Is lying genetic
Everything you need to know
Pathological liars tell compulsive lies without a clear motive. This type of lying is different than nonpathological lying, where the lie is often beneficial in some way.
Lying is a common feature of social interactions among humans. This behavior even occurs in some animals, such as monkeys.
Lies often lead to some benefit. For example, a person may lie to avoid social embarrassment. While some people lie more frequently than others, it is not typically a sign of a mental health condition.
Pathological lying is different. It may be a sign of an underlying mental health condition, such as a personality disorder.
In this article, we discuss pathological lying in more detail, including how to recognize it and how to cope with this behavior in others.
Share on PinterestA pathological liar is someone who lies compulsively and without any clear benefit.Lying refers to making a false statement to deceive others intentionally, often for some form of personal gain.
Nonpathological lying is commonplace and not a sign of any disorder. A person who pathologically lies will lie compulsively and without any clear benefit to themselves.
There have been some attempts to outline the differences between a pathological and a nonpathological lie, but more research is necessary to make appropriate distinctions.
A key feature of a pathological lie is that it has no obvious motivation. It is usually possible to determine why someone has told a lie — such as to benefit themselves or avoid an embarrassing or stressful social situation — but pathological lying occurs for no clear reason and does not seem to benefit the individual.
It is unclear whether a person who pathologically lies is aware of their deceit or is capable of thinking rationally about their lies.
Pathological lying can make socializing difficult and lead to significant interpersonal problems with loved ones and colleagues.
There has been little research in this area, and the causes of pathological lying are unknown.
It is unclear whether pathological lying is a symptom of another condition or a condition itself.
For instance, compulsive lying is a feature of several other conditions, such as factitious disorder and personality disorders.
Factitious disorder
Factitious disorder — sometimes called Munchausen’s syndrome — is a condition in which a person acts as though they are physically or mentally ill when they are not.
Munchausen’s syndrome by proxy is when someone lies about another person having an illness. This condition is most common in mothers, who feign illness in their child and lie to a doctor about it.
The causes of factitious disorder are unknown. Theories include:
- biological or genetic causes
- childhood abuse or neglect
- low self-esteem
- the presence of a personality disorder
- substance abuse
- depression
Personality disorders
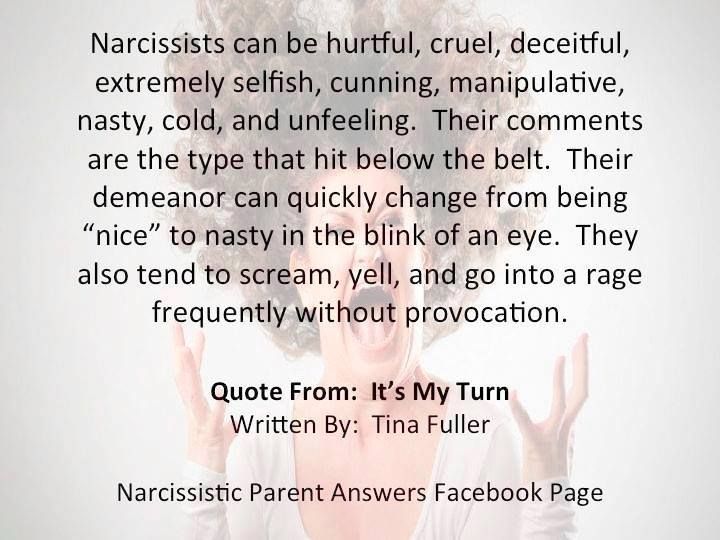
Pathological lying is a possible symptom of certain personality disorders, including:
- borderline personality disorder (BPD)
- narcissistic personality disorder (NPD)
- antisocial personality disorder (APD)
BPD is a condition that makes it difficult for a person to regulate their emotions. People with BPD may experience severe mood swings, feel greater instability and insecurity, and not have a stable sense of self.
People with BPD may experience severe mood swings, feel greater instability and insecurity, and not have a stable sense of self.
The hallmarks of NPD are fantasies of immense importance and the need for admiration and special treatment.
Researchers argue that while pathological lying may, in theory, occur in people with APD, those with this condition often lie for personal gain or pleasure.
A person with BPD or NPD may lie to distort reality into something that fits with the emotions that they are feeling, rather than the facts.
These personality disorders can lead to significant challenges with interpersonal relationships.
Frontotemporal dementia
A case study of one person showing signs of pathological lying found that their behavior patterns were similar to those that can occur with frontotemporal dementia.
Frontotemporal dementia is a form of dementia that affects the frontal and temporal brain regions and causes changes in behavior and language.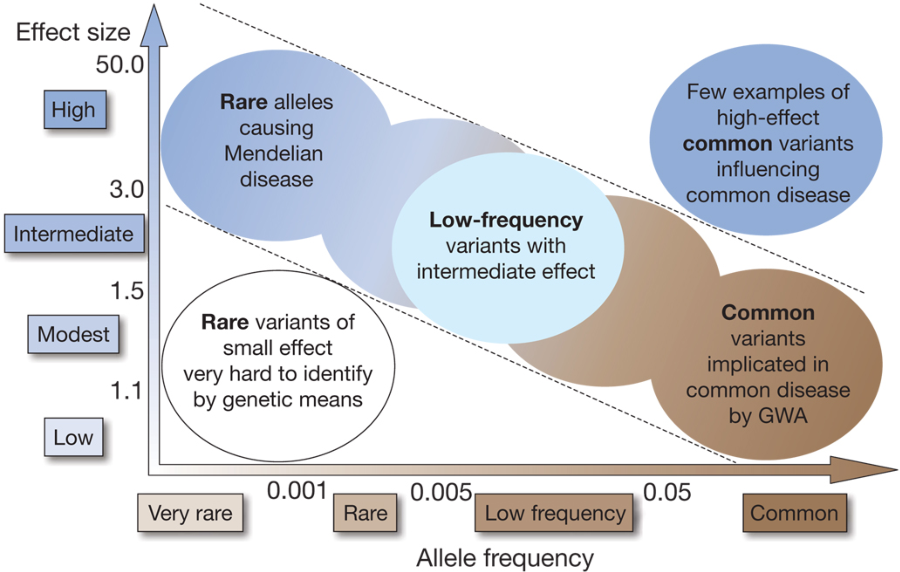
These changes can include:
- inappropriate social behavior
- lack of empathy
- loss of insight into the behavior of others and oneself
- changes in food preferences
- compulsive behavior
- boredom
- agitation
Share on PinterestPathological lies often differ from ordinary lies in that they are easy for others to verify as incorrect.
Pathological lies are compulsive and may start small. The lies can gradually become more elaborate and dramatic, particularly if they are necessary to cover up for an earlier lie. They often become complicated by unnecessary amounts of detail.
People who lie frequently are not necessarily pathological liars. The most distinguishing feature of a pathological lie is that it does not have a motive.
Therefore, a person who frequently exaggerates stories to make themselves appear more interesting or consistently lies to cover up mistakes that they have made is unlikely to be pathologically lying.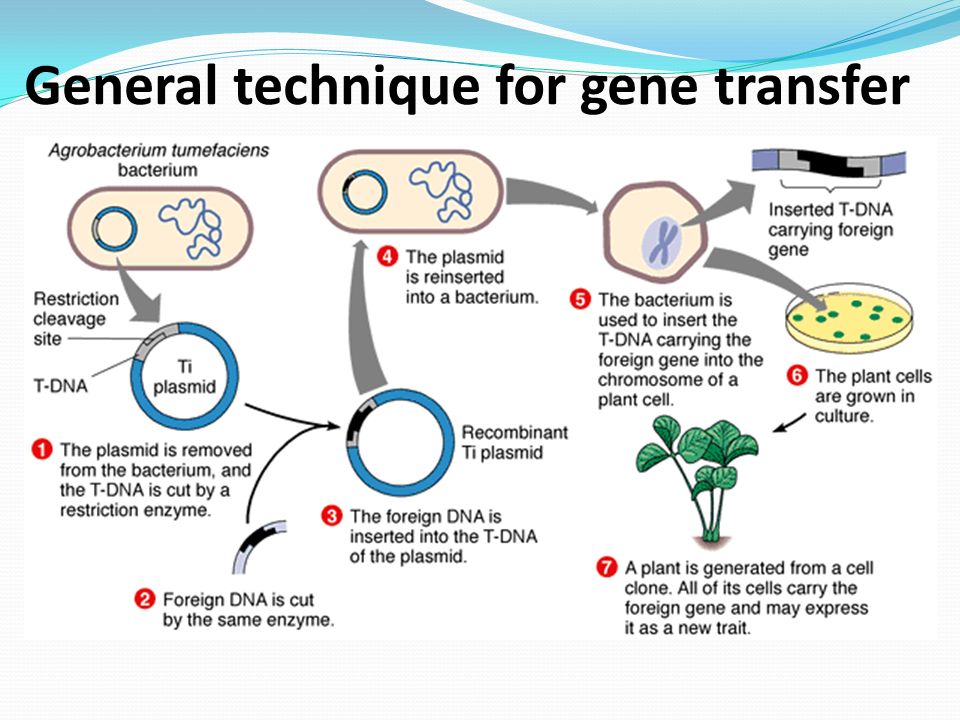 These are clear motives that advance particular interests.
These are clear motives that advance particular interests.
Pathological lies are easy for others to verify, which can ultimately be harmful to the person who tells them. For example, the individual may make false accusations or grandiose claims about their past that are simple for others to check.
Pathological lying is not a formal diagnosis, but a doctor or therapist may recognize the behavior as a sign of another underlying condition, such as a personality disorder or factitious disorder.
These disorders include overlapping symptoms, including compulsive lying. People with these conditions also display other signs.
It is possible for pathological lying to be an independent symptom, as some people engage in pathological lying without having any underlying medical condition.
It can be challenging for a doctor to determine whether someone is engaging in pathological lying because there are no psychological or biological tests for it.
To diagnose most mental health conditions, a doctor will use a clinical interview.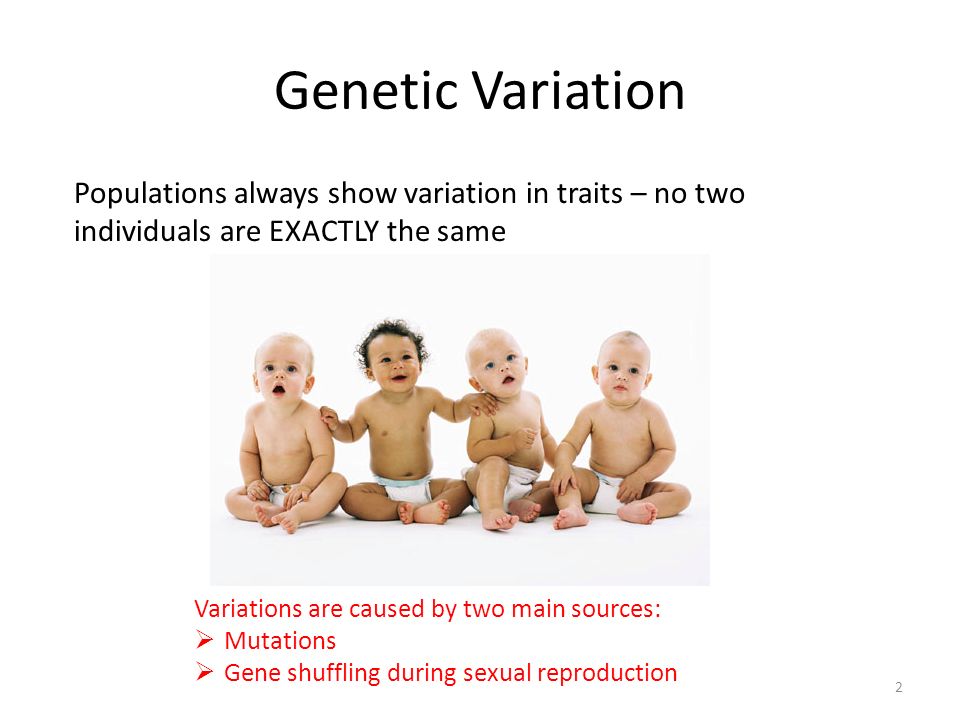 If the person is not honest about their lying, it could be necessary for the doctor to talk with family members or friends to help identify patterns of pathological lying.
If the person is not honest about their lying, it could be necessary for the doctor to talk with family members or friends to help identify patterns of pathological lying.
Coping with someone who lies pathologically can be challenging. Forming and maintaining a trusting relationship with this person can take time and patience.
It is important to remember that the person may not intend to cause harm or benefit from these lies. Pathological lying can be a compulsion, and it often leads to negative consequences for the person telling the lies. Therefore, try to avoid responding angrily or blaming them for the lies.
It is also helpful to be aware that pathological lying may be a sign of an underlying mental health condition. Talking to the person about whether they have any other symptoms can help them identify the problem and seek help from a doctor or therapist.
Share on PinterestIf a doctor suspects pathological lying is part of an underlying personality disorder, they may suggest psychotherapy.
As pathological lying is not a recognized condition, there are no formal treatments for it.
If a doctor suspects that an underlying condition is causing the lying, they may suggest treatment for that condition.
For example, treatment for personality disorders usually involves psychotherapy or medication.
As pathological lying can be harmful to others, a doctor may also suggest therapy for those close to the individual. A therapist will work with them to help them manage their responses to the problem.
Pathological lying is when a person compulsively lies without a clear motive for doing so. The lies may become elaborate and detailed, but they are often easy to verify.
Pathological lies do not lead to any lasting benefit for the person who tells them, and they can be harmful to others.
It is vital to remember that the lying is a compulsion and that a person who pathologically lies does not intend to harm others or better themselves.
As pathological lying is not a recognized condition, there are no formal treatments for it. However, pathological lying may be a sign of an underlying condition that a doctor can help with, such as a personality disorder.
However, pathological lying may be a sign of an underlying condition that a doctor can help with, such as a personality disorder.
Everything you need to know
Pathological liars tell compulsive lies without a clear motive. This type of lying is different than nonpathological lying, where the lie is often beneficial in some way.
Lying is a common feature of social interactions among humans. This behavior even occurs in some animals, such as monkeys.
Lies often lead to some benefit. For example, a person may lie to avoid social embarrassment. While some people lie more frequently than others, it is not typically a sign of a mental health condition.
Pathological lying is different. It may be a sign of an underlying mental health condition, such as a personality disorder.
In this article, we discuss pathological lying in more detail, including how to recognize it and how to cope with this behavior in others.
Share on PinterestA pathological liar is someone who lies compulsively and without any clear benefit.
Lying refers to making a false statement to deceive others intentionally, often for some form of personal gain.
Nonpathological lying is commonplace and not a sign of any disorder. A person who pathologically lies will lie compulsively and without any clear benefit to themselves.
There have been some attempts to outline the differences between a pathological and a nonpathological lie, but more research is necessary to make appropriate distinctions.
A key feature of a pathological lie is that it has no obvious motivation. It is usually possible to determine why someone has told a lie — such as to benefit themselves or avoid an embarrassing or stressful social situation — but pathological lying occurs for no clear reason and does not seem to benefit the individual.
It is unclear whether a person who pathologically lies is aware of their deceit or is capable of thinking rationally about their lies.
Pathological lying can make socializing difficult and lead to significant interpersonal problems with loved ones and colleagues.
There has been little research in this area, and the causes of pathological lying are unknown.
It is unclear whether pathological lying is a symptom of another condition or a condition itself.
For instance, compulsive lying is a feature of several other conditions, such as factitious disorder and personality disorders.
Factitious disorder
Factitious disorder — sometimes called Munchausen’s syndrome — is a condition in which a person acts as though they are physically or mentally ill when they are not.
Munchausen’s syndrome by proxy is when someone lies about another person having an illness. This condition is most common in mothers, who feign illness in their child and lie to a doctor about it.
The causes of factitious disorder are unknown. Theories include:
- biological or genetic causes
- childhood abuse or neglect
- low self-esteem
- the presence of a personality disorder
- substance abuse
- depression
Personality disorders
Pathological lying is a possible symptom of certain personality disorders, including:
- borderline personality disorder (BPD)
- narcissistic personality disorder (NPD)
- antisocial personality disorder (APD)
BPD is a condition that makes it difficult for a person to regulate their emotions. People with BPD may experience severe mood swings, feel greater instability and insecurity, and not have a stable sense of self.
People with BPD may experience severe mood swings, feel greater instability and insecurity, and not have a stable sense of self.
The hallmarks of NPD are fantasies of immense importance and the need for admiration and special treatment.
Researchers argue that while pathological lying may, in theory, occur in people with APD, those with this condition often lie for personal gain or pleasure.
A person with BPD or NPD may lie to distort reality into something that fits with the emotions that they are feeling, rather than the facts.
These personality disorders can lead to significant challenges with interpersonal relationships.
Frontotemporal dementia
A case study of one person showing signs of pathological lying found that their behavior patterns were similar to those that can occur with frontotemporal dementia.
Frontotemporal dementia is a form of dementia that affects the frontal and temporal brain regions and causes changes in behavior and language.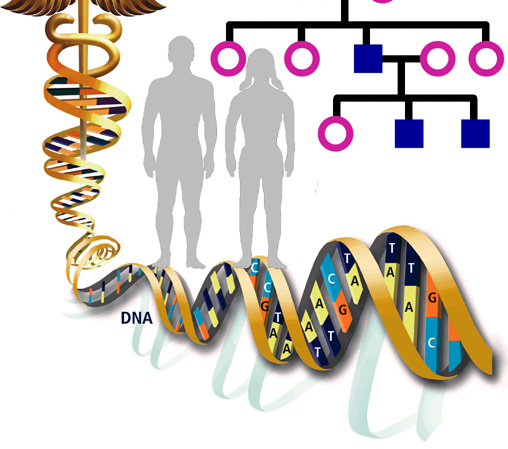
These changes can include:
- inappropriate social behavior
- lack of empathy
- loss of insight into the behavior of others and oneself
- changes in food preferences
- compulsive behavior
- boredom
- agitation
Share on PinterestPathological lies often differ from ordinary lies in that they are easy for others to verify as incorrect.
Pathological lies are compulsive and may start small. The lies can gradually become more elaborate and dramatic, particularly if they are necessary to cover up for an earlier lie. They often become complicated by unnecessary amounts of detail.
People who lie frequently are not necessarily pathological liars. The most distinguishing feature of a pathological lie is that it does not have a motive.
Therefore, a person who frequently exaggerates stories to make themselves appear more interesting or consistently lies to cover up mistakes that they have made is unlikely to be pathologically lying. These are clear motives that advance particular interests.
These are clear motives that advance particular interests.
Pathological lies are easy for others to verify, which can ultimately be harmful to the person who tells them. For example, the individual may make false accusations or grandiose claims about their past that are simple for others to check.
Pathological lying is not a formal diagnosis, but a doctor or therapist may recognize the behavior as a sign of another underlying condition, such as a personality disorder or factitious disorder.
These disorders include overlapping symptoms, including compulsive lying. People with these conditions also display other signs.
It is possible for pathological lying to be an independent symptom, as some people engage in pathological lying without having any underlying medical condition.
It can be challenging for a doctor to determine whether someone is engaging in pathological lying because there are no psychological or biological tests for it.
To diagnose most mental health conditions, a doctor will use a clinical interview.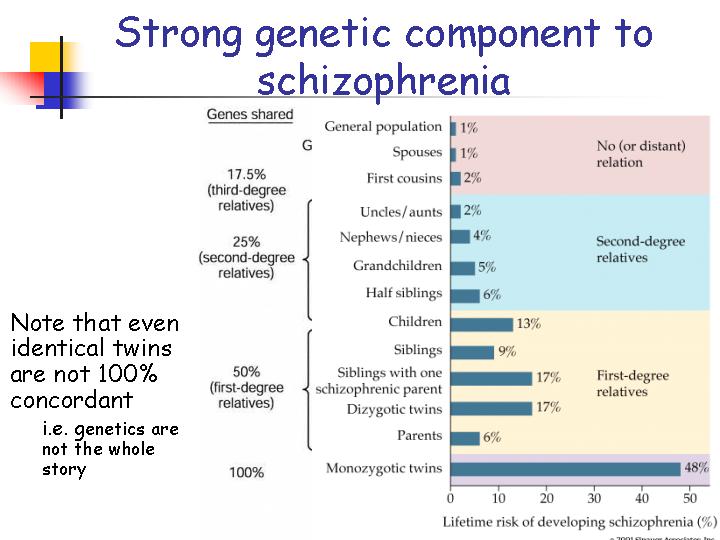 If the person is not honest about their lying, it could be necessary for the doctor to talk with family members or friends to help identify patterns of pathological lying.
If the person is not honest about their lying, it could be necessary for the doctor to talk with family members or friends to help identify patterns of pathological lying.
Coping with someone who lies pathologically can be challenging. Forming and maintaining a trusting relationship with this person can take time and patience.
It is important to remember that the person may not intend to cause harm or benefit from these lies. Pathological lying can be a compulsion, and it often leads to negative consequences for the person telling the lies. Therefore, try to avoid responding angrily or blaming them for the lies.
It is also helpful to be aware that pathological lying may be a sign of an underlying mental health condition. Talking to the person about whether they have any other symptoms can help them identify the problem and seek help from a doctor or therapist.
Share on PinterestIf a doctor suspects pathological lying is part of an underlying personality disorder, they may suggest psychotherapy.
As pathological lying is not a recognized condition, there are no formal treatments for it.
If a doctor suspects that an underlying condition is causing the lying, they may suggest treatment for that condition.
For example, treatment for personality disorders usually involves psychotherapy or medication.
As pathological lying can be harmful to others, a doctor may also suggest therapy for those close to the individual. A therapist will work with them to help them manage their responses to the problem.
Pathological lying is when a person compulsively lies without a clear motive for doing so. The lies may become elaborate and detailed, but they are often easy to verify.
Pathological lies do not lead to any lasting benefit for the person who tells them, and they can be harmful to others.
It is vital to remember that the lying is a compulsion and that a person who pathologically lies does not intend to harm others or better themselves.
As pathological lying is not a recognized condition, there are no formal treatments for it. However, pathological lying may be a sign of an underlying condition that a doctor can help with, such as a personality disorder.
However, pathological lying may be a sign of an underlying condition that a doctor can help with, such as a personality disorder.
How Genes Affect Character, Intelligence, and Mental Health - T&P
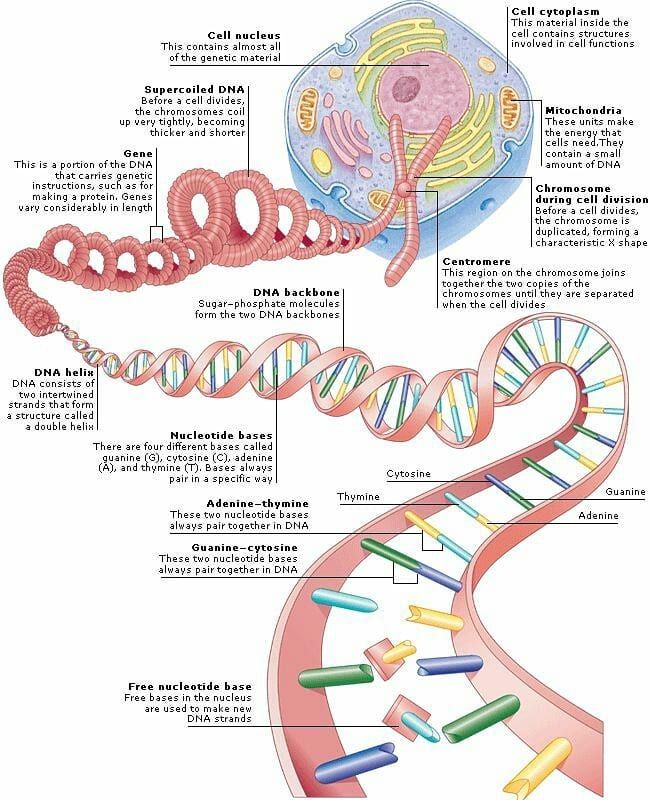
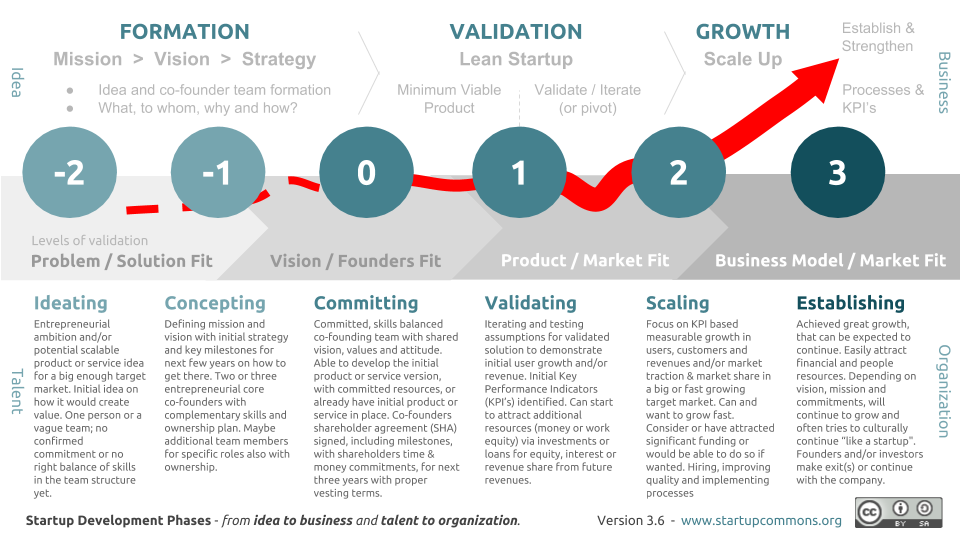
Psychogenetics describes how hereditary factors affect the functioning of the psyche of animals and humans. Which mental illnesses are genetic and which are not? Can genes determine character? Is there a tendency to criminal acts hereditary? Psychogenetics answers all these questions. T&P talk about what scientists do within this scientific field.
In the English-language literature, the term “behavioral genetics” is used to define psychogenetics. Some scientists say that this discipline lies at the intersection of psychology, neuroscience, genetics and statistics; others consider it a field of psychology that simply uses the methods of genetics to study the nature and origin of individual differences in humans and animals. The last definition seems to be closer to the essence of this scientific direction, since its focus is on the structure and work of the psyche, and the genetic component is rather a factor that affects it. nine0005
nine0005
Psychogenetics of sex: a boy who was raised as a girl
Differences in behavior between people of different sexes is one of the issues that this area deals with. A textbook example that defined modern ideas about the psychogenetics of sex is the case of David Reimer, a boy who was raised as a girl. David (who had a twin brother) was born into a poor Canadian family and experienced an accident as an infant in which he lost his penis. The Raymers could not find a way out of this situation for a long time, and then accidentally learned about the theory of John Money (the creator of the term "gender"), who was sure that gender role is determined by upbringing, and not by DNA. There was no data to refute this at that time. nine0005
The state of the art of surgery did not allow for reconstructive surgery, and David's parents decided to have sex reassignment surgery, hoping to raise their son as a daughter. The child was given a new name - Brenda. Brenda had toys, clothes and activities for girls, her brother treated her like a sister, and her parents treated her like a daughter. However, it soon became clear that both psychologically and outwardly the girl was developing according to a masculine type. Brenda did not develop relationships at school (she was not interested in her peers, and the boys did not want to play with the girl), and in her diary she wrote that she had "nothing to do with her mother." In the end, the girl began to think about suicide, and then her parents decided to tell her the truth. Brenda made three unsuccessful suicide attempts, after which she decided to become a boy again. She underwent hormonal therapy and underwent surgery to restore primary sexual characteristics. nine0005
However, it soon became clear that both psychologically and outwardly the girl was developing according to a masculine type. Brenda did not develop relationships at school (she was not interested in her peers, and the boys did not want to play with the girl), and in her diary she wrote that she had "nothing to do with her mother." In the end, the girl began to think about suicide, and then her parents decided to tell her the truth. Brenda made three unsuccessful suicide attempts, after which she decided to become a boy again. She underwent hormonal therapy and underwent surgery to restore primary sexual characteristics. nine0005
Dr. Money's theory has been disproved. David was paid significant compensation for his suffering, but his psychological problems were never fully resolved. As an adult, Reimer married and adopted three children, but soon after the death of his brother, who died from an overdose of antidepressants, he nevertheless committed suicide. At that time he was 38 years old.
Today we know that gender is genetically determined. It is impossible to make a person a man or a woman through education, pressure or manipulation: the mechanisms laid down by genetics are incomparably stronger than all this. That is why people with a diagnosis of "transgender" today are prescribed a sex change operation in order to bring their biological sex into line with their psychological one. nine0005
Phenylketonuria: an attack on neurons
The influence of genetic mechanisms on the functioning of the psyche can manifest itself not only in fundamental issues like gender. Another example is phenylketonuria, an inherited metabolic disorder of amino acids, primarily phenylalanine. This substance is present in the proteins of all known living organisms. Normally, liver enzymes should convert it into tyrosine, which, among other things, is necessary for the synthesis of neurotransmitters. But with phenylketonuria, the necessary enzymes are absent or lacking, so phenylalanine becomes phenylpyruvic acid, which is toxic to neurons. This leads to severe CNS damage and dementia. nine0005
This leads to severe CNS damage and dementia. nine0005
Phenylalanine is found in meat, poultry, seafood, eggs, plant foods (in smaller amounts), as well as carbonated drinks, chewing gum and other products, so for normal mental development, patients with phenylketonuria in childhood need to diet and drink drugs containing tyrosine.
Phenylketonuria is a vivid example of how a genetic failure, which at first glance is not related to brain functions, affects its work in a critical way. At the same time, in the end, the fate of such patients in childhood depends on external factors: with proper treatment, they develop intellectually along with their peers. If a child with impaired phenylalanine metabolism does not receive medication and does not follow a diet, mental retardation awaits him, and this is an irreversible diagnosis. nine0005
Pathology constructor: how schizophrenia is inherited
Today, scientists believe that schizophrenia, like autism, is inherited.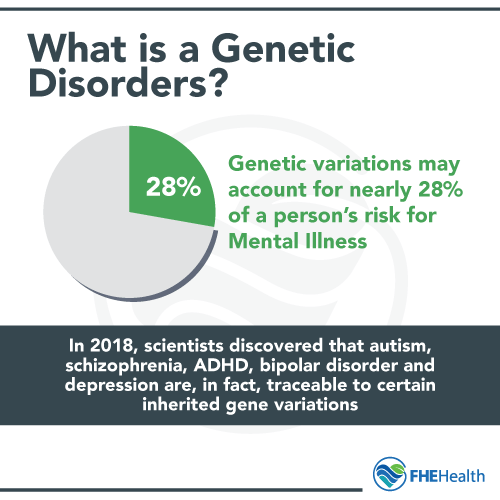 According to studies, the probability of getting sick with it is:
According to studies, the probability of getting sick with it is:
- 1% if the diagnosis has not been observed in the family before;
- 6% if one of the parents has schizophrenia;
- 9% if it is observed in a brother or sister;
- 48% if we are talking about one of the identical twins.
At the same time, there is no specific “schizophrenia gene”: we are talking about dozens or even hundreds of genome fragments in which anomalies are observed. We are all carriers of certain mutations, including those associated with schizophrenia, but they do not have any effect on our lives until they “get together”. nine0005
So far, scientists have not been able to find anomalies whose presence leads to schizophrenia. Nevertheless, they still managed to find several problematic areas in the human genome. The most famous among them is the 16th chromosome: the absence of its 16p11.2 region may be one of the factors underlying autism and mental retardation. The 16p11. 2 doubling also seems to lead to autism, mental retardation, epilepsy, and schizophrenia. There are other chromosomal regions (15q13.3 and 1q21.1) in which mutations can be associated with mental illness. nine0005
2 doubling also seems to lead to autism, mental retardation, epilepsy, and schizophrenia. There are other chromosomal regions (15q13.3 and 1q21.1) in which mutations can be associated with mental illness. nine0005
A child's chance of inheriting schizophrenia decreases as his mother's age increases. But in the case of the father, the opposite is true: the older the father, the higher the probability. The reason is that with age, more germ cell mutations occur in men, which leads to the appearance of de novo mutations in children, while this is not typical for women.
Experts have yet to solve the puzzle that represents the genetic architecture of schizophrenia. Indeed, de facto, this disease is inherited much more often than genetic studies show, even if relatives are separated and lead completely different lifestyles. The same picture, however, is observed in the case of hereditary obesity, abnormally high or abnormally short growth and other genetically determined parameters that deviate from the norm.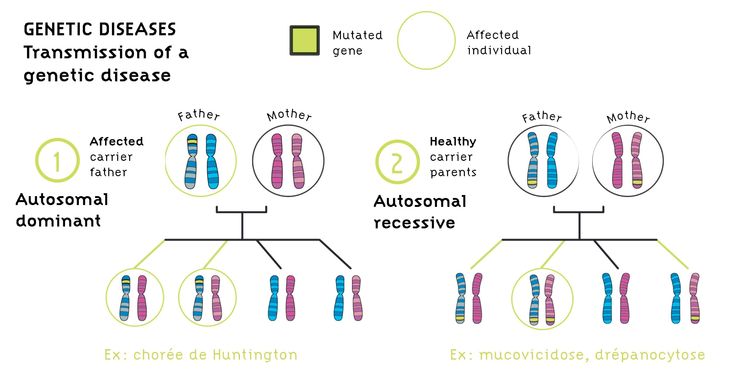 nine0005
nine0005
Grandma's mind: hereditary IQ
Today we know that many brain parameters are inherited, and not the result of environmental influences. For example, the volume of the cerebral cortex is inherited by 83%, and the ratio of gray and white matter in identical twins is almost identical. The level of IQ, of course, does not depend on the size of the brain, but it is also partly recognized as a 50% hereditary parameter.
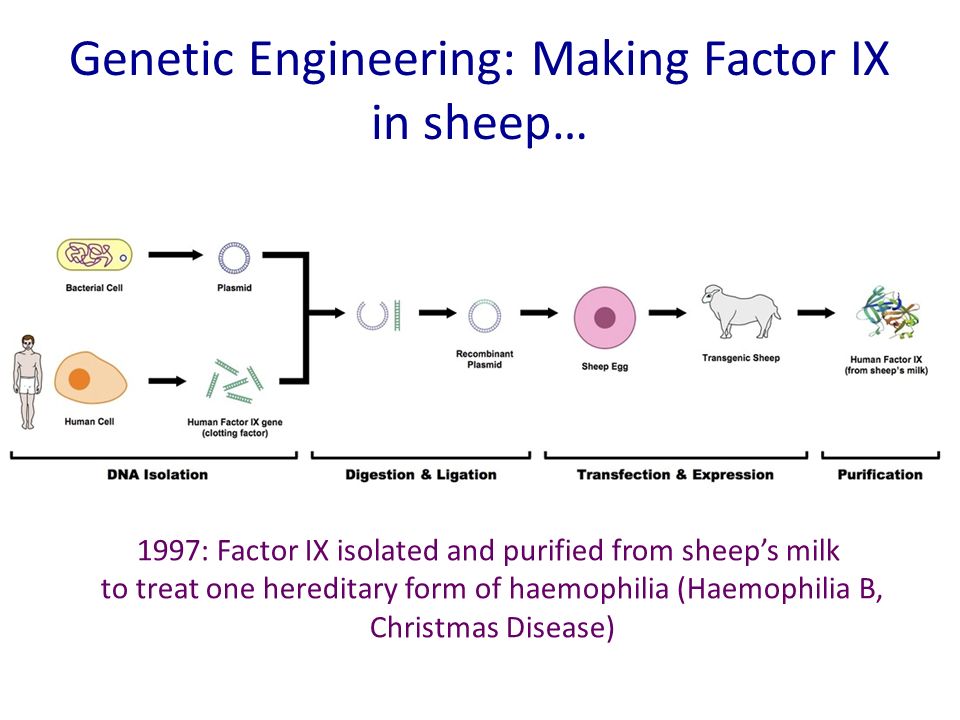
Unfortunately, today we know no more about the mechanisms of inheritance of high IQ than about schizophrenia. More recently, 200 experts studied genome fragments from more than 126,500 participants, but as a result they found only that the coding elements associated with IQ are located on the 1st, 2nd and 6th chromosomes. Scientists are confident that the picture will become clearer when more people take part in the experiments. In addition, in the case of IQ, it seems that a new system for isolating the necessary sections of the genome is needed: you need to look for it on the X chromosome. Researchers have long noted that boys are more likely to be mentally retarded (IQ < 70) than girls. Obviously, this happens because of the X chromosome: men have one, while women have two. The X chromosome is associated with more than 150 disorders, including hemophilia and Duchenne muscular dystrophy. In order for a girl to manifest genetically determined mental retardation (or hemophilia, or another similar pathology), the mutation must occur in two places at once, while in the case of a boy, one anomaly is enough. nine0005
Researchers have long noted that boys are more likely to be mentally retarded (IQ < 70) than girls. Obviously, this happens because of the X chromosome: men have one, while women have two. The X chromosome is associated with more than 150 disorders, including hemophilia and Duchenne muscular dystrophy. In order for a girl to manifest genetically determined mental retardation (or hemophilia, or another similar pathology), the mutation must occur in two places at once, while in the case of a boy, one anomaly is enough. nine0005
Anna Kozlova
geneticist, specialist of the laboratory of sports pharmacology and nutrition of the Republican Scientific and Practical Center for Sports (Minsk)
“There are a number of hereditary diseases, one of the symptoms of which is mental retardation: as a rule, these are violations of the number or structure of chromosomes. The classic example is Down syndrome; lesser known ones - for example, Williams syndrome (elf face syndrome), Angelman syndrome, and so on. But there are also mutations of individual genes. In total, there are more than a thousand genes in which mutations can lead to mental retardation of one degree or another, according to the latest data. nine0005
But there are also mutations of individual genes. In total, there are more than a thousand genes in which mutations can lead to mental retardation of one degree or another, according to the latest data. nine0005
In addition, there are a number of disorders that are polygenic in nature - they are also called multifactorial. Their appearance and development is determined not only by heredity, but also by the influence of the environment, and if we are talking about hereditary factors, then this is always the result of the action of not one, but many genes. Today, such illnesses are considered to include schizophrenia, autism spectrum disorders, depressive spectrum disorders (clinical depression, postpartum depression), bipolar affective disorder (what used to be known as manic-depressive psychosis), manic syndrome, and others.
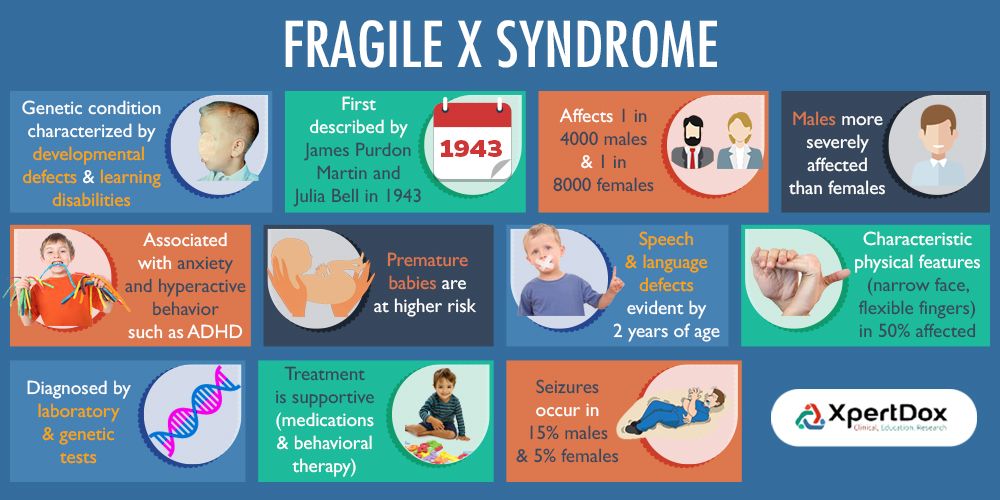
Apart from obvious chromosomal diseases (say, Down syndrome - trisomy of the 21st chromosome, Williams syndrome - microdeletion of chromosome 7q11.23, and so on), then there is, for example, fragile X syndrome, in which mutation of a specific gene on the X chromosome, which causes, among other things, mental retardation. In general, a fairly significant number of such pathologies are associated with mutations in the X chromosome, and they are well studied.
In general, a fairly significant number of such pathologies are associated with mutations in the X chromosome, and they are well studied.
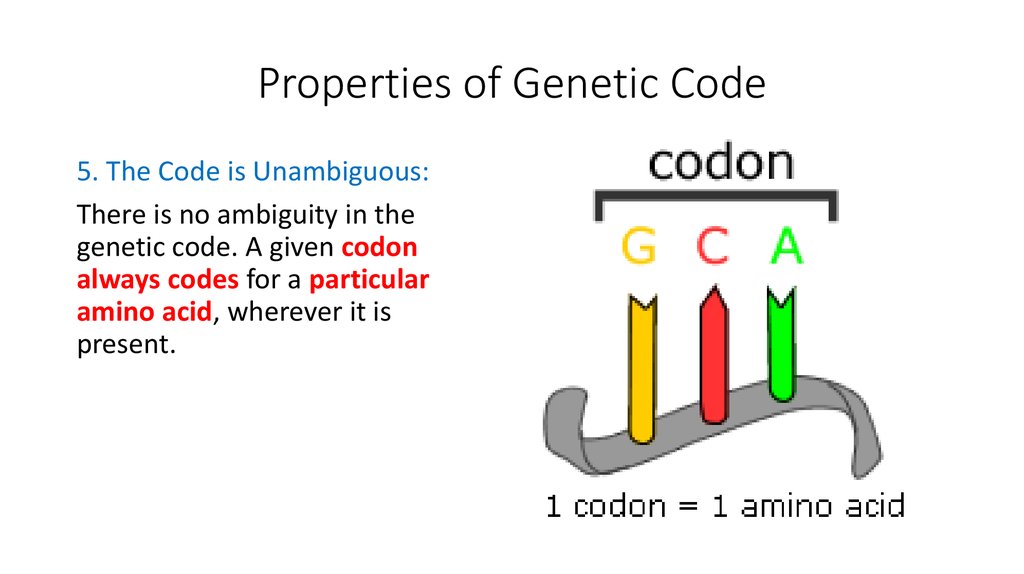
Regarding the influence of hereditary factors on IQ, as far as I know, there is no exact and unambiguous answer yet (except for situations where one of the symptoms of a hereditary disease is a decrease in intelligence). In general, only the so-called "reaction norm" is genetically determined, that is, the range of variability of a trait, and how this is realized within the range is already associated with environmental conditions (upbringing, training, stress, living conditions). It is believed that intelligence is just a classic example of a trait for which a fairly wide range, rather than a specific IQ value, is genetically determined. But at the same time, there are a number of polymorphic alleles, for which, for example, an association has been shown with maintaining the level of cognitive abilities under conditions of increased physical and mental stress. According to various sources, the influence of hereditary factors on memory ranges from 35% to 70%, and on IQ and attention - from 30% to 85%. nine0005
According to various sources, the influence of hereditary factors on memory ranges from 35% to 70%, and on IQ and attention - from 30% to 85%. nine0005
Psychogenetics deals with the study of how hereditary factors influence the mental qualities of a living being. For example, the influence of individual genetic characteristics on temperament, aggressiveness, indicators of introversion-extroversion, novelty seeking, avoidance of harm (damage), dependence on rewards (encouragement), IQ, memory, attention, reaction speed, speed of disjunctive response (responding to situations with mutually exclusive choice) and other qualities. But in general, unlike most morphological and biochemical traits, mental characteristics are less dependent on genetics. The more complex a person's behavioral activity, the greater the role of the environment and the less of the genome. That is, for simple motor skills, heritability is higher than for complex ones; for indicators of intelligence - higher than for personality traits, and the like. On average (the spread of data, unfortunately, is quite large: this is due to differences in methods, sample sizes, insufficient consideration of population characteristics), the heritability of mental characteristics rarely exceeds 50–70%. For comparison: the contribution of genetics to the type of constitution reaches 98%.
On average (the spread of data, unfortunately, is quite large: this is due to differences in methods, sample sizes, insufficient consideration of population characteristics), the heritability of mental characteristics rarely exceeds 50–70%. For comparison: the contribution of genetics to the type of constitution reaches 98%.
Why is that? In particular, because a huge number of genes are involved in the formation of these features (complex and complex), and the more genes are involved in any process, the lower the contribution of each individually. For example, if we have ten varieties of receptors that are susceptible to one neurotransmitter, and each is encoded by a separate gene, then a decrease in expression or even a knockout of one of the genes will not turn off the entire system as a whole.
Icons: 1) A.L. Hu, 2) Aenne Brielmann, 3) Michael Thompson, 4) Alex Auda Samora — from the Noun Project. nine0076
Glycogenoses. What is Glycogenosis?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment.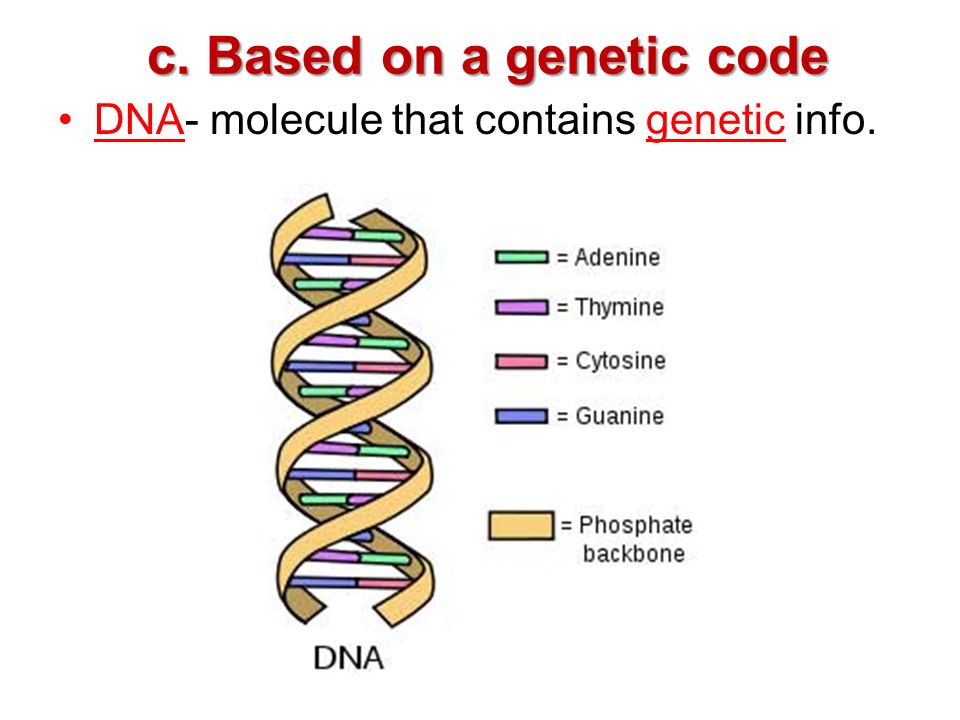 In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Glycogenoses are hereditary diseases based on a genetic defect in the production of enzymes involved in the metabolism of carbohydrates. A characteristic common symptom is the excessive deposition of glycogen in myocytes, hepatocytes and other cells of the body. Glycogenoses are manifested by symptoms of hypoglycemia, hepatomegaly, muscle weakness, hepatic, cardiac, respiratory and renal failure. Diagnostics includes a biochemical blood test, a morphological study of muscle and liver biopsy material, the determination of enzyme activity, and molecular genetic tests. Treatment is based on therapeutic nutrition, drug correction of metabolic disorders, in some cases surgery is required. nine0005
ICD-10
E74.0 Glycogen storage diseases
- Causes of glycogenoses
- Pathogenesis
- Classification
- Symptoms of glycogenoses
- Complications
- Diagnostics
- Treatment of glycogenosis
- Prognosis and prevention
- Prices for treatment
General
Glycogenoses have been studied since 1910.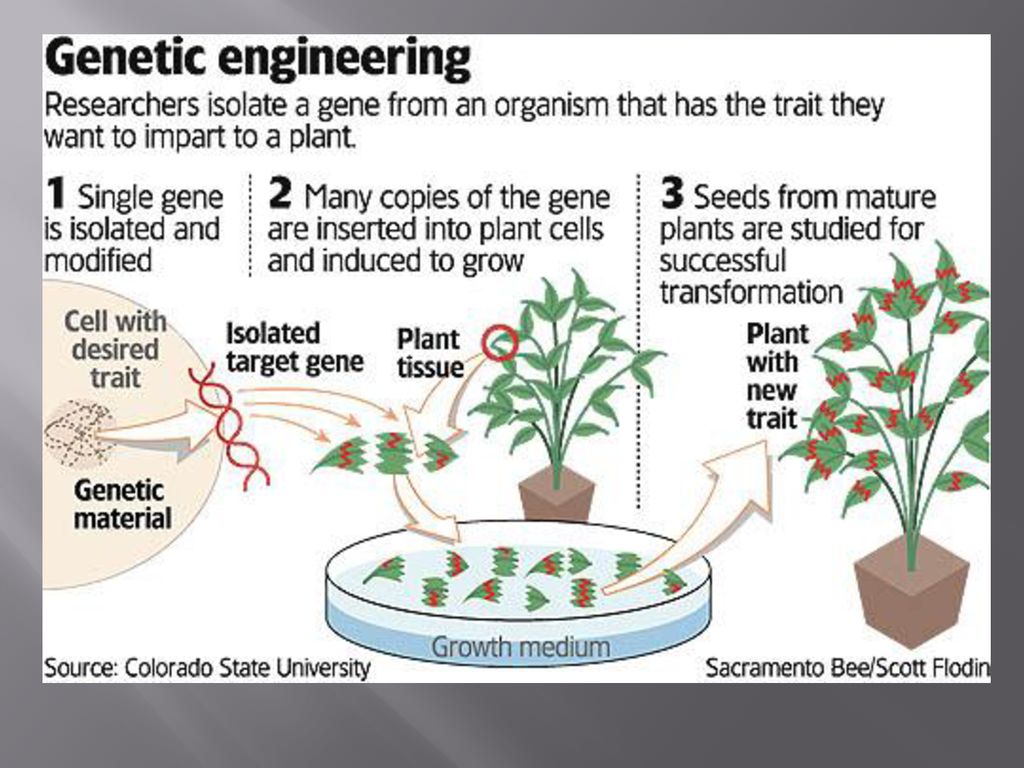 In 1928-29, the symptoms of type I glycogenosis - "glycogen storage disease" - were described. Only at 1952 succeeded in identifying an enzyme defect and establishing its connection with the development of symptoms. Pathogenetic mechanisms and methods of treatment are still not fully understood. To date, 12 types of glycogenosis have been identified, 9 have been most fully studied. The prevalence is low, on average 1 case per 40-68 thousand of the population. Epidemiological indicators are the same among both sexes, but with X-recessive inheritance, men get sick more often. Symptoms appear in the neonatal period or in early childhood, the course is often continuously progressive. nine0005
In 1928-29, the symptoms of type I glycogenosis - "glycogen storage disease" - were described. Only at 1952 succeeded in identifying an enzyme defect and establishing its connection with the development of symptoms. Pathogenetic mechanisms and methods of treatment are still not fully understood. To date, 12 types of glycogenosis have been identified, 9 have been most fully studied. The prevalence is low, on average 1 case per 40-68 thousand of the population. Epidemiological indicators are the same among both sexes, but with X-recessive inheritance, men get sick more often. Symptoms appear in the neonatal period or in early childhood, the course is often continuously progressive. nine0005
Glycogenoses
Causes of glycogenoses
The only factor provoking the development of glycogen diseases is a genetic defect, which results in a deficiency of a certain enzyme involved in glucose metabolism. All glycogenoses, with the exception of type IX, are inherited in an autosomal recessive manner.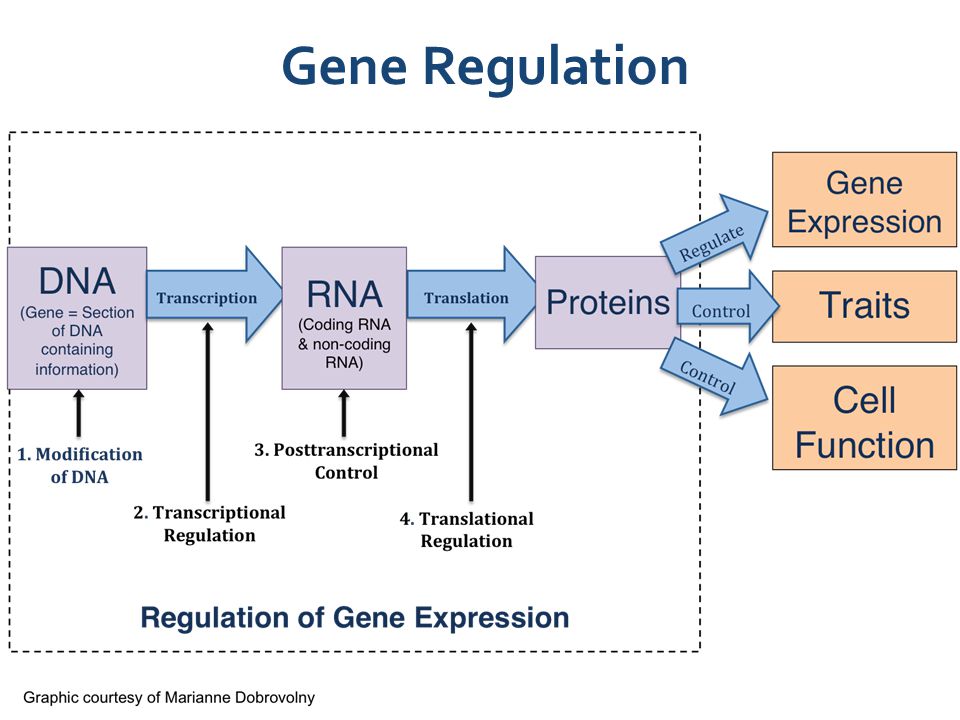 This means that the mutational gene is located on a chromosome that is not sex-linked, the manifestation of the disease is possible only when the mutations are inherited from each of the parents - if there are two recessive altered genes in the allele. If one gene from a pair is defective, then the other - dominant, normal - provides the body with a sufficient amount of the enzyme. At the same time, a person becomes a carrier of glycogenosis, but does not get sick. In couples where both partners are carriers, the probability of having an affected child is 25%. In type IX glycogenosis, the abnormal gene is located on the sex X chromosome. Hemizygous males have an XY pair, always have glycogenosis, and pass the defect on to all their daughters. The probability of passing the mutation from a female carrier to children of both sexes is 50%. nine0005
This means that the mutational gene is located on a chromosome that is not sex-linked, the manifestation of the disease is possible only when the mutations are inherited from each of the parents - if there are two recessive altered genes in the allele. If one gene from a pair is defective, then the other - dominant, normal - provides the body with a sufficient amount of the enzyme. At the same time, a person becomes a carrier of glycogenosis, but does not get sick. In couples where both partners are carriers, the probability of having an affected child is 25%. In type IX glycogenosis, the abnormal gene is located on the sex X chromosome. Hemizygous males have an XY pair, always have glycogenosis, and pass the defect on to all their daughters. The probability of passing the mutation from a female carrier to children of both sexes is 50%. nine0005
Pathogenesis
The pathogenetic basis of all glycogenosis is the impossibility of the process of synthesis and breakdown of glycogen, its accumulation in tissues.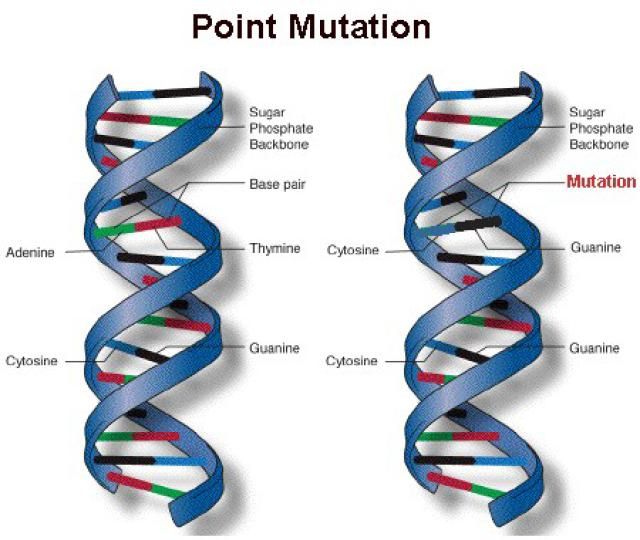 Glycogen is the only reserve polysaccharide of the body, a kind of energy "depot" - after eating, excess glucose is converted into liver and muscle glycogen, then gradually broken down back to glucose. Thanks to this mechanism, a stable level of sugar in the blood plasma is maintained, the cells and tissues of the body are continuously provided with energy. With aglycogenosis (type 0) - there is no enzyme glycogen synthetase, which is responsible for the production of glycogen. Patients suffer from severe hypoglycemia. nine0005
Glycogen is the only reserve polysaccharide of the body, a kind of energy "depot" - after eating, excess glucose is converted into liver and muscle glycogen, then gradually broken down back to glucose. Thanks to this mechanism, a stable level of sugar in the blood plasma is maintained, the cells and tissues of the body are continuously provided with energy. With aglycogenosis (type 0) - there is no enzyme glycogen synthetase, which is responsible for the production of glycogen. Patients suffer from severe hypoglycemia. nine0005
In glycogen diseases types 1-11, a genetically determined deficiency of an enzyme that catalyzes the glucose-glycogen-glucose chain occurs. Type 1 is characterized by a defect in glucose-6-phosphatase and glucose-6-phosphate translocase, type 2 - alpha-1,4-glucosidase, type 3 - amyl-1,6-glucosidase, type 4 - D-1,4-glucano-α -glucosyltransferases, type 5 - myocyte glycogen phosphorylase, type 6 - hepatocyte starch phosphorylase, type 7 - phosphoglucomutase, type 8 - phosphofructomutase, type 9 - hepatocyte phosphorylase kinase.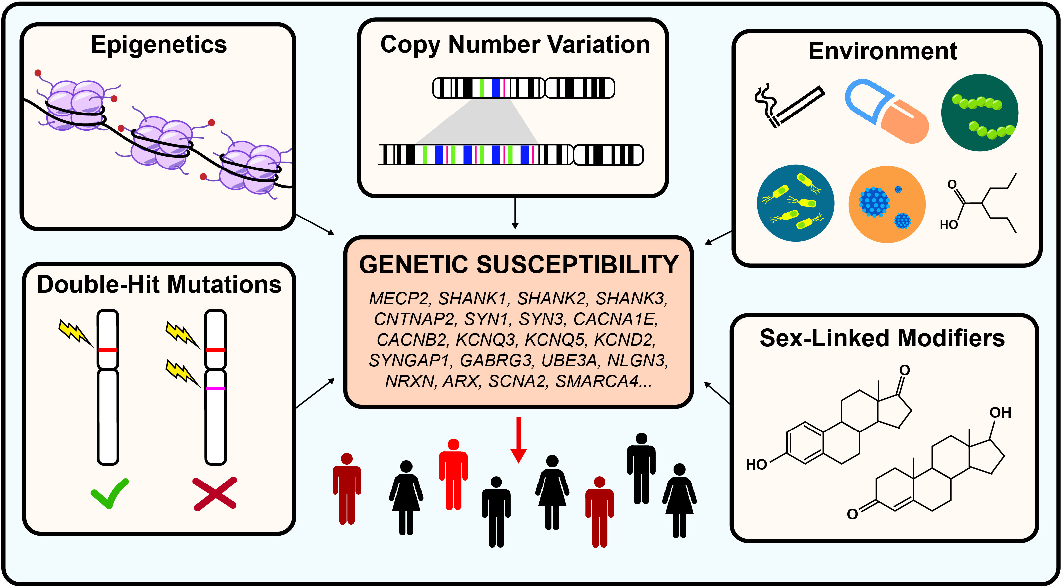 Due to the reduced activity or complete absence of the enzyme, glycogen accumulates in the muscles, liver, and rarely in other tissues. The structure and functionality of organs changes, various forms of organ failure develop. nine0005
Due to the reduced activity or complete absence of the enzyme, glycogen accumulates in the muscles, liver, and rarely in other tissues. The structure and functionality of organs changes, various forms of organ failure develop. nine0005
Classification
Taking into account the enzymatic defect and the characteristics of clinical manifestations, 12 variants of glycogenoses are distinguished, from 0 to XI. In addition, cases of combined types are described, when a deficiency of two enzymes is determined, as well as cases of unidentifiable types, in which it is not possible to isolate the enzyme defect. According to the leading pathogenetic mechanism, glycogen diseases are divided into three large groups:
- Hepatic. Includes glycogenoses of all types except II, V and VII. Glycogen is deposited mainly in hepatocytes. Characterized by hepatomegaly, hypoglycemia 2 hours after the intake of carbohydrates. In type I disease, the kidneys are also affected; in types III and IV, myopathies develop.
 nine0094
nine0094 - Muscular. This group includes diseases of types VII and V. The enzymatic activity in the muscle tissue is changed, the energy supply of the muscles is disrupted. Typical symptoms are myalgia, convulsions.
- Mixed. Type II glycogenosis differs in that all glycogen-containing tissues are involved in the pathological process. Glycogen accumulates in the lysosomes and cytoplasm of cells. Many organs are affected, and the risk of death due to heart or respiratory failure increases.
Symptoms of glycogenosis
Aglycogenosis develops in the neonatal period or early childhood. The low content of glycogen in the liver is manifested by pronounced hypoglycemia on an empty stomach. There is lethargy, deep sleep, loss of consciousness, pale skin, nausea, vomiting, convulsions at night and in the morning. Outwardly, patients are short, have low bone density, and an increased risk of fractures. With Gierke's disease (type I), symptoms debut in the first 4 months of life.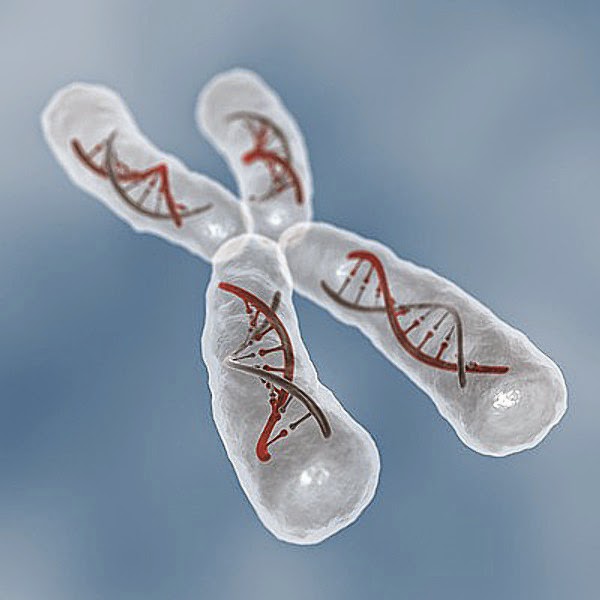 Characterized by poor appetite, bouts of vomiting, lack of weight, enlarged liver, disproportionate body structure - a round face, a large belly, thin limbs. nine0005
Characterized by poor appetite, bouts of vomiting, lack of weight, enlarged liver, disproportionate body structure - a round face, a large belly, thin limbs. nine0005
Clinical signs of Pompe disease (type II) are determined within a few weeks after birth. Children are lethargic, inactive, with a weakened sucking reflex, reduced appetite. Hepatomegaly changes the proportions of the body - the abdomen increases, the arms and legs remain thin. The heart, lungs, nervous system are affected. High risk of heart and lung failure. Patients with Forbes disease (type III) have mild to moderate symptoms. The hypoglycemia of the post-absorption period, hepatomegaly, and the accumulation of subcutaneous fat in the trunk area come to the fore. The leading symptoms of Andersen's disease (type IV) are muscle weakness, poor exercise tolerance, convulsions. nine0005
Thomson's disease is represented by hepatomegaly, nystagmus, ataxia, progressive neurological disorders with muscular hypertension, decerebration. Typical manifestations of McArdle's disease (type V) are pain, spasmodic contractions, excessive fatigue and muscle weakness even after a slight load. Sometimes tonic convulsions become generalized, which is accompanied by general stiffness. The manifestations of Hers disease (type VI) are less pronounced, patients are able to endure light and moderate physical activity without experiencing discomfort. Additionally, signs of liver damage are found - appetite suppression, vomiting, nausea, pain in the right side. nine0005
Typical manifestations of McArdle's disease (type V) are pain, spasmodic contractions, excessive fatigue and muscle weakness even after a slight load. Sometimes tonic convulsions become generalized, which is accompanied by general stiffness. The manifestations of Hers disease (type VI) are less pronounced, patients are able to endure light and moderate physical activity without experiencing discomfort. Additionally, signs of liver damage are found - appetite suppression, vomiting, nausea, pain in the right side. nine0005
The course of Tarui disease (type VII) includes exercise intolerance, accompanied by nausea and vomiting, and painful muscle spasms. Glucose intake does not increase the ability to perform physical activities. Symptoms worsen after eating. The mildest course is characteristic of Haga's disease (type IX). In sick children, the liver enlarges, motor development and growth are delayed, and muscle hypotension is formed. Symptoms improve on their own with age.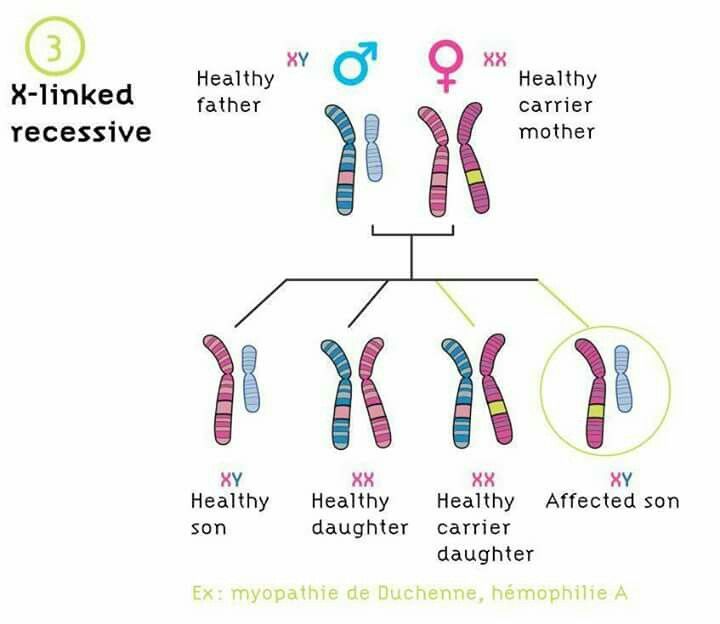 Glycogenosis type X is extremely rare, characterized by hepatomegaly, with a long course, exercise tolerance decreases. Type XI glycogenosis is accompanied by a significant increase in the liver, growth retardation and physical development, and rickets. In adolescents, there is often a decrease in the volume of the liver, acceleration of growth. nine0005
Glycogenosis type X is extremely rare, characterized by hepatomegaly, with a long course, exercise tolerance decreases. Type XI glycogenosis is accompanied by a significant increase in the liver, growth retardation and physical development, and rickets. In adolescents, there is often a decrease in the volume of the liver, acceleration of growth. nine0005
Complications
With varieties of glycogenosis, accompanied by hypoglycemia, there is a risk of developing hypoglycemic coma. As a rule, a pronounced decrease in blood glucose occurs when you skip meals, especially after a night's sleep (skipping breakfast). Patients experience dizziness and convulsions, lose consciousness. Severe forms of muscle glycogenosis with prolonged course and lack of therapy lead to skeletal muscle dystrophy, heart failure. Cirrhosis of the liver is a complication of some hepatic glycogenoses. nine0005
Diagnostics
If glycogenosis is suspected, the child is advised to consult a geneticist, pediatrician, gastroenterologist, hepatologist.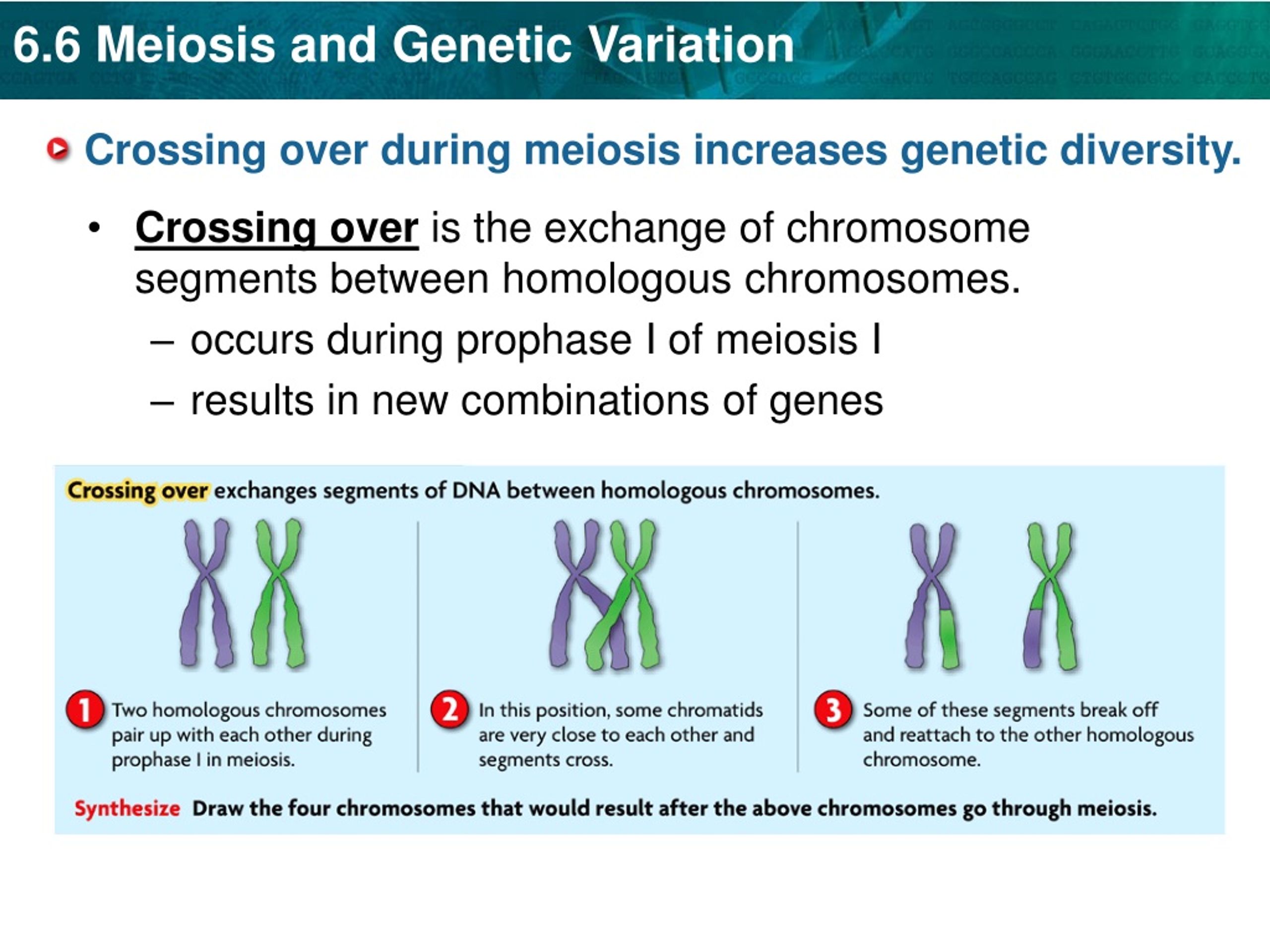 First of all, the specialist collects an anamnesis, conducts a clinical interview and examination. Because the disease is transmitted in an autosomal recessive manner, familial cases are rare. Complaints of weakness, apathy of the child, pallor and yellowness of the skin, refusal to eat or increased appetite, difficulty waking up in the morning, tremors, convulsions are common. On examination, the doctor notes an increase in the size of the liver, bulging of the abdomen, growth retardation, muscle wasting, specific deposition of subcutaneous fat, xanthomas. Laboratory and instrumental methods allow confirming the diagnosis of glycogenosis, excluding congenital syphilis, toxoplasmosis, cytomegaly, liver pathologies, Gaucher disease, myotonia, progressive muscular dystrophy, amyotrophy. Mandatory research methods include: nine0005
First of all, the specialist collects an anamnesis, conducts a clinical interview and examination. Because the disease is transmitted in an autosomal recessive manner, familial cases are rare. Complaints of weakness, apathy of the child, pallor and yellowness of the skin, refusal to eat or increased appetite, difficulty waking up in the morning, tremors, convulsions are common. On examination, the doctor notes an increase in the size of the liver, bulging of the abdomen, growth retardation, muscle wasting, specific deposition of subcutaneous fat, xanthomas. Laboratory and instrumental methods allow confirming the diagnosis of glycogenosis, excluding congenital syphilis, toxoplasmosis, cytomegaly, liver pathologies, Gaucher disease, myotonia, progressive muscular dystrophy, amyotrophy. Mandatory research methods include: nine0005
- Biochemical blood test. According to the results of the analysis, hypoglycemia is detected with a fasting glucose level of 0.6-3 mmol / l, lactic acidosis with a lactic acid concentration of 3-10 mmol / l (except for type 4 glycogenosis).
 Additionally, an increase in triglycerides, total cholesterol, LDL, VLDL, uric acid, liver enzymes is detected.
Additionally, an increase in triglycerides, total cholesterol, LDL, VLDL, uric acid, liver enzymes is detected. - Examination of a biopsy of the liver, muscles. When studying liver tissue, the most common characteristics are an increased amount of glycogen and its clumpy distribution in the cytoplasm of hepatocytes, sometimes in vacuolated nuclei. A pronounced protein and / or large- and small-drop fatty degeneration of hepatocytes, their necrosis, limited foci of fibrosis in places of cell death are determined. There may be signs of cirrhosis. In muscle types of diseases, a muscle biopsy is examined, in which subsarcolemmal accumulations of structurally normal glycogen are seen. nine0094
- Research of enzymes. The activity of enzymes is studied in the culture of skin fibroblasts, biopsy of muscle and liver tissue, leukocytes. In glycogenosis with a chronic slowly progressive course, the decrease in the functionality of the enzyme is mild or moderate. In severe cases, the enzyme is absent or its activity is minimal.
- Abdominal ultrasound. There is marked enlargement of the liver, especially its left lobe. Characterized by hyperechogenicity and structural diffuse heterogeneity of the parenchyma (multiple small hyperechoic echoes distributed evenly). In the distal parts of the parenchyma, the passage of ultrasound is weakened. Perhaps the detection of structurally diverse hepatic adenomas, an increase in the size of the kidneys, spleen and pancreas. nine0094
The complex of diagnostic studies is selected individually depending on the age of the patient and the presumed type of glycogen disease. Molecular genetic diagnostics (gene sequencing to detect mutations), electromyography, ECHO-KG, OAC, coagulogram may be required.
Treatment of glycogenosis
Specific methods of therapy have not been developed. Pathogenetic treatment is carried out conservatively, aimed at eliminating hypoglycemia, metabolic acidosis, ketosis, hyperlipidemia, correction of dysfunction of the hepatobiliary complex and the gastrointestinal tract. With the development of complications (serious damage to internal organs), surgical operations are performed. Medical care for patients includes the following areas: nine0005
With the development of complications (serious damage to internal organs), surgical operations are performed. Medical care for patients includes the following areas: nine0005
- Diet therapy. To minimize metabolic disturbances, an individual nutrition plan is drawn up. Patients are advised to reduce the amount of fat, sucrose, fructose and galactose to reduce hyperlipidemia and acidosis. In the first type of glycogenosis, a diet with increased carbohydrate intake is prescribed. In particular, the use of raw corn starch with slow digestibility is shown, which helps to prevent hypoglycemia. In types 3, 4 and 9, a diet with a predominance of animal protein and fractional nutrition is introduced. nine0094
- Drug treatment of symptoms. As part of complex treatment, cocarboxylase is used to increase the production of acetylcoenzyme A, corticosteroids and glucagon to stimulate gluconeogenesis. Carnitine deficiency is compensated by levocarnitine. With secondary tubulopathies, hepatic and biliary dysfunctions, choleretic drugs, hepatoprotectors, lipotropic substances are used.
 With signs of acidosis, alkaline solutions are indicated intravenously. With renal dysfunction, proteinuria - ACE inhibitors. For hyperuricemia, uricodepressors. With neutropenia - granulocyte colony-stimulating factor. nine0094
With signs of acidosis, alkaline solutions are indicated intravenously. With renal dysfunction, proteinuria - ACE inhibitors. For hyperuricemia, uricodepressors. With neutropenia - granulocyte colony-stimulating factor. nine0094 - Surgical treatment. Patients with severe fatal liver injury may require orthotopic organ transplantation. The indication for surgery is cirrhosis with complications, often developing in the third and fourth types of pathology. In some cases, surgical intervention is advisable for liver adenomas with a high risk of transformation into a malignant tumor. Kidney transplantation is sometimes performed in patients with chronic renal failure.
Prognosis and prevention
The effectiveness of therapy, the likelihood of complications and death depend on the type of pathology. Some glycogenoses slightly worsen the quality of life of patients, are compensated as they grow older, others are not amenable to treatment and inevitably end in death.