How long does paxil stay in your system
How Long Does Paxil (Paroxetine) Stay In Your System (Urine, Blood)?
Manufactured by GlaxoSmithKline, Paxil (paroxetine) is a medication prescribed by physicians to treat major depression and other complications. Paxil is classified as a selective serotonin reuptake inhibitor (SSRI), which helps to increase the number of chemicals that stabilize mood in a person. While some people have found that Paxil is a particularly effective drug, other people have experienced a number of adverse effects including birth defects, nausea, suicidal tendencies, weight gain and other complications.
As a result, some people who take Paxil decide to go off the medication. Withdrawal from Paxil, however, can result in very serious complications. Because of this, many people inquire about how long Paxil remains in your system after stopping the medication. In response to these questions, this article will review some of the important information that you should know about withdrawing from Paxil.
Some important information that any person who takes Paxil should know includes the following details:
- Do not discontinue use of Paxil, even if you begin to feel better. If you are interested in discontinuing the medication, you should first speak with a medical professional.
- Try not to miss a dose of Paxil (paroxetine). This can result in an increased risk of relapse of the symptoms that caused you to go on the medication.
- Avoid drinking alcohol or using illegal drugs while taking Paxil (paroxetine) because this can worsen your conditions.
- There are no problems associated with long-term use of the medication, but Paxil (paroxetine) is a very powerful medication that has serious complications in withdrawal cases.
Paroxetine is prescribed for major depressive disorder, anxiety, hot flashes, panic disorder, PTSD and social phobias. Some of the medications besides Paxil that contain paroxetine include Brisdelle and Pexeva.
Paxil (paroxetine) is classified as a Schedule V drug, which means that the drug has a low addictive quality and a largely accepted medical use. Based on the amount of drug that is involved, possession of Paxil without a prescription can result in thousands of dollars of fines and a prison sentence.
Based on the amount of drug that is involved, possession of Paxil without a prescription can result in thousands of dollars of fines and a prison sentence.
To understand how long Paxil (paroxetine) will remain in your system, it is important to understand the half-life of the medication. The half-life of Paxil is documented at 21 to 24 hours, which means that 50% of the drug is eliminated from a person’s system within 21 hours after stopping the medication. For example, if you took a single dose of 10 mg of Paxil (paroxetine), in 21 hours, there would be 5 mg of medication left in your system.
After another 21 hours, this amount would further reduce to 2.5 mg. Due to this half-life, Paxil tends to stay in a person’s system for approximately five days. While Paxil is classified as one of the SSRIs with the shortest half-life, this does not mean that withdrawal from the medication is not without some potentially serious complications.
While further research is needed on the subject, SSRIs like Paxil (paroxetine) are believed to work because the medication blocks serotonin from being reabsorbed by the nerve cells from which they are released. While serotonin that is reabsorbed into the brain and nerves does not help to stabilize mood outside of the brain, these neurons are particularly effective at decreasing depression and other various conditions.
While serotonin that is reabsorbed into the brain and nerves does not help to stabilize mood outside of the brain, these neurons are particularly effective at decreasing depression and other various conditions.
Several factors influence the seriousness of side effects that a person can experience while withdrawing from Paxil (paroxetine), which include the following:
- Stopping Methods. Stopping cold turkey frequently results in more complications than gradually tapering off of the medication.
- Dosage. Paxil (paroxetine) is administered in doses of 10 mg, 20 mg, 40 mg and 60 mg. Controlled versions of the medication also come in 12.5 mg, 25 mg, 37.5 mg and other doses. The difference between controlled release and standard Paxil (paroxetine) is that in the controlled dose, the medication is released more slowly. The larger the dosage that a person takes, the more difficult it is to withdraw from the condition.
- Individual physiology.
 There are a variety of physiology factors among different people that influence the length and ease with which Paxil (paroxetine) withdrawal occurs.
There are a variety of physiology factors among different people that influence the length and ease with which Paxil (paroxetine) withdrawal occurs. - The time that a person was on Paxil (paroxetine). The amount of time that you were on Paxil plays a significant role in how your body responds to stopping the medication. Generally, discontinuing the medication if you have taken it for an extended period of time results in more serious complications.
How long Paxil (paroxetine) remains in a person’s blood has already been discussed, but there is also a risk of traces of Paxil (paroxetine) showing up in a urine test. 64% of Paxil (Paroxetine) is excreted from the body within urine primarily in the form metabolites and a smaller unchanged amount of paroxetine. As a result, there is a risk that Paxil (paroxetine) might remain in your system after use.
Read Previous
Paxil Withdrawal & Detox
Read Next
Mixing Alcohol and Paxil
Medical Disclaimer
The Recovery Village aims to improve the quality of life for people struggling with substance use or mental health disorder with fact-based content about the nature of behavioral health conditions, treatment options and their related outcomes.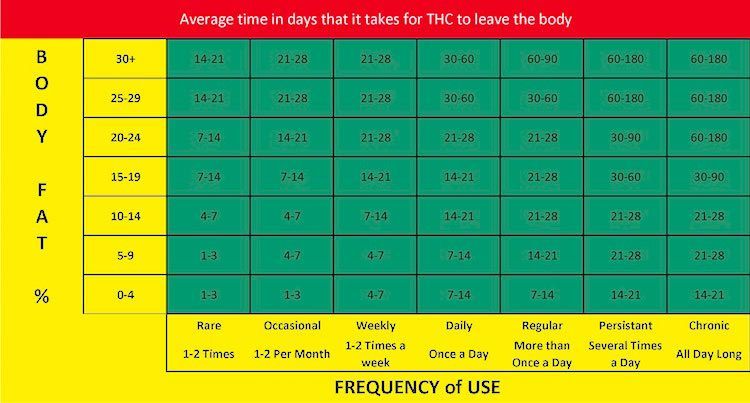 We publish material that is researched, cited, edited and reviewed by licensed medical professionals. The information we provide is not intended to be a substitute for professional medical advice, diagnosis or treatment. It should not be used in place of the advice of your physician or other qualified healthcare providers.
We publish material that is researched, cited, edited and reviewed by licensed medical professionals. The information we provide is not intended to be a substitute for professional medical advice, diagnosis or treatment. It should not be used in place of the advice of your physician or other qualified healthcare providers.
Paxil (Paroxetine) Withdrawal & Detox: Symptoms, Timeline and Treatment
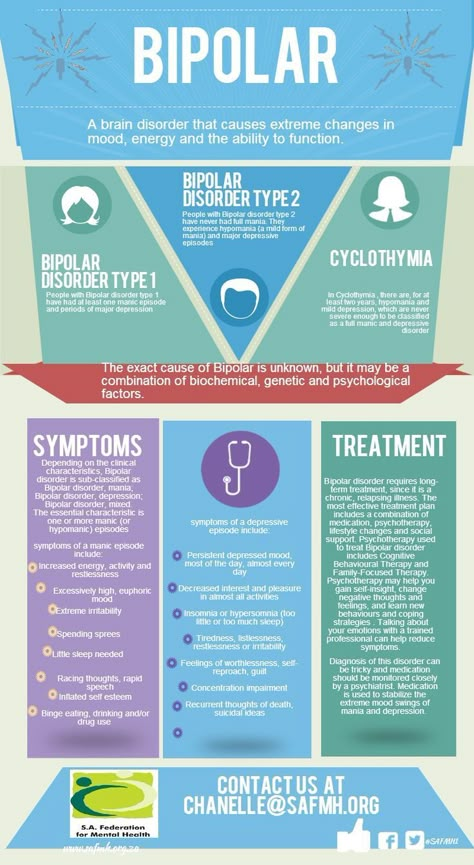
Paxil, which also goes by the generic name paroxetine, is a common type of antidepressant classified as a selective serotonin reuptake inhibitor (SSRI). It’s considered non-addictive by both the medical community and the federal government. Patients who stop taking the drug still experience withdrawal symptoms referred to as discontinuation syndrome.
Doctors routinely prescribe SSRIs like Paxil to patients in drug and alcohol recovery when they fit the criteria for major depressive disorder. Mental health disorders like depression are common among people with substance misuse issues, and they often go undiagnosed.
For recovering addicts whose depression is caused by serotonin deficiency, paroxetine can reduce withdrawal symptoms while improving overall brain chemistry.
Paroxetine inhibits the reabsorption of serotonin in the brain. In doing so, Paxil increases serotonin’s ability to improve mood and reduce symptoms of depression. For most people who take paroxetine, the drug, at some point, becomes ineffective. Getting off of an SSRI like Paxil isn’t nearly as challenging as recovering from recreational drug use. Symptoms are usually mild and are easily managed by gradually decreasing the dose.
The following are common paroxetine withdrawal symptoms: insomnia, irritability, dizziness, headache, flu-like symptoms, vertigo, nausea, confusion, anxiety, excessive dreaming and suicidal ideation. Suicidal thoughts are most common when the patient unexpectedly misses a dose or stops taking the drug without first consulting their doctor.
How long symptoms last and the severity of those symptoms are largely dependent on the unique physiology of the individual, the size and frequency of the doses being taken at the time of cessation, and the length of time that the patient has been taking the drug.
Withdrawal symptoms usually begin within the first 24-48 hours of reducing the dose. Symptoms peak in intensity at four to five days. For most people, withdrawal symptoms cease completely after two to three weeks. New research suggests that it can take as long as 90 days before the brain has fully adjusted to being off of Paxil. During this period, it’s critical for the patient and doctor to keep a close eye on fluctuations in symptoms.
Symptoms of discontinuation syndrome from Paxil are most severe when doses stop abruptly. Accidentally missing treatments can trigger the onset of withdrawals. A person who has been taking large and frequent doses of paroxetine will, on average, have more intense withdrawal symptoms than someone who’s been prescribed smaller doses.
Paxil doses range from 10 mg to 60 mg depending on the country in which the drug is administered. Patients who have been taking 50 mg doses for a year will take longer to wean off of paroxetine than someone who has been taking infrequent doses of 25 mg extended-release pills.
When doses are stopped all of a sudden, the best way to manage and reduce symptoms is to get back on the prescribed dose and then gradually decrease doses from there.
Never stop taking Paxil without first consulting your doctor and formulating a plan for getting off the drug.
Eating a low-inflammation diet and exercising can also be helpful for managing withdrawal symptoms. Long-term use of prescription medications can lead to inflammation that damages the gut lining. Eating plenty of dense leafy greens and supplementing with pharmaceutical-grade probiotics can help recolonize healthy gut bacteria and reduce symptoms of anxiety. Exercise can help normalize metabolic activities as well as reduce levels of the stress hormone cortisol.
Even gradually reducing the dose of Paxil can trigger the onset of feelings of depression, anxiety and persistent thoughts of suicide. Suicidal ideations are most common in individuals under the age of 25. If symptoms worsen, notify your doctor immediately. Fixing the problem is often as simple as temporarily increasing the dose.
Fixing the problem is often as simple as temporarily increasing the dose.
Your doctor may also try putting you on fluoxetine. Fluoxetine is an SSRI similar to paroxetine and has a shorter half-life. The shorter half-life of fluoxetine, in many cases, results in milder withdrawal symptoms.
The doctor that has been prescribing and monitoring the drug’s administration is the most well-equipped to provide support during the discontinuation phase. No one else is more aware of the patient’s history and reactions to relevant medications.
Transitioning off of Paxil can be incredibly difficult for some people and uneventful for others. Regularly sharing how you’re feeling with the people closest to you is also essential. Those who know you well will be the first to notice concerning changes in behavior so that symptoms can be managed early.
Read Previous
Paxil Signs, Symptoms & Side Effects
Read Next
How Long Does Paxil Stay In Your System?
Medical Disclaimer
The Recovery Village aims to improve the quality of life for people struggling with substance use or mental health disorder with fact-based content about the nature of behavioral health conditions, treatment options and their related outcomes. We publish material that is researched, cited, edited and reviewed by licensed medical professionals. The information we provide is not intended to be a substitute for professional medical advice, diagnosis or treatment. It should not be used in place of the advice of your physician or other qualified healthcare providers.
We publish material that is researched, cited, edited and reviewed by licensed medical professionals. The information we provide is not intended to be a substitute for professional medical advice, diagnosis or treatment. It should not be used in place of the advice of your physician or other qualified healthcare providers.
Antidepressants in gastroenterology practice uMEDp
Antidepressants are widely used in modern gastroenterology. The article discusses the indications for prescribing antidepressants to patients with digestive disorders, discusses the features of antidepressant therapy in gastroenterological patients with comorbid pathology of the cardiovascular system. The main groups of antidepressants - selective serotonin reuptake inhibitors and tricyclic antidepressants - were compared in terms of their therapeutic effects and potential side effects.
Pharmacological effects and clinical manifestations of potential side effects of TCAs
Antidepressants are an extensive group of drugs, the mechanism of action of which (with rare exceptions) is determined by a direct effect on the metabolism of neurotransmitters, primarily serotonin, as well as norepinephrine, and less often dopamine [1].
The main therapeutic effect of antidepressants is achieved due to their ability to influence pathologically reduced mood - depression. In this regard, the main indication for prescribing antidepressants are depressive states, which in somatic medicine (including in the practice of a gastroenterologist) include primarily endoform and somatogenic depressions pathogenetically associated with a somatic disease, as well as depressive reactions to the situation of the disease [2 ].
In gastroenterological practice, the anti-anxiety effect is of no less importance. The drugs of this group can be used as a monotherapy for an anxiety disorder or combined with gastroenterological agents in cases where disorders in the digestive system are somatic manifestations of an anxiety or somatoform disorder.
An indication for the appointment of antidepressants may be the relief of symptoms of the overlap of chronic diseases of the digestive system and depression, manifested by a variety of algic syndromes. For example, they include bulimia nervosa and anorexia, which often provoke a malfunction in the digestive organs.
For example, they include bulimia nervosa and anorexia, which often provoke a malfunction in the digestive organs.
Since the middle of the last century, many antidepressants with different mechanisms of action have been synthesized, and their number continues to grow. The main criteria for choosing an antidepressant, along with therapeutic efficacy, are safety, good tolerability, the absence of severe side effects, and a minimal risk of unwanted interactions with somatotropic drugs [3].
Currently, antidepressants are divided into three groups [1].
First-generation antidepressants include tricyclic antidepressants (TCAs) - amitriptyline, imipramine, pipofezin; as well as irreversible non-selective monoamine oxidase inhibitors - pirlindol. The drugs of this group have a powerful and undifferentiated effect on multiple receptor systems of the body. This mechanism of action causes a high probability of side effects of antidepressants of this group.
Second-generation drugs are selective serotonin reuptake inhibitors (SSRIs) - fluoxetine, fluvoxamine, sertraline, citalopram, as well as selective serotonin and norepinephrine reuptake inhibitors (SNRIs) - duloxetine.
Next-generation drugs include drugs with other and (or) mixed mechanisms of action, which are currently used by gastroenterologists relatively rarely.
Thus, in somatic practice, the use of second-generation drugs is preferable [3–5].
Use of SSRIs
SSRI drugs meet all of the above selection criteria.
The ratio of the severity of various effects (actually antidepressant, stimulant, anti-anxiety, sedative, anticholinergic) differs in different drugs of the group. The most important is the degree of stimulant and anti-anxiety effects, which serves to divide SSRIs [6, 7] into drugs with a predominantly stimulant effect (fluoxetine, paroxetine), drugs with a predominantly anti-anxiety effect (fluvoxamine) and drugs with a balanced effect (sertraline, citalopram).
This difference is important when determining the indications for choosing one or another drug depending on the clinical features of depression in a particular patient. In addition, drugs with a pronounced stimulating effect at the beginning of treatment cause increased anxiety, therefore, in the first two (sometimes four) weeks of treatment, it is necessary to prescribe anxiolytic drugs to prevent this undesirable effect.
In addition, drugs with a pronounced stimulating effect at the beginning of treatment cause increased anxiety, therefore, in the first two (sometimes four) weeks of treatment, it is necessary to prescribe anxiolytic drugs to prevent this undesirable effect.
Further, when describing drugs of the SSRI group [8], their international names are indicated, and in brackets are the most common trade names.
Fluoxetine (Prozac) is the most powerful of the stimulant drugs, so anxiolytics must be added in the first two to four weeks of treatment. The intrinsic anti-anxiety effect of fluoxetine is relatively weak and begins to appear no earlier than two weeks later. Due to the effect on appetite in the direction of reducing it, fluoxetine helps to reduce body weight, which is the purpose of its appointment in bulimia and obesity. The advantages in gastroenterological practice include the absence of nausea and constipation, the disadvantages are the lengthening of the time to reach orgasm (in about 40% of patients).
Paroxetine (Paxil, Reksetin) has a strong stimulating effect, as a result of which it can significantly increase anxiety at the beginning of therapy. In addition, this drug has the strongest effect on mood, up to its pathological increase. For this reason, gastroenterologists are not recommended to prescribe paroxetine without joint observation of the patient with a psychiatrist.
Fluvoxamine (Fevarin) differs from all drugs in the group by the strongest sedative effect with the weakest stimulating effect. In this regard, it is considered the drug of choice for anxious depression or in cases of prescribing an antidepressant for anxiety disorder. At the same time, it is used as monotherapy without additional enhancement of anxiolytic therapy. The advantages include a minimal negative effect on sexual function in comparison with other drugs in this group.
Sertraline (Zoloft, Stimuloton, Asentra) is one of the most widely used antidepressants in the world. Along with a pronounced antidepressant effect, the drug has an anxiolytic and mild stimulating effect. It is well tolerated and therefore can be used in elderly patients without dose reduction. Relatively rarely affects the decrease in libido (
Along with a pronounced antidepressant effect, the drug has an anxiolytic and mild stimulating effect. It is well tolerated and therefore can be used in elderly patients without dose reduction. Relatively rarely affects the decrease in libido (
Citalopram (Cipramil, Siozam, PRAM) and Escitalopram (Cipralex, Elycea, Selectra) are the weakest drugs of the SSRI group in terms of the strength of the antidepressant effect. The positive aspects in this case are the best tolerability, safety when used with somatotropic agents, and the absence of cardiotoxicity. These drugs are recommended in the treatment of depression in somatic patients, as they are characterized by a balanced effect and rarely increase anxiety.
Based on the foregoing, a differentiated approach to prescribing an antidepressant is as follows:
- fluvoxamine is the drug of choice for anxious depression, as it has the most pronounced anti-anxiety effect;
- with the predominance of apathy and asthenia in the clinical picture, it is advisable to prescribe fluoxetine, since its stimulating effect manifests itself literally from the first days of administration;
- in anxiety-depressive disorder, antidepressants with a balanced effect should be recommended;
- in algic syndrome, the drug from the SNRI group duloxetine (Cymbalta) is more effective (compared to SSRIs).
When choosing a drug for antidepressant therapy in gastroenterological practice, in addition to the generally accepted ones, the following clarifications should be made:
- Nausea is a fairly common early side effect of SSRIs. The patient should be warned about this, adding that most often this symptom is mild and transient. Otherwise, the patient may assume an exacerbation of his gastroenterological disease and refuse to take the antidepressant. A much more rare manifestation of side effects may be vomiting;
- Nausea is most severe during treatment with fluvoxamine. If this symptom is present as a sign of an exacerbation of a gastroenterological disease, it is better to initially choose a different antidepressant;
- Many SSRIs aggravate constipation. In the presence of persistent constipation, fluoxetine is the drug of choice;
- Long-term side effects of antidepressants that are important for gastroenterological practice include dry mouth.
 When conducting antidepressant therapy, it is necessary to control the intensity of this symptom. Since dry mouth is a manifestation of the excessive anticholinergic effect of the antidepressant, if this symptom is significant, it is necessary to reduce the dose of the antidepressant if possible;
When conducting antidepressant therapy, it is necessary to control the intensity of this symptom. Since dry mouth is a manifestation of the excessive anticholinergic effect of the antidepressant, if this symptom is significant, it is necessary to reduce the dose of the antidepressant if possible; - used in patients with chronic liver diseases, the hepatoprotector ademetionine (Heptral) has an antidepressant effect, but the strength of this effect is insignificant.
Before starting treatment with SSRIs, the patient must be explained the advisability of prescribing an antidepressant, possible side effects and the duration of treatment. When prescribing a drug with a stimulating effect, it is necessary to justify the need for additional prescription of a drug with an anxiolytic effect. In addition, it is worth emphasizing that the expected effect occurs no earlier than after four to six weeks of taking the drug at a therapeutic dose. Without knowing about this feature, the patient may stop taking the antidepressant without waiting for a therapeutic response.
Antidepressant therapy with SSRIs includes three stages [3, 8].
The first stage is the selection of a therapeutic dose. The first dose of the drug is 1/4 or 1/2 of a single dose, followed by a gradual increase depending on tolerance. Individual sensitivity to the drug may play a role, but it is difficult to predict before the start of therapy.
Therapy is considered ineffective if a clear improvement does not occur after four to six weeks of taking a sufficient dose of the drug. In this case, the question arises of replacing the drug. In most cases, by the 10-12th week of treatment, the symptoms of depression completely disappear. As practice shows, some patients perceive this as a cure, which is the reason for self-cessation of the drug.
At the second stage, maintenance therapy is carried out. Numerous clinical observations indicate that the interruption of antidepressant therapy immediately after improvement in well-being in 80–90% of cases leads to a relapse of the disease. Contrary to popular belief, antidepressants are not associated with the risk of drug dependence, so the treatment of depression and panic disorder should be long enough. The course of maintenance therapy should be carried out for at least six to nine months. It is quite obvious that the patient will comply with these recommendations only if the drug is well tolerated.
Contrary to popular belief, antidepressants are not associated with the risk of drug dependence, so the treatment of depression and panic disorder should be long enough. The course of maintenance therapy should be carried out for at least six to nine months. It is quite obvious that the patient will comply with these recommendations only if the drug is well tolerated.
The third stage is to cancel the drug. The general rule is the gradual withdrawal of any drug. It is recommended to first take a half dose for a month, then a half dose every other day. If symptoms of depression return, treatment should be continued.
Application of TCA
The therapeutic effect of TCAs is manifested by powerful antidepressant and anti-anxiety effects. In addition, their advantage is a strong analgesic effect, which is more pronounced in comparison with SSRIs [3, 8].
It is very important to emphasize the interaction of TCAs with various receptor structures and, as a result, the development of multiple effects (anticholinergic, adrenolytic, adrenomimetic). With significant severity, these effects are manifested by side effects of TCAs [3, 4]. The table presents the clinical manifestations of potential side effects of TCAs in comparison with the spectrum of their pharmacological effects.
With significant severity, these effects are manifested by side effects of TCAs [3, 4]. The table presents the clinical manifestations of potential side effects of TCAs in comparison with the spectrum of their pharmacological effects.
The indicated side effects are most likely in the presence of comorbid somatic pathology, and therefore it is not recommended to prescribe TCAs to elderly and senile patients [3].
In young patients with moderate or moderate depression without comorbidities, TCAs still remain an important component of therapy. At the same time, it is necessary to remember such contraindications to the appointment of TCAs as glaucoma, heart rhythm disturbance, atrioventricular blockade, convulsive syndrome.
Amitriptyline (Triptizol) has received the greatest distribution in gastroenterology and is widely used in small doses. At the same time, it should be borne in mind that doses of 50 mg or less do not have an antidepressant effect, but only cause a sedative, anti-anxiety and hypnotic effect.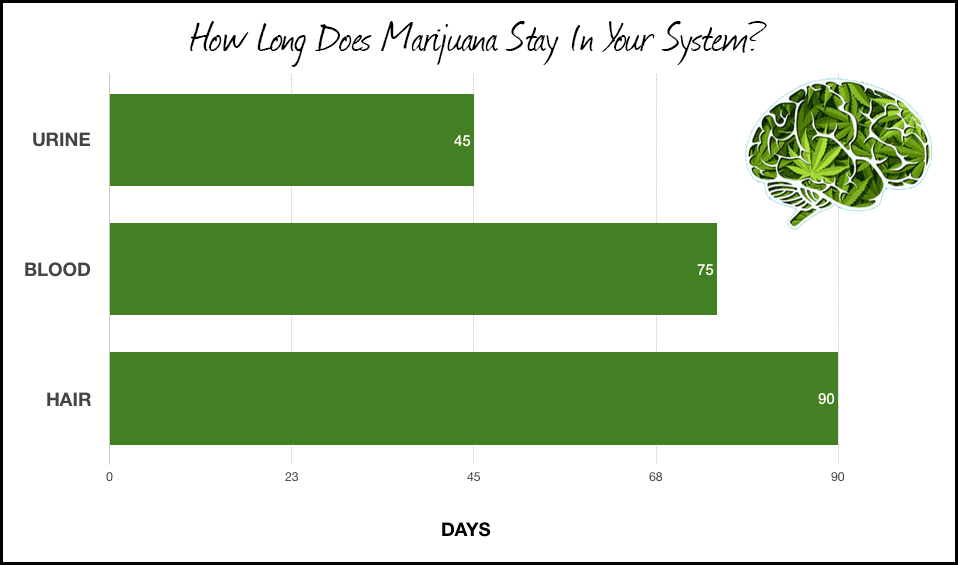 The initial dose is 12.5 mg an hour before bedtime with a gradual increase depending on tolerance.
The initial dose is 12.5 mg an hour before bedtime with a gradual increase depending on tolerance.
The antidepressant effect is achieved in a daily dose of at least 100 mg, which is poorly tolerated by somatic patients due to the above effects. In this regard, increasing the dose is possible only when observed together with a psychiatrist.
A useful property is the analgesic effect, which is more pronounced than that of SSRIs.
Side effects are associated with its anticholinergic (dry mucous membranes, constipation, urinary retention, tachycardia, disturbance of accommodation) and antihistamine (drowsiness, sedation) effects.
Pipofezin (Azaphen) is practically not used in psychiatry due to the weakness of the antidepressant effect. Indications for use are limited to shallow depressive disorders of the neurotic level. Anticholinergic side effects and cardiotoxicity are almost absent. It can be used in elderly, somatically debilitated patients, including in outpatient practice.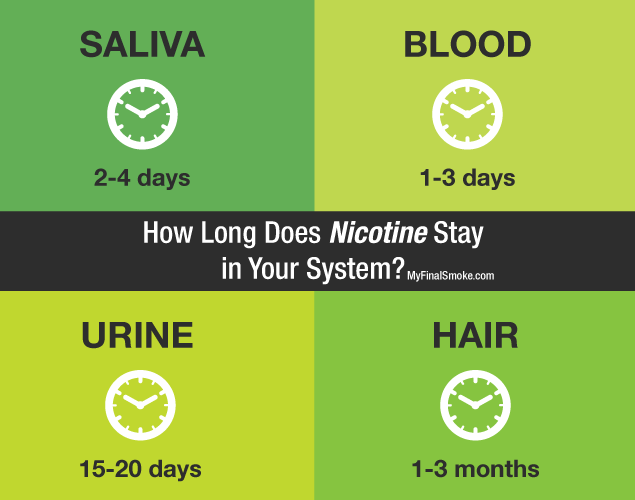 The recommended dose is 75 mg per day divided into three doses.
The recommended dose is 75 mg per day divided into three doses.
The effectiveness of TCA treatment can be assessed no earlier than three to four weeks after the start of therapy.
When prescribing antidepressants to patients with chronic diseases of the digestive system, it is necessary to take into account comorbidity, primarily with diseases of the cardiovascular system.
Based on the likelihood and severity of possible side effects, three groups of antidepressants are distinguished depending on the degree of their cardiotoxicity [9]. In patients with comorbidity of gastroenterological and cardiac diseases, the use of drugs with a low degree of cardiotoxic risk is recommended. This group includes SSRIs (fluoxetine, sertraline, citalopram, fluvoxamine, paroxetine), from drugs of other groups - pirlindol, tianeptine, mirtazapine, mianserin, trazodone.
The average cardiotoxic risk includes the use of low doses of TCAs, which can cause side effects from the cardiovascular system (orthostatic hypotension, sinus tachycardia, rhythm and conduction disturbances, depression of contractility and a decrease in heart rate variability). When using them, it is necessary to take into account the possibility of worsening the somatic condition of the patient. Treatment with these drugs, if indicated, should be carried out in conjunction with a psychiatrist.
When using them, it is necessary to take into account the possibility of worsening the somatic condition of the patient. Treatment with these drugs, if indicated, should be carried out in conjunction with a psychiatrist.
Drugs with a high cardiotoxic risk (which, in particular, include TCAs in medium and high doses) should not be used to treat patients with cardiovascular diseases.
Conclusion
Without a doubt, antidepressants have a wide range of indications for the appointment of gastroenterological patients. The drugs of choice are SSRIs, which have high efficacy, better tolerance compared to TCAs, and a convenient dosing regimen in the form of a single dose of the drug per day. The effect of treatment with antidepressants increases significantly with simultaneous individual psychotherapy.
Awareness in the issues of antidepressant therapy significantly increases the level of professionalism of a gastroenterologist.
Antidepressants, facts, withdrawal syndrome.
 All you need to know
All you need to know This topic has already been covered in our blog earlier, but indirectly, then we wrote about depression in general. In this article, we want to analyze for our beloved readers the topic of antidepressants in more detail, because the topic of methods of dealing with depression in modern society is becoming more and more relevant every day.
So, what is hidden under the word antidepressant? Do people need them? Do they harm or benefit? Now we will deal with this issue.
Antidepressants drugs containing substances that affect the functioning of the central nervous system (CNS) are used to treat depression.
How do antidepressants work? Acting on the central nervous system, they remove such unpleasant symptoms as: longing, anxiety, apathy, anxiety, insomnia, irritability, improve mental and physical activity, sleep and appetite.
How do antidepressants work? Antidepressants are not a magic pill that works with lightning speed. They work gently and gradually, ie. have a cumulative effect. The action of antidepressants is to properly balance the work of the so-called neurotransmitter hormones, namely, to block their decay or capture by neurons in time, after which these hormones increase in the central nervous system and the signs of depression begin to gradually fade away.
have a cumulative effect. The action of antidepressants is to properly balance the work of the so-called neurotransmitter hormones, namely, to block their decay or capture by neurons in time, after which these hormones increase in the central nervous system and the signs of depression begin to gradually fade away.
According to research, there are 2 sides of the coin when taking any neurodrugs. The unpleasant side of antidepressants is the so-called withdrawal syndrome, which every patient who is prescribed antidepressants should be aware of in advance.
The most important thing that every person who takes antidepressants should know and understand is that only a doctor can cancel them, under no circumstances do it yourself, this can lead to very serious consequences. An experienced psychotherapist knows how to adjust the dose of antidepressants to a particular patient. Most often, this happens very smoothly and gradually, so that the body begins to produce the necessary hormones on its own.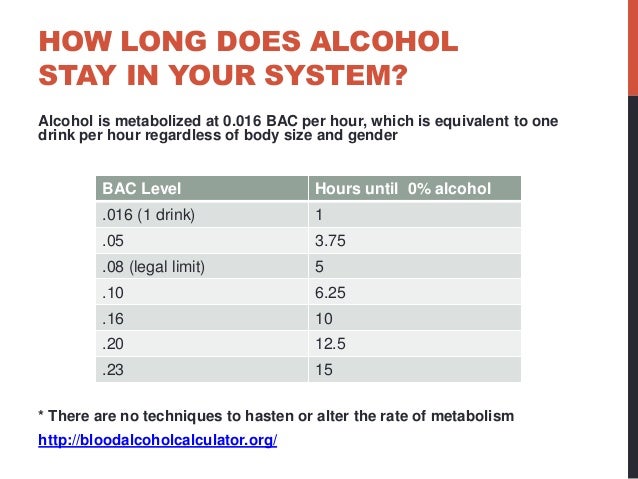
Medical Information System MC+ will help you find an experienced psychotherapist. Our system not only meets the requirements of the NSZU and the standards of the Ministry of Health, but has also been tested by many years of experience in the medical market, our doors are open to all patients, as well as to any clinics, no matter what city they are in. The MIS MS+ team is always happy to help, advise and answer any question you may have.
What awaits you? In the best case, nothing, but this rarely happens. Before describing to you the possible negative consequences during the withdrawal syndrome, we want to remind you that all this that can happen is only temporary difficulties, it is not forever, and it will just have to be endured and experienced.
Signs of withdrawal syndrome include:
— panic attacks and palpitations;
- a strong surge of emotions;
- violation of coordination of movement;
- inability to concentrate on anything, dizziness;
- lack of normal sleep and / or nightmares;
- chills;
- nausea, diarrhea/constipation;
- lack of appetite;
Once again we want to draw your attention to the fact that all this will pass, on average, the withdrawal syndrome lasts up to 2-3 weeks, but each person is different, someone may need 5 days and he will be normal, and someone that month.
Antidepressants and nervous system
Everyone knows that the human nervous system consists of a large number of nerve cells of neurons. In turn, neurons must transmit an impulse from one cell to another; this work of neurons is cyclical. The mediators in the transmission of impulses are the same neurotransmitters that we wrote about above, so if there are not enough of them in the body, the impulses pass poorly and the whole body fails. And in this case, antidepressants work just by these same neurotransmitters.
In addition, there is one more nuance. Neurotransmitters are substances of different nature, in particular, among them there are norepinephrine, serotonin and dopamine. These substances are hormones. Therefore, in addition to transmitting nerve impulses, they perform many more functions as hormones. They affect the work of individual organs and systems, the processes of contractility of muscles, blood vessels, and partly on mood and internal sensations.
Depression, is there a way out?
Doctors diagnose depression if the patient has obvious psycho-emotional disorders that affect not only the feelings, thoughts and line of everyday behavior of a person, but the whole organism as a whole. When depression is diagnosed and has a large number of negative consequences, drug treatment is recommended, that's when they start taking antidepressants. We want to draw your attention to the fact that antidepressants for depression are prescribed only after a psychotherapist diagnoses a state of moderate or severe depression, you cannot make a decision on the use of these drugs on your own.
As for whether there is a way out, the answer is unequivocal: of course there is. As long as a person is alive, no matter how hard it is for him, he always has a way out, you just need not be afraid to look for it. In the case of depression, it is very important not to be afraid to ask for help, to take antidepressants, if the situation requires it and on time, according to the scheme, start to refuse them, while remembering that each person is unique, love yourself and accept yourself, then everything will definitely work out.
Types of antidepressants
The most powerful antidepressants include three types of drugs:
- TCA tricyclic antidepressants or tricyclics;
- MAOI monoamine oxidase inhibitors;
- SSRIs selective serotonin reuptake inhibitors.
So, let's analyze these classifications of antidepressants in more detail.
The TCA group is a rather strong drug based on a triple carbon ring. The meaning of the action is to block the capture of norepinephrine, serotonin, dopamine, and also TCAs inhibit antihistamine and anticholinergic effects. Doctors usually prescribe drugs from the TCA group for the treatment of various types of depression, anxiety and panic attacks, manic-depressive states, as they have a calming effect on the patient.
Today, the TCA group belongs to the old generation of drugs and they have a lot of side effects, which often leads to patients refusing to use these drugs.
The MAOI group is a series of antidepressants whose action is aimed at increasing the concentration in the blood of substances that are responsible for good mood. MAOIs inhibit the breakdown of monoaminooxidases and increase the volume of hormones: phenylethylamine, serotonin, tryptamine, norepinephrine, dopamine, as a result of which a person’s working activity increases, he becomes more concentrated, mood improves and emotional background stabilizes.
MAOIs inhibit the breakdown of monoaminooxidases and increase the volume of hormones: phenylethylamine, serotonin, tryptamine, norepinephrine, dopamine, as a result of which a person’s working activity increases, he becomes more concentrated, mood improves and emotional background stabilizes.
Drugs from the MAOI group treat anxiety, panic attacks, various types of depression, schizophrenia, vegetovascular dystonia, and in some cases they are used to treat pathological drowsiness, to reduce weight in case of eating disorders, to treat social phobia, so they give the patient confidence in themselves, reduce stiffness, increase sociability.
MAOIs are divided into natural and synthetic antidepressants. The main three types of MAOIs: 1. Non-selective irreversible, 2. Reversible selective, 3. Irreversible selective. All of them have a stimulation effect, but you need to be extremely careful with them, because. they are addictive, similar to drugs.
SSRI group, the main principle of action of drugs in this group is that the inhibitor prevents brain tissues from absorbing serotonin, the inhibitor remains on the receptors and, as it were, prolongs the effects of joy and excitement, which leads to a good mood.
What is important, the group of these drugs is the most modern and safest, it is not addictive. They are used to treat anxiety and depression, psychosomatic pain, eating disorders, phobias, alcoholism, etc., assist in controlling the emotional and mental state.
Not only drugs can act as antidepressants, there are also natural antidepressants. First of all, these include 100% relaxation, swimming, relaxing massage, walks in the forest, for some it can be picking mushrooms, for some, visiting a spa, and for some, just snuggle up to a loved one. pet, the most important thing at the moment of relaxation is to disconnect from the hustle and bustle and all that is very annoying, to immerse yourself in your personal natural antidepressant therapy. But the most important thing is that it be useful for you and your environment, and not cause any harm to anyone!
There are also herbal antidepressants, they are also natural antidepressants, which include natural herbs and plants. Most of them are sold in pharmacies without prescriptions, but they should not be abused either, since even a decoction of ordinary mint or chamomile in unlimited quantities can harm your body.
Most of them are sold in pharmacies without prescriptions, but they should not be abused either, since even a decoction of ordinary mint or chamomile in unlimited quantities can harm your body.
Harms and benefits of antidepressants
Many people wonder what are the dangers of antidepressants? In the case of antidepressants, you should always understand that you are dealing with risks. And here it is important to always weigh whether the game is worth the candle. If a person has a very difficult psycho-emotional state, then the risk of getting side effects from antidepressants is justified, because it is more important for him to undergo treatment and bring his life back to normal. And vice versa, if a person just wants to play it safe and it seems to him that he needs medication, then he risks getting those very side effects, in which case the risk is not justified, it is better to just calm down and use herbal or natural antidepressants.
Dependence on antidepressants
How quickly antidepressants help depends not only on the dose of the drug, but also on the individual. All antidepressants have a cumulative effect, so it is very important to strictly adhere to the treatment regimen prescribed by the doctor.
All antidepressants have a cumulative effect, so it is very important to strictly adhere to the treatment regimen prescribed by the doctor.
Antidepressants are not tranquilizers, so they are not addictive or addictive as commonly believed in society, with the exception of the MAOI group, which includes some drugs that cause addiction. It is important not to confuse addiction with withdrawal syndrome, which we wrote about above, these are completely different things.
It has been proven that antidepressants are not addictive, a person taking antidepressants experiences different types of emotions just like other people. Only a qualified specialist can correctly answer the question of whether it is possible to take antidepressants all my life, because each patient is a separate special case. If the treatment regimen prescribed by your doctor involves taking antidepressants every day, you must adhere to this regimen perfectly and change it only in consultation with your doctor.
Use of antidepressants with alcohol and during pregnancy
There has been a lot of controversy around the topic of taking antidepressants during pregnancy for years. The most frequently asked question is can a pregnant woman take antidepressants and will it affect the baby? Many experts have different answers to this question, but the main thing to be guided by is the ratio of benefits for the mother / harm to the child, do not forget about the very risks that we wrote about earlier. Experts, if they recommend antidepressants to pregnant women, then only from the SSRI group, since they are the safest of all types, but the risk of harming the fetus even with them is very high, so it’s up to the pregnant woman and her doctor to decide whether or not to take them.
As far as alcohol is concerned, antidepressants are incompatible with alcohol. Combining antidepressants and alcohol, you risk not only aggravating your depression, but setting foot on the path to alcoholism.