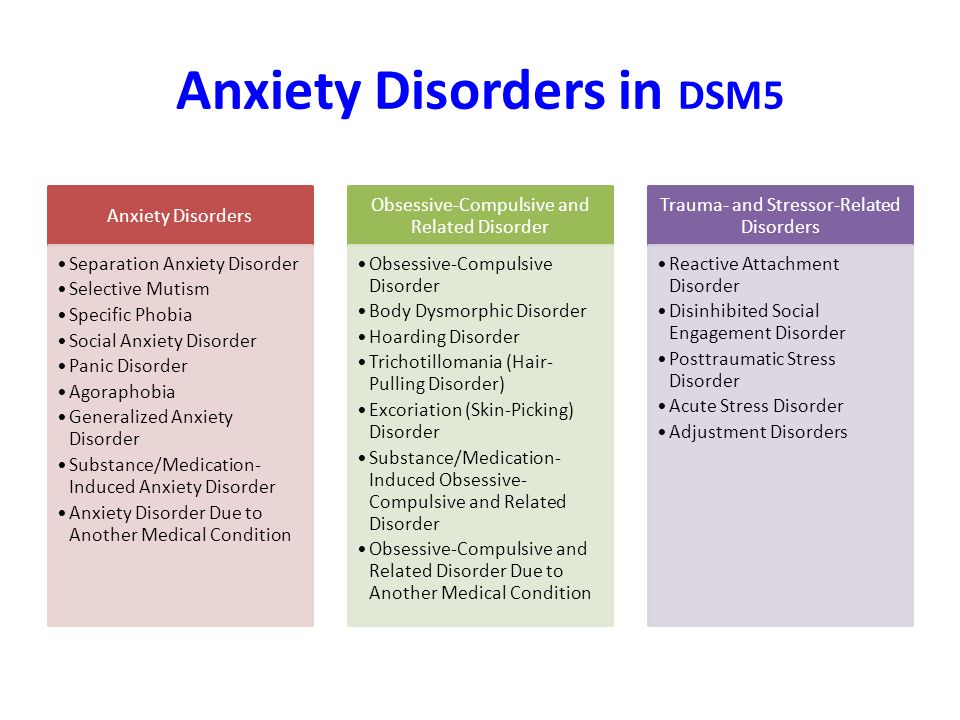 I. Evdokimov. Moscow, 2012. 177 p.
I. Evdokimov. Moscow, 2012. 177 p.
3. Pose. I.B. Clinical and psychological predictors of an unfavorable course of agoraphobia with panic disorder: Abstract of the thesis. dis. for the degree of Ph.D. Moscow State Medical University named after A.I. Evdokimov. Moscow, 2012. 177 p. nine0003
4. Kolyutskaya E.V. Obsessive-phobic disorders in schizophrenia and schizophrenia spectrum disorders: Abstract of the thesis. dis. for the degree of Ph.D. NCPZ RAMS. Moscow, 2001. 152 p.
5. Poze. I.B. Clinical and psychological predictors of an unfavorable course of agoraphobia with panic disorder: Abstract of the thesis. dis. for the degree of Ph.D. Moscow State Medical University named after A.I. Evdokimov. Moscow, 2012. 177 p.
1. Seguij, Salvador-Carulla L, Marquez M, Garcia L, Canet j, et al. Differential clinical features of late-onset panic disorder. J Affect Discord. 2000;57(1-3):115-124. DOI: 10.1016/s0165-0327(99)00082-8
2. Kessler RC, Chiu wT, jin R, Ruscio AM, Shear K, walters EE.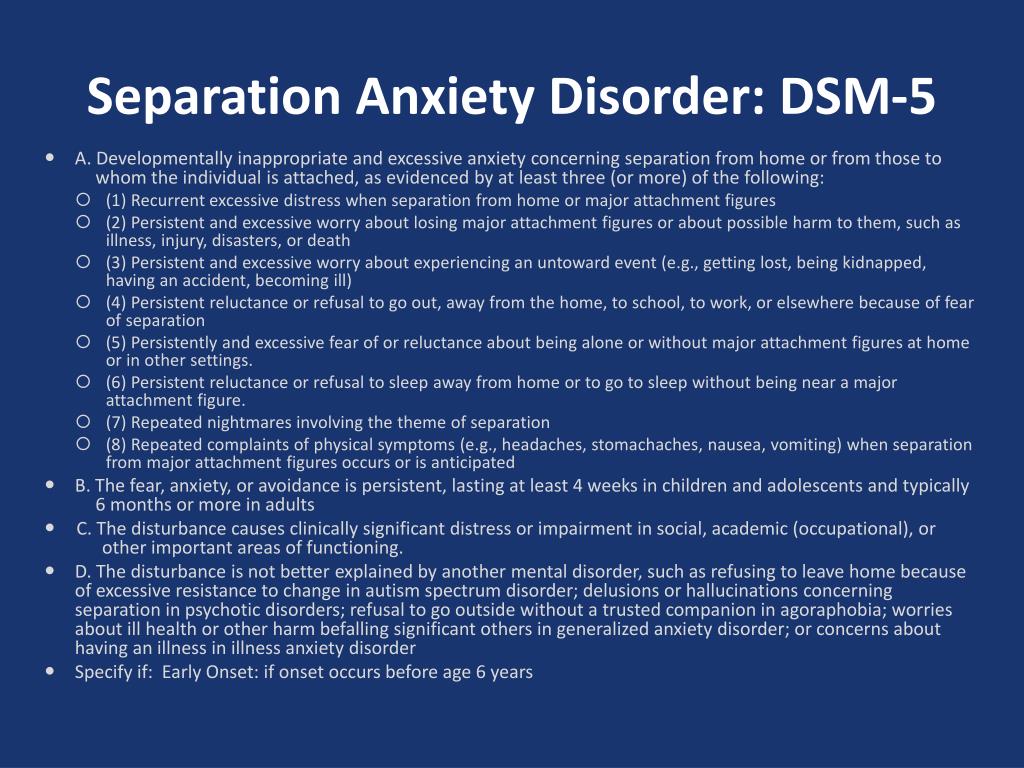 The epidemiology of panic attacks, panic disorder, and agoraphobia in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2006;63(4):415-24. DOI: 10.1001/archpsyc.63.4.415
The epidemiology of panic attacks, panic disorder, and agoraphobia in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2006;63(4):415-24. DOI: 10.1001/archpsyc.63.4.415
3. Carlbring P, Gustafsson H, Ekselius L, Andersson G. 12-month prevalence of panic disorder with or without agoraphobia in the Swedish general population. Soc Psychiatry Psychiatr Epidemiol. 2002;37(5):207-11. DOI: 10.1007/s00127-002-0542-y
4. weissman MM, Bland RC, Canino Gj, Faravelli C, Greenwald S, et al. The cross-national epidemiology of panic disorder. Arch Gen Psychiatry. 1997;54(4):305-9. DOI: 10.1001/archpsyc.1997.01830160021003
5. wittchen HU, Nocon A, Beesdo K, Pine DS, Hofler M, et al. Agoraphobia and panic. Prospective-longitudinal relations suggest a rethinking of diagnostic concepts. Psychother Psychosom. 2008;77(3):147-57. DOI: 10.1159/000116608
6. Aleksandrovsky Yu.A. Borderline mental disorders. M.: Medicine; 2000.
7. Pfaltz MC, Michael T, Meyer AH, wilhelm FH. Reexperiencing symptoms, dissociation, and avoidance behaviors in daily life of patients with PTSD and patients with panic disorder with agoraphobia. J Trauma Stress. 2013;26(4):443-50. DOI: 10.1002/jts.21822
Reexperiencing symptoms, dissociation, and avoidance behaviors in daily life of patients with PTSD and patients with panic disorder with agoraphobia. J Trauma Stress. 2013;26(4):443-50. DOI: 10.1002/jts.21822
8. Carrera M, Herrán A, Ayuso-Mateos jL, Sierra-Biddle D, Ramírez ML, et al. Quality of life in early phases of panic disorder: predictive factors. J Affect Discord. 2006;94(1-3):127-34. DOI: 10.1016/j.jad.2006.03.006
9. Croft A, Hackmann A. Agoraphobia: an outreach treatment programme. Behav Cogn Psychother. 2013;41(3):359-64. DOI: 10.1017/S135246581200077x
10. Kozlov V.V., Vlasov N.A. Models of short-term psychotherapy of agoraphobia. Human factor: Social psychologist. 2020;1(39):356-363. eLIBRARY ID: 42969608
11. Carpiniello B, Baita A, Carta MG, Sitzia R, Macciardi AM, et al. Clinical and psychosocial outcome of patients affected by panic disorder with or without agoraphobia: results from a naturalistic follow-up study. Euro Psychiatry. 2002;17(7):394-8.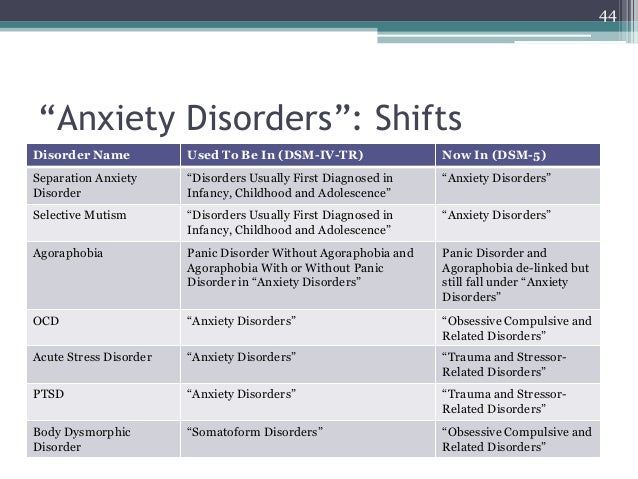 DOI: 10.1016/s0924-9338(02)00701-0
DOI: 10.1016/s0924-9338(02)00701-0
12. Katerndahl DA. Predictors of the development of phobic avoidance. J Clin Psychiatry. 2000;61(8):618-23; quiz 624. DOI: 10.4088/jcp.v61n0813a
13. Goodwin RD, Hamilton SP. The early-onset fearful panic attack as a predictor of severe psychopathology. Psychiatry Res. 2002;109(1):71-9. DOI: 10.1016/s0165-1781(01)00357-2
14. Yonkers KA, Zlotnick C, Allsworth j, warshaw M, Shea T, Keller MB. Is the course of panic disorder the same in women and men? Am J Psychiatry. nineteen98;155(5):596-602. DOI: 10.1176/ajp.155.5.596
15. Statsenko O.A., Ivanova T.I. Clinical and dynamic features of agoraphobia with panic disorder of neurotic origin. Siberian Bulletin of Psychiatry and Narcology. 2011;(1):27-30. eLIBRARY ID: 16158300
16. wittchen HU, Zhao S, Kessler RC, Eaton ww. DSM-III-R generalized anxiety disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51(5):355-64. DOI: 10.1001/archpsyc.1994.03950050015002
17. Golden wL. Cognitive-behavioral hypnotherapy in the treatment of irritable-bowel-syndrome-induced agoraphobia. Int J Clin Exp Hypn. 2007;55(2):131-46. DOI: 10.1080/00207140601177889
Golden wL. Cognitive-behavioral hypnotherapy in the treatment of irritable-bowel-syndrome-induced agoraphobia. Int J Clin Exp Hypn. 2007;55(2):131-46. DOI: 10.1080/00207140601177889
18. Statsenko O.A., Usov G.M. Symptom complex of agoraphobia with panic disorder, comorbid with depression. Journal of Neurology and Psychiatry. S.S. Korsakov. Special issues. 2021;121(5-2):49-54. DOI 10.17116/jnevro20211210549
19. Frank E, Shear MK, Rucci P, Cyranowski jM, Endicott j, et al. Influence of panic-agoraphobic spectrum symptoms on treatment response in patients with recurrent major depression. Am J Psychiatry. 2000;157(7):1101-7. DOI: 10.1176/appi.ajp.157.7.1101
20. Sareen j, Cox Bj, Afifi TO, de Graaf R, Asmundson Gj, et al. Anxiety disorders and risk for suicidal ideation and suicide attempts: a population-based longitudinal study of adults. Arch Gen Psychiatry. 2005;62(11):1249-57. DOI: 10.1001/archpsyc.62.11.1249
21. Placidi GP, Oquendo MA, Malone KM, Brodsky B, Ellis SP, Mann jj.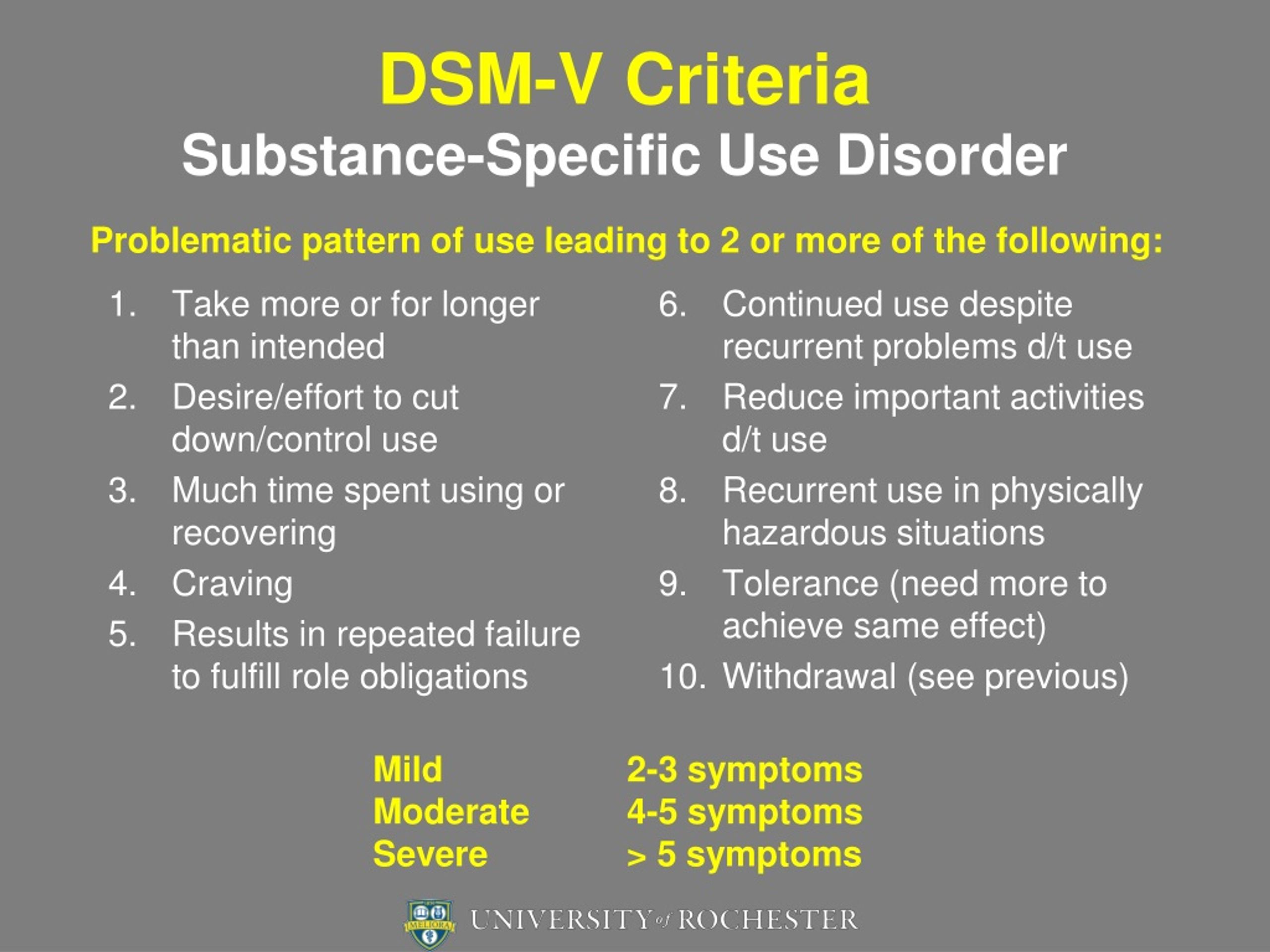 Anxiety in major depression: relationship to suicide attempts. Am J Psychiatry. 2000;157(10):1614-8. doi: 10.1176/appi.ajp.157.10.1614
Anxiety in major depression: relationship to suicide attempts. Am J Psychiatry. 2000;157(10):1614-8. doi: 10.1176/appi.ajp.157.10.1614
22. Bernstein IH, Rush Aj, Yonkers K, Carmody Tj, woo A, et al. Symptom features of postpartum depression: are they distinct? Depress Anxiety. 2008;25(1):20-6. DOI: 10.1002/da.20276
23. Allen LB, white KS, Barlow DH, Shear MK, Gorman jM, woods Sw. Cognitive-Behavior Therapy (CBT) for Panic Disorder: Relationship of Anxiety and Depression Comorbidity with Treatment Outcome. J Psychopathol Behav Assess. 2010;32(2):185-192. DOI: 10.1007/s10862-009-9151-3
24. Feldner MT, Smith RC, Babson KA, Sachs-Ericsson N, Schmidt NB, Zvolensky Mj. Test of the role of nicotine dependence in the relation between posttraumatic stress disorder and panic spectrum problems. J Trauma Stress. 2009;22(1):36-44. DOI: 10.1002/jts.20384
25. Cougle jR, Feldner MT, Keough ME, Hawkins KA, Fitch KE. Comorbid panic attacks among individuals with posttraumatic stress disorder: associations with traumatic event exposure history, symptoms, and impairment. J Anxiety Discord. 2010;24(2):183-8. DOI: 10.1016/j.janxdis.2009.10.006
J Anxiety Discord. 2010;24(2):183-8. DOI: 10.1016/j.janxdis.2009.10.006
26. Andrews G., Charney D. S., Sirovatka P. j., Regier D. A., eds. Stress-induced and fear circuitry disorders: Refining the research agenda for DSM-V. Arlington, VA: American Psychiatric Association; 2009. DOI: 10.1176/appi.ajp.2009.09071033
27. Hinton DE, Hofmann SG, Pitman RK, Pollack MH, Barlow DH. The panic attack-posttraumatic stress disorder model: applicability to orthostatic panic among Cambodian refugees. Cogn Behav Ther. 2008;37(2):101-16. DOI: 10.1080/16506070801969062
28. Grant BF, Hasin DS, Stinson FS, Dawson DA, Patricia Chou S, et al. Co-occurrence of 12-month mood and anxiety disorders and personality disorders in the US: results from the national epidemiologic survey on alcohol and related conditions. J Psychiatrist Res. 2005;39(1):1-9. DOI: 10.1016/j.jpsychires.2004.05.004
29. Cassano GB, Michelini S, Shear MK, Coli E, Maser jD, Frank E. The panic-agoraphobic spectrum: a descriptive approach to the assessment and treatment of subtle symptoms .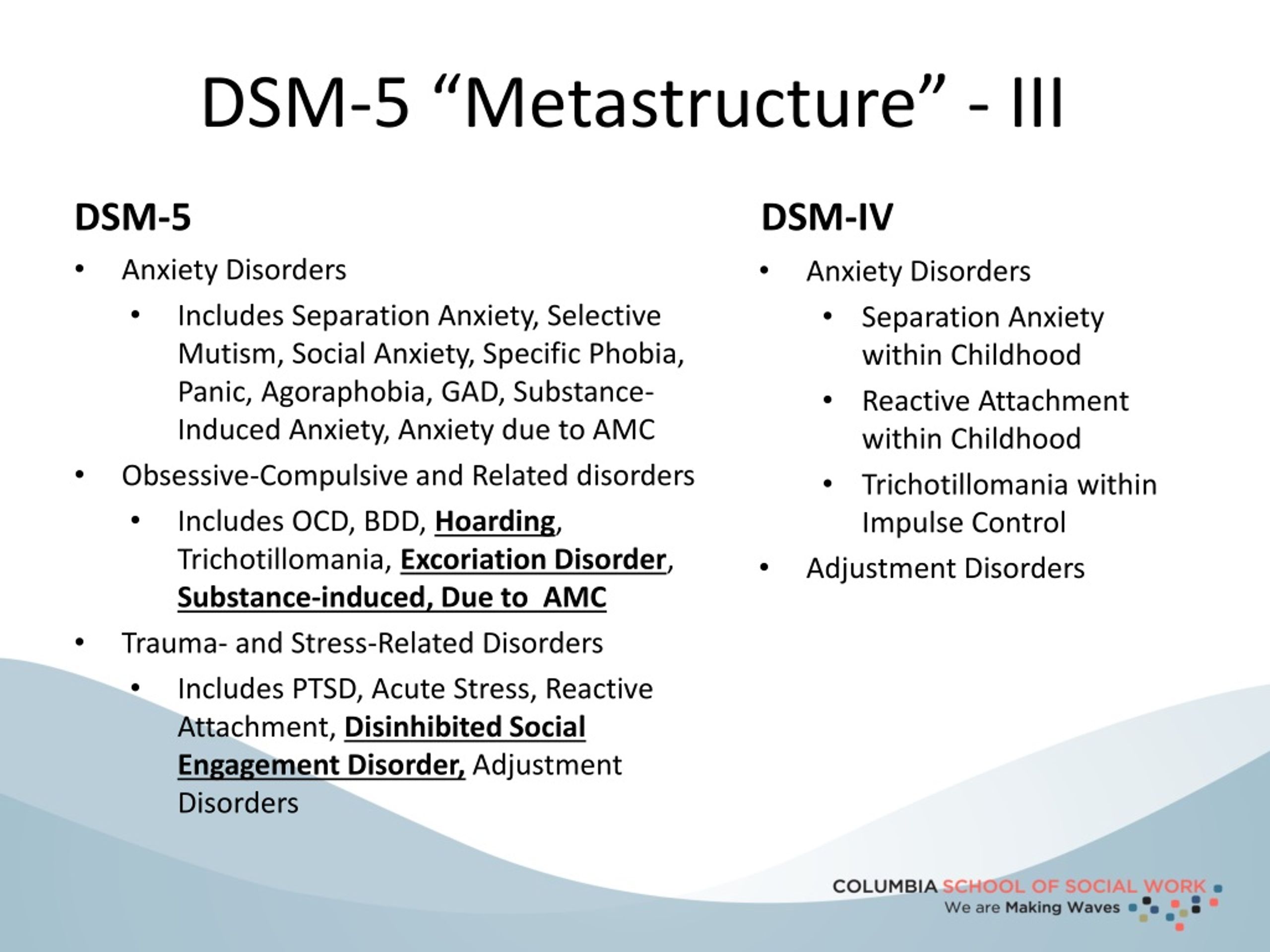 Am J Psychiatry. 1997;154(6 Suppl):27-38. DOI: 10.1176/ajp.154.6.27
Am J Psychiatry. 1997;154(6 Suppl):27-38. DOI: 10.1176/ajp.154.6.27
30. Marchesi C, Cantoni A, Fontò S, Giannelli MR, Maggini C. The effect of pharmacotherapy on personality disorders in panic disorder: a one year naturalistic study. J Affect Discord. 2005;89(1-3):189-94. DOI: 10.1016/j.jad.2005.07.007
31. Ozkan M, Altindag A. Comorbid personality disorders in subjects with panic disorder: do personality disorders increase clinical severity? Compr Psychiatry. 2005;46(1):20-6. DOI: 10.1016/j.comppsych.2004.07.015
32. Ulas H, Alptekin K, Akdede BB, Tumuklu M, Akvardar Y, et al. Panic symptoms in schizophrenia: comorbidity and clinical correlates.Psychiatry Clin Neurosci.2007;61(6):678-80. DOI: 10.1111/j.1440-1819.2007.01724.x
33. Voges M, Addington j. The association between social anxiety and social functioning in first episode psychosis. Schizophr Res. 2005;76(2-3):287-92. DOI: 10.1016/j.schres.2005.01.001
34. Seedat S, Fritelli V, Oosthuizen P, Emsley RA, Stein Dj.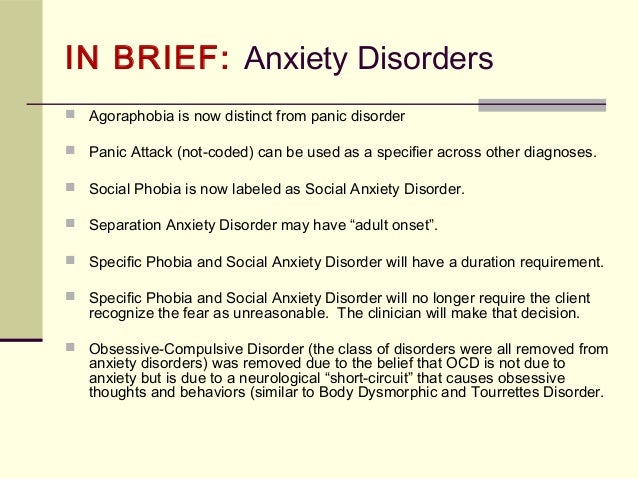 Measuring anxiety in patients with schizophrenia. J Nerv Ment Dis. 2007;195(4):320-4. DOI: 10.1097/01.nmd.0000253782.47140.ac
Measuring anxiety in patients with schizophrenia. J Nerv Ment Dis. 2007;195(4):320-4. DOI: 10.1097/01.nmd.0000253782.47140.ac
35. Niehaus Dj, Koen L, Muller j, Laurent C, Stein Dj, et al. Obsessive compulsive disorder—prevalence in xhosaspeaking schizophrenia patients. S Afr Med J. 2005;95(2):120-2. PMID: 15751207
36. Achim AM, Maziade M, Raymond E, Olivier D, Mérette C, Roy MA. How are prevalent anxiety disorders in schizophrenia? A meta-analysis and critical review on a significant association. Schizophr Bull. 2011;37(4):811-21. DOI: 10.1093/schbul/sbp148
37. Tsygankov B.D., Ovsyannikov S.A. Psychiatry: a guide for physicians. Moscow: GetAR-Media; 2011.
38. Bobrov A.S., Pavlova O.N. Phobic disorders in the clinic of schizophrenia with paroxysmal course. Siberian Medical Journal. 2011;(6):99-102. eLIBRARY ID: 17053529
39. Schneider U, Altmann A, Baumann M, Bernzen j, Bertz B, et al. Comorbid anxiety and affective disorder in alcoholdependent patients seeking treatment: the first Multicentre Study in Germany.