Intrusive thoughts disorder
Obsessive-compulsive disorder (OCD) - Symptoms and causes
Overview
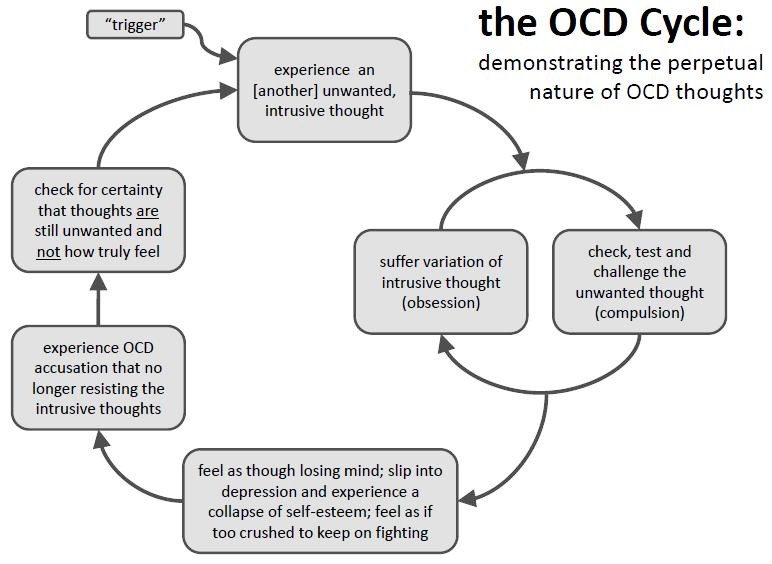
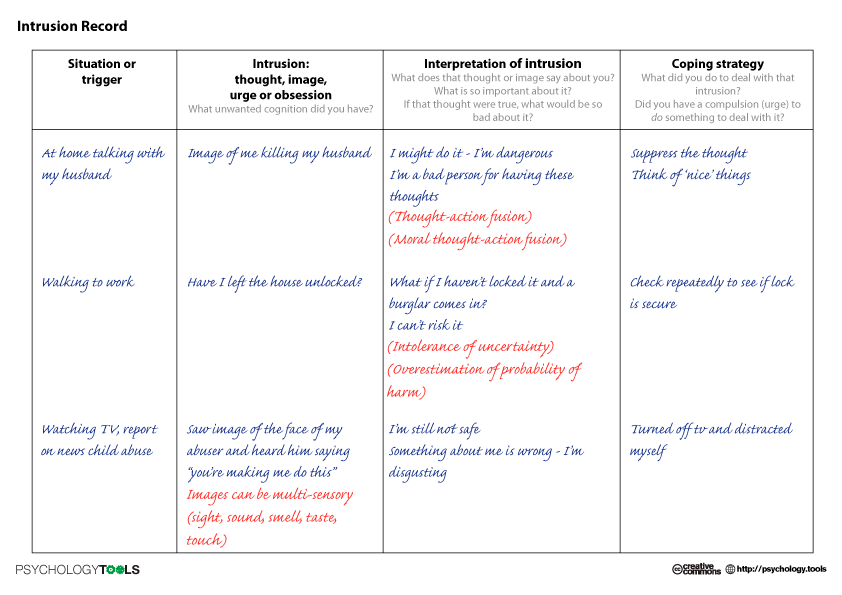
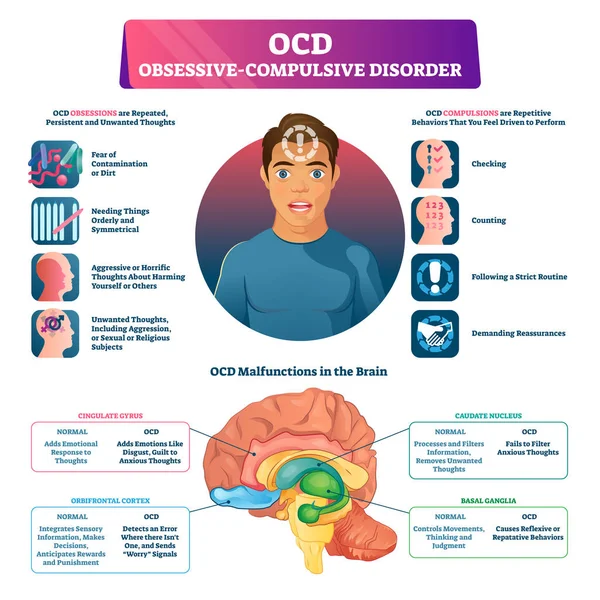
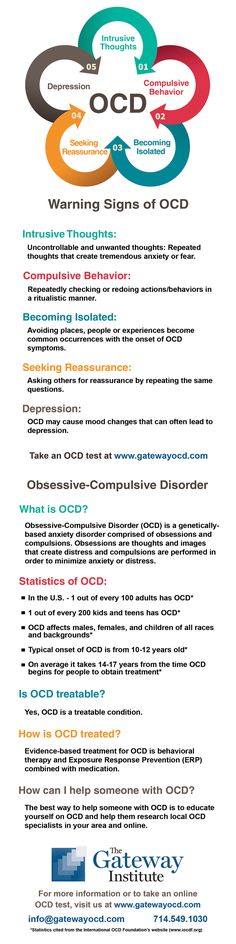
Obsessive-compulsive disorder (OCD) features a pattern of unwanted thoughts and fears (obsessions) that lead you to do repetitive behaviors (compulsions). These obsessions and compulsions interfere with daily activities and cause significant distress.
You may try to ignore or stop your obsessions, but that only increases your distress and anxiety. Ultimately, you feel driven to perform compulsive acts to try to ease your stress. Despite efforts to ignore or get rid of bothersome thoughts or urges, they keep coming back. This leads to more ritualistic behavior — the vicious cycle of OCD.
OCD often centers around certain themes — for example, an excessive fear of getting contaminated by germs. To ease your contamination fears, you may compulsively wash your hands until they're sore and chapped.
If you have OCD, you may be ashamed and embarrassed about the condition, but treatment can be effective.
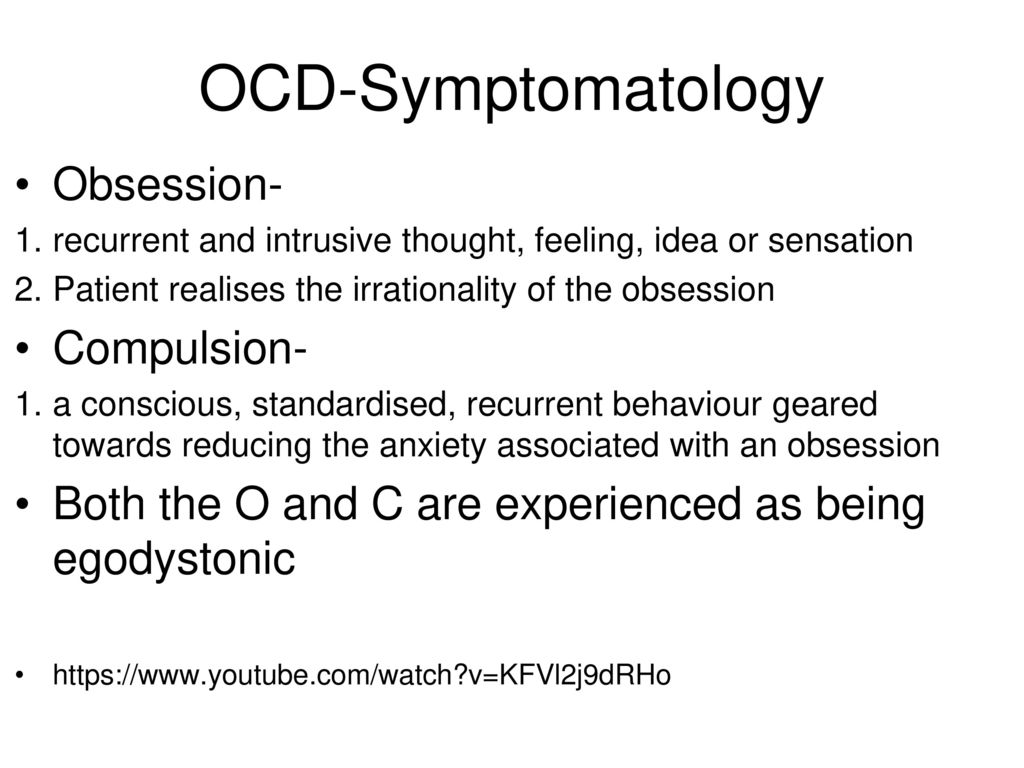
Symptoms
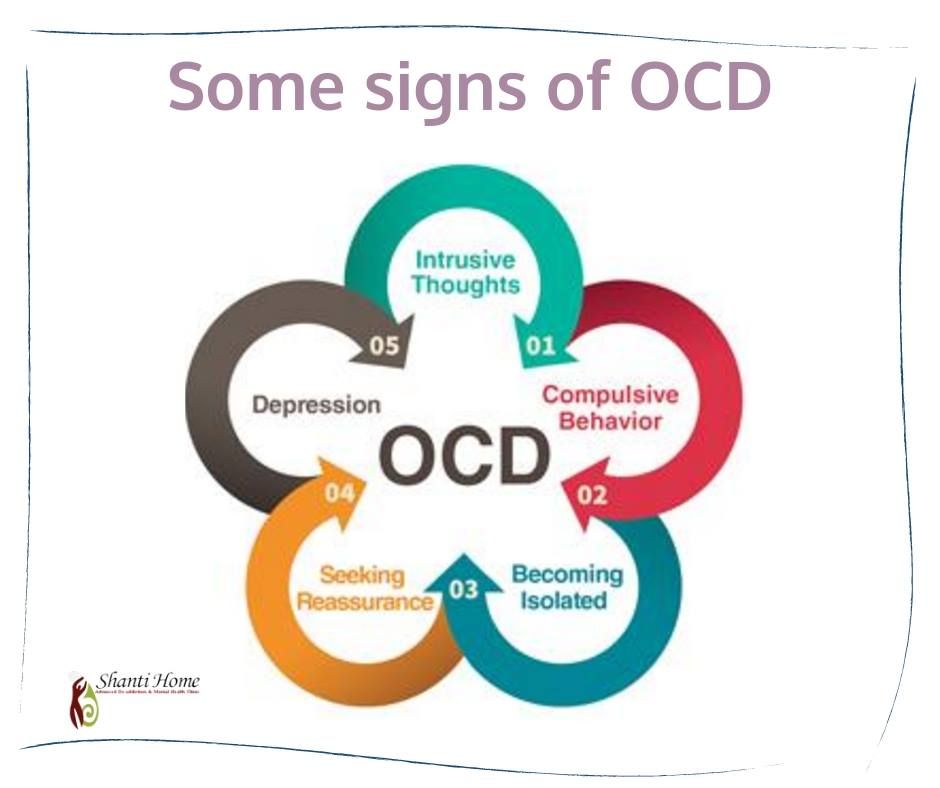
Obsessive-compulsive disorder usually includes both obsessions and compulsions. But it's also possible to have only obsession symptoms or only compulsion symptoms. You may or may not realize that your obsessions and compulsions are excessive or unreasonable, but they take up a great deal of time and interfere with your daily routine and social, school or work functioning.
Obsession symptoms
OCD obsessions are repeated, persistent and unwanted thoughts, urges or images that are intrusive and cause distress or anxiety. You might try to ignore them or get rid of them by performing a compulsive behavior or ritual. These obsessions typically intrude when you're trying to think of or do other things.
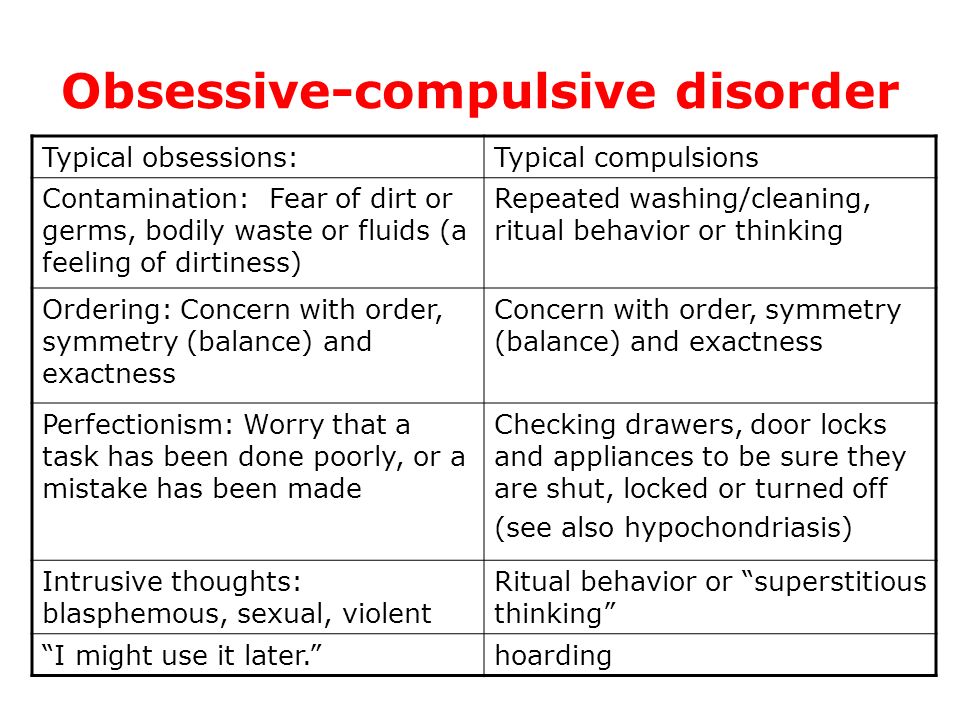
Obsessions often have themes to them, such as:
- Fear of contamination or dirt
- Doubting and having difficulty tolerating uncertainty
- Needing things orderly and symmetrical
- Aggressive or horrific thoughts about losing control and harming yourself or others
- Unwanted thoughts, including aggression, or sexual or religious subjects
Examples of obsession signs and symptoms include:
- Fear of being contaminated by touching objects others have touched
- Doubts that you've locked the door or turned off the stove
- Intense stress when objects aren't orderly or facing a certain way
- Images of driving your car into a crowd of people
- Thoughts about shouting obscenities or acting inappropriately in public
- Unpleasant sexual images
- Avoidance of situations that can trigger obsessions, such as shaking hands
Compulsion symptoms
OCD compulsions are repetitive behaviors that you feel driven to perform. These repetitive behaviors or mental acts are meant to reduce anxiety related to your obsessions or prevent something bad from happening. However, engaging in the compulsions brings no pleasure and may offer only a temporary relief from anxiety.
These repetitive behaviors or mental acts are meant to reduce anxiety related to your obsessions or prevent something bad from happening. However, engaging in the compulsions brings no pleasure and may offer only a temporary relief from anxiety.
You may make up rules or rituals to follow that help control your anxiety when you're having obsessive thoughts. These compulsions are excessive and often are not realistically related to the problem they're intended to fix.
As with obsessions, compulsions typically have themes, such as:
- Washing and cleaning
- Checking
- Counting
- Orderliness
- Following a strict routine
- Demanding reassurance
Examples of compulsion signs and symptoms include:
- Hand-washing until your skin becomes raw
- Checking doors repeatedly to make sure they're locked
- Checking the stove repeatedly to make sure it's off
- Counting in certain patterns
- Silently repeating a prayer, word or phrase
- Arranging your canned goods to face the same way
Severity varies
OCD usually begins in the teen or young adult years, but it can start in childhood.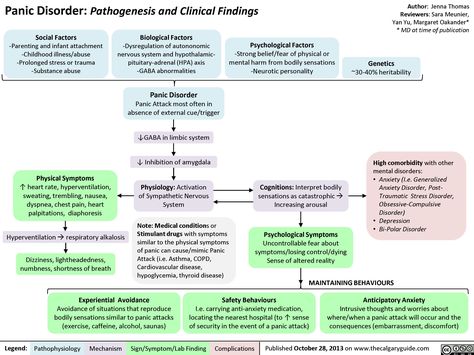 Symptoms usually begin gradually and tend to vary in severity throughout life. The types of obsessions and compulsions you experience can also change over time. Symptoms generally worsen when you experience greater stress. OCD, usually considered a lifelong disorder, can have mild to moderate symptoms or be so severe and time-consuming that it becomes disabling.
Symptoms usually begin gradually and tend to vary in severity throughout life. The types of obsessions and compulsions you experience can also change over time. Symptoms generally worsen when you experience greater stress. OCD, usually considered a lifelong disorder, can have mild to moderate symptoms or be so severe and time-consuming that it becomes disabling.
When to see a doctor
There's a difference between being a perfectionist — someone who requires flawless results or performance, for example — and having OCD. OCD thoughts aren't simply excessive worries about real problems in your life or liking to have things clean or arranged in a specific way.
If your obsessions and compulsions are affecting your quality of life, see your doctor or mental health professional.
Request an appointment
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health. Click here for an email preview.
Click here for an email preview.
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Causes
The cause of obsessive-compulsive disorder isn't fully understood. Main theories include:
- Biology.
 OCD may be a result of changes in your body's own natural chemistry or brain functions.
OCD may be a result of changes in your body's own natural chemistry or brain functions. - Genetics. OCD may have a genetic component, but specific genes have yet to be identified.
- Learning. Obsessive fears and compulsive behaviors can be learned from watching family members or gradually learned over time.
Risk factors
Factors that may increase the risk of developing or triggering obsessive-compulsive disorder include:
- Family history. Having parents or other family members with the disorder can increase your risk of developing OCD.
- Stressful life events. If you've experienced traumatic or stressful events, your risk may increase. This reaction may, for some reason, trigger the intrusive thoughts, rituals and emotional distress characteristic of OCD.
- Other mental health disorders. OCD may be related to other mental health disorders, such as anxiety disorders, depression, substance abuse or tic disorders.
Complications
Problems resulting from obsessive-compulsive disorder may include, among others:
- Excessive time spent engaging in ritualistic behaviors
- Health issues, such as contact dermatitis from frequent hand-washing
- Difficulty attending work, school or social activities
- Troubled relationships
- Overall poor quality of life
- Suicidal thoughts and behavior
Prevention
There's no sure way to prevent obsessive-compulsive disorder. However, getting treatment as soon as possible may help prevent OCD from worsening and disrupting activities and your daily routine.
By Mayo Clinic Staff
Related
Associated Procedures
Managing intrusive thoughts - Harvard Health
Disturbing thoughts that pop into your mind unbidden may make you feel uneasy, but they are common — and there are strategies you can use to manage them.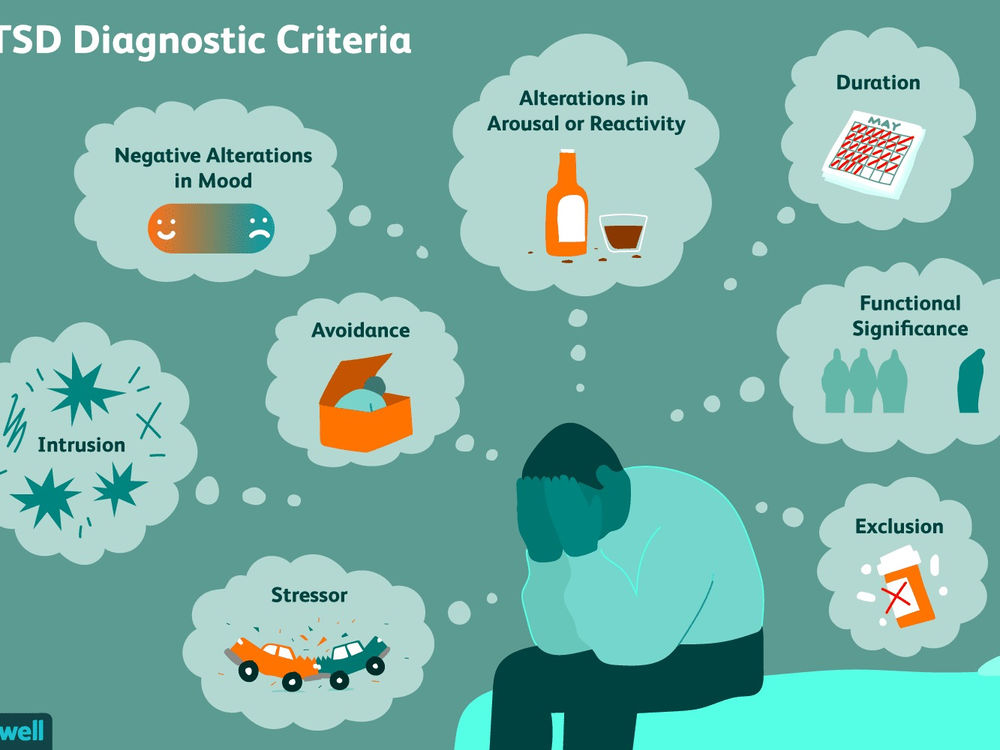
It seems to come out of nowhere — a strange, disturbing thought or a troubling image that pops into your mind. It might be violent or sexual, or a recurring fear that you’ll do something inappropriate or embarrassing. Whatever the content, it’s often unsettling and may bring on feelings of worry or shame. The more you try to push the thought from your mind, the more it persists.
Intrusive thoughts, as these are called, are thought to affect some six million Americans, according to the Anxiety and Depression Association of America.
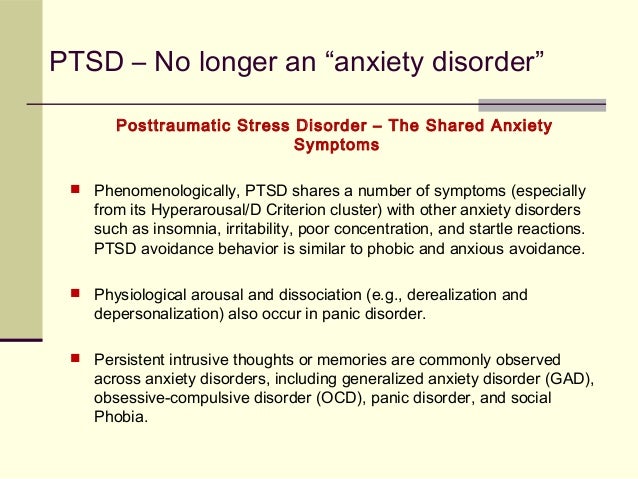
Sometimes intrusive thoughts are associated with a mental health disorder, such as obsessive-compulsive disorder, where thoughts become so bothersome that they prompt repetitive behaviors or compulsions to try to prevent them from occurring. They are also common in post-traumatic stress disorder, which can be triggered by a life-threatening or extremely stressful event, such as an accident or violent attack. But many people who experience these thoughts don’t have a mental health disorder, says Dr. Kerry-Ann Williams, a lecturer in psychiatry at Harvard Medical School.
Kerry-Ann Williams, a lecturer in psychiatry at Harvard Medical School.
Intrusive thoughts are often triggered by stress or anxiety. They may also be a short-term problem brought on by biological factors, such as hormone shifts. For example, a woman might experience an uptick in intrusive thoughts after the birth of a child.
"Any life stressor, if big enough, can increase your risk of having intrusive thoughts," says Dr. Williams.
Periods of stress and isolation
These days many women have experienced significant stress from the isolation caused by the pandemic, says Dr. Olivera Bogunovic, an assistant professor of psychiatry at Harvard Medical School. Anxiety symptoms may also commonly occur as women transition to a different stage of their life. They may become more isolated, or develop a fear of aging or of developing physical ailments, she says. This can lead to an uptick in anxiety, and in some instances, obsessive thinking.
While intrusive thoughts may be disturbing, they aren’t harmful or a sign that you have a secret desire to do the things that popped into your mind.
People are often too embarrassed or ashamed to talk about it, says Dr. Williams. "A lot of times when patients bring it up to me, they might preface it with something like, ‘I’m not crazy, but this weird thought comes into my mind,’" she says. "They might think about hurting a family member, such as a baby. When the thought happens, they’re horrified—‘I can’t even believe that came into my mind. I shouldn’t tell anyone; they might think something is wrong with me.’"
Identifying intrusive thoughts
So, how can you tell if you are experiencing intrusive thoughts? There are some signs to look for.
The thought is unusual for you. An intrusive thought is usually very different from your typical thoughts. "For example, it might be uncharacteristically violent," says Dr. Williams.
The thought is bothersome. If a thought is disturbing and it’s something you want to push out of your mind, it might be an intrusive thought.
The thought feels hard to control.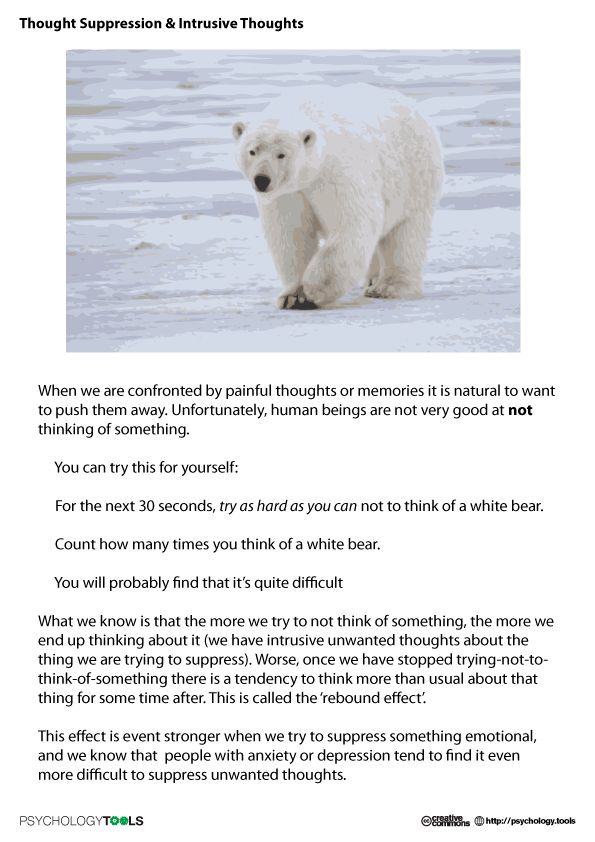 Intrusive thoughts are often repetitive and won’t go away.
Intrusive thoughts are often repetitive and won’t go away.
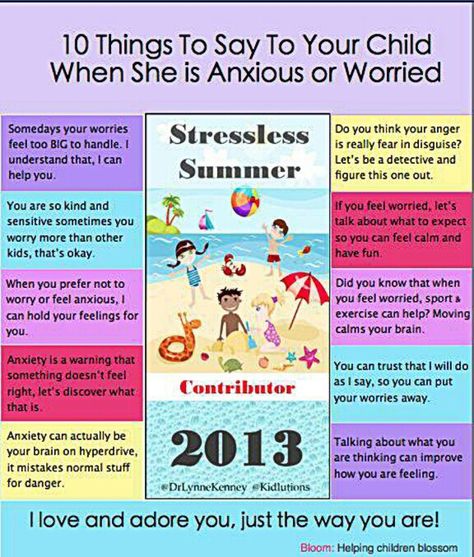
"The more you think about it, the more anxious you get and the worse the thoughts get," says Dr. Williams. Instead of fighting intrusive thoughts, it’s better to learn to live with them. When these thoughts emerge, try taking the following steps:
1. Identify the thought as intrusive. "Think to yourself, ‘that’s just an intrusive thought; it’s not how I think, it’s not what I believe, and it’s not what I want to do,’" says Dr. Williams.
2. Don’t fight with it. When you have an intrusive thought, just accept it. "Don’t try to make it go away."
3. Don’t judge yourself. Know that having a strange or disturbing thought doesn’t indicate that something is wrong with you.
When to seek help
See a mental health professional if unwanted thoughts are starting to disrupt your daily life, particularly if they’re impairing your ability to work or to do things you enjoy. However, even if intrusive thoughts aren’t affecting your life in a significant way, you can still see someone to get help.
However, even if intrusive thoughts aren’t affecting your life in a significant way, you can still see someone to get help.
Cognitive behavioral therapy is one strategy that is often successful in helping people manage intrusive thoughts. The process may help you to shift some of your general thought patterns, which can enable you to better manage these thoughts when they do occur and might lessen their frequency.
Intrusive thoughts can also be managed by addressing the underlying problem, such as anxiety, stress, or a personal history of trauma. While it may be helpful to share the particular thoughts you are having, keep in mind that even if you aren’t comfortable talking about them in detail, a therapist can still help. Women should also know that intrusive thoughts typically respond well to therapy, says Dr. Bogunovic.
"Keep in mind that you might not need help forever," says Dr. Williams. "It may be a very short-term thing."
Image: © Aleutie/Getty Images
Obsessional neurosis.
 What is obsessive compulsive disorder?
What is obsessive compulsive disorder? IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Obsessive-compulsive disorder is a mental disorder, which is based on obsessive thoughts, ideas and actions that occur outside the mind and will of a person. Obsessive thoughts often have content alien to the patient, however, despite all efforts, he cannot get rid of them on his own. The diagnostic algorithm includes a thorough questioning of the patient, his psychological testing, the exclusion of organic CNS pathology using neuroimaging methods. The treatment uses a combination of drug therapy (antidepressants, tranquilizers) with psychotherapy methods (thought stop method, autogenic training, cognitive behavioral therapy).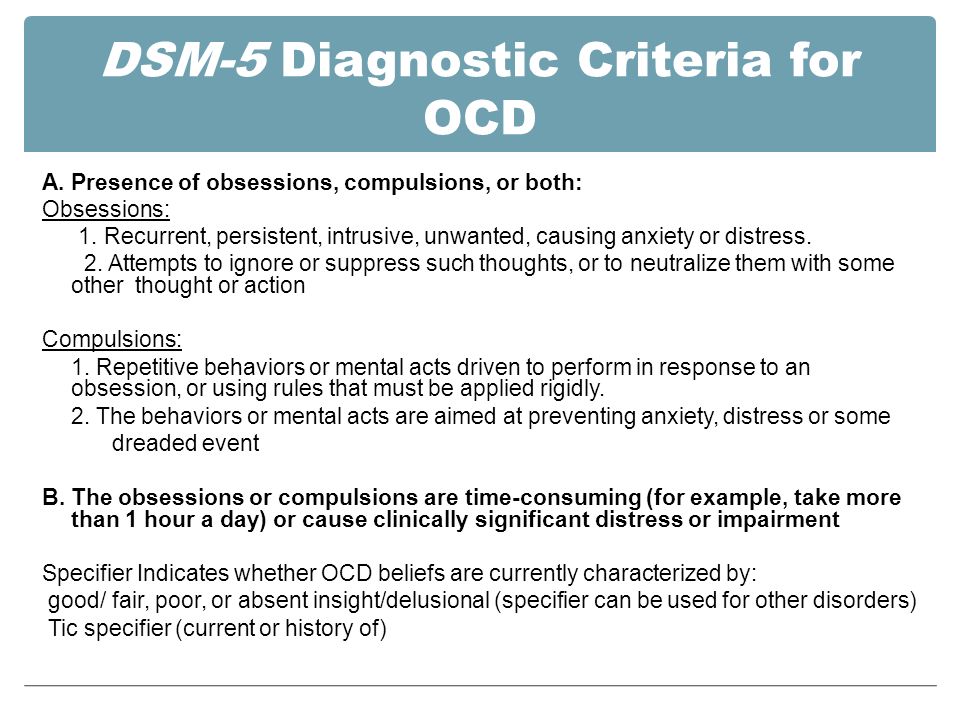
- Causes
- Symptoms and course of neurosis
- Types of obsessions
- Diagnostics
- Treatment
- Prognosis and prevention
- Prices for treatment
General
Obsessional neurosis was first described in 1827. Domenic Esquirol, who gave it the name "disease of doubt". Then the main feature of the obsessions that haunt the patient with this type of neurosis was determined - their alienation to the patient's consciousness. Currently, 2 main components of the clinic of obsessive-compulsive disorder have been identified: obsessions (obsessive thoughts) and compulsions (obsessive actions). In this regard, in practical neurology and psychiatry, the disease is also known as obsessive-compulsive disorder (OCD).
Obsessional neurosis is not as common as hysterical neurosis or neurasthenia. According to various sources, they suffer from 2 to 5% of the population of developed countries. The disease has no gender predisposition: it is equally often observed in both sexes. It should be noted that isolated obsessions (for example, fear of heights or fear of insects) are also observed in healthy people, but at the same time they are not of such an uncontrollable and irresistible character as in patients with neurosis.
The disease has no gender predisposition: it is equally often observed in both sexes. It should be noted that isolated obsessions (for example, fear of heights or fear of insects) are also observed in healthy people, but at the same time they are not of such an uncontrollable and irresistible character as in patients with neurosis.
obsessive-compulsive disorder
Causes
According to modern researchers, obsessive compulsive disorder is based on metabolic disorders of such neurotransmitters as norepinephrine and serotonin. The result is a pathological change in thought processes and increased anxiety. In turn, disturbances in the work of neurotransmitter systems can be caused by hereditary and acquired factors. In the first case, we are talking about inherited anomalies in the genes responsible for the synthesis of substances that are part of the neurotransmitter systems and affect their functioning. In the second case, among the OCD trigger factors, one can name various external influences that destabilize the work of the central nervous system: chronic stress, acute psychotrauma, TBI and other severe injuries, infectious diseases (viral hepatitis, infectious mononucleosis, measles), chronic somatic pathology (chronic pancreatitis, gastroduodenitis, pyelonephritis, hyperthyroidism).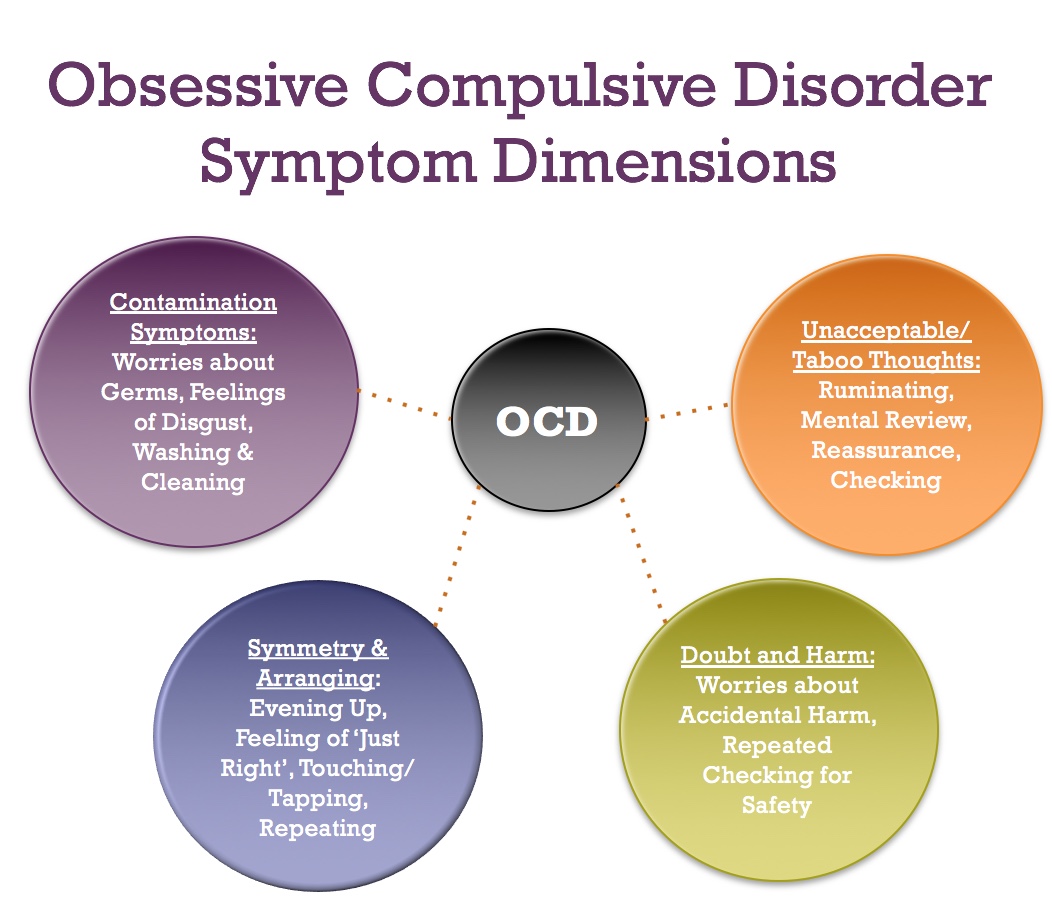
Probably, obsessive compulsive disorder is a multifactorial pathology in which hereditary predisposition is realized under the influence of various triggers. It has been noted that people with increased suspiciousness, hypertrophied concern about how their actions look and what others will think about them, people with great conceit and its reverse side - self-abasement are predisposed to the development of obsessive-compulsive disorder.
Symptoms and course of neurosis
The basis of the clinical picture of obsessive-compulsive disorder is obsessions - irresistibly obsessive thoughts (imaginations, fears, doubts, cravings, memories) that cannot be "thrown out of the head" or ignored. At the same time, patients are quite critical of themselves and their condition. However, despite repeated attempts to overcome it, they do not achieve success. Along with obsessions, compulsions arise, with the help of which patients try to reduce anxiety, distract themselves from annoying thoughts. In some cases, patients carry out compulsive acts covertly or mentally. This is accompanied by some absent-mindedness and slowness in the performance of official or domestic duties.
In some cases, patients carry out compulsive acts covertly or mentally. This is accompanied by some absent-mindedness and slowness in the performance of official or domestic duties.
The severity of symptoms can vary from mild, practically not affecting the quality of life of the patient and his ability to work, to significant, leading to disability. With mild severity, acquaintances of a patient with obsessive-compulsive disorder may not even guess about his existing disease, attributing the quirks of his behavior to character traits. In severe advanced cases, patients refuse to leave the house or even their room, for example, to avoid infection or contamination.
Obsessive compulsive disorder can proceed according to one of 3 options: with the constant persistence of symptoms for months and years; with a relapsing course, including periods of exacerbation, often provoked by overwork, illness, stress, unfriendly family or work environment; with steady progression, expressed in the complication of the obsessive syndrome, the appearance and aggravation of changes in character and behavior.
Types of obsessive states
Obsessive fears (fear of failure) - a painful fear that it will not turn out properly to perform this or that action. For example, go out in front of the public, remember a learned poem, have sexual intercourse, fall asleep. This also includes erythrophobia - the fear of blushing in front of strangers.
Obsessive doubts - uncertainty about the correctness of the implementation of various actions. Patients suffering from obsessive doubts constantly worry about whether they turned off the tap with water, turned off the iron, whether they indicated the address in the letter correctly, etc. Pushed by uncontrollable anxiety, such patients repeatedly check the performed action, sometimes reaching complete exhaustion.
Obsessive phobias - have the widest variation: from the fear of getting sick with various diseases (syphilophobia, cancerophobia, heart attack, cardiophobia), fear of heights (hypsophobia), closed spaces (claustrophobia) and too open areas (agoraphobia) to fear for their loved ones and fear of turning to yourself someone's attention.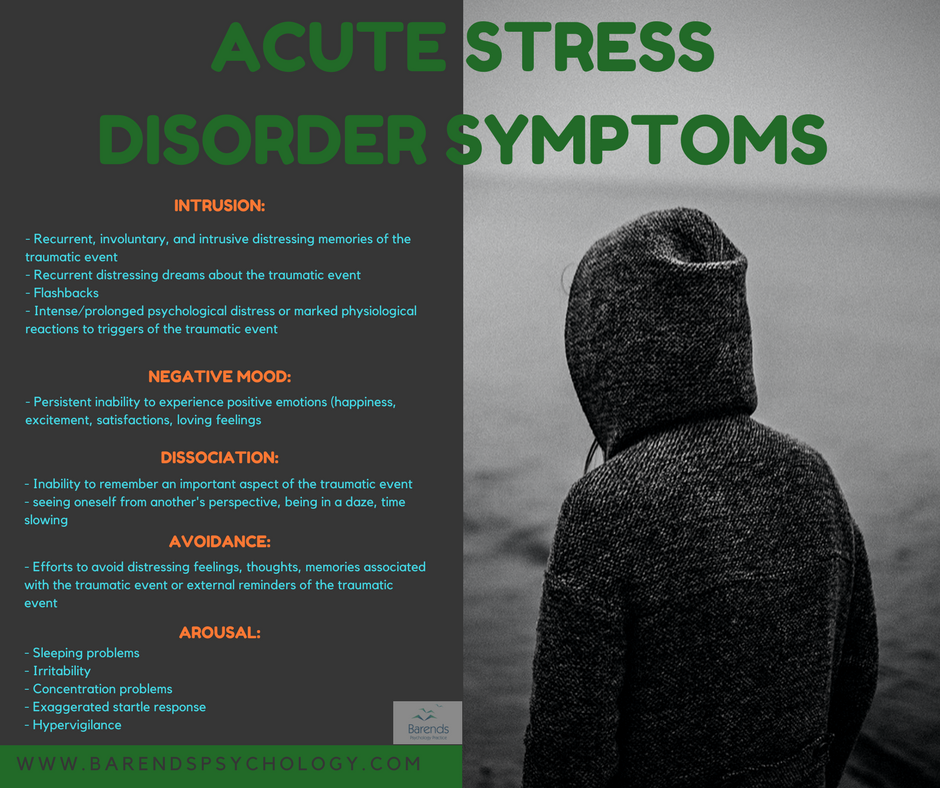 Common phobias among OCD patients are fear of pain (algophobia), fear of death (thanatophobia), fear of insects (insectophobia).
Common phobias among OCD patients are fear of pain (algophobia), fear of death (thanatophobia), fear of insects (insectophobia).
Obsessive thoughts - stubbornly "climbing" into the head names, lines from songs or phrases, surnames, as well as various thoughts that are opposite to the patient's life ideas (for example, blasphemous thoughts in a believing patient). In some cases, there is obsessive philosophizing - empty endless thoughts, for example, about why trees grow taller than people or what will happen if two-headed cows appear.
Intrusive memories are memories of certain events that arise against the patient's wishes, which, as a rule, have an unpleasant coloring. This also includes perseverations (obsessive ideas) - bright sound or visual images (melodies, phrases, pictures) that reflect a traumatic situation that occurred in the past.
Obsessive actions - repeatedly repeated in addition to the will of the sick movement. For example, squinting eyes, licking lips, straightening hair, grimacing, winking, scratching the back of the head, rearranging objects, etc. Some clinicians separately distinguish obsessive drives - an uncontrollable desire to count or read something, rearranging words, etc. this group also includes trichotillomania (hair pulling), dermatillomania (damage to one's own skin), and onychophagia (compulsive nail biting).
For example, squinting eyes, licking lips, straightening hair, grimacing, winking, scratching the back of the head, rearranging objects, etc. Some clinicians separately distinguish obsessive drives - an uncontrollable desire to count or read something, rearranging words, etc. this group also includes trichotillomania (hair pulling), dermatillomania (damage to one's own skin), and onychophagia (compulsive nail biting).
Diagnostics
Obsessive-compulsive disorder is diagnosed on the basis of patient complaints, neurological examination data, psychiatric examination and psychological testing. It is not uncommon for patients with psychosomatic obsessions to be treated unsuccessfully by a gastroenterologist, internist or cardiologist for somatic pathology before being referred to a neurologist or psychiatrist.
Significant for the diagnosis of OCD are daily obsessions and / or compulsions that take at least 1 hour per day and disrupt the patient's usual course of life.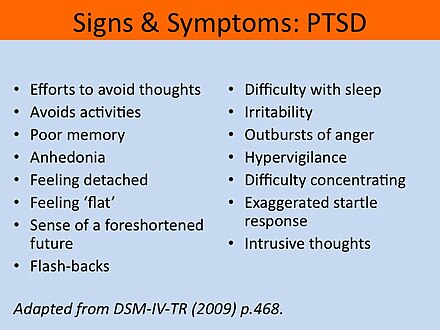 The patient's condition can be assessed using the Yale-Brown scale, a psychological study of personality, and pathopsychological testing. Unfortunately, in some cases, psychiatrists diagnose OCD patients with schizophrenia, which entails improper treatment, leading to the transition of neurosis into a progressive form.
The patient's condition can be assessed using the Yale-Brown scale, a psychological study of personality, and pathopsychological testing. Unfortunately, in some cases, psychiatrists diagnose OCD patients with schizophrenia, which entails improper treatment, leading to the transition of neurosis into a progressive form.
Examination by a neurologist can reveal hyperhidrosis of the palms, signs of autonomic dysfunction, tremor of the fingers of outstretched hands, and a symmetrical increase in tendon reflexes. If a cerebral pathology of organic origin is suspected (intracerebral tumor, encephalitis, arachnoiditis, cerebral aneurysm), MRI, MSCT or CT of the brain is indicated.
Treatment
It is possible to effectively treat obsessive-compulsive disorder only by following the principles of an individual and integrated approach to therapy. It is advisable to combine drug and psychotherapeutic treatment, hypnotherapy.
Drug therapy is based on the use of antidepressants (imipramine, amitriptyline, clomipramine, St. John's wort extract). The best effect is provided by third-generation drugs, the action of which is to inhibit serotonin reuptake (citalopram, fluoxetine, paroxetine, sertraline). With a predominance of anxiety, tranquilizers (diazepam, clonazepam) are prescribed, with a chronic course - atypical psychotropic drugs (quetiapine). Pharmacotherapy of severe cases of obsessive-compulsive disorder is carried out in a psychiatric hospital.
John's wort extract). The best effect is provided by third-generation drugs, the action of which is to inhibit serotonin reuptake (citalopram, fluoxetine, paroxetine, sertraline). With a predominance of anxiety, tranquilizers (diazepam, clonazepam) are prescribed, with a chronic course - atypical psychotropic drugs (quetiapine). Pharmacotherapy of severe cases of obsessive-compulsive disorder is carried out in a psychiatric hospital.
Of the methods of psychotherapeutic influence, cognitive-behavioral therapy has proven itself well in the treatment of OCD. According to her, the psychotherapist first identifies the patient's obsessions and phobias, and then gives him the installation to overcome his anxieties by becoming face to face with them. The exposure method has become widespread, when the patient, under the supervision of a psychotherapist, is faced with a disturbing situation to make sure that nothing terrible will follow. For example, a patient with a fear of germs who constantly washes his hands is instructed not to wash his hands in order to make sure that no illness occurs.
A part of complex psychotherapy can be a method of "stopping thoughts", consisting of 5 steps. The first step is to determine the list of obsessions and psychotherapeutic work on each of them. Step 2 is to teach the patient the ability to switch to some positive thoughts when obsessions occur (remember a favorite song or imagine a beautiful landscape). In step 3, the patient learns to stop the obsession by saying aloud the command to stop. Doing the same thing, but saying "stop" only mentally is the task of step 4. The last step is to develop the patient's ability to find positive aspects in emerging negative obsessions. For example, if you are afraid of drowning, imagine yourself in a life jacket next to the boat.
Along with these methods, individual psychotherapy, autogenic training, and hypnosis treatment are additionally used. In children, fairy tale therapy and game methods are effective.
The use of psychoanalytic methods in the treatment of obsessive-compulsive disorder is limited because they can provoke outbreaks of fear and anxiety, have a sexual connotation, and in many cases of obsessive-compulsive disorder have a sexual accent.
Prognosis and prevention
Complete recovery is rare. Adequate psychotherapy and drug support significantly reduce the manifestations of neurosis and improve the patient's quality of life. Under adverse external conditions (stress, severe illness, overwork), obsessive-compulsive disorder may reappear. However, in most cases, after 35-40 years, there is some smoothing of symptoms. In severe cases, obsessive-compulsive disorder affects the patient's ability to work, a 3rd group of disability is possible.
Given the character traits that predispose to the development of OCD, it can be noted that a good prevention of its development will be a simpler attitude towards oneself and one's needs, life for the benefit of the people around.
Sources
- In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.

treatment, causes, how to deal with obsessive thoughts
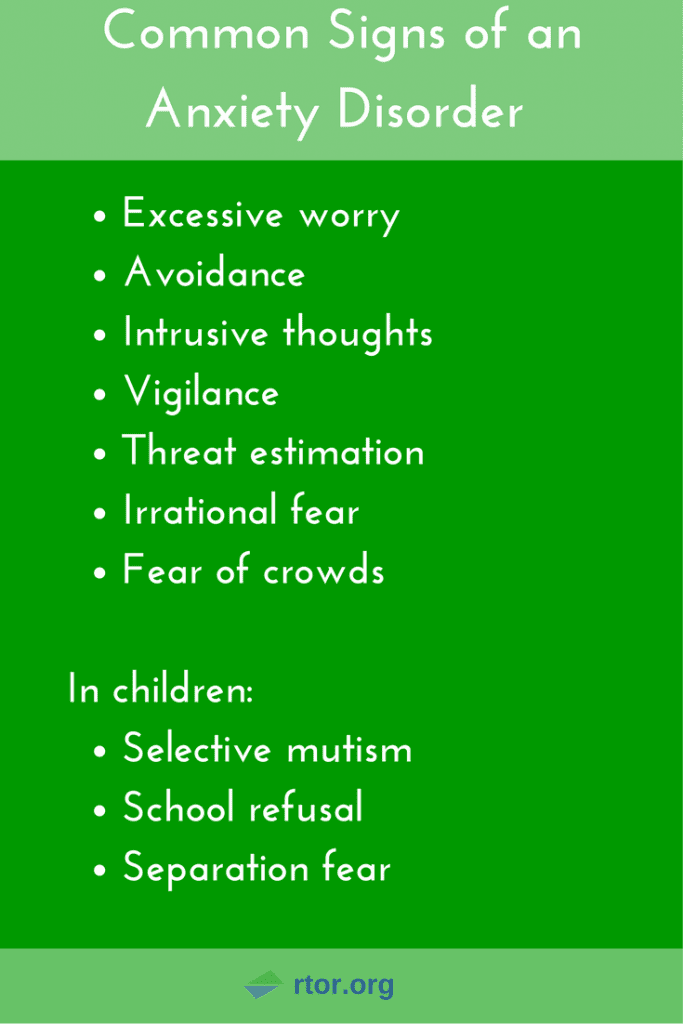
Obsessive thoughts (obsessions) are images or urges that uncontrollably, against the will of a person, invade consciousness. Attempts to get rid of these thoughts lead to outbreaks of anxiety and bring great discomfort. A person experiences constant fears and bad thoughts. If you do not seek help in time, obsessions lead to psychological exhaustion, social isolation and depression.
Obsessive thoughts are found in many diseases: neurosis, depression, obsessive-compulsive disorder (obsessive-compulsive disorder) and even schizophrenia.
Features that distinguish obsessive thoughts syndrome:
- a person cannot influence the appearance of such thoughts, thoughts arise against desire;
- obsessive thoughts are not connected with the usual thoughts of a person - they are separate, alien images;
- the syndrome of obsessive thoughts cannot be overcome by an effort of will;
- the disorder is associated with intense anxiety, irritability;
- clarity of consciousness and critical perception of one's condition are usually preserved.

The disorder is extremely difficult to bear. Usually a person realizes what obsessive thoughts mean, understands all the irrationality of the images that arise in the head, but cannot fight them. Attempts to stop the appearance of thoughts and the coercive actions associated with them are unsuccessful and lead to even greater experiences.
It is not difficult to convince people who suffer from this disorder that their obsessive thoughts have no basis. But it doesn't help to get rid of the problem. Situations repeat themselves over and over. A necessary step to get rid of painful conditions is to seek help from a specialist before complications arise.
What are obsessive thoughts
Obsessive thoughts torment a person, they are unpleasant and disturbing, you want to hide from them, run away. There are all kinds of obsessions.
Here are some examples of intrusive thoughts:
- concerns about pollution and disease;
- pathological need for order and symmetry;
- obsessive and uncontrolled account;
- obsessive thoughts about the bad: a person constantly thinks about accidents that can happen to him, to his relatives, to his property, or even to humanity as a whole;
- groundless and unreasonable avoidance of certain actions or objects;
- religious, sexual, aggressive or any other thoughts that are alien to the patient's thinking and arise against the will.
Constant intrusive thoughts cause unbearable discomfort. Of course, a person has a desire to succumb to these ideas and try to correct the situation. In this case, compulsions appear - actions that a person is forced to periodically perform, even if he does not want to, in order to control what is happening in his head. When obsessive thoughts (obsessions) and obsessive actions (compulsions) are present together, time-consuming, disruptive, and distressing, it indicates the presence of a disease such as obsessive-compulsive disorder (OCD).
A person begins to avoid cracks in the asphalt or touches every tree on the road because alien thoughts “tell” him that if he does not do this, something bad will happen.
Usually compulsions make you do something over and over again, like a ritual. By giving in to coercion, the person hopes that they can prevent or reduce the anxiety that accompanies obsessions. For example, he begins to avoid cracks in the asphalt or touches every tree on the road because alien thoughts "tell" him that if he does not do this, something bad will happen.
 Unfortunately, such actions do not bring relief and only get worse over time, taking the form of an endless ritual.
Unfortunately, such actions do not bring relief and only get worse over time, taking the form of an endless ritual. In addition to OCD, there are other diseases in psychiatry that are characterized by different types of obsessive thoughts. Here are some of them:
- phobias,
- neurasthenia,
- schizophrenia.
A phobia is an anxiety disorder characterized by panic and an uncontrollable, irrational fear of certain situations or objects. Strong anxiety can arise even when thinking about a frightening situation, so the patient tries with all his might to avoid a terrible object. All terrible obsessive thoughts and anxieties are associated exclusively with this object.
There are different types of phobias. The most common:
- agoraphobia — fear of open spaces or crowded places;
- social phobia - fear of social interactions. There are other specific phobias that can relate to anything: airplanes, specific animals, the sight of blood.

A phobic disorder may include panic attacks - attacks of fear, which are accompanied by a feeling of impending death and physical sensations: retrosternal pain, interruptions in the heart, dizziness, feeling short of breath, numbness of the extremities, intestinal disorders. All this significantly limits the personal life and performance of a person.
Neurasthenia is a disorder that is associated with exhaustion of the nervous system. It happens after a long illness, physical overload, severe or prolonged stress. Characterized by persistent headache, symptoms of cardiovascular disorders, indigestion and sleep.
Intrusive delusional thoughts may be one of the manifestations of schizophrenia, but the diagnosis is made only in the presence of other signs of schizophrenia.
The disease has three forms-stages that develop one after another. In the hypersthenic form, emotional lability, irritability and intolerance are observed.
 In the second phase, which is called "irritable weakness", aggression and irritation are quickly replaced by emotional exhaustion and impotence. In the third, hyposthenic form, the patient arrives in a state of constant fatigue and bad mood. He focuses on his inner feelings, which depresses him even more. This phase is characterized by obsessive thoughts of a hypochondriacal nature.
In the second phase, which is called "irritable weakness", aggression and irritation are quickly replaced by emotional exhaustion and impotence. In the third, hyposthenic form, the patient arrives in a state of constant fatigue and bad mood. He focuses on his inner feelings, which depresses him even more. This phase is characterized by obsessive thoughts of a hypochondriacal nature. Schizophrenia is a complex polymorphic mental illness characterized by a fundamental impairment of perception and the breakdown of thought processes. The clinical picture is varied and depends on the form of the disease: hallucinations, delusions, loss of natural mental functions, personality distortion, and much more.
A sick person who suffers from this disease needs full treatment from a psychiatrist. Intrusive delusional thoughts may be one of the manifestations of schizophrenia, but the diagnosis is made only in the presence of other signs that are specific, diagnostically significant criteria for this disorder.
Causes of obsessive thoughts
The occurrence of obsessions is directly related to the underlying disease. For treatment to be effective, an accurate diagnosis is essential. It is not always possible to accurately answer the question of where obsessive thoughts come from. Factors that contribute to the occurrence of this disorder have been identified:
- genetic predisposition;
- brain dysfunction due to organic or biochemical causes, including imbalance of neurotransmitters;
- mental trauma and stress;
- personality traits: people with sensitive and labile temperament;
- the presence of somatic and infectious diseases, disability, pregnancy are predisposing causes of obsessive thoughts.
There are many disorders in which this syndrome occurs, so the diagnosis should be carried out by a highly qualified psychiatrist who can understand the intricacies of the clinical picture and understand why obsessive thoughts arise.
 When conducting diagnostics, the following methods are used:
When conducting diagnostics, the following methods are used: - Psychiatric examination: a specialist will collect an anamnesis, understand the clinical manifestations and personal characteristics of each patient.
- Pathopsychological study: an effective and comfortable technique that, with the help of special experiments, surveys and observations, allows you to conduct a qualitative analysis of mental disorders and understand why obsessive thoughts come.
- Laboratory and instrumental examination: modern diagnostic tests, such as Neurotest and Neurophysiological test system, allow assessing the severity of pathological processes and making an accurate differential diagnosis. Functional methods will help to exclude organic pathology.
How to deal with obsessive thoughts
Mental illnesses that underlie the syndrome in question are a reason to immediately consult a psychiatrist. The symptoms vary greatly, and it is not always easy to notice the distinctive features.
 Therefore, it is necessary to address the question of what to do with obsessive thoughts to an experienced specialist.
Therefore, it is necessary to address the question of what to do with obsessive thoughts to an experienced specialist. It happens that a person is afraid to seek help or tries to independently find a way to cope with obsessive thoughts that are so annoying. One of the most common decisions is the use of alcohol and drugs. If a person manages to be distracted, the illusion may be created for a short time that the problem has disappeared. In fact, the situation is only getting worse. You should not try to "kill" intrusive thoughts in this way, because it is likely that obsessions will only intensify when intoxicated.
Talk to someone you trust, such as your parents or friends. A great option is to go to group therapy, in a society of people with similar problems. This will allow you to share experiences and get support.
The consequences of drinking alcohol can be unpredictable. Even if there is a brief relief, thoughts will still arise again, and with even greater force.
 As a result, new health problems are added, dependence on alcohol or drugs develops, and the disorder worsens. With neurosis of obsessive thoughts, only a specialist will tell you how to get rid of or alleviate the condition.
As a result, new health problems are added, dependence on alcohol or drugs develops, and the disorder worsens. With neurosis of obsessive thoughts, only a specialist will tell you how to get rid of or alleviate the condition. In addition to the stages of treatment that the doctor will select for you, you need to remember about self-control, rehabilitation and prevention. Here are a few tips beyond basic treatment to help you deal with intrusive thoughts:
- Learn more about your disorder. Learning about your condition will help you quickly accept the problem, calm down and motivate you to better adhere to the treatment plan.
- Talk to someone you trust, such as your parents or friends. A great option is to go to group therapy, in a society of people with similar problems. This will allow you to share experiences and get support.
- Normalization of lifestyle: proper sleep, diet, avoidance of alcohol and strong psychotropic substances, moderate physical activity.
- Do not give up your normal activities. Build a career, study, devote time to your favorite hobby. Spend time with family and friends. Don't let illness interfere with your life.
- Avoid Stress: The idea that a strong outburst of emotions will make the fight against obsessive thoughts more effective is false. It will be possible to be distracted only for a short time, but then the nervous system will become even more vulnerable.
Treatment of obsessive thoughts
With the help of modern medicine, it is possible to mitigate the intensity of manifestations, and often completely get rid of obsessions and compulsions.
For obsessive thoughts syndrome, treatment is most effective when combined with psychotherapy and medication. In some cases, one thing is enough. A competent specialist will select an individual program, which will depend on the clinical picture and the severity of the condition.
For obsessive thoughts, treatment may consist of psychotherapy and pharmacotherapy.

Psychotherapy allows you to fully analyze the situation and work out behavioral, psychological and social problems. Communication with a highly qualified psychotherapist teaches you how to manage symptoms, overcome fears and protect yourself from stress. The arsenal of a modern specialist includes cognitive behavioral therapy, hypno-suggestive techniques, auto-training and other effective approaches. Psychotherapy for obsessive thoughts is a key treatment that will help you understand the problem and deal with it.
Pharmacotherapy. Modern medicines help to correct neurotic symptoms, relieve fear and anxiety, and keep mood under control. Mild antidepressants, antipsychotics and tranquilizers are used.
Fortunately, modern psychiatry knows how to cure obsessive thoughts, reduce or completely eliminate symptoms. Thanks to effective treatment and rehabilitation provided by a competent specialist, patients return to an active life without fears and restrictions.