How to write therapy progress notes
5 Tips for Writing Better Therapy Notes
Tips
Therapy notes are a vital component in treatment and recovery. They allow clinical professionals to document and share the progress or lack thereof for each of their patients. Documenting every encounter helps the communication across the patient life cycle and helps ensure your facility remains compliant with industry regulations and standards. In this article, we’ll go over five tips for writing therapy notes.
Talk To Our Experts
1. Be Clear & Concise
Therapy notes should be straight to the point but contain enough information to give others a clear picture of what transpired. It is essential to stick to the facts while providing supporting evidence. For example, let’s take a look at the following note:
“Kelly indicated that she fears abandonment because her father left her and her mother three times. The first instance was when Kelly was four and he did not return into her life again until she was 7. Her parents had another child at that time, and her father left again when Kelly was 9. He moved to another state across the country. When Kelly was 12, her father returned again. He left for the final time when Kelly was 17 and she has not seen or heard from him since.”
This note can be clearer and more concise by implementing some small edits:
“Kelly indicated that she fears abandonment because her father left their family three times throughout her childhood, with one case where he moved across the country. The last incident occurred when Kelly was 17, and she has not seen or heard from him since.”
2. Remain Professional
Therapy notes are intended to document the progress of a patient and be shared across the patient lifecycle; therefore, it’s incredibly important to remain professional while documenting your observations. For example, let’s take a look at the following note:
“Steven came to group with a poor attitude and went into a fit of rage when called upon to share his experience.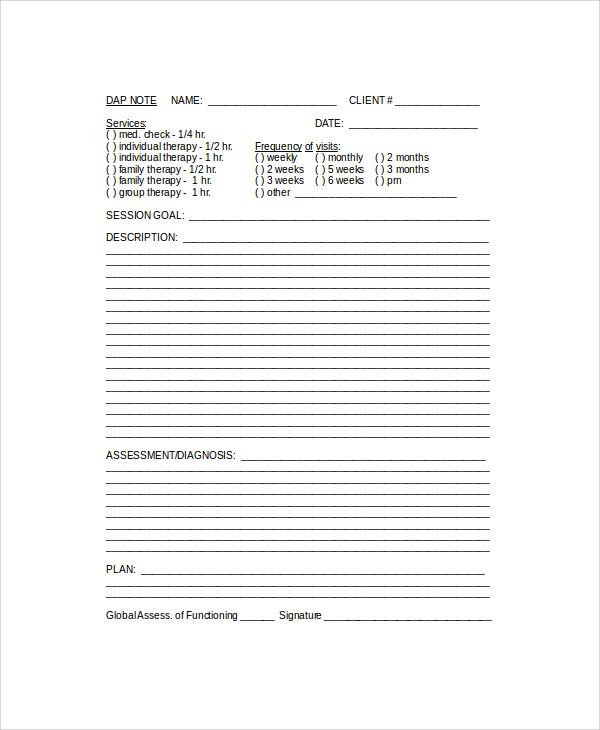 He must have been drinking last night to be that much of a jerk. He has been a jerk many times, but now he’s proven to be a real piece of work. He even just up and left halfway through.”
He must have been drinking last night to be that much of a jerk. He has been a jerk many times, but now he’s proven to be a real piece of work. He even just up and left halfway through.”
We can adjust this note and be more professional by writing something like:
“Steven came to group with a poor attitude and began yelling in objection when asked to participate. His agitation increased throughout the session until he abrupted walked out after 30 minutes.”
3. Write for Everyone
Remember that other people will be reading and reviewing your therapy notes. It is important to be conscientious about that fact. Don’t use shorthand, jargon, or your own unique acronyms – stick to commonly used terminology and grammar. This will help all your team members understand your notes and thus more effectively help the patient progress through recovery.
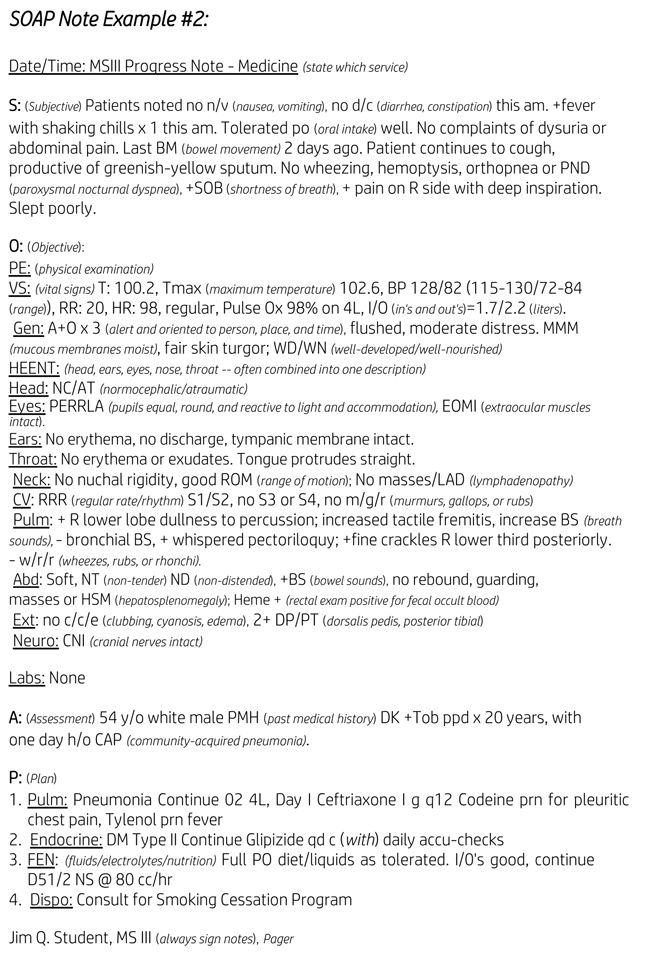
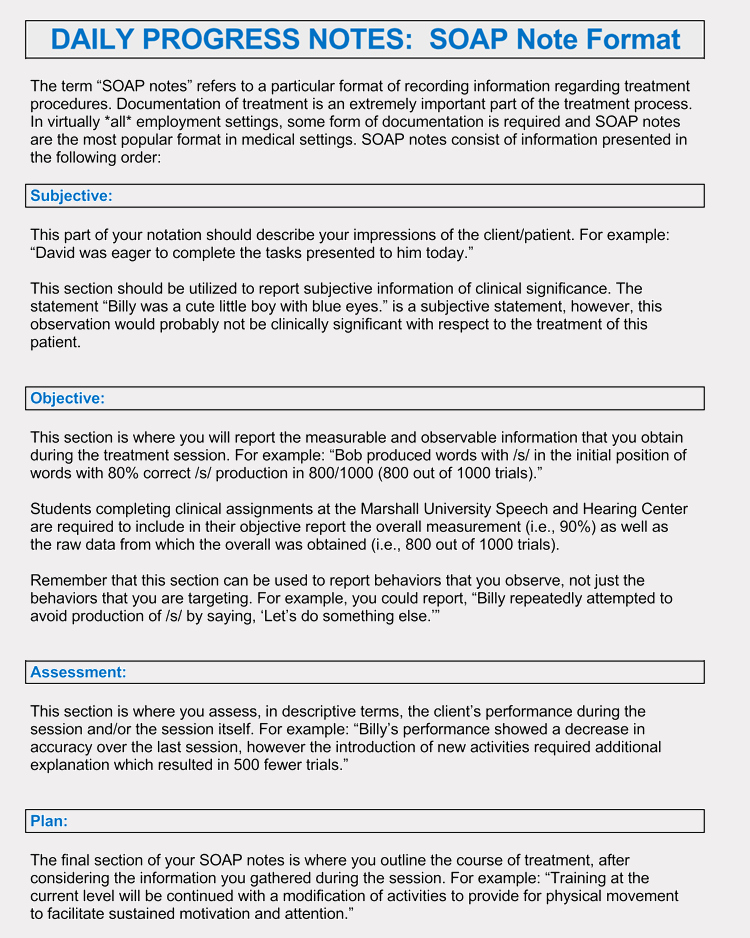
4. Use SOAP
Let’s start with what SOAP is. (Hint: it’s not what you use to wash your hands in this case. ) SOAP stands for subjective, objective, assessment, plan, and it is a process that was developed to help clinicians document the critical points within an interaction or session. This method enables you to focus on vital and pertinent information, which means you’ll be successful at staying clear and concise.
) SOAP stands for subjective, objective, assessment, plan, and it is a process that was developed to help clinicians document the critical points within an interaction or session. This method enables you to focus on vital and pertinent information, which means you’ll be successful at staying clear and concise.
Subjective is what the patient expresses as their experience and feelings. It is from the patient’s perspective. For example, a subjective portion of a note could be, “David expressed that he feels anxious and distracted often.”
Objective is a statement of fact and/or raw data that is tied to the subjective feeling or experience. For example, “David continuously tapped his feet throughout the session.” It is important to consider that objective statements can either support or contradict the subjective statements.
Assessment takes into account the subjective and objective items from above. You will document your interpretations of the information that has been gathered – which may or may not lead to a diagnosis.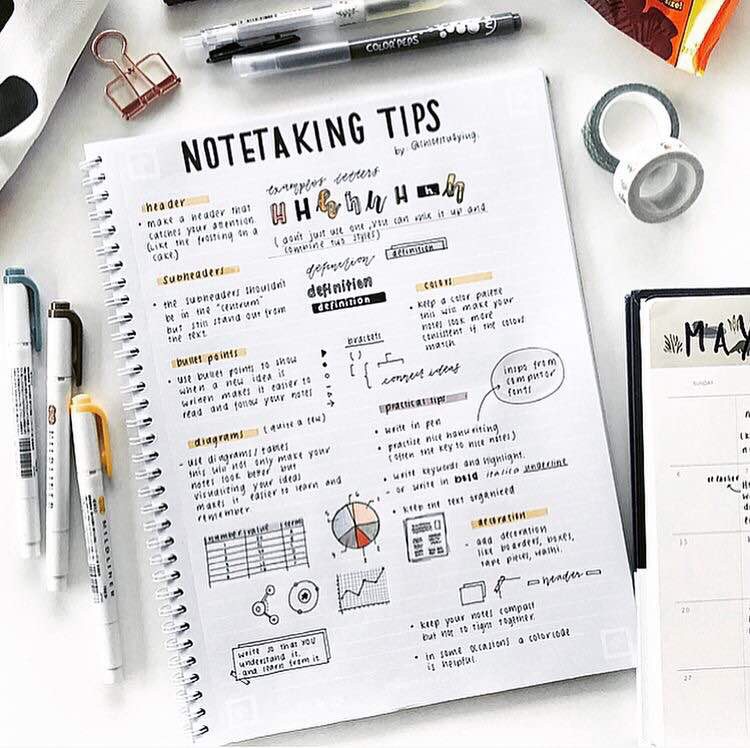 Certain conditions can be easily diagnosed early, whereas other conditions may require many sessions and assessments are more related to progress. As with the other items, assessments should be concise and only contain necessary information.
Certain conditions can be easily diagnosed early, whereas other conditions may require many sessions and assessments are more related to progress. As with the other items, assessments should be concise and only contain necessary information.
Finally, the three pieces above come together to inform a plan. A plan should contain any treatment provided in the session, justification for that treatment, the patient’s response to the treatment, next steps and appointments, follow up instructions, goals, and outcome measurements. Plan notes should include actionable items for each problem or condition. Ultimately the goal is to address each item in the assessment.
5. Focus on Progress & Adjust as Necessary
Notes are vital for understanding the progress of your patients, and as that progress ebbs and flows, the plan will need to be adjusted. Remember to stay focused on the progress or lack thereof to ensure you are identifying any need to adjust and then documenting accordingly.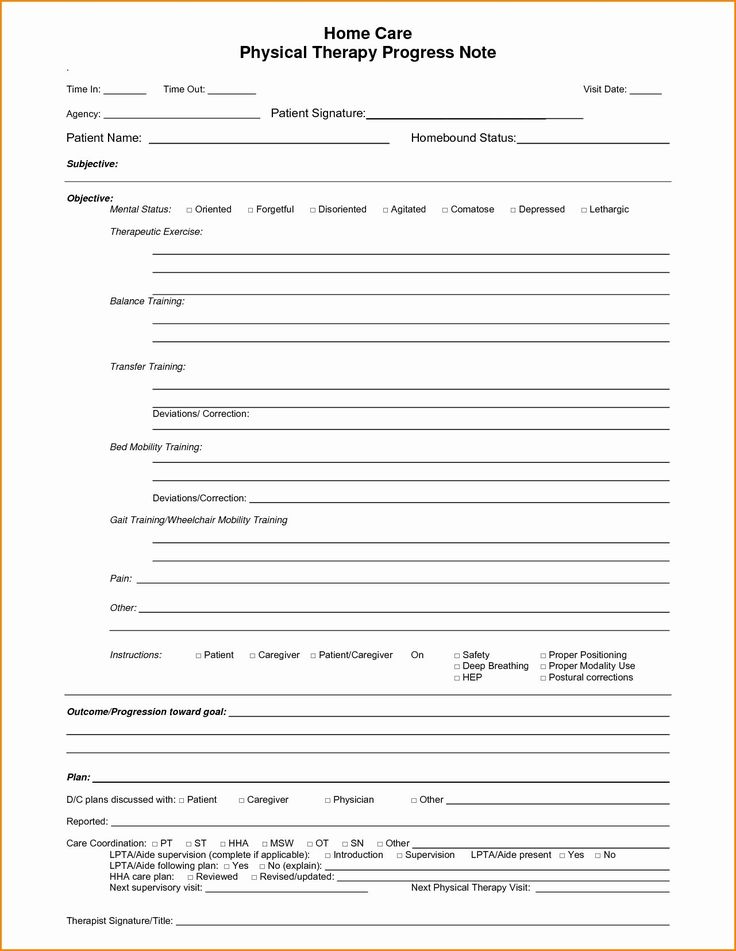
Overall, therapy notes are a key component to a successful recovery. Becoming thorough and yet efficient at documenting sessions will help you and your team produce better results. Team members will communicate better, plans will be more productive, and patients will lead better lives. Sunwave’s unified treatment platform is custom-built for substance use disorder treatment and can help you follow these tips for writing therapy notes. Schedule a demo with one of our platform experts and we’ll be happy to show you how.
How To Write Therapy Progress Notes: 8 Templates & Examples
Clear, concise, and accurate therapy progress notes are beneficial to practitioners and their clients. They’re instrumental in monitoring a patient’s progress, the efficacy of their treatment, and helping professionals understand their patient’s personal experiences.
To be helpful and informative, though, progress notes in mental health need to follow some guidelines. In this overview, we’ll introduce their key elements, a step-by-step guide to writing therapy progress notes, and some of the best therapy software you can use to create excellent progress notes efficiently.
Before getting started, we recommend trying Quenza, our therapy notes software for e-mental health practitioners.
Quenza is a complete suite of blended care tools that includes everything you need to make and store clear, professional therapy progress notes on a HIPAA-compliant platform.
What Are Progress Notes in Mental Health?
Progress notes are clinical notes made by psychologists, therapists, clinical counselors, psychiatrists, and other practitioners involved in a patient’s treatment and care.
More specifically, they contain clinical facts and medical reasoning about “the care delivered to patients and the clinical events relevant to diagnosis and treatment.”[1]
Progress notes are professional documents that communicate important information on a patient’s condition between multiple providers. In mental health contexts, they must be stored privately and securely in a HIPAA-compliant manner.
Difference Between Progress & Psychotherapy Notes
Progress notes are professional documents that communicate important information on a patient’s condition between multiple providers.
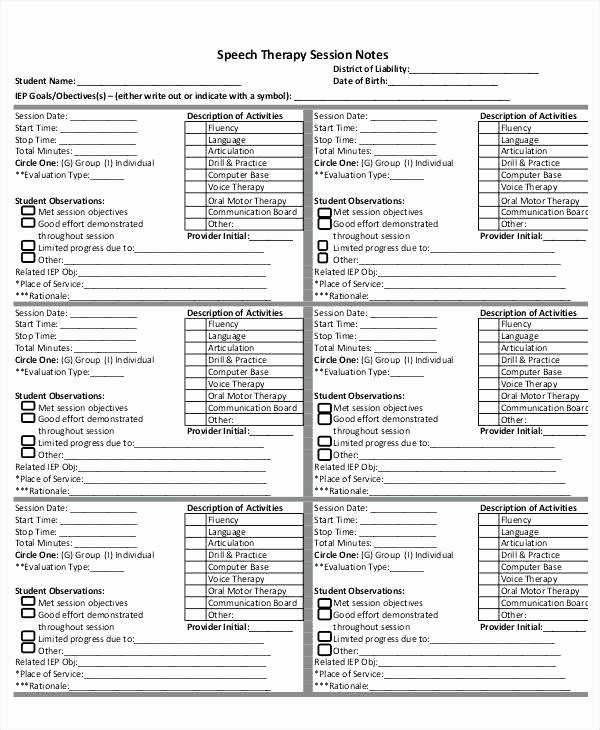
As medical and mental healthcare providers will know, progress notes play a vital role in treatment planning and service delivery across a wide range of helping professions, such as occupational, physical, and speech therapy.
This distinguishes them from psychotherapy notes, which contain information exclusively related to a patient’s therapy sessions. Also, unlike progress notes, psychotherapy notes are only written by counselors, therapists, and mental health practitioners who are actively involved in their therapy.
This table outlines a few more differences between progress and psychotherapy notes.
Progress Notes | Psychotherapy Notes | |
|---|---|---|
Purpose |
|
|
Written by | Any care provider involved in a patient’s treatment plan, e. | Psychologist, Psychiatrist, Counselor, Psychotherapist |
Content | May include:
| May include:
|
Privacy |
|
|
10 Steps For Writing Effective Progress Notes
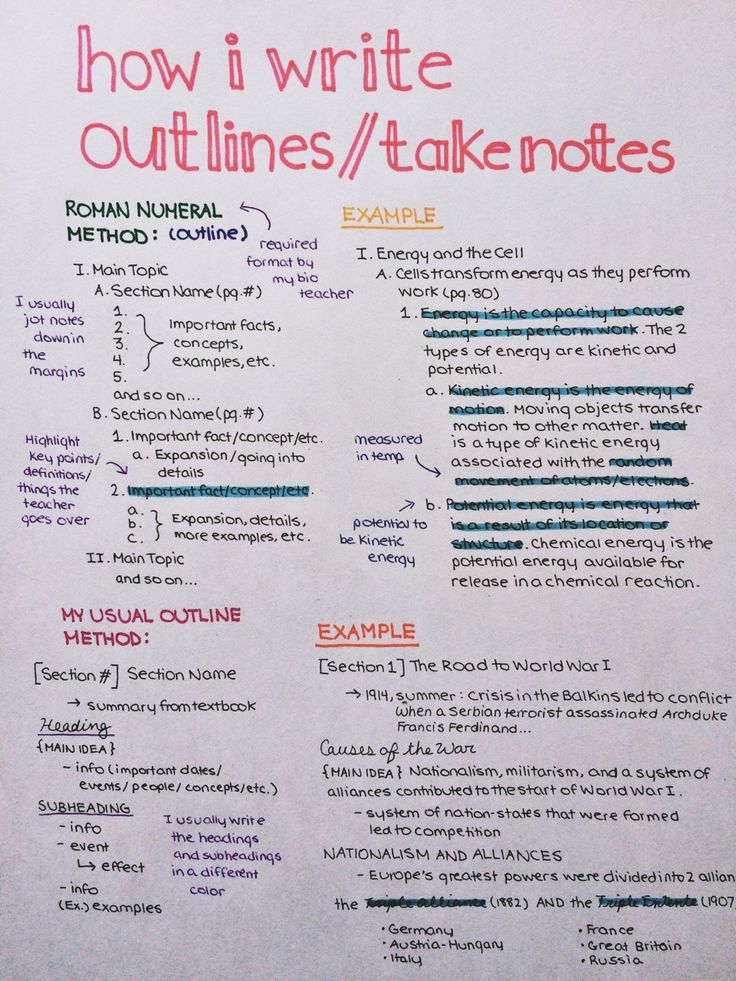
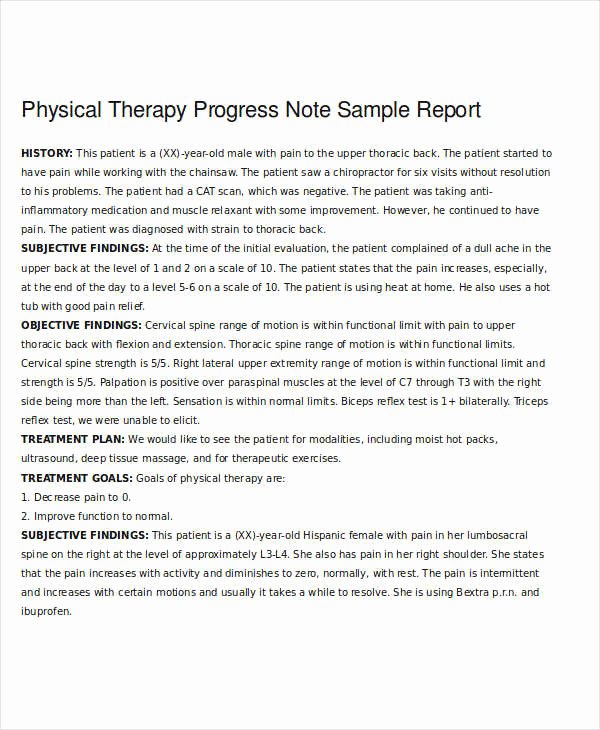
Following a template is an easy way to ensure all important details and information are included in your therapy progress notes.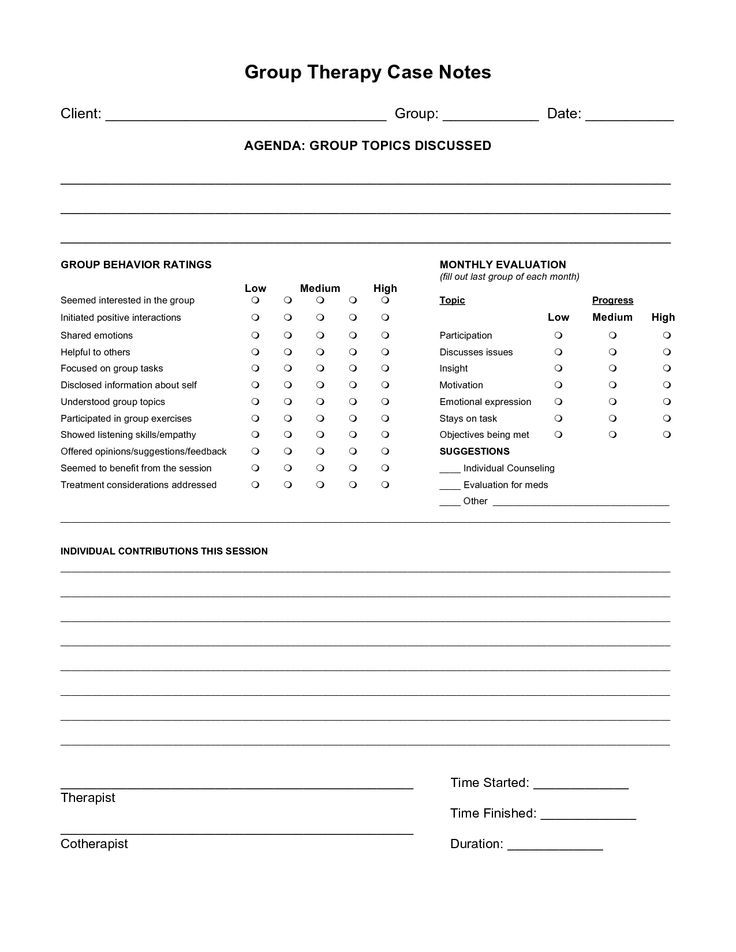
Many treatment software solutions offer this functionality, with a variety of formats and outlines for different healthcare subsectors – psychiatry, counseling, and more.
For instance, Therapy Notes comes with Psychotherapy Progress Notes templates and a step-by-step guide to help psychologists write effective progress notes. Each step corresponds with a different field in the note, starting with patient information and ending with a digital clinician signature:[2]
- Note Header: A brief overview of the essential practitioner, patient, and session information, such as when the appointment took place, its duration, and service codes for practice administration.
- Diagnosis: ICD-10 or DMS5 codes might be relevant here if the patient has been diagnosed with a mental health condition.
- Patient Presentation: A description of how the client appears, using different modalities, e.
 g., cognitive functioning, affect, or behavior.
g., cognitive functioning, affect, or behavior. - Safety Issues: Any important information regarding the patient’s well-being.
- Medications: For prescribing clinicians such as psychiatrists and general MDs.
- Symptom Description and Subjective Report: This includes reports and direct quotes regarding the patient’s status. These may come from the client themself and/or their key caregiver and might relate to how the patient is feeling, how they view their progress, or their opinions on the mental health treatment plan.
- Relevant Content: Objective data such as test results, documents, and therapy notes might be included here – this section is for relevant e-mental health information that could ‘complete the picture’ drawn by the progress note.
- Interventions Used: This step involves documenting the treatment interventions applied and the broader field that they fall into.
 Examples might include cognitive restructuring within CBT or relaxation techniques as part of a mindfulness training program.
Examples might include cognitive restructuring within CBT or relaxation techniques as part of a mindfulness training program. - Treatment Plan Progress: Each progress note should mention whether a client’s treatment plan objectives are being met.
- Signatures: Most telecounseling software includes the ability to e-sign documents and store them in a secure, HIPAA-compliant manner.
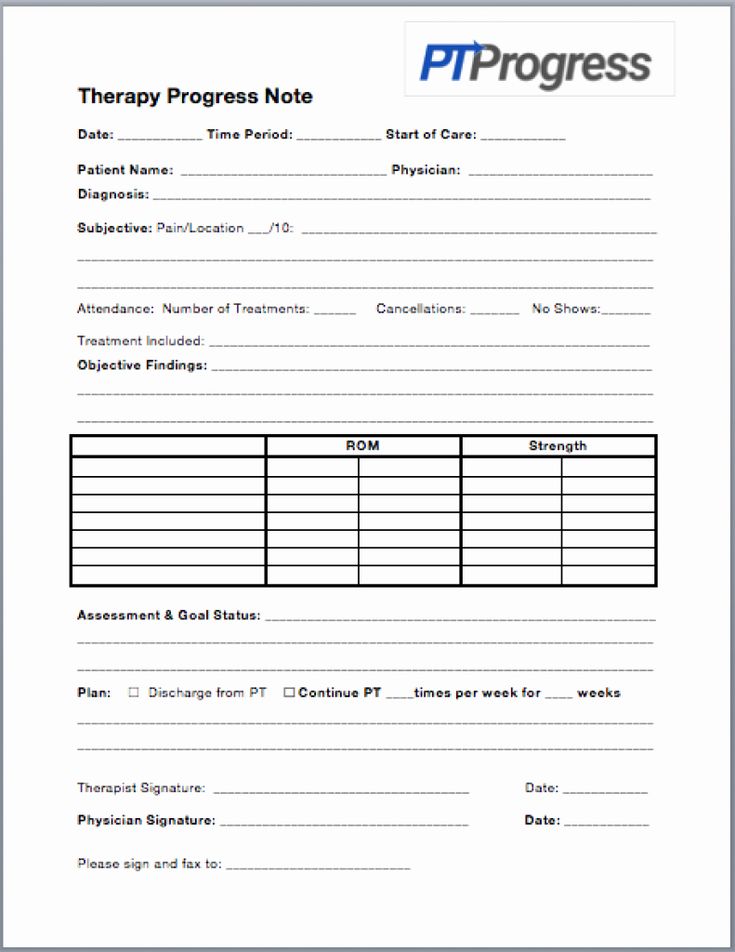
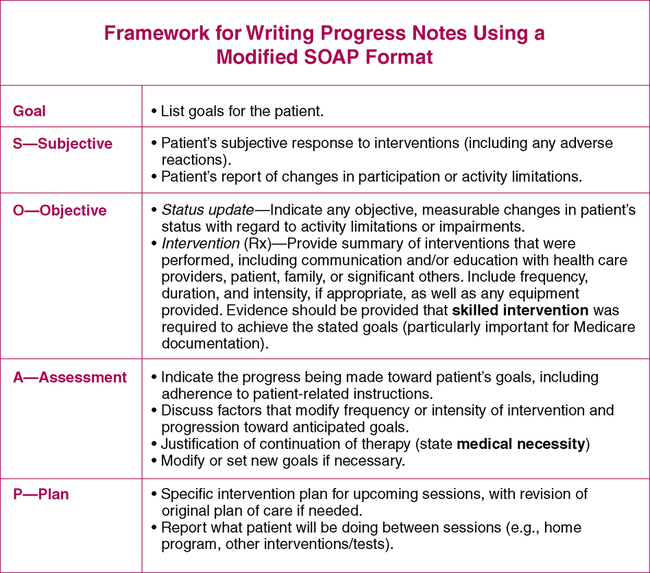
A Brief Look At The SOAP Method
If the step-by-step guide above seems familiar, it’s likely because this particular therapy progress notes template leverages central elements of the SOAP note format.
SOAP Notes follow a standard 4-point layout covering critical information on a patient’s health status. A specific type of progress note, SOAP notes can be shared with any other therapists and care professionals the client may be working with.
The four sections of a SOAP method note are:
- Subjective Data on a patient’s feelings, experiences, or thoughts, such as direct quotes or their observations
- Objective Data regarding their mental or general health status, e.
 g., details from their therapy appointment
g., details from their therapy appointment - Assessment Information that integrates subjective and objective details with a therapist’s professional interpretation, and
- Plan details regarding any adjustments or next steps that the counselor and client feel are needed.
Read Writing SOAP Notes: Step-by-Step Guide, Examples, and Templates for a little more detail on what each section should feature, as well as a host of helpful formats and walkthroughs.
3 Helpful Templates and Formats
Therapy progress notes can range from the very basic to more comprehensive, detailed structures.
SOAP Notes aren’t the only format used in mental health documentation. Mental health progress notes can range from the very basic to more comprehensive structures, like the 10-step example Therapy Notes above.
To illustrate, here are some useful free templates for practitioners to use and download.
Quenza Therapy Notes Templates
Quenza offers free evaluation, assessment, and intake document templates for e-counselors in its Expansion Library, including a range of forms that can be customized to use as therapy progress note templates. The Outcome Rating Scale, shown below, captures data on a client’s individual, interpersonal, social, and overall functioning for including in progress notes.
Therapy progress notes often include information on different areas of functioning that can change as a result of therapeutic intervention, as assessed by Quenza’s Outcome Rating Scale.These insights can help practitioners keep track of how a client is progressing with therapy and can be used to populate more detailed therapy notes that include the session’s focus, client’s name, and more. With professional therapy notes software, this is often as simple as including custom fields for additional information.
SampleTemplates
SampleTemplates also provides healthcare progress notes formats for physical therapists, pediatricians, general clinicians, and therapists.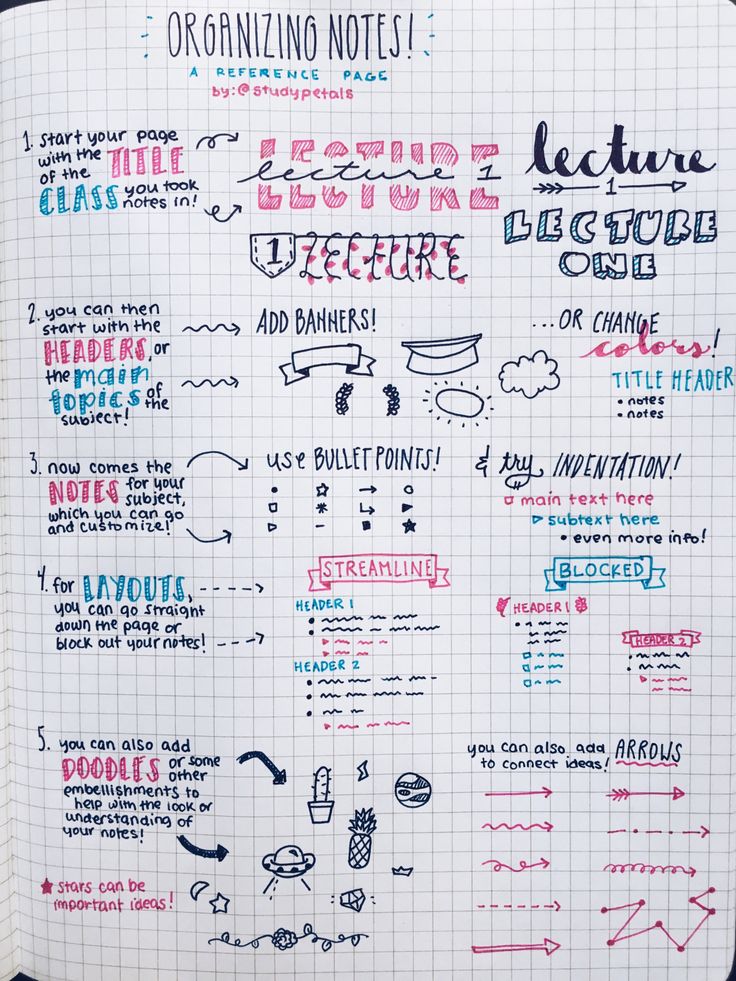
These include BIRP Note templates, SOAP Note structures, integrated progress notes and billing forms, and digital samples for electronic note-taking.
HarmResearch.org
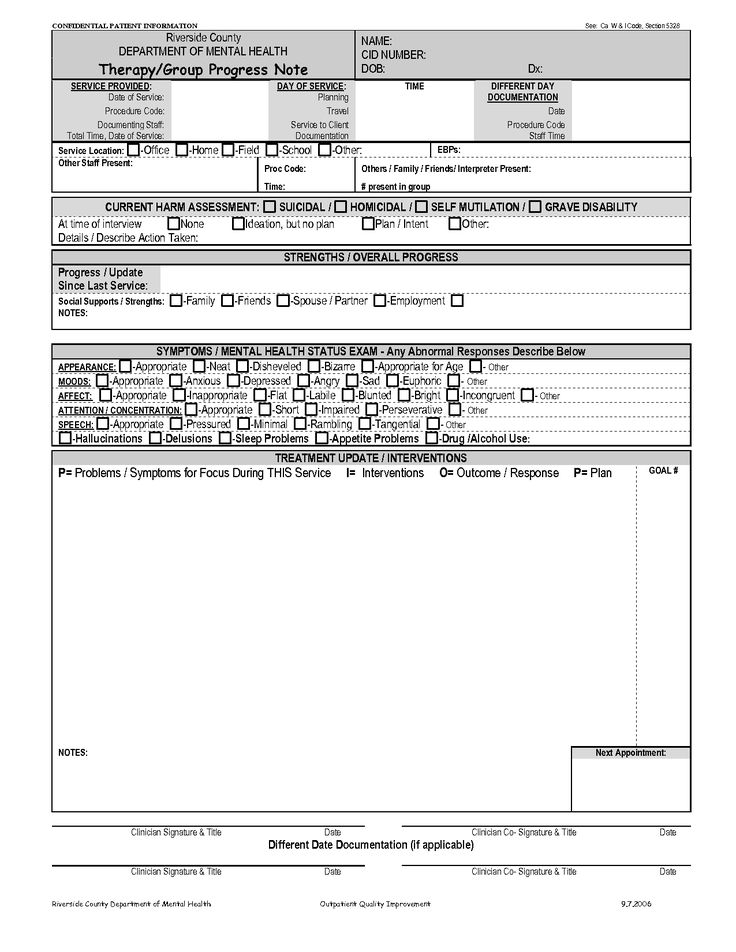
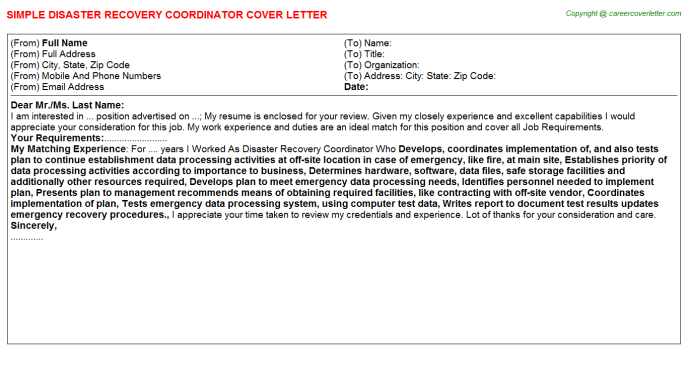
HarmResearch.org sells Psychiatric and versatile Visit Progress Note templates for professional use. Their psychiatric progress note template includes fields for:
- Patient demographics
- Presenting problem
- Past psychiatric history
- Diagnostic interview summaries
- Past medical history, and other key fields.
List of Interventions & Common Terminology
When documenting interventions and treatments as part of progress note-taking, appropriate language and abbreviations can greatly speed up the process.
Clinical terminology also ensures a common professional language exists between practitioners; it facilitates better understanding and establishes a consistent frame of reference.
In therapy for mental health, appropriate terminology can be a combination of diagnostic references, such as DSM5 or ICD-10 codes, and descriptive terms for subjective sections progress notes.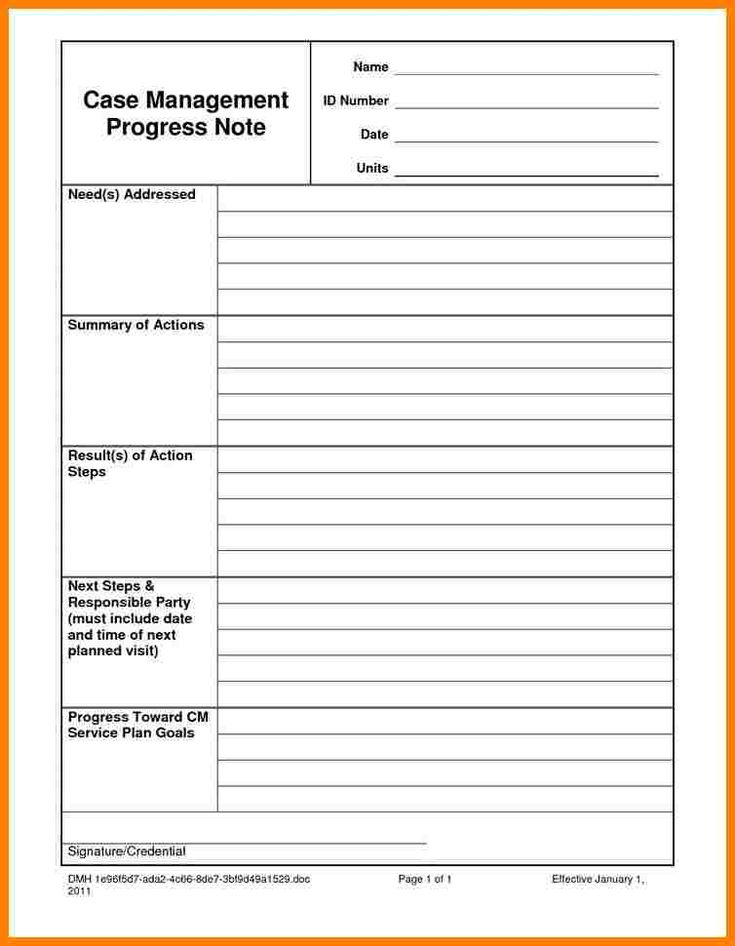
Common Terminology
The County of Santa Clara suggests a helpful Counselor’s Thesaurus in its Clinician’s Guide Toolkit. This covers commonly-used descriptors to detail different aspects of a client’s health, appearance, and more.[3]
The Thesaurus covers categories such as:
- Affect, Mood, or Disposition – e.g. Lighthearted/carefree, Depressed/Dejected/Dispirited/Disheartened, Flat/Shallow/Dull/Listless
- Attitude – such as Apathetic/Inert/Absence of Affect, Belligerent/Quarrelsome/Disagreeable
- Behavior – ideas include Over-cautious/Too Careful, Lethargic/Sluggish, or Spontaneous/Immediate
- Work Habits, Cognition, Orientation, and more.
Interventions
Having a list of frequently-used interventions on hand for quick reference can be particularly useful in multi-provider contexts, helping different practitioners understand what treatments a client is pursuing with other specialists.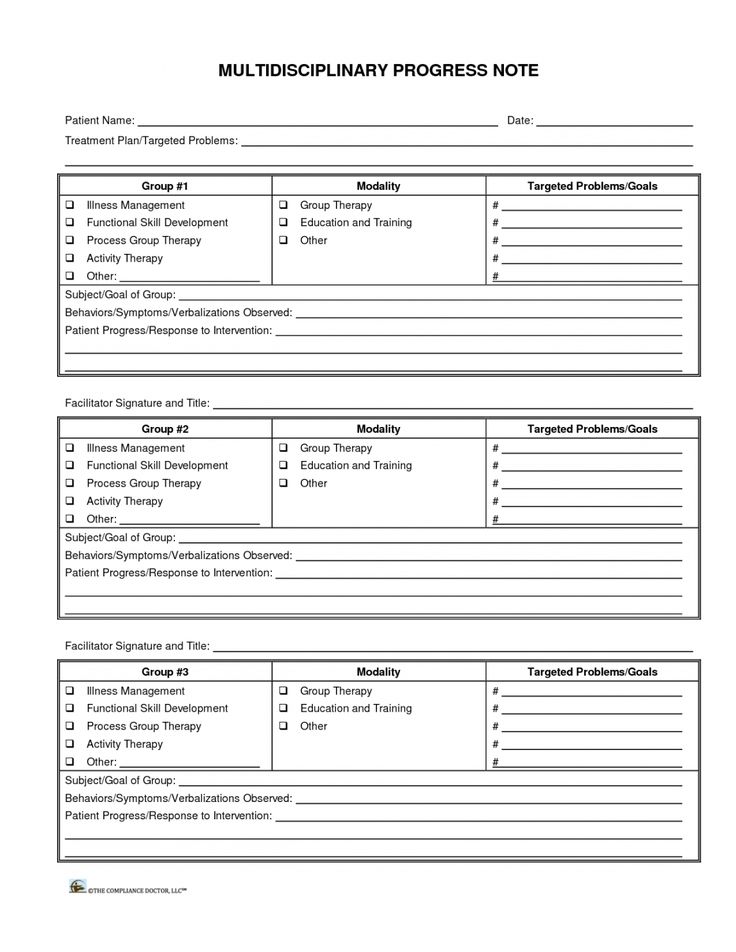
In mental health disciplines, these interventions might address:[4]
- Anger Management for healthier self-expression
- Behavior Reinforcement, commonly part of intrinsic coaching methodologies
- Collaborative Problem-solving for relationship counseling, family therapy, conflict resolution, and other
- Cognitive Restructuring – a thought-based CBT intervention
- Communication Skills Development – e.g., as part of interpersonal therapy
- Coping Strategies Development for addressing a diversity of mental health conditions
- Eye Movement Desensitization and Reprocessing (EMDR) for trauma counseling
- Progress/Objective Review, which might involve collaborative goal-setting as part of mental health coaching
- Identifying Triggers, as seen in therapy for substance abuse, or anger management
- Imagery – e.
 g., within a graded exposure treatment for anxiety
g., within a graded exposure treatment for anxiety - Mindfulness – covering Mindfulness-Based Stress Reduction (MBSR), Mindfulness-Based Cognitive Therapy (MBCT), and formal/informal Mindfulness Training
- Problem-Solving Skills Development – another versatile CBT intervention, and
- Stress Management – which can include both therapist-guided activities and lower-intensity Stepped Care interventions.
Individual & Group Therapy Notes: 3 Examples
Progress notes for individual and group therapy will differ in a few ways, as different sections may be required for distinct criteria. Their overall purpose, however, remains the same.
This means that both documentation types should include details on the particular patient or client’s progress overall, important identifiers, and relevant notes from the session that took place.
The snapshot below shows part of an Individual Progress Note created using the ICANotes software, in which behavior, content of therapy, intervention, diagnoses, and treatment plan details are included:[5]
Comparing this with an ICANotes Group Therapy Progress Note Example, we can see the latter varies only slightly with regard to structure and content.
Both individual and group therapy notes are legal documents and must be stored securely.
Another clever way to integrate subjective data into therapy progress notes is by inviting clients to contribute their own notes from sessions.
One example template in Quenza’s Expansion Library, Session Notes for Clients, offers a structured form for patients to fill out with insights, reflections, and other observations from a therapy appointment:
Quenza’s Expansion Library includes free example therapy progress note templates such as the Session Notes for Clients form.By collecting a patient’s own observations online, professionals can easily copy and paste direct quotes into their private progress notes. All data is securely stored on the one HIPAA-compliant therapy platform, and visible only to the client and their therapist.
Smart Solutions: 3 Apps and Software Systems
Whether you’re looking for a lightweight, dedicated Progress Notes software or a bigger solution, these apps and systems all come with templates for therapists and other mental health specialists.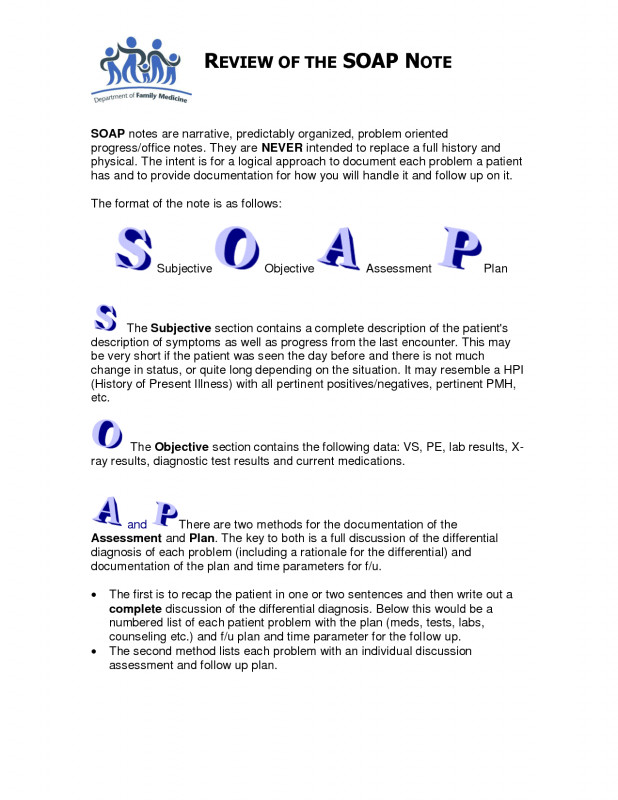
Software | Details |
|---|---|
| MyClientsPlus is a versatile mental health system for small practices and solo practitioners – it’s also relatively simple to use after an initial learning curve. With MCP’s Therapy Progress Notes capabilities, counselors and psychologists can choose between templates for psychiatry, counseling, general psychology, and more. Within different sub-sectors, you’ll find even more predesigned formats to make documentation more effective and efficient. Examples include Therapy Intake Forms, Treatment Plans, and Client Information Forms. MyClientsPlus further streamlines Progress Note creation with diagnostic codes and e-signatures and is one of the more affordable solutions on the market. | |
| Name | MyClientsPlus |
| Price | $24.95+ monthly |
| Good For | Psychologists, e-Counselors, Therapists, Mental Health Coaches |
| Website | https://www. myclientsplus.com/ myclientsplus.com/ |
Software | Details |
|---|---|
| Both mental health treatment plans and progress notes are easy to create with Quenza’s browser-based software and apps. Templates for different note types, such as SOAP notes, BIRP notes, and more can be built quickly using drag-and-drop tools, and the software stores all progress notes privately and securely on a GDPR- and HIPAA-compliant system. Forms can be shared through a private Portal on free client iPhone and Android apps, and all progress and results are shared in real-time with the therapist. Even better, Quenza comes with a huge Expansion Library of freely customizable note templates. | |
| Name | Quenza |
| Price | $1+ monthly |
| Good For | Psychologists, e-Counselors, Physical Therapy, Speech Therapy, Occupational Therapy, Mental Health Coaches, Mental Health Apps |
| Website | https://quenza. com/ com/ |
Software | Details |
|---|---|
| TherapyNotes has a library of Progress Note templates for solo practitioners and teams and comes with video therapy software for telehealth sessions. Psychotherapy Progress Notes, as shown above, can be populated using clinical codes before they are linked with a client’s appointments for easier admin and use in sessions. When a Therapy Session starts, the software automatically creates a To-Do list item reminding users to create the relevant documentation. | |
| Name | TherapyNotes |
| Price | $49+ monthly |
| Good For | Psychologists, e-Counselors, Therapists, Mental Health Coaches |
| Website | https://www.therapynotes.com/ |
Final Thoughts
From basic SOAP frameworks to detailed psychiatry notes, there’s no one way to write a great progress note. ICANotes. (2020). Sample Notes Therapy Notes. Retrieved from https://www.icanotes.com/features/charting/therapy/sample-notes/
ICANotes. (2020). Sample Notes Therapy Notes. Retrieved from https://www.icanotes.com/features/charting/therapy/sample-notes/
THIRD AND SUBSEQUENT SESSIONS . Cognitive therapy. Complete guide
Starting from the third, the sessions are held in the same format. The content varies depending on the patient's complaints, concerns and goals, as well as the goals of the therapist. In this section, we will touch on the course of therapy throughout the sessions. More information about treatment planning can be found in chapter 16.
As we have already mentioned, in the beginning the therapist takes over setting the agenda, actively assisting the patient in identifying and evaluating automatic thoughts, assigning homework and debriefing the session. Over time, responsibility gradually shifts to the patient. By the end of therapy, most of the agenda is set by the patient. He also uses tools such as the Dysfunctional Thought Worksheet (DDM) to assess his own thinking (see Chapter 9), sets a homework assignment for himself and sums up the final conclusion of the therapy session.
During the course of therapy, the focus shifts from automatic thoughts to an exploration of the patient's ingrained beliefs (see chapters 10 and 11). There are also changes in the relative emphasis of behavioral
aspects, although they are less predictable. Patients with depression should be encouraged from the start of therapy to plan their activities and lead a more active lifestyle (see Chapter 12). (Patients suffering from major depression may initially be unable to do cognitive work, so the therapist tries to increase their behavioral activity and refrains from cognitive interventions until the patient's condition improves at least to some extent.) When therapy approaches the final stage , the focus shifts to preparing the patient for the end of treatment and teaching them how to prevent relapse (see Chapter 15).
When planning an individual session, the therapist takes into account the current stage of therapy. As emphasized in chapter 2, he guides the therapy process using the patient's conceptualization.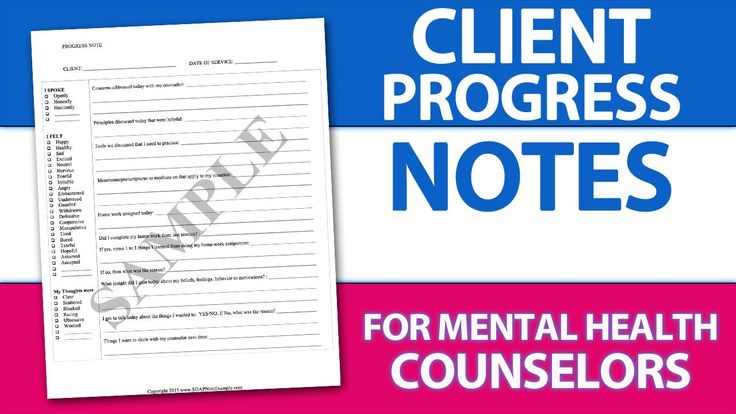 Before the session begins, the therapist enters the items on the agenda on the "Therapy Notes" form (see Figure 4.3), but is prepared to disregard them if necessary. As the client talks about his mood, how the week went, and sets out agenda items, the therapist mentally formulates a specific goal or goals for the session. For example, in the third session, the therapist's goals are to train Sally to evaluate her automatic thoughts in a structured way and to convince her to continue planning for enjoyable leisure activities. During the fourth session, the therapist discusses with the patient problems with finding a part-time job and teaches how to properly respond to negative automatic thoughts. The therapist constantly seeks to align his goals with the issues proposed by the patient as an agenda. So he teaches her problem solving and cognitive restructuring skills in the context of the situations she brings to therapy. This combination of problem solving and helping the patient respond to his thoughts usually gives both therapist and patient enough time to consider only one or two issues on the agenda for a given session.
Before the session begins, the therapist enters the items on the agenda on the "Therapy Notes" form (see Figure 4.3), but is prepared to disregard them if necessary. As the client talks about his mood, how the week went, and sets out agenda items, the therapist mentally formulates a specific goal or goals for the session. For example, in the third session, the therapist's goals are to train Sally to evaluate her automatic thoughts in a structured way and to convince her to continue planning for enjoyable leisure activities. During the fourth session, the therapist discusses with the patient problems with finding a part-time job and teaches how to properly respond to negative automatic thoughts. The therapist constantly seeks to align his goals with the issues proposed by the patient as an agenda. So he teaches her problem solving and cognitive restructuring skills in the context of the situations she brings to therapy. This combination of problem solving and helping the patient respond to his thoughts usually gives both therapist and patient enough time to consider only one or two issues on the agenda for a given session.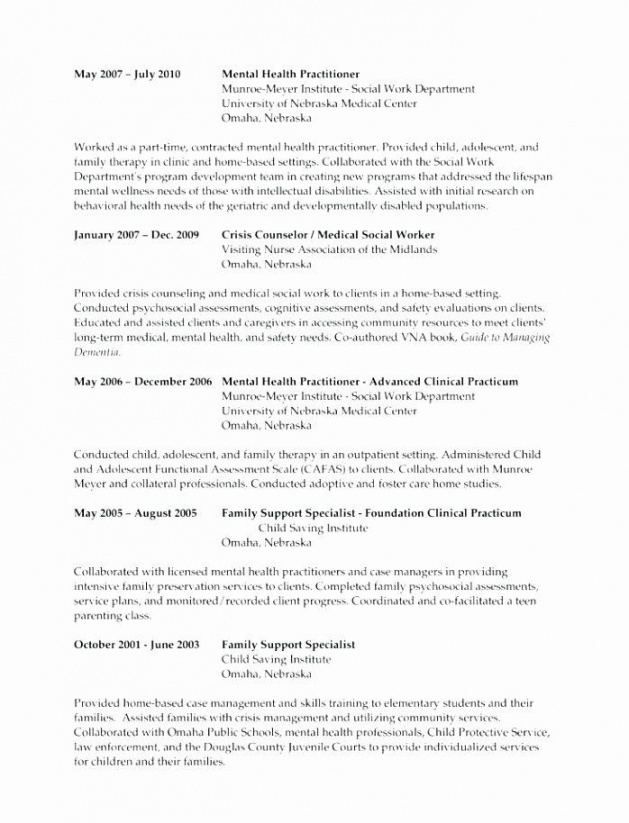
During the session, the therapist takes notes to help refine the conceptualization, keep track of the session, and plan subsequent sessions (see Figure 4.3). In addition, the therapist keeps a copy of the patient's notes. It is useful to note the issues discussed, dysfunctional thoughts and beliefs (written word for word), the degree of the patient's initial belief in them, interventions during therapy, the relative success of these interventions, new, changed thoughts and beliefs and the patient's degree of confidence in them, the content of homework and proposed agenda items for the next session. Even experienced therapists do not always manage to remember these important facts without notes.
This chapter discusses the structure and format of a typical early therapy session and briefly describes the therapy process. Next chapter
deals with the problems that arise during the structuring of sessions, and chapter 16 details the principles of treatment planning before the start of each session, between sessions, and throughout the course of therapy.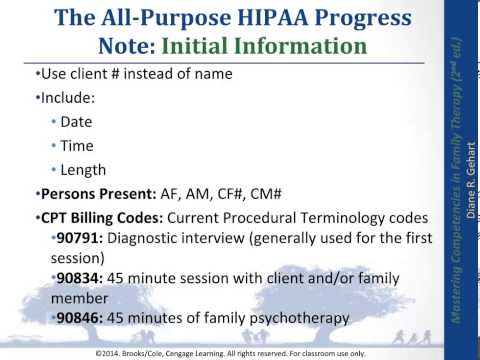
Fig. 4.3. Therapy notes
Psychotherapy is not what it seems. Why You Shouldn't Expect a Miraculous Solution to All Your Problems from a Therapist - Knife
"Say at a party: 'My therapist says...' and don't say another word for the rest of the evening. Everyone around will jump into the conversation to share what their therapist says,” writes philosophy professor Lou Marinoff ironically.
The Wall Street Journal calls Millennials (people who grew up around the turn of the century) the Therapy Generation. This, of course, is about American realities, but there is a similar trend in Russia. Even in the post-Soviet space, working with a psychotherapist is no longer perceived as a sign of a mental disorder, a manifestation of an unworthy weakness, or the indulgence of a bizarre whim. The idea that in a life crisis it is normal to turn to a psychologist becomes habitual.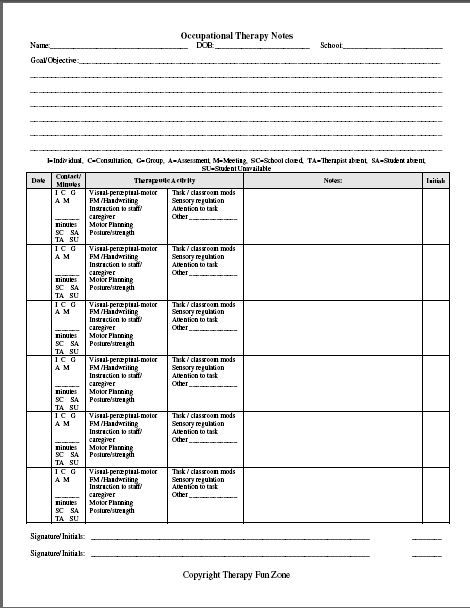
Moreover, from a crisis measure, psychotherapy is turning into a habitual, if not everyday, component of a lifestyle along with yoga, meditation, and healthy eating. Advertising texts, blogs of psychologists and books in the self-help genre create and support the image of psychological assistance as something utilitarian, practical and certainly useful: you need to brush your teeth and take a shower twice a day, but once a week you need to come to therapist's office for psychological hygiene.
At the same time, ideas about the therapist began to spread as a wise mentor or "right" parent: someone who will change the life of his client almost magically.
And don't you think that "my therapist thinks..." sounds suspiciously similar to "and our pastor says..." heard from religious friends?
If you share these fantasies about psychotherapy, chances are the reality will surprise you. Because therapy is not magic and does not involve miraculous healing.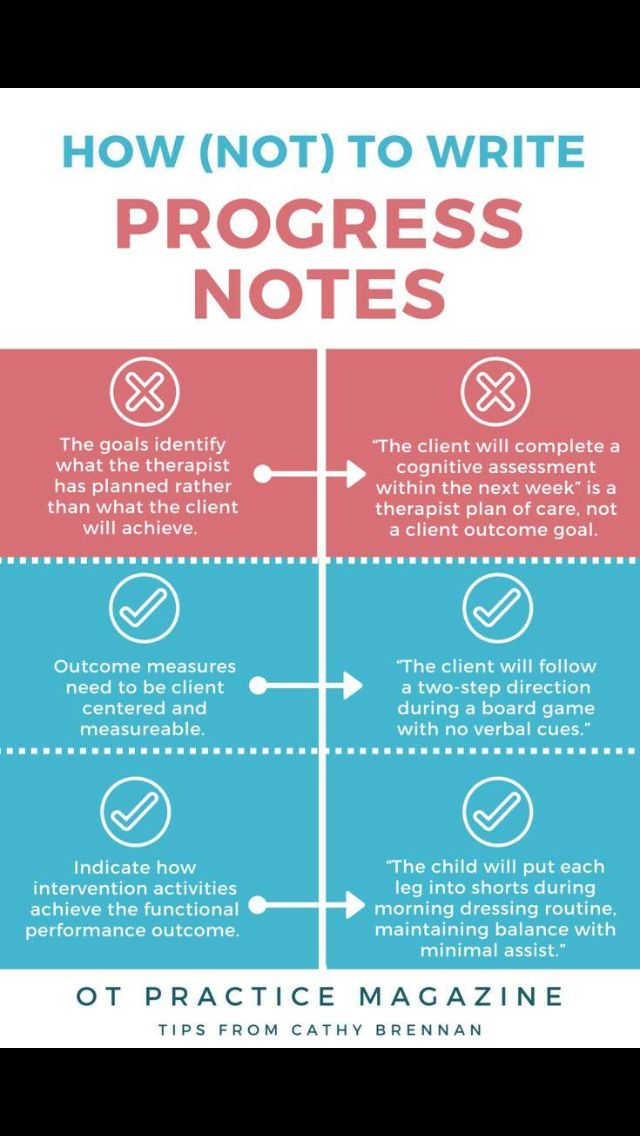 A person who idealizes therapy will very quickly begin to feel that something is “wrong” with her.
A person who idealizes therapy will very quickly begin to feel that something is “wrong” with her.
Here are six major "wrongs" you'll encounter.
1. Therapy is a relationship and it needs to be “built” too
No one comes into a new relationship from scratch – we all have expectations. The psychologist is most often endowed with expectations from the parental figure. The client unconsciously expects to meet during the session either with the ideal parent (warm, unconditionally loving and always making advances), or with one of the adults from his childhood: cold and distant; overprotective; dependent and weak or severe and punishing.
If you expect from a therapist that he will be an ideal parent for you, who will teach you everything and protect you from the evil world, then you will soon find out that in fact this is an ordinary living person who can make mistakes, not have answers to all questions, be confused and not know what to do (yes, this happens), or inadvertently hurt with a word.
 And it will be terrible.
And it will be terrible. When expectations from therapy are not met, the client may experience indignation, confusion, anger, disappointment. And doubts: maybe you need to contact another specialist? Or is therapy not mine at all?
Meanwhile, these expectations and the feelings that a person experiences in connection with them are valuable material for analysis. Instead of abandoning the process without reaping its fruits, it is better to have an open conversation with a psychologist about your feelings. Exploring the imperfection of the therapist, a person begins to treat his own mistakes, confusion, ignorance with great acceptance. It turns out that this is possible, and there is nothing wrong with that, but in order to find out, you need to go through your own feelings.
If, however, you unconsciously expect the therapist to be like the imperfect adults from your childhood, you may find that relationships in your adult life do not have to be like your experience with your parents.
For example, you can say “no” to a therapist (and then learn to do it in life outside of the office). And it's terribly scary: what if he gets angry now and kicks him out? You can share something burningly shameful and suddenly find that you won’t be scolded for it, but will look with empathy - this is also scary, will you suddenly be deceived and hurt in return? It is possible to be angry with the therapist, and he will not only bear it, but he will be able to discuss this anger, instead of demanding "stop immediately and behave."
However, it sounds easy in words, but in reality it is very difficult to share such experiences. Moreover, it can be difficult to admit to oneself that they exist, especially if they have been banned from childhood.
For example, if in childhood you were told that your anger or fear is something bad, you need to be smart and behave well, "otherwise we will give you to that uncle over there." In this case, you are likely to unconsciously avoid these feelings.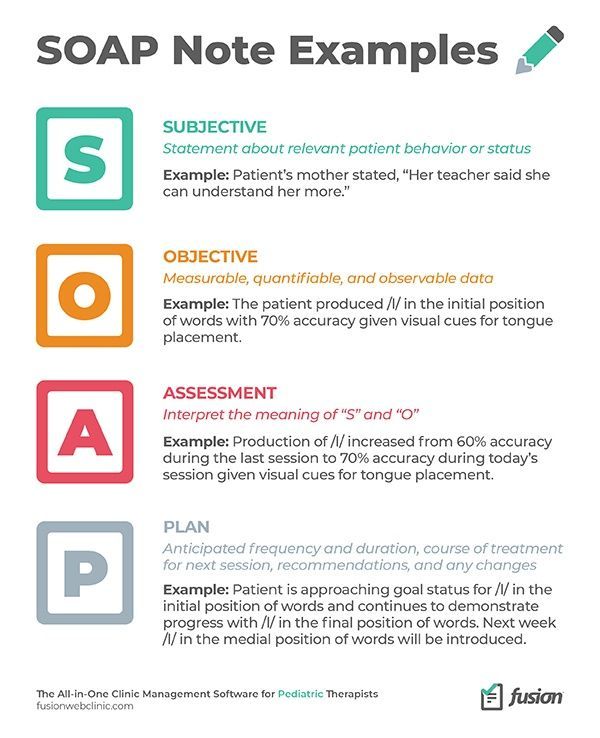 In therapy, this, again, can manifest itself in resistance: the decision to change a specialist, to quit. Or in sabotage, when a person begins to systematically skip, cancel or reschedule sessions.
In therapy, this, again, can manifest itself in resistance: the decision to change a specialist, to quit. Or in sabotage, when a person begins to systematically skip, cancel or reschedule sessions.
The solution here is the same as above: discuss the experience with the therapist (however, he himself can draw your attention to frequent omissions and offer to find out what is happening). Then you can finally acknowledge your feelings and live them.
2. Ten sessions are not enough
Perhaps the biggest disappointment in therapy is the stage that reminds of the old joke about the first grader Vovochka: he went to the line happy and with a bouquet of gladioli, and returned gloomy, indignantly asking his parents why he they did not warn that this bagpipe was for eleven years.
In 2016, the Society for the Development of Psychotherapy published statistics on client expectations. Most expect a successful solution to the problem in 9 sessions.
 However, in most cases, 9 sessions are not enough, and here's why.
However, in most cases, 9 sessions are not enough, and here's why. Usually what the client calls a "problem" and what comes to therapy with is only a symptom. Something like if a person went to the doctor about a high temperature, and the case turned out to be a viral infection. You can bring down the symptom, or you can work with the root cause.
15-20 sessions can really be enough to work with a symptom - on average, according to the American Psychological Association, it takes 50% of clients that much time to feel a significant improvement or complete cessation of a symptom. For example, a person asked about a crisis in a relationship and after several months of working with a psychologist, he became better aware of his needs and learned not only to communicate them to his partner, but also to look for different ways of satisfaction - in a word, he began to cope better.
But in order to deal with the underlying causes of one's feelings and behavior, in order to achieve sustainable changes at the system level (that is, to feel and behave differently over time), one will have to turn to previous life experience.
After all, the problem does not exist on its own, but is a piece of the puzzle from personal history, personality, as well as life circumstances and the influence of the environment. Yes, and the system took years to develop - is it possible to believe that a few weeks will be enough for restructuring?
It is not enough to understand what the problem is, do a dozen exercises and master a few techniques. And the realization of this fact is not easy. At this moment, doubts may begin: maybe the psychologist deliberately complicates everything in order to pull money longer? Or is he not so professional, someone else would have done it faster?
Here again an open conversation about doubts will help, as well as clarification of agreements: whether the therapy will be short-term and with a specific, point goal - or long-term and systemic.
3. Relatives will not like all this
One of the most frequent requests to a psychologist is: "Fix me.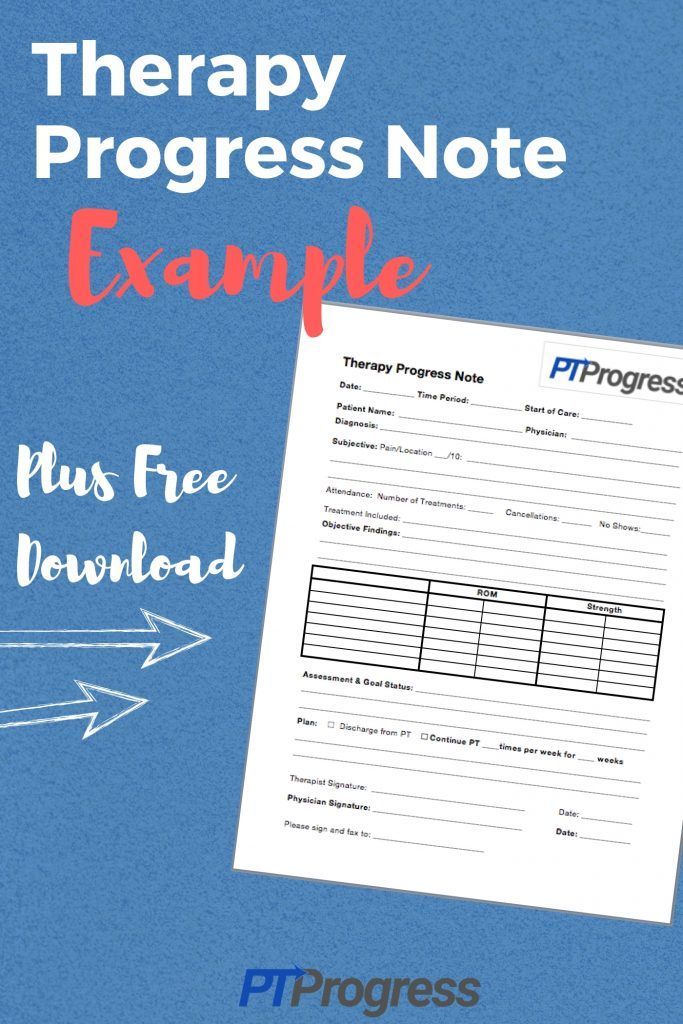 " For example, make it so that I never again get angry at my mother, boss and my child. Or for me to enjoy doing work that makes me sick. Or that I should always be full of energy and enjoy life. After all, the purpose of therapy is to change life?
" For example, make it so that I never again get angry at my mother, boss and my child. Or for me to enjoy doing work that makes me sick. Or that I should always be full of energy and enjoy life. After all, the purpose of therapy is to change life?
But it turns out that a psychologist cannot "cure" unwanted feelings or conditions. No therapist will "cut off" anger so that it is never felt again. After all, it is one of the natural feelings that tells us that something is not right. Losing it means losing a valuable signal.
But if the experience of your life has shown you that your anger is objectionable to others, scolded or punished for it, you will stubbornly consider this feeling bad, requiring expulsion. Of course, a therapist who offers to make contact with anger arouses suspicion - seriously, are you suggesting adding fuel to the fire instead of putting it out?
In therapy, you will quickly find that instead of helping you become more socially digestible, the psychologist, on the contrary, will invite you to get to know and acknowledge all your experiences and needs - even unpleasant and socially unacceptable.
If relatives are used to the fact that you are always convenient for them and try to adapt to them to the detriment of their own interests, then the designation and defense of their boundaries, as well as a change of priorities (“I am my boss”) can be perceived by them as selfishness, rudeness, and even cruelty. “Spoiled you in this therapy of yours!” and "your psychologist turned you against us!" - arguments that can be heard even from the closest people.
Then hard hard work begins. If the relationship is valuable and you want to keep it, then you have to learn how to be in it in a new way - both. Sometimes it also happens that relationships do not experience this, and parting is easy for few people.
In addition, you may find that you are generally not satisfied with your social circle and you would like other relationships built on closer values, respect for boundaries, sincere interest in each other. Old acquaintances can become uninteresting, or even burdensome, and it takes time to find new ones and establish contact.
It is worth being prepared for the fact that therapy will bring such changes - as far as it is possible to be ready for this.
4. Everything will get even worse
And it's not even about periodic rollbacks after progress, when it seems that all the work done is in vain, nothing has changed and will never change.
It happens, for example, that you have learned long and hard not to let yourself be destroyed by biased critics and have achieved success in this. But just one harsh comment on Facebook and you fall into the abyss of self-abasement. Such recessions are a natural part of the process.
Moreover, they are more likely to happen periodically for the rest of your life - for example, during periods when there is a lot of stress in life or you have few resources. At such moments, the psyche chooses the least labor-intensive - that is, habitual, well-known - reactions and behaviors. However, they will also become less intense over time (self-deprecation will stop, although the comment can still be upsetting), and it will be much easier to get out of such rollbacks.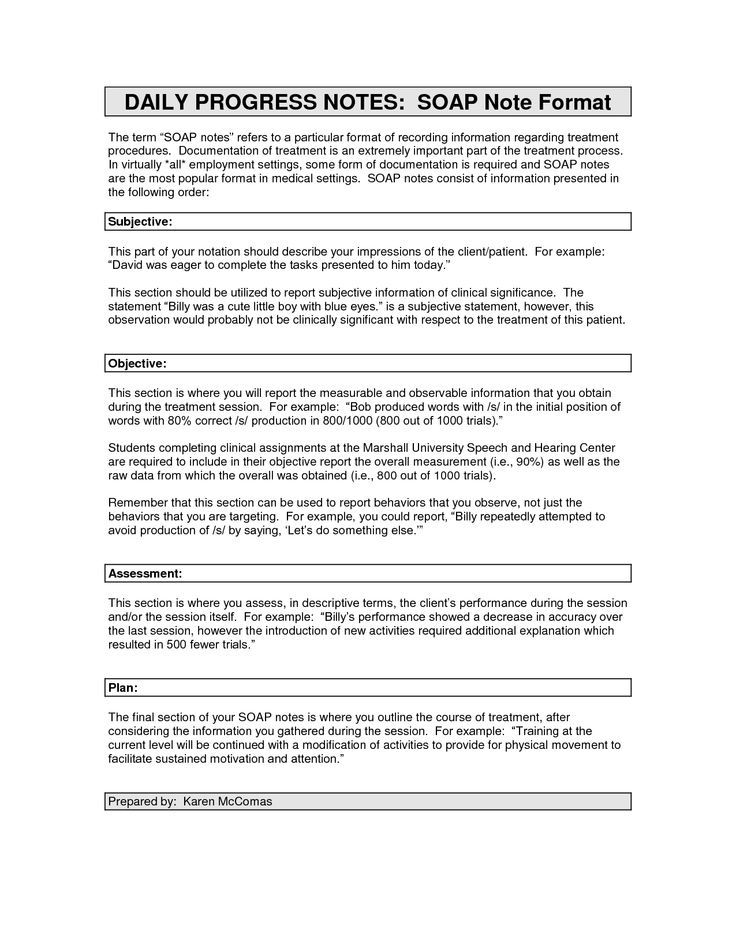
In addition to recessions, it happens differently: there seems to be progress, a lot has already been worked out, changes are taking place in life, but more and more new layers of problems are opening up, one more terrible than the other. It starts to feel like it will never end.
This happens if you had a strong traumatic experience in the past. The first months (and sometimes years) usually go to work with more accessible problems that require less vitality to solve.
In addition, as time goes by, you have more and more trust not only in the therapist, but also in yourself—that steady, supportive, independent adult that you have nurtured in yourself during therapy. This means that they are more and more ready to discover completely dark places of their inner world, securely hidden from themselves, where there was no access before.
It's hard to believe, but sometimes, when things only get worse, this is the most striking sign that you are on the right path to where you will finally feel good.
Usually you understand this after the fact, when the path through the inner hell has been passed, and the door to it is securely closed.
5. The therapist will not do your job
Research confirms that the outcome of therapy is influenced not only by therapeutic factors (approach, technique, relationship, therapist's personality, setting, etc.), but also extra-therapeutic factors, that is, that is directly related to the client: the environment and surroundings, his actions or inactions in life outside the office, personal philosophy, life circumstances and, of course, how the client handles the material from therapeutic meetings - how much he accepts, comprehends and uses it in life.
According to various researchers , the proportion of non-therapeutic factors ranges from 50% to 87%: it turns out that it is not enough to realize how and why the problem arose. To change something, you have to do something.
At least be more attentive, listen to yourself, observe and analyze your experiences, reactions, behavior. And over time, it comes to serious steps.
And over time, it comes to serious steps.
For the first time to say no to my mother after ten years of disciplined help digging potatoes on weekends instead of resting. Declare a desire for a salary increase and a new position. Confess to your partner that sex does not suit you. To change yourself and continue to live in the old environment is a very uncomfortable experience. But to create a new environment or change an old one, you have to make an effort.
And it turns out that the steps above are just the beginning. You will have to deal with the consequences: build relationships with your mother so that she respects “no” (or accept that this will not happen and choose what to do in this case), defend your right to higher pay and prove it with deeds, live through the crisis in relationship. And all this is on your own.
6. Therapy will end and it may seem boring
Can therapy last forever? Hypothetically, there will always be a problem that can be discussed in a session, or a memory from the past that you want to parse.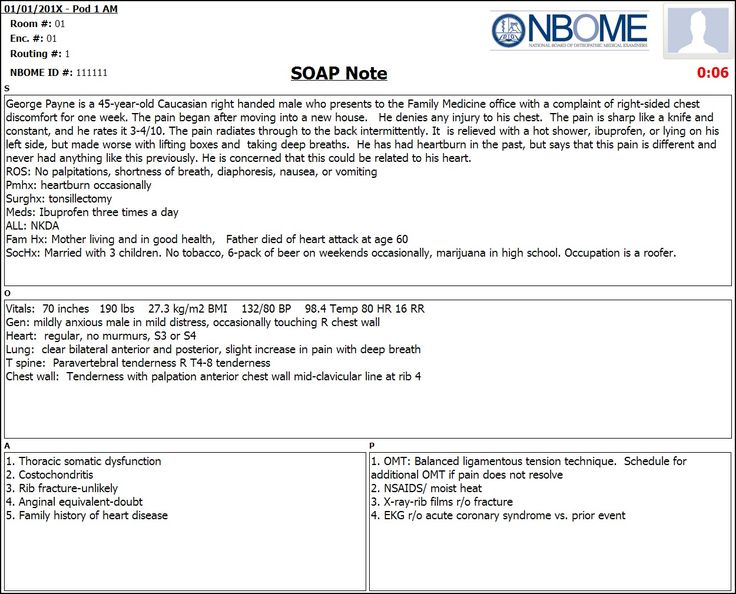 When to stop?
When to stop?
It happens that in the process of therapy, a person suddenly begins to think that now everything is fine. This happens, for example, during a period of emotional upsurge and high physical energy: I cope with everything, my mood is excellent, and all problems look quite on the shoulder. If such a state came “suddenly”, and even at the last session you spoke with the therapist that it was difficult for you to deal with some kind of life situation, you take the particular for the general.
I really want to believe that the effect of therapy has been achieved, and this will always be the case now. Unfortunately, this is an illusion.
Sustained change does not come all at once. Only with time will you begin to notice that in familiar situations you feel and behave differently. At first, these changes may be small and require some effort from you, but little by little the new state - more calm, stable - will become familiar.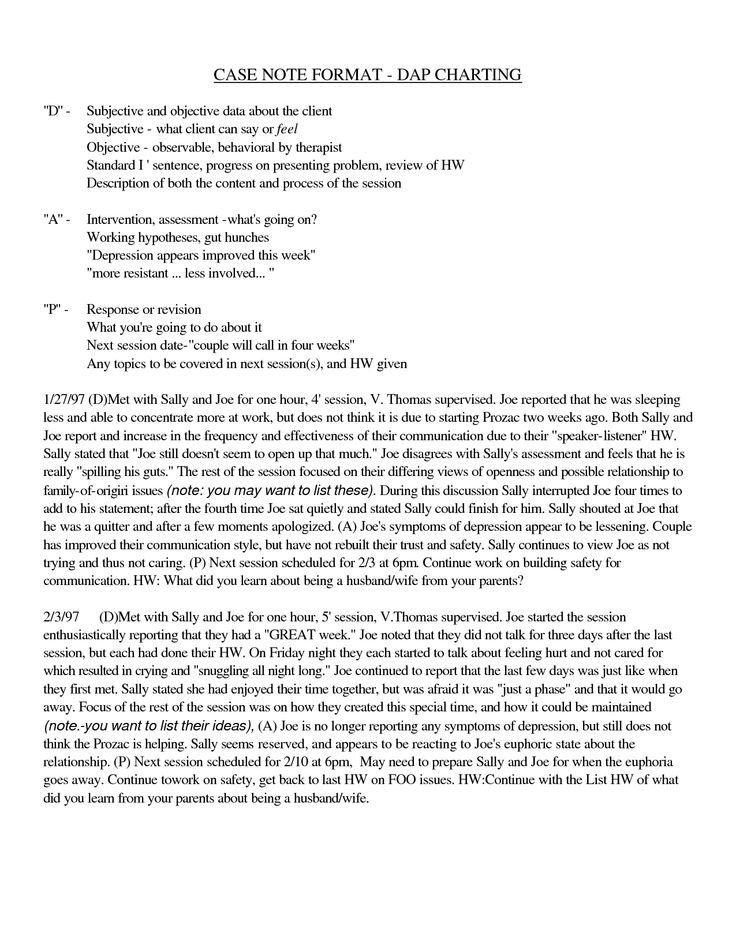 In addition, you already know from experience that you can fall out of this state under the influence of external factors - for example, in a stressful situation or during an illness. But when life gets better, peace and stability will return.
In addition, you already know from experience that you can fall out of this state under the influence of external factors - for example, in a stressful situation or during an illness. But when life gets better, peace and stability will return.
There is a famous half-joke: the therapist works to ensure that the client never comes back to him. No matter what request a person comes with, the global goal is really the same: to help him gain independence and find the “good enough” state.
Everyone will have their own such point. For some, those very 10–15 sessions are really enough, while for some, the journey takes several years.
The only way to know when to stop is to learn to listen and trust yourself. And in the process, discuss the course of therapy with a psychologist, talk about progress, goals, deadlines - remembering that goals and deadlines can change along the way.
Authentic and sustainable “good enough” can be boring on the outside. When life brings enough joy (although sometimes, of course, it upsets), the environment is quite harmonious (although sometimes there are conflicts and misunderstandings), and in general, a person copes with all life's troubles quite independently (and knows when and from whom to ask for help, if needed).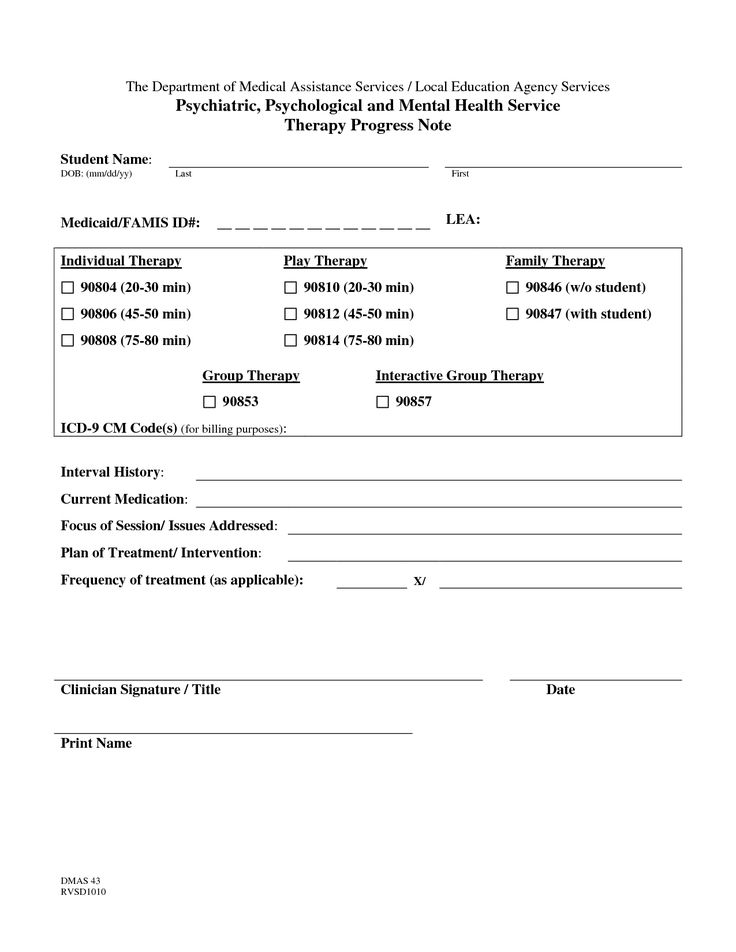
 g., Social/Case Workers, GPs.
g., Social/Case Workers, GPs.